Advances in Electrical Impedance Tomography: From Deep Learning Reconstruction to Clinical and Preclinical Applications
This article provides a comprehensive overview of the latest methodological advancements in Electrical Impedance Tomography (EIT), a non-invasive, radiation-free functional imaging technique.
Advances in Electrical Impedance Tomography: From Deep Learning Reconstruction to Clinical and Preclinical Applications
Abstract
This article provides a comprehensive overview of the latest methodological advancements in Electrical Impedance Tomography (EIT), a non-invasive, radiation-free functional imaging technique. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles of EIT and the complete electrode model. It delves into cutting-edge reconstruction algorithms, particularly deep learning-based methods, and their application across scales—from lung and brain monitoring in patients to intracellular imaging in drug discovery. The content further addresses critical challenges in hardware implementation and system optimization, and provides a framework for the functional validation and comparative analysis of different EIT approaches, synthesizing key insights to guide future research and clinical integration.
The Fundamentals of EIT: Principles, Models, and the Ill-Posed Inverse Problem
Core Physical Principles and the Complete Electrode Model
Electrical Impedance Tomography (EIT) is a non-invasive, radiation-free medical imaging modality that generates real-time images by measuring the bioimpedance distribution within biological tissues [1]. It operates on the fundamental principle that different tissues possess distinct electrical conductivity and permittivity properties, which can be exploited to create cross-sectional images of the body [1]. This application note details the core physical principles underpinning EIT, with a specific focus on the Complete Electrode Model (CEM), which is essential for accurate image reconstruction. The content is framed within a broader research thesis on advancing EIT imaging methodologies for clinical and research applications, including potential use in drug development for monitoring physiological changes.
Core Physical Principles of EIT
Fundamentals of Bioimpedance
Bioimpedance is a measure of a biological tissue's opposition to the flow of electric current. Tissue impedance (Z) consists of two primary components: resistance (R), which dissipates energy as heat, and capacitance (C), which stores and releases energy [1].
- Resistance and Capacitance in Tissues: The resistance of an aqueous tissue solution behaves similarly under both direct current (DC) and alternating current (AC) fields. In contrast, capacitance arises primarily from the phospholipid bilayer of cell membranes. This bilayer blocks DC but, in an AC field, stores and releases energy, facilitating current flow in a frequency-dependent manner [1].
- Frequency-Dependent Behavior: In AC fields, the overall tissue impedance is determined by both resistance and capacitance. This relationship varies with frequency due to the influence of cellular and extracellular structures [1].
- At low frequencies, current flows primarily around cells (extracellularly) because the cell membrane acts as a capacitor blocking current.
- At high frequencies, the capacitive reactance of the cell membrane decreases, allowing current to penetrate and flow through the intracellular compartments [1].
- Cole-Cole Plots: The frequency-dependent impedance spectrum of biological tissues is often visualized using Cole-Cole plots, where resistance and reactance form a characteristic semicircular curve over a range of frequencies [1].
The Inverse Problem in EIT
EIT belongs to a class of mathematical challenges known as ill-posed inverse problems [1]. The process involves:
- Forward Problem: Predicting surface voltage measurements based on a known internal conductivity distribution and applied currents. This is a well-posed problem with a stable, unique solution.
- Inverse Problem: Estimating the internal conductivity distribution from a set of boundary voltage measurements. This is ill-posed because [1]:
- Small errors or noise in voltage measurements can lead to large instabilities in the reconstructed image.
- The number of independent measurements is finite, while the conductivity distribution to be estimated is a continuous function within the object, making the solution non-unique.
Table 1: Comparison of EIT with Other Imaging Modalities [1]
| Parameter | EIT | CT | MRI | Ultrasound |
|---|---|---|---|---|
| Mechanism | Electrical Impedance | X-rays | Radio Waves | High-Frequency Sound |
| Cost | Low | Moderate | High | Low |
| Radiation Type | Non-ionizing | Ionizing | Non-ionizing | Non-ionizing |
| Portability | Portable | Non-portable | Non-portable | Portable |
| Spatial Resolution | Low | 50-200 μm | 25-100 μm | 50-500 μm |
| Temporal Resolution | 20-100 ms (can be as fast as 0.1 ms) | 83-135 ms | 20-50 ms | 1-20 ms |
The Complete Electrode Model (CEM)
Model Definition and Significance
The Complete Electrode Model (CEM) is a mathematical model that provides a more accurate representation of the physical reality at the electrode-skin interface compared to simpler models like the Gap Model or Shunt Model. It is considered the gold standard for forward modeling in EIT because it accounts for several critical, real-world phenomena that other models neglect. The CEM is essential for achieving quantitatively accurate image reconstructions, particularly in clinical settings.
Key Physical Phenomena Accounted for by the CEM
The CEM explicitly incorporates three major factors:
- Discrete Electrode Size and Shape: Real electrodes have finite size and specific geometry, which directly influences the current injection pattern and the measured voltage profile. The CEM models this, unlike simpler models that assume point electrodes.
- Contact Impedance: The interface between the electrode and the skin is not perfect. It is characterized by a thin layer of high impedance, known as the contact impedance or electrode-skin impedance. This layer arises from electrochemical effects and the skin's stratum corneum. The CEM includes this as a key parameter (
z_c), which can vary from electrode to electrode due to differences in skin preparation, pressure, and gel quality. - Shunting Effect: The highly conductive metal electrode causes a "shunting" effect, meaning the electric potential is constant across the entire surface of a single electrode. The CEM enforces this as a boundary condition.
Mathematical Formulation
The CEM consists of the following set of equations that govern the electric potential, u, within the domain Ω:
Governing Equation (Conservation of Charge):
∇ ⋅ (σ ∇u) = 0inΩThis states that in the absence of internal current sources, the divergence of the current density is zero.Boundary Conditions on the Electrodes (
e_l):- Current Injection:
∫_(e_l) σ (∂u / ∂n) dS = I_lThe integral of the current density over the electrode surface equals the total applied current for that electrode. - Shunting Effect and Contact Impedance:
u + z_l σ (∂u / ∂n) = U_lone_lThis equation couples the internal potential at the boundary to the measured voltageU_lon thel-th electrode, via the contact impedancez_l.
- Current Injection:
Boundary Conditions on the Skin (non-electrode areas):
σ (∂u / ∂n) = 0on∂Ω \ ∪ e_lThis states that no current flows into or out of the domain through the skin areas not covered by electrodes.
Experimental Protocols and Workflows
Standard EIT Data Acquisition Protocol
This protocol outlines the methodology for acquiring EIT data from a human subject, such as for thoracic or cerebral monitoring.
I. Materials and Setup
- EIT system with a capable signal generator and data acquisition unit.
- Set of 16 or 32 electrodes (typically Ag/AgCl).
- Electrode gel.
- Measuring tape and skin marker.
- Computer with EIT control and reconstruction software (e.g., EIDORS).
II. Pre-Acquisition Procedure
- Subject Preparation: Clean the skin area where electrodes will be placed (e.g., thoracic region at the 4th-5th intercostal space for lung imaging, or around the head for cerebral application) with alcohol swabs to reduce contact impedance [1] [2].
- Electrode Placement: Pre-gel the electrodes. Place them equidistantly around the cross-section of the target organ. For cerebral EIT, 16 electrodes are commonly arranged in a single plane around the head [2]. Secure the electrode strap to ensure consistent contact pressure.
- System Calibration: Power on the EIT system and initialize the software. Perform a system self-test and calibration according to the manufacturer's instructions to minimize instrumental errors.
III. Data Acquisition
- Reference Measurement: Acquire a reference data set. In time-difference EIT, this is a baseline measurement before a physiological change (e.g., start of ventilation). In multi-frequency absolute EIT, this step is part of the single measurement frame [1] [2].
- Application of Current: The system applies a small, safe alternating current (typically ≤5 mA) through a pair of drive electrodes [1].
- Voltage Measurement: Simultaneously, the system measures the resulting electrical potentials at all other passive electrode pairs. This process is repeated for multiple independent drive electrode pairs following a specific pattern (e.g., adjacent or opposite). A complete data set with 16 electrodes typically yields 208 voltage measurements [1].
- Frame Generation: Steps 2 and 3 are repeated rapidly. Modern EIT systems can achieve a frame rate of 10-50 frames per second, providing high temporal resolution for dynamic monitoring [1].
- Multi-Frequency Acquisition (for MFEIT/fdEIT): For multi-frequency EIT, repeat steps 2-4 across a range of frequencies (e.g., 21 kHz to 100 kHz) to capture the impedance spectrum of tissues [2].
IV. Post-Acquisition
- Store the raw voltage data securely.
- Remove electrodes and clean the subject's skin.
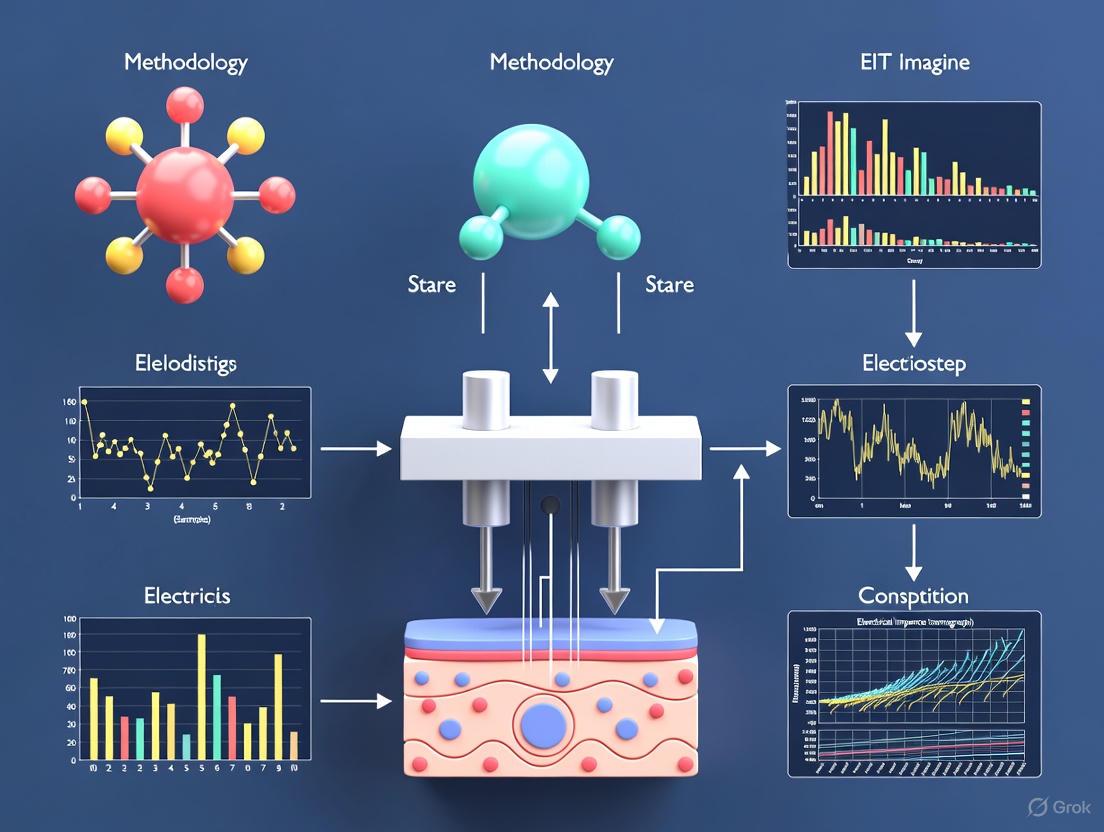
Diagram 1: EIT Data Acquisition and Image Reconstruction Workflow.
Protocol for Multifrequency EIT (MFEIT) in Cerebral Application
This specific protocol is adapted for the rapid detection of intracranial abnormalities, such as stroke or hemorrhage [2].
I. Subject Groups
- Healthy volunteers (control group).
- Patients with confirmed brain diseases (e.g., intracranial hemorrhage via CT/MRI).
II. MFEIT Data Acquisition
- Acquire cerebral MFEIT data at multiple frequencies (e.g., 9 frequencies in the 21 kHz - 100 kHz range) using an MFEIT system [2].
- Ensure consistent electrode placement for all subjects.
III. Image Reconstruction and Feature Extraction
- Reconstruct MFEIT image sequences using a frequency-difference (fdEIT) algorithm.
- For each image, define a Region of Interest (ROI). Extract the following quantitative indices [2]:
AR_ROI: The area ratio of the ROI.MVRRC_ROI: The mean value of the reconstructed resistivity change within the ROI.
- Calculate asymmetry indices to compare left and right hemispheres:
GAI(Geometric Asymmetry Index): Based onAR_ROI.IAI(Intensity Asymmetry Index): Based onMVRRC_ROI.
IV. Statistical Analysis
- Perform statistical analysis (e.g., t-test) to compare the
GAIandIAIbetween the healthy volunteer group and the patient group. - A significantly higher asymmetry index in patients indicates a potential intracranial abnormality [2].
Data Presentation and Analysis
Table 2: Comparison of EIT Reconstruction Algorithms [1]
| Method | Description | Advantages | Limitations |
|---|---|---|---|
| Back-projection | Analytical, fast, low computational cost. | Simple, capable of real-time imaging. | Poor spatial resolution, prone to artifacts. |
| D-bar Method | Non-iterative direct method, improved stability. | Better robustness against noise. | Limited to certain domain types (e.g., 2D). |
| Regularized Newton-Raphson | Iterative, handles nonlinearity, requires regularization. | High accuracy, flexible. | Computationally intensive. |
| Machine Learning-Based | Data-driven, captures complex patterns (e.g., CNN). | Adaptive, potentially higher resolution. | Requires large training datasets; "black box" interpretability. |
Table 3: Standardized EIT Ventilation Indices for Pulmonary Monitoring [1]
| Term | Full Name | Explanation and Clinical Significance |
|---|---|---|
| GI | Global Inhomogeneity | Measures uniformity of lung ventilation. A higher value indicates uneven distribution. |
| CoV | Center of Ventilation | Identifies the central position of airflow, helping assess ventilation distribution. |
| RVD | Regional Ventilation Delay | Indicates delays in ventilation across regions, suggesting airway obstruction. |
| EELI | End-Expiratory Lung Impedance | Reflects alveolar inflation and residual lung volume at the end of expiration. |
| TIV | Tidal Impedance Variation | Quantifies ventilation changes during each breathing cycle. |
The Scientist's Toolkit: Research Reagents and Materials
Table 4: Essential Materials for EIT Research
| Item | Function and Description |
|---|---|
| Ag/AgCl Electrodes | Silver/Silver-Chloride electrodes are the standard for bioimpedance measurement due to their stable half-cell potential and low noise characteristics. |
| Electrode Gel (Conductive) | Hydrogel containing electrolytes (e.g., NaCl) to ensure good electrical contact between the electrode and the skin, reducing contact impedance. |
| EIT System with Active Electrodes | Modern systems integrate preamplifiers at the electrode-skin interface (active electrodes) to minimize cable-induced artifacts and improve signal fidelity [1]. |
| Multi-Frequency EIT System | A system capable of applying AC currents across a range of frequencies (e.g., 10 kHz - 1 MHz) to perform MFEIT/fdEIT and exploit tissue impedance spectra [2]. |
| EIDORS Software | An open-source software suite for EIT (Electrical Impedance Tomography and Diffuse Optical Tomography Reconstruction). It provides a rich environment for simulation, image reconstruction, and algorithm development. |
| Tank Phantoms | Physical models (often with saline) containing insulating or conducting inclusions, used to validate EIT systems and reconstruction algorithms before clinical use [2]. |
Diagram 2: Logical Relationships of the Complete Electrode Model (CEM).
Understanding the Severely Ill-Posed Nature of the EIT Inverse Problem
Electrical Impedance Tomography (EIT) is a non-invasive imaging technique that reconstructs the internal electrical conductivity (and sometimes permittivity) distribution of an object by making electrical measurements on its surface [3] [4]. Its non-invasive nature, lack of ionizing radiation, and capability for real-time monitoring make it particularly attractive for medical applications such as lung and brain imaging, as well as for industrial process monitoring [3] [5].
Despite these advantages, EIT faces a fundamental mathematical challenge: the inverse problem of EIT is severely ill-posed in the sense of Hadamard [6] [7]. This means it lacks at least one of the three required properties for a well-posed problem: existence of a solution, uniqueness of the solution, and stability of the solution dependent on continuous data [7]. The EIT inverse problem is especially plagued by non-uniqueness and extreme sensitivity to noise and modeling errors, which leads to instability—small errors in measured data can cause large errors in the reconstructed image [6] [3]. This paper explores the nature of this ill-posedness, reviews contemporary solutions, and provides detailed protocols for addressing this central challenge in EIT research.
The Mathematical Foundation of EIT and Its Ill-Posedness
The Forward and Inverse Problem of EIT
The EIT forward problem is governed by the conductivity equation. Consider a bounded body domain ( \Omega ) with a conductivity distribution ( \sigma(x) > 0 ). The electrical potential ( u ) in the absence of internal current sources satisfies the elliptic partial differential equation:
[ \nabla \cdot (\sigma \nabla u) = 0 \quad \text{in} \ \Omega ]
Subject to appropriate boundary conditions, such as the Neumann condition ( \sigma \frac{\partial u}{\partial n} = j ) on ( \partial \Omega ), where ( j ) is the applied current density [6] [4]. The forward problem involves computing boundary voltages for a known conductivity and applied currents. The inverse problem—the central challenge of EIT—is to reconstruct ( \sigma ) from boundary measurements of current and voltage [7].
In practical applications, the relationship between measurements and the internal conductivity distribution is described by:
[ V = F(\sigma) + e ]
where ( V ) is the measured voltage, ( F(\cdot) ) is the nonlinear forward map, and ( e ) represents measurement noise [4].
Factors Contributing to Severe Ill-Posedness
The severe ill-posedness of the EIT inverse problem stems from several mathematical and physical realities [6]:
- The Smoothing Nature of the Forward Operator: The forward map ( F ) is a smoothing operator, meaning that high-frequency components of the internal conductivity are severely attenuated in the boundary measurements. Consequently, inverting this process amplifies high-frequency noise.
- Incomplete Boundary Data: In practical settings, only a finite number of measurements (typically from 8 to 128 electrodes) are available. This limited data fails to uniquely determine a continuous conductivity distribution.
- Nonlinearity: The mapping from conductivity to boundary measurements is inherently nonlinear, complicating the inversion process compared to linear problems.
Table 1: Fundamental Challenges of the EIT Inverse Problem
| Challenge | Mathematical Description | Practical Consequence |
|---|---|---|
| Non-Uniqueness | Different internal conductivity distributions can produce identical boundary measurements [7]. | Inability to distinguish between different tissue types or anomalies without prior information. |
| Instability | The inverse operator ( F^{-1} ) is discontinuous (unbounded); small measurement errors cause large reconstruction errors [6]. | High sensitivity to noise, requiring robust regularization methods for stable images. |
| Incomplete Data | Finite number of electrode measurements provide limited information about an infinite-dimensional parameter space [3]. | Low spatial resolution compared to modalities like CT or MRI. |
| Nonlinearity | The parameter-to-data map ( \mathcal{G}(u) ) is nonlinear [7]. | Requires iterative solutions or linearization approximations, increasing computational cost. |
Contemporary Approaches to Mitigating Ill-Posedness
Traditional Regularization and Algorithmic Families
Traditional approaches to managing EIT ill-posedness incorporate a priori information about the expected solution through regularization. These methods can be broadly categorized as follows [6] [4]:
- Variational Regularization Methods: These methods formulate the inverse problem as an optimization problem, minimizing a objective function that includes a data fidelity term and a regularization term. A classical example is the Tikhonov regularization, which incorporates a penalty on the ( L^2 ) norm (or other norms) of the solution or its derivatives.
- Iterative Reconstruction Algorithms: Examples include the Gauss-Newton method, which iteratively linearizes the problem and solves a regularized linear system at each step. These methods can achieve high accuracy but are computationally intensive and require careful choice of regularization parameters [6].
- Non-Iterative Direct Methods: Methods like the D-bar method and Calderón's method are based on theoretical breakthroughs involving Complex Geometrical Optics (CGO) solutions [6]. They are computationally efficient and avoid iterative forward problem solutions, but often produce images with lower resolution and are generally less accurate than iterative approaches [6].
The Rise of Learning-Enhanced and Hybrid Methods
Recently, deep learning and operator learning have emerged as powerful paradigms for solving inverse problems, offering alternatives to classical regularization [7] [4].
- End-to-End Inverse Operator Learning: This approach aims to directly learn the mapping from measured data ( y ) to the unknown parameters ( u ) using deep neural networks, effectively approximating the inverse operator [7]. These methods can leverage vast amounts of simulated or experimental data to implicitly learn prior information and regularization strategies.
- Hybrid "Learning-Enhanced" Methods: These approaches integrate deep learning with traditional algorithms to leverage the strengths of both. A prominent example is the Learning-Enhanced Variational Regularization via Calderón's method (LEVR-C) [6]. This method uses a deep neural network to extract a priori information about the shape and location (support) of the unknown conductivity contrast from an initial reconstruction provided by the computationally efficient Calderón's method. This learned information is then incorporated as a regularization term within a variational framework, which is subsequently solved by a Gauss-Newton method. This combines the speed of direct methods with the accuracy of iterative methods [6].
- Physics-Informed Neural Networks (PINNs) and Advanced Variants: PINNs embed the constraints of the governing differential equations into the loss function of a neural network [8]. For problems with extreme discontinuities, advanced frameworks like Information-Distilled PINNs (DR-PINNs) have been proposed. DR-PINNs combine reduced-order modeling, multi-level domain decomposition, and an ill-conditioning-suppression mechanism to handle singularities introduced by discontinuous loads or material properties [8].
Table 2: Comparison of EIT Reconstruction Algorithm Families
| Algorithm Family | Examples | Strengths | Weaknesses |
|---|---|---|---|
| Variational/Iterative | Tikhonov, Total Variation, Gauss-Newton [6] | High accuracy with good regularizers; strong theoretical foundations. | Computationally expensive; sensitive to regularization parameter choice. |
| Direct/Non-Iterative | Calderón's method, D-bar method [6] | Computationally efficient; non-iterative, avoiding forward problem solving. | Lower resolution and accuracy; often limited to linearized approximations. |
| Deep Learning (End-to-End) | Convolutional Neural Networks (CNNs), Neural Operators [7] [4] | Fast inference; can learn powerful priors from data; grid-free. | "Black-box" nature; large, high-quality datasets required; generalization concerns. |
| Hybrid Learning | LEVR-C [6], Post-processing networks [4] | Combines efficiency and accuracy; incorporates physical models. | Increased complexity from multiple components. |
| Physics-Informed Learning | PINNs, DR-PINNs [8] | Respects underlying physics; does not require paired training data. | Can struggle with sharp discontinuities (standard PINNs); training can be challenging. |
Experimental Protocols for Investigating EIT Ill-Posedness
Protocol 1: Implementing a Learning-Enhanced Variational Framework (LEVR-C)
This protocol outlines the methodology for combining Calderón's method with deep learning and variational regularization, as detailed in [6].
1. Objective: To reconstruct a high-contrast conductivity distribution ( \sigma(x) = 1 + m(x) ) by incorporating learned support information as a priori regularization.
2. Research Reagent Solutions:
Table 3: Key Reagents and Computational Tools for LEVR-C
| Item | Function/Description |
|---|---|
| EIT Measurement System | (e.g., ACT 5 system). Provides experimental boundary voltage data ( V ) from applied currents [9]. |
| Finite Element Software | (e.g., COMSOL, FEniCS). Used to solve the forward problem and generate training data. |
| Deep Learning Framework | (e.g., PyTorch, TensorFlow). For building and training the support-prediction network ( M_\Theta ). |
| Computational Atlas | An anatomical atlas of conductivity distributions, used for training or as a prior [9]. |
3. Methodology:
Step 1: Data Generation and Network Training for Support Learning
- Generate a large dataset of paired conductivity distributions ( {\sigmai} ) and their corresponding initial reconstructions ( {Ci} ) using Calderón's method.
- Train a deep neural network ( M_\Theta ) to map the initial Calderón reconstruction ( C ) to an approximate support mask ( D ) of the true contrast ( m ). The network learns to identify the likely shape and location of conductivity anomalies.
Step 2: Formulate the Learning-Enhanced Variational Problem
- Define the cost functional:
[
\min{m \in L^2(\Omega)} \|F(1+m) - V\|^2{\mathcal{Y}} + \alpha \|m\|^2{L^2(\Omega)} + \beta \|m - D\|^2{L^2(\Omega)}
]
where:
- ( F(1+m) - V ) is the data fidelity term.
- ( \|m\|^2 ) is the standard Tikhonov regularization for stability.
- ( \|m - D\|^2 ) is the learning-enhanced term, penalizing deviations from the learned support ( D ).
Step 3: Numerical Solution via Gauss-Newton Method
- Solve the above minimization problem using an iterative Gauss-Newton method. The learned support term ( D ) acts as a spatially varying prior, effectively guiding the solution towards physically plausible configurations.
The following workflow diagram illustrates the integrated structure of the LEVR-C protocol:
Protocol 2: Anatomical Atlas-Driven Real-Time Reconstruction
This protocol describes the use of an anatomical atlas to provide strong prior information for reconstructing ventilation and pulsatile perfusion in preterm infants [9].
1. Objective: To achieve real-time EIT imaging with improved spatial resolution by incorporating an anatomical atlas into the reconstruction process.
2. Methodology:
Step 1: Atlas Construction
- Collect a database of anatomical images (e.g., CT scans) from a representative population (e.g., 89 infant scans).
- Segment the images into key tissues (soft tissue, lung, bone, etc.) and assign representative conductivity ( \sigma ) and susceptivity ( \omega\epsilon ) values at the operating frequency (e.g., 93 kHz).
- Compute the mean conductivity distribution ( \sigma_{\text{atlas}} ) across the registered datasets to create the prior atlas.
Step 2: The MEAN (MEan Atlas Noser-based) Algorithm
- Use the mean atlas conductivity ( \sigma_{\text{atlas}} ) as a non-constant initial estimate, rather than a homogeneous distribution.
- Compute the Jacobian (sensitivity) matrix around this prior estimate.
- Perform a single Newton-type step (e.g., similar to NOSER) to find the perturbation from the prior that best fits the measured data. This single-step approach enables real-time performance.
Step 3: Post-processing with Schur Complement
- To further enhance resolution, apply the Schur complement method as a post-processing step. This technique helps to sharpen organ boundaries and improve contrast in the reconstructed image.
The integration of a fixed atlas provides a powerful spatial prior, mitigating the non-uniqueness problem by constraining the solution to anatomically plausible configurations.
Visualization of the Core EIT Inverse Problem Challenge
The following diagram maps the fundamental information flow in the EIT inverse problem, highlighting the sources of ill-posedness and the points where regularization and prior information must be applied to achieve a stable, unique solution.
The severely ill-posed nature of the EIT inverse problem remains a central challenge that dictates the design and performance of all EIT imaging systems. While traditional regularization methods provide a mathematical framework for addressing instability and non-uniqueness, the emergence of deep learning and hybrid approaches marks a significant advancement. Techniques such as the LEVR-C method, which distill prior information from data, and anatomical atlas integration, which provides strong spatial constraints, demonstrate the power of combining computational intelligence with physical models. Furthermore, specialized frameworks like DR-PINNs show great promise for handling the extreme discontinuities that exacerbate ill-posedness. Future research will continue to blend these paradigms, moving toward more robust, high-resolution, and clinically reliable EIT imaging by directly confronting its foundational mathematical instability.
Application Notes
Electrical Impedance Tomography (EIT) is a non-invasive, radiation-free imaging modality that reconstructs internal conductivity distributions by measuring boundary voltages. Its value lies in providing real-time, bedside functional imaging, particularly for dynamic physiological processes. Two domains where EIT demonstrates significant practical impact are clinical management of acute respiratory failure and experimental quantification of pulmonary edema in industrial research.
Medical Diagnostics: Multimodal Assessment of Post-Lung Transplantation ARDS
A 2025 clinical study demonstrates EIT's critical role in a multimodal framework for assessing ventilation/perfusion (V/Q) mismatch in patients with Acute Respiratory Distress Syndrome (ARDS) following lung transplantation [10]. The research highlights that EIT-derived parameters are more sensitive than quantitative CT for stratifying ARDS severity.
Key Quantitative Findings from Clinical EIT Application [10]
| Parameter | Description | Clinical Correlation |
|---|---|---|
| Global Inhomogeneity Index (GI) | Index of ventilation homogeneity; lower values indicate more homogeneous ventilation. | Higher in severe ARDS, indicating worsened ventilation distribution. |
| Center of Ventilation (COV) | Gravity-dependent distribution of ventilation. | Shifts with patient positioning and pathology. |
| Regional Ventilation Delay Index (RVDI) | Quantifies tidal ventilation delays, indicating obstructive pathology. | Significantly higher in low P/F group (severe ARDS). |
| EIT-Dead Space | EIT-derived fraction of unperfused ventilation. | Significantly higher in low P/F group; showed substantial agreement with ventilator-measured dead space. |
| EIT-V/Q Match | EIT-derived measure of regional ventilation and perfusion matching. | Significantly lower in low P/F group (P/F < 200 mmHg). |
| Ventilatory Ratio (VR) | Bedside estimate of physiological dead space. | Significantly higher in low P/F group; correlated positively with EIT-Dead Space. |
The study concluded that in lung transplant recipients with ARDS, the group with severe hypoxemia (P/F < 200 mmHg) showed significantly elevated VR, RVDI, and EIT-Dead Space, alongside reduced EIT-V/Q matching. Notably, quantitative CT-derived lesion volume parameters showed no significant difference between severity groups, underscoring EIT's superior sensitivity for functional assessment compared to static anatomical imaging [10].
Industrial Monitoring: Non-Invasive Quantification of Pulmonary Edema
In an industrial research context, EIT provides a non-invasive method for quantifying extravascular lung water (EVLW), a key metric in pharmaceutical development and toxicology studies for assessing drug-induced pulmonary toxicity or therapeutic efficacy. A seminal study developed a novel EIT-based metric, the lung water ratioEIT, which leverages gravity-dependent impedance changes during lateral body rotation to distinguish pulmonary edema from other thoracic fluids [11].
Key Quantitative Findings from Industrial EIT Application [11]
| Parameter/Metric | Description | Experimental Outcome |
|---|---|---|
lung water ratioEIT |
Novel EIT parameter calculating ventilation redistribution during lateral body rotation. | Significantly correlated with postmortem gravimetric analysis (r=0.80, p<0.05), the experimental gold standard. |
| Experimental Model | Porcine model with two injury types: saline lavage (direct) and oleic acid (vascular). | Significantly changes after lung injury induction in both models. |
| Comparison Standard | Transcardiopulmonary Thermodilution (TCPTD). | Tracked changes in EVLW measured by TCPTD, a clinical monitoring tool. |
This EIT-based approach fulfills a critical need in industrial research for a non-invasive, bedside-capable, and reproducible tool to quantify pulmonary edema, eliminating the need for terminal procedures or invasive catheterization required by gold-standard methods [11].
Experimental Protocols
Protocol 1: EIT for V/Q Mismatch in ARDS
This protocol outlines the methodology for using EIT in a multimodal assessment of ARDS, as described in the 2025 clinical study [10].
Workflow
The experimental workflow for assessing V/Q mismatch in ARDS patients using EIT and CT is visually summarized below.
Methodology
- Subject Enrollment: Recruit patients meeting the Berlin definition for ARDS, such as a cohort of post-lung transplant patients. Key inclusion criteria: P/F ratio ≤ 300 mmHg, mechanical ventilation with no spontaneous breathing effort, and both EIT monitoring and high-resolution CT performed within 24 hours of qualifying P/F measurement [10].
- EIT Data Acquisition:
- Place a 32-electrode EIT belt around the patient's thorax.
- Acquire EIT data for a minimum of 120 seconds under stable ventilator settings.
- For V/Q assessment, perform contrast-enhanced EIT using a bolus of hypertonic saline to calculate EIT-Dead Space and EIT-Shunt fractions [10].
- Multimodal Data Collection:
- CT Imaging: Perform high-resolution chest CT. Subsequently, process images using a computer-aided diagnostic model for semi-automated lung segmentation, lesion identification, and quantification of volumes (total lung, lesion, percentage lesion) [10].
- Gas Exchange & Respiratory Mechanics: Record arterial blood gases for P/F ratio calculation. Collect ventilator data to calculate the Ventilatory Ratio (VR) [10].
- Data Processing & Analysis:
- EIT Parameters: From the EIT data, calculate key parameters:
- Global Inhomogeneity Index (GI)
- Center of Ventilation (COV)
- Regional Ventilation Delay Index (RVDI)
- EIT-Dead Space and EIT-V/Q Match [10].
- Stratification: Divide subjects into groups based on P/F ratio (e.g., low P/F < 200 mmHg vs. high P/F 200-300 mmHg) [10].
- Statistical Analysis: Compare EIT parameters, CT metrics, and clinical parameters between the stratified groups to assess EIT's sensitivity and correlation with disease severity.
- EIT Parameters: From the EIT data, calculate key parameters:
Protocol 2: EIT for Quantifying Pulmonary Edema in Industrial Research
This protocol is adapted from the 2016 experimental study that validated the lung water ratioEIT against the gravimetric gold standard [11].
Workflow
The following diagram illustrates the core operational principle of the lung water ratioEIT measurement based on lateral body rotation.
Methodology
- Experimental Setup:
- Subject Preparation: Anesthetize and instrument research subjects (e.g., porcine model). Place an EIT belt with 32 electrodes around the thorax. Secure the subject in a vacuum mattress to prevent electrode movement [11].
- Lung Injury Models: Randomize subjects into groups, including a sham group, a direct lung injury group (e.g., via saline lavage), and a vascular injury group (e.g., via oleic acid injection) [11].
- EIT Data Acquisition with Positional Changes:
- With the subject in a supine position, record baseline EIT data for at least 120 seconds.
- Rotate the subject to a 45° left lateral tilt. Allow 20 minutes for equilibration of fluid distribution, then record EIT data.
- Rotate the subject to a 45° right lateral tilt. After another 20-minute equilibration, record EIT data [11].
- Induce lung injury according to the experimental group assignment.
- Three hours post-injury, repeat the EIT data acquisition in all three body positions [11].
- Data Processing and
lung water ratioEITCalculation:- Process EIT datasets offline. For each body position, calculate the tidal variation (TV) of impedance for the left and right lungs.
- The
lung water ratioEITis calculated based on the differences in TV between the left and right lungs across the different tilts, which reflects the gravity-dependent redistribution of pulmonary edema [11].
- Validation against Gold Standard:
- Upon completion of the protocol, perform postmortem gravimetric analysis of the lungs to determine the actual EVLW content, which serves as the gold standard [11].
- Statistically correlate the
lung water ratioEITvalues with the gravimetrically obtained EVLW to validate the EIT method.
The Scientist's Toolkit
Table: Essential Research Reagents and Materials for EIT Experiments
| Item | Function/Application |
|---|---|
| 32-Electrode EIT Belt & Data Acquisition System | Core hardware for applying safe alternating currents and measuring boundary voltage changes on the thorax. Essential for all EIT experiments [10] [11]. |
| Hypertonic Saline Bolus | Used as an intravenous contrast agent during EIT monitoring to enable the calculation of perfusion-related parameters and V/Q matching maps [10]. |
| Mechanical Ventilator | Provides standardized, controlled ventilation during EIT data acquisition, eliminating confounders from variable spontaneous breathing efforts [10] [11]. |
| Arterial Blood Gas (ABG) Kits | For measuring PaO2 and FiO2 to calculate the P/F ratio, a key parameter for patient stratification and correlation with EIT findings [10]. |
| Quantitative CT Analysis Software | Enables semi-automated lung segmentation and quantification of high-density lesion volumes, providing anatomical context to complement EIT's functional data [10]. |
| Lung Injury Agents (e.g., Oleic Acid) | Used in industrial research settings to induce specific, reproducible models of vascular lung injury for validating EIT biomarkers like lung water ratioEIT [11]. |
The Complete Electrode Model as a Standard for Real-World Applications
Electrical Impedance Tomography (EIT) is a non-invasive imaging modality that reconstructs the internal conductivity distribution of an object based on electrical measurements taken from surface electrodes [3]. Its appeal in medical and industrial settings stems from its non-invasive nature, real-time imaging capability, portability, and low cost compared to modalities like CT and MRI [3] [12]. The core challenge in EIT, however, lies in accurately modeling the galvanic interaction between the electrodes and the material under investigation, as this interaction significantly influences the generated electric field and, consequently, the reliability of the impedance analysis [13].
The Complete Electrode Model (CEM) has emerged as the state-of-the-art for addressing this challenge. It accounts for the crucial effects of electrode properties and their contact with the material, which are often overlooked in simpler models [13]. This document details the role of CEM as a standard in real-world EIT applications, providing a structured overview of its principles, a comparison with other models, quantitative tissue data, experimental protocols, and an exploration of advanced methodologies.
The Complete Electrode Model (CEM): Foundation and Formulation
The CEM's fundamental innovation is its realistic representation of the electrode-material interface. It explicitly models the electrochemical effects that occur at the boundary where the electrode meets the material (e.g., skin or tissue). The key physical phenomenon it captures is the shunting effect, where current preferentially travels through the highly conductive electrode itself, leading to a nearly constant electrical potential on the electrode surface [13].
The model incorporates two critical parameters:
- Contact Impedance ((z_c)): A simplified representation of the complex electrochemical interface, often modeled as a series impedance with the material [13].
- Electrode Potentials ((U_l)): The voltages measured on the electrodes, which are modeled as the sum of the voltage drops across both the material and the electrode impedance [13].
The mathematical formulation of the CEM consists of the following key equations that govern the electric potential, (u), within the domain (\Omega):
- Governing Equation:
∇ ⋅ (σ ∇u) = 0inΩ. This represents the conservation of charge in the interior of the domain [13]. - Boundary Conditions on Electrodes:
u + z_c σ (∂u/∂n) = U_lon each electrodee_l. This mixed condition couples the potential in the domain to the measured electrode voltage [13]. - Current Injection Condition:
∫_{e_l} σ (∂u/∂n) dS = I_lon each electrodee_l. This specifies the known injected current [13]. - Insulating Boundary Condition:
σ (∂u/∂n) = 0on the boundary not covered by electrodes. This ensures no current flows out except through the electrodes [13].
This comprehensive set of equations allows the CEM to minimize artifacts caused by inaccurate boundary modeling, providing a robust foundation for image reconstruction algorithms [13].
Comparative Analysis of Electrode Models
The following table contrasts the CEM with other common electrode models, highlighting its advantages for real-world applications.
Table 1: Comparison of Electrode Models in EIT
| Model Name | Key Assumptions | Limitations | Advantages of CEM |
|---|---|---|---|
| Gap Model | Electrodes are point-like; contact impedance is infinite. | Highly inaccurate; fails to predict real-world measurements. | Accounts for finite electrode size and finite contact impedance. |
| Shunt Model | Electrodes are perfectly conducting; contact impedance is zero. | Neglects voltage drop at contact interface; less accurate. | Explicitly models the voltage drop across the contact layer. |
| Complete Electrode Model (CEM) | Finite electrode size; finite contact impedance ((z_c)). | Computationally more intensive. | Gold Standard: Most accurately represents physical electrode behavior; minimizes reconstruction artifacts [13]. |
EIT Applications and Tissue Properties
The effectiveness of EIT, and by extension the CEM, relies on the significant electrical property contrasts between different biological tissues and physiological states.
Table 2: Electrical Conductivity of Biological Tissues (at frequencies common in EIT) [3] [14]
| Tissue / Material | Conductivity (mS/m) | Clinical / Experimental Relevance |
|---|---|---|
| Cerebrospinal Fluid (CSF) | 1450 - 2000 | Reference conductive medium; high conductivity impacts brain EIT [3] [14]. |
| Blood | 500 - 750 | Perfusion monitoring; detection of hemorrhage or ischemia [3] [14]. |
| Muscle | 200 - 450 | Direction-dependent conductivity (anisotropy); affects thoracic imaging [3]. |
| Gray Matter | 75 - 150 | Neural activity monitoring; stroke detection [14]. |
| Liver / Organs | 300 - 560 | Abdominal and cancerous tissue imaging [12]. |
| Fat | 20 - 50 | Poor conductor; provides contrast in thoracic and abdominal imaging [3]. |
| Lung (Inspired) | ~200 | Highly variable with air content; primary target for ventilation monitoring [3]. |
| Lung (Expired) | ~600 | Conductivity increases as air volume decreases [3]. |
| Bone (Cortical) | 6 - 20 | Highly resistive; acts as an electrical barrier in head and thoracic EIT [3] [14]. |
Key Application Areas
- Pulmonary Monitoring: EIT is extensively used for real-time, bedside monitoring of lung ventilation. It can identify sub-phenotypes of Acute Respiratory Distress Syndrome (ARDS) by clustering regional ventilation and perfusion data, guiding personalized PEEP therapy [15]. It also correlates with quantitative CT in assessing asthma, providing dynamic functional data [16].
- Hemorrhagic and Ischemic Stroke Detection: The significant conductivity difference between bleeding (high conductivity due to blood) and ischemic regions (low conductivity due to cytotoxic edema) makes EIT a promising tool for non-invasive cerebral monitoring [14].
- Hemolysis Monitoring: An EIT sensor with 16 electrodes can dynamically monitor blood hemolysis by detecting conductivity changes associated with the release of hemoglobin, offering a potential method for real-time, in-line blood quality control [17].
- Tactile Sensing: Flexible EIT sensors with lattice-structured conductive channels are used in robotics and electronic skin. Pressure deforms the channels, altering local conductivity and allowing reconstruction of touch location and force [18].
Experimental Protocol: CEM-Based Hemolysis Monitoring
The following protocol, adapted from Peng et al. (2025), outlines a specific application of EIT for real-time monitoring of hemolysis (the breakdown of red blood cells) using a CEM-based system [17].
Application: Real-time, in-line monitoring of dynamic hemolysis in stored blood samples or extracorporeal circulation. Principle: The release of hemoglobin and other intracellular components during red blood cell breakdown alters the electrical conductivity of the blood sample. The EIT sensor tracks these spatio-temporal conductivity changes.
Research Reagent Solutions & Materials
Table 3: Essential Materials for EIT-based Hemolysis Monitoring
| Item Name | Specification / Function |
|---|---|
| EIT Sensor Array | 16-electrode circular PCB array (e.g., FR-4 substrate, copper electrodes). Configures the boundary for current injection and voltage measurement [17]. |
| Voltage-Controlled Current Source (VCCS) | Generates a high-frequency (e.g., 50-100 kHz), low-amplitude alternating current for safe and accurate tissue interrogation [12]. |
| Data Acquisition (DAQ) System | High-precision unit for synchronously measuring boundary voltages from all electrode pairs. A key source of measurement noise if of low quality [17]. |
| Blood Sample | Whole blood, typically anticoagulated (e.g., with EDTA or Heparin). The sample under test [17]. |
| Hemolysis Inducer | Physical (e.g., ultrasound), chemical (e.g., saponin reagent), or material-based (e.g., copper wire) agent to simulate hemolysis [17]. |
| Reference Measurement System | Spectrophotometer for validating free hemoglobin concentration via optical density (OD) measurement at 545 nm [17]. |
Detailed Step-by-Step Workflow
Step 1: System Setup and Calibration
- Assemble the EIT system: Connect the 16-electrode sensor array to the DAQ hardware and the VCCS.
- Place the blood sample in the sensor's measurement chamber.
- Perform a system calibration by measuring a set of reference voltages ((V_{ref})) across all electrode pairs with a stable, non-hemolyzed blood sample or a calibration solution with known conductivity.
Step 2: Data Acquisition and Hemolysis Induction
- Initiate Baseline Monitoring: Acquire boundary voltage data for 60 seconds to establish a stable baseline.
- Induce Hemolysis: Introduce the hemolysis-inducing agent (e.g., insert a copper wire into the blood sample).
- Continuous Monitoring: Acquire boundary voltage data continuously throughout the hemolysis process and subsequent diffusion. A single data frame should include all voltage measurements from all combinations of drive and measurement electrodes.
Step 3: Data Pre-processing and Image Reconstruction
- Calculate Voltage Change: Compute the differential voltage set,
ΔV = V_touch - V_ref, for each time point. - Solve Inverse Problem: Input
ΔVinto the EIT image reconstruction algorithm (e.g., based on the CEM and a regularized Gauss-Newton method) to compute the change in conductivity distribution (Δσ) over time. - Generate 2D Images: Reconstruct a time-series of 2D conductivity distribution images visualizing the initiation and diffusion of the hemolysis process.
Step 4: Data Validation and Analysis
- Correlate with Gold Standard: Periodically sample the blood and measure free hemoglobin concentration using a spectrophotometer to obtain Optical Density (OD) values.
- Establish Correlation: Plot the EIT parameter (e.g., the sum of all voltage changes, (U_s)) against the OD values to create a calibration curve for quantifying hemolysis levels from EIT data alone.
Diagram 1: Hemolysis monitoring experiment workflow.
Advanced Methodologies and Future Directions
While the CEM is the current standard, research continues to advance the field of EIT. Two prominent areas of development are detailed below.
Beyond CEM: The Continuous Electrode Model
A recent innovation proposes a Continuous Electrode Model, which represents a significant generalization of the CEM. This method uses the same differential equation to model the entire measurement assembly—the electrodes, the material, and their interaction—using continuous functions [13].
Key Advantage: It allows for the calculation of the analytical solution's values at any point in the assembly without the discretization errors common in numerical methods like the Finite Element Method (FEM). This provides a more accurate and potentially more robust basis for EIT measurement modeling, especially for complex electrode geometries or material properties [13].
Deep Learning in EIT Reconstruction
The EIT inverse problem is severely ill-posed and non-linear. Deep learning (DL) has emerged as a powerful tool to address this.
- Approaches: DL methods for EIT include fully-learned networks (directly mapping voltage to conductivity), post-processing networks (refining images from traditional algorithms), and learned iterative methods (unrolling classical iterations with learned parameters) [19].
- Performance vs. Generalization: A 2025 review demonstrates that while fully-learned methods can outperform model-based approaches on data similar to their training set, they often face challenges in generalizing to out-of-distribution or real-world data. Hybrid methods, which incorporate physical models, strike a favorable balance between accuracy and adaptability [19].
The integration of precise models like the CEM or the Continuous Electrode Model into these learning frameworks is crucial for enhancing their physical plausibility and reliability.
Diagram 2: EIT inverse problem solution methods.
Next-Generation EIT Methodologies: Algorithms and Translational Applications from Bedside to Benchtop
Electrical Impedance Tomography (EIT) is a powerful, non-invasive imaging modality with critical applications in medical diagnostics, industrial process monitoring, and environmental studies. The core inverse problem of EIT—inferring the internal conductivity distribution of an object from boundary voltage measurements—is severely ill-posed [19] [20] [21]. This ill-posedness means the reconstruction is highly sensitive to noise and small errors in measurement data, making traditional computational approaches challenging.
The emergence of deep learning (DL) has driven significant progress in EIT image reconstruction. Deep learning methods can learn complex prior distributions directly from large datasets, offering greater flexibility than traditional hand-crafted priors [21]. These learned approaches have demonstrated potential to enhance reconstruction quality, increase computational speed, and improve robustness to noise. Current DL-based reconstruction methods can be broadly categorized into three paradigms: fully-learned, post-processing, and learned iterative methods [19] [21]. This article explores these revolutionary approaches, providing structured comparisons, detailed experimental protocols, and essential resource information to equip researchers with practical tools for implementation.
Comparative Analysis of Deep Learning Methods in EIT
Table 1: Comparison of Deep Learning-Based EIT Reconstruction Methods
| Method Category | Key Principle | Advantages | Limitations | Representative Performance |
|---|---|---|---|---|
| Fully-Learned | Directly maps voltage measurements to conductivity images using a deep neural network [20]. | Fast reconstruction speed; eliminates iterative solving [20]. | Limited generalization to unseen data types; requires large, diverse datasets [19] [21]. | High accuracy on in-distribution data; outperforms model-based methods in simulated ellipse datasets [19]. |
| Post-Processing | Uses a DL network to enhance initial images from traditional algorithms (e.g., Calderón's method) [20] [6]. | Leverages strengths of classical methods; more stable than fully-learned approaches [6]. | Final image quality constrained by the initial reconstruction [6]. | Effectively improves resolution of initial guesses; successful support information extraction via Calderón's method [6] [22]. |
| Learned Iterative | Unfolds traditional iterative algorithms into network layers, learning parameters from data [21]. | Incorporates physical model; good balance of accuracy and adaptability [19]. | Complex training process; computationally intensive during training [21]. | Exhibits strong generalization on out-of-distribution and real-world data (e.g., KIT4 dataset) [19]. |
| Hybrid / LEVR-C | Combines learned support information from Calderón's method with variational regularization [6]. | Incorporates valuable prior knowledge; stable convergence [6]. | Performance depends on the accuracy of the learned support [6]. | Superior reconstruction performance and generalization ability in numerical experiments [6]. |
Table 2: Quantitative Performance Overview from Experimental Studies
| Study / Dataset | Evaluation Metric | Model-Based Methods | Fully-Learned Methods | Hybrid Methods |
|---|---|---|---|---|
| Simulated Ellipses (In-Distribution) [19] | Reconstruction Accuracy | Lower accuracy | Highest accuracy | High accuracy |
| Out-of-Distribution Data [19] | Generalization Ability | Moderate performance | Significant performance drop | Best balance |
| KIT4 (Real Measurements) [19] [23] | Adaptability to Real Data | Lower spatial resolution | Challenges with measurement noise | Good accuracy and adaptability |
| Kuopio Challenge 2023 [23] | Segmented Image Quality (Level 1) | - | - | Score: ~0.74-0.98 |
| Kuopio Challenge 2023 [23] | Segmented Image Quality (Level 7) | - | - | Score: ~0.16-0.80 |
Experimental Protocols for Key Methodologies
Protocol 1: Implementation of a Fully-Learned Reconstruction Network
This protocol outlines the procedure for training a fully-learned deep neural network to solve the EIT inverse problem, directly mapping boundary measurements to conductivity images.
Data Preparation and Simulation
- Forward Model: Utilize the Complete Electrode Model (CEM) to accurately simulate real-world measurement conditions, including electrode modeling and contact impedance [21].
- Dataset Generation:
- Define a range of plausible conductivity distributions (e.g., inclusion shapes, sizes, and contrasts). For example, the Kuopio Tomography Challenge 2023 used a circular water tank with conductive and resistive inclusions of various shapes [23].
- Use the CEM to simulate boundary voltage measurements for each conductivity distribution.
- Add realistic noise to the simulated voltage data to improve model robustness.
- Data Split: Randomly partition the dataset into training, validation, and testing subsets (e.g., 70%/15%/15%).
Network Architecture and Training
- Architecture Selection: Employ a Convolutional Neural Network (CNN) with an encoder-decoder structure, or a fully-connected network for smaller problems.
- Loss Function: Use the Mean Squared Error (MSE) or Structural Similarity Index (SSIM) between the network output and the ground truth conductivity.
- Training Process:
- Optimize using the Adam optimizer.
- Implement early stopping based on validation loss to prevent overfitting.
- Validate reconstruction performance on the simulated test set.
Generalization Testing
- Out-of-Distribution Test: Evaluate the trained model on a test set with conductivity distributions that differ from the training data (e.g., different inclusion shapes) [19].
- Real Data Application: Finally, test the model on experimental datasets, such as the publicly available KIT4 or Kuopio Challenge 2023 data, to assess real-world performance [19] [23].
Protocol 2: Learned-Enhanced Variational Regularization via Calderón's Method (LEVR-C)
This protocol details a hybrid approach that combines the efficiency of a direct analytical method with the precision of a learned iterative scheme [6].
Initial Reconstruction Using Calderón's Method
- Compute an initial, low-resolution reconstruction of the conductivity contrast from the boundary measurements using the computationally efficient Calderón's method [6].
Learning the Support Information
- Network Training: Train a deep neural network to extract the approximate shape and location (support) of conductivity inclusions from the initial Calderón reconstruction.
- Input/Output: The network takes the initial Calderón image as input and outputs an estimate of the support region of the inclusions.
Variational Regularization with Learned Prior
- Formulate Optimization Problem:
- Define a cost function that includes a data fidelity term and a regularization term.
- Incorporate the learned support information as an explicit constraint or prior within the variational model.
- Solve the Inverse Problem:
- Use an iterative optimization algorithm, such as the Gauss-Newton method, to solve the regularized inverse problem.
- The learned support constraint guides the algorithm to produce a more accurate and stable final reconstruction.
- Formulate Optimization Problem:
Table 3: Key Research Reagents and Computational Tools for EIT Research
| Category | Item / Resource | Specifications / Function | Example Use Case |
|---|---|---|---|
| Experimental Hardware | KIT4 EIT System [23] | A laboratory EIT system for acquiring real-world voltage data. | Data collection for algorithm validation. |
| Circular Water Tank with Electrodes [23] | A phantom setup with controlled inclusions (conductive/resistive plastics, metals). | Generating experimental training and test data. | |
| Ag/AgCl Electrodes [24] | Low-impedance electrodes for medical-grade EIT measurements. | Intracranial EIT monitoring in animal studies. | |
| Computational Models | Complete Electrode Model (CEM) [21] | A realistic mathematical model that accounts for electrode contact impedance. | Forward problem simulation for dataset generation. |
| Calderón's Method [6] [22] | A direct, non-iterative reconstruction method. | Providing initial guesses for hybrid/post-processing methods. | |
| Software & Data | Kuopio Tomography Challenge 2023 Dataset [23] | A publicly available dataset of real EIT measurements with ground truth. | Benchmarking and testing algorithm performance. |
| MATLAB / Python with EIT Toolboxes | Implementation platforms for EIT forward solvers and reconstruction algorithms. | Prototyping and deploying DL models. | |
| Deep Learning Frameworks | TensorFlow / PyTorch | Open-source libraries for building and training deep neural networks. | Implementing fully-learned, post-processing, and learned iterative networks. |
The integration of deep learning into EIT reconstruction represents a paradigm shift, moving from purely model-based approaches to data-driven methodologies. Fully-learned methods offer unparalleled speed for in-distribution data but face generalization challenges. Post-processing techniques provide a practical balance by enhancing existing algorithms. Learned iterative methods and other hybrid approaches like LEVR-C currently offer the most promising balance, embedding physical models within learned frameworks to achieve robust and accurate reconstructions, even on experimental data [19] [6].
Future research will likely focus on optimizing dataset construction to mitigate generalization issues, developing more efficient network architectures, and further refining the integration of physical models with deep learning. The ultimate goal is the creation of intelligent, integrated EIT diagnostic systems that leverage the full potential of these revolutionary reconstruction methods [20].
Clinical Significance of EIT in Critical Care
Electrical impedance tomography (EIT) has emerged as a transformative, non-invasive imaging modality for real-time monitoring of pulmonary function in both neonatal and adult critical care settings. This technology generates dynamic images of regional lung ventilation by measuring tissue bioimpedance, utilizing harmless alternating currents to reconstruct conductivity distributions that reflect tissue properties and air content [1]. The clinical significance of EIT stems from its unique combination of continuous bedside monitoring, absence of ionizing radiation, and high temporal resolution (20-100 milliseconds), enabling clinicians to visualize and quantify pulmonary dynamics not accessible through conventional imaging modalities [1] [25].
In neonatal critical care, EIT addresses a particularly urgent clinical need. The respiratory system of neonates exhibits unique physiological and anatomic attributes that increase vulnerability to respiratory distress and failure [5] [26]. Preterm infants face heightened risks from mechanical ventilation, including ventilator-induced lung injury (VILI) and bronchopulmonary dysplasia (BPD) [26]. EIT offers a potential solution through precision monitoring that may reduce complications like pneumothorax, intraventricular hemorrhage, and BPD by guiding individualized lung-protective ventilation strategies [5]. The technology's capability for real-time assessment of pulmonary function enables clinicians to make informed interventions based on continuous data rather than intermittent snapshots [26].
For adult ICU patients, EIT provides crucial insights into managing complex respiratory conditions, particularly in mechanically ventilated patients with acute respiratory distress syndrome (ARDS) [25]. Its applications extend to optimizing positive end-expiratory pressure (PEEP), assessing lung recruitment, detecting adverse events like pneumothoraces, and guiding weaning from mechanical ventilation [1] [25]. The recent publication of evidence-based recommendations with strong expert consensus (15 recommendations with >95% agreement) underscores EIT's evolving role in detecting dynamic pulmonary abnormalities that significantly influence clinical management and diagnosis [27].
Table 1: Comparative Analysis of EIT Against Traditional Pulmonary Imaging Modalities
| Parameters | EIT | CT | MRI | Ultrasound |
|---|---|---|---|---|
| Mechanism | Impedance | X-rays | Radio waves | High frequency sound |
| Cost | Low | Moderate | High | Low |
| Radiation Type | Non-ionizing | Ionizing | Non-ionizing | Non-ionizing |
| Portability | Portable | Non-portable | Non-portable | Portable |
| Spatial Resolution | Low | 50-200 μm | 25-100 μm | 50-500 μm |
| Temporal Resolution | 20-100 ms | 83-135 ms | 20-50 ms | 1-20 ms |
| Primary Limitations | Not mature yet, low spatial resolution | Ionizing radiation | Noisy, cost, low sensitivity | Operator dependency |
Technical Foundations and Physiological Principles
Fundamental Bioimpedance Principles
The physiological basis of EIT centers on the intrinsic electrical properties of biological tissues. Tissue impedance consists of both resistance and capacitance, with the aqueous components of tissue demonstrating similar resistance in both direct current (DC) and alternating current (AC) fields, while the phospholipid bilayer of cell membranes creates capacitance that blocks DC but stores and releases energy in AC fields [1]. This frequency-dependent behavior underpins EIT's ability to discriminate between tissues: at low frequencies, electrical current is confined to extracellular spaces, whereas at higher frequencies, it penetrates cell membranes [1]. The complex relationship between resistance, capacitance, and frequency produces unique impedance spectra for different tissues, typically visualized as Cole-Cole plots, which form the basis for imaging contrast in EIT [1].
In pulmonary applications, EIT capitalizes on the significant impedance differences between air and fluid-filled spaces. Lung tissue resistivity correlates strongly with air volume, changing substantially between expiration (approximately 7 ohm-meters) and inspiration (approximately 24 ohm-meters) [26]. This variation occurs because air, being a poor electrical conductor, increases overall impedance as alveolar spaces expand and tissue layers thin during inspiration [26]. Conversely, increased lung fluid content (as in pulmonary edema) decreases impedance, providing a quantifiable marker of pathological processes [26].
EIT System Architecture and Operation
Modern EIT systems typically employ 16 electrodes arranged in a circular strap around the thorax, with most systems utilizing four active electrodes per measurement cycle [1]. A small alternating current (≤5 mA) is applied between one electrode pair while voltages are recorded from the remaining electrodes, generating approximately 208 measurements within 80 milliseconds [1]. This rapid data acquisition enables EIT to achieve 10-50 frames per second, providing the high temporal resolution essential for capturing ventilation and perfusion dynamics [1].
EIT operates in two primary modes: absolute imaging (reconstructing conductivity distribution at a fixed time) and time-differential imaging (imaging changes relative to a baseline) [1]. Clinical applications predominantly utilize time-differential imaging as it reduces instrument and contact errors, enhancing stability and reliability [1]. Reconstruction algorithms address the mathematically challenging "inverse problem" of estimating internal conductivity from boundary measurements, employing methods ranging from back-projection and sensitivity matrices to iterative techniques like variational or subspace-based optimization [1]. Recently, machine learning approaches including convolutional neural networks (CNNs) and ensemble learning have shown promise in improving reconstruction accuracy and speed, though challenges remain in model interpretability and retraining requirements [1].
Table 2: EIT Reconstruction Algorithms: Comparative Analysis
| Method | Description | Advantages | Limitations | Example Applications |
|---|---|---|---|---|
| Back-projection | Analytical, fast, low computational cost | Simple, real-time capable | Poor spatial resolution, artifacts | GREIT algorithm |
| D-bar Method | Non-iterative direct method, improved stability | Better noise robustness | Limited to certain domains | 2D domain EIT |
| Regularized Newton-Raphson | Iterative, handles nonlinearity, requires regularization | High accuracy, flexible | Computationally intensive | Gauss-Newton with Tikhonov regularization |
| Machine Learning-Based | Data-driven, captures complex patterns | Adaptive, potentially higher resolution | Requires large training datasets | CNN-based impedance reconstruction |
Standardized Application Protocols
EIT Acquisition and Setup Protocol
Proper electrode placement is fundamental to obtaining reliable EIT data. For most pulmonary applications, the electrode belt should be positioned transversely between the 4th and 5th intercostal spaces, measured at the parasternal line [25]. Placement accuracy is critical - positioning too low introduces artifacts from diaphragmatic movement, while placement too high may underrepresent dorsal lung regions [25]. Belt rotation should be avoided as it distorts the reconstructed image, and a truly transverse orientation (not oblique) is essential for accurate dorsal ventilation assessment [25].
Belt size selection should follow manufacturer recommendations based on half-chest perimeter (measured from sternum to spine) to ensure optimal inter-electrode spacing and skin contact [25]. Electrode-skin contact can be enhanced using water, crystalloid fluids, ultrasound gel, or device-specific contact agents [25]. The system should include a signal quality check and calibration when possible, with recordings initiated after at least one minute of signal stability to ensure baseline reliability [25].
When clinical factors prevent ideal belt placement (e.g., chest tubes, wounds, or bandages), a higher placement is recommended over a lower one [25]. Most EIT systems can function properly with one or two non-functioning electrode pairs (for 16 and 32 electrode belts, respectively) [25]. For longitudinal measurements, marking the belt position with a skin marker enhances comparability between recording sessions [25].
Protocol for Controlled Mechanical Ventilation
EIT provides critical insights for managing mechanically ventilated patients, particularly in optimizing PEEP and preventing ventilator-induced lung injury (VILI). The following step-by-step protocol outlines the standardized approach:
Initial Setup: Position the EIT belt correctly and ensure stable signal acquisition. Record baseline ventilation for at least 5 minutes with current ventilator settings [25].
PEEP Titration Maneuver:
- Conduct a low-flow inflation maneuver or PEEP trial with incremental/decremental PEEP changes [25].
- Monitor end-expiratory lung impedance (EELI) changes to assess recruitment/derecruitment [1].
- Analyze global inhomogeneity (GI) index to identify PEEP levels that minimize ventilation heterogeneity [1].
- Calculate regional ventilation delay (RVD) to detect poorly ventilated areas [1].
Tidal Volume Distribution Assessment:
Recruitment Assessment:
Ongoing Monitoring:
Protocol for Spontaneous Breathing Trials
EIT enhances prediction of weaning outcomes during spontaneous breathing trials (SBT). The standardized protocol includes:
Pre-SBT Baseline: Record at least 10 minutes of stable EIT data during mechanical ventilation [1].
SBT Monitoring:
Failure Prediction Criteria:
Post-SBT Analysis: Compare pre- and post-SBT parameters to identify patients at risk of extubation failure [1].
Neonatal-Specific Application Protocol
Neonatal EIT application requires special considerations due to unique physiological characteristics:
Device Configuration: Use specially designed neonatal electrode belts with appropriate sizing for chest circumference [5] [26].
Monitoring Applications:
Data Interpretation Adjustments:
EIT Data Processing and Analysis Framework
Signal Processing Workflow
EIT signal processing involves sequential steps to extract clinically meaningful information from raw impedance data:
Filtering: Remove noise and artifacts while preserving respiratory and cardiovascular signals. Low-pass filters typically eliminate cardiovascular artifacts, but more sophisticated approaches (e.g., frequency-based separation) may be employed during offline processing [25]. Filtering should be applied to pixel impedance data before summation to avoid phase-related distortions [25].
Lung Segmentation: Identify functional lung regions within the EIT image. This process separates ventilation-related impedance changes from cardiac activity and other sources [25]. Multiple algorithms exist for automated lung segmentation, with consistency being crucial for longitudinal comparisons [25].
Region of Interest (ROI) Selection: Divide the lung into clinically relevant regions for quantitative analysis. The standard approach partitions the lung into four equal vertical regions (ROI1-ROI4 from ventral to dorsal) [1] [25]. Some applications may benefit from alternative segmentation strategies based on specific clinical questions.
Functional Parameter Calculation: Compute quantitative EIT indices including:
- Tidal Impedance Variation (TIV): Reflects tidal volume changes [1]
- End-Expiratory Lung Impedance (EELI): Tracks end-expiratory lung volume changes [1]
- Global Inhomogeneity (GI) Index: Quantifies ventilation distribution heterogeneity [1]
- Center of Ventilation (CoV): Identifies the central position of ventilation [1]
- Regional Ventilation Delay (RVD): Detects delayed ventilation in specific regions [1]
Technical Limitations and Mitigation Strategies
Despite its clinical utility, EIT faces several technical challenges:
The Inverse Problem: Image reconstruction from surface measurements is mathematically ill-posed, resulting in limited spatial resolution and quantitative inaccuracy [1]. Modern reconstruction algorithms and machine learning approaches help mitigate these limitations [1].
Electrode Contact Variability: Skin-electrode impedance variations introduce artifacts [1]. Active electrode systems with integrated preamplifiers minimize these effects [1].
Limited Anatomical Coverage: Conventional EIT monitors a single transverse plane, excluding apical and basal regions [1]. Multiplane systems and rotating electrode belts are under development to address this constraint [1].
Sensitivity to Non-Ventilation Factors: Pleural effusions, pneumothoraces, and body position changes affect impedance measurements [25]. Recognizing characteristic patterns of these conditions enables their identification and, in some cases, quantitative assessment [25].
Diagram 1: Comprehensive EIT Data Acquisition and Processing Workflow. This diagram illustrates the sequential process from patient setup to clinical decision-making, mapping the five core EIT processes defined by the TREND consensus group [26].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Components for EIT Investigation
| Component Category | Specific Examples | Research Function | Technical Considerations |
|---|---|---|---|
| EIT Hardware Platforms | Commercial systems (Swisstom, Dräger); Open-source platforms [28] | Data acquisition and voltage measurement | Active electrode systems minimize artifacts; ASIC/SoC designs improve integration [1] |
| Electrode Arrays | 16-32 electrode belts; Neonatal-specific belts; Multi-plane configurations | Current application and voltage sensing | Optimal inter-electrode spacing critical; Belt size affects image quality [25] |
| Contact Enhancement Solutions | Ultrasound gel; Saline solution; Device-specific contact agents | Improve electrode-skin interface | Reduce impedance variability; Minimize motion artifacts [25] |
| Image Reconstruction Software | EIDORS; Custom MATLAB/Python algorithms; Commercial software | Solve inverse problem; Generate tomographic images | Algorithm choice balances speed/accuracy; Machine learning approaches emerging [1] |
| Signal Processing Tools | Digital filters; Frequency separation algorithms; Artifact correction | Extract respiratory/cardiac signals | Sophisticated filters preserve harmonic content; Pixel-level filtering recommended [25] |
| Synchronization Interfaces | Ventilator data inputs; Physiological monitoring inputs | Correlate EIT with physiological events | Essential for breath-by-breath analysis; Reference maneuvers aid synchronization [25] |
| Calibration References | Spirometry; Plethysmography; CT correlation | Convert arbitrary units to absolute volumes | Point calibrations require repetition with condition changes [25] |
Future Directions and Innovation Pathways
The evolving landscape of EIT research encompasses several promising directions aimed at addressing current limitations and expanding clinical applications:
Hardware Innovations: Next-generation EIT systems incorporate multi-frequency excitation to exploit impedance spectroscopy for enhanced tissue differentiation [1]. Active electrodes with integrated amplifiers minimize cable-induced artifacts, while System-on-Chip (SoC) architectures consolidate signal generation, switching, and data acquisition to improve spatial resolution [1]. These advancements address fundamental limitations in signal fidelity and system portability.
Computational Advances: Machine learning approaches, particularly convolutional neural networks (CNNs) and ensemble learning methods, are revolutionizing image reconstruction by modeling non-linear relationships and capturing physical effects overlooked by traditional algorithms [1]. Physics-informed learning represents a particularly promising direction that combines the adaptive power of data-driven approaches with the robustness of physical models [1].
Clinical Protocol Standardization: Recent expert consensus meetings have established standardized recommendations for EIT acquisition, processing, and clinical application [25] [27]. These guidelines promote reproducible research and facilitate the integration of EIT into personalized mechanical ventilation strategies. Ongoing efforts focus on establishing uniform nomenclature and validation methodologies across research centers.
Expanded Clinical Applications: Beyond ventilation monitoring, EIT shows growing promise in perfusion assessment using cardiac-related impedance signals, ventilation-perfusion mismatch quantification, and monitoring novel interventions such as phrenic nerve stimulation [25]. The technology's ability to provide continuous, non-invasive assessment of both ventilation and perfusion simultaneously positions it as a comprehensive pulmonary monitoring tool.
As EIT technology matures and standardization efforts progress, this imaging modality is poised to transition from a research tool to an integral component of personalized critical care, offering unprecedented insights into regional lung function at the bedside without exposing vulnerable patients to ionizing radiation.
Electrical Impedance Tomography (EIT) is a non-invasive imaging modality that reconstructs internal conductivity distributions by applying safe alternating currents and measuring boundary voltages [3]. Unlike structural imaging methods like CT or MRI, EIT excels in real-time functional monitoring, particularly for pulmonary and cardiac applications, benefiting from its portability, absence of ionizing radiation, and low operational cost [3] [29]. However, traditional EIT systems face challenges including low spatial resolution, limited signal-to-noise ratio (SNR) at high frequencies, and the ill-posed nature of the inverse problem [30].
Innovative hardware architectures are crucial to overcoming these limitations. This article details two transformative approaches: modular systems, which enhance scalability and maintenance, and semi-parallel data acquisition systems (DAS), which significantly improve data collection speed and signal quality. By framing these developments within the context of EIT imaging methodology research, we provide a structured guide—complete with quantitative comparisons, experimental protocols, and visualization tools—to empower researchers and engineers in advancing this promising technology.
Modular EIT System Design
Core Principles and Architecture
Modular EIT design involves constructing a system from discrete, interchangeable hardware units, each dedicated to a specific function (e.g., signal generation, voltage measurement, or electrode control). This philosophy contrasts with monolithic designs and offers key advantages: enhanced scalability (easily adapting the electrode count to specific applications), simplified maintenance and upgrades (troubleshooting or replacing individual modules), and improved signal integrity by minimizing the distance between electrodes and their corresponding front-end electronics [30].
The SJTU Mk-1 system exemplifies this architecture. Its core components are connected via a ribbon cable with seventeen slots, creating a circular topology that mimics the shape of the sensing region [30].
Quantitative Performance of Modular Systems
The performance of a modular system like the SJTU Mk-1 can be evaluated through its transfer impedance accuracy and stability across a wide frequency range, which is essential for probing the intracellular properties of tissues at higher frequencies [30].
Table 1: Performance Calibration of the SJTU Mk-1 EIT System
| Frequency | Excitation Current | Transfer Impedance Magnitude Error | Phase Error | SNR |
|---|---|---|---|---|
| 1 kHz | < 0.5 mA | 0.13% | 0.20° | > 85 dB |
| 50 kHz | < 0.5 mA | 0.18% | 0.35° | > 80 dB |
| 250 kHz | < 0.5 mA | 0.21% | 0.60° | > 75 dB |
| 500 kHz | < 0.5 mA | 0.25% | 1.20° | > 70 dB |
| 1 MHz | < 0.5 mA | 0.32% | 2.50° | > 65 dB |
Data adapted from Ma et al. (2017) [30]. Performance was calibrated using a resistor phantom with excitation currents set below the 0.5 mA safety threshold for medical applications.
Experimental Protocol: Validation of a Modular EIT System
Objective: To validate the imaging performance and accuracy of a modular EIT system using a lung phantom model. Materials:
- Modular EIT system (e.g., SJTU Mk-1 architecture)
- Cylindrical water tank (20 cm diameter)
- Saline solution (conductivity: ~900 µS/cm)
- Two agar models (lung-shaped, conductivity: ~1.5 µS/cm)
- 16-electrode array
Procedure:
- System Setup: Arrange the 16 frontend modules around the ribbon cable. Attach the electrode array to the inner wall of the water tank.
- Baseline Data Acquisition: Fill the tank with saline solution only. Collect a reference dataset by performing a full scan using all electrode combinations.
- Phantom Imaging: Place the two agar models into the tank to simulate lungs. Ensure they are positioned symmetrically and do not touch the tank walls.
- Target Data Acquisition: Collect a new dataset with the agar models in place.
- Image Reconstruction: Use a differential reconstruction algorithm (e.g., one-step Gauss-Newton with Tikhonov regularization) to generate an image of conductivity change.
- Validation: Compare the reconstructed image with the known physical configuration of the phantom. The agar models should be clearly distinguishable as low-conductivity regions against the higher-conductivity saline background [30].
Semi-Parallel EIT Data Acquisition
Core Principles and Architecture
Semi-parallel DAS represents a hybrid approach that balances performance and complexity. It employs a single current source for injection but multiple, synchronized voltage measurement channels to read boundary voltages in parallel [31] [30]. This architecture directly addresses a major bottleneck in serial systems, where a single voltmeter sequentially scans all channels, limiting frame rates.
The primary advantage is a dramatic increase in data acquisition speed, enabling high-frame-rate imaging crucial for capturing dynamic physiological processes like cardiac-induced impedance changes [32]. Furthermore, by reducing the number of times analog multiplexers must switch during a full frame capture, the system minimizes errors introduced by the parasitic capacitances of these components, thereby improving overall accuracy, especially at higher frequencies [30].
Implementation and Quantitative Analysis
Modern implementations often leverage integrated impedance analyzers. For instance, a wearable system was developed using five AD5933 chips operating in parallel [31]. A central microcontroller (STM32) coordinates their operation, while an external clock chip (ICS553) and an I²C multiplexer (TCA9548A) ensure high synchronization. This semi-parallel configuration allows the system to achieve a frame rate sufficient for real-time lung respiration imaging at a low cost [31].
Table 2: Comparison of EIT System Architectures
| Feature | Serial Architecture | Fully-Parallel Architecture | Semi-Parallel Architecture |
|---|---|---|---|
| Current Sources / Voltmeters | One each | Multiple each | One source, multiple voltmeters |
| Data Acquisition Speed | Low | Very High | High |
| System Complexity & Cost | Low | Very High | Moderate |
| Effect of Multiplexer Parasitics | Significant | None (no multiplexers) | Reduced |
| Example Systems | Sheffield Mk3.5 [30] | KHU Mark2, Dartmouth (2008) [30] | SJTU Mk-1, Wearable AD5933 System [31] [30] |
Integrated System Workflow and Signaling
The synergy between modular and semi-parallel designs creates a high-performance EIT system. The following diagram illustrates the signal pathway and logical workflow of such an integrated architecture, from signal generation to image reconstruction.
Diagram 1: Signal flow and system control in a modular semi-parallel EIT architecture. The control module orchestrates the current injection and parallel voltage measurement via multiplexers, with synchronization managed by a global clock.
The Scientist's Toolkit: Research Reagent Solutions
For researchers developing or working with these EIT systems, a standardized set of materials and reagents is essential for system calibration, validation, and experimental procedures.
Table 3: Essential Research Reagents and Materials for EIT Experiments
| Item Name | Function/Description | Typical Specification/Usage |
|---|---|---|
| Saline Solution | Acts as a homogeneous background medium in phantom experiments. | Conductivity ~0.9 S/m, adjusted to mimic body fluid conductivity [30]. |
| Agar Phantoms | Creates stable, tissue-mimicking inclusions for imaging validation. | Molded into specific shapes (e.g., lungs); conductivity tunable with NaCl/CuSO4 [30]. |
| Resistor Phantom | Provides a stable, known impedance network for system calibration. | Network of precision resistors (e.g., 330Ω) arranged in a ring to validate transfer impedance accuracy [30]. |
| Hypertonic Saline (10% NaCl) | Serves as an ionic contrast agent for perfusion imaging studies. | Injected as a 5-10 ml bolus during breath-hold to enhance conductivity in blood [32]. |
| Electrode Gel | Ensures stable electrical contact between electrodes and the subject's skin. | High conductivity, medical-grade electrolyte gel to minimize skin-electrode impedance. |
| AD5933 Impedance Analyzer | Core IC for low-cost, portable systems; performs signal generation and analysis. | Integrated DDS and DSP; used in parallel for semi-parallel voltage measurement [31]. |
Advanced Protocol: Pulmonary Perfusion and Ventilation/Quantification (V/Q) Matching
Objective: To non-invasively monitor and assess the matching of lung ventilation (V) and perfusion (Q) in an animal model using a high-performance EIT system. Materials:
- High-performance EIT system (e.g., EC-100 pro, SNR > 100 dB, accuracy > 0.01‰) [32]
- 16-electrode belt
- Animal preparation (e.g., anesthetized pig, tracheal intubation, central venous catheter)
- Physiological monitor (for ECG, blood pressure, SpO₂)
- Hypertonic saline (10% NaCl)
Procedure:
- Animal Preparation: Anesthetize and intubate the subject. Place a central venous catheter. Shave the chest and attach the 16-electrode belt in a transverse plane around the thorax.
- Data Acquisition for Ventilation: Record continuous EIT data at 40-100 fps during normal ventilation to establish a baseline for lung ventilation.
- Perfusion Imaging via Pulsatility:
- At end-expiration, temporarily halt the ventilator.
- Acquire EIT data over approximately 20 cardiac cycles.
- Use the PPG-synchronized impedance signals to extract the cardiac-paced component of the impedance change, which corresponds to pulmonary perfusion [32].
- Perfusion Imaging via Saline Bolus (Control):
- At end-expiration, inject 5 ml of 10% NaCl rapidly via the central venous catheter.
- Continue EIT acquisition during the breath-hold to capture the transient conductivity increase as the bolus passes through the pulmonary vasculature.
- Image Analysis and V/Q Calculation:
- Reconstruct separate images for ventilation (from step 2) and perfusion (from step 3 or 4).
- Calculate the V/Q match ratio by determining the spatial overlap between the ventilated and perfused regions within the lung. A high correlation (e.g., r = 0.72, as reported) indicates good V/Q matching [32].
The workflow for this advanced protocol is detailed below.
Diagram 2: Experimental workflow for assessing pulmonary ventilation/perfusion (V/Q) matching using EIT. The protocol compares a non-invasive pulsatility method with a saline bolus control method.
The evolution of EIT hardware through modular and semi-parallel architectures marks a significant leap toward realizing the full clinical potential of this technology. Modular designs offer the robustness, scalability, and signal fidelity required for diverse research and clinical environments. Semi-parallel data acquisition directly tackles the critical limitations of speed and accuracy, enabling high-fidelity, real-time dynamic imaging.
When integrated, these architectures form a powerful platform for advanced physiological studies, such as the detailed monitoring of lung V/Q matching. As research continues, the convergence of these sophisticated hardware designs with artificial intelligence-driven reconstruction algorithms [29] and further miniaturization will undoubtedly expand the frontiers of EIT, solidifying its role as an indispensable tool in functional medical imaging.
Functional cellular imaging is pivotal for modern drug discovery, providing insights into the physiological state of cells beyond what structural imaging can offer. Electrical impedance tomography (EIT) has emerged as a powerful, label-free technique for non-invasively monitoring the electrical properties of biological systems. Recent technological breakthroughs have now enabled intracellular conductivity imaging at the single-cell level, opening new frontiers for preclinical assessment of drug efficacy and toxicity. This Application Note details a novel micro-EIT system capable of mapping subcellular conductivity distributions, providing detailed protocols for its application in drug discovery platforms. By quantifying electrical properties of the cytoplasm and nucleoplasm, this methodology offers a transformative approach for evaluating cellular responses to therapeutic compounds in their most natural, unperturbed state.
Traditional impedance-based cellular analysis is limited to extracellular measurements or population-level assessments, lacking the spatial resolution to resolve intracellular compartments. The newly developed micro-EIT system overcomes these limitations through two key innovations: a custom-designed microsensor fabricated via electron beam lithography and a frequency-differential EIT (fdEIT) approach coupled with a single-cell equivalent circuit reconstruction algorithm [33] [34].
System Specifications and Performance Metrics
Table 1: Technical Specifications of the Micro-EIT System for Intracellular Imaging
| Parameter | Specification | Significance for Intracellular Imaging |
|---|---|---|
| Electrode Width | 7 μm | Enables single-cell scale resolution |
| Electrode Spacing | 40 μm | Optimized for cellular dimensions |
| Electrode Material | Gold (50 nm) with Titanium adhesion layer (5 nm) | Biocompatibility and stable frequency response |
| Signal-to-Noise Ratio | 50-200 | Ensures data fidelity for quantitative reconstruction |
| Spatial Resolution | Subcellular structures | Distinguishes cytoplasm and nucleoplasm |
| Measurement Frequencies | fext, fcyt, fnuc (frequency-dependent) | Selectively probes different cellular compartments |
This system represents the first demonstration of non-invasive intracellular conductivity mapping that distinguishes subcellular structures based on their intrinsic electrical properties, without requiring labels or invasive procedures [33].
Experimental Protocols
Protocol 1: Micro-EIT System Setup and Calibration
Purpose: To properly configure and calibrate the micro-EIT system for intracellular conductivity imaging.
Materials:
- Custom micro-EIT sensor (8 electrodes, 7 μm width, 40 μm spacing on glass substrate)
- Polydimethylsiloxane (PDMS) sheet with corn-shaped hole structure (70 μm bottom size)
- Impedance analyzer and multiplexer system
- Optical microscope for alignment and verification
Procedure:
- Sensor Preparation: Mount the custom micro-EIT sensor on the PCB platform, ensuring the inspection hole is aligned for microscopic observation.
- Fluidic Chamber Assembly: Align and place the PDMS sheet with the corn-shaped hole structure at the center of the micro-EIT sensor. This structure confines single cells within the sensor area.
- System Connection: Connect the electrode pads to the multiplexer via gold-ball bonding and protect all connections with epoxy coating.
- Electrical Verification: Perform impedance sweep (typically 100 kHz to 5 MHz) on the system without cells to establish baseline performance and ensure stable frequency response.
- Frequency Calibration: Determine the three critical operating frequencies through preliminary equivalent circuit analysis:
- fext (∼400 kHz): Where resistance reaches maximum (extracellular fluid dominant)
- fcyt: Cytoplasm dominant frequency
- fnuc: Nucleoplasm dominant frequency [34]
Protocol 2: Intracellular Conductivity Imaging of Adherent Cells
Purpose: To obtain quantitative intracellular conductivity distributions from single living cells.
Materials:
- MRC-5 human lung fibroblast cell lines (or other adherent cell types)
- Appropriate cell culture media and supplements
- Trypsin-EDTA solution for cell passaging
- Micro-EIT system with temperature control (maintain at 37°C)
- Phosphate Buffered Saline (PBS) for washing
- Validation: Brightfield and fluorescence microscopy setup
Procedure:
- Cell Seeding:
- Trypsinize and resuspend cells at appropriate density (∼1×10⁵ cells/mL).
- Introduce cell suspension into the micro-EIT PDMS chamber and allow cells to settle and adhere for 4-24 hours.
- Verify single-cell distribution within the sensor area using brightfield microscopy.
Impedance Data Acquisition:
- Replace culture media with fresh, pre-warmed media to ensure consistent ionic composition.
- Apply alternating current (safe amplitude, typically ≤5 mA) through electrode pairs using adjacent drive pattern [35].
- Measure voltage signals from all remaining electrodes simultaneously.
- Repeat measurements across the determined frequency spectrum (fext, fcyt, fnuc).
- For each frequency, complete a full data set by rotating current injection through all possible electrode pairs.
Image Reconstruction:
- Apply frequency-difference EIT (fdEIT) algorithm:
- For cytoplasm conductivity (σcyt): Use fext as reference and fcyt as objective data.
- For nucleoplasm conductivity (σnuc): Use fcyt as reference and fnuc as objective data.
- Utilize single-cell equivalent circuit-based reconstruction algorithm to convert boundary measurements to internal conductivity distributions.
- Reconstruct 2D conductivity maps showing subcellular compartmentalization.
- Apply frequency-difference EIT (fdEIT) algorithm:
Validation and Co-Registration:
Protocol 3: Drug Response Assessment Using Intracellular Conductivity
Purpose: To evaluate compound effects on cellular physiology through changes in intracellular conductivity.
Materials:
- Test compounds (e.g., ion channel modulators, cytotoxic agents)
- DMSO or appropriate vehicle control
- Micro-EIT system with continuous perfusion capability
- Time-lapse imaging software
Procedure:
- Baseline Acquisition:
- Perform intracellular conductivity imaging on target cells following Protocol 2 to establish baseline σcyt and σnuc values.
- Acquire multiple baseline measurements over 30-60 minutes to confirm stability.
Compound Application:
- Prepare compound solutions at desired concentrations in pre-warmed culture media.
- Gently perfuse compound solution through the measurement chamber while maintaining temperature.
- Record exact time of compound introduction for temporal analysis.
Time-Series Monitoring:
- Continuously monitor impedance changes at the three characteristic frequencies.
- Reconstruct conductivity images at regular intervals (e.g., every 5-15 minutes).
- Continue monitoring for duration appropriate to compound mechanism (typically 2-24 hours).
Data Analysis:
- Quantify temporal changes in σcyt and σnuc relative to baseline.
- Compare conductivity changes between different cell types or treatment conditions.
- Correlate conductivity changes with cell viability or functional assays if available.
- Perform statistical analysis on replicates to determine significance [33] [36].
Data Analysis and Interpretation
Quantitative Conductivity Parameters
Table 2: Intracellular Conductivity Parameters in Different Cell Models
| Cell Type / Condition | Cytoplasm Conductivity (σcyt) | Nucleoplasm Conductivity (σnuc) | Biological Significance |
|---|---|---|---|
| MRC-5 Human Lung Fibroblast (Wild Type) | Baseline value | Baseline value | Reference physiological state |
| MRC-5 with Protein Expression Variant A | Significantly increased | No significant change | Indicates altered cytoplasmic composition |
| MRC-5 with Protein Expression Variant B | No significant change | Significantly decreased | Suggests nucleoplasmic structural changes |
| Cells Treated with Ion Channel Blocker | Decreased | Decreased | Reflects altered ion homeostasis |
| Cells Undergoing Apoptosis | Progressive decrease | Progressive decrease | Indicates loss of membrane integrity and content leakage |
The successful reconstruction of σcyt and σnuc in three types of MRC-5 human lung fibroblast cell lines with different protein expressions has revealed clear differences corresponding to these variations, demonstrating the sensitivity of this method to detect phenotypic changes at the subcellular level [33] [34].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for Intracellular Conductivity Imaging
| Item | Function / Application | Specifications / Notes |
|---|---|---|
| Micro-EIT Sensor | Core measurement device | 8 electrodes, 7 μm width, 40 μm spacing, fabricated via electron beam lithography |
| PDMS Microchamber | Single-cell confinement | Corn-shaped hole structure (70 μm bottom size) aligned to sensor center |
| Human Lung Fibroblasts | Cellular model system | MRC-5 cell lines with different protein expressions for method validation |
| Equivalent Circuit Model | Data interpretation | Includes Rext, Cmem, Rcyt, Cn-m, Rnuc for frequency response analysis |
| Frequency-difference EIT Algorithm | Image reconstruction | Enables separation of cytoplasmic and nucleoplasmic conductivity |
| Optical Validation System | Method verification | Brightfield and fluorescence microscopy for coordinate and size verification |
Workflow Visualization
Figure 1: Experimental workflow for intracellular conductivity imaging, highlighting the frequency-dependent current pathways that enable subcellular resolution.
Figure 2: Drug discovery assessment platform using intracellular conductivity imaging for cardiotoxicity screening and mechanism of action studies.
The integration of micro-EIT technology for intracellular conductivity imaging represents a significant advancement in preclinical drug discovery platforms. This methodology provides quantitative, label-free assessment of subcellular physiology that can detect subtle changes in cellular state long before morphological alterations become apparent. The detailed protocols outlined in this Application Note enable researchers to implement this cutting-edge technology for enhanced cardiotoxicity screening, mechanism of action studies, and phenotypic drug discovery. As the field progresses, combining EIT with machine learning approaches and multi-modal imaging will further strengthen its predictive power in the drug development pipeline [4] [36].
Overcoming EIT Challenges: System Optimization, Noise Reduction, and Generalization
Electrical Impedance Tomography (EIT) is a non-invasive, radiation-free functional imaging technique that reconstructs internal conductivity distributions by applying safe alternating currents and measuring resulting boundary voltages. Its hardware architecture directly determines critical performance parameters including data acquisition speed, image resolution, power consumption, cost, and portability. This application note analyzes the fundamental trade-offs between serial, parallel, and semi-parallel EIT system architectures, providing structured quantitative comparisons and detailed experimental protocols to guide researchers in selecting optimal configurations for specific biomedical applications ranging from single-cell analysis to clinical lung monitoring.
EIT hardware architectures are primarily classified based on how current injection and voltage measurement operations are coordinated across electrode arrays. In serial systems, a single current source and voltage measurement module sequentially interrogate electrode pairs, creating a inherent bottleneck that limits acquisition speed but minimizes hardware complexity and cost [31]. In fully parallel systems, multiple independent current sources and voltmeters operate simultaneously across all excitation channels, maximizing data throughput and reducing parasitic effects at the expense of significant hardware complexity, cost, and calibration challenges [30]. The semi-parallel architecture emerges as a pragmatic compromise, employing a single current source paired with parallel voltage measurement modules, balancing improved acquisition speed against manageable system complexity [31] [30].
The evolution of EIT from bulk tissue imaging to intracellular resolution [34] [37] has further accentuated these architectural trade-offs, requiring researchers to make informed decisions based on their specific resolution, speed, and cost constraints.
Quantitative Comparison of EIT Architectures
Table 1: Performance Characteristics Across EIT System Architectures
| Architectural Parameter | Serial Systems | Semi-Parallel Systems | Fully Parallel Systems |
|---|---|---|---|
| Measurement Approach | Sequential channel switching via multiplexers [31] | Single current injection with parallel voltage measurements [30] | Simultaneous current injection and voltage measurement [30] |
| Data Acquisition Speed | Low (θ(N) latency) [38] | Moderate (improved via parallel voltage measurement) [31] | High (maximum theoretical throughput) [30] |
| Hardware Complexity | Low (minimal components) [31] | Moderate (multiple ADCs, single source) [31] | High (multiple sources and meters) [30] |
| System Cost | Low [31] | Moderate [30] | High (e.g., >$25k for NI-based systems) [30] |
| Parasitic Effects | Significant at high frequencies [30] | Reduced through minimized multiplexing [31] | Minimized (no multiplexers required) [30] |
| Calibration Complexity | Simple | Moderate [30] | High (multiple current sources) [30] |
| Typical Applications | Basic research, low-frequency applications [30] | Medical monitoring, portable systems [31] | Research systems, high-frequency applications [30] |
Table 2: Representative Implementations of EIT Architectures
| System Implementation | Architecture Type | Electrode Count | Frequency Range | Key Features |
|---|---|---|---|---|
| Sheffield Mk3.5 [31] | Serial | 8 electrodes | 2 kHz - 1.6 MHz | 8 data acquisition boards with DSP, 40 dB SNR |
| SJTU Mk-1 [30] | Semi-Parallel | 16 frontend modules | 1 kHz - 1 MHz | Modular design, ribbon cable connection |
| Wearable AD5933 System [31] | Semi-Parallel | Configurable | 1 kHz - 100 kHz | 5 parallel AD5933, Bluetooth, battery-powered |
| KHU Mark2 [30] | Fully Parallel | Configurable | 10 Hz - 500 kHz | No multiplexers, high-frequency capability |
| Dartmouth System (2008) [30] | Fully Parallel | Configurable | Up to 2 MHz | Minimal analog circuits, reduced parasitics |
| Micro-EIT Intracellular [34] | Specialized Serial | 8 microelectrodes | 100 kHz - 5 MHz | 7μm electrode width, 40μm spacing, single-cell resolution |
Architectural Trade-off Analysis
Performance Versus Complexity Trade-offs
The fundamental tension in EIT design balances computational performance against hardware complexity. Serial architectures exemplify the simplicity extreme with minimal components but suffer from θ(N) latency as measurements scale with electrode count [38]. Parallel systems achieve optimal throughput through hardware replication but encounter carry propagation challenges analogous to digital adder design [38]. The semi-parallel approach strategically distributes complexity, maintaining a single current source while parallelizing voltage measurement, thus avoiding the calibration burden of multiple current sources while significantly improving acquisition speed [31] [30].
This performance-complexity relationship manifests distinctly in frequency domain behavior. Serial systems experience significant parasitic capacitance effects from multiplexers above 250 kHz, constraining practical operation to lower frequencies [30]. Fully parallel systems eliminate multiplexers entirely, enabling operation to 2 MHz and beyond [30], while semi-parallel designs strategically minimize multiplexer usage in critical signal paths to achieve 1 MHz performance [30].
Power Versus System Performance Optimization
EIT systems face intrinsic power-performance trade-offs where computational throughput typically scales with energy consumption [39]. Wearable systems exemplify this challenge, requiring careful balance between measurement frequency and battery life. The wearable AD5933-based system addresses this through dynamic power management, incorporating Bluetooth for efficient data transmission and lithium battery power for portability [31]. As with embedded systems generally, EIT designers must consider whether additional processing capabilities justify their power costs, particularly for continuous monitoring applications [39].
Cost Versus Reliability Considerations
Engineering economics fundamentally influence EIT architecture selection. Serial systems offer lowest implementation cost but may compromise reliability through extensive analog multiplexing [31] [39]. Commercial parallel systems like National Instruments implementations exceed $25,000, providing maximum performance but limiting accessibility [30]. Semi-parallel designs strategically balance these factors, with the SJTU Mk-1 demonstrating that moderate-cost systems (~$150 per channel for semi-parallel vs. potentially >$500 per channel for full parallel) can achieve reliable medical-grade performance [30].
Experimental Protocols for EIT System Validation
Protocol 1: System Performance Calibration for Medical Application
Purpose: To characterize EIT system transfer impedance accuracy across operational frequency spectrum under medical safety constraints.
Materials:
- EIT system under test (serial, parallel, or semi-parallel architecture)
- 16-element cylindrical resistor phantom with known impedance values
- Saline phantom with calibrated conductivity (900 μS/cm)
- Temperature measurement probe
- Data acquisition software
Procedure:
- Set excitation current to 0.5 mA RMS maximum, complying with medical safety standards [30]
- Measure transfer impedances at seven frequency points: 1 kHz, 20 kHz, 50 kHz, 250 kHz, 500 kHz, 750 kHz, and 1 MHz
- For each frequency, collect 100 repeated measurements to calculate signal-to-noise ratio (SNR)
- Compute mean and standard deviation of transfer impedance magnitude and phase
- Compare measured values against known reference impedances
- Calculate percentage error for both magnitude and phase
Validation Metrics:
- SNR > 80 dB for high-performance systems [31]
- Phase error < 1° for systems with 1 MHz capability [30]
- Magnitude error < 1% across frequency range [30]
Protocol 2: Intracellular Conductivity Imaging of Single Cells
Purpose: To reconstruct intracellular conductivity distributions distinguishing cytoplasmic and nucleoplasmic compartments using micro-EIT.
Materials:
- Custom micro-EIT sensor (7 μm electrode width, 40 μm spacing) [34]
- PDMS chamber with corn-shaped hole structure (70 μm bottom diameter)
- MRC-5 human lung fibroblast cell lines
- Frequency response analyzer (100 kHz to 5 MHz)
- Brightfield and fluorescence microscope for validation
Procedure:
- Culture MRC-5 cells in standard conditions and transfer single cell to micro-EIT sensor chamber
- Acquire impedance spectra from 100 kHz to 5 MHz using 8-electrode array
- Identify characteristic frequencies via Nyquist plot analysis:
- fext = 400 kHz (extracellular dominant, rightmost Nyquist point) [34]
- fcyt = cytoplasmic dominant frequency from equivalent circuit fitting
- fnuc = nucleoplasmic dominant frequency from equivalent circuit fitting
- Apply frequency-difference EIT (fdEIT) reconstruction:
- Reconstruct cytoplasm using fext (reference) and fcyt (objective)
- Reconstruct nucleoplasm using fcyt (reference) and fnuc (objective)
- Validate reconstruction results with brightfield and fluorescence microscopy
Validation Metrics:
- Signal-to-noise ratio between 50-200 [34]
- Successful differentiation of σcyt and σnuc for three cell types [34]
- Spatial correlation >90% with microscopic validation [34]
System Architecture Visualization
Diagram 1: EIT System Architecture Comparison. Serial uses sequential measurement; semi-parallel employs parallel voltage measurement with single current source; fully parallel uses simultaneous current injection and voltage measurement.
Diagram 2: EIT Experimental Workflow. Decision flow for architecture selection with frequency optimization for intracellular imaging.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for EIT System Development and Validation
| Category | Item/Reagent | Specifications | Research Function |
|---|---|---|---|
| Impedance Chips | AD5933 | 12-bit ADC, 1 kHz-100 kHz [31] | Core impedance measurement for cost-sensitive designs |
| AFE4300 | 6-bit DAC, up to 250 kHz [30] | Integrated analog frontend for medical applications | |
| Electrode Materials | Titanium (Ti) | 5 nm adhesion layer [34] | Glass substrate bonding for micro-EIT sensors |
| Gold (Au) | 50 nm conductive layer [34] | Direct sample contact for impedance measurement | |
| Sensor Fabrication | Electron Beam Lithography | <10 μm feature size [34] | Micro-EIT electrode patterning |
| PDMS Sheet | Corn-shaped hole structure [34] | Single-cell confinement chamber | |
| Calibration Standards | Resistor Phantom Rings | Known impedance values [30] | System transfer impedance calibration |
| Saline Solutions | 900 μS/cm conductivity [30] | Biological tissue mimicking phantom | |
| Cell Lines | MRC-5 Human Lung Fibroblast | Three protein expression variants [34] | Intracellular conductivity imaging validation |
| Software Tools | SPICE Simulators | Circuit analysis [34] | Current response simulation and analysis |
| EIT Reconstruction Algorithms | Frequency-difference methods [34] | Conductivity distribution calculation |
EIT system architecture selection involves multidimensional trade-offs where no single approach dominates across all applications. Serial architectures provide accessible entry points for basic research and educational applications with constrained budgets. Fully parallel systems deliver maximum performance for high-frequency research applications regardless of cost. Semi-parallel designs offer the most pragmatic balance for clinical and portable implementations where both performance and practical constraints must be respected. The ongoing miniaturization of EIT systems toward single-cell resolution [34] [37] and integration with artificial intelligence reconstruction algorithms [29] will continue to refine these architectural trade-offs, enabling new biomedical applications while maintaining the fundamental performance-complexity relationships analyzed in this application note.
Mitigating Parasitic Capacitances and Ensuring Patient Safety in High-Frequency Operation
Parasitic capacitance represents a primary challenge in the development and operation of high-frequency Electrical Impedance Tomography (EIT) systems, particularly as the field advances toward multifrequency applications operating from kilohertz to megahertz ranges [40] [41]. These stray capacitances, inherent in system components, cables, and connections, create unintended pathways for leakage currents to ground, significantly compromising measurement accuracy at higher frequencies [40] [41]. For EIT systems targeting biomedical applications such as lung monitoring and brain imaging, mitigating these effects is crucial not only for data fidelity but also for ensuring patient safety [25] [2]. This document establishes standardized protocols for quantifying, mitigating, and compensating for parasitic capacitances in EIT systems, with particular emphasis on high-frequency operation within safe physiological parameters.
Background and Significance
The Impact of Parasitic Capacitances in EIT Systems
In EIT instrumentation, parasitic capacitances originate from multiple sources, including printed circuit board (PCB) traces, cable shielding, multiplexers, and the electrode-tissue interface itself [40] [31]. At high frequencies, these capacitances form low-impedance shunt paths that divert injected current away from the target biological tissues, leading to signal oscillations, leakage currents, and ultimately, erroneous impedance measurements [40] [31]. This effect is particularly pronounced in tetrapolar measurement systems, where the capacitive nature of electrode impedance can introduce significant phase errors when coupled with parasitic capacitances [40].
The relationship between operating frequency and measurement error is not linear; as frequency increases, the capacitive reactance (Xc = 1/2πfC) decreases, creating more significant shunt paths. This phenomenon explains why multifrequency EIT systems operating in the 100 kHz to 1 MHz range require exceptionally careful design to maintain signal integrity [41] [31].
Safety Implications in Biomedical Applications
The presence of parasitic capacitances introduces not only technical challenges but also potential safety concerns. Uncontrolled leakage currents pose electrical safety risks to patients, particularly in critical care settings where multiple monitoring devices may be connected simultaneously [25]. Furthermore, inaccurate impedance measurements resulting from uncompensated parasitic effects could lead to clinical misinterpretation in applications such as lung ventilation monitoring or intracranial abnormality detection [25] [2]. Ensuring both accurate performance and patient safety requires a systematic approach to parasitic capacitance management throughout the EIT system design and deployment process.
Table 1: Tissue Conductivity Values at Typical EIT Frequencies
| Tissue Type | Conductivity Range (mS/m) | Frequency Dependency |
|---|---|---|
| Cerebrospinal Fluid | 1450 - 1800 | Low |
| Blood | 500 - 650 | Moderate |
| Muscle | 200 - 400 | High (anisotropic) |
| Lung | Varies with air content | Very High |
| Fat | 50 | Low |
| Bone | 6 | Very Low |
Quantitative Analysis of Parasitic Effects
Parasitic Capacitance in System Components
The effective parasitic capacitance in an EIT system arises from the cumulative effect of distributed capacitances throughout the signal chain. Experimental characterization of a typical EIT data acquisition system revealed stray capacitances ranging from 10 pF to 150 pF across different channels, with significant impact on measurements above 100 kHz [41]. These values are consistent across multiple EIT system architectures, though the specific distribution varies with design implementation.
The electrode-tissue interface itself contributes additional frequency-dependent capacitance through the Helmholtz double layer effect and subsequent electrochemical processes. This interface can be modeled as a Constant Phase Element (CPE) with impedance defined by ZCPE = K(jω)^β, where K is a tissue-dependent constant and β is the dispersion factor [40]. The resulting capacitance (CCPE = 1/K(jω)^(β-1)) varies significantly with excitation frequency and electrode potential, creating a dynamic, non-linear component that must be considered in high-frequency operation [40].
Frequency-Dependent Error Propagation
The cumulative effect of parasitic capacitances manifests as progressive measurement degradation with increasing frequency. Without compensation, the signal-to-noise ratio of EIT systems can decrease by 20-40 dB when operating from 10 kHz to 1 MHz [31]. This degradation directly impacts image quality in clinical applications, particularly in cerebral EIT where the high resistivity of the skull already presents significant challenges [2].
Table 2: Error Sources in High-Frequency EIT Operation
| Error Source | Typical Magnitude | Impact on Measurement |
|---|---|---|
| Cable Capacitance | 50-200 pF/m | Phase shift, amplitude attenuation |
| Multiplexer Channel Capacitance | 10-50 pF | Cross-talk, signal leakage |
| Electrode-Tissue Interface Capacitance | 1-100 nF | Frequency-dependent phase error |
| PCB Trace Capacitance | 0.5-5 pF/cm | High-frequency signal integrity loss |
| Input Amplifier Capacitance | 1-10 pF | Gain reduction, stability issues |
Experimental Protocols for Parasitic Capacitance Characterization
Protocol 1: Bayesian Inference for System-Wide Capacitance Estimation
Objective: To comprehensively characterize parasitic capacitances throughout an EIT data acquisition system using statistical inference methods.
Materials and Equipment:
- EIT data acquisition system with programmable current source
- Precision reference resistors (10Ω - 1kΩ)
- Network analyzer or impedance analyzer
- MATLAB or Octave with statistical toolbox
- Custom PCB test fixture with known layout capacitances
Procedure:
- System Modeling: Develop a forward model of the EIT system using modified Kirchhoff's current law that incorporates parasitic capacitances as unknown parameters [41].
- Reference Measurements: Connect precision resistors in a ring configuration to the electrode channels and perform frequency-dependent measurements across the operational spectrum (e.g., 10 kHz - 1 MHz) [41].
- Bayesian Inference: Implement both Maximum a Posteriori (MAP) estimation and Markov Chain Monte Carlo (MCMC) methods to solve the inverse problem for capacitance values [41].
- Uncertainty Quantification: Use the posterior distribution from MCMC analysis to establish confidence intervals for each estimated capacitance value [41].
- Model Validation: Compare predicted system behavior with actual measurements using untested load configurations to validate the model accuracy.
Bayesian Capacitance Estimation Workflow
Protocol 2: Electrode-Tissue Interface Capacitance Characterization
Objective: To quantify the frequency-dependent capacitance of the electrode-tissue interface under realistic operating conditions.
Materials and Equipment:
- Tetrapolar electrode configuration setup
- Electrolytic solutions mimicking tissue conductivity (0.1-1.0 S/m)
- Ag/AgCl electrodes or gold-plated electrodes
- Potentiostat or precision impedance analyzer
- Temperature-controlled bath (37°C ± 0.5°C)
Procedure:
- Interface Modeling: Configure the electrode-electrolyte system using the simplified Helmholtz model, accounting for both resistive and capacitive components [40].
- Impedance Spectroscopy: Perform sweep measurements from 1 kHz to 1 MHz at multiple electrode potentials (±100 mV range) [40].
- Parameter Extraction: Fit measured data to the CPE model to extract K and β parameters using non-linear regression techniques [40].
- Capacitance Calculation: Derive the frequency-dependent capacitance using C_CPE = 1/K(jω)^(β-1) across the measured spectrum [40].
- Validation in Biological Tissue: Repeat measurements in ex vivo tissue samples (when available) to confirm physiological relevance.
Mitigation Strategies and Compensation Techniques
Hardware-Based Compensation Methods
1. Negative Impedance Converters (NIC):
- Implementation: Incorporate NIC circuits in the current source output to actively cancel parasitic capacitances [40].
- Effectiveness: Highly effective for fixed, known capacitances; less effective for dynamically changing electrode-tissue interface capacitance [40].
- Circuit Requirements: Precision matched resistors, high-speed operational amplifiers, stability compensation networks.
2. Layout Optimization and Shielding:
- PCB Design: Minimize trace lengths, use ground planes strategically, and implement guard rings around high-impedance nodes [31].
- Cable Management: Use driven shields that actively buffer signal potential on shield layers to reduce effective capacitance [31].
- Component Selection: Choose multiplexers with low channel capacitance (<10 pF) and high off-isolation [31].
3. System Architecture Adjustments:
- Voltage Excitation Approach: Implement voltage excitation with current measurement instead of traditional current injection to reduce sensitivity to parasitic capacitances [31].
- Frequency Adaptation: Design systems to operate at frequencies where capacitive effects are manageable while still providing sufficient tissue differentiation [2].
Signal Processing and Model-Based Compensation
1. Measurement Processing Compensation:
- Forward Model Integration: Incorporate known parasitic capacitances into the reconstruction algorithm to correct measurements [40] [41].
- Frequency-Domain Filtering: Apply digital filters specifically designed to counteract phase shifts introduced by parasitic elements [25].
- Calibration-Based Correction: Use reference measurements on known loads to derive correction factors for different operating frequencies [41].
2. Advanced Reconstruction Techniques:
- Bayesian Framework: Treat parasitic capacitances as uncertain parameters in a probabilistic reconstruction model [41].
- Multi-Frequency Differential Imaging: Utilize frequency-difference EIT (fdEIT) to cancel systematic errors including those from parasitic effects [2].
Table 3: Compensation Technique Comparison
| Technique | Implementation Complexity | Effectiveness | Limitations |
|---|---|---|---|
| Negative Impedance Converters | High | High for fixed capacitances | Stability concerns, complex tuning |
| Layout Optimization | Medium | Medium | Physical design constraints |
| Voltage Excitation Method | Low | Medium | Different error profile |
| Bayesian Model Compensation | Very High | Very High | Computational intensity |
| Frequency-Difference EIT | Medium | High | Requires multi-frequency operation |
Safety Protocols for High-Frequency EIT Operation
Electrical Safety Standards Implementation
Current Limiting Protocols:
- Implement hardware current limiters ensuring maximum injection current remains below 5 mA RMS across all operating frequencies [31].
- Incorporate redundant safety circuits including optical isolation and fast-acting fuses on all electrode driver circuits [25].
- Perform regular leakage current measurements under simulated fault conditions to verify isolation integrity [25].
Patient Interface Safety:
- Use certified medical-grade electrodes with proven biocompatibility [25].
- Implement impedance-based fault detection that monitors for electrode detachment or degradation during operation [25].
- Establish strict protocols for skin preparation and electrode placement to minimize interface impedance variations [25].
Clinical Application-Specific Safety Considerations
ICU Ventilation Monitoring:
- Verify compatibility with other life-support equipment, particularly pacemakers and ICDs, which may require special filtering or operating restrictions [25].
- Establish clear contraindications for patients with implanted electronic devices based on current medical guidelines [25].
- Implement artifact detection algorithms to identify and flag measurements potentially compromised by patient movement or external interference [25].
Cerebral EIT Applications:
- Employ additional conservative current limits (recommended < 2 mA RMS) for transcranial applications [2].
- Implement additional reference measurements to detect improper electrode contact or positioning [2].
- Establish rigorous protocols for head bandage placement and electrode positioning to ensure consistent measurements [2].
EIT Safety Protocol Flowchart
Research Reagent Solutions and Materials
Table 4: Essential Research Materials for EIT System Development
| Item | Specification | Research Function |
|---|---|---|
| AD5933 Impedance Converter | 12-bit, 1 kHz-100 kHz | Core impedance measurement IC for compact EIT systems [31] |
| Precision Multiplexers (ADG506) | <15 pF channel capacitance | Signal routing with minimal parasitic injection [41] |
| Howland Current Source | Programmable output 0.1-5 mA | Precision current injection with high output impedance [41] |
| Ag/AgCl Electrodes | 1-2 cm² contact area | Reliable skin interface with stable impedance characteristics [25] |
| Tissue-Equivalent Phantoms | σ = 0.1-1.0 S/m, εr = 10^3-10^6 | System validation without biological variability [2] |
| Bayesian Inference Software | MATLAB/Octave with MCMC toolbox | Parasitic parameter estimation and uncertainty analysis [41] |
Standardized Operating Procedure for High-Frequency EIT
Pre-Measurement System Validation
Parasitic Capacitance Characterization:
- Perform reference measurements on known resistive loads across operational frequency range
- Estimate system parasitic capacitances using Bayesian inference protocol (Section 4.1)
- Verify that measured capacitances are within design specifications (<50 pF per channel recommended)
Safety System Verification:
- Test current limitation circuits with simulated fault conditions
- Verify isolation measurements meet medical safety standards (>4 kV isolation)
- Confirm electrode connection integrity detection functionality
In-Operation Monitoring and Quality Assurance
Real-Time Signal Quality Metrics:
- Monitor phase coherence between injection and measurement channels
- Track signal-to-noise ratio degradation with frequency
- Implement automatic alerting when measurements deviate from expected patterns
Adaptive Compensation:
- Apply model-based correction using characterized parasitic parameters
- Adjust operating frequency if parasitic effects exceed compensation capabilities
- Document all compensation methods applied for post-processing reference
The mitigation of parasitic capacitances in high-frequency EIT operation requires a comprehensive approach spanning hardware design, signal processing, and operational protocols. Through the systematic application of the characterization methods and compensation techniques outlined in this document, researchers can achieve improved measurement accuracy while maintaining essential patient safety standards. The continued advancement of EIT technology, particularly for demanding applications such as cerebral imaging and critical care monitoring, depends on effectively addressing these fundamental electrical challenges. Future work should focus on real-time adaptive compensation techniques capable of addressing dynamic changes in electrode-tissue interface capacitance throughout prolonged monitoring sessions.
Electrical Impedance Tomography (EIT) has emerged as a powerful, non-invasive functional imaging technique with significant applications in pulmonary monitoring, cell detection, and critical care medicine. However, a fundamental challenge persists across all EIT applications: the generalization gap between high performance on standardized in-distribution (ID) data and diminished robustness on out-of-distribution (OOD) clinical cases. This gap represents a critical limitation in translating EIT methodologies from controlled research environments to diverse clinical settings where pathological variations, anatomical differences, and technical heterogeneities routinely occur.
The generalization problem in EIT manifests distinctly across its applications. In medical EIT, models trained on specific patient populations (e.g., single-center studies) often experience performance degradation when applied to different clinical sites, disease variants, or demographic groups [10]. Similarly, in single-cell EIT imaging, techniques optimized for specific cell types struggle when encountering cells with different protein expressions or subcellular structures [34]. This methodological fragility underscores the pressing need for systematic approaches that balance traditional accuracy metrics with OOD robustness guarantees.
This Application Note establishes a comprehensive framework for quantifying, analyzing, and addressing the generalization gap in EIT imaging methodology. We integrate recent advances from both EIT-specific research and broader machine learning robustness principles to provide researchers with standardized protocols for developing more reliable and clinically translatable EIT systems.
Quantitative Analysis of EIT Performance Across Domains
Comparative Performance in Clinical ARDS Assessment
Table 1: EIT versus Quantitative CT for ARDS Stratification [10]
| Parameter | Low P/F Group (P/F < 200 mmHg) | High P/F Group (200 ≤ P/F ≤ 300 mmHg) | Statistical Significance (p-value) |
|---|---|---|---|
| EIT-derived Parameters | |||
| Ventilation Ratio (VR) | Significantly elevated | Lower | < 0.05 |
| Regional Ventilation Delay Index (RVDI) | Significantly elevated | Lower | < 0.05 |
| EIT-Dead Space | Significantly elevated | Lower | < 0.05 |
| EIT-V/Q Match | Significantly reduced | Higher | < 0.05 |
| EIT-Shunt | No significant difference | No significant difference | > 0.05 |
| CT-derived Parameters | |||
| Lung Volume | No significant difference | No significant difference | > 0.05 |
| Lesion Volume | No significant difference | No significant difference | > 0.05 |
| Percentage Lesion Volume | No significant difference | No significant difference | > 0.05 |
Single-Cell EIT Imaging Performance
Table 2: Micro-EIT System Specifications for Intracellular Imaging [34]
| Parameter | Specification | Impact on Robustness |
|---|---|---|
| Electrode width | 7 μm | Enables subcellular resolution |
| Electrode spacing | 40 μm | Determines spatial sampling density |
| Electrode material | Ti (5 nm)/Au (50 nm) | Biocompatibility and signal stability |
| Number of electrodes | 8 | Limited view angles affect reconstruction |
| Azimuthal alignment | 45° intervals | Determines angular sampling |
| Signal-to-Noise Ratio | 50-200 | Critical for weak intracellular signals |
| Spatial resolution | Single-cell scale | Enables cytoplasmic/nucleoplasmic distinction |
Protocol for Robust EIT Imaging in Heterogeneous Populations
Multi-Center Validation Protocol for Clinical EIT
Objective: Establish standardized procedures for assessing and improving EIT robustness across diverse clinical populations and imaging conditions.
Materials and Equipment:
- EIT system with calibrated current sources and voltage measurement circuits
- 16-32 electrode array with consistent positioning harness
- Physiological signal references (PPG, ventilator signals)
- Data phantoms with known electrical properties
- Reference imaging modalities (CT, MRI) for validation
Procedure:
Pre-imaging Calibration
- Perform system calibration using resistive phantoms with known impedance values spanning the expected biological range (10 Ωm to 1000 Ωm)
- Verify electrode-skin contact impedance below 1 kΩ at 50 kHz for all electrodes
- Establish baseline drift compensation using reference measurements
Multi-Population Data Acquisition
- Acquire EIT data from at least 3 distinct patient cohorts with varying:
- Pathologies (e.g., ARDS, COPD, pulmonary edema)
- Demographic characteristics (age, sex, BMI)
- Clinical centers with different equipment and operators
- For each subject, collect simultaneous reference measurements:
- Acquire EIT data from at least 3 distinct patient cohorts with varying:
Domain-Shift Analysis
- Calculate performance metrics separately for each subpopulation
- Identify specific failure modes across domains using error decomposition:
- Reconstruction artifacts
- Parameter estimation errors
- Clinical classification mistakes
- Quantify distribution shift using statistical distance measures between feature representations
Robustness Optimization
- Implement domain-invariant reconstruction algorithms using adversarial training
- Apply data augmentation simulating physiological variations (edema, consolidation, atelectasis)
- Integrate Bayesian uncertainty estimation to flag low-confidence predictions [42]
Validation Metrics:
- Cross-domain variance in clinical parameters (e.g., EIT-Dead Space, EIT-V/Q Match)
- Agreement with reference standards across all subpopulations
- Failure rate consistency across domains
- Uncertainty calibration for OOD detection
Protocol for Single-Cell EIT Generalization Assessment
Objective: Ensure intracellular conductivity measurements generalize across cell types and physiological states.
Materials:
- Custom-designed micro-EIT sensor with 7 μm electrode width, 40 μm spacing [34]
- Polydimethylsiloxane (PDMS) sheet with corn-shaped hole structure (1 mm top, 70 μm bottom)
- Cell cultures with verified protein expression differences
- Frequency-difference EIT system capable of 100 fps acquisition [34]
Procedure:
Sensor Characterization and Standardization
- Verify electrode impedance consistency across all channels (< 5% variation)
- Calibrate using micro-phantoms with known conductivity values
- Establish stability metrics through repeated measurements over 24-hour period
Cross-Cell-Type Validation
- Apply identical imaging protocols to at least 3 cell types with different:
- Protein expression profiles [34]
- Morphological characteristics
- Cell cycle stages
- For each cell type, acquire:
- Brightfield and fluorescence reference images [34]
- Impedance spectra from 100 kHz to 5 MHz
- Time-series data for dynamic processes
- Apply identical imaging protocols to at least 3 cell types with different:
Frequency Selection Optimization
- Determine characteristic frequencies through equivalent circuit analysis:
- fext (extracellular dominant, ~400 kHz) [34]
- fcyt (cytoplasmic dominant, based on fitted element values)
- fnuc (nucleoplasmic dominant, based on membrane capacitance values)
- Validate frequency selection through current response simulation
- Determine characteristic frequencies through equivalent circuit analysis:
Subcellular Feature Consistency
- Reconstruct cytoplasmic (σcyt) and nucleoplasmic (σnuc) conductivity distributions
- Verify anatomical consistency with fluorescence markers
- Quantify measurement variance across cell types and physiological states
Validation:
- Statistical significance of conductivity differences between cell types
- Reconstruction accuracy compared to fluorescence reference across all cell types
- Consistency of subcellular feature identification
Visualization Frameworks for EIT Robustness Analysis
Experimental Workflow for Robust EIT Development
Computational Framework for Robust EIT
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Robust EIT Development
| Category | Item | Specifications | Function in Robustness Research |
|---|---|---|---|
| Sensor Components | Micro-EIT Electrodes | 7 μm width, 40 μm spacing, Ti/Au layers [34] | High-resolution intracellular imaging |
| 16-Electrode Array | Medical-grade stainless steel, pediatric/adult sizes | Clinical pulmonary EIT applications | |
| Calibration Standards | Resistive Phantoms | Known impedance values (10-1000 Ωm) | System calibration and performance validation |
| Anatomical Thorax Phantoms | Realistic geometry, heterogeneous conductivity | Reconstruction algorithm testing | |
| Contrast Agents | Hypertonic Saline | 5-10 ml of 10% NaCl solution [43] [32] | Pulmonary perfusion imaging validation |
| Cell Culture Materials | PDMS Microstructures | Corn-shaped hole: 1 mm top, 70 μm bottom [34] | Single-cell immobilization for micro-EIT |
| MRC-5 Human Lung Fibroblasts | Multiple protein expression variants [34] | Cross-cell-type validation | |
| Computational Tools | EIT Reconstruction Software | Multiple algorithms (GREIT, Gauss-Newton) | Method comparison and optimization |
| Domain Adaptation Framework | Adversarial training, style transfer | Explicit robustness enhancement |
Addressing the generalization gap in EIT imaging requires a systematic methodology that prioritizes robustness alongside traditional accuracy metrics. Through the protocols and analyses presented herein, researchers can now quantitatively assess and improve the OOD performance of their EIT systems across both clinical and laboratory applications.
The integration of multi-domain validation, explicit robustness optimization, and comprehensive uncertainty quantification represents a paradigm shift in EIT methodology development. As the field advances toward more complex applications including single-cell analysis and personalized medicine, these robustness-focused approaches will become increasingly critical for clinical translation and scientific impact.
Future work should focus on developing standardized robustness benchmarks for EIT, establishing domain-general reconstruction frameworks, and creating shared multi-domain datasets for systematic methodology evaluation. Only through such concerted efforts can we fully bridge the generalization gap and unlock the complete potential of EIT across its diverse applications in medical imaging and basic science.
Calibration Techniques and Signal Integrity Strategies for High-Precision Data Acquisition
Electrical Impedance Tomography (EIT) is a non-invasive imaging modality that reconstructs the internal conductivity or permittivity distribution of an object by making electrical measurements on its surface [29]. For researchers in fields ranging from pulmonary monitoring to single-cell analysis, achieving high-precision data acquisition in EIT is paramount, as the quality of the raw measurement data directly dictates the fidelity of the reconstructed images [44] [32]. This application note details essential calibration techniques and signal integrity strategies, framed within the context of EIT imaging methodology research. The protocols herein are designed to empower scientists and drug development professionals to optimize their EIT systems for maximal accuracy and reliability in high-stakes research and diagnostic applications.
Calibration Techniques for EIT Systems
Calibration is a critical step to ensure that an EIT system provides accurate and reproducible quantitative data. It involves characterizing and correcting for systematic errors inherent in the measurement hardware.
Electrode-Tissue Interface Impedance Calibration
The electrode-skin or electrode-tissue interface is a primary source of impedance and potential measurement error. A stable interface is crucial for reliable data.
- Protocol Objective: To characterize and minimize the variability and drift associated with the electrode-contact impedance.
- Materials:
- EIT system with impedance measurement capability.
- Set of surface electrodes (e.g., 16 or 32 electrodes).
- Electrode gel or saline solution.
- Test resistor with known value (e.g., 1 kΩ ± 0.1%).
- Procedure:
- Baseline Measurement: Connect the test resistor between two adjacent electrodes of the EIT system. Measure the impedance across a relevant frequency range (e.g., 10 kHz to 1 MHz). The measured value should match the known value within the system's specified accuracy.
- Electrode Preparation: Prepare the subject's skin or the phantom surface by cleaning and, if necessary, lightly abrading to reduce dead skin cells. Apply a consistent amount of electrode gel or saline solution.
- Interface Impedance Measurement: Before the main EIT experiment, use the system to measure the impedance at each electrode individually, typically by injecting a current between that electrode and a common reference or all other electrodes connected together, and measuring the resulting voltage.
- Threshold Setting: Establish a maximum acceptable impedance threshold (e.g., 1 kΩ at 50 kHz) and a maximum variation (e.g., < 10%) across all electrodes. Electrodes failing this check should be re-applied or replaced.
- Continuous Monitoring (Optional): For long-term studies, implement periodic checks of contact impedance to identify and correct for drift during the experiment.
System Gain and Phase Calibration
Variations in the analog front-end electronics (e.g., current sources, voltage amplifiers, filters) can introduce channel-dependent gain and phase offsets.
- Protocol Objective: To characterize and correct for amplitude and phase mismatches between different measurement channels of the EIT system.
- Materials:
- EIT system.
- Precision calibration phantom with known, homogeneous impedance (e.g., a saline tank with precise conductivity).
- Precision reference resistors (e.g., 100 Ω, 1 kΩ).
- Procedure:
- Homogeneous Phantom Measurement: Fill the calibration phantom with a saline solution of known conductivity (e.g., 0.9% NaCl). Connect all electrodes to the phantom.
- Data Acquisition: Collect a full set of EIT measurements (all possible injection-measurement pairs) at the operational frequency/frequencies.
- Analysis: For a given current injection pair, the measured voltages on all other electrodes should, in theory, be identical for a perfectly homogeneous domain and a perfect EIT system. Calculate a correction factor for each measurement channel to normalize the measured voltages.
- Reference Resistor Validation: Connect known reference resistors between different electrode pairs and verify that the measured impedance matches the known value after calibration factors are applied.
Frequency Response Calibration
For multi-frequency EIT (MFEIT) or frequency-difference EIT, the system's performance must be consistent across the entire operating frequency band.
- Protocol Objective: To map and correct for the frequency-dependent behavior of the EIT system.
- Procedure:
- Using a simple resistive network (e.g., a single resistor between two electrodes), measure the apparent impedance across the entire frequency spectrum of interest.
- The measured response should be flat for a pure resistor. Any deviation is attributed to the system's frequency response.
- Generate a complex-valued correction factor for each frequency to compensate for these deviations.
Table 1: Key Parameters for EIT System Calibration
| Calibration Type | Key Parameter | Target Value / Tolerance | Validation Method |
|---|---|---|---|
| Electrode-Tissue Interface | Contact Impedance | < 1 kΩ, variation < 10% across all electrodes [32] | Direct measurement via EIT system or dedicated impedance analyzer |
| System Gain/Phase | Channel Mismatch | Gain error < 0.1%; Phase error < 0.1° [45] | Measurement on homogeneous saline phantom or precision resistors |
| Frequency Response | Flatness & Phase Linearity | Deviation < 0.01% over frequency band [32] | Measurement on resistive load across frequency sweep |
Signal Integrity Strategies for EIT Data Acquisition
Signal integrity ensures that the acquired electrical signals are a true representation of the impedance distribution under investigation, free from corruption by noise or other artifacts.
Strategies for Noise Reduction
Noise can originate from various sources, including the electronics themselves, ambient electromagnetic interference, and physiological motion.
- Stochastic Noise Reduction:
- Averaging: Acquire multiple frames of data and average them. This reduces random noise but at the cost of temporal resolution.
- High-Performance Electronics: Use EIT systems with a high signal-to-noise ratio (SNR). State-of-the-art systems report measurement accuracy better than 0.01‰ and SNRs ranging from 50 to 200 for micro-EIT applications [33] [32].
- Deterministic Noise Reduction:
- Power Line Interference (50/60 Hz): Use differential measurements and driven shield cables to reject common-mode noise. Synchronize the EIT sampling clock to the power line frequency.
- Cardiogenic and Respiratory Oscillations: For non-physiological imaging (e.g., cell cultures), these are noise sources. Employ adaptive filtering or frequency-difference techniques to isolate the desired impedance signal [33].
- Circuit-Induced Noise: Modify current source architectures, such as the Howland pump, to reduce low-frequency (1/f) noise that can interfere with signals of interest. Adding a series capacitance in the positive feedback path can lower the output impedance at low frequencies, thereby reducing current noise [45].
Managing Crosstalk and Parallel Signal Acquisition
In systems with many channels, crosstalk between adjacent measurement paths can corrupt data.
- Physical Layout: Ensure proper spacing between signal-carrying traces on PCBs and within cables. Use guard traces to isolate sensitive analog lines [46] [47].
- Parallel Acquisition Systems: Modern EIT systems like the ACT 5 use fully parallel architectures where currents are applied and voltages are measured on all electrodes simultaneously [45]. This eliminates switching artifacts and allows for truly simultaneous data capture, which is crucial for imaging dynamic processes. Ensuring adequate channel-to-channel isolation in these systems is a key design priority.
Co-Acquisition of Physiological Signals (EIT/ECG)
The simultaneous acquisition of EIT and Electrocardiogram (ECG) signals provides critical timing information for interpreting pulsatile impedance changes, such as those related to cardiac output or pulmonary perfusion.
- Challenge: EIT signals are typically in the 10 kHz-1 MHz range, while ECG signals are low-frequency (0.05-150 Hz). Recovering the small ECG signal from electrodes that are also actively delivering high-frequency EIT current is difficult [45].
- Solution:
- Circuit Modification: Employ a modified Howland current source with a capacitor in the positive feedback path. This reduces the source's output impedance at low frequencies, preventing it from shunting the endogenous ECG signal to ground [45].
- Digital Signal Processing (DSP):
- The combined signal is digitized.
- A digital demodulation step (e.g., an integrate-and-dump filter) extracts the low-frequency envelope, which contains the ECG.
- Adaptive filtering can further clean the recovered ECG waveform.
- Benefit: This provides perfect temporal synchronization between the EIT images and the cardiac cycle, aiding in the interpretation of perfusion images [45].
Application Protocol: Intracellular Conductivity Mapping
The following is a detailed protocol for a specific, cutting-edge EIT application, illustrating the practical application of the above principles.
- Background: Frequency-differential EIT can be used to non-invasively map the intracellular conductivity of single cells, distinguishing subcellular structures like the cytoplasm and nucleoplasm based on their electrical properties [33].
- Objective: To reconstruct the intracellular conductivity distributions (σcyt and σnuc) of different cell lines and correlate them with protein expression levels.
Materials and Experimental Setup
Table 2: Research Reagent Solutions & Essential Materials for Micro-EIT
| Item Name | Function / Description | Example/Specification |
|---|---|---|
| Micro-EIT Sensor | Custom-designed sensor for single-cell scale measurement. | Electron-beam lithography on glass; 7 µm electrode width, 40 µm spacing [33]. |
| High-Performance EIT System | Instrument for data acquisition. | Capable of frequency-difference EIT; 16-256 channels; broad frequency range (e.g., 100 Hz – 1 MHz); high SNR (e.g., 50-200) [33] [44]. |
| Cell Culture Media | Maintain cell viability during imaging. | Standard culture media appropriate for the cell line (e.g., for MRC-5 human lung fibroblasts) [33]. |
| Contrast Agents (Optional) | For validation of EIT results. | Fluorescent dyes for specific organelle staining (e.g., for nucleus/cytoplasm) [33]. |
| Phantom Materials | For system calibration and validation. | Saline solutions of known conductivity; microfluidic channels. |
Step-by-Step Protocol
System Calibration:
- Perform all calibration procedures described in Section 2 using a microfluidic phantom with a channel filled with a saline solution of known conductivity.
- Verify the system's spatial resolution and SNR using a structured phantom.
Cell Preparation and Mounting:
- Culture the target cells (e.g., MRC-5 human lung fibroblast cell lines) directly on the micro-EIT sensor or transfer a single cell to the measurement chamber.
- Confirm cell viability and stable attachment using brightfield microscopy.
Data Acquisition:
- Setup: Place the sensor onto the microscope stage and connect it to the EIT system.
- Impedance Spectrum Measurement: Acquire EIT data across a broad frequency range (e.g., from 10 kHz to 1 MHz). The frequency sweep is critical as the impedance of the cell membrane changes, allowing the current to penetrate into the intracellular space at higher frequencies.
- Frame Rate: Use a sufficiently high frame rate (e.g., 40 fps or higher) to capture any dynamic cellular processes [32].
Image Reconstruction:
- Algorithm: Use a frequency-differential EIT reconstruction algorithm coupled with a single-cell equivalent circuit model.
- Process: The algorithm uses the impedance spectra to separate and reconstruct the conductivity distributions of the cytoplasm (σcyt) and the nucleoplasm (σnuc) [33].
Validation and Analysis:
- Correlative Microscopy: After EIT imaging, perform brightfield and fluorescence microscopy on the same cell to verify the coordinates and size of the cytoplasm and nucleoplasm.
- Quantitative Analysis: Compare the reconstructed σcyt and σnuc values across different cell types (e.g., with varying protein expressions) to identify statistically significant differences.
High-precision data acquisition in EIT is a cornerstone of reliable and quantitative imaging. It is achieved not by a single action, but through a rigorous, multi-layered approach encompassing meticulous system calibration and robust signal integrity strategies. The protocols outlined—from basic electrode impedance checks to advanced co-acquisition of EIT and ECG signals—provide a framework for researchers to optimize their experimental setups. The application of these techniques in advanced domains like intracellular conductivity mapping demonstrates their power to push the boundaries of what is possible with EIT, offering new tools for researchers and drug development professionals in their pursuit of non-invasive, functional imaging.
Benchmarking EIT Performance: Functional Validation Frameworks and Algorithmic Comparisons
Electrical impedance tomography (EIT) has emerged as a valuable functional imaging technique for monitoring regional lung ventilation in mechanically ventilated patients. Unlike anatomical imaging modalities, EIT provides real-time, radiation-free assessment of pulmonary function at the bedside, making it particularly suitable for guiding protective ventilation strategies in critical care settings [48] [49]. However, the transition of EIT from research to clinical practice has been hampered by the lack of standardized validation methodologies that adequately assess its functional performance.
Traditional validation approaches comparing EIT to anatomical reference techniques like CT and MRI face significant limitations, including mismatched temporal resolutions and inherent low spatial resolution of EIT that creates substantial partial volume effects [50] [49]. More critically, anatomical validation proves insufficiently sensitive to evaluate how well EIT detects clinically relevant functional changes in regional ventilation distribution.
This application note proposes a functional validation framework that uses well-defined physiological references to assess EIT imaging performance. By testing algorithms against known physiological responses rather than anatomical benchmarks, this approach directly validates the capability of EIT to provide clinically meaningful information for ventilation therapy guidance [51] [49].
Conceptual Framework for Functional Validation
Core Principle
The fundamental principle underlying functional validation is that EIT reconstruction algorithms should correctly reflect known physiological changes induced through controlled ventilator manipulations. This framework shifts focus from morphological accuracy to functional accuracy, ensuring that EIT-derived parameters reliably represent actual physiological phenomena relevant to clinical decision-making [49].
The backbone of this approach involves creating discrete, well-defined shifts in global and regional lung air content through manipulation of ventilator settings in experimental models. These induced changes serve as physiological references against which EIT algorithms can be quantitatively evaluated [50].
Advantages Over Anatomical Validation
- Temporal compatibility: EIT's high frame rate (typically 13-50 frames/second) aligns better with functional changes than slow anatomical imaging
- Clinical relevance: Directly tests parameters used in clinical decision-making for ventilator adjustment
- Algorithm discrimination: Reveals performance differences between reconstruction methods that anatomical validation may miss
- Physiological fidelity: Ensures EIT measurements reflect actual lung mechanics and ventilation distribution
Experimental Protocol for Functional Validation
Animal Preparation and Instrumentation
Subjects: Eight healthy pigs (body weight 25±5 kg) served as experimental subjects. The choice of porcine model reflects similarities to human thoracic anatomy and physiology [50] [49].
Anesthesia and Monitoring:
- Induction with azaperon (8 mg/kg bw) and propofol (6-12 mg/kg bw per hour)
- Continuous monitoring of heart rate, partial pressure of CO₂, arterial O₂ saturation, airway pressures, and respiratory system compliance
- Muscle paralysis with vecuronium bromide (0.1 mg/kg bw) to suppress spontaneous breathing
Ventilator Setup:
- Volume-controlled ventilation mode
- Respiratory rate: 20 breaths/minute
- Inspiration-to-expiration ratio: 1:2
- Normocapnia maintenance (end-tidal PCO₂ 35-45 mmHg)
EIT Instrumentation:
- 16 self-adhesive electrodes placed in one transverse thoracic plane at approximately the 6th intercostal space
- Goe-MF II EIT device or equivalent system
- Adjacent current injection pattern with 50 kHz, 5 mArms current
- Frame rate: 13 images/second
- Measurement duration: 60 seconds per condition [50] [49]
Experimental Design and Ventilator Manipulations
The experimental protocol induces defined physiological changes through manipulation of three ventilator parameters while maintaining constant tidal volume. This generates predictable shifts in ventilation distribution that serve as references for EIT validation [49].
Experimental Sequence:
- Baseline: FIO₂ 21% with zero end-expiratory pressure (ZEEP)
- Condition 1: FIO₂ 100% with ZEEP → induces absorption atelectasis in dependent lung regions
- Condition 2: FIO₂ 100% with PEEP 5 cmH₂O → redistributes ventilation to dependent regions
- Condition 3: FIO₂ 21% with PEEP 5 cmH₂O → reverses atelectasis effects while maintaining PEEP
- Return to baseline: FIO₂ 21% with ZEEP → confirms measurement reproducibility [49]
Data Acquisition and Analysis
EIT Data Collection:
- Continuous data acquisition during 60-second intervals for each condition
- Simultaneous recording of ventilator parameters and physiological signals
- Six complete measurement sets per animal (one for each condition)
Primary EIT-derived Parameters:
- Global tidal variation (V_T): Sum of impedance changes over the entire tidal breath
- Center of ventilation (CoV): Gravitational center of regional ventilation distribution
- Regional ventilation distribution: Quantification of ventilation in dependent vs. non-dependent lung regions
Validation Metrics: Algorithm performance is assessed by testing against expected physiological responses defined in Table 1 [49].
Performance Evaluation Framework
Physiological Reference Standards
The functional validation framework uses specific, predictable physiological responses to ventilator manipulations as reference standards. These references enable quantitative assessment of how accurately different EIT algorithms detect clinically relevant changes in ventilation distribution [49].
Algorithm Performance Assessment
Twelve EIT reconstruction algorithms were evaluated using the functional validation framework, including backprojection, GREIT, truncated singular value decomposition (TSVD), and several variants of Gauss-Newton and iterative approaches [50]. The table below summarizes the statistical performance of selected algorithms against physiological references.
Table 1: Algorithm Performance Against Physiological Reference Standards [49]
| Physiological Reference | Backprojection | GREIT | TSVD | GN (3D FEM) |
|---|---|---|---|---|
| V_T independent of PEEP | 0.224 | 0.268 | 0.512 | 0.838 |
| V_T independent of FIO₂ | 0.010 | 0.009 | 0.000 | 0.010 |
| V_T reproducible | 0.003 | 0.003 | 0.001 | 0.012 |
| CoV PEEP-dependent | 0.088 | 0.088 | 0.136 | 0.114 |
| CoV FIO₂-dependent | 0.012 | 0.012 | 0.020 | 0.020 |
Note: Table values represent p-values from statistical tests comparing algorithm performance against physiological references. Higher p-values (closer to 1.0) indicate better agreement with the reference standard for V_T tests, while lower p-values (closer to 0.0) indicate better agreement for CoV tests. V_T = tidal volume, CoV = center of ventilation, PEEP = positive end-expiratory pressure, FIO₂ = fraction of inspired oxygen, GN = Gauss-Newton, FEM = finite element model.
Key Findings from Validation Studies
Backprojection performance: Despite its vintage and ad-hoc formulation, backprojection performed surprisingly well in functional tests, supporting the validity of previous lung EIT studies using this algorithm [50] [49]
Advanced algorithm advantages: While image appearance varied considerably between algorithms, clinically relevant parameters showed less variation among advanced algorithms [49]
Functional sensitivity: The framework successfully discriminated between well-performing and suboptimal algorithms, revealing significant differences in their ability to detect physiological changes [50]
Clinical translation: Algorithms that performed well in functional validation demonstrated better potential for clinical application in guiding ventilator therapy
Research Reagent Solutions
Table 2: Essential Research Materials and Equipment for EIT Functional Validation
| Item | Specifications | Function/Purpose |
|---|---|---|
| EIT Device | Goe-MF II or equivalent; 16-electrode system, 50 kHz frequency, 5 mArms current | Data acquisition and image reconstruction |
| Electrodes | Self-adhesive (Blue Sensor BR-50-K), 16-electrode configuration | Surface electrical contact for impedance measurements |
| Ventilator | Siemens Servo 900 C or equivalent with volume-controlled mode | Precise control of ventilation parameters |
| Anesthesia System | Propofol (6-12 mg/kg/hr) and sufentanil (10 μg/kg/hr) infusion | Maintenance of stable physiological conditions |
| Monitoring Equipment | S/5 anesthesia monitoring with gas-density compensation | Continuous physiological parameter tracking |
| Experimental Subjects | Healthy pigs (25±5 kg), n=8 per study | Physiological model for ventilation studies |
| Image Reconstruction Software | EIDORS suite with multiple algorithm implementations | Algorithm testing and comparison |
Advanced Applications and Methodological Extensions
Intracellular Conductivity Imaging
Recent advances in EIT technology have enabled subcellular imaging of electrical properties in living cells. Micro-EIT systems with custom-designed sensors achieve high spatial resolution (7 μm electrode width, 40 μm spacing) and signal-to-noise ratios ranging from 50 to 200 [33]. This emerging application demonstrates:
- Non-invasive mapping of cytoplasmic and nucleoplasmic conductivity
- Discrimination of subcellular structures based on electrical properties
- Detection of variations in protein expression through conductivity differences
- Validation through brightfield and fluorescence microscopy [33]
Ventilation/Perfusion (V/Q) Monitoring
Advanced EIT applications now extend to monitoring ventilation/perfusion matching, a crucial indicator of lung function. The pulsatility method analyzes cardiac-induced impedance variations to assess pulmonary blood flow, while the hypertonic saline method uses conductivity contrast agents [32].
Key methodological considerations:
- High-performance EIT systems with measurement accuracy better than 0.01‰
- Simultaneous acquisition of ventilation and perfusion data
- Correlation with reference techniques (r = 0.7248 reported between pulsatility and saline methods)
- Capacity to detect V/Q changes during different body positions and breath-holding states [32]
Protocol Variations and Specialized Applications
- Cell detection studies: MRC-5 human lung fibroblast cell lines with different protein expressions [33]
- Perfusion imaging: Hypertonic saline (5 ml of 10% NaCl) as conductivity contrast agent [32]
- Long-term monitoring: Continuous data acquisition over 30-minute periods for stability assessment [32]
- Multi-position studies: Supine and prone positioning to assess gravitational effects [32]
The establishment of functional validation frameworks with physiological references represents a critical advancement in EIT methodology. By focusing on clinically relevant functional changes rather than anatomical correspondence, this approach provides more meaningful assessment of EIT performance for ventilation monitoring applications.
The experimental protocol detailed in this application note offers a standardized methodology for comparing reconstruction algorithms, validating new imaging techniques, and advancing EIT toward broader clinical adoption. The integration of physiological references ensures that validation outcomes directly reflect the capability of EIT to guide clinical decision-making in ventilator therapy.
As EIT technology continues to evolve, with extensions to intracellular imaging and V/Q monitoring, functional validation frameworks will remain essential for translating technical innovations into clinically useful tools for patient care.
Electrical Impedance Tomography (EIT) is a non-invasive, radiation-free imaging modality that reconstructs the internal conductivity distribution of a subject from boundary voltage measurements. It has gained significant traction in medical diagnostics and industrial monitoring due to its real-time imaging capabilities, portability, and cost-effectiveness [29]. The core challenge in EIT is solving its severely ill-posed inverse problem, which requires sophisticated computational algorithms to produce accurate and reliable images [19] [52].
This application note provides a comparative analysis of two dominant algorithmic paradigms: conventional model-based reconstruction and modern deep learning-based approaches. We evaluate their performance, scalability, and practical implementation within the context of EIT imaging methodology, providing detailed protocols for researchers and scientists engaged in method development and drug discovery research.
Background and Fundamental Principles
The EIT Inverse Problem
The EIT inverse problem involves estimating an unknown conductivity distribution (σ) within a domain (Ω) from measured boundary voltages (V). The governing equation is derived from Maxwell's equations, often simplified to the Laplace equation for low-frequency applications:
∇ · (σ(r)∇Φ(r)) = 0, r ∈ Ω
where Φ represents the internal potential distribution. The observational model is expressed as:
V = F(σ) + e
where F is the non-linear forward operator mapping conductivity to boundary voltages, and e represents measurement noise [4]. The problem's ill-posedness necessitates regularization techniques to achieve stable solutions [19] [53].
Algorithm Classifications
EIT reconstruction algorithms can be broadly categorized as follows:
- Conventional Model-Based Methods: Iterative or non-iterative approaches that incorporate physical models and explicit mathematical regularization.
- Deep Learning-Based Methods: Data-driven approaches that leverage neural networks to learn the mapping from measurement data to conductivity distributions.
- Hybrid Methods: Architectures that integrate physical models with data-driven deep learning components [19] [54] [53].
The following diagram illustrates the logical relationships and workflow between these algorithmic families in addressing the EIT inverse problem.
Comparative Performance Analysis
Quantitative Performance Metrics
The table below summarizes the key performance characteristics of conventional and deep learning-based EIT reconstruction algorithms, synthesized from recent comparative studies [19] [52] [54].
Table 1: Quantitative Comparison of EIT Reconstruction Algorithms
| Algorithm Category | Specific Methods | Reconstruction Accuracy (SSIM) | Computational Speed (Frames/s) | Noise Robustness | Generalization to OOD Data |
|---|---|---|---|---|---|
| Conventional (Non-Iterative) | Tikhonov Regularization | 0.61-0.75 | 50-100 | Moderate | Good |
| TSVD | 0.58-0.70 | 50-100 | Moderate | Good | |
| Conventional (Iterative) | Gauss-Newton | 0.70-0.82 | 1-5 | Moderate-High | Good |
| Total Variation | 0.75-0.85 | 1-5 | High | Good | |
| Deep Learning (Fully-Learned) | CNN Mapping | 0.85-0.94 | 50-200 | Low-Moderate | Poor |
| Conditional GAN | 0.88-0.95 | 30-100 | Moderate | Poor | |
| Deep Learning (Post-Processing) | D-bar + U-Net | 0.82-0.91 | 20-50 | Moderate | Moderate |
| CGAN Refinement | 0.86-0.93 | 20-50 | Moderate | Moderate | |
| Hybrid Methods | MCS-U-Net [54] | 0.90-0.96 | 10-30 | High | Moderate-Good |
| Deep Prior Embedding [53] | 0.89-0.95 | 10-20 | High | Good |
Key Performance Observations
- In-Distribution vs. Out-of-Distribution Performance: Deep learning methods significantly outperform conventional algorithms on in-distribution data (simulated ellipses dataset) but face challenges with out-of-distribution data (real-world KIT4 dataset), where hybrid methods demonstrate a more favorable balance [19].
- Computational Efficiency: Non-iterative conventional methods and fully-learned deep networks offer the highest frame rates, suitable for real-time monitoring. Iterative conventional methods are substantially slower but provide more reliable results [52].
- Noise Robustness: Traditional methods with strong regularization (e.g., Total Variation) and hybrid approaches maintain better performance under high noise conditions (e.g., 20% Gaussian noise) compared to pure deep learning methods [54].
- Edge Preservation: Total Variation and dedicated deep learning architectures (e.g., U-Net with skip connections) demonstrate superior edge preservation capabilities compared to smoothing priors like Tikhonov regularization [52] [54].
Detailed Experimental Protocols
Protocol 1: Benchmarking Reconstruction Algorithms
Objective: Systematically compare the performance of conventional, deep learning, and hybrid EIT reconstruction algorithms using standardized datasets.
Materials:
- EIT data acquisition system (e.g., 16-electrode array)
- Computational platform with GPU acceleration
- Standardized datasets (simulated ellipses, KIT4 real measurements)
Procedure:
- Data Preparation:
- Utilize three distinct datasets: simulated in-distribution data (ellipses), simulated out-of-distribution data, and real measurement data (KIT4)
- Partition data into training/validation/test sets (70/15/15 split)
- For conventional methods, use full datasets; for deep learning, use training sets for model development
Algorithm Implementation:
- Conventional Methods: Implement Tikhonov regularization, Gauss-Newton, and Total Variation methods using established libraries
- Deep Learning Methods: Train U-Net, CNN mapping, and CGAN architectures using Adam optimizer
- Hybrid Methods: Implement MCS-U-Net framework combining Modified Contrast Source with U-Net refinement [54]
Evaluation Metrics:
- Calculate Structural Similarity Index (SSIM), Relative Error, and Contrast-to-Noise Ratio (CNR)
- Measure computational time for reconstruction
- Assess robustness by adding 20% Gaussian noise to measurement data
Analysis:
- Perform statistical analysis (ANOVA) to determine significant differences between algorithms
- Generate reconstructed images for qualitative comparison
Protocol 2: Hybrid MCS-U-Net Reconstruction
Objective: Implement and validate a hybrid physics-informed deep learning approach for EIT reconstruction.
Materials:
- Simulated EIT dataset with known ground truth conductivities
- Python with PyTorch/TensorFlow and scientific computing libraries
- High-performance computing resources with GPU support
Procedure:
- Forward Model Setup:
- Create finite element model (FEM) mesh of imaging domain
- Implement complete electrode model with contact impedance
- Generate synthetic measurement data with added noise
Iterative Modified Contrast Source (MCS):
- Initialize contrast source and conductivity distribution
- Implement MCS iteration for TE and TM polarization modes
- Run for fixed iterations (e.g., 50) or until convergence
- Output preliminary conductivity estimate [54]
U-Net Refinement:
- Architecture: 4-level encoder-decoder with skip connections
- Input: MCS preliminary reconstruction
- Output: Refined conductivity distribution
- Loss function: Combined MSE and structural similarity loss
Training Protocol:
- Training epochs: 200
- Batch size: 16
- Learning rate: 1e-4 with decay schedule
- Validation: Monitor reconstruction error on holdout set
Validation:
- Compare with ground truth conductivity distributions
- Benchmark against conventional CSI and DCS methods
- Evaluate performance under different noise conditions
The Scientist's Toolkit
Essential Research Reagents and Materials
Table 2: Key Research Materials for EIT Reconstruction Studies
| Category | Item | Specification/Function | Example Applications |
|---|---|---|---|
| Data Acquisition | Multi-channel EIT System | 16-32 electrodes, simultaneous current injection/voltage measurement | Clinical pulmonary monitoring [9] |
| Electrode Arrays | Flexible PCB with Ag/AgCl electrodes, configurable geometries | Hemolysis monitoring sensor [17] | |
| Computational Tools | FEM Software | COMSOL, EIDORS for forward problem solution | Sensitivity matrix calculation [52] |
| Deep Learning Frameworks | PyTorch, TensorFlow with GPU support | U-Net, GAN implementation [54] [53] | |
| Algorithm Components | Anatomical Atlas | Pre-segmented CT/MRI templates for prior information | Infant lung imaging [9] |
| Regularization Operators | Tikhonov, Total Variation matrices | Ill-posed problem stabilization [19] [52] | |
| Validation Materials | Experimental Phantoms | Saline tanks with insulating/including targets | System characterization [17] |
| Standardized Datasets | KIT4, EIT-ellipses benchmarks | Algorithm comparison [19] |
Implementation Workflows
The following diagram illustrates the typical workflow for implementing a hybrid deep learning EIT reconstruction system, showing the integration of physical modeling with data-driven components.
This comparative analysis demonstrates that while deep learning-based EIT reconstruction algorithms achieve superior performance on in-distribution data, hybrid approaches that integrate physical models with data-driven components offer the most promising balance of accuracy, robustness, and generalizability for practical applications.
Future research should focus on improving the generalization capabilities of deep learning methods through physics-informed architectures and transfer learning strategies. The development of standardized benchmarking frameworks and large-scale diverse datasets will be crucial for advancing the field. Additionally, real-time implementation of hybrid algorithms on clinical hardware represents a critical translational challenge that requires further optimization.
For researchers in drug development and clinical applications, hybrid EIT reconstruction methods show particular promise for monitoring dynamic physiological processes, offering the reliability of model-based approaches with the enhanced resolution of deep learning.
Electrical Impedance Tomography (EIT) has emerged as a valuable non-invasive, radiation-free imaging modality for real-time bedside monitoring, particularly in critical care and pulmonary medicine [55] [1]. The core strength of EIT lies in its high temporal resolution, portability, and ability to provide dynamic functional images of internal physiology [1]. However, the inherent ill-posed nature of the EIT inverse problem presents significant challenges for achieving high spatial resolution and quantitative accuracy [56] [1]. Consequently, rigorous performance evaluation using standardized metrics and datasets is fundamental to advancing EIT methodology from research laboratories to clinical adoption. This application note provides a comprehensive framework for assessing EIT system performance, focusing on the critical pillars of image reconstruction accuracy, algorithmic adaptability, and demonstrated clinical relevance, with specific protocols for standardized evaluation.
Performance Metrics for EIT Evaluation
A multi-faceted approach is essential for thorough EIT assessment. The following metrics provide a framework for evaluating system performance across computational and clinical domains. These metrics can be quantitatively summarized from experimental and clinical studies for direct comparison.
Table 1: Core Quantitative Metrics for EIT Image Reconstruction Accuracy
| Metric Category | Specific Metric | Description | Interpretation & Benchmark |
|---|---|---|---|
| Image Fidelity | Relative Image Error | ( |\sigma{true} - \sigma{recon}| / |\sigma_{true}| ) | Lower values indicate better agreement with ground truth. |
| Structural Similarity Index (SSIM) | Measures perceptual similarity between true and reconstructed images. | Range 0-1; values closer to 1 indicate better structural preservation. | |
| Spatial Resolution | Point Spread Function (PSF) Width | Measures blurring of a point inclusion. | Smaller full-width at half-maximum (FWHM) indicates superior resolution. |
| Global Inhomogeneity (GI) Index | Quantifies ventilation distribution heterogeneity [1]. | A decreasing GI suggests more uniform ventilation and improved response to therapy. | |
| Quantitative Accuracy | Contrast-to-Noise Ratio (CNR) | Ability to distinguish an inclusion from background. | Higher values indicate better differentiation of tissue types or pathologies. |
| Conductivity Value Accuracy | Difference between reconstructed and true conductivity values. | Critical for absolute EIT; lower error indicates better quantitative performance. |
Table 2: Metrics for Clinical and Functional Relevance
| Metric Category | Specific Metric | Description | Clinical Relevance |
|---|---|---|---|
| Ventilation Monitoring | Tidal Impedance Variation (TIV) | Reflects volume changes during breathing cycle [1]. | Monitors tidal volume and ventilation distribution. |
| End-Expiratory Lung Impedance (EELI) | Reflects alveolar inflation and residual capacity at end-expiration [1]. | Tracks lung recruitment and derecruitment. | |
| Ventilation Distribution | Center of Ventilation (CoV) | Identifies the central position of airflow [1]. | A shift toward dorsal regions often indicates successful recruitment. |
| Regional Ventilation Delay (RVD) | Indicates delays in regional ventilation [1]. | Helps identify airway obstruction and asynchronous filling. | |
| Algorithmic Performance | Reconstruction Time | Time to produce one image frame. | Must be <100 ms for real-time bedside monitoring [1]. |
| Noise Robustness | Change in image quality with added measurement noise. | Essential for reliability in electrically noisy clinical environments. |
Experimental Protocols for Standardized Evaluation
Protocol 1: Phantom-Based Validation of Reconstruction Accuracy
Objective: To quantitatively assess the spatial resolution and quantitative accuracy of an EIT reconstruction algorithm using a well-characterized phantom.
Materials:
- EIT system with data acquisition hardware.
- Standardized 2D or 3D EIT phantom (e.g., 3D printed with conductive material [57] or salt bath phantom).
- Data processing workstation with reconstruction software.
Methodology:
- Phantom Setup: Utilize a phantom with known, stable conductivity contrasts. 3D printed phantoms, where resistivity is controlled via infill percentage, are recommended for their high spatial resolution and stability [57].
- Data Acquisition: Place the electrode belt according to the phantom's specification. Collect voltage measurement data ( V ) for all specified current injection patterns.
- Image Reconstruction: Reconstruct the conductivity distribution ( \rho ) using the algorithm under test, minimizing the objective functional ( E(\rho) = \|V - U(\rho)\|^2_2 ), where ( U(\rho) ) are the predicted voltages [56].
- Metric Calculation: Compare the reconstructed image ( \sigma{recon} ) to the ground truth phantom geometry ( \sigma{true} ).
- Calculate the Relative Image Error and SSIM (Table 1).
- For a localized inclusion, measure the PSF width.
- Calculate the CNR between the inclusion and the background.
- Robustness Testing: Repeat steps 2-4 with varying levels of synthetic Gaussian noise added to the voltage measurements ( V ) to assess noise robustness.
Protocol 2: Clinical Benchmarking on In-Silico Datasets
Objective: To evaluate the algorithm's performance under physiologically realistic conditions and its ability to inform clinical decisions.
Materials:
- Computational human thorax model (finite element mesh).
- Simulated pathological scenarios (e.g., pneumothorax, regional collapse, ARDS).
- Library of EIT indices calculation scripts (e.g., for GI, CoV, RVD).
Methodology:
- Forward Modeling: Generate simulated boundary voltage data ( V{sim} ) for a range of known pathological conductivity distributions ( \sigma{path} ) using the forward model.
- Blinded Reconstruction: Provide ( V{sim} ) (with added noise) to the EIT reconstruction algorithm to obtain ( \sigma{recon} ).
- Functional Index Extraction: From ( \sigma_{recon} ), calculate key clinical EIT indices (Table 2).
- Global Inhomogeneity (GI): Calculate the sum of absolute deviations between tidal image and the global median value [1].
- Center of Ventilation (CoV): Determine the ventral-to-dorsal center of gravity of the tidal impedance variation.
- Tidal Impedance Variation (TIV): Quantify the sum of impedance changes within the lung region over a breath.
- Validation: Correlate the extracted indices from ( \sigma{recon} ) with the known "ground truth" values from ( \sigma{path} ). Evaluate the algorithm's sensitivity and specificity in detecting specific pathologies like pneumothorax.
Protocol 3: Computational Performance and Adaptability Assessment
Objective: To benchmark the computational efficiency and adaptive capabilities of novel reconstruction algorithms.
Materials:
- High-performance computing node.
- Standardized dataset (phantom or in-silico).
- Algorithms for comparison (e.g., traditional, deep learning-based, quantum-assisted).
Methodology:
- Baseline Profiling: For each algorithm, measure the average reconstruction time per frame and memory usage across the standardized dataset.
- Adaptive Mesh Refinement Test: For algorithms supporting adaptive meshing, start with a coarse mesh and refine elements with high conductivity gradients ( \Delta\rhoi = \sum{\text{edges}} |\rhoi - \rhoj|^2 / l_{ij} ) for a smoother reconstruction and better spatial resolution [56]. Document the improvement in image error versus computational cost.
- Algorithm-Specific Workflows:
- Adaptive Kaczmarz: Evaluate the convergence speed by monitoring the solution update ( \rho{k,i} = \rho{k,i-1} + a{k,i}J{k,i}^T(J{k,i}J{k,i}^T + \lambda{k,i}I)^{-1}[Vi - Ui(\rho{k,i-1})] ) across iterations [56].
- AI/Quantum-Assisted Models: For frameworks like QuantEIT, document the parameter count (e.g., 0.2% of classical DL models) and assess reconstruction quality versus model complexity [58].
The following diagram illustrates the logical workflow integrating these three evaluation protocols into a comprehensive assessment framework for an EIT system.
The Scientist's Toolkit: Key Research Reagents & Materials
Successful EIT research and development relies on a suite of specialized hardware, software, and experimental materials. The following table details essential components of the EIT researcher's toolkit.
Table 3: Essential Research Reagents and Materials for EIT Methodology Research
| Item | Function & Application | Key Specifications |
|---|---|---|
| 3D Printed Conductive Phantom [57] | Provides a stable, geometrically precise platform for validating image reconstruction accuracy and spatial resolution. | - Material: Conductive PLA (e.g., Protopasta).- Control: Resistivity controlled via infill percentage. |
| Active Electrode System with SoC/ASIC [1] | Minimizes cable-induced artifacts and improves signal fidelity for high-quality data acquisition. | - Architecture: System-on-Chip (SoC) or Application-Specific Integrated Circuit (ASIC).- Feature: Integrated preamplifiers. |
| Multi-Frequency EIT Hardware [1] | Enables tissue characterization based on impedance spectroscopy, enhancing contrast for differentiating tissues. | - Frequency Range: Typically from kHz to MHz. |
| EIDORS Software [1] | Open-source environment for EIT image reconstruction and simulation, facilitating algorithm development and testing. | - Functions: Forward problem solving, inverse problem algorithms, and mesh generation. |
| Standardized FEM Meshes | Provides a common ground for fair comparison between different reconstruction algorithms. | - Types: Both forward (fine) and inverse (coarse) meshes [56]. |
| Hypertonic Saline Contrast Agent [55] | A bolus of this agent temporarily alters blood conductivity, allowing EIT to assess pulmonary perfusion at the bedside. | - Application: Used during a brief respiratory pause to map lung blood flow. |
Visualization of a Clinical Benchmarking Workflow
The protocol for clinical benchmarking (Protocol 2) involves a multi-stage process from model creation to clinical correlation. The workflow below details the specific steps for validating algorithms against clinically relevant metrics.
The rigorous, multi-modal evaluation framework outlined in this application note—encompassing phantom validation, clinical benchmarking, and computational profiling—provides a robust methodology for advancing EIT imaging. By standardizing performance metrics and experimental protocols, researchers can objectively compare novel algorithms, hardware innovations, and AI-integrated approaches. This is crucial for translating EIT from a promising research tool into a reliable modality for clinical decision-making, ultimately fulfilling its potential to enable personalized, predictive critical care. Future work should focus on establishing large, publicly available standardized datasets and benchmarks to further accelerate innovation in the field.
The Role of Hybrid Methods in Achieving an Optimal Balance Between Accuracy and Generalizability
Electrical Impedance Tomography (EIT) is a non-invasive, radiation-free functional imaging technique that reconstructs the internal conductivity distribution of an object by applying a safe alternating current to surface electrodes and measuring the resulting boundary voltages [29]. The core inverse problem in EIT—inferring conductivity from voltage measurements—is severely ill-posed and non-linear, requiring advanced computational approaches for reliable image reconstruction [19] [4].
Traditional image reconstruction methods can be broadly categorized into model-based approaches (e.g., sparsity regularization, regularized Gauss-Newton iteration) and fully-learned deep learning techniques. While model-based methods generally exhibit better generalization to unseen data types due to their foundation in physical principles, they often lack the accuracy and resolution of data-driven approaches. Fully-learned methods, typically employing deep neural networks, demonstrate superior performance on data similar to their training sets but frequently face challenges in generalizing to out-of-distribution or real-world data that differs from their training simulations [19].
This application note explores how hybrid reconstruction methods, which integrate deep learning architectures with model-based physical constraints, create a synergistic effect that balances the strengths of both approaches. These methods have demonstrated a "good balance of accuracy and adaptability" across simulated and clinical datasets [19].
Quantitative Performance Analysis of EIT Reconstruction Methods
The performance of various EIT reconstruction methodologies has been systematically evaluated across multiple datasets, including simulated data of ellipses, an out-of-distribution simulated dataset, and the KIT4 dataset containing real-world measurements [19]. The following tables summarize key quantitative findings, providing a comparative analysis of method performance and clinical parameter utility.
Table 1: Comparative Analysis of EIT Reconstruction Method Performance on Different Data Types
| Method Category | Key Characteristics | In-Distribution Data Performance | Out-of-Distribution Data Performance | Clinical Application Strengths |
|---|---|---|---|---|
| Fully-Learned Methods | End-to-end deep neural networks; minimal physical models | High accuracy and resolution [19] | Limited generalization; performance degradation [19] | Excellent for specialized, controlled applications |
| Model-Based Methods | Physics-based regularization; traditional inversion | Moderate, consistent accuracy [19] | Moderate, consistent accuracy [19] | Reliable for diverse patient populations and conditions |
| Hybrid Methods | Deep learning integrated with physical models | High accuracy, comparable to fully-learned [19] | Good generalization; maintains robust performance [19] | Optimal for clinical use with varying and unpredictable patient physiology |
Table 2: Clinical Validation of EIT Parameters in ARDS Stratification Post-Lung Transplantation (n=21) [10] [59]
| Parameter | Description | Low P/F Group (P/F <200 mmHg) | High P/F Group (P/F 200-300 mmHg) | Statistical Significance (p-value) | Correlation with Reference Standard |
|---|---|---|---|---|---|
| EIT-Dead Space | EIT-based assessment of non-perfused ventilation | Significantly elevated [10] [59] | Lower levels | Significant | Substantial agreement with ventilator-measured dead space fraction [10] [59] |
| EIT-V/Q Match | EIT-based ventilation/perfusion matching | Significantly reduced [10] [59] | Higher levels | Significant | N/A |
| RVDI | Regional Ventilation Delay Index | Significantly elevated [10] [59] | Lower levels | Significant | Indicator of asynchronous ventilation |
| Quantitative CT Parameters (Lesion volume, percentage lesion volume) | CT-based structural lesion assessment | No significant difference [10] [59] | No significant difference | Not Significant | Poor correlation with physiological impairment in this cohort |
Detailed Experimental Protocols
Protocol 1: Hybrid EIT Reconstruction for Pulmonary Imaging
This protocol outlines the procedure for implementing a hybrid EIT reconstruction method for monitoring pulmonary function in critically ill patients, combining statistical shape models with deep learning components.
Materials and Equipment
- EIT Device: High-performance EIT system with measurement accuracy better than 0.01‰ and frame rate of at least 40 fps [32]
- Electrode Belt: 16- or 32-electrode belt with appropriate size selection based on half-chest perimeter [25]
- Contact Agent: Ultrasound gel or device-specific contact agent to improve electrode-skin contact [25]
- Reference Electrode: If required by device, for placement on abdomen or shoulder [25]
- Physiological Monitors: Synchronized recording equipment for respiratory waveforms, esophageal pressure, and ECG [25]
Procedure
Patient Preparation and Belt Placement
- Shave chest hair if necessary and clean skin with alcohol [32]
- Measure half-chest perimeter from sternum to spine to select appropriate belt size [25]
- Position electrode belt transversely between the 4th and 5th intercostal space in the parasternal line, ensuring a transverse plane orientation [25]
- Apply contact agent to electrodes and secure belt with consistent tension
- Place reference electrode 15-20 cm from belt plane if required [25]
System Calibration and Signal Verification
- Initiate EIT device calibration according to manufacturer specifications
- Record baseline signal for at least 1 minute to ensure stability [25]
- Verify signal quality through real-time impedance waveform display
- Check for negative inspiratory impedance changes that may indicate artifacts or pathological conditions [25]
Data Acquisition and Synchronization
Hybrid Image Reconstruction
- Extract raw voltage measurements from acquired data
- Apply traditional reconstruction algorithm (e.g., regularized Gauss-Newton) to generate initial conductivity distribution [19]
- Process initial reconstruction through deep neural network trained on paired simulated and clinical data [19]
- Incorporate statistical shape constraints for thoracic anatomy using pre-trained shape models [60]
- Apply dynamic regularization framework that adapts based on data fidelity and shape prior agreement [60]
Parameter Calculation and Analysis
Protocol 2: Intracellular Conductivity Imaging for Cell Detection
This protocol details the application of frequency-differential EIT with equivalent circuit-based reconstruction for non-invasive intracellular conductivity mapping at the single-cell level.
Materials and Equipment
- Micro-EIT Sensor: Custom-designed sensor fabricated on glass substrate with 7 μm electrode width and 40 μm spacing via electron beam lithography [33]
- Cell Culture System: Platform for maintaining living cells during imaging
- Frequency Generator: System capable of delivering multiple excitation frequencies
- Signal Processing Unit: High-precision amplifier and data acquisition system
Procedure
Sensor Preparation and Cell Positioning
- Sterilize micro-EIT sensor using appropriate method (UV light, ethanol)
- Seed target cells (e.g., MRC-5 human lung fibroblast cell lines) onto sensor surface [33]
- Allow cells to adhere and stabilize under controlled culture conditions
Multi-Frequency Impedance Measurement
Frequency-Differential Data Processing
Hybrid Reconstruction with Circuit Constraints
- Implement traditional inverse solution for baseline conductivity distribution
- Incorporate equivalent circuit model as physical constraint during reconstruction [33]
- Apply deep learning component for noise reduction and resolution enhancement
- Reconstruct separate conductivity distributions for cytoplasm (σcyt) and nucleoplasm (σnuc) [33]
Validation and Analysis
Visualization of Hybrid EIT Methodology
Workflow Diagram: Hybrid EIT Reconstruction Framework
Hybrid EIT Reconstruction Workflow: This diagram illustrates the integration of model-based reconstruction with statistical shape priors and deep learning components, demonstrating how hybrid methods leverage both physical constraints and data-driven enhancement.
Signaling Pathway: Ventilation/Perfusion Assessment in ARDS
V/Q Mismatch Pathway in ARDS: This diagram outlines the pathophysiological pathway from alveolar damage to impaired gas exchange, highlighting how EIT-derived parameters quantitatively track the functional progression of ARDS.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Hybrid EIT Methodology
| Item | Specifications | Function/Application | Representative Use Cases |
|---|---|---|---|
| High-Performance EIT System | Measurement accuracy >0.01‰, Frame rate: 40-100 fps [32] | Core data acquisition for voltage measurement | Pulmonary monitoring in ICU [25] |
| Micro-EIT Sensor | 7 μm electrode width, 40 μm spacing, Glass substrate [33] | Single-cell scale impedance measurements | Intracellular conductivity imaging [33] |
| Electrode Belts | 16 or 32 electrodes, Multiple sizes based on chest perimeter [25] | Surface contact for current injection/voltage measurement | Clinical thoracic EIT [25] |
| Hypertonic Saline Contrast | 5-10 ml of 10% NaCl solution [32] | Bolus injection for perfusion imaging | V/Q matching assessment [32] |
| Contact Agents | Ultrasound gel, Crystalloid fluids, Water [25] | Improve electrode-skin contact impedance | Standard clinical EIT monitoring [25] |
| Statistical Shape Models | Derived from CT/MRI databases [60] | Anatomical constraints for reconstruction | Hybrid reconstruction algorithms [60] |
| Deep Learning Frameworks | Custom neural networks for EIT reconstruction [19] [4] | Image enhancement and noise reduction | Hybrid method implementation [19] |
| Equivalent Circuit Models | Single-cell circuit parameters [33] | Constraining reconstruction for cellular EIT | Intracellular conductivity mapping [33] |
Hybrid EIT methods represent a significant advancement in electrical impedance tomography by successfully integrating the generalization capacity of model-based approaches with the high accuracy of deep learning techniques. The protocols and analyses presented demonstrate their superior performance across diverse applications—from single-cell intracellular imaging to clinical ARDS management—where they provide an optimal balance between reconstruction fidelity and adaptability to novel data types. As EIT technology continues to evolve, further refinement of these hybrid frameworks, particularly through improved neural network architectures and enhanced physical modeling, will likely expand their clinical utility and establish them as the standard methodology for robust EIT image reconstruction across biomedical applications.
Conclusion
The field of Electrical Impedance Tomography is undergoing a significant transformation, driven largely by the integration of deep learning and advanced hardware design. While learned reconstruction methods demonstrate superior performance for in-distribution data, hybrid approaches that combine physical models with data-driven learning currently offer the most promising balance of accuracy and adaptability for real-world clinical and preclinical use. Future directions must focus on improving the generalizability of deep learning models across diverse patient populations and conditions, the continued miniaturization and optimization of hardware for specific applications like wearable monitors and single-cell analysis, and the establishment of standardized, functionally-grounded validation protocols. The convergence of high-resolution micro-EIT for drug discovery and robust clinical EIT for patient monitoring positions EIT as a pivotal tool for the future of personalized medicine and translational research.
References
- 1. Electrical impedance tomography: from technical innovations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12444238/]
- 2. Exploratory study of a multifrequency EIT-based method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10457004/]
- 3. Electrical Impedance Tomography – Recent Applications and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8667811/]
- 4. Advances of deep learning in electrical impedance ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.1019531/full]
- 5. Electrical impedance tomography in neonates: a review [https://pubmed.ncbi.nlm.nih.gov/39987341/]
- 6. Learning-Enhanced Variational Regularization for ... [https://www.sciencedirect.com/science/article/abs/pii/S0021999125005923]
- 7. A Operator learning meets inverse problems [https://arxiv.org/html/2508.20207v1]
- 8. Information-distilled physics informed deep learning for ... [https://www.nature.com/articles/s44172-025-00476-5]
- 9. Use of an anatomical atlas in real-time EIT reconstructions ... [https://www.nature.com/articles/s41598-025-15543-2]
- 10. EIT Outperforms Quantitative CT in Stratifying ARDS Severity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12612634/]
- 11. Electrical impedance tomography (EIT) for quantification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4722629/]
- 12. Past, present, and future of electrical impedance ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1486789/full]
- 13. Continuous Electrode Models and Application of Exact ... [https://www.mdpi.com/2079-9292/13/1/66]
- 14. Applications of Electrical Impedance Tomography in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10258591/]
- 15. Omics approach to chest electrical impedance tomography ... [https://annalsofintensivecare.springeropen.com/articles/10.1186/s13613-025-01514-3]
- 16. Electrical impedance tomography-based temporal signals ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1660948/full]
- 17. Development and evaluation of an electrical impedance ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267025002065]
- 18. Optimized Lattice-Structured Flexible EIT Sensor for Tactile ... [https://arxiv.org/html/2505.00161v2]
- 19. Deep Learning Based Reconstruction Methods for ... [https://arxiv.org/abs/2508.06281]
- 20. Advances of deep learning in electrical impedance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9794741/]
- 21. Deep Learning Based Reconstruction Methods for ... [https://arxiv.org/html/2508.06281v1]
- 22. Learned enclosure method for experimental EIT data [https://www.aimsciences.org/article/doi/10.3934/ammc.2025008]
- 23. Kuopio tomography challenge 2023 – electrical impedance... [https://www.aimsciences.org/article/doi/10.3934/ammc.2024009]
- 24. Intracranial Electrical Impedance Tomography: A Method of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3783592/]
- 25. Electrical impedance tomography monitoring in adult ICU ... [https://ccforum.biomedcentral.com/articles/10.1186/s13054-024-05173-x]
- 26. Electrical impedance tomography in neonates: a review [https://www.nature.com/articles/s41390-025-03929-x]
- 27. Recommendations for lung ventilation and perfusion ... [https://www.sciencedirect.com/science/article/pii/S2589537025005085]
- 28. A modular open-source platform for electrical impedance ... [https://www.sciencedirect.com/science/article/pii/S2468067225000768]
- 29. Electrical Impedance Tomography in Medical Imaging [https://www.atlantis-press.com/proceedings/iciaai-25/126015341]
- 30. A new modular semi-parallel EIT system for medical ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809417301647]
- 31. Design of a Wearable Parallel Electrical Impedance ... [https://arxiv.org/html/2505.19146v1]
- 32. Feasibility of the dynamic EIT technique for non-invasive ... [https://www.nature.com/articles/s41598-025-91660-2]
- 33. Electrical impedance tomography (EIT)-based intracellular ... [https://pubs.rsc.org/en/content/articlelanding/2025/lc/d5lc00466g]
- 34. based intracellular conductivity imaging for non-invasive cell ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00466g]
- 35. Electrical Impedance Tomography: From the Traditional ... [https://www.mdpi.com/1424-8220/23/3/1182]
- 36. Intelligent in-cell electrophysiology [https://www.nature.com/articles/s41467-024-55571-6]
- 37. Electrical impedance tomography (EIT)-based intracellular ... [https://pubmed.ncbi.nlm.nih.gov/41059550/]
- 38. 12. Design Tradeoffs [https://computationstructures.org/notes/tradeoffs/notes.html]
- 39. 3 Modern Trade-offs in Embedded Systems Design [https://www.designnews.com/embedded-systems/3-modern-trade-offs-in-embedded-systems-design]
- 40. Parasitic Effects on Electrical Bioimpedance Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC9693567/]
- 41. Parasitic capacitances estimation of an Electrical ... [https://www.sciencedirect.com/science/article/abs/pii/S0263224121000270]
- 42. On the Out of Distribution Robustness of Foundation ... [https://arxiv.org/abs/2311.11096]
- 43. Feasibility of the dynamic EIT technique for non-invasive ... [https://pubmed.ncbi.nlm.nih.gov/41023117/]
- 44. Electrical Impedance Tomography (EIT) | Scalable Imaging [https://sciospec.com/eit/]
- 45. Simultaneous Acquisition of EIT and ECG Signals on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11928262/]
- 46. Signal Integrity: Problems and Solutions [https://www.ema-eda.com/ema-resources/blog/signal-integrity-problems-and-solutions-emd/]
- 47. Signal Integrity Analysis and PCB Design for High-Speed ... [https://rfpcb.org/signal-integrity-analysis-and-pcb-design-for-high-speed-digital-analog-mixed-circuits/]
- 48. Electrical impedance tomography (EIT) in applications ... [https://pubmed.ncbi.nlm.nih.gov/10847187/]
- 49. Functional Validation and Comparison Framework for EIT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4128601/]
- 50. Functional Validation and Comparison Framework for EIT ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0103045]
- 51. Functional validation and comparison framework for EIT ... [https://pubmed.ncbi.nlm.nih.gov/25110887/]
- 52. Comparing Image Reconstruction Methods with Electrical ... [https://www.siam.org/publications/siam-news/articles/comparing-image-reconstruction-methods-with-electrical-impedance-tomography-data/]
- 53. Deep prior embedding method for Electrical Impedance ... [https://www.sciencedirect.com/science/article/abs/pii/S0893608025002989]
- 54. Deep Learning-Enhanced Iterative Modified Contrast ... [https://www.mdpi.com/2227-7390/13/22/3711]
- 55. Electrical Impedance Tomography, Artificial Intelligence ... [https://www.mdpi.com/2075-4426/14/7/677]
- 56. Adaptive Techniques in Electrical Impedance Tomography ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5595150/]
- 57. A novel two-dimensional phantom for electrical impedance ... [https://www.nature.com/articles/s41598-024-52696-y]
- 58. QuantEIT: Ultra-Lightweight Quantum-Assisted Inference ... [https://arxiv.org/html/2507.14031v1]
- 59. EIT Outperforms Quantitative CT in Stratifying ARDS ... [https://pubmed.ncbi.nlm.nih.gov/41229381/]
- 60. Dynamic chest Electrical Impedance Tomography with ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809425000448]