Validating Machine Learning Models for Ventricular Tachycardia Ablation: From Algorithm Development to Clinical Integration
This article provides a comprehensive framework for the development and validation of machine learning (ML) models aimed at improving outcomes in ventricular tachycardia (VT) ablation.
Validating Machine Learning Models for Ventricular Tachycardia Ablation: From Algorithm Development to Clinical Integration
Abstract
This article provides a comprehensive framework for the development and validation of machine learning (ML) models aimed at improving outcomes in ventricular tachycardia (VT) ablation. It explores the foundational clinical challenges that motivate ML applications, details the methodological pipeline from data preparation to model selection, and addresses critical troubleshooting aspects like handling class imbalance and ensuring model interpretability. Furthermore, it outlines rigorous internal, external, and real-world validation paradigms, including comparative analyses against traditional statistical methods and clinical benchmarks. Designed for researchers and drug development professionals, this review synthesizes current evidence and best practices to guide the creation of robust, clinically translatable ML tools that can enhance risk stratification, procedural planning, and long-term prognosis for patients undergoing VT ablation.
The Clinical Imperative: Foundational Challenges in Ventricular Tachycardia Ablation Driving ML Innovation
Machine learning has revolutionized cardiovascular prognostication, yet a significant gap persists in understanding long-term heart failure and mortality risks following catheter ablation for ventricular tachyarrhythmias. While existing models largely target peri-procedural complications, recurrence, or immediate procedural success [1], patients undergoing ablation remain susceptible to cerebrovascular events and cumulative excess mortality—hazards seldom quantified in contemporary literature. This prognostic gap limits clinicians' ability to deliver truly personalized follow-up care for a growing population of ablation recipients [1].
The integration of machine learning into cardiac electrophysiology research represents a paradigm shift, offering powerful tools to decipher complex patterns in multidimensional patient data. This review examines the current landscape of machine learning applications for predicting long-term outcomes post-ablation, with particular focus on model architectures, performance benchmarks, and methodological frameworks for translating algorithmic predictions into clinically actionable insights.
Comparative Performance of Machine Learning Models
Model Architectures and Performance Metrics
Table 1: Machine learning model performance for predicting three-year outcomes after PVC ablation
| Prediction Task | Best Performing Model | ROC AUC | Alternative Models | Sampling Method | Key Predictors |
|---|---|---|---|---|---|
| Three-year heart failure | LightGBM with ROSE | 0.822 | Logistic Regression, Decision Tree, Random Forest, XGBoost | ROSE | Age, prior HF, malignancy, ESRD |
| Three-year mortality | Logistic Regression with ROSE | 0.886 | LightGBM with ROSE (AUC: 0.882) | ROSE | Age, prior HF, malignancy, ESRD |
| VT ablation target localization | Random Forest | 0.821 | Other ML algorithms | None | EGM features from substrate mapping |
Multiple studies have demonstrated the superior performance of ensemble methods and gradient boosting algorithms for long-term outcome prediction. In a nationwide cohort of 4,195 patients who underwent PVC ablation, LightGBM with random over-sampling examples (ROSE) achieved the highest ROC AUC (0.822) for predicting three-year heart failure, while logistic regression with ROSE and LightGBM with ROSE showed balanced performance for three-year mortality prediction with ROC AUCs of 0.886 and 0.882, respectively [1]. Pairwise DeLong tests indicated these leading models formed a high-performing cluster without significant differences in ROC AUC [1].
For the specialized task of ventricular tachycardia ablation target localization, random forest algorithms have demonstrated exceptional capability. In a porcine model of chronic myocardial infarction, random forest classification based on unipolar signals from sinus rhythm mapping achieved an AUC of 0.821 with sensitivity and specificity of 81.4% and 71.4%, respectively, for identifying critical sites for ablation [2]. This approach analyzed 46 signal features representing functional, spatial, spectral, and time-frequency properties from 35,068 electrograms [2].
Addressing Class Imbalance in Clinical Datasets
The challenge of class imbalance—where adverse events are relatively rare—represents a critical methodological consideration in prognostic model development. Studies have systematically compared techniques such as synthetic minority over-sampling technique (SMOTE) and random over-sampling examples (ROSE) to address this limitation [1]. For predicting three-year outcomes post-ablation, ROSE consistently yielded superior performance with both logistic regression and LightGBM models, suggesting the importance of tailored sampling strategies for specific clinical endpoints [1].
Stacking ensemble models that integrate multiple base learners have also shown promise for mortality prediction in complex cardiac patients. In patients with heart failure and atrial fibrillation, a stacking model that combined Random Forest, XGBoost, LightGBM, and K-Nearest Neighbor algorithms achieved an AUC of 0.768 in the testing set, outperforming individual base classifiers [3].
Experimental Protocols and Methodological Frameworks
Cohort Selection and Feature Engineering
Table 2: Methodological approaches for dataset construction in ablation outcome studies
| Study Component | NHIRD Cohort Study [1] [4] | Porcine VT Model [2] | AF Mortality Prediction [5] |
|---|---|---|---|
| Population/Sample | 4,195 adults with PVC ablation | 13 pigs with chronic MI | 18,727 hospitalized AF patients |
| Data Sources | Taiwan National Health Insurance Research Database | Multipolar catheters (Advisor HD Grid) | Electronic medical records |
| Key Variables | Demographics, comorbidities, medications | 46 EGM features | 79 clinical variables |
| Outcome Measures | 3-year HF and all-cause mortality | Localized VT critical sites | In-hospital cardiac mortality |
| Class Handling | SMOTE and ROSE | Not applicable | Downsampling and class weighting |
The foundation of robust machine learning models begins with rigorous cohort selection and feature engineering. The National Health Insurance Research Database (NHIRD) study implemented a PRISMA-style flow diagram for patient selection, identifying adults with PVC who underwent catheter ablation between 2004 and 2016 [1]. Exclusion criteria specifically removed patients with atrial fibrillation, atrial flutter, or paroxysmal supraventricular tachycardia within 180 days before enrollment to focus the analytical cohort [1]. Baseline demographic and clinical data encompassed age, gender, comorbidities including ventricular tachycardia, acute coronary syndrome, hypertension, diabetes, and various cardiac medications [1].
In the porcine VT ablation target localization study, researchers employed a sophisticated feature extraction pipeline computing 46 signal features representing functional, spatial, spectral, and time-frequency properties from each bipolar and unipolar electrogram [2]. Mapping sites within 6 mm from critical VT circuit components (early, mid-, and late diastolic) were considered potential ablation targets, creating a labeled dataset for supervised learning [2].
Model Training and Validation Protocols
A consistent theme across high-performing studies is the implementation of rigorous validation frameworks. The NHIRD study employed stratified five-fold cross-validation using area under the receiver operating characteristic curve (ROC AUC) [1]. Because rare events can bias ROC analysis, researchers also examined precision-recall (PR) curves as a complementary performance metric [1]. This dual-assessment approach provides a more comprehensive evaluation of model performance on imbalanced datasets.
For the in-hospital mortality prediction study in AF patients, researchers implemented a five-fold cross-validation technique with careful hyperparameter optimization [5]. The dataset was partitioned with 80% for training and 20% for independent validation, with continuous variables showing less than 3% missing data imputed using median values [5]. This methodology ensured robustness despite the real-world nature of the electronic health record data.
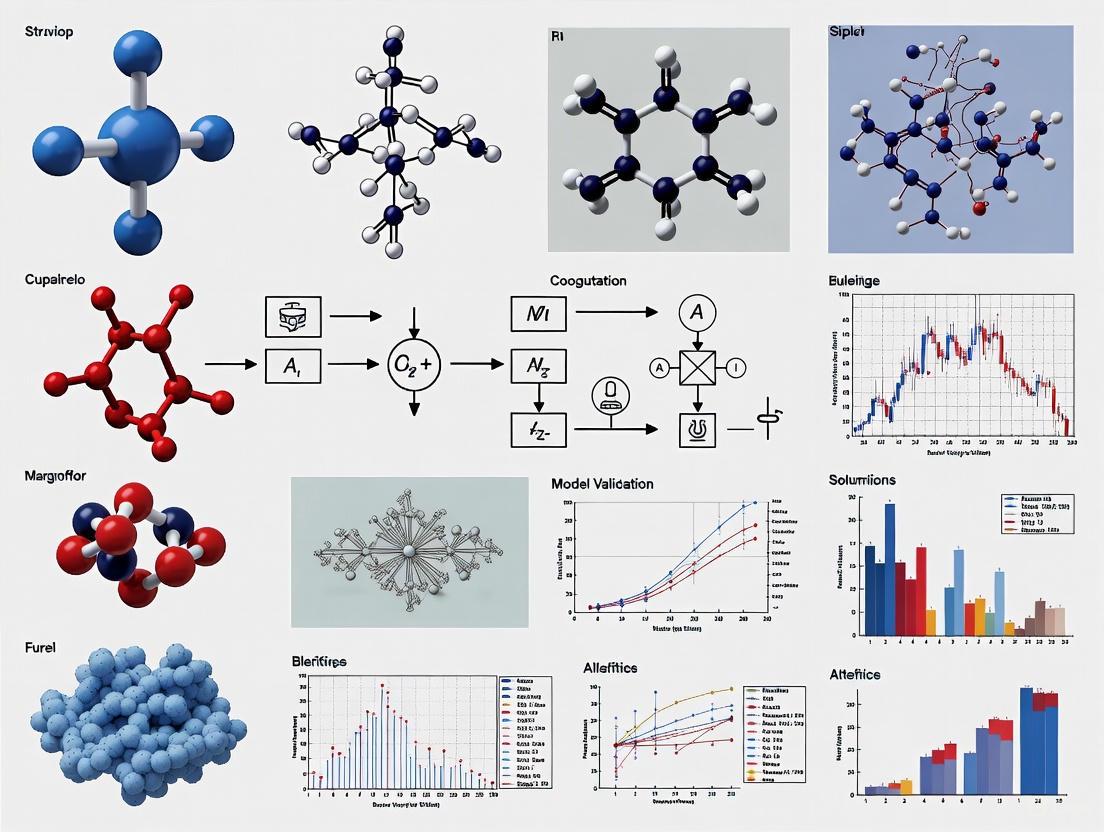
Figure 1: Machine learning workflow for ablation outcome prediction
Table 3: Essential research reagents and computational tools for ablation outcome studies
| Tool Category | Specific Resource | Application in Research | Representative Use Case |
|---|---|---|---|
| Data Sources | Taiwan NHIRD | Nationwide cohort studies | Long-term outcomes in 4,195 PVC ablation patients [1] |
| Mapping Systems | EnSite Precision with Advisor HD Grid | High-density substrate mapping | Collection of 56 substrate maps and 35,068 EGMs [2] |
| ML Algorithms | LightGBM, XGBoost, Random Forest | Outcome prediction and target localization | Three-year HF prediction (AUC: 0.822) [1] |
| Interpretation | SHAP (SHapley Additive exPlanations) | Model explainability | Quantifying feature contributions [1] |
| Sampling Methods | SMOTE, ROSE | Addressing class imbalance | Improving sensitivity for rare events [1] |
The research toolkit for machine learning in ablation outcomes encompasses both data resources and analytical methods. The Taiwan National Health Insurance Research Database (NHIRD) represents a particularly valuable resource, encompassing over 99% of Taiwan's 23 million residents and providing comprehensive coverage of healthcare services across medical centers, regional hospitals, and primary care clinics [1] [4]. This population breadth enables investigation of rare outcomes and long-term trajectories.
For electrophysiological feature extraction, high-density mapping systems such as the Advisor HD Grid with EnSite Precision provide the resolution necessary for machine learning approaches [2]. These systems enable collection of tens of thousands of electrical signals for analysis of functional, spatial, spectral, and time-frequency properties that inform ablation target identification [6].
Interpretability frameworks, particularly SHAP (SHapley Additive exPlanations), have emerged as critical components for clinical translation of machine learning models. By quantifying feature contributions and directionality at both cohort and patient levels, SHAP values help bridge the gap between algorithmic predictions and clinical decision-making [1] [5].
The integration of machine learning into ventricular tachycardia ablation research has generated powerful tools for addressing long-term prognostic gaps in heart failure and mortality. Modern ensemble methods, particularly LightGBM and random forest, consistently demonstrate superior performance for both outcome prediction and ablation target localization. The methodological consistency across studies—including rigorous validation frameworks, appropriate handling of class imbalance, and implementation of model explanation techniques—provides a template for future research in this domain.
As the field progresses, key challenges remain in transporting these models across healthcare systems and integrating them into clinical workflows. The promising performance of explainable models like logistic regression with advanced sampling techniques suggests a path forward that balances predictive power with interpretability. Future research directions should focus on external validation across diverse populations, real-world implementation in electronic health record systems, and prospective evaluation of model-guided clinical decision-making for post-ablation care planning.
Ventricular tachycardia (VT) in the setting of structural heart disease is a life-threatening arrhythmia that poses a significant challenge for clinical management. The heterogeneity of the electrophysiological substrate formed after myocardial infarction plays a crucial role in the development and perpetuation of reentrant VT circuits. Characterization of this substrate heterogeneity, particularly as influenced by infarct location, has become a central focus in developing effective ablation strategies. The complex architectural organization of scar tissue, border zones, and surviving myocardial channels creates the necessary milieu for reentry to occur, with critical isthmus sites often located in scar border zones that harbor abnormal electrograms [7] [8]. This review comprehensively compares current technologies and methodologies for characterizing VT substrate heterogeneity, with particular emphasis on how infarct location influences substrate properties and the subsequent implications for ablation therapy. We examine the experimental protocols, performance metrics, and clinical validation of approaches ranging from novel digital twin technology and machine learning algorithms to advanced electrogram mapping techniques, providing researchers and clinicians with a structured framework for evaluating these rapidly evolving tools in the context of personalized medicine for VT ablation.
Comparative Analysis of VT Substrate Characterization Technologies
The table below summarizes the quantitative performance data and key characteristics of major technologies for VT substrate characterization.
Table 1: Performance Comparison of VT Substrate Characterization Technologies
| Technology | Primary Methodology | Sensitivity (%) | Specificity (%) | AUC | Spatial Agreement | Key Limitations |
|---|---|---|---|---|---|---|
| Heart Digital Twins [7] | MRI-based computational modeling | 81.3 | 83.8 | - | κ=0.46 (moderate) | Limited spatial resolution; Computational intensity |
| Machine Learning (EGM Analysis) [2] | Random forest on electrogram features | 81.4 | 71.4 | 0.821 | - | Limited clinical validation; Animal model data |
| Multi-domain ML with Ensemble Trees [9] | Time, frequency, time-scale, and spatial feature analysis | - | - | - | Accuracy: 93% (cross-val) 84% (leave-one-subject-out) | Small patient cohort (n=9); Single-center study |
| Vector Field Heterogeneity Mapping [10] | Omnipolar mapping of propagation discontinuities | - | - | - | Significant differences between isthmus and normal tissue (p<0.001) | Substantial site overlap; Not stand-alone |
| Conventional Substrate Mapping [8] | Bipolar voltage criteria (scar <0.5 mV, border zone 0.5-1.5 mV) | - | - | - | Established clinical standard | Limited functional assessment; Directional sensitivity |
Table 2: Target Identification Capabilities by Mapping Approach
| Mapping Approach | Critical Site Identification | Infarct Location Considerations | Clinical Validation |
|---|---|---|---|
| Local Abnormal Ventricular Activities (LAVA) [11] | Low-amplitude, high-frequency potentials after or within far-field EGM | Effective for endocardial and epicardial substrates; Non-ischemic and ischemic cardiomyopathy | Elimination correlated with reduced VT recurrence/death (HR 0.49) |
| Late Potentials (LPs) [11] | Signals occurring after terminal portion of surface QRS | Identifies slow conduction regions across infarct locations | 90.5% freedom from VT recurrence with complete LP elimination |
| Isochronal Late Activation Maps (ILAM) [11] | Closely packed isochrone lines indicating slow conduction | Highlights conduction barriers specific to infarct geometry | 75% reduction in VT recurrence compared to standard mapping |
| High-Density Multipolar Mapping [8] [11] | Uncovering low-voltage EGMs and conduction channels | Reveals detailed architecture regardless of infarct location | 97% freedom from device-detected therapies with Advisor HD Grid |
Experimental Protocols for VT Substrate Assessment
Digital Twin Creation and Simulation
The protocol for heart digital twin generation begins with acquisition of 3D late gadolinium-enhanced cardiac magnetic resonance (LGE-CMR) images using either 3T or 1.5T scanners, adapted for patients with cardiac devices [7]. Following image acquisition, myocardial tissue is categorized through semi-automated segmentation with landmark control points placed at various endocardial and epicardial surfaces, with boundaries automatically defined using a variational implicit method. Finite-element meshes with approximately 400 µm resolution are generated, containing ~4 million individual nodes [7]. Fiber directionality is overlaid using a validated rule-based approach, and tissue characteristics (healthy tissue, border zone, dense scar) are superimposed using signal thresholding via the full-width half-maximum approach. Electrophysiological properties are applied to each tissue region: healthy tissue uses the 10 Tusscher ionic model, border zones incorporate longer action potential duration and reduced conduction velocity based on experimental models, and wavefront propagation is simulated by solving the reaction-diffusion partial differential equation using openCARP software on parallel computing systems [7]. VT induction is simulated through pacing protocols applied sequentially to 7 left ventricular sites based on a condensed American Heart Association 17-segment model, with preferential projection onto the closest scar border zone. Pacing delivers a train of 6 beats at 600 ms cycle length followed by up to 3 extrastimuli, with reentry defined as at least 2 rotational cycles at the same site [7].
Machine Learning Model Development
The development of machine learning algorithms for VT substrate characterization follows structured protocols depending on the data modality. For electrogram-based classification, as implemented in the porcine model study, data collection involves invasive electrophysiological studies using multipolar catheters during sinus rhythm and pacing from multiple sites [2]. A total of 46 signal features representing functional, spatial, spectral, and time-frequency properties are computed from each bipolar and unipolar electrogram. For the detection of arrhythmogenic sites in post-ischemic VT, features are extracted across multiple domains: time domain (peak-to-peak amplitude, fragmentation measure), frequency domain, time-scale domain, and spatial domain [9]. The dataset construction involves careful annotation by experienced electrophysiologists blinded to case details and potential positions, using specialized MATLAB graphical interfaces. The machine learning workflow employs a training-validation-testing design with random sampling of patients into respective cohorts (approximately 81%, 9%, and 10% splits). Model training iteratively tests multiple classifiers (random forest, ensemble trees, logistic regression) with performance evaluation through area under the curve (AUC) calculations from internal validation datasets to determine optimal discretization cutoff thresholds [2] [12]. For the 12-lead ECG classification of outflow tract VT origins, the protocol implements a multistage scheme with automated feature extraction from standard ECGs, incorporating features from both sinus rhythm and PVC/VT QRS complexes [12].
High-Density Functional Substrate Mapping
Functional substrate mapping protocols utilize high-density multipolar catheters with closely spaced electrodes (2-6-2 mm spacing) to acquire detailed electroanatomical maps during sinus rhythm [8] [11]. The mapping procedure begins with system setup using 3D electroanatomical mapping systems (CARTO, EnSite Precision, or Rhythmia). The protocol involves obtaining a geometry of the cardiac chamber of interest, followed by high-density mapping with the multipolar catheter ensuring stable catheter contact and position. Points are acquired with a projection distance below 8 mm for accurate spatial localization [9]. During map acquisition, specific attention is directed toward identifying regions of slow conduction characterized by local abnormal ventricular activities (LAVA), late potentials (LPs), and fractionated electrograms. Functional assessment may be enhanced through pacing protocols using short-coupled extrastimuli to uncover hidden slow conduction areas not apparent during baseline rhythm [11]. The definition of unexcitable scar is confirmed by the absence of visible electrograms and lack of local pacing capture, particularly when using mapping catheters with smaller and narrower-spaced bipolar electrodes [8].
Diagram 1: Integrated Workflow for VT Substrate Characterization Technologies
Impact of Infarct Location on Substrate Heterogeneity
The location of myocardial infarction significantly influences the characteristics of the resulting arrhythmogenic substrate, with specific implications for mapping and ablation strategies. Septal infarcts create particularly challenging substrates due to the complex transmural architecture and involvement of the conduction system [8]. In these cases, high-density mapping with multipolar catheters has demonstrated superior capability in identifying conducting channels through the septum that may be missed by conventional point-by-point mapping [8]. Anteroseptal scars specifically require careful differentiation between endocardial and epicardial substrates, with unipolar voltage mapping playing a crucial role in detecting epicardial VT substrate in patients with non-ischemic left ventricular cardiomyopathy [2].
Inferior wall infarcts often exhibit more predictable transmmural patterns but may involve the papillary muscles and peri-valvular regions, creating complex three-dimensional reentry circuits [8]. The functional properties of these substrates demonstrate location-specific characteristics, with inferior scars showing greater prevalence of late potentials in the peri-infarct zone compared to anterior scars [11]. Apical infarcts create substrates with distinct functional properties, often exhibiting smaller critical isthmuses that require higher mapping density for accurate identification [8]. The recent advent of omnipolar mapping technology has proven particularly valuable in characterizing apical substrates by providing voltage, timing, and activation direction independent of catheter orientation [11].
The heterogeneity within infarct border zones also demonstrates location-dependent patterns. Anterior infarcts typically show more extensive border zones with greater electrogram fragmentation compared to inferior infarcts [8]. Vector field heterogeneity mapping has revealed that the entrance sites of VT isthmuses exhibit significantly higher heterogeneity values (0.61 ± 0.24) compared to exit sites (0.44 ± 0.27), with these patterns showing consistent location-specific variations [10]. These findings highlight the importance of tailored mapping approaches based on infarct location to optimize identification of critical ablation targets.
Research Reagent Solutions for VT Substrate Investigation
Table 3: Essential Research Materials for VT Substrate Characterization Studies
| Category | Specific Product/Technology | Research Application | Key Features |
|---|---|---|---|
| Electroanatomical Mapping Systems | CARTO 3 (Biosense Webster) [8] [9] | 3D substrate mapping and navigation | Integration of anatomical and electrophysiological data; Ripple mapping capability |
| EnSite Precision (Abbott) [2] [11] | High-density automated mapping | Advisor HD Grid compatibility; Wavefront direction analysis | |
| Rhythmia (Boston Scientific) [11] | Ultra-high-density mapping | Automatic signal annotation; Lumipoint algorithm | |
| Mapping Catheters | PentaRay (Biosense Webster) [8] [9] | High-resolution substrate mapping | 2-6-2 mm electrodes; Multiple splines for comprehensive coverage |
| Advisor HD Grid (Abbott) [2] [11] | Direction-agnostic mapping | 16 electrodes in 4x4 configuration; 3 mm interelectrode spacing | |
| Octaray (Biosense Webster) [11] | High-density activation mapping | 2-5 mm interelectrode spacing; 48 electrodes total | |
| Computational Modeling Tools | openCARP [7] | Digital twin creation and simulation | Open-source platform for cardiac electrophysiology simulation |
| MATLAB with Custom GUI [9] | Electrogram analysis and annotation | Development of specialized interfaces for signal classification | |
| Imaging Modalities | 3T/1.5T Cardiac MRI [7] | Preprocedural scar characterization | Late gadolinium enhancement for scar visualization |
| Intracardiac Echocardiography [12] | Real-time anatomical guidance | Identification of anatomical structures during ablation |
Discussion and Future Directions
The characterization of VT substrate heterogeneity relative to infarct location represents a critical frontier in personalizing ablation therapy for ventricular arrhythmias. Our analysis demonstrates that while conventional bipolar voltage mapping remains the established standard for substrate assessment, emerging technologies each offer distinct advantages for specific aspects of substrate characterization. Heart digital twins provide unparalleled capability for preprocedural planning and non-invasive identification of VT circuits, achieving sensitivity of 81.3% and specificity of 83.8% for detecting critical VT sites [7]. However, their current limitations in spatial resolution (κ coefficient of 0.46 for agreement with clinical VT sites) and computational demands present barriers to widespread clinical implementation [7].
Machine learning approaches applied to electrogram analysis demonstrate robust performance in automated identification of arrhythmogenic sites, with ensemble tree classifiers achieving 93% accuracy in cross-validation and 84% in leave-one-subject-out validation [9]. The random forest model applied to unipolar signals from sinus rhythm maps provided an AUC of 0.821 with sensitivity of 81.4% and specificity of 71.4% [2]. These approaches show particular promise for reducing operator dependence and procedural time, though they remain limited by dataset sizes and need for broader clinical validation.
The impact of infarct location on substrate characterization efficacy is evident across all technologies. High-density mapping with multipolar catheters has demonstrated remarkable success in addressing the challenges of complex infarct geometries, with one study reporting 97% freedom from device-detected therapies over mean follow-up of 372 days when using the Advisor HD Grid catheter [11]. This represents a substantial improvement over conventional point-by-point mapping (33% freedom from therapies) and even Pentaray mapping (64% freedom from therapies) [11]. The superior performance of high-density mapping in these scenarios highlights the critical importance of mapping resolution and density for accurately characterizing the complex substrate heterogeneity associated with different infarct locations.
Future research directions should focus on integrating multiple complementary technologies into unified platforms that leverage the strengths of each approach. The combination of digital twin preprocedural planning with high-density functional mapping and machine learning-based electrogram classification represents a promising pathway toward comprehensive substrate characterization. Additionally, further investigation is needed to develop infarct location-specific algorithms that optimize mapping and ablation strategies based on the unique characteristics of anterior, inferior, septal, and lateral infarcts. As these technologies continue to evolve and validate in larger clinical trials, their integration into clinical practice promises to significantly improve outcomes for patients with scar-related ventricular tachycardia.
Ventricular tachycardia (VT) is a life-threatening cardiac condition, and catheter ablation remains a cornerstone of its treatment. However, the procedure is plagued by high recurrence rates, often exceeding 50% within one year post-procedure, primarily due to the difficulty in accurately locating critical sites responsible for arrhythmogenesis [13]. The clinical workflow for VT ablation encompasses two critical phases: pre-procedural planning and intra-operative guidance. Traditionally, both phases have relied heavily on electrophysiologists' expertise and conventional substrate mapping techniques, which often depend on single-parameter analysis such as low-voltage areas or delayed potentials [14].
The emergence of machine learning (ML) models is poised to redefine this workflow. These computational approaches offer the potential to extract hidden patterns from complex electrophysiological data, enabling more precise identification of ablation targets. This guide provides an objective comparison of traditional workflows against novel ML-based approaches, with a specific focus on the validation of ML models for VT ablation surgery research. We present structured experimental data and detailed methodologies to equip researchers and scientists with the analytical framework necessary to evaluate these emerging technologies.
Workflow Comparison: Traditional vs. ML-Augmented Approaches
The standard clinical workflow for VT ablation and the emerging ML-augmented alternative represent two distinct paradigms in procedural planning and execution. The table below systematically compares their characteristics across key stages of the procedure.
Table 1: Comparison of Traditional and ML-Augmented VT Ablation Workflows
| Workflow Stage | Traditional Workflow | ML-Augmented Workflow | Key Differentiators |
|---|---|---|---|
| Pre-procedural Planning | Analysis of pre-operative MRI/CT scans; manual review of electroanatomic maps (EAM); subjective identification of low-voltage zones and abnormal potentials. | Automated analysis of EAMs using ML models; extraction of multi-domain features from intracardiac electrograms (EGMs); data-driven prediction of critical sites. | Shift from subjective, single-parameter analysis to objective, multi-parametric prediction. |
| Target Identification | Relies on visual inspection of EAMs for scar and border zones; focal activation mapping during VT; pace mapping. | ML model (e.g., Random Forest) processes 46+ EGM features to classify and predict arrhythmogenic sites with a probabilistic output. | Moves beyond geometric and activation-based mapping to a feature-based, algorithmic classification. |
| Intra-operative Guidance | Real-time EAM creation; fluoroscopic/electroanatomic navigation; manual annotation of ablation lesions. | Real-time visualization of ML-predicted targets overlaid on the EAM; potential for dynamic updates based on new data points. | Provides a quantitative, continuously updated roadmap, potentially reducing subjective interpretation during the procedure. |
| Post-procedural Validation | Acute procedural success defined by non-inducibility of VT; long-term follow-up for recurrence via Holter monitoring. | Correlation of ML-predicted ablation sites with acute termination sites and long-term clinical outcomes; model refinement based on recurrence data. | Enables a feedback loop for model validation and improvement, linking specific mapped features to clinical success. |
Performance Data: Quantitative Comparison of Mapping Strategies
The efficacy of a mapping and ablation strategy is ultimately quantified by its accuracy and predictive power. The following table summarizes key performance metrics from recent studies, comparing traditional substrate mapping with the novel multi-feature machine learning approach.
Table 2: Quantitative Performance Metrics of Target Identification Strategies
| Mapping Strategy | AUC (Area Under Curve) | Sensitivity | Specificity | Key Predictive Features | Validation Model |
|---|---|---|---|---|---|
| Traditional Low-Voltage Mapping | 0.67 [14] | Not Specified | Not Specified | Bipolar/Unipolar Voltage | Chronic MI Porcine Model |
| ML-Based Multi-Feature Mapping (Random Forest) | 0.821 [14] [2] | 81.4% [13] [2] | 71.4% [13] [2] | Repolarization Time (RT), High-Frequency Components (R120-160), Spatial Repolarization Heterogeneity (GradARI) [14] | Chronic MI Porcine Model |
Experimental Protocols for ML Model Validation
A critical understanding of ML model performance requires a detailed examination of the experimental methodologies used for their development and validation. The following section outlines the core protocols from a seminal study in the field.
Data Acquisition and Pre-processing
- Animal Model: The protocol was developed and validated in a chronic myocardial infarction (MI) porcine model (n=13), chosen for its physiological similarity to human cardiac size and function [14] [13] [2].
- Electrophysiological Data Collection: Fifty-six substrate maps were acquired using a high-density multipolar catheter (Advisor HD Grid) under the EnSite Precision system. Data included 35,068 intracardiac electrograms (EGMs) recorded during sinus rhythm and pacing from multiple sites (left, right, and biventricular) [14] [2].
- Ground Truth Definition: Ventricular tachycardia was induced in all subjects, leading to the mapping and precise localization of 36 VT circuits. Critical sites within the circuit (e.g., exhibiting early, mid, or late diastolic components) were identified. Mapping points within a 6 mm radius of these sites were defined as positive samples (potential ablation targets) for the ML model [2].
Feature Engineering and Model Training
- Feature Extraction: A custom MATLAB algorithm was used to extract 46 distinct features from each bipolar and unipolar EGM signal. These features spanned multiple domains [14]:
- Functional: Activation time (AT), repolarization time (RT).
- Spatial: Repolarization dispersion (GradARI).
- Spectral & Time-Frequency: Central frequency (fU), signal energy in specific bands (e.g., E0-160, R120-160).
- Model Development: Several machine learning models were trained and evaluated. The Random Forest classifier, an ensemble learning method, demonstrated superior performance, particularly when trained on unipolar EGM signals from sinus rhythm maps [14] [2]. Unipolar signals are thought to provide a more comprehensive picture by capturing both local and far-field electrical activity [14].
The workflow for this experimental protocol is visualized below.
For researchers aiming to replicate or build upon this work, the following table details key materials and computational tools referenced in the foundational studies.
Table 3: Essential Research Reagents and Solutions for VT Ablation ML Research
| Item | Specification / Function | Experimental Role |
|---|---|---|
| Chronic Myocardial Infarction Porcine Model | Large animal model with induced MI to simulate human ischemic cardiomyopathy and VT substrate. | Provides a physiologically relevant platform for data acquisition and model validation [14] [2]. |
| High-Density Grid Catheter | Advisor HD Grid Catheter (e.g., 16 electrodes). | Enables high-resolution, simultaneous acquisition of intracardiac electrograms from multiple vectors for detailed substrate mapping [14] [2]. |
| Electroanatomic Mapping System | EnSite Precision or comparable system. | Provides the platform for 3D spatial localization of mapping points, signal recording, and visualization of substrate maps [2]. |
| Custom MATLAB Algorithm | Algorithm for extracting 46 multi-domain features from EGM signals. | Converts raw EGM signals into a structured feature set that serves as the input for machine learning models [14]. |
| Machine Learning Algorithms | Random Forest, Logistic Regression, etc. (via Scikit-learn, R, or similar). | Classifies mapping points as targets or non-targets based on the input features; Random Forest demonstrated top performance in initial studies [14] [2] [15]. |
Analytical Framework and Future Directions
The logical relationship between EGM features, the ML model, and the clinical outcome is central to understanding this technology. The following diagram illustrates this pathway and its potential future evolution.
The path forward for ML in VT ablation is rich with potential. Future developments are likely to focus on the integration of AI with Digital Twin technology, creating patient-specific virtual heart models that incorporate scar anatomy, fiber orientation, and simulated electrical propagation to refine target prediction beyond statistical correlations [14]. Furthermore, the advent of 5G technology promises to facilitate real-time remote collaboration and guidance, potentially standardizing and democratizing expert-level procedural planning and support [16]. As these models evolve, a critical focus will remain on rigorous validation in human randomized controlled trials and the seamless integration of these computational tools into existing clinical workflows, ensuring they augment rather than disrupt the electrophysiologist's decision-making process.
In the field of ventricular tachycardia (VT) ablation, the precise definition of a "successful ablation site" is the cornerstone for developing and validating new targeting technologies, particularly machine learning (ML) models. The gold standard serves as the fundamental ground truth against which the performance of all predictive algorithms is measured. However, establishing this standard is complex, as it is not a single entity but a concept defined through a convergence of evidence from various mapping techniques and procedural outcomes. This guide provides a comparative analysis of the methodologies and technologies used to define and target these critical sites, framing the discussion within the broader need for robust validation in computational research.
Comparative Analysis of Ground-Truth Definitions
The definition of a successful ablation site varies significantly depending on the mapping strategy and technological approach employed. The table below synthesizes the performance data and defining characteristics of the primary methods used in contemporary practice and research.
Table 1: Comparative Performance of Ablation Target Localization Methods
| Method / Technology | Key Defining Metric for Success | Reported Performance/Accuracy | Primary Clinical Context | Key Limitations |
|---|---|---|---|---|
| In-Silico Pace-Mapping [17] | Distance between computed pacing site and visual exit site (ground truth). | High-Res Scar: 7.3 ± 7.0 mmLow-Res Scar: 8.5 ± 6.5 mmNo-Scar: 13.3 ± 12.2 mm | Pre-procedural planning in patient-specific computational models. | Relies on the accuracy of the underlying heart model and scar reconstruction. |
| Machine Learning (Random Forest on EGMs) [2] | Automated localization of VT critical sites based on electrogram features. | AUC: 0.821Sensitivity: 81.4%Specificity: 71.4% | Intra-procedural target identification from substrate maps in a porcine model. | Model trained and validated in an animal model; requires human clinical validation. |
| Entrainment Mapping [18] | Concealed fusion with PPI - TCL < 30 ms and S-QRS < 50% of TCL. | Success rates up to 70% for RF ablation at defined sites. | Intra-procedural mapping of hemodynamically stable, reentrant VT. | Infeasible for unstable VT; prone to confusion from bystander sites. |
| Paced Field Ablation (PFA) - VCAS Trial [19] | Freedom from VT recurrence at follow-up. | 78% freedom from VT. | Treatment of scar-related VT with a novel contact-force PFA system. | Early-stage data (first-in-human trial); two of 22 patients had significant worsening of heart failure. |
| Activation Mapping [18] | Identification of the earliest presystolic electrogram preceding the QRS complex (for focal VT) or the critical isthmus (for reentry). | N/A (Qualitative assessment) | Intra-procedural mapping of hemodynamically stable VT. | Feasibility can be as low as 10-30% due to VT instability. |
Detailed Experimental Protocols
To ensure the reproducibility of ML validation studies, a clear understanding of the experimental protocols used to establish ground truth is essential. The following section details the methodologies from key cited works.
Protocol 1: In-Silico Pace-Mapping for VT Exit Site Localization
This protocol outlines a computational method for identifying VT exit sites, which can serve as a pre-procedural, non-invasive ground truth [17].
- Objective: To investigate how the anatomical detail of scar reconstructions within computational heart models influences the ability of in-silico pace mapping to identify VT origins.
- Materials: Patient-specific heart models were reconstructed from high-resolution contrast-enhanced cardiac magnetic resonance (CMR) from 15 patients.
- Workflow:
- Model Creation & VT Simulation: Patient-specific models were created from CMR. VT was simulated in these high-resolution models.
- Scar Alteration: The scar anatomy in the models was altered to mimic low-quality imaging and the absence of scar data.
- Pace-Mapping Simulation: The ECG of each simulated VT was used as input. The models were then paced from 1,000 random sites surrounding the infarct.
- Correlation & Accuracy Assessment: Correlations between the VT and paced ECGs were computed. The accuracy was assessed by measuring the distance (d) between visually identified exit sites (ground truth) and the pacing locations with the strongest correlation.
Protocol 2: Machine Learning for Ablation Target Localization from Substrate Maps
This protocol describes the development of an ML model that uses electrogram features to localize VT critical sites in a pre-clinical animal model [2].
- Objective: To propose a machine learning approach for improved identification of ablation targets based on intracardiac electrograms (EGMs) features.
- Materials: 13 pigs with chronic myocardial infarction; Advisor HD grid multipolar catheter with EnSite Precision mapping system.
- Workflow:
- Data Acquisition: 56 substrate maps and 35,068 EGMs were collected during sinus rhythm and pacing.
- Ground Truth Definition: 36 VTs were induced and mapped. Sites within 6 mm of a confirmed critical site (e.g., early, mid, or late diastolic components of the circuit) were labeled as positive ablation targets.
- Feature Extraction: Forty-six signal features representing functional, spatial, spectral, and time-frequency properties were computed from each bipolar and unipolar EGM.
- Model Training & Validation: Several machine learning models were trained to classify sites as targets or non-targets. The random forest model was identified as the best performer and validated.
Protocol 3: VT Simulation-Guided Transcoronary Ethanol Ablation
This case report protocol illustrates a hybrid approach using simulation to plan an alternative ablation strategy when conventional approaches fail [20].
- Objective: To utilize VT simulation to identify an epicardial re-entry circuit and guide a transcoronary venous ethanol ablation.
- Materials: Late gadolinium-enhanced cardiac magnetic resonance (LGE-CMR) imaging; mapping and ablation catheters; equipment for coronary venography and ethanol infusion.
- Workflow:
- Simulation: A patient-specific heart model was constructed from LGE-CMR. The simulation identified a sustained epicardial re-entry in the apical region that was not accessible via standard endocardial ablation.
- Endocardial Ablation Attempt: Conventional endocardial mapping and radiofrequency ablation were attempted but failed to eliminate the VT.
- Coronary Venous Mapping & Ethanol Ablation: The coronary venous system was mapped. A branch coursing through the simulated epicardial target region was identified. Ethanol was infused into this branch, resulting in the disappearance of premature beats and non-inducibility of VT.
The following workflow diagram synthesizes the key steps from these experimental protocols, highlighting the role of computational and mapping data in defining the ablation target.
The Scientist's Toolkit: Essential Research Reagents & Materials
For researchers designing experiments to validate new ML models or ablation technologies, the following table catalogues critical tools and their functions as derived from the analyzed studies.
Table 2: Key Research Reagent Solutions for VT Ablation Studies
| Tool / Technology | Function in Research | Example Use Case |
|---|---|---|
| Late Gadolinium-Enhanced CMR (LGE-CMR) | Provides high-resolution 3D scar anatomy, differentiating core scar from border zone. | Reconstruction of patient-specific computational models for VT simulation [17] [20]. |
| Multipolar Mapping Catheter (e.g., Advisor HD Grid) | High-density acquisition of intracardiac electrograms (EGMs) for substrate characterization. | Collecting EGM signal features for machine learning model training [2]. |
| 3D Electroanatomic Mapping System (EAM) | Integrates electrical data with anatomical geometry to create a 3D substrate map. | Core platform for intra-procedural mapping and annotation of ground truth sites [2] [18]. |
| Computational Modeling & Simulation Software | Enables in-silico testing of arrhythmia mechanisms and ablation strategies without patient risk. | Assessing the robustness of pace-mapping to image quality [17] and planning ablation [20]. |
| Pulsed Field Ablation (PFA) System | A non-thermal ablation energy source that may create more predictable, full-thickness lesions. | Evaluating a new technology's efficacy in treating scar-related VT (e.g., VCAS Trial) [19]. |
| BVFP | BVFP, MF:C13H8BrF3N2O, MW:345.11 g/mol | Chemical Reagent |
| Sodium difluoro(oxalato)borate | Sodium difluoro(oxalato)borate, CAS:1016545-84-8, MF:C2BF2NaO4, MW:159.82 g/mol | Chemical Reagent |
Establishing the gold standard for successful VT ablation sites is a multi-faceted process. No single method operates in isolation; rather, the most reliable ground truth emerges from the convergence of pre-procedural computational simulations, intra-procedural mapping data (activation, pace, and entrainment), and acute procedural outcomes. As novel technologies like machine learning and pulsed field ablation continue to evolve, their validation will depend on a critical comparison against this composite standard. The experimental protocols and tools detailed in this guide provide a framework for researchers to rigorously assess new targeting strategies, ultimately accelerating the development of more effective and personalized therapies for ventricular tachycardia.
Methodological Pipeline: Building and Applying ML Models for VT Ablation
The validation of machine learning models for ventricular tachycardia (VT) ablation surgery research represents a critical frontier in precision cardiology. Accurately predicting patient-specific risks and outcomes, such as procedural success, recurrence of arrhythmias, or long-term complications, is essential for improving clinical decision-making. This guide provides a structured, objective comparison of common machine learning algorithms, from the foundational logistic regression to advanced ensembles like XGBoost and LightGBM, within this specific clinical context. We summarize quantitative performance data from recent studies, detail experimental protocols, and provide visual resources to inform researchers and clinicians in their model selection process.
Performance Benchmarking in VT Ablation Research
The selection of an optimal algorithm is contingent on the specific clinical endpoint. The following tables consolidate performance metrics from recent studies, providing a direct comparison of logistic regression, decision trees, random forest, XGBoost, and LightGBM.
Table 1: Benchmarking Model Performance for Various Cardiovascular Endpoints
| Clinical Endpoint | Best Performing Model(s) | Key Performance Metrics (AUROC) | Comparative Model Performance |
|---|---|---|---|
| 3-Year Heart Failure (Post-PVC Ablation) | LightGBM [1] | 0.822 (with ROSE) | LightGBM > XGBoost > Random Forest > Logistic Regression > Decision Tree |
| 3-Year Mortality (Post-PVC Ablation) | Logistic Regression, LightGBM [1] | 0.886, 0.882 (both with ROSE) | Logistic Regression ≈ LightGBM > XGBoost > Random Forest > Decision Tree |
| Malignant Ventricular Arrhythmia (MVA) (Post-AMI) | LightGBM [21] | 0.827 (Internal Validation) | LightGBM > XGBoost > Random Forest |
| In-Hospital Death (Post-AMI) | Random Forest [21] | 0.784 (Internal Validation) | Random Forest > XGBoost > LightGBM |
| Atrial Fibrillation Recurrence (Post-Ablation) | LightGBM [22] | 0.848 (Testing Set) | LightGBM > SVM > AdaBoost > Gradient Boosting |
| Etiological Diagnosis of VT | XGBoost [23] | Precision: 88.4%, Recall: 88.5%, F1: 88.4% | XGBoost > Other Models Tested |
Table 2: Architectural and Practical Comparison of XGBoost and LightGBM
| Aspect | XGBoost | LightGBM |
|---|---|---|
| Tree Growth Strategy | Level-wise (builds trees breadth-first) [24] [25] | Leaf-wise (builds trees depth-first, focusing on promising leaves) [24] [25] |
| Handling of Categorical Features | Requires pre-processing (e.g., one-hot encoding) [25] | Native support (can specify categorical columns) [25] |
| Computational Efficiency | Slower training speed on large datasets, more memory-intensive [24] [25] | Faster training speed, lower memory usage [24] [25] |
| Overfitting Tendency | More robust on smaller datasets due to level-wise growth [24] | Can overfit on small datasets; controlled with max_depth [24] [25] |
| Ideal Use Case | Smaller datasets, high-stakes scenarios requiring model robustness [24] | Large-scale datasets, high-dimensional/sparse data, rapid prototyping [24] |
Detailed Experimental Protocols from Cited Studies
To ensure reproducible and clinically relevant model validation, the following methodologies are commonly employed in the field.
Data Preprocessing and Class Imbalance Handling
Cardiovascular outcome datasets often suffer from class imbalance (e.g., few patients experience mortality). To address this, studies use sophisticated techniques within a cross-validation framework to avoid biased performance estimates [1] [22].
- Synthetic Minority Over-sampling Technique (SMOTE): Generates synthetic examples of the minority class in the feature space [1] [22].
- Random Over-Sampling Examples (ROSE): Creates a smoothed bootstrap sample by generating new cases from a kernel density estimate of the classes [1].
Model Training and Validation Framework
A robust validation strategy is non-negotiable for clinical machine learning models. The stratified five-fold cross-validation approach is a gold standard [1] [21] [22].
- Cohort Splitting: The patient dataset is first randomly split into a training set (typically 70-80%) and a held-out testing set (20-30%). This split is often stratified to preserve the proportion of the outcome class in both sets [22].
- Cross-Validation on Training Set: The training set is further divided into five folds. The model is trained on four folds and validated on the remaining one; this process is repeated five times so that each fold serves as the validation set once. Performance metrics (e.g., AUC) are averaged over the five iterations [1].
- Hyperparameter Tuning: This is performed within the cross-validation loop to select the parameters that yield the best average validation performance.
- Final Evaluation: The final model, trained on the entire training set with the best parameters, is evaluated on the untouched testing set to report an unbiased estimate of its performance [22].
Model Interpretability and Clinical Explanation
For clinical adoption, model predictions must be interpretable. SHapley Additive exPlanations (SHAP) is the dominant method used to quantify the contribution of each feature to an individual prediction, aligning model outputs with clinical knowledge [1] [26] [22]. For example, studies have consistently identified age, prior heart failure, and specific comorbidities like malignancy and end-stage renal disease as the most influential predictors for long-term heart failure risk after ablation, validating the model's clinical face-validity [1].
Workflow Diagram for Model Benchmarking
The following diagram illustrates the logical workflow for benchmarking machine learning algorithms in clinical research, from data preparation to model selection.
Building and validating machine learning models for clinical research requires a suite of computational and data resources.
Table 3: Essential Research Reagents and Solutions
| Tool/Resource | Function/Benefit | Example Use in Context |
|---|---|---|
| Structured Clinical Datasets | Provides labeled data for model training and testing. | Nationwide claims databases (e.g., NHIRD [1]) or single-center EHR data [23] with ICD codes for patient cohort identification. |
| SHAP (SHapley Additive exPlanations) | Explains model output by quantifying feature contribution for each prediction [26] [23]. | Identifies key predictors (e.g., BNP, NLR [22]) for VT recurrence, fostering clinical trust and model validation. |
| Synthetic Minority Over-sampling (SMOTE) | Addresses class imbalance by generating synthetic minority class samples [1] [22]. | Improves model sensitivity in predicting rare but critical events like mortality or malignant arrhythmias. |
| Stratified K-Fold Cross-Validation | Robust validation technique that preserves class distribution across folds [1] [21]. | Provides a reliable estimate of model generalizability and mitigates overfitting during algorithm benchmarking. |
| High-Performance Computing (GPU) | Accelerates the training process of computationally intensive ensemble models [24] [25]. | Essential for rapid iteration and hyperparameter tuning of XGBoost (using tree_method='gpu_hist') and LightGBM (using device='gpu'). |
The benchmarking data clearly indicates that no single algorithm dominates all clinical prediction tasks in VT ablation research. While LightGBM demonstrates superior speed and often leads in performance for large datasets predicting heart failure and arrhythmia recurrence, XGBoost provides robust and highly accurate models for etiological diagnosis and other tasks. Notably, the transparent Logistic Regression baseline remains highly competitive for certain endpoints like mortality prediction, especially when paired with resampling techniques. The ultimate algorithm selection must be guided by the specific clinical question, dataset size and structure, and the imperative for model interpretability. A rigorous, protocol-driven approach to validation and explanation is paramount for the successful translation of these models into clinical research and practice.
The management of ventricular tachycardia (VT) and premature ventricular complexes (PVCs) has entered a transformative phase with the integration of artificial intelligence (AI) and machine learning (ML) models. These computational approaches are revolutionizing the prediction of arrhythmia origins, recurrence risks post-ablation, and long-term clinical complications. For researchers and drug development professionals, understanding these key prediction tasks is critical for developing targeted therapies and improving patient stratification. ML models leverage complex electrophysiological data, imaging parameters, and clinical variables to generate predictive insights that surpass traditional statistical methods, offering unprecedented opportunities for personalized medicine in cardiology.
The validation of these ML models requires rigorous comparison against established diagnostic and prognostic methods. This guide provides a comprehensive comparison of model performances, experimental protocols, and essential research tools, framing the discussion within the broader thesis of ML model validation for VT ablation research. By objectively analyzing the data and methodologies, we aim to establish a framework for evaluating the clinical readiness and implementation potential of these emerging technologies.
Prediction Task I: Localizing Arrhythmia Origins
Accurately determining the anatomical origin of ventricular arrhythmias is fundamental for successful ablation therapy. Traditional approaches rely on electrocardiographic (ECG) characteristics and invasive mapping, but ML algorithms are demonstrating superior capabilities in processing complex spatial and signal data.
Electrocardiographic Predictors and Features
The 12-lead surface ECG remains the initial diagnostic tool for approximating VT/PVC origins. Specific features provide localization clues, particularly for arrhythmias originating from challenging regions like the left ventricular summit (LVS). Table 1 summarizes key ECG characteristics and their predictive values for localization.
Table 1: ECG Predictors for Localizing Ventricular Arrhythmia Origins
| Predictor | Anatomical Implication | Predictive Performance | Clinical Utility |
|---|---|---|---|
| Maximum Deflection Index (MDI) >0.54 [27] | Suggests epicardial origin | Sensitivity: ~71-81%; Specificity: ~71-81% [27] [2] | Differentiates epicardial from endocardial sites |
| Q-wave ratio in aVL/aVR >1.85 [27] | Indicates origin in accessible LVS area | Sensitivity: 100%; Specificity: 72% when combined with other criteria [27] | Guides decision for epicardial access |
| "Breakthrough pattern" in V2 [27] | Suggests septal origin near LAD | Not quantified | Identifies challenging sites near coronary arteries |
| Pseudodelta wave >34 ms [27] | Indicates epicardial origin | Not quantified | Supports epicardial origin hypothesis |
| R-wave ratio in V1/V2 [27] | Differentiates RVOT from LVOT origins | Not quantified | Distinguishes right/left outflow tracts |
Machine Learning Approaches for Automated Localization
ML models trained on intracardiac electrogram features can automatically identify ablation targets. A recent study developed and validated an ML approach for locating VT ablation targets from substrate maps in a porcine model of chronic myocardial infarction [2].
Experimental Protocol:
- Animal Model: Thirteen pigs with chronic myocardial infarction.
- Data Acquisition: Multipolar catheters (Advisor HD Grid, EnSite Precision) were used to collect 56 substrate maps and 35,068 intracardiac electrograms (EGMs) during sinus rhythm and pacing from multiple sites.
- Feature Extraction: Forty-six signal features representing functional, spatial, spectral, and time-frequency properties were computed from each bipolar and unipolar EGM.
- Ground Truth: Thirty-six VTs were localized and mapped with early, mid-, and late diastolic components of the circuit. Mapping sites within 6 mm from critical sites were labeled as potential ablation targets.
- Model Training: Several ML models were developed and compared, including random forest, logistic regression, and others.
The random forest classifier achieved the best performance using unipolar signals from sinus rhythm maps, with an area under the curve (AUC) of 0.821, sensitivity of 81.4%, and specificity of 71.4% [2]. This demonstrates the potential of ML to augment clinical decision-making during substrate-based ablation procedures.
Figure 1: Machine Learning Workflow for VT Localization. This diagram illustrates the experimental pipeline for developing ML models to localize VT ablation targets from substrate maps in a porcine model.
Prediction Task II: Estimating Recurrence Risk After Ablation
Predicting the likelihood of arrhythmia recurrence after catheter ablation is crucial for patient selection, follow-up planning, and clinical trial design. Recurrence rates vary significantly based on underlying cardiomyopathy, procedural success, and patient characteristics.
Recurrence Rates Across Patient Populations
Table 2 compares VT recurrence rates across different patient populations and ablation contexts, providing essential benchmarking data for model validation.
Table 2: VT/PVC Recurrence Rates After Catheter Ablation
| Patient Population | Recurrence Rate | Follow-up Duration | Predictors of Recurrence |
|---|---|---|---|
| Ischemic Cardiomyopathy (ICMP) [28] | 54.8% | 36 months | Older age, lower LVEF, more comorbidities, higher number of inducible VTs |
| Non-Ischemic Cardiomyopathy (NICMP) [28] | 38.9% | 36 months | Less frequent than ICMP |
| Pediatric PVCs [29] | 42.5% (persistent) | 45 months | Older age at onset, female sex |
| ICMP with first-line ablation [30] | 50.7% (composite endpoint) | 4.3 years | Not specified |
| ICMP with first-line AAD [30] | 60.6% (composite endpoint) | 4.3 years | Not specified |
Machine Learning for Recurrence Prediction
A dedicated study designed an ML model specifically to determine the recurrence rate of PVCs and idiopathic VT after radiofrequency catheter ablation [31]. While complete performance metrics are not provided in the available excerpt, the study compares multiple ML approaches including logistic regression (LR), decision trees (DT), support vector machines (SVM), multilayer perceptron (MLP), and extreme gradient boosting (XGBoost) [31]. This represents a direct application of ML to the recurrence prediction task, moving beyond traditional clinical factor analysis.
Prediction Task III: Forecasting Long-Term Complications
Beyond arrhythmia recurrence, predicting long-term clinical outcomes including mortality, cardiomyopathy development, and drug-related adverse events is essential for comprehensive risk assessment.
Mortality and Adverse Event Rates
Table 3 compares long-term outcomes after VT ablation and antiarrhythmic drug therapy, providing critical data for prognostic model validation.
Table 3: Long-Term Complications and Outcomes After VT Therapy
| Outcome Measure | ICM Patients | NICM Patients | Therapy Context |
|---|---|---|---|
| Overall Mortality [28] | 22% | 7% | VT ablation |
| Cardiac Mortality [28] | 19% | 6% | VT ablation |
| All-cause Death (Ablation) [30] | 22.2% | Not reported | First-line therapy |
| All-cause Death (AAD) [30] | 25.4% | Not reported | First-line therapy |
| PVC-Induced Cardiomyopathy Risk [27] | 12-15% over 1-2 years | Not specified | High PVC burden (>20%) |
| Major Bleeding (Ablation) [30] | 1% | Not reported | Procedure-related |
| Drug-Related Adverse Events [30] | 21.6% | Not reported | Amiodarone or sotalol |
PVC-Induced Cardiomyopathy Prediction
A high PVC burden is a recognized risk factor for developing cardiomyopathy. Studies report that 10-15% of patients with PVCs from the LVS develop PVC-induced cardiomyopathy, particularly with daily PVC burden exceeding 20% [27]. In pediatric populations, a high initial PVC burden (≥25%) is associated with persistent PVCs and potential ventricular dysfunction [29].
The VANISH2 trial provides crucial comparative data on first-line ablation versus antiarrhythmic drugs, demonstrating that catheter ablation reduces the composite endpoint of death, VT storm, appropriate ICD shock, or treated sustained VT (50.7% vs. 60.6%; HR, 0.75) compared to AAD therapy in ischemic cardiomyopathy patients [30].
Figure 2: PVC Complication Pathway and Outcomes. This diagram illustrates the progression from high PVC burden to cardiomyopathy and subsequent treatment outcomes.
The Scientist's Toolkit: Essential Research Reagents and Materials
Advancing research in VT/PVC prediction requires specialized tools and platforms. Table 4 catalogs essential research reagents and their applications in experimental protocols.
Table 4: Essential Research Reagents and Platforms for VT/PVC Research
| Reagent/Platform | Specification | Research Application |
|---|---|---|
| Multipolar Catheter [2] | Advisor HD Grid | High-density electrophysiological mapping |
| Electroanatomic Mapping System [2] | EnSite Precision | 3D reconstruction of cardiac geometry and substrate |
| Signal Processing Software [2] | Custom MATLAB/Python | Extraction of 46 EGM features (functional, spatial, spectral, time-frequency) |
| Machine Learning Libraries [31] | Scikit-learn, XGBoost | Implementation of LR, DT, SVM, MLP, XGBoost algorithms |
| Porcine MI Model [2] | Chronic myocardial infarction | Validation of ablation target localization algorithms |
| Holter Monitoring System [29] | 24-hour ambulatory ECG | PVC burden quantification and morphology analysis |
| qc1 | qc1, MF:C23H16F3N3O2S, MW:455.5 g/mol | Chemical Reagent |
| Mafp | Mafp, MF:C21H36FO2P, MW:370.5 g/mol | Chemical Reagent |
The prediction of VT/PVC origins, recurrence risk, and long-term complications represents a critical frontier in clinical electrophysiology. Traditional clinical factors provide foundational prognostic information, but ML approaches demonstrate emerging superiority in processing complex electrophysiological signals for precise localization and personalized risk assessment. The validation of these models requires rigorous benchmarking against the performance metrics and experimental protocols outlined in this guide. As the field advances, standardized evaluation frameworks will be essential for translating algorithmic predictions into improved clinical outcomes for patients with ventricular arrhythmias.
The volume and complexity of patient data in electrophysiology have grown exponentially, creating significant cognitive burden for clinicians navigating fragmented electronic health record (EHR) interfaces during complex procedures such as ventricular tachycardia (VT) ablation [32]. In high-pressure environments like the electrophysiology laboratory, where time-critical decisions must be made based on rapidly accessible information, poor EHR usability and unfiltered data presentation contribute to inefficiencies, potential errors, and clinician burnout [32]. Patient-centered dashboards that automatically extract and visually organize relevant clinical data offer a promising strategy to mitigate these challenges by supporting clinical reasoning and rapid comprehension [32]. For VT ablation research and practice, integrating machine learning (ML) risk prediction models directly into EHR dashboards represents a transformative approach to personalizing procedural planning and long-term management. This guide objectively compares the current landscape of EHR integration frameworks, visualization strategies, and validation methodologies for procedural decision support in ablation therapy.
EHR Dashboard Design Frameworks for Procedural Support
Core Design Principles and Data Filtering Methodologies
Effective EHR dashboards for procedural support employ either rule-based systems or AI-driven models to filter and prioritize clinically relevant parameters from extensive patient records [32]. These systems emphasize alignment with clinicians' cognitive workflows, presenting key parameters such as medications, allergies, vital signs, past medical history, and care directives through intuitive visual interfaces [32].
The design processes often incorporate user-centered and iterative methods, though the rigor of evaluation varies widely across implementations [32]. Successful dashboards function as a central visual interface that interprets and displays vital performance measurements and patient information, breaking down complex siloed data into simplified visual forms such as charts, graphs, and summary tables [33]. These systems provide role-specific views that present only relevant KPIs to different users (physicians, nurses, administrators), with real-time data refresh capabilities and drill-down functionalities for accessing detailed patient records [33].
Quantitative Assessment of Dashboard Efficacy
Table 1: Measured Outcomes of Implemented EHR Dashboard Systems
| Implementation Setting | Productivity Metric | Improvement Percentage | Key Functionalities |
|---|---|---|---|
| General Provider Practices | Administrative & Clinical Task Completion | 40% faster [33] | Centralized task automation, real-time patient flow tracking, rapid analytics visualization |
| UCHealth Nursing Staff | Initial Training Satisfaction | 75% increase [34] | Asynchronous learning integration, multiple access points for educational materials |
| UCHealth Nursing Staff | Self-Reported Efficiency | 27% increase [34] | Workflow-embedded training resources, just-in-time information access |
| M Health Fairview | Net EHR Experience Score (NEES) | 19-point higher vs. peers [34] | Centralized learning library, support chat, provider efficiency sessions |
| M Health Fairview | EHR-Enabled Efficiency Agreement | 15 percentage-point higher [34] | Single source of truth architecture, workflow-integrated training |
Machine Learning Model Performance for Ablation Risk Stratification
Comparative Algorithm Performance in Cardiovascular Applications
ML-based prediction models have demonstrated superior discriminatory performance compared to conventional risk scores across multiple cardiovascular applications. A 2025 systematic review and meta-analysis of 10 studies (n=89,702 individuals) found that ML-based models significantly outperformed conventional risk scores for predicting major adverse cardiovascular and cerebrovascular events (MACCEs) in patients with acute myocardial infarction who underwent percutaneous coronary intervention [35].
Table 2: Machine Learning vs. Conventional Risk Score Performance for Cardiovascular Event Prediction
| Prediction Task | ML Model Type | Conventional Comparator | Performance Metric | ML Performance | Conventional Score Performance |
|---|---|---|---|---|---|
| Mortality post-PCI | Random Forest, Logistic Regression [35] | GRACE, TIMI [35] | ROC AUC | 0.88 (95% CI 0.86-0.90) [35] | 0.79 (95% CI 0.75-0.84) [35] |
| 3-Year HF after PVC Ablation | LightGBM with ROSE [1] | Logistic Regression Baseline [1] | ROC AUC | 0.822 [1] | Not specified |
| 3-Year Mortality after PVC Ablation | LightGBM with ROSE [1] | Logistic Regression with ROSE [1] | ROC AUC | 0.882 [1] | 0.886 [1] |
For predicting three-year heart failure after premature ventricular contraction (PVC) ablation, the LightGBM model with random over-sampling examples (ROSE) achieved the highest ROC AUC at 0.822, while for three-year mortality, both logistic regression with ROSE and LightGBM with ROSE showed balanced performance with ROC AUCs of 0.886 and 0.882, respectively [1]. Pairwise DeLong tests indicated these leading models formed a high-performing cluster without significant differences in ROC AUC [1].
Key Predictors in Ablation Risk Stratification Models
Explainability analysis through SHAP (SHapley Additive exPlanations) values identified age, prior heart failure, malignancy, and end-stage renal disease as the most influential predictors for long-term outcomes after PVC ablation [1]. Similarly, the systematic review by [35] identified age, systolic blood pressure, and Killip class as top-ranked predictors of mortality in both ML and conventional risk scores. These findings highlight that the most robust predictors across models primarily comprise nonmodifiable clinical characteristics, suggesting an important limitation in current modeling approaches that largely exclude psychosocial and behavioral variables [35].
Experimental Protocols for ML Model Validation in VT Ablation Research
Dataset Curation and Preprocessing Methodology
The development of robust ML models for VT ablation research requires meticulous dataset curation. The study protocol in [1] utilized a nationwide claims database (National Health Insurance Research Database) encompassing 4195 adults who underwent PVC ablation. To address class imbalance—a critical challenge in rare event prediction—the researchers implemented two sophisticated sampling techniques: Synthetic Minority Over-sampling Technique (SMOTE) and Random Over-Sampling Examples (ROSE) [1].
The model comparison framework evaluated five supervised algorithms: logistic regression, decision tree, random forest, XGBoost, and LightGBM [1]. Discrimination was assessed by stratified five-fold cross-validation using the area under the receiver operating characteristic curve (ROC AUC). Given that rare events can bias ROC analysis, the protocol additionally examined precision-recall (PR) curves for a more comprehensive performance assessment [1].
Validation Standards and Integration Workflows
To ensure clinical relevance and translational potential, ML models for VT ablation require rigorous validation frameworks. The TRIPOD+AI (Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis + AI) checklist provides essential guidance for reporting standards [35]. Additionally, the Prediction Model Risk of Bias Assessment Tool (PROBAST) and CHARMS (Checklist for Critical Appraisal and Data Extraction for Systematic Reviews of Prediction Modelling Studies) offer structured methodologies for quality appraisal [35].
Successful integration of validated models into clinical workflows follows a structured pathway from development to implementation, with continuous validation checkpoints to ensure real-world performance. This workflow encompasses data extraction, model application, clinical decision support, and outcomes tracking, creating a closed-loop system for model refinement and validation.
Diagram 1: ML Model Development and Clinical Integration Workflow. This workflow outlines the comprehensive process from data extraction through clinical implementation, highlighting critical validation checkpoints and the continuous learning cycle essential for maintaining model performance in real-world settings.
Table 3: Essential Resources for VT Ablation Prediction Research
| Resource Category | Specific Tool/Solution | Research Application Function |
|---|---|---|
| Data Standards | FHIR (Fast Healthcare Interoperability Resources) APIs [36] | Enables structured data formatting for seamless exchange of lab results, prescriptions, and clinical notes across systems |
| Class Imbalance Handling | SMOTE (Synthetic Minority Over-sampling Technique) [1] | Generates synthetic examples of minority classes to address bias in rare event prediction |
| Class Imbalance Handling | ROSE (Random Over-Sampling Examples) [1] | Creates artificial cases based on the original data distribution to balance dataset classes |
| Model Explainability | SHAP (SHapley Additive exPlanations) [1] | Quantifies feature contributions and directionality at cohort and patient levels for model transparency |
| Performance Validation | Stratified k-Fold Cross-Validation [1] | Maintains class distribution across folds for robust performance estimation on imbalanced datasets |
| Performance Metrics | Precision-Recall (PR) Curves [1] | Provides complementary assessment to ROC AUC for models predicting rare events |
| EHR Integration Framework | Role-Based Access Controls [36] | Ensures appropriate data visibility across research team roles while maintaining security compliance |
| 3D Mapping Integration | EnSite Precision Mapping System [37] | Provides electroanatomical mapping data for procedure planning and outcome correlation |
Implementation Challenges and Interoperability Considerations
Technical and Adoption Barriers
Despite promising performance metrics, implementing ML-enhanced dashboards faces significant challenges. Vendor lock-in and closed ecosystems present substantial barriers, with 68% of private clinics using legacy EHRs reporting costs exceeding £20,000 annually for third-party integration tools [36]. Data silos and inconsistent formats further complicate implementation, with one rheumatology clinic reporting 15 hours weekly spent manually reconciling mismatched lab results and EHR entries [36].
Additionally, model opacity reduces clinician trust and hinders adoption, as many complex algorithms exhibit black-box behavior that limits interpretability [1]. Transportability and stability are challenged by data heterogeneity, label noise, and tuning sensitivity, which can induce overfitting despite strong retrospective metrics [1]. Privacy and governance constraints further limit data sharing, and even federated approaches show inconsistent cross-institutional performance [1].
Interoperability Solutions for Research Environments
Effective interoperability solutions form the foundation for successful ML model integration. Cloud-based EHR platforms with native FHIR support reduce patient onboarding delays by 35% and significantly decrease lab sync errors [36]. The RESTful API architecture of FHIR standards enables real-time data exchange between EHRs, research databases, and visualization tools, creating a seamless pipeline for model input and output [36].
Modern interoperability solutions also incorporate granular access controls that allow researchers to access specific data elements while maintaining compliance with GDPR, HIPAA, and institutional review board requirements [36]. These technical capabilities, combined with phased implementation rollouts that start with core functionality before adding advanced analytics, reduce adoption barriers and support longitudinal research initiatives across multiple institutions [36].
Integration of machine learning models into EHR dashboards for VT ablation procedural support represents a promising frontier in personalized cardiology. Current evidence demonstrates that ML-based models consistently outperform conventional risk scores in discrimination metrics, with tree-based algorithms and gradient boosting methods showing particular promise for long-term outcome prediction. The translation of these statistical advantages into clinical value depends on addressing key implementation challenges, including model explainability, interoperability barriers, and workflow integration. Future research should focus on prospective validation of ML-enhanced dashboards in real-world VT ablation settings, incorporation of modifiable psychosocial and behavioral predictors, and development of standardized implementation frameworks that maintain model performance across diverse healthcare environments.
Troubleshooting and Optimization: Overcoming Imbalance, Bias, and the Black Box
In the field of ventricular tachycardia (VT) ablation research, a significant challenge in developing robust machine learning (ML) models is the frequent occurrence of class imbalance. This happens when the number of patients who experience an outcome (e.g., VT recurrence or mortality) is vastly outnumbered by those who do not. Models trained on such imbalanced data can become biased, showing high accuracy for the majority class while failing to identify the critical minority class events.
To address this, techniques like the Synthetic Minority Over-sampling Technique (SMOTE) and Random Over-Sampling Examples (ROSE) are essential. This guide objectively compares their performance and methodologies, providing researchers with the data needed to select the appropriate technique for validating predictive models in VT ablation surgery research.
â—–â—— Technique Comparison: SMOTE vs. ROSE
The following table summarizes the core characteristics, performance data, and practical applications of SMOTE and ROSE, drawing from recent clinical ML studies.
| Feature | SMOTE (Synthetic Minority Over-sampling Technique) | ROSE (Random Over-Sampling Examples) |
|---|---|---|
| Core Principle | Generates synthetic examples for the minority class by interpolating between existing minority instances [38]. | Creates a new, artificially balanced dataset by randomly sampling with replacement from the original data, focusing on the feature space around minority class examples [1]. |
| Key Advantage | Increases diversity of the minority class without simple duplication [38]. | Effectively handles the bias introduced by rare events and is particularly suited for medical prognostication tasks [1]. |
| Performance in VT Research Context | Proven effective in general ECG analysis; used in deep learning pipelines for arrhythmia detection, achieving high accuracy (e.g., 99.74% on MITDB with CNN) [38]. | Demonstrated superior performance in predicting long-term outcomes after cardiac ablation. For predicting 3-year mortality, logistic regression with ROSE achieved an ROC AUC of 0.886, and for 3-year heart failure, LightGBM with ROSE achieved an ROC AUC of 0.822 [1]. |
| Considerations | May introduce synthetic data that does not fully reflect real-world physiological variations, potentially leading to overfitting if not carefully validated [38]. | As a non-parametric bootstrapping technique, it may be less complex than SMOTE and highly effective for clinical tabular data [1]. |
| Ideal Use Case | High-dimensional data and complex models like deep neural networks for signal processing (e.g., raw ECG classification) [38] [39]. | Predictive modeling of clinical outcomes (e.g., mortality, heart failure) using electronic health record data and tree-based models like LightGBM [1]. |
â—“ Experimental Protocols for Validation
To ensure the reliable validation of ML models using these techniques, a rigorous experimental protocol is required. The following workflow, derived from a benchmark study on predicting long-term outcomes after ablation, outlines the key steps [1].
Detailed Methodological Breakdown
Dataset and Preprocessing: The study utilized a nationwide cohort of 4,195 adults who underwent catheter ablation for premature ventricular contractions (PVCs). Baseline demographic and clinical data, including comorbidities and medications, were extracted [1]. Features were likely normalized, and the dataset was split for cross-validation.
Handling Class Imbalance: The imbalanced dataset was addressed by applying both SMOTE and ROSE within each fold of the cross-validation process. This critical step prevents data leakage and ensures that the synthetic data generated during training does not influence the test set, leading to a more reliable performance estimate [1].
Model Benchmarking: Five supervised learning algorithms were trained and compared to establish a robust benchmark:
- Logistic Regression (as an interpretable baseline)
- Decision Tree
- Random Forest
- XGBoost
- LightGBM This approach tests whether modern, complex models offer a significant advantage over traditional, interpretable ones when combined with advanced resampling techniques [1].
Validation and Evaluation:
- Stratified 5-Fold Cross-Validation: The entire process was evaluated using stratified cross-validation, which preserves the percentage of samples for each class in every fold, providing a more accurate performance measure on imbalanced data [1].
- Performance Metrics: Discrimination was primarily assessed using the Area Under the Receiver Operating Characteristic Curve (ROC AUC). Because ROC AUC can be overly optimistic with imbalanced data, the Area Under the Precision-Recall Curve (PR AUC) was also examined, as it gives a more informative view of the model's performance on the minority class [1].
- Model Explainability: To foster clinical trust and interpretability, SHAP (SHapley Additive exPlanations) values were used to quantify the contribution and directionality of each feature in the model's predictions [1].
â—‘ The Scientist's Toolkit: Research Reagent Solutions
The table below details key computational and data resources essential for implementing the described experimental protocols.
| Tool/Resource | Function in Research |
|---|---|
SMOTE/ROSE R Packages (smotefamily, ROSE) |
Provides open-source implementations of the over-sampling algorithms for direct use within the R programming environment [1]. |
| Scikit-learn (Python) | Offers a comprehensive suite of ML models (logistic regression, decision trees) and utilities for data preprocessing, cross-validation, and evaluation [1]. |
| XGBoost & LightGBM | High-performance, gradient-boosting frameworks that are particularly effective for structured/tabular data and often achieve state-of-the-art results in classification tasks [1]. |
| SHAP (SHapley Additive exPlanations) | A unified game-theoretic framework for explaining the output of any machine learning model, crucial for clinical interpretability [1] [38]. |
| National Health Insurance Research Database (NHIRD) | An example of a large-scale, real-world data source (claims database) that can be used to develop and validate prognostic models in cardiology [1]. |
| TSTU | TSTU, MF:C9H16BF4N3O3, MW:301.05 g/mol |
| MAZ51 | MAZ51, MF:C21H18N2O, MW:314.4 g/mol |
For researchers validating machine learning models in ventricular tachycardia ablation, the choice between SMOTE and ROSE is context-dependent. The experimental data indicates that ROSE may be particularly effective for predicting long-term clinical outcomes like mortality and heart failure using electronic health record data, especially when combined with powerful tree-based models like LightGBM [1].
However, for tasks involving high-dimensional signal data, such as raw ECG analysis for arrhythmia detection, SMOTE remains a strong and validated choice [38] [39]. Ultimately, employing a rigorous benchmarking protocol that tests both techniques against a transparent logistic regression baseline, as outlined in this guide, is the most reliable path to developing robust, clinically interpretable, and trustworthy predictive models.
Preventing Data Leakage and Ensuring Generalizability
In the field of ventricular tachycardia (VT) ablation research, machine learning (ML) models offer promising potential for predicting arrhythmia recurrence and identifying arrhythmogenic sites. However, their transition from experimental tools to clinically reliable instruments hinges on addressing two fundamental methodological challenges: preventing data leakage and ensuring generalizability. Data leakage occurs when information from outside the training dataset inadvertently influences the model, creating optimistically biased performance estimates that fail to predict real-world performance. Generalizability refers to a model's ability to maintain its predictive accuracy when applied to new, unseen datasets from different populations or institutions. The current literature reveals that while ML and deep learning models can achieve high performance in predicting malignant ventricular arrhythmias, widespread methodological limitations hinder their clinical adoption [40].
This comparison guide objectively evaluates contemporary experimental protocols and validation methodologies used in ML-driven VT ablation research, providing researchers with a structured framework for developing robust, clinically translatable models.
Core Concepts and Methodological Framework
Defining the Validation Spectrum
The validation of ML models in medical research exists on a spectrum, with each level providing increasingly strong evidence of real-world applicability:
- Internal Validation: The process of testing an AI model on data originating from the same source as the data used for training. This represents an initial step to ensure the model can generalize within a single dataset but provides limited evidence for broader applicability [41].
- External Validation: The testing of an AI model on data originating from different sources than those used in its training, ensuring the model's robustness and reliability across varied populations and clinical settings. This represents a critical step for wider clinical deployment [41].
- Generalizability: The ultimate goal of model development, reflecting consistent performance across diverse patient populations, healthcare institutions, and clinical practice patterns.
Data Leakage Pathways in VT Ablation Research
Data leakage can occur through multiple pathways in VT ablation studies, each requiring specific methodological safeguards:
Table: Common Data Leakage Pathways and Prevention Strategies
| Leakage Pathway | Description | Prevention Strategy |
|---|---|---|
| Temporal Leakage | Using future data to predict past outcomes | Strict chronological split of training and testing datasets |
| Patient Duplication | Multiple samples from same patient in both training and test sets | Patient-level splitting with all samples from individual patients confined to single partitions |
| Preprocessing Leakage | Applying normalization or feature selection before data splitting | Perform all preprocessing steps separately on training and testing partitions |
| Feature Leakage | Including variables in training that would not be available at prediction time | Careful temporal alignment of predictor variables with clinical decision points |
Comparative Analysis of Validation Methodologies
Performance Metrics for Model Evaluation
Rigorous validation requires multiple complementary metrics to fully capture model performance across different clinical contexts:
Table: Essential Performance Metrics for VT Ablation ML Models
| Metric | Definition | Clinical Interpretation | Strength | Limitation |
|---|---|---|---|---|
| Area Under ROC (AUROC) | Measures model's ability to distinguish between recurrence and non-recurrence | Probability that model ranks random positive higher than random negative | Robust to class imbalance | May overestimate performance in imbalanced datasets |
| Area Under PRC (AUPRC) | Trade-off between precision and recall | Better metric for imbalanced datasets where positive cases are rare | More informative than AUROC for skewed classes | Less intuitive clinical interpretation |
| F1 Score | Harmonic mean of precision and recall | Balances false positives and false negatives | Useful when both precision and recall are important | Doesn't capture true negative rate |
| Sensitivity | Proportion of actual positives correctly identified | Ability to correctly identify patients who will have VT recurrence | Critical for safety-focused applications | Doesn't account for false positives |
| Specificity | Proportion of actual negatives correctly identified | Ability to correctly identify patients who will not have recurrence | Important for avoiding unnecessary treatments | Doesn't account for false negatives |
Experimental Protocols for Robust Validation
Cross-Validation Techniques
Different cross-validation approaches offer varying levels of protection against overoptimistic performance estimates:
- K-Fold Cross-Validation: The dataset is randomly partitioned into k equal-sized folds, with each fold used once as validation while the remaining k-1 folds form the training set. This approach provides efficient data usage but carries risk of data leakage if patient duplicates exist across folds [42].
- Stratified K-Fold Cross-Validation: Preserves the percentage of samples for each class in every fold, maintaining consistent outcome distribution across partitions. This is particularly important for VT recurrence prediction where recurrence rates are typically 20-40% [22].
- Leave-One-Subject-Out Validation (LOSO): Each patient's data is held out as the test set once, with the model trained on all other patients. This approach guarantees complete patient-level separation but is computationally intensive, especially with large datasets [9].
Hold-Out Validation Strategies
For larger datasets, hold-out validation provides a more straightforward assessment of model performance:
- Single Hold-Out: Random split of data into training (typically 70-80%) and testing (20-30%) sets, with stratification by outcome to maintain similar recurrence rates in both partitions [22].
- Temporal Hold-Out: Training on earlier temporal cohorts and testing on later ones, which better simulates real-world deployment and accounts for potential temporal shifts in clinical practice [42].
Comparative Performance of ML Models in VT Ablation
Model Architectures and Their Applications
Different ML architectures offer distinct advantages for various aspects of VT ablation research:
Table: Machine Learning Model Performance in VT Ablation Applications
| Model Type | Reported Performance | Application Context | Strengths | Limitations |
|---|---|---|---|---|
| Random Forest | AUC 0.73 for 1-month VT recurrence [42] | VT recurrence prediction | Handles non-linear relationships, provides feature importance | May overfit with noisy data |
| LightGBM | AUC 0.827 for MVA prediction [21] | Malignant ventricular arrhythmia prediction | Computational efficiency, works well with large feature sets | Requires careful hyperparameter tuning |
| XGBoost | AUC 0.792 for composite endpoint [21] | Prediction of post-MI ventricular arrhythmias | Regularization prevents overfitting, handles missing data | Complex implementation, longer training times |
| CNN-based DL | AUROC 0.856-0.876 for VA/SCD prediction [40] | Electrophysiological signal analysis | Automatic feature extraction from raw signals | "Black box" nature, requires large datasets |
| Ensemble Tree | Accuracy >93% (cross-val), 84% (LOSO) for arrhythmogenic site detection [9] | Identification of ablation targets | Combines multiple weak learners for robust performance | Computationally intensive, complex interpretation |
Real-World Performance in External Validation
The most critical test for any ML model is its performance on external validation datasets:
- Performance Degradation: Models typically show 10-30% reduction in performance metrics when moving from internal to external validation. For example, one study reported an AUROC drop from 0.792 in internal validation to 0.726 in external validation for predicting post-MI ventricular arrhythmias [21].
- Dataset Shift Impact: Models developed on public datasets often show higher pooled performance (AUROC 0.919) compared to those using targeted clinical data acquisition, but they carry higher risk of bias due to reuse and overlap of small ad-hoc datasets [40].
- Institutional Generalizability: A systematic review found that only 39% of ML models in cardiac ablation studies underwent external validation, with most models (61%) showing high risk of bias due to validation exclusively on internal datasets [43].
Experimental Protocols for Robust Validation
Data Partitioning and Preprocessing Workflow
Proper experimental design begins with meticulous data partitioning to prevent data leakage:
Diagram 1: Data partitioning workflow to prevent leakage
Feature Selection and Engineering Protocols
The selection of predictive features represents a critical methodological decision point:
- Clinical Feature Selection: Studies predicting VT recurrence after ablation have identified optimal feature sets including hemodynamic instability, incessant VT, ICD shock, left ventricular ejection fraction, TAPSE, and non-inducibility of clinical VT [42].
- Electrophysiological Signal Features: For arrhythmogenic site detection, multi-domain features (time, frequency, time-scale, and spatial domains) have demonstrated high discriminatory power, with ensemble tree classifiers achieving >93% accuracy in cross-validation and 84% in leave-one-subject-out validation [9].
- Feature Standardization: Prior to LASSO analysis or similar feature selection techniques, continuous variables should be standardized using Z-score transformation to prevent bias from variables with different scales [22].
Addressing Class Imbalance
VT recurrence datasets typically exhibit significant class imbalance (recurrence rates of 18-35%), requiring specialized handling techniques [42]:
- Synthetic Minority Oversampling (SMOTE): Generates synthetic examples for the minority class to create a balanced training set, preventing model bias toward the majority class [22].
- Algorithmic Approaches: Utilization of focal loss or class-weighted loss functions that increase the cost of misclassifying minority class examples during model training [44].
- Stratified Evaluation: Maintaining the original class distribution in the test set while using balanced training, providing an unbiased benchmark for evaluating real-world predictive performance [22].
Research Reagent Solutions for ML in VT Ablation
The successful implementation of ML models for VT ablation research requires both computational and clinical resources:
Table: Essential Research Reagents and Computational Tools
| Resource Category | Specific Tools/Techniques | Function/Purpose | Implementation Considerations |
|---|---|---|---|
| Electrophysiological Data | Bipolar electrograms from mapping systems (CARTO 3, EnSite) | Raw input for feature extraction | Standardize sampling rates (1kHz), band-pass filtering (16-500Hz) [9] |
| Clinical Variables | Echocardiographic parameters, medical history, medication use | Predictive features for recurrence models | Ensure temporal alignment (e.g., echo within 30 days pre-procedure) [42] |
| ML Algorithms | Random Forest, XGBoost, LightGBM, CNN | Model development for classification/regression | Select based on dataset size, feature types, and interpretability needs [42] [21] |
| Validation Frameworks | PROBAST, TRIPOD+AI, EHRA AI checklist | Methodological quality assessment | Address domains: participants, predictors, outcome, analysis [40] [41] |
| Interpretability Tools | SHAP (SHapley Additive exPlanations) | Model interpretation and feature importance | Quantify each feature's contribution to predictions [22] |
| Computational Infrastructure | Python/R with scikit-learn, TensorFlow, PyTorch | Model development and training | Ensure reproducibility through version control and containerization |
Validation Hierarchies and Generalizability Assessment
A comprehensive validation strategy requires multiple assessment levels to establish true generalizability:
Diagram 2: Validation hierarchy for assessing generalizability
The development of ML models for VT ablation research requires meticulous attention to validation methodologies to ensure clinical relevance. Preventing data leakage through rigorous experimental designs—including patient-level data splitting, temporal validation, and proper preprocessing protocols—forms the foundation for reliable performance estimates. Furthermore, establishing generalizability demands external validation across multiple institutions and diverse patient populations, with explicit documentation of performance degradation metrics.
The field is progressing toward standardized reporting frameworks, such as the EHRA AI checklist, which addresses critical aspects often underreported in current literature, including trial registration, participant details, data handling, and training performance [41]. By adopting these rigorous methodologies, researchers can develop ML models that not only achieve statistical significance but also demonstrate clinical utility in improving VT ablation outcomes.
Future directions should focus on prospective validation in real-world clinical settings, implementation of explainable AI techniques for clinician trust and adoption, and development of adaptive learning systems that maintain performance across temporal shifts in clinical practice.
The adoption of machine learning (ML) in clinical medicine, particularly in specialized fields like ventricular tachycardia (VT) ablation research, is often hampered by the "black-box" nature of complex models. Clinicians and researchers require not just high predictive accuracy but, more importantly, transparent and interpretable models to foster trust and facilitate clinical decision-making. Explainable AI (XAI) has thus emerged as a crucial subfield of ML, aiming to render AI models and their decision-making transparent and understandable [45]. This guide provides an objective comparison of SHapley Additive exPlanations (SHAP) against other interpretability methods, framed within the context of validating ML models for VT ablation surgery research.
SHAP provides a mathematically unified approach to interpreting model predictions based on cooperative game theory, specifically the Shapley value concept. It quantifies the contribution of each input feature to a model's individual prediction, ensuring consistency and local accuracy [46] [47]. For clinical researchers developing predictive models for VT etiology or ablation outcomes, SHAP offers a mechanism to move beyond mere performance metrics and understand which patient factors drive specific predictions, thereby aligning computational outputs with clinical knowledge.
Comparative Analysis of Interpretability Methods
SHAP vs. LIME: A Technical Comparison
For researchers selecting interpretability methods, understanding the technical distinctions between SHAP and Local Interpretable Model-agnostic Explanations (LIME) is crucial. The table below summarizes their core characteristics:
Table 1: Technical Comparison of SHAP and LIME
| Characteristic | SHAP (SHapley Additive exPlanations) | LIME (Local Interpretable Model-agnostic Explanations) |
|---|---|---|
| Theoretical Foundation | Cooperative game theory (Shapley values) [47] | Local surrogate models [48] |
| Explanation Scope | Local & Global (consistent across both) [48] | Primarily Local (instance-level) [48] |
| Output | Additive feature attribution values [46] | Feature importance from a local surrogate model [49] |
| Stability/Consistency | High (theoretically grounded) [48] | Can exhibit variability due to random sampling [48] |
| Computational Demand | Can be high for some model types | Generally lower [48] |
Performance Comparison in Clinical Contexts
Empirical evaluations, particularly in clinical settings, provide critical data for method selection. A 2025 study published in npj Digital Medicine directly compared the impact of different explanation methods on clinician decision-making [50]. The research measured effects on advice acceptance, trust, satisfaction, and system usability when clinicians were presented with AI recommendations accompanied by different explanations.
Table 2: Impact of Explanation Methods on Clinical Decision-Making [50]
| Explanation Type | Weight of Advice (WOA) | Trust in AI Score | Explanation Satisfaction | System Usability (SUS) |
|---|---|---|---|---|
| Results Only (RO) | 0.50 | 25.75 | 18.63 | 60.32 (Marginal) |
| Results with SHAP (RS) | 0.61 | 28.89 | 26.97 | 68.53 (Marginal) |
| Results with SHAP & Clinical Explanation (RSC) | 0.73 | 30.98 | 31.89 | 72.74 (Good) |
This study found that while SHAP plots alone improved metrics over providing only results, the highest levels of clinician acceptance, trust, and satisfaction were achieved when SHAP outputs were accompanied by a clinical explanation that translated the quantitative outputs into medical context [50].
Furthermore, a 2024 study on ML for VT etiological diagnosis demonstrated that the XGBoost model, when explained using SHAP, provided high performance (Precision: 88.4%, Recall: 88.5%, F1: 88.4%) and was highly favored by clinicians for decision-making support [45].
Experimental Protocols for Model Interpretation
Workflow for Interpretable ML Model Development
The following diagram illustrates a generalized experimental workflow for developing and interpreting a machine learning model in a clinical research context, such as VT ablation studies.
Protocol: VT Etiology Classification with SHAP
A specific protocol from a 2024 study on VT etiological diagnosis outlines a robust methodology [45]:
- Data Collection and Preprocessing: The study included 1305 VT patient records. Variables with >30% missing data were removed, while others were handled using K-Nearest Neighbours Imputation (KNN) to estimate missing values via weighted averages from known data points [45].
- Feature Selection: A multi-method approach was employed, using statistical tests, Gini importance from Random Forests, and Maximal Information Coefficient (MIC) to select features significantly associated with the target variable [45].
- Model Training and Explanation: Multiple ML models (Logistic Regression, Random Forest, XGBoost, LightGBM) were trained. The TreeExplainer from the SHAP library was then applied to the best-performing model (XGBoost) to calculate SHAP values, generating both local and global explanations [45] [47].
Protocol: Evaluating Clinical Utility of Explanations
The 2025 comparative study provides a protocol for assessing the real-world impact of explanations [50]:
- Study Design: A counterbalanced design where clinicians made decisions based on different explanation formats.
- Metrics: Quantitative measures included Weight of Advice (WOA) to quantify acceptance, standardized Trust and Explanation Satisfaction scales, and the System Usability Scale (SUS).
- Analysis: Statistical tests (Friedman test with Conover post-hoc analysis) and correlation analysis were used to determine significant differences and relationships between explanation type and outcome metrics.
Implementation Guide for SHAP in Clinical Research
The Researcher's Toolkit for SHAP Analysis
Table 3: Essential Research Reagents and Computational Tools
| Item/Tool | Function in SHAP Analysis | Example/Note |
|---|---|---|
| Python SHAP Library | Core library for computing SHAP values. | Install via pip install shap [47]. |
| TreeExplainer | High-speed exact algorithm for tree ensembles. | Use for XGBoost, LightGBM, scikit-learn trees [47]. |
| KernelExplainer | Model-agnostic explainer for any function. | Slower but generalizable; good for custom models [47]. |
| Medical Dataset | Domain-specific data for model training and validation. | e.g., VT patient data including medical history, vital signs, echocardiographic results, and lab tests [45]. |
| XGBoost Model | A high-performance gradient-boosting model. | Often a strong performer for structured clinical data [45]. |
| Ctop | CTOP|Research Grade Biochemical|KareBay Bio | CTOP is a selective opioid receptor antagonist for research use. This product is for Research Use Only and not intended for diagnostic or therapeutic procedures. |
Generating and Interpreting Key SHAP Visualizations
The following diagram illustrates the logical relationship between different SHAP visualization types and their primary uses in the research narrative.
Implementation Code Snippet:
The comparative analysis reveals that SHAP provides a mathematically robust framework for model interpretability, capable of delivering both local and global insights. However, its clinical utility is maximized when SHAP outputs are translated into clinician-friendly explanations that align with medical reasoning and domain knowledge [50]. For researchers in VT ablation and other specialized medical fields, the strategic integration of SHAP into the model validation pipeline—complemented by clinical expertise—offers a powerful path toward developing transparent, trustworthy, and clinically actionable AI systems.
Hyperparameter Tuning and Performance Optimization Strategies
The validation of machine learning models for ventricular tachycardia (VT) ablation surgery research represents a critical frontier in precision cardiology. These models aim to predict arrhythmia recurrence, optimize ablation strategies, and ultimately improve patient outcomes. The performance of these models is heavily dependent on the rigorous application of hyperparameter tuning and performance optimization strategies, which enable researchers to transform raw algorithmic potential into clinically reliable tools. This guide provides a comprehensive comparison of prevailing methodologies, supporting experimental data, and essential protocols for developing robust ML models in this specialized domain.
Comparative Performance of Machine Learning Models
Model Performance in Cardiovascular Prediction Tasks
Table 1: Performance Metrics of ML Models in Cardiovascular Applications
| Application Context | Best-Performing Model(s) | Key Performance Metrics | Reference |
|---|---|---|---|
| VT Prediction from Single-Lead ECG | VAE-SVM (Variational Autoencoder with Support Vector Machine) | F1 Score: 0.66, Recall: 0.77 | [51] |
| False VT Alarm Reduction in ICU | 1D CNN with Multi-Head Attention | ROC-AUC: >0.96 | [52] |
| AF Recurrence Post-Ablation | Light Gradient Boosting Machine (LightGBM) | AUC: 0.848, Accuracy: 0.721 | [22] |
| 3-Year Heart Failure Post-PVC Ablation | LightGBM with Random Over-Sampling Examples (ROSE) | ROC AUC: 0.822 | [1] |
| 3-Year Mortality Post-PVC Ablation | Logistic Regression with ROSE / LightGBM with ROSE | ROC AUC: 0.886 / 0.882 | [1] |
| Mitral Valve Repair Durability | Random Survival Forest | Concordance Index: 0.874 | [53] |
The performance data reveal that no single algorithm dominates all prediction tasks. Ensemble methods like LightGBM and Random Survival Forest excel in handling tabular clinical data for long-term outcome prediction [22] [53] [1]. In contrast, for signal processing tasks such as analyzing ECG waveforms, deep learning architectures (e.g., CNNs) and hybrid approaches (e.g., VAE-SVM) demonstrate superior performance [51] [52]. This highlights the importance of matching model architecture to data modality.
Hyperparameter Optimization Techniques Across Studies
Table 2: Hyperparameter Tuning and Class Imbalance Strategies
| Study / Application | Optimization / Validation Approach | Class Imbalance Handling | Key Hyperparameters Tuned |
|---|---|---|---|
| False VT Alarm Classification [52] | Train/Validation/Test Split (80/10/10); Benchmark Dataset | SMOTE; Class Weighting | Network Architecture, Attention Mechanisms |
| AF Recurrence Prediction [22] | Stratified 5-Fold Cross-Validation; Training/Testing (70/30) | SMOTE on Training Set Only | Algorithm-specific parameters for LightGBM, SVM, AdaBoost, GradientBoosting |
| Heart Failure/Mortality Prediction [1] | Stratified 5-Fold Cross-Validation | SMOTE; ROSE (Random Over-Sampling Examples) | Parameters for Logistic Regression, Decision Tree, Random Forest, XGBoost, LightGBM |
| VT Early Prediction [51] | Not Explicitly Stated | Not Explicitly Stated | LSTM architecture; CNN spectrogram parameters; VAE-SVM feature extraction |
A consistent theme across studies is the use of sophisticated resampling techniques to address class imbalance, a common challenge in clinical outcome prediction where events like VT recurrence or mortality are relatively rare. SMOTE was the most frequently employed technique [22] [1] [52]. For validation, stratified cross-validation and strict hold-out test sets were standard practice to ensure unbiased performance estimation [22] [1].
Experimental Protocols and Methodologies
Data Preprocessing and Feature Engineering Protocols
A critical step in model development involves standardizing and cleansing raw data. A common protocol for waveform data (e.g., ECG) includes:
- Data Loading: Using specialized libraries (e.g.,
wfdb) to load physiological waveform data from standard formats [52]. - Handling Missing Values: Applying imputation techniques, such as mean imputation, to address gaps in data caused by signal artifacts [52].
- Normalization: Scaling features to a consistent range, often [0, 1] using Min-Max scaling, to ensure model stability and convergence [52].
- Feature Extraction: For temporal signals, this involves generating both time-domain (e.g., mean, standard deviation, kurtosis) and frequency-domain features (e.g., spectral entropy, wavelet energy) to comprehensively represent the signal's characteristics [52].
For structured clinical data, protocols often include standardization (Z-score normalization) prior to applying feature selection algorithms like LASSO regression, which performs L1 regularization to shrink irrelevant feature coefficients to zero, enhancing model interpretability and managing multicollinearity [22].
Model Training and Validation Workflow
The following diagram illustrates a consolidated experimental workflow derived from the cited studies, common to many ML projects in VT ablation research.
Experimental Workflow for ML in VT Ablation
Model Interpretation and Explainability Protocols
Beyond predictive performance, clinical applicability demands model interpretability. The SHapley Additive exPlanations (SHAP) methodology is a widely adopted protocol for quantifying the contribution of each input feature to a model's predictions [22] [1]. For deep learning models applied to ECG, techniques like latent space traversal and correlation analysis are employed to interpret model behavior and identify physiologically meaningful features associated with VT onset [51].
Table 3: Key Computational Tools and Datasets for VT Ablation Research
| Tool / Resource Name | Type | Primary Function in Research | Example Use Case |
|---|---|---|---|
| VTaC Dataset [52] | Data | Benchmark dataset for developing/evaluating VT alarm algorithms. | Provides over 5,000 annotated VT alarm events with ECG, PPG, and ABP waveforms for training models to reduce false alarms in ICUs. |
| SHAP (SHapley Additive exPlanations) [22] [1] | Software Library | Explains output of any ML model. | Identifies key clinical predictors (e.g., BNP, NLR) for AF recurrence post-ablation and quantifies their impact on the model's output. |
| SMOTE / ROSE [22] [1] [52] | Algorithm | Synthetic minority over-sampling to handle class imbalance. | Balances the training dataset for predicting rare events like 3-year heart failure after PVC ablation, improving model sensitivity. |
| LightGBM / XGBoost [22] [1] | Algorithm | Gradient boosting frameworks for tabular data. | Achieves state-of-the-art performance for predicting long-term outcomes (heart failure, mortality) using electronic health record data. |
| 1D CNN with Multi-Head Attention [52] | Model Architecture | Deep learning model for sequential data analysis. | Processes raw waveform data from ICU monitors to accurately classify true and false VT alarms, capturing both local patterns and long-range dependencies. |
| Stratified K-Fold Cross-Validation [22] [1] | Validation Protocol | Robust model validation technique. | Ensures reliable performance estimation for an AF recurrence prediction model by maintaining class distribution across all training/validation folds. |
The strategic implementation of hyperparameter tuning and performance optimization is paramount for advancing machine learning applications in ventricular tachycardia ablation research. The experimental data and protocols outlined in this guide demonstrate that success hinges on a multifaceted approach: selecting models aligned with data modalities, rigorously addressing class imbalance, employing robust validation schemes, and prioritizing model interpretability. Future progress will depend on the development of larger, multi-center datasets and the prospective validation of these optimized models within clinical workflows to fully realize their potential in personalizing patient care.
Validation and Comparative Analysis: Rigorous Evaluation and Benchmarking for Clinical Trust
In the development of machine learning models for high-stakes clinical applications, such as predicting outcomes for ventricular tachycardia (VT) ablation surgery, robust validation is paramount to ensure model reliability and patient safety. Validation frameworks protect against overfitting, where a model memorizes training data noise rather than learning generalizable patterns, ultimately ensuring that predictive performance translates to unseen clinical data [54] [55]. Without proper validation, models may fail catastrophically in real-world deployment, with serious implications for patient care.
This guide provides an objective comparison of two fundamental validation approaches: the hold-out method and cross-validation. We frame this comparison within the context of clinical prediction models, drawing on examples from healthcare research, including a specific cross-validation study from the RAVENTA trial on stereotactic arrhythmia radioablation (STAR) [56]. We summarize quantitative performance data, detail experimental protocols, and provide visual workflows to equip researchers with the knowledge to select and implement the most appropriate validation framework for their clinical ML projects.
Comparative Analysis of Hold-Out and Cross-Validation
The hold-out method and k-fold cross-validation represent two different philosophies for estimating a model's performance on unseen data. The core difference lies in the number of times the model is trained and evaluated on different data partitions.
The hold-out method is the most straightforward approach. It involves a single, random partition of the dataset into two subsets: a larger portion for training the model (e.g., 70-80%) and a smaller, held-out portion for testing its performance (e.g., 20-30%) [57] [58]. This method provides a quick, computationally efficient performance estimate and is suitable for very large datasets or initial model prototyping [57] [59].
In contrast, k-fold cross-validation provides a more robust performance estimate by repeatedly training and testing the model on different data subsets. The dataset is first split into k equal-sized folds (a common choice is k=5 or k=10 [59]). The model is then trained k times, each time using k-1 folds for training and the remaining single fold for validation. The final performance metric is the average of the scores from all k iterations [57] [54]. This process ensures that every data point is used exactly once for validation, leading to a more reliable estimate of generalization error, which is particularly valuable with smaller datasets [60] [55].
The table below summarizes the key characteristics and trade-offs between these two methods.
Table 1: A direct comparison of the Hold-Out and K-Fold Cross-Validation methods.
| Feature | Hold-Out Method | K-Fold Cross-Validation |
|---|---|---|
| Data Split | Single split into training and test sets [59]. | Dataset divided into k folds; multiple train-test rotations [57] [59]. |
| Training & Testing | Model is trained and tested only once [59]. | Model is trained and tested k times; each fold serves as the test set once [57]. |
| Bias & Variance | Higher risk of bias if the single split is not representative of the overall data distribution; results can vary significantly with different splits [57] [61]. | Generally provides a lower bias estimate; variance depends on the value of k, but is typically more stable than a single hold-out [59] [55]. |
| Computational Cost | Faster, as it involves only one training and testing cycle [57] [61]. | Slower, especially for large datasets and high values of k, as the model is trained k times [57] [59]. |
| Best Use Cases | Very large datasets, time-constrained environments, or initial model building [57] [58]. | Small to medium-sized datasets where an accurate and reliable performance estimate is critical [59] [60]. |
| Data Efficiency | Only uses a portion (e.g., 70-80%) of the data for training, which may not leverage all available information [61]. | Uses all data for both training and testing, making it more data-efficient [59]. |
A simulation study comparing internal validation methods highlighted that while cross-validation and hold-out produced comparable discrimination (AUC) in a specific clinical prediction task, the hold-out method resulted in a model with higher uncertainty [60]. This finding underscores that a single train-test split can yield a performance estimate that is highly dependent on a "lucky" or "unlucky" data partition.
Experimental Protocols and Performance Data
Detailed Methodologies
The choice between hold-out and cross-validation is often dictated by the dataset's size and the modeling goal (e.g., simple evaluation vs. hyperparameter tuning).
Hold-Out for Model Evaluation and Selection: For basic model evaluation, the dataset is split once. A more advanced protocol uses three splits for hyperparameter tuning [58] [55]:
- Split: The dataset is divided into a training set (e.g., 70%), a validation set (e.g., 20%), and a test set (e.g., 10%).
- Train: Multiple models with different hyperparameters are trained on the training set.
- Tune: The models are evaluated on the validation set, and the best-performing model is selected.
- Final Test: The chosen model's generalization is finally assessed on the held-out test set, which has not been used in any previous step.
K-Fold Cross-Validation Protocol:
- Choose k: Select a value for k (commonly 5 or 10) [59].
- Shuffle and Split: Randomly shuffle the dataset and partition it into k folds of approximately equal size.
- Iterate: For each of the k iterations:
- Designate one fold as the validation fold.
- Use the remaining k-1 folds as the training fold.
- Train the model on the training fold.
- Validate the model on the validation fold and record the performance score.
- Average: Calculate the final model performance by averaging the scores from all k iterations [54] [59].
Stratified K-Fold for Imbalanced Data: In clinical settings, outcomes like mortality or disease progression are often rare. Standard random splitting can create folds with unrepresentative class distributions. Stratified k-fold cross-validation ensures each fold retains the same proportion of class labels (e.g., cases vs. controls) as the complete dataset, leading to more reliable performance estimates [59] [62].
Nested Cross-Validation: For both model selection and evaluation without bias, nested (or double) cross-validation is the gold standard [62]. It consists of two loops:
- Inner Loop: A k-fold cross-validation is performed on the training set from the outer loop to tune the model's hyperparameters.
- Outer Loop: A separate k-fold cross-validation is used to evaluate the performance of the model with the optimally tuned hyperparameters. While computationally expensive, this approach provides an almost unbiased estimate of the true model performance [62].
Quantitative Performance Comparison
The following table synthesizes performance data from various studies, including a clinical simulation study [60] and a multi-center cross-validation in VT research [56], to illustrate the practical differences between these validation methods.
Table 2: Experimental performance data comparing validation frameworks in different scenarios.
| Experiment Context | Validation Method | Reported Performance Metric | Notes / Key Finding |
|---|---|---|---|
| Simulated Clinical Data (n=500) [60] | 5-Fold Repeated CV | AUC: 0.71 ± 0.06 | More precise and stable performance estimate. |
| Simulated Clinical Data (n=500) [60] | Hold-Out (100 patients) | AUC: 0.70 ± 0.07 | Comparable AUC but with higher uncertainty. |
| Simulated Clinical Data (n=500) [60] | Bootstrapping | AUC: 0.67 ± 0.02 | Lower AUC estimate in this simulation. |
| RAVENTA Trial (STAR Targets) [56] | Cross-Validation (2 methods) | Dice Coefficient: 0.84 ± 0.04 | Used to validate two software solutions for target transfer, showing high agreement. |
| Theoretical / Best Practices [57] [61] | Hold-Out with different random seeds | Varying R² Score / MSE | Demonstrates high variance; model performance is sensitive to the specific data split. |
Visualization of Validation Workflows
To clarify the logical flow of data in each validation framework, the following diagrams were created using the DOT language, adhering to the specified color and contrast guidelines.
Hold-Out Validation Methodology
The diagram below illustrates the single data split characteristic of the hold-out method. The clear separation between the training and testing phases emphasizes that the model's performance is evaluated only once on unseen data.
K-Fold Cross-Validation Methodology
This diagram visualizes the iterative process of k-fold cross-validation (with k=5). The rotation of the validation fold across all data subsets ensures that every sample contributes to both training and validation, leading to a more robust performance estimate.
The Scientist's Toolkit: Key Research Reagents and Materials
Implementing these validation frameworks requires both computational tools and methodological rigor. The following table details essential "research reagents" for conducting robust validation in machine learning for clinical research.
Table 3: Essential tools and materials for implementing validation frameworks in clinical ML research.
| Item / Solution | Function / Explanation | Relevance to Clinical Validation |
|---|---|---|
| Stratified Splitting | A data splitting technique that preserves the percentage of samples for each class (e.g., disease vs. healthy) in every fold [59] [62]. | Critical for imbalanced clinical datasets (e.g., rare diseases) to ensure all folds are representative and performance estimates are valid. |
| Subject-Wise Splitting | A splitting method where all data from a single patient (or subject) are kept in the same fold, preventing data leakage [62]. | Essential when multiple samples/records come from the same patient. Prevents over-optimism by ensuring the model is tested on truly new patients. |
| Scikit-learn Library (Python) | A comprehensive machine learning library providing tools for train_test_split, cross_val_score, KFold, and StratifiedKFold [54] [59]. |
The standard toolkit for implementing both hold-out and cross-validation workflows with minimal code, facilitating reproducible research. |
| Nested Cross-Validation | A double loop of cross-validation for hyperparameter tuning and model evaluation without bias [62]. | Provides the most reliable estimate of how a model will perform on external clinical datasets, crucial for assessing true generalizability. |
| Pipeline Object (e.g., Scikit-learn) | A tool to chain together data preprocessing (e.g., standardization) and model training steps [54]. | Prevents data leakage by ensuring preprocessing parameters (like mean and SD) are learned from the training fold and applied to the validation fold within each CV iteration. |
| Dice Similarity Coefficient | A spatial overlap metric ranging from 0 (no overlap) to 1 (perfect overlap) [56]. | Used as a performance metric in clinical imaging and target definition studies (e.g., the RAVENTA trial) to validate the consistency of segmentations or target volumes. |
In the high-stakes field of ventricular tachycardia (VT) ablation surgery research, the selection of appropriate machine learning (ML) performance metrics is not merely a technical consideration but a fundamental aspect of model validation that directly impacts clinical decision-making. ML models are increasingly being developed to predict optimal ablation approaches, identify arrhythmia origins, and stratify patient risk, creating an urgent need for rigorous evaluation frameworks tailored to this specialized domain. The validation of these models requires a nuanced understanding of various performance metrics—including AUC-ROC, AUC-PR, F1-Score, and confusion matrices—each providing complementary insights into model behavior, particularly when dealing with imbalanced datasets common in medical applications.
This guide provides an objective comparison of these key evaluation metrics within the context of VT ablation research, supported by experimental data from recent studies. By examining the strengths, limitations, and appropriate use cases for each metric, we aim to equip researchers and clinicians with the analytical tools necessary to critically evaluate ML models proposed for enhancing VT ablation procedures.
Key Performance Metrics Explained
Confusion Matrix: The Foundation
The confusion matrix provides the foundational components from which many other metrics are derived by tabulating actual versus predicted classifications. It comprises four key elements [63] [64]:
- True Positives (TP): Cases correctly identified as positive (e.g., correctly predicting need for epicardial access)
- True Negatives (TN): Cases correctly identified as negative (e.g., correctly predicting endocardial-only approach suffices)
- False Positives (FP): Cases incorrectly identified as positive (Type I error)
- False Negatives (FN): Cases incorrectly identified as negative (Type II error)
In VT ablation research, the confusion matrix offers immediate clinical interpretability by quantifying specific error types. For instance, in predicting epicardial VT ablation necessity, false negatives might represent patients in whom epicardial access was incorrectly deemed unnecessary, potentially leading to procedural failure [65].
AUC-ROC (Area Under the Receiver Operating Characteristic Curve)
The Receiver Operating Characteristic (ROC) curve visualizes the trade-off between sensitivity (True Positive Rate) and specificity (1 - False Positive Rate) across all possible classification thresholds [63] [66]. The Area Under the ROC Curve (AUC-ROC) provides a single measure of overall model performance, with 1.0 representing perfect classification and 0.5 representing random guessing [64].
- True Positive Rate (TPR) = Recall = TP / (TP + FN)
- False Positive Rate (FPR) = FP / (FP + TN)
AUC-ROC is particularly valuable when both positive and negative classes are equally important. However, in imbalanced datasets common in medical applications (where one class is rare), it can provide overly optimistic performance estimates because the large number of true negatives dominates the FPR calculation [66].
AUC-PR (Area Under the Precision-Recall Curve)
The Precision-Recall (PR) curve plots precision against recall at various classification thresholds, with AUC-PR representing the area under this curve [66]. Unlike ROC, PR curves focus exclusively on the model's performance regarding the positive class, making them particularly valuable for imbalanced datasets where the positive class (e.g., patients requiring epicardial access) is the primary interest [66].
- Precision = TP / (TP + FP)
- Recall = TP / (TP + FN)
AUC-PR is more informative than AUC-ROC when the positive class is rare or when false positives carry significant clinical consequences [66].
F1-Score
The F1-score represents the harmonic mean of precision and recall, providing a single metric that balances both concerns [63] [64]. Unlike accuracy, which can be misleading in imbalanced datasets, the F1-score gives equal weight to both precision and recall, making it particularly useful when seeking a balance between identifying true positives while minimizing false positives and false negatives [66].
- F1-Score = 2 × (Precision × Recall) / (Precision + Recall)
The F1-score is especially valuable in clinical contexts where both false positives and false negatives carry significant consequences, such as predicting VT ablation outcomes where unnecessary procedures (false positives) and missed necessary interventions (false negatives) both present substantial risks [65] [66].
Comparative Analysis in VT Ablation Context
Metric Performance on Imbalanced Clinical Data
VT ablation datasets typically exhibit significant class imbalance, with only 17-38% of patients requiring epicardial approach [65]. This imbalance profoundly affects metric performance and interpretation:
Table 1: Metric Behavior in Class-Imbalanced VT Ablation Datasets
| Metric | Performance with Class Imbalance | Clinical Interpretation in VT Context |
|---|---|---|
| Accuracy | Often misleadingly high; a model predicting only endocardial approach would achieve ~63-83% accuracy in typical VT cohorts [65] | Overestimates clinical utility; insufficient for ablation decision support |
| AUC-ROC | Generally robust but may be optimistic due to high TN count; less sensitive to false positives in rare class [66] | Useful for overall discrimination but may mask poor performance in identifying epicardial cases |
| AUC-PR | More informative than ROC for imbalanced data; directly reflects performance on positive class [66] | Better captures model's ability to identify patients truly needing epicardial access |
| F1-Score | Focuses on positive class; balances precision and recall [63] [64] | Clinically relevant balance between identifying epicardial cases (recall) and avoiding unnecessary procedures (precision) |
Experimental Comparison from Recent Studies
Recent research in VT ablation provides concrete examples of these metrics in practice:
Table 2: Performance Metrics from Recent VT Ablation and Arrhythmia Detection Studies
| Study & Model | Clinical Application | AUC-ROC | AUC-PR | F1-Score | Accuracy |
|---|---|---|---|---|---|
| EPI-VT-Score [65] | Predicting need for epicardial VT ablation | 0.990 (95% CI: 0.978-1.000) | Not reported | Not reported | 92.2% sensitivity, 100% specificity |
| Fusion-DMA-Net [67] | PPG-based arrhythmia classification | Not reported | Not reported | 99.04% | 99.05% |
| ML-enabled IVA Origin Prediction [68] | Predicting origins of idiopathic ventricular arrhythmia | Not reported | Not reported | 98.56% (Scheme 4) | 98.24% (Scheme 4) |
| SNN Arrhythmia Detection [69] | ECG-based arrhythmia classification | Exceeded 0.88 across classes | Not reported | Exceeded 0.88 across classes | 94.4% |
The EPI-VT-Score study exemplifies the exceptional discrimination possible with carefully selected features, achieving near-perfect AUC-ROC of 0.990 in predicting epicardial ablation necessity. This score incorporated four predictors: underlying cardiomyopathy, left ventricular ejection fraction, number of prior VT ablations, and VT-QRS interval [65]. Notably, the researchers reported sensitivity and specificity rather than F1-score, possibly because clinical consequences of false negatives (missing necessary epicardial access) and false positives (unnecessary epicardial access) differ significantly in this context.
Experimental Protocols in VT Ablation Research
EPI-VT-Score Development and Validation
The development of the EPI-VT-Score illustrates a comprehensive validation methodology for clinical prediction models [65]:
Study Population: Retrospective analysis of 138 patients (mean age 64.9±11.3 years, 89.9% male) who underwent VT ablation between 2018-2024, with 51 (37.0%) requiring epicardial approach.
Predictor Selection: Four clinically available parameters were identified as predictive:
- Underlying cardiomyopathy (ischemic cardiomyopathy=1 point, dilated cardiomyopathy=2 points, cardiac disease=3 points)
- Left ventricular ejection fraction (≤35%=1 point, 35-45%=2 points, ≥45%=3 points)
- Number of prior VT ablations (0=1 point, 1=2 points, ≥2=3 points)
- VT-QRS interval (≤180ms=1 point, 180-220ms=2 points, ≥220ms=3 points)
Validation Approach: The score (range: 4-12 points) was validated with a threshold ≥8 indicating epicardial necessity with 92.2% sensitivity and 100% specificity. Patients scoring <8 were effectively managed with endocardial-only ablation [65].
ML-Based Arrhythmia Origin Prediction
An alternative approach demonstrates the intensive data requirements for direct ML classification of arrhythmia origins [68]:
Dataset: 18,612 ECG recordings from 545 patients who underwent successful catheter ablation for idiopathic ventricular arrhythmias.
Classification Schemes: Four hierarchical schemes ranging from 3 general regions to 21 specific anatomical sites.
Methodology: 98 distinct ML models with hyperparameter optimization via grid search, with oversampling to address class imbalance.
Performance: Achieving 98.24% accuracy for predicting 21 possible sites of origin, demonstrating the potential of comprehensive ML approaches for complex ablation planning [68].
Research Reagent Solutions
Table 3: Essential Research Materials and Platforms for ML in VT Ablation Research
| Resource Category | Specific Examples | Function in Research |
|---|---|---|
| Electroanatomical Mapping Systems | Carto 3 (J&J MedTec), Ensite Precision/X (Abbott) | High-density 3D mapping of ventricular substrate and voltage abnormalities [65] |
| Mapping Catheters | PentaRay NAV, OctaRay NAV (J&J MedTec), HD-Grid (Abbott) | Multipolar mapping for detailed substrate characterization [65] |
| Computational Platforms | Intel Loihi, IBM TrueNorth | Neuromorphic computing for energy-efficient SNN implementation [69] |
| ECG/PPG Datasets | PhysioNet PTB Diagnostic ECG Database, MIT-BIH Arrhythmia Database, Chapman University ECG Database | Standardized, annotated datasets for model training and validation [69] [67] |
| ML Frameworks | Scikit-learn, LightGBM | Model development, hyperparameter optimization, and performance evaluation [63] [66] |
| Ablation Tools | Steerable sheaths (Carto Vizigo, Agilis), Irrigation systems | Epicardial and endocardial access and ablation delivery [65] |
Workflow Visualization
The selection of performance metrics for validating machine learning models in ventricular tachycardia ablation research requires careful consideration of clinical context and dataset characteristics. AUC-ROC provides excellent overall discrimination assessment but may be less informative for imbalanced datasets where the epicardial approach is necessary in a minority of cases. AUC-PR and F1-score offer valuable complementary perspectives by focusing on the positive class, with F1-score particularly useful when seeking a balance between precision and recall. Confusion matrices remain essential for understanding the specific nature of classification errors.
The exceptional performance of recently developed models like the EPI-VT-Score (AUC-ROC: 0.990) demonstrates the potential of well-validated clinical prediction tools [65]. However, researchers should maintain a comprehensive evaluation approach utilizing multiple metrics to fully characterize model performance and ensure clinical relevance in this high-stakes domain where model predictions directly influence procedural strategy and patient outcomes.
In the field of ventricular tachycardia (VT) ablation surgery research, the transition from traditional statistical models to machine learning (ML) frameworks represents a significant evolution in predictive analytics. Accurate prediction of ablation targets and procedural outcomes is critical for improving the success rates of catheter ablation, a cornerstone therapy for drug-refractory VT. While traditional statistical methods have provided foundational insights, they often struggle with the high-dimensional, complex data inherent to cardiac electrophysiology. This guide provides an objective, data-driven comparison of these competing methodologies, offering researchers a clear framework for model selection in VT research.
Performance Benchmarking: Quantitative Data Comparison
The following tables summarize the performance of machine learning models against traditional statistical baselines as reported in recent peer-reviewed studies.
Table 1: Performance Benchmarking in VT Ablation Target Localization
| Model Type | Specific Model | Task | AUC | Sensitivity | Specificity | Citation |
|---|---|---|---|---|---|---|
| Machine Learning | Random Forest | Localizing VT ablation targets from substrate maps in a porcine model | 0.821 | 81.4% | 71.4% | [2] |
| Machine Learning | Multistage Diagnostic Scheme (Proprietary Features) | Classifying Left & Right Outflow Tract VT origins | 0.99 | 96.97% | 100% | [12] |
| Traditional Statistical | Conventional QRS Morphological Measurements | Classifying Left & Right Outflow Tract VT origins | (Performance significantly lower than ML counterpart) | - | - | [12] |
Table 2: Performance Benchmarking in Predicting Arrhythmia Recurrence
| Model Type | Specific Model / Data | Task | AUC | Key Predictors Identified | Citation |
|---|---|---|---|---|---|
| Machine Learning | Light Gradient Boosting Machine (LightGBM) | Predicting AF recurrence post-ablation using clinical data | 0.848 | BNP, Neutrophil-to-Lymphocyte Ratio | [22] |
| Machine Learning | Merged Framework (CT imaging + clinical data) | Predicting AF ablation outcome | 0.821 | Deep features from CT, clinical data | [70] |
| Traditional Statistical | Clinical Models/Scores (Typical Range) | Predicting success after catheter ablation | 0.55 - 0.65 | Left atrial size, sphericity index | [70] |
| Machine Learning | Explainable ML (xML) with SHAP | Predicting arrhythmia recurrence post-AF ablation | 0.80 | Large LA, low post-ablation scar, prior cardioversion | [71] |
Detailed Experimental Protocols
To ensure the reproducibility of the cited benchmarks, this section outlines the core methodologies employed in the key studies.
Protocol for ML-Based VT Ablation Target Localization
A study detailed in European Heart Journal - Digital Health developed an ML model to automate the localization of ventricular tachycardia ablation targets. The protocol was as follows [2]:
- Subject Data: The study utilized 56 substrate maps and 35,068 intracardiac electrograms (EGMs) collected from 13 pigs with chronic myocardial infarction.
- Feature Engineering: Forty-six signal features representing functional, spatial, spectral, and time-frequency properties were computed from each bipolar and unipolar EGM.
- Labeling: Mapping sites within 6 mm from localized critical sites of induced VT circuits were defined as positive ablation targets.
- Model Training & Validation: Several machine learning models were developed. The best-performing model, a Random Forest classifier, was evaluated based on its ability to localize these pre-defined targets. The model's performance was validated, resulting in an AUC of 0.821 [2].
Protocol for Outflow Tract VT Classification
Research published in Frontiers in Physiology established a high-precision algorithm for classifying Left and Right Outflow Tract VT origins [12]:
- Patient Cohort: 420 patients who underwent successful catheter ablation for VT or premature ventricular complexes (PVC) were included. Effective ablation sites confirmed by the procedure provided the ground-truth labels (RVOT or LVOT).
- Data Input: Three cardiac electrophysiologists unanimously selected one QRS complex during sinus rhythm and one during VT/PVC from each patient's ECG.
- Feature Extraction: A proprietary algorithm extracted 1,600,800 features from the 12-lead ECGs, far exceeding the capacity of manual measurement.
- Model Development and Evaluation: An extreme gradient boosting tree (XGBoost) model was trained. The study employed a rigorous training–validation–testing design (81%-9%-10% split). The model achieved an exceptional AUC of 0.99 on the testing set, significantly outperforming models based on conventional ECG measurements [12].
Protocol for Traditional Statistical Benchmarking
The performance of traditional statistical models is often derived from clinical scores based on simpler, hypothesis-driven frameworks [70] [72]:
- Data Input: These models typically rely on a limited set of clinically derived parameters, such as left atrial size or sphericity index from imaging studies, and patient demographics.
- Modeling Approach: Techniques like linear or logistic regression are used to establish a parametric relationship between the input variables and the outcome (e.g., recurrence).
- Inherent Limitations: The focus is on hypothesis testing and understanding relationships between variables rather than pure prediction. This approach requires manual feature selection and struggles with complex, non-linear interactions in the data, resulting in the lower AUC range (0.55-0.65) observed in benchmarks [70] [72].
Workflow Visualization
The fundamental difference between the two approaches can be visualized in their respective workflows.
ML Model Development Workflow
ML Workflow for VT Ablation Research. This diagram illustrates the iterative, data-centric process of developing a machine learning model, from raw data collection to final prediction, highlighting the crucial feedback loop for model optimization [2] [12].
Traditional Statistical Modeling Workflow
Traditional Statistical Modeling Workflow. This diagram outlines the sequential, hypothesis-driven process of traditional statistical modeling, emphasizing the initial definition of variables and testing of assumptions before model fitting [72].
The Scientist's Toolkit: Essential Research Reagents & Materials
The following tools are critical for conducting experimental research in this field.
Table 3: Essential Research Reagents and Solutions
| Item Name | Function/Application | Relevance to Research |
|---|---|---|
| Multipolar Catheter (e.g., Advisor HD Grid) | High-density electrophysiological mapping | Acquires intracardiac electrogram (EGM) signals for feature extraction in ML models [2]. |
| Electroanatomic Mapping System (e.g., CARTO, NavX) | 3D visualization of cardiac anatomy and electrical activity | Creates the spatial substrate maps used to define features and validate ablation targets [2] [12]. |
| Late Gadolinium Enhanced Magnetic Resonance (LGE-MRI) | Tissue characterization to identify fibrotic or scarred myocardium | Provides critical imaging biomarkers for both traditional and ML models predicting recurrence [70] [71]. |
| Irrigated Ablation Catheter (e.g., Navistar) | Delivery of radiofrequency energy for ablation | The primary tool for creating lesions; successful application defines the ground-truth labels for ML training [12]. |
| SHapley Additive exPlanations (SHAP) | Model interpretability framework | Explains the output of complex ML models, identifying key predictive features for clinical transparency [71] [22]. |
| Synthetic Minority Over-sampling (SMOTE) | Data preprocessing for imbalanced datasets | Addresses class imbalance (e.g., few recurrence events) to improve ML model robustness [22]. |
The integration of artificial intelligence (AI) into ventricular tachycardia (VT) ablation research represents a paradigm shift in cardiac electrophysiology. However, the transition from promising algorithm to clinically adopted tool requires rigorous validation through prospective studies and randomized controlled trials (RCTs). This pathway ensures that AI models not only achieve technical excellence but also deliver tangible improvements in patient outcomes and clinical workflows.
The clinical implementation of AI solutions faces a significant translational gap; despite extensive technical development and FDA approvals, most AI tools remain confined to retrospective validations and pre-clinical settings, seldom advancing to prospective evaluation in critical decision-making workflows [73]. This gap is particularly critical in VT ablation, where AI-powered models for risk stratification, ablation targeting, and outcome prediction must meet the highest evidence standards to gain clinical trust and regulatory endorsement. A framework modeled after traditional clinical trials—progressing from safety and efficacy to effectiveness and post-deployment monitoring—provides a structured pathway for validating these tools [74]. For AI solutions claiming direct clinical benefit for patients, the requirement for formal RCTs becomes imperative, analogous to the drug development process [73].
Performance Comparison of AI Validation Methodologies
The evaluation of AI models requires multiple methodological approaches, each providing distinct evidence about performance and clinical readiness. The following table summarizes the key validation paradigms and their documented effectiveness in cardiac electrophysiology research.
Table 1: Comparative Performance of AI Validation Methodologies in Cardiac Electrophysiology
| Validation Type | Primary Objective | Typical Cohort Size | Key Performance Metrics | Strengths | Limitations |
|---|---|---|---|---|---|
| Retrospective Validation [75] | Initial technical feasibility and model tuning | Hundreds to thousands of patient records | Area Under the ROC Curve (AUC), Accuracy, F1-score | Efficient use of existing data; Identifies promising algorithms | High risk of data leakage; Poor generalizability to real-world settings |
| Prospective Validation (Silent Trial) [74] | Assess efficacy under ideal, real-time conditions without impacting care | Dozens to hundreds of patients | Sensitivity, Specificity, Positive Predictive Value (PPV) | Tests real-time data pipelines; No patient risk | Does not measure clinical utility or workflow impact |
| Randomized Controlled Trial (RCT) [73] [75] | Establish causal evidence of clinical benefit and safety | Hundreds to thousands of patients | Clinical outcome rates (e.g., VT recurrence), Physician adoption rates, Workflow efficiency | Highest level of evidence; Directly measures patient impact | Resource-intensive; Complex to design and execute |
| Post-Market Surveillance [74] | Monitor long-term performance, safety, and equity after deployment | Thousands of patients across diverse settings | Model performance drift, Adverse event rates, Equity metrics across demographics | Ensances sustained safety and effectiveness in real-world use | Requires integrated, continuous monitoring systems |
The performance metrics used in these validation stages are critical for interpretation. In classification tasks common to VT prediction, the confusion matrix is the fundamental output, from which metrics like sensitivity, specificity, and positive predictive value are derived [75]. The F1-score (the harmonic mean of sensitivity and PPV) is particularly valuable in cases of class imbalance, such as predicting rare but dangerous VT events, as it provides a more robust performance estimate than accuracy alone [75].
Experimental Protocols for Rigorous AI Validation
Cohort Selection and Data Partitioning Protocol
Proper cohort design is foundational to avoiding biased performance estimates. The following protocol ensures rigorous separation of data for training, validation, and testing:
- Patient-Level Partitioning: In datasets with multiple records per patient (e.g., sequential ECGs), all records from a single patient must be assigned to the same partition (training, validation, or testing) to prevent data leakage. This ensures the interpretation is "model performance on unseen, similar patients" rather than "performance in this cohort only" [75].
- K-Fold Cross-Validation: The training-validation cohort should be divided using K-fold cross-validation (typically K=5 or 10). This approach (1) enables validation predictions for all patients in the training cohort, (2) produces an estimate of model variation, (3) avoids an "unlucky split," and (4) allows for creating ensemble models that typically outperform individual models [75].
- Hold-Out Testing Set: A final hold-out testing set must be reserved for a single, final evaluation after all model development and hyperparameter tuning is complete. The model may not be changed after "unblinding" to testing set results [75].
Prospective Validation (Silent Trial) Protocol
The "silent trial" represents a critical bridge between retrospective development and full RCT, deploying AI in live clinical environments without impacting patient care [74]:
- Integration: Embed the AI model within the clinical data pipeline (e.g., EHR system) to process real-time patient data.
- Background Execution: Run the model in "silent mode" where predictions are generated but not displayed to clinicians and do not influence clinical decisions.
- Parallel Assessment: Compare AI predictions against (a) the eventual clinical diagnoses and (b) the decisions made by clinicians without AI assistance.
- Workflow Mapping: Use this phase to identify and organize the necessary data pipelines and determine which team members (e.g., electrophysiologist, nurse) would act on the AI output in a future active deployment [74].
Randomized Controlled Trial Design Protocol
For AI tools intended to directly influence VT ablation procedures, RCTs represent the gold standard for validation [73]:
- Randomization Scheme: Implement cluster randomization (by clinician or clinical site) or patient-level randomization to an AI-assisted arm versus standard care arm.
- Blinding: While often impossible to blind clinicians, outcome assessors (e.g., those adjudicating VT recurrence) should be blinded to treatment allocation.
- Primary Endpoint Selection: Define clinically meaningful primary endpoints relevant to VT ablation, such as:
- Acute procedural success (non-inducibility of VT)
- VT recurrence-free survival at 6/12 months
- Procedure time or radiation exposure
- Reference Model Comparison: The AI model must be compared to a reference model without machine learning, such as standard clinical risk scores, to establish additive value [75].
- Sample Size Calculation: Perform power calculations based on the primary endpoint to ensure the trial is adequately powered to detect a clinically significant effect.
Workflow Visualization for AI Validation
The following diagram illustrates the complete pathway from model development to clinical adoption, integrating the key validation stages discussed.
Figure 1: The pathway for clinical adoption of AI models in VT ablation research, from initial development through rigorous validation stages to sustained clinical use.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the validation pathway requires specific methodological tools and resources. The following table details key solutions for implementing robust AI validation in VT ablation research.
Table 2: Essential Research Reagents and Methodological Solutions for AI Validation
| Tool/Reagent | Category | Primary Function | Implementation Example in VT Research |
|---|---|---|---|
| Structured Data Partitioner [75] | Software Tool | Ensures strict patient-level separation between training, validation, and testing sets to prevent data leakage. | Scripts to guarantee all ECG episodes from a single patient reside in only one data partition. |
| K-Fold Cross-Validation Framework [75] | Statistical Protocol | Provides robust performance estimation during model development and enables creation of ensemble models. | Dividing a training set of 500 patient records into 5 folds for iterative training and validation. |
| Silent Trial Integration Platform [74] | Software Infrastructure | Allows AI models to run in live clinical environments ("background") without impacting patient care. | An EHR-integrated system that processes incoming intracardiac signals but does not display predictions to the electrophysiologist. |
| Clinical Outcome Adjudication Committee [73] | Human Resource | Provides blinded, expert assessment of primary clinical endpoints (e.g., VT recurrence) for RCTs. | A panel of independent cardiologists reviewing patient Holter and device data, blinded to AI arm assignment. |
| Model Drift Detection System [74] | Monitoring Software | Continuously tracks AI model performance post-deployment to identify degradation due to data shifts. | Automated alerts triggered when the feature distribution of new VT ablation patients deviates significantly from the training cohort. |
| Explainability Methods (e.g., Attention Maps) [75] | Analytical Tool | Provides insights into model reasoning by highlighting input features (e.g., ECG segments) driving predictions. | Using gradient-weighted class activation mapping to identify which parts of an electrogram most influenced a VT source prediction. |
The path to clinical adoption for AI in ventricular tachycardia ablation research is unequivocally anchored in prospective validation and randomized trials. While technical performance on retrospective datasets is a necessary first step, it is insufficient evidence for clinical integration. The structured progression from silent trials to full-scale RCTs, modeled after the established framework for drug and device development, provides the methodological rigor needed to ensure safety, efficacy, and ultimately, improved patient outcomes. As the field advances, this rigorous validation pathway will separate clinically transformative AI tools from mere technical curiosities, ensuring that promising algorithms successfully transition from research environments to routine clinical practice in cardiac electrophysiology.
Conclusion
The validation of machine learning models for VT ablation represents a paradigm shift towards data-driven, personalized cardiology. Synthesizing the key intents reveals that successful model development hinges on addressing specific clinical challenges with a rigorous methodological pipeline, while proactively troubleshooting issues of data imbalance and interpretability. The future of this field lies in conducting large-scale, prospective, multi-center randomized trials—such as the AUTOMATED-WCT and CAAD-VT designs—to firmly establish clinical utility. Future research must focus on the seamless integration of validated algorithms into electronic health records, enabling real-time decision support that can optimize ablation strategy, improve long-term survival, and ultimately redefine standards of care for patients with ventricular tachycardia.
References
- 1. Machine Learning-Based Prediction of Three-Year Heart ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607369/]
- 2. Machine learning approach for automated localization of ... [https://pubmed.ncbi.nlm.nih.gov/40703139/]
- 3. Predicting in-hospital mortality in patients with heart failure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11667998/]
- 4. Long-Term Outcomes and Post-Ablation Medication De ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593862/]
- 5. Machine learning model for predicting in-hospital cardiac ... [https://www.nature.com/articles/s41598-025-14579-8]
- 6. Pinpointing the heart's trouble spots with artificial intelligence [https://sciencenews.dk/en/pinpointing-the-hearts-trouble-spots-with-artificial-intelligence]
- 7. Heart Digital Twins Predict Features of Invasive Reentrant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12313252/]
- 8. How to Identify Ventricular Tachycardia Substrate [https://www.innovationsincrm.com/cardiac-rhythm-management/articles-2019/march/1415-how-to-identify-ventricular-tachycardia-substrate]
- 9. Computer-aided detection of arrhythmogenic sites in post- ... [https://www.nature.com/articles/s41598-023-33866-w]
- 10. Vector field heterogeneity as a novel omnipolar mapping ... [https://www.sciencedirect.com/science/article/pii/S1547527124035318]
- 11. Functional Substrate Mapping | AER Journal [https://www.aerjournal.com/articles/functional-substrate-mapping-new-frontier-treatment-ventricular-tachycardia-structural?language_content_entity=en]
- 12. A High-Precision Machine Learning Algorithm to Classify ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2021.641066/full]
- 13. 利用人工智能工具帮助定ä½å®¤æ€§å¿ƒåŠ¨è¿‡é€Ÿä¸çš„问题心è„细胞 [https://news.bioon.com/article/8a648939e1a8.html]
- 14. 基于机器å¦ä¹ 的心室心动过速消èžé¶ç‚¹è‡ªåŠ¨å®šä½æ–°ç–ç•¥ [https://www.ebiotrade.com/newsf/2025-6/20250611113905137.htm]
- 15. 基于机器å¦ä¹ 的慢性瓣膜病åˆå¹¶å¿ƒæˆ¿é¢¤åŠ¨æ‚£è€…è¡ŒCox迷宫IV手术 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10930048/]
- 16. 医å¦æ‰‹æœ¯è§„划和手术导航åŠå¯¼èˆªä¸VR技术使用原创 [https://blog.csdn.net/q610098308/article/details/146334517]
- 17. Reconstructed scar morphology in patient-specific ... [https://www.sciencedirect.com/science/article/pii/S0010482525005803]
- 18. Approaching Ventricular Tachycardia Ablation in 2024 [https://www.mdpi.com/2077-0383/13/17/5017]
- 19. Heart Rhythm 2025 Showcases New Advancements in ... [https://www.hrsonline.org/news/hr2025-showcases-new-advancements-emerging-paf-technology/]
- 20. Case report of ventricular tachycardia simulation facilitated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12396111/]
- 21. Explainable Artificial Intelligence-Driven Risk Assessment ... [https://www.sciencedirect.com/science/article/pii/S0828282X25011675]
- 22. Machine learning-based prediction model for recurrence ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1642409/full]
- 23. Interpretable Clinical Decision-Making Application for ... [https://www.mdpi.com/2075-4418/14/20/2291]
- 24. XGBoost vs LightGBM - It's Amit - Medium [https://mr-amit.medium.com/xgboost-vs-lightgbm-b6ca76620156]
- 25. XGBoost vs LightGBM: How Are They Different [https://neptune.ai/blog/xgboost-vs-lightgbm]
- 26. CardioForest: An Explainable Ensemble Learning Model ... [https://arxiv.org/html/2509.25804v2]
- 27. Idiopathic Ventricular Arrhythmias Originating from the Left ... [https://www.mdpi.com/2077-0383/14/12/4261]
- 28. Long-term outcomes of ventricular tachycardia ablation in ... [https://pubmed.ncbi.nlm.nih.gov/40633673/]
- 29. Predicting factors for unresolved premature ventricular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11866866/]
- 30. Efficacy and Safety of Catheter Ablation vs. Antiarrhythmic ... [https://www.acc.org/Latest-in-Cardiology/Articles/2025/06/17/11/53/Efficacy-and-Safety-of-Catheter-Ablation-vs-Antiarrhythmic-Drugs-For-VT-VANISH2]
- 31. Determining the recurrence rate of premature ventricular ... [https://www.sciencedirect.com/science/article/pii/S2352320424000257]
- 32. Automated Filtering and Visualization of Patient-Centered ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12517296/]
- 33. Improve Provider Productivity by 40% with EHR Dashboard [https://www.capminds.com/blog/effective-ehr-dashboard-boosts-productivity/]
- 34. Why EHR satisfaction should be on your 2025 radar - uPerform [https://www.uperform.com/blog/why-ehr-satisfaction-should-be-on-your-2025-radar/]
- 35. Comparing the Performance of Machine Learning Models ... [https://www.jmir.org/2025/1/e76215]
- 36. EHR Interoperability Solutions in 2025: What Actually Works? [https://www.medesk.net/en/blog/ehr-interoperability-solutions/]
- 37. Acute and long-term procedural outcomes, arrhythmia ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1582753/full]
- 38. An explainable deep learning framework for trustworthy ... [https://www.nature.com/articles/s41598-025-22986-0]
- 39. GAN-SkipNet: A Solution for Data Imbalance in Cardiac ... [https://www.mdpi.com/2227-7390/12/17/2693]
- 40. Machine learning of electrophysiological signals for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9945642/]
- 41. State of the Art of Artificial Intelligence in Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12123071/]
- 42. Machine-Learning-Based Prediction of 1-Year Arrhythmia ... [https://www.mdpi.com/2306-5354/10/12/1386]
- 43. Machine Learning in the Management of Patients ... [https://www.jmir.org/2025/1/e60888/]
- 44. Multimodal prediction of catheter ablation outcomes in ... [https://www.sciencedirect.com/science/article/abs/pii/S0893608025007154]
- 45. Interpretable Clinical Decision-Making Application for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11506268/]
- 46. Understanding SHAP : Unlocking Values in Interpretability ... Machine [https://kishanakbari.medium.com/understanding-shap-values-unlocking-interpretability-in-machine-learning-ee1f4a9b3a8c]
- 47. shap/shap: A game theoretic approach to explain the ... [https://github.com/shap/shap]
- 48. LIME vs SHAP: A Comparative Analysis of Interpretability ... [https://www.markovml.com/blog/lime-vs-shap]
- 49. Exploring SHAP, LIME, PDPs, and ICEs [https://medium.com/@kumar9059300448/understanding-interpretable-machine-learning-exploring-shap-lime-pdps-and-ices-9239b497f065]
- 50. Comparison of SHAP and clinician friendly explanations ... [https://www.nature.com/articles/s41746-025-01958-8]
- 51. Machine Learning Framework for Early Prediction of ... [https://digital.lib.washington.edu/researchworks/items/a20cc5d6-893d-420d-bbce-907976ee5a83/full]
- 52. Reducing False Ventricular Tachycardia Alarms in ICU ... [https://arxiv.org/html/2503.14621v1]
- 53. An artificial intelligence and machine learning model for ... [https://www.sciencedirect.com/science/article/pii/S0022522325005744]
- 54. 3.1. Cross-validation: evaluating estimator performance [https://scikit-learn.org/stable/modules/cross_validation.html]
- 55. Holdouts and Cross Validation: Why the Data Used t... [https://community.alteryx.com/t5/Data-Science/Holdouts-and-Cross-Validation-Why-the-Data-Used-to-Evaluate-your/ba-p/448982]
- 56. A multi-center cross-validation study within the RAVENTA ... [https://www.sciencedirect.com/science/article/pii/S0167814024007692]
- 57. Hold-out vs. Cross-validation in Machine Learning [https://medium.com/@jaz1/holdout-vs-cross-validation-in-machine-learning-7637112d3f8f]
- 58. Understanding Hold-Out Methods for Training Machine ... [https://www.comet.com/site/blog/understanding-hold-out-methods-for-training-machine-learning-models/]
- 59. Cross Validation in Machine Learning [https://www.geeksforgeeks.org/machine-learning/cross-validation-machine-learning/]
- 60. External validation: a simulation study to compare cross ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9464671/]
- 61. “From Hold-Out to K-Fold: Understanding Cross-Validation ... [https://medium.com/@kavyasrirelangi100/from-hold-out-to-k-fold-understanding-cross-validation-methods-in-machine-learning-37402f406759]
- 62. Practical Considerations and Applied Examples of Cross ... [https://ai.jmir.org/2023/1/e49023]
- 63. Understanding F , Accuracy, 1 - Score & ROC - AUC Metrics PR AUC [https://www.deepchecks.com/f1-score-accuracy-roc-auc-and-pr-auc-metrics-for-models/]
- 64. Model Evaluation: Precision, Recall, F , 1 - Score ... | Medium ROC AUC [https://medium.com/@kirti07arora/model-evaluation-precision-recall-f1-score-roc-auc-and-cross-validation-machine-learning-359e26855f9a]
- 65. A Novel Predictive Score to Identify the Necessity for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12614129/]
- 66. vs F vs Accuracy vs 1 : Which Evaluation... Score ROC AUC PR AUC [https://neptune.ai/blog/f1-score-accuracy-roc-auc-pr-auc]
- 67. Multi-Classification Model for PPG Signal Arrhythmia Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12526570/]
- 68. A High Precision Machine Learning-Enabled System for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8962834/]
- 69. A neuromorphic approach to early arrhythmia detection [https://www.nature.com/articles/s41598-025-23248-9]
- 70. Atrial fibrillation ablation outcome prediction with a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10857794/]
- 71. Predicting arrhythmia recurrence post-ablation in atrial ... [https://www.nature.com/articles/s43856-025-01058-4]
- 72. Machine Learning Models vs. Statistical Models [https://infomineo.com/blog/machine-learning-models-vs-statistical-models/]
- 73. AI in Drug Development: Clinical Validation and ... [https://globalforum.diaglobal.org/issue/june-2025/ai-in-drug-development-clinical-validation-and-regulatory-innovation-are-dual-imperatives/]
- 74. Clinical trials informed framework for real world ... [https://www.nature.com/articles/s41746-025-01506-4]
- 75. Evaluating artificial intelligence-enabled medical tests in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12419123/]