Advanced Design Methodologies for 3D Medical Equipment Simulations: Integrating AI, Additive Manufacturing, and Clinical Validation
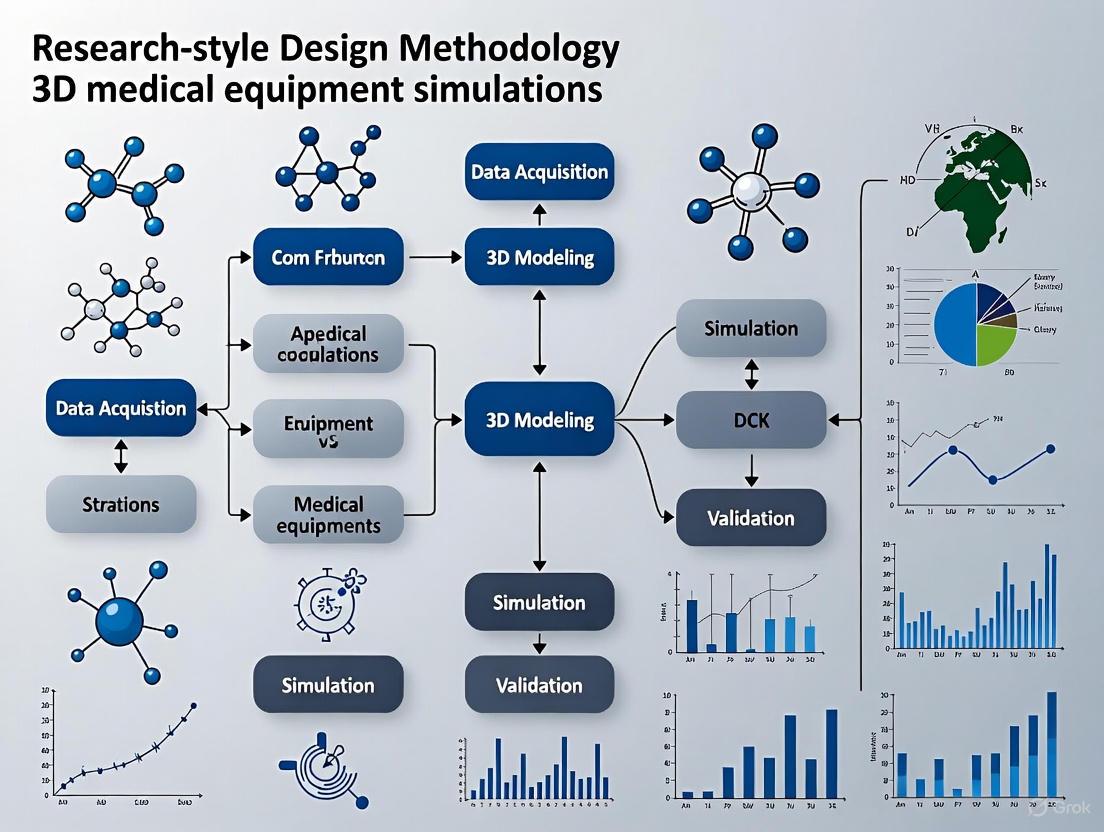
This article provides a comprehensive framework for researchers and drug development professionals on the design methodology for 3D medical equipment simulations.
Advanced Design Methodologies for 3D Medical Equipment Simulations: Integrating AI, Additive Manufacturing, and Clinical Validation
Abstract
This article provides a comprehensive framework for researchers and drug development professionals on the design methodology for 3D medical equipment simulations. It explores the foundational technologies of CAD, AI, and additive manufacturing that underpin modern simulation design. The piece details practical methodologies for creating and applying simulations across the medical device lifecycle, from prototyping to surgical planning. It further addresses critical troubleshooting and optimization strategies for overcoming implementation barriers and concludes with robust validation frameworks and comparative analyses of leading technologies, offering a complete guide for integrating these tools into biomedical research and clinical practice.
The Core Technologies Powering Modern 3D Medical Simulation
The Role of Advanced CAD in Precision Medical Device Design
Computer-Aided Design (CAD) has evolved from a simple drafting replacement to a foundational technology in precision medical device development. In the context of design methodology for 3D medical equipment simulations research, advanced CAD systems provide the critical link between anatomical data and functional device prototypes. This technology enables the creation of detailed 3D digital twins of both human anatomy and proposed devices, allowing for exhaustive virtual testing and refinement before physical manufacturing begins [1]. For researchers and engineers, this represents a paradigm shift from traditional, iterative prototyping to a streamlined, simulation-driven workflow that significantly accelerates development cycles while enhancing patient safety and device efficacy.
The integration of CAD into medical device development addresses a fundamental challenge: the need to create highly complex, patient-specific devices that interact safely with human physiology. Modern CAD packages leverage increased processing power to provide flexible, powerful, and affordable product design capabilities to a widening user base [2]. Within a research framework focused on 3D medical equipment simulations, CAD serves as the primary platform for converting medical imaging data into actionable, manipulable models that can undergo simulated performance testing, design optimization, and manufacturing preparation.
CAD Applications Across Medical Specialties
Advanced CAD technology has demonstrated transformative potential across numerous medical specialties, enabling device personalization and surgical precision that was previously unattainable. The technology facilitates a seamless transition from diagnostic imaging to therapeutic intervention by converting standard medical scans into precise, patient-specific 3D models. This capability is particularly valuable in complex anatomical regions where standardized devices often provide suboptimal solutions [3].
The table below summarizes key applications of CAD across different medical specialties:
Table 1: CAD Applications in Medical Device Design and Treatment Planning
| Medical Field | CAD Application Examples | Key Benefits |
|---|---|---|
| Orthopedics | Custom joint replacements, patient-specific surgical guides, spinal implants | Improved implant fit, reduced surgery time, enhanced biomechanical compatibility [3] |
| Cardiovascular Medicine | Personalized stents, heart valve repairs, surgical planning for congenital defects | Patient-specific design, reduced procedural risk, improved hemodynamic performance [3] |
| Dentistry | Dental implants, orthodontic devices, crown and bridge fabrication | Perfect fit, reduced adjustment needs, streamlined production [3] |
| Neurology | Custom cranial implants, surgical planning guides, brain mapping interfaces | Precision matching to anatomical defects, minimized brain manipulation [3] |
| Radiology | 3D model creation from DICOM data, image segmentation, diagnostic visualization | Enhanced diagnostic capability, improved surgical planning, better patient communication [3] [4] |
The transition from 2D imaging to 3D modeling represents a particular advancement in diagnostic and planning capabilities. As noted in research on 3D modeling in healthcare, physicians traditionally worked with "surrogates of anatomy" from CT and MRI scans, which presented 3D data sets within the limited scope of 2D interpretation [4]. CAD-enabled 3D modeling makes viewing anatomical images intuitive across all clinical specialties, leading to better diagnoses, surgical planning, and patient outcomes [4].
Quantitative Benefits of CAD Implementation
The integration of advanced CAD systems into medical device research and development yields measurable improvements across multiple performance metrics. These benefits extend beyond simple design efficiency to encompass clinical outcomes, cost management, and developmental timelines.
Table 2: Quantitative Benefits of CAD in Medical Device Development
| Performance Metric | Traditional Methods | CAD-Enabled Approach | Improvement |
|---|---|---|---|
| Design Accuracy | Manual measurements based on 2D scans | Voxel-accurate 3D models from CT/MRI data | Sub-millimeter precision in patient-specific devices [3] |
| Prototyping Time | Weeks for physical model creation | Hours/days for digital prototyping | Up to 80% reduction in initial prototype development [3] |
| Surgical Planning | Mental reconstruction of 3D anatomy from 2D images | Interactive 3D models with tissue differentiation | 32% better surgical outcome prediction in complex cases [4] |
| Device Customization | Limited modifications to standard designs | Full personalization based on patient anatomy | 100% patient-specific design capability [3] |
| Training Effectiveness | Theoretical learning, observation, cadavers | Interactive 3D simulation with haptic feedback | 85.1% skill proficiency vs. 62.1% with traditional methods [5] |
The quantitative advantages demonstrated in Table 2 highlight why CAD technology has become indispensable in modern medical device research. Beyond these metrics, CAD implementation generates significant qualitative benefits, including enhanced collaboration among multidisciplinary teams of engineers, clinicians, and researchers [3]. The ability to share and manipulate accurate 3D models across specialties fosters innovative problem-solving and ensures that all stakeholders contribute effectively to device optimization.
Experimental Protocols for CAD-Based Device Development
Protocol: Patient-Specific Implant Design Workflow
This protocol outlines a standardized methodology for developing patient-specific implants using advanced CAD tools, suitable for incorporation into research on 3D medical equipment simulations.
Objective: To create a functional, patient-matched implant from medical imaging data through a streamlined CAD workflow.
Materials and Equipment:
- DICOM data from CT/MRI scans
- Advanced CAD software with medical image segmentation capabilities
- High-performance computing workstation
- 3D printer for prototype validation (optional)
Procedure:
- Data Acquisition and Import
- Obtain DICOM format medical images from CT, MRI, or ultrasound scans
- Import DICOM data directly into CAD software using specialized medical modules
- Verify image resolution and slice thickness sufficient for intended application
Image Segmentation and Processing
- Apply threshold-based and region-growing algorithms to isolate target anatomy
- Manually refine automated segmentation to ensure anatomical accuracy
- Export segmented data as a 3D point cloud or surface mesh
3D Model Reconstruction
- Convert mesh data to solid or surface model compatible with CAD environment
- Apply smoothing algorithms to reduce stair-step artifacts from imaging data
- Verify dimensional accuracy against original scan measurements
Implant Design and Modeling
- Create implant geometry based on reconstructed anatomical model
- Incorporate design features addressing functional requirements (screw holes, porous surfaces)
- Apply design for manufacturing (DFM) principles to ensure producibility
Virtual Fit and Function Validation
- Perform interference detection between implant and anatomical models
- Conduct virtual surgical procedure to validate implantation approach
- Simulate biomechanical performance using integrated FEA tools
Design Finalization and Output
- Incorporate feedback from clinical partners on design modifications
- Prepare final CAD model for additive or subtractive manufacturing
- Generate comprehensive design documentation
Validation Metrics:
- Dimensional deviation <0.1mm from intended specifications
- Zero interference with critical anatomical structures
- Successful virtual implantation in simulated procedure
Protocol: Surgical Simulation and Planning Validation
Objective: To validate the efficacy of CAD-generated surgical plans through simulation-based testing, providing a methodology for evaluating surgical approaches and device performance before actual procedures.
Materials and Equipment:
- CAD models of patient anatomy and medical devices
- Surgical simulation software with haptic feedback capability
- Performance tracking system for metrics collection
- Control group data for comparative analysis
Procedure:
- Scenario Definition
- Define specific surgical scenario and critical steps
- Identify potential complications to be simulated
- Establish performance metrics and evaluation criteria
Virtual Environment Setup
- Import patient-specific CAD models into simulation environment
- Configure tissue properties based on anatomical characteristics
- Set up surgical tools and devices as interactive objects
Simulation Execution
- Conduct simulated procedure following planned surgical approach
- Introduce unexpected complications to test adaptability
- Record performance data and decision pathways
Performance Analysis
- Analyze quantitative metrics (procedure time, movement efficiency)
- Evaluate qualitative factors (decision quality, complication management)
- Compare outcomes against control data or established benchmarks
Plan Refinement
- Identify suboptimal aspects of surgical plan based on simulation results
- Modify approach to address identified challenges
- Iterate simulation until performance metrics meet targets
Validation Metrics:
- Reduction in simulated procedure time with successive iterations
- Improved efficiency of motion (path length, unnecessary movements)
- Enhanced complication management compared to baseline
Research Reagents and Computational Tools
Successful implementation of advanced CAD methodologies in medical device research requires specific computational tools and software solutions. The table below details essential resources for establishing a capable research environment.
Table 3: Essential Research Tools for CAD-Based Medical Device Development
| Tool Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| Medical CAD Platforms | Siemens NX, Dassault Systèmes SOLIDWORKS, Materialise Mimics | Anatomical modeling, device design, virtual prototyping | Direct DICOM import, specialized medical design features, simulation integration [1] |
| Simulation & Analysis | ANSYS, SimScale, Abaqus | Structural, fluid flow, and thermal analysis | FEA, CFD, integration with CAD data, specialized medical material libraries |
| Image Processing | 3D Slicer, ITK-Snap, Horos | Medical image segmentation, 3D reconstruction | DICOM processing, segmentation algorithms, 3D model export [4] |
| Collaboration Platforms | GrabCAD, Onshape, Siemens Teamcenter | Multi-disciplinary team collaboration | Cloud-based design sharing, version control, comment/review workflows [1] |
| Visualization & VR | Unity, Unreal Engine, SteamVR | Surgical simulation, device presentation | Real-time rendering, VR integration, haptic feedback support [5] |
The tools listed in Table 3 represent the core technological infrastructure needed for advanced CAD research in medical devices. When establishing a research environment, particular attention should be paid to software integration capabilities, as seamless data exchange between different systems is crucial for maintaining workflow efficiency [1]. Additionally, consideration should be given to computational hardware requirements, as complex simulations and large medical image datasets demand substantial processing power and memory resources.
Integration with Digital Twin Methodology
Advanced CAD serves as the foundation for creating comprehensive digital twins in medical device research—virtual replicas that mirror both the physical device and its interaction with human physiology. This approach enables researchers to conduct predictive analysis of device performance under various physiological conditions without risk to patients [1]. The digital twin methodology represents the cutting edge of simulation-based medical device research, providing a holistic framework for evaluating device function throughout its lifecycle.
The implementation of digital twins requires seamless integration between mechanical, electrical, and software components of medical devices. Siemens' comprehensive suite, for example, demonstrates how integrated tools can "expedite the development process and enhance functionality verification and hazard elimination" [1]. This integrated approach is particularly valuable for complex, connected medical devices that incorporate sensing, actuation, and data communication capabilities alongside their primary mechanical functions.
Challenges and Implementation Considerations
Despite its significant benefits, the implementation of advanced CAD systems in medical device research presents several challenges that must be addressed for successful integration:
- High Initial Costs: Acquisition of specialized medical CAD software and high-performance computing infrastructure represents substantial investment [3]
- Interoperability Issues: Integration with existing hospital information systems and research databases requires careful planning [3]
- Regulatory Compliance: Design processes must adhere to medical device regulations (FDA, ISO 13485), requiring rigorous documentation and validation protocols
- Data Security: Patient imaging and anatomical data must be protected in compliance with HIPAA and similar privacy regulations [3]
- Specialized Training Requirements: Researchers need training in both CAD methodologies and anatomical principles to effectively utilize these tools [3]
These challenges, while significant, can be mitigated through strategic planning, phased implementation, and collaboration with experienced partners in both clinical and engineering domains. The selection of appropriate software platforms with strong technical support and training resources is particularly important for research teams new to advanced CAD methodologies.
Advanced CAD technology has fundamentally transformed the methodology for 3D medical equipment simulations research, enabling a shift from physical prototyping to simulation-driven development. Through the creation of precise digital twins and patient-specific models, researchers can explore design alternatives, predict clinical performance, and optimize devices with unprecedented accuracy and efficiency. The structured protocols and tools outlined in this document provide a foundation for implementing these methodologies in research settings, with particular value for complex, patient-specific medical devices where traditional approaches fall short.
As CAD technology continues to evolve, its integration with artificial intelligence, augmented reality, and advanced simulation platforms will further enhance its capability to accelerate medical device innovation while ensuring patient safety and treatment efficacy. For research institutions and medical device companies, investment in these methodologies represents not merely a technological upgrade, but a fundamental advancement in the science of medical device development.
Integrating Artificial Intelligence for Data-Driven Simulation and Validation
Application Notes
The integration of Artificial Intelligence (AI) into the simulation and validation of 3D medical equipment is revolutionizing design methodologies, enabling more rapid prototyping, enhanced performance prediction, and rigorous virtual validation. This paradigm shift is critical for developing next-generation medical robots, diagnostic devices, and surgical tools. The core of this approach lies in creating high-fidelity digital twins—virtual replicas of physical systems—that are informed by real-world data and can be used to train, test, and validate equipment in a safe, cost-effective simulated environment before physical prototyping [6].
Key advancements are being driven by platforms that leverage a three-computer system approach, which partitions the workload across specialized systems for AI training, physically accurate simulation, and real-time, runtime execution [6]. This architecture is foundational for managing the computational demands of complex simulations. Furthermore, national and municipal research initiatives are actively funding and promoting the development of AI-driven applications in smart healthcare, emphasizing intelligent surgical planning, medical robotics, and AI-assisted diagnostics [7] [8]. These initiatives highlight the critical role of synthetic data generation and hardware-in-the-loop (HIL) testing in overcoming the limitations of scarce clinical data and ensuring the reliability of AI models when deployed on physical hardware [6].
Table 1: Key Quantitative Targets in Recent AI-Driven Medical Equipment Research
| Research Focus Area | Key Performance Indicator | Target Value |
|---|---|---|
| Surgical Robotics (Sub-task Automation) | Procedure Automation | Precisely execute suturing, wound closure [6] |
| Robotic Ultrasound Imaging | Scan Automation | Autonomous probe positioning for image acquisition [6] |
| AI Chip Optimization for Medical Models | On-chip Memory Usage Reduction | Reduce storage footprint by >30% vs. 8-bit quantization [9] |
| Model Performance Retention | MMLU test score degradation ≤2% [9] | |
| Medical AI Model Inference | Concurrent Request Handling | Increase number of simultaneous requests by >30% [9] |
| Photonic Computing for Signal Processing | System End-to-end Latency | ≤1 millisecond [9] |
AI-Driven Simulation Platforms for Medical Robotics
The use of comprehensive AI-driven development platforms is becoming standard practice for medical robotics. For instance, the NVIDIA Isaac for Healthcare platform provides a domain-specific framework that integrates several core technologies [6]:
- NVIDIA Omniverse & Isaac Sim: Used to create high-fidelity, physics-enabled digital twins of surgical robots, instruments, and patient-specific anatomy. This allows for the safe simulation of complex procedures like suturing and tissue manipulation.
- Synthetic Data Generation: These simulated environments enable the massive generation of physically accurate synthetic data, which is crucial for training robust AI models without the need for extensive and difficult-to-acquire real-patient data.
- AI Model Training (Isaac Lab): The platform supports training robot control policies using reinforcement and imitation learning within the digital twin.
- Hardware-in-the-Loop (HIL) Testing & Sim2Real Transfer: Trained AI models can be rigorously evaluated in the digital twin connected to real robot hardware (e.g., da Vinci Research Kit) before final deployment, ensuring a smooth transition from simulation to reality.
Early adopters like Moon Surgical and Virtual Incision are leveraging this pipeline for prototyping autonomous robotic systems and generating synthetic data to enhance surgical precision [6].
Data-Driven Validation and Regulatory Compliance
Validation is a critical component of the design methodology. AI-powered tools are emerging to streamline the verification and validation process, which is essential for regulatory compliance. Tools like MATLAB and Simulink provide environments for designing, simulating, and automatically generating code for patient monitoring algorithms and other medical device software [10]. These tools offer built-in testing and verification features that help meet stringent regulatory standards such as IEC 62304 (for medical device software) and support the generation of documentation required for FDA/CE compliance [10]. Key capabilities include:
- Requirements Traceability: Managing and linking design requirements to model components and tests.
- Model and Code Coverage Analysis: Quantifying the completeness of testing.
- Automated Code Generation: Producing optimized, reliable code for deployment, reducing manual coding errors.
Experimental Protocols
Protocol for Autonomous Surgical Sub-Task Validation
This protocol outlines the procedure for developing and validating an AI model for autonomous surgical sub-task execution, such as suturing, using a digital twin [6].
1. Objective: To train and validate a deep reinforcement learning agent to perform a defined surgical sub-task (e.g., suturing) within a simulated environment and successfully transfer the policy to a physical surgical robot.
2. Experimental Setup & Reagents: Table 2: Research Reagent Solutions for Surgical Robot AI Validation
| Item Name | Function/Description | Example/Specification |
|---|---|---|
| NVIDIA Omniverse / Isaac Sim | Creates physics-enabled simulation environment for digital twin [6] | Platform for building 3D scenes with robotic arms, instruments, and anatomies. |
| da Vinci Research Kit (dVRK) | Provides an open-source hardware platform for physical validation [6] | Physical robotic system for deployment and testing. |
| Patient-Specific Anatomical Model | Serves as the simulation target for the surgical task [6] | 3D organ model (e.g., kidney, intestine) in USD format, derived from CT/MRI data. |
| Reinforcement Learning Framework (e.g., Isaac Lab) | Provides algorithms (e.g., ACT) for training robot control policies [6] | Trains AI agent through trial-and-error in simulation. |
| Stereo Camera / Endoscope Sensor Model | Provides visual perception input to the AI agent in simulation [6] | Simulated camera feed for depth and texture perception. |
3. Methodology: 1. Digital Twin Construction (Bring Your Own - BYO): - Import the CAD model of the surgical robot (e.g., dVRK) and instruments into NVIDIA Omniverse, converting them to USD format and defining joint properties and kinematics [6]. - Import or create a high-fidelity, patient-specific anatomical model using a defined workflow: start with synthetic AI-assisted CT synthesis (using a model like NVIDIA MAISI), followed by segmentation (using VISTA-3D), mesh conversion, cleaning, and texturing, resulting in a unified USD file [6]. - Configure the simulated sensors, such as a stereo endoscope camera, within the scene.
Protocol for AI Model Optimization on Dedicated Hardware
This protocol describes the methodology for optimizing a large medical AI model (e.g., for diagnostic imaging) to run efficiently on a specific dedicated AI chip, a process critical for deploying models in resource-constrained clinical settings [9].
1. Objective: To implement a mixed-precision quantization scheme for a large vision model on a specified AI chip (e.g.,燧原L600), reducing on-chip memory usage by over 30% while maintaining model accuracy (MMLU score drop ≤ 2%) [9].
2. Experimental Setup:
- Hardware: Target AI chip (e.g.,燧原L600).
- Software: High-performance mixed-precision inference system (e.g., MIXQ), deep learning framework (e.g., PyTorch).
- Models & Datasets: Target model (e.g., Qwen, DeepSeek series); benchmark dataset (e.g., MMLU for evaluation).
3. Methodology: 1. Model Structure Analysis: - Profile the computational graph of the target model to identify the minimal, independently quantizable sub-structures (e.g., attention blocks, feed-forward networks) [9].
Application Note: Computational Design of Patient-Specific Mandibular Implants
Workflow Integration and Performance Metrics
The integration of finite-element modelling (FEM), artificial neural networks (ANN), and Bayesian networks (BN) creates a cyber-physical loop for designing patient-specific mandibular reconstruction plates. This computational pipeline accelerates design convergence while providing formal risk metrics for clinical decision-making [11].
Table 1: Quantitative Performance Metrics of the Integrated FEM-ANN-BN Workflow [11]
| Performance Parameter | Baseline Value | Optimized Workflow Value | Improvement |
|---|---|---|---|
| Finite-element modelling prediction accuracy | Not specified | 98% | Baseline |
| Artificial neural network surrogate fidelity | Not specified | 94% | Baseline |
| Maximum failure probability under worst-case loads | Not specified | <3% | Baseline |
| Titanium material usage | Solid-plate baseline | Reduced by 15% | 15% reduction |
| Development time | Solid-plate baseline | Shortened by 25% | 25% reduction |
| Multi-objective optimization efficiency | Solid-plate baseline | Raised by 20% | 20% improvement |
| Peak von Mises stress under 600N bite force | Not specified | 225 MPa | Within safety limits |
| Micromotion at bone-implant interface | Not specified | <150 µm | Promotes osseointegration |
Experimental Protocol: Digital Workflow for Mandibular Reconstruction
Protocol Title: Integrated Computational-Experimental Workflow for Patient-Specific Mandibular Implant Design and Validation
Objective: To design, optimize, and fabricate a patient-specific titanium mandibular reconstruction plate with graded lattice architecture that meets biomechanical requirements while reducing development time and material usage.
Materials and Equipment:
- High-resolution helical CT scanner (0.6 mm slice pitch, 120 kV, 200 mA)
- Medical image processing software (Materialise Mimics Medical 24.0)
- Reverse engineering software (Materialise 3-matic Medical)
- Finite-element analysis software (ANSYS Mechanical 2024 R2)
- Machine learning framework (TensorFlow 2.15)
- Probabilistic programming library (PyMC 5.10)
- Direct metal laser sintering (DMLS) system (Concept Laser MLab)
- Medical-grade Ti-6Al-4V powder (Rematitan, particle size 15–45 µm)
- Vacuum heat treatment furnace
Procedure:
Medical Image Acquisition and Segmentation
- Acquire preoperative CT images of the patient's cranio-mandibular region using standardized protocols
- Import DICOM data into segmentation software and apply bone-threshold mask (>200 HU)
- Use automatic region-growing followed by manual editing to remove dental artefacts and floating bone islands
- Apply Laplacian smoothing kernel (λ = 0.5, five iterations) to generate watertight surface suitable for engineering
Anatomical Reconstruction and Implant Design
- Mirror intact contralateral hemimandible and blend across defect plane to establish target reconstruction contour
- Design fully integrated fixation plate (2.4 mm thickness) with screw apertures (2.5 mm diameter) at 8 mm pitch
- Loft plate seamlessly into buccal surface and apply 1 mm fillets to all sharp features to minimize stress concentrations
- Validate occlusal clearance and nerve-canal avoidance before exporting as STEP file
Finite-Element Model Development
- Construct high-fidelity finite-element model using quadratic tetrahedral elements (mean edge 0.8 mm in bone/plate, 0.4 mm in screws)
- Generate approximately 1.2 million elements to ensure computational accuracy
- Assign isotropic, linear-elastic properties (Ti-6Al-4V: E = 110 GPa, ν = 0.33; cortical bone: E = 13 GPa, ν = 0.30)
- Define frictionless contact for bone-implant interaction and bonded contacts for screw fixation
- Apply boundary conditions: fully constrain condylar heads and apply unilateral bite forces (300 N for average mastication, 600 N for maximum clench)
Surrogate Model Training and Validation
- Generate FEM database comprising 384 Latin-Hypercube variations in plate thickness, screw layout, and graded-lattice porosity
- Train fully connected ANN (64–32–16 hidden neurons, ReLU activation) on FEM results
- Validate surrogate using five-fold cross-validation to achieve mean absolute error below 6% and R² of 0.94
Uncertainty Quantification and Probabilistic Optimization
- Implement Bayesian network with No-U-Turn Sampler (5000 draws) to propagate input uncertainties
- Sample patient-to-patient variation in cortical-bone modulus (±20%), bite-force scatter (±30%), and build-porosity fluctuation (±5%)
- Apply genetic algorithm for multi-objective optimization with BN probabilistic constraints (failure probability <3%)
Additive Manufacturing and Post-Processing
- Prepare build data with 45° orientation relative to build plate to balance support volume with accuracy
- Generate hollow, self-detachable lattice supports on non-functional surfaces only
- Process medical-grade Ti-6Al-4V powder using DMLS parameters: layer thickness 25 µm, laser power 95 W, laser spot diameter 50 µm, scan speed 800 mm/s
- Perform post-processing vacuum heat treatment: ramp to 820°C over 4 hours, hold for 1.5 hours, cool under vacuum
Experimental Validation
- Fabricate fifteen candidate scaffolds for mechanical testing
- Validate FEM predictions against experimental measurements of stress and stiffness
- Verify that final selected design resists 600 N bite force with peak von Mises stress of 225 MPa and micromotion <150 µm
Figure 1: Computational-Experimental Workflow for Patient-Specific Mandibular Implants
Application Note: Biphasic Osteochondral Implants with Zonal Design
Workflow from MRI to Implantation
The fabrication of patient-specific, biphasic implants for osteochondral defect regeneration requires a specialized workflow from clinical MRI data to implantation. This approach addresses the complex zonal architecture of osteochondral tissue through advanced additive manufacturing techniques [12].
Table 2: Key Components in Biphasic Osteochondral Implant Fabrication [12]
| Component | Material System | Manufacturing Technique | Functional Role |
|---|---|---|---|
| Bony phase | Calcium phosphate bone cement | Extrusion-based 3D printing | Provides mechanical support and promotes bone regeneration |
| Cartilaginous phase | Hydrogel | Extrusion-based 3D printing | Mimics native cartilage extracellular matrix |
| Interface design | Zonal gradient architecture | Multi-material 3D printing | Recapitulates native osteochondral interface |
| Imaging source | Clinical MRI data | Patient-specific design | Ensures anatomical conformity |
| Design framework | Computer-aided design (CAD) | Digital workflow | Enables precise control over zonal architecture |
Experimental Protocol: Fabrication of Biphasic Osteochondral Implants
Protocol Title: Additive Manufacturing of Zonal Biphasic Implants for Osteochondral Defect Regeneration
Objective: To fabricate patient-specific, biphasic implants with zonal design for regeneration of osteochondral defects using clinical MRI data and extrusion-based 3D printing.
Materials and Equipment:
- Clinical MRI scanner
- Medical image processing software with CAD capabilities
- Extrusion-based 3D printing system with multi-material capability
- Calcium phosphate bone cement
- Hydrogel bioink (composition tailored to application)
- Sterile fabrication environment
Procedure:
Patient-Specific Data Acquisition
- Acquire high-resolution MRI data of the affected joint
- Segment osteochondral defect geometry using appropriate thresholding and region-growing algorithms
- Identify zonal boundaries between cartilage and subchondral bone regions
Biphasic Implant Design
- Create 3D model of the defect region using CAD software
- Design biphasic structure with bone-facing region and cartilage-facing region
- Incorporate zonal gradient at the interface to mimic native tissue transition
- Optimize pore architecture for each phase to facilitate tissue ingrowth
Material Preparation
- Prepare calcium phosphate bone cement according to manufacturer specifications
- Formulate hydrogel bioink with appropriate rheological properties for printing
- Sterilize all materials following established protocols for biomedical applications
Extrusion-Based 3D Printing
- Calibrate printing parameters for each material separately
- Program multi-material printing path based on the zonal design
- Fabricate implant using layer-by-layer deposition with precise material placement
- Maintain sterile conditions throughout the printing process
Post-Processing and Sterilization
- Crosslink hydrogel phase if required by material formulation
- Cure calcium phosphate phase according to established protocols
- Perform final sterilization using method compatible with both materials
- Package implants following regulatory requirements
Quality Control
- Verify dimensional accuracy against original CAD model
- Assess mechanical properties of each phase and the interface
- Confirm sterility through appropriate testing methods
Figure 2: Biphasic Osteochondral Implant Fabrication Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Additive Manufacturing of Medical Models and Implants [12] [11] [13]
| Material/Reagent | Composition/Type | Primary Function | Application Context |
|---|---|---|---|
| Medical-grade Ti-6Al-4V | Titanium alloy with 6% aluminum, 4% vanadium | Provides high strength-to-weight ratio and excellent biocompatibility for load-bearing implants | Mandibular reconstruction plates, orthopedic implants [11] |
| Calcium phosphate bone cement | Ceramic-based material with composition similar to natural bone mineral | Serves as osteoconductive scaffold for bone regeneration | Bony phase of osteochondral implants, bone defect fillers [12] |
| Hydrogel bioink | Polymer network (e.g., gelatin methacrylate, polyethylene glycol) crosslinked in water | Mimics native extracellular matrix for cartilage tissue engineering | Cartilaginous phase of osteochondral implants, soft tissue models [12] |
| Polymethyl methacrylate (PMMA) | Transparent thermoplastic polymer | Provides optical clarity for educational models and temporary surgical guides | Dental surgical guides, anatomical training models [14] |
| Polylactic acid (PLA) | Biodegradable thermoplastic aliphatic polyester | Serves as low-cost material for anatomical models and surgical guides | Educational models, preoperative planning models [13] [14] |
| Polyetheretherketone (PEEK) | Semi-crystalline thermoplastic with excellent mechanical and chemical resistance | Provides radiolucency and mechanical properties similar to bone for implants | Patient-specific cranial implants, orthopedic applications [14] |
| Medical imaging contrast agents | Iodinated compounds or gadolinium-based agents | Enhances visibility of anatomical structures in medical imaging | Improves segmentation accuracy for patient-specific model design [11] |
| 10-Formyl-7,8-dihydrofolic acid | 10-Formyldihydrofolate|Research Chemical | Bench Chemicals | |
| Acetylshengmanol Arabinoside | Acetylshengmanol Arabinoside, CAS:402513-88-6, MF:C37H58O10, MW:662.8 g/mol | Chemical Reagent | Bench Chemicals |
Application Note: Educational Implementation of 3D-Printed Patient-Specific Models
Validation in Dental Education
The implementation of patient-specific 3D-printed models in structured educational programs demonstrates significant benefits for clinical training. A study involving postgraduate periodontics and implantology students revealed high satisfaction with 3D-printed mandibular and maxillary models derived from Cone Beam Computed Tomography (CBCT) scans [14].
Table 4: Educational Outcomes from 3D-Printed Model Implementation in Dental Training [14]
| Educational Metric | Measurement Method | Results | Implications |
|---|---|---|---|
| Procedural comprehension improvement | 5-point Likert scale | Mean score: 8.38 ± 0.82 | Significant enhancement in understanding surgical procedures |
| Technical skill acquisition | Student self-assessment | Vast majority reported improvements | Better preparation for live patient procedures |
| Confidence in clinical application | Pre/post training assessment | Increased confidence levels | Reduced anxiety during transition to patient care |
| Educational Impact factor | Exploratory Factor Analysis | 53.09% of variance | Primary dimension of educational benefit |
| Technological Adoption factor | Exploratory Factor Analysis | 12.02% of variance | Secondary dimension emphasizing technology acceptance |
| Cumulative variance explained | Factor Analysis | 65.11% | Strong validation of two-dimensional framework |
| Bridge between theory and practice | Qualitative feedback | Overwhelmingly positive | Effective translation of knowledge to clinical skills |
Experimental Protocol: Integration of 3D-Printed Models in Surgical Training Curriculum
Protocol Title: Implementation and Validation of Patient-Specific 3D-Printed Models in Postgraduate Dental Surgical Training
Objective: To integrate patient-specific 3D-printed anatomical models into structured surgical training curriculum and evaluate their educational impact on postgraduate students.
Materials and Equipment:
- Cone Beam Computed Tomography (CBCT) scanner
- 3D printing system (appropriate for anatomical model fabrication)
- Dental model materials (various polymers/composites)
- Validated perceptions questionnaire
- Statistical analysis software
Procedure:
Patient Data Selection and Model Fabrication
- Select representative CBCT scans from clinical cases
- Segment anatomical structures of interest (mandible/maxilla)
- Design 3D-printed models maintaining patient-specific anatomy
- Fabricate models using appropriate 3D printing technology and materials
Curriculum Integration
- Develop structured training program incorporating 3D-printed models
- Design hands-on surgical exercises using patient-specific models
- Schedule training sessions within existing curriculum framework
- Prepare supporting educational materials
Participant Recruitment and Training
- Recruit postgraduate students in relevant specialties (periodontics, implantology)
- Conduct training sessions using 3D-printed models
- Provide supervised practice of surgical techniques
- Facilitate feedback and discussion sessions
Data Collection
- Administer validated perceptions questionnaire post-training
- Collect quantitative data using Likert-scale items
- Gather qualitative feedback through structured questions
- Ensure anonymity and voluntary participation
Data Analysis
- Perform exploratory factor analysis to identify key dimensions
- Calculate reliability metrics (Cronbach's alpha) for questionnaire
- Analyze quantitative data for trends and significance
- Conduct thematic analysis of qualitative feedback
Curriculum Refinement
- Incorporate feedback into model design and training methodology
- Optimize balance between technological innovation and educational objectives
- Address identified limitations (e.g., tactile realism improvements)
- Plan for longitudinal assessment of clinical skill transfer
The integration of immersive technologies—Virtual Reality (VR), Augmented Reality (AR), and the Metaverse—is fundamentally reshaping the methodology behind surgical training and planning. These platforms address critical limitations in traditional medical education by creating controlled, repeatable, and risk-free environments for skill acquisition. The core value proposition lies in their ability to enhance procedural accuracy, improve knowledge retention, and accelerate the development of clinical decision-making skills [15]. For researchers designing 3D medical equipment simulations, understanding this technological landscape is paramount. These are not merely visualization tools but represent a paradigm shift towards data-rich, interactive simulation environments that can provide quantitative feedback on user performance, thereby informing better design choices for future medical training systems [16] [17].
The metaverse, conceptualized as a convergence of VR, AR, and other digital assets, creates a persistent virtual space for user interaction. Its applicability to surgical education stems from four key characteristics: immersive virtuality, which provides high-fidelity 3D environments; openness and interoperability, allowing seamless integration across platforms; user-generated content, enabling the creation of tailored medical simulations; and the use of blockchain technology for secure certification of skills and outcomes [15]. This framework offers an unprecedented opportunity to develop standardized, yet highly customizable, simulation-based training modules that can be collaboratively used and assessed across global institutions.
Current Applications and Performance Metrics
Immersive technologies are being deployed across a spectrum of surgical disciplines, from orthopaedics to general surgery, with measurable impacts on educational and clinical outcomes. The applications can be broadly categorized into three domains: procedural skills training, preoperative planning, and intraoperative guidance.
Table 1: Quantitative Performance Metrics of Immersive Technology in Surgical Training
| Application Area | Key Metric | Reported Improvement | Source / Context |
|---|---|---|---|
| VR Procedural Training | Procedural Step Accuracy | 92% accuracy achieved by VR-trained learners [16] | Osso VR platform studies |
| Error Reduction | 67% fewer errors and instructor prompts [16] | Randomized studies on VR training | |
| Procedural Completion Time | 25% faster completion of procedures [16] | Comparison with traditional methods | |
| Procedural Competence Scores | Up to 300% higher scores than traditional methods [16] | Orthopedic surgical training | |
| AR-Based Surgical Training | Surgical Accuracy | 25-35% better performance [18] | Training at King Faisal Specialist Hospital |
| Error Rates | Reduced by nearly one-third [18] | Augmented reality training programs | |
| 3D Model-Based Education | Learning Skills & Knowledge | Higher scores in most randomized trials [19] | Systematic scoping review of 15 RCTs |
| Test-Taking Times | Generally favored the 3D model group [19] | Assessment of 1659 medical students |
In surgical training, VR platforms like Osso VR provide clinically accurate simulations for practicing procedures, offering immediate performance-based feedback. This multi-modal approach combines individual and collaborative learning, rapidly scaling onboarding for nursing and surgical staff [16]. For preoperative planning, 3D modeling and AR are transforming how surgeons prepare for complex operations. For instance, the Advanced Imaging and Modeling (AIM) program converts 2D CT and MRI scans into interactive 3D models, allowing for improved understanding of anatomy and pathology, such as visualizing how a tumor wraps around organs [4]. In intraoperative settings, AR systems overlay medical images directly onto the patient, providing surgical guidance. FDA-cleared devices like the xvision Spine System and Medivis's Surgical AR project 3D models into the surgeon's visual field, enhancing precision in procedures like spinal instrumentation and tumor resection [20] [21].
Experimental Protocols for Validation
Validating the efficacy of immersive technologies within a design methodology framework requires rigorous, standardized experimental protocols. The following sections detail methodologies for two key types of validation studies: assessing skill acquisition and evaluating visualization workflows.
Protocol for VR Surgical Skill Acquisition Study
This protocol is designed to quantify the impact of VR simulation training on the development of surgical competency, providing a model for validating new 3D simulation equipment [15].
Objective: To evaluate the efficacy of a VR training module in improving procedural accuracy, reducing error rates, and decreasing time-to-competence for a specific surgical procedure (e.g., arthroscopic meniscectomy).
Materials and Reagents:
- VR Simulation Platform: A head-mounted display (e.g., Oculus Quest, HTC Vive) with the targeted surgical training software installed [15].
- Assessment Metrics Software: Integrated system for capturing performance data (e.g., time to completion, path length of instruments, number of errors).
- Control Group Materials: Traditional training assets (e.g., video tutorials, cadaveric specimens, or box trainers).
- Pre- and Post-Testing Tools: Written knowledge tests and global rating scales for technical skills (e.g., Objective Structured Assessment of Technical Skills - OSATS).
Methodology:
- Participant Recruitment and Randomization:
- Recruit surgical trainees (e.g., residents) with minimal prior exposure to the target procedure.
- Randomly assign participants to an intervention group (VR training) or a control group (traditional training).
Baseline Assessment:
- All participants complete a pre-test, which includes a knowledge exam and a baseline skill assessment on a physical model or the VR simulator itself.
Intervention Phase:
- VR Group: Complete a structured, self-guided curriculum within the VR simulator. This involves repeated practice of the procedure until a pre-defined proficiency level is reached.
- Control Group: Undergo an equivalent duration of training using standard methods (e.g., video review and practice on a physical model).
Post-Training Assessment:
- All participants perform the procedure in a simulated environment (e.g., a high-fidelity physical model or a live animal tissue model).
- Blinded expert evaluators assess performance using validated metrics like procedural checklists and global rating scales.
Data Analysis:
- Compare post-test scores between groups for statistical significance using t-tests for continuous data (e.g., time, accuracy scores) and chi-square tests for categorical data (e.g., error rates).
- Analyze learning curves within the VR group based on simulator-generated metrics.
Protocol for AR Visualization Workflow (VR-Prep)
This protocol outlines the use of an open-source workflow, "VR-prep," for processing medical imaging data for enhanced AR visualization on consumer devices. This is critical for research into making 3D simulations more accessible and efficient [22].
Objective: To optimize and assess a pipeline for converting DICOM image series into 3D models suitable for AR visualization on smartphones and tablets, evaluating processing time and image quality.
Materials and Reagents:
- Software: 3D Slicer (open-source), Fiji (ImageJ, open-source), Medical Imaging XR (MIXR) mobile application.
- Hardware: Standard workstation for image processing, smartphone or tablet (iOS/Android).
- Input Data: De-identified DICOM series from CT, MRI, or PET-CT scans.
Methodology:
- Data Preparation:
- Anonymize the DICOM data set as per institutional review board protocols.
VR-Prep Processing (Experimental Workflow):
- Load the DICOM series into Fiji.
- Execute the VR-prep macro, which performs:
- File Size Reduction: Reduces the number of frames and overall data volume.
- Isotropic Voxel Conversion: Ensures uniform voxel dimensions for optimal 3D rendering.
- Slope and Bit-Depth Adjustment: Standardizes intensity values for accurate display.
- Save the processed image stack using 3D Slicer.
Control Workflow:
- Upload the original, unprocessed DICOM series directly to the MIXR web portal.
Quantitative Metrics Collection:
- Record the file size (MB), number of frames, and time required for upload and QR-code generation for both the original and VR-prepped data sets.
- Record the download time of the 3D object onto the mobile device.
Qualitative Image Quality Assessment:
- Have independent, blinded clinical raters evaluate both the original and VR-prepped 3D models in the MIXR app.
- Use a 5-point Likert scale to rate parameters like Look-Up Table (LUT) representation, sharpness, signal-to-noise ratio, and confidence in use for diagnostics.
Table 2: Research Reagent Solutions for Immersive Technology Research
| Item | Function | Example Products / Platforms |
|---|---|---|
| VR Simulators | Provides immersive environments for procedural practice and skill assessment. | Osso VR [16], Surgical Theater [20] |
| AR Visualization Software | Converts 2D medical images into 3D models for overlay in the real world. | Medivis Surgical AR [20], 3D Slicer [22] |
| Head-Mounted Displays (HMDs) | Hardware for delivering immersive VR/AR experiences. | Apple Vision Pro [20], Meta Quest, Microsoft HoloLens [20] |
| Open-Source Data Pipelines | Workflows for processing and optimizing medical data for XR. | VR-prep workflow (Fiji, 3D Slicer, MIXR) [22] |
| Performance Analytics Platforms | Captures and analyzes user performance data from simulations. | Osso Loop learning platform [16] |
Visualization of Workflows and System Architecture
The effective implementation of immersive technologies relies on coherent workflows and system architectures. The following diagrams, generated using Graphviz DOT language, illustrate the logical relationships and data flows in key processes.
The integration of VR, AR, and the metaverse into surgical training and planning represents a significant advancement in design methodology for 3D medical simulations. Evidence consistently demonstrates that these technologies enhance learning efficacy, procedural accuracy, and spatial understanding of complex anatomy [16] [18] [19]. The experimental protocols and workflows detailed herein provide a foundation for researchers to systematically validate new simulation tools and contribute to an evolving ecosystem.
Future development in this field will likely focus on overcoming existing challenges, which include high technological costs, the complexity of content development, data security concerns, and the need for seamless integration with clinical workflows like Electronic Health Records (EHR) [15] [17] [20]. The convergence of AI with spatial computing promises optimized procedures through intelligent overlays and advanced data analysis [20]. Furthermore, the FDA's establishment of a dedicated list for authorized AR/VR medical devices underscores the regulatory pathway maturation, encouraging continued innovation [21]. For researchers, the trajectory is clear: the next generation of 3D medical equipment simulations will be more immersive, interoperable, and intelligent, fundamentally transforming how surgical skills are acquired and refined.
Building and Deploying 3D Simulations: From Concept to Clinic
The integration of three-dimensional (3D) printing into medicine represents a paradigm shift from conventional mass production to personalized, additive manufacturing [23]. This technology fundamentally transforms two-dimensional (2D) radiological data into tangible, patient-specific anatomical models, thereby enhancing surgical planning, medical education, and clinical device simulation [24] [25]. Establishing a robust, repeatable digital workflow is critical for ensuring the accuracy and clinical validity of the resulting 3D printed parts, which is a cornerstone of effective design methodology for 3D medical equipment simulations research. This protocol details the end-to-end process, from data acquisition to a validated 3D printable model, providing a structured framework for researchers and developers.
The Digital Workflow Process
The journey from a medical scan to a 3D printed model is a multi-stage process that requires precision at every step. The following diagram illustrates the complete workflow, from patient imaging to the final application of the 3D printed model in a research or clinical setting.
Stepwise Protocol and Methodology
Step 1: Data Acquisition and Verification The process begins with the acquisition of high-quality medical imaging data. Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) are the most common sources, providing the necessary cross-sectional data of the patient's anatomy [24] [26]. The Digital Imaging and Communications in Medicine (DICOM) standard is used for all data transfers.
- Experimental Protocol:
- Imaging Parameters: For CT, use the highest practical spatial resolution and low slice thickness (preferably ≤1 mm) to maximize detail. For MRI, select sequences that optimize contrast between the tissue of interest and surrounding structures.
- Verification Check: Inspect the DICOM series for artifacts, motion blur, and sufficient coverage of the anatomical region of interest (ROI). Ensure the data is complete and that the imaging parameters are documented.
Step 2: Image Segmentation Segmentation is the most critical and time-consuming step, involving the isolation of the ROI from the background image data. This process defines which pixels constitute the anatomy to be printed.
- Experimental Protocol:
- Software Loading: Import the verified DICOM series into specialized segmentation software (e.g., 3D Slicer, Mimics, Vital Images) [24].
- Thresholding: For CT data, use Hounsfield unit thresholds to automatically differentiate between bone (high HUs) and soft tissue (low HUs).
- Manual Refinement: Employ manual painting, erasing, and region-growing tools to correct errors in the automatic segmentation, particularly in areas where tissues have similar radiodensity or signal intensity.
- Output: Generate a labeled mask of the ROI.
Step 3: 3D Model Reconstruction and Mesh Creation The segmented 2D mask is converted into a 3D surface model. This process generates a polygonal mesh, typically composed of triangles, which represents the outer surface of the anatomy.
- Experimental Protocol:
- Algorithm Selection: Apply a marching cubes or surface rendering algorithm within the software to create the initial 3D mesh from the segmented mask.
- File Generation: The initial mesh is often generated in a proprietary format before being exported to a standard polygonal mesh format.
Step 4: Model Optimization and Repair The raw 3D mesh is often not suitable for 3D printing and requires optimization to ensure it is "watertight" (a manifold surface without holes) and structurally sound [26].
- Experimental Protocol:
- Software Tools: Use mesh editing software (e.g., Meshmixer, 3-Matic, MeshLab).
- Watertight Check: Run an automated check for holes, non-manifold edges, and self-intersections. Repair any identified issues.
- Decimation: Reduce the triangle count of the mesh if it is overly complex and detailed beyond the capability of the 3D printer, preserving critical anatomical features.
- Smoothing: Apply smoothing algorithms to reduce the "stair-step" appearance from the segmentation process, but avoid over-smoothing which can erase anatomical detail.
Step 5: Export to 3D Printable File The optimized mesh is exported into a file format that is universally recognized by 3D printing software.
- Experimental Protocol:
- Format Selection: Export the model in the Standard Tessellation Language (STL) or OBJ file format [24].
- Scale Verification: Confirm that the exported model's scale and units (e.g., millimeters) are correct.
Step 6: Physical 3D Printing The STL file is imported into a slicer program, which converts the 3D model into a series of 2D layers (G-code) that instruct the 3D printer.
- Experimental Protocol:
- Technology Selection: Choose the appropriate 3D printing technology based on the application. Fused Deposition Modeling (FDM) is common for cost-effective anatomical models, while Stereolithography (SLA) or Selective Laser Sintering (SLS) offer higher resolution for complex structures [24] [23].
- Orientation and Supports: Orient the model on the build plate to minimize supports and maximize strength. Generate necessary support structures for overhanging features.
- Print Execution: Initiate the print using a material suitable for the intended use (e.g., biocompatible resin for surgical guides, flexible filament for vascular models).
Step 7: Post-Processing and Validation After printing, the model requires finishing and must be validated against the original imaging data to ensure anatomical accuracy.
- Experimental Protocol:
- Post-Processing: Remove support structures, sand, and (if necessary) paint the model to enhance anatomical features [26].
- Validation: The principal investigator or a qualified medical expert must compare the physical 3D model directly with the original source imaging to verify that it accurately represents the patient's anatomy [26]. This is a critical quality control step before use in simulation or research.
Essential Digital Tools and Research Reagents
The digital workflow relies on a suite of software tools, each fulfilling a specific function. The table below categorizes and describes these key "research reagents" for the digital phase of model creation.
Table 1: Key Software Tools for the Medical 3D Printing Digital Workflow
| Tool Category | Example Software | Primary Function in Workflow | Research Application |
|---|---|---|---|
| Segmentation & Modeling | 3D Slicer, Mimics, Vital Images, 3D Doctor [24] | Converts DICOM images into segmented masks and initial 3D meshes. | Core platform for extracting specific anatomical geometries from patient data for device simulation. |
| Mesh Editing & Repair | Meshmixer, MeshLab, Netfabb [26] | Optimizes and repairs mesh models; makes them watertight and printable. | Ensures model integrity and readiness for manufacturing, crucial for generating reliable physical prototypes. |
| Computer-Aided Design (CAD) | SOLIDWORKS, CATIA [27] | Creates or modifies geometric designs; used for adding custom features or surgical guides. | Allows for the design of patient-specific medical devices or simulation apparatus that interface with the anatomical model. |
| Simulation & Analysis | Finite Element Analysis (FEA), Electromagnetic Simulation [27] | Virtually tests device performance and safety under simulated conditions. | Enables in-silico testing of medical devices against the anatomical model, reducing physical prototyping needs. |
| Collaborative Platforms | Synergy3dMed, 3DEXPERIENCE [27] [25] | Manages workflow, enables real-time communication, and stores data securely. | Supports cross-disciplinary collaboration between radiologists, engineers, and researchers, streamlining the development process. |
Advanced Considerations for Research
Integration with Medical Device Design and Simulation
The digital model serves as the foundation for advanced research applications. It can be incorporated into a Virtual Twin of human anatomy to run sophisticated simulations, such as drop tests, stress analysis, or electromagnetic compatibility, before any physical part is manufactured [27]. This aligns directly with the rigorous simulation testing requirements for medical devices, which demand validation under defined operating conditions that mimic the human body [28]. The accurate anatomical models produced by this workflow provide a superior in-vitro testing environment compared to simple mechanical fixtures.
Protocol for Model Validation and Fidelity Assessment
A key tenet of scientific research is the verification of methods. For 3D printed anatomical models, this involves quantifying their fidelity to the source data.
- Experimental Protocol:
- Dimensional Analysis: Use coordinate measuring machines (CMM) or micro-CT scanning to measure critical dimensions on the 3D printed model. Compare these measurements to the same dimensions taken from the source DICOM images.
- Volume Comparison: Calculate the volume of the segmented ROI in the software and compare it to the volume of the physical model, measured via water displacement or from the printed model's sliced data.
- Landmark Distance Error: Identify specific anatomical landmarks in the source images and on the 3D printed model. The spatial distance between corresponding landmarks quantifies the geometric error of the entire workflow.
Addressing Workflow Challenges
Researchers must be aware of inherent challenges. Segmentation accuracy is a primary source of error and is highly dependent on image quality and operator skill [24]. Software and training costs can be prohibitive, and the limited range of biocompatible materials approved for 3D printing can constrain the development of implantable devices [23]. Furthermore, the regulatory landscape for 3D printed patient-specific devices and anatomical models is still evolving, requiring careful consideration in any research program aimed at clinical translation [29] [23].
Point-of-care (PoC) 3D printing is revolutionizing healthcare by enabling the just-in-time creation of patient-specific anatomic models, surgical instruments, and implants within the hospital environment [30]. This approach transforms patient care by moving manufacturing directly to the clinical setting, blurring traditional lines between healthcare provider and device manufacturer. The technology has expanded beyond cranio-maxillofacial and orthopedic applications into congenital heart disease and oncology, where patient-specific models improve surgical precision and patient outcomes [31]. By 2025, advancements in automation, AI integration, and operational efficiency are making personalized medicine more accessible and scalable than ever before [31].
The fundamental value proposition of in-hospital 3D printing labs lies in their ability to create patient-matched solutions that would be impossible or impractical with traditional manufacturing approaches. From anatomical models for surgical planning to custom surgical guides and implants, PoC manufacturing offers unprecedented flexibility for clinical teams [32] [33]. This guide provides comprehensive application notes and protocols for establishing and maintaining a robust PoC 3D printing facility, with specific consideration to design methodology for 3D medical equipment simulations research.
Laboratory Setup and Operational Framework
Centralized Laboratory Configuration
A centralized operational model for hospital-based 3D printing offers significant advantages over distributed departmental approaches. Centralization enables resource optimization, standardized quality control, and regulatory compliance [32]. Successful implementation requires careful consideration of spatial organization, workflow design, and technical integration.
Table 1: Facility Zoning Requirements for Point-of-Care 3D Printing Labs
| Zone | Primary Functions | Environmental Controls | Equipment Examples |
|---|---|---|---|
| Material Storage | Raw material inventory, bioink storage | Temperature control (4-8°C for bioinks), dry conditions | Material handling equipment, refrigeration units [34] |
| Digital Processing | Medical image segmentation, 3D modeling, simulation | Standard office environment | Workstations with medical image manipulation software [34] |
| Pre-processing & Buffer | Sterile preparation, material handling | HEPA-filtered airflow, UV-C sterilization capabilities | Biosafety cabinets, material preparation stations [34] |
| Printing Operations | Additive manufacturing processes | Temperature control (4-65°C for printbed, 4-250°C for printheads) [34] | 3D printers (FDM, SLA, Material Jetting, SLS) [32] |
| Post-processing | Support removal, cleaning, finishing | Ventilation for chemical fumes, safety equipment | UV curing stations, chemical baths, finishing tools [32] |
| Quality Control | Dimensional verification, mechanical testing, biological assessment | Controlled environment for measurement equipment | Coordinate measuring machines, mechanical testers, microscopes [34] |
The centralized laboratory model managed by Biomedical Engineering or Radiology departments allows for consolidated expertise and more efficient use of financial resources [32]. This structure supports higher equipment utilization rates and reduces total staff hours required for maintenance and processing on a per-print basis. The technical resources within these groups and strong clinical relationships with key departments facilitate successful implementation [32].
Technology Selection and Integration
Selecting appropriate 3D printing technologies requires matching technical capabilities to clinical applications. A multi-technology approach typically provides the greatest flexibility for addressing diverse clinical needs.
Table 2: 3D Printing Technology Comparison for Medical Applications
| Process | Materials | Clinical Applications | Advantages | Limitations |
|---|---|---|---|---|
| Fused Deposition Modeling (FDM) | Thermoplastic filament (PLA, ABS) | Prototypes, surgical guides, anatomical models | Ease of use, functional prints, inexpensive | Variable durability, anisotropic properties, limited resolution [32] |
| Stereolithography (SLA) | Photo-polymer liquid resin | Surgical guides, dental models, hearing aids | Superior accuracy, excellent surface finish, wide material properties | Significant post-processing, support placement considerations [32] [35] |
| Selective Laser Sintering (SLS) | Powdered polymers (Nylon, TPU) | Functional prototypes, custom instruments | Strong prints, no support structures needed | Environmental concerns, porous surface finish [32] |
| Material Jetting | Photo-polymers | Multi-material anatomical models, realistic simulations | Mixture of multiple materials, wide range of material properties | Expensive, significant post-processing [32] |
| Binder Jetting | Powdered materials | Anatomical models with color texture | Full-color capabilities, fast printing | Fragile prints, significant post-processing [32] [33] |
Institutional needs assessment should guide technology acquisition. A balanced approach targets clearly identified clinical use cases while maintaining flexibility for diverse applications [32]. For comprehensive support, traditional subtractive manufacturing equipment (CNC mills, lathes) can complement 3D printing capabilities, allowing selection of the optimal technology for each application [32].
Digital Workflow and Simulation Protocols
Medical Image to Printable Model
The transformation of medical imaging data into printable 3D models requires specialized software and meticulous segmentation protocols. The process begins with acquiring high-quality DICOM data from CT, MRI, or other medical imaging modalities, with scan parameters optimized for the intended application.
Segmentation Protocol:
- Data Import: Load DICOM images into specialized medical segmentation software (e.g., Materialise Mimics, 3D Slicer)
- Thresholding: Apply Hounsfield unit-based or signal intensity thresholds to isolate target tissues
- Region Growing: Use connectedness algorithms to select contiguous anatomical structures
- Manual Editing: Refine selections through slice-by-layer correction of automation errors
- Mesh Generation: Convert segmented masks to 3D surface models using marching cubes algorithm
- Model Cleanup: Repair mesh errors, reduce polygon count, and smooth surfaces
- Design Modification: Add orientation markers, labeling, or analytical features
The integration of AI-enabled segmentation tools significantly reduces processing time while improving accuracy and reproducibility [31]. These systems leverage deep learning algorithms trained on annotated medical image datasets to automatically identify and segment anatomical structures.
Printing Process Simulation
Simulation software plays a critical role in predicting and mitigating printing failures before physical manufacturing begins. These tools create virtual environments that mirror the physical behavior of the printer, material, and model during the printing process [36].
Simulation-Based Optimization Protocol:
- Model Preparation: Import STL file into simulation platform (e.g., Autodesk Netfabb, ANSYS Additive Suite)
- Material Parameterization: Input material-specific properties (thermal expansion coefficient, elastic modulus, viscosity)
- Process Parameter Definition: Set printing parameters (layer height, print speed, temperature settings)
- Thermal Analysis: Execute thermal simulation to predict temperature distribution and cooling behavior
- Stress Analysis: Calculate residual stress accumulation throughout the build process
- Distortion Prediction: Generate deformation maps showing anticipated geometric deviations
- Support Optimization: Identify critical areas requiring support structures and optimize placement
- Compensation Algorithm Application: Apply geometric compensation to counteract predicted distortion
- Iterative Refinement: Modify design and process parameters based on simulation results
Advanced simulation platforms incorporate machine learning algorithms trained on historical print data to improve prediction accuracy over time [36]. This approach is particularly valuable for metal additive manufacturing where deformation from thermal stress is common and costly, though increasingly applied to polymer-based processes for applications requiring tight tolerances [36].
Materials and Reagent Solutions
Research Reagent Solutions
Table 3: Essential Materials for Medical 3D Printing Applications
| Material Category | Specific Formulations | Primary Applications | Key Properties | Sterilization Compatibility |
|---|---|---|---|---|
| Photopolymers (SLA) | Biocompatible resins (Class I/II), Dental SG resin | Surgical guides, dental models, hearing aids | High resolution, smooth surface finish | Ethylene oxide, gamma radiation, autoclave (specific formulations) [35] |
| Thermoplastics (FDM) | PLA, ABS, PETG, Nylon, PEEK | Anatomical models, instrument prototypes, custom jigs | Mechanical strength, thermal stability | Varied by material; most tolerate ethylene oxide [32] |
| Powder Materials (SLS) | PA12, PA11, TPU | Functional prototypes, custom instruments, prosthetics | Excellent mechanical properties, chemical resistance | Ethylene oxide compatible [32] |
| Bioinks | Alginate, gelatin methacryloyl, silk fibroin, chitosan | Tissue engineering, disease modeling, drug testing | Cell compatibility, tunable mechanical properties | Aseptic processing required; limited sterilization options [34] |
Material selection must balance mechanical requirements, biological compatibility, and regulatory considerations. For patient-specific devices, biocompatibility and sterilization capability are paramount, requiring rigorous material qualification [34] [35]. Natural polymers like alginate and chitosan offer enhanced biocompatibility but may lack mechanical strength, while synthetic options like PEEK provide superior mechanical properties but require thorough biological validation [34].
Quality Management and Regulatory Compliance
Quality Management System Framework
Implementing a robust Quality Management System (QMS) is essential for ensuring consistent production of safe and effective 3D printed medical devices [31] [30]. The QMS should encompass all aspects of the production process from design input to final device validation.
Quality Management Protocol:
- Design Control Implementation: Establish and maintain design history files for all patient-matched devices
- Process Validation: Execute installation qualification, operational qualification, and performance qualification for all manufacturing equipment
- Material Control: Maintain certificates of analysis for all raw materials and establish supplier qualification programs
- Equipment Maintenance: Implement preventive maintenance schedules and calibration protocols for all critical equipment
- Personnel Training: Develop comprehensive training programs with competency assessment and documentation
- Document Control: Establish controlled documentation systems for standard operating procedures, specifications, and records
Hospitals are increasingly adopting robust QMS to standardize processes and ensure compliance with regulatory expectations [31]. Software solutions such as Materialise Mimics Flow help hospitals document their case processes and achieve greater efficiency in quality management [31].
Regulatory Compliance Strategy
The regulatory landscape for PoC 3D printing spans multiple FDA centers, including the Center for Devices and Radiological Health (CDRH), Center for Biologics Evaluation and Research (CBER), and Center for Drug Evaluation and Research (CDER) [37] [30]. Understanding device classification is fundamental to developing an appropriate regulatory strategy.
Device Classification Framework:
- Class I Devices: Present minimal risk and are typically exempt from Premarket Notification (e.g., anatomical models for visual reference)
- Class II Devices: Require Premarket Notification through the 510(k) pathway (e.g., diagnostic use anatomic models, surgical guides)
- Class III Devices: Demand Premarket Approval with clinical trial evidence (e.g., life-supporting implants) [30]
Most PoC 3D printed devices fall into Class I or II categories, though classification depends on intended use and risk profile [30]. The FDA does not regulate the practice of medicine, allowing physicians to use 3D printed devices without regulatory submission when not marketed or sold [30]. However, institutions should maintain comprehensive documentation including design history files, process validation records, and quality management system certification [34].
Validation and Testing Protocols
Mechanical Testing Protocol
Comprehensive mechanical validation ensures 3D printed devices meet performance requirements for their intended clinical applications. Testing should simulate anticipated in-use conditions.
Tensile Testing Methodology:
- Specimen Preparation: Print standardized test specimens (Type V dog bone per ASTM D638) in orientations representing production parts
- Conditioning: Condition specimens at 23±2°C and 50±5% relative humidity for at least 40 hours before testing
- Equipment Setup: Calibrate universal testing machine and install appropriate load cell (typically 5-50 kN capacity)
- Testing Parameters: Set initial grip separation to 115 mm, crosshead speed to 5 mm/min, and pre-load to 0.1 N
- Data Collection: Record load and extension data at minimum 10 Hz frequency until specimen failure
- Analysis: Calculate ultimate tensile strength, yield strength, elastic modulus, and elongation at break
- Statistical Analysis: Apply Weibull analysis to assess structural reliability and predict failure probability [38]
Compressive Strength Testing:
- Specimen Geometry: Prepare cylindrical specimens (12.7 mm diameter × 25.4 mm height) or cube specimens (10 mm × 10 mm × 10 mm)
- Test Configuration: Apply compressive load at constant crosshead speed of 1.3 mm/min
- Data Collection: Record load and displacement until specimen failure or 80% strain
- Analysis: Calculate compressive strength and modulus from stress-strain relationship
Dimensional Verification Protocol
Ensuring geometric accuracy is critical for patient-specific devices, particularly those interfacing directly with anatomy.
Coordinate Measurement Machine (CMM) Protocol:
- Equipment Preparation: Qualify CMM probe using reference sphere and establish machine coordinate system
- Part Fixturing: Secure 3D printed part using non-deforming fixtures that avoid measurement obstruction
- Feature Alignment: Align part coordinate system to CAD model coordinate system using datum features
- Measurement Plan Execution: Automatically measure critical features according to predefined measurement plan
- Data Analysis: Compare measured points to nominal CAD geometry and calculate deviation metrics
- Reporting: Generate comprehensive report including color deviation maps and statistical analysis
For complex internal geometries not accessible via CMM, micro-computed tomography (μCT) provides a non-destructive alternative for comprehensive volumetric analysis.
Process Validation Using Statistical Methods
Statistical methods play a crucial role in qualifying 3D printing processes and optimizing parameters for medical applications [38].
Taguchi Methodology for Parameter Optimization:
- Parameter Selection: Identify critical process parameters (layer height, print orientation, infill density, print temperature)
- Orthogonal Array Design: Select appropriate orthogonal array (L9, L18, L27) based on parameters and levels
- Experiment Execution: Print test specimens according to array configuration in randomized order
- Response Measurement: Quantify critical quality attributes (dimensional accuracy, surface roughness, mechanical properties)
- Signal-to-Noise Analysis: Calculate S/N ratios for each experimental run using "larger-is-better," "smaller-is-better," or "nominal-is-best" approaches
- Analysis of Variance: Determine statistical significance of each parameter and identify optimal level combinations
- Confirmation Experiment: Verify optimal parameters through additional experimental runs
The Taguchi Method represents a statistically rigorous approach to quality building that is economical through reduced experimental requirements [38]. This methodology has been successfully applied to optimize various 3D printing technologies including Fused Deposition Modeling and Laser-Based Powder Bed Fusion [38].
Emerging Trends and Future Directions
The field of point-of-care 3D printing continues to evolve rapidly, with several key trends shaping its development. Extended reality (XR) technologies are transforming how clinicians interact with 3D planning data, making patient-specific planning faster and more accessible while reducing the need for physical prints [31]. AI integration is driving market expansion through streamlined workflows, automation, and improved software integration [31]. Progress in reimbursement policies is lowering financial barriers to adoption, with standardized coding structures making it easier for hospitals to submit claims for 3D printed medical models and devices [31].
Miniaturization represents another significant trend, with micro 3D printing enabling applications in ultra-targeted drug delivery, microfluidic devices for pharmaceutical research, and miniatured surgical instruments [39]. The growing demand for advanced materials with specific properties like temperature sensitivity and enhanced biocompatibility continues to drive innovation in material science for medical 3D printing [39].
As point-of-care 3D printing matures, hospitals are strengthening their focus on quality and regulatory compliance, adopting robust quality management systems to standardize processes and ensure patient safety [31]. These developments collectively support the transition of 3D planning and printing from an innovative tool to an indispensable part of modern healthcare delivery [31].
Table 1: Perceived Educational Impact of 3D-Printed Anatomical Models in Medical Training [40] [14]
| Metric | Orthopedic Resident Findings | Postgraduate Dental Student Findings |
|---|---|---|
| Overall Participant Satisfaction | Mean scores ranged from 6.9 to 7.9 (out of 10) based on training year [40] | Mean score of 8.38 ± 0.82 (out of 10) on educational impact [14] |
| Enhanced Understanding of Anatomy/Procedures | 85.6% of residents reported enhanced understanding [40] | Significant improvements in procedural comprehension reported [14] |
| Impact on Confidence & Anxiety | Not explicitly measured | Decreased anxiety and greater readiness for clinical practice reported [14] |
| Preferred Group Setting | Small group settings (4-6 participants) preferred by 76.3% of respondents [40] | Not explicitly measured |
| Highest-Rated Educational Feature | Physical manipulation of models (mean score 8.1/10) [40] | Realistic, risk-free training environment [14] |
| Reported Limitations | Production time (45.8%), material durability (38.6%), limited model varieties (35.6%) [40] | Cost, material optimization, limitations in tactile realism for incision training [14] |
Experimental Protocol for Model Creation and Educational Integration
Workflow for Patient-Specific Model Production
The following diagram outlines the core technical and educational workflow for creating and implementing 3D-printed anatomical models.
Digital Workflow for 3D-Printed Anatomical Guides
Detailed Methodological Steps
Step 1: Image Acquisition and Segmentation [40]
- Imaging Modalities: Acquire patient-specific computed tomography (CT) scans or Cone Beam Computed Tomography (CBCT) scans, stored in standard DICOM format.
- Segmentation Software: Utilize specialized medical image processing software (e.g., Mimics by Materialise).
- Process: Perform a semi-automated segmentation to isolate anatomical regions of interest. This process requires a trained technician and takes approximately 2–4 hours per model.
- Output: Convert the segmented data into a stereolithography (STL) file format, the standard for 3D printing.
Step 2: 3D Printing and Model Fabrication [40] [14]
- Printing Technology: Employ Fused Deposition Modeling (FDM).
- Printing Material: Use cost-effective materials like Polylactic Acid (PLA) for educational models. Other applicable materials include polymers and composites like polymethyl methacrylate (PMMA) and Polyetheretherketone (PEEK) for surgical guides [14].
- Printing Parameters: Print at a high resolution (e.g., 12.5 µm for the x/y axes) to ensure anatomical fidelity.
- Time: The average printing time is 8–12 hours, depending on model size and complexity.
Step 3: Structured Educational Implementation [40]
- Session Format: Conduct small-group teaching sessions lasting 60–90 minutes.
- Group Size: Optimal groups contain 4–6 residents, a setting preferred by 76.3% of trainees.
- Instructional Method:
- An attending surgeon demonstrates key anatomical features and surgical principles using the model.
- This is followed by a period of supervised, hands-on practice by the residents.
- Target Concepts: Focus on complex anatomical cases such as comminuted acetabular fractures, severe spinal deformities, and complex tibial plateau fractures.
Research Reagents and Material Solutions
Table 2: Essential Materials and Digital Tools for 3D Medical Model Research
| Item Name | Function/Application | Specification Notes |
|---|---|---|
| Polylactic Acid (PLA) | Primary printing material for cost-effective anatomical models [40] | Biocompatible polymer; suitable for Fused Deposition Modeling (FDM); offers good printability and anatomical precision [14] |
| Medical Image Segmentation Software (e.g., Mimics) | Converts 2D DICOM images into 3D digital models via semi-automated segmentation [40] | Enables isolation of anatomical regions of interest; process requires ~2-4 hours per model; critical for creating STL files [40] |
| Fused Deposition Modeling (FDM) Printer | Fabricates physical models from digital STL files using additive manufacturing [40] | Accessible printing technology; uses PLA filament; typical build time of 8-12 hours per model [40] |
| Cone Beam CT (CBCT) / CT Scans | Provides the initial patient-specific anatomical data in DICOM format [14] | Source data for segmentation; essential for ensuring model accuracy and patient-specificity [40] [14] |
| Open-Source Design Databases | Platforms for sharing and distributing 3D-printed simulator designs to enhance accessibility [41] | Aims to build partnerships between universities and nonprofits; must address intellectual property protection to prevent commercialization [41] |
Research Framework and Implementation Strategy
Integration within Design Methodology for Medical Simulations
The application of patient-specific 3D-printed models represents a critical nexus in the design methodology for medical equipment simulations, bridging digital design with tangible, clinical training tools. This methodology emphasizes "transferring art and technology" into clinical education, where digital modeling and anatomical accuracy are enhanced by an artistic sensibility towards aesthetic detail and visual realism [14].
A key research direction involves the development of open-source databases and repositories for distributing 3D-printed simulator designs. This strategy facilitates partnerships between university-based research centers, hospitals, and non-profit organizations (NPOs), aiming to overcome barriers of cost, accessibility, and expertise. A central challenge within this design framework is modifying intellectual property (IP) laws to protect designs shared via open-source platforms from commercialization, ensuring they remain accessible for educational and research purposes [41].
Efficacy and Outcome Measures
The educational impact of this methodology is quantified across several domains [40]:
- Anatomical Comprehension: Significant enhancement in understanding complex 3D spatial relationships.
- Surgical Planning Proficiency: Improved proficiency in preoperative planning and procedural confidence.
- Clinical Teaching Utility: High perceived value in small-group, instructor-led teaching sessions.
Studies note that the highest educational value is derived from the physical manipulation of models, underscoring the importance of tactile, hands-on learning in surgical training [40]. Furthermore, the multisensory nature of these models aligns with educational theory that supports multimodal learning for enhanced knowledge retention and skill transfer [40].
Simulating Treatment Protocols and Device-Tissue Interaction with AI
Application Note: AI-Driven Clinical Trial Protocol Optimization
Artificial Intelligence is revolutionizing clinical trial design by enabling sophisticated simulations that predict outcomes and optimize protocols before patient enrollment. This approach addresses chronic industry challenges, including prolonged timelines and high costs, by transitioning from static, predetermined protocols to dynamic, adaptive trial frameworks [42] [43]. By leveraging historical data and predictive analytics, AI systems can model complex trial variables, allowing researchers to refine study designs, enhance patient recruitment strategies, and improve the likelihood of regulatory and clinical success.
Key Quantitative Data on AI in Clinical Trials
The adoption of AI in clinical research is accelerating, marked by significant market growth and its impact on critical trial metrics.
Table 1: AI in Clinical Trials - Market Size and Impact Metrics
| Metric | 2024 Value | 2025 Value | Projected 2030 Value | Key Impact Areas |
|---|---|---|---|---|
| Global Market Size | USD 7.73 Billion | USD 9.17 Billion | USD 21.79 Billion (CAGR ~19%) | Trial Design, Patient Recruitment, Data Analysis [43] |
| Avg. Trial Delay from Patient Recruitment | 37% of trials delayed | - | - | AI accelerates recruitment via EHR and data analysis [43] |
| Non-Enrolling Sites | 10-50% of sites across industry | - | - | AI-driven site selection automates matching [42] |
Experimental Protocol: AI-Assisted Trial Design and Simulation
Protocol Title: In-silico Optimization of Clinical Trial Protocol using Predictive AI and Historical Data.
Objective: To simulate and refine clinical trial protocols by predicting patient enrollment rates, identifying inclusion/exclusion criterion bottlenecks, and forecasting operational outcomes.
Materials and Software:
- Historical Clinical Trial Data Repository: Structured databases containing anonymized protocol designs, patient demographics, enrollment logs, and site performance records.
- AI-Powered Simulation Platform: Software such as VISIONAL (for enrollment prediction and budget forecasting) or comparable systems capable of machine learning and scenario modeling [42].
- Computing Infrastructure: High-performance computing environment suitable for running complex, multi-parametric simulations.
Methodology:
- Data Aggregation and Curation:
- Collect and clean historical trial data, including protocol documents, patient enrollment records per site, and detailed inclusion/exclusion criteria.
- Annotate data with outcomes such as enrollment duration, screen failure rates, and overall trial timelines.
Model Training and Calibration:
- Utilize machine learning algorithms to train models on the historical dataset. The model should learn the relationship between protocol characteristics (e.g., stringency of criteria, number of sites) and operational outcomes (e.g., enrollment rate, delay probability).
- Calibrate model predictions against a held-out validation dataset to ensure accuracy.
Protocol Simulation and Scenario Analysis:
- Input the draft protocol design into the calibrated AI model.
- Run multiple simulation iterations to generate predictions for key performance indicators (KPIs):
- Enrollment Trajectory: Predict the rate of patient accrual over time.
- Criterion Bottleneck Analysis: Identify which inclusion/exclusion criteria are most likely to cause screen failures and slow enrollment [42].
- Site Performance Forecasting: Model the expected performance of pre-selected clinical sites.
- Use constraint-based algorithms to model different scenarios, such as relaxing specific criteria or adding new recruitment sites [42].
Protocol Refinement:
- Analyze simulation outputs to identify weaknesses in the initial protocol.
- Iteratively modify the protocol design and re-run simulations to quantify the improvement in predicted KPIs.
- Finalize the protocol design that the simulation indicates has the highest probability of rapid enrollment and successful completion.
Outputs:
- A optimized clinical trial protocol with data-driven inclusion/exclusion criteria.
- A predictive report detailing expected enrollment timelines, site activation sequences, and potential operational risks.
Application Note: Modeling Device-Tissue Interaction for Surgical Simulation
Accurate modeling of the interaction between medical devices and biological tissue is a critical requirement for developing high-fidelity surgical simulators and optimizing wearable assistive device design [44] [45]. These simulations present a safe, effective method for surgical training and pre-operative planning. The core challenge lies in creating models that are both physically realistic, incorporating the complex viscoelastic and nonlinear properties of soft tissue, and computationally efficient enough to run in real-time [44].
Key Modeling Approaches for Tissue and Device Interaction
Research in tool-tissue interaction modeling can be broadly classified based on the underlying physical principles and the type of surgical operation being simulated.
Table 2: Modeling Approaches for Surgical Tool-Tissue Interactions
| Model Category | Underlying Principle | Representative Surgical Actions | Key Considerations |
|---|---|---|---|
| Linear Elastic Finite Element (FE) | Hooke's Law; stress-strain relationship is linear [44]. | Deformation (via indentation) [44] | Computationally efficient but invalid for large strains (>1-2%) common in surgery [44]. |
| Nonlinear/Hyperelastic FE | Accounts for nonlinear, large-strain deformation of materials like soft tissue [44]. | Deformation, Cutting [44] | More physiologically accurate but computationally expensive [44]. |
| Other Methods (Mass-Spring-Damper, etc.) | Simplified mechanics not based on continuum physics [44]. | Deformation, Rupture [44] | Enables real-time simulation but may sacrifice physical accuracy for speed [44]. |
| Interface Compliance Models | Focuses on force transmission loss and misalignment at device-tissue interface [45]. | Force application from wearable devices [45] | Critical for exoskeleton design; accounts for up to 50% power loss in assistive devices [45]. |
Experimental Protocol: Finite Element Analysis of Soft Tissue Indentation
Protocol Title: Hyperelastic Modeling of Soft Tissue Indentation for Surgical Simulator Fidelity Validation.
Objective: To develop and validate a finite element model of soft tissue that accurately simulates deformation under a surgical tool's indentation.
Materials and Software:
- FE Software: A computational mechanics platform with nonlinear, hyperelastic material modeling capabilities.
- Material Property Data: Experimentally derived mechanical properties (e.g., coefficients for Mooney-Rivlin or Ogden hyperelastic models) for the target tissue (e.g., liver, kidney) [44].
- Experimental Validation Setup (Optional): A mechanical testing system and tissue phantom for correlating simulation results with physical measurements.
Methodology:
- Geometry and Mesh Generation:
- Create a 3D geometric model of the biological tissue and the surgical indenter tool (e.g., a spherical probe).
- Generate a finite element mesh, refining the region where the tool and tissue interact to ensure solution accuracy.
Material Model Assignment:
- Assign a hyperelastic material model to the tissue geometry. Populate the model with experimentally acquired tissue parameters to represent its nonlinear elasticity [44].
- Assign a rigid material model to the tool.
Boundary Conditions and Interaction Definition:
- Constrain the bottom and sides of the tissue model to represent underlying anatomical support.
- Define the contact interaction between the tool and tissue surface, specifying friction properties if applicable.
Simulation Execution:
- Apply a displacement-controlled load to the tool, indenting it into the tissue model to a specified depth.
- Run a nonlinear quasi-static simulation to calculate the tissue's deformation and the resulting reaction forces on the tool.
Model Validation:
- Compare the simulation-predicted force-displacement curve with data obtained from physical indentation tests on tissue or a validated tissue phantom.
- Iteratively refine the material properties and mesh in the model until the simulation outputs fall within an acceptable error margin of the experimental data.
Outputs:
- A validated FE model of soft tissue indentation.
- Quantitative data on stress distribution within the tissue and interaction forces, which can be used to provide realistic haptic feedback in a surgical simulator [44].
Visualizing Workflows and Relationships
AI-Driven Clinical Trial Optimization Workflow
The following diagram outlines the integrated workflow for using AI to optimize clinical trial protocols, from data preparation to final design.
Device-Tissue Interaction Modeling Methodology
This diagram illustrates the key considerations and research focus areas in modeling the interaction between devices and biological tissue.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Simulation Development
| Item Name | Type | Function / Application |
|---|---|---|
| Hyperelastic Material Model Parameters | Software/Data | Coefficients for mathematical models (e.g., Mooney-Rivlin, Ogden) that define the non-linear stress-strain behavior of soft biological tissues in FE simulations [44]. |
| Tissue-Mimicking Phantoms | Physical Material | Hydrogels or other synthetic materials with mechanical properties calibrated to mimic specific biological tissues (e.g., liver, muscle); used for experimental validation of simulation models [44]. |
| Musculoskeletal Human Models (MHMs) | Software/Digital Model | Digital human models that simulate the musculoskeletal system; used to evaluate the biomechanical effects of wearable assistive devices on parameters like muscle activation and joint forces [45]. |
| AI-Powered Predictive Analytics Platform | Software | A platform combining machine learning and predictive analytics (e.g., VISIONAL, INTELIA CORE) to automate clinical trial document generation, forecast enrollment, and optimize site selection [42] [43]. |
| Knowledge Graphs with NLP | Software/Data Structure | A data integration structure that uses natural language processing (NLP) to interlink disparate clinical data sources, enabling more accurate and immediate knowledge extraction for trial design [42]. |
| Betamethasone Valerate | Betamethasone Valerate | Betamethasone valerate is a synthetic glucocorticoid for research. This product is For Research Use Only and is not intended for diagnostic or therapeutic use. |
| Amthamine dihydrobromide | Amthamine dihydrobromide, CAS:142457-00-9, MF:C6H13Br2N3S, MW:319.06 g/mol | Chemical Reagent |
Overcoming Implementation Hurdles and Optimizing Simulation Workflows
Quantitative Analysis of Key Barriers in 3D Medical Simulation
Table 1: Quantified Impact of Primary Barriers to 3D Medical Simulation Adoption [46] [47] [48]
| Barrier Category | Specific Factor | Quantitative Impact | Supporting Data Source |
|---|---|---|---|
| Cost | High Initial Investment | ★★★★☆ (High Impact) | Key restraint for small institutions & budget-sensitive markets [47]. |
| Projected market growth to USD 9.2 billion by 2035 indicates high cost of adoption [47]. | |||
| Infrastructure | Limited Infrastructure | 56% of users report as a challenge [46]. | Thematic analysis from a global mixed-methods study [46]. |
| Technology Integration | ★★★☆☆ (Moderate Impact) | Challenges with system compatibility and infrastructure requirements [47]. | |
| Digital Literacy | Need for Context-Specific Training | 49% of users report as a challenge [46]. | Thematic analysis from a global mixed-methods study [46]. |
| Improved Confidence Post-Training | Significant increase (e.g., VR simulators: 2.8 to 4.2 on 5-point scale) [46]. | Pre- and post-training survey results from a global study [46]. |
Table 2: Global Medical Simulation Market Growth & Segment Analysis (2025-2035) [47] [48] [49]
| Market Segment | 2025 Market Value (USD Billion) | 2035 Projected Value (USD Billion) | Compound Annual Growth Rate (CAGR) | Key Drivers |
|---|---|---|---|---|
| Overall Market | 1.9 [47] - 3.05 [49] | 9.2 [47] - 12.94 [49] | 15.54% [49] - 17.1% [47] | Patient safety initiatives, workforce expansion, VR/AR adoption [47]. |
| Healthcare Anatomical Models | 41.6% market share [47] | ~40% market share [47] | - | Procedural efficiency, educational optimization [47]. |
| 3D Printing Technology | 43.8% market share [47] | 39-42% market share [47] | - | Customized model production, patient-specific surgical planning [47]. |
Experimental Protocols for Barrier Mitigation
Protocol: A Frugal Workflow for 3D Model Generation and Collaborative Review in Low-Resource Settings
This protocol is adapted from a feasibility study conducted in Uganda, demonstrating a cost-effective and infrastructure-light approach to 3D medical modeling [50].
2.1.1 Research Reagent Solutions
Table 3: Essential Materials for Frugal 3D Model Generation [50]
| Item | Function / Rationale | Specific Example |
|---|---|---|
| Smartphone with Camera | Data acquisition device; uses ubiquitous technology to minimize cost. | Google Pixel 7a [50]. |
| AI-Enhanced 3D Scanning App | Software to process 2D photographs into 3D models; cloud-processing reduces local hardware needs. | MagiScan app (Version 1.8) [50]. |
| VR Head-Mounted Displays (HMDs) | Consumer-grade hardware for immersive visualization and remote collaboration. | Meta Quest 2 (standalone) or Oculus Rift S (tethered) [50]. |
| Collaborative VR Software Platform | Creates a shared virtual space for multiple users to review and annotate 3D models simultaneously. | XR Dissection Master (Medicalholodeck) [50]. |
2.1.2 Step-by-Step Methodology
- Patient Consent and Preparation: Obtain written informed consent. Position the patient so the pathology is fully exposed. Ensure indirect, uniform lighting to avoid shadows and artifacts [50].
- Data Acquisition:
- Using the smartphone camera, capture approximately 45 images of the patient's condition.
- Execute a full 360° circumferential movement around the patient, capturing images from all relevant angles and orientations.
- Instruct the patient to remain stable to ensure image consistency [50].
- 3D Model Generation:
- Upload the photo set to the 3D scanning app.
- The AI-driven photogrammetry software autonomously processes the images on a cloud server, generating a detailed 3D model.
- Export the final model in a compatible format (e.g., GLTF) for import into the VR platform [50].
- Virtual Collaborative Review:
- Participants in different geographical locations don VR HMDs and log into the shared VR software platform.
- Import the 3D patient model into the shared virtual space.
- Conduct the case conference using integrated audio communication. Surgeons can collaboratively discuss strategies and use virtual tools to mark incision lines and surgical approaches directly on the digital model [50].
The entire process from data acquisition to model creation was reported to take under 8 minutes per case, demonstrating high time-efficiency [50].
Frugal 3D Modeling & Collaborative Review Workflow
Protocol: A Structured Training Intervention to Overcome Digital Literacy Barriers
This protocol is derived from a global, mixed-methods study that successfully improved healthcare professionals' confidence in using immersive technologies [46].
2.2.1 Research Reagent Solutions
Table 4: Essential Materials for Structured Simulation Training [46]
| Item | Function / Rationale |
|---|---|
| VR Simulators | Provide hands-on experience in a risk-free environment; focus on procedural repetition and skill acquisition. |
| Metaverse Platforms | Train users in virtual consultations and interdisciplinary collaborative planning. |
| 3D Display Systems | Facilitate understanding of complex anatomical spatial relationships through high-fidelity visualization. |
| Pre- and Post-Training Surveys | Quantitative tools to measure changes in user confidence and knowledge (e.g., 5-point Likert scale). |
2.2.2 Step-by-Step Methodology
- Pre-Training Assessment:
- Prior to the workshop, administer a pre-training survey to all participants.
- Assess baseline confidence in using VR, metaverse, and 3D display systems using a 5-point Likert scale (1 = Not confident at all, 5 = Very confident) [46].
- Hands-On Workshop Intervention:
- Conduct a structured, approximately 4-hour workshop.
- The session should be highly interactive, providing direct, hands-on experience with the three core technologies:
- VR Simulators: Allow participants to practice specific surgical or clinical procedures.
- Metaverse Platforms: Guide participants through virtual telemedicine consultations and collaborative treatment planning sessions.
- 3D Display Systems: Enable participants to interact with and manipulate 3D anatomical models for education and surgical planning [46].
- Post-Training Assessment and Analysis:
- Immediately following the training, administer a post-training survey identical to the pre-training survey.
- Use paired statistical tests (e.g., paired t-tests) to determine the significance of changes in self-reported confidence scores [46].
- Qualitative Feedback Integration:
- Collect structured qualitative feedback from participants via open-ended questions.
- Perform thematic analysis on this feedback to identify nuanced challenges, perceived benefits, and context-specific issues not captured by quantitative scores. This informs future curriculum refinements [46].
The referenced study resulted in significant confidence improvements across all technologies, with VR simulator confidence increasing from 2.8 to 4.2 on a 5-point scale [46].
Digital Literacy Training & Assessment Protocol
Integrated Design Methodology and Future Outlook
The protocols and data presented herein form the core of a design methodology that is frugal, scalable, and user-centric. The strategic use of consumer-grade hardware (smartphones, standalone VR headsets) and cloud-based processing directly attacks the cost and infrastructure barriers [50]. Furthermore, the validated, short-format training protocol directly targets the digital literacy gap, proving that confidence can be built efficiently [46].
The strong projected market growth, with a CAGR of over 17%, underscores that these technologies are moving beyond innovation into a phase of broader integration [47]. Future research in this field should focus on standardizing these frugal protocols, developing robust quality metrics for AI-generated 3D models, and creating adaptive training curricula that can be automatically tailored to individual learner's progress. The integration of AI and machine learning will be pivotal in creating intelligent simulation systems that provide dynamic feedback, further enhancing training efficacy and helping to automate the path to digital literacy [49].
For researchers and scientists developing 3D medical equipment simulations, navigating the regulatory landscape is a critical component of the design methodology. The U.S. Food and Drug Administration (FDA) establishes a comprehensive regulatory framework to ensure medical devices are safe and effective for public use. This framework encompasses Quality System Regulations (QSR) that govern manufacturing practices and Medical Device Reporting (MDR) requirements for post-market surveillance. Understanding these regulations is essential for integrating computational models and simulations into medical device development and regulatory submissions. The FDA's Center for Devices and Radiological Health (CDRH) conducts regulatory science research, including the Credibility of Computational Models Program, to address the unique challenges posed by advanced modeling techniques [51]. For research focused on 3D medical equipment simulations, compliance with these regulations ensures that innovative design methodologies can be successfully translated into approved clinical technologies.
Quality Management Systems (QMS) Requirements
QMS Regulations and Standards
A Medical Device Quality Management System (QMS) is a structured framework of policies, processes, and procedures designed to ensure that medical devices consistently meet safety, quality, and regulatory requirements throughout their entire lifecycle [52]. The FDA's Quality System Regulation (21 CFR Part 820) establishes minimum requirements for medical device QMS to ensure product safety and effectiveness. A significant development is the FDA's issuance of the Quality Management System Regulation (QMSR) Final Rule in January 2024, which incorporates by reference the international standard ISO 13485:2016 [53]. This harmonization aims to align the U.S. regulatory framework with that used by many other regulatory authorities globally. The rule becomes effective on February 2, 2026, after which manufacturers must comply with the revised QMSR [54] [53].
Table: Quality Management System Regulatory Requirements
| Regulation/Standard | Scope | Key Focus Areas | Status/Timeline |
|---|---|---|---|
| FDA 21 CFR Part 820 (Quality System Regulation) | United States market | Design controls, production and process controls, complaint handling [52] | Current standard; enforced until Feb 1, 2026 [53] |
| ISO 13485:2016 | International markets | Risk-based approach to quality management, regulatory compliance, risk management integration [52] | Basis for the new QMSR; already recognized internationally |
| FDA QMSR (Revised 21 CFR Part 820) | United States market | Harmonization with ISO 13485:2016; additional requirements to ensure consistency with FDA expectations [53] | Effective and enforced beginning February 2, 2026 [53] |
QMS Documentation Structure and Core Processes
The documentation structure of a medical device QMS typically follows a hierarchy that includes: a Quality Manual (high-level document defining QMS structure and scope), Policies (reflect organizational commitment to quality and compliance), Procedures or Standard Operating Procedures (SOPs) (structured frameworks for consistent quality processes), Work Instructions (WIs) (task-specific guidance), and Records (documented evidence of compliance) [52].
The core processes of an effective medical device QMS include [52]:
- Document Control: Manages creation, approval, distribution, revision, and retirement of QMS documents
- Change Management: Controls implementation of changes in design, processes, or documentation
- Training Management: Ensures staff competency through tracking and documentation
- Nonconformance Management: Identifies, records, and resolves nonconforming materials, products, or processes
- Complaint Handling: Structured process for capturing, investigating, and resolving customer complaints
- CAPA Management: Focuses on identifying, resolving, and preventing recorded issues
- Audit Management: Systematic planning, execution, and review of internal and external audits
- Supplier Management: Framework for evaluating, selecting, and monitoring suppliers
Medical Device Reporting (MDR) Requirements
Mandatory Reporting Obligations
The Medical Device Reporting (MDR) regulation (21 CFR Part 803) contains mandatory requirements for manufacturers, importers, and device user facilities to report certain device-related adverse events and product problems to the FDA [55]. These requirements are essential for post-market surveillance and monitoring device safety. Manufacturers must report to the FDA when they learn that any of their devices may have caused or contributed to a death or serious injury. Manufacturers must also report when they become aware that their device has malfunctioned and would be likely to cause or contribute to a death or serious injury if the malfunction were to recur [55]. For manufacturers pursuing 3D simulation research, understanding these reporting triggers is crucial for establishing appropriate post-market surveillance protocols for computationally-designed devices.
Table: Medical Device Reporting Requirements and Timelines
| Reporter | What to Report | Report Form | To Whom | When |
|---|---|---|---|---|
| Manufacturers | 30-day reports of deaths, serious injuries, and malfunctions | Form FDA 3500A* | FDA | Within 30 calendar days of becoming aware [55] |
| Manufacturers | 5-day reports for events designated by FDA or requiring remedial action | Form FDA 3500A* | FDA | Within 5 work days of becoming aware [55] |
| Importers | Reports of deaths and serious injuries | Form FDA 3500A* | FDA and the manufacturer | Within 30 calendar days of becoming aware [55] |
| Importers | Reports of malfunctions | Form FDA 3500A* | Manufacturer | Within 30 calendar days of becoming aware [55] |
| User Facilities | Device-related deaths | Form FDA 3500A | FDA and manufacturer | Within 10 work days of becoming aware [55] |
| User Facilities | Device-related serious injuries | Form FDA 3500A | Manufacturer (FDA only if manufacturer unknown) | Within 10 work days of becoming aware [55] |
Note: *Or electronic equivalent [55].
Electronic Reporting and Compliance
The FDA requires manufacturers and importers to submit MDRs electronically in a format that the FDA can process, review, and archive [55]. The eMDR system facilitates this electronic submission process. It's important to note that complaint files are linked to MDR event files because a complaint must be evaluated to determine if it is a reportable adverse event [55]. For research scientists developing 3D simulation methodologies, integrating these reporting requirements into the design control process ensures comprehensive traceability from initial simulation through post-market surveillance.
Computational Modeling in Regulatory Submissions
Credibility Assessment Framework
For researchers focusing on 3D medical equipment simulations, the FDA's approach to Computational Modeling and Simulation (CM&S) is particularly relevant. The FDA has issued guidance on "Assessing the Credibility of Computational Modeling and Simulation in Medical Device Submissions" to provide a framework that manufacturers can use to show that CM&S models supporting regulatory submissions are credible [51]. The FDA defines the credibility of a computational model as "the trust, based on all available evidence, in the predictive capability of the model" [51]. This guidance applies specifically to physics-based or mechanistic CM&S models, which are fundamental to 3D medical equipment simulations.
The FDA's Credibility of Computational Models Program addresses several regulatory science gaps and challenges including [51]:
- Unknown or low credibility of existing models
- Insufficient quality experimental or clinical data for model development and validation
- Insufficient analytic methods for code verification and validation metrics
- Lack of established CM&S best practices
- Lack of credibility assessment tools
Regulatory Science Research Priorities
The FDA promotes the use of in silico clinical trials using CM&S, in which a device is tested on a cohort of virtual patients, which may potentially replace or supplement traditional clinical trials [51]. This approach aligns with advanced design methodologies for 3D medical equipment simulations research. The Credibility of Computational Models Program focuses on regulatory science research in several key areas, including new credibility assessment frameworks and domain-specific research related to credibility of computational models relevant to current and expected regulatory submissions [51]. For research scientists, engaging with these regulatory science priorities ensures that simulation methodologies meet evolving regulatory expectations.
Experimental Protocols for Regulatory Compliance
Protocol for Credibility Assessment of Computational Models
Objective: To establish a standardized methodology for verifying and validating computational models used in 3D medical equipment simulations, ensuring they meet regulatory standards for credibility as defined in FDA guidance [51].
Materials and Reagents:
- High-Performance Computing Cluster: Essential for running complex 3D simulations with appropriate processing speed and capacity
- CAD Software with Simulation Capabilities: Provides topology optimization, finite element analysis, and manufacturability validation [56]
- Anatomic Data Sets: Quality experimental or clinical data for model development and validation, particularly human physiological data under in vivo conditions [51]
- Verification Test Suite: Standardized test problems for code verification [51]
- Validation Metrics Toolkit: Tools for appropriate validation metrics and methods to evaluate acceptability of virtual cohort members [51]
Methodology:
- Model Definition: Precisely define the model's purpose, context of use, and the required accuracy for its predictions
- Code Verification: Ensure the computational code correctly implements the intended algorithms using standardized test problems
- Calculation Verification: Confirm that numerical solutions are sufficiently accurate (addressing discretization errors, iterative convergence, etc.)
- Model Validation: Compare computational results to experimental data to assess predictive capability, using appropriate validation metrics
- Uncertainty Quantification: Evaluate the effects of input uncertainty and model form uncertainty on simulation results
- Credibility Documentation: Compile evidence establishing model credibility for the specific context of use
Application Notes:
- Maintain comprehensive design history files throughout the simulation development process
- Implement rigorous version control for all computational models and associated data
- Document all assumptions, limitations, and validation activities in accordance with QMS documentation requirements
Protocol for Integration of QMS in Simulation Research
Objective: To implement Quality Management System requirements within a research environment focused on 3D medical equipment simulations, ensuring compliance with both current QS Regulation and upcoming QMSR.
Materials and Reagents:
- Electronic Quality Management System (eQMS): Software platform that streamlines QMS processes, improves traceability, and ensures compliance [52]
- Document Control System: Managed environment for creation, approval, and revision of QMS documents [52]
- Training Management Platform: System for tracking and documenting staff competency on QMS processes and regulatory requirements [52]
- Change Control Documentation: Standardized forms and procedures for managing changes in design, processes, or documentation [52]
Methodology:
- Gap Analysis: Conduct a comparative analysis between current practices and QMSR requirements based on ISO 13485:2016
- Documentation Development: Create and implement required QMS documentation, including Quality Manual, SOPs, and work instructions specific to computational research
- Design Controls Implementation: Establish and maintain procedures for design and development planning, input, output, review, verification, validation, and transfer
- Risk Management Integration: Apply risk management principles throughout the product lifecycle, from initial simulation through post-market surveillance
- Training Program Development: Implement comprehensive training on QMS requirements, specific to roles involved in computational modeling research
- Internal Audit Program: Establish scheduled internal audits to assess QMS compliance with applicable regulatory requirements
Application Notes:
- Focus on establishing robust design history files for all simulation projects, linking computational models to design controls
- Implement specific procedures for software validation when computational tools are used as part of quality systems
- Prepare for increased FDA access to records including internal audits, supplier audits, and management review reports under QMSR [53]
Visualization of Regulatory Workflows
Medical Device Regulatory Pathway
QMS Transition Timeline
Computational Model Credibility Assessment
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Essential Research Reagents and Computational Tools
| Item | Function/Application | Regulatory Consideration |
|---|---|---|
| CAD Software with Simulation Capabilities | Creates precise 3D device models; enables topology optimization, finite element analysis, and manufacturability validation [56] | Part of design controls; requires software validation under QMS |
| High-Fidelity Anatomic Data Sets | Provides realistic human physiological data for model development and validation [51] | Must represent target population; considerations for data quality and relevance to context of use |
| Credibility Assessment Tools | Facilitates code verification, calculation verification, and identifiability analysis [51] | Supports credibility argument for regulatory submissions |
| Electronic Quality Management System (eQMS) | Manages QMS processes including document control, change management, training, and CAPA [52] | Must be validated for intended use; maintains inspection readiness |
| 3D Printing/Additive Manufacturing Equipment | Creates functional prototypes for validation testing; produces patient-specific anatomical models [56] | Equipment calibration and process validation required; output is part of design history file |
| Verification & Validation Test Suites | Standardized test problems for computational code verification [51] | Provides objective evidence of model correctness and accuracy |
| (Rac)-Salvianic acid A | (Rac)-Salvianic acid A, CAS:23028-17-3, MF:C9H10O5, MW:198.17 g/mol | Chemical Reagent |
| Decamethylcyclopentasiloxane | Decamethylcyclopentasiloxane, CAS:541-02-6, MF:C10H30O5Si5, MW:370.77 g/mol | Chemical Reagent |
Successfully navigating the regulatory landscape for 3D medical equipment simulations requires integrating Quality Management System principles throughout the research and development process. The upcoming transition to the Quality Management System Regulation (QMSR) in February 2026 underscores the importance of harmonizing with international standards, particularly ISO 13485:2016. For computational researchers, establishing model credibility through rigorous verification and validation protocols is essential for regulatory acceptance. By implementing robust QMS processes, understanding MDR obligations, and following FDA guidance on computational modeling, researchers can advance innovative 3D simulation methodologies while maintaining compliance with regulatory requirements. This integrated approach ensures that cutting-edge research in medical device simulation can successfully transition from concept to clinically-approved technology.
Optimizing for Biocompatibility and Material Selection in 3D Printed Devices
Biocompatible polymers have emerged as essential materials in medical 3D printing, enabling the fabrication of scaffolds, tissue constructs, drug delivery systems, and biosensors for applications in and on the human body [57]. The selection of appropriate materials is fundamental to the success of any 3D printed medical device, influencing not only its functional performance but also its biological safety and regulatory pathway. This document provides a structured framework for researchers and scientists to navigate the complex landscape of material selection and biocompatibility optimization, framed within the context of design methodology for 3D medical equipment simulations research.
The paradigm of medical device manufacturing is shifting toward personalization, driven by the capacity of additive manufacturing to create custom-designed solutions rapidly and cost-effectively [58]. Critical to this shift is the biocompatibility of the materials used, which should allow long-term tissue culture without affecting cell viability or inducing an inflammatory response for in vitro and in vivo applications [59]. Understanding the processing-property relationships of these materials is essential for leveraging their full potential in clinical applications.
Material Selection Framework
Classification of Biocompatible 3D Printing Materials
Medical 3D printing utilizes a diverse range of materials, each with specific properties tailored to different clinical applications. These materials can be broadly categorized into metals, polymers, ceramics, and bio-inks.
Table 1: Fundamental Material Classes for Medical 3D Printing
| Material Class | Example Materials | Key Properties | Primary Applications |
|---|---|---|---|
| Biocompatible Metals | Titanium, Cobalt-Chrome, Stainless Steel | High strength, corrosion resistance, osseointegration capability | Orthopedic implants, dental implants [58] |
| Medical Polymers | PEEK, PEKK, PLA, PMMA, Nylon, Photopolymer Resins | Variable mechanical properties, lightweight, manufacturability | Surgical guides, lightweight prosthetics, drug delivery systems [60] [58] |
| Ceramics | Zirconia, Alumina | High compressive strength, wear resistance, bioinertness | Dentistry, orthopedics [58] |
| Bio-inks | Cells, Collagen, Gelatin, Biomaterial composites | Biologically active, tissue-mimetic properties | Bioprinting of tissues and organoids [58] |
Technical Performance Specifications
Quantitative assessment of material properties enables informed selection based on application-specific requirements. The following table summarizes critical performance metrics for common medical-grade polymers.
Table 2: Quantitative Comparison of Medical-Grade Polymer Properties
| Material | Tensile Strength (MPa) | Elongation at Break (%) | Young's Modulus (GPa) | Printing Technology | Sterilization Methods |
|---|---|---|---|---|---|
| PLA | 30-60 | 4-10 | 3.0-4.0 | FDM | Gamma radiation, ETO [60] |
| PEEK | 90-100 | 30-50 | 3.6-4.5 | FDM, SLS | Autoclave, Gamma radiation [60] |
| PEKK | 85-95 | 5-10 | 4.5-5.5 | FDM, SLS | Autoclave [60] |
| Medical ABS | 30-45 | 10-25 | 2.0-2.6 | FDM | ETO, Gamma radiation [60] |
| MED610 Photopolymer | 50-65 | 10-20 | 2.0-3.0 | Polyjet | ETO, Chemical solutions [59] |
Application-Material-Process Alignment
Different clinical applications demand specific material properties and manufacturing approaches. The alignment between application requirements, material selection, and printing technology is critical for device success.
Table 3: Application-Specific Material Selection Guidelines
| Application | Recommended Materials | Suitable Printing Technologies | Critical Performance Metrics |
|---|---|---|---|
| Orthopedic Implants (Load-bearing) | PEEK, PEKK, Titanium alloys | FDM, SLS, SLM/DMLS | tensile strength >80 MPa, compressive strength >100 MPa, fatigue resistance [60] |
| Surgical Guides | MED610, Nylon, PLA | SLA, FDM, SLS | dimensional accuracy (<0.5 mm deviation), rigidity, sterilizability [60] [59] |
| Prosthetics (Non-load-bearing) | PLA, ABS, Nylon | FDM | lightweight (<1.2 g/cm³), impact resistance, cost-effectiveness [60] |
| Tissue Engineering Scaffolds | PLA, PCL, Bio-inks | FDM, Bioprinting | controlled porosity (60-90%), biodegradability, surface chemistry [57] |
| Drug Delivery Systems | PLA, PLGA, Hydrogels | FDM, SLA | controlled release kinetics, biodegradability, encapsulation efficiency [57] |
Biocompatibility Optimization Protocols
Post-Printing Treatment Methodology
Post-processing is critical for ensuring the biocompatibility of 3D printed medical devices, particularly for photopolymerized materials that may contain residual monomers or leaching compounds. The following optimized protocol has demonstrated significant improvement in cytocompatibility both in vitro and in vivo [59].
Optimized Sonication Cleaning Protocol for Photopolymers:
Initial Rinse: Upon completion of printing, immediately submerge the construct in clean isopropanol (IPA) for 5 minutes with gentle agitation to remove excess uncured resin.
Sonication Cycle: Transfer the construct to a fresh IPA bath and subject to ultrasonic sonication at 40 kHz for 10 minutes. Maintain bath temperature below 30°C to prevent material deformation.
Intermediate Rinse: Remove from sonication bath and rinse with fresh IPA for 2 minutes with continuous agitation.
Secondary Sonication: Transfer the construct to deionized water and repeat ultrasonic sonication at 40 kHz for 10 minutes.
Final Rinse: Rinse thoroughly with sterile deionized water for 5 minutes with agitation.
UV Post-Curing: Subject the cleaned construct to UV post-curing at 365 nm wavelength for 30 minutes per side to ensure complete polymerization of residual monomers.
Sterilization: For sterile applications, utilize appropriate sterilization methods (e.g., ethylene oxide, gamma radiation) compatible with the material composition.
Validation Metrics:
- In vitro: Cell viability >90% relative to control in indirect cytotoxicity tests per ISO 10993-5 [59]
- In vivo: Significant reduction in foreign body response (p = 0.0161) and giant cell formation (p = 0.0368) compared to manufacturer's cleaning protocol [59]
Biocompatibility Testing Framework
A comprehensive testing strategy should be implemented to validate biocompatibility according to international standards. The following workflow outlines a tiered approach to biocompatibility assessment.
Diagram 1: Biocompatibility Testing Workflow
Advanced Material Systems and Research Frontiers
Reinforced Polymer Composites and Nanocomposites
The integration of reinforcement materials into polymer matrices significantly expands the functional properties available for medical devices. Reinforced polymer composites with tailored surface chemistries offer enhanced mechanical performance and biological functionality [57].
Key Advancements:
- Ceramic-Filled Polymers: Composites incorporating hydroxyapatite or tricalcium phosphate in PEEK or PLA matrices demonstrate improved osseointegration for orthopedic applications [57].
- Carbon-Reinforced Systems: Carbon fiber-reinforced PEEK and Nylon provide enhanced strength-to-weight ratios for load-bearing implants and prosthetics [61].
- Antibacterial Composites: Silver nanoparticle-infused polymers reduce infection risk in implantable devices [57].
Bioinks for Tissue Engineering Applications
Bioinks represent a specialized category of materials designed to support living cells during and after the printing process. These materials enable the fabrication of complex tissue constructs for regenerative medicine and drug testing applications [57].
Essential Bioink Properties:
- Printability: Appropriate viscosity and shear-thinning behavior for extrusion-based printing
- Structural Integrity: Maintenance of dimensional accuracy during crosslinking and maturation
- Biocompatibility: Support of cell viability, proliferation, and differentiation
- Biodegradability: Controlled degradation matching tissue formation rates
Research Reagent Solutions for Biocompatibility Testing
Table 4: Essential Research Reagents for Biocompatibility Assessment
| Reagent/Cell Line | Function in Testing | Application Context |
|---|---|---|
| Primary Mouse Myoblasts | Assessment of direct and indirect cytotoxicity | In vitro biocompatibility screening [59] |
| L929 Mouse Fibroblast Cell Line | Standardized cytotoxicity testing per ISO 10993-5 | Initial material screening |
| Alamar Blue/MTS Assay | Quantitative measurement of cell viability | Metabolic activity assessment |
| Live/Dead Staining Kit | Visualization of live and dead cells | Qualitative viability assessment |
| ELISA Kits (IL-1β, TNF-α, IL-6) | Quantification of inflammatory response | In vitro immunogenicity testing |
| RNA Extraction & qPCR Reagents | Analysis of gene expression related to inflammation and tissue remodeling | Molecular mechanism investigation |
Implementation Considerations for Research Applications
Technology Selection Framework
The selection of appropriate 3D printing technology is interdependent with material choice and application requirements. The following diagram illustrates the decision-making workflow for technology selection in medical device research.
Diagram 2: 3D Printing Technology Selection Workflow
Regulatory and Standardization Considerations
The medical device regulatory landscape presents significant challenges for 3D printed solutions. A lack of standardization has been noted with regards to the amount and quality of information provided with materials, requiring due diligence by researchers when selecting materials for specific applications [62].
Key Considerations:
- Material Certifications: Require complete biocompatibility certification (ISO 10993 series) from material suppliers
- Process Validation: Establish validated printing and post-processing parameters for consistent outcomes
- Quality Management: Implement quality systems compliant with FDA QSR or ISO 13485 throughout the research and development process
- Documentation: Maintain comprehensive documentation of all material sources, processing parameters, and testing results
The optimization of biocompatibility and material selection in 3D printed medical devices requires a systematic approach integrating materials science, biological evaluation, and manufacturing engineering. The protocols and frameworks presented herein provide researchers with structured methodologies for navigating this complex interdisciplinary domain. As the field continues to evolve, emerging trends in polymer composites, hybrid printing strategies, and advanced bioinks will further expand the frontiers of personalized medical devices, ultimately enabling more effective patient-specific healthcare solutions [57]. The translation of these technologies from research to clinical practice necessitates rigorous attention to both biological performance and manufacturing consistency throughout the development process.
Strategies for Cost and Timeline Reduction in the Simulation Design Cycle
The development of 3D medical equipment represents a complex, high-stakes endeavor where traditional design cycles are often protracted and costly. Simulation-driven design (SDD) has emerged as a transformative methodology, shifting simulation from a mere validation tool at the end of the design process to a central role from the earliest conceptual stages [63]. This paradigm allows researchers and engineers to explore design alternatives comprehensively, optimize for performance and manufacturability, and identify potential failures virtually before committing to physical prototypes. Within the context of 3D medical equipment—spanning from personalized implants to surgical instruments and diagnostic devices—adopting a strategic approach to the simulation cycle is not merely an efficiency gain but a critical component for achieving rapid innovation, regulatory compliance, and successful market entry. This document outlines targeted strategies and detailed protocols to significantly reduce both cost and timeline in the simulation design cycle for medical technology research and development.
Strategic Framework for Efficient Simulation
Core Principles of Simulation-Driven Design
A simulation-driven design ethos is foundational to reducing iterations and associated costs. This approach is characterized by several key principles:
- Front-Loading Simulation: Integrating simulation at the initial design stage enables the exploration of a wider design space and the identification of optimal concepts before significant resources are invested in detailed design and prototyping. This "joined-up thinking" from concept to validated product removes errors and oversights early [63].
- Balancing Conflicting Requirements: Successful medical device design must simultaneously address performance (e.g., strength, weight), sustainability (e.g., material efficiency), and affordability (e.g., product cost, warranty claims) [63]. Simulation provides the quantitative data needed to make informed trade-offs between these often competing goals.
- Democratization of Simulation: Providing product design engineers with accessible simulation tools—without requiring the specialized expertise of a dedicated FEA analyst—empowers them to gain deep, actionable insights into design performance independently, accelerating decision-making [63] [64].
Quantitative Business Impact
The business case for a strategic simulation investment is compelling. Research presented by McKinsey & Co., in collaboration with NAFEMS, quantifies the significant benefits organizations can achieve [64].
Table 1: Business Benefits of Strategic Simulation Implementation
| Metric | Improvement Range | Primary Impact |
|---|---|---|
| Time to Market | 20% - 30% acceleration [64] | Reduced development duration, earlier market entry |
| Product Performance | 5% - 30% improvement [64] | Enhanced device efficacy and patient outcomes |
| Product Cost | 5% - 30% reduction [64] | Lower cost of goods sold, increased affordability |
| Engineering Cost | Significant reduction [64] | Improved resource efficiency and productivity |
| Prototyping Costs | Up to 100% reduction (Zero Prototyping) [64] | Elimination of physical prototype iterations |
These improvements directly address the core objectives of cost and timeline reduction. Furthermore, simulation helps avoid costly late-stage problems that are often only detectable during physical testing of expensive prototypes, thereby de-risking the entire development process [64].
Application Notes: Protocols for Medical Equipment Simulation
Protocol 1: Integrated Design Optimization for Patient-Specific Implants
Objective: To streamline the development of a patient-specific cranial implant by combining medical imaging, simulation-driven design, and manufacturing process validation in a single, integrated workflow. This protocol aims to reduce the end-to-end design time by over 50% compared to traditional methods.
Background: The design of patient-specific implants requires a high degree of anatomical accuracy and performance assurance. Traditional workflows involving multiple physical prototypes are time-consuming and costly.
Table 2: Research Reagent Solutions for Implant Design
| Item / Software | Function | Application Context |
|---|---|---|
| Materialise Mimics | AI-enabled segmentation of DICOM data to create 3D anatomical models [31] | Converting CT/MRI scans into a simulation-ready 3D model of the defect site. |
| Altair HyperWorks | Multi-physics simulation (structural, thermal) and optimization [63] | Performing topology optimization to minimize implant weight while maintaining mechanical strength. |
| Altair Material Data Center | Provides a single source of validated, industry-grade material data [63] | Selecting biocompatible materials (e.g., PEEK, Titanium alloys) with accurate simulation properties. |
| 3D Printing System (e.g., SLS, SLA) | Additive manufacturing of the final implant or surgical guide [31] [65] | Prototyping and final manufacturing; enables complex geometries achieved via optimization. |
Methodology:
- Data Acquisition and Segmentation: Import patient DICOM data (CT scan) into segmentation software (e.g., Materialise Mimics). Use AI-enabled tools to rapidly isolate the region of interest and generate a 3D model of the cranial defect and surrounding anatomy [31].
- Initial Model Generation: Create a preliminary implant design that conforms to the anatomical defect. This serves as the "design space" for optimization.
- Simulation-Driven Optimization:
- Setup: Import the design space into simulation software (e.g., Altair Inspire). Define material properties from a trusted database (e.g., Altair Material Data Center).
- Boundary Conditions: Apply physiological load cases (e.g., pressure, impact) representative of in-vivo conditions.
- Optimization Goal: Set up a topology optimization study with the objective of minimizing mass, subject to a constraint on maximum stress and a minimum stiffness requirement.
- Manufacturing Validation: Integrate the manufacturing process simulation. For a 3D-printed implant, this involves simulating the printing process to identify potential issues like warping or residual stresses that could compromise the final part [63] [31].
- Design Refinement: Interpret the optimization results and apply smoothing and CAD-ready features to create the final, manufacturable implant geometry. The entire process from segmentation to final design is managed within a unified platform to reduce errors and data transfer delays.
The following workflow diagram illustrates this integrated protocol:
Protocol 2: AI-Augmented Drug Delivery System (DDS) Optimization
Objective: To accelerate the design and optimization of a polymer-based drug delivery system by employing molecular dynamics (MD) and machine learning (ML) to predict drug-polymer interactions and release kinetics, reducing reliance on wet-lab experimentation.
Background: The intricate interplay between drug formulations and delivery systems poses significant challenges. Simulations have emerged as indispensable tools for comprehending these interactions and enhancing DDS performance [66].
Table 3: Research Reagent Solutions for DDS Simulation
| Item / Software | Function | Application Context |
|---|---|---|
| Molecular Dynamics (MD) Software | Simulates atomic-level interactions and dynamics over time [66] | Modeling the diffusion of an API (Active Pharmaceutical Ingredient) through a polymer matrix. |
| Machine Learning (ML) Platform | Identifies complex patterns and creates predictive models from simulation and experimental data [66] | Predicting drug release profiles based on polymer properties and API characteristics. |
| Finite Element Analysis (FEA) | Models macro-scale phenomena like fluid flow and degradation [66] | Simulating the overall drug release from a device in a physiological environment. |
| Dissipative Particle Dynamics (DPD) | Simulates meso-scale structures in soft matter systems [66] | Studying the self-assembly of polymeric nanoparticles for drug encapsulation. |
Methodology:
- Data Curation and Feature Engineering: Compile a dataset of polymer properties (e.g., molecular weight, hydrophobicity), API properties (e.g., solubility, molecular size), and known experimental release profiles from literature or previous experiments.
- Multi-Scale Simulation:
- Micro-Scale (MD): Run MD simulations to calculate the binding free energy and diffusion coefficient of the API within the candidate polymer. This provides foundational parameters for larger-scale models.
- Meso-Scale (DPD): Use DPD to simulate the formation and stability of the drug-loaded polymer system at a larger scale.
- Macro-Scale (FEA/CFD): Incorporate the parameters derived from MD/DPD into a finite element model of the entire drug delivery device (e.g., an implantable scaffold) to simulate the full drug release profile over time under physiological conditions.
- Machine Learning Model Training: Use the results from the multi-scale simulation stack, along with the curated dataset, to train an ML model. The model learns to map input features (polymer/API properties) directly to output predictions (release kinetics).
- Virtual Screening and Optimization: Employ the trained ML model to rapidly screen thousands of virtual polymer-API combinations in silico, identifying the most promising candidates for further experimental validation. This drastically narrows the focus of costly wet-lab work to only the highest-potential leads.
The following diagram illustrates this AI-augmented, multi-scale simulation approach:
Critical Success Factors and Implementation Roadmap
Building a Cross-Functional and Data-Ready Infrastructure
Successful implementation of these strategies requires more than just software acquisition; it demands organizational and infrastructural readiness.
- Establish a Cross-Functional Team: Effective simulation requires skilled personnel and organizational alignment. Successful organizations establish steering committees incorporating stakeholders from R&D, engineering, clinical affairs, and finance. This ensures that simulation efforts are aligned with business goals and that results are communicated effectively to all decision-makers [67] [64].
- Invest in High-Quality Data Infrastructure: Simulation accuracy is entirely dependent on data quality. Equipment specifications, process parameters, material data, and workflow documentation must be current, complete, and directly relevant. This data structuring phase is critical and often the most time-intensive part of implementation [67]. Utilizing a centralized material data center, as seen with the Altair Material Data Center, is crucial for ensuring consistency and confidence in simulation results [63].
- Start with a Focused Pilot Program: Begin with a concentrated project targeting a specific, high-value medical device or component. A pilot program enables rapid identification of data gaps, demonstrates immediate operational impact, and builds momentum for broader organizational adoption [67].
The Role of Emerging Technologies
The future of efficient simulation cycles is intertwined with the adoption of cutting-edge technologies.
- AI and Machine Learning: AI/ML is revolutionizing simulation by predicting material properties, exploring design alternatives faster, and optimizing manufacturing process parameters. Manufacturing simulation software enhanced with AI can generate predictions up to 1,000 times faster than conventional simulations, allowing teams to evaluate a much wider portfolio of concepts [63] [67].
- Digital Twins: A digital twin is a dynamic virtual replica of a physical product or process that is updated with real-time sensor data. For medical equipment, this allows for continuous monitoring and predictive simulation of performance in the field, enabling predictive maintenance and providing invaluable data for the next design iteration, thus closing the loop on the product lifecycle [67].
- Extended Reality (XR): Virtual and Augmented Reality platforms allow clinicians and engineers to interact with 3D planning results and simulation data digitally. This reduces the need for physical prints, saves time and costs, and enhances collaborative decision-making across medical teams [31].
Adopting the outlined strategies—shifting to a simulation-driven design paradigm, implementing integrated and AI-augmented protocols, and building a supportive infrastructure—provides a clear and actionable pathway to drastically reduce the cost and timeline of the simulation design cycle for 3D medical equipment. By strategically leveraging these methodologies, researchers and drug development professionals can foster greater innovation, enhance product performance and safety, and ultimately bring advanced medical solutions to patients more rapidly and efficiently. The quantitative evidence and detailed protocols presented herein serve as a foundation for transforming design methodology within the medical technology research landscape.
Proving Efficacy: Validation Frameworks and Technology Comparisons
The validation of new medical technologies, including 3D simulation software for medical equipment and training, requires a structured methodological pathway that begins with feasibility assessment and culminates in definitive randomized controlled trials (RCTs). This pathway ensures that innovative solutions are not only technologically sound but also clinically effective and ready for implementation in real-world healthcare settings. Within the broader thesis on design methodology for 3D medical equipment simulations research, this protocol outlines a structured approach to clinical validation, providing researchers with a framework to rigorously evaluate their innovations from initial concept to definitive trial.
The terms "feasibility" and "pilot" study are often used interchangeably, but a defined conceptual framework exists. A feasibility study asks whether a future study can be done, should we proceed with it, and if so, how. A pilot study is a specific type of feasibility study that includes a key design feature: conducting the future study, or part of it, on a smaller scale [68]. This progression is essential for 3D medical simulations, where testing logistical aspects, user acceptance, and preliminary efficacy in a controlled environment de-risks the subsequent large-scale clinical evaluation.
Conceptual Framework and Validation Pathway
The journey from initial concept to a definitive RCT follows a logical sequence, with each stage addressing distinct questions. The following diagram illustrates this pathway and the core questions each stage aims to answer.
Phase 1: Feasibility Assessment
Feasibility studies are preliminary projects conducted to answer the question "Can this study be done?" [68]. They are crucial for identifying potential problems before committing to a full-scale RCT, particularly for complex interventions like 3D medical simulation platforms.
Key Feasibility Indicators and Assessment Methods
A robust feasibility assessment should evaluate multiple domains using quantitative and qualitative methods. The table below summarizes core feasibility indicators, their definitions, and recommended assessment strategies.
Table 1: Feasibility Indicators and Assessment Methods for 3D Simulation Research
| Feasibility Domain | Definition & Key Indicators | Recommended Assessment Methods |
|---|---|---|
| Recruitment & Retention | Ability to identify, enroll, and retain participants in the study [69].• Recruitment rate (participants/month)• Eligibility rate (% of screened participants eligible)• Retention/follow-up completion rates | • Screening logs • Qualitative interviews on barriers to participation•> |
| Intervention Fidelity | The degree to which the intervention is delivered as intended [69].• Interventionist adherence to protocol• Competence in delivery• Participant exposure to intervention | • Direct observation (checklists)• Audio/video recording review• Interventionist self-report logs |
| Acceptability | Perception among stakeholders that the intervention is agreeable, palatable, or satisfactory [69].• Satisfaction ratings• Perceived burden• Willingness to use the simulation again | • Structured surveys (Likert scales)• Semi-structured interviews• Focus groups with end-users (trainees, clinicians) |
| Data Collection Procedures | The practicality and reliability of planned data collection methods [69].• Completion rates for questionnaires/assessments• Time required for assessments• Amount of missing data• Reliability of outcome measures | • Administrative tracking of completion• Timing of assessment sessions• Preliminary psychometric analysis of outcome scores |
Experimental Protocol: Conducting a Feasibility Study for a 3D Neurology Simulation
Objective: To assess the feasibility of methods and procedures for a future RCT evaluating the efficacy of a 3D neurology simulation software for training physiotherapy students [70].
Step 1: Define Scope and Population
- Population: Recruit a small, convenience sample of 15-20 physiotherapy students.
- Intervention: Provide access to the 3D simulation software for a defined training module (e.g., muscle strength examination in stroke patients) [70].
- Duration: A short-term study spanning 4-6 weeks is typically sufficient.
Step 2: Implement and Monitor Feasibility Metrics
- Recruitment: Track the number of students approached, eligible, and consented over one month.
- Retention: Monitor and record participant dropouts and reasons for withdrawal.
- Acceptability: Distribute a post-intervention acceptability questionnaire. Sample items include:
- "The simulation software was easy to use." (1-Strongly Disagree to 5-Strongly Agree)
- "The instructions provided were clear." (1-Strongly Disagree to 5-Strongly Agree)
- "What did you like most/least about using the simulation?"
- Data Collection: Administer a pre- and post-intervention knowledge test. Record completion rates, time taken, and any technical difficulties encountered.
Step 3: Analyze and Interpret Feasibility Data
- Quantitative Analysis: Calculate descriptive statistics (rates, means, percentages) for all feasibility indicators. There should be no emphasis on hypothesis testing for efficacy.
- Qualitative Analysis: Transcribe interviews and focus groups. Use thematic analysis to identify key themes related to usability and acceptability.
- Decision Point: Based on pre-defined "stop/go" criteria (e.g., >70% recruitment rate, >80% retention, high acceptability scores), decide whether to proceed to a pilot study, modify the protocol, or abandon the research trajectory.
Phase 2: The Pilot Randomized Controlled Trial
A pilot RCT is a smaller-scale version of the future definitive RCT and is conducted to test whether all components of the main study can work together [68]. It incorporates the key design feature of randomization.
Core Objectives of a Pilot RCT
- Test RCT Workflow: Evaluate the integration of recruitment, randomization, intervention delivery, blinding, and follow-up procedures.
- Estimate Key Parameters: Obtain robust estimates for the primary and secondary outcomes to inform the sample size calculation for the main RCT. This should focus on estimating confidence intervals around parameters like means, proportions, and event rates, rather than relying on underpowered hypothesis tests [69].
- Refine Interventions: Identify any necessary refinements to the 3D simulation intervention or comparator training based on pilot data.
- Assess Preliminary Safety: Monitor for any unforeseen adverse events related to the simulation training.
Experimental Protocol: Pilot RCT of 3D Simulation vs. Traditional Training
Objective: To conduct a pilot RCT of a 3D neurology simulation software versus traditional training methods to inform the design of a future definitive RCT.
Step 1: Finalize Pilot RCT Design
- Design: A two-arm, randomized, controlled pilot trial.
- Participants: 40-50 physiotherapy students (a rule of thumb is 10-20% of the anticipated sample for the main RCT).
- Randomization: Web-based 1:1 randomization to either the 3D simulation group or the traditional training (control) group.
- Blinding: Outcome assessors should be blinded to group allocation.
Step 2: Define and Measure Outcomes
- Feasibility Outcomes: Continue to track recruitment, retention, and acceptability as in the feasibility study.
- Clinical Outcomes (to inform main RCT):
- Primary Outcome: Muscle strength examination competency score (0-100) assessed via an Objective Structured Clinical Examination (OSCE). This will be used to estimate the standard deviation and effect size for the main RCT sample size calculation.
- Secondary Outcomes: Knowledge test scores, student self-confidence ratings, time to complete the examination.
Step 3: Execute the Pilot Trial and Analyze Data
- Follow the main RCT protocol on a smaller scale, meticulously documenting all procedures and any deviations.
- Statistical Analysis: Focus on estimation. Report means and proportions with 95% confidence intervals for all outcomes. For example, report the between-group difference in OSCE scores with its 95% CI. Avoid reporting p-values for efficacy, as the study is not powered for such tests [69].
Table 2: Key Parameters to Estimate from a Pilot RCT for Main RCT Sample Size Calculation
| Parameter | Description | How it Informs the Main RCT |
|---|---|---|
| Standard Deviation (SD) | The variability of the primary continuous outcome (e.g., OSCE score) in the control group or pooled across groups. | A larger SD requires a larger sample size to detect a given effect. |
| Event Rate | The proportion of participants experiencing an event in the control group (for binary outcomes, e.g., % achieving competence). | Used to calculate the required sample size for a binary outcome. |
| Recruitment & Retention Rates | The average number of participants recruited per month and the proportion retained until primary outcome assessment. | Allows for realistic planning of the recruitment period and inflation of the initial sample size to account for dropouts. |
| Effect Size Estimate | The anticipated difference between intervention and control groups, expressed as a standardized mean difference or risk ratio. | The smaller the effect size one wishes to detect, the larger the sample size required. |
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential methodological components and their functions in the clinical validation pathway for 3D medical simulation research.
Table 3: Essential Methodological Components for Clinical Validation Research
| Item | Function & Application in Validation Research |
|---|---|
| Feasibility Framework | A structured set of indicators (recruitment, retention, fidelity, acceptability) used to systematically assess the practicality of a future larger study [69]. |
| Sample Size Justification (Pilot) | Rationale for the number of participants in a pilot trial, based on precision (e.g., width of CI) for estimating a parameter, rather than power for a statistical test [69]. |
| Mixed-Methods Approach | The integration of quantitative data (e.g., scores, rates) and qualitative data (e.g., interviews) to provide a comprehensive understanding of feasibility and acceptability [69]. |
| Structured Scenario | A researcher-developed, standardized script detailing the use case for the 3D simulation, ensuring consistent intervention delivery and evaluation across participants [70]. |
| Expert Validation Panel | A group of content experts (e.g., physiotherapy professors) used to validate research instruments, scenarios, and outcome measures, often using Content Validity Index (CVI) calculations [70]. |
| Objective Structured Clinical Exam (OSCE) | A performance-based assessment tool used to evaluate clinical competence in a standardized setting, often serving as a primary outcome in training-related RCTs. |
| Dexamethasone Cipecilate | Dexamethasone Cipecilate, CAS:132245-57-9, MF:C33H43FO7, MW:570.7 g/mol |
A rigorous, stage-gated approach to clinical validation, moving systematically from feasibility assessment to pilot RCT and finally to a definitive RCT, is fundamental to generating credible evidence for 3D medical simulation technologies. This protocol emphasizes the critical distinction between asking "Can it be done?" (feasibility) and "How do the components work together?" (pilot) [68]. By focusing on feasibility indicators and estimation in early-phase studies, researchers can optimize their protocols, manage resources efficiently, and ultimately increase the likelihood of a successful definitive trial that validly demonstrates the impact of their innovative medical simulation tools.
The objective evaluation of surgical performance in simulation-based training requires a robust framework of quantitative metrics. These metrics are critical for assessing the efficacy of 3D-printed simulators and immersive technologies in bridging the gap between theoretical design and clinical application. This document outlines standardized metrics and protocols for measuring impact across three critical domains: surgical time, surgical precision, and patient outcomes, providing researchers with validated methodologies for equipment simulation research.
Core Quantitative Metrics and Data Presentation
Surgical Time Metrics
Surgical time is a fundamental efficiency metric with direct implications for operating room utilization and healthcare costs. The table below summarizes key performance indicators (KPIs) derived from recent studies.
Table 1: Key Metrics for Surgical Time and Scheduling Accuracy
| Metric | Definition | Measurement Method | Exemplary Findings |
|---|---|---|---|
| Duration of Surgery (DOS) | Time from incision to closure. | Retrospective analysis of EHR data; prediction using ML models [71]. | ML models predicted DOS for TKA/THA with 78.1% and 75.4% accuracy (30-min buffer) [71]. |
| Scheduling Accuracy | Conformance of actual to scheduled time [72]. | Percentage of cases within ±30 min (±20% for procedures <150 min) of scheduled time [72]. | Education reduced scheduling manipulation from 19.8% to 7.6%, raising accuracy from 41.7% to 47.9% [72]. |
| Overtime/Underutilization | Operating room time used beyond or below planned schedule. | Summing daily minutes outside scheduled blocks in simulation [71]. | ML-predict-then-optimize scheduling reduced overtime by 300-500 minutes weekly versus mean-DOS scheduling [71]. |
Surgical Precision and Skill Acquisition Metrics
Surgical precision transcends speed, encompassing technical skill and procedural quality. Immersive simulation platforms enable detailed tracking of these metrics.
Table 2: Metrics for Surgical Precision and Proficiency
| Metric Category | Specific Metrics | Measurement Tools |
|---|---|---|
| Technical Proficiency | Path length of instruments, tool-tissue force, number of movements [46]. | VR simulator software, motion tracking sensors, force-sensitive equipment. |
| Procedural Knowledge | Correct order of steps, appropriate instrument selection, error rate. | Expert observation using structured checklists, automated analysis of simulator logs. |
| User Confidence | Self-rated confidence in performing procedures or using technology. | Pre- and post-training surveys on a 5-point Likert scale [46]. |
Patient Outcome Metrics
The ultimate validation of surgical simulation is its impact on patient care. Research correlates simulation training with improved clinical results.
Table 3: Patient Outcome Metrics Linked to Simulation Training
| Metric | Rationale | Data Source |
|---|---|---|
| Operative Wait Times | Efficient scheduling and skilled surgeons reduce patient backlog. | Hospital administration records [71]. |
| Patient Satisfaction | Accurate scheduling minimizes delays and cancellations [72]. | Patient-reported satisfaction surveys [72]. |
| Rate of Medical Errors | Simulation allows practice in risk-free environments, reducing real-world mistakes [41]. | Clinical incident reports, EHR data. |
Experimental Protocols for Metric Validation
Protocol A: Predict-Then-Optimize Operating Room Scheduling
This protocol validates machine learning models for improving surgical time efficiency [71].
- Objective: To determine if ML-predicted DOS, combined with schedule optimization, improves operating room utilization over using historical mean DOS.
- Data Collection:
- Source data from a clinical database (e.g., ACS NSQIP) including patient age, BMI, procedure type, and actual DOS for thousands of procedures (e.g., TKA and THA) [71].
- Define institutional constraints: number of operating rooms, cleaning time, surgeon availability.
- Prediction Model Training:
- Partition data into training, validation, and test sets (e.g., 2014-2017, 2018, 2019).
- Train a multilayer perceptron model to predict DOS using patient-specific variables.
- Validate model performance using Mean Squared Error (MSE) and accuracy within a defined time buffer (e.g., 30 minutes).
- Schedule Optimization & Simulation:
- Formulate optimization problems (e.g., "Any", "Split", "MSSP") with constraints on surgeon-to-room assignments [71].
- Run multi-year daily scheduling simulations using both ML-predicted and mean DOS values.
- Key Output Metrics: Total weekly overtime, total weekly underutilization, and schedule accuracy percentage.
Workflow for ML-driven OR scheduling.
Protocol B: Evaluating Simulation-Based Training Efficacy
This protocol measures the impact of VR and 3D simulator training on surgical precision and confidence.
- Objective: To quantify the improvement in technical skill and user confidence following immersive simulation training.
- Study Design: Mixed-methods educational implementation study with pre- and post-training assessments [46].
- Participant Recruitment:
- Recruit healthcare professionals (surgeons, residents, students) via institutional emails and professional networks. Target sample size ~350 [46].
- Intervention:
- Conduct structured workshops providing hands-on experience with:
- VR simulators for procedural rehearsal.
- 3D display systems for anatomical visualization.
- Metaverse platforms for collaborative planning.
- Conduct structured workshops providing hands-on experience with:
- Data Collection:
- Quantitative: Administer pre- and post-workshop surveys measuring self-reported confidence on a 5-point Likert scale [46].
- Qualitative: Collect structured feedback on usability and barriers.
- Performance Data: Record simulator-generated metrics (path length, time, error rate).
- Data Analysis:
- Use paired t-tests to compare pre- and post-confidence scores.
- Perform thematic analysis on qualitative feedback to identify key themes (e.g., cost, infrastructure).
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Resources for Surgical Simulation and Metrics Research
| Item / Technology | Function in Research | Specific Examples/Models |
|---|---|---|
| Virtual Reality (VR) Simulators | Provides a risk-free environment for procedural rehearsal and objective skill assessment [46]. | Surgical training platforms for laparoscopy, arthroscopy, etc. |
| 3D Display & Printing Systems | Creates high-fidelity anatomical models and visualizations for preoperative planning and hands-on training [41] [46]. | 3D printers for producing organ models; 3D monitors for visualization. |
| Metaverse Platforms | Facilitates remote, collaborative surgical planning and interdisciplinary consultation in shared virtual spaces [46]. | Customizable virtual reality environments for team meetings. |
| Electronic Health Record (EHR) Data | Serves as the primary data source for developing predictive models of surgical duration and outcomes [72] [71]. | Epic EHR system; ACS NSQIP database [72] [71]. |
| Machine Learning Frameworks | Enables the development of predictive models for surgery duration and optimization algorithms. | PyTorch multilayer perceptron models [71]. |
Research system input-output flow.
Comparative Analysis of Leading 3D Printing Technologies for Medical Applications
Additive manufacturing, or 3D printing, is revolutionizing healthcare by shifting the paradigm from mass production to personalized medicine. This technology enables the creation of patient-specific medical devices, implants, and anatomical models with unparalleled precision, thereby enhancing surgical outcomes, accelerating drug development, and paving the way for regenerative medicine [58]. This document provides a comparative analysis of leading 3D printing technologies within the context of a design methodology for 3D medical equipment simulations, offering detailed application notes and experimental protocols for researchers and drug development professionals.
Quantitative Comparison of Leading 3D Printing Technologies
The selection of an appropriate 3D printing technology is critical and depends on the intended application, required material properties, and necessary resolution. The following table summarizes the key characteristics of prominent technologies used in medical applications.
Table 1: Comparative Analysis of 3D Printing Technologies in Healthcare
| Technology | Key Medical Applications | Common Materials | Key Characteristics & Advantages |
|---|---|---|---|
| Photopolymerization (SLA, DLP) [23] [73] | Dental ceramics, tissue engineering scaffolds, detailed anatomical models | Photopolymer resins, ceramic slurries | High spatial resolution, excellent surface finish; suitable for complex geometries [74]. |
| Fused Deposition Modeling (FDM) [23] [58] | Low-cost prosthetics, surgical guides, medical device prototypes | Medical-grade polymers (PEEK, Nylon) | Widely accessible, cost-effective; functional parts with good mechanical properties [58]. |
| Selective Laser Sintering (SLS) [23] | Porous implants, clinical study devices | Nylon, metal powders (Ti, CoCr) | Creates strong, functional parts without need for support structures [58]. |
| Binder Jetting (BJ) [23] | Drug dosage forms, bone-like scaffolds | Powdered materials, including pharmaceuticals | High speed, multi-material capability; enables complex drug release profiles [23]. |
| PolyJet Printing [75] [58] | Multi-colored anatomical models, simulators, soft-tissue prototypes | Photopolymer resins | Multi-material and full-color capabilities; high detail for realistic models [75]. |
Application Notes and Methodologies for Medical Research
Experimental Protocol: Comparative Analysis of 3D-Printed vs. Milled Zirconia
Background: This protocol outlines a methodology for comparing the mechanical and surface properties of 3D-printed and milled zirconia, a common material for dental restorations and implants [74].
Workflow Diagram: The following diagram illustrates the experimental workflow for the comparative analysis of zirconia specimens.
Diagram Title: Zirconia Specimen Test Workflow
Methodology:
- Specimen Preparation and Fabrication:
- Design: Create a digital model (e.g., a crown or a 10 mm diameter, 2 mm thick disc) and export in STL format [74].
- Milled Group: Fabricate specimens using a 5-axis milling machine from 3 mol% yttria-stabilized zirconia blocks, followed by sintering according to manufacturer guidelines [74].
- 3D-Printed Group: Fabricate specimens using a lithography-based ceramic printer (e.g., Lithoz CeraFab system). Utilize a zirconia slurry with a layer thickness of 25 µm. After printing, clean with solvent, then proceed with debinding and sintering [74].
- Post-Processing: Polish and glaze all specimens. Subject them to thermocycling (e.g., 5000 cycles) to simulate oral aging [74].
- Property Testing:
- Fracture Resistance: Measure using a universal testing machine. Perform fractographic analysis using Scanning Electron Microscopy (SEM) [74].
- Surface Roughness: Measure using a contact profilometer on both glazed and unglazed specimens [74].
- Microhardness: Measure on unglazed specimens using a Vickers microhardness tester [74].
- Data Analysis: Perform statistical analysis (e.g., independent samples t-test, two-way ANOVA) to compare results between groups, with a significance level set at p < 0.05 [74].
Application-Specific Workflows
Diagram Title: Medical 3D Printing Project Flow
Key Applications:
- Implants and Prosthetics: 3D printing enables patient-specific implants (orthopedic, cranial) and prosthetics with perfect anatomical fit, improving comfort and surgical outcomes [58].
- Surgical Planning and Guides: Anatomical models derived from patient scans allow surgeons to simulate complex procedures. Patient-specific surgical guides ensure precise placement of instruments and implants [58].
- Pharmaceutical Printing (3DP): Enables the production of personalized medications with tailored dosages, drug combinations, and complex release profiles (e.g., controlled release, orodispersible formulations) [23].
- Bioprinting: Uses bio-inks containing living cells to fabricate tissue constructs (skin, cartilage) and organoids for research and regenerative medicine, aiming to address the global organ shortage [76] [58].
The Scientist's Toolkit: Essential Research Reagents & Materials
A critical aspect of experimental design is the selection of appropriate materials. The following table details key materials used in medical 3D printing research.
Table 2: Essential Materials for Medical 3D Printing Research
| Material Category | Specific Examples | Research Application & Function |
|---|---|---|
| Biocompatible Metals | Titanium, Cobalt-Chrome alloys [58] | Used for creating load-bearing orthopedic and dental implants due to their high strength, durability, and biocompatibility. |
| Medical Polymers | PEEK, Nylon, Photopolymer Resins [58] | Employed in fabricating surgical guides, lightweight prosthetics, and detailed anatomical models for simulation. |
| Advanced Ceramics | 3 mol% Yttria-Stabilized Zirconia [74] | Ideal for dental crowns and implants due to high fracture toughness, biocompatibility, and aesthetic properties. |
| Bio-inks | Cell-laden hydrogels (Collagen, Gelatin) [58] | The foundation of bioprinting; used to create scaffolds and 3D tissue constructs for regenerative medicine and drug testing. |
| Pharmaceutical Powders | Active Pharmaceutical Ingredients (APIs) with excipients [23] | Enable the additive manufacturing of personalized drug dosage forms with specific release characteristics. |
Challenges and Future Outlook
Despite its promise, the field faces several challenges. These include high initial equipment costs, the need for stringent and evolving regulatory compliance (FDA, MDR), and a limited range of fully validated biocompatible materials [23] [58]. Furthermore, ensuring consistent quality control for personalized products and scaling up production remain significant hurdles [23].
The future of medical 3D printing is closely tied to technological convergence. The integration of Artificial Intelligence (AI) is anticipated to optimize design and printing parameters [73]. The expansion of bioprinting capabilities continues to advance toward functional tissues and organs [76] [58]. Finally, the trend toward point-of-care manufacturing within hospitals is set to reduce lead times and further personalize patient care [73] [58].
Evaluating Software Platforms for Medical 3D Modeling and Simulation
Application Note: Platform Selection for Research-Grade Medical Simulation
The selection of software platforms for medical 3D modeling and simulation requires a rigorous methodology aligned with both technological capabilities and evidence-based educational science. Within a research context focused on 3D medical equipment simulations, platforms must support the creation of valid, reliable, and reproducible simulated experiences. The Healthcare Simulation Standards of Best Practice (HSSOBP) provide a critical framework for ensuring quality and consistency in simulation-based research and training [77]. This document outlines criteria and protocols for evaluating software platforms to ensure they meet the demands of academic research and clinical skill development.
Key Evaluation Criteria for Research Software
Software platforms should be assessed against a multi-faceted set of criteria to determine their suitability for academic and clinical research. The following table summarizes the core quantitative and qualitative metrics.
Table 1: Core Evaluation Criteria for Medical 3D Simulation Software
| Evaluation Dimension | Specific Metrics & Considerations | Relevance to Research |
|---|---|---|
| Fidelity & Realism | Anatomical accuracy, physical material properties, haptic feedback integration, visual rendering quality | Determines the validity and ecological relevance of the simulation experience [5]. |
| Interoperability | Support for DICOM import, compatibility with CAD formats, API availability for custom instrumentation | Essential for creating simulations based on real patient data and integrating with research equipment [78]. |
| Specialized Functionality | Tools for surgical planning, procedure rehearsal, device prototyping, and physics-based deformation analysis | Directly supports the design methodology for 3D medical equipment and procedural training [5] [78]. |
| Compliance & Standards | Alignment with HSSOBP (e.g., in simulation design, facilitation, and debriefing), data privacy (HIPAA/GDPR) | Ensures research methodologies are grounded in recognized best practices and ethical guidelines [77] [79]. |
| Output & Analysis | Data logging capabilities, performance metrics export, and compatibility with data analysis tools (e.g., Python, R) | Enables quantitative analysis of user performance and outcomes for rigorous research. |
Experimental Protocols for Platform Validation
Protocol 1: Quantitative Fidelity and Usability Assessment
1. Objective: To quantitatively evaluate the anatomical fidelity and user interactivity of a 3D modeling platform in recreating a complex anatomical structure.
2. Background: High-fidelity simulation has been shown to improve skill scores in medical diagnosis and treatment, particularly in specialized fields like neurology and neurosurgery [5]. This protocol provides a standardized method for assessing these qualities in a new software platform.
3. Materials & Reagents: Table 2: Research Reagent Solutions for Fidelity Assessment
| Item | Function/Description | Example Sources/Alternatives |
|---|---|---|
| Source Medical Imaging Data | Provides the ground-truth dataset for model creation (e.g., MRI, CT scans in DICOM format). | Public repositories (e.g., The Cancer Imaging Archive). |
| Reference Anatomical Atlas | Serves as a gold standard for verifying anatomical accuracy. | Published scientific atlases (e.g., Atlas of Human Anatomy). |
| 3D Modeling & Simulation Software | The platform under evaluation. | Materialise, 3D Systems, Siemens PLM [78]. |
| Haptic Input Device | Enables physical interaction with the virtual model, assessing usability and force feedback. | Geomagic Touch, other force-feedback interfaces. |
4. Methodology:
- Step 1: Data Import and Segmentation. Import a standardized DICOM dataset (e.g., a cranial CT scan) into the software. Use the platform's tools to segment key anatomical structures (e.g., the circle of Willis).
- Step 2: 3D Model Generation. Generate a 3D mesh model from the segmented data. Document the time required and the number of manual corrections needed.
- Step 3: Metric Analysis.
- Accuracy: Compare the software-generated 3D model to the reference anatomical atlas by measuring dimensional variances (in mm) at 10 predefined anatomical landmarks.
- Usability: Task five expert neurosurgeons with performing a virtual vessel dissection procedure. Record task completion time and score performance using a validated instrument like the Objective Structured Assessment of Technical Skill (OSATS).
- Step 4: Data Collection. Collect all quantitative measurements (dimensional variances, time, OSATS scores) for statistical analysis.
5. Statistical Analysis: Perform a one-sample t-test to compare the dimensional variances of the software-generated model against the null hypothesis of zero variance (perfect accuracy). Report descriptive statistics (mean, standard deviation) for usability metrics.
The workflow for this validation protocol is outlined below.
Protocol 2: Integration with Simulation-Based Education Best Practices
1. Objective: To validate that a software platform can effectively support a simulation-based experience (SBE) designed and executed in accordance with the Healthcare Simulation Standards of Best Practice (HSSOBP).
2. Background: Appropriately designed simulation activities that utilize rigorous frameworks are critical for effective learning, yet their consistent application remains a challenge [79]. This protocol tests a platform's ability to facilitate key standards.
3. Materials:
- Software platform under test.
- A pre-written simulation scenario (e.g., managing an acute ischemic stroke) with defined objectives and outcomes [5].
- Assessment tools (e.g., checklists, surveys) for learner performance and satisfaction.
4. Methodology:
- Step 1: Prebriefing - Preparation and Briefing. Use the software to create and display orientation materials about the virtual environment and the scenario objectives, directly supporting the HSSOBP Prebriefing standard [77].
- Step 2: Simulation Design & Facilitation. Execute the scenario within the platform. The researcher/facilitator should use the platform's features (e.g., pausing, environmental changes) to apply appropriate facilitation methods as per HSSOBP [77].
- Step 3: Debriefing Process. Utilize the software's data logging and playback features to support a structured debriefing. Key moments and performance metrics captured by the software should be used for guided reflection, aligning with the HSSOBP Debriefing standard [77].
- Step 4: Evaluation of Learning. Analyze the performance metrics automatically logged by the software (e.g., time to administer tPA, accuracy of decisions) against the predefined objectives, supporting the HSSOBP Evaluation of Learning and Performance standard [77].
5. Outcome Measures: The primary outcome is a binary determination (Yes/No) of whether the platform's features adequately support each of the four targeted HSSOBP standards (Prebriefing, Simulation Design, Facilitation, and Debriefing). Secondary outcomes include qualitative feedback from facilitators and learners on the platform's utility in each phase.
The logical relationship between HSSOBP and the platform validation is as follows.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for 3D Medical Simulation
| Item | Function/Description | Research Application Example |
|---|---|---|
| High-Fidelity Patient Simulator | A full-body manikin that replicates physiological responses (e.g., pulse, breathing). | Integrated with a 3D visualizer to create a hybrid simulation for studying team-based responses to clinical deterioration [77]. |
| Haptic Feedback Device | Provides force feedback and tactile sensation to the user during virtual interactions. | Essential for research on the psychomotor skill acquisition of surgical procedures, such as catheter manipulation or tumor resection [5] [78]. |
| 3D Anatomical Phantom | A physical, patient-specific model created via 3D printing from medical imaging data. | Serves as a ground-truth, tangible validation tool for the accuracy of virtual models created in the software platform. |
| Eye-Tracking System | Records where, when, and what a user looks at while performing a task. | Used in usability studies to assess the cognitive load and visual attention of trainees during a virtual simulation, identifying interface confusions. |
| Physiological Data Logger | Records biometric data such as EEG, heart rate variability, and galvanic skin response. | Correlates stress and cognitive engagement with performance metrics during high-fidelity, high-stress simulation scenarios [5]. |
Conclusion
The integration of 3D simulation methodologies is fundamentally reshaping the design and testing of medical equipment, moving the industry toward a future of personalized, data-driven medicine. The synergistic application of CAD, AI, and additive manufacturing compresses development timelines, enhances precision, and facilitates robust clinical validation. For researchers and drug development professionals, mastering these methodologies is no longer optional but essential for driving innovation. Future directions will involve greater convergence of generative AI for predictive design, expanded use of bioresorbable materials, and the maturation of regulatory pathways for software-as-a-medical-device. The continued adoption of these technologies promises to accelerate biomedical research, improve clinical trial design, and ultimately deliver more effective and personalized patient therapies.
References
- 1. Conquer medical device development complexity with advanced modeling tools - Medical Devices & Pharmaceuticals [https://blogs.sw.siemens.com/medical-devices-pharmaceuticals/2025/03/06/conquer-medical-device-development-complexity-with-advanced-modeling-tools/]
- 2. CAD in the medical device industry - PubMed [https://pubmed.ncbi.nlm.nih.gov/10186990/]
- 3. ã€2025】What Is CAD in Medical Terms? Understanding Its Role in Healthcare | CAD CAM CAE Lab [https://cad-kenkyujo.com/en/3dcad/cad-medical/]
- 4. The Importance of 3D Modeling in Healthcare [https://www.osfinnovation.org/jump-simulation/blog/the-importance-of-3d-modeling-in-healthcare]
- 5. Medical simulation: an essential tool for training, diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12235771/]
- 6. 隆é‡æŽ¨å‡ºNVIDIA Isaac 医疗å¥åº·ç‰ˆï¼šä¸€æ¬¾AI 驱动的 ... [https://developer.nvidia.cn/blog/introducing-nvidia-isaac-for-healthcare-an-ai-powered-medical-robotics-development-platform/]
- 7. AI驱动医疗å˜é©ï¼é¦–届深圳市人工智能医院建设与å‘展大会 ... [https://wjw.sz.gov.cn/wzx/content/post_12465021.html]
- 8. 上海市å«ç”Ÿå¥åº·å§”员会关于组织申报2025å¹´æ™ºæ…§åŒ»ç–—ä¸“é¡¹ç ”ç©¶ ... [https://wsjkw.sh.gov.cn/kjjy2/20250603/e0132d8c522d4d409619687f91b0e88e.html]
- 9. 上海市科å¦æŠ€æœ¯å§”员会关于å‘布2025å¹´åº¦åŸºç¡€ç ”ç©¶è®¡åˆ’â€œæŽ¢ç´¢ ... [https://www.sues.edu.cn/60/06/c17467a286726/page.htm]
- 10. 医疗设备- 患者监护- MATLAB & Simulink - MathWorks [https://ww2.mathworks.cn/solutions/medical-devices/patient-monitoring.html]
- 11. Data-Driven Design and Additive Manufacturing of Patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12470917/]
- 12. Additive manufacturing of patient-specific, biphasic ... [https://www.sciencedirect.com/science/article/pii/S2590006425004181]
- 13. Additive manufacturing for biomedical applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC9793824/]
- 14. Educational use of patient-specific 3D-printed models in ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-025-07821-4]
- 15. The application of the metaverse in surgical clinical teaching [https://pmc.ncbi.nlm.nih.gov/articles/PMC12380747/]
- 16. Osso VR [https://www.ossovr.com/]
- 17. The metaverse in orthopaedics: Virtual, augmented and ... [https://pubmed.ncbi.nlm.nih.gov/40622017/]
- 18. Augmented Reality Is Transforming Surgical Training and ... [https://www.cbs42.com/business/press-releases/ein-presswire/861551704/augmented-reality-is-transforming-surgical-training-and-medical-education-at-kfshrc]
- 19. Efficacy of three-dimensional models for medical education [https://pmc.ncbi.nlm.nih.gov/articles/PMC9932677/]
- 20. Metaverse Meets Medicine: Spatial Computing's Game- ... [https://www.eos-intelligence.com/perspectives/medical-devices/metaverse-meets-medicine-spatial-computings-game-changing-potential/]
- 21. Augmented Reality and Virtual Reality in Medical Devices [https://www.fda.gov/medical-devices/digital-health-center-excellence/augmented-reality-and-virtual-reality-medical-devices]
- 22. VR-prep improves visualization of medical data in ... [https://www.nature.com/articles/s41598-025-26856-7]
- 23. The Future of Medicine: How 3D Printing Is Transforming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11946218/]
- 24. From Pixels to Prototypes: 3D Printing Innovations in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563727/]
- 25. Enhancing Planning with Medical 3D Printing Apps [https://inoxoft.com/blog/how-medical-3d-printing-apps-improve-workflow/]
- 26. Generative AI for medical 3D printing: a comparison of ... [https://threedmedprint.biomedcentral.com/articles/10.1186/s41205-023-00186-8]
- 27. Teaching Medical Device Engineering with the ... [https://www.3ds.com/edu/education/academics/3dexperience/medical-package]
- 28. How to Meet the New Simulation Testing Requirements [https://www.mddionline.com/testing/how-to-meet-the-new-simulation-testing-requirements]
- 29. Medical Device Design: The Complete 2025 Guide [https://www.jacksonhedden.com/iterate/medical-device-design-guide]
- 30. Interpretation of regulatory factors for 3D printing at hospitals ... [https://threedmedprint.biomedcentral.com/articles/10.1186/s41205-022-00134-y]
- 31. 3D Planning and Printing at Point of Care: 2025 Trends [https://www.materialise.com/en/inspiration/articles/trends-3d-planning-printing-point-of-care-2025]
- 32. 3D Printing in a hospital: Centralized clinical implementation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10734340/]
- 33. 3D Anatomic Modeling Laboratories - Overview [https://www.mayoclinic.org/departments-centers/anatomic-modeling-laboratories/overview/ovc-20473121]
- 34. 3D Bioprinting in 2025: What Medical Device Makers Need to ... [https://diasurgemed.com/ng/3d-bioprinting-in-2025-what-medical-device-makers-need-to-know-now/]
- 35. Guide to 3D Printing Medical Devices [https://formlabs.com/blog/3d-printing-medical-devices/?srsltid=AfmBOoo8ee225hj3ZCyOdNS0EUA_UJoVs7eLzBwDNxUz25HW5Ps60XSb]
- 36. 3D printing simulation software for accurate, reliable prints [https://sinterit.com/3d-printing-guide/software-for-3d-printing/3d-printing-simulation-software/]
- 37. 3D Printing of Medical Devices [https://www.fda.gov/medical-devices/products-and-medical-procedures/3d-printing-medical-devices]
- 38. Statistical methods for design and testing of 3D-printed polymers [https://pmc.ncbi.nlm.nih.gov/articles/PMC9976681/]
- 39. Predictions for high precision 3D printing and healthcare ... [https://www.medicaldesignandoutsourcing.com/high-precision-3d-printing-healthcare-innovation-predictions-bmf/]
- 40. Orthopedic Trainees' Perception of the Educational Utility of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12345946/]
- 41. Exploring the Distribution of 3D-Printed Simulator Designs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11165279/]
- 42. SCOPE 2025 Highlights: AI, Digital Protocols & Other ... [https://psi-cro.com/scope-2025-highlights-ai-digital-protocols-innovations/]
- 43. AI In clinical trials in 2025: the edge of tech [https://clinicaltrialrisk.org/clinical-trial-design/ai-in-clinical-trials-the-edge-of-tech/]
- 44. Modeling of Tool-Tissue Interactions for Computer-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2813063/]
- 45. Modelling the interaction between wearable assistive ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.1044275/full]
- 46. a global mixed-methods study of VR, metaverse, and 3D ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1632528/full]
- 47. Medical Simulation Market | Global Market Analysis Report [https://www.factmr.com/report/medical-simulation-market]
- 48. Medical Simulation Market Outlook Report 2026-2034: [https://www.globenewswire.com/news-release/2025/11/13/3187638/0/en/Medical-Simulation-Market-Outlook-Report-2026-2034-Expansion-Driven-by-Shift-Toward-Simulation-First-Training-Models-and-Rising-Demand-for-Risk-Reduction-and-Outcome-Optimization.html]
- 49. Healthcare Simulation Market Forecast 2025 to 2034 Key ... [https://www.towardshealthcare.com/insights/healthcare-simulation-market-sizing]
- 50. AI-Enhanced 3D Models in Global Virtual Reality Case ... [https://formative.jmir.org/2025/1/e69300]
- 51. Credibility of Computational Models Program: Research on ... [https://www.fda.gov/medical-devices/medical-device-regulatory-science-research-programs-conducted-osel/credibility-computational-models-program-research-computational-models-and-simulation-associated]
- 52. Medical Device Quality Management System (QMS) [https://simplerqms.com/medical-device-quality-management-system/]
- 53. Quality Management System Regulation: Final Rule [https://www.fda.gov/medical-devices/quality-system-qs-regulationmedical-device-current-good-manufacturing-practices-cgmp/quality-management-system-regulation-final-rule-amending-quality-system-regulation-frequently-asked]
- 54. Quality System (QS) Regulation/Medical Device Current ... [https://www.fda.gov/medical-devices/postmarket-requirements-devices/quality-system-qs-regulationmedical-device-current-good-manufacturing-practices-cgmp]
- 55. Manufacturers, Importers and Device User Facilities [https://www.fda.gov/medical-devices/postmarket-requirements-devices/mandatory-reporting-requirements-manufacturers-importers-and-device-user-facilities]
- 56. Breakthrough Trends in Medical Device Design 2025 [https://pshdesign.com/breakthrough-trends-in-medical-device-design-2025/]
- 57. New Frontiers in 3D Printing Using Biocompatible Polymers [https://pubmed.ncbi.nlm.nih.gov/40869336/]
- 58. 2025 Guide to Medical 3D Printing: Applications and Benefits [https://www.weerg.com/guides/medical-3d-printing]
- 59. Optimising the biocompatibility of 3D printed photopolymer ... [https://pubmed.ncbi.nlm.nih.gov/30795002/]
- 60. Choosing 3D Printing Materials for Medical Applications [https://www.novusls.com/post/medical-3d-printing-material-selection-guide?srsltid=AfmBOoqiMs1gISrrnq4NpIt0Cs7nFpqN-siYwqhA2J5suczc1k_gTdwx]
- 61. Guide to 3D Printing Materials: Types, Applications, and ... [https://formlabs.com/blog/3d-printing-materials/?srsltid=AfmBOopILnkkDmWnkcr1CfT9J-Yp_n4OXir3TvIN21CKnLlWDfMJqW0a]
- 62. Biocompatible 3D printing resins for medical applications [https://www.sciencedirect.com/science/article/pii/S2666964121000394]
- 63. Simulation-Driven Design: Performance, Sustainability & ... [https://altair.com/blog/articles/simulation-driven-design-performance]
- 64. The Business Case for Simulation-Led Design [https://www.digitalengineering247.com/article/the-business-case-for-simulation-led-design]
- 65. 3d-printing-medical-devices-transforming-healthcare [https://www.marketsandmarkets.com/blog/HC/3d-printing-medical-devices-transforming-healthcare]
- 66. Simulation-based approaches for drug delivery systems [https://www.sciencedirect.com/science/article/pii/S0167732223026958]
- 67. Why Simulation Software is the Hidden Key to Smart ... [https://www.simio.com/why-simulation-software-is-the-hidden-key-to-smart-factory-success-transforming-data-into-manufacturing-excellence/]
- 68. Defining Feasibility and Pilot Studies in Preparation for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0150205]
- 69. Guidelines for Designing and Evaluating Feasibility Pilot ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8849521/]
- 70. Design specifications and capabilities of a 3D simulation ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-05547-3]
- 71. Using Machine Learning to Predict-Then-Optimize Elective ... [https://medinform.jmir.org/2025/1/e70857]
- 72. Intervention with surgeons improves the accuracy of ... [https://www.wolterskluwer.com/en/news/intervention-with-surgeons-improves-the-accuracy-of-predicted-operating-room-time]
- 73. 3D Printing Healthcare Analysis 2025-2033: Unlocking ... [https://www.datainsightsmarket.com/reports/3d-printing-healthcare-1195213]
- 74. a comparative analysis of 3D printing and milling techniques [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291343/]
- 75. Full Color 3D Printing Best Practices [https://www.xometry.com/resources/3d-printing/full-color-3d-printing/]
- 76. A roadmap for the implementation of 3D-printed organs in ... [https://www.sciencedirect.com/science/article/pii/S2666998625001607]
- 77. Healthcare Simulation Standards of Best Practice® [https://www.inacsl.org/healthcare-simulation-standards-of-best-practice-]
- 78. Top 3D Imaging Software Companies & How to Compare ... [https://www.linkedin.com/pulse/top-3d-imaging-software-companies-how-compare-them-h383f]
- 79. The Application and Integration of Evidence-Based Best ... [https://www.sciencedirect.com/science/article/pii/S1876139923001093]