4D-Printed Smart Biomaterials: Engineering Dynamic Tissue Scaffolds for Regenerative Medicine
This article provides a comprehensive analysis of 4D printing for creating intelligent, dynamic tissue scaffolds.
4D-Printed Smart Biomaterials: Engineering Dynamic Tissue Scaffolds for Regenerative Medicine
Abstract
This article provides a comprehensive analysis of 4D printing for creating intelligent, dynamic tissue scaffolds. Aimed at researchers and biomedical engineers, it explores the foundational principles of smart biomaterials (e.g., shape-memory polymers, hydrogels) and their stimuli-responsive behaviors. It details the core methodologies, including material selection, advanced printing techniques (e.g., DLP, extrusion-based), and precise programming for temporal shape transformation. The article addresses critical challenges in printing fidelity, biocompatibility, and degradation control, offering optimization strategies. Finally, it evaluates scaffold performance through in vitro and in vivo validation, comparing 4D printing to static 3D counterparts. The synthesis concludes with future directions for clinical translation in tissue engineering and drug delivery.
What Are Smart Biomaterials? The Science Behind 4D Printing for Tissue Engineering
4D printing is an advanced additive manufacturing (AM) process that creates objects which can change shape, property, or functionality over time in response to specific external stimuli. It integrates smart, stimuli-responsive materials (often biomaterials) with precise 3D printing techniques, where the "fourth dimension" is the time-dependent transformation. Within the thesis context of smart biomaterials for dynamic tissue scaffolds, 4D printing enables the fabrication of scaffolds that can morph, degrade, or activate therapeutic functions post-implantation to better mimic natural tissue dynamics and enhance regeneration.
Table 1: Stimuli-Responsive Mechanisms in 4D Printed Biomaterials
| Stimulus Type | Example Material Class | Typical Response Time (Range) | Shape Change Magnitude (e.g., Bending Angle/Curvature) | Key Application in Tissue Scaffolds |
|---|---|---|---|---|
| Aqueous/Humidity | Hydrogels (alginate, gelatin-methacryloyl, PNIPAM) | 10 sec - 2 hours | 15° - 180° (folding) | Swelling-induced pore size change for cell entrapment/drug release. |
| Temperature | Shape Memory Polymers (PCL, PLA), PNIPAM | 30 sec - 10 min (trigger) | Up to 100% strain recovery | Self-tightening sutures or deployable stents triggered by body heat. |
| pH | Chitosan, PMAA-based hydrogels | 5 - 60 min | Swelling ratio: 1.5 - 4.0 | Drug release in specific inflammatory (acidic) microenvironments. |
| Ionic Strength | Alginate, polyelectrolyte complexes | 2 - 30 min | Variable layer thickness change | Controlled stiffness modulation to guide cell differentiation. |
| Magnetic Field | Ferromagnetic particle-doped polymers | < 1 sec (near instant) | Complex 3D reconfiguration | Remote-controlled scaffold actuation for mechanical conditioning. |
| Enzymatic/Biochemical | Peptide-crosslinked hydrogels | 1 - 24 hours | Degradation-tuned shape change | Cell-responsive scaffold remodeling during tissue growth. |
Table 2: Comparison of 4D Printing Techniques for Biomaterials
| Printing Technique | Compatible Smart Materials | Typical Resolution (XY) | Stimulus Integration Method | Key Advantage for Scaffolds |
|---|---|---|---|---|
| Direct Ink Writing (DIW) | Shear-thinning hydrogels, SMPs | 50 - 500 µm | Multi-material printing for anisotropic response | High cell viability, excellent for soft hydrogels. |
| Stereolithography (SLA/DLP) | Photopolymerizable resins, hydrogels | 10 - 100 µm | Grayscale or multi-wavelength for property gradients | High resolution for micro-architecture. |
| Fused Deposition Modeling (FDM) | SMP filaments (PCL, PU) | 100 - 400 µm | Pre-strain programming during deposition | Robust mechanical structures. |
| Digital Light Processing (DLP) | Bio-inks with photo-initiators | 25 - 100 µm | Voxelated curing for localized stiffness | Fast, high-detail structures. |
| PolyJet/Multi-Material Jetting | Acrylic-based photopolymers, hydrogels | 20 - 50 µm | Multiple print heads for composite voxels | Unparalleled multi-material design. |
Application Notes & Experimental Protocols
Protocol 3.1: Fabrication of a Temperature-Responsive 4D Bilayer Tissue Scaffold
Objective: To print a bilayer scaffold that undergoes rolling/unrolling in response to temperature change, mimicking vascular tissue dynamics.
A. Materials & Pre-Printing Preparation
- Ink A (Active Layer): Poly(N-isopropylacrylamide) (PNIPAM)-based hydrogel prepolymer (25% w/v) with 0.5% LAP photoinitiator. Function: Undergoes significant volume contraction above its Lower Critical Solution Temperature (LCST ~32°C).
- Ink B (Passive Layer): Methacrylated gelatin (GelMA, 15% w/v) with 0.5% LAP. Function: Swells slightly but remains dimensionally stable across 20-37°C, providing a mechanical constraint.
- Equipment: Extrusion-based bioprinter with dual-printhead, UV crosslinking module (365 nm, 5-10 mW/cm²), controlled stage (Peltier plate, 15-45°C).
B. Printing & Programming Workflow
- Model Design: Design a flat, rectangular bilayer construct (20mm x 5mm). The bottom layer (Ink B, 200 µm thick) is 10% wider than the top layer (Ink A, 150 µm thick).
- Printing Parameters:
- Nozzle Diameter: 250 µm.
- Printing Temperature: 20°C (below PNIPAM LCST).
- Print Speed: 8 mm/s.
- Layer-by-layer printing: First, deposit Ink B (Passive). Immediately print Ink A (Active) aligned atop it.
- Simultaneous UV curing after deposition of each full layer.
- Post-Printing: Incubate the flat scaffold in PBS at 20°C for 24h for hydration equilibrium.
C. Activation & Characterization
- Stimulus Application: Transfer scaffold to a PBS bath at 37°C. The PNIPAM layer will dehydrate and contract, while the GelMA layer remains swollen.
- Kinetic Analysis: Record the shape change (rolling into a tube) via time-lapse photography over 10 minutes. Measure the radius of curvature every 30s.
- Cell Studies (Optional): Seed fibroblasts on the scaffold at 20°C (flat state). Raise temperature to 37°C; the rolling action will encapsulate cells, creating a 3D tissue model.
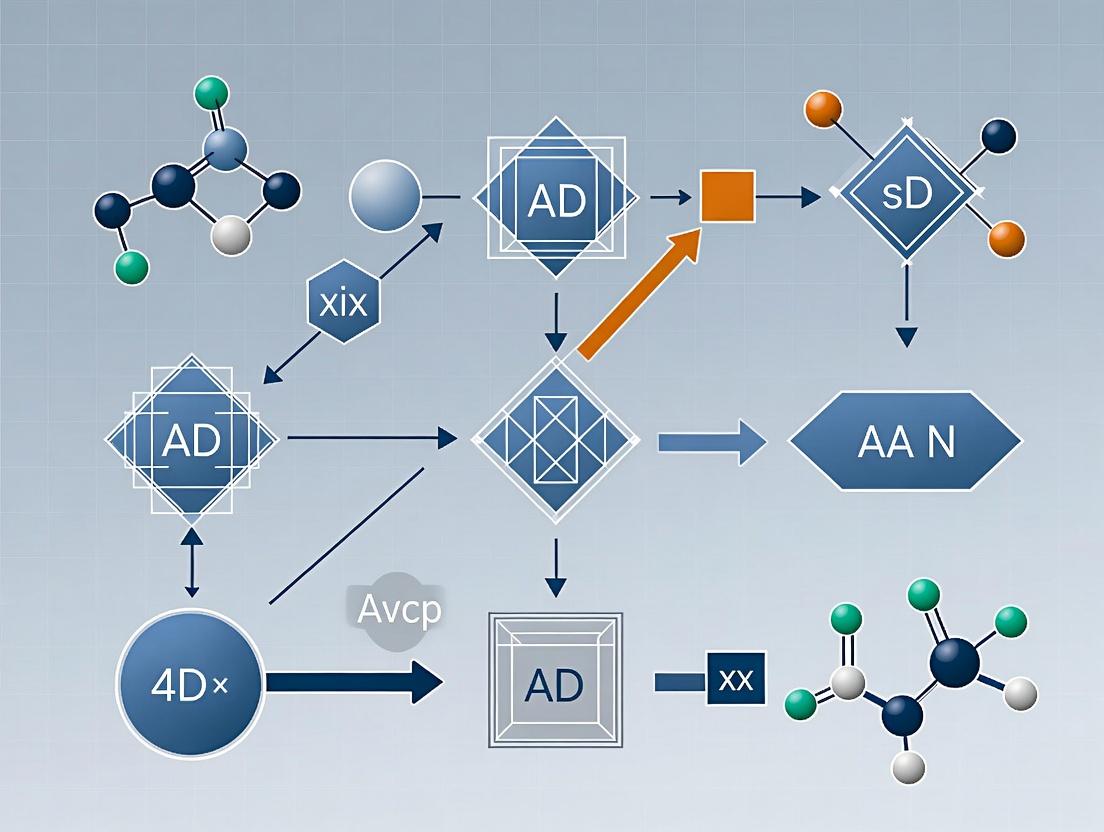
DOT Diagram: 4D Scaffold Printing and Activation Workflow
Protocol 3.2: Enzymatically Triggered Degradation & Shape Change in 4D Printed Scaffolds
Objective: To create a cell-responsive scaffold where matrix metalloproteinase (MMP) activity, indicative of cell remodeling, triggers localized degradation and shape recovery.
A. Materials & Pre-Printing Preparation
- Ink Formulation: MMP-sensitive peptide (e.g., GCGPQGIWGQGCG) crosslinked into a hyaluronic acid methacrylate (HAMA) network. Include 1% w/v LAP photoinitiator.
- Control Ink: Same HAMA network crosslinked with a non-degradable dithiol (PEG-DTT).
B. Printing & Programming Workflow
- Design: Print a compressed, "pre-strained" lattice structure using the MMP-sensitive ink.
- Programming: After printing and initial UV crosslinking, mechanically deform (compress) the scaffold and a second, permanent crosslinking (e.g., with a non-sensitive PEG-diacrylate) is performed to "lock in" the temporary shape.
- Post-Printing: Release the constraint; the scaffold remains in its temporary, compressed shape.
C. Activation & Characterization
- Stimulus Application: Immerse the scaffold in a collagenase solution (2 µg/mL in PBS) or seed with MMP-secreting cells (e.g., mesenchymal stem cells).
- Response: Enzymatic cleavage of the MMP-sensitive crosslinks releases the "locked-in" strain, causing the scaffold to gradually expand to its original, printed shape over 3-7 days.
- Quantification: Measure recovery of height/volume over time. Correlate with MMP activity via fluorometric assays.
DOT Diagram: MMP-Responsive 4D Scaffold Mechanism
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for 4D Printing of Smart Biomaterial Scaffolds
| Reagent/Material | Function in 4D Printing | Example Supplier/Cat. No. (Research-Grade) | Critical Parameters for Protocols |
|---|---|---|---|
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable, biocompatible hydrogel base; passive/active layer component. | Advanced BioMatrix, Sigma-Aldrich | Degree of methacrylation (60-90%), concentration (5-20%). |
| Poly(N-isopropylacrylamide) (PNIPAM) | Temperature-responsive polymer for active layers (LCST ~32°C). | Sigma-Aldrich, Polymersource | Molecular weight, co-monomer type for LCST tuning. |
| Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Highly efficient, biocompatible photoinitiator for UV/VIS crosslinking. | Tokyo Chemical Industry | Concentration (0.1-1.0% w/v), cytocompatibility at low %. |
| MMP-Sensitive Peptide Crosslinker | Provides enzymatic responsiveness for cell-driven scaffold remodeling. | Genscript, Bachem | Peptide sequence (e.g., for MMP-2), solubility. |
| Poly(ε-caprolactone) (PCL) Diol/Diacrylate | Shape Memory Polymer precursor; provides elasticity and programmable temporary shapes. | Sigma-Aldrich, Polysciences | Molecular weight (Mn ~2k-10k), crystallinity. |
| Magnetic Nanoparticles (Fe3O4) | Enables remote actuation via magnetic fields for dynamic mechanical stimulation. | Sigma-Aldrich, nanoComposix | Particle size (20-50 nm), surface coating for dispersion. |
| Rhodamine B Isothiocyanate (RITC)-dextran | Fluorescent tracer for quantifying swelling/deswelling kinetics and diffusion. | Sigma-Aldrich | Molecular weight (e.g., 70kDa), conjugation stability. |
| Poly(ethylene glycol) Diacrylate (PEGDA) | Used as a secondary, permanent crosslinker to "lock in" temporary shapes. | Sigma-Aldrich, Laysan Bio | Mn (575, 3400), functionality. |
Application Notes
Hydrogels
Hydrogels are three-dimensional, hydrophilic polymer networks capable of absorbing large amounts of water or biological fluids. Their high water content, tunable porosity, and biocompatibility make them ideal for mimicking the extracellular matrix (ECM). For 4D-printed dynamic tissue scaffolds, hydrogels can be designed to respond to stimuli (pH, temperature, enzymes) to modulate cell behavior, release therapeutic agents, or gradually degrade to be replaced by native tissue.
Key Applications in 4D Printing:
- Cell-Laden Bioprinting: Encapsulation of living cells (e.g., chondrocytes, stem cells) within bioinks for direct fabrication of tissue constructs. Responsive gels can stiffen post-printing to provide mechanical integrity.
- Drug Release Scaffolds: Printing of hydrogel scaffolds with embedded growth factors (e.g., VEGF, BMP-2) for spatiotemporally controlled release triggered by physiological cues.
- Dynamic Morphing Structures: Printing of bilayer or gradient structures with differential swelling properties, enabling pre-programmed shape changes (e.g., curling tubes) upon immersion in aqueous media.
Shape-Memory Polymers (SMPs)
SMPs are materials that can be deformed from a permanent shape, fixed into a temporary shape, and later recover their original shape upon application of an external stimulus (heat, light, magnetic field). In 4D-printed scaffolds, this allows for minimally invasive implantation (temporary compact shape) and subsequent shape recovery to a complex, functional geometry in vivo.
Key Applications in 4D Printing:
- Self-Fitting Implants: Printing of porous SMP scaffolds in a compact temporary shape for endoscopic delivery; body temperature triggers expansion to fill a tissue defect.
- Mechanically Adaptive Scaffolds: Programming SMPs to change stiffness after implantation—soft for initial integration, then stiff to support load-bearing (e.g., bone).
- Actuating Structures: Creating scaffolds that apply gradual, gentle force to surrounding tissue, useful in applications like mandibular distraction osteogenesis.
Liquid Crystal Elastomers (LCEs)
LCEs combine the molecular order of liquid crystals with the elastic properties of elastomers. This unique combination results in materials capable of large, reversible, and directional shape changes (actuation) in response to heat, light, or other stimuli. They offer precise control over the magnitude and direction of deformation.
Key Applications in 4D Printing:
- Biomimetic Actuators: Printing of LCE scaffolds that mimic the anisotropic contraction of muscle tissue, providing dynamic mechanical cues to seeded myocytes or cardiomyocytes.
- Stimuli-Responsive Pores: Creating pore architectures that open or close in response to specific stimuli (e.g., near-infrared light), enabling controlled cell infiltration or release of metabolites.
- Cellular Mechanotransduction Studies: Fabrication of platforms that cyclically stretch or compress cells in a controlled, programmable manner to study cell response to dynamic mechanical forces.
Table 1: Comparative Properties of Core Smart Biomaterial Classes for 4D Printing
| Property | Hydrogels | Shape-Memory Polymers (SMPs) | Liquid Crystal Elastomers (LCEs) |
|---|---|---|---|
| Primary Stimulus | pH, Temp, Ionic, Light | Heat, Light, Magnetic | Heat, Light (NIR/UV) |
| Key Response | Swell/Shrink, Degrade | Shape Recovery (One-way) | Reversible Actuation |
| Typical Strain | 10-200% (Swelling) | 100-1000% (Recovery) | 20-400% (Actuation) |
| Response Time | Seconds to Hours | Seconds to Minutes | Milliseconds to Seconds |
| Mechanical Modulus (Hydrated) | 0.1 kPa - 10 MPa | 10 MPa - 3 GPa (glassy) | 0.1 - 100 MPa |
| Cell Compatibility | Excellent (High water content) | Good (Surface modification often needed) | Moderate (Requires biofunctionalization) |
| 4D Printability | Excellent (Direct ink writing, stereolithography) | Good (Fused deposition modeling, polyjet) | Emerging (Direct ink writing of LCE inks) |
Experimental Protocols
Protocol: 4D Printing of a Thermoresponsive Bilayer Hydrogel Actuator
Aim: To fabricate a scaffold that undergoes programmed curling upon temperature change, mimicking dynamic tissue environments. Materials: See Scientist's Toolkit section.
Methodology:
- Ink Formulation:
- Prepare Ink A (Passive Layer): 15% w/v GelMA, 0.25% w/v LAP in PBS. Heat at 60°C until fully dissolved. Filter sterilize (0.22 µm).
- Prepare Ink B (Active Layer): 10% w/v PNIPAm (or commercial thermogel), 2% w/v Alginate, 0.25% w/v LAP in culture medium. Dissolve on ice. Filter sterilize.
Printing Setup:
- Use a stereolithography (SLA) or digital light processing (DLP) bioprinter equipped with a dual-vat system or sequential printing capability.
- Set build platform temperature to 15°C.
Printing Process:
- Layer 1 (Active): Load Ink B. Print the first layer pattern using UV light (365 nm, 10 mW/cm² for 15s per 100 µm layer).
- Layer 2 (Passive): Without moving the platform, switch vats to Ink A. Print the second layer pattern directly atop the first (365 nm, 15 mW/cm² for 20s per 100 µm layer).
- Repeat for 10 bilayers to create a rectangular strip (20mm x 5mm x 1mm).
Post-Processing:
- Gently rinse the printed structure in sterile PBS at 15°C to remove unreacted monomers.
- Crosslink the alginate in Ink B by immersing in 100mM CaCl₂ solution for 5 minutes.
- Rinse again with PBS.
4D Actuation Test:
- Immobilize one end of the strip.
- Transfer to a cell culture medium bath at 37°C.
- Record the deformation (curling angle vs. time) using a time-lapse camera over 30 minutes.
- Quantitative Data: Measure the radius of curvature (R) of the strip after equilibrium at 37°C.
Workflow for 4D-Printed Bilayer Hydrogel Actuation
Protocol: Programming a 4D-Printed Shape-Memory Polymer Scaffold
Aim: To create a porous SMP scaffold that can be compressed for implantation and recover its shape at body temperature. Materials: See Scientist's Toolkit section.
Methodology:
- Printing Permanent Shape (Porous Scaffold):
- Load poly(ε-caprolactone) (PCL) or poly(L-lactide-co-trimethylene carbonate) filaments into a fused deposition modeling (FDM) printer.
- Print a 10x10x5mm³ porous scaffold (e.g., 0/90° laydown pattern, 60% porosity, 400 µm strand distance). This defines the permanent shape.
Programming the Temporary Shape:
- Heat the printed scaffold in an oven to Ttrans + 10°C (e.g., 65°C for PCL, Ttrans ~55°C).
- Once soft, apply uniaxial compressive force (using a calibrated mechanical tester) to reduce scaffold height by 70%.
- Hold the strain constant while cooling the scaffold to T_trans - 20°C (e.g., 35°C). This "freezes" the molecular chains in the deformed state.
- Release the load. The scaffold maintains the compressed temporary shape.
Shape Recovery Analysis:
- Place the programmed scaffold in a phosphate-buffered saline (PBS) bath at 37°C.
- Use a camera to record the recovery process.
- Calculate the Shape Recovery Ratio (Rr): Rr(%) = (εm - εt) / εm * 100, where εm is the maximum strain applied during programming, and ε_t is the residual strain at time t.
SMP Programming and Thermal Recovery Cycle
Protocol: Characterizing Photothermal Actuation of a 4D-Printed LCE Scaffold
Aim: To quantify the reversible, light-induced actuation strain of a printed LCE grid scaffold. Materials: See Scientist's Toolkit section.
Methodology:
- Ink Preparation & Printing:
- Use a pre-formulated, photo-polymerizable LCE ink containing mesogens, crosslinkers, and a photoinitiator.
- Load ink into a direct ink writing (DIW) printer with a heated syringe (typically 80-100°C to reduce viscosity).
- Print a simple grid structure (15mm x 15mm, single layer) onto a glass substrate. Maintain print bed at 60°C to align mesogens via shear forces during extrusion.
- Immediately cure the printed filament using UV light (365 nm) to lock in the alignment (monomeric "glassy" state).
Thermal Post-Curing:
- Transfer the printed grid to an oven at 120°C (above the nematic-isotropic transition, T_ni) for 2 hours to complete the crosslinking, establishing the polydomain permanent shape.
Photothermal Actuation Test:
- Clamp one end of the LCE grid. Attach a non-contact video extensometer or use digital image correlation (DIC) software for strain measurement.
- Expose the entire grid to a near-infrared (NIR) laser (808 nm, 1.5 W/cm², 5mm spot diameter, scanning if needed) for 30 seconds.
- The incorporated photothermal agent (e.g., graphene, gold nanorods) converts light to heat, raising the local temperature above T_ni, causing contraction along the nematic director.
- Turn off the laser and allow the grid to cool and recover for 60 seconds.
- Repeat for 10 cycles to assess reversibility and fatigue.
- Quantitative Data: Calculate Actuation Strain (ε): ε(%) = (L0 - L) / L0 * 100, where L_0 is initial length and L is contracted length.
LCE Photothermal Actuation and Recovery Mechanism
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for 4D Printing Smart Biomaterial Scaffolds
| Material/Reagent | Function/Description | Example Supplier/Catalog |
|---|---|---|
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable hydrogel derivative of gelatin; provides cell-adhesive RGD motifs. | Advanced BioMatrix, 7505-50 |
| Poly(N-isopropylacrylamide) (PNIPAm) | Thermoresponsive polymer; undergoes reversible swelling/deswelling at Lower Critical Solution Temperature (LCST ~32°C). | Sigma-Aldrich, 535311 |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Highly efficient, water-soluble photoinitiator for UV (365-405 nm) crosslinking of hydrogels. | TCI Chemicals, L0366 |
| Poly(ε-caprolactone) (PCL) | Biodegradable, thermoplastic polyester; common SMP for FDM printing with T_trans ~55°C. | Corbion, PURASORB PC 12 |
| Poly(L-lactide-co-trimethylene carbonate) (PLLA-TMC) | Amorphous, flexible copolymer with tunable T_g for SMPs; degrades via hydrolysis. | Evonik, RESOMER LT 706 S |
| RM257 / RM82 Mesogens | Diacrylate liquid crystal monomers used to formulate LCE inks; provide mesogenic order. | Wilshire Technologies, WT-257 / WT-82 |
| Gold Nanorods (AuNRs) | Photothermal agent; absorbs NIR light and converts it to localized heat for LCE actuation. | nanoComposix, AUNR-10-800 |
| Alginic Acid Sodium Salt | Ionic polysaccharide; used as a rheology modifier and for secondary ionic crosslinking. | Sigma-Aldrich, A0682 |
| Calcium Chloride (CaCl₂) Solution | Ionic crosslinker for alginate, stabilizing printed hydrogel structures. | Various |
| Digital Light Processing (DLP) BioPrinter | Printer for high-resolution, layer-wise photopolymerization of hydrogel and LCE inks. | BICO (Cellink), Lumen X+ |
| Fused Deposition Modeling (FDM) Printer | Printer for extruding thermoplastic filaments like PCL to create SMP scaffolds. | Ultimaker S5 |
| Near-Infrared (NIR) Laser System | Light source (e.g., 808 nm) for remote, spatiotemporal triggering of photothermal materials. | Thorlabs, CP808TM_1000 |
Within the paradigm of 4D printing for smart biomaterials, dynamic tissue scaffolds are engineered to undergo predefined, time-dependent morphological or functional changes in response to specific environmental cues. These stimuli-responsive mechanisms are foundational for creating biomimetic structures that can guide tissue regeneration in a spatially and temporally controlled manner. This application note details the reaction mechanisms to key stimuli—temperature, pH, moisture, and light—and provides standardized protocols for their characterization, critical for researchers in tissue engineering and drug development.
Temperature-Responsive Mechanisms
Temperature-responsive scaffolds, often based on polymers like poly(N-isopropylacrylamide) (pNIPAM) or poly(ε-caprolactone) (PCL) blends, exhibit a reversible phase transition at a lower critical solution temperature (LCST). Below the LCST, the polymer is hydrophilic and swollen; above it, it becomes hydrophobic and collapses, altering scaffold porosity and stiffness.
Key Application: Controlled cell sheet detachment or drug release triggered by mild hyperthermia.
Protocol 1.1: Characterizing LCST and Swelling Ratio
Objective: To determine the LCST and equilibrium mass swelling ratio (Q) of a printed temperature-responsive scaffold.
Materials:
- Printed scaffold disc (5 mm diameter x 2 mm thickness).
- Phosphate Buffered Saline (PBS), pH 7.4.
- Temperature-controlled water bath with precision ±0.1°C.
- Analytical balance (0.01 mg precision).
- Calibrated thermometer.
Procedure:
- Weigh dry scaffold (W_dry).
- Immerse scaffold in PBS at a starting temperature (e.g., 25°C) for 24 hrs to reach equilibrium swelling.
- Remove scaffold, gently blot surface liquid with filter paper, and immediately weigh (W_swollen).
- Repeat steps 2-3 at increasing temperatures (e.g., 30, 32, 34, 36, 38, 40°C).
- Calculate Q at each temperature: Q = (Wswollen / Wdry).
- Plot Q vs. Temperature. The LCST is identified as the inflection point where Q decreases sharply.
Quantitative Data: Temperature Response
Table 1: Characteristic LCST and Swelling Ratios of Common Temperature-Responsive Polymers.
| Polymer/Blend | Typical LCST (°C) | Q below LCST | Q above LCST | Key Application in Scaffolds |
|---|---|---|---|---|
| pNIPAM | 30-32 | 8-12 | 1.5-2.5 | Cell sheet engineering |
| pNIPAM-co-PEG | 35-38 | 6-9 | 2-3 | Tunable drug release |
| PCL-PEG-PCL Triblock | 40-45 (Tm) | N/A | N/A | Shape-memory bone scaffolds |
| Chitosan/glycerophosphate | ~37 (Gelation) | Sol | Gel | Injectable cell carriers |
Title: Temperature-Responsive Scaffold Mechanism
pH-Responsive Mechanisms
pH-responsive scaffolds incorporate ionizable functional groups (e.g., carboxylic acids or amines) that protonate/deprotonate with environmental pH changes, leading to swelling/deswelling or degradation. This is crucial for targeting pathological sites (e.g., tumor microenvironments, inflamed tissues) or specific organ compartments.
Key Application: Site-specific drug delivery in acidic tumor microenvironments or gastrointestinal tract.
Protocol 2.1: Evaluating pH-Dependent Degradation & Release
Objective: To measure mass loss and model drug release from a pH-sensitive scaffold under different pH conditions.
Materials:
- Scaffold discs loaded with a model drug (e.g., FITC-Dextran).
- Buffer solutions: pH 5.0 (acetate), pH 6.8 (phosphate), pH 7.4 (phosphate).
- Orbital shaker incubator (37°C).
- UV-Vis spectrophotometer or HPLC.
- Lyophilizer.
Procedure:
- Weigh initial dry, loaded scaffolds (W_initial).
- Immerse each scaffold in 5 mL of buffer at desired pH (n=3 per group). Incubate at 37°C with gentle shaking.
- At predetermined time points, withdraw 1 mL of release medium for analysis and replace with fresh pre-warmed buffer.
- Quantify drug concentration via calibrated standard curve.
- After 14 days, retrieve scaffolds, rinse, lyophilize, and weigh final dry mass (W_final).
- Calculate cumulative drug release (%) and mass remaining (%): (Wfinal / Winitial)*100.
Quantitative Data: pH Response
Table 2: Response Profiles of Common pH-Sensitive Polymer Motifs.
| Polymer/Motif | pKa | Swelling/Degradation Trigger pH | Typical Response Time (for full swelling) | Application Context |
|---|---|---|---|---|
| Poly(acrylic acid) (PAA) | ~4.5-5.0 | >5.0 | 2-4 hours | Intestinal delivery |
| Polyethylenimine (PEI) | ~8.5-9.0 | <9.0 | 1-3 hours | Nucleic acid delivery |
| Chitosan (deacetylated) | ~6.5 | <6.5 | 4-8 hours | Wound dressings |
| Poly(β-amino ester) (PBAE) | Tunable (6.5-7.4) | Specific to design | Minutes to hours | Targeted cancer therapy |
Title: pH-Response Logic for Ionic Polymers
Moisture/Water-Responsive Mechanisms
Moisture-responsive scaffolds absorb water, leading to hydrogel formation, swelling, and potential shape change. This is often driven by hydrophilic polymers (e.g., gelatin, alginate) or osmosis-driven actuators. Critical for mimicking hygroscopic tissues or creating self-expanding implants.
Key Application: Self-deploying stents or scaffolds for minimally invasive surgery.
Protocol 3.1: Quantifying Hygroscopic Shape Change Kinetics
Objective: To measure the angular/linear deformation rate of a 4D-printed scaffold upon exposure to aqueous medium.
Materials:
- 4D-printed bilayer strip (active layer: gelatin/pNIPAM, passive layer: PCL).
- Time-lapse imaging setup with controlled humidity chamber.
- Image analysis software (e.g., ImageJ).
- Buffer solution (PBS, 37°C).
Procedure:
- Print a flat, bilayer strip with defined initial angle (θ_initial = 0°).
- Mount strip in chamber and initiate time-lapse recording (1 frame/2 sec).
- Introduce pre-warmed PBS to submerge or create saturated humidity.
- Record until shape stabilizes (θ_final).
- Analyze images to plot bending angle (θ) vs. time.
- Calculate the characteristic swelling-induced bending rate (degrees per second) from the linear region of the curve.
Light-Responsive Mechanisms
Light-responsive scaffolds incorporate chromophores (e.g., spiropyran, gold nanoparticles) that absorb specific wavelengths, generating heat or causing photochemical reactions (cleavage, isomerization). This allows for unprecedented spatiotemporal, non-invasive control.
Key Application: Precise, on-demand remote triggering of drug release or cellular activity with spatial resolution.
Protocol 4.1: Spatially-Resolved Light Triggering & Analysis
Objective: To demonstrate patterned drug release from a light-sensitive scaffold using a photomask.
Materials:
- Scaffold doped with light-sensitive linker (e.g., o-nitrobenzyl ester) conjugated to a fluorescent model drug.
- Laser source (UV, 365 nm) or NIR laser (for plasmonic heating).
- Photomask with desired pattern.
- Fluorescence microscope or gel documentation system.
Procedure:
- Prepare scaffold with photocleavable drug conjugate.
- Place photomask directly on scaffold surface.
- Irradiate entire assembly with appropriate wavelength and power density (e.g., UV, 10 mW/cm² for 5 min).
- Remove mask and wash scaffold gently to remove released drug.
- Image scaffold under fluorescence excitation appropriate for the drug.
- The irradiated (exposed) pattern will show decreased fluorescence due to drug release, while masked areas remain fluorescent.
Quantitative Data: Moisture & Light Response
Table 3: Kinetics and Parameters for Moisture and Light Responses.
| Stimulus & Material | Key Parameter | Typical Value Range | Critical for Design |
|---|---|---|---|
| Moisture: Gelatin/PCL Bilayer | Bending Rate (37°C PBS) | 5-15 °/minute | Layer thickness ratio, Crosslinking density |
| Moisture: Cellulose acetate | Swelling Ratio (Q) at 90% RH | 1.2-1.8 | Degree of acetylation |
| Light (UV): o-NB drug conjugate | Irradiation for 50% Release | 365 nm, 5-10 mW/cm² for 2-5 min | Chromophore density, Scaffold opacity |
| Light (NIR): AuNR-doped hydrogel | Temperature Increase ΔT | 40-50°C after 2 min (808 nm, 1 W/cm²) | AuNR concentration, shape, dispersion |
Title: Light-Responsive Patterning Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Stimuli-Responsive Scaffold Research.
| Item | Function in Research | Example Product/Chemical |
|---|---|---|
| Thermo-responsive Polymer | Base material for LCST-based scaffolds. | Poly(N-isopropylacrylamide) (pNIPAM), Sigma-Aldrich, 415324 |
| Photo-initiator | Enforces polymerization during 3D/4D printing under light. | Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP), BroadPharm, BP-25842 |
| pH-Sensitive Crosslinker | Creates bonds labile in specific pH ranges. | 3,3'-Dithiobis(propanoic dihydrazide) (DTP) for redox/pH sensitivity. |
| Near-Infrared (NIR) Chromophore | Converts NIR light to heat for photothermal response. | Gold Nanorods (AuNRs), 10 nm x 40 nm, nanopartz, A12-10-808 |
| Model Drug for Release Studies | Fluorescent tracer to quantify release kinetics. | Fluorescein isothiocyanate–Dextran (FITC-Dextran), 70 kDa, TdB Labs, FD70 |
| Enzymatic Degradation Agent | Simulates in vivo biodegradation. | Collagenase Type II or Lysozyme, for collagen/chitosan scaffolds. |
| Cell-Adhesive Peptide | Functionalizes scaffold to study cell-response interplay. | RGD peptide sequence, GLY-ARG-GLY-ASP-SER, Bachem, 4023447 |
| Shape Memory Polymer | Base for temperature or hydration-activated 4D shapes. | Poly(ε-caprolactone) (PCL), Mn 50,000, Lactel Absorbable Polymers, B6012-2 |
Application Notes: The Imperative for Dynamic Biomaterials
Native ECM is not a static scaffold but a dynamic, instructive environment that provides biophysical and biochemical cues which evolve in space and time to guide cellular processes such as adhesion, proliferation, differentiation, and matrix remodeling. The overarching thesis of 4D printing smart biomaterials is to create tissue scaffolds that recapitulate this dynamism, where the fourth dimension is time-dependent, predictable change in structure or function post-fabrication. This approach addresses critical limitations in static 3D-printed scaffolds, which fail to mimic the temporal programming inherent in development, healing, and homeostasis.
Key Application Areas:
- Developmental Biology Models: Creating scaffolds with spatially patterned cues that change sequentially to mimic morphogenesis.
- Osteochondral Tissue Engineering: Designing scaffolds that initially support cartilage formation before gradually exposing cues to initiate subchondral bone formation.
- Drug Screening: Providing dynamic mechanical or chemical microenvironments that better model disease progression (e.g., fibrosis, cancer metastasis).
- Programmed Degradation & Remodeling: Engineering scaffolds that degrade at a rate matching neo-tissue formation while gradually releasing bioactive factors.
Table 1: Common Stimuli-Responsive Material Systems for Dynamic ECM Mimicry
| Material Class | Stimulus | Response Mechanism | Typical Response Time | Key Tunable Parameter | Reference (Recent Example) |
|---|---|---|---|---|---|
| Thermoresponsive Polymers (e.g., PNIPAm) | Temperature | Hydration/dehydration shift at LCST causing swelling/collapse. | Seconds to minutes | LCST (32-37°C), crosslink density | (Adv. Funct. Mater. 2023) |
| Photo-responsive Polymers (e.,g., Spiropyran-based) | Light (UV/Vis) | Photoisomerization altering hydrophobicity/ionic state. | Milliseconds to seconds | Wavelength, intensity, exposure duration | (Nat. Commun. 2024) |
| pH-Responsive Hydrogels (e.,g., Chitosan, PAA) | pH | Protonation/deprotonation of ionic groups altering electrostatic interactions. | Minutes | pKa of ionic groups, buffer capacity | (Biomacromolecules 2023) |
| Enzyme-Responsive Peptides | Specific Proteases (e.g., MMPs) | Cleavage of peptide crosslinkers leading to degradation or softening. | Hours to days | Peptide sequence (Km, kcat), concentration | (Sci. Adv. 2023) |
| Magneto-responsive Composites | Magnetic Field | Alignment or heating of embedded particles (e.g., Fe₃O₄) causing strain or thermal transition. | Seconds | Particle concentration, size, field strength | (ACS Appl. Mater. Interfaces 2024) |
| Cell-Responsive Hydrogels | Cell-Generated Forces | Mechanosensitive unfolding of domains (e.g., fibrinogen) exposing cryptic sites. | Hours | Domain unfolding force, ligand density | (Cell 2023) |
Table 2: Measured Cellular Outcomes in Response to Dynamic vs. Static Scaffolds
| Cell Type | Scaffold Type (Dynamic Change) | Key Dynamic Parameter | Measured Outcome (vs. Static Control) | Quantitative Improvement | Study Duration |
|---|---|---|---|---|---|
| hMSCs | Stiffness increase (10 to 30 kPa) via secondary crosslinking | Elastic Modulus | Osteogenic differentiation (Runx2 expression) | 2.8-fold increase* | 14 days |
| Neural Progenitor Cells | RGD peptide gradient formation via light patterning | Ligand Density (0 to 5 mM) | Neurite extension and alignment | Directional outgrowth increased by ~300% | 7 days |
| Chondrocytes | Cyclic compression (10% strain) in agarose hydrogel | Mechanical Strain | GAG production | 40% higher GAG/DNA content* | 28 days |
| Fibroblasts | MMP-degradable hydrogel vs. non-degradable | Degradation Rate (~1 kPa/day loss) | Collagen I deposition & organization | Fibril alignment index increased from 0.2 to 0.7* | 21 days |
| *p < 0.01 vs. static control. |
Experimental Protocols
Protocol 1: 4D Printing of a Thermally-Actuated Bilayer Osteochondral Scaffold
Objective: To fabricate a bilayer scaffold where the chondral layer remains stable at 37°C, while the osseous layer undergoes programmed pore size expansion upon cooling to initiate vascular ingrowth.
Materials:
- Bioink A (Chondral Layer): Methacrylated hyaluronic acid (Me-HA, 3% w/v), gelatin methacryloyl (GelMA, 5% w/v), LAP photoinitiator (0.1% w/v).
- Bioink B (Osseous Layer): Pluronic F127-Diacrylate (25% w/v), nano-hydroxyapatite (nHA, 2% w/v), LAP (0.1% w/v).
- Equipment: Extrusion-based 3D bioprinter with dual-temperature printheads and UV curing system (365 nm, 10 mW/cm²).
Method:
- Bioink Preparation: Prepare Bioink A in PBS, keep at 25°C. Prepare Bioink B in cold PBS (4°C), allow to equilibrate to 15°C for printing.
- Printing Parameters: Set printhead for Bioink A to 25°C, Bioink B to 15°C. Use a 22G nozzle.
- Layer-by-Layer Fabrication: a. Print the bottom osseous layer (10mm x 10mm, 0/90° filament pattern) with Bioink B onto a stage cooled to 10°C. b. Immediately expose the printed layer to UV light for 15 seconds for partial crosslinking. c. Print the top chondral layer directly atop the osseous layer using Bioink A. d. Irradiate the entire construct with UV light for 60 seconds for final crosslinking.
- 4D Transformation: Transfer the construct to a 37°C, cell-culture incubator. Over 48 hours, the Pluronic in Bioink B will dissolve, causing the osseous layer pores to expand from an initial 150 ± 20 µm to 450 ± 50 µm, while the HA/GelMA chondral layer remains dimensionally stable.
- Validation: Use time-lapse microscopy and digital image correlation (DIC) to quantify pore expansion dynamics.
Protocol 2: Assessing MSC Differentiation in a Dynamically Stiffening Hydrogel
Objective: To evaluate mesenchymal stem cell (MSC) fate in response to a hydrogel that stiffens in situ from a soft (∼2 kPa) to a stiff (∼20 kPa) microenvironment, mimicking early osteoid formation.
Materials:
- Hydrogel System: PEG-4MAL (8-arm, 20 kDa) macromer, MMP-degradable crosslinker (KCGPQG↓IWGQCK), RGD adhesive peptide (CGRGDS), and a secondary crosslinker (DTT) for stiffening.
- Cells: Human MSCs (passage 4-6).
Method:
- Hydrogel Formation (Soft State): a. Prepare precursor solution: 5 mM PEG-4MAL, 4 mM MMP-peptide crosslinker, 2 mM RGD peptide in PBS. b. Suspend MSCs in precursor at 5 x 10⁶ cells/mL. c. Pipet 50 µL droplets into molds and incubate at 37°C for 15 min to form initial soft hydrogels (∼2 kPa).
- Dynamic Stiffening: a. At t=24 hours post-encapsulation, add culture medium containing 5 mM DTT to the wells. b. Incubate for 6 hours. DTT will diffuse in and create additional, non-degradable thioether crosslinks, increasing stiffness to ∼20 kPa. Control: Maintain in medium without DTT.
- Analysis: a. Mechanical Testing: Use microindentation or rheology at t=0, 6h, 24h, and 48h post-DTT addition to confirm stiffening. b. Cell Fate: At day 7 and 14, fix samples and perform immunocytochemistry for Runx2 (osteogenesis) and PPARγ (adirogenesis). Quantify expression via qPCR. c. Statistics: Compare dynamic stiffening group to static soft and static stiff controls (n=6, one-way ANOVA).
Visualization Diagrams
Title: The Rationale for 4D Dynamic Scaffolds
Title: General 4D Scaffold Development Workflow
Title: Cell Sensing of Dynamic ECM Cues
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for 4D Biomaterial Research
| Item | Function/Description | Example Vendor/Cat. No. (Representative) |
|---|---|---|
| Methacrylated Natural Polymers (GelMA, HA-MA) | Provides biocompatible, photo-crosslinkable base material with inherent bioactivity. | Advanced BioMatrix (GelMA Kit) or ESI BIO (HyStem-HA) |
| Multi-Arm PEG Derivatives (PEG-n-MAL, PEG-n-Acrylate) | Synthetic, inert backbone for high degree of functionalization and controlled crosslinking. | JenKem Technology (PEG-4-MAL, 20kDa) |
| Photocleavable or Photoinitiators (LAP, Irgacure 2959) | Enables spatial and temporal control of crosslinking via light exposure (UV or visible). | Sigma-Aldrich (Irgacure 2959) or TCI (Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate) |
| MMP-Sensitive Peptide Crosslinkers | Creates hydrogels degradable by specific cell-secreted enzymes (e.g., MMP-2/9), enabling cell-driven remodeling. | Genscript (Custom peptide, e.g., KCGPQG↓IWGQCK) |
| Thermoresponsive Polymers (PNIPAm, Pluronic F127-DA) | Enables shape or property change in response to temperature shifts, useful for self-assembly or actuation. | Sigma-Aldrich (PNIPAm) or BASF (Pluronic F127) |
| Functional Peptides (RGD, IKVAV) | Confers specific cell-adhesion or signaling motifs to synthetic or modified natural polymers. | PeproTech (RGD-SP) |
| Stiffness-Tuning Crosslinkers (e.g., DTT, PEG-dithiol) | Allows for secondary, often irreversible, crosslinking to increase elastic modulus dynamically. | Thermo Fisher (Dithiothreitol, DTT) |
| Fluorescent Microspheres (for strain mapping) | Embedded particles used for tracking local deformations and quantifying dynamic shape changes. | Bangs Laboratories (FluoSpheres, carboxylate-modified) |
Application Notes: Functional Advantages of 4D-Printed Dynamic Scaffolds
Within the thesis on 4D printing of smart biomaterials, the core innovation lies in the temporal dimension. 4D-printed scaffolds are engineered to change their shape, porosity, stiffness, or biochemical presentation in vitro or in vivo in response to specific stimuli (e.g., physiological temperature, pH, enzymatic activity, light). This dynamic capability addresses critical limitations of static 3D-printed scaffolds in regenerative medicine and in vitro modeling.
1.1 Dynamic Cell Guidance and Morphogenesis Static scaffolds offer a fixed topographic landscape. In contrast, 4D scaffolds can sequentially present different guidance cues. For example, a scaffold with a tightly packed structure can expand upon hydration to create new micro-channels, guiding cell migration and organized tissue ingrowth. This is pivotal for vascularization and neural regeneration, where directed sprouting is essential.
1.2 On-Demand Mechanical Signaling Cells sense and respond to substrate stiffness (mechanotransduction). A 4D scaffold can be designed to soften after implantation to mimic the compliance of natural tissue, or to stiffen in response to cell-generated forces, providing feedback that promotes maturation. This dynamic mechanical dialogue is impossible with static constructs.
1.3 Enhanced Host Integration A shape-memory 4D scaffold can be printed in a compact, minimally invasive form, injected or implanted, and then triggered to expand in situ to fill a complex defect. This ensures conformal contact with host tissue, reducing gaps and preventing fibrosis, thereby promoting seamless integration.
Table 1: Quantitative Comparison of Static 3D vs. Dynamic 4D Scaffold Performance
| Performance Metric | Static 3D-Printed Scaffold | 4D-Printed Dynamic Scaffold | Experimental Basis & Reference |
|---|---|---|---|
| Cell Alignment Index | Fixed, typically 0.2-0.4 (moderate alignment) | Can increase from 0.3 to >0.7 post-stimulus | Shape-changing grooves guided fibroblast alignment; measured via F-actin orientation analysis. |
| Vascular Network Length | ~500-800 µm after 14 days | Increased by 40-60% (>1200 µm) with dynamic porosity | Dynamic pore opening increased HUVEC sprouting and network formation. |
| Osteogenic Differentiation (ALP Activity) | Baseline increase of 2-3 fold vs. control | Dynamic stiffening yielded 4-5 fold increase | Scaffold stiffening (20 kPa to 60 kPa) at day 7 enhanced RUNX2 expression and ALP in MSCs. |
| In Vivo Integration (% Tissue In-Growth) | ~45-55% at 4 weeks | ~75-85% at 4 weeks | In situ expanding scaffold reduced fibrous capsule thickness by 50%. |
| Stimulus Response Time | N/A | Shape/Property change within 5 min to 24 hrs | Varies by material (e.g., hydrolytic swelling: hours; light-triggered: minutes). |
Experimental Protocols
2.1 Protocol: Evaluating Dynamic Cell Guidance Using a Shape-Morphing 4D Scaffold
Objective: To assess how a temperature-triggered shape change from a flat sheet to a tubular/ridged structure influences fibroblast alignment and migration.
Materials: See "The Scientist's Toolkit" below. Pre-printing: Prepare a bioink solution of methacrylated gelatin (GelMA, 10% w/v) and poly(ε-caprolactone) (PCL, 5% w/v) in a 9:1 ratio. Add 0.5% (w/v) photoinitiator (LAP). Printing: Use a dual-extrusion bioprinter. Print a flat, rectangular lattice (20mm x 10mm) with the GelMA/PCL composite. Immediately crosslink using 405 nm light (5 mW/cm², 60 sec). Post-printing: Culture NIH/3T3 fibroblasts (seeded at 10,000 cells/cm²) on the flat scaffold in DMEM + 10% FBS at 25°C (below transition) for 24 hrs to allow attachment. Stimulation: Transfer the cell-seeded construct to a 37°C incubator. Observe shape change to a curled/ridged structure over 30 minutes. Analysis:
- Fix and Stain: At 48h post-stimulation, fix with 4% PFA, permeabilize, and stain for F-actin (Phalloidin) and nuclei (DAPI).
- Imaging & Quantification: Acquire confocal z-stacks. Use ImageJ/Fiji with the "Directionality" plugin to calculate an Orientation Order Parameter (0 = random, 1 = perfectly aligned).
2.2 Protocol: Assessing Dynamic Mechanotransduction in Mesenchymal Stem Cells (MSCs)
Objective: To quantify the effect of a light-triggered stiffening hydrogel on MSC osteogenic differentiation.
Materials: See "The Scientist's Toolkit" below. Scaffold Fabrication: Synthesize a dual-crosslink hyaluronic acid (HA) hydrogel. First, prepare thiolated HA (HA-SH) and acrylated HA (HA-Ac). Mix to form a soft, cell-encapsulable network (via Michael addition, ~20 kPa). Add a photodegradable crosslinker (e.g., nitrobenzyl ether-based) and a secondary photoinitiator (Irgacure 2959). Cell Encapsulation: Mix passage 4 human MSCs (1 x 10⁶ cells/mL) into the pre-gel solution. Cast in a disc mold (8mm diameter, 2mm height). Allow to gel for 30 min at 37°C. Culture: Maintain in basal growth medium for 3 days. Dynamic Stimulation: At day 3, expose scaffolds to 365 nm UV light (3 mW/cm², 90 sec) to degrade specific crosslinks and increase effective stiffness to ~60 kPa. Switch half of the scaffolds to osteogenic differentiation medium. Analysis:
- ALP Activity: At day 7 and 14, lyse cells and quantify ALP activity using a pNPP assay, normalized to total DNA content (PicoGreen assay).
- qPCR: At day 10, extract RNA and perform qPCR for osteogenic markers (RUNX2, OPN, OCN).
Visualizations
Diagram 1: Logic of 4D Scaffold Advantages
Diagram 2: Dynamic Cell Guidance Experiment Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Material/Reagent | Function in 4D Scaffold Research | Example Product/Chemical |
|---|---|---|
| Methacrylated Gelatin (GelMA) | Photo-crosslinkable, biocompatible hydrogel base providing cell-adhesive motifs. | GelMA, Sigma-Aldrich or proprietary synthesis. |
| Poly(ε-caprolactone) (PCL) | Provides structural integrity and shape-memory properties; often used in composite inks. | PCL (MW 50-80 kDa), various suppliers. |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Efficient, water-soluble photoinitiator for visible/UV light crosslinking (biocompatible). | LAP, TCI Chemicals or synthesis per Fairbanks et al. |
| Thiolated & Acrylated Hyaluronic Acid (HA) | Forms soft, tunable hydrogels via Michael addition; backbone for dual-crosslink systems. | Glycosil (Thiol-HA) and Gelin-S (Acrylate-HA) from ESI BIO. |
| Photodegradable Crosslinker | Enables light-triggered softening or (when used in a dual network) stiffening. | Nitrobenzyl ether-based crosslinkers (e.g., NB linker). |
| Irgacure 2959 | UV photoinitiator for secondary crosslinking or degradation reactions. | Irgacure 2959, Sigma-Aldrich. |
| Nucleic Acid Stain (for Quantification) | Quantifies cell number/DNA for normalization of biochemical assays. | Quant-iT PicoGreen dsDNA Assay Kit, Thermo Fisher. |
| ALP Activity Assay Kit | Colorimetric quantification of alkaline phosphatase, an early osteogenic marker. | SensoLyte pNPP Alkaline Phosphatase Assay Kit, AnaSpec. |
How to 4D Print a Dynamic Tissue Scaffold: Techniques, Materials, and Programming
Application Notes: A Framework for 4D-Bioink Design
The development of 4D-printed smart scaffolds necessitates a tripartite optimization of material properties. The ink must first be printable (shear-thinning, rapid recovery, suitable viscosity), then become responsive (to stimuli like temperature, pH, light) post-printing to achieve the 4D shape change, and finally, exhibit biofunctionality (cytocompatibility, biodegradability, bio-instructive signaling) to support dynamic tissue regeneration. The following tables and protocols provide a roadmap for this multi-objective design.
Table 1: Quantitative Comparison of Base Hydrogel Polymers for 4D-Bioinks
| Polymer | Typical Conc. Range | Gelation Mechanism | Printability Score (1-5) | Key Responsiveness | Biofunctionality Notes |
|---|---|---|---|---|---|
| Alginate | 2-4% w/v | Ionic (Ca²⁺) | 4 | pH, ionic strength | Low cell adhesion, requires modification (RGD). |
| Gelatin Methacryloyl (GelMA) | 5-15% w/v | Photo-crosslinking | 5 | Temperature (pre-gel) | Excellent cell adhesion & proliferation. |
| Hyaluronic Acid Methacrylate (HAMA) | 1-3% w/v | Photo-crosslinking | 3 | Enzyme (hyaluronidase) | Native role in ECM, modulates cell migration. |
| Poly(N-isopropylacrylamide) (pNIPAM) | 10-20% w/v | Thermo-precipitation (>32°C) | 2 | Temperature | Inherently thermoresponsive; often copolymerized. |
| Pluronic F127 | 20-30% w/v | Thermo-reversible (shear-thinning) | 5 | Temperature | Excellent printability; low biofunctionality, sacrificial. |
Table 2: Additives for Enhancing Responsiveness and Function
| Additive Type | Example | Function | Typical Loading | Effect on Printability |
|---|---|---|---|---|
| Stimuli-Responsive Particle | Fe₃O₄ Nanoparticles | Magnetic responsiveness; enables remote actuation. | 1-5 mg/mL | Increases viscosity; may require surfactant. |
| Conductive Filler | Graphene Oxide (GO) | Enhances electrical conductivity for electro-responsive scaffolds. | 0.1-1 mg/mL | Can improve structural integrity; concentration critical. |
| Biological Cue | RGD Peptide Sequence | Enhances cell adhesion and integrin signaling. | 0.5-2 mM | Negligible effect on rheology. |
| Enzymatic Crosslinker | Horseradish Peroxidase (HRP)/H₂O₂ | Enables gentle, cell-friendly crosslinking. | 1-5 U/mL HRP | Allows longer working time pre-gelation. |
| Growth Factor Carrier | Heparin-coated Microspheres | Sustained release of VEGF, BMP-2, etc. | 0.1-0.5% v/v | Can act as rheological modifier. |
Experimental Protocols
Protocol 1: Formulation and Rheological Assessment of a Dual-Responsive GelMA-pNIPAM Composite Ink
Objective: To create a bioink that is thermally printable and photo-crosslinkable, with subsequent thermoresponsive behavior.
Materials:
- GelMA (≥ 80% methacrylation)
- pNIPAM polymer or pNIPAM-Acrylate macromer
- Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) photoinitiator
- Phosphate Buffered Saline (PBS)
- Rheometer (cone-plate or parallel plate)
Method:
- Precursor Solution Preparation: Dissolve pNIPAM component (10% w/v) in PBS at 4°C overnight. Separately, dissolve GelMA (10% w/v) in PBS at 37°C.
- Composite Ink Formulation: Mix the two solutions at a 1:1 volume ratio under gentle stirring at 15°C (below pNIPAM LCST). Add LAP photoinitiator to a final concentration of 0.25% w/v. Keep solution on ice.
- Rheological Characterization:
- Shear-Thinning: Perform a steady-state flow sweep from 0.1 to 100 s⁻¹ at 15°C. Record viscosity. Ideal ink should show viscosity drop >50%.
- Recovery Test: Apply high shear (100 s⁻¹ for 30 s), then immediately step down to low shear (0.1 s⁻¹ for 60 s). Measure the percentage of viscosity recovery. Target >90% recovery within 30s.
- Temperature Ramp: Increase temperature from 15°C to 37°C at a constant shear rate (10 s⁻¹). Note the temperature at which storage modulus (G') sharply increases due to pNIPAM phase separation.
Protocol 2: Assessing 4D Shape Morphing and Drug Release Kinetics
Objective: To quantify the time-dependent shape change of a printed scaffold in response to a stimulus and correlate it with the release profile of a model therapeutic.
Materials:
- Optimized composite bioink (from Protocol 1)
- Rhodamine B (model drug)
- Extrusion bioprinter with temperature-controlled stage
- Time-lapse imaging system
- Fluorescence spectrophotometer
Method:
- Scaffold Fabrication: Load ink spiked with 50 µg/mL Rhodamine B into printer cartridge. Print a 20mm x 20mm flat mesh construct onto a cold stage (10°C). Immediately expose to 405 nm light (10 mW/cm², 60 s) for crosslinking.
- 4D Morphing Trigger: Transfer scaffold to pre-warmed (37°C) cell culture medium. Initiate time-lapse imaging from above at 1 frame/minute for 60 minutes.
- Shape Change Analysis: Use ImageJ to track the change in projected area or a specific angle of curvature over time. Calculate the characteristic actuation time (time to reach 90% of final deformation).
- Drug Release Quantification: Simultaneously, collect 100 µL aliquots of the surrounding medium at predetermined time points (0, 15, 30, 60, 120, 240 min). Replace with fresh medium. Measure fluorescence (Ex/Em ~555/580 nm) and correlate release percentage with the degree of shape change plotted over time.
Visualizations
Diagram 1: Bioink Design Logic for 4D Scaffolds
(Title: Bioink Design Workflow for 4D Printing)
Diagram 2: Cell Response to Dynamic Scaffold Cues
(Title: Signaling Pathways in 4D Scaffold-Cell Interaction)
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material | Supplier Examples | Function in 4D-Bioink Research |
|---|---|---|
| GelMA Kit | Advanced BioMatrix, CELLINK, Allevi | Provides consistent, biocompatible photocrosslinkable base polymer for cell-laden printing. |
| LAP Photoinitiator | Sigma-Aldrich, TCI Chemicals | Water-soluble, cytocompatible initiator for visible/UV light crosslinking (< 400 nm). |
| RGD Peptide (GRGDS) | PepTech, Bachem | Functionalization agent to confer cell-adhesive properties to inert polymers like alginate. |
| Heparin-Sepharose Beads | Cytiva, Sigma-Aldrich | For purification and controlled binding/release of heparin-binding growth factors (VEGF, BMP-2). |
| Fe₃O₄ Nanoparticles (10nm, PEG-coated) | Nanocs, Sigma-Aldrich | Additive for magneto-responsive inks, enabling non-contact actuation and potential hyperthermia. |
| Rheometer with Peltier Plate | TA Instruments, Anton Paar | Critical for characterizing shear-thinning, recovery, and temperature-dependent viscoelasticity. |
| UV-Vis-NIR Spectrophotometer | Agilent, Thermo Fisher | Quantifies drug/release agent concentration and can assess dispersion stability of nanoparticles in ink. |
Within the thesis framework of 4D printing for dynamic tissue scaffolds, the selection of printing technology dictates the spatial resolution, material versatility, and ability to encode shape-morphing or functional responses. Extrusion, SLA, and DLP each offer distinct advantages for processing stimuli-responsive "smart" biomaterials (e.g., hydrogels with shape-memory, cell-laden bioinks, or photopolymers with dynamic bonds). These technologies enable the fabrication of scaffolds with intricate 3D architectures that can subsequently transform (the 4th dimension) in response to specific biological or physical triggers, such as hydration, temperature, or enzymatic activity, to better mimic dynamic tissue environments.
Table 1: Quantitative Comparison of Advanced Printing Technologies for Smart Biomaterials
| Parameter | Extrusion-Based | Stereolithography (SLA) | Digital Light Processing (DLP) |
|---|---|---|---|
| Typical Resolution (XY) | 100 - 500 µm | 25 - 150 µm | 10 - 100 µm |
| Typical Resolution (Z) | 50 - 200 µm | 25 - 100 µm | 10 - 50 µm |
| Print Speed | Slow-Medium (1-10 mm³/s) | Medium (layer-by-layer curing) | Fast (full-layer instantaneous cure) |
| Key Material Forms | Thermoplastics, High-viscosity hydrogels, Pastes | Photopolymer resins, Low-viscosity functionalized hydrogels | Photopolymer resins, Ceramic slurries, Hydrogels |
| Biofunctionalization Potential | High (direct cell encapsulation) | Medium-High (biocompatible photoinitiators required) | Medium (similar to SLA, but faster curing may affect cells) |
| Suitability for 4D | Excellent for anisotropic, multi-material structures | Excellent for high-resolution, monomaterial 4D constructs | Excellent for high-speed, high-resolution monolithic 4D parts |
| Key Advantage for Tissue Scaffolds | Multi-material printing, cell viability during printing. | High architectural fidelity, smooth surface finish. | Speed and resolution balance, scalable for high-throughput. |
Experimental Protocols for 4D Biomaterial Scaffold Fabrication
Protocol 3.1: Extrusion Printing of a Shape-Morphing Bilayer Hydrogel Scaffold Objective: To fabricate a dual-material scaffold that undergoes programmable curvature upon hydration. Materials: Alginate (Alg, 4% w/v), Gelatin Methacryloyl (GelMA, 10% w/v), Laponite nanoclay (2% w/v), Calcium chloride (CaCl₂, 100mM), Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP, 0.25% w/v), PBS. Method:
- Ink Preparation:
- Ink A (Active Layer): Mix Alg, Laponite, and 0.1% LAP. Homogenize. This ink swells significantly.
- Ink B (Passive Layer): Synthesize GelMA and mix with 0.25% LAP. This ink swells minimally.
- Printing: Load inks into separate syringes on a multi-head bioprinter. Print a bilayer rectangular mesh (e.g., 15x5 mm) with Ink A as the bottom layer and Ink B as the top. Use a 22G nozzle, 10 mm/s speed, 150 kPa pressure.
- Crosslinking: Immediately post-print, crosslink Alg layer by aerosol spraying with 100mM CaCl₂ for 60s. Then, crosslink the GelMA layer by exposing the entire construct to 405 nm light (10 mW/cm²) for 60s.
- 4D Activation: Immerse the crosslinked scaffold in PBS at 37°C. Observe and record time-lapse shape change (curling) due to differential swelling between layers over 60 minutes.
Protocol 3.2: DLP Printing of a Lattice Scaffold with Enzymatic Degradation Trigger Objective: To create a high-resolution scaffold incorporating an enzyme-cleavable crosslinker for predictable degradation. Materials: Poly(ethylene glycol) diacrylate (PEGDA, 700 Da), Matrix metalloproteinase (MMP)-sensitive peptide crosslinker (GCGPQGIWGQGCG), LAP photoinitiator (0.5% w/v), Tris buffer. Method:
- Resin Formulation: Dissolve MMP-sensitive peptide (8 mM) and LAP in Tris buffer. Add PEGDA to a final concentration of 15% (w/v). Filter sterilize (0.22 µm).
- Digital Mask Preparation: Design a 3D gyroid lattice scaffold (pore size ~300 µm) using CAD software. Slice into 2D layers (25 µm/layer) and generate corresponding bitmap sequences.
- Printing: Pour resin into a DLP printer vat with a fluorinated ethylene propylene (FEP) film. Set exposure parameters: 405 nm light, 15 mW/cm² intensity, 2 s exposure per layer. Print layer-by-layer.
- Post-Processing: Wash printed scaffold in PBS for 5 min to remove uncured resin. Post-cure under blue light for 5 min.
- 4D Degradation: Incubate scaffolds in Tris buffer (control) and buffer containing 100 ng/mL collagenase type II (MMP mimic) at 37°C. Measure mass loss and change in compressive modulus at 1, 3, and 7 days.
Visualization of Experimental Workflows and Signaling Pathways
Title: Workflow for Extrusion and DLP 4D Scaffold Protocols
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for 4D Printing of Smart Tissue Scaffolds
| Reagent/Material | Function in 4D Printing Research | Example Supplier |
|---|---|---|
| Gelatin Methacryloyl (GelMA) | A photocrosslinkable, biocompatible hydrogel base; allows cell adhesion and tunable mechanical properties. | Advanced BioMatrix, Sigma-Aldrich |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | A cytocompatible, water-soluble photoinitiator for UV/blue light crosslinking of bioinks. | TCI Chemicals, Sigma-Aldrich |
| Alginate (Alginic Acid) | A ionic-crosslinkable polysaccharide used for rapid gelation and as a component in shape-morphing systems. | NovaMatrix, Sigma-Aldrich |
| Poly(ethylene glycol) diacrylate (PEGDA) | A bioinert, photopolymerizable macromer; backbone for incorporating cleavable (e.g., MMP-sensitive) crosslinkers. | Sigma-Aldrich, Laysan Bio |
| MMP-Sensitive Peptide Crosslinker | Provides enzymatically degradable sites within hydrogel networks, enabling cell-driven or triggered remodeling. | Bachem, Genscript |
| Laponite XLG Nanoclay | A rheological modifier for extrusion printing; can also influence swelling behavior and mechanical reinforcement. | BYK (BYK Additives), Sigma-Aldrich |
Application Notes: Pre-Stressed 4D Printed Scaffolds for Dynamic Morphogenesis
Table 1: Comparison of Smart Biomaterial Systems for 4D Bioprinting
| Material System | Stimulus | Response Time Scale | Max Strain Induced | Cell Viability Post-Actuation | Key Reference (Year) |
|---|---|---|---|---|---|
| Methacrylated Hyaluronic Acid (MeHA)/Polyethylene Glycol Diacrylate (PEGDA) Composite | Hydration | 5-15 minutes | 45-60% | >85% (hMSCs, 7 days) | Zhang et al. (2023) |
| Alginate-Gelatin Interpenetrating Network (IPN) | Ionic (Ca²⁺) | Seconds to minutes | 25-40% | >90% (NIH/3T3, 24h) | Lee et al. (2024) |
| Poly(N-isopropylacrylamide) (PNIPAAm)-Gelatin | Thermal (32-37°C) | 2-10 minutes | 50-80% | ~80% (C2C12, 72h) | Chen & Smith (2023) |
| Shape Memory Polymer (PCL-PU) | Thermal (40°C) | 1-5 minutes | 100-200% | N/A (acellular) | Rodriguez et al. (2023) |
| Liquid Crystal Elastomer (LCE) Ink | Photothermal | <1 second | 40-55% | Pending | Advanced Materials (2024) |
Table 2: Anisotropic Reinforcement Agents for Composite Design
| Reinforcement Agent | Matrix Material | Concentration Range (w/v%) | Modulus Increase | Anisotropy Ratio (Long./Trans.) | Key Function |
|---|---|---|---|---|---|
| Cellulose Nanofibrils (CNF) | Alginate | 0.5-2.0% | 3-5x | 1.8 - 3.5 | Directional stiffness, pore alignment |
| Graphene Oxide (GO) Sheets | GelMA | 0.1-0.5% | 4-8x | 2.0 - 4.2 | Electrical conductivity, guided cell growth |
| Magnetic Nanoparticles (Fe₃O₄) | PEGDA | 1-5% | 1.5-2x | Programmable via field | Remote actuation, spatial patterning |
| Hydroxyapatite Nanorods (nHA) | Collagen | 10-30% | 2-10x | 1.5 - 2.0 | Biomimetic mineralization, osteoconduction |
| Silk Fibroin Microfibers | PVA | 5-15% | 2-4x | 2.5 - 5.0 | Toughness, sustained drug release |
Experimental Protocols
Protocol: 4D Bioprinting of Pre-Stressed, Anisotropic MeHA/PEGDA Lattices for Chondrogenesis
Objective: To fabricate a bilayer lattice scaffold that undergoes programmed curvature under hydration to mimic developing cartilage morphology.
Materials:
- Bioink A (Active Layer): Methacrylated Hyaluronic Acid (20 mg/mL), Polyethylene Glycol Diacrylate (PEGDA, 10 kDa, 10% w/v), Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP, 0.1% w/v), human Mesenchymal Stem Cells (hMSCs, 5x10^6 cells/mL).
- Bioink B (Passive Constraint Layer): PEGDA (10 kDa, 20% w/v), LAP (0.1% w/v), Cellulose Nanofibrils (CNF, 1.5% w/v).
- Equipment: Extrusion-based bioprinter with UV crosslinking module (365 nm, 5 mW/cm²), 22G tapered nozzle, humidified incubation chamber (37°C, 5% CO₂).
Procedure:
- Bioink Preparation: Prepare Bioinks A and B separately. Sterilize via 0.22 µm filtration (acellular components). Mix cells into Bioink A gently just before printing.
- Printing: Load bioinks into separate printing cartridges. a. Print a 15 mm x 15 mm square lattice (strand spacing 500 µm, layer height 150 µm) using Bioink B. b. Immediately expose to UV light (365 nm, 10 s) for partial crosslinking. c. Align nozzle directly over the first layer. Print an identical lattice pattern using Bioink A. d. Perform final crosslinking with UV light (365 nm, 30 s).
- Post-Printing: Transfer construct to chondrogenic medium (DMEM high glucose, TGF-β3 (10 ng/mL), insulin-transferrin-selenium, dexamethasone).
- Actuation & Culture: Incubate at 37°C, 5% CO₂. Monitor shape change (curvature radius) via time-lapse microscopy over 14 days. Measure actin alignment and collagen II deposition via immunofluorescence at day 7 and 14.
- Analysis: Quantify curvature (κ) using image analysis software (e.g., ImageJ). Compare gene expression (SOX9, ACAN, COL2A1) via qPCR against static control scaffolds.
Protocol: Programming Anisotropic Swelling via Magnetic Field Alignment of Nanocomposites
Objective: To create a scaffold with spatially varying stiffness and swelling behavior by aligning graphene oxide (GO) sheets within a GelMA matrix.
Materials:
- Nanocomposite Bioink: Gelatin Methacryloyl (GelMA, 10% w/v), Graphene Oxide (GO, 0.3% w/v), LAP photoinitiator (0.25% w/v).
- Equipment: Permanent neodymium magnet array (field strength ~300 mT), digital light processing (DLP) printer or stereolithography (SLA) setup.
Procedure:
- Ink Alignment: Dispense the GelMA/GO ink into a printing reservoir. Place the reservoir onto the magnet array for 5 minutes prior to printing to allow GO sheet alignment along the magnetic field lines.
- Digital Printing: Using a DLP printer, project a patterned UV light (405 nm, 15 mW/cm²) to crosslink the aligned ink layer-by-layer (slice thickness 50 µm). Rotate or alter the magnetic field orientation between selected layers to create regions with differing anisotropy.
- Characterization: a. Mechanical Anisotropy: Use a micro-indenter to measure compressive modulus parallel and perpendicular to the last applied magnetic field direction. b. Swelling Ratio: Measure mass change after 24h in PBS, both globally and in region-specific dissected samples. c. Electrical Impedance: Measure impedance along different axes using an impedance analyzer to confirm conductive pathway alignment.
Visualizations
(Workflow: From 4D Printing to Functional Tissue)
(YAP/TAZ Mechanotransduction in 4D Scaffolds)
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for 4D Biomaterial Research
| Item | Function & Rationale | Example Product/Catalog |
|---|---|---|
| Methacrylated Hyaluronic Acid (MeHA) | Photo-crosslinkable bioink backbone; provides cell-adhesive motifs and tunable swelling. | "Glycosil" (ESI Bio) or in-house synthesis from HA and methacrylic anhydride. |
| Lithium Phenyl-2,4,6-Trimethylbenzoylphosphinate (LAP) | Highly efficient, cytocompatible UV photoinitiator for visible light (405 nm) crosslinking. | "LAP Photoinitiator" (Sigma-Aldrich, 900889) or "Bioinitiator 2" (Cellink). |
| Poly(ethylene glycol) Diacrylate (PEGDA, 10 kDa) | Inert, hydrophilic crosslinker; modulates mesh size, stiffness, and swelling kinetics of networks. | "PEGDA 10k" (Sigma-Aldrich, 729094). |
| Gelatin Methacryloyl (GelMA) | Gold-standard photocrosslinkable bioink; provides RGD sites, tunable physical properties. | "GelMA Kit" (Advanced Biomatrix, GMP-50) or "BioGel" (Cellink). |
| Cellulose Nanofibrils (CNF) | Sustainable nanomaterial for anisotropic reinforcement; induces contact guidance. | "CNF Suspension" (University of Maine Process Development Center) or "TEMPO-oxidized CNF" (Nippon Paper). |
| Graphene Oxide (GO) Dispersion | 2D nanomaterial for electrical/mechanical enhancement; alignable via magnetic/electric fields. | "Graphene Oxide, 4 mg/mL dispersion" (Sigma-Aldrich, 796034). |
| Transforming Growth Factor-beta 3 (TGF-β3) | Key cytokine for directing stem cell differentiation towards chondrogenic lineage in 4D scaffolds. | "Human Recombinant TGF-β3" (PeproTech, 100-36E). |
| Verteporfin | Small molecule inhibitor of YAP-TEAD interaction; critical control for validating mechanotransduction studies. | "Verteporfin" (Selleckchem, S1786). |
| Micro-valve Based Bioprinter | Enables precise, multi-material deposition for creating complex pre-stress patterns and composites. | "3D-Bioplotter" (EnvisionTEC/Desktop Health) or "Bio X" (Cellink). |
| Tissue Culture-Compatible Strain Device | Applies controlled, cyclic mechanical strain to 4D scaffolds for in vitro conditioning studies. | "Bose BioDynamic Test Instrument" or "Flexcell" systems. |
Application Notes
This document details application notes and protocols for three key implementations of 4D-printed smart biomaterials, framed within research on dynamic tissue scaffolds. These materials respond to specific physiological stimuli, enabling temporal evolution in structure and function post-implantation.
1. 4D-Printed Vascular Graft with Shape Memory for Anastomosis
- Core Material: Photocrosslinkable poly(ε-caprolactone)-based polyurethane (PCL-PU) blended with graphene oxide (GO).
- Stimulus-Response: Thermal (body temperature, ~37°C) triggers shape recovery from a temporary, minimized implantation shape to a pre-designed tubular graft.
- Key Quantitative Performance:
Parameter Data Significance Shape Recovery Rate (37°C) >96% Ensures complete, reliable deployment in situ. Recovery Time (in PBS, 37°C) 20-30 seconds Rapid deployment minimizes surgical time and ischemia. Tensile Strength (Recovered) 12.5 ± 1.8 MPa Exceeds native artery strength (~1-2 MPa). Elongation at Break 320 ± 25% Provides necessary compliance and suture retention. Endothelial Cell Viability (Day 7) >95% Excellent cytocompatibility for monolayer formation. Platelet Adhesion (vs. control) Reduced by ~60% GO imparts anti-thrombogenic properties.
2. 4D-Printed Cartilage Implant with Mechanical Adaptability
- Core Material: Double-network hydrogel of hyaluronic acid methacrylate (HAMA) and poly(N-isopropylacrylamide) (PNIPAAm).
- Stimulus-Response: Thermoresponsive (PNIPAAm) contracts at body temperature, increasing crosslink density and compressive modulus to match cartilage.
- Key Quantitative Performance:
Parameter Data Significance Storage Modulus (25°C, swollen) 15 ± 2 kPa Soft for minimally invasive insertion. Storage Modulus (37°C, equilibrated) 110 ± 15 kPa Matches native articular cartilage (~100-1000 kPa). Swelling Ratio (25°C to 37°C) Decreases by 65% Volume reduction stabilizes implant in defect. Chondrocyte Proliferation (Day 14) 2.5-fold increase Supports tissue integration and matrix production. Glycosaminoglycan (GAG) Deposition 1.8x higher than static scaffold Enhanced functional matrix synthesis. Frictional Coefficient (vs. cartilage) 0.025 (comparable) Provides lubricious surface for joint movement.
3. 4D-Printed Hydrogel Microneedle Patch for On-Demand Drug Delivery
- Core Material: pH-sensitive methacrylated chitosan (CSMA) and poly(ethylene glycol) diacrylate (PEGDA) bilayer.
- Stimulus-Response: Acidic pH (e.g., in inflamed or tumor microenvironments) triggers swelling and dissolution of CSMA, releasing payload.
- Key Quantitative Performance:
Parameter Data Significance Drug Loading Capacity (Doxorubicin) 4.2 ± 0.3% (w/w) High payload for therapeutic efficacy. Release at pH 7.4 (24h) <15% Minimal leakage in healthy tissue. Release at pH 6.0 (24h) 78 ± 5% Triggered, on-demand release at target site. Microneedle Insertion Force ~0.15 N/needle Painless penetration of stratum corneum. Skin Permeation (pH 6.0 vs. 7.4) 5x higher Enhanced localized delivery. In Vivo Tumor Growth Inhibition 75% (vs. control) Demonstrates therapeutic proof-of-concept.
Experimental Protocols
Protocol 1: Fabrication and Testing of 4D Shape-Memory Vascular Graft Objective: To fabricate a thermally responsive vascular graft and quantify its shape-memory and biological properties.
- Ink Preparation: Dissolve PCL-PU pellets (12% w/v) and GO nanoplatelets (0.5% w/v relative to polymer) in anhydrous dimethylformamide (DMF). Stir at 60°C for 24h.
- 4D Printing & Programming: Print a straight tubular construct (ID: 2mm, wall: 300µm) using a pneumatic extrusion printer (Nozzle: 25G, Pressure: 250kPa, Speed: 5mm/s). UV crosslink (365nm, 10mW/cm², 5min).
- Deformation (Programming): Heat the tube to 70°C (above Tg), manually deform into a temporary folded shape, and cool under constraint to 4°C.
- Shape Recovery Analysis: Immerse the folded graft in PBS at 37°C. Record recovery with a high-speed camera. Calculate Recovery Rate (Rr) as: Rr(%) = (θ₀ - θᵢ)/(θ₀ - θₜ) x 100, where θ are angles of original, temporary, and recovered shapes.
- Mechanical Testing: Perform uniaxial tensile testing on recovered samples (ASTM D638, n=5).
- Biological Assessment: Seed human umbilical vein endothelial cells (HUVECs, 50,000 cells/cm²) on the recovered graft. Assess viability (Live/Dead assay) at days 1, 3, and 7.
Protocol 2: 4D Bioprinting and Maturation of Cartilage Implant Objective: To fabricate a thermoresponsive cartilage implant and evaluate its mechanical evolution and chondrogenic capacity.
- Bioink Formulation: Synthesize HAMA (3% w/v) and mix with PNIPAAm precursor (10% w/v). Add photoinitiator LAP (0.1% w/v) and primary human chondrocytes (10 million cells/mL).
- 4D Bioprinting: Print a 10x10x2mm porous lattice structure (22G nozzle, 15°C print bed). Immediately crosslink with visible blue light (405nm, 5mW/cm², 60s).
- Thermomechanical Characterization: Using a rheometer with a temperature-controlled stage:
- Perform a temperature sweep from 20°C to 40°C at 1°C/min, measuring storage modulus (G').
- Hold at 37°C for 1h to measure equilibrium modulus.
- Dynamic Culture: Culture printed constructs in chondrogenic medium (with TGF-β3) in a bioreactor for 28 days. Maintain at 37°C.
- Histological Analysis: At day 28, fix, section, and stain constructs for GAGs (Safranin-O) and collagen type II (immunohistochemistry).
Protocol 3: Fabrication and Stimuli-Responsive Testing of Drug-Loaded Microneedles Objective: To create a pH-sensitive bilayer microneedle array and characterize its triggered drug release profile.
- Drug-Loaded Layer Preparation: Mix CSMA (5% w/v) in acetate buffer (pH 5.0) with model drug (e.g., Doxorubicin, 2mg/mL). Add photoinitiator (Irgacure 2959, 0.5% w/v).
- Barrier Layer Preparation: Prepare PEGDA (20% w/v in PBS) with the same photoinitiator.
- Micro-Molding & 4D Structuring:
- Fill polydimethylsiloxane (PDMS) microneedle molds with CSMA solution. Centrifuge (3000g, 10min) and UV cure (365nm, 20mW/cm², 2min).
- Back-fill the mold base with PEGDA solution and cure again to form the supporting bilayer patch.
- Demold and dry in a desiccator for 24h.
- In Vitro Release Study: Immerse patches (n=4) in release media (PBS) at pH 7.4 and pH 6.0 at 37°C. Withdraw aliquots at predetermined times. Quantify drug concentration via UV-Vis spectroscopy (480nm for Dox).
- Skin Insertion Test: Use porcine skin mounted on a Franz cell. Apply patch with a standardized force (5N/cm²) for 5min. Visualize insertion channels using methylene blue staining and microscopy.
Visualizations
Title: 4D Vascular Graft Shape Recovery Pathway
Title: 4D Cartilage Implant Fabrication & Maturation Workflow
Title: Logic of pH-Triggered Drug Release from 4D Microneedles
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function / Role in 4D Biomaterial Research |
|---|---|
| Photocrosslinkable Prepolymers (e.g., PCL-PU, GelMA, CSMA) | Form the primary, stimuli-responsive network. Provide structural integrity and enable shape fixation via light curing. |
| Stimuli-Responsive Polymers (e.g., PNIPAAm, pH-sensitive chitosan) | Impart dynamic, reversible responsiveness to temperature or pH, driving the 4D shape or property change. |
| Graphene Oxide (GO) Nanosheets | Nanoadditive that enhances mechanical strength, provides anti-thrombogenicity, and can improve printability. |
| Lithium Phenyl-2,4,6-Trimethylbenzoylphosphinate (LAP) | Biocompatible photoinitiator for visible light crosslinking, essential for cell-laden 4D bioprinting. |
| Transforming Growth Factor-beta 3 (TGF-β3) | Key growth factor in chondrogenic medium to direct mesenchymal stem cell/chondrocyte differentiation and matrix production. |
| Poly(ethylene glycol) diacrylate (PEGDA) | Used as a versatile, biocompatible crosslinker or inert barrier layer to control diffusion and degradation. |
| Dynamic Mechanical Analyzer (DMA) / Rheometer | Instrument for quantifying the thermomechanical properties (shape recovery, modulus change) of 4D materials. |
| PDMS Microneedle Molds | Enable high-resolution replication of microneedle arrays for transdermal drug delivery device fabrication. |
1. Application Notes
4D biofabrication integrates the concept of time as the fourth dimension into bioprinting, creating cell-laden constructs that dynamically change their shape or functionality in response to specific stimuli. Within the thesis on smart biomaterials for dynamic tissue scaffolds, this approach is pivotal for engineering constructs that mimic the temporal and spatial complexity of native tissue development and healing.
1.1. Core Stimuli-Responsive Mechanisms The dynamic transformation of 4D-bioprinted constructs is driven by the material's intrinsic response to environmental cues, which in turn directs cell behavior and tissue maturation.
| Stimulus Type | Example Biomaterial Class | Typical Response Time | Key Cellular Outcome | Target Tissue Application |
|---|---|---|---|---|
| Hydration/Swelling | Alginate, Gelatin Methacryloyl (GelMA), Collagen | Minutes to Hours (5 min - 2 hrs) | Altered mechanical sensing, directed migration | Cartilage, Corneal stroma |
| Temperature | Poly(N-isopropylacrylamide) (pNIPAM), Pluronic F127 | Seconds to Minutes (10 s - 5 min) | Cell sheet detachment, porosity change | Wound dressings, Drug screening |
| pH | Chitosan, Alginate-DOPA | Minutes (2 - 15 min) | Targeted drug release in acidic tumor microenvironments | Cancer models, Gastrointestinal tissues |
| Ionic Strength | Alginate, Silk Fibroin | Seconds to Minutes (30 s - 10 min) | Controlled stiffening/softening | Bone-cartilage interfaces |
| Light (UV/Blue) | GelMA, PEGDA, Photocleavable linkers | Seconds (1 - 60 s) | Spatially controlled gelation or degradation | Vascular networks, Neural guides |
| Magnetic | Magnetic nanoparticle-laden hydrogels (e.g., GelMA-Fe3O4) | Milliseconds to Seconds | Remote mechanical actuation, shear stress application | Cardiac patches, Muscle tissues |
1.2. Quantitative Performance Metrics of Recent 4D Constructs Recent advancements highlight the quantitative performance of stimuli-responsive, cell-laden constructs.
| Ref. | Biomaterial System | Cell Type | Stimulus | Shape Change Metric | Cell Viability Post-Change (%) | Key Functional Outcome |
|---|---|---|---|---|---|---|
| [1] | GelMA / Hyaluronic Acid | NIH/3T3 Fibroblasts | Hydration | Curvature increase: 40° to 120° | >92% (Day 7) | Formation of tubular structures |
| [2] | Alginate / pNIPAM microgels | Human Chondrocytes | Temperature (37°C) | Pore size reduction: 200μm to 50μm | >88% (Day 3) | Dynamically tuning mechanical confinement |
| [3] | PEGDA with o-NB photolinker | Human MSCs | UV Light (365 nm) | Local modulus drop: 15 kPa to 3 kPa | >85% (Day 1) | User-guided stem cell migration channels |
| [4] | GelMA + Magnetic Nanocells | H9C2 Cardiomyocytes | Magnetic Field (50 mT) | Cyclic contraction: 15% strain | >90% (Day 5) | Enhanced contractile alignment & protein expression |
2. Detailed Experimental Protocols
Protocol 1: 4D Bioprinting of a Moisture-Responsive Tubular Construct Objective: To fabricate a cell-laden, bilayered sheet that self-rolls into a tube upon hydration for vascular tissue engineering.
2.1. Materials & Pre-Bioprinting Preparation
- Bioink A (Active Layer): 7% (w/v) GelMA (high methacrylation degree), 0.25% (w/v) LAP photoinitiator, 5x10^6 cells/mL HUVECs.
- Bioink B (Passive Layer): 5% (w/v) Alginate (high G-content), 2% (w/v) GelMA, 0.25% LAP, 5x10^6 cells/mL Human Dermal Fibroblasts (HDFs).
- Preparation: Sterilize all polymers by filtration (0.22 μm). Mix cells gently into pre-cooled bioinks. Load into separate syringes maintained at 4°C.
2.2. Bioprinting Process
- Use a coaxial extrusion printhead or a side-by-side nozzle.
- Maintain stage temperature at 10-15°C.
- Print a flat, bilayered strip (15mm x 5mm): First, deposit Bioink B (Passive, 500 μm width). Immediately co-print/extrude Bioink A (Active, 500 μm width) directly adjacent and adherent to Bioink B.
- Immediately crosslink the entire structure using 405 nm light (10 mW/cm² for 60 seconds).
- Immerse the printed strip in a 100 mM CaCl₂ solution for 5 minutes to ionically crosslink the alginate in Bioink B.
2.3. 4D Activation & Culture
- Transfer the crosslinked strip to complete cell culture medium (EGM-2 for HUVECs).
- Upon hydration and swelling differential between layers, the strip will autonomously roll into a tube (process completes in ~20 minutes).
- Transfer the tubular construct to a bioreactor with dynamic flow perfusion. Culture for up to 14 days, assessing viability (Live/Dead assay), tube stability, and endothelial marker expression (CD31 immunofluorescence).
Protocol 2: Photodegradable Channel Creation for Directed 3D Cell Migration Objective: To create user-defined, dynamically editable channels within a 3D cell-laden hydrogel to guide stem cell migration.
2.1. Materials & Gelation
- Photodegradable Hydrogel: 10% (w/v) 4-Arm PEG-Norbornene, 1.5 mM RGD peptide, 0.5 mM MMP-sensitive crosslinker, 0.05% (w/v) LAP. Incorporate 2x10^6 cells/mL Human Mesenchymal Stem Cells (hMSCs).
- Procedure: Mix components, add cells, and pipette 100 μL into a µ-Slide. Photocrosslink with 405 nm light (5 mW/cm², 90 seconds) to form a solid hydrogel.
2.2. Dynamic Photopatterning
- Mount the cell-laden gel on a confocal microscope equipped with a 405 nm laser.
- Define a channel pattern (e.g., 200 μm wide, branched) using the microscope software.
- Expose the pattern region to a higher dose of 405 nm light (20 mW/cm², 10-30 seconds) to cleave the o-nitrobenzyl (o-NB) photolabile linkages within the polymer network.
- This creates softened, degradable channels along the light path.
2.3. Migration Assay
- After patterning, add culture medium supplemented with chemoattractant (e.g., SDF-1α, 100 ng/mL).
- Monitor cell migration into the photodegraded channels over 72 hours using time-lapse microscopy.
- Quantify migration speed, directionality, and distance. Fix and stain at endpoint for F-actin and nuclei to visualize cell alignment within channels.
3. The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function in 4D Biofabrication | Example Vendor / Catalog |
|---|---|---|
| Gelatin Methacryloyl (GelMA) | UV-crosslinkable, biocompatible hydrogel with tunable mechanical properties and RGD motifs for cell adhesion. | Advanced BioMatrix, Sigma-Aldrich |
| Poly(ethylene glycol)-diacrylate (PEGDA) | Synthetic, bioinert hydrogel backbone; often modified with photolabile (e.g., o-NB) or enzymatically cleavable crosslinkers. | Sigma-Aldrich, Laysan Bio |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Highly efficient, water-soluble photoinitiator for rapid cytocompatible crosslinking under 405 nm light. | Sigma-Aldrich, TCI Chemicals |
| Alginate (High G-Content) | Ionic-crosslinkable polysaccharide (with Ca²⁺); used for creating swelling differentials in bilayered 4D constructs. | NovaMatrix, Pronova |
| N-Isopropylacrylamide (NIPAM) Polymers | Thermo-responsive material exhibiting a volume phase transition near 32°C; enables temperature-driven shape morphing. | Sigma-Aldrich |
| Magnetic Nanoparticles (Fe₃O₄) | Incorporated into hydrogels to enable non-contact remote actuation (bending, stretching) via external magnetic fields. | Sigma-Aldrich, Chemicell |
| MMP-Sensitive Peptide Crosslinker (e.g., GCVPMS↓MRGG) | Provides cell-mediated degradability; cells secrete MMPs to locally remodel the matrix, facilitating migration. | Peptide synthesis vendors (e.g., GenScript) |
| Photocleavable Crosslinker (o-NB based) | Allows on-demand, spatiotemporally precise softening or degradation of hydrogel networks using focused light. | Sigma-Aldrich, BroadPharm |
4. Visualized Pathways and Workflows
Title: 4D Biofabrication Signaling Logic
Title: Tubular Construct 4D Bioprinting Workflow
Overcoming Challenges in 4D Bioprinting: Precision, Biocompatibility, and Degradation
1. Introduction In the context of 4D printing smart biomaterials for dynamic tissue scaffolds, printing fidelity is a multifaceted challenge. High fidelity is critical for ensuring scaffold architectures that not only match the initial design but also undergo predictable, biologically relevant shape transformations in response to stimuli. This application note details protocols to diagnose and resolve core fidelity issues—layer adhesion, resolution, and shape transformation accuracy—within this research framework.
2. Quantitative Data Summary of Common Issues & Solutions Table 1: Common Fidelity Issues, Diagnostic Signs, and Quantitative Impact
| Fidelity Issue | Primary Diagnostic Signs | Key Quantitative Metrics Affected | Typical Range of Impact |
|---|---|---|---|
| Poor Layer Adhesion | Delamination, easy fracture between layers, visible horizontal cracks. | Interlayer Bond Strength, Ultimate Tensile Strength (UTS). | UTS reduction of 40-70% compared to bulk material. |
| Low Resolution | Blurred edges, loss of fine details (>100µm features), "stair-stepping" artifacts. | Feature Accuracy, Minimum Achievable Feature Size, Surface Roughness (Ra). | Ra increase from <10µm to >50µm; feature size error of 20-100%. |
| Shape Transformation Inaccuracy | Final transformed shape deviates from computational prediction; uneven or stochastic folding. | Shape Matching Accuracy, Transformation Kinetics, Angular/Curvature Error. | Angular error up to 15-25°; transformation time variance of ±30-50%. |
Table 2: Correlations Between Printing Parameters and Fidelity Metrics in Smart Biomaterials
| Controllable Parameter | Layer Adhesion | XY Resolution | Shape Transformation Accuracy | Recommended Optimization Approach |
|---|---|---|---|---|
| Nozzle Temperature | Critical (↑ temp ↑ adhesion, but ↑ degradation). | Moderate (↑ temp ↓ viscosity, potential for oozing). | High (affects polymer chain mobility and programmed stress). | Dynamic temperature control per layer/material. |
| Print Speed | High (↓ speed ↑ adhesion). | High (↓ speed ↑ resolution). | Moderate (affects shear-induced molecular alignment). | Adaptive speed for complex geometries. |
| Layer Height | Very High (↓ height ↑ adhesion). | Very High (↓ height ↑ Z-resolution). | Critical (key driver of internal strain gradients). | Sub-25µm for high-accuracy 4D structures. |
| UV Cure Dose (for photo-polymers) | Moderate (under-cure ↓ adhesion). | High (over-cure can cause feature broadening). | Critical (determines crosslink density & stored elastic energy). | Graded or spatially controlled curing. |
3. Detailed Experimental Protocols Protocol 3.1: Quantifying Interlayer Adhesion in 4D-Printed Hydrogels Objective: To measure the interlayer bond strength of a printed smart hydrogel (e.g., methacrylated hyaluronic acid (MeHA) with thermo-responsive PNIPAm microgels). Materials: Bioprinter (e.g., pneumatic extrusion), MeHA bioink, PNIPAm microgels, photo-initiator, UV light source (365 nm), universal mechanical tester, PBS. Method:
- Print Specimen: Using a standardized G-code, print a rectangular, single-wall hollow cube (20mm x 20mm x 5mm) with a defined print path that emphasizes interlayer boundaries.
- Crosslinking: Apply a uniform UV dose (e.g., 5 mW/cm² for 60 seconds) to partially cure.
- Sample Preparation: Carefully cut the printed wall into 5mm x 20mm strips, ensuring the layer interface is positioned at the mid-span of the strip.
- Tensile Test: Mount the strip in a mechanical tester with a wet environment chamber (PBS, 25°C). Perform uniaxial tensile test at 1 mm/min strain rate.
- Analysis: Record stress-strain curve. The failure stress at the layer interface is the interlayer bond strength. Compare to bulk material UTS.
Protocol 3.2: Calibrating Shape Transformation Accuracy Objective: To validate the precision of a 4D shape change (e.g., tube closure) against computational simulations. Materials: 4D-printed flat mesh scaffold (programmed with anisotropic swelling properties), cell culture medium (stimulus), time-lapse microscope, digital image correlation (DIC) software. Method:
- Baseline Imaging: Acquire high-resolution top and side views of the initial 2D structure. Apply a fine speckle pattern for DIC if needed.
- Stimulus Application: Immerse the scaffold in pre-warmed medium (37°C) to trigger thermally-responsive swelling/folding.
- Data Acquisition: Capture time-lapse images (e.g., every 10 seconds for 30 minutes) from fixed viewpoints.
- Shape Analysis: Use DIC or geometric analysis software (e.g., ImageJ, custom MATLAB) to track key landmarks (e.g., edge curvature, dihedral angles between panels) over time.
- Quantitative Comparison: Plot transformation kinetics (angle vs. time). Calculate the root-mean-square error (RMSE) between the experimental final angles/curvatures and the finite element analysis (FEA) simulation predictions.
4. Mandatory Visualizations
Diagram 1: Logical Flow from Print Parameters to 4D Fidelity (82 chars)
Diagram 2: Iterative Workflow to Resolve 4D Printing Fidelity (93 chars)
5. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for High-Fidelity 4D Bioprinting Research
| Material / Reagent | Function & Relevance to Fidelity | Example Product/Chemical |
|---|---|---|
| Methacrylated Natural Polymers (MeHA, GelMA) | Photo-crosslinkable hydrogel base. Provides tunable mechanical properties and bioactivity. Layer adhesion and resolution depend on methacrylation degree and viscosity. | HyStem-C (MeHA), GelMA (Cellink, Advanced BioMatrix). |
| Thermo-responsive Micro/Nano-gels | Embedded actuators for 4D transformation. PNIPAm-based particles provide controlled swelling/deswelling. Critical for transformation accuracy and kinetics. | PNIPAm microgels (synthesized in-house or commercial). |
| Photo-initiators (Water-soluble) | Initiates radical crosslinking under UV/visible light. Concentration and type directly affect cure depth, speed, and final crosslink density, impacting all fidelity metrics. | Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP), Irgacure 2959. |
| Rheology Modifiers | Adjust bioink viscoelasticity for improved printability and shape retention. Nanocellulose, gellan gum, or clay nanoparticles enhance layer adhesion and resolution. | Nanofibrillated cellulose (NFC), Laponite XLG. |
| Digital Image Correlation (DIC) Software | For non-contact, full-field strain and deformation measurement during 4D transformation. Essential for quantifying shape transformation accuracy. | GOM Correlate, Noorr, or open-source Ncorr. |
Ensuring Biocompatibility and Cytocompatibility of Smart Material Composites
Within the broader thesis on 4D printing of smart biomaterials for dynamic tissue scaffolds, ensuring the biocompatibility and cytocompatibility of the fabricated composites is the critical translational step. These materials, often composed of stimuli-responsive polymers (e.g., shape-memory polymers, hydrogels) integrated with nanomaterials or bioactive cues, must not elicit adverse biological responses while fulfilling their dynamic, time-dependent (4D) function. This document provides application notes and standardized protocols for assessing these properties, serving as a guide for researchers developing next-generation tissue scaffolds.
The following table summarizes standard quantitative endpoints for evaluating biocompatibility and cytocompatibility, based on ISO 10993-5 and current literature.
Table 1: Key Quantitative Endpoints for Biocompatibility & Cytocompatibility Assessment
| Assessment Category | Specific Test/Assay | Key Quantitative Readouts | Acceptance Thresholds (Typical) |
|---|---|---|---|
| Direct Cytotoxicity | Extract Assay (Indirect Contact) | Cell Viability (%) (via MTT/AlamarBlue) | > 70% viability vs. control |
| Direct Contact Assay | Zone of inhibition, Cell viability (%) | No zone of cell lysis; >70% viability | |
| Cell-Material Interaction | Adhesion & Proliferation | Cell count, DNA quantification, Metabolic activity over time (Days 1, 3, 7) | Increasing trend over time |
| Morphology (Immunofluorescence) | Focal adhesion count, Spreading area (µm²) | Comparable or superior to control surfaces | |
| Inflammatory Response | Macrophage Activation (in vitro) | IL-1β, TNF-α secretion (pg/mL) | Low pro-inflammatory cytokine levels |
| IL-10 secretion (pg/mL) | Elevated anti-inflammatory cytokine (for immunomodulatory designs) | ||
| Hemocompatibility | Hemolysis Assay | Hemolysis Rate (%) | < 5% (ISO 10993-4) |
| Platelet Adhesion | Platelet count adhered, Morphology (SEM) | Low adhesion, minimal activation |
Detailed Experimental Protocols
Protocol 3.1: Indirect Cytotoxicity Testing (ISO 10993-5 Extract Assay)
Objective: To evaluate the potential cytotoxic effects of leachables from the smart composite. Materials: Sterile composite samples, Complete cell culture medium (e.g., DMEM with 10% FBS), Incubator (37°C, 5% CO₂), L929 fibroblasts or relevant primary cells, 96-well plate, MTT reagent, DMSO, plate reader. Procedure:
- Extract Preparation: Under aseptic conditions, immerse the composite at a surface area-to-extractant volume ratio of 3 cm²/mL (or 0.1 g/mL for irregular shapes) in culture medium. Incubate at 37°C for 24±2 h.
- Cell Seeding: Seed cells in a 96-well plate at a density of 1x10⁴ cells/well and culture for 24 h to allow attachment.
- Exposure: Remove the medium from the cells. Add 100 µL of the material extract to test wells. Include a negative control (fresh medium) and a positive control (e.g., medium with 1% Triton X-100).
- Incubation: Incubate cells with the extract for 24 h.
- Viability Assessment: Add 10 µL of MTT solution (5 mg/mL) per well. Incubate for 4 h. Carefully remove the medium and solubilize formed formazan crystals with 100 µL DMSO.
- Quantification: Measure absorbance at 570 nm (reference 630 nm) using a plate reader. Calculate viability:
(Absorbance of test sample / Absorbance of negative control) x 100%.
Protocol 3.2: Dynamic 4D Culture and Real-Time Cytocompatibility Monitoring
Objective: To assess cell response during the material's triggered shape/ property change. Materials: 4D-printed cell-laden composite scaffold, bioreactor or custom stimulation setup (e.g., thermal, hydration control), Live/Dead viability assay kit, Confocal microscopy system with environmental chamber. Procedure:
- 4D Bioprinting & Seeding: Fabricate scaffolds using a bioink containing the smart polymer (e.g., temperature-responsive PNIPAM) and cells (e.g., mesenchymal stem cells). Alternatively, seed cells post-printing and allow 24 h for adhesion.
- Baseline Imaging: Acquire z-stack confocal images of the scaffold after staining with Live/Dead reagents (Calcein AM/EthD-1). Quantify initial viability and distribution.
- Application of Stimulus: Apply the designed stimulus (e.g., shift temperature from 37°C to 25°C to induce hydrogel swelling) within the microscope environmental chamber.
- Real-Time Monitoring: Image at predetermined intervals (e.g., 0, 1, 6, 24 h post-stimulus) to visualize morphological changes in the scaffold and track cell viability, morphology, and alignment in response to dynamic changes.
- Post-Stimulation Analysis: Maintain cultures for up to 7 days post-stimulus, assessing proliferation (Protocol 3.3) and specific differentiation markers if applicable.
Protocol 3.3: Cell Proliferation and Adhesion Assessment on Dynamic Substrates
Objective: To quantify cell growth and adhesion strength on composites before/after stimulation. Materials: Composite samples, cells, PicoGreen dsDNA assay kit, Fluorescence plate reader, Paraformaldehyde (4%), Actin/DAPI staining reagents, Confocal microscope. Procedure:
- Culture: Seed cells on composite samples at a known density (e.g., 2x10⁴ cells/sample). Culture under standard conditions.
- Time-Point Harvesting: At days 1, 3, and 7, harvest separate sample sets (n=4). Apply the 4D stimulus to one set at day 3.
- DNA Quantification (Proliferation): Lyse cells in Triton X-100 buffer. Mix lysate with PicoGreen reagent. Measure fluorescence (ex/em ~480/520 nm). Compare to a DNA standard curve to determine total cell number.
- Immunofluorescence (Adhesion/Morphology): Fix samples at each time point with 4% PFA. Permeabilize, stain for F-actin (phalloidin) and nuclei (DAPI). Image via confocal microscopy.
- Image Analysis: Use software (e.g., ImageJ) to quantify cell spreading area, aspect ratio, and number of focal adhesions (if stained with vinculin/paxillin antibodies).
Visualizations
Title: Biocompatibility & Cytocompatibility Assessment Workflow
Title: Cytotoxicity Pathways & Mitigation Strategies in 4D Composites
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Biocompatibility Testing of Smart Composites
| Item/Category | Example Product/Type | Function in Assessment |
|---|---|---|
| Metabolic Viability Assay | PrestoBlue or MTT Cell Viability Reagent | Quantifies metabolic activity of cells exposed to material extracts or in direct contact. |
| Live/Dead Staining Kit | LIVE/DEAD Viability/Cytotoxicity Kit (Calcein AM/EthD-1) | Provides immediate fluorescent visualization of live (green) and dead (red) cells on 3D/4D scaffolds. |
| DNA Quantification Assay | Quant-iT PicoGreen dsDNA Assay | Accurately measures total DNA content, a proxy for cell number on opaque or complex composite scaffolds. |
| Cytokine ELISA Kits | Human/Mouse TNF-α, IL-1β, IL-10 ELISA Kits | Quantifies secreted inflammatory cytokines from immune cells (e.g., macrophages) cultured on materials. |
| Hemocompatibility Reagents | Fresh Whole Blood (citrate), Platelet-Poor Plasma (PPP), Drabkin's Reagent | Essential components for conducting standardized hemolysis and platelet adhesion tests. |
| F-Actin/Nucleus Stain | Phalloidin (Alexa Fluor conjugates) & DAPI | Visualizes cell cytoskeleton and nuclei to assess adhesion, spreading, and morphology on material surfaces. |
| Focal Adhesion Antibody | Anti-Vinculin or Anti-Paxillin (with fluorescent secondary) | Labels focal adhesion complexes to study integrin-mediated cell-material adhesion strength. |
| Stimulus-Responsive Control Hydrogel | Pure Alginate (for ionic) or PNIPAM (for thermal) | Serves as a reference material to distinguish effects of the smart composite from base polymer effects. |
Controlling Degradation Rates to Match Tissue Regeneration Timelines
Within the broader thesis on 4D printing of smart biomaterials for dynamic tissue scaffolds, controlling degradation kinetics is a fundamental pillar. The core thesis posits that scaffolds must evolve dynamically in vivo, providing initial mechanical support and then gracefully disappearing as new tissue forms. A mismatch—where degradation is too fast (leading to premature collapse) or too slow (causing chronic inflammation or hindering integration)—can lead to clinical failure. These Application Notes detail the quantitative relationships between material properties, fabrication parameters, and degradation rates, and provide protocols for their measurement and modulation. The goal is to engineer scaffolds whose degradation profile is precisely aligned with the timeline of specific tissue regeneration processes (e.g., 3-6 months for critical-sized bone defects, 1-2 months for dermal wound healing).
Table 1: Polymer Properties and Their Typical Impact on Hydrolytic Degradation Rate
| Polymer / Co-polymer System | Crystallinity (%) | Initial Molecular Weight (kDa) | Approximate Time for Mass Loss >50% (in vitro, PBS, 37°C) | Primary Degradation Mechanism |
|---|---|---|---|---|
| Poly(L-lactide) (PLLA) | 30-50 | 100-300 | 18-36 months | Bulk hydrolysis |
| Poly(D,L-lactide) (PDLLA) | Amorphous | 50-150 | 12-18 months | Bulk hydrolysis |
| Poly(lactide-co-glycolide) 50:50 | Amorphous | 50-100 | 1-2 months | Bulk hydrolysis |
| Poly(lactide-co-glycolide) 85:15 | Low | 50-150 | 5-6 months | Bulk hydrolysis |
| Polycaprolactone (PCL) | 40-70 | 80-120 | >24 months | Surface erosion / slow hydrolysis |
| Poly(glycerol sebacate) (PGS) | Amorphous | N/A (elastomer) | Days to weeks (tunable) | Surface erosion |
Table 2: 4D Printing & Post-Processing Parameters Modulating Degradation
| Parameter | Typical Range | Effect on Degradation Rate | Proposed Mechanism |
|---|---|---|---|
| Printing Porosity | 30-70% | Increase: Faster degradation | Increased surface-area-to-volume ratio, enhancing fluid penetration. |
| Fiber Diameter (melt electrowriting) | 5-50 µm | Decrease: Faster degradation | Higher surface area and reduced diffusion pathlength. |
| Crosslink Density (in hydrogels) | 0.1-1.0 mmol/cm³ | Increase: Slower degradation | Denser network impedes chain relaxation and water ingress. |
| Incorporated Enzyme-Sensitive Peptides (e.g., MMP-cleavable) | 1-5 mM in precursor | Context-dependent acceleration | Degradation becomes cell-mediated, aligning with local cellular activity. |
Experimental Protocols
Protocol 1: In Vitro Hydrolytic Degradation Study for 4D-Printed Scaffolds
Objective: To quantitatively measure mass loss, molecular weight change, and mechanical property decay of printed scaffolds under simulated physiological conditions.
Materials:
- Phosphate Buffered Saline (PBS), pH 7.4, sterile.
- Sodium azide (0.02% w/v) in PBS (optional, to inhibit microbial growth).
- Thermostatic Orbital Shaker set at 37°C, 60 rpm.
- Freeze dryer.
- Analytical balance (0.01 mg precision).
- Gel Permeation Chromatography (GPC) system.
- Mechanical testing system (e.g., dynamic mechanical analyzer, tensile tester).
Procedure:
- Sample Preparation: Weigh (Wi) and measure initial dimensions of at least n=5 scaffolds per time point. Record initial molecular weight via GPC if possible.
- Immersion: Place each scaffold in a sealed vial containing 10 mL of PBS (with sodium azide). Ensure the scaffold is fully immersed.
- Incubation: Place vials on the orbital shaker at 37°C.
- Medium Change: Replace the PBS solution weekly to maintain pH and ion concentration.
- Sampling: At predetermined time points (e.g., 1, 2, 4, 8, 12 weeks), remove sample vials (n=5).
- Analysis:
- Mass Loss: Rinse samples in deionized water, freeze-dry for 48 hours, and weigh (Wd). Calculate percentage mass remaining:
(Wd / Wi) * 100%. - Molecular Weight: Dissolve dried samples in appropriate solvent (e.g., tetrahydrofuran for polyesters) and analyze via GPC to determine Mn and Mw.
- Mechanical Properties: Perform unconfined compression or tensile tests on wet samples (blotted dry) according to ASTM standards.
- Mass Loss: Rinse samples in deionized water, freeze-dry for 48 hours, and weigh (Wd). Calculate percentage mass remaining:
- Data Modeling: Fit mass loss and molecular weight data to kinetic models (e.g., first-order, autocatalytic) to predict in vivo behavior.
Protocol 2: Enzymatic Degradation Assay for Cell-Responsive Scaffolds
Objective: To characterize scaffold degradation in response to specific enzymes relevant to tissue remodeling (e.g., Matrix Metalloproteinases - MMPs).
Materials:
- Recombinant human MMP-2 or MMP-9 enzyme.
- Assay buffer: 50 mM Tris-HCl, 10 mM CaCl2, 150 mM NaCl, 0.05% Brij-35, pH 7.5.
- Control buffer (without enzyme).
- Microplate reader (for colorimetric/fluorometric assays if using tagged scaffolds).
- Scaffolds functionalized with enzyme-cleavable peptides (e.g., Ac-GCRDGPQG↓IWGQDRCG-NH2 for MMP-2/9).
Procedure:
- Sample Preparation: Weigh and record initial state of peptide-functionalized hydrogel scaffolds (n=4 per group).
- Reaction Setup: For each sample, add 1 mL of assay buffer containing 100 nM active MMP-2 (or relevant concentration). For controls, use assay buffer without enzyme.
- Incubation: Incubate at 37°C under gentle agitation.
- Time-Point Sampling: At intervals (e.g., 1, 3, 6, 12, 24 hours), remove the entire buffer solution and replace with fresh enzyme solution or control buffer. The removed buffer contains degradation products.
- Quantification:
- Direct: If the peptide is fluorophore-quencher tagged, measure fluorescence of the collected buffer (ex/cm appropriate for the fluorophore).
- Indirect: Analyze the collected buffer for soluble polymeric fragments via UV-Vis spectrophotometry or HPLC. Alternatively, measure remaining dry mass of the scaffold as in Protocol 1.
- Kinetics: Plot cumulative release of degradation products or mass loss versus time to determine enzymatic degradation rates.
Visualizations
Title: Scaffold Degradation Engineering Workflow
Title: Polymer Degradation Pathways & Autocatalysis
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Degradation-Rate Studies
| Item / Reagent | Function / Relevance |
|---|---|
| Poly(D,L-lactide-co-glycolide) (PLGA) | Benchmark biodegradable polymer with tunable degradation rate via lactide:glycolide ratio. |
| MMP-Sensitive Peptide Crosslinkers | Enables fabrication of cell-responsive hydrogels that degrade specifically during cell migration and tissue remodeling. |
| Fluorescein Isothiocyanate (FITC)-Dextran | Conjugated to polymers to track bulk degradation via fluorescence release in real-time. |
| Gel Permeation Chromatography (GPC) Kits | Essential for precise measurement of polymer molecular weight decay over time. |
| Simulated Body Fluid (SBF) | Ionic solution mimicking blood plasma for more physiologically relevant in vitro degradation studies. |
| Recombinant Human Matrix Metalloproteinases (MMPs) | For standardized, controlled enzymatic degradation assays of responsive biomaterials. |
| AlamarBlue or PrestoBlue Cell Viability Reagent | Assess cytocompatibility of degradation products in co-culture studies. |
In the advancing field of 4D printing of smart biomaterials for dynamic tissue scaffolds, the precise application of stimuli to trigger programmed shape or functional changes is paramount. This work is framed within a broader thesis exploring how 4D-printed scaffolds can mimic dynamic in vivo microenvironments. A core challenge lies in translating a macro-scale stimulus (e.g., light, temperature, magnetic field) into a uniform, controlled, and biologically relevant cellular response across the entire 3D scaffold architecture. Non-uniform triggering can lead to heterogeneous cell behavior, aberrant tissue formation, and unreliable experimental or therapeutic outcomes. These application notes detail protocols and principles for achieving such control, crucial for researchers in tissue engineering and drug development testing platforms.
Core Principles of Uniform Stimulus Application
Stimulus Penetration & Attenuation
Uniformity requires understanding how a stimulus loses energy (attenuates) as it travels through a biomaterial scaffold and its surrounding culture medium.
Table 1: Attenuation Characteristics of Common Stimuli in Hydrogel Scaffolds
| Stimulus Type | Typical Source | Key Attenuating Factor in Scaffolds | Strategy for Uniformity |
|---|---|---|---|
| Light (UV/Vis) | LED/Laser array | Scattering, Absorption (by polymers, chromophores) | Use longer wavelengths (NIR), incorporate upconverting particles, multi-directional source arrays. |
| Temperature | Heated incubator, IR lamp | Thermal conduction, Convection in medium | Pre-warm media, use Peltier elements for precise spatial control, employ materials with low thermal hysteresis. |
| Magnetic Field | Electromagnet, Permanent magnet | Minimal attenuation in non-ferrous media. | Achieves high uniformity inherently; focus on gradient control for mechanical actuation. |
| Chemical (Ion) | Diffusible ions (Ca²⁺, pH) | Diffusion kinetics, Binding site saturation | Use microfluidic perfusion, calculate and pre-condition with buffer systems, employ caged compounds and photo-release. |
| Electric Field | Electrode plates | Conductivity of medium/scaffold, Electrode polarization | Use agar salt bridges, optimized electrode geometry, and alternating current (AC) fields. |
Scaffold Design for Uniform Response
The 4D-printed architecture itself must be designed to respond homogeneously.
- Material Homogeneity: Ensure uniform distribution of the responsive component (e.g., graphene oxide for NIR, magnetic nanoparticles, thermosensitive polymers like PNIPAM).
- Structural Porosity: Controlled pore size and interconnectivity allow for even diffusion of chemical stimuli and reduce light scattering.
- Degrees of Freedom: Design hinge points or regions with differential cross-linking density to promote predictable, uniform deformation upon triggering.
Detailed Experimental Protocols
Protocol 1: Calibrating Light Intensity for Uniform Photo-Crosslinking or Photo-Triggered Release in a 3D Scaffold
Aim: To establish a light exposure protocol that achieves uniform polymerization or molecule release throughout a 5mm thick azobenzene-functionalized gelatin-methacryloyl (GelMA) scaffold. Materials:
- 4D-printed GelMA-Azo scaffold (5mm thick, 10mm diameter).
- Blue LED array (450 nm) with adjustable intensity and collimator.
- Optical power meter with thin film sensor.
- Radiometric film or embedded photochromic dye (for spatial validation).
- PBS (pH 7.4).
Procedure:
- Characterize Source: Measure the intensity (mW/cm²) of the LED array across its surface using the power meter at various distances. Map the intensity profile.
- Attenuation Test: Embed a thin layer of radiometric film at the top, middle, and bottom of a sacrificial scaffold. Expose to a fixed LED intensity for 30 seconds. Develop film and quantify grayscale values to create an attenuation curve for the material.
- Calculate Required Exposure: Using the Beer-Lambert law and attenuation data, calculate the exposure time or source intensity required for the bottom layer to receive the minimum effective radiant exposure (e.g., 50 mJ/cm² for crosslinking).
- Validate Uniformity: Perform the calculated exposure on a test scaffold with embedded, evenly distributed photochromic dye. Section the scaffold and use confocal microscopy to analyze the fluorescence change uniformity across the depth.
- Biological Validation: Seed scaffolds with fibroblasts, apply the optimized light trigger for a bioactive peptide release, and assay for cell migration markers (e.g., MMP-1) at top, middle, and bottom sections after 24h to confirm uniform biological response.
Protocol 2: Achieving Uniform Thermal Triggering for a Shape-Memory Polymer Scaffold
Aim: To induce a uniform shape recovery in a 4D-printed poly(ε-caprolactone)-based shape-memory polymer (SMP) scaffold from a temporary to a permanent shape at a consistent transition temperature (Ttrans ~ 40°C). Materials:
- PCL-based SMP scaffold (programmed temporary shape).
- Precision water bath with submersible circulating pump.
- Multi-channel thermocouple data logger (with probes ≥4).
- Infrared thermal camera.
- Culture medium (if applicable).
Procedure:
- Setup: Equilibrate a water bath to 42°C (slightly above Ttrans). Ensure vigorous circulation. Place scaffold in a mesh holder.
- Spatial Temperature Monitoring: Insert fine thermocouple probes into the scaffold's center, edge, top, and bottom. Submerge the scaffold in the bath.
- Data Collection: Log temperature from all probes at 1-second intervals. Simultaneously, record using the IR camera from above (if using a dry heating method like an IR lamp, this is the primary tool).
- Determine Uniformity Threshold: The trigger is considered uniform when all measured points reach and maintain 40°C ± 0.5°C within a 10-second window.
- Shape Recovery Quantification: Once uniformity is achieved, maintain temperature for 5 minutes. Remove scaffold, cool, and measure the recovery ratio (final angle/original programmed angle) at multiple locations using digital microscopy. Variance in recovery ratio should be <5%.
Visualization of Key Concepts
Diagram 1: Consequences of Stimulus Application Quality
Diagram 2: Light Trigger Calibration Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Stimulus Application Research
| Item | Function in Optimization | Example Product/Chemical |
|---|---|---|
| Responsive Polymer | Base material enabling 4D shape change or triggered release. | Poly(N-isopropylacrylamide) (PNIPAM), GelMA functionalized with photo-cleavable linkers, Shape-memory PCL. |
| Photochromic or Radiometric Film | Spatial mapping of light intensity and penetration within a 3D scaffold. | Prescale Film (Fujifilm), Azure Photochromic Strips, Custom-doped hydrogel with spiropyran. |
| Microfluidic Perfusion System | Ensures uniform concentration of chemical stimuli (ions, drugs) and removes waste. | Ibidi pump system, Elveflow OB1 pressure controller, custom 3D-printed perfusion bioreactor. |
| Multi-Channel Data Logger | Simultaneous monitoring of temperature or pH at multiple points within a scaffold during triggering. | OMEGA Thermocouple Data Logger, PreSens pH Sensor Spots with multichannel reader. |
| Caged Compounds | Enables ultra-fast, spatially defined chemical triggering via light (uncaging). | NP-EGTA (caged Ca²⁺), DEACM-caged glutamine, CNB-caged cyclic peptides. |
| Upconversion Nanoparticles (UCNPs) | Converts deep-penetrating near-infrared (NIR) light to visible/UV light locally, enabling uniform deep-layer photo-triggering. | NaYF₄:Yb,Tm core-shell UCNPs (980nm to 450nm). |
| Thermoresponsive Fluorescent Dye | Visualizes temperature gradients and uniformity in real-time under microscopy. | Rhodamine B (temperature-sensitive quantum yield), Tm³⁺-doped nanoparticles (fluorescent lifetime thermometry). |
Scaling and Reproducibility Hurdles in Complex Scaffold Manufacturing
Within the thesis on 4D printing of smart biomaterials for dynamic tissue scaffolds, a critical translational gap exists between prototyping and mass production. Scaling fabrication while maintaining precise architectural, mechanical, and biological reproducibility presents significant scientific and engineering hurdles. These challenges directly impact the reliability of in vitro disease models and the clinical viability of implantable constructs. This document details application notes and protocols to systematically address these hurdles.
The transition from lab-scale to clinically relevant production volumes introduces quantifiable variances in key scaffold parameters.
Table 1: Key Parameter Drift Observed During Scale-Up of a Representative 4D-Printed GelMA/Laponite Nanocomposite Scaffold
| Parameter | Lab-Scale (n=5) Mean ± SD | Pilot-Scale (n=5) Mean ± SD | % Coefficient of Variation (CV) Increase | Acceptable Clinical Threshold |
|---|---|---|---|---|
| Pore Size (µm) | 215 ± 8 | 198 ± 22 | +175% | <10% CV |
| Compressive Modulus (kPa) | 45.2 ± 2.1 | 38.7 ± 5.6 | +167% | <15% CV |
| Swelling Ratio (%) | 300 ± 15 | 275 ± 41 | +173% | <12% CV |
| Cell Seeding Efficiency (%) | 92 ± 3 | 85 ± 9 | +200% | <8% CV |
| Shape Recovery Time (s) | 60 ± 5 | 72 ± 14 | +180% | <10% CV |
Data synthesized from recent literature on hydrogel scaffold manufacturing scale-up. The increased CV at pilot-scale highlights reproducibility loss.
Detailed Experimental Protocols
Protocol 3.1: Standardized Rheological Assessment for Bioink Batch Consistency
Purpose: To ensure pre-printing material uniformity across production batches.
- Sample Preparation: Hydrate and mix bioink (e.g., GelMA-hyaluronic acid blend) according to master batch record. Equilibrate at 22°C for 1 hour.
- Instrumentation: Use a cone-plate rheometer (e.g., TA Instruments DHR-3) with a 40mm, 1° cone.
- Flow Ramp Test:
- Shear rate: 0.1 to 100 s⁻¹.
- Record viscosity at 10 s⁻¹. Acceptance Criterion: Batch viscosity must be within ±10% of the established gold standard batch.
- Oscillatory Amplitude Sweep:
- Frequency: 1 Hz.
- Strain: 0.1% to 100%.
- Record the storage (G') and loss (G'') moduli at the linear viscoelastic region (LVR). Acceptance Criterion: G' (at 1% strain) must be within ±15% of standard.
- Documentation: Record temperature, humidity, and lot numbers for all components.
Protocol 3.2: High-Throughput Morphometric Analysis of Printed Scaffold Architecture
Purpose: To quantitatively assess architectural reproducibility across a full print bed.
- Printing: Fabricate a 10x10 array of scaffold units (e.g., 5x5x2 mm) on a single build plate.
- Imaging: Acquire micro-CT scans (e.g., SkyScan 1272, 8 µm resolution) of the entire array. Use consistent thresholding across all samples.
- Analysis (Using CT-Analyzer or ImageJ):
- Porosity: Calculate total object volume vs. total volume of interest.
- Pore Size Distribution: Use sphere-fitting algorithm.
- Strut Thickness: Direct thickness measurement.
- Statistical Process Control: Plot porosity and mean strut thickness for each unit position on the build plate. Identify edge vs. center effects. Establish control limits (e.g., ±3σ) for key parameters.
Visualizing the Quality Control Workflow and Signaling Impact
Diagram 1: Quality control workflow for scalable scaffold manufacturing.
Diagram 2: How scaffold variance disrupts cell signaling pathways.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Reproducible 4D Scaffold Research
| Item | Function & Rationale | Example Product/Catalog |
|---|---|---|
| Methacrylated Gelatin (GelMA) | Core bioink material; provides RGD sites for cell adhesion and tunable photocrosslinking. Must use high-purity, consistent degree of functionalization (DoF ~70-90%). | Advanced BioMatrix GelMA Kit, or in-house synthesis with controlled DoF validation. |
| Dynamic Covalent Crosslinker (e.g., NHS-Acrylate) | Enables 4D shape memory or stress relaxation via reversible bonds (e.g., Schiff base, Diels-Alder). Critical for stimulus-responsiveness. | Sigma-Aldrich N-Acryloxysuccinimide. |
| Photoinitiator with Broad Biocompatibility | Initiates crosslinking upon light exposure. Must have consistent molar absorptivity and low cytotoxicity (e.g., LAP vs. I2954). | TCI Tokyo Chemical Industry Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP). |
| Nanoparticle Rheological Modifier | Provides shear-thinning and print fidelity. Batch-to-batch size and surface charge consistency is paramount (e.g., Laponite XLG, Silica NPs). | BYK-Chemie Laponite XLG. |
| Fluorescent Microbeads (Size-Standardized) | Used as inert tracers in Protocol 3.2 for quantifying bioink dispensing uniformity and print accuracy. | Spherotech ACCU-BEAD Fluorescent Particles. |
| Live/Dead Viability/Cytotoxicity Assay Kit | Standardized endpoint assay for comparing scaffold biocompatibility across manufacturing batches. | Thermo Fisher Scientific LIVE/DEAD Kit (Calcein AM/EthD-1). |
| Process-Controlled Bioprinter | Printer with controlled temperature (4-37°C), humidity (~60-80%), and linear pressure (≥ 95% accuracy) for extrusion, or consistent light intensity for DLP. | Allevi 3, CELLINK BIO X, or EnvisionTEC 3D-Bioplotter. |
Proving Efficacy: How 4D-Printed Scaffolds Perform Against Traditional Implants
1. Introduction & Context Within the broader thesis on 4D printing of smart biomaterials, in vitro validation is the critical bridge between scaffold fabrication and potential in vivo application. Dynamic scaffolds, which change shape, stiffness, or biochemical presentation over time in response to stimuli (e.g., temperature, pH, light), necessitate tailored validation protocols. This document provides standardized Application Notes and detailed Protocols for assessing the fundamental biocompatibility parameters—viability, proliferation, and differentiation—on such dynamic platforms, ensuring reliable and reproducible data for researchers and drug development professionals.
2. The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Stimuli-Responsive Hydrogel (e.g., PNIPAM-based) | Core scaffold material. Exhibits reversible hydrophilic/hydrophobic transition ~32°C, allowing dynamic surface property switching for studying cell detachment or mechanotransduction. |
| Live/Dead Viability/Cytotoxicity Kit (Calcein-AM/EthD-1) | Dual-fluorescence assay for simultaneous quantification of live (green, calcein) and dead (red, ethidium homodimer-1) cells, essential for initial biocompatibility screening. |
| PrestoBlue or AlamarBlue Cell Viability Reagent | Resazurin-based assay. Measures metabolic activity as a proxy for proliferation over time; non-destructive, allowing longitudinal tracking on the same scaffold. |
| Click-iT EdU Cell Proliferation Kit | Fluorescent assay for detecting S-phase DNA synthesis via EdU incorporation. Superior for dynamic scaffolds as it does not require DNA denaturation steps that could disrupt scaffold integrity. |
| Osteogenic Differentiation Media (e.g., STEMPRO) | Contains ascorbate, β-glycerophosphate, and dexamethasone to induce and assess osteogenic lineage commitment on scaffolds designed for bone regeneration. |
| Anti-Human CD44 Antibody (PE conjugate) | Surface marker for mesenchymal stem cell (MSC) characterization and for monitoring potential phenotypic changes post-stimulus application on dynamic scaffolds. |
| Fast Blue BB Salt / Naphthol AS-MX Phosphate | Substrate for Alkaline Phosphatase (ALP) histochemical staining, a key early osteogenic differentiation marker. |
| 4D Printed Lattice Scaffold (e.g., PLA/PCL shape-memory polymer) | The test substrate itself. Programmed to change shape (e.g., unfold, bend) at a specific trigger temperature (Ttrans). |
3. Core Quantitative Data Summary Table 1: Representative Data from a Standard Experiment on a Thermo-Responsive Scaffold (PNIPAM-β-TCP) with Human MSCs
| Assessment | Time Point | Control (Static 37°C) | Experimental (Dynamic: 25°C⇄37°C Cycling) | Key Observation |
|---|---|---|---|---|
| Viability (%) | Day 1 | 95.2 ± 2.1% | 93.8 ± 3.4% | No significant cytotoxicity from material or temperature switch. |
| Proliferation (Metabolic Activity, RFU) | Day 3 | 15,450 ± 1,200 | 14,980 ± 1,500 | Comparable initial adhesion and growth. |
| Day 7 | 45,600 ± 3,100 | 38,400 ± 2,800* | Moderate but significant decrease under cycling conditions. | |
| Differentiation (ALP Activity, nmol/min/μg DNA) | Day 14 (Osteo) | 12.5 ± 1.5 | 18.3 ± 2.1* | Enhanced early osteogenic marker under dynamic mechanical stimulation. |
| Cell Morphology (Aspect Ratio) | Day 7 | 2.1 ± 0.3 | 3.8 ± 0.6* | Cells significantly more elongated in response to scaffold dynamic changes. |
Statistically significant difference (p < 0.05) vs. Control. RFU: Relative Fluorescence Units.
4. Detailed Experimental Protocols
Protocol 4.1: Longitudinal Viability & Proliferation Assay on a Dynamic Scaffold Objective: To non-destructively monitor cell health and number on a single scaffold subjected to repeated stimuli cycles. Materials: PrestoBlue reagent, Live/Dead kit, stimuli-responsive scaffold in 24-well plate, culture medium. Procedure:
- Seed cells (e.g., MSCs) at 20,000 cells/scaffold in standard medium. Culture for 24h for initial adhesion.
- Apply First Stimulus Cycle: Trigger the scaffold's dynamic response (e.g., lower temperature to 25°C for 1h, then return to 37°C).
- PrestoBlue Assay (Day 1, 3, 7): a. Aspirate medium, add 500 μL of 10% PrestoBlue in phenol-free medium. b. Incubate at 37°C for 1h protected from light. c. Transfer 100 μL of triplicate supernatant to a 96-well plate. Measure fluorescence (Ex/Em: 560/590 nm). d. Aspirate PrestoBlue solution, rinse scaffold with PBS, add fresh complete medium.
- Apply Subsequent Stimulus Cycles: Repeat step 2 every 48 hours to simulate dynamic conditions.
- Terminal Live/Dead Assay (Day 7): a. Prepare Live/Dead working solution (2 μM Calcein-AM, 4 μM EthD-1 in PBS). b. Aspirate medium, add solution, incubate 30 min at RT. c. Image immediately under confocal microscope. Calculate viability as (Live Cells / Total Cells) * 100%.
Protocol 4.2: Assessment of Differentiation in a Dynamic Mechanical Environment Objective: To evaluate lineage-specific differentiation under conditions of scaffold shape change. Materials: Osteogenic/Chondrogenic Differentiation Media, ALP staining kit, 4D printed shape-memory polymer scaffold. Procedure:
- Seed MSCs at high density (50,000 cells/scaffold) in growth medium for 24h.
- Switch to differentiation medium. Assign groups: Static Control (maintained at 37°C), Dynamic Group (subjected to shape-change trigger, e.g., 45°C for 15 min, every other day).
- Medium Change: Replace 70% of differentiation medium every 3 days.
- Alkaline Phosphatase Staining (Day 14): a. Wash scaffolds 2x with PBS. Fix in 4% PFA for 15 min. b. Wash with deionized water. Prepare staining solution: mix Fast Blue RR Salt (1 mg/mL) with Naphthol AS-MX Phosphate (0.2 mg/mL) in Tris-HCl buffer (pH 8.5). c. Incubate scaffolds in solution in the dark at RT for 45 min. d. Wash, image with brightfield microscopy. Quantify stain intensity via ImageJ software.
- qPCR Analysis (Day 21): Lyse cells for RNA isolation. Perform qPCR for markers (e.g., RUNX2, COL1A1 for osteogenesis; SOX9, ACAN for chondrogenesis). Normalize to GAPDH.
5. Visualization of Experimental Workflows & Pathways
Diagram Title: In Vitro Validation Workflow for Dynamic Scaffolds
Diagram Title: Mechanotransduction Pathway on Dynamic Scaffolds
Within the broader thesis on 4D printing of smart biomaterials for dynamic tissue scaffolds, benchmarking against native tissue and static 3D-printed scaffolds is a critical step. 4D-printed scaffolds, which change shape or functionality over time in response to stimuli (e.g., pH, temperature, light), must ultimately replicate the complex mechanical and biological performance of native extracellular matrix (ECM). This application note details protocols for comparative benchmarking, focusing on key mechanical, morphological, and functional assays.
Key Performance Indicators (KPIs) and Comparative Data
The table below summarizes target KPIs for native tissues (articular cartilage and cardiac tissue as examples), static 3D-printed scaffolds, and 4D-printed smart scaffolds, based on recent literature.
Table 1: Benchmarking Targets for Scaffold Performance
| Performance Indicator | Native Articular Cartilage | Native Cardiac Tissue | Typical 3D-Printed Scaffold (PCL/Gelatin) | Target for 4D-Printed Smart Scaffold (e.g., Shape-Memory Polymer) | Standard Test Method |
|---|---|---|---|---|---|
| Young's Modulus (Compressive) | 0.5 - 2 MPa | 10 - 50 kPa (relaxed) | 1 - 10 MPa (tuned via porosity) | 0.1 - 2 MPa (stimuli-responsive range) | ASTM D695 / ISO 604 |
| Ultimate Tensile Strength (UTS) | 5 - 25 MPa | 20 - 100 kPa | 2 - 15 MPa | 1 - 10 MPa (pre/post-transformation) | ASTM D638 |
| Porosity | N/A (dense ECM) | N/A (dense ECM) | 50 - 80% | 60 - 85% (dynamic porosity) | Micro-CT Analysis |
| Pore Size | N/A | N/A | 100 - 500 µm | 200 - 600 µm (changeable) | SEM Image Analysis |
| Degradation Rate (mass loss) | N/A (homeostatic) | N/A (homeostatic) | 5-20% / month (hydrolytic) | 5-30% / month (stimuli-responsive) | Gravimetric Analysis |
| Cell Viability (Post-Seeding) | N/A | N/A | 70-90% (Day 7) | >85% (pre/post-stimulus) | Live/Dead Assay (ISO 10993-5) |
| Shape Recovery Ratio (for 4D) | N/A | N/A | N/A | >95% (after stimulus) | Optical Analysis of Actuation |
Detailed Experimental Protocols
Protocol 3.1: Tri-Phasic Mechanical Benchmarking
Objective: To compare compressive, tensile, and shear moduli of native tissue, 3D-printed, and 4D-printed scaffolds.
Materials:
- Native tissue sample (e.g., porcine articular cartilage).
- 3D-printed scaffold (control, e.g., PCL).
- 4D-printed smart scaffold (e.g., photocrosslinked PLA-PEG with incorporated cellulose nanocrystals).
- Phosphate-Buffered Saline (PBS), pH 7.4.
- Universal mechanical tester (e.g., Instron 5944) with environmental chamber.
- Load cells: 10 N (for soft tissues), 500 N (for scaffolds).
Procedure:
- Hydration: Soak all samples (n=5 per group) in PBS at 37°C for 24 hours.
- Compression Test:
- Configure the tester with a 10 mm diameter platen.
- Pre-load samples to 0.01 N.
- Compress at a strain rate of 1% per minute until 20% strain is reached.
- Record force-displacement data. Calculate Young's Modulus from the linear elastic region (typically 5-15% strain).
- Tensile Test:
- Dog-bone samples (ASTM D638 Type V) are required.
- Grip samples and apply tension at a rate of 1 mm/min until failure.
- Record UTS and elongation at break.
- Shear Test:
- Use a parallel plate shear fixture.
- Apply oscillatory shear strain (0.1-10% strain, 0.1-10 Hz frequency) in a dynamic mechanical analysis (DMA) mode to determine complex shear modulus (G*).
- For 4D Scaffolds Only: Repeat steps 2-4 after applying the designated stimulus (e.g., immersion in 37°C warm water for shape recovery).
Protocol 3.2: Functional Benchmarking via Metabolic Activity and ECM Deposition
Objective: To assess the biofunctionality of scaffolds in supporting cell growth and tissue-specific matrix production compared to native tissue benchmarks.
Materials:
- Human mesenchymal stem cells (hMSCs) or tissue-specific primary cells.
- Standard cell culture medium (e.g., DMEM/F-12 + 10% FBS + 1% P/S).
- Differentiation media (e.g., chondrogenic: TGF-β3; cardiac: ascorbic acid).
- AlamarBlue or MTT assay kit.
- Quantification kits for collagen type II (COL2A1) and glycosaminoglycans (GAGs; e.g., DMMB assay) or cardiac markers (cTnT, α-actinin).
- Confocal microscope.
Procedure:
- Sterilization & Seeding: Sterilize scaffolds (UV, 70% ethanol, rinse). Seed at a density of 1x10^5 cells/scaffold.
- Culture: Maintain in standard medium for 3 days, then switch to differentiation medium for up to 28 days.
- Metabolic Activity (Weekly):
- Incubate samples in medium with 10% AlamarBlue reagent for 4 hours at 37°C.
- Measure fluorescence (Ex560/Em590). Report as % reduction relative to control.
- ECM Deposition Analysis (Day 14, 28):
- GAG Content: Digest samples in papain buffer (65°C, 24h). Mix digestate with DMMB reagent and measure absorbance at 525 nm. Compare to a chondroitin sulfate standard curve.
- Immunofluorescence Staining: Fix samples (4% PFA), permeabilize (0.1% Triton X-100), block (5% BSA), and incubate with primary antibodies (anti-COL2A1, anti-α-actinin). Stain with fluorescent secondaries and DAPI. Image via confocal microscopy and quantify fluorescence intensity/area.
Visualization Diagrams
Diagram 1: Benchmarking Workflow for 4D Scaffold R&D
Diagram 2: 4D Scaffold Mechanotransduction Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Benchmarking Experiments
| Item | Function in Benchmarking | Example Product/Specification |
|---|---|---|
| Shape-Memory Polymer (SMP) | Core material for 4D printing; provides stimuli-responsive shape change. | Photocurable PLA-PEG resin with cellulose nanocrystal fillers. |
| Bioactive Ceramic Fillers | Enhances osteoconductivity and modulates scaffold stiffness. | β-Tricalcium Phosphate (β-TCP) powder, < 100 nm particle size. |
| Crosslinking Agent | Provides structural integrity and can be stimuli-cleavable for dynamic softening. | Methacrylated gelatin (GelMA), N,N'-methylenebisacrylamide (MBAA). |
| Live/Dead Viability/Cytotoxicity Kit | Dual-fluorescence staining for immediate post-printing and post-stimulus cell viability assessment. | Thermo Fisher Scientific, Kit containing Calcein AM (live/green) & Ethidium homodimer-1 (dead/red). |
| Glycosaminoglycan (GAG) Assay | Quantifies cartilage-like matrix deposition, key functional benchmark. | Blyscan Sulfated GAG Assay (Biocolor) or DMMB-based kits. |
| Tissue-Specific Growth Factors | Drives seeded cells toward target lineage for functional comparison to native tissue. | Recombinant Human TGF-β3 (chondrogenesis), VEGF (vascularization). |
| Dynamic Mechanical Analyzer (DMA) with Environmental Chamber | Measures viscoelastic properties (storage/loss modulus) under controlled stimuli (temp, hydration). | TA Instruments Q800 with submersion clamp. |
| Micro-Computed Tomography (Micro-CT) Scanner | Non-destructively quantifies 3D porosity, pore size distribution, and degradation over time. | Scanco Medical µCT 50, resolution < 10 µm. |
Within the thesis on "4D Printing of Smart Biomaterials for Dynamic Tissue Scaffolds," in vivo animal studies are the critical translational step to validate scaffold performance. These studies assess the dynamic, time-dependent (4th dimension) response of printed scaffolds—such as shape-morphing, degradation, or stimulus-responsive drug release—and their ability to guide functional tissue regeneration. This document provides application notes and detailed protocols for key in vivo evaluations.
Key Evaluation Parameters & Quantitative Metrics
Table 1: Core In Vivo Evaluation Parameters for 4D-Printed Scaffolds
| Parameter | Key Metrics | Common Assessment Methods | Typical Timeline (Post-Implant) |
|---|---|---|---|
| Host Integration | - Fibrous capsule thickness (µm)- Direct bone/implant contact (%)- Presence of M1/M2 macrophages | - Histology (H&E, Masson's Trichrome)- Immunofluorescence (CD68, CD206)- Micro-CT (for bone) | 2, 4, 8, 12 weeks |
| Vascularization | - Vessel density (vessels/mm²)- Vessel diameter (µm)- Perfusion (contrast uptake) | - Immunohistochemistry (CD31, α-SMA)- Laser Doppler perfusion imaging- Micro-CT angiography | 1, 2, 4, 8 weeks |
| Functional Tissue Formation | - New bone volume/Tissue volume (BV/TV, %)- Collagen alignment/organization- Biomechanical strength (MPa) | - Histology (special stains)- Micro-CT analysis- Tensile/compression testing | 4, 8, 12, 24 weeks |
| Scaffold Degradation & 4D Response | - Mass loss (%)- Shape change angle (°) or strain (%)- Porosity change (%) | - Explant weight measurement- Ex vivo micro-CT/Microscopy- Serum polymer byproducts (HPLC) | Serial time points |
Detailed Experimental Protocols
Protocol 3.1: Subcutaneous Implantation for Initial Biocompatibility & Vascularization
Objective: To assess early host response, integration, and angiogenic potential of a 4D-printed scaffold. Animal Model: Immunocompetent mouse (e.g., C57BL/6) or rat. Materials: See "Scientist's Toolkit" (Section 5). Procedure:
- Pre-surgical: Sterilize scaffolds (Ethylene Oxide or 70% EtOH + UV). Anesthetize animal.
- Implantation: Make a 1-1.5 cm dorsal midline incision. Create subcutaneous pockets bilaterally using blunt dissection.
- Insertion: Place one scaffold per pocket. For 4D activation, a stimulus (e.g., PBS for hydration-triggered morphing) can be applied in situ before wound closure.
- Closure: Suture muscle layer with absorbable suture (e.g., Vicryl 5-0) and skin with non-absorbable suture or staples.
- Post-op: Administer analgesia (Buprenorphine) and monitor daily.
- Endpoint & Analysis: Euthanize at predetermined time points (e.g., 1, 2, 4 weeks).
- Explant: Harvest scaffold with surrounding tissue.
- Fixation: Immerse in 4% PFA for 24-48h.
- Analysis: Process for histology (H&E, Trichrome) and IHC (CD31 for endothelial cells).
Protocol 3.2: Critical-Sized Calvarial Defect for Bone Regeneration
Objective: To evaluate osteointegration and guided bone formation by an osteoconductive/inductive 4D scaffold. Animal Model: Rat (e.g., Sprague Dawley) or mouse. Procedure:
- Defect Creation: Make a midline scalp incision, expose the parietal bones. Using a trephine bur (5-8 mm diameter) under constant saline irrigation, create a full-thickness defect.
- Implantation: Irrigate defect. Implant the 4D scaffold, ensuring snug fit. The scaffold's 4D shape-memory may be triggered by body heat to conform to defect margins.
- Closure: Sutured periosteum and skin.
- Endpoint & Analysis: Euthanize at 8-12 weeks.
- Micro-CT Scan: Ex vivo scan of explanted calvarium at high resolution (10-20 µm). Analyze for BV/TV (%) and bone mineral density (mg HA/ccm).
- Histology: Decalcify explants, section, stain with H&E, Masson's Trichrome, and for osteocalcin (IHC).
Protocol 3.3: Doppler Perfusion Imaging for Vascularization Quantification
Objective: To non-invasively monitor functional blood vessel formation within and around an implanted scaffold. Equipment: Laser Doppler Perfusion Imager (e.g., Moor Instruments). Procedure:
- Animal Preparation: Anesthetize and depilate the implantation area.
- Baseline Scan: Acquire a pre-implantation perfusion map.
- Longitudinal Scanning: At weekly intervals, position the animal under the scanner. Maintain body temperature (heating pad) to ensure consistent blood flow.
- Image Acquisition: Capture 2D perfusion images. Use a consistent region of interest (ROI) covering the implant site and contralateral control tissue.
- Data Analysis: Use instrument software to calculate perfusion units (PU) within the ROI. Express data as a ratio of implant site PU to control site PU.
Signaling Pathways in Host Response & Integration
Diagram 1: Key Signaling Pathways in Scaffold Integration & Vascularization
Diagram 2: Experimental Workflow for In Vivo Evaluation
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Materials for In Vivo Studies
| Item | Function/Application | Example Product/Catalog |
|---|---|---|
| 4D-Printed Scaffold | The test article; provides 3D structure and dynamic, time-dependent functionality. | Custom fabricated from shape-memory polymer (e.g., PCL/PLGA blends) or stimulus-responsive hydrogel. |
| Animal Model | Provides the physiological environment for testing. | Rodent (mouse/rat) for screening; large animal (rabbit, sheep) for pre-clinical. |
| Isoflurane & System | Safe and controllable inhalation anesthesia for rodents. | VetFlo or similar precision vaporizer. |
| Buprenorphine SR | Extended-release analgesic for post-operative pain management. | Buprenorphine SR-Lab (0.5-1.0 mg/kg, SC). |
| Paraformaldehyde (4%) | Tissue fixative for preserving explant morphology for histology. | Prepared from PFA powder or commercial solution. |
| Primary Antibodies (IHC) | Label specific cell types for analysis (e.g., endothelial cells, macrophages). | Anti-CD31 (vascular endothelium), Anti-CD68 (pan-macrophage), Anti-OSTEOCALCIN (osteoblasts). |
| Laser Doppler Perfusion Imager | Non-invasive measurement of functional blood flow (perfusion). | Moor Instruments moorFLPI-2. |
| High-Resolution Micro-CT Scanner | Ex vivo 3D quantification of bone formation and scaffold architecture/degradation. | Scanco Medical μCT 50, Bruker Skyscan 1276. |
| Histology Embedding Media | For paraffin or cryo-sectioning of explanted tissue-scaffold constructs. | Paraplast X-TRA, OCT Compound. |
| Special Stains | Differentiate tissue components in histological sections. | Masson's Trichrome (collagen), Alizarin Red (calcium), Tartrate-Resistant Acid Phosphatase (osteoclasts). |
Within the thesis framework of 4D printing for dynamic tissue scaffolds, the choice of base biomaterial is paramount. Electrospinning and decellularized extracellular matrix (dECM) represent two foundational approaches for scaffold fabrication, each offering distinct advantages and drawbacks for creating "smart" platforms that can morph or respond post-printing (the 4th dimension). This analysis provides a comparative overview and detailed protocols for their application in this advanced context.
Quantitative Comparison: Strengths and Limitations
Table 1: Head-to-Head Comparative Analysis
| Parameter | Electrospinning | Decellularized ECM (dECM) |
|---|---|---|
| Primary Strength | Superior control over fiber diameter (50 nm - 10 µm), alignment, and porosity. High surface-to-volume ratio. Excellent mechanical tunability. | Innate biological complexity. Contains native tissue-specific proteins, glycosaminoglycans (GAGs), and cytokines. Inherent bioactivity and cell-instructive cues. |
| Key Limitation | Limited mimicry of natural ECM complexity. Often requires post-processing for biofunctionalization. Potential small pore size limiting cell infiltration. | Batch-to-batch variability. Inherently weak mechanical properties (low stiffness, rapid degradation). Difficult to process into stable, complex 3D/4D structures. |
| Typical Fiber Diameter | 50 nm - 5 µm (common range for tissue engineering) | Not applicable (nanofibrous but not discrete, continuous fibers) |
| Elastic Modulus (Approx.) | 1 - 2000 MPa (highly tunable with polymer blend) | 0.1 - 50 kPa (highly tissue-source dependent) |
| Degradation Rate | Days to years (precisely tunable via polymer chemistry) | Hours to weeks (enzymatic, rapid unless crosslinked) |
| Bioactivity | Low (unless functionalized with peptides, proteins, or blended with dECM) | Very High (native ligands and signals) |
| Suitability for 4D Printing | High. Compatible with melt- or solution-based 3D printing (e.g., melt electrowriting). Ideal for creating anisotropic, shape-morphing scaffolds via programmed fiber alignment. | Moderate. Often used as a bioink component. Enables 4D responses via cell-driven contraction or matrix remodeling. Pure dECM lacks structural integrity for freestanding 4D constructs. |
| Process Scalability | High for random mats; moderate for aligned/patterned constructs. | Low to Moderate. Tissue sourcing and decellularization are resource-intensive. |
| Cost & Throughput | Relatively low cost, moderate to high throughput. | High cost, low to moderate throughput. |
Application Notes & Detailed Protocols
Protocol 3.1: Fabrication of Anisotropic, Shape-Memory PLGA/Gelatin Electrospun Scaffolds for 4D Applications
- Objective: To create a bilayer electrospun mesh capable of temperature-triggered shape change (self-folding) for dynamic tissue scaffolding.
- Materials:
- Solution A: 12% w/v PLGA (85:15 LA:GA) in Hexafluoro-2-propanol (HFIP).
- Solution B: 10% w/v Gelatin (Type A) in Acetic Acid (90% v/v).
- Programmable syringe pumps, high-voltage power supply (0-30 kV), cylindrical mandrel collector.
- Method:
- Bilayer Fabrication: Electrospin Solution A (PLGA) for 2 hours at 18 kV, 1.5 mL/hr, 15 cm tip-to-collector distance onto a flat collector to create a first layer.
- Immediately electrospin Solution B (Gelatin) onto the same PLGA mat for 1 hour at 15 kV, 1.0 mL/hr. This creates a integrated bilayer.
- Programming the 4D Shape: Cut the bilayer mat into strips (10mm x 2mm). Heat to 37°C (above gelatin's glass transition) and manually deform into a coiled "temporary" shape. Cool and fix at 4°C for 12 hours.
- 4D Activation: Upon immersion in 37°C PBS, the gelatin layer softens, allowing the stored elastic energy in the PLGA layer to release, causing the coil to unroll into its "permanent" flat shape. The shape-change kinetics can be quantified via time-lapse imaging.
Protocol 3.2: Preparation of a Cardiac dECM Bioink for 4D Cell-Driven Scaffold Remodeling
- Objective: To generate a printable, cell-laden dECM hydrogel bioink that undergoes cell-mediated contraction and alignment post-printing (4D biological transformation).
- Materials:
- Porcine or rat ventricular tissue.
- Decellularization reagents: 1% (w/v) Sodium Dodecyl Sulfate (SDS), 1% (v/v) Triton X-100, DNase/RNase solutions, PBS.
- Lyophilizer, pepsin (from porcine gastric mucosa), 0.1M HCl.
- Method:
- Decellularization: Mince ventricular tissue. Stir in 1% SDS for 48h, rinse in PBS for 72h. Treat with 1% Triton X-100 for 24h. Incubate with DNase/RNase (50 U/mL) for 6h at 37°C. Perform extensive washing until no detergent remains.
- dECM Bioink Processing: Lyophilize the acellular matrix. Mill into powder. Digest with 0.1M HCl containing 1% (w/w) pepsin at room temperature for 48h until a viscous solution forms.
- Printing & 4D Culture: Neutralize the pre-gel solution on ice with 0.1M NaOH and 10x PBS. Mix with human cardiac fibroblasts (5 x 10^6 cells/mL). Extrude into a grid structure using a cold print bed (4°C). Incubate at 37°C for 30 min to gel.
- 4D Observation: Over 7-14 days in culture, cell-generated forces will cause the soft dECM lattice (initial storage modulus ~500 Pa) to globally contract (>30% area reduction) and locally align, forming a denser, anisotropic tissue-like construct. Monitor via confocal microscopy of actin cytoskeleton.
Visualized Workflows and Pathways
Electrospinning Fabrication Workflow
Tissue Decellularization Pathway
Cell-Driven 4D Remodeling of dECM
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Featured Experiments
| Reagent/Material | Supplier Examples | Key Function in Protocol |
|---|---|---|
| PLGA (85:15) | Sigma-Aldrich, Lactel Absorbable Polymers | Synthetic polymer backbone providing structural integrity and tunable degradation for electrospun scaffolds. |
| Hexafluoro-2-propanol (HFIP) | Apollo Scientific, Sigma-Aldrich | High-volatility solvent for electrospinning synthetic polymers like PLGA, enabling fine fiber formation. |
| Gelatin, Type A | Gelita, Sigma-Aldrich | Natural polymer providing thermoresponsive behavior and improved cell adhesion in composite electrospun fibers. |
| Sodium Dodecyl Sulfate (SDS) | Bio-Rad, Thermo Fisher Scientific | Ionic detergent for decellularization; lyses cells and solubilizes cytoplasmic components. |
| Triton X-100 | Sigma-Aldrich, Thermo Fisher Scientific | Non-ionic detergent for decellularization; disrupts lipid-lipid and lipid-protein interactions. |
| DNase I / RNase A | Worthington Biochemical, Qiagen | Enzymes that degrade residual nucleic acids after detergent treatment, reducing immunogenic potential. |
| Pepsin | Sigma-Aldrich | Enzyme used to digest dECM into a solubilized pre-gel for bioink formulation. |
| Matrigel (or Collagen I) | Corning | Often used as a comparator or additive to dECM bioinks to modulate gelation kinetics and mechanics. |
| Live/Dead Viability Assay Kit | Thermo Fisher Scientific, Biotium | Standard assay to quantify cell viability and cytocompatibility of fabricated scaffolds post-printing/processing. |
Within the broader thesis on 4D printing of smart biomaterials for dynamic tissue engineering, establishing standardized success metrics is paramount. 4D scaffolds are defined as three-dimensionally printed constructs fabricated from stimuli-responsive ("smart") biomaterials that undergo predefined, time-dependent morphological or functional changes in response to specific physiological or external triggers. This document outlines the critical characterization standards and protocols necessary to quantitatively evaluate the success of these dynamic systems, ensuring reproducibility and meaningful comparison across research studies for both academic and translational drug development applications.
Core Success Metrics: Quantitative Framework
The success of a 4D scaffold is multi-faceted. The following table consolidates the primary quantitative metrics into a standardized framework.
Table 1: Core Quantitative Metrics for 4D Scaffold Evaluation
| Metric Category | Specific Parameter | Measurement Technique(s) | Target/Desired Outcome (Example) | Relevance to Dynamic Function |
|---|---|---|---|---|
| Printability & Initial Structure | Printing Fidelity | Micro-CT, SEM | >95% match to CAD model | Ensures precise starting geometry for predictable transformation. |
| Porosity & Pore Size | Micro-CT, Mercury Porosimetry | 60-80% porosity, 100-300 μm pore size | Dictates cell infiltration, nutrient diffusion, and deformation mechanics. | |
| Dynamic Transformation | Transformation Kinetics | Time-lapse imaging, DIC | Complete shape change in 24-48h (physiological) | Defines the "4th Dimension" - rate of response. |
| Trigger Specificity | Controlled stimulus application | Response only within ±10% of target pH/Temp/etc. | Ensures spatiotemporal control in biological environments. | |
| Shape Change Accuracy | 3D vs. 4D model comparison | >90% geometric accuracy to predicted final state | Fidelity of the programmed response. | |
| Actuation Force | Micromechanical load cells | 1-10 mN (tissue-scale relevant) | Ability to exert mechanical influence on cells/tissue. | |
| Mechanical Properties | Modulus (Initial/Final) | Dynamic Mechanical Analysis (DMA), AFM | 0.1-10 kPa (soft tissue matching) | Mechanical cues for cell differentiation; integrity during change. |
| Cyclic Durability | Fatigue testing | >1000 transformation cycles without failure | For scaffolds intended for pulsatile or repetitive stimuli. | |
| Biological Performance | Cytocompatibility (Post-Transformation) | Live/Dead assay, ISO 10993-5 | >90% cell viability | Non-toxic transformation byproducts/conditions. |
| Cell Alignment/ Differentiation | Immunofluorescence, qPCR | Alignment index >0.8; Upregulation of target markers | Evidence of beneficial cell guidance from dynamic cues. | |
| Degradation Rate (in situ) | Mass loss, GPC | Matches tissue ingrowth rate (e.g., 3-6 months) | Synchronization of scaffold disappearance with new tissue formation. |
Application Notes & Detailed Protocols
AN-1: Protocol for Quantifying pH-Triggered Shape Change Kinetics
Application: This protocol is designed for hydrogels containing pH-sensitive moieties (e.g., carboxylate groups) intended for dynamic scaffolds in environments with shifting pH (e.g., during inflammation or tumor targeting).
Research Reagent Solutions & Essential Materials:
| Item | Function |
|---|---|
| 4D Bioink (e.g., Alginate-Methacrylate/Chitosan) | pH-responsive hydrogel matrix providing the dynamic shape-morphing capability. |
| Phosphate Buffered Saline (PBS), 1x | Physiological ionic strength buffer for maintaining osmolarity during testing. |
| HCl (0.1M) and NaOH (0.1M) Solutions | For precise titration and adjustment of pH in the immersion medium. |
| Calcein-AM Stain | Fluorescent live-cell dye for simultaneous visualization of cells and scaffold deformation (if cell-laden). |
| Confocal or Macro Time-Lapse Imaging System | For capturing high-resolution 3D images over time to quantify geometric changes. |
| Digital pH Meter with Micro-probe | For accurate, real-time monitoring of environmental pH. |
| Analysis Software (e.g., ImageJ/FIJI, MATLAB) | For processing time-lapse images and calculating deformation metrics. |
Experimental Workflow:
- Scaffold Fabrication: Print scaffold using established parameters (e.g., DIW, SLA) into a neutral pH (7.4) gelation bath. Cure/ crosslink fully.
- Baseline Imaging: Acquire high-resolution 3D scan (micro-CT or confocal stack) of scaffold in PBS at pH 7.4. This is the reference geometry (G_ref).
- Trigger Initiation: Rapidly transfer scaffold to a pre-warmed (37°C) immersion bath at target trigger pH (e.g., pH 6.5). Start timer and pH recording.
- Time-Lapse Acquisition: Immediately begin time-lapse imaging. For macro deformation, use a fixed-interval (e.g., 30 sec) 2D setup. For 3D volumetric change, acquire confocal z-stacks at longer intervals (e.g., 5 min).
- Data Acquisition Period: Continue until no further geometric change is observed (plateau).
- Data Analysis:
- Shape Recovery Ratio (R):
R(t) = (A_0 - A_t) / (A_0 - A_f), where A is a geometric parameter (angle, diameter),A_0is initial,A_tis at time t, andA_fis final. - Rate Constant (k): Fit
R(t)vs.tdata to a suitable kinetic model (e.g., exponential association) to derivek. - Final Fidelity: Calculate % similarity between final scanned geometry (Gfinal) and the digitally predicted target geometry (Gtarget) using 3D registration software.
- Shape Recovery Ratio (R):
Protocol Title: Quantifying pH-Triggered Shape Change Kinetics
AN-2: Protocol for Integrated Bio-Mechanical Characterization During Transformation
Application: To evaluate the evolving mechanical properties of a 4D scaffold during its shape change, providing crucial data for predicting cell response and in vivo performance.
Experimental Workflow:
- Instrument Setup: Mount a DMA rheometer with a plate-plate geometry or a tensile tester in a climate-controlled chamber. Equip with a fluid bath if testing in liquid.
- Scaffold Loading: Carefully load the pre-shaped 4D scaffold onto the test fixtures. For rheology, use a slight normal force to ensure contact.
- Equilibration: Allow scaffold to equilibrate in testing environment (e.g., 37°C, pH 7.4 buffer) for 15 min.
- Baseline Measurement: Perform a frequency sweep (e.g., 0.1-10 Hz) at 1% strain to establish initial storage (G') and loss (G'') moduli.
- Trigger Application & Real-Time Monitoring: Introduce the stimulus to the chamber/bath.
- Method A (Chemical): Gently perfuse trigger buffer (e.g., low pH) while sealing chamber.
- Method B (Thermal): Program chamber temperature change.
- Continuous Oscillatory Test: Immediately initiate a time-sweep experiment (fixed low frequency and strain) to monitor G' and G'' continuously throughout the transformation period.
- Post-Transformation Sweep: Once moduli plateau, perform a final frequency sweep to characterize the final mechanical state.
- Data Analysis: Plot G'(t) and G''(t) to identify the trigger latency, rate of mechanical change, and final modulus. Correlate with visual time-lapse data.
Protocol Title: Biomechanical Characterization During 4D Transformation
Pathway for 4D Scaffold-Mediated Cell Guidance
The ultimate success metric is the ability to direct cell behavior through dynamic cues. The following pathway summarizes key mechanotransduction and signaling events initiated by a transforming scaffold.
Diagram Title: Cell Signaling Pathway for 4D Scaffold Guidance
Standardized Experimental Workflow for 4D Scaffold Validation
A comprehensive validation pipeline integrates all characterization modules.
Diagram Title: Comprehensive 4D Scaffold Validation Workflow
Conclusion
4D printing of smart biomaterials represents a paradigm shift in tissue engineering, moving from passive, static implants to active, dynamic systems that guide biological processes. This synthesis demonstrates that success hinges on a deep understanding of material science (Intent 1), refined fabrication and programming techniques (Intent 2), robust solutions to biocompatibility and manufacturing challenges (Intent 3), and rigorous biological validation against established benchmarks (Intent 4). The future of the field lies in developing more sophisticated, multi-stimuli-responsive materials, achieving higher resolution in 4D bioprinting with living cells, and advancing towards patient-specific, clinically translatable implants. This technology holds immense promise not only for regenerative medicine but also for advanced in vitro disease models and smart drug delivery platforms, ultimately enabling more harmonious integration between synthetic constructs and living biology.