Challenge-Based vs. Traditional Biomedical Education: Analyzing Student Learning Outcomes for Enhanced Research and Drug Development
This article provides a comprehensive analysis of challenge-based learning (CBL) versus traditional instruction in biomedical education, targeting researchers, scientists, and drug development professionals.
Challenge-Based vs. Traditional Biomedical Education: Analyzing Student Learning Outcomes for Enhanced Research and Drug Development
Abstract
This article provides a comprehensive analysis of challenge-based learning (CBL) versus traditional instruction in biomedical education, targeting researchers, scientists, and drug development professionals. It explores foundational theories, methodological applications, troubleshooting strategies, and comparative validations to assess impacts on critical thinking, problem-solving, and real-world readiness, drawing on current research and empirical evidence.
Foundations of Challenge-Based and Traditional Biomedical Learning: Theory and Evolution
Defining Challenge-Based Learning (CBL) and Traditional Pedagogical Approaches
In the evolving landscape of biomedical education, Challenge-Based Learning (CBL) has emerged as a significant pedagogical innovation, contrasting sharply with Traditional Teaching Methods. This guide provides an objective, data-driven comparison of their performance, focusing on experimental outcomes relevant to researchers, scientists, and drug development professionals.
Conceptual Frameworks and Key Distinctions
What is Challenge-Based Learning (CBL)?
CBL is an experiential, student-centered approach where learners collaborate to address complex, real-world problems. It emphasizes the development of competencies through a structured process of engaging with, investigating, and acting upon a relevant challenge [1] [2]. In biomedical contexts, this often mirrors real-life clinical or research scenarios.
What are Traditional Pedagogical Approaches?
Traditional methods, often termed Teacher-Centered Instruction, primarily rely on didactic lectures where students passively receive knowledge. Learning is typically structured around content delivery, with assessment focused on examinations that test recall and understanding of discrete facts [3] [4].
The core difference lies in the learning model: CBL prioritizes competency development and application through real-world problem-solving, while traditional methods focus on content acquisition and knowledge transfer [5] [2].
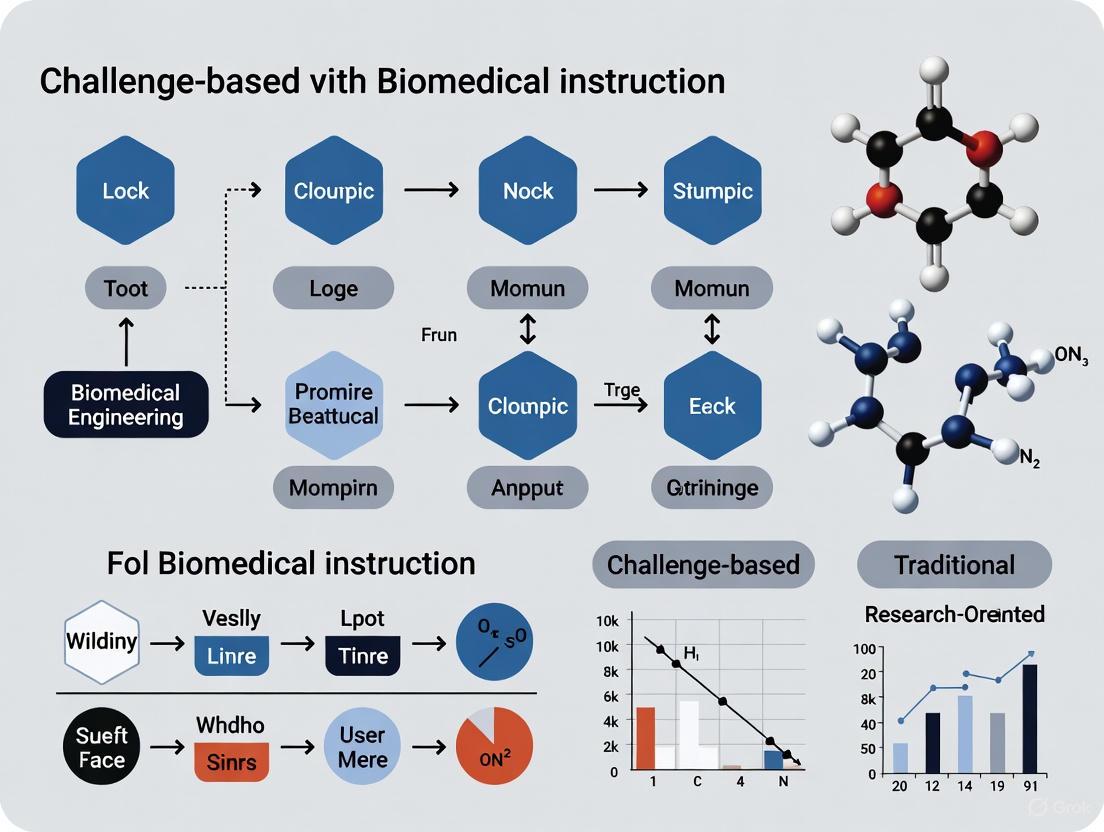
Figure 1: Comparative Workflow of Traditional versus CBL Pedagogical Approaches
Comparative Experimental Data on Educational Outcomes
Quantitative Academic Performance Metrics
The table below summarizes key experimental findings comparing CBL and traditional methods across multiple disciplines in higher education.
Table 1: Quantitative Comparison of Academic Outcomes in CBL vs. Traditional Pedagogy
| Study Focus & Population | Experimental Design | Key Outcome Measures | CBL Performance | Traditional Method Performance | Statistical Significance |
|---|---|---|---|---|---|
| Engineering Physics (1,705 students) [5] | Quasi-experimental, 7 semesters | Final course grades | Improved by 9.4% | Baseline | Significant |
| ECG Interpretation (Medical Students) [6] | Prospective interventional | Post-test scores (MCQ) | Higher scores | Lower scores | p < 0.05 |
| Retention test scores | Higher retention | Lower retention | Significant | ||
| Critical Thinking (Nursing Students) [3] | Descriptive design (n=28) | CCTST Total Mean Score | 27.39/34 | Not reported | N/A |
| Analysis sub-scale | Significant improvement | p = 0.016 | |||
| Evaluation sub-scale | Significant improvement | p = 0.007 | |||
| Oncology Postgraduates (n=80) [4] | Randomized controlled trial | Examination performance | Significantly better | Lower performance | Significant |
| Problem-solving ability | High satisfaction | Lower satisfaction | Significant |
Competency and Skill Development
Beyond academic grades, CBL demonstrates significant advantages in developing essential competencies for biomedical professionals:
Critical Thinking Skills: Nursing students exposed to CBL showed significantly improved scores in analysis (p=0.016), evaluation (p=0.007), and deductive reasoning (p=0.025) on the California Critical Thinking Skills Test [3].
Problem-Solving Ability: In medical oncology education, postgraduate students in CBL groups demonstrated significantly enhanced problem-solving capabilities compared to traditional lecture-based groups [4].
Motivational Factors: In sports science education, students in CBL conditions exhibited higher competence satisfaction and lower competence frustration compared to traditional teaching groups [7].
Detailed Experimental Protocols
Objective: To examine the impact of CBL on critical thinking in clinical decision-making among student nurses.
Population: 28 fourth-year nursing students at Kampala International University.
Intervention:
- CBL pedagogy implemented using Framework for Teaching (FFT)
- Focused on "Anemia in Pregnancy" as core clinical case
- Single 3-hour CBL session featuring:
- Progressive case disclosure mimicking real-life scenarios
- Small group work with facilitated discussion
- Teacher as facilitator with probing questions
Assessment:
- California Critical Thinking Skills Test (CCTST) questionnaire
- 34-point scale measuring analysis, evaluation, inference, deductive and inductive reasoning
- Data analyzed using percentages, descriptive statistics, and ANOVA
Key Finding: CBL produced statistically significant improvements in analysis, evaluation, and deductive reasoning sub-scales.
Objective: To measure effectiveness of CBL versus previous learning (PL) model in engineering education.
Design: Quasi-experimental study spanning seven semesters (Spring 2018 to Spring 2021).
Population: 1,705 freshman engineering students (57% in CBL, 43% in PL model).
CBL Implementation:
- Emphasis on developing disciplinary and transversal competencies
- Explicit integration of physics, math, and computing concepts
- Solution of real-life challenges through collaborative work
Assessment Metrics:
- Final exam grades
- Challenge/project report grades
- Final course grades
- Student perception surveys (n=570)
Key Finding: Overall student performance improved by 9.4% in CBL model compared to PL model.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Assessment Tools and Technologies for Educational Research
| Tool/Technology | Function | Example Use Case |
|---|---|---|
| California Critical Thinking Skills Test (CCTST) | Standardized assessment of critical thinking skills | Measuring analytical and evaluative reasoning in nursing students [3] |
| BioDigital Human/Complete Anatomy | 3D anatomy visualization software | Enhancing anatomy education in technology-enhanced CBL [8] |
| Generative AI Virtual Patient Platform | Simulated patient interactions for clinical practice | History-taking and communication skills development [8] |
| Immersive Learning Suite | Projection-based environment for simulated scenarios | Emergency medical simulation training [8] |
| Five-Point Likert Scale Feedback | Quantitative measurement of student perceptions | Comparing student satisfaction between CBL and traditional methods [6] |
| 20-O-Demethyl-AP3 | 20-O-Demethyl-AP3, CAS:23052-80-4, MF:C3H8NO5P, MW:169.07 g/mol | Chemical Reagent |
| Sc-43 | Sc-43, CAS:1400989-25-4, MF:C21H13ClF3N3O2, MW:431.8 g/mol | Chemical Reagent |
Figure 2: CBL Implementation Framework Showing Key Technological and Assessment Components
Discussion and Implications for Biomedical Education
The experimental evidence consistently demonstrates that CBL enhances critical thinking, problem-solving abilities, and knowledge retention compared to traditional methods. For biomedical researchers and drug development professionals, these findings suggest that CBL approaches may better prepare students for the complex, interdisciplinary challenges they will face in research and clinical practice.
The 9.4% improvement in academic performance observed in engineering education [5], coupled with significant gains in critical thinking skills in nursing education [3], provides compelling evidence for the efficacy of CBL in STEM and biomedical domains. Furthermore, the higher retention of complex concepts like ECG interpretation [6] indicates that CBL fosters deeper learning that persists beyond immediate assessment.
The successful integration of CBL in diverse educational contexts—from Mexican engineering programs [5] [2] to Ugandan nursing education [3] and Indian medical training [6]—suggests its applicability across institutional and cultural boundaries. This is particularly relevant for global drug development teams requiring standardized competencies across international research sites.
For implementation, the three-phase CBL framework (Engage, Investigate, Act) [1] provides a structured yet flexible approach that can be adapted to various biomedical contexts, from clinical case discussions to research methodology training. The role of the educator shifts from knowledge transmitter to facilitator, guiding students through complex problem-solving processes that mirror real-world scientific challenges.
The evolution of biomedical education demands sophisticated pedagogical approaches grounded in established learning theories. Among these, constructivism and behaviorism represent two fundamentally different perspectives on how students acquire knowledge and develop professional competencies. Behaviorism, with its focus on observable behaviors and environmental stimuli, provides a framework for mastering procedural tasks through reinforcement [9] [10]. In contrast, constructivism emphasizes active knowledge construction through experience and social interaction, positioning learners as active creators of their understanding [11] [12]. The highly interdisciplinary nature of biomedical engineering—which blends engineering principles with biological sciences and clinical practice—creates a complex educational landscape where both theoretical approaches find relevant applications [13]. This article examines the roles of these frameworks within biomedical education, with particular attention to their manifestation in challenge-based and traditional instructional models, providing researchers and drug development professionals with evidence-based insights for curricular design.
Theoretical Foundations: Core Principles and Characteristics
Behaviorism: Focusing on Observable Outcomes
Behaviorism operates on the principle that learning results in a measurable change in behavior driven by environmental stimuli rather than internal mental processes [9] [10]. This theoretical approach utilizes techniques such as reward systems, repetition, feedback, and reinforcement to shape desired behaviors through conditioning [9]. In biomedical education, behaviorism proves particularly valuable when mastering specific clinical skills or procedures where correct performance can be clearly defined and measured [9]. The teacher's role in behaviorism is central—they structure the learning environment, demonstrate desired behaviors, and provide systematic reinforcement to strengthen correct responses [9]. This approach emphasizes mastery of prerequisite steps before progressing to subsequent skills, building competency in incremental stages [9].
Constructivism: Emphasizing Active Knowledge Construction
Constructivism posits that learners actively construct knowledge and meaning through their experiences and reflections, building upon existing cognitive structures [11] [14] [12]. This theory encompasses several variants, including cognitive constructivism (focusing on individual knowledge construction) and social constructivism (emphasizing knowledge building through social interaction and collaboration) [12] [15]. The core principles of constructivism include the understanding that knowledge is personally and socially constructed rather than passively absorbed, learning is an active process requiring engagement, and motivation drives learning by connecting new information to existing understanding [12]. In constructivist classrooms, teachers act as facilitators who guide discovery and create environments where students can develop their understanding through experimentation, collaboration, and problem-solving [9] [12].
Comparative Theoretical Framework
Table 1: Fundamental Differences Between Behaviorism and Constructivism
| Aspect | Behaviorism | Constructivism |
|---|---|---|
| View of Knowledge | External truth to be acquired | Internally constructed through experience |
| Learning Process | Passive response to environmental stimuli | Active construction and discovery |
| Teacher's Role | Director who transmits knowledge | Facilitator who guides discovery |
| Student's Role | Passive recipient of information | Active creator of knowledge |
| Assessment Focus | Observable behaviors and correct responses | Understanding processes and conceptual development |
| Typical Strategies | Drill and practice, demonstration, structured feedback | Problem-based learning, collaborative projects, inquiry |
| Primary Contributors | Watson, Skinner [14] | Piaget, Vygotsky [14] [12] |
Experimental Evidence: Comparing Learning Outcomes
Research in biomedical education contexts provides empirical evidence for the applications and outcomes associated with behaviorist and constructivist approaches. These frameworks manifest differently across various instructional models, particularly when comparing traditional and challenge-based learning environments.
Behaviorism in Traditional Biomedical Instruction
Traditional biomedical education often incorporates behaviorist principles through structured skill development and direct instruction. In clinical skills courses, behaviorism proves appropriate as "correct responses in performing skills can be learnt slowly over time as students are being provided feedback, rewards and encouragement by teachers" [9]. These environments utilize checklists, rating forms, and direct observation to assess performance and provide reinforcement [9]. A qualitative study on medical classroom behavior found that the learning environment—including teacher approaches and educational content—significantly influences student behaviors and academic progress, highlighting the behaviorist concern with environmental impact on observable outcomes [10].
Constructivism in Challenge-Based Learning Environments
Challenge-based learning (CBL) represents a robust application of constructivist principles in biomedical education. CBL engages students in collaborative problem-solving of real-world challenges, requiring them to design, prototype, and test solutions [16]. This approach emphasizes purposeful learning-by-doing in contrast to passive absorption of information [16]. Implementation of CBL in a bioinstrumentation course at Tecnologico de Monterrey demonstrated that students "strongly agreed that this course challenged them to learn new concepts and develop new skills" despite the substantial time investment required from educators [16]. Another study noted that CBL provides a platform for "situated learning experience doing real things," which increases student engagement and learning effectiveness [16].
The NICE (New frontier, Integrity, Critical and creative thinking, Engagement) strategy in biomedical engineering education exemplifies constructivist principles through its case-based approach and industry engagement [13]. This strategy employs active learning methods including research article analysis using AI tools, case studies of scientific integrity, and industry-sponsored projects [13]. These constructivist approaches resulted in improved student understanding of emerging technologies, enhanced critical thinking skills, and better preparation for practical product development processes [13].
Comparative Learning Outcomes
Table 2: Learning Outcomes in Behaviorist vs. Constructivist Approaches
| Outcome Category | Behaviorist Approaches | Constructivist Approaches |
|---|---|---|
| Skill Acquisition | Mastery of prerequisite steps before moving to subsequent skills [9] | Development of integrated skill sets through project work [16] |
| Knowledge Retention | Remembering and reproducing information [11] | Deep understanding through application and connection to real-world contexts [12] |
| Critical Thinking | Following prescribed procedures and protocols [9] | Analyzing complex problems and generating novel solutions [13] |
| Professional Identity | Adopting standardized professional behaviors [10] | Developing personal understanding of professional roles through experience [15] |
| Student Engagement | Compliance with instructional requirements [9] | High intrinsic motivation through relevance and autonomy [16] [12] |
| Assessment Metrics | Observable performance against standardized criteria [9] | Diverse products and processes demonstrating understanding [16] |
Methodological Approaches: Experimental Protocols in Educational Research
Protocol for Challenge-Based Learning Implementation
The implementation of challenge-based learning in biomedical education follows a structured protocol that reflects constructivist principles. In a study conducted at Tecnologico de Monterrey, researchers implemented CBL in a third-year bioinstrumentation course with thirty-nine students divided into fourteen teams [16]. The experimental protocol included:
- Challenge Design: Students were challenged to "design, prototype, and test a respiratory or cardiac gating device for radiotherapy" in collaboration with an industry partner [16].
- Blended Learning Activities: The course combined online communication, lab experiments, and in-person CBL activities [16].
- Team-Based Approach: Student teams worked collaboratively through the entire problem-solving process, from initial research to prototype development [16].
- Assessment Method: Researchers used an institutional student opinion survey to assess the implementation success, measuring perceptions of new learning, skill development, and student-lecturer interaction [16].
This protocol resulted in positive student feedback despite increased planning and tutoring requirements, demonstrating the resource-intensive nature of constructivist approaches [16].
Protocol for Behaviorist Skill Development
Research on behaviorist approaches in medical education often follows experimental protocols focused on measurable skill acquisition:
- Structured Skill Sequencing: Complex procedures are broken down into discrete, sequential steps mastered through repetition [9].
- Immediate Feedback: Correct performance is reinforced through immediate feedback from instructors or through structured assessment tools like checklists [9].
- Environmental Manipulation: Learning environments are carefully controlled to eliminate distractions and provide optimal conditions for skill practice [10].
- Standardized Assessment: Observable behaviors are evaluated against predetermined criteria to ensure competency before progression [9].
These protocols emphasize external shaping of behavior through environmental design and systematic reinforcement, contrasting with the internal construction of knowledge emphasized in constructivist approaches.
Qualitative Research on Clinical Clerkships
A study on clinical clerkships employed qualitative methods based on social constructivism to understand the "black box" of clinical learning [15]. The research protocol included:
- Participant Selection: Eight sixth-year medical students who had completed a two-year rotation-based clerkship were selected through purposive sampling [15].
- Data Collection: Researchers conducted semi-structured, in-depth individual interviews averaging 90 minutes, supplemented by reflective journals and institutional documents [15].
- Theoretical Framework: Data analysis was guided by Lave and Wenger's situated learning theory and Wenger's social theory of learning, focusing on professional identity formation through participation and reification [15].
- Data Analysis: Interview transcripts were analyzed to identify emerging themes related to identity development and learning processes in clinical settings [15].
This approach revealed that students developed different aspects of their professional identities through negotiation of meaning in clinical environments, highlighting the complex social learning processes that constructivism helps illuminate [15].
Visualizing the Conceptual Relationships
The following diagram illustrates the key processes and relationships in constructivist and behaviorist learning approaches within biomedical education:
Constructivism and Behaviorism Learning Processes
This diagram illustrates the sequential processes in both theoretical frameworks and their integration in biomedical education. The behaviorism cycle (blue) shows the stimulus-response-reinforcement pattern leading to changed behavior, while the constructivism cycle (green) demonstrates the experiential learning process leading to constructed knowledge. Both ultimately contribute to comprehensive biomedical education (yellow).
Table 3: Key Research Reagents and Tools for Educational Experiments
| Resource/Tool | Function/Application | Example Use in Research |
|---|---|---|
| AI Literature Search Tools (e.g., ChatGPT, DeepSeek) | Assist students in literature search and concept clarification in CBL | Used in NICE strategy to help students understand cutting-edge research [13] |
| Structured Assessment Rubrics | Provide objective criteria for evaluating skill performance | Behaviorist assessment of clinical skills using checklists and rating forms [9] |
| Case Studies (positive and negative examples) | Illustrate ethical principles and professional standards | Analysis of Theranos fraud case to teach research integrity [13] |
| Industry Partnership Frameworks | Connect academic learning with real-world applications | Company-provided objectives for student design projects [13] |
| Semi-Structured Interview Protocols | Collect qualitative data on student learning experiences | Understanding clinical clerkship experiences from student perspective [15] |
| Reflective Journals/Portfolios | Document learning processes and identity formation | Tracking professional development in clinical settings [15] |
| Project-Based Learning Kits | Provide materials for prototype development and testing | Bioinstrumentation projects creating cardiac gating devices [16] |
Discussion: Implications for Biomedical Education Research
The comparative analysis of constructivism and behaviorism reveals distinct yet potentially complementary roles in biomedical education. Behaviorist approaches provide structured methodologies for mastering foundational skills and procedures essential to biomedical practice, particularly in technical and clinical domains where precision and standardization are critical [9] [10]. Constructivist approaches, particularly through challenge-based learning models, foster adaptive expertise, critical thinking, and innovation capabilities necessary for addressing novel problems in rapidly evolving biomedical fields [16] [13].
The integration of both theoretical frameworks may offer the most comprehensive approach to biomedical education. Foundational knowledge and skills can be efficiently developed through behaviorist-influenced methods, while higher-order competencies and professional identity formation benefit from constructivist approaches [11] [17]. This balanced perspective acknowledges that different learning outcomes require different instructional strategies, with behaviorism excelling in developing technical proficiency and constructivism fostering innovation and adaptive problem-solving.
Future research should explore optimal integration of these frameworks across the biomedical education continuum, from undergraduate training through professional development. Particular attention should be given to longitudinal studies comparing long-term outcomes of graduates from different instructional approaches, especially their performance in research and drug development contexts where both technical precision and creative problem-solving are essential.
Historical Context and Evolution of Instructional Methods in Biomedicine
The landscape of biomedical education has undergone significant transformation, evolving from traditional, lecture-based formats towards innovative, student-centered pedagogical models. This shift is driven by the need to prepare healthcare professionals and biomedical engineers who can navigate complex, real-world challenges and innovate in dynamic work environments [18] [19]. Among these innovative approaches, Challenge-Based Learning (CBL) has emerged as a prominent method, emphasizing the practical application of knowledge to solve authentic problems. This guide provides a objective comparison of student learning outcomes in challenge-based versus traditional instructional methods within biomedical education, supported by experimental data and detailed methodological protocols.
Historical Context of Biomedical Education
The evolution of biomedical education is marked by a continual adaptation to scientific advancement and societal needs.
- Early Foundations: Modern biomedical education traces its roots to the post-World War II era, which saw the convergence of biological experimentation and medical practice, creating the foundational "biomedical complexes" characterized by intensified life sciences research and a hunt for novel therapeutic molecules [18].
- Traditional Paradigm: For much of the twentieth century, medical education followed a two-pillar model established by the Flexner Report (1910), separating foundational basic sciences in pre-clinical years from clinical sciences training in later years [20]. This teacher-centered, lecture-based approach prioritized the transmission of established scientific knowledge.
- Shift to Integration and Competency: Recent decades have witnessed a paradigm shift towards integrated, competency-based curricula [20]. This movement aims to produce physicians and engineers "fit for the twenty-first century" by blending basic science with clinical application and emphasizing the demonstration of competencies over mere knowledge acquisition [20].
- Rise of Active Learning: This shift has facilitated the adoption of active learning strategies like CBL, which positions students as active participants in their learning journey, collaboratively developing solutions to real-world problems [21].
Comparative Analysis: Challenge-Based vs. Traditional Learning
Experimental studies directly comparing these pedagogical approaches reveal distinct patterns in learning outcomes and skill development.
Key Comparative Studies and Outcomes
The table below summarizes quantitative findings from pivotal studies comparing student performance in CBL and traditional instructional settings.
Table 1: Summary of Key Comparative Studies on CBL vs. Traditional Instruction
| Study Focus | Study Design & Participants | Knowledge Gains (Traditional vs. CBL) | Innovative Thinking & Problem-Solving | Overall Performance & Perception |
|---|---|---|---|---|
| Biomedical Engineering (Biotransport) [22] [23] | Comparative study; intervention group taught with HPL-based CBL, control with traditional lectures. | Equivalent gains between HPL (CBL) and traditional students [22] [23]. | HPL (CBL) students showed significantly greater improvement in innovative problem-solving abilities [22] [23]. | Not specified in available excerpts. |
| Engineering Education (Physics) [5] | Quasi-experimental study; 1,705 freshman engineering students over seven semesters. | Final exam grades were one measure among others. | Challenge grades in CBL were similar to project grades in the traditional model. | Final course grades improved by 9.4% in the CBL model. 71% of students had a favorable perception of CBL for competency development [5]. |
| Bioinstrumentation Course [16] | Implementation case study; 39 students in a blended CBL course. | Students reported being challenged to learn new concepts. | Students reported developing new skills through the CBL experience. | Students rated their learning experience and student-lecturer interaction positively, despite increased planning time for instructors [16]. |
Synthesis of Comparative Findings
The data indicates a consistent trend: while traditional instruction remains effective for the transfer of core disciplinary knowledge, CBL offers a significant advantage in fostering higher-order cognitive skills.
- Knowledge Acquisition: Students in CBL environments achieve equivalent knowledge gains to their peers in traditional courses, as demonstrated by pre/post-test results and final exam performance [22] [23] [5].
- Innovative Problem-Solving: CBL students consistently demonstrate superior abilities in innovative thinking and adapting knowledge to novel contexts [22] [23]. This aligns with the development of "adaptive expertise," a key goal of modern engineering and medical education [22].
- Student Engagement and Performance: Large-scale studies show that CBL can lead to improved overall academic performance, as reflected in higher final course grades, and is met with positive student perceptions regarding skill development [5].
Experimental Protocols in CBL Research
To ensure the validity and reproducibility of comparative studies, researchers adhere to structured experimental protocols.
Protocol 1: Comparative Study in a Core Biomedical Course
This protocol is modeled on the study comparing biotransport instruction [22] [23].
- Objective: To compare the efficacy of CBL (specifically, the "How People Learn" (HPL) framework) with traditional lecture-based instruction in developing subject knowledge and innovative problem-solving skills.
- Population: Undergraduate students enrolled in a core biomedical engineering course (e.g., biotransport).
- Group Allocation:
- Intervention Group: Receives instruction via the CBL/HPL method.
- Control Group: Receives instruction via traditional didactic lectures.
- Intervention (CBL/HPL Method): The learning environment is designed to be learner-centered, knowledge-centered, assessment-centered, and community-centered. Instruction is built around real-world challenges that require students to engage in a full cycle of inquiry, collaboration, and solution development [22].
- Outcome Measures:
- Knowledge Test: A standardized pre-test and post-test covering core domain knowledge.
- Innovative Problem-Solving Assessment: A pre-test and post-test featuring novel, non-routine problems to assess adaptive expertise.
- Data Analysis: Comparison of normalized learning gains on both the knowledge and innovation assessments between the intervention and control groups using appropriate statistical tests (e.g., t-tests).
Protocol 2: Quasi-Experimental Implementation at Program Level
This protocol is based on the institutional study of the Tec21 model [5].
- Objective: To assess the impact of a large-scale, competency-based CBL model on student academic performance and perceptions.
- Population: A large cohort of freshman engineering students (e.g., n=1705) over multiple semesters.
- Group Allocation:
- CBL Cohort: Students enrolled after the implementation of the CBL model.
- Traditional (PL) Cohort: Students enrolled under the previous traditional learning model.
- Intervention (CBL Model): The curriculum is restructured around real-life challenges crafted in conjunction with industrial partners. Students work collaboratively to research and develop solutions, integrating academic content from multiple disciplines (e.g., physics, math, computing) [5].
- Outcome Measures:
- Academic Performance: Final exam grades, challenge/project report grades, and final course grades.
- Student Perception: Standardized opinion surveys measuring students' views on competency development and problem-solving skills.
- Data Analysis: Statistical comparison of average grades between cohorts and thematic analysis of survey responses.
The following workflow diagrams illustrate the structural differences and key stages of these two pedagogical approaches.
Diagram 1: Comparison of Instructional Workflows. This diagram contrasts the linear, content-focused path of Traditional Instruction with the iterative, inquiry-driven cycles of Challenge-Based Learning.
The Scientist's Toolkit: Research Reagents for CBL Experiments
Implementing and studying CBL requires specific "research reagents" – the conceptual tools and frameworks that ensure rigorous educational design and evaluation.
Table 2: Essential Reagents for CBL Implementation and Research
| Tool/Reagent | Category | Function in CBL Experimentation |
|---|---|---|
| HPL Framework [22] | Theoretical Framework | Guides the design of learning environments to be learner-centered, knowledge-centered, assessment-centered, and community-centered. |
| Real-World Challenge [16] [5] | Core Intervention | Serves as the central, authentic problem that drives student inquiry, collaboration, and solution development. |
| Industry/Clinical Training Partner [16] [5] | Contextual Resource | Provides real-world relevance, formalizes the challenge, and offers expert feedback on proposed solutions. |
| Adaptive Expertise Assessment [22] | Evaluation Tool | Measures the ability to apply knowledge innovatively in novel contexts, a key outcome of CBL. |
| Competency Rubrics [5] | Evaluation Tool | Provides structured criteria for assessing the development of both disciplinary and transversal competencies (e.g., collaboration, critical thinking). |
| Structured Reflection Prompts [19] | Metacognitive Tool | Facilitates student self-assessment and consolidation of learning throughout the challenge process. |
| BMVC | BMVC Reagent | BMVC is a research-use only (RUO) fluorescent probe for studying DNA G-quadruplex structures and developing photodynamic therapy (PDT) applications. |
| SQDG | SQDG Sulfoquinovosyl Diacylglycerol |
The comparative analysis between challenge-based and traditional instruction in biomedicine reveals a nuanced picture. Traditional methods demonstrate enduring effectiveness in facilitating the acquisition of core knowledge. However, the evidence strongly indicates that Challenge-Based Learning equips students with a critical complementary skill set. CBL significantly enhances innovative problem-solving abilities, adaptive expertise, and student engagement, producing equivalent content knowledge gains while better preparing researchers, scientists, and biomedical professionals for the complex, unpredictable challenges of the modern workplace. The choice of instructional method, therefore, should be guided by the specific learning objectives, with CBL representing a powerful evidence-based approach for fostering the innovators and agile problem-solvers required in contemporary biomedicine.
Key Differences in Learning Objectives and Student Engagement Strategies
Biomedical education has undergone significant transformation in recent decades, moving from traditional, instructor-centered approaches toward innovative, student-centered methodologies. This shift is particularly evident in the comparison between challenge-based learning (CBL) and traditional didactic instruction. As biomedical fields evolve at an unprecedented pace, educators face increasing pressure to develop instructional strategies that not only convey essential knowledge but also cultivate the adaptive problem-solving capabilities required for professional success. This comprehensive analysis examines key differences in learning objectives and engagement strategies between these two educational approaches, drawing on empirical evidence from biomedical engineering and medical education contexts. The framework for understanding these distinctions lies in their fundamental educational philosophies: traditional methods prioritize knowledge transmission and content mastery, while challenge-based approaches emphasize knowledge application and adaptive expertise development [22] [24] [23].
Research indicates that the choice between these instructional paradigms has significant implications for student outcomes. While traditional instruction has demonstrated effectiveness in building foundational knowledge, challenge-based approaches appear to offer distinct advantages in developing higher-order thinking skills and professional competencies. This article systematically compares these models across multiple dimensions, including learning objectives, engagement strategies, assessment outcomes, and implementation requirements, providing educators and curriculum designers with evidence-based insights to inform pedagogical decisions [25] [22] [16].
Comparative Analysis of Learning Objectives
Foundational Philosophies and Goal Structures
The learning objectives in traditional versus challenge-based biomedical instruction reflect fundamentally different conceptions of what constitutes valuable learning. Traditional didactic instruction typically emphasizes the systematic acquisition of disciplinary knowledge through structured content delivery, with learning objectives often focusing on content coverage, factual recall, and procedural application within well-defined parameters. In contrast, challenge-based learning frames objectives around authentic problems drawn from professional practice, emphasizing the development of adaptive expertise that enables students to transfer knowledge to novel situations [22] [24].
Table 1: Comparison of Primary Learning Objectives
| Objective Category | Traditional Instruction | Challenge-Based Learning |
|---|---|---|
| Knowledge Focus | Content mastery within defined curriculum | Knowledge integration across disciplines |
| Skill Development | Procedural competence in standard methods | Innovative problem-solving in novel contexts |
| Thinking Processes | Analytical thinking within established frameworks | Adaptive and generative thinking abilities |
| Professional Preparation | Foundation for further specialized training | Readiness for complex professional environments |
Knowledge Types and Cognitive Processes
The taxonomy of learning objectives differs substantially between approaches. Traditional instruction often prioritizes declarative knowledge (knowing what) and procedural knowledge (knowing how) within established disciplinary boundaries. Assessments typically measure students' abilities to reproduce and apply this knowledge in structured formats. Conversely, challenge-based learning targets conditional knowledge (knowing when and why) and strategic knowledge (knowing how to learn), with objectives focused on students' capacities to navigate ambiguous problems, make strategic decisions about solution approaches, and monitor their own learning processes [22] [23].
Research by Martin et al. demonstrated that while both instructional approaches produced equivalent gains in foundational knowledge, challenge-based instruction led to significantly greater development of innovative thinking abilities. Students in the challenge-based condition demonstrated superior performance when transferring their knowledge to novel problem contexts, suggesting that this approach more effectively develops the adaptive expertise required for professional innovation [22] [23].
Student Engagement Strategies
Structural Frameworks for Engagement
Engagement strategies in traditional biomedical education typically center on structured participation mechanisms such as in-class questions, scheduled discussions, and assigned homework. These strategies operate within a predictable framework where instructors maintain primary control over the learning process. In contrast, challenge-based learning employs authentic problem contexts to create intrinsic motivation, positioning students as active agents in their learning process. The CBL framework typically includes: engaging with a big idea relevant to professional practice, formulating essential questions, addressing a concrete challenge, developing and implementing solution strategies, and sharing results with authentic audiences [24] [16].
Table 2: Engagement Strategy Comparison
| Engagement Dimension | Traditional Instruction | Challenge-Based Learning |
|---|---|---|
| Motivational Source | Extrinsic (grades, requirements) | Intrinsic (problem relevance, autonomy) |
| Student Role | Knowledge recipient | Active problem-solver and co-creator |
| Instructor Role | Primary knowledge source | Facilitator and guide |
| Social Structure | Individual achievement focus | Collaborative team-based work |
| Feedback Mechanisms | Structured and scheduled | Continuous through iteration |
Implementation and Impact of Engagement Strategies
Empirical studies demonstrate that the engagement strategies employed in challenge-based learning environments lead to measurable differences in student behaviors and attitudes. Research examining CBL implementations in bioinstrumentation courses reported significantly higher levels of cognitive engagement, collaborative integration, and persistence in problem-solving compared to traditional formats [16]. These engagement patterns correlate with the development of professional competencies including self-directed learning capabilities, collaborative skills, and creative confidence [24] [16].
Blended learning approaches that combine digital platforms with flipped classroom models have shown particular promise for enhancing engagement in biomedical education. Studies comparing blended and traditional formats found significantly higher learning satisfaction and more positive self-evaluations among students in blended environments that incorporated challenge-based elements. These findings suggest that strategic technology integration can amplify the engagement benefits of challenge-based approaches [25].
Experimental Evidence and Outcome Data
Comparative Studies in Biomedical Education
Rigorous comparative studies provide compelling evidence regarding the differential impacts of traditional and challenge-based instructional approaches. A 2007 study published in Annals of Biomedical Engineering directly compared student learning in challenge-based and traditional biotransport courses [22] [23]. This research employed a controlled design with pre- and post-testing to measure knowledge acquisition and innovative thinking abilities. The results demonstrated equivalent knowledge gains between groups but significantly greater improvement in innovative problem-solving among students in the challenge-based condition [22] [23].
More recent research examining blended learning in evidence-based medicine education found that students in the experimental (blended challenge-based) group showed significantly greater improvement from pre-test to post-test compared to the traditional group (score increases of 4.05 vs. 2.00 points) [25]. These students also reported substantially higher learning satisfaction and more positive self-evaluations of their learning outcomes [25].
Meta-Analytic Evidence
Broad-scale analyses of active learning approaches provide additional evidence for the effectiveness of challenge-based pedagogies. A 2024 systematic review and meta-analysis examined self-directed learning (a key component of challenge-based approaches) versus traditional didactic learning in undergraduate medical education [26]. The analysis included 14 studies with 1,792 students and found that self-directed learning approaches significantly outperformed traditional methods on exam scores (overall mean difference = 2.399, 95% CI [0.121-4.678]) [26].
Similarly, a 2025 meta-analysis of problem-based learning combined with seminar teaching (a close relative of challenge-based learning) demonstrated superior outcomes across multiple domains including theoretical knowledge, clinical skills, case analysis ability, and learning interest compared to traditional instruction [27]. These findings suggest that the benefits of challenge-based approaches extend beyond specific contexts to broader educational applications.
Table 3: Quantitative Outcomes from Comparative Studies
| Study | Knowledge Gains | Problem-Solving Improvements | Engagement Metrics |
|---|---|---|---|
| Martin et al. (2007) [22] [23] | Equivalent to traditional | Significantly greater than traditional | Not reported |
| Blended EBM Study (2024) [25] | Greater improvement (4.05 vs. 2.00) | Not assessed | Significantly higher satisfaction |
| SDL Meta-Analysis (2024) [26] | Superior to traditional (MD = 2.399) | Not separately assessed | Not quantitatively synthesized |
| PBL+Seminar Meta-Analysis (2025) [27] | Significantly higher (MD = 4.99) | Case analysis significantly better | Learning interest significantly higher |
Methodological Approaches in Key Studies
Experimental Designs and Implementation Models
The evidence base comparing challenge-based and traditional instruction in biomedical education incorporates diverse methodological approaches. A representative example comes from a 2024 study implementing CBL in a bioinstrumentation course [16]. This implementation followed a structured framework: students worked in teams to tackle authentic challenges (designing respiratory or cardiac gating devices for radiotherapy), engaged in blended learning activities combining online and in-person work, and collaborated with industry partners to ensure real-world relevance [16].
Another rigorous comparison in evidence-based medicine education employed a cohort design with careful controls [25]. The traditional learning group received lecture-based instruction with in-class question sessions, while the blended challenge-based group engaged with pre-class materials, developed debriefing slides in subgroups, and participated in instructor-facilitated synthesis sessions [25]. This methodology allowed direct comparison of knowledge acquisition while also capturing differences in engagement and satisfaction.
Assessment Strategies and Outcome Measures
Research in this domain has employed diverse assessment strategies to capture the multidimensional impacts of different instructional approaches. The Martin et al. study utilized a novel assessment framework that separately measured knowledge acquisition (through standard content tests) and innovative thinking (through transfer problems requiring adaptation to novel contexts) [22] [23]. This approach revealed the distinctive advantage of challenge-based learning in developing adaptive capacities beyond content mastery.
Other studies have incorporated comprehensive evaluation matrices including quantitative metrics (test scores, skill assessments), self-report measures (satisfaction, self-efficacy, engagement surveys), and behavioral observations (participation patterns, collaboration quality) [25] [16]. This multidimensional assessment approach provides a more complete picture of how different instructional strategies influence the student learning experience.
Decision Framework for Biomedical Instructional Strategies
Essential Research Reagents and Methodological Tools
Implementing rigorous comparisons between instructional approaches requires specific "research reagents" – the conceptual and methodological tools needed to design, implement, and assess educational interventions.
Table 4: Essential Research Methodologies for Educational Comparisons
| Method Category | Specific Tools | Application in Research |
|---|---|---|
| Experimental Designs | Controlled cohort studies | Comparing outcomes between instructional conditions [25] |
| Pre-post testing with transfer assessments | Measuring knowledge gains and adaptive expertise [22] [23] | |
| Assessment Instruments | Content knowledge tests | Quantifying foundational knowledge acquisition [25] [26] |
| Innovative problem-solving measures | Assessing application and adaptation capabilities [22] [23] | |
| Engagement and satisfaction surveys | Capturing student experiences and perceptions [25] [16] | |
| Implementation Frameworks | CBL structured protocols | Ensuring consistent challenge-based implementation [24] [16] |
| Blended learning models | Combining digital and in-person learning elements [25] | |
| Analysis Approaches | Meta-analytic synthesis | Aggregating findings across multiple studies [26] [27] |
| Multivariate statistical methods | Accounting for confounding variables and interactions |
These methodological tools enable rigorous investigation of the complex relationships between instructional strategies and learning outcomes. Their appropriate application requires specialized knowledge in both biomedical content and educational research methods.
The comparative analysis of challenge-based and traditional instructional approaches in biomedical education reveals distinct profiles of strengths and limitations. Traditional didactic methods demonstrate effectiveness in building foundational knowledge efficiently and predictably, making them appropriate for content-heavy foundational courses. Conversely, challenge-based approaches excel at developing adaptive expertise, innovative problem-solving capabilities, and professional competencies that transfer to novel situations [22] [24] [23].
The emerging evidence suggests that strategic integration of both approaches may offer the most powerful educational pathway. Blended models that combine the structured knowledge building of traditional methods with the authentic application focus of challenge-based learning demonstrate particular promise [25] [16]. Future research should explore optimal sequencing and integration of these approaches across biomedical curricula, with attention to longitudinal impacts on professional success and adaptive capacity in evolving biomedical fields.
For educational researchers and curriculum designers, these findings highlight the importance of aligning instructional strategies with specific learning objectives. When the goal is efficient knowledge transmission within established paradigms, traditional methods remain effective. When the objective extends to developing innovators capable of advancing biomedical practice, challenge-based approaches offer distinct advantages that merit their increased implementation costs and logistical complexities [16]. The evolving landscape of biomedical education will likely continue to leverage both paradigms, with strategic selection guided by explicit learning priorities and evidence-based practice.
Implementing Challenge-Based Learning in Biomedical Curricula: Methods and Real-World Applications
Designing Effective CBL Modules for Biomedical and Drug Development Courses
Table 1: Summary of Key Comparative Findings
| Educational Modality | Exam Performance (vs. LBL) | Skill Development | Knowledge Retention | Student Satisfaction |
|---|---|---|---|---|
| Case-Based Learning (CBL) | Significantly higher (SMD = 0.58, P < 0.05) [28] | Enhanced communication, problem-solving, and clinical skills [28] | Improved retention in therapeutic drug monitoring (82.5% vs 78.1%) [29] | Higher satisfaction (RR = 1.63, P < 0.05) [28] |
| CBL with Virtual Patients | No significant difference in initial knowledge (85.5% vs 87.0%) [29] | N/A | Better calculation retention (90.3% vs 86.9%, p=0.032) [29] | N/A |
| CBL with Standardized Patients (SP) | Significantly higher (MD = 5.91, P < 0.001) [30] | Improved clinical performance (MD = 7.62, P < 0.001) [30] | N/A | Substantially higher (OR = 7.19, P < 0.001) [30] |
| Challenge-Based Learning (CBL) | Equivalent knowledge gains [31] | Significantly greater improvement in innovative thinking [31] | N/A | Increased engagement and contextual awareness [16] |
| Team-Based Learning (TBL) | Enhanced but not statistically significant (MD = 2.27) [32] | N/A | N/A | N/A |
The complex, interdisciplinary nature of modern biomedical engineering and drug development demands educational strategies that move beyond knowledge transmission to foster robust problem-solving, innovation, and clinical reasoning. Traditional, lecture-based learning (LBL) has been the cornerstone of science education for decades. However, its limitations in preparing students for real-world challenges have become increasingly apparent [30] [28]. In response, active learning modalities like Case-Based Learning (CBL) and Challenge-Based Learning (CBL) are gaining prominence. These methods immerse learners in realistic scenarios, bridging the gap between theoretical knowledge and professional application. This guide provides a data-driven comparison of these innovative approaches against traditional instruction, offering evidence-based protocols for designing effective educational modules for scientists, researchers, and drug development professionals.
Quantitative Outcomes: A Meta-Analytic Perspective
Systematic reviews and meta-analyses provide the highest level of evidence for evaluating educational interventions. The data demonstrates a clear, positive trend for active learning strategies over traditional methods.
Case-Based Learning (CBL)
A 2025 meta-analysis of 11 randomized controlled trials (RCTs) in pharmacy education provided compelling evidence for CBL's effectiveness. The analysis, encompassing 1,339 students, found that CBL not only improved exam scores but also cultivated a range of essential competencies crucial for biomedical professionals [28].
Table 2: CBL Effectiveness on Skills and Satisfaction (from Meta-Analysis) [28]
| Outcome Measure | Risk Ratio (RR) or Standardized Mean Difference (SMD) | 95% Confidence Interval | P-value |
|---|---|---|---|
| Exam Scores | SMD = 0.58 | [0.39, 0.77] | < 0.05 |
| Communication & Collaboration Skills | RR = 2.49 | [1.17, 5.27] | < 0.05 |
| Problem-Solving Abilities | RR = 2.19 | [1.26, 3.80] | < 0.05 |
| Clinical Practice Skills | RR = 2.39 | [1.46, 3.92] | < 0.05 |
| Class Satisfaction | RR = 1.63 | [1.22, 2.18] | < 0.05 |
Integrated Methodologies: CBL with Standardized Patients
The combination of CBL with Standardized Patients (SP) creates a powerful, immersive learning environment. A 2025 meta-analysis of 31 RCTs (n=2,674) in Chinese medical education quantified the impact of this integrated approach, showing substantial improvements across all three domains of Kirkpatrick's evaluation model: reaction, learning, and behavior [30].
Table 3: Effectiveness of SP Combined with CBL (from Meta-Analysis) [30]
| Outcome Domain | Mean Difference (MD) or Odds Ratio (OR) | 95% Confidence Interval | P-value | GRADE Evidence |
|---|---|---|---|---|
| Teaching Satisfaction | OR = 7.19 | [3.80, 13.60] | < 0.001 | Moderate |
| Theoretical Knowledge | MD = 5.91 | [4.63, 7.18] | < 0.001 | Low (due to inconsistency) |
| Clinical Practice Performance | MD = 7.62 | [6.16, 9.08] | < 0.001 | Low (due to inconsistency) |
Subgroup analyses further revealed that improvements in theoretical knowledge were more pronounced among medical students, while enhancements in clinical performance were more significant among resident physicians, highlighting the value of tailoring interventions to the learner's stage of professional development [30].
Experimental Protocols in Practice
Translating educational theory into practice requires structured protocols. The following are detailed methodologies from cited studies that can be adapted for course design.
Protocol 1: Virtual Patient CBL for Therapeutic Drug Monitoring
This protocol was successfully implemented in a pharmacy curriculum to teach antibiotic dosing and monitoring with reduced contact hours [29].
- Course Structure: The 2-credit course met twice weekly for one-hour sessions. The first weekly session covered conceptual material with practice cases, and the second was a dedicated case-day.
- Case Design & Platform: All practice and graded cases were built using a simulated Electronic Health Record (EHR) with virtual patients (e.g., EHR Go Platform) to mimic an inpatient Advanced Pharmacy Practice Experience (APPE).
- Session Workflow:
- In-Class Practice: Students completed review and answered practice cases during course time with instructor facilitation.
- Graded Assignments: Following practice, students completed graded cases individually or in groups within 24 hours. Submissions required a pharmacokinetic consult note and calculations.
- Assessment Shift: The course grade was weighted toward application, with graded cases comprising 40% of the final grade, exams 50%, and quizzes/pre-class assignments 10%.
Virtual Patient CBL Workflow
Protocol 2: Case-Based VR Simulation for Severe Pelvic Trauma
This protocol from orthopedic surgery education integrates CBL with Virtual Reality (VR) to teach complex clinical reasoning and procedural skills for a high-stakes, low-frequency medical scenario [33].
- Case Development:
- Collaborative Design: Specialists in basic and clinical medicine design cases based on literature, real patient cases, and course syllabi.
- Scenario Progression: A representative case follows a patient from the emergency department to the intensive care unit and operating room as their condition worsens, allowing learners to acquire both declarative and procedural knowledge.
- Scripting: Detailed scripts are created for different clinical environments (emergency room, ICU, OR), specifying learner interactions with the Electronic Standardized Patient (ESP) for history taking, physical examination, and auxiliary tests.
- Framework Construction:
- A 3D pelvic fracture model is developed using tools like Maya and ZBrush, based on real clinical data.
- The VR system architecture includes multiple ports and modules to support the learning journey.
- Implementation & Evaluation:
- A comprehensive training plan is rolled out for administrators, instructors, and students.
- Learning is evaluated using a one-group pretest-posttest design, assessing knowledge, procedural skills, and confidence.
Protocol 3: Challenge-Based Learning in Biomedical Instrumentation
This protocol was implemented in a third-year biomedical engineering blended course, challenging students to design, prototype, and test a respiratory or cardiac gating device for radiotherapy [16].
- The CBL Framework: The process follows a structured progression:
- Big Idea: A broad concept like improving radiotherapy safety.
- Essential Question: What is required to accurately gate radiation delivery?
- The Challenge: A concrete, actionable goal—e.g., "Design a cardiac gating device."
- Solution Development: Teams research, design, and prototype their solutions.
- Assessment & Implementation: Solutions are evaluated for connection to the challenge, technical accuracy, and potential efficacy.
- Publishing: Results and experiences are documented and shared.
- Industry Partnership: Collaboration with an industry partner ensures the challenge is authentic and provides real-world context and feedback.
- Blended Format: The experience combines online communication, lab experiments, and in-person CBL activities.
CBL Framework Progression
The Scientist's Toolkit: Key Reagents for Implementation
Table 4: Essential Resources for Developing CBL and CBL Modules
| Tool Category | Specific Example | Function in Educational Design |
|---|---|---|
| Simulated EHR Platforms | EHR Go Platform [29] | Provides an authentic, risk-free environment for students to access patient data, make clinical decisions, and document care, replicating a real clinical setting. |
| Virtual Reality (VR) Systems | Custom ESP for Severe Pelvic Trauma [33] | Creates immersive, interactive simulations of complex clinical scenarios, allowing for repetitive practice of both cognitive and procedural skills without consuming physical resources. |
| AI & Active Learning Libraries | DeepChem [34] | Offers machine learning tools, including active learning algorithms, which can be used to optimize in-silico drug discovery processes and teach these advanced concepts. |
| Domain-Specific Language Models | PharmBERT [35] | A large language model pre-trained on drug labels, useful for teaching and automating the extraction of critical pharmacokinetic and pharmacodynamic information from complex regulatory documents. |
| Structured Pedagogical Frameworks | Kirkpatrick's Four-Level Model [30] | Provides a validated structure for evaluating educational interventions from student satisfaction (Level 1) to applied learning (Level 2) and broader impacts. |
| DTP3 | DTP3, CAS:1809784-29-9, MF:C26H35N7O5, MW:525.6 g/mol | Chemical Reagent |
| 2-Methoxy-4-[(5,6,7,8-tetrahydrobenzo[4,5]thieno[2,3-d]pyrimidin-4-yl)-hydrazonomethyl]-phenol | 2-Methoxy-4-[(5,6,7,8-tetrahydrobenzo[4,5]thieno[2,3-d]pyrimidin-4-yl)-hydrazonomethyl]-phenol, CAS:304684-77-3, MF:C18H18N4O2S, MW:354.4 g/mol | Chemical Reagent |
The collective evidence demonstrates that active learning modalities—particularly CBL, CBL, and their technology-enhanced variants—consistently match or surpass traditional lecture-based instruction in foundational knowledge acquisition while significantly outperforming it in developing critical applied skills, enhancing knowledge retention, and boosting student satisfaction and engagement. The choice of modality depends on the specific learning objectives: CBL is exceptional for teaching clinical reasoning within defined parameters, CBL fosters innovative thinking and problem-solving for open-ended challenges, and TBL promotes collaborative learning.
For researchers and educators in biomedical engineering and drug development, the implication is clear: integrating these evidence-based, active learning strategies is crucial for preparing a workforce capable of tackling the complex, interdisciplinary problems that define the future of healthcare and therapeutic innovation.
The rapid evolution of the biomedical fields demands educational approaches that equip researchers, scientists, and drug development professionals with robust theoretical knowledge and the problem-solving skills necessary for clinical and laboratory practice. For years, lecture-based learning (LBL), a quintessential traditional teaching approach, has been widely utilized in biomedical education [36] [28]. However, modern educational reforms are increasingly shifting toward active learning strategies. Case-Based Learning (CBL), a problem-oriented teaching model centered on clinical cases, requires students to apply relevant professional knowledge and clinical thinking to solve problems [36]. This guide provides an objective, data-driven comparison of CBL and traditional learning methods across three critical biomedical education contexts: pharmacology, clinical research, and laboratory training, framing the analysis within the broader thesis of challenge-based versus traditional instructional research.
Quantitative Outcomes: A Meta-Analytic Comparison
A systematic review and meta-analysis of CBL in pharmacy education offers high-level evidence of its effectiveness. The analysis, which included 11 randomized controlled trials (RCTs) involving 1,339 pharmacy students, provides standardized quantitative outcomes across several critical competencies [36] [28].
Table 1: Meta-Analysis Results of CBL vs. LBL in Pharmacy Education
| Outcome Measure | Statistical Result | Significance |
|---|---|---|
| Exam Scores | SMD = 0.58, 95% CI [0.39, 0.77] | P < 0.05 |
| Communication/Collaboration Skills | RR = 2.49, 95% CI [1.17, 5.27] | P < 0.05 |
| Problem-Solving Abilities | RR = 2.19, 95% CI [1.26, 3.80] | P < 0.05 |
| Clinical Practice Skills | RR = 2.39, 95% CI [1.46, 3.92] | P < 0.05 |
| Student Satisfaction | RR = 1.63, 95% CI [1.22, 2.18] | P < 0.05 |
SMD: Standardized Mean Difference; RR: Risk Ratio; CI: Confidence Interval
The data demonstrates that CBL consistently leads to better outcomes than LBL, with significantly higher exam scores and a greater than two-fold likelihood of students developing enhanced communication, problem-solving, and clinical skills [36].
Experimental Protocols in Practice
Case Study: Pharmacology Education
A comparative study in pharmacology for second-year MBBS students employed a crossover design to evaluate CBL against traditional teaching methods (TTM) [37] [38].
- Objective: To compare the effectiveness of CBL and TTM in teaching topics like myocardial infarction, diabetes mellitus, and anti-ulcer drugs in terms of knowledge gained [37] [38].
- Participants: 90 second-year MBBS students [38].
- Methodology:
- Students were divided into two groups: Didactic Lecture (DDL) and CBL.
- The CBL group was further subdivided into smaller subgroups of 15 students.
- The study was conducted over 8 sessions for 4 separate topics.
- A crossover was performed after the first topic, meaning groups switched learning methods for subsequent topics to mitigate bias.
- Knowledge gain was assessed via pre-test and post-test questionnaires for both groups [38].
- Outcome Analysis: Paired t-tests were used to analyze pre- and post-test scores within groups, and an unpaired t-test was used to compare post-test scores between the DDL and CBL groups [38].
Case Study: Laboratory Training in Clinical Biochemistry
A study on laboratory training designed a student-centred program based on CBL to improve quality management awareness according to ISO 15189 requirements [39].
- Objective: To improve students' awareness and ability in total testing process (TTP) quality management, with a focus on error-prone preanalytical and postanalytical stages [39].
- Participants: 357 undergraduate medical laboratory science students randomly assigned to a test group (CBL, n=185) and a control group (traditional training, n=172) [39].
- CBL Intervention (4-Stage Protocol):
- Establish Testing Process: Students received a patient case 2-4 days before class. They individually answered questions about the diagnosis, detection indicators, and the pre-analysis, analysis, and post-analysis procedures. Answers were then shared and discussed in small groups with teacher facilitation (≈30 minutes).
- Clarify Principles: Instruction on current methods and principles for the tests (≈30 minutes).
- Improve Operational Skills: Hands-on laboratory work, including evaluation of lab and equipment conditions, use of internal controls, and sample processing per standard operating procedures (SOPs) (≈45 minutes).
- Review and Continuous Improvement: Analysis of results combined with ISO 15189 requirements. Students learned to identify abnormal results and decide if they could be reported, repeating the check if necessary (≈30 minutes) [39].
- Control Group: Received teacher-centred experimental teaching where the instructor explained principles, operations, and medical significance before students performed the experiment [39].
- Outcome Evaluation: Assessment included laboratory operational skills and total examination scores, alongside a questionnaire survey [39].
Case Study: Clinical Research and Therapeutic Drug Monitoring
A study investigated the impact of converting a Therapeutic Drug Monitoring (TDM) course from a traditional format to a CBL one utilizing virtual patients [29].
- Objective: To compare student knowledge and knowledge retention of antibiotic dosing and monitoring between a traditional 4-credit TDM course and a redesigned 2-credit CBL course [29].
- Participants: Third-year pharmacy (P3) students from the traditional course (Spring 2019) and the redesigned CBL course (Spring 2020) [29].
- CBL Intervention:
- The course was reduced from 4 to 2 credit hours but redesigned to be case-based.
- Classes involved conceptual lectures with practice cases, followed by a "case-day."
- Students completed virtual patient cases within a simulated Electronic Health Record (EHR) to mimic an inpatient Advanced Pharmacy Practice Experience (APPE).
- Students completed 3 practice and 3 graded cases on antimicrobial dosing and monitoring.
- The grade distribution shifted to emphasize application: graded cases (40%), exams (50%), and pre-class assignments/quizzes (10%) [29].
- Traditional Comparison: The traditional course spent over 85% of class time on concepts and practice problems, with grades based solely on exams (80%) and quizzes (20%) [29].
- Data Collection: Students completed a knowledge assessment immediately after the course and a knowledge retention assessment before their Internal Medicine APPE in their fourth year (P4) [29].
Visualizing the CBL Workflow
The following diagram illustrates the structured, iterative process common to CBL implementations in biomedical education, particularly evident in the laboratory training case study [39].
Figure 1: The CBL Cycle in Biomedicine. This workflow maps the student journey from initial case exposure to competency achievement, highlighting the integration of self-directed learning, collaboration, and practical application [39].
The Scientist's Toolkit: Key Reagents for CBL Experiments
Successful implementation of CBL in biomedical education relies on specific "research reagents" or essential components.
Table 2: Essential Components for Implementing CBL
| Component | Function in the CBL Experiment |
|---|---|
| Clinical Cases | Adapted from real clinical scenarios, these form the core problem statement that drives learning and application of knowledge [36] [38]. |
| Simulated Electronic Health Record (EHR) | Provides an authentic, risk-free environment for students to practice therapeutic drug monitoring, data analysis, and clinical decision-making [29]. |
| Standardized Operating Procedures (SOPs) | Guide students in practical laboratory work, ensuring adherence to quality standards like ISO 15189 and fostering professional habits [39]. |
| Structured Assessment Rubrics | Tools for objectively evaluating competencies beyond factual recall, including laboratory skills, problem-solving, and clinical reasoning [39] [29]. |
| Facilitator Guidelines | A guide for instructors to ensure consistency in facilitating group discussions, providing feedback, and guiding—rather than directing—student learning [29]. |
| PCTA | PCTA |
| Dexamethasone 17-acetate | Dexamethasone 17-acetate, CAS:25122-35-4, MF:C24H31FO6, MW:434.5 g/mol |
The evidence from pharmacology, clinical research, and laboratory training consistently demonstrates the efficacy of CBL over traditional methods. The quantitative meta-analysis shows clear, significant benefits across multiple learning domains [36] [28]. The individual case studies reveal that these benefits persist even when contact hours are substantially reduced, as seen in the TDM course, and that CBL effectively fosters crucial practical skills and knowledge retention [39] [29].
A key strength of CBL is its engagement of students through interaction with content, peers, and self, moving them from passive recipients to active participants in their education [40]. Furthermore, online CBL has shown promise in fostering clinical reasoning, though challenges like decreased engagement and unrealistic case presentations must be managed, often through blended learning approaches [41].
In conclusion, for educating the next generation of biomedical researchers, scientists, and drug development professionals, CBL provides a superior pedagogical framework. It effectively bridges the gap between theoretical knowledge and the complex, practical competencies required in real-world clinical and laboratory settings.
Integrating Digital Tools and Simulations for Enhanced Learning Experiences
Higher education institutions are actively reviewing teaching methodologies to align graduate competencies with evolving socioeconomic and professional demands [21]. In biomedical science and drug development education, this has catalyzed a transition from traditional, content-delivery models towards innovative, experiential approaches [5] [42]. Among these, Challenge-Based Learning (CBL) has emerged as a prominent pedagogical strategy, emphasizing real-world problem-solving and competency development [21]. Concurrently, digital tools like clinical simulations and virtual laboratories are gaining traction for their ability to provide immersive, low-risk training environments [42] [43]. This guide objectively compares the performance of Challenge-Based Learning against traditional instructional models within biomedical education, presenting supporting experimental data to inform researchers, scientists, and drug development professionals.
Defining the Educational Frameworks
Challenge-Based Learning (CBL)
CBL is a student-centered approach that immerses learners in real-world, collaborative problems requiring the application of knowledge to develop actionable solutions [5] [21]. It shifts the educator's role from a knowledge transmitter to a facilitator who guides the learning process, provides resources, and offers timely feedback [21]. In CBL, the problems or "challenges" are often crafted in collaboration with industry partners, adding formality and rigor to the proposed solutions and enhancing professional relevance [5].
Traditional Learning Models
Traditional learning (TL) in this context refers to instructor-centered methodologies primarily based on lectures and structured course activities, where academic performance is often assessed through final exams [5]. While traditional methods may incorporate projects, they typically follow more predefined steps and are less open-ended than CBL challenges [5].
The Role of Digital Simulations
Although distinct from CBL, digital simulations often serve as powerful enabling tools within this framework. They create synthetic recreations of authentic processes or situations, allowing students to develop knowledge, competencies, and professional attitudes through direct engagement and hands-on practice without real-world risks [42] [43]. In biomedical sciences, simulations range from virtual laboratories for basic science principles to clinical scenarios for developing patient-facing skills [42] [43].
Comparative Experimental Data on Academic Outcomes
Robust, large-scale studies provide quantitative evidence comparing the efficacy of these educational approaches.
Table 1: Comparative Academic Performance in Engineering Education (Alvarez et al., 2025)
| Metric | Traditional Learning (PL) Model | Challenge-Based Learning (CBL) Model | Change |
|---|---|---|---|
| Overall Student Performance (Average Final Course Grades) | Baseline | +9.4% Improvement [5] | |
| Project/Challenge Grades | Project Average Grades | Challenge Average Grades | Comparable [5] |
| Student Perception (Favorable View on Competency Development & Problem-Solving) | Not Reported | 71% of Students | Not Applicable [5] |
Table 2: Comparative Outcomes in Statistics Education for Health Disciplines (PMC, 2025)
| Metric | Traditional Learning (Online) | Competency-Based Learning (Online) | Statistical Significance |
|---|---|---|---|
| Knowledge Score Improvement (Hypothesis Testing) | Improved | Improved | p = 0.02 [44] |
| Knowledge Score Improvement (Measures of Central Tendency) | Improved | Improved | p = 0.001 [44] |
| Knowledge Score Improvement (Research Design) | Improved | Improved | p = 0.001 [44] |
| Overall Knowledge Mean Scores | Improved | Improved | No significant difference (p = 0.10) [44] |
| Current Statistics Self-Efficacy (CSSE) | Improved (p < 0.001) | Improved (p < 0.001) | Significant in both groups [44] |
| Self-Efficacy to Learn Statistics (SELS) | Improved (p = 0.02) | Improved (p < 0.001) | Significant in both groups [44] |
Table 3: Student Perception of Clinical Simulations in Biomedical Science (Sciencedirect, 2025)
| Perception Metric | Percentage of Students in Agreement |
|---|---|
| Positive Learning Experience | 97% [43] |
| Enjoyed Taking Part | 100% [43] |
| Supported Development of Communication & Teamwork | 90% [43] |
| Improved Perceived Employability | 84% [43] |
| Desire for Simulations Embedded in Core Curriculum | 90% [43] |
| Belief Simulations are Better than Traditional Dyadic Styles | 91% [43] |
Detailed Experimental Protocols in Educational Research
Protocol 1: Quasi-Experimental Comparison of CBL vs. Traditional Models
A large-scale quasi-experimental study compared the CBL and traditional (PL) models over seven semesters [5].
- Population and Scope: The study involved 1705 freshman engineering students (43% in PL, 57% in CBL) in physics courses, spanning from Spring 2018 to Spring 2021 [5].
- Intervention (CBL Model): The CBL model presented students with crafted, ad-hoc challenges tailored to their semester and major. These challenges were designed to explicitly integrate concepts from physics, math, and computing, often with input from industrial training partners to ensure real-world relevance [5].
- Comparison (PL Model): The traditional model was based on the institution's previous educational framework, which emphasized lectures and final exams [5].
- Outcome Measures: The primary quantitative metrics for comparison were (i) final exam grades, (ii) project (PL) and challenge (CBL) report grades, and (iii) final course grades [5].
- Supplementary Qualitative Data: Opinion surveys were administered to 570 students over two years to gauge their perception of the CBL model concerning their competency development and problem-solving abilities [5].
Protocol 2: Pre-Test/Post-Test Study of Competency-Based Statistics Learning
A descriptive study examined differences in statistical knowledge and self-efficacy among undergraduate health students [44].
- Population: 20 nursing and interdisciplinary undergraduate students from a Midwestern university enrolled in introductory, asynchronous online statistics courses [44].
- Study Groups: Students were divided into two groups: one enrolled in a competency-based learning course (n=8) and the other in a traditional learning course (n=12) [44].
- Competency-Based Learning Course: This section featured self-paced modules. Each module included pretests and posttests with randomized questions, interactive vocabulary exercises, recorded lectures, and application assignments set within the context of interdisciplinary biomedical and biobehavioral research problems. The design allowed students to repeat content until mastery was demonstrated [44].
- Traditional Learning Course: This section involved instructor-led sessions via Zoom with opportunities for active learning. Students watched recorded lectures on their own time, representing a traditional structure delivered asynchronously [44].
- Outcome Measures:
- Statistical Knowledge: Assessed via multiple-choice quizzes on specific content areas (e.g., Hypothesis Testing, Central Tendency) administered as pre-tests and post-tests [44].
- Self-Efficacy: Measured using the validated 14-item Current Statistics Self-Efficacy (CSSE) scale and the 14-item Self-Efficacy to Learn Statistics (SELS) scale, which use a 6-point Likert-type scale [44].
Visualization of Educational Model Workflows
The following diagrams illustrate the structural and logical relationships within the traditional and CBL educational models.
Diagram 1: Traditional vs CBL Workflow
Diagram 2: Key Dimensions of Effective CBL
The Scientist's Toolkit: Essential Reagents for Educational Research
For researchers designing studies in educational methodology, the following table details key "research reagents" or essential components used in the featured experiments.
Table 4: Essential Materials for Educational Intervention Research
| Item / Concept | Function in Educational Research |
|---|---|
| Real-World Challenges | Core CBL component; Authentic, crafted problems from industry/community that drive student learning and application of knowledge [5] [21]. |
| Clinical Simulation Scenarios | Designed clinical situations (e.g., patient consultation, ethical dilemmas) delivered in a simulation suite to foster transferable skills like communication and teamwork [43]. |
| Self-Paced Learning Modules | Foundational element of competency-based learning; allows students to progress and repeat content until mastery is demonstrated, promoting flexibility [44]. |
| Training Partners | External companies or organizations that provide real-world challenges, context, and formal feedback to students, adding rigor to the CBL process [5]. |
| Validated Self-Efficacy Scales (CSSE, SELS) | Psychometrically tested instruments used to quantitatively measure students' confidence in their current statistical abilities and their belief in their capacity to learn statistics [44]. |
| Pre-Test/Post-Test Design | A robust experimental protocol that measures knowledge or self-efficacy before and after an educational intervention to quantify its impact [44]. |
| Technology-Enhanced Learning Tools (VR, AR) | Virtual and Augmented Reality platforms used to create immersive simulated experiences that enhance motivation and skills acquisition [42]. |
| NAT | NAT |
Discussion and Interpretation of Findings
The experimental data reveals a nuanced picture of the relative strengths of CBL and traditional instruction. The 9.4% improvement in final grades observed in the large-scale engineering study [5] strongly suggests that the CBL model, with its integration of concepts through real-world problem-solving, fosters a deeper understanding that translates to superior overall academic performance. This aligns with the theoretical framework that active, experiential learning enhances student engagement and knowledge retention [5] [21].
However, the comparable performance in project/challenge grades between models [5] and the lack of a significant difference in overall knowledge scores in the statistics study [44] indicate that both well-structured traditional and CBL approaches can effectively teach specific procedural or conceptual knowledge. The critical differentiator may lie in the development of broader competencies. The overwhelming student perception (71% favorable for CBL [5] and over 90% for simulations [43]) that these methods improve problem-solving, communication, teamwork, and employability underscores a principal advantage of CBL and simulation-based learning.
The significant improvements in self-efficacy across both statistics course formats [44] are noteworthy. Self-efficacy—the belief in one's capability to succeed—is a powerful predictor of academic motivation and resilience [44]. The finding that both methods can build confidence is positive, though the pedagogical flexibility of CBL and competency-based models appears particularly effective for supporting students from diverse backgrounds [43].
Within biomedical and drug development education, the integration of digital tools and Challenge-Based Learning frameworks presents a compelling evolution beyond traditional instruction. The evidence indicates that while both traditional and innovative models can convey core knowledge, CBL and simulations offer significant advantages in developing the holistic competencies required of modern professionals—including critical thinking, collaborative problem-solving, and adaptability [5] [21] [43]. For institutions and program directors, the implication is to strategically blend these approaches, using traditional methods for foundational knowledge and deliberately embedding CBL experiences and digital simulations to cultivate the advanced skills essential for success in complex, real-world environments like drug development and healthcare.
Best Practices for Facilitating CBL in Academic and Professional Settings
The rapid evolution of biomedical science demands educational approaches that prepare professionals for complex, real-world challenges. Traditional instructional methods, while effective at transmitting foundational knowledge, often fall short in developing the innovative thinking and adaptive problem-solving skills required in contemporary research and development settings. Challenge-Based Learning (CBL) has emerged as a promising pedagogical framework that engages learners in solving authentic, relevant problems while acquiring content knowledge. Within biomedical education, this approach bridges the gap between theoretical understanding and practical application, potentially fostering more versatile and creative scientists, engineers, and healthcare professionals.
This guide objectively compares student learning outcomes in challenge-based versus traditional biomedical instruction, drawing upon empirical research and implementation case studies. The analysis focuses on quantitative academic performance, development of non-cognitive competencies, and practical considerations for implementation in academic and professional training environments. By synthesizing evidence from multiple educational contexts, this guide aims to inform researchers, educators, and drug development professionals seeking to optimize learning methodologies.
Comparative Outcomes: CBL vs. Traditional Instruction
Research studies conducted across biomedical engineering, nursing, and related disciplines consistently demonstrate distinct outcome patterns between instructional approaches. The table below summarizes key quantitative findings from comparative studies.
Table 1: Comparative Student Outcomes in Challenge-Based and Traditional Learning Environments
| Study Context | Knowledge Acquisition | Innovative Thinking | Overall Performance | Collaboration Skills |
|---|---|---|---|---|
| Biotransport Engineering (2007) | No significant difference between CBL and traditional [22] [45] | Significantly greater improvement in CBL students [22] [45] | Not reported | Not specifically measured |
| Freshman Engineering Physics (2025) | Not directly measured | Not directly measured | 9.4% improvement in final course grades with CBL [5] | Not specifically measured |
| Nursing Education (2024) | Not directly measured | Not directly measured | Not reported | Significant increases in multidisciplinary collaboration competencies [46] |
| Bioinstrumentation (2024) | Not directly measured | Not directly measured | Positive student feedback on learning experience [16] | Enhanced industry collaboration skills [16] |
The comparative data reveals a consistent pattern: CBL environments produce equivalent or superior content knowledge acquisition while significantly enhancing higher-order cognitive and collaborative skills. This combination addresses a critical need in biomedical professions where technical expertise must be coupled with innovative capacity to solve novel problems.
Experimental Protocols and Methodologies
Biomedical Engineering Biotransport Study
A seminal comparative study conducted across multiple research institutions implemented a rigorous experimental design to evaluate CBL effectiveness [22] [45] [47]. The intervention group was taught using the How People Learn (HPL) framework, a challenge-based approach emphasizing knowledge-centered, learner-centered, assessment-centered, and community-centered instruction [47].
- Participants: 136 consenting engineering students from three research institutions (54 in HPL condition, 52 in traditional condition completing both pre-post assessments) [47]
- Intervention: The HPL/CBL method presented real-world challenges requiring students to identify knowledge gaps, research solutions, and develop innovative approaches [22]
- Control: Traditional didactic lecture methods with weekly problem sets and periodic assessments [22]
- Measures: Pre-post assessments measuring (1) domain knowledge acquisition and (2) innovative problem-solving abilities in novel contexts [22] [47]
- Analysis: Comparison of gain scores between instructional conditions using quantitative methods [47]
This study established that while both groups made equivalent knowledge gains, CBL students demonstrated significantly greater improvement in innovative thinking abilities – a crucial component of adaptive expertise [22] [45].
Large-Scale Engineering Implementation
A more recent quasi-experimental study evaluated the institutional implementation of a CBL model across engineering programs [5].
- Scale: 1,705 freshman engineering students (43% in previous learning model, 57% in CBL model) across seven semesters [5]
- Measures: Final exam grades, challenge/project report grades, final course grades, and student perception surveys [5]
- Design: Comparative analysis of academic performance metrics between cohorts experiencing different instructional models [5]
- Context: Implementation of the Tec21 educational model emphasizing competency development through real-world challenges [5]
This large-scale implementation demonstrated the feasibility of institutional CBL adoption while documenting significant improvements in overall student performance [5].
The CBL Framework: Structure and Workflow
Challenge-Based Learning follows a structured yet flexible framework that guides learners through solving authentic problems. The typical workflow progresses through three central phases, incorporating both divergent and convergent thinking processes.
Figure 1: CBL Implementation Workflow
The CBL process begins with the Engage phase, where learners identify a complex real-world problem and define an actionable challenge within a broader thematic area [48] [49]. This phase combines divergent thinking (exploring multiple problem dimensions) and convergent thinking (focusing on a specific, actionable challenge) [48].
In the Investigate phase, students conduct guided and open research to develop deeper understanding of the challenge context and brainstorm potential solutions [48] [49]. This phase typically incorporates both conceptual learning and skill development relevant to addressing the challenge.
The Act phase involves implementing solutions, testing their effectiveness, refining approaches based on feedback, and sharing results with relevant audiences [48] [49]. This implementation component distinguishes CBL from other inquiry-based approaches by emphasizing tangible action and impact.
Successful CBL implementation requires specific resources and supports to create effective learning environments. The table below details key "research reagent solutions" for CBL facilitation.
Table 2: Essential Resources for CBL Implementation in Biomedical Contexts
| Resource Category | Specific Tools/Components | Function in CBL Process |
|---|---|---|
| Framework Resources | Apple CBL Framework [48] [50], Design Thinking Double Diamond [48] | Provides structured progression from problem identification to solution implementation |
| Thinking Tools | Six Thinking Hats, Wishful Thinking, Impact-Effort Matrix [48] | Supports divergent and convergent thinking processes during investigation and solution development |
| Stakeholder Elements | Industry partners, clinical collaborators, community clients [16] [48] | Ensures authenticity of challenges and provides real-world feedback on proposed solutions |
| Physical Environment | Movable furniture, digital whiteboards, prototyping materials [48] | Facilitates collaborative work and iterative development processes |
| Digital Infrastructure | Learning management systems, video conferencing, collaborative documents [48] | Supports communication, resource sharing, and remote collaboration |
| Assessment Tools | Rubrics, portfolios, reflection diaries, peer feedback mechanisms [16] [48] | Evaluates both disciplinary learning and competency development |
These implementation resources create the necessary scaffolding for effective CBL experiences while maintaining the authenticity and open-endedness essential for developing adaptive expertise.
Discussion and Implementation Considerations
The empirical evidence demonstrates that CBL produces learning outcomes equivalent to traditional methods in content knowledge acquisition while significantly enhancing innovative thinking abilities, collaborative competencies, and overall academic performance [22] [5] [46]. These advantages align with the needs of modern biomedical research and drug development environments, where professionals must continually adapt to novel challenges and work across disciplinary boundaries.
However, implementing effective CBL requires addressing several practical considerations:
- Faculty Development: Educators must transition from content-delivery roles to learning facilitation, requiring training in guiding open-ended inquiry processes [16] [48]
- Time Investment: CBL typically requires increased planning time and more continuous student interaction compared to traditional lectures [16]
- Assessment Strategies: Evaluating process skills and innovative thinking necessitates alternative assessment methods beyond traditional exams [16] [48]
- Stakeholder Management: Industry and community partnerships require careful coordination to align educational objectives with real-world constraints [16] [48]
For biomedical professionals and researchers, these findings suggest that challenge-based approaches in both academic and professional development contexts can enhance innovative capacity and collaborative problem-solving – competencies essential for advancing drug development and healthcare solutions. The CBL framework provides a structured methodology for bridging the gap between theoretical knowledge and practical application in complex biomedical domains.
Overcoming Challenges in Challenge-Based Biomedical Instruction: Strategies for Optimization
Common Pitfalls in CBL Implementation and How to Address Them
Challenge-Based Learning (CBL) represents a significant evolution in biomedical education, shifting from traditional instructor-led models to experiential, student-centered approaches. This guide examines CBL implementation by synthesizing current experimental data and qualitative research, directly comparing its effectiveness against traditional didactic methods. Evidence reveals that while CBL significantly enhances critical thinking, problem-solving abilities, and knowledge retention, its implementation faces consistent challenges across adaptation periods, group dynamics, and facilitation quality. Data from controlled educational settings demonstrate that structured support systems and strategic faculty development can successfully mitigate these pitfalls, providing a roadmap for effective integration of CBL in biomedical curricula.
Biomedical education is undergoing a paradigm shift from traditional, passive learning methods toward active, collaborative, and problem-centered approaches. Challenge-Based Learning (CBL) has emerged as a particularly effective framework that immerses students in real-world problems requiring collaborative, creative, and critical thinking for resolution [21]. This pedagogical strategy positions students at the center of their educational journey, contrasting sharply with traditional lecture-based formats where knowledge transmission flows primarily from instructor to student [21].
The core CBL framework operates through three interdependent phases: Engage, Investigate, and Act [51]. This structure provides a customizable starting point for learners to identify significant challenges, conduct thoughtful inquiry, and develop actionable solutions. Unlike similar methodologies like Problem-Based Learning (PBL), CBL uniquely involves students in formulating the specific challenges they will address, providing greater autonomy and investment in the learning process [52]. This approach aims to develop essential competencies for future researchers and drug development professionals, including critical analysis, innovative problem-solving, teamwork, and adaptive thinking skills crucial for navigating complex biomedical challenges [21].
Experimental Comparisons: CBL Versus Traditional Instruction
Quantitative Assessment of Learning Outcomes
Recent controlled studies in medical education provide compelling quantitative evidence regarding CBL effectiveness compared to traditional didactic lectures (DL). The table below summarizes key findings from prospective interventional studies measuring knowledge acquisition.
Table 1: Comparative Learning Outcomes in Biomedical Education
| Study & Topic | Instructional Method | Pre-test Mean Score | Post-test Mean Score | Knowledge Gain | Statistical Significance (p-value) |
|---|---|---|---|---|---|
| Bhat et al., 2024 [53]: Nephrotic Syndrome | CBL | 5.30 | 11.36 | +6.06 | p < 0.001 |
| Didactic Lecture | 4.83 | 9.00 | +4.17 | p < 0.001 | |
| Bhat et al., 2024 [53]: Thalassemia | CBL | 4.61 | 10.98 | +6.37 | p < 0.001 |
| Didactic Lecture | 5.44 | 9.68 | +4.24 | p < 0.001 |
The consistent pattern across studies demonstrates that CBL produces significantly greater knowledge gains than traditional lectures. Statistical analysis confirms these differences are highly significant, not attributable to chance variation. Both instructional methods improve scores from pre-to-post testing, confirming that structured learning occurs regardless of methodology. However, the enhanced gains under CBL suggest its approach fosters deeper conceptual understanding and better information integration.
Qualitative Assessment of Learner Experiences
Beyond test scores, research reveals crucial differences in the educational experience between CBL and traditional formats. Studies utilizing structured group feedback sessions and thematic analysis identify several distinctive features of CBL that contribute to its effectiveness [54]:
- Increased Peer Interaction and Bonding: CBL's collaborative nature naturally facilitates student connection, creating supportive learning communities particularly valuable in multicultural educational settings [54].
- Psychological Safety Requirements: Students note that effective participation requires an environment where they feel safe to express ideas without judgment, highlighting the importance of facilitator skill in cultivating inclusive spaces [54].
- Authenticity and Relevance: Learners report higher engagement when cases mirror real-world clinical scenarios, making knowledge acquisition more meaningful and memorable [54].
- Adaptation to Uncertainty: Some students initially struggle with the ambiguous nature of CBL compared to the structured clarity of lectures, indicating a need for graduated exposure to build tolerance for uncertainty [54].
Implementation Pitfalls and Evidence-Based Solutions
Despite its demonstrated benefits, CBL implementation faces consistent challenges across educational contexts. The following diagram maps the primary pitfalls and their interrelationships within the CBL implementation process.
Diagram 1: CBL Implementation Pitfalls and Corresponding Solutions
Adaptation Challenges and Transition Support
The Pitfall: The transition from traditional learning methods to CBL creates significant psychological and academic strain. Research on nursing students transitioning from Case-Based Learning to Problem-Based Learning (a related pedagogical shift) reveals these changes can negatively affect "academic, psychological, emotional, or social well-being," potentially leading to "high failure rates, anxiety disorders, a loss of uniqueness, and fear of the unknown" [55]. This adjustment period is particularly pronounced for students from educational backgrounds with highly structured, teacher-centered approaches.
The Solution: Implement structured transition scaffolding that gradually introduces CBL elements. This includes:
- Providing explicit orientation sessions that articulate the philosophical underpinnings and expected benefits of CBL [55].
- Creating low-stakes preliminary challenges that allow students to practice the CBL process without significant grade consequences.
- Establishing clear guidelines for self-directed learning and time management specific to CBL requirements [55].
- Developing mentorship programs where experienced CBL students guide newcomers through the initial adjustment phase.
Group Dynamics and Collaborative Learning
The Pitfall: Effective collaboration does not occur automatically in group settings. Student surveys identify "group work" as a significant challenge in active learning environments, with issues including uneven participation, conflicting work styles, and communication barriers [55]. In multicultural learning environments, these challenges can be exacerbated by differing communication norms and language proficiencies [54].
The Solution: Foster psychological safety and clear collaboration protocols through:
- Facilitation that explicitly establishes and reinforces group norms for respectful interaction and equitable participation [54].
- Team charters developed collaboratively by student groups that outline expectations, roles, and processes for conflict resolution.
- Structured peer feedback mechanisms that allow for early identification and resolution of group dynamic issues.
- Activities specifically designed to build interpersonal trust and cross-cultural communication skills before commencing substantive work.
Assessment Alignment and Evaluation Methods
The Pitfall: Traditional assessment methods often fail to capture the multidimensional learning outcomes of CBL. Studies specifically note "challenges regarding assessment" when implementing alternative learning methodologies [55]. When evaluations focus exclusively on content recall rather than process skills, critical thinking, or solution quality, they undermine the perceived value of the CBL approach and create goal confusion for students.
The Solution: Develop diversified assessment methods that align with CBL objectives:
- Multidimensional rubrics that evaluate not only final solutions but also research quality, collaboration, iteration, and reflection processes.
- Authentic assessment tasks that mirror real-world deliverables relevant to biomedical professionals, such as research proposals, literature reviews, or protocol designs.
- Combined individual and group evaluation components that acknowledge both collaborative efforts and individual mastery.
- Peer and self-assessment elements that develop metacognitive skills and professional self-regulation.
Facilitation Quality and Faculty Development
The Pitfall: The shift from instructor to facilitator proves challenging for many faculty. Research identifies "lack of proper guidance from lecturers" as a significant student concern during implementation of problem-centered learning [55]. Without specific training, educators may either over-direct the learning process (undermining student agency) or provide insufficient structure (leading to student frustration and misdirection).
The Solution: Implement comprehensive facilitator training programs that address:
- Techniques for balancing guidance with autonomy, knowing when to intervene and when to step back [54].
- Questioning strategies that prompt deeper inquiry without providing direct answers.
- Approaches for managing dominant voices while encouraging participation from all group members, particularly important in diverse classrooms [54].
- Discipline-specific coaching on recognizing productive struggle versus unproductive frustration in the problem-solving process.
Resource Demands and Time Management
The Pitfall: CBL implementation requires substantial time investment from both students and faculty. Students report "workload and insufficient time for PBL content" as significant stressors [55]. The investigatory phase of CBL often demands more time than traditional lecture preparation, while faculty spend considerable time developing robust challenges and facilitating group processes.
The Solution: Adopt realistic time allocation and strategic scheduling:
- Curriculum redesign that explicitly allocates sufficient contact and self-directed time for CBL activities, recognizing they cannot be fit into traditional lecture schedules.
- Development of reusable, well-documented challenge resources that can be refined across multiple iterations.
- Technology integration that streamlines collaboration and resource sharing outside formal class meetings.
- Phased implementation that begins with CBL modules within traditional courses rather than entire course conversions, allowing for incremental adaptation.
Table 2: Research Reagent Solutions for CBL Implementation
| Tool Category | Specific Resource | Function in CBL Implementation |
|---|---|---|
| Assessment Instruments | Pre-/Post-test Knowledge Assessments | Quantifies knowledge gains and enables comparative effectiveness research between instructional methods [53]. |
| Multidimensional CBL Rubrics | Evaluates complex outcomes including critical thinking, collaboration, and problem-solving processes. | |
| Learning Environment Tools | Structured Group Feedback Protocols | Collects qualitative data on student experiences and identifies implementation barriers [54]. |
| Psychological Safety Measures | Monitors classroom climate and ensures inclusive participation across diverse student groups [54]. | |
| Faculty Resources | Facilitator Development Guides | Builds instructional capacity for effective facilitation rather than direct instruction [55]. |
| Challenge Design Templates | Supports creation of robust, real-world problems with appropriate scaffolding and resource guidance. | |
| Digital Infrastructure | Collaborative Online Platforms | Enables student teamwork and resource sharing across locations and outside classroom hours [55]. |
| Digital Assessment Systems | Streamlines evaluation of multidimensional learning outcomes and provides efficient feedback mechanisms. |
Implementation of Challenge-Based Learning in biomedical education presents a series of manageable yet significant challenges that can undermine effectiveness if unaddressed. The evidence consistently demonstrates that the substantial benefits of CBL—including significantly greater knowledge gains, enhanced critical thinking, and better preparation for professional practice—justify the investment in strategic implementation. Success requires acknowledging the adaptation period for both students and faculty, aligning assessment with learning objectives, developing skilled facilitation, and allocating appropriate resources. By anticipating these pitfalls and implementing the evidence-based solutions outlined here, educational researchers and curriculum designers can more effectively harness CBL's potential to develop the next generation of biomedical innovators and problem-solvers.
Enhancing Student Motivation, Collaboration, and Inclusivity in CBL Environments
The evolving demands of the biomedical field necessitate educational frameworks that equip students with both deep disciplinary knowledge and the adaptive skills to innovate in novel contexts. Traditional, lecture-based instruction has been the dominant model in engineering education, but there is growing evidence that active learning strategies foster superior competencies. This guide objectively compares Challenge-Based Learning (CBL) with traditional instructional methods within biomedical engineering education, drawing on empirical data to analyze their impact on student motivation, collaboration, and inclusivity. Framed within broader thesis on comparative learning research, this analysis provides researchers, scientists, and drug development professionals with evidence-based insights into effective educational paradigms.
Comparative Analysis of CBL and Traditional Instruction
A foundational study in biotransport education directly compared learning outcomes between students in an inquiry-based CBL environment, designed around the "How People Learn" (HPL) framework, and those in a traditional lecture-based course [22] [45].
Table 1: Comparative Learning Outcomes in a Biotransport Course
| Metric of Comparison | Challenge-Based Learning (HPL) Group | Traditional Lecture Group |
|---|---|---|
| Knowledge Acquisition (Pre/Post-test) | Equivalent gains | Equivalent gains [22] [45] |
| Innovative Problem-Solving | Significantly greater improvement [22] [45] | Less improvement |
| Development of Adaptive Expertise | Strongly facilitated [22] [45] | Less facilitated |
| Primary Skill Focus | Subject knowledge & innovative thinking [22] [45] | Subject knowledge |
The data demonstrates that while both instructional methods are effective for conveying core knowledge, CBL holds a distinct advantage in cultivating the innovative thinking abilities essential for adaptive expertise [22]. Adaptive expertise—the combination of deep subject knowledge and the ability to think innovatively in new contexts—is a critical skill for biomedical engineers tackling unforeseen challenges in research and development [22] [45].
Detailed Experimental Protocols in CBL Research
Protocol 1: The HPL-Based Biotransport Study
This comparative study serves as a model for evaluating pedagogical efficacy in a controlled setting [22] [45].
- Intervention Design: The experimental group was taught a core biomedical engineering course in biotransport using the HPL method. This approach is characterized by its focus on learner-centered environments, knowledge-centeredness, formative assessment, and community building [45].
- Control Design: The control group was taught the same material by the same instructor using traditional didactic lecture methods.
- Outcome Measurement: Student learning was measured in two dimensions. A pre- and post-test assessed knowledge acquisition (domain learning), while a separate instrument assessed the development of innovative problem-solving abilities [22] [45].
- Analysis: HPL and traditional students' test scores were statistically compared to determine significant differences in learning outcomes.
Protocol 2: Bioinstrumentation CBL Implementation
A more recent implementation provides a protocol for integrating CBL into a technical, blended course [16].
- Challenge Scenario: Thirty-nine students were challenged to design, prototype, and test a respiratory or cardiac gating device for radiotherapy, a problem presented in collaboration with an industry partner [16].
- Instructional Model: The CBL framework followed the "Engage, Investigate, and Act" phases. Students worked in teams in a blended format, combining online communication, lab experiments, and in-person activities [16].
- Evaluation Method: The success of the CBL implementation was assessed via an institutional student opinion survey, which gathered data on students' perceptions of their learning, skill development, and the overall experience [16].
Diagram 1: CBL Workflow in Bioinstrumentation Course. This diagram illustrates the experimental protocol and logical flow of the CBL experience, from industry engagement to solution development [16].
The CBL Framework: A Mechanism for Enhancing Engagement and Inclusion
The effectiveness of CBL can be attributed to its structured yet flexible framework, which naturally promotes key engagement and inclusivity drivers.
The Three-Phase CBL Workflow
The canonical CBL model, exemplified by the Apple-derived framework, consists of three iterative phases [56]:
- Engage: Learners use essential questioning to collaboratively define the terms of a real-life challenge. This phase leverages cognitive and identity diversity to ensure the problem is understood from multiple perspectives, fostering intrinsic motivation and establishing personal relevance [56].
- Investigate: Students self-direct their learning and working process, conducting research and analysis to understand the problem and propose a wide variety of solutions. Instructors act as coaches, introducing theoretical concepts as needed. This phase relies on cognitive diversity to fuel innovation [56].
- Act: Students develop, prototype, test, and refine their solution concepts. They implement and evaluate their ideas in a cooperative way, while also reflecting on the learning process. This phase creates a strong sense of belonging and team cohesion [56].
Diagram 2: The Core CBL Cycle. This diagram shows the three-phase Engage, Investigate, and Act framework that structures the CBL process and promotes inclusivity [56].
Drivers of Student Engagement and Inclusivity
Research identifies several key reasons why CBL is more engaging than traditional instruction, which also serve as mechanisms for creating a more inclusive environment [57] [56].
Table 2: Key Engagement Drivers and Their Relationship to Inclusivity in CBL
| Engagement Driver | Impact on Student Motivation | Connection to Diversity & Inclusion (D&I) |
|---|---|---|
| Collaboration with Peers | Students are excited to connect with and learn from diverse teammates, increasing motivation [57]. | Multidisciplinary teams leverage cognitive diversity, teaching students to productively deal with differences and value varied perspectives [56]. |
| Freedom to Create | Students appreciate the freedom to self-direct learning and become creators, not passive recipients [57]. | Empowers students from all backgrounds to contribute their unique ideas and solutions, fostering equity of voice. |
| Real-World Relevance | Students are empowered and motivated by tackling meaningful, tangible problems [57]. | Connects learning to a variety of societal and community contexts, making education relevant to a wider range of student experiences and values. |
| Non-Traditional Learning | Pushing beyond the comfort zone of lectures is ultimately motivating and eye-opening [57]. | Creates an alternative pathway to success for students who may not thrive in traditional, lecture-based competitive environments. |
The Scientist's Toolkit: Research Reagents for CBL Environments
Implementing effective CBL requires a suite of conceptual, technological, and assessment "reagents." The table below details essential components for creating robust CBL research and learning environments.
Table 3: Key "Research Reagents" for CBL Implementation
| Item Name | Type | Function in the CBL Environment |
|---|---|---|
| HPL Framework | Conceptual Model | Provides a pedagogical foundation based on learning science principles to design effective, learner-centered environments [22] [45]. |
| Real-World Challenge | Core Stimulus | Serves as the authentic, relevant problem that drives the learning process, ensuring engagement and contextualizing knowledge [16] [56]. |
| Industry Partner | External Agent | Provides real-world challenges, acts as a stakeholder, and offers feedback, grounding the academic exercise in professional practice [16]. |
| LLM-Based Virtual Patients | Digital Tool | Simulates realistic clinical scenarios for practice of clinical reasoning and communication skills, offering scalable, interactive learning experiences [58]. |
| Collaborative Multidisciplinary Teams | Social Structure | Creates a microcosm of the professional world, enabling peer learning and forcing the integration of diverse knowledge and perspectives to solve complex problems [57] [56]. |
| Formative & Summative Assessment Rubrics | Assessment Tool | Provides criteria for evaluating both the final solution (summative) and the learning process (formative), guiding student effort and measuring competency development [16]. |
The comparative data is clear: while traditional instruction effectively transmits foundational knowledge, Challenge-Based Learning provides a superior framework for developing the innovative problem-solving skills and adaptive expertise required by the modern biomedical sector. The structured yet flexible CBL methodology, centered on real-world challenges and collaborative teamwork, directly enhances student motivation and provides a powerful vehicle for creating inclusive learning environments. For researchers and professionals focused on advancing biomedical innovation, embracing and refining CBL pedagogies is not merely an educational preference but a strategic imperative for cultivating a future workforce capable of tackling complex health challenges.
Optimizing Assessment Techniques for Complex Skills and Competencies
The evolving demands of the biomedical sector necessitate educational frameworks that equip researchers and drug development professionals with robust complex competencies. Challenge-based learning (CBL) has emerged as a significant pedagogical model, shifting the focus from traditional content delivery to experiential, real-world problem-solving. This guide provides a comparative analysis of assessment techniques within CBL and traditional learning (TL) models, drawing on experimental data to evaluate their effectiveness in cultivating and measuring the advanced skills required for modern biomedical research.
Theoretical Foundations and Key Concepts
Challenge-Based Learning (CBL) is a student-centered pedagogical approach that immerses learners in real-world, collaborative problems. In the context of biomedical education, this could involve designing a novel drug delivery system or developing a clinical trial protocol for a new therapeutic. CBL emphasizes the development of transversal competencies such as critical thinking, collaborative work, digital literacy, and problem-solving [5]. The professor's role transforms from a knowledge transmitter to a facilitator and mentor, guiding students through the process of integrating academic content into practical solutions [5] [21].
In contrast, Traditional Learning (TL) models often emphasize lectures and final exams as primary assessment methods, focusing more on content acquisition than practical application [5]. The assessment in TL environments tends to prioritize the "assessment of learning" (AoL), which is summative in nature, whereas CBL creates more opportunities for "assessment for learning" (AfL) and "assessment as learning" (AaL), where students self-regulate their learning [59].
Comparative Analysis of Learning Models: Experimental Data
A quasi-experimental study conducted at the Tecnologico de Monterrey provides robust quantitative data comparing CBL and TL models. The research involved 1705 freshman engineering students, with 57% enrolled in the CBL model and 43% in the traditional previous learning (PL) model, spanning seven semesters [5].
Table 1: Comparative Student Performance in CBL vs. Traditional Models
| Performance Metric | CBL Model | Traditional Learning (PL) Model | Change |
|---|---|---|---|
| Average Final Course Grade | Improved | Baseline | +9.4% |
| Challenge/Project Grade | Similar to TL project grades | Baseline | No significant difference |
| Student Perception (Competency Development) | 71% favorable | Not reported | N/A |
The data reveal that while the CBL model led to a significant improvement in overall course performance, the grades on the CBL challenges themselves were comparable to project grades in the traditional model. This suggests that CBL enhances overall learning outcomes without compromising academic rigor [5].
Beyond general academic performance, specific competency development shows notable differences:
Table 2: Skill Development and Assessment Focus Across Models
| Competency Area | CBL Model Assessment Approach | Traditional Model Assessment Approach |
|---|---|---|
| Problem-Solving | Real-world challenge resolution [5] | Abstract problem sets and exams [5] |
| Collaborative Work | Embedded in methodology; essential for challenge completion [5] | Often secondary or separate from core assessments |
| Critical Thinking & Creativity | Explicitly emphasized and assessed through solution innovation [5] | Less emphasized compared to technical knowledge |
| Self-Efficacy | Developed through iterative, mastery-oriented modules [44] | Less directly fostered in standard curricula |
| Knowledge Acquisition | Applied context; no significant improvement over TL in meta-analysis [60] | Primary focus through lectures and examinations |
Detailed Experimental Protocols and Assessment Methodologies
Protocol 1: Evaluating CBL in Engineering Education
A comprehensive study provides a replicable protocol for comparing CBL and TL [5]:
- Population: 1705 freshman engineering students enrolled in physics courses.
- Intervention Group: CBL model emphasizing disciplinary and transversal competencies through real-world challenges.
- Control Group: Traditional previous learning (PL) model with standard lecture and exam format.
- Duration: Seven semesters (Spring 2018 to Spring 2021).
- Assessment Measures:
- Final exam grades
- Challenge and project report grades
- Final course grades
- Student opinion surveys (n=570) on competency development and problem-solving skills
- Statistical Analysis: Comparative analysis of academic performance metrics across cohorts.
This protocol's longevity and large sample size strengthen its validity, demonstrating CBL's effectiveness in improving overall academic performance while maintaining rigorous assessment standards [5].
Protocol 2: Assessment-as-Learning in Medical Education
A quasi-experimental mixed-methods study explores innovative assessment techniques in biomedical education [59]:
- Population: Second-year preclinical medical students in a cardiovascular system module.
- Intervention: Students created scenario-based multiple-choice questions (MCQs) targeting high cognitive levels.
- Control Group: Students who did not create items but were exposed to the same mock exams.
- Outcome Measures:
- Formative assessment scores
- GPA comparison
- Self-administered questionnaires and focused group discussions
- Results: Item creators showed significantly higher formative scores (34.3 ±10.5 vs. 29.6 ±10.6; p=0.010) and higher GPA (B+ grade: 42.4% vs. 21.7%; p=0.015). The strategy positively correlated with GPAs (rs=0.74) and number of developed items (rs=0.39) [59].
This "assessment as learning" approach demonstrates how active engagement in assessment creation can enhance knowledge integration and clinical reasoning skills essential for drug development professionals.
Protocol 3: Competency-Based vs. Traditional Statistics Education
A pretest-posttest study compared competency-based and traditional learning in statistics education for health disciplines [44]:
- Population: 20 nursing and interdisciplinary undergraduate students in introductory statistics courses.
- Intervention Group: Competency-based learning (CBL) course with self-paced modules, pretests/posttests, interactive exercises, and application assignments.
- Control Group: Traditional learning course with Zoom classes, recorded lectures, and active learning opportunities.
- Measures:
- Statistical knowledge assessment (hypothesis testing, central tendency, research design)
- Current Statistics Self-Efficacy (CSSE) scale
- Self-Efficacy to Learn Statistics (SELS) scale
- Results: Both groups showed significant knowledge improvement in specific areas (hypothesis testing p=.02, measures of central tendency p=.001, research design p=.001), with no significant difference in overall mean scores between groups (p=.10). Both groups showed significant improvement in self-efficacy measures, with students describing competency-based learning as "at least as beneficial as traditional learning for studying statistics while allowing more flexibility to repeat content until it was mastered" [44].
Visualization of Comparative Assessment Frameworks
The following diagram illustrates the key structural differences and assessment focus between Traditional Learning and Challenge-Based Learning models, highlighting their distinct pathways to competency development.
The Scientist's Toolkit: Research Reagent Solutions for Educational Assessment
Implementing effective assessment strategies requires specific methodological "reagents" tailored to educational research. The following table details essential components for rigorous evaluation of complex skill development.
Table 3: Essential Methodological Components for Assessing Complex Skills
| Research Component | Function in Assessment | Exemplary Applications |
|---|---|---|
| Quasi-Experimental Design | Compares intervention and control groups when random assignment isn't feasible | Comparing CBL vs. traditional cohorts across multiple semesters [5] |
| Mixed-Methods Approach | Combines quantitative metrics with qualitative insights for comprehensive evaluation | Integrating academic performance data with student perception surveys [5] [59] |
| Current Statistics Self-Efficacy (CSSE) Scale | Measures confidence in applying statistical knowledge | Evaluating self-efficacy gains in competency-based statistics courses [44] |
| Scenario-Based MCQ Development | Assesses higher-order cognitive skills and clinical reasoning | Engaging preclinical students in creating assessment items [59] |
| Facial Expression Recognition Technology | Provides objective, real-time feedback on student engagement and comprehension | Capturing emotional responses to adjust teaching strategies [61] |
| Augmented/Mixed Reality (AR/MR) | Creates immersive simulation environments for skill practice and assessment | Medical skills training with improved performance scores and reduced failure rates [60] |
The comparative analysis of assessment techniques reveals that Challenge-Based Learning offers distinct advantages for developing complex competencies essential for biomedical researchers and drug development professionals. While traditional assessments effectively measure knowledge acquisition, CBL and its associated assessment methodologies—including authentic challenge resolution, assessment-as-learning strategies, and technologically-enhanced simulations—provide more robust frameworks for cultivating and evaluating the integrative problem-solving, collaboration, and adaptive thinking skills required to navigate the complexities of modern therapeutic development.
The experimental data consistently demonstrate that CBL environments can enhance overall academic performance while fostering critical transversal competencies. For organizations seeking to optimize talent development in the biomedical sector, integrating these innovative assessment techniques represents a strategic opportunity to bridge the gap between theoretical knowledge and real-world application.
Resource Management and Faculty Development for Sustainable CBL Programs
Challenge-based learning (CBL) and traditional instructional methods represent two distinct approaches to biomedical engineering education. While traditional methods typically employ structured lectures and standardized laboratory exercises, CBL engages students in collaborative efforts to solve complex, real-world problems [16]. This pedagogical shift demands significant changes in resource allocation and faculty roles, moving from knowledge dissemination to facilitation of student-directed inquiry. The growing body of research comparing these approaches indicates that while both can effectively transmit core disciplinary knowledge, they differ substantially in their development of students' innovative capacities and adaptive expertise [22].
This comparison guide examines the empirical evidence supporting CBL implementation in biomedical engineering contexts, with particular focus on resource implications and faculty development requirements. The analysis synthesizes findings from controlled studies and implementation reports to provide educators and administrators with evidence-based recommendations for developing sustainable CBL programs. Rather than suggesting a complete replacement of traditional methods, this guide identifies specific contexts where CBL's resource-intensive nature yields maximal educational benefit, particularly in developing competencies essential for biomedical innovation and professional practice.
Comparative Experimental Data: Learning Outcomes and Resource Investment
Quantitative Learning Outcomes in Biotransport Education
A controlled comparative study examined student learning in a biomedical engineering biotransport course taught through both CBL (referred to as How People Learn or HPL method) and traditional lecture-based instruction [22]. The study employed pre- and post-test measurements to assess knowledge acquisition and innovative thinking abilities across both instructional formats. The results provide compelling evidence for the distinctive benefits of each approach, summarized in Table 1.
Table 1: Comparative Learning Outcomes in Biomedical Engineering Education
| Assessment Metric | CBL/HPL Method | Traditional Instruction | Comparative Significance |
|---|---|---|---|
| Knowledge Gains | Equivalent | Equivalent | No statistically significant difference |
| Innovative Problem-Solving | Significantly greater improvement | Standard improvement | CBL students demonstrated significantly greater enhancement (p<0.05) |
| Adaptive Expertise | Stronger development | Limited development | CBL better prepares students for novel problem contexts |
| Content Mastery | Solid foundation | Solid foundation | Both approaches effectively deliver core biotransport concepts |
Resource Implementation and Operational Requirements
The operational implementation of CBL programs necessitates distinct resource allocation compared to traditional instruction. Research examining CBL in an undergraduate bioinstrumentation course reveals specific operational requirements and their associated resource implications, detailed in Table 2.
Table 2: Resource Management Comparison for CBL vs. Traditional Programs
| Resource Category | CBL Implementation | Traditional Program | Implementation Notes |
|---|---|---|---|
| Faculty Time | Substantial increase in planning and tutoring | Standard preparation and delivery | CBL requires approximately 30-50% more faculty time [16] |
| Industry Partnership | Essential for authentic challenges | Optional enhancement | CBL necessitates ongoing industry collaboration for challenge design |
| Student Support | Continuous mentoring and feedback | Scheduled office hours | CBL demands more frequent and intensive student-faculty interaction |
| Physical Resources | Flexible learning spaces | Standard classrooms/labs | CBL benefits from adaptable environments for collaborative work |
| Assessment Methods | Multifaceted (rubrics, portfolios, presentations) | Traditional exams and quizzes | CBL assessment is more labor-intensive but provides richer data |
Experimental Protocols and Methodologies
CBL Intervention Design in Bioinstrumentation
A 2024 study implemented CBL in a third-year bioinstrumentation course for biomedical engineering students, providing a detailed protocol for CBL integration [16]. The methodology encompassed several key phases:
Challenge Formulation Phase: Students were presented with an authentic, industry-relevant challenge: designing, prototyping, and testing a respiratory or cardiac gating device for radiotherapy applications. This challenge was developed in collaboration with an industrial partner to ensure real-world relevance and appropriate complexity level for undergraduate students [16].
Team Formation and Structured Inquiry: Thirty-nine students enrolled across two sections formed fourteen teams. The CBL framework followed a structured progression: (1) big idea identification (medical device innovation), (2) essential question formulation, (3) specific challenge definition, (4) solution development through prototyping, (5) implementation and testing, and (6) results dissemination [16].
Blended Learning Integration: The course combined online communication, laboratory experiments, and in-person CBL activities. This multimodal approach allowed students to access theoretical content asynchronously while dedicating face-to-face time to collaborative problem-solving and mentorship.
Assessment Protocol: Student learning was evaluated through multiple measures including project rubrics, design documentation, prototype functionality tests, and final presentations. Additionally, students completed an institutional opinion survey to assess their learning experience and skill development.
Comparative Research Methodology
The seminal 2007 comparative study employed a rigorous experimental design to evaluate learning outcomes across instructional methods [22]:
Participant Groups: The study compared an intervention group taught using CBL/HPL principles with a control group taught through traditional didactic lecture methods within the same biotransport course.
Learning Assessment: Researchers developed specialized instruments to measure two distinct dimensions of learning: (1) knowledge acquisition within the biotransport domain, measured through standardized content tests; and (2) innovative problem-solving abilities, assessed through tasks requiring transfer of knowledge to novel contexts.
Measurement Timeline: Pre-test assessments established baseline knowledge and problem-solving capabilities at the beginning of the course. Identical post-test assessments measured gains in both dimensions after instructional intervention.
Control Variables: The study maintained consistency across groups in core content coverage, instructor expertise, and total instructional time, isolating the instructional method as the primary variable.
Visualization of CBL Implementation Framework
CBL Instructional Workflow
The CBL framework follows a structured progression from initial engagement to solution implementation. This workflow transforms traditional educational dynamics by creating iterative cycles of inquiry and refinement, as visualized below:
Resource Management Ecosystem
Sustainable CBL implementation requires a coordinated ecosystem of institutional support, faculty development, and physical resources. This ecosystem demands strategic investment distinct from traditional program support structures:
Successful CBL implementation requires specific "research reagents" - the essential resources and supports that enable effective program execution. These components represent the foundational elements necessary for creating authentic, impactful learning experiences in biomedical engineering education.
Table 3: Essential Resource Solutions for CBL Implementation
| Resource Category | Specific Components | Function in CBL Ecosystem |
|---|---|---|
| Trained Faculty | CBL pedagogy training; mentorship models; interdisciplinary collaboration skills | Facilitates student-directed inquiry; provides appropriate scaffolding; guides collaborative problem-solving [16] |
| Industry Partnerships | Challenge co-design; authentic context; professional feedback; real-world validation | Ensures relevance of challenges; connects academic learning to professional practice; provides technical validation [16] |
| Physical Infrastructure | Prototyping facilities; collaborative workspaces; digital collaboration platforms | Supports hands-on solution development; enables team-based work; facilitates documentation and communication |
| Assessment Tools | Multidimensional rubrics; portfolio systems; peer evaluation mechanisms | Captures complex learning outcomes; documents progressive skill development; encourages reflective practice [16] |
| Administrative Systems | Flexible scheduling; interdisciplinary course structures; resource allocation models | Enables adaptation to project timelines; supports cross-disciplinary collaboration; ensures sustainable resource provision [16] |
Discussion: Strategic Implementation for Sustainable CBL Programs
The comparative evidence indicates that CBL and traditional instructional methods yield equivalent knowledge gains but differ significantly in their development of innovative thinking capabilities [22]. This distinction carries important implications for resource allocation and faculty development in biomedical engineering programs. The strategic integration of CBL elements into traditionally structured curricula may offer a balanced approach that preserves content coverage while enhancing innovation capacity.
Faculty development represents perhaps the most critical investment for sustainable CBL programs. The transition from traditional instruction to CBL facilitation requires significant pedagogical shifts and time commitments [16]. Effective CBL faculty must master the art of guided inquiry without directive problem-solving, develop assessment strategies for complex project-based work, and manage the dynamic uncertainties of open-ended challenges. These competencies do not develop spontaneously but require intentional, supported development programs.
Resource efficiency remains a legitimate concern in CBL implementation. Evidence suggests that CBL requires substantially more faculty time for planning, student tutoring, and maintaining industry partnerships [16]. However, the educational return on this investment manifests in students' enhanced adaptive expertise and innovative capacities - competencies increasingly demanded in evolving biomedical engineering fields. Strategic implementation may involve targeting specific courses or modules where CBL's benefits align most closely with learning objectives, rather than wholesale curriculum conversion.
The decision between CBL and traditional approaches should be guided by specific program goals rather than assumed superiority of either method. Traditional instruction demonstrates efficiency in building foundational knowledge, while CBL excels at developing transferable problem-solving frameworks. Future research should explore hybrid models that strategically blend both approaches to maximize their respective strengths while managing resource constraints.
Comparative Analysis of Learning Outcomes: Validating CBL vs. Traditional Methods in Biomedicine
In biomedical education, a shift from traditional, lecture-based instruction towards challenge-based learning (CBL) is underway. This guide provides a quantitative comparison of these pedagogical approaches, focusing on core metrics of exam performance, knowledge retention, and skill acquisition to inform curriculum design for training the next generation of scientists and drug development professionals.
The table below summarizes key quantitative findings from a comparative study of challenge-based and traditional instruction in a biomedical engineering biotransport course.
| Metric Category | Traditional Instruction | Challenge-Based Instruction (HPL) | Key Implication |
|---|---|---|---|
| Knowledge Gain (Post-test Score) | Equivalent significant gains | Equivalent significant gains [22] | Both methods are effective for foundational knowledge transfer. |
| Innovative Problem-Solving | Standard improvement | Significantly greater improvement [22] | CBL better develops adaptive expertise for novel challenges. |
| Primary Advantage | Efficient content delivery | Cultivates innovative thinking and application [22] | Aligns with modern workforce needs for flexibility and innovation. |
Detailed Experimental Analysis
Study Design and Protocol
A comparative study was designed to evaluate the efficacy of challenge-based instruction against traditional methods in an undergraduate biomedical engineering course [22].
- Intervention Group: The experimental group was taught using the "How People Learn" (HPL) framework, a challenge-based model. Instruction was designed around iterative problem-solving of complex, real-world challenges [22] [31].
- Control Group: The control group was taught the same biotransport content through traditional, didactic lecture methods [22].
- Measurement Tools: Student learning was measured using a pre/post-test assessment designed to evaluate two distinct dimensions [22]:
- Domain Knowledge Acquisition: Measured using standardized test questions on core biotransport concepts.
- Innovative Problem-Solving Ability: Assessed through tasks requiring students to adapt and apply knowledge to novel problems, measuring the development of adaptive expertise (AE) [22].
Quantitative Results and Data Interpretation
Analysis of the pre- and post-test data revealed critical distinctions between the two instructional methods [22]:
- Exam Performance (Knowledge Acquisition): Both student groups demonstrated statistically equivalent and significant gains in their knowledge of core biotransport concepts [22]. This indicates that the challenge-based method did not compromise the foundational learning of standard curriculum material.
- Skill Acquisition (Adaptive Expertise): The HPL group demonstrated significantly greater improvement in their innovative thinking abilities compared to the traditional group [22]. This key finding shows that the CBL approach was more effective at helping students develop adaptive expertise—the capacity to transfer knowledge and innovate in unfamiliar situations.
Methodologies and Measurement Protocols
Core Quantitative Metrics Explained
Effective training evaluation relies on specific, measurable metrics. Below is a breakdown of common quantitative metrics used to assess training outcomes, applicable from corporate training to biomedical education [62] [63].
| Metric | Definition | Measurement Method | Relevance |
|---|---|---|---|
| Proficiency Scores | Level of skill or knowledge acquired post-training [62]. | Standardized exams, practical tests, rubric-graded assignments [62]. | Directly measures achievement of learning objectives. |
| Time-to-Competency | Duration for a learner to become proficient in a new skill [62]. | Track time from training start to successful demonstration of a skill or passing a performance check. | Measures efficiency of training; reduced time indicates higher effectiveness. |
| Error Rates | Frequency of mistakes made during task performance [62]. | Analysis of errors in simulations, hands-on exercises, or on-the-job assessments [62]. | Indicates practical understanding and areas needing improvement. |
| Retention Percentages | Proportion of information retained over time [62]. | Delayed post-testing (e.g., follow-up tests weeks or months after training) [62]. | Assesses long-term knowledge retention, crucial for complex fields. |
| Training ROI | Monetary benefit of training compared to its cost [63]. | Calculation: (Benefits - Costs) / Costs * 100 [63]. |
Justifies training expenditures by linking them to financial or performance outcomes. |
Assessment Methods for Knowledge and Skills
Different learning outcomes require tailored assessment strategies.
Assessing Skill Acquisition: Effective methods focus on application and performance [62].
- Simulations: Replicate real-world scenarios in a controlled environment to assess skill application [62].
- Hands-on Exercises & On-the-Job Assessments: Require learners to demonstrate abilities through practical tasks or during actual work [62].
- Role-Playing: Evaluates interpersonal skills, decision-making, and complex professional behaviors [62].
Assessing Knowledge Retention: These methods gauge how well information is remembered over time [62] [64].
- Quizzes and Tests: Standard assessments for memory and understanding [62].
- Spaced Repetition: A technique involving reviewing information at increasing intervals to enhance long-term retention and combat the "forgetting curve" [62].
- Follow-up Surveys & Knowledge Audits: Post-training surveys and periodic audits can assess how much information employees remember and apply, identifying gaps [62] [64].
Visualizing the Challenge-Based Learning Workflow
The following diagram illustrates the core iterative process of Challenge-Based Learning, which drives the development of adaptive expertise.
The Scientist's Toolkit: Essential Reagents for Educational Research
For researchers seeking to replicate or build upon this comparative research, the table below details key methodological components.
| Research Reagent / Tool | Function in Experiment |
|---|---|
| Pre/Post-Test Instrument | A validated assessment tool to quantitatively measure gains in both domain-specific knowledge and innovative problem-solving abilities [22]. |
| HPL (How People Learn) Framework | The structured, challenge-based instructional protocol used as the intervention. It creates a learner-centered environment focused on in-depth inquiry [22]. |
| Traditional Lecture Curriculum | The standard, didactic instruction protocol used as the control for establishing a baseline of learning outcomes [22]. |
| Complex, Open-Ended Challenges | The core "reagent" for the intervention group. These are real-world, multifaceted problems with no single correct answer, designed to trigger iterative problem-solving [22]. |
| Coding Rubrics for Innovative Thinking | Standardized scoring guides used by blinded assessors to quantify qualitative aspects of problem-solving, such as solution novelty and flexibility in thinking [22]. |
Quantitative data demonstrates that while challenge-based and traditional instruction are equally effective for foundational knowledge acquisition, CBL holds a distinct advantage in cultivating the critical skill of adaptive expertise. For biomedical training programs aiming to develop innovators capable of tackling novel problems in drug development and research, integrating challenge-based modules offers a data-driven strategy to enhance training outcomes.
The evolution of biomedical engineering education has prompted a significant shift from traditional, lecture-based instruction toward innovative pedagogical strategies that emphasize real-world problem-solving. Among these, Challenge-Based Learning (CBL) has emerged as a prominent experiential approach, positioning students to collaboratively tackle authentic, complex problems [5] [16]. This guide provides a comparative analysis of CBL against traditional learning models, focusing on qualitative measures including student feedback, critical thinking development, and innovation capabilities. Framed within broader thesis research on biomedical instruction, this analysis synthesizes experimental data and implementation methodologies to offer researchers and professionals an evidence-based perspective on these educational frameworks.
Methodological Protocols in CBL Research
Core CBL Implementation Framework
The Tec21 educational model, developed by Tecnologico de Monterrey, represents a systematic implementation of CBL in engineering education. This model is structured around three foundational pillars: (1) flexible, personalized academic programs; (2) CBL as the central pedagogical approach; and (3) inspirational professors who create appropriate learning environments [16]. In practice, CBL involves students working with stakeholders to define authentic, relevant challenges from their environment, then collaborating to develop viable solutions [16].
Comparative Research Design
Studies evaluating CBL effectiveness typically employ quasi-experimental designs comparing outcomes between CBL and traditional instruction cohorts. One comprehensive investigation analyzed 1,705 freshman engineering students across seven semesters, with 57% enrolled in the CBL model and 43% in the previous traditional learning (PL) model [5]. This longitudinal approach allowed researchers to measure academic performance, competency development, and student perceptions across different instructional methodologies.
Table 1: Key Experimental Protocols in CBL Research
| Study Component | Protocol Description | Data Collection Methods |
|---|---|---|
| Participant Recruitment | Natural grouping through existing course enrollment; comparison of CBL vs. traditional cohorts | Institutional enrollment data; demographic information [5] |
| Intervention Implementation | CBL model emphasizing real-world challenges with industry partners; PL model using standard lecture/project approach | Curriculum documentation; challenge design specifications [5] [16] |
| Performance Assessment | Measurement of knowledge gains through exams; evaluation of applied skills through projects/challenges | Final exam scores; challenge/project reports; final course grades [5] |
| Qualitative Data Collection | Perception surveys and focus groups to gauge student experiences | Likert-scale surveys; open-ended questions; structured interviews [5] [65] |
| Competency Evaluation | Assessment of disciplinary and transversal competencies development | Rubrics evaluating problem-solving, critical thinking, collaboration [5] [66] |
Comparative Analysis of Educational Outcomes
Academic Performance Metrics
Comparative studies reveal distinct performance patterns between CBL and traditional approaches. Research with 1,705 engineering students showed that the overall student performance, measured by average final course grades, improved by 9.4% in the CBL model compared to the traditional PL model [5]. Interestingly, while overall performance was higher in CBL environments, challenge average grades in CBL were similar to project average grades in traditional settings, suggesting different skill emphasis between the approaches [5].
Table 2: Academic Performance Comparison (CBL vs. Traditional Instruction)
| Performance Metric | CBL Model Results | Traditional Model Results | Comparative Advantage |
|---|---|---|---|
| Average Final Course Grade | 9.4% improvement | Baseline | CBL superior [5] |
| Challenge/Project Grades | Similar average grades | Similar average grades | Equivalent [5] |
| Knowledge Gains | Significant improvements | Significant improvements | Equivalent [31] |
| Innovative Thinking | Significantly greater improvement | Moderate improvement | CBL superior [31] |
| Problem-Solving Transfer | Strong framework development | Limited transfer capability | CBL superior [31] |
Critical Thinking and Innovation Capabilities
CBL demonstrates pronounced advantages in developing higher-order thinking skills. Students in challenge-based environments show significantly greater improvement in innovative thinking abilities compared to traditionally instructed peers, despite equivalent knowledge gains in content areas [31]. This innovation advantage stems from CBL's emphasis on creative critical thinking - the integration of creative idea generation with critical analysis of feasibility and real-world constraints [66].
The development of adaptive expertise represents another CBL strength. Research indicates that CBL promotes the formation of transferable frameworks and enhanced confidence for engineering problem-solving, preparing students to tackle novel challenges beyond specific course content [31]. This manifests particularly in biomedical engineering contexts where students must design, prototype, and test medical devices in response to authentic clinical needs [16] [67].
Student Feedback and Perception Analysis
Quantitative Perception Data
Systematic collection of student feedback provides crucial insights into CBL effectiveness. In opinion surveys administered to 570 students across two years, 71% expressed favorable perceptions of the CBL model regarding competency development and problem-solving abilities [5]. Survey implementation in bioinstrumentation courses revealed that students strongly agreed that CBL challenged them to learn new concepts and develop new skills, despite the increased cognitive demand [16].
Table 3: Student Perception Survey Results
| Perception Dimension | Favorable Rating | Neutral Rating | Unfavorable Rating | Sample Size |
|---|---|---|---|---|
| Competency Development | 71% | 21% | 8% | 570 students [5] |
| Problem-Solving Skills | 71% | 21% | 8% | 570 students [5] |
| New Concept Learning | Strong agreement | Moderate agreement | Limited agreement | 39 students [16] |
| Skill Development | Strong agreement | Moderate agreement | Limited agreement | 39 students [16] |
| Student-Lecturer Interaction | Positive rating | Neutral rating | Negative rating | 39 students [16] |
Qualitative Feedback Themes
Analysis of open-ended student responses identifies several recurring themes in CBL experiences. Students report increased engagement and motivation when tackling authentic challenges with real-world relevance [5] [16]. The opportunity to address actual problems from companies or organizations provides meaningful context that reinforces academic content and practical application [5].
The development of professional skills emerges as another prominent theme. Students recognize value in cultivating collaborative project management abilities, communication skills, and digital literacy through CBL experiences [66]. These competencies align closely with employer priorities and professional requirements in biomedical fields.
Some challenges noted in student feedback include the substantial time investment required for CBL implementation and the need for adjustment to increased ambiguity compared to structured traditional approaches [16]. Students occasionally report initial discomfort with the reduced direct guidance characteristic of CBL environments.
The CBL Experimental Workflow
The implementation of Challenge-Based Learning follows a structured yet flexible workflow that distinguishes it from traditional educational approaches. The process integrates specific phases that promote iterative development and authentic problem-solving capabilities.
Essential Research Reagents for CBL Implementation
Table 4: Research Reagents for CBL Implementation and Evaluation
| Reagent Category | Specific Tools & Methods | Function in CBL Research |
|---|---|---|
| Assessment Instruments | Likert-scale surveys; Rubrics; Focus group protocols; Performance evaluations | Measure learning outcomes, student perceptions, and competency development [5] [65] |
| Learning Analytics Platforms | Learning management systems; Grade tracking databases; Student engagement metrics | Quantify academic performance and participation patterns [5] |
| Challenge Design Resources | Industry partnership frameworks; Clinical problem databases; Prototyping equipment | Create authentic, relevant challenges with real-world application [16] [67] |
| Collaboration Tools | Team communication platforms; Project management software; Document sharing systems | Facilitate collaborative problem-solving and project coordination [16] [66] |
| Feedback Mechanisms | Structured feedback models; Multi-source feedback protocols; Reflection guides | Support continuous improvement and self-regulated learning [65] [68] |
Discussion and Synthesis
Interpretation of Comparative Outcomes
The evidence indicates that CBL and traditional instruction each offer distinct advantages depending on educational objectives. While traditional methods remain effective for content transmission, CBL demonstrates superior performance in developing innovative capabilities, adaptive expertise, and professional competencies [5] [31]. The 9.4% improvement in overall student performance within CBL environments suggests that the integration of physics, math, and computing concepts through real-life challenges strengthens student engagement and learning outcomes [5].
The development of critical thinking in CBL deserves particular emphasis. This approach uniquely bridges the gap between creative idea generation and critical analysis, producing graduates capable of both innovating and implementing practical solutions [66] [69]. This combined "crea-critical" skill set aligns precisely with workforce needs in biomedical fields, where technical expertise must be coupled with innovative capacity [66] [69].
Implementation Considerations and Challenges
Successful CBL implementation requires addressing several practical challenges. The resource intensity of CBL presents logistical constraints, with substantial time investments needed for planning, student tutoring, and maintaining communication with industry partners [16]. Additionally, the transition from traditional instruction requires significant faculty development to shift from content-delivery roles toward facilitation and mentorship [21].
The assessment complexity in CBL environments also merits attention. While quantitative metrics like exam scores remain important, comprehensive evaluation requires qualitative measures of critical thinking, innovation capabilities, and professional competencies [5] [65]. Developing valid, reliable assessment tools for these complex skills represents an ongoing challenge in educational research.
This comparative analysis demonstrates that Challenge-Based Learning offers distinct advantages over traditional instruction for developing critical thinking, innovation capabilities, and professional competencies in biomedical education. The favorable student feedback, coupled with demonstrated performance improvements and enhanced innovative thinking, positions CBL as a valuable pedagogical approach for preparing students to address complex challenges in biomedical fields. Future research should further refine assessment methodologies and explore hybrid models that leverage the strengths of both CBL and traditional approaches to optimize biomedical education outcomes.
Empirical Evidence from Recent Studies in Biomedical Education and Training
Biomedical education faces the dual challenge of keeping pace with rapid technological advancements and preparing students for the complexities of modern healthcare environments. In response, active learning methodologies such as Challenge-Based Learning (CBL) have emerged as promising alternatives to traditional lecture-based instruction. This guide provides an objective comparison of these pedagogical approaches, synthesizing empirical evidence from recent studies to inform educators and curriculum developers in biomedical sciences.
Methodological Approaches in Biomedical Education
Challenge-Based Learning (CBL) Framework
CBL is an experiential learning approach where students collaborate to develop solutions to real-world, socially relevant challenges [16]. The process typically follows a structured framework:
- Big Idea Identification: Students explore a broad concept with multiple potential investigation pathways
- Essential Question Formulation: Learners identify what they need to know to address the challenge
- Challenge Definition: Students create a specific, actionable challenge statement
- Solution Development: Teams design, prototype, and test their solutions
- Implementation and Evaluation: Students implement their solutions and assess effectiveness
- Results Publishing: Findings are documented and shared with a larger audience [16]
In a study conducted at Tecnologico de Monterrey, CBL was implemented in a bioinstrumentation course where 39 students worked in 14 teams to design, prototype, and test respiratory or cardiac gating devices for radiotherapy in collaboration with industry partners [16].
Traditional Instruction Model
Traditional biomedical education typically employs lecture-based learning (LBL) characterized by:
- Teacher-centered knowledge transmission
- Structured curriculum delivery through didactic lectures
- Passive student reception of information
- Individual assessment through standardized examinations
- Theoretical emphasis with limited practical application [25]
Blended Learning Approaches
Hybrid models combining digital education with traditional methods have also been investigated. A 2024 study on evidence-based medicine education implemented a blended approach incorporating "internet plus" and flipped classroom strategies where students reviewed materials before class and used classroom time for interactive problem-solving [25].
Comparative Experimental Data
Table 1: Knowledge Acquisition Outcomes Across Instructional Methods
| Study | Instructional Method | Sample Size | Knowledge Gain | Statistical Significance |
|---|---|---|---|---|
| Martin et al. (2007) [22] | CBL vs. Traditional | 131 students | Equivalent gains | p > 0.05 (NSD) |
| Tang et al. (2024) [46] | CBL in Nursing | 94 students | Significant improvement | p < 0.0001 |
| Blended EBM Study (2024) [25] | Blended vs. Traditional | 76 students | BL: 4.05±4.26 vs TL: 2.00±2.85 | p = 0.022 |
| Systematic Review (2020) [70] | Blended vs. Traditional | 9,943 participants | SMD: 1.07 (0.85-1.28) | p < 0.001 |
Table 2: Skill Development and Higher-Order Thinking Outcomes
| Competency Domain | CBL Performance | Traditional Instruction | Statistical Significance |
|---|---|---|---|
| Innovative Thinking [22] | Significant improvement | Limited improvement | p < 0.05 |
| Multidisciplinary Collaboration [46] | Significant enhancement (10.78±7.09) | Minimal change | p < 0.0001 |
| Clinical Skill Acquisition [27] | Superior outcomes | Moderate outcomes | p < 0.00001 |
| Case Analysis Ability [27] | Significantly stronger | Limited development | p < 0.00001 |
| Learning Satisfaction [25] | Higher ratings | Lower ratings | p = 0.001 |
Table 3: Implementation Considerations and Resource Requirements
| Factor | CBL Approach | Traditional Approach |
|---|---|---|
| Faculty Time | Substantial increase in planning and tutoring [16] | Moderate preparation requirements |
| Industry Partnership | Essential for authentic challenges [16] | Optional or non-existent |
| Student Support | Multiple levels required throughout process [16] | Primarily content delivery |
| Assessment Methods | Complex rubrics, presentations, prototypes [16] | Standardized tests and examinations |
| Infrastructure Needs | Prototyping facilities, collaboration spaces [67] | Traditional classroom settings |
CBL Implementation Workflow
The following diagram illustrates the typical workflow for implementing Challenge-Based Learning in biomedical education:
Table 4: Key Implementation Resources for CBL in Biomedical Education
| Resource Category | Specific Tools/Methods | Function in CBL Implementation |
|---|---|---|
| AI-Powered Research Tools [71] | DeepSeek, ChatGPT, Kimi | Assist literature review, concept clarification, and research summarization |
| Collaboration Assessment [46] | Adapted Collaboration Scale (Masse et al.) | Measure multidisciplinary collaboration competencies |
| Prototyping Resources [16] [67] | 3D printers, electronic components, simulation software | Create functional prototypes of biomedical devices |
| Industry Partnership Frameworks [16] [71] | Structured collaboration protocols, IP agreements | Facilitate authentic challenge design and mentorship |
| Assessment Rubrics [16] | Multidimensional evaluation tools | Assess both process and outcomes in CBL projects |
Discussion and Implications
The empirical evidence demonstrates that CBL approaches produce equivalent content knowledge acquisition while significantly enhancing innovative thinking abilities compared to traditional instruction [22]. This suggests that CBL effectively develops adaptive expertise - the capacity to apply knowledge creatively in novel situations - which is particularly valuable in rapidly evolving biomedical fields.
The NICE strategy (New frontier, Integrity, Critical and creative thinking, Engagement) represents a comprehensive framework that incorporates CBL elements to address multiple challenges in biomedical education simultaneously [71]. This approach explicitly develops both technical competencies and ethical reasoning capabilities essential for biomedical professionals.
Implementation success factors identified across studies include:
- Adequate institutional support for resource-intensive active learning methods
- Faculty development to transition from knowledge-deliverer to learning-facilitator
- Authentic assessment strategies aligned with CBL processes and outcomes
- Structured industry partnerships that provide relevant challenges and mentorship [16] [71]
The synthesis of recent empirical studies indicates that Challenge-Based Learning consistently enhances higher-order thinking skills, innovation capabilities, and professional competencies compared to traditional instructional methods in biomedical education, while maintaining equivalent content knowledge acquisition. These findings support the strategic integration of CBL and blended approaches into biomedical curricula to better prepare students for complex, interdisciplinary challenges in contemporary healthcare and research environments. Future research should investigate long-term outcomes of CBL graduates and determine optimal implementation scales across diverse institutional contexts.
Long-Term Impacts on Career Readiness and Contributions to Drug Development
This guide objectively compares the long-term career preparedness and potential for impact in drug development of graduates from Challenge-Based Learning (CBL) environments versus those from Traditional Instructional models within biomedical education.
Quantitative Comparison of Educational Outcomes
The table below summarizes key experimental data from comparative studies, highlighting the distinct strengths of each pedagogical approach.
| Metric of Comparison | Challenge-Based Learning (CBL) / Active Learning | Traditional Instruction | Research Context |
|---|---|---|---|
| Knowledge Acquisition | Equivalent gains in domain-specific knowledge [22] [23] | Equivalent gains in domain-specific knowledge [22] [23] | Biomedical Engineering (Biotransport course) [22] [23] |
| Innovative Problem-Solving | Significantly greater improvement in innovative thinking and problem-solving abilities [22] [23] | Standard improvement | Biomedical Engineering (Biotransport course) [22] [23] |
| Self-Efficacy | Increase in self-efficacy scores, particularly for female students [72] | Lesser increase in self-efficacy [72] | Medical Education (Haematology course) [72] |
| Academic Performance | Increase in academic scores [72] | Standard academic performance [72] | Medical Education (Haematology course) [72] |
| Skill Transfer & Employability | 90% of students reported improved employability and development of transferable skills (e.g., communication, teamwork) [43] | Not directly measured, but implied to be less focused | Biomedical Sciences (Clinical simulation) [43] |
| Key Differentiator | Develops Adaptive Expertise (AE): A combination of core knowledge and the ability to apply it innovatively in new contexts [22] [21] | Focuses primarily on foundational knowledge acquisition | Synthesis of multiple studies [22] [21] [73] |
Detailed Experimental Protocols
The data in the comparison table is derived from rigorously designed studies. The methodologies for two key experiments are detailed below.
Protocol 1: Comparing Adaptive Expertise in Biotransport
This foundational study directly compared CBL (framed as How People Learn or HPL instruction) with traditional lectures in a core engineering course [22] [23].
- Objective: To identify instructional methods that facilitate the early development of adaptive expertise (AE) in undergraduate biomedical engineering students. AE requires both solid subject knowledge and the ability to think innovatively in new contexts [22] [23].
- Intervention Design:
- CBL/HPL Group: The intervention group was taught using an inquiry-based method following the National Research Council's "How People Learn" principles. This approach is student-centered and emphasizes deep understanding and application [22] [23].
- Control Group: The control group was taught the same content in biotransport through traditional didactic lecture methods [22] [23].
- Duration: The study spanned a full core course in biotransport [22] [23].
- Measures and Tools:
- Data Analysis: HPL and traditional students' test scores were statistically compared to determine significant differences in learning outcomes [22] [23].
Protocol 2: Evaluating Self-Efficacy and Performance in Haematology
This quasi-experimental study investigated the impact of a flipped learning classroom (a form of active learning) versus traditional instruction on medical students [72].
- Objective: To investigate the impact of flipped learning versus traditional instruction on medical students' academic performance and self-efficacy in a haematology course, and to examine gender differences [72].
- Intervention Design:
- Duration: The experiment was conducted over a 10-week haematology course [72].
- Participants: 86 third-year medical students (46 males, 40 females) were assigned to either the flipped learning group (n=41) or the traditional lecture group (n=45) [72].
- Measures and Tools:
- Data Analysis: Data were analyzed using descriptive statistics and t-tests to compare within-group and between-group differences [72].
Educational Pathways to Drug Development Competencies
The following diagram illustrates the conceptual link between educational models and the development of key competencies for drug development careers.
The Scientist's Toolkit: Key Reagents for Educational Research
The table below details essential "research reagents"—core components and methods—used in designing and evaluating modern biomedical educational experiments.
| Tool or Solution | Function in Educational Research |
|---|---|
| Real-World Clinical Scenarios | Serves as the authentic "challenge" in CBL, requiring students to apply knowledge to realistic, complex problems in a safe environment (e.g., simulated patient consultations, process improvement in hospitals) [43] [73]. |
| Structured Debriefing & Feedback | A critical reagent for solidifying learning. This facilitated reflection after simulation or project work allows students to analyze their performance, correct errors, and reinforce correct practices [74]. |
| Transdisciplinary Teaching Teams | A catalyst for complex learning. Combining faculty from biomedical engineering, industrial engineering, and clinical practice provides students with integrated knowledge and models collaborative problem-solving [73]. |
| Pre-/Post-Intervention Assessments | The primary assay for measuring educational impact. These parallel tests (knowledge exams, skills surveys, self-efficacy scales) quantitatively gauge learning gains and skill development [22] [72]. |
| Hybrid & Blended Learning Formats | A delivery vehicle for content. This blend of synchronous (in-person/virtual) and asynchronous (e-learning) instruction provides flexibility, supports diverse learning styles, and enhances accessibility [75]. |
Experimental Workflow: CBL vs. Traditional Instruction
The diagram below contrasts the fundamental structures of CBL and Traditional instructional approaches, highlighting the sequence of learning activities.
Conclusion
Challenge-based learning demonstrates superior outcomes in fostering critical thinking, problem-solving, and real-world application skills compared to traditional biomedical instruction, though it requires careful implementation and optimization. Key takeaways highlight the need for balanced pedagogical approaches, with future directions focusing on longitudinal studies, adaptive frameworks for emerging technologies, and implications for enhancing clinical research and drug development pipelines through better-trained professionals.
References
- 1. CBL Framework Today and CBL Learning Outcomes [https://link.springer.com/chapter/10.1007/978-3-031-67011-4_2]
- 2. An Exploratory Study of the Challenge-Based Learning ... [https://www.mdpi.com/2227-7102/13/3/234]
- 3. Impact of Case-based Learning on Critical Thinking in Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527965/]
- 4. Comparison of case-based learning and traditional method ... [https://pubmed.ncbi.nlm.nih.gov/31215320/]
- 5. A comparative study of a new challenge-based learning ... [https://www.frontiersin.org/journals/education/articles/10.3389/feduc.2025.1545071/full]
- 6. A Comparative Study of Case-Based Learning (CBL ... [https://pubmed.ncbi.nlm.nih.gov/40151742/]
- 7. Challenge-based learning approach to teach sports [https://www.sciencedirect.com/science/article/pii/S1473837623000163]
- 8. A pilot study investigating the efficacy of technology ... [https://www.nature.com/articles/s41598-025-99764-5]
- 9. Learning Theories: The Basics to Learn in Medical Education [https://pmc.ncbi.nlm.nih.gov/articles/PMC5769162/]
- 10. Explaining the classroom behavior process of medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11756675/]
- 11. Some Learning Theories for Medical Educators - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8368150/]
- 12. Constructivism in Education: What Is Constructivism? | NU [https://www.nu.edu/blog/what-is-constructivism-in-education/]
- 13. Biomedical engineering teaching: challenges and the ... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0003/html?srsltid=AfmBOoqiD2RTgreRCUPYYMeZsCpBpdi8YuBtJtZWbLNM30EHFxXP0fkq]
- 14. What is the Best Method to Teach Special Needs Students? [https://pmc.ncbi.nlm.nih.gov/articles/PMC9930485/]
- 15. Becoming a doctor: using social constructivism and situated ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-05113-x]
- 16. Implementing a challenge-based learning experience in a ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-05462-7]
- 17. Application of educational theories in undergraduate ... [https://jeths.org/archive/volume/9/issue/2/article/10452]
- 18. The Era of Biomedicine: Science, Medicine, and Public Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2570449/]
- 19. Practical tips for organizing challenge-based learning in ... [https://pubmed.ncbi.nlm.nih.gov/38144873/]
- 20. Contemporary Medical Education: Revolution versus ... [https://www.intechopen.com/chapters/77833]
- 21. Systematic Review: Revisiting Challenge-Based Learning ... [https://www.mdpi.com/2227-7102/14/9/1008]
- 22. Comparison of student learning in challenge-based and ... [https://pubmed.ncbi.nlm.nih.gov/17393336/]
- 23. Comparison of Student Learning in Challenge-based and ... [https://www.ovid.com/journals/abioen/pdf/10.1007/s10439-007-9297-7~comparison-of-student-learning-in-challenge-based-and]
- 24. The positive education of challenge: innovative integration of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10727089/]
- 25. Comparison of blended learning and traditional lecture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11188531/]
- 26. Self-directed learning versus traditional didactic learning in ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-06449-0]
- 27. Effect of problem-based learning combined with seminar ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1592199/full]
- 28. The effectiveness of case-based learning compared with ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-025-07927-9]
- 29. Traditional Lecture versus Case-Based Learning in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9598975/]
- 30. Effects of standardised patients (SP) combined with case ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12410676/]
- 31. [PDF] Comparison of Student Learning in Challenge-based ... [https://www.semanticscholar.org/paper/Comparison-of-Student-Learning-in-Challenge-based-Martin-Rivale/b45ad0278ec29752da9cc9abefd3b2943ef15c06]
- 32. Team-based learning versus traditional teaching effect on ... [https://www.sciencedirect.com/science/article/pii/S1319016424000677]
- 33. Case-Based Virtual Reality Simulation for Severe Pelvic ... [https://mededu.jmir.org/2025/1/e59850]
- 34. Deep Batch Active Learning for Drug Discovery [https://elifesciences.org/reviewed-preprints/89679]
- 35. AI In Action: Redefining Drug Discovery and Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC11800368/]
- 36. a systematic review and meta-analysis - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492731/]
- 37. Comparative study of case based learning with traditional ... [https://www.ijbcp.com/index.php/ijbcp/article/view/466]
- 38. CASE BASED LEARNING VS TRADITIONAL DIDACTIC ... [https://jptcp.com/index.php/jptcp/article/view/3095]
- 39. Evaluating the effectiveness of a new student-centred ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10224780/]
- 40. Challenge-Based Learning vs. Traditional Learning [https://prepr.org/blog/challenge-based-learning-vs-traditional-learning-which-engages-students-more/]
- 41. Does online case-based learning foster clinical reasoning ... [https://www.sciencedirect.com/science/article/pii/S251466452401600X]
- 42. Use of simulation for teaching biomedical sciences to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465261/]
- 43. Leveraging simulations to support patient-facing careers [https://www.sciencedirect.com/science/article/pii/S2665944125000124]
- 44. TEACHING STATISTICS ONLINE - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11056686/]
- 45. Comparison of Student Learning in Challenge-based and ... [https://link.springer.com/article/10.1007/s10439-007-9297-7]
- 46. Preliminary Effect of Challenge-Based Learning on ... [https://www.sciencedirect.com/science/article/abs/pii/S1557308724001136]
- 47. Comparison Of Student Learning In Challenge Based And ... [https://peer.asee.org/comparison-of-student-learning-in-challenge-based-and-traditional-instruction-in-biotransport-engineering-classrooms]
- 48. Practical tips for organizing challenge-based learning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10739181/]
- 49. Engaging Students With Challenge Based Learning [https://www.edutopia.org/article/challenge-based-learning-engages-students/]
- 50. Challenge Based Learning Guide and Toolkit [https://portal.synapses-academies.eu/challenge-based-learning-guide-and-toolkit/]
- 51. Challenge Based Learning | Take Action. Make a Difference. [https://www.challengebasedlearning.org/]
- 52. 7 Things You Should Know About Challenge-Based ... [https://library.educause.edu/resources/2012/1/7-things-you-should-know-about-challengebased-learning]
- 53. of Case Based Learning ( Implementation ) approach in... CBL [https://www.alliedacademies.org/articles/implementation-of-case-based-learning-cbl-approach-in-paediatrics-a-prospective-observational-study-30893.html]
- 54. Medical student experiences of Case-Based Learning (CBL ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-06585-7]
- 55. Challenges Regarding Transition from Case-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10056298/]
- 56. The Convergence between Challenge-Based Learning ... [https://www.linkedin.com/pulse/convergence-between-challenge-based-learning-diversity-vincent-merk]
- 57. 5 Top Reasons Why Challenge-Based Learning Engages ... [https://prepr.org/blog/5-top-reasons-why-challenge-based-learning-engages-students-more/]
- 58. Embracing the Future of Medical Education With Large ... [https://www.jmir.org/2025/1/e79091]
- 59. Assessment as Learning: A Mixed-Methods Study on Pre ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12519963/]
- 60. The effectiveness of augmented reality/mixed reality in ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-025-08166-8]
- 61. Auxiliary Teaching and Student Evaluation Methods Based on ... [https://humanfactors.jmir.org/2025/1/e72838]
- 62. Measuring Skill Acquisition vs. Knowledge Retention - SID [https://www.soundidea.co.za/measuring-skill-acquisition-vs-knowledge-retention/]
- 63. 7 Key Employee Training Metrics to Track in 2025 [https://www.edstellar.com/blog/employee-training-metrics]
- 64. What is Knowledge Retention? Definition, Benefits and Strategies [https://blog.smart-tribune.com/en/knowledge-retention]
- 65. The evaluation of an evidence-based model of feedback ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-022-03630-1]
- 66. 4 Top Innovative Skills Gained from Challenge-Based ... [https://prepr.org/blog/4-top-innovative-skills-gained-from-challenge-based-learning/]
- 67. Challenge-Based Learning in Biomedical Engineering [https://online-journals.org/index.php/i-joe/article/view/51795]
- 68. Feedback in Medical Education: An Evidence-based Guide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10284500/]
- 69. Creativity, Critical Thinking, Communication, and Collaboration [https://pmc.ncbi.nlm.nih.gov/articles/PMC10054602/]
- 70. Blended Learning Compared to Traditional Learning in ... [https://www.jmir.org/2020/8/e16504/]
- 71. Biomedical engineering teaching: challenges and the ... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0003/html?srsltid=AfmBOor6qtT58u6d_0cQwHX_60sZ3X9yxrQYpiITMMGK7pV3eFaYJq5F]
- 72. Biomedical students' self-efficacy and academic ... [https://pubmed.ncbi.nlm.nih.gov/38658898/]
- 73. Transdisciplinary experiential learning in biomedical ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-023-04171-x]
- 74. The impact of simulation-based training in medical education [https://pmc.ncbi.nlm.nih.gov/articles/PMC11224887/]
- 75. Blended Learning Guides Early Talent Down Long-Term ... [https://acrpnet.org/2025/09/10/blended-learning-guides-early-talent-down-long-term-clinical-research-paths]