Persistent Gait Deficits After Ankle Fracture Surgery: A Systematic Comparative Analysis of Spatiotemporal Parameters, Muscle Function, and Rehabilitation Efficacy
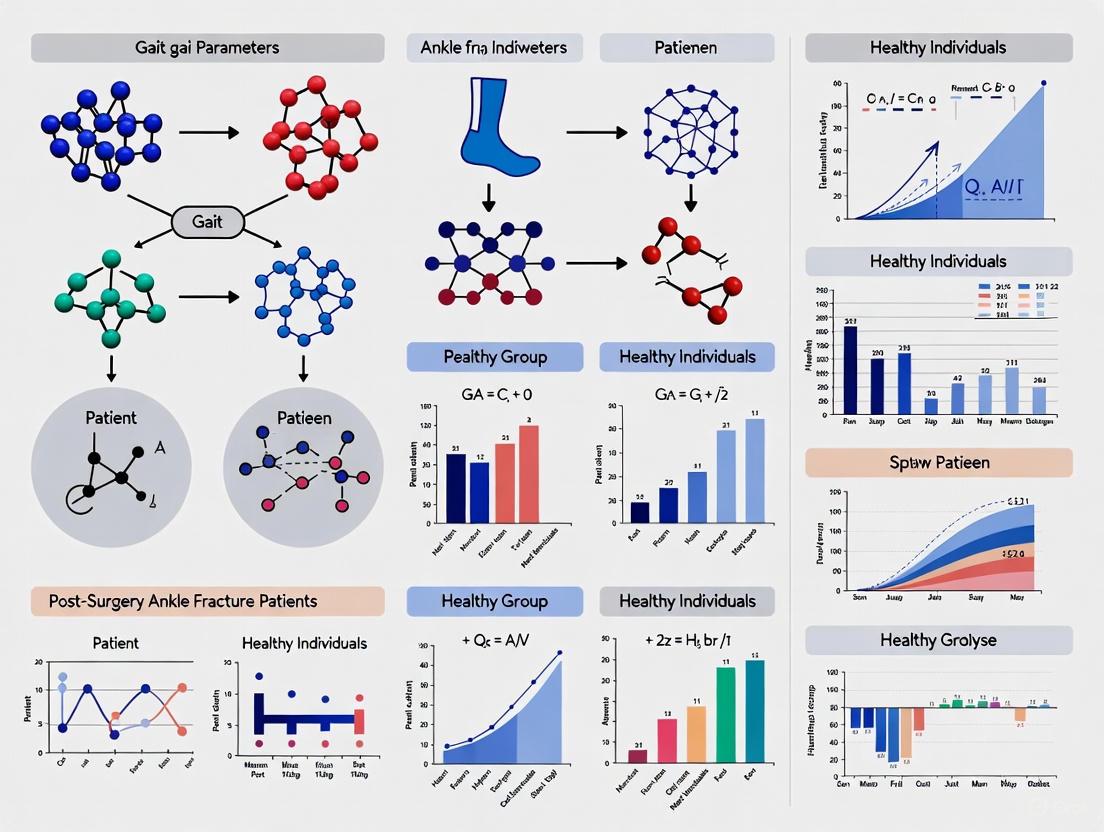
This article provides a comprehensive synthesis of current evidence comparing gait parameters, muscle strength, and functional outcomes between post-surgery ankle fracture patients and healthy individuals.
Persistent Gait Deficits After Ankle Fracture Surgery: A Systematic Comparative Analysis of Spatiotemporal Parameters, Muscle Function, and Rehabilitation Efficacy
Abstract
This article provides a comprehensive synthesis of current evidence comparing gait parameters, muscle strength, and functional outcomes between post-surgery ankle fracture patients and healthy individuals. Drawing upon recent systematic reviews and primary clinical studies, we analyze persistent deficits in spatiotemporal parameters including walking speed, step length, single support time, and cadence. We further explore methodological approaches for gait assessment, identify key rehabilitation challenges, and evaluate the efficacy of current intervention strategies. This analysis is particularly relevant for researchers and clinical professionals developing targeted rehabilitation protocols and pharmaceutical interventions aimed at optimizing functional recovery and addressing long-term mobility impairments following surgical fixation of ankle fractures.
Quantifying Persistent Gait Impairments: A Meta-Analysis of Post-Operative Ankle Fracture Recovery
Spatiotemporal gait parameters—walking speed, step length, and cadence—serve as crucial biomarkers for assessing locomotor function and rehabilitation outcomes across diverse patient populations. Within clinical research and practice, quantitative gait analysis provides an objective framework for evaluating functional recovery following surgical interventions. This meta-analysis systematically examines spatiotemporal gait deficits in post-surgery ankle fracture patients compared to healthy individuals, contextualizing these findings within the broader landscape of gait alterations associated with various physiological and cognitive challenges. The establishment of definitive normative values across age groups and pathologies enables more precise clinical assessments and facilitates targeted therapeutic interventions to restore optimal gait function.
Comparative Analysis of Gait Parameters
Post-Surgery Ankle Fracture Patients vs. Healthy Controls
A comprehensive meta-analysis of 12 studies comprising 219 postoperative ankle fracture patients and 192 healthy controls revealed significant impairments across multiple spatiotemporal gait parameters [1]. Despite surgical intervention and subsequent rehabilitation, patients consistently failed to regain pre-injury levels of locomotor function, exhibiting characteristic alterations in their gait patterns.
Table 1: Gait Parameter Deficits in Post-Surgery Ankle Fracture Patients
| Gait Parameter | Weighted Mean Difference (WMD) | 95% Confidence Interval | P-value | Statistical Significance |
|---|---|---|---|---|
| Walking Speed (m/s) | -0.13 | [-0.45, -0.16] | < 0.001 | Significant |
| Step Length (m) | -0.15 | [-0.18, -0.12] | < 0.001 | Significant |
| Cadence (steps/min) | -8.44 | [-10.87, -6.01] | < 0.001 | Significant |
| Single Support Time (%) | -16.59 | [-19.18, -14.00] | < 0.001 | Significant |
| Peak Dorsiflexion Angular Velocity (°/s) | -7.93 | [-13.45, -2.41] | 0.005 | Significant |
| Peak Plantarflexion Angular Velocity (°/s) | -49.64 | [-99.98, 0.71] | 0.053 | Not Significant |
The meta-analysis further indicated that both muscle strength and plantar pressure were notably reduced in postoperative patients, contributing to the observed gait alterations. The persistence of these deficits highlights the complex nature of functional recovery beyond mere bone healing, emphasizing the need for targeted rehabilitation protocols addressing neuromuscular control and proprioception [1].
Contextualizing Gait Deficits Across Populations and Conditions
To properly contextualize the gait deficits observed in ankle fracture patients, it is instructive to compare these findings with other populations experiencing locomotor challenges. Spatiotemporal parameters vary considerably across pathological conditions, age groups, and challenging circumstances such as dual-task walking.
Table 2: Comparative Gait Alterations Across Populations and Conditions
| Population/Condition | Walking Speed | Step/Stride Length | Cadence | Other Key Alterations |
|---|---|---|---|---|
| Texting While Walking [2] | Significant decrease | Significant decrease | Significant decrease | Increased double support time, reduced single support |
| Visual Impairment [3] | Slower | Shorter stride length | Decreased | Increased step width, prolonged double support, reduced single support |
| Aging (>60 years) [4] | Progressive decline | Reduced stride length | Variable trends | Increased gait variability and asymmetry |
| Frailty/Pre-frailty [5] | Slower | Shorter steps | Reduced | Longer stride times, fragmented walking patterns |
| Parkinson's Disease [6] | - (8-11)% | - (7-17)% | -6% | +76% stride time variability, +24% double support time |
The comparative analysis reveals that ankle fracture patients share several gait characteristics with other populations experiencing mobility challenges, particularly in terms of reduced speed and step length. However, the magnitude and specific pattern of deficits may serve as distinctive biomarkers for this population, potentially guiding more targeted rehabilitation approaches.
Experimental Protocols and Methodologies
Standardized Gait Assessment Protocols
The primary meta-analysis on ankle fracture patients employed rigorous methodology in accordance with PRISMA 2020 guidelines [1]. Literature searches were conducted across multiple databases (PubMed, EMBASE, Cochrane Library, and Web of Science) up to February 2024, using PICOS criteria for study selection. Eligible studies included cross-sectional and non-randomized observational designs comparing gait analysis outcomes, muscle strength, and plantar pressure between postoperative ankle fracture patients and healthy controls.
Quality assessment was performed using the Agency for Healthcare Research and Quality (AHRQ) tool for cross-sectional studies and the Methodological Index for Non-Randomized Studies (MINORS) for observational studies [1]. Meta-analytical procedures included calculation of weighted mean differences with 95% confidence intervals, with heterogeneity assessed using Cochrane's Q test and I² statistic. Sensitivity analysis was performed using the leave-one-out method to evaluate the robustness of the findings.
Emerging Methodologies in Gait Analysis
Recent advances in gait assessment methodologies have expanded beyond traditional laboratory-based systems toward more accessible technologies:
Markerless Motion Capture Systems: Theia3D represents an emerging markerless motion capture technology that uses synchronized video data and deep learning algorithms to estimate three-dimensional human pose without skin-mounted markers [7]. Validation studies demonstrate excellent agreement with marker-based systems for gait speed (mean difference: 0.00 m/s) and good to excellent agreement for distance-based parameters, though timing parameters like stance duration showed wider limits of agreement [7].
Inertial Measurement Units (IMUs): Wearable sensors containing accelerometers, gyroscopes, and magnetometers enable gait assessment in ecological settings beyond laboratory constraints. IMU measurements have been validated against laboratory analysis techniques (r > 0.83) and can capture free-living gait in community settings [6]. Normative databases have been established using sternum-placed IMUs during 50-meter walks, demonstrating consistent age-related declines in gait speed [6].
Computer Vision Approaches: Open-source pose estimation algorithms like MediaPipe enable gait analysis from standard video footage, making assessment possible in resource-limited settings [8]. This approach uses deep convolutional neural networks trained on extensive image datasets to extract body landmarks from 2D video, facilitating the calculation of stability parameters such as the Margin of Stability (MoS) in older adults [8].
Research Reagent Solutions for Gait Analysis
Table 3: Essential Materials and Technologies for Gait Research
| Research Tool | Function/Application | Key Features |
|---|---|---|
| GAITRite Electronic Walkway [9] | Gold standard for spatiotemporal parameter assessment | Portable pressure-sensitive walkway; Validated for step length, velocity, cadence, and timing parameters |
| Inertial Measurement Units (IMUs) [6] [5] | Wearable sensor for laboratory and free-living gait assessment | Triaxial accelerometer, gyroscope, magnetometer; Enables long-term monitoring in ecological settings |
| Markerless Motion Capture (Theia3D) [7] | 3D human pose estimation without physical markers | Uses deep learning algorithms; Eliminates marker placement artifacts; Suitable for non-laboratory environments |
| OptoGait System [10] | Optical measurement system for gait parameters | Photoelectric cell-based; Synchronizes with video recording; Provides comprehensive spatiotemporal data |
| MediaPipe Pose [8] | Open-source pose estimation framework | Markerless 2D/3D pose estimation from video; Accessible for resource-limited settings |
| Health&Gait Dataset [10] | Video-based gait analysis dataset | 1,564 videos from 398 participants; Includes anthropometric data and gait parameters |
Standardized Assessment Protocols
10-Meter Walk Test (10MWT): A clinically accessible assessment demonstrating high test-retest reliability for measuring comfortable and fast gait speed (ICC = 0.95-0.96) and step length (ICC = 0.91-0.98) in adolescents and adults with brain injury [9]. This test shows fair-to-moderate agreement with GAITRite during comfortable walking speeds (ICC = 0.46-0.89) and high agreement during maximal walking speeds (ICC = 0.91-0.96) [9].
Dual-Task Paradigms: Assessment of gait while performing concurrent cognitive tasks (e.g., visuospatial memory tasks) [9]. This approach detects deficits that may not manifest during single-task walking, particularly relevant for concussion management and neurodegenerative conditions [2] [9].
Six-Minute Walk Test: Used in datasets like DUO-GAIT to assess endurance and gait patterns under prolonged walking conditions, sometimes combined with cognitive tasks to evaluate dual-task costs [10].
This meta-analysis establishes that postoperative ankle fracture patients exhibit significant deficits in walking speed, step length, and cadence compared to healthy controls, with weighted mean differences of -0.13 m/s, -0.15 m, and -8.44 steps/minute, respectively [1]. These impairments persist despite surgical intervention and rehabilitation, highlighting the complex nature of functional recovery that extends beyond bone healing to encompass neuromuscular control and proprioceptive function.
The contextualization of these findings within the broader landscape of gait alterations reveals common patterns across diverse populations, suggesting possible shared mechanisms in the neural control of locomotion under challenging conditions. Emerging methodologies in gait assessment, particularly markerless motion capture and wearable sensors, offer promising avenues for more ecological monitoring of recovery trajectories and rehabilitation efficacy.
For researchers and clinicians, these findings underscore the importance of comprehensive gait assessment using validated technologies and standardized protocols. The establishment of definitive normative values and pathological patterns enables more precise evaluation of interventions aimed at restoring optimal locomotor function in postoperative patients and other populations experiencing mobility challenges.
The following tables synthesize quantitative findings from a 2025 systematic review and meta-analysis, which encompassed 12 studies comparing 219 post-surgery ankle fracture patients with 192 healthy controls [1] [11].
Table 1: Gait Parameter Alterations Post-Ankle Fracture Surgery
| Gait Parameter | Weighted Mean Difference (WMD) vs. Healthy Controls | 95% Confidence Interval | P-value |
|---|---|---|---|
| Walking Speed | -0.13 m/s | [-0.45, -0.16] | < 0.001 |
| Step Length | -0.15 m | [-0.18, -0.12] | < 0.001 |
| Cadence | -8.44 steps/min | [-10.87, -6.01] | < 0.001 |
| Single Support Time | -16.59 % | [-19.18, -14.00] | < 0.001 |
| Peak Dorsiflexion Angular Velocity | -7.93 °/s | [-13.45, -2.41] | 0.005 |
| Peak Plantarflexion Angular Velocity | -49.64 °/s | [-99.98, 0.71] | 0.053 (NS) |
NS: Not Statistically Significant
Table 2: Muscle Strength and Plantar Pressure Deficits
| Measured Parameter | Post-Surgery Alteration | Key Findings |
|---|---|---|
| Peak Torque (Dorsiflexion) | Significantly Reduced [1] | Major contributor to impaired gait. |
| Peak Torque (Plantarflexion) | Significantly Reduced [1] | Impacts push-off power during walking. |
| Plantar Pressure | Notable Reduction [1] | Altered distribution and magnitude. |
| Overall Functional Recovery | Incomplete [1] | Patients often fail to regain pre-injury levels of walking speed, muscle strength, and normal plantar pressure distribution despite rehabilitation. |
Experimental Protocols and Methodologies
The comparative data are derived from standardized experimental protocols designed to objectively quantify functional deficits.
Gait Analysis Protocol
- Objective: To quantify spatiotemporal and kinematic gait parameters in a controlled environment [1].
- Equipment: Three-dimensional motion analysis systems with synchronized camera and force plate technology [1] [12].
- Procedure: Participants walk at a self-selected speed along a walkway. Data from multiple gait cycles are captured, focusing on the sagittal plane kinematics of the ankle joint [1].
- Measured Variables: Walking speed, step length, cadence, single-limb support time, and peak angular velocities for dorsiflexion and plantarflexion during specific gait phases [1].
Muscle Strength Assessment Protocol
- Objective: To measure the isometric and/or isokinetic strength of ankle dorsiflexor and plantarflexor muscle groups [1].
- Equipment: Isokinetic dynamometer [1].
- Procedure: The participant's foot is securely fastened to the dynamometer's footplate. They perform maximal voluntary contractions against resistance through the ankle's full range of motion, typically in a seated position with knee flexed [1].
- Primary Outcome: Peak torque, which is the highest torque output produced during the movement, measured in Newton-meters (Nm). This is a direct indicator of muscle functional capacity [1].
Plantar Pressure Measurement Protocol
- Objective: To assess the distribution and magnitude of pressure across the plantar surface of the foot during standing and walking [1].
- Equipment: Pressure sensor platforms (e.g., Novel emed) or in-shoe sensor insoles (e.g., Novel pedar). The 2025 meta-analysis highlighted the use of such systems [1] [13].
- Procedure: Participants perform barefoot walking trials, stepping onto the pressure platform. For in-shoe analysis, flexible sensor sheets are placed inside the subject's footwear to capture data during prolonged activity [13].
- Data Processing & Analysis: Software algorithms process the raw sensor data to generate metrics such as peak pressure (maximum pressure under any sensor), mean pressure, pressure-time integral (the cumulative load over time), and contact area. The use of open-source tools like the
pressuReR package allows for standardized processing and regional mask analysis (e.g., separating heel, midfoot, forefoot) [13]. - Key Metric: Peak Plantar Pressure is a critical variable for identifying areas of high loading risk and understanding altered biomechanics [1] [13].
Experimental Workflow and Logical Relationships
The diagram below illustrates the structured pathway from patient recruitment to data synthesis in comparative post-surgery research.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Resources for Biomechanical Research
| Item | Category | Function in Research |
|---|---|---|
| Isokinetic Dynamometer | Hardware | The gold-standard instrument for objectively quantifying peak torque and muscle endurance of ankle dorsiflexors and plantarflexors [1]. |
| Pressure Measurement Platform | Hardware | A rigid plate embedded with sensor arrays to capture dynamic barefoot plantar pressure distribution during gait [1] [13]. |
| In-Shoe Pressure Insoles | Hardware | Flexible sensor sheets placed inside footwear to measure plantar pressure distribution over multiple steps in real-world conditions [13] [14]. |
| 3D Motion Capture System | Hardware | A multi-camera system used for high-precision kinematic analysis of joint angles and spatiotemporal gait parameters [1] [12]. |
pressuRe R Package |
Software | An open-source tool for standardizing the processing, analysis, and visualization of plantar pressure data from various hardware systems, promoting reproducibility [13]. |
| Self-Administered Foot Evaluation Questionnaire (SAFE-Q) | Patient-Reported Outcome | A validated instrument to assess quality of life and function from the patient's perspective, covering pain, daily living, and social functioning [12]. |
| 2-(Diethylamino)ethyl (3-(octyloxy)phenyl)carbamate hydrochloride | 2-(Diethylamino)ethyl (3-(octyloxy)phenyl)carbamate hydrochloride, CAS:32223-82-8, MF:C21H37ClN2O3, MW:401.0 g/mol | Chemical Reagent |
| SI-2 | SI-2, MF:C15H15N5, MW:265.31 g/mol | Chemical Reagent |
Ankle fractures represent one of the most common lower limb fractures worldwide, with increasing incidence particularly among individuals over 50 years of age [15] [16]. While surgical intervention successfully achieves fracture union in most cases, a growing body of evidence indicates that anatomical healing does not necessarily translate to functional recovery. This comparative analysis examines the persistent functional deficits observed in patients at 4.5 years post-surgery, comparing their gait parameters, muscle strength, and functional performance against healthy control subjects. Understanding these long-term limitations is crucial for researchers and clinicians aiming to develop more effective rehabilitation protocols and outcome measures that extend beyond radiographic healing.
Comparative Analysis of Gait Parameters and Functional Outcomes
Spatiotemporal Gait Parameters: Patients vs. Healthy Controls
Table 1: Comparative analysis of spatiotemporal gait parameters between post-surgery ankle fracture patients and healthy individuals
| Gait Parameter | Post-Surgery Patients | Healthy Controls | Weighted Mean Difference (WMD) | P-value |
|---|---|---|---|---|
| Walking speed (m/s) | Reduced | Normal | -0.13 (95% CI: -0.45, -0.16) | <0.001 |
| Step length (m) | Shorter | Normal | -0.15 (95% CI: -0.18, -0.12) | <0.001 |
| Single support time (%) | Reduced | Normal | -16.59 (95% CI: -19.18, -14.00) | <0.001 |
| Cadence (steps/min) | Lower | Normal | -8.44 (95% CI: -10.87, -6.01) | <0.001 |
| Peak dorsiflexion angular velocity (°/s) | Impaired | Normal | -7.93 (95% CI: -13.45, -2.41) | 0.005 |
| Peak plantarflexion angular velocity (°/s) | Lower | Normal | -49.64 (95% CI: -99.98, 0.71) | 0.053 |
A comprehensive meta-analysis of 12 studies comprising 219 postoperative ankle fracture patients and 192 healthy controls revealed significant impairments across multiple gait parameters [11] [17]. Despite surgical intervention and subsequent rehabilitation, patients failed to regain pre-injury levels of walking speed, step length, and cadence. The most pronounced differences were observed in single support time and walking speed, indicating fundamental alterations in gait mechanics that persist long after fracture healing [11].
Functional Performance and Clinical Outcomes
Table 2: Long-term functional outcomes after ankle fracture surgery (4.5-year follow-up)
| Functional Measure | Surgical Side | Non-Surgical Side | P-value | Clinical Scores |
|---|---|---|---|---|
| Heel Rise Test (cm) | Significant deficit | Normal | 0.020 | - |
| Weight-Bearing Lunge Test (cm) | Significant deficit | Normal | 0.006 | - |
| AOFAS Ankle-Hindfoot Scale | - | - | - | 86.5 |
| Olerud-Molander Ankle Score (OMAS) | - | - | - | 80 |
At a mean follow-up of 4.5 years post-surgery, patients demonstrated significant functional limitations despite favorable clinical scores [15] [16]. The Heel Rise Test, which assesses ankle plantarflexion strength, and the Weight-Bearing Lunge Test (WBLT), which evaluates ankle dorsiflexion mobility, both showed substantial deficits on the surgical side compared to the non-surgical side. This discrepancy between objective functional measures and clinical scoring systems highlights the limitation of relying solely on questionnaire-based outcomes for evaluating recovery [15].
The long-term nature of these deficits is further corroborated by a 5-year follow-up study which found that 63% of patients still complained of stiffness, 45% reported ankle swelling, and 50% experienced persistent pain [18]. Additionally, 39% of patients felt they had not fully recovered, and 38% did not return to their pre-injury sporting activities [18].
Experimental Protocols and Methodologies
Gait Analysis Protocol
The experimental assessment of gait parameters followed standardized protocols across multiple studies. Spatiotemporal gait parameters were evaluated using the GAITRite system, an electronic walkway mat that captures precise measurements of various gait components [15] [16]. Participants walked barefoot along a 6-meter walkway three times at their normal walking speed, with trials starting 2 meters before the walkway to ensure consistent velocity upon entry [16].
Specific measured parameters included:
- Step time and step length
- Stride length
- Base of support
- Single and double support time
- Walking speed
- Cadence
Data analysis was performed using statistical packages such as SPSS, with intraclass correlation coefficients (ICCs) calculated to determine inter-trial reliability [16]. Standard Error of Measurement (SEM) and Minimal Detectable Change (MDC) values were established to ensure measurement precision.
Functional Performance Testing
Two key functional tests were administered to assess specific ankle functions:
Heel Rise Test Protocol:
- Participants performed repeated unilateral heel lifts while standing
- Total heel rise height was measured in centimeters
- The test primarily assesses plantarflexion strength and endurance [15] [16]
Weight-Bearing Lunge Test (WBLT) Protocol:
- Participants performed a forward lunge with the tested foot flat on the ground
- Maximum distance from the great toe to the wall was measured while maintaining heel contact
- This test specifically evaluates weight-bearing ankle dorsiflexion range of motion [15] [16]
Both tests demonstrated excellent intrarater reliability, with ICC values of 0.98 for the Heel Rise Test and 0.99 for the WBLT, confirming their suitability for longitudinal assessment [15].
Research Workflow and Signaling Pathways
The Scientist's Toolkit: Essential Research Materials
Table 3: Key research reagents and equipment for ankle fracture recovery studies
| Research Tool | Specific Function | Application in Ankle Fracture Research |
|---|---|---|
| GAITRite Electronic Walkway | Captures spatiotemporal gait parameters | Quantitative assessment of walking speed, step length, cadence, and support times [15] [16] |
| Isokinetic Dynamometer | Measures peak torque of dorsiflexion and plantarflexion | Objective evaluation of ankle muscle strength deficits [11] [17] |
| Pressure Platform System | Assesses plantar pressure distribution | Analysis of weight-bearing patterns and pressure abnormalities [11] |
| AOFAS Ankle-Hindfoot Scale | Patient-reported clinical outcome measure | Subjective assessment of pain, function, and alignment [15] [16] |
| Olerud-Molander Ankle Score (OMAS) | Disease-specific functional rating | Evaluation of daily activity performance and symptom severity [15] [18] |
| Weight-Bearing Lunge Test Apparatus | Measures ankle dorsiflexion range of motion | Assessment of joint stiffness and mobility restrictions [15] [16] |
| PPHP | PPHP Polypropylene Homopolymer Resin | |
| kn-92 | kn-92, CAS:176708-42-2, MF:C24H25ClN2O3S, MW:457 g/mol | Chemical Reagent |
The evidence from 4.5-year follow-up studies demonstrates conclusively that ankle fracture patients experience persistent functional deficits long after radiographic union has been achieved. These limitations manifest as altered gait patterns, reduced muscle strength, impaired range of motion, and functional performance deficits, despite seemingly favorable clinical scores. The discrepancy between objective functional measures and subjective clinical outcomes underscores the need for more sophisticated assessment protocols in both clinical and research settings. Future research should focus on developing targeted rehabilitation strategies that address the specific soft tissue mobility and muscle function impairments identified in these long-term studies, with the goal of restoring pre-injury functional levels rather than merely achieving fracture healing.
The successful recovery of motor function following ankle fracture surgery does not always equate to a successful quality of life (QOL) outcome from the patient's perspective. This guide provides a comparative analysis of objective gait parameters and their correlation with patient-reported outcomes, specifically the Self-Administered Foot Evaluation Questionnaire (SAFE-Q). It synthesizes current research to help professionals in drug development and clinical research understand how weight-bearing ankle dorsiflexion and gait speed serve as critical biomarkers for patient recovery and QOL, providing a framework for evaluating rehabilitation interventions and therapeutic outcomes.
Comparative Analysis of Key Parameters
Gait Parameters: Patients vs. Healthy Norms
Post-surgical ankle fracture patients demonstrate significant deficits in gait parameters when compared to healthy individuals. The table below summarizes quantitative findings from meta-analyses and comparative studies.
Table 1: Gait Parameter Comparison Between Post-Surgery Ankle Fracture Patients and Healthy Individuals
| Gait Parameter | Post-Surgery Patients | Healthy Individuals (Normative Data) | Statistical Significance | Source |
|---|---|---|---|---|
| Walking Speed | Slower | ~1.34 m/s (comfortable pace) [19] | P < 0.001 [11] | Systematic Review [11] |
| Cadence | Significantly lower (WMD: -8.44 steps/min) [11] | 90-120 steps/min [19] | P < 0.001 [11] | Systematic Review [11] |
| Step Length | Shorter (WMD: -0.15 m) [11] | ~70 cm [19] | P < 0.001 [11] | Systematic Review [11] |
| Single Support Time | Significantly reduced (WMD: -16.59) [11] | Not Reported | P < 0.001 [11] | Systematic Review [11] |
| Peak Dorsiflexion Angular Velocity | Significantly lower (WMD: -7.93) [11] | Not Reported | P = 0.005 [11] | Systematic Review [11] |
Abbreviation: WMD, Weighted Mean Difference.
Correlations with SAFE-Q Quality of Life Domains
The functional impairments detailed in Table 1 have a direct and measurable impact on patient quality of life, as quantified by the SAFE-Q questionnaire. The SAFE-Q is a validated, region-specific patient-reported outcome measure with high test-retest reliability (ICC >0.7 for all subscales) [20] [21]. It evaluates QOL across multiple subscales, each scored from 0 (least healthy) to 100 (healthiest) [22] [20].
Table 2: Correlation of Physical Factors with SAFE-Q Subscales in Post-Operative Ankle Fracture Patients
| Physical Factor | SAFE-Q Subscale | Statistical Correlation | Clinical Interpretation | Source |
|---|---|---|---|---|
| Weight-Bearing Ankle Dorsiflexion ROM (Deep Squat Sitting) | Pain and Pain-Related | β = 0.584, P < 0.001 [22] | Strong, positive association; greater ROM linked to less pain. | Cross-Sectional Study [22] |
| Physical Functioning and Daily Living | β = 0.376, P = 0.006 [22] | Moderate, positive association; greater ROM linked to better physical function. | Cross-Sectional Study [22] | |
| Social Functioning | β = 0.317, P = 0.045 [22] | Moderate, positive association; greater ROM linked to improved social activity. | Cross-Sectional Study [22] | |
| General Health and Well-Being | β = 0.483, P = 0.005 [22] | Moderate to strong, positive association; greater ROM linked to better overall well-being. | Cross-Sectional Study [22] | |
| Gait Speed | Physical Functioning and Daily Living | β = 0.555, P < 0.001 [22] | Strong, positive association; faster speed linked to better daily function. | Cross-Sectional Study [22] |
| Social Functioning | β = 0.514, P = 0.002 [22] | Strong, positive association; faster speed linked to improved social activity. | Cross-Sectional Study [22] |
Abbreviations: ROM, Range of Motion; β, Standardized Partial Regression Coefficient.
Experimental Protocols and Methodologies
Measuring the Key Variables
Weight-Bearing Ankle Dorsiflexion Protocol
The association with QOL is particularly strong for weight-bearing dorsiflexion measurements, which better replicate the demands of daily life than non-weight-bearing tests [22].
- Objective: To quantify weight-bearing ankle dorsiflexion range of motion (ROM) using methods that correlate with quality of life.
- Equipment: Standard goniometer.
- Methodologies:
- Rear Ankle with Knee Extended: The participant steps forward with the non-measured leg and leans the lower leg of the measured side forward as far as possible, keeping the knee extended and the heel on the ground. The angle is measured between a perpendicular line to the floor and a line connecting the fibular head and lateral malleolus [22].
- Rear Ankle with Knee Flexed: The same as above, but performed with the knee of the measured side flexed during a forward lunge [22].
- Front Ankle during Forward Lunge: The participant steps forward with the lower leg being measured and leans forward in a lunge position against a wall for balance [22].
- Deep Squat Sitting: The participant squats to the deepest position they can maintain for 3 seconds, keeping the heels on the ground and arms extended forward parallel to the floor. The goniometer is used to measure the ankle angle in this position [22]. This specific method was identified as an independent variable for all four primary SAFE-Q subscales [22].
- Data Collection: Measurements are repeated twice for each method to ensure reliability. The minimum value is 1° [22].
Gait Analysis Protocol
- Objective: To obtain spatiotemporal gait parameters such as velocity, cadence, and step length.
- Equipment: Three-dimensional motion analyzer [22] or an electronic walkway system (e.g., GAITRite) [23] [24]. For clinical settings, a stopwatch and measured walkway can be used for speed and cadence.
- Procedure: Participants complete multiple walks at their self-selected, comfortable walking speed. Walks are initiated and terminated a meter before and after the walkway to account for acceleration and deceleration, ensuring data is collected at a constant velocity [23].
- Key Parameters: The software typically calculates gait speed (m/s), cadence (steps/min), step length (m), stride length (m), and single/double support times (s or % of gait cycle) automatically [19] [23].
Patient-Reported Outcome Measure: SAFE-Q
- Instrument: The Self-Administered Foot Evaluation Questionnaire (SAFE-Q) version 2 [20] [21].
- Administration: Patients complete the 34-item questionnaire independently. Items are scored on a Likert scale (0-4) or a visual analog scale (for specific questions) [22].
- Scoring: Scores for each of the five core subscales (Pain and Pain-Related, Physical Functioning and Daily Living, Social Functioning, Shoe-Related, and General Health and Well-Being) are calculated and scaled from 0 (worst) to 100 (best) [22] [20]. The Sports Activity subscale is optional.
The logical relationship between these protocols and the core findings of the research is summarized in the workflow below.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key materials and instruments required for conducting research in this field, based on the methodologies cited in the reviewed literature.
Table 3: Essential Research Reagents and Materials for Gait and QOL Analysis
| Item | Function/Application | Example from Research |
|---|---|---|
| SAFE-Q Questionnaire | A validated, patient-reported outcome measure to assess foot- and ankle-specific health-related quality of life. It provides subscale scores for pain, physical function, social function, and general well-being [22] [20]. | The primary QOL metric in recent studies correlating physical function with life impact [22]. |
| Three-Dimensional Motion Analysis System | The gold standard for comprehensive gait analysis, using multiple cameras and reflective markers to capture detailed kinematic and kinetic data during walking [22]. | Used to measure gait parameters in experimental settings [22]. |
| Electronic Walkway (e.g., GAITRite) | A portable system with pressure-sensitive sensors that automatically calculates spatiotemporal gait parameters (speed, cadence, step length, etc.) as a subject walks across it [23] [24]. | Used for efficient and reliable gait data collection in lab and clinical environments [23] [24]. |
| Isokinetic Dynamometer (e.g., Biodex) | An instrument used to objectively measure muscle strength (peak torque) of ankle plantarflexors and dorsiflexors under controlled conditions and velocities [22]. | Used to assess ankle strength as a physical factor post-surgery [22]. |
| Standard Goniometer | A simple, low-cost tool for measuring joint range of motion. Essential for assessing weight-bearing and non-weight-bearing ankle dorsiflexion [22]. | The tool specified for measuring all ankle dorsiflexion ROM in the cited study [22]. |
| T2AA | T2AA, CAS:1380782-27-3, MF:C15H15I2NO3, MW:511.09 | Chemical Reagent |
| PX 2 | PX 2, MF:C22H25FN4O2, MW:396.5 | Chemical Reagent |
Discussion and Path Forward
The evidence clearly demonstrates that gait speed and weight-bearing ankle dorsiflexion ROM, particularly in a functional position like a deep squat, are not just performance metrics but are significant biomarkers for patient-reported quality of life after ankle fracture surgery [22]. The strong, independent correlations with multiple SAFE-Q subscales underscore that rehabilitation programs must target the restoration of these specific functions to achieve meaningful patient outcomes.
Future research should focus on developing and testing targeted rehabilitation interventions designed to improve weight-bearing dorsiflexion and gait speed. Furthermore, the integration of these objective measures with validated patient-reported outcomes like the SAFE-Q provides a robust framework for evaluating new pharmacological adjuvants or physical therapies in clinical trials, ensuring that treatments are assessed against metrics that truly matter to patients' lives.
Advanced Gait Analysis Methodologies: From Laboratory Systems to Clinical Applications
The quantitative analysis of human gait is indispensable in clinical diagnostics, rehabilitation monitoring, and biomedical research. Following surgical interventions such as ankle fracture repair, gait analysis provides objective data to evaluate functional recovery and compare patient outcomes to healthy baseline performance [1] [11]. Multiple technologies are available for capturing spatiotemporal gait parameters, ranging from sophisticated laboratory-based systems to portable clinical tools and consumer-grade devices. This guide provides a comparative analysis of three prominent approaches: laboratory-grade 3D motion analysis systems, electronic walkways like the GAITRite system, and smartphone applications. Framed within research comparing post-surgery ankle fracture patients to healthy individuals, this comparison evaluates each tool's performance characteristics, supported by experimental data, to inform researchers and clinicians in selecting appropriate assessment technologies.
The table below summarizes the core characteristics, performance data, and optimal use cases for the three primary gait assessment technologies.
Table 1: Comprehensive Comparison of Gait Assessment Technologies
| Feature | GAITRite Electronic Walkway | 3D Motion Analysis (Lab) | Smartphone Applications |
|---|---|---|---|
| Technology Type | Electronic pressure-sensitive walkway [25] | Optoelectronic systems (e.g., Vicon) with force plates [26] | Embedded inertial sensors (accelerometers, gyroscopes) [27] [28] |
| Key Measured Parameters | Spatial: Step/stride length, step width [23].Temporal: Gait speed, cadence, step/stride time, stance/swing phase % [23] [25]. | Comprehensive kinematics (joint angles, velocities), kinetics (ground reaction forces), and spatiotemporal parameters [26]. | Spatiotemporal: Gait speed, cadence, step time, distance [27] [28]. |
| Validity & Reliability | High validity (ICC >0.93) and test-retest reliability for core parameters (speed, stride length, cadence) across populations [25] [29]. | Considered the gold standard for kinematic and kinetic data [26] [30]. | High agreement with GAITRite for speed & cadence (ICC 0.78-0.99) [28]. Moderate-to-excellent reliability in older adults [27]. |
| Key Strengths | High accuracy for spatiotemporal metrics; quick setup; excellent reliability; suitable for clinical environments [25]. | Comprehensive biomechanical data; gold standard for detailed movement analysis [26]. | Extreme portability and low cost; enables monitoring in free-living environments; high user acceptability [27] [28]. |
| Key Limitations | Limited capture area; measures only a few consecutive strides; cannot assess kinematics or kinetics [25]. | High cost, complex setup, and laboratory-confined; requires technical expertise [26]. | Lower accuracy for complex parameters (e.g., step asymmetry); performance varies with placement and algorithm [27] [28]. |
| Context in Ankle Fracture Research | Effectively identifies deficits in gait speed, step length, and cadence in patients vs. controls [1]. | Can reveal underlying mechanisms like reduced peak dorsiflexion angular velocity [1]. | Potential for continuous, low-cost monitoring of walking speed as a functional outcome in community settings [27]. |
Detailed Performance Data and Experimental Protocols
Comparative Data in Pathological and Healthy Populations
Research on post-surgery ankle fracture patients quantitatively illustrates the sensitivity of these tools in detecting functional impairments. A systematic review and meta-analysis of 12 studies revealed that, despite rehabilitation, patients show significant deficits compared to healthy controls when assessed with instrumented systems [1] [11]. Key findings include:
- Walking Speed: Patients walked significantly slower (Weighted Mean Difference [WMD] = -0.13 m/s) [1].
- Step Length: Patients had shorter steps (WMD = -0.15 m) [1].
- Cadence: Patients exhibited a lower step rate (WMD = -8.44 steps/min) [1].
- Single Support Time: The time spent on the affected limb was reduced (WMD = -16.59%) [1].
These parameters, which are reliably captured by both GAITRite and smartphone systems, highlight the persistent gait impairments in this patient population [1] [28].
The following table synthesizes key reliability and validity metrics for the assessed technologies, as reported in the literature.
Table 2: Summary of Key Reliability and Validity Metrics
| Technology | Parameter | Metric & Population | Reported Value |
|---|---|---|---|
| GAITRite | Gait Speed, Stride Length, Cadence | Test-Retest Reliability (ICC) across multiple populations [25] | ICC > 0.75 |
| GAITRite | Spatial Measures | Validity vs. Paper-and-Pencil Method (ICC) [29] | ICC > 0.95 |
| GAITRite | Temporal Measures | Validity vs. Video-Based Method (ICC) [29] | ICC > 0.93 |
| Smartphone App | Walking Velocity, Cadence | Validity vs. GAITRite (ICC) in Healthy Adults [28] | ICC 0.778 - 0.999 |
| Smartphone App | Gait Speed | Validity & Reliability in Older Adults [27] | ICC ~ 0.9 |
Standardized Experimental Protocols
To ensure the validity and comparability of data, studies typically follow standardized protocols:
- GAITRite Protocol: Participants are instructed to walk at a self-selected comfortable speed across the walkway, initiating and terminating their gait several feet before and after the mat to capture steady-state walking [23]. Multiple walking trials are averaged to obtain a representative sample.
- Smartphone Assessment Protocol: The smartphone is securely attached to the participant's body, most commonly on the lower back near the sacrum (center of mass) using an elastic belt [28]. Participants then perform walking tasks, such as at preferred, slow, and fast speeds, while data is collected via a custom or commercial application [28].
- 3D Motion Analysis Protocol: Participants walk along a walkway instrumented with force plates. Reflective markers are placed on anatomical landmarks, and multiple cameras capture their trajectory. Data from the cameras and force plates are synchronized to compute joint kinematics and kinetics [26].
Gait Assessment Workflow
The following diagram illustrates the general workflow for conducting a gait assessment study, from participant preparation to data interpretation, which is common across technologies but differs in the core measurement step.
The Scientist's Toolkit: Essential Research Reagent Solutions
This section details key materials and tools required for conducting gait analysis research.
Table 3: Essential Reagents and Tools for Gait Analysis Research
| Item | Function/Application | Examples & Specifications |
|---|---|---|
| Electronic Walkway | Captures footfall patterns to compute spatiotemporal gait parameters in a controlled setting. | GAITRite system (CIR Systems Inc.) with an active sensor area [23] [25]. |
| 3D Motion Capture System | Provides gold-standard, comprehensive analysis of body movement in three dimensions, including joint kinematics and kinetics. | Vicon or similar optoelectronic system with infrared cameras and force plates [26]. |
| Inertial Measurement Units (IMUs) | Wearable sensors for capturing gait data outside the lab. Can be standalone or embedded in smartphones. | Gait Up Physilog5 [26]; Smartphone accelerometers (e.g., Samsung Galaxy S20) [28]. |
| Data Processing Software | Transforms raw sensor data into quantifiable gait metrics and facilitates statistical analysis. | GAITRite Platinum software [23]; Custom algorithms (e.g., in Visual Studio) [28]. |
| Standardized Walkway | Provides a designated, clear path for walking trials to ensure consistency across measurements. | A straight, level path of sufficient length (e.g., with 2m acceleration/deceleration zones) [28]. |
| XAC | XAC, MF:C21H28N6O4.2HCl, MW:501.41 | Chemical Reagent |
| JW67 | JW67, CAS:442644-28-2, MF:C21H18N2O6, MW:394.4 g/mol | Chemical Reagent |
The accurate measurement of weight-bearing ankle dorsiflexion range of motion (ROM) is a critical component in biomechanical research and clinical practice, particularly in the context of evaluating functional recovery in post-surgery ankle fracture patients. Deficits in dorsiflexion are a well-documented impairment following ankle fracture, directly impacting fundamental activities like walking, stair climbing, and squatting [31] [32]. Instrumental gait analysis has revealed that postoperative ankle fracture patients exhibit significant alterations in gait parameters, including reduced walking speed, shorter step length, and lower peak dorsiflexion angular velocity compared to healthy individuals [11] [17]. This comparative analysis examines the primary techniques for assessing weight-bearing dorsiflexion ROM, with a specific focus on their application in research comparing postoperative ankle fracture patients with healthy controls.
Comparative Analysis of Measurement Techniques
Reliability and Measurement Error of Primary Techniques
Table 1: Comparative reliability and measurement parameters of weight-bearing dorsiflexion assessment techniques
| Measurement Technique | Intrarater Reliability (ICC) | Interrater Reliability (ICC) | Standard Error of Measurement (SEM) | Minimal Detectable Change (MDC) |
|---|---|---|---|---|
| Tape Measure (Distance-to-Wall) | 0.98 - 0.99 [33] | 0.80 - 0.99 [33] | 0.4 - 0.6 cm [34] | 1.1 - 1.5 cm [34] |
| Digital Inclinometer | 0.96 - 0.97 [34] | 0.88 [34] | 1.3 - 1.4° [34] | 3.7 - 3.8° [34] |
| Standard Goniometer | 0.85 - 0.96 [34] | 0.89 [34] | 1.8 - 2.8° [34] | 5.0 - 7.7° [34] |
| Smartphone Inclinometer App | 0.72 - 0.82 [35] | 0.65 - 0.73 [35] | Not reported | Not reported |
Table 2: Functional correlates and clinical applications of dorsiflexion measurement techniques
| Technique | Equipment Requirements | Administration Time | Key Advantages | Considerations for Post-Fracture Assessment |
|---|---|---|---|---|
| Weight-Bearing Lunge Test | Tape measure, wall [33] | 5-10 minutes | Excellent reliability, minimal equipment, functional position [33] [34] | Heel contact maintenance may be challenging in early rehabilitation; correlates with gait speed [11] |
| Inclinometer Methods | Digital inclinometer or smartphone with app [34] [35] | 5-10 minutes | Reduced alignment error, digital output [34] | Higher cost; requires tibial tuberosity palpation which may be difficult with edema |
| Goniometer | Standard goniometer [34] | 5-10 minutes | Low cost, widely available [34] | Higher technical proficiency required for alignment [34] |
| Deep Squat Assessment | Camera for video analysis (optional) [32] | 5 minutes | Assesses integrated mobility chain | May be contraindicated in early post-surgical phases |
The quantitative comparison reveals a clear hierarchy in measurement precision. The tape measure method (Weight-Bearing Lunge Test) demonstrates superior reliability coefficients and lower measurement error compared to other techniques [33] [34]. This methodological advantage is particularly relevant in the context of ankle fracture research, where the tape measure's minimal detectable change of 1.1-1.5 cm translates to approximately 4.0-5.4° of dorsiflexion (using the conversion factor of 1 cm ≈ 3.6°) [33]. This sensitivity to change is crucial for detecting clinically meaningful improvements during postoperative rehabilitation.
The functional implications of dorsiflexion limitations are substantial in ankle fracture populations. Research demonstrates that restricted dorsiflexion ROM directly correlates with altered gait patterns, including reduced walking speed, shorter step length, and decreased single-limb support time [11] [17]. These functional deficits persist long-term in a significant subset of patients, with approximately 15% reporting considerable impairment years after surgery, and those with trimalleolar fractures showing the poorest outcomes [36].
Experimental Protocols for Dorsiflexion Assessment
Weight-Bearing Lunge Test (Knee-to-Wall Test) Protocol
Purpose: To assess weight-bearing dorsiflexion range of motion in a functional position that mimics the biomechanical demands of daily activities [33].
Equipment Required: Tape measure (cm), vertical wall surface [33].
Procedure:
- Position the tape measure perpendicular to the wall, secured to the floor [33].
- Instruct the participant to stand facing the wall, barefoot or wearing minimalist shoes [32].
- The participant places the test foot with the great toe aligned at a starting position approximately 10 cm from the wall [34].
- The non-test leg is positioned comfortably or can rest on the floor for support [33].
- The participant is instructed to lunge forward, flexing the knee while keeping the heel firmly planted on the floor [33].
- The knee must move in line with the second toe throughout the movement to control for lower extremity rotation [32].
- If the knee touches the wall comfortably, the foot is moved further from the wall in 1 cm increments until the maximum distance where the knee can just touch the wall without heel lift is identified [33] [34].
- If the knee cannot touch the wall at the initial position, the foot is moved closer until contact is achieved [34].
- The maximum distance from the wall to the tip of the big toe is recorded to the nearest 0.1 cm [34].
- The process is repeated for three trials on each limb, with the average used for analysis [34].
Data Interpretation: Each centimeter of distance corresponds to approximately 3.6° of ankle dorsiflexion [33]. Normative values in healthy young adults typically range from 12-15 cm (approximately 4.5-6 inches) [32].
Considerations for Post-Surgical Assessment: In ankle fracture populations, pain or apprehension may initially limit performance. The non-weight-bearing limb can be positioned for greater support, and participants may use the wall for upper extremity support [33]. The tester should monitor for compensatory movements, particularly heel lift or foot rotation, which invalidate the measurement.
Inclinometer-Based Dorsiflexion Measurement Protocol
Purpose: To obtain direct angular measurement of tibial inclination during weight-bearing dorsiflexion.
Equipment Required: Digital inclinometer or smartphone with inclinometer application (e.g., Spirit Level Plus), wall for support [34] [35].
Procedure:
- The participant assumes the same starting position as the Weight-Bearing Lunge Test [34].
- The participant lunges forward to their maximal dorsiflexion range while maintaining heel contact [34].
- The inclinometer is placed on the distal tibia, approximately 1 cm above the most prominent point of the distal tibia [35].
- For smartphone applications, the device is positioned with its short axis along the tibial shaft [35].
- The inclinometer is zeroed to horizontal before each measurement session [34].
- The angle relative to the horizontal is recorded in degrees [34].
- Three measurements are taken for each limb, with the average used for analysis [34].
Data Interpretation: The angle represents the total dorsiflexion ROM. Normal values typically range from 35-45° in healthy adults, though significant inter-individual variation exists [32].
Technical Considerations: Digital inclinometers demonstrate excellent intrarater reliability (ICC = 0.96-0.97) and reduce measurement error compared to goniometers [34]. Smartphone applications show moderate to good reliability (ICC = 0.65-0.82), offering an accessible alternative with slightly higher measurement error [35].
Diagram 1: Weight-bearing dorsiflexion ROM assessment workflow. This flowchart illustrates the standardized procedure for assessing dorsiflexion using either tape measure or inclinometer methods, highlighting key decision points for accurate measurement.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential equipment for weight-bearing dorsiflexion research
| Tool/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Distance Measurement | Standard metric tape measure | Primary outcome for Weight-Bearing Lunge Test; distance converted to angular equivalent [33] [34] | Ensure perpendicular alignment to wall; measure to nearest 0.1 cm |
| Angular Measurement | Digital inclinometer (e.g., Acumar); Universal goniometer | Direct angular measurement of tibial inclination [34] | Digital inclinometers show higher reliability; zero device to horizontal reference |
| Digital Integration | Smartphone applications (e.g., Spirit Level Plus, TiltMeter) | Accessible alternative to dedicated inclinometers; good validity and reliability [35] | Calibrate before use; ensure consistent device placement |
| Motion Capture | 3D stereophotogrammetry; Inertial Measurement Units (IMUs) | Gold standard for comprehensive gait analysis; captures dynamic dorsiflexion during functional tasks [31] | Requires specialized laboratory setup; provides kinematic data beyond static ROM |
| Pressure Monitoring | Pressure-sensitive walkway; In-shoe pressure systems | Assesses plantar pressure distribution during dorsiflexion; correlates with loading patterns [31] [17] | Identifies compensatory weight-shifting in pathological populations |
| Support Equipment | Adjustable slant boards; Weighted bars | Standardizes foot position; enables progressive overload in intervention studies [32] | Controls for foot orientation; allows quantification of stretch intensity |
| HNHA | HNHA, CAS:926908-04-5, MF:C17H21NO2S, MW:303.4 g/mol | Chemical Reagent | Bench Chemicals |
| Dnca | Dnca, MF:C45H82N4O4, MW:743.2 g/mol | Chemical Reagent | Bench Chemicals |
Methodological Selection in Clinical Research Context
The choice of dorsiflexion assessment method should align with research objectives and patient population characteristics. For large-scale screening or field-based studies, the tape measure method offers an optimal balance of reliability, cost-effectiveness, and practicality [33] [34]. When highest precision is required for biomechanical analysis, digital inclinometers provide superior metrological properties [34]. Smartphone applications represent a viable alternative when budget constraints preclude specialized equipment, though with slightly reduced reliability [35].
In post-surgical ankle fracture research, the functional nature of weight-bearing measurements is particularly relevant. These assessments demonstrate stronger correlation with gait parameters than non-weight-bearing measurements, capturing the integrated neuromuscular control required for daily activities [34] [31]. The persistent dorsiflexion limitations observed in ankle fracture patients [11] [17] underscore the importance of selecting sensitive measurement techniques capable of detecting clinically meaningful change throughout the rehabilitation continuum.
Diagram 2: Decision pathway for dorsiflexion assessment method selection. This algorithm guides researchers in selecting appropriate measurement techniques based on study objectives, population characteristics, and available resources.
The comparative analysis of weight-bearing dorsiflexion measurement techniques reveals distinct advantages and applications for each method. The Weight-Bearing Lunge Test with tape measurement emerges as the most reliable and practical option for clinical research, particularly in studies involving post-surgical ankle fracture patients where functional assessment is paramount. Inclinometer-based methods offer excellent reliability for precise angular measurement, while smartphone applications provide an accessible alternative with moderate reliability. The selection of appropriate assessment methodology is crucial for generating valid, reproducible data on dorsiflexion recovery in ankle fracture populations, ultimately contributing to enhanced rehabilitation strategies and improved functional outcomes.
Integrating Surface EMG with Computerized Dynamic Posturography for Neuromuscular Analysis
The objective quantification of neuromuscular control is essential for understanding postural stability in both clinical and research settings. The integration of surface electromyography (sEMG), which directly records muscle activation patterns, with computerized dynamic posturography (CDP), which quantifies balance performance through center of pressure (COP) movements, provides a comprehensive framework for analyzing the neuromuscular basis of postural control [37]. This multimodal approach is particularly valuable in clinical populations, such as patients recovering from ankle fractures, where disrupted sensorimotor integration leads to significant balance impairments [38] [39]. While CDP output reflects the net result of balance control mechanisms, sEMG illuminates the specific muscular strategies employed to maintain stability [37]. This guide compares the performance of this integrated approach against using either methodology in isolation, providing researchers with experimental data and protocols for implementing this combined assessment strategy.
Comparative Framework: Integrated sEMG-CDP vs. Isolated Techniques
The following table summarizes the core capabilities of the integrated approach compared to the individual technologies.
Table 1: Performance Comparison of Neuromuscular Assessment Techniques
| Assessment Feature | CDP Alone | sEMG Alone | Integrated sEMG-CDP |
|---|---|---|---|
| Balance Output Measure | Directly quantifies COP displacement, Limits of Stability (LOS) [40] [37] | No direct balance output | Directly quantifies COP displacement and LOS |
| Muscle Activation Timing | No muscle-specific data | Directly records onset, duration, and amplitude of muscle activity [38] [41] | Directly records muscle activation patterns |
| Neuromuscular Strategy | Inferred indirectly from COP data [37] | Identifies muscular coordination patterns [42] | Reveals direct relationship between muscle activation and balance output [37] |
| Sensory Integration Analysis | Excellent; can manipulate visual/somatosensory inputs [40] | Limited | Excellent; links sensory conditions to specific muscular responses |
| Clinical Application | Diagnoses balance deficit severity [40] | Identifies impaired muscle control [43] | Pinpoints whether deficit is strategic (muscle use) or mechanical (force output) [38] [37] |
| Data Correlation | Not applicable | Not applicable | Enables cross-correlation of EMG signals with COP trajectories (EMG-COP correlation) [37] |
Experimental Data from Integrated sEMG-CDP Studies
Key Findings in Post-Surgery Ankle Fracture Patients
Integrated assessment reveals specific neuromuscular alterations in patients following bimalleolar ankle fracture surgery, which are not fully discernible through single-modality testing.
Table 2: Summary of Neuromuscular Findings in Ankle Fracture Patients via Integrated Assessment
| Study Parameter | 6 Months Post-Surgery | 12 Months Post-Surgery | Assessment Method |
|---|---|---|---|
| Limb × Muscle Interaction | Significant interaction (F=30.806, p<0.001) in Y-Balance Test anterior direction [38] [39] | Differences diminish | sEMG + Y-Balance Test (Dynamic Balance) |
| Lateral Gastrocnemius Activation | Greater activation associated with limited dorsiflexion ROM [38] [39] | Trend toward normalization | sEMG + Y-Balance Test |
| Proximal (Hip) Muscle Recruitment | Increased reliance on hip strategy during dynamic balance [38] | -- | sEMG of gluteus medius during balance tasks |
| Dynamic Balance Performance | Significantly impaired [38] | Deficits persist, though improved | Y-Balance Test |
Key Findings in Other Neurological and Traumatic Conditions
- Chronic Traumatic Brain Injury (TBI): During CDP reactive balance tests, adults with chronic severe TBI exhibit greater composite lower extremity EMG activity compared to matched controls, correlating significantly with poorer reactive balance performance. This indicates higher physiological effort is required to maintain balance even when independent ambulation is achieved [41].
- Post-Stroke Hemiplegia: Nonlinear network indices of sEMG (e.g., clustering coefficient, degree centrality) derived during standing reveal neuromuscular conditions in ankle-foot dysfunction that are not identified by traditional linear sEMG indices or CDP alone. These include altered inter-muscular coordination and reduced contribution of specific muscles like the medial gastrocnemius to the muscle network [42].
Essential Experimental Protocols for Integrated Assessment
Protocol 1: Static and Dynamic Balance with sEMG
This protocol is adapted from studies on ankle fractures and postural control [38] [37] [39].
1. Participant Preparation:
- sEMG Electrode Placement: Following SENIAM standards, place bipolar surface electrodes on key lower limb muscles. Essential muscles include: Tibialis Anterior (TA), Peroneus Longus (PL), Medial/Lateral Gastrocnemius (MG/LG), Soleus (SOL), Biceps Femoris (BF), and Gluteus Medius [38] [37]. Skin should be shaved, abraded, and cleaned with alcohol to achieve electrode-skin impedance below 6 kΩ [37].
- CDP Calibration: Calibrate the force plate according to manufacturer specifications (e.g., AMTI OR6 series, Bertec Balance Advantage) [40] [37].
2. Experimental Tasks:
- Static Balance: Participants perform bipedal standing on both stable and unstable surfaces for 30-80 seconds, looking straight ahead with hands on hips [37]. A minimum of three trials is recommended.
- Dynamic Balance: Participants perform the Y-Balance Test (YBT), reaching maximally in anterior, posteromedial, and posterolateral directions while standing on a single leg [38] [39]. The Limits of Stability (LOS) test can also be used, where participants volitionally shift their COP toward visual targets [40].
3. Data Collection and Analysis:
- sEMG Data: Record raw signals at a minimum sampling rate of 1500 Hz. Process signals using band-pass filtering (e.g., 20-450 Hz), rectification, and smoothing. Calculate Root Mean Square (RMS) for amplitude and Median Frequency (MF) for spectral analysis [42]. For muscle synergy, compute nonlinear indices like Clustering Coefficient (C) and Degree Centrality (DC) [42].
- CDP Data: Record COP data at 1250 Hz. Calculate traditional sway parameters (path length, velocity, area) and LOS sub-measures: Reaction Time, Directional Control, Movement Velocity, Endpoint Excursion, and Maximum Excursion [40].
- Integrated Analysis: Use cross-correlation analysis to examine the temporal relationship between individual EMG signals and COP displacements in the anteroposterior and mediolateral directions (EMG-COP correlation) [37].
Protocol 2: Reactive Balance with sEMG
This protocol is based on research with neurologically impaired populations like TBI [41].
1. Instrumentation:
- Use a computerized dynamic posturography system capable of delivering unexpected, multi-directional perturbations (e.g., PROPRIO 4000, Bertec Balance Advantage) [40] [41].
- Apply sEMG electrodes as described in Protocol 1 on muscles including Vastus Lateralis, Medial Hamstrings, Tibialis Anterior, and Medial Gastrocnemius [41].
2. Procedure:
- Participants stand on the platform, wearing a safety harness. The system delivers progressively increasing platform tilts (e.g., up to 14° at rates from 6°/s to 60°/s) for 120 seconds or until a balance loss criterion is met [41].
- Multiple trials (e.g., three) should be conducted with rest periods.
3. Data Analysis:
- Reactive Balance Score: Provided by the posturography system based on the magnitude of perturbation tolerated.
- EMG Analysis: Calculate composite EMG activity across all muscles for each epoch of the test. Correlate this composite activity with the overall reactive balance score [41].
Visualization of the Integrated Assessment Workflow
The following diagram illustrates the logical workflow and data integration points for a combined sEMG-CDP assessment.
Integrated sEMG-CDP Assessment Workflow
The Scientist's Toolkit: Key Research Reagents and Equipment
Table 3: Essential Materials for Integrated sEMG-CDP Research
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| High-Density sEMG System | Records myoelectric activity with high spatial resolution to study motor unit properties and muscle excitation [44]. | Systems with 2+ channels per muscle; Delsys Trigno, Noraxon TeleMyo [42] [37]. |
| Computerized Dynamic Posturography System | Precisely quantifies postural sway and reactive balance by measuring center of pressure (COP) [40] [41]. | Bertec Balance Advantage, Neurocom Smart Balance Master, PROPRIO 4000 [40] [41]. |
| Multiaxial Unstable Platform | Challenges the sensorimotor system to reveal compensatory neuromuscular strategies and deficits [37]. | MFT Challenge Disc, wobble boards [37]. |
| Disposable Surface Electrodes | Detects myoelectric signals at the skin surface. Pre-gelled Ag/AgCl electrodes ensure good signal quality. | Bipolar adhesive electrodes (e.g., Ambu Neuroline) with 20-25 mm inter-electrode distance [37]. |
| Skin Preparation Supplies | Reduces skin impedance to improve sEMG signal-to-noise ratio and reduce motion artifacts. | Abrasive gel, alcohol wipes, razors [42] [37]. |
| Signal Processing Software | Processes and analyzes raw sEMG and CDP data to extract relevant metrics and correlations. | MATLAB, Visual3D, custom scripts for nonlinear indices and cross-correlation analysis [42] [41]. |
| Dgts | Dgts, MF:C42H81NO7, MW:712.1 g/mol | Chemical Reagent |
| Dgdg | Dgdg, MF:C51H84O15, MW:937.2 g/mol | Chemical Reagent |
The integration of surface EMG and computerized dynamic posturography moves beyond singular-dimensional assessment to provide a powerful, multi-faceted tool for decoding neuromuscular control. As the comparative data demonstrates, this approach is uniquely capable of linking specific muscle activation patterns—such as the compensatory gastrocnemius activation in ankle fracture patients or the generalized co-contraction in TBI—directly to functional balance outcomes [38] [41]. For researchers conducting comparative analyses of gait and postural control, this methodology offers a more sensitive and informative framework. It not only identifies the presence of a deficit but also illuminates the underlying neuromuscular strategy, thereby guiding the development of more targeted and effective rehabilitation interventions.
Gait analysis is a critical tool for diagnosing mobility issues and monitoring rehabilitation, particularly after orthopedic events such as ankle fractures. Traditional laboratory-based systems, while accurate, are costly and impractical for widespread clinical use [45]. The emergence of smartphone-based gait analysis offers a promising alternative, providing a portable, cost-effective, and accessible means of quantifying gait parameters. This review objectively compares the performance of smartphone-based gait analysis technologies against established alternatives, framed within the critical context of rehabilitating post-surgery ankle fracture patients. We summarize validation data, detail experimental protocols, and provide visual workflows to guide researchers and clinicians in evaluating these novel tools.
Performance Comparison: Smartphone Gait Analysis vs. Alternative Modalities
The following tables synthesize quantitative data on the performance of various gait analysis technologies, with a specific focus on their application in post-surgery ankle fracture recovery.
Table 1: Comparative Performance of Gait Analysis Technologies in Clinical Validation
| Technology | Key Measured Parameters | Validation against Gold Standard | Strengths | Limitations |
|---|---|---|---|---|
| Smartphone (Embedded IMU) | Stride time, step time, swing phase, double support [45] | Moderate to excellent validity for step/stride time (r=0.628-0.977); Poor-moderate for swing/double support [45] | High accessibility, cost-effective, enables mass screening & home monitoring [45] [46] | Lower validity for phase-specific parameters; Requires ~100 steps for reliable data [45] |
| Wearable IMU Systems (e.g., RunScribe, G-Sensor) | Gait speed, stride length, cadence, stance/swing phases [47] | High agreement for speed, length, cadence (ICC>0.90); More variability in stance/swing phases [47] | Reliable home-based monitoring; Provides rich, real-world data [47] | Requires multiple dedicated sensors; Potential for less natural gait with multiple attachments [45] |
| Computer Vision (e.g., iGait) | Spatiotemporal gait parameters from video [48] | Successful deployment in clinical rehab; Low fail rates (<10%) in capturing data [48] | Passive, markerless assessment; Scalable from mono- to multi-camera setups [48] | Emerging technology; Validation metrics and clinical interpretation still developing [48] |
| 3D Motion Capture (VICON) | Comprehensive kinematic data, gait events [45] | Considered the laboratory "gold standard" [45] | High accuracy and reliability for detailed biomechanical analysis [45] | Cost-prohibitive, non-portable, requires specialized lab and operators [45] |
Table 2: Gait Parameter Deficits in Post-Surgery Ankle Fracture Patients vs. Healthy Individuals
| Gait Parameter | Post-Surgery Ankle Fracture Patients vs. Healthy Controls | Clinical Implications |
|---|---|---|
| Walking Speed | Significantly slower (WMD = -0.13 m/s, P < 0.001) [11] [17] [49] | Indicator of overall mobility impairment and functional decline [46] |
| Step Length | Significantly shorter (WMD = -0.15 m, P < 0.001) [11] [17] [49] | Suggests reduced confidence or propulsive force on the injured side [46] |
| Single Support Time | Significantly reduced on injured limb (WMD = -16.59%, P < 0.001) [11] [17] [49] | Reflects pain, instability, or weakness during weight-bearing [17] |
| Cadence | Significantly lower (WMD = -8.44 steps/min, P < 0.001) [11] [17] [49] | Compensatory strategy to improve stability by slowing the gait cycle [17] |
| Peak Dorsiflexion Velocity | Significantly lower (WMD = -7.93 °/s, P = 0.005) [11] [17] | Indicates restricted and altered ankle joint kinematics and push-off [17] |
Experimental Protocols for Key Studies
Smartphone IMU Validation Protocol
A 2025 study established the validity and reliability of a smartphone-based gait assessment application [45].
- Participants: 26 healthy young adults.
- Sensor Placement: A Samsung Galaxy S22 smartphone was fixed horizontally on the waist at the L4-L5 level using a semi-elastic belt.
- Data Collection: Participants walked at a comfortable pace on a 10-meter pathway. Gait data were simultaneously captured by the smartphone's built-in IMU (accelerometer and gyroscope) and a 16-camera VICON motion capture system, with synchronization via a Bluetooth signal.
- Data Processing: Heel strike and toe-off events were detected from the smartphone's sensor signals using a peak detection algorithm. Temporal parameters (stride time, step time, swing phase, double support) were calculated and compared between the two systems.
- Analysis: Concurrent validity was assessed using Pearson's Correlation, and test-retest reliability was examined with Intraclass Correlation Coefficients (ICCs) across two sessions scheduled 1-4 weeks apart [45].
Smartphone-Based Recovery Prediction Protocol
A 2025 study assessed the use of pre-injury smartphone data to predict mobility recovery after lower-extremity fracture [46].
- Study Design: Retrospective cohort study of 107 patients with surgically treated pelvic or lower-extremity fractures.
- Data Extraction: Consenting patients exported historical mobility metrics collected passively by their Apple iPhones via the Apple Health app. Data included step count, walking speed, step length, walking asymmetry, and double-support time from up to a year before the injury.
- Data Analysis: Pre-injury mobility baselines were established from data from the 6 months preceding the injury. Post-fracture outcomes were parameterized weekly. Nonlinear models were used to predict post-injury mobility, adjusting for age, sex, fracture location, and other covariates [46].
Multi-Pathology Gait Dataset Protocol
A 2025 study created a large, open-access dataset to support the development of gait analysis algorithms [50].
- Participants: 260 individuals, including healthy controls and patients with neurological or orthopedic conditions.
- Sensor System: Participants were equipped with four synchronized IMUs placed on the head, lower back (L4/L5), and the dorsal part of each foot.
- Protocol: A standardized test involved standing still, walking 10 meters, turning around, walking back, and stopping. This resulted in over 11 hours of gait time-series data, annotated with relevant clinical scores for each pathology [50].
Workflow and Pathway Diagrams
Smartphone Gait Analysis Workflow
The following diagram illustrates the end-to-end process for conducting and validating smartphone-based gait analysis, from data collection to clinical application.
Ankle Fracture Recovery Pathway
This diagram outlines the pathological gait profile of ankle fracture patients and how smartphone data can model the recovery process, linking impaired parameters to their functional consequences.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Materials and Tools for Smartphone Gait Analysis Research
| Item | Specification / Example | Primary Function in Research |
|---|---|---|
| Smartphone with IMU | Samsung Galaxy S22 (LSM6DSO IMU) [45] / Apple iPhone (Health app) [46] | Primary data collection device; captures raw accelerometer and gyroscope signals during gait. |
| Gold-Standard Validation System | VICON Nexus 2 (16-camera system) [45] | Provides criterion measure for validating the accuracy of smartphone-derived gait parameters. |
| Dedicated IMU Sensors | XSens, Technoconcept I4 Motion, G-Sensor [50] [47] | Used as alternative wearable benchmarks or to create multi-sensor reference datasets. |
| Data Synchronization Tool | Arduino-produced analogue signal via Bluetooth [45] | Precisely synchronizes the start time of smartphone data collection with gold-standard systems. |
| Adhesive Straps & Belts | Manufacturer-designed straps, semi-elastic belt [45] [50] | Securely fixes sensors or smartphones to standardized body locations (e.g., waist, feet). |
| Algorithm & Software Packages | Peak detection algorithm [45], R packages (e.g., scam, splines) [46] | Processes raw sensor data to detect gait events and calculate spatiotemporal parameters. |
| Standardized Clinical Scores | Disease-specific clinical/radioclinical scores [50] | Provides essential clinical context and ground truth for correlating gait parameters with pathology severity. |
| (4R)-4-Decanol | (4R)-4-Decanol, CAS:138256-82-3, MF:C10H22O, MW:158.28 g/mol | Chemical Reagent |
| PROTAC SMARCA2 degrader-3 | PROTAC SMARCA2 degrader-3, MF:C37H42N8O4, MW:662.8 g/mol | Chemical Reagent |
Rehabilitation Challenges and Protocol Optimization: Addressing Strength and Functional Asymmetries
Post-surgical immobilization and disuse trigger rapid and pronounced muscle atrophy and strength loss, presenting a significant clinical challenge in rehabilitation. Disuse atrophy (DA) particularly affects anti-gravitational muscles such as the quadriceps and calf muscles, with research indicating that spaceflight-induced DA results in approximately 15% muscle loss in quadriceps and gastrocnemius within just two weeks [51]. Similarly, 15 days of immobilization causes a significant decline in both volume (-2.8%) and thickness (-12.9%) of the medial gastrocnemius muscle [51]. This rapid deterioration of muscle tissue directly impairs functional capacity, as evidenced by studies of postoperative ankle fracture patients who exhibit significant impairments in gait parameters, muscle strength, and plantar pressure distribution compared to healthy individuals, often failing to regain pre-injury functional levels despite rehabilitation [11].
The relationship between muscle atrophy and strength deficits is particularly pronounced in peak torque production - the maximum torque output generated by a muscle group, which is crucial for functional movements. Middle-aged and older adults demonstrate notable declines in knee extensor peak torque, with studies revealing that knee extensor strength declines annually by 1.1-1.4% in adults aged 40-59 years [52]. This deterioration occurs even in the absence of significant changes in muscle mass, suggesting that neuromuscular factors substantially contribute to functional limitations [52]. In postoperative populations, these deficits become even more pronounced, creating a compelling clinical imperative for targeted strength training protocols specifically designed to overcome muscle atrophy and peak torque deficits.
Comparative Analysis of Functional Deficits in Post-Surgical Patients
Quantitative assessments of postoperative ankle fracture patients reveal persistent functional deficits despite surgical intervention and standard rehabilitation. A systematic review and meta-analysis comprising 12 studies and 219 patients demonstrated that postoperative ankle fracture patients exhibit significant impairments across multiple gait parameters compared to healthy controls [11]. These patients showed slower walking speed (WMD = -0.13, 95% CI [-0.45, -0.16], P < 0.001), reduced peak dorsiflexion angular velocity (WMD = -7.93, 95% CI [-13.45, -2.41], P = 0.005), and shorter mean step length (WMD = -0.15, 95% CI [-0.18, -0.12], P < 0.001) [11]. Single support time was also significantly reduced (WMD = -16.59, 95% CI [-19.18, -14.00], P < 0.001), along with significantly lower cadence (WMD = -8.44, 95% CI [-10.87, -6.01], P < 0.001) [11].
Long-term functional analyses confirm these deficits persist years after surgery. A prospective study of individuals with unilateral trimalleolar fractures at 4.5-year follow-up revealed that the surgical side exhibited significantly reduced heel rise height and limited ankle dorsiflexion despite high American Orthopaedic Foot and Ankle Society (AOFAS) and Olerud-Molander Ankle Score (OMAS) scores [16]. These functional limitations directly impact quality of life, with weight-bearing ankle dorsiflexion range of motion during deep squat sitting significantly correlating with multiple domains of the Self-Administered Foot Evaluation Questionnaire (SAFE-Q), including pain and pain-related symptoms, physical functioning, social functioning, and general health [12].
Table 1: Comparative Gait Parameters Between Post-Surgery Ankle Fracture Patients and Healthy Individuals
| Gait Parameter | Healthy Individuals | Post-Surgery Ankle Fracture Patients | Statistical Significance |
|---|---|---|---|
| Walking Speed | Normal | Slower (WMD = -0.13) | P < 0.001 |
| Peak Dorsiflexion Angular Velocity | Normal | Reduced (WMD = -7.93) | P = 0.005 |
| Step Length | Normal | Shorter (WMD = -0.15) | P < 0.001 |
| Single Support Time | Normal | Reduced (WMD = -16.59) | P < 0.001 |
| Cadence | Normal | Lower (WMD = -8.44) | P < 0.001 |
| Muscle Strength | Normal | Notably reduced | P < 0.05 |
| Plantar Pressure | Normal distribution | Significantly altered | P < 0.05 |
Resistance Exercise Training as a Countermeasure for Disuse Atrophy
Substantial evidence supports the efficacy of resistance exercise training (RET) in attenuating disuse-induced muscle atrophy and strength loss. A comprehensive meta-analysis of randomized controlled trials demonstrated that RET elicits substantial benefits for preserving quadriceps muscle volume (n = 5, MD = 252.56, 95% CI = 151.92, 353.21, p < 0.001) during immobilization/disuse conditions [51]. RET also demonstrated a statistically significant preventive effect on the reduction of maximal voluntary contraction (MVC) in both quadriceps (n = 4, MD = 338.59, 95% CI = 247.49, 429.69, p < 0.001) and calf muscles (n = 3, MD = 478.59, 95% CI = 160.42, 796.77, p < 0.01) [51].
The mechanisms through which RET preserves muscle function extend beyond volume maintenance to include specific torque-related parameters. RET significantly improved peak power of quadriceps muscles (n = 4, MD = 166.08, 95% CI = 28.44, 303.73, p < 0.05) and calf muscles (n = 2, MD = 176.58, 95% CI = 102.36, 250.79, p < 0.001) [51]. Furthermore, RET significantly ameliorated the weakening of both concentric and eccentric peak force in quadriceps (concentric: n = 2, MD = 470.95, 95% CI = 355.45, 586.44, p < 0.001; eccentric: n = 1, MD = 351.51, 95% CI = 254.43, 448.58, p < 0.001) and calf muscles (concentric: n = 2, MD = 867.52, 95% CI = 548.18, 1186.86, p < 0.001; eccentric: n = 1, MD = 899.86, 95% CI = 558.17, 1241.55, p < 0.001) [51]. These findings collectively indicate that RET effectively minimizes deterioration of muscle volume and muscle function during immobilization/disuse, particularly in anti-gravitational muscles most susceptible to disuse atrophy.
Table 2: Efficacy of Resistance Exercise Training on Muscle Volume and Function During Disuse
| Outcome Measure | Muscle Group | Effect Size (Mean Difference) | Statistical Significance |
|---|---|---|---|
| Muscle Volume Preservation | Quadriceps | MD = 252.56, 95% CI = 151.92, 353.21 | P < 0.001 |
| MVC Maintenance | Quadriceps | MD = 338.59, 95% CI = 247.49, 429.69 | P < 0.001 |
| MVC Maintenance | Calf Muscles | MD = 478.59, 95% CI = 160.42, 796.77 | P < 0.01 |
| Peak Power Improvement | Quadriceps | MD = 166.08, 95% CI = 28.44, 303.73 | P < 0.05 |
| Peak Power Improvement | Calf Muscles | MD = 176.58, 95% CI = 102.36, 250.79 | P < 0.001 |
| Concentric Peak Force | Quadriceps | MD = 470.95, 95% CI = 355.45, 586.44 | P < 0.001 |
| Eccentric Peak Force | Quadriceps | MD = 351.51, 95% CI = 254.43, 448.58 | P < 0.001 |
Advanced Training Modalities for Severe Deficits
Blood Flow Restriction Training
For patients with severe, persistent muscle atrophy and strength deficits that have proven resistant to conventional rehabilitation, blood flow restriction training (BFRT) has emerged as a promising therapeutic intervention. A clinical study involving patients with chronic atrophic postoperative quadriceps and hamstrings muscles demonstrated that BFRT produced statistically significant improvements in peak quadriceps and hamstring torque measurements after just 9 sessions, with continued improvements observed after 18 sessions [53]. These improvements occurred in patients who had participated in closely supervised postoperative therapy programs for an average of 5.3 months after knee surgery without demonstrating previous improvement in quadriceps and hamstring strength [53]. The mechanism of BFRT involves partially restricting arterial inflow and fully restricting venous return in the proximal portion of the limb during low-intensity resistance exercise (typically 20-30% of 1 repetition maximum), creating a metabolic environment that stimulates muscle hypertrophy and strength gains comparable to those achieved with high-intensity training.
Progressive Resistance Training
Progressive resistance training (PRT) represents another evidence-based approach for addressing peak torque deficits, particularly in vulnerable populations such as older adults with demonstrated mobility limitations. A randomized controlled trial involving mobility-limited older adults (Short Physical Performance Battery [SPPB] ≤ 9) compared PRT to home-based flexibility training three times per week for 12 weeks [54]. At follow-up, the PRT group improved significantly in torque capacity, with a mean between-group difference of 466.19 (95% CI: 138.4, 793.97) Nm (p = .006), and maximal strength 127.3 (95% CI: 60.96, 193.61) Nm (p = .0003) compared to the flexibility group [54]. The PRT protocol consisted of leg press, seated row, leg extension, chest press, and leg curl exercises, with participants initially performing two sets of 10 repetitions progressing to three sets of 12 repetitions throughout the 12-week intervention period at 80% of their 1 repetition maximum [54].
Molecular and Neuromuscular Adaptations to Strength Training
The functional improvements observed following resistance training protocols are supported by underlying molecular and neuromuscular adaptations. Resistance training induces significant neuromuscular adaptations that enhance maximum strength and functional capacity [55]. A systematic review and meta-analysis of 20 studies revealed a significant effect of resistance training on maximal skeletal muscle strength (SMD = 0.77, 95% CI 0.57-0.98, P < 0.05), while 54 studies examining the relationship between resistance training and peak torque demonstrated similarly significant effects (SMD = 0.77, 95% CI 0.62-0.93, P < 0.05) [55].
At the molecular level, maximal resistance training activates satellite cells and the mTOR signaling pathway, contributing to muscle repair, hypertrophy, and strength improvement [55]. Structural muscle adaptations include increased agonist muscle thickness, a higher proportion of Type I and Type IIa fibers, a reduction in Type IIx fibers, and an increase in pennation angle [55]. Neural adaptations are reflected in heightened EMG amplitude, though the effect size varies with muscle contraction type and training experience [55]. These multifaceted adaptations collectively contribute to the improvement in peak torque production and functional capacity observed following targeted resistance training interventions.
Molecular and Neuromuscular Adaptations to Resistance Training
Experimental Protocols and Methodologies
Resistance Training During Disuse
The efficacy of RET in preventing disuse-induced muscle atrophy and peak torque deficits has been established through rigorous randomized controlled trials. These studies typically employ comprehensive RET protocols implemented during periods of immobilization, bed rest, or unilateral lower-limb suspension [51]. The exercise regimens generally include concentric, eccentric, and isometric muscle contractions performed against external resistance, with training frequency typically ranging from 3-5 sessions per week [51]. Intensity is progressively increased throughout the intervention period based on individual tolerance and objective measures of strength capacity. Outcome measures include muscle volume quantification through magnetic resonance imaging (MRI), maximal voluntary contraction (MVC) testing, isokinetic dynamometry for peak torque assessment, and functional performance tests specific to the muscle groups being studied [51].
Blood Flow Restriction Training Protocol
The BFRT protocol for severe postoperative muscle atrophy involves the application of a pneumatic cuff to the proximal portion of the affected limb, with pressure individualized based on limb circumference and patient characteristics [53]. Training typically consists of low-intensity resistance exercises (20-30% of 1RM) performed to volitional fatigue for 3-4 sets per exercise (1 initial set of 30 repetitions followed by 3 sets of 15 repetitions), with 30-60 seconds rest intervals between sets [53]. The protocol is implemented 2-3 times per week with at least 48 hours between sessions, and progression is achieved through gradual increases in exercise intensity and cuff pressure based on individual tolerance and adaptation [53]. The inclusion criteria for BFRT generally includes postoperative 20% or greater difference from the contralateral extremity in isometric quadriceps or hamstrings strength or 2 cm or greater thigh muscle atrophy compared to the contralateral extremity [53].
Isokinetic Strength Testing Protocol
Standardized isokinetic testing protocols are essential for objectively quantifying peak torque deficits and training-induced improvements. The testing is typically performed using isokinetic dynamometers such as the Biodex System, with participants positioned according to manufacturer guidelines and joint alignment verified [52] [54]. For knee extension peak torque assessment, participants perform 5 repetitions at angular velocities of 60°/s through a defined range of motion (typically 90° to 15° of knee flexion) [52]. For fatigue assessment, protocols may involve 120 maximal effort knee extensions traveling through a range of motion of 75° at a velocity of 120°/s, with a contraction performed every 2 seconds [54]. Participants receive standardized verbal encouragement throughout testing, and gravity correction procedures are implemented to account for limb weight [52]. Peak torque values are typically normalized to body weight (Nm/kg) to enable comparison across individuals [52].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Equipment for Muscle Function Studies
| Research Tool | Specific Function | Application Example |
|---|---|---|
| Isokinetic Dynamometer | Quantifies peak torque, work, and power during controlled movements | Measuring knee extension peak torque at 60°/s angular velocity [52] [54] |
| Magnetic Resonance Imaging (MRI) | Precisely measures muscle volume, cross-sectional area, and fatty infiltration | Quantifying quadriceps muscle volume changes during disuse and rehabilitation [51] [56] |
| Electromyography (EMG) | Records electrical activity associated with muscle contraction | Assessing neural adaptations and motor unit recruitment patterns [55] |
| ELISA Kits | Quantifies circulating biomarkers of neuromuscular status | Measuring serum neurofilament light chain (NfL) and C-terminal agrin fragment (CAF) [52] |
| Gait Analysis Systems | Objectively assesses spatiotemporal gait parameters | Evaluating step length, single support time, and cadence in postoperative patients [11] [16] |
| Blood Flow Restriction Cuffs | Applies precise external pressure to partially restrict blood flow | Implementing BFRT protocols with low-intensity resistance exercise [53] |
The evidence collectively demonstrates that targeted strength training protocols effectively counteract disuse-induced muscle atrophy and peak torque deficits across diverse clinical populations. Resistance exercise training preserves muscle volume and function during immobilization, while specialized approaches like blood flow restriction training and progressive resistance training address more severe or persistent deficits. The molecular and neuromuscular adaptations underlying these improvements include enhanced neural drive, activation of hypertrophic signaling pathways, and favorable structural changes in muscle architecture.
These findings have significant implications for rehabilitation following surgical procedures such as ankle fracture fixation, where persistent functional deficits commonly impair quality of life despite anatomical restoration. Future research should focus on optimizing training parameters for specific patient populations, exploring combinations of different training modalities, and investigating the potential role of pharmacological agents in augmenting exercise-induced adaptations. Additionally, more studies are needed to examine the translation of strength improvements to meaningful functional outcomes and quality of life measures in postoperative patients.
Regaining symmetrical gait remains a significant challenge for patients recovering from lower limb surgeries, particularly ankle fractures. Quantitative gait analysis reveals that despite surgical intervention and rehabilitation, postoperative patients often exhibit persistent deficits in critical gait parameters compared to healthy individuals. This comparative analysis examines the specific alterations in single-limb support and step length—two fundamental components of efficient locomotion—and evaluates evidence-based strategies for their correction. The profound impact of these asymmetries on functional mobility underscores their importance as therapeutic targets in rehabilitation protocols.
Research demonstrates that ankle fracture patients exhibit significant impairments across multiple gait domains long after surgical healing. A recent systematic review and meta-analysis of 12 studies comparing 219 postoperative ankle fracture patients with 192 healthy controls revealed statistically significant deficits in walking speed, step length, and single support time [1] [11]. These parameters are not merely clinical metrics but reflect fundamental alterations in locomotor control that impact patients' ability to perform daily activities and return to pre-injury function levels.
Quantitative Comparison: Post-Surgical Patients vs. Healthy Controls
The table below summarizes key gait parameter differences between post-surgery ankle fracture patients and healthy individuals, based on meta-analytical findings:
Table 1: Gait Parameter Comparisons Between Post-Surgery Ankle Fracture Patients and Healthy Individuals
| Gait Parameter | Healthy Individuals | Post-Surgery Ankle Fracture Patients | Weighted Mean Difference (WMD) | Statistical Significance |
|---|---|---|---|---|
| Walking speed | Normal self-selected speed | Significantly slower | -0.13 m/s (95% CI: -0.45, -0.16) | P < 0.001 |
| Step length | Normal stride | Significantly shorter | -0.15 m (95% CI: -0.18, -0.12) | P < 0.001 |
| Single support time | Normal single-leg stance | Significantly reduced | -16.59 (95% CI: -19.18, -14.00) | P < 0.001 |
| Cadence | Normal step frequency | Significantly lower | -8.44 steps/min (95% CI: -10.87, -6.01) | P < 0.001 |
| Peak dorsiflexion angular velocity | Normal range | Significantly reduced | -7.93°/s (95% CI: -13.45, -2.41) | P = 0.005 |
| Peak plantarflexion angular velocity | Normal range | Reduced but not statistically significant | -49.64°/s (95% CI: -99.98, 0.71) | P = 0.053 |
Data sourced from systematic review and meta-analysis of 12 studies comprising 219 patients and 192 controls [1] [11]
Beyond these quantitative differences, patients also demonstrate notable reductions in muscle strength and alterations in plantar pressure distribution during gait [1]. These findings suggest that the functional impairments extend beyond simple kinematic alterations to include fundamental changes in force generation and weight-bearing capacity, which must be addressed through targeted rehabilitation strategies.
Experimental Approaches for Studying Gait Asymmetry
Constraint-Induced Asymmetry Models
Researchers have developed sophisticated experimental protocols to study gait adaptations under controlled asymmetric conditions. One innovative approach utilizes a within-subject design with a unilateral knee constraint to emulate hemiparetic gait, effectively isolating the effects of functional asymmetry while eliminating inter-individual variability [57].
Table 2: Key Methodological Components of Constraint-Induced Asymmetry Studies
| Component | Specification | Research Application |
|---|---|---|
| Participants | 19 neurotypical young adults (age 30±8 years) | Within-subject control design |
| Constraint Type | Passive knee brace locked in full extension (0°) on left leg | Emulates reduced knee flexion in hemiparetic gait |
| Walking Speeds | 0.4, 0.8, and 1.1 m/s | Tests adaptations across functional speeds |
| Cadence Variations | 90%, 95%, 100%, 110%, 120% of preferred cadence | Examines speed-frequency interactions |
| Data Collection | Marker data (100 Hz), GRF (1000 Hz) | Comprehensive biomechanical analysis |
| Trial Structure | 5-minute trials, 30 total conditions | Robust within-session data collection |
Methodology adapted from BaÄek et al. (2024) as cited in Frontiers in Bioengineering and Biotechnology [57]
This methodological approach reveals that functional asymmetry disproportionately impacts propulsion mechanics, with constrained-leg push-off force decreasing significantly at higher speeds, while step length symmetry remains relatively stable [57]. This suggests a neural prioritization of spatial over kinetic symmetry, likely to optimize walking energetics and maintain anterior-posterior balance.
Comprehensive Gait Asymmetry Assessment
The Combined Gait Asymmetry Metric (CGAM) provides researchers with a sophisticated tool for synthesizing multiple gait parameters into a unified asymmetry index. This metric employs modified Mahalanobis distances to combine asymmetries across spatial, temporal, kinematic, and kinetic parameters, effectively balancing the influence of each parameter through normalization [58] [59].
The CGAM algorithm follows this calculation method:
Symmetry Index Calculation:
Modified CGAM Calculation:
Where:
- Data = matrix with n columns (parameters) and m rows (number of steps)
- Σ = covariance of the data
- inv(Σ) = inverse covariance matrix [58]
This comprehensive approach is particularly valuable when assessing therapeutic interventions, where improvements in one parameter may come at the expense of another. Research demonstrates that CGAM effectively captures overall gait changes that correlate with functional clinical measures, showing strong correlation with the 6-minute walk test and gait velocity [58] [60].
The following diagram illustrates the integrated workflow for gait asymmetry assessment and intervention evaluation:
Figure 1: Comprehensive Gait Asymmetry Assessment Workflow
Research Toolkit: Essential Reagents and Equipment
Table 3: Essential Research Toolkit for Gait Asymmetry Investigation
| Tool/Equipment | Specification | Research Application |
|---|---|---|
| 3D Motion Capture System | Multi-camera setup (100Hz recommended) | Captures kinematic data and segment trajectories |
| Instrumented Treadmill | Dual-belt with force plates (1000Hz) | Collects ground reaction forces during walking |
| Custom Knee Orthosis | 3D-printed cuffs with locking mechanism (0° extension) | Induces functional asymmetry for controlled studies |
| OptoGait System | Optical measurement system | Precisely measures spatio-temporal parameters |
| CGAM Algorithm | Modified Mahalanobis distance calculation | Computes composite asymmetry scores from multiple parameters |
| Metronome Pacing System | Auditory cadence cues (90-120% preferred cadence) | Controls walking cadence across experimental conditions |
| Electromyography | Surface EMG sensors | Monitors muscle activation patterns |
| Computer Vision Algorithms | Pose estimation from video | Extracts gait parameters from 2D video recordings [10] |
Correction Strategies for Single-Limb Support and Step Length Asymmetries
Targeted Asymmetry Rehabilitation
Emerging evidence suggests that traditional approaches aiming for perfect symmetry may be misguided. Instead, contemporary rehabilitation embraces the concept of balanced asymmetry, where the goal is to optimize overall function rather than achieve perfect symmetry in all parameters [60]. This approach recognizes that individuals with physical impairments are inherently asymmetric systems and attempts to force perfect symmetry may lead to compensatory patterns that are detrimental long-term.
Research using the Gait Enhancing Mobile Shoe (GEMS) demonstrates that providing asymmetric training can improve functional outcomes. Patients trained with GEMS showed improvements in clinical measures such as timed up and go (TUG) and six-minute walk test (6MWT), despite showing lower step length symmetry as intended by the device [60]. This suggests that strategically manipulating specific asymmetric parameters can lead to overall functional improvements.
Biofeedback and Split-Belt Training
Biofeedback strategies that target specific gait parameters show promise for correcting single-limb support and step length asymmetries. Studies indicate that individuals naturally prioritize spatial symmetry (step length) over kinetic symmetry (propulsion forces) when adapting to asymmetric constraints [57]. This understanding allows researchers to design biofeedback protocols that specifically target the most compromised parameters.
Split-belt treadmill training has emerged as a particularly effective intervention for addressing temporal and spatial asymmetries. This approach uses two independently controlled treadmill belts to create asymmetric walking conditions, which can be calibrated to each patient's specific deficit pattern. Studies with transfemoral amputees have shown definitive improvements in double limb support, swing time, and step length symmetry following split-belt training [60]. The aftereffects of this training often transfer to overground walking, making it a valuable clinical tool.
Proprioceptive and Strength Training
The significant reductions in single-limb support time observed in postoperative patients [1] highlight the importance of interventions targeting weight-bearing capacity and proprioceptive control. Targeted strength training of the plantar flexors is particularly crucial, as propulsive force generation strongly correlates with step length and walking speed.
Studies implementing distal mass addition to the non-paretic limbs of stroke victims have shown improvements in walking speed, step length, cadence, and weight bearing on the paretic limb [59]. This approach leverages the biomechanical principles of limb dynamics to alter movement patterns, though researchers must carefully consider the energy costs associated with such interventions.
The comparative analysis between postoperative ankle fracture patients and healthy individuals reveals persistent deficits in single-limb support and step length that transcend simple structural healing. Effective correction strategies must address the complex interplay between spatial, temporal, and kinetic parameters through targeted, individualized approaches. Contemporary rehabilitation paradigms are shifting from pursuing perfect symmetry toward optimizing functional asymmetry through technologies like instrumented biofeedback, split-belt training, and comprehensive assessment metrics like CGAM.
Future research directions should focus on developing more sophisticated predictive models that can guide personalized intervention protocols, incorporating advances in artificial intelligence and wearable sensor technology [61]. By embracing the inherent asymmetry of impaired gait and strategically targeting the most functionally limiting parameters, researchers and clinicians can develop more effective rehabilitation strategies that restore meaningful mobility and quality of life for patients with gait impairments.
Proprioceptive and Neuromuscular Retraining for Dynamic Stability and Fall Prevention
This comparative analysis examines the efficacy of proprioceptive and neuromuscular retraining against alternative interventions for restoring dynamic stability and preventing falls, with a specific focus on post-surgery ankle fracture patients. Synthesizing data from randomized controlled trials and systematic reviews, we quantify the effects of various interventions on biomechanical parameters, fall rates, and functional outcomes. Proprioceptive training demonstrates significant advantages in improving joint position sense, dynamic balance, and neuromuscular control, contributing to a 23-50% reduction in fall and injury recurrence rates across patient populations. This review provides evidence-based protocols and comparative outcome measures to guide clinical practice and future research in postoperative rehabilitation.
Regaining dynamic stability following surgical ankle fixation represents a critical rehabilitation challenge, with proprioceptive deficits significantly contributing to persistent gait abnormalities and increased fall risk. Proprioception, defined as the neural process of sensing joint position, movement, and force, serves as a fundamental component of neuromuscular control and dynamic joint stability [62]. Following musculoskeletal injury and surgery, this afferent feedback pathway becomes disrupted, creating a deficit that impairs protective reflexes and motor coordination [63] [62].
Neuromuscular retraining encompasses therapeutic interventions designed to reprogram the central nervous system's interpretation of sensory information and execution of motor responses. Within the context of post-surgical ankle fracture recovery, the comparative effectiveness of different therapeutic approaches—ranging from proprioceptive training to bracing and strength training—remains a pivotal clinical question. This review systematically evaluates experimental data to determine how proprioceptive and neuromuscular interventions impact gait parameters, dynamic stability, and fall prevention outcomes compared to alternative strategies, providing evidence-based guidance for optimizing rehabilitation protocols in this vulnerable patient population.
Comparative Efficacy of Interventions for Stability and Fall Prevention
Quantitative Comparison of Intervention Outcomes
Table 1: Comparative Efficacy of Interventions for Stability and Fall Prevention
| Intervention Type | Primary Population | Key Outcome Measures | Reported Efficacy | Comparative Effect Size |
|---|---|---|---|---|
| Proprioceptive/Neuromuscular Training | Chronic Ankle Instability [63] | Ankle Inversion Discrimination (AIDAL) | Significantly improved vs. controls (p<0.001, d=0.78) | Large effect |
| Older Adults [64] [65] | Fall Incidence | 23-34% reduction in fall rates | Moderate to large effect | |
| Athletes [66] [67] | Ankle Sprain Recurrence | ~50% reduction in recurrence | Large effect | |
| Multicomponent Exercise | Community-dwelling older adults [65] | Medically-attended injurious falls | Significant reduction | Moderate effect |
| Older Adults [64] | Balance, Strength, Mobility | Significant improvements | Moderate effect | |
| Bracing | Athletes [68] | Ankle Sprain Recurrence | No significant difference vs. PNT (p=0.97) | Equivalent to PNT |
| Resistance Training | Older Adults [64] [65] | Lower extremity strength, Mobility | Significant improvements | Moderate effect |
Mechanistic Insights into Intervention Efficacy
The superior performance of proprioceptive and neuromuscular training interventions stems from their targeted approach to addressing underlying sensorimotor deficits. Following injury, damage to mechanoreceptors in joints, muscles, and ligaments creates impaired sensory feedback, disrupting the efferent neuromuscular control essential for dynamic stability [67]. Proprioceptive training directly addresses this impairment by re-educating the neuromuscular system to process afferent signals more effectively and execute appropriate stabilizing responses.
The comparative effectiveness of different interventions appears population-dependent. For instance, while bracing provides immediate mechanical support and shows equivalent efficacy to PNT in reducing ankle sprain recurrence in athletes [68], it does not address the underlying neuromuscular impairment. In contrast, active movement interventions yield the most significant gains in sensorimotor function for most populations, likely because they engage the neuromuscular system in integrated, functional patterns that enhance motor learning and cortical adaptation [69]. For older adults and postoperative patients, multicomponent interventions that integrate strength, balance, and proprioceptive elements demonstrate particular efficacy by addressing multiple physiological contributors to instability simultaneously [64] [65].
Experimental Methodologies and Assessment Protocols
Standardized Proprioceptive and Neuromuscular Assessment
Table 2: Standardized Methodologies for Assessing Proprioception and Dynamic Stability
| Assessment Method | Measured Parameters | Protocol Details | Population Applications | Reliability/Validity |
|---|---|---|---|---|
| Ankle Inversion Discrimination Apparatus for Landing (AIDAL) [63] | Proprioceptive discrimination during functional task | Participants jump from platform, land on inclined surfaces (10°, 12°, 14°, 16° inversion); identify angles without visual cues | Chronic Ankle Instability; Post-surgical populations | Good test-retest reliability |
| Joint Position Sense Error (JPSE) [69] | Active and passive joint position sense accuracy | Therapist moves joint to target angle; participant actively reproduces position without visual feedback | Neurological populations; Older adults; Joint injury | High feasibility for clinical use |
| Dynamic Balance Measures [70] | Dynamic gait index, Mini-BESTest, Timed Up and Go | Functional tasks including transitions, walking, turns, dual-task conditions | Multiple sclerosis; Older adults; Fall-risk populations | Mini-BESTest shows 86% specificity for identifying fallers |
| Electromyography (EMG) Analysis [63] | Muscle activation timing, amplitude, coordination | Surface electrodes on key muscles (e.g., tibialis anterior, medial gastrocnemius) during functional tasks | Sports science; Neuromuscular rehabilitation | High temporal resolution |
Key Intervention Protocols
Proprioceptive Training Regimen: Evidence supports protocols utilizing 2-3 sessions per week over 12-week periods as optimal for inducing significant neuromuscular adaptations [67]. Sessions typically progress from static stable surface exercises (single-leg stands) to dynamic unstable surface challenges (balance pad activities), with eventual incorporation of sport-specific or ADL-specific movements [66] [67]. The progression should systematically reduce visual input (eyes closed), incorporate dual-task challenges, and increase movement complexity to continually challenge the sensorimotor system [70].
Multicomponent Exercise Program: The Otago Exercise Programme exemplifies an evidence-based approach integrating strength, balance, and functional training [71]. Protocols typically include lower limb strengthening using resistance bands (2-3 sets of 8-15 repetitions targeting hip and ankle musculature), balance retraining (tandem stance, single-leg standing, walking turns), and functional activities like sit-to-stand transitions [65] [71]. Programs are typically delivered twice weekly for 10 weeks, with session duration progressing from 30 to 60 minutes as tolerance improves [71].
Neurophysiological Pathways and Mechanisms
Proprioceptive Signaling and Neuromuscular Integration
Diagram Title: Neuromuscular Signaling Pathway for Joint Stability
The neurophysiological mechanism underlying proprioceptive training effects involves complex neural pathways that detect, process, and respond to joint position and movement. Peripheral mechanoreceptors (muscle spindles, Golgi tendon organs, joint capsule receptors) detect mechanical deformation from joint movement and transmit signals via afferent pathways through the spinal cord to central processing centers [67]. The cerebellum acts as the primary integration center, comparing intended movement with actual body position and coordinating precise temporal muscle activation patterns [62].
Proprioceptive and neuromuscular retraining enhances dynamic stability by targeting three levels of motor control: spinal reflexes for rapid automated responses, cognitive programming for voluntary movement strategies, and brainstem activity for postural control and balance adjustments [62]. This multi-level approach explains why active movement interventions yield superior results compared to passive support devices, as they engage the entire sensorimotor system in functional patterns that promote neuromuscular adaptation and cortical reorganization [69].
Research Reagents and Methodological Tools
Essential Research Materials for Proprioceptive Studies
Table 3: Key Research Reagents and Methodological Tools
| Tool/Reagent Category | Specific Examples | Primary Function | Research Application |
|---|---|---|---|
| Electromyography Systems | Noraxon EMG System [63] | Quantifies muscle activation timing, amplitude, and coordination | Assessing neuromuscular control deficits; Measuring intervention efficacy |
| Proprioceptive Assessment Apparatus | Ankle Inversion Discrimination Apparatus for Landing (AIDAL) [63] | Measures proprioceptive discrimination during functional landing tasks | Evaluating joint-specific proprioception in CAI and post-surgical patients |
| Dynamic Balance Measures | Mini-BESTest, Berg Balance Scale, Dynamic Gait Index [70] | Assesses dynamic balance during functional tasks and transitions | Identifying fall risk; Quantifying balance improvements in intervention studies |
| Pressure-Sensitive Platforms | Computerized force platforms, Pressure mats [70] | Quantifies center of pressure movement and postural sway | Objective static and dynamic balance assessment |
| Clinical Outcome Measures | Timed Up and Go Test, Falls Efficacy Scale International [71] | Assesses functional mobility and fear of falling | Patient-reported and performance-based outcome measurement |
Proprioceptive and neuromuscular retraining demonstrates significant advantages for restoring dynamic stability and reducing fall risk in post-surgical and vulnerable populations. The evidence confirms that targeted interventions produce superior outcomes compared to generalized exercise programs or passive support devices, with 23-50% reductions in fall and injury recurrence rates across multiple populations. The most effective protocols integrate progressive challenge through unstable surfaces, sensory manipulation, and functional movement patterns delivered in 2-3 weekly sessions over 10-12 week periods.
Future research should prioritize standardized assessment methodologies, particularly for quantifying proprioceptive-specific gains separate from general balance improvements. Further investigation is needed to determine optimal dosing parameters, long-term retention effects, and the neuroplastic mechanisms underlying proprioceptive training benefits. For clinical implementation, protocols should be tailored to specific population needs, with postoperative ankle fracture patients particularly benefiting from early, targeted proprioceptive retraining to address fundamental sensorimotor deficits contributing to gait abnormalities and fall risk.
The management of ankle fractures following surgical intervention has undergone a significant paradigm shift in recent years, transitioning from traditional prolonged immobilization toward evidence-based early mobilization protocols. Structured progressive weight-bearing represents a critical component of modern rehabilitation strategies designed to optimize functional recovery while maintaining fracture stability. Current orthopedic research increasingly demonstrates that early controlled loading, when implemented according to specific protocols, accelerates functional recovery without increasing complication rates [72]. This approach challenges historical practices that emphasized extended non-weight-bearing periods, which often led to detrimental effects including joint stiffness, muscle atrophy, and prolonged disability [73].
The theoretical foundation for progressive weight-bearing rests on the principle of mechanotransduction, whereby controlled mechanical loading stimulates cellular responses that promote bone and soft tissue healing. Biomechanical studies confirm that early axial loading optimizes stress distribution across the healing fracture site [72]. Furthermore, contemporary understanding of ligamentous healing emphasizes that controlled stress application promotes collagen alignment and tensile strength recovery, particularly crucial for patients with concomitant syndesmotic injuries [73]. The integration of progressive weight-bearing within postoperative care pathways therefore represents a convergence of biological understanding and clinical evidence, facilitating a more physiological approach to rehabilitation that aligns with the natural healing processes.
Comparative Analysis of Gait Parameters: Defining the Recovery Benchmark
A fundamental understanding of the gait abnormalities persisting after ankle fracture surgery provides critical benchmarks for evaluating the efficacy of progressive weight-bearing protocols. Comprehensive meta-analyses quantitatively demonstrate that postoperative patients exhibit significant deviations from healthy individuals across multiple spatiotemporal gait parameters [11] [17]. These objective measures serve as crucial indicators for assessing rehabilitation progress and defining recovery milestones.
Table 1: Gait Parameter Comparisons Between Post-Surgery Ankle Fracture Patients and Healthy Individuals
| Gait Parameter | Healthy Individuals | Post-Op Ankle Fracture Patients | Weighted Mean Difference (WMD) | P-value |
|---|---|---|---|---|
| Walking speed (m/s) | Normal | Slower | -0.13 [-0.45, -0.16] | <0.001 |
| Peak dorsiflexion angular velocity (°/s) | Normal | Reduced | -7.93 [-13.45, -2.41] | 0.005 |
| Step length (m) | Normal | Shorter | -0.15 [-0.18, -0.12] | <0.001 |
| Single support time (%) | Normal | Reduced | -16.59 [-19.18, -14.00] | <0.001 |
| Cadence (steps/min) | Normal | Lower | -8.44 [-10.87, -6.01] | <0.001 |
| Peak plantarflexion angular velocity (°/s) | Normal | Reduced | -49.64 [-99.98, 0.71] | 0.053 |
The tabulated data synthesizes findings from twelve studies comprising 219 postoperative ankle fracture patients and 192 healthy controls, revealing statistically significant impairments across nearly all measured parameters [17]. These gait deviations manifest functionally as reduced walking efficiency, increased energy expenditure during ambulation, and alterations in lower extremity kinetics that may predispose patients to secondary complications. Notably, despite comprehensive rehabilitation, many patients fail to fully regain pre-injury levels of walking speed, muscle strength, and normal plantar pressure distribution, highlighting the critical importance of optimized rehabilitation protocols [11].
Long-term follow-up studies further substantiate these findings, with surgical patients demonstrating persistent functional deficits even at 4.5-year follow-up, including reduced heel rise height and limited ankle dorsiflexion despite high American Orthopaedic Foot and Ankle Society (AOFAS) and Olerud-Molander Ankle Score (OMAS) scores [16]. This dissociation between clinical scoring instruments and objective functional measures underscores the necessity of incorporating quantitative gait analysis into rehabilitation assessment protocols.
Diagram 1: Gait Parameter Deficits in Post-Operative Ankle Fracture Patients. This workflow illustrates the quantitative differences in key gait parameters between postoperative patients and healthy individuals, and their impact on functional recovery.
Experimental Protocols and Methodologies for Weight-Bearing Rehabilitation
Early Versus Delayed Weight-Bearing: Systematic Review Methodology
A comprehensive meta-analysis evaluating early weight-bearing (EWB) efficacy employed rigorous systematic review methodology following PRISMA 2020 guidelines [72]. The search strategy encompassed six electronic databases (PubMed, EMBASE, Cochrane CENTRAL, Web of Science, CINAHL, PEDro) from January 2015 to February 2025, identifying twelve studies with 1,847 participants that met strict inclusion criteria. The experimental protocol defined EWB as initiation within ≤2 weeks post-surgery, compared with delayed weight-bearing (DWB) protocols exceeding this timeframe. Primary outcomes included functional scores (AOFAS, OMAS), pain visual analog scale (VAS), range of motion (ROM), complication rates, and return-to-work timelines [72].
Methodological quality was assessed using design-specific tools: Cochrane RoB 2.0 for randomized controlled trials and modified Newcastle-Ottawa Scale for observational studies. Two methodologists independently evaluated seven domains including randomization adequacy, allocation concealment, blinding methodology, outcome data completeness, and analysis integrity, demonstrating excellent inter-rater reliability (κw = 0.81) [72]. The intervention taxonomy characterized weight-bearing protocols using a hierarchical classification system: non-weight-bearing (<10% body weight), partial weight-bearing (10-80% body weight with graduated progression), and full weight-bearing (>80% body weight). Each protocol underwent parametric extraction using 17 implementation variables, including initiation timing, progression algorithms, loading parameters, and monitoring methodologies, with excellent coding reliability (ICC = 0.88-0.94) between two rehabilitation specialists [72].
Syndesmotic Injury Rehabilitation Protocol
A specialized experimental protocol for ankle fractures with syndesmotic injuries directly compared EWB and late weight-bearing (LWB) groups [73]. The surgical approach standardized anatomical reduction under fluoroscopy, lateral malleolar fixation with 1/3 tubular plates (≥6 cortices), medial malleolar fixation with two 4.0-mm cannulated screws, and syndesmotic fixation with a 3.5-mm quadricortical screw at 2 cm proximal to the plafond following positive hook test. Intraoperative stability was quantitatively verified using intraoperative CT (O-arm), requiring <1 mm syndesmotic displacement on axial views after stress testing [73].
The LWB protocol employed strict non-weight-bearing for 0-6 weeks with short leg cast immobilization, transitioning to partial weight-bearing (20% body weight) at 6-12 weeks with gradual progression to full weight-bearing. In contrast, the EWB protocol initiated progressive weight-bearing at 2 weeks post-surgery, starting with 10% of body weight and increasing by 10-15% weekly within pain tolerance [73]. Both groups performed active range of motion exercises, with the EWB group conducting more frequent sessions (4 times/day, 20 min/session versus 3 times/day, 15 min/session in LWB). Outcome assessments occurred at 6 weeks, 12 weeks, 6 months, and 12 months post-surgery, measuring OMAS, VAS pain scores, ROM, return-to-work/sports timing, and complications [73].
Long-Term Functional Deficit Assessment Protocol
A prospective long-term functional analysis study evaluated patients with unilateral trimalleolar fractures at mean 4.5-year follow-up [16]. The assessment protocol employed the GAITRite electronic walkway system to measure spatiotemporal parameters including step time, step length, stride length, base of support, single support time, double support time, walking speed, and cadence. Participants walked barefoot twice along a 6-meter walkway three times at normal walking speed, starting 2 meters before the walkway to ensure consistent velocity [16].
Functional performance was quantified using the Heel Rise Test to assess plantarflexion strength and endurance, and the Weight-Bearing Lunge Test (WBLT) to measure ankle dorsiflexion range of motion. These objective measures complemented patient-reported outcomes including AOFAS and OMAS [16]. Statistical analysis included intraclass correlation coefficients (ICC3,1) for inter-trial reliability, standard error of measurement (SEM), and minimal detectable change (MDC) calculations, ensuring methodological rigor in quantifying persistent functional deficits.
Quantitative Outcomes of Structured Weight-Bearing Protocols
Early Versus Delayed Weight-Bearing: Meta-Analysis Results
The systematic comparison of EWB versus DWB protocols demonstrated statistically significant advantages for EWB across multiple outcome domains [72]. Meta-analysis revealed EWB provided superior pain reduction (SMD: +0.32, 95% CI: 0.21-0.43) and enhanced ankle dorsiflexion (SMD: +0.38, 95% CI: 0.26-0.50). Critically, the EWB group returned to work 12.3 weeks earlier than DWB patients and achieved clinically significant pain reduction 6 weeks sooner [72]. These functional improvements occurred without increased complication risk, with the EWB group showing favorable complication rates (RR: 0.89, 95% CI: 0.69-1.14) and reduced immobilization-related complications including deep vein thrombosis (2.5% vs. 6.3%) and complex regional pain syndrome (1.8% vs. 4.7%) [72].
Table 2: Outcomes of Early Versus Delayed Weight-Bearing After Ankle Fracture Surgery
| Outcome Measure | Early Weight-Bearing (EWB) | Delayed Weight-Bearing (DWB) | Treatment Effect | Statistical Significance |
|---|---|---|---|---|
| Pain reduction (SMD) | Significant improvement | Less improvement | SMD: +0.32 | 95% CI: 0.21-0.43 |
| Ankle dorsiflexion (SMD) | Significant improvement | Less improvement | SMD: +0.38 | 95% CI: 0.26-0.50 |
| Return to work | Earlier | Later | 12.3 weeks faster | P < 0.01 |
| OMAS at 6 weeks | Higher scores | Lower scores | Significantly higher | P < 0.01 |
| VAS pain at 6 weeks | Lower scores | Higher scores | Significantly lower | P < 0.01 |
| Complication rate | Lower | Higher | RR: 0.89 | 95% CI: 0.69-1.14 |
| DVT incidence | 2.5% | 6.3% | — | — |
| CRPS incidence | 1.8% | 4.7% | — | — |
Subgroup analyses identified specific patient populations deriving particular benefit from EWB protocols. Weber B fractures, younger patients (<45 years), and those without syndesmotic injury demonstrated optimal outcomes with early mobilization [72]. Interestingly, diabetic patients showed enhanced benefits from EWB compared to delayed protocols, contradicting traditional conservative approaches for this population [72].
Syndesmotic Injury Specific Outcomes
For patients with syndesmotic injuries, EWB initiated at 2 weeks post-surgery demonstrated significant functional advantages over traditional delayed protocols [73]. At 6-week follow-up, the EWB group exhibited significantly higher OMAS scores (P<0.01) and lower VAS pain scores (P<0.01) compared to LWB controls. Range of motion measurements at both 6 and 12 weeks post-surgery were significantly greater in the EWB group (both P<0.01) [73].
Critically, the EWB group returned to both work and sports significantly earlier than the LWB group (P=0.01 and P=0.04, respectively), highlighting the real-world functional impact of accelerated rehabilitation. These clinical improvements occurred without increased complications, confirming the safety of appropriately implemented EWB even in complex ankle fractures with syndesmotic involvement [73].
Diagram 2: Outcomes of Early Versus Late Weight-Bearing Rehabilitation. This decision pathway illustrates the comparative outcomes between early and late weight-bearing protocols and identifies patient characteristics associated with optimal response to early mobilization.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Methodologies and Assessment Tools for Weight-Bearing Rehabilitation Studies
| Research Tool | Primary Function | Application Context | Key Metrics |
|---|---|---|---|
| 3D Gait Analysis System | Quantifies spatiotemporal gait parameters | Objective functional assessment | Walking speed, step length, cadence, support time |
| GAITRite Electronic Walkway | Measures walking patterns | Long-term functional deficit analysis | Step time, stride length, base of support, velocity |
| Isokinetic Dynamometer | Assesses muscle strength | Recovery progression monitoring | Peak torque, strength endurance, torque curves |
| Pedobarographic Mat | Evaluates plantar pressure distribution | Foot loading pattern analysis | Mean/peak plantar pressure, contact time, force distribution |
| Olerud-Molander Ankle Score (OMAS) | Patient-reported functional assessment | Subjective outcome measurement | 0-100 point scale evaluating function, pain, stiffness |
| AOFAS Ankle-Hindfoot Scale | Clinician-reported assessment | Clinical outcome evaluation | 0-100 point scale assessing pain, function, alignment |
| Visual Analog Scale (VAS) | Quantifies subjective pain experience | Pain progression monitoring | 0-100 mm scale rating pain intensity |
| Intraoperative CT (O-arm) | Verifies surgical reduction accuracy | Syndesmotic stability assessment | Syndesmotic displacement measurement (<1mm threshold) |
This methodological toolkit enables comprehensive assessment across the rehabilitation spectrum, from intraoperative stability verification to long-term functional outcomes. The integration of objective biomechanical measures with patient-reported outcomes provides multidimensional evaluation of protocol efficacy, facilitating evidence-based optimization of weight-bearing progression algorithms [72] [17] [73].
The synthesized evidence unequivocally demonstrates that structured progressive weight-bearing protocols, particularly when initiated within two weeks post-surgery, yield superior functional outcomes compared to traditional delayed weight-bearing approaches. The significant advantages in pain reduction, range of motion recovery, and accelerated return to work—without increased complication risks—support EWB as a safe and effective rehabilitation strategy for appropriately selected patients [72] [73]. The integration of quantitative gait analysis into rehabilitation assessment provides objective benchmarks for progress evaluation and protocol adjustment, addressing the persistent functional deficits observed even in long-term follow-up studies [11] [16].
Successful implementation requires careful patient stratification, with optimal outcomes observed in Weber B fractures, younger patients (<45 years), and those without syndesmotic injuries [72]. However, emerging evidence suggests that even complex cases, including diabetic patients and those with syndesmotic injuries, may benefit from appropriately monitored early mobilization protocols [72] [73]. Future research directions should focus on refining patient selection criteria, optimizing load progression algorithms, and developing standardized assessment protocols that integrate both objective biomechanical measures and patient-reported outcomes to further enhance rehabilitation efficacy and functional recovery following surgical management of ankle fractures.
Validating Recovery Outcomes: Comparative Analysis of Surgical Results and Rehabilitation Efficacy
The evaluation of patient recovery following foot and ankle surgery, particularly after ankle fractures, relies on two distinct approaches: subjective Patient-Reported Outcome Measures (PROMs) and objective functional gait metrics. PROMs capture the patient's perception of their pain, function, and quality of life, while instrumented gait analysis provides quantifiable data on walking ability. Understanding the correlation between these two types of measures is critical for clinicians and researchers to fully assess treatment efficacy and patient progress. This guide provides a comparative analysis of three prominent region-specific PROMs—the American Orthopaedic Foot & Ankle Society (AOFAS) Ankle-Hindfoot Scale, the Olerud-Molander Ankle Score (OMAS), and the Self-Administered Foot Evaluation Questionnaire (SAFE-Q)—against objective gait parameters, summarizing their validation data and applicability in clinical research.
Outcome Instrument Profiles and Validation
Core Characteristics and Quantitative Validation Data
The AOFAS Ankle-Hindfoot Scale, OMAS, and SAFE-Q are region-specific instruments designed to evaluate functional limitations related to foot and ankle pathologies. Their core characteristics and key performance metrics from validation studies are summarized in the table below.
Table 1: Instrument Profiles and Validation Data
| Instrument (Developer) | Primary Design & Scope | Scoring Range | Reliability (Test-Retest ICC) | Internal Consistency (Cronbach's α) | Construct Validity Correlation (r/rho) | Responsiveness & Ceiling Effects |
|---|---|---|---|---|---|---|
| AOFAS Ankle-Hindfoot Scale (American Orthopaedic Foot & Ankle Society) | Clinician-administered; combines patient-reported and physician-evaluated items [74]. | 0-100 (Higher=Better) | Not fully patient-reported; ICC not applicable in standard PROM context. | Inadequate for total scale (α=0.585); Adequate for function subscale (α=0.863) [74]. | Low correlation with SF-36 (r= 0.02 to 0.36) [75]. | Inadequate longitudinal validity; pronounced ceiling effects from 6 months post-trauma [74]. |
| OMAS (Olerud & Molander) | Disease-specific, self-reported; designed for ankle fracture patients [76] [77]. | 0-100 (Higher=Better) | Excellent (ICC= 0.94-0.98) [76] [77]. | Adequate to Excellent (α= 0.76-0.84) [76] [77]. | Strong correlation with FAOS (rho= 0.80-0.86) [76]. Very good with SF-12 PCS (r=0.72) [77]. | No floor/ceiling effects in acute injury; capable of recording change over time [76]. |
| SAFE-Q (Japanese Society for Surgery of the Foot) | Region-specific, self-reported; evaluates QOL across five foot and ankle domains [20]. | 0-100 (Higher=Better) | High (ICC >0.7 for all subscales) [20]. | High (details not specified) [20]. | Statistically significant correlation with JSSF Scale and SF-36 subscales (p<0.001) [20]. | Separates patients from non-patients; sports subscale available [20]. |
Advantages, Disadvantages, and Recommended Use
Each instrument has distinct strengths and limitations, making it suitable for different research and clinical scenarios.
Table 2: Advantages, Disadvantages, and Recommendations
| Instrument | Key Advantages | Key Disadvantages | Ideal Use Case |
|---|---|---|---|
| AOFAS Ankle-Hindfoot Scale | One of the most widely used tools in foot surgery; includes clinical alignment assessment [74]. | Poor construct validity per SF-36 correlation [75]; requires a clinician for completion [74]; significant ceiling effects limit longitudinal use [74]. | Cross-sectional studies where a clinician-rated alignment component is valuable. |
| OMAS | High reliability and validity specifically for ankle fractures [76] [77]; self-administered; no floor/ceiling effects in acute phase [76]. | Limited to ankle fracture population; may be less specific for other foot/ankle pathologies. | Longitudinal studies tracking functional recovery in ankle fracture patients. |
| SAFE-Q | Comprehensive QOL assessment with multiple subscales [20]; high test-retest reliability; valid for a wide range of foot/ankle pathologies [20]. | Less established in English-language literature; responsiveness requires further testing [20]. | Studies requiring a detailed quality-of-life assessment across diverse foot and ankle conditions. |
Experimental Protocols for Validation
The validation of PROMs involves rigorous methodological protocols to ensure they are reliable, valid, and responsive. The following workflow generalizes the process used in the studies cited in this article.
Figure 1: Generalized workflow for the translation, cultural adaptation, and validation of patient-reported outcome measures, synthesizing methodologies from multiple studies [74] [76] [77].
Detailed Methodology Breakdown
The validation of a PROM is a multi-stage process designed to ensure it is scientifically sound and clinically useful.
- Study Population and Design: Validation studies typically employ a prospective, observational, and often multi-center design [74] [76]. Patient cohorts are defined by specific diagnoses (e.g., unilateral hindfoot fractures, surgically treated ankle fractures) and inclusion/exclusion criteria. Sample sizes in the cited studies ranged from about 100 to 130 patients [74] [77].
- Translation & Cultural Adaptation: For non-English versions, guidelines like those by Beaton are followed [77]. This process involves forward translation by two independent translators, synthesis by a committee, back-translation, and pre-testing with a pilot group of patients to ensure conceptual equivalence and comprehensibility [77].
- Reliability Assessment: This evaluates the instrument's consistency and freedom from measurement error.
- Internal Consistency: Measured using Cronbach's alpha, it indicates how well the items within a (sub)scale measure the same construct. A value between 0.70 and 0.95 is generally considered adequate [74] [77].
- Test-Retest Reliability: Assesses score stability over time in stable patients. Patients complete the questionnaire twice, typically 7-14 days apart [76] [77]. The Intraclass Correlation Coefficient (ICC) is the preferred statistic, with a value >0.70 indicating adequate reliability [74] [76].
- Validity Assessment: This determines how well an instrument measures what it is intended to measure.
- Construct Validity: This is tested by formulating hypotheses about the expected correlations between the new instrument and legacy instruments (e.g., SF-36, FAAM, FFI). A predetermined percentage (e.g., ≥75%) of these hypotheses must be confirmed for validity to be deemed adequate [74] [76]. Correlations are calculated using Spearman's rho or Pearson's r.
- Responsiveness and Interpretability: This is the ability of an instrument to detect clinically important change over time.
- Ceiling/Floor Effects: Occur when a large proportion of respondents achieve the maximum or minimum score, limiting the instrument's ability to detect improvement or deterioration. A ceiling effect was notably present in the AOFAS scale from 6 months post-injury onwards [74].
- Smallest Detectable Change (SDC): The smallest change in score that can be interpreted as a real change beyond measurement error [74] [76].
The Scientist's Toolkit: Essential Research Reagents and Materials
Conducting high-quality research in this field requires a suite of validated tools and technologies for both subjective and objective measurement.
Table 3: Key Materials and Tools for Outcome and Gait Analysis Research
| Tool / Reagent | Function / Utility | Example from Search Results |
|---|---|---|
| Validated PROMs | Quantify patient's subjective experience of pain, function, and quality of life. | OMAS [76] [77], AOFAS [74], SAFE-Q [20], FAAM [77], SF-36/SF-12 [75] [77]. |
| Instrumented Insoles / Wearables | Provide objective, real-time gait metrics outside the lab setting. | OpenGO instrumented insoles with pressure sensors and IMU (accelerometer/gyroscope) for measuring force, pressure distribution, and angular velocity [78]. Apple HealthKit for gait speed, step count, and 6-minute walk test estimation [79]. |
| Gait Analysis Laboratory | Provides gold-standard, high-fidelity spatial and temporal gait data. | Equipment for analyzing step time, swing/stance time, stride time, and cadence in a controlled environment [80]. |
| Statistical Analysis Software | Performs reliability and validity calculations, and models longitudinal data. | SPSS [74] [77], R, and MATLAB [78] for advanced data processing and statistical modeling (e.g., linear mixed effects models). |
| Reference Standards (for Validation) | Serve as a benchmark to test the construct validity of a new PROM. | SF-36 and FFI were used as reference standards to validate the AOFAS-DLV [74]. FAOS and a Global Self-Rated Function scale were used to validate OMAS [76]. |
The comparative analysis of AOFAS, OMAS, and SAFE-Q reveals that the choice of a PROM must be tailored to the specific research question and patient population. The AOFAS Ankle-Hindfoot Scale, while historically prevalent, shows significant limitations in construct validity and is hampered by ceiling effects, making it less suitable for longitudinal studies [74] [75]. The OMAS demonstrates excellent reliability and validity specifically for ankle fracture patients, with no floor or ceiling effects in the acute phase, making it a robust tool for this population [76] [77]. The SAFE-Q offers a comprehensive, multi-domain quality-of-life assessment with high reliability, proving valid for a wide range of foot and ankle pathologies [20].
Crucially, recent evidence underscores that PROMs and objective gait metrics capture distinct aspects of recovery. A 2025 study on total knee arthroplasty found consistently low correlations (r ≈ 0.2-0.3) between PROMs and real-time gait metrics from Apple HealthKit [79]. Similarly, a 2025 study on tibial/malleolar fractures found that objective gait parameters from instrumented insoles improved rapidly in the first 3 months, while PROMs improved later and followed a different trajectory [78]. Therefore, a comprehensive outcome assessment in post-surgery ankle fracture patients should integrate a validated, disease-specific PROM like the OMAS with objective gait analysis to obtain a complete picture of both the patient's lived experience and their functional performance.
Gait symmetry, a cornerstone of human locomotion, refers to the kinetic and kinematic equivalence between left and right limbs during walking. In clinical practice, assessing gait symmetry is paramount for evaluating functional recovery following lower limb surgery. This review delves into the specific context of ankle fracture surgery, a common orthopedic procedure, to objectively compare gait parameters between the surgically treated limb and the non-surgical limb. Despite successful fracture union and stable fixation, a growing body of evidence suggests that patients often develop compensatory mechanisms that lead to persistent, quantifiable asymmetries. These asymmetries can impact long-term functional outcomes, joint health, and overall mobility. By synthesizing data from clinical gait analysis studies, this guide provides a comparative framework for researchers and clinicians to understand the extent of post-surgical gait deviations and the efficacy of different rehabilitation protocols.
Tabular Comparison of Gait Parameters
The following tables synthesize quantitative data from meta-analyses and clinical studies, comparing key gait parameters between the surgical and non-surgical limbs of ankle fracture patients, and between patients and healthy controls.
Table 1: Spatiotemporal Gait Asymmetry (Surgical vs. Non-Surgical Limb)
| Gait Parameter | Direction of Asymmetry | Clinical Significance |
|---|---|---|
| Step Length | Increased on surgical side [16] | May indicate a compensatory strategy to reduce load on the affected limb. |
| Double Support Time | Reduced on surgical side [16] | Suggests altered weight-bearing patterns and potential instability. |
| Single Support Time | Significantly reduced on surgical side [11] [17] | Directly indicates an inability to fully bear weight on the surgical limb. |
| Plantar Pressure Distribution | Increased loading in lateral forefoot of injured leg; Decreased pressure under metatarsal heads [81] | Illustrates compensatory mechanisms to regain overall gait symmetry after trauma. |
Table 2: Functional & Biomechanical Deficits (Surgical vs. Non-Surgical Limb)
| Parameter | Deficit on Surgical Side | Implied Impairment |
|---|---|---|
| Heel Rise Height | Significantly reduced [16] | Deficits in ankle plantarflexion strength and endurance. |
| Weight-Bearing Lunge Test | Significantly limited [16] | Restricted ankle dorsiflexion range of motion. |
| Plantarflexion Peak Torque | Notably reduced [11] [17] | General weakness in the posterior calf muscles. |
| Dorsiflexion Peak Torque | Notably reduced [11] [17] | Weakness in the anterior tibial muscles, affecting gait clearance. |
Table 3: Patient vs. Healthy Control Gait Parameters (Meta-Analysis Findings)
| Gait Parameter | Weighted Mean Difference (WMD) vs. Healthy | P-value |
|---|---|---|
| Walking Speed | WMD = -0.13 m/s [-0.45, -0.16] [11] [17] | P < 0.001 |
| Cadence | WMD = -8.44 steps/min [-10.87, -6.01] [11] [17] | P < 0.001 |
| Step Length | WMD = -0.15 m [-0.18, -0.12] [11] [17] | P < 0.001 |
| Single Support Time | WMD = -16.59 [-19.18, -14.00] [11] [17] | P < 0.001 |
| Peak Dorsiflexion Angular Velocity | WMD = -7.93 deg/s [-13.45, -2.41] [11] [17] | P = 0.005 |
Experimental Protocols for Gait Analysis
To ensure the validity and reliability of the data presented in the comparison tables, researchers adhere to standardized experimental protocols. The following section details common methodologies used in the cited literature.
Instrumented Walkway Test (GAITRite System)
This protocol is designed for high-precision, laboratory-based assessment of spatiotemporal gait parameters.
- Objective: To quantify spatiotemporal gait parameters (e.g., step time, length, velocity) in a controlled environment.
- Procedure:
- Setup: A 6-meter long electronic walkway mat (e.g., GAITRite) is placed on a level walking path.
- Preparation: Participants walk barefoot to eliminate the variable of footwear.
- Walking Trial: Participants are instructed to walk at their comfortable, self-selected speed. They start walking 2 meters before the start of the walkway to ensure a steady-state gait is achieved upon entry, and continue for 2 meters after exiting the mat.
- Data Collection: Each participant performs a minimum of three passes along the walkway. The system automatically captures footfall data which is then processed to extract key parameters [16].
Inertial Measurement Unit (IMU) Based Protocol
This protocol leverages wearable sensors for more flexible gait assessment, capable of capturing a wider range of kinematics outside a strict laboratory setting.
- Objective: To collect kinematic gait data, including pelvic movement and gait phase timing, using wearable sensors.
- Procedure:
- Sensor Placement: Multiple IMU sensors are securely attached to the participant's body. Standardized placements include:
- Protocol: Participants perform a walking test, such as the "Walk+" test, which involves walking a 7-meter hallway for six lengths (three round trips), turning at each end. Only the straight-line walking segments are used for analysis [82]. Alternatively, a 10-meter walk test with a 180° turn in the middle may be used [50].
- Data Processing: Raw accelerometer and gyroscope data are recorded at 100+ Hz. Software algorithms (e.g., BTS G-Studio) segment the data into gait cycles, detect events like heel-strike and toe-off, and compute parameters such as the Gait Quality Index, Propulsion Index, and pelvic kinematics [82]. Path length is a critical consideration, as shorter paths (e.g., 5m) can significantly alter gait patterns compared to the recommended 30m path [83].
Visualization of Gait Analysis Workflow
The following diagram illustrates the standard workflow for conducting a comparative gait analysis study, from participant recruitment to data interpretation.
The Scientist's Toolkit: Research Reagent Solutions
This section outlines the essential tools and technologies used in modern clinical gait analysis research.
Table 4: Essential Tools for Clinical Gait Analysis
| Tool / Technology | Primary Function | Application in Gait Analysis |
|---|---|---|
| Inertial Measurement Units (IMUs) | Wearable sensors containing accelerometers and gyroscopes to measure motion. | Captures kinematic data (e.g., joint angles, accelerations) outside traditional labs. Placed on feet, shanks, and pelvis [50] [82]. |
| 3D Motion Capture Systems | Multi-camera systems that track reflective markers placed on the body. | The gold standard for precise, high-accuracy kinematic measurement of joint movements in a lab [84]. |
| Force Platforms | Embedded plates that measure ground reaction forces (GRFs). | Quantifies forces between the foot and the ground, essential for calculating kinetics and asymmetry indices [84] [85]. |
| Instrumented Walkways | Pressure-sensitive mats that record footfall patterns. | Provides highly accurate spatiotemporal parameters (step length, time, velocity) with minimal patient setup [16]. |
| Electromyography (EMG) | Measures electrical activity produced by skeletal muscles. | Assesses muscle activation patterns and timing during gait to identify neuromuscular deficits. |
| Data Processing & Analysis Software | Algorithms for processing raw sensor data into quantitative gait metrics. | Transforms time-series data into clinically meaningful parameters (e.g., symmetry indices, gait phase timing) [50] [82]. |
Ankle fractures represent one of the most common lower limb fractures worldwide, with incidence rates ranging from 100 to 150 cases per 100,000 person-years [17]. While surgical intervention through Open Reduction and Internal Fixation (ORIF) successfully stabilizes the fracture in most cases, the ultimate goal of rehabilitation extends beyond bone healing to the restoration of pre-injury functional capacity. Recovery benchmarks have traditionally relied on time-based protocols or subjective patient-reported outcomes, creating a critical gap in evidence-based rehabilitation science. This guide establishes objective, biomechanically-grounded recovery targets by directly comparing post-surgical patients against healthy control data, providing clinicians and researchers with standardized metrics for evaluating rehabilitation progress and determining appropriate discharge criteria.
The significance of this comparative approach lies in its ability to quantify the precise functional deficits that persist despite standard rehabilitation. As [11] demonstrates, "despite rehabilitation leading to improvements, patients often failed to regain pre-injury levels of walking speed, muscle strength, and normal plantar pressure distribution." This systematic meta-review of 12 studies comprising 219 postoperative patients and 192 healthy controls provides compelling evidence that current rehabilitation practices may be insufficient for restoring optimal gait function. By establishing clear biomechanical targets derived from healthy population data, clinicians can implement more effective, evidence-based rehabilitation protocols tailored to address specific functional limitations.
Quantitative Gait Analysis: Establishing Performance Benchmarks
Comprehensive gait analysis reveals significant disparities between post-surgical ankle fracture patients and healthy controls across multiple biomechanical parameters. These deficits persist throughout the rehabilitation timeline and provide crucial objective markers for establishing recovery benchmarks. The following synthesis of current research quantifies these differences to establish evidence-based recovery targets.
Table 1: Gait Parameter Comparisons Between Post-Surgery Ankle Fracture Patients and Healthy Controls
| Gait Parameter | Healthy Controls | Post-Surgery Patients | Weighted Mean Difference (WMD) | Clinical Significance |
|---|---|---|---|---|
| Walking Speed | Normalized baseline | Significantly reduced | WMD = -0.13, 95% CI [-0.45, -0.16], P < 0.001 [11] | Directly impacts functional mobility and community participation |
| Peak Dorsiflexion Angular Velocity | Normalized baseline | Significantly reduced | WMD = -7.93, 95% CI [-13.45, -2.41], P = 0.005 [11] | Affects shock absorption and forward propulsion during gait |
| Step Length | Normalized baseline | Significantly reduced | WMD = -0.15, 95% CI [-0.18, -0.12], P < 0.001 [11] | Reflects cautious gait pattern and impaired weight acceptance |
| Single Support Time | Normalized baseline | Significantly reduced | WMD = -16.59, 95% CI [-19.18, -14.00], P < 0.001 [11] | Indicates reduced stability and weight-bearing tolerance |
| Cadence | Normalized baseline | Significantly reduced | WMD = -8.44, 95% CI [-10.87, -6.01], P < 0.001 [11] | Demonstrates altered gait timing and rhythm |
| Peak Plantarflexion Angular Velocity | Normalized baseline | Reduced | WMD = -49.64, 95% CI [-99.98, 0.71], P = 0.053 [11] | Impacts push-off power and propulsion generation |
The data presented in Table 1 reveals a consistent pattern of gait alteration in post-surgical patients, characterized by slower, more cautious movement patterns with reduced joint mobility and propulsion capacity. These quantitative differences provide concrete targets for rehabilitation specialists seeking to restore normal gait function. For instance, rehabilitation programs should specifically target improving walking speed toward healthy control values, as this parameter integrates multiple aspects of gait performance including balance, strength, and confidence in the injured limb.
Beyond basic temporal-spatial parameters, sophisticated kinematic analyses using methods like the Heidelberg Foot Measurement Method (HFMM) have identified specific joint-level deficits. [86] reported "significant differences for the Foot Tibia Dorsal Flexion for patients after 9 weeks (53–75% of gait cycle: p = 0.001) and patients after 26 weeks (58–70%: p = 0.011) compared to healthy participants." These findings indicate that limitations in ankle dorsiflexion persist throughout the gait cycle, potentially contributing to the observed reductions in walking speed and step length. Furthermore, ground reaction force analysis reveals altered loading patterns, with patients demonstrating significant differences in force application throughout the stance phase [86]. These objective biomechanical measures provide precise targets for rehabilitation interventions aimed at restoring normal movement patterns.
Experimental Protocols for Comparative Gait Analysis
Three-Dimensional Gait Analysis with the Heidelberg Foot Measurement Method (HFMM)
The Heidelberg Foot Measurement Method represents a sophisticated approach to capturing multi-segmental foot kinematics during gait. The protocol implemented by [86] involves a precise marker placement system and data collection methodology:
Participant Preparation and Marker Placement: Following appropriate ethical approvals and informed consent, participants should be gait-ready with appropriate footwear (or barefoot depending on research questions). A total of 17 retro-reflective markers are placed on defined bony landmarks of both lower limbs according to Simon et al. [86]. This includes 5 markers on the knee and 12 on the foot, with additional markers placed on the pelvis according to standard procedures for instrumented 3D gait analysis. The specific foot markers capture the complex multi-segmental motion of the rearfoot, midfoot, and forefoot.
Data Collection and Processing: Marker coordinate data is collected at 120 Hz using a VICON motion capture system with a minimum of 12 cameras to ensure comprehensive spatial coverage [86]. The standard Y-X-Z Cardan sequence (sagittal, frontal, and transverse respectively) is used for calculating joint angles. Simultaneously, ground reaction forces are collected using force plates (e.g., KISTLER force plates) embedded in the walkway, normalized to the gait cycle (101 data points) and the body weight of the individual participant. A minimum of five successful trials per limb is recommended to ensure data reliability.
Statistical Parametric Mapping (SPM): Unlike traditional gait analysis that examines discrete points in the gait cycle, SPM performs continuous analysis across the entire gait cycle, identifying specific intervals where significant differences occur between groups [86]. This method offers enhanced sensitivity for detecting alterations in movement patterns that might be missed by traditional analytical approaches.
Y-Balance Test Protocol with Electromyographic Analysis
The Y-Balance Test (YBT) provides a standardized method for assessing dynamic balance and neuromuscular control, with specific adaptations for electromyographic (EMG) analysis as described by [38]:
Test Setup and Protocol: The YBT kit consists of a central stance platform with three extensions positioned in the anterior, posteromedial, and posterolateral directions. Participants maintain a single-leg stance on the operated limb while reaching as far as possible with the contralateral limb along each direction, pushing a reach indicator block with their toes. Three practice trials in each direction are followed by three test trials, with the maximum reach distance recorded for each direction and normalized to limb length.
Electromyographic Data Collection: Surface EMG electrodes are placed on five key lower limb muscles according to SENIAM recommendations: tibialis anterior, peroneus longus, lateral gastrocnemius, biceps femoris, and gluteus medius [38]. Raw EMG signals are collected at a minimum sampling rate of 1000 Hz, band-pass filtered (20-450 Hz), and normalized to maximum voluntary isometric contractions (MVICs) for each muscle. EMG activity is analyzed during the reach phase of the YBT, focusing on muscle activation amplitude and timing.
Data Interpretation: [38] identified "a significant interaction effect (limb × proximal [hip]—distal [ankle] muscle) (F = 30.806, p < 0.001) in the anterior direction of the Y-Balance Test at 6 months post-surgery," highlighting the value of this protocol for detecting compensatory movement patterns. The anterior direction appears particularly sensitive for identifying neuromuscular alterations in this population.
Conceptual Framework for Establishing Recovery Targets
The following conceptual framework illustrates the integrated approach to establishing evidence-based recovery targets and discharge criteria for ankle fracture rehabilitation:
Diagram 1: Framework for Establishing Recovery Targets
This framework emphasizes the cyclical nature of rehabilitation assessment and intervention, with ongoing progress monitoring informing potential modifications to recovery targets. The integration of multiple assessment methodologies provides a comprehensive picture of functional recovery, ensuring that discharge decisions are based on objective achievement of biomechanical benchmarks rather than arbitrary time-based criteria.
The Scientist's Toolkit: Essential Research Reagents and Equipment
Table 2: Essential Research Equipment for Comparative Gait Analysis
| Equipment Category | Specific Examples | Primary Function | Key Applications in Ankle Fracture Research |
|---|---|---|---|
| Motion Capture Systems | VICON motion capture system, Qualisys, OptiTrack | High-precision tracking of retro-reflective markers in 3D space | Quantifying joint kinematics, segmental coordination, and gait deviations [86] |
| Force Measurement Platforms | KISTLER force plates, AMTI force platforms | Measuring ground reaction forces during stance phase | Assessing loading asymmetry, weight-bearing tolerance, and propulsion generation [86] |
| Electromyography Systems | Surface EMG systems (e.g., Delsys Trigno, Noraxon) | Recording muscle activation patterns and timing | Evaluating neuromuscular control strategies and compensatory muscle recruitment [38] |
| Dynamic Balance Assessment | Y-Balance Test kit, Biodex Balance System | Quantifying dynamic postural control and reach distance | Assessing functional stability and identifying balance deficits [38] |
| Plantar Pressure Measurement | Pedar system, Tekscan F-Scan, EMED pressure platform | Mapping pressure distribution across the foot surface | Identifying altered loading patterns and pressure redistribution [11] |
| Strength Assessment | Hand-held dynamometry (microFET2), Biodex Isokinetic dynamometer | Quantifying maximal voluntary muscle contraction | Documenting strength deficits and monitoring recovery progress [38] |
| Patient-Reported Outcome Measures | AOFAS scale, Olerud-Molander Ankle Score | Capturing patient perspective on function and symptoms | Correlating objective biomechanical data with subjective patient experience [86] [38] |
This comprehensive toolkit enables researchers to capture the multifaceted nature of recovery following ankle fracture surgery. The integration of kinematic, kinetic, and electromyographic data provides insights into the complex sensorimotor adaptations that occur following injury and during the recovery process. As [38] demonstrated through combined YBT and EMG assessment, "neuromuscular patterns differ between operated and non-operated limbs during the YBTA at 6 months post-surgery," highlighting the value of integrated assessment approaches for identifying subtle neuromuscular alterations that may not be apparent through clinical observation alone.
The comparative analysis between post-surgical ankle fracture patients and healthy controls provides unequivocal evidence for persistent functional deficits despite standard rehabilitation. The quantitative data presented in this guide establishes clear, objective targets for rehabilitation programs and discharge criteria. Specifically, recovery should be measured against healthy control benchmarks for walking speed (>0.13 m/s improvement target), step length (>0.15 m improvement target), single support time (>16% improvement target), and dynamic balance performance.
Future research should focus on establishing validated cutoff values for each parameter that predict successful long-term outcomes, enabling more precise discharge decision-making. Additionally, investigations into the specific rehabilitation interventions that most effectively address the identified gait deficits will help bridge the current gap between patient performance and healthy control benchmarks. Through the adoption of these evidence-based benchmarks and assessment methodologies, clinicians can transform ankle fracture rehabilitation from a time-based process to a targeted, outcomes-driven approach that maximizes functional recovery and reduces the risk of long-term complications.
Within the framework of a broader thesis on the comparative analysis of gait parameters between post-surgery ankle fracture patients and healthy individuals, evaluating the efficacy of rehabilitation interventions is paramount. Restoring functional gait is a primary goal following surgical fixation of ankle fractures, yet quantitative evidence reveals that patients often fail to regain pre-injury levels of walking speed, muscle strength, and normal plantar pressure distribution compared to healthy controls [11] [17]. This guide provides an objective comparison of rehabilitation approaches, drawing on evidence from randomized controlled trials (RCTs) and longitudinal studies. It synthesizes data on conventional therapy, technology-assisted interventions, and emerging methodologies like machine learning and pragmatic trial designs, offering researchers and drug development professionals a consolidated view of experimental data and protocols.
Comparative Efficacy of Rehabilitation Interventions
The effectiveness of rehabilitation is measured through distinct yet complementary paradigms, ranging from restoring specific physical functions to reducing overall disability.
Gait and Functional Recovery in Post-Surgery Ankle Fractures
Table 1: Quantitative Gait Parameter Deficits in Post-Surgery Ankle Fracture Patients vs. Healthy Individuals
| Gait Parameter | Weighted Mean Difference (WMD) in Patients vs. Healthy | Statistical Significance (P-value) | Heterogeneity (I²) |
|---|---|---|---|
| Walking Speed | WMD = -0.13 m/s [17] | P < 0.001 [17] | 90.7% [17] |
| Step Length | WMD = -0.15 m [17] | P < 0.001 [17] | Not Reported |
| Single Support Time | WMD = -16.59 % [17] | P < 0.001 [17] | Not Reported |
| Cadence | WMD = -8.44 steps/min [17] | P < 0.001 [17] | Not Reported |
| Peak Dorsiflexion Angular Velocity | WMD = -7.93 °/s [17] | P = 0.005 [17] | Not Reported |
| Peak Plantarflexion Angular Velocity | WMD = -49.64 °/s [17] | P = 0.053 (Not Significant) [17] | Not Reported |
A systematic review and meta-analysis of 12 studies found that despite rehabilitation, post-operative ankle fracture patients show significant impairments across multiple gait metrics [17]. These deficits in walking speed, step length, and muscle strength indicate that current standard rehabilitation may be insufficient for restoring a normal gait pattern [11]. The high heterogeneity (I² = 90.7%) for walking speed suggests considerable variability in patient recovery, potentially influenced by factors such as fracture severity or specific rehabilitation protocols [17]. Studies specifically on trimalleolar fractures have shown the poorest functional outcomes, with operative fixation failing to restore normal gait function even at 6 months post-operatively [49].
Reduction of Disability Across Various Health Conditions
Table 2: Efficacy of Rehabilitation Interventions on Disability Reduction Measured by WHODAS 2.0
| Health Condition | Rehabilitation Interventions | Reported Effect on WHODAS 2.0 Scores |
|---|---|---|
| Stroke | Conventional Therapy, Robot-Assisted Arm Training, Virtual Reality, Telerehabilitation | Decrease in scores post-rehabilitation [87] |
| Chronic Heart Failure | Not Specified | Decrease in scores post-rehabilitation [87] |
| Chronic Obstructive Pulmonary Disease (COPD) | Not Specified | Decrease in scores post-rehabilitation [87] |
| Parkinson's Disease | Not Specified | Decrease in scores post-rehabilitation [87] |
| Chronic Pain | Not Specified | Decrease in scores post-rehabilitation [87] |
| Cancer | Not Specified | Decrease in scores post-rehabilitation [87] |
| Frail Elderly | Not Specified | Decrease in scores post-rehabilitation [87] |
A systematic review of 18 articles demonstrated that a wide range of rehabilitation techniques effectively reduce disability, as measured by the World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0), across various comorbidities [87]. The WHODAS 2.0 questionnaire, which assesses six domains of life activities, has proven to be an efficient and reliable tool for measuring disability, with scores showing a consistent tendency to decrease following rehabilitation interventions [87]. This indicates that the benefits of rehabilitation extend beyond specific gait metrics to encompass broader improvements in patient functioning and participation.
Experimental Protocols and Methodologies
Protocol for Gait Analysis in Ankle Fracture Research
The methodological framework for comparing gait parameters between patient groups and healthy controls is critical for generating valid evidence.
Gait Analysis Experimental Workflow
A systematic review and meta-analysis protocol provides a rigorous methodology for this field [17]. Key phases include:
- Patient Recruitment and Group Stratification: Studies typically include surgically treated ankle fracture patients, with fracture type (unimalleolar, bimalleolar, trimalleolar) often documented. Control groups consist of participants with healthy limb function [17].
- Standardized Assessment: Core outcomes include:
- Gait Analysis Parameters: Walking speed (m/s), peak dorsiflexion and plantarflexion angular velocity (°/s), step length (m), single support time (%), and cadence (steps/min) [17].
- Muscle Strength: Peak torque of dorsiflexion and plantarflexion, often measured using isokinetic dynamometry [17].
- Plantar Pressure: Mean and peak plantar pressure and contact time [17].
- Patient-Reported Outcome Measures (PROMs): Functional outcomes specific to the ankle [17].
- Data Synthesis and Analysis: Meta-analyses calculate Weighted Mean Differences (WMDs) with 95% confidence intervals. Statistical heterogeneity is assessed using Cochrane's Q test and the I² statistic. Subgroup analyses based on age, fracture diagnosis, and study design explore sources of heterogeneity [17].
Protocol for Disability Assessment Using WHODAS 2.0
The WHODAS 2.0 provides a standardized framework for assessing disability across diverse populations and interventions.
WHODAS 2.0 Assessment Workflow
The application of WHODAS 2.0 in rehabilitation research typically follows a structured approach:
- Research Question Framing: Using the PICO (Population, Intervention, Comparison, Outcome) method:
- Population: Patients with disabilities from various conditions (stroke, cardiovascular disease, COPD, etc.) [87].
- Intervention: Rehabilitation programs or specific interventions (conventional therapy, virtual reality, robot-assisted training, exergaming, telerehabilitation) [87].
- Comparison: Baseline measurement before intervention, standard care, or a control group receiving conventional therapy [87].
- Outcome: Improvement in WHODAS 2.0 questionnaire scores [87].
- Questionnaire Administration: The WHODAS 2.0, available in 36-item and 12-item versions, captures functioning in six domains over the last 30 days. Respondents rate difficulty on a 5-point scale from "none" to "extreme or cannot do" [87].
- Outcome Analysis: Studies assess changes in scores from pre- to post-rehabilitation, with a decrease indicating a reduction in disability levels [87].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Materials and Tools for Rehabilitation Research
| Item | Function in Research |
|---|---|
| 3D Motion Capture System | Quantifies kinematic parameters (joint angles, velocities) during gait analysis [17]. |
| Force Plates / Pressure Mats | Measures ground reaction forces and plantar pressure distribution during walking [17]. |
| Isokinetic Dynamometer | Assesses muscle strength (peak torque) for dorsiflexion and plantarflexion [17]. |
| WHODAS 2.0 Questionnaire | Standardized tool for measuring disability across six domains of functioning [87]. |
| Patient-Reported Outcome Measures (PROMs) | Captures the patient's perspective on functional status, symptoms, and quality of life [17] [88]. |
| InMotion Robotic Systems | Used in sensorimotor rehabilitation interventions (e.g., for arm and wrist training in stroke) [89]. |
| Transcranial Direct Current Stimulation (tDCS) | Non-invasive brain stimulation technique to modulate cortical excitability in neurorehabilitation [89]. |
| Machine Learning Algorithms (e.g., Random Forest) | Analyzes complex datasets to predict rehabilitation outcomes and identify key predictors [90] [91] [89]. |
Emerging Research Methodologies and Technologies
Machine Learning for Outcome Prediction
Machine learning (ML) is transforming rehabilitation research by enabling accurate prediction of patient outcomes. In spinal cord injury (SCI), Random Forest (RF) and XGBoost models significantly outperformed traditional statistical models in predicting discharge Functional Independence Measure (FIM) scores, with RF achieving an R-squared of 0.52 and a Mean Squared Error (MSE) of 1.37 on the test dataset [92]. Similarly, for traumatic brain injury (TBI), a Gradient Boosting Tree Model (GBM) was the most consistent predictor across outcomes like length of stay, discharge destination, and cognitive function [91]. In chronic stroke, ML models like RF and k-nearest neighbors (KNN) effectively predicted clinically significant health-related quality of life (HRQOL) improvement, with accuracy reaching 85% [89]. These models help identify crucial predictors of recovery, such as baseline functional scores, age, and time from injury to rehabilitation start [91] [89] [92].
Pragmatic and Hybrid Trial Designs
To enhance the external validity of rehabilitation research, pragmatic and hybrid trial designs are gaining prominence. Traditional RCTs often use strict eligibility criteria and controlled environments, limiting the generalizability of findings to routine clinical practice [88]. Pragmatic trials address this by:
- Employing broad inclusion criteria to recruit a diverse patient population that reflects real-world cases [88].
- Allowing flexible interventions that can be individualized based on clinical judgment, while operating within a defined protocol [88].
- Using clinically relevant outcomes like functional recovery and patient-reported outcomes [88].
- Testing interventions across heterogeneous treatment settings (outpatient, inpatient, home-based) [88].
Hybrid effectiveness-implementation designs (Type 1, 2, and 3) further accelerate the translation of evidence into practice by simultaneously evaluating clinical effectiveness and implementation processes [88].
Conclusion
The synthesized evidence confirms that patients following ankle fracture surgery exhibit significant and persistent deficits in key gait parameters, muscle strength, and plantar pressure distribution compared to healthy individuals, even after radiological healing. These functional impairments, including reduced walking speed, shorter step length, diminished single support time, and asymmetric gait patterns, directly impact patient quality of life and functional independence. Future research must prioritize the development of standardized, targeted rehabilitation protocols that specifically address identified deficits in weight-bearing dorsiflexion, plantarflexion strength, and dynamic stability. For biomedical researchers and pharmaceutical developers, these findings highlight critical opportunities for interventions targeting muscle preservation during immobilization and enhancing neurological re-education for proprioceptive recovery. The integration of advanced motion analysis technologies into routine clinical practice will be essential for objectively quantifying recovery and validating the efficacy of emerging therapeutic strategies.
References
- 1. Comparison of gait parameters between post-surgery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584260/]
- 2. Does texting while walking affect spatiotemporal gait ... [https://pubmed.ncbi.nlm.nih.gov/36696854/]
- 3. The spatiotemporal gait parameters among people with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10697262/]
- 4. Spatiotemporal gait characteristics across the adult ... [https://www.sciencedirect.com/science/article/pii/S0966636224000043]
- 5. Gait parameters and daily physical activity for distinguishing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12173000/]
- 6. Normative Database of Spatiotemporal Gait Metrics Across ... [https://www.mdpi.com/1424-8220/25/2/581]
- 7. Assessment of spatiotemporal gait parameters using a ... [https://www.sciencedirect.com/science/article/abs/pii/S0021929021001949]
- 8. Gait stability prediction through synthetic time-series and ... [https://www.frontiersin.org/journals/sports-and-active-living/articles/10.3389/fspor.2025.1646146/full]
- 9. Clinical Assessment of Spatiotemporal Parameters of Gait ... [https://ijspt.scholasticahq.com/article/133493-clinical-assessment-of-spatiotemporal-parameters-of-gait-when-performing-a-visuospatial-cognitive-task]
- 10. Health & Gait: a dataset for gait-based analysis [https://www.nature.com/articles/s41597-024-04327-4]
- 11. Comparison of gait parameters between post-surgery ... [https://pubmed.ncbi.nlm.nih.gov/41188844/]
- 12. Association between weight-bearing ankle dorsiflexion ... [https://www.frontiersin.org/journals/rehabilitation-sciences/articles/10.3389/fresc.2025.1645621/full]
- 13. pressuRe: an R package for analyzing and visualizing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10556014/]
- 14. Open-Source Strain Gauge System for Monitoring Pressure ... [https://www.mdpi.com/1424-8220/23/4/2323]
- 15. Persistent functional deficits after ankle fracture surgery [https://pubmed.ncbi.nlm.nih.gov/40519779/]
- 16. Persistent functional deficits after ankle fracture surgery [https://www.sciencedirect.com/science/article/abs/pii/S0972978X25001916]
- 17. Comparison of gait parameters between post-surgery ankle ... [https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-025-01463-9]
- 18. Five-year functional outcome analysis of ankle fracture ... [https://pubmed.ncbi.nlm.nih.gov/17888434/]
- 19. Gait Definitions [https://www.physio-pedia.com/Gait_Definitions]
- 20. Validity and reliability of a self-administered foot evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3607735/]
- 21. Validity and reliability of a self-administered foot evaluation ... [https://www.sciencedirect.com/science/article/pii/S094926581530508X]
- 22. Association between weight-bearing ankle dorsiflexion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12358486/]
- 23. Normative Spatiotemporal Gait Parameters in Older Adults [https://pmc.ncbi.nlm.nih.gov/articles/PMC3104090/]
- 24. Gait Parameters in Healthy Older Adults in Korea [https://www.e-jmd.org/journal/view.php?number=542]
- 25. The reliability of gait parameters captured via instrumented ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9987464/]
- 26. Comparability between wearable inertial sensors and an ... [https://www.sciencedirect.com/science/article/abs/pii/S0966636224000924]
- 27. Gait Assessment Using Smartphone Applications in Older ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11270307/]
- 28. Smartphone Accelerometer for Gait Assessment: Validity ... [https://www.mdpi.com/2076-3417/14/23/11321]
- 29. The validity and reliability of the GAITRite system's ... [https://pubmed.ncbi.nlm.nih.gov/11245768/]
- 30. Comparative Analysis of Gait Speed Estimation Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8982681/]
- 31. Gait Alterations in Adults after Ankle Fracture: A Systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8774579/]
- 32. How To Improve Ankle Dorsiflexion Range Of Motion [https://e3rehab.com/ankle-dorsiflexion/]
- 33. Knee to Wall Test [https://www.physio-pedia.com/Knee_to_Wall_Test]
- 34. RELIABILITY OF THREE MEASURES OF ANKLE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3362988/]
- 35. Reliability of the weight-bearing ankle dorsiflexion range ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8464192/]
- 36. A 15-22-Year Follow-up Study of 125 Patients [https://pubmed.ncbi.nlm.nih.gov/40916875/]
- 37. Neuromuscular Control in Postural Stability: Insights into ... [https://www.mdpi.com/2624-6120/6/1/6]
- 38. Changes in Motor Strategy and Neuromuscular Control ... [https://www.mdpi.com/1424-8220/24/21/6798]
- 39. Changes in Motor Strategy and Neuromuscular Control ... [https://pubmed.ncbi.nlm.nih.gov/39517697/]
- 40. Vestibular Rehabilitation Using Dynamic Posturography [https://pmc.ncbi.nlm.nih.gov/articles/PMC12379862/]
- 41. Lower extremity muscle activity during reactive balance ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2024.1432293/full]
- 42. Neuromuscular conditions in post-stroke ankle-foot ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11304728/]
- 43. Functional and neuromuscular effects of rehabilitation in ... [https://www.sciencedirect.com/science/article/pii/S1067251625002327]
- 44. Applying high-density surface EMG to the study of ... [https://pubmed.ncbi.nlm.nih.gov/40913923/]
- 45. Validity and Reliability of a Smartphone-Based Gait ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294008/]
- 46. Predicting Post-Fracture Recovery with Smartphone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12281417/]
- 47. Monitoring Mobility at Home: The GAIT-HUB Sensor-Based ... [https://pubmed.ncbi.nlm.nih.gov/40740790/]
- 48. Gait analysis from a smartphone for use in clinical routine [https://www.sciencedirect.com/science/article/pii/S0966636225003315]
- 49. Comparison of gait parameters between post-surgery ... [https://www.semanticscholar.org/paper/Comparison-of-gait-parameters-between-post-surgery-Long-Yang/098ef61a65852e8b5a1521ee733b62675a7e83da]
- 50. A Dataset of Clinical Gait Signals with Wearable Sensors ... [https://www.nature.com/articles/s41597-025-05959-w]
- 51. Resistance exercise training improves disuse-induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11806896/]
- 52. Comparative Analysis of Physical Activity and ... [https://www.mdpi.com/2076-3417/15/18/9952]
- 53. Blood Flow Restriction Training Can Improve Peak Torque ... [https://www.sciencedirect.com/science/article/abs/pii/S0749806321002796]
- 54. Progressive Resistance Training Improves Torque ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6625591/]
- 55. Effects of strength training on neuromuscular adaptations ... [https://www.nature.com/articles/s41598-025-03070-z]
- 56. analysis of secondary outcomes from a randomised clinical trial [https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-022-05907-4]
- 57. Gait adaptations in step length and push-off force during ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1550710/full]
- 58. Human Gait Analysis Metric for Gait Retraining - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6877909/]
- 59. Comparing Gait with Multiple Physical Asymmetries Using ... [https://www.frontiersin.org/journals/neurorobotics/articles/10.3389/fnbot.2018.00002/full]
- 60. Rehabilitating Asymmetric Gait Using Asymmetry [https://digitalcommons.usf.edu/etd/7438/]
- 61. Artificial intelligence in foot and ankle surgery [https://pmc.ncbi.nlm.nih.gov/articles/PMC10692015/]
- 62. The role of proprioception in the management and rehabilitation of athletic injuries - PubMed [https://pubmed.ncbi.nlm.nih.gov/9006708/]
- 63. Comparison of muscle activation and proprioception during ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505775/]
- 64. Mechanism-Driven Strategies for Reducing Fall Risk in the Elderly: A Multidisciplinary Review of Exercise Interventions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11641686/]
- 65. Effectiveness of exercise interventions on fall prevention in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10435089/]
- 66. Effects of proprioceptive training on sports performance: a systematic review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11225257/]
- 67. Balance & Proprioception Training: Next-Level Injury Prevention - Healix Therapy - Physical Therapy Exercises, Manual Therapy at Home [https://healixtherapy.com/balance-proprioception-injury-prevention/]
- 68. EFFECTIVENESS OF PROPRIOCEPTIVE AND ... [https://world.physio/congress-proceeding/effectiveness-proprioceptive-and-neuromuscular-training-compared-bracing]
- 69. Frontiers | The Effectiveness of Proprioceptive Training for Improving Motor Performance and Motor Dysfunction: A Systematic Review [https://www.frontiersin.org/journals/rehabilitation-sciences/articles/10.3389/fresc.2022.830166/full]
- 70. Targeting Dynamic Balance in Falls-Prevention ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4321459/]
- 71. A randomized controlled trial on impact of group exercise ... [https://www.jgerontology-geriatrics.com/article/view/540]
- 72. Early weight-bearing after ankle fracture surgery: a systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12372276/]
- 73. Effect of early weight bearing on rehabilitation in ankle ... [https://www.nature.com/articles/s41598-025-18920-z]
- 74. Validation of the American Orthopaedic Foot and Ankle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5695419/]
- 75. Evaluation of the validity of the AOFAS Clinical Rating ... [https://pubmed.ncbi.nlm.nih.gov/12540082/]
- 76. The Swedish version of OMAS is a reliable and valid outcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3614453/]
- 77. Translation, cross-cultural adaptation, reliability and validity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6197354/]
- 78. Recovery of Patient-Reported Outcome Measures vs Gait ... [https://mhealth.jmir.org/2025/1/e71022]
- 79. How Do Patient-Reported Outcomes Correlate With Real ... [https://pubmed.ncbi.nlm.nih.gov/39667590/]
- 80. Gait analysis and functional outcomes after twelve-week ... [https://www.sciencedirect.com/science/article/abs/pii/S0966636216301436]
- 81. Gait asymmetry following successful surgical treatment of ankle fractures in young adults - PubMed [https://pubmed.ncbi.nlm.nih.gov/7634584/]
- 82. Comparative analysis of spatiotemporal gait parameters in patients with distal femoral megaprosthesis and healthy subjects using an inertial measurement unit (IMU) - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12170936/]
- 83. Impact of Walking Path Length on Gait Parameters During ... [https://www.mdpi.com/2673-7078/5/4/82]
- 84. Assessment of a New Gait Asymmetry Index in Patients After Unilateral Total Hip Arthroplasty - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11594978/]
- 85. Comparative analysis of ground reaction forces and ... [https://pubmed.ncbi.nlm.nih.gov/40197475/]
- 86. Short-term results of gait with the Heidelberg foot... analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8742407/]
- 87. Assessing the Effectiveness of Rehabilitation Interventions ... [https://www.mdpi.com/2077-0383/13/5/1252]
- 88. Bridging the gap: Enhancing external validity in ... [https://journalmsr.com/bridging-the-gap-enhancing-external-validity-in-rehabilitation-research-through-pragmatic-and-hybrid-trial-designs/]
- 89. Machine learning predicts clinically significant health ... [https://www.nature.com/articles/s41598-022-14986-1]
- 90. Enhancing patient rehabilitation outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12105185/]
- 91. How do different machine learning methods compare to ... [https://biausa.org/professionals/research/tbi-model-systems/how-do-different-machine-learning-methods-compare-to-one-another-when-used-to-predict-inpatient-rehabilitation-outcomes-for-patients-with-tbi]
- 92. Machine learning predicts improvement of functional ... [https://www.frontiersin.org/journals/rehabilitation-sciences/articles/10.3389/fresc.2025.1594753/full]