Biomaterials in Tissue Engineering: From Scaffold Design to Clinical Translation and Future Directions
This article provides a comprehensive overview of the pivotal role of biomaterials in tissue engineering, tailored for researchers, scientists, and drug development professionals.
Biomaterials in Tissue Engineering: From Scaffold Design to Clinical Translation and Future Directions
Abstract
This article provides a comprehensive overview of the pivotal role of biomaterials in tissue engineering, tailored for researchers, scientists, and drug development professionals. It explores the foundational principles of biomaterial science, including the properties of natural, synthetic, and smart polymers. The scope extends to methodological advances in fabrication techniques like 3D and 4D printing, detailed applications across key tissues, and the integration of stem cells. It further addresses critical challenges in immunogenicity, manufacturing, and regulation, and concludes with an analysis of clinical validation, market trends, and future pathways for next-generation biomaterials in regenerative medicine.
The Foundation of Regeneration: Core Principles and Classes of Biomaterials
Biomaterials represent an evolving field at the intersection of materials science, biology, and engineering, serving as a cornerstone for many breakthroughs in healthcare and life sciences [1]. These materials are specifically engineered to interact with biological systems for medical or therapeutic purposes, playing a pivotal role in tissue engineering and regenerative medicine [1]. The fundamental goal of tissue engineering is to merge biology, engineering, and medicine to craft functional replacement tissues and organs [2]. This interdisciplinary approach involves combining biomaterials, cells, and growth factors to regenerate damaged tissues, where cells are sourced from the patient or a donor, combined with a scaffold to provide structural support, and nurtured to form three-dimensional tissues [2].
The performance and success of biomaterials in medical applications depend on their ability to meet specific requirements based on their intended function [1]. These requirements can be categorized into three essential properties: biocompatibility, biodegradability, and bioactivity. This triad of properties collectively determines whether a biomaterial can perform effectively in tissue engineering applications, ensuring it supports rather than hinders the regenerative process. Understanding these properties is critical to ensuring that biomaterials can perform their intended function within the human body without causing harm while actively promoting tissue regeneration [1]. As the field advances, these core properties guide the development of next-generation biomaterials that increasingly mimic the natural extracellular matrix (ECM) - the highly sophisticated biological framework that actively orchestrates fundamental cellular processes through integrated biomechanical and biochemical cues [3].
Defining Biocompatibility: From Phenomenology to Host Integration
The Evolution of a Critical Concept
Biocompatibility stands as the defining characteristic of any biomaterial [1]. The term has undergone significant conceptual evolution since its early applications. The first widely accepted definition was ratified at a biomaterials consensus conference in Chester, England in 1986 and published in 1987: "the ability of a material to perform with an appropriate host response in a specific application" [4]. This definition was reaffirmed in recent conferences on biomaterial definitions despite its limitations in suggesting assessment methods or improvement strategies [4].
A more contemporary definition emerging from interdisciplinary tissue engineering approaches reframes biocompatibility as "the ability of tissue engineering scaffold or matrix to support the appropriate cellular activity, including the facilitation of molecular and mechanical signaling systems, to optimize tissue regeneration, without eliciting any undesirable local or systemic response in the eventual host" [5]. This evolution in terminology reflects a shift from passive acceptance to active integration, emphasizing the dynamic role biomaterials play in supporting cellular functions essential for tissue regeneration.
Assessment Methodologies and Standards
The assessment of biocompatibility has evolved from early phenomenological observations to standardized toxicological testing. Contemporary biocompatibility evaluation typically follows International Organization for Standardization (ISO) guidelines, particularly the ISO-10993 series, which involves extracting "migratable chemical moieties" from materials and assessing their effects on cells in culture and living research animals [4]. These tests evaluate local and systemic effects in vivo, with implantation studies examining the tissue response over specified periods.
A critical aspect of biocompatibility assessment in tissue engineering involves evaluating the peri-material reaction. In response to host response, implanted material is typically layered with macrophages on the inner zone and fibroblasts and connective tissue on the outer zone [5]. The magnitude of this peri-material reaction and subsequent inflammatory layer formation serves as an index of biocompatibility [5]. For bone tissue engineering applications, biocompatibility also influences the scaffold's osteoinductive and osteoconductive nature [5].
Table 1: Key Standards for Assessing Biocompatibility According to ISO 10993
| Standard Part | Focus Area | Key Assessment Parameters |
|---|---|---|
| ISO 10993-1 | Evaluation and testing within a risk management process | Provides framework for biological evaluation of medical devices |
| ISO 10993-3 | Tests for genotoxicity, carcinogenicity, and reproductive toxicity | Identifies potential mutagenic and carcinogenic effects |
| ISO 10993-4 | Selection of tests for interactions with blood | Hemocompatibility including thrombosis, coagulation, platelets |
| ISO 10993-5 | Tests for in vitro cytotoxicity | Cell culture tests using mammalian cells |
| ISO 10993-6 | Tests for local effects after implantation | Tissue response to implanted materials in animal models |
| ISO 10993-10 | Tests for skin sensitization and irritation | Identification of potential sensitizers and irritants |
| ISO 10993-11 | Tests for systemic toxicity | Potential toxic effects beyond the implantation site |
The Foreign Body Response and Contemporary Challenges
The introduction of any biomaterial into living tissue triggers a complex sequence of events known as the foreign body response (FBR). This process begins with protein adsorption to the material surface within seconds of implantation, followed by inflammatory cell recruitment, and potentially culminating in the formation of a fibrous capsule that walls off the implant [4]. The FBR represents a significant challenge for many medical devices, as the resulting fibrotic scar can impede device function - inhibiting electrical communication for electrodes, slowing drug transport for delivery systems, impeding analyte diffusion for sensors, and causing deformation or pain in cosmetic implants [4].
Current research focuses on developing "pro-healing" biomaterials that can diminish or eliminate the scar capsule and lead to vascularized, reconstructive healing [4]. These advanced materials represent the next frontier in biocompatibility, moving beyond mere tolerance to active integration with host tissues.
Biodegradability: Programmed Material Lifecycle in Tissue Regeneration
Fundamental Principles and Mechanisms
Biodegradability is a desirable property for biomaterials intended for temporary applications, such as tissue scaffolds or drug delivery systems [1]. Biodegradable materials are designed to break down naturally within the body, either being absorbed or excreted once they have served their purpose. The rate of degradation can be controlled by adjusting the material's composition and structure, ensuring that the biomaterial remains functional for the necessary period before dissolving without causing harm [1].
In tissue engineering, biodegradable scaffolds provide structural support for growing tissues before gradually being replaced by the body's natural tissue [1]. This temporary support function is crucial for guiding tissue regeneration, as the scaffold must maintain mechanical integrity during the initial healing phase while progressively transferring load-bearing responsibilities to the newly formed tissue. The degradation process typically occurs through hydrolysis, enzymatic activity, or cellular processes, with the breakdown products needing to be non-toxic and readily metabolized or excreted by the body.
Material Classes and Degradation Profiles
Various material classes exhibit biodegradable properties suitable for tissue engineering applications. These include natural polymers (e.g., collagen, silk, alginate), synthetic polymers (e.g., polylactic acid [PLA], polyglycolic acid [PGA], polycaprolactone [PCL]), and certain ceramics (e.g., calcium phosphates). Each class offers distinct degradation profiles and mechanical properties that can be tailored to specific applications.
Natural polymers generally demonstrate higher bioactivity and cellular recognition but may present challenges in controlling degradation rates and mechanical properties. Synthetic polymers offer greater control over degradation kinetics and mechanical behavior but may lack inherent bioactivity. Hybrid approaches combining natural and synthetic materials seek to leverage the advantages of both systems.
Table 2: Degradation Profiles of Common Biodegradable Polymers in Tissue Engineering
| Polymer | Degradation Mechanism | Typical Degradation Time | Key Applications | Degradation Products |
|---|---|---|---|---|
| Collagen | Enzymatic degradation | 2 weeks - 6 months | Skin regeneration, soft tissue repair | Amino acids |
| Polyglycolic Acid (PGA) | Hydrolysis | 2-4 months | Sutures, tissue scaffolds | Glycolic acid |
| Polylactic Acid (PLA) | Hydrolysis | 6 months - 2 years | Bone fixation devices, scaffolds | Lactic acid |
| Polycaprolactone (PCL) | Hydrolysis | 2-3 years | Long-term implants, drug delivery | Caproic acid |
| Poly(lactic-co-glycolic acid) (PLGA) | Hydrolysis | 1-6 months (ratio-dependent) | Drug delivery, temporary scaffolds | Lactic and glycolic acids |
| Chitosan | Enzymatic degradation | 2 weeks - 3 months | Wound healing, cartilage repair | Glucosamine |
Experimental Protocols for Degradation Analysis
Standardized protocols exist for evaluating the degradation behavior of biomaterials in simulated physiological conditions. These typically involve incubating material samples in phosphate-buffered saline (PBS) at pH 7.4 and 37°C, with or without enzymatic additives to simulate in vivo conditions more accurately. Key parameters monitored include:
- Mass Loss Measurement: Samples are periodically removed, dried, and weighed to calculate percentage mass loss over time.
- Molecular Weight Changes: Gel permeation chromatography (GPC) tracks reductions in polymer molecular weight.
- Mechanical Property Decay: Tensile testing, compression testing, or dynamic mechanical analysis monitors the decline in mechanical integrity.
- Morphological Changes: Scanning electron microscopy (SEM) visualizes surface erosion or bulk degradation patterns.
- pH Monitoring: Changes in medium pH indicate acidic or alkaline degradation products.
The degradation profile must be carefully matched to the specific tissue regeneration timeline. For example, bone regeneration scaffolds typically require longer degradation periods (3-6 months) to support mechanical function during healing, while skin regeneration scaffolds may degrade more rapidly (2-4 weeks) as new tissue forms.
Bioactivity: Beyond Passive Function to Biological Dialogue
Defining Bioactive Interactions
Bioactivity refers to the ability of a material to interact with biological tissues in a way that promotes healing, cell attachment, or regeneration [1]. Bioactive materials can stimulate specific biological responses, such as the growth of new tissue or the healing of wounds [1]. Unlike merely biocompatible materials that passively avoid harmful effects, bioactive materials actively participate in biological processes, influencing cellular behavior through controlled interactions at the material-tissue interface.
The development of bioactive materials represents a significant advancement in biomaterials science, as these materials can not only support biological functions but actively enhance the body's natural healing processes [1]. For instance, bioactive glass used in bone implants can release ions that encourage bone formation, while bioactive polymers can promote skin cell growth in wound healing applications [1]. This capacity for active biological engagement positions bioactivity as a crucial property for next-generation tissue engineering scaffolds.
Molecular Mechanisms of Bioactive Materials
Bioactive materials function through several molecular mechanisms to influence cellular behavior and tissue regeneration:
Integrin-Mediated Signaling: Bioactive materials often present specific peptide sequences (e.g., RGD from fibronectin) that engage integrin receptors on cell surfaces [3]. This engagement initiates intracellular signaling cascades that regulate cell adhesion, migration, proliferation, and differentiation. The activation of integrin signaling begins with ECM ligand binding, which induces conformational changes that promote receptor clustering and the assembly of focal adhesion complexes [3]. These specialized structures serve as mechanical and biochemical signaling hubs, recruiting adaptor proteins including talin, vinculin, and paxillin to bridge the connection between integrins and the actin cytoskeleton [3].
Growth Factor Delivery: Many bioactive scaffolds incorporate growth factors (e.g., BMP-2 for bone formation, VEGF for vascularization) that are released in a controlled manner to direct tissue regeneration.
Ion Release: Certain bioceramics and bioactive glasses release ions (e.g., silicon, calcium, phosphate) that stimulate cellular responses and promote mineralized tissue formation.
Topographical Cues: Nanoscale and microscale surface patterns can influence cell morphology, alignment, and differentiation through contact guidance.
The following diagram illustrates the key signaling pathways activated by integrin engagement with bioactive materials:
Experimental Assessment of Bioactivity
Evaluating the bioactive properties of biomaterials requires a multifaceted approach combining in vitro and in vivo methods:
In Vitro Assessment Protocols:
- Cell Adhesion Assays: Quantifying cell attachment and spreading over time using fluorescence microscopy or colorimetric methods.
- Proliferation Studies: Measuring cell growth rates using MTT, Alamar Blue, or DNA quantification assays.
- Differentiation Analysis: Assessing lineage-specific differentiation through gene expression (qPCR), protein production (immunocytochemistry, Western blot), and functional assays (alkaline phosphatase for osteogenesis, GAG deposition for chondrogenesis).
- Gene Expression Profiling: RNA sequencing or microarray analysis to evaluate global transcriptional responses to material cues.
In Vivo Assessment Protocols:
- Histological Analysis: Tissue sectioning and staining (H&E, Masson's Trichrome, immunohistochemistry) to evaluate tissue integration, cellular infiltration, and matrix deposition.
- Mechanical Integration: Push-out tests or tensile testing to measure bond strength between implant and host tissue.
- Functional Recovery: Assessing restoration of tissue function through biomechanical testing, imaging, or physiological measurements.
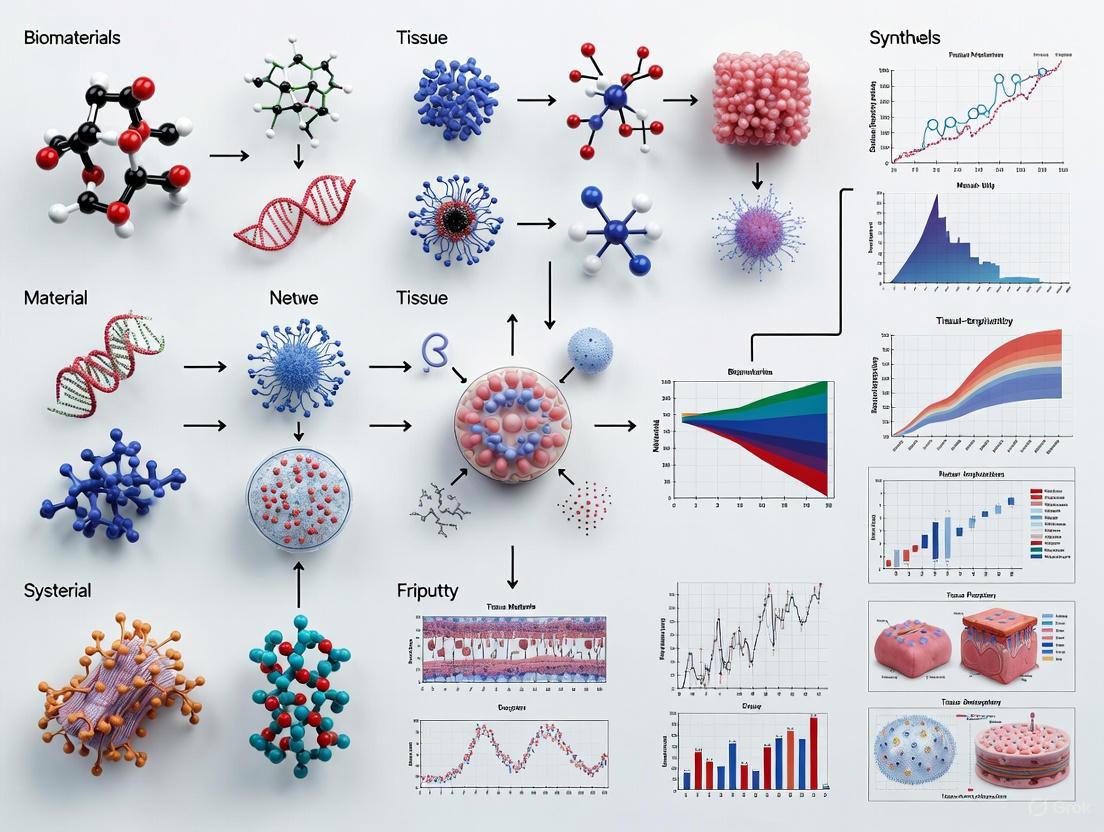
Integrated Workflow for Biomaterial Development and Testing
The development of advanced biomaterials for tissue engineering follows a systematic workflow from conceptualization through characterization to biological validation. The following diagram outlines this comprehensive process:
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful biomaterials research requires specialized reagents and materials to properly evaluate the triad of key properties. The following table details essential components of the biomaterials research toolkit:
Table 3: Essential Research Reagents for Biomaterial Characterization
| Reagent/Material Category | Specific Examples | Function in Biomaterials Research |
|---|---|---|
| Cell Culture Systems | Mesenchymal stem cells (MSCs), osteoblasts, fibroblasts, endothelial cells | Evaluate cell-material interactions, biocompatibility, and bioactivity |
| Molecular Biology Assays | qPCR reagents, ELISA kits, Western blot materials | Assess cellular responses at genetic and protein levels |
| Histological Stains | Hematoxylin & Eosin (H&E), Masson's Trichrome, Alizarin Red | Visualize tissue integration and specific matrix components |
| Polymer Synthesis Reagents | Lactide, glycolide, ε-caprolactone monomers, initiators (Sn(Oct)₂) | Synthesize biodegradable polymers with tailored properties |
| Crosslinking Agents | Genipin, glutaraldehyde, carbodiimides (EDC/NHS) | Modify mechanical properties and degradation rates |
| Bioactive Factors | RGD peptides, BMP-2, VEGF, TGF-β3 | Enhance specific biological responses and tissue regeneration |
| Characterization Standards | ISO 10993 series, ASTM standards for biomaterials | Ensure reproducible and comparable evaluation methods |
The triad of biocompatibility, biodegradability, and bioactivity represents the fundamental framework for designing effective biomaterials in tissue engineering. These properties are not isolated characteristics but interconnected elements that must be carefully balanced to create successful regenerative therapies. Biocompatibility ensures harmonious existence with living systems, biodegradability provides temporary support that gracefully exits once its function is fulfilled, and bioactivity enables dynamic communication with cells to direct the regenerative process.
As the field advances, we are witnessing a shift from biomaterials that merely avoid harm to those that actively orchestrate regeneration [4]. This evolution is driven by increasingly sophisticated understanding of ECM biology [3] and the molecular mechanisms governing cell-material interactions. The future of biomaterials in tissue engineering lies in developing increasingly intelligent systems that can dynamically respond to physiological cues, selectively direct cellular behavior, and seamlessly integrate with host tissues to restore function. By mastering the interplay between biocompatibility, biodegradability, and bioactivity, researchers can create next-generation biomaterials that truly bridge the gap between synthetic constructs and living tissues.
Natural biomaterials, primarily derived from biological sources, play an indispensable role in advancing tissue engineering and regenerative medicine (TE-RM). These materials, which include alginates, celluloses, chitosan, and collagen, serve as scaffolds that mimic the native extracellular matrix (ECM), providing structural support and biochemical cues that guide tissue regeneration [6]. Their widespread application stems from inherent properties such as excellent biocompatibility, biodegradability, and low immunogenicity. This whitepaper provides a technical guide to these four key natural biomaterials, detailing their fundamental characteristics, mechanisms of action, and practical experimental methodologies. Framed within the broader context of a thesis on biomaterials in tissue engineering research, this document serves as a comprehensive resource for researchers, scientists, and drug development professionals, equipping them with the foundational knowledge and protocols needed to leverage these materials in their work.
Fundamental Properties and Comparative Analysis
The utility of a biomaterial is determined by a suite of physicochemical and biological properties. The table below provides a quantitative comparison of the key characteristics of alginates, celluloses, chitosan, and collagen.
Table 1: Comparative Analysis of Key Natural Biomaterials
| Biomaterial | Source | Key Characteristics | Typical Compressive Modulus | Degradation Timeline | Cell Adhesion |
|---|---|---|---|---|---|
| Alginate | Brown seaweed, bacteria [6] | Hydrophilic, anionic polysaccharide; forms hydrogels via ionic crosslinking [6] | 20–40 kPa (unmodified) [6] | Weeks to months (tunable) [6] | Poor (unless modified with RGD) [6] |
| Cellulose | Plants (CNC, CNF), bacteria (BNC) [7] [8] | High purity, excellent mechanical strength, biocompatibility [8] | High (BNC provides robust scaffolds) [8] | Low degradation in mammals | Moderate |
| Chitosan | Crustacean shells | Cationic polysaccharide, antimicrobial, bioadhesive [7] | <10 kPa (hydrogels) [6] | Tunable via degree of deacetylation | Good (supports stem cell adhesion) [7] |
| Collagen | Animal tissues, recombinant systems [9] | Major ECM protein; excellent biocompatibility and bioactivity [9] | Varies by form and crosslinking | Tunable via crosslinking density | Excellent (native RGD motifs) [9] |
The selection of a biomaterial is highly application-dependent. Alginate is prized for its rapid, mild gelation conditions but often requires composite strategies or chemical functionalization to improve its mechanical strength and cellular interactions [6] [10]. Cellulose nanoparticles, particularly bacterial cellulose (BC), provide exceptional mechanical strength and are ideal for hard tissue regeneration, though their degradation profile can be a limitation [7] [8]. Chitosan offers inherent antimicrobial properties and supports stem cell adhesion, making it suitable for wound healing and soft tissue engineering, though its mechanical strength is relatively low [6] [7]. Collagen, as a native component of the ECM, offers superior bioactivity and cell signaling capabilities. The ratio of its types, particularly Collagen I and III, is critical for tissue function; a lower Col I/III ratio is associated with more flexible, elastic tissues and reduced scarring, as seen in fetal wound healing [9] [11].
Table 2: Impact of Collagen I/III Ratio in Different Tissues
| Tissue/Condition | Typical Collagen I/III Ratio | Functional Implication |
|---|---|---|
| Adult Skin | ~4:1 [11] | Provides tensile strength and structural integrity. |
| Fetal Skin | ~1:1 [9] | Promotes regenerative, scarless healing. |
| Blood Vessels | High abundance of Type III [9] | Confers elasticity and distensibility. |
| Hypertrophic Scars | Altered ratio and organization [9] | Leads to disorganized ECM and loss of function. |
Molecular Mechanisms and Signaling Pathways
Natural biomaterials direct cellular behavior through specific molecular interactions. The following diagrams illustrate key signaling pathways and structural relationships.
Alginate Functionalization and Cell Signaling
This diagram outlines the process of modifying alginate to make it bioactive and the subsequent integrin-mediated signaling pathway it activates to promote cell survival and proliferation.
Collagen I/III Ratio in Tissue Remodeling
This diagram shows how the ratio of Collagen I to III influences tissue mechanical properties and its therapeutic application in scaffold design.
Experimental Protocols and Methodologies
Protocol: Preparation of Ionically Crosslinked Alginate Hydrogel
This is a fundamental method for creating alginate hydrogels for cell encapsulation or drug delivery [6] [10].
- Step 1: Solution Preparation. Dissolve high-G content sodium alginate powder in deionized water or physiological buffer (e.g., 0.9% NaCl) to a typical concentration of 1-3% (w/v). Stir continuously until the solution is clear and free of particulates. Sterilize the solution by autoclaving or sterile filtration.
- Step 2: Crosslinking Agent Preparation. Prepare a crosslinking solution containing a divalent cation, most commonly Calcium Chloride (CaCl₂), at a concentration of 50-200 mM in deionized water. Sterilize by filtration.
- Step 3: Gelation via the "Egg-Box" Model.
- Droplet Method: Slowly drip the alginate solution into the crosslinking solution using a syringe pump or pipette. This forms stable, crosslinked alginate beads. Incubate for 10-15 minutes to ensure complete gelation.
- Bulk Gel Method: For larger hydrogels, mix the alginate and crosslinking solutions rapidly and thoroughly. The gel will form within seconds to minutes.
- Step 4: Post-Processing. Wash the resulting hydrogel three times with sterile buffer or culture medium to remove excess crosslinking ions and to equilibrate the pH. The hydrogel is now ready for cell culture, mechanical testing, or further modification.
Protocol: Fabrication of a Chitosan-Alginate Composite Scaffold
Combining chitosan and alginate leverages the benefits of both materials, creating a polyelectrolyte complex with improved stability and bioactivity [6] [10].
- Step 1: Polymer Solution Preparation.
- Prepare a 2% (w/v) chitosan solution by dissolving chitosan in a 1% (v/v) acetic acid solution. Stir until fully dissolved.
- Prepare a 2% (w/v) sodium alginate solution in deionized water as described in Protocol 4.1.
- Step 2: Composite Formation. Mix the chitosan and alginate solutions in a desired volume ratio (e.g., 1:1) under constant stirring. The oppositely charged polymers will form a polyelectrolyte complex, which may result in a precipitate or a viscous solution.
- Step 3: Scaffold Fabrication. The composite mixture can be processed into various forms:
- Porous Scaffolds: Pour the mixture into a mold and freeze at -20°C overnight, then lyophilize to create a porous sponge.
- Hydrogels: Induce further crosslinking by exposing the mixture to a CaCl₂ solution or by raising the pH to neutralize the chitosan.
- Step 4: Characterization. Characterize the scaffold's morphology using Scanning Electron Microscopy (SEM), its mechanical properties via compression testing, and its biological performance through cell viability assays (e.g., with MSCs).
The Scientist's Toolkit: Essential Research Reagents
Successful research with natural biomaterials requires a suite of key reagents and tools. The following table details essential items for a laboratory working in this field.
Table 3: Key Research Reagent Solutions for Biomaterial Research
| Reagent / Material | Function and Application |
|---|---|
| High-Guluronic Acid (High-G) Alginate | Forms stiffer, more stable hydrogels via ionic crosslinking, ideal for load-bearing tissue models [6] [10]. |
| Recombinant Human Type III Collagen (rhCol III) | Provides a safe, xenogeneic-free collagen source with customizable properties for scaffolds that promote regenerative healing [9]. |
| Bacterial Nanocellulose (BNC) | Serves as a mechanically robust, highly pure scaffold material for engineering hard tissues like bone and cartilage [7] [8]. |
| RGD Peptide | A critical biochemical modifier; covalently grafted onto alginate to confer cell-adhesive properties [6]. |
| Calcium Chloride (CaCl₂) | The most common ionic crosslinker for alginate hydrogels, enabling rapid gelation under mild conditions [6] [10]. |
| Methacrylated Alginate (SAMA) | A chemically modified alginate for photopolymerization; allows fabrication of stable, tunable hydrogels via UV light [10]. |
| Mesenchymal Stem Cells (MSCs) | A primary cell type used in TE-RM; their interaction with biomaterial scaffolds is a standard model for evaluating regenerative potential [7]. |
Alginates, celluloses, chitosan, and collagen represent a powerful toolkit for addressing complex challenges in tissue engineering and regenerative medicine. While each material has distinct advantages and limitations, ongoing research focused on chemical modification, composite formation, and a deeper understanding of molecular interactions with cells is rapidly advancing the field. The translation of these biomaterials from laboratory research to clinical applications hinges on rigorous, standardized experimental methodologies and a clear comprehension of their structure-function relationships. As the field progresses, these natural biomaterials will undoubtedly remain cornerstone elements in the development of next-generation therapeutic strategies for tissue repair and regeneration.
Synthetic biodegradable polymers have emerged as cornerstone materials in tissue engineering and regenerative medicine, providing a versatile platform for creating scaffolds that mimic the native extracellular matrix (ECM). Among these, poly(lactic-co-glycolic acid) (PLGA), polycaprolactone (PCL), and polylactic acid (PLA) stand out due to their tunable properties, biocompatibility, and predictable degradation profiles. These polymers serve as temporary structural templates that support cell attachment, proliferation, and differentiation while gradually degrading to be replaced by newly formed tissue [3] [12]. The fundamental advantage of these synthetic materials lies in their precise engineerability—researchers can systematically modify their chemical composition, molecular weight, and copolymer ratios to control mechanical strength, degradation kinetics, and bioactivity for specific therapeutic applications ranging from bone regeneration to drug delivery systems [13].
The significance of these biomaterials extends beyond their structural function. They actively participate in the regenerative process by providing biochemical cues through surface functionalization, controlling the release of therapeutic agents, and interacting with cellular components through integrin-mediated signaling pathways [3]. This whitepaper provides a comprehensive technical analysis of PLGA, PCL, and PLA, focusing on their structure-property relationships, advanced fabrication methodologies, and experimental protocols for characterizing their performance in biomedical applications.
Material Properties and Characterization
The functional performance of PLGA, PCL, and PLA in tissue engineering applications is governed by their distinct chemical compositions, thermal behaviors, and degradation mechanisms. Understanding these properties enables researchers to select and tailor materials for specific regenerative medicine applications.
Comparative Analysis of Polymer Properties
Table 1: Fundamental Properties of PLGA, PCL, and PLA
| Property | PCL | PLA | PLGA |
|---|---|---|---|
| Chemical Composition | Semi-crystalline aliphatic polyester from ε-caprolactone monomers [13] | Aliphatic polyester derived from L-lactide and D-lactide isomers [13] | Copolymer of lactic acid (LA) and glycolic acid (GA) with tunable ratios [13] |
| Crystallinity | 20-33% (high crystallinity) [13] | Varies by D/L isomer ratio (low D = crystalline, high D = amorphous) [13] | Amorphous to semi-crystalline depending on LA:GA ratio [13] |
| Melting Point (°C) | 58-61 [13] | 150-160 [13] | Not well-defined; varies by LA:GA ratio, typically amorphous [13] |
| Glass Transition (°C) | ≈ -60 [13] | ≈ 60 [13] | 40-60 (higher LA → higher Tg) [13] |
| Mechanical Properties | Flexible; low tensile strength; strength increases with crystallinity [13] | Tensile strength: 50-70 MPa; Elastic modulus: 3-4 GPa [13] | Varies with LA:GA ratio; generally lower tensile strength than PLA [12] |
| Degradation Time | Very slow (months to years) [13] [14] | Intermediate (months to years) [13] | Fastest at 50:50 LA:GA ratio (weeks to months) [13] |
| Key Characteristics | High hydrophobicity, slow degradation, excellent ductility [13] [14] | High strength, stiffness, degradation rate depends on crystallinity [13] | Precise degradation control via LA:GA ratio, tunable hydrophilicity [13] |
Degradation Mechanisms and Drug Release Kinetics
The degradation of these polyesters occurs primarily through hydrolysis of their ester bonds, but the rates and patterns differ significantly based on their crystallinity, hydrophobicity, and copolymerization ratios [13]. PCL's high crystallinity and hydrophobicity limit water penetration, resulting in very slow degradation that makes it suitable for long-term drug release (several months to years) and applications requiring extended structural support [13] [14]. PLA degrades via non-enzymatic hydrolysis, with rates varying from months to years depending on its crystallinity, molecular weight, and processing history [13]. PLGA offers the most tunable degradation profile, with the 50:50 LA:GA ratio exhibiting the fastest degradation due to enhanced water absorption [13].
The degradation behavior directly influences drug release kinetics. PCL's hydrophobic nature and slow degradation suppress initial burst release and enable consistent sustained release over extended periods [13]. PLA provides an intermediate release profile that can be controlled from days to months through processing parameters and molecular weight adjustments [13]. PLGA's drug release pattern can be precisely engineered by varying the LA:GA ratio, with higher glycolide content accelerating release and higher lactide content favoring sustained delivery [13]. Additionally, the hydrophobicity/hydrophilicity of incorporated drugs significantly influences their release profiles from these polymer matrices [13].
Figure 1: Degradation Pathways of Synthetic Polymers. This diagram illustrates the hydrolytic degradation process common to PLGA, PCL, and PLA, highlighting key influencing factors and material-specific outcomes that determine their performance in tissue engineering applications.
Experimental Protocols and Methodologies
Fabrication of 3D-Printed PLGA/nHA/GO Composite Scaffolds
The development of bone tissue engineering scaffolds using low-temperature 3D printing and freeze-drying techniques represents a sophisticated approach to creating functional constructs for bone defect repair [15].
Materials and Reagents:
- PLGA (LA/GA = 75/25; Hangzhou Regenovo Biotechnology) as the structural matrix [15]
- nHA (nano-hydroxyapatite, 200 nm particle size; Shanghai Yien Chemical Technology) to replicate bone's inorganic composition [15]
- GO (graphene oxide; Shanghai Yien Chemical Technology) to enhance mechanical properties and bioactivity [15]
- 1,4-Dioxane (Shanghai Macklin Biochemical) as solvent for polymer dissolution [15]
- Phosphate-buffered saline (PBS, pH 7.4) for degradation studies [15]
Scaffold Fabrication Protocol:
- Solution Preparation: Dissolve PLGA pellets (2g) in 15 mL 1,4-dioxane under magnetic stirring for 30 minutes at room temperature [15].
- Composite Formulation: For PLGA/nHA/GO group, add nHA (0.5g) and GO (0.01g) to the base PLGA solution. Use vortex dispersion for 1 minute followed by magnetic stirring until complete homogenization (mass ratios: PLGA:nHA = 4:1; nHA:GO = 100:2) [15].
- 3D Printing Parameters: Utilize a pre-cooled 3D printer (Bio-Architect wS) with optimized parameters:
- Post-processing: Immediately transfer printed scaffolds to -80°C refrigerator for 2 hours, followed by freeze-drying for 24 hours [15].
- Sterilization: Immerse scaffolds in 75% ethanol with ultraviolet light irradiation for 3 hours, then wash with PBS to remove residual ethanol [15].
Characterization Methods:
- Mechanical Testing: Perform compression testing according to ASTM D695 at a compression rate of 1 mm/min with 60% strain rate [15].
- Degradation Study: Immerse scaffolds in PBS (pH 7.4) and measure mass loss at predetermined time points using the formula: Degradation rate (mg/w) = (M1 - M2)/2w, where M1 is initial mass and M2 is mass at time point [15].
- Water Absorption: Measure dry mass (m1), immerse in deionized water, then measure wet mass (m2) at 3, 6, 9, and 12 hours. Calculate water absorption as: (m2 - m1)/m1 × 100% [15].
In Vivo Evaluation of 3D-Printed PCL Tracheal Scaffolds
The assessment of medical-grade versus research-grade PCL in rabbit tracheal defect models provides critical insights into the importance of material selection for specific clinical applications [16].
Experimental Design:
- Scaffold Fabrication: Manufacture customized scaffolds for rabbit segmental defects using extrusion-based 3D printing with research-grade (RG) and medical-grade (MG) PCL [16].
- Surgical Implantation: Transplant scaffolds into tracheal defects in rabbit models following approved IACUC protocols (The Catholic University of Korea, 2020-0213-01) [16].
- Evaluation Timeline: Excise transplanted areas after 6 months for analysis [16].
Analytical Methods:
- Mechanical Characterization: Assess ultimate stress and strain of explanted scaffolds to compare strength and ductility retention [16].
- Molecular Weight Analysis: Use Gel Permeation Chromatography (GPC) to compare molecular weight changes before and after transplantation and after gamma radiation sterilization [16].
- Histological Evaluation: Employ tissue staining techniques to analyze mucosal tissue regeneration and overall tissue reconstruction at implantation site [16].
- Endoscopic Examination: Monitor tissue integration and structural integrity in vivo [16].
Key Findings: Medical-grade PCL scaffolds demonstrated superior ultimate stress, strain, and tissue reconstruction compared to research-grade scaffolds, with better strength, ductility, and mucosal regeneration. However, MG PCL degraded more rapidly in vivo, as indicated by significant molecular weight reduction post-transplantation [16].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Polymer Scaffold Development
| Reagent/Material | Function/Application | Technical Specifications | Supplier Examples |
|---|---|---|---|
| PLGA Polymers | Structural matrix for scaffolds with tunable degradation | LA:GA ratios (e.g., 75:25); inherent viscosity varies by application | Hangzhou Regenovo Biotechnology [15] |
| Medical-grade PCL | High-purity polymer for implantation studies | Controlled molecular weight distribution; sterilizable | Perstorp (CAPA 6400) [16] [14] |
| Nano-Hydroxyapatite (nHA) | Bone mineral mimic for osteoconduction | 200 nm particle size; enhances bioactivity | Shanghai Yien Chemical Technology [15] |
| Graphene Oxide (GO) | Mechanical reinforcement and bioactivity enhancement | Specific surface area; functional group density | Shanghai Yien Chemical Technology [15] |
| 1,4-Dioxane | Solvent for polymer processing | Anhydrous grade for solution-based fabrication | Shanghai Macklin Biochemical [15] |
| Gamma Irradiation | Terminal sterilization method | Standard dosage (25 kGy); maintains polymer integrity | Contract sterilization services [16] |
| Gel Permeation Chromatography | Molecular weight distribution analysis | Tetrahydrofuran as mobile phase for polyesters | Waters, Agilent Technologies [16] |
Advanced Applications and Functional Design Strategies
Porosity Optimization for Tissue Engineering Scaffolds
The strategic design of scaffold architecture, particularly porosity, plays a critical role in determining the success of tissue engineering constructs. Research has demonstrated that porosity directly influences mechanical properties, cellular responses, and microbial interactions [17].
Table 3: Effect of Porosity on PLA Scaffold Properties
| Porosity Level | Tensile Strength | Human Skin Fibroblast Viability | Bacterial Adhesion Response |
|---|---|---|---|
| 20% | 4 MPa | Moderate proliferation | Species-specific adherence patterns |
| 40% | 8 MPa | Good proliferation | S. aureus peak adhesion (40-60%) |
| 60% | 8 MPa | High viability | S. aureus peak adhesion (40-60%) |
| 80% | 16 MPa | Highest viability | P. aeruginosa maximum adhesion |
| 100% | 28 MPa | Moderate viability | S. epidermidis and E. coli peak adhesion |
Studies have revealed that intermediate porosity levels (60-80%) create an optimal balance between mechanical integrity and biological performance. PLA scaffolds with 80% porosity demonstrated the highest human skin fibroblast viability while maintaining sufficient tensile strength (16 MPa) for many soft tissue applications [17]. The relationship between porosity and bacterial adhesion showed species-specific responses, informing infection-resistant scaffold design strategies [17].
Polymer Blending for Soft Tissue Reconstruction
The combination of PLA and PCL in knitted scaffolds has shown significant promise for soft tissue engineering applications, particularly in adipose tissue reconstruction [14]. By adjusting the PLA/PCL ratio, researchers can precisely control the mechanical properties and degradation profiles to match specific tissue requirements.
PLA90/PCL10 scaffolds maintain better structural integrity and stiffness, making them suitable for applications requiring mechanical support during the initial healing phase. These scaffolds demonstrated superior performance in vivo with enhanced vascularization and reduced macrophage infiltration in rat models [14].
PLA70/PCL30 scaffolds with higher PCL content exhibit enhanced elasticity and porosity, facilitating cell infiltration and nutrient transport. These scaffolds showed excellent biocompatibility in vitro but slightly reduced efficacy in supporting adipogenic differentiation compared to PLA90/PCL10 variants [14].
The fabrication of these scaffolds via melt-spinning and knitting techniques enables the production of three-dimensional porous structures with multiscale porosity and elasticity tailored to soft tissue properties [14]. This approach represents a significant advancement over traditional fabrication methods like electrospinning and FDM, particularly for applications requiring flexibility and adaptability to anatomical contours.
Figure 2: Biomaterial Design Framework. This diagram outlines the strategic approach to developing polymer-based scaffolds for specific tissue engineering applications, highlighting the interconnected decision points from material selection to functional outcomes.
Synthetic polymers PLGA, PCL, and PLA continue to evolve as fundamental building blocks in tissue engineering, offering unparalleled versatility through their tunable properties and processing adaptability. The strategic selection and combination of these materials enable researchers to create customized scaffolds that address specific clinical challenges, from load-bearing bone defects to delicate soft tissue reconstruction. Medical-grade materials have demonstrated superior performance in vivo compared to research-grade equivalents, highlighting the importance of material quality in translational research [16]. The integration of bioactive components such as nano-hydroxyapatite and graphene oxide further enhances the functionality of these polymer systems, creating composite constructs that more closely mimic the native tissue environment [15].
Future developments in this field will likely focus on smart polymer systems with responsive degradation profiles, advanced fabrication techniques for creating vasculature networks, and personalized scaffolds based on patient-specific imaging data. As research progresses, the continued refinement of PLGA, PCL, and PLA-based technologies will undoubtedly expand their impact in regenerative medicine, offering new solutions for complex tissue repair and regeneration challenges.
Inorganic and metallic biomaterials represent a cornerstone of modern tissue engineering and regenerative medicine. These materials are engineered to interact with biological systems, providing structural support, guiding tissue regeneration, and actively participating in the healing process. Within this domain, calcium phosphates, bioactive glasses, and titanium alloys have emerged as three pivotal classes of materials, each offering a unique combination of properties that make them indispensable for clinical applications. This whitepaper provides an in-depth technical examination of these materials, focusing on their properties, mechanisms of action, and experimental methodologies relevant to researchers and drug development professionals. Framed within the broader thesis on the role of biomaterials in tissue engineering research, this review underscores how these materials transcend their traditional passive roles to actively orchestrate biological responses for enhanced tissue repair and integration.
Calcium Phosphates
Properties and Classification
Calcium phosphates (CaPs) are a family of bioceramics that closely mimic the mineral composition of native bone, making them one of the most prominent materials for bone tissue regeneration [18] [19]. Their primary advantage lies in their bioactivity, osteoconductivity, and tunable resorption rates. The biological performance of CaPs is highly dependent on their phase composition, stoichiometry, and crystallinity, which are directly influenced by the synthesis method and parameters [18].
Table 1: Characteristics of Major Calcium Phosphates Used in Biomedicine
| Material | Chemical Formula | Ca/P Ratio | Key Properties | Primary Applications |
|---|---|---|---|---|
| Hydroxyapatite (HAp) | Ca₁₀(PO₄)₆(OH)₂ | 1.67 | High bioactivity, osteoconductivity, chemical stability, slow degradation | Bone defect fillers, coatings for metal implants, dental applications [18] [20] |
| β-Tricalcium Phosphate (β-TCP) | Ca₃(PO₄)₂ | 1.50 | Biodegradable, osteoconductive, higher resorption rate than HAp | Bioresorbable bone grafts, bone cements [18] [20] |
| Biphasic Calcium Phosphate (BCP) | Mixture of HAp and β-TCP | 1.50-1.67 | Controllable degradation/bioactivity ratio via HAp/β-TCP ratio | Bone tissue engineering scaffolds [18] [20] |
| Amorphous Calcium Phosphate (ACP) | Non-stoichiometric | 1.15-1.67 | High reactivity, lack of long-range order | Precursor for bone mineral, component in composite biomaterials [18] |
Synthesis and Experimental Protocol
The properties of calcium phosphates can be precisely controlled through the synthesis route. The following is a detailed protocol for the acid-base precipitation method, a common wet chemical technique [18].
Protocol: Synthesis of HAp Powders via Acid-Base Precipitation
- Objective: To synthesize stoichiometric hydroxyapatite (Ca/P = 1.67) powders with controlled morphology and phase purity.
Principle: The method involves the neutralization reaction between a calcium source and a phosphorus source under controlled pH, leading to the precipitation of HAp.
Materials and Reagents:
- Calcium hydroxide (Ca(OH)₂)
- Orthophosphoric acid (H₃PO₄), 0.3 M
- Ammonia water (NH₄OH, 25%) for pH control
- Deionized water
Equipment:
- Laboratory stirrer with heating mantle
- pH meter
- Centrifuge
- Drying oven
- High-temperature furnace (for calcination, if required)
Procedure:
- Preparation of Reactants: Suspend an appropriate mass of Ca(OH)₂ in 500 mL of deionized water to create a slurry. The mass is calculated based on the desired final Ca/P molar ratio (e.g., 1.67 for HAp). Simultaneously, prepare 500 mL of 0.3 M H₃PO₄ solution.
- Precipitation Reaction: Gradually add the H₃PO₄ solution to the Ca(OH)₂ suspension under constant stirring. The addition rate should be slow to avoid localized precipitation and ensure homogeneity.
- pH Control: Maintain the reaction pH at a constant value (typically between 9-11) by the dropwise addition of 25% ammonia water throughout the synthesis. Precise pH control is critical for obtaining the desired phase composition.
- Ageing: After complete addition, continue stirring the suspension for a further 12-24 hours at room temperature to allow for complete crystal maturation.
- Washing and Separation: Separate the precipitate from the mother liquor by centrifugation. Wash the precipitate repeatedly with deionized water until the supernatant reaches a neutral pH.
- Drying and Calcination: Dry the washed precipitate in an oven at 80-100°C for 24 hours. The resulting powder can be further calcined in a furnace at high temperatures (e.g., 800-1100°C) to improve crystallinity, if required for the application.
Characterization: The synthesized powder should be characterized using X-ray diffraction (XRD) for phase identification, Fourier-Transform Infrared Spectroscopy (FT-IR) for functional groups, Scanning Electron Microscopy (SEM) for morphology, and Inductively Coupled Plasma (ICP) analysis for determining the exact Ca/P ratio [18].
Signaling Pathways in Bone Regeneration
Calcium phosphates promote bone healing through direct interaction with the biological environment. They release calcium (Ca²⁺) and phosphate (PO₄³⁻) ions, which are known to activate intracellular signaling cascades that promote osteogenic differentiation [3]. A key mechanism involves integrin-mediated signaling. The adsorbed proteins on the CaP surface facilitate cell adhesion through integrin receptors (e.g., αvβ3, α5β1), leading to the formation of focal adhesion complexes and activation of Focal Adhesion Kinase (FAK). This triggers downstream pathways such as MAPK/ERK and PI3K/Akt, which regulate gene expression for cell proliferation, survival, and differentiation into osteoblasts [3]. Furthermore, the released ions can influence the Wnt/β-catenin pathway, another critical regulator of osteogenesis.
CaP-Induced Osteogenic Signaling Pathway
Bioactive Glasses
Composition and Bioactivity Mechanism
Bioactive glasses (BGs) are a class of surface-reactive bioceramics known for their ability to form a strong bond with both hard and soft tissues [21]. The bioactivity mechanism of silicate-based BGs, such as the pioneering 45S5 Bioglass, involves a well-defined series of surface reactions when implanted.
Table 2: Common Bioactive Glass Compositions (mol%)
| Glass Type | SiO₂ | P₂O₅ | CaO | Na₂O | CaF₂ | B₂O₃ | Key Features |
|---|---|---|---|---|---|---|---|
| 45S5 | 45.0 | 6.0 | 24.5 | 24.5 | - | - | Gold standard, high bioactivity [21] |
| 58S | 58.2 | 9.2 | 32.6 | - | - | - | Sol-gel derived, high surface area [21] |
| 13-93 | 53.0 | 4.0 | 20.0 | 6.0 | - | - | Contains K₂O and MgO, for bone scaffolds [21] |
| 13-93B3 | - | 3.7 | 18.5 | 5.5 | - | 56.6 | Borate-based, fast degradation [21] |
The sequence of events leading to bioactivity is as follows:
- Rapid Ion Exchange: Na⁺ or other network modifiers from the BG exchange with H⁺ from the surrounding fluid, leading to a local increase in pH.
- Silica Hydrolysis: Breakdown of the silica network occurs, forming silanol (Si-OH) groups on the surface.
- Polycondensation: Silanol groups condense to form a porous silica-rich gel layer.
- Precipitation: Ca²⁺ and PO₄³⁻ ions from the glass and body fluid migrate to the surface, forming an amorphous calcium phosphate (ACP) layer.
- Crystallization: The ACP layer incorporates hydroxyl and carbonate ions from the fluid and crystallizes into a bone-like carbonated hydroxyapatite (HCA) layer.
This HCA layer is responsible for the chemical bonding with living tissue [21]. Borate and phosphate-based BGs follow a similar but often faster conversion process, where the glass network former (e.g., B₂O₃) dissolves completely, leading to direct HA precipitation [21].
Experimental Workflow: Sol-Gel Synthesis
The sol-gel process allows for the production of BGs with high purity, homogeneity, and controlled porosity at lower temperatures than the traditional melt-quenching route.
Sol-Gel Synthesis of Bioactive Glass
Protocol: Sol-Gel Synthesis of 58S Bioactive Glass (60 mol% SiO₂, 36 mol% CaO, 4 mol% P₂O₅)
Materials and Reagents:
- Tetraethyl orthosilicate (TEOS) - SiO₂ precursor
- Triethyl phosphate (TEP) - P₂O₅ precursor
- Calcium nitrate tetrahydrate (Ca(NO₃)₂·4H₂O) - CaO precursor
- Deionized water
- Nitric acid (HNO₃) or Ammonia (NH₄OH) as catalyst
- Ethanol
Equipment:
- Polypropylene beaker with sealed lid
- Magnetic stirrer
- Drying oven
- High-temperature furnace
Procedure:
- Hydrolysis of TEOS: Add TEOS to a mixture of deionized water and ethanol (as a mutual solvent) under vigorous stirring. Add a few drops of nitric acid to catalyze the hydrolysis reaction (pH ~1-2). Stir for 1 hour.
- Addition of TEP: Add TEP to the solution and continue stirring for another 45 minutes.
- Addition of Calcium Nitrate: Add the calcium nitrate tetrahydrate to the solution. Stir until it is completely dissolved.
- Gelation: Seal the container and allow the mixture to gel at room temperature. This process may take several days.
- Aging: Once gelled, the monolith is aged in its own pore solution (or a similar solvent) for 24-48 hours to strengthen the gel network.
- Drying: Carefully transfer the aged gel to a drying oven and dry slowly at 60-120°C for several days to remove all liquid and form a "xerogel."
- Thermal Stabilization: Heat the xerogel in a furnace to a temperature between 600-700°C at a controlled heating rate. This step is crucial to remove residual nitrates and organic groups and to stabilize the porous glass structure without crystallizing it.
Titanium and Its Alloys
Properties and Classification
Titanium and its alloys are the dominant metallic biomaterials in orthopedics and dentistry due to their exceptional corrosion resistance, high specific strength, and excellent biocompatibility [22] [23] [24]. A key feature is the spontaneous formation of a protective, adherent surface oxide layer (primarily TiO₂), which is responsible for their passivity and bio-inertness in the physiological environment [22].
Table 3: Classification and Properties of Titanium-Based Biomaterials
| Alloy Type | Alloy Examples | Phases Present | Key Properties | Common Applications |
|---|---|---|---|---|
| Commercially Pure Ti (cpTi) | Grade 1-4 | α | Excellent corrosion resistance, biocompatibility, lower strength | Dental implants, non-load bearing components [22] |
| (α + β) Alloys | Ti-6Al-4V (Grade 5) | α + β | High strength, good fatigue resistance | Load-bearing orthopedic implants (hip stems, bone plates) [22] [24] |
| Near-β / β Alloys | Ti-13Nb-13Zr, Ti-12Mo-6Zr-2Fe | Predominantly β | Lower Young's Modulus (~55-80 GPa), better strain compatibility with bone | Next-generation orthopedic implants to reduce stress shielding [23] [24] |
A primary driver of titanium's success in bone applications is osseointegration—the direct structural and functional connection between living bone and the implant surface [22]. The native titanium oxide surface is conducive to bone apposition, and this process can be significantly enhanced through surface modifications like sandblasting, acid-etching, or the application of a CaP coating [22] [24].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Materials for Biomaterials Research
| Item | Function / Application | Example Use Case |
|---|---|---|
| L929 Mouse Fibroblasts | Biocompatibility and cytotoxicity testing according to ISO 10993 standards [18]. | Evaluating the biological tolerance of newly synthesized CaP powders [18]. |
| hFOB 1.19 Human Osteoblasts | Assessing osteoconductivity and cell-material interactions specific to bone. | Measuring alkaline phosphatase (ALP) activity and osteogenic gene expression on Ti surfaces [18]. |
| Simulated Body Fluid (SBF) | In vitro bioactivity assessment of materials. | Testing the ability of bioactive glass to form a hydroxyapatite layer on its surface [21]. |
| Roswell Park Memorial Institute (RPMI)-1640 / DMEM | Cell culture media for maintaining and growing mammalian cells. | Standard culture of L929 fibroblasts and other cell lines for biological assays [18]. |
| 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) | Colorimetric assay for measuring cell metabolic activity and proliferation. | Quantifying the viability of cells cultured in the presence of biomaterial extracts [18]. |
| Lipopolysaccharide (LPS) | Potent immune stimulant; used to induce an inflammatory response in cell cultures. | Activating the NF-κB pathway in immune cells to study the immunomodulatory properties of BGs [18]. |
Calcium phosphates, bioactive glasses, and titanium alloys each play a distinct yet complementary role in advancing tissue engineering research. Calcium phosphates offer unmatched biomimicry of bone mineral, bioactive glasses provide unparalleled surface reactivity and bonding capacity, and titanium alloys deliver the necessary mechanical robustness for load-bearing applications. The ongoing research and development in this field are increasingly focused on creating smart, composite, and multifunctional materials that not only provide structural support but also actively direct the regenerative process through controlled ion release, surface engineering, and the incorporation of biological molecules. As our understanding of the biological signaling pathways influenced by these materials deepens, the next generation of inorganic and metallic biomaterials will be precisely engineered to resolve complex clinical challenges, from chronic wound healing to the regeneration of large bone defects, thereby fulfilling their critical role in the future of regenerative medicine.
The field of tissue engineering has progressively shifted from using static, passive biomaterials to dynamic, interactive systems that actively participate in the healing process. Smart biomaterials represent a paradigm shift in this domain, engineered to sense and respond to specific physiological or external stimuli in a predictable manner. These stimuli-responsive systems—reacting to temperature, pH, magnetic fields, and other cues—are revolutionizing therapeutic strategies by enabling unprecedented spatiotemporal control over tissue regeneration processes. The evolution toward four-dimensional (4D) materials, which incorporate time as a transformative dimension, allows fabricated constructs to dynamically change their shape or function post-implantation, more closely mimicking the living, adaptive nature of native biological tissues [25].
The core principle underpinning smart biomaterials is their nonlinear feedback to minimal environmental changes, resulting in pronounced alterations in their physical properties, such as shape, volume, solubility, or conformational structure [26] [27]. This responsiveness is critical for advancing tissue engineering beyond static scaffolds to systems that can guide complex tissue morphogenesis, deliver bioactive agents on demand, and integrate seamlessly with the host's physiology. By leveraging characteristic signals of specific tissue microenvironments—such as the slightly acidic pH of tumor tissue or inflamed wounds, or the temperature gradients associated with diseased states—these materials achieve targeted, localized therapeutic action, thereby maximizing efficacy while minimizing off-target effects [28] [29]. The integration of these intelligent systems is paving the way for a new era of personalized and adaptive regenerative medicine.
Fundamental Mechanisms of Stimuli Responsiveness
Smart biomaterials achieve their dynamic functionality through carefully engineered molecular architectures and material compositions that transduce an external signal into a functional output. The mechanisms vary significantly across different stimulus types.
Temperature-Responsive Mechanisms
Temperature-responsive polymers undergo reversible phase transitions at a specific temperature known as the lower critical solution temperature (LCST). Below the LCST, the polymer chains are hydrated and expanded, while above the LCST, they dehydrate and collapse into a hydrophobic, collapsed state. A quintessential example is Poly(N-isopropylacrylamide) (PNIPAm), with an LCST of approximately 32°C [26]. This property is exploited for cell-sheet engineering and drug delivery, where a slight increase from ambient to body temperature triggers material aggregation or release. The LCST can be precisely tuned by copolymerizing with more hydrophilic or hydrophobic monomers [30] [26].
pH-Responsive Mechanisms
pH-sensitive materials contain ionizable functional groups (weak acids or bases) that accept or donate protons in response to changes in environmental pH. Common ionizable groups include carboxylic acids (e.g., in poly(acrylic acid)), which deprotonate at higher pH, and tertiary amines (e.g., in poly(N,N-dimethylaminoethyl methacrylate)), which protonate under acidic conditions [28] [25] [29]. The change in ionization state alters the polymer's charge density, leading to dramatic shifts in chain conformation, solubility, and swelling ratio. This mechanism is particularly useful for targeting specific physiological compartments like the acidic tumor microenvironment (pH ~6.5), endosomes (pH ~5.5-6.0), or lysosomes (pH ~4.5-5.0) [28] [29].
Magneto-Responsive Mechanisms
Magneto-responsive materials are typically composite systems that incorporate magnetic fillers such as iron oxide nanoparticles (Fe₃O₄) into a polymer matrix (e.g., shape-memory polymers or hydrogels) [30]. When exposed to an alternating magnetic field, these nanoparticles generate heat through hysteresis loss or Neel relaxation, which can be used to trigger shape recovery in shape-memory polymers or accelerate drug release from a hydrogel. Alternatively, static magnetic fields can exert mechanical forces on the embedded particles, causing macroscopic deformation or alignment of the material [30]. This allows for non-invasive, remote control over material behavior from outside the body.
Figure 1: Mechanisms of stimulus-responsive behavior in smart biomaterials, showing how different environmental signals trigger distinct material changes that enable specific therapeutic applications.
Material Classes and Their Responsive Behaviors
Shape Memory Polymers (SMPs)
SMPs are a class of stimuli-responsive smart materials capable of recovering from a temporary, deformed shape to their original, permanent configuration upon application of a specific external stimulus. Their molecular architecture typically consists of a fixed phase (netpoints) and a reversible phase (molecular switches) [30]. The fixed phase determines the permanent shape, while the reversible phase softens and allows deformation upon stimulus exposure and solidifies upon stimulus removal to fix the temporary shape. Common triggers include temperature, light, electricity, or magnetic fields. In biomedical applications, SMPs are particularly promising for minimally invasive implantation, where a compact, temporary device can be inserted through a small incision and then expanded to its functional shape in situ [30]. For instance, cardiac occluders made from SMPs can be fixed into a miniaturized configuration for delivery and subsequently recover to their original volumetric state to block pathological blood flow channels upon reaching body temperature [30].
Stimuli-Responsive Hydrogels (SRHs)
SRHs are three-dimensional, crosslinked polymer networks that can absorb large amounts of water while maintaining their structure. Their swelling/deswelling behavior, mechanical properties, and permeability can be drastically altered by environmental cues. Physical hydrogels are formed by reversible, non-covalent interactions like hydrogen bonding, hydrophobic assembly, and host-guest supramolecular interactions, which can impart self-healing properties [27]. Chemical hydrogels are formed by permanent covalent crosslinks (e.g., via "click" chemistry or photo-polymerization), providing greater mechanical stability [27]. A key application is in drug delivery, where a hydrogel can be designed to release its payload in response to a specific tissue's pH or temperature. For example, an injectable Pluronic F127 hydrogel undergoes sol-gel transition near body temperature, forming a depot for sustained drug release [26] [27].
Liquid Crystal Elastomers (LCEs)
LCEs synergistically integrate the molecular alignment of liquid crystals with the elastic properties of polymer networks. This unique combination allows them to demonstrate large, reversible deformations and chromic transitions upon exposure to diverse external stimuli like heat or light [30]. The direction and magnitude of their actuation are programmed by the alignment of the liquid crystal mesogens during fabrication. Their energy-transducing capability, inherent responsiveness, and programmable actuation trajectories position them as frontrunners in next-generation adaptive biomedical systems, particularly for bioinspired artificial muscles and dynamic tissue scaffolds that can provide mechanical cues to cells [30].
Table 1: Key Classes of Smart Biomaterials and Their Characteristics
| Material Class | Stimulus | Key Mechanism | Common Materials | Tissue Engineering Applications |
|---|---|---|---|---|
| Shape Memory Polymers (SMPs) | Temperature, Light, Magnetic Field | Phase transition (glass/rubber) in reversible phase; elasticity of netpoints | Polyurethanes, Poly(ε-caprolactone), Polyvinyl alcohol [30] | Minimally invasive implants, cardiac occluders, self-tightening sutures [30] |
| Stimuli-Responsive Hydrogels (SRHs) | pH, Temperature, Ionic Strength, Light | Swelling/deswelling via ionization, LCST transition, bond cleavage | PNIPAm, Chitosan, Alginate, Poly(acrylic acid), GelMA [25] [27] | Drug delivery depots, 3D cell culture scaffolds, injectable fillers [25] [27] |
| Liquid Crystal Elastomers (LCEs) | Temperature, Light | Reversible change in mesogen orientation coupled with network elasticity | Polysiloxane-based LCEs, Acrylate-based LCEs [30] | Bioinspired actuators, dynamic scaffolds for muscle tissue [30] |
Experimental Protocols and Methodologies
Synthesis of a pH-Responsive Hydrogel for Drug Delivery
Objective: To synthesize an injectable, pH-sensitive hydrogel based on chitosan and poly(acrylic acid) for controlled drug release in the acidic tumor microenvironment.
Materials:
- Chitosan (high molecular weight, >75% deacetylated)
- Poly(acrylic acid) (PAA, Mw ~100,000)
- 1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide (EDC) as a crosslinker
- Doxorubicin hydrochloride (model chemotherapeutic drug)
- Phosphate Buffered Saline (PBS) at various pH (7.4, 6.5, 5.0)
Protocol:
- Polymer Solution Preparation: Dissolve 2% (w/v) chitosan in a 1% (v/v) acetic acid solution under constant stirring until fully dissolved. Separately, prepare a 4% (w/v) solution of PAA in deionized water.
- Hydrogel Formation: Slowly add the PAA solution to the chitosan solution in a 1:1 volume ratio under vigorous stirring. The mixture will form a polyelectrolyte complex via electrostatic interactions between the ammonium groups of chitosan and the carboxylate groups of PAA.
- Crosslinking: Add EDC (20 mM final concentration) to the mixture to crosslink the carboxylic acid groups of PAA with the amine groups of chitosan, forming stable amide bonds. Stir for 2 hours at room temperature.
- Drug Loading: Add doxorubicin (1 mg/mL final concentration) to the pre-gel solution and mix thoroughly. The drug will be physically encapsulated within the forming hydrogel network.
- Gelation and Purification: Transfer the solution into a mold and allow it to crosslink completely for 24 hours at 4°C. Wash the resulting hydrogel extensively with PBS (pH 7.4) to remove unreacted crosslinker and any surface-bound drug.
Characterization and Release Study:
- Swelling Ratio: Weigh the hydrated gel (Wₛ), lyophilize it, and weigh the dry gel (W𝒹). Calculate the swelling ratio as (Wₛ - W𝒹)/W𝒹. Perform this in PBS at pH 7.4, 6.5, and 5.0 to demonstrate pH-dependent swelling.
- In Vitro Drug Release: Immerse the loaded hydrogel in PBS at pH 7.4 and pH 6.5 at 37°C under gentle agitation. At predetermined time intervals, withdraw release medium and analyze doxorubicin concentration using UV-Vis spectroscopy at 480 nm. Replenish with fresh buffer to maintain sink conditions. Expect a significantly faster release at the acidic pH due to protonation of amine groups, leading to hydrogel swelling and bond dissociation [28] [29].
4D Printing of a Temperature-Responsive Shape Memory Polymer
Objective: To fabricate a 4D-printed vascular stent that expands at body temperature using a temperature-responsive shape memory polymer.
Materials:
- Poly(ε-caprolactone) (PCL) pellets, a biodegradable polymer with a melting point of ~60°C and a shape memory transition temperature near 40-45°C.
- Fused Deposition Modeling (FDM) 3D printer with a high-temperature print head.
- Phosphate Buffered Saline (PBS).
- Water bath or incubator set to 37°C and 45°C.
Protocol:
- Filament Preparation: Dry PCL pellets thoroughly in a vacuum oven to remove moisture. Use a filament extruder to process the pellets into a uniform 1.75 mm diameter filament for FDM printing.
- CAD Model and "Permanent Shape" Design: Design a 3D model of the fully expanded stent using computer-aided design (CAD) software.
- 3D Printing ("Programming"): Print the stent model using the FDM printer. The printing process involves heating the PCL above its melting point and depositing it layer-by-layer. As it cools and solidifies below its transition temperature, this printed form is considered the permanent shape.
- Deformation to "Temporary Shape": Heat the printed stent to a temperature above its transition temperature (e.g., 45°C) but below its melting point. While hot and soft, mechanically deform it into a compact, temporary shape (e.g., a stretched, narrow-diameter tube). Cool and fix the stent in this temporary shape under constraint.
- Shape Recovery Testing: Immerse the constrained, temporary-shaped stent in a PBS bath at 37°C (simulating body temperature). Release the constraint and record the recovery process using a camera. Quantify the shape recovery ratio (Rᵣ) as Rᵣ = (εₘ - ε(𝓉)) / εₘ × 100%, where εₘ is the strain in the temporary shape and ε(𝓉) is the strain at time 𝓉 [30] [25].
Figure 2: Experimental workflow for 4D printing a temperature-responsive vascular stent, illustrating the process from digital design to triggered shape recovery in a physiological environment.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Reagents and Materials for Research on Smart Biomaterials
| Reagent/Material | Function/Description | Key Characteristics & Considerations |
|---|---|---|
| Poly(N-isopropylacrylamide) (PNIPAm) | Thermo-responsive polymer for cell sheets & drug delivery [26]. | LCST ~32°C; can be copolymerized to adjust transition temperature; check biocompatibility of final product. |
| Chitosan | Natural, pH-responsive cationic polysaccharide [25] [27]. | Soluble in acidic solutions; biocompatible and biodegradable; reactivity of amine groups allows for chemical modification. |
| Poly(acrylic acid) (PAA) | Anionic, pH-responsive polymer for hydrogels & composites [28] [25]. | Swells at high pH due to carboxylate group ionization; often used with cationic polymers for complexation. |
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable, bioactive hydrogel derived from denatured collagen [27]. | Excellent cell adhesion; mechanical and physical properties tunable via degree of methacrylation and crosslinking. |
| Poly(ε-caprolactone) (PCL) | Biodegradable, synthetic polyester for SMPs & 4D printing [30] [25]. | Low melting point (~60°C); shape memory effect; slow degradation rate suitable for long-term implants. |
| Iron Oxide (Fe₃O₄) Nanoparticles | Magnetic filler for magneto-responsive composites [30]. | Enables remote actuation via magnetic fields; requires homogeneous dispersion in polymer matrix; surface modification may be needed. |
| Pluronic F127 (Poloxamer 407) | Thermo-responsive triblock copolymer for injectable hydrogels [27]. | Forms free-flowing sol at low temps, gel at body temp; reverse thermal gelling; can be used for drug encapsulation. |
| 1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide (EDC) | Zero-length crosslinker for carboxyl and amine groups [27]. | Facilitates formation of amide bonds; used for stabilizing hydrogels; avoids incorporation of large crosslinker molecules. |
Quantitative Data and Performance Metrics
The efficacy of smart biomaterials is quantified through a series of standardized metrics that evaluate their responsive behavior, mechanical properties, and biological performance.
Table 3: Key Performance Metrics for Stimuli-Responsive Biomaterials
| Performance Metric | Definition & Formula | Significance in Tissue Engineering |
|---|---|---|
| Shape Memory Properties | ||
| Shape Fixity Ratio (Rf) | Rf = εu / εm × 100% εu: fixed strain after cooling & load removal ε_m: maximum strain under load [30] | Measures ability to be fixed in a temporary shape. Critical for minimally invasive delivery of implants. |
| Shape Recovery Ratio (Rr) | Rr = (εm - εr) / εm × 100% ε_r: residual strain after recovery [30] | Measures ability to recover the original, permanent shape. Ensures device functionality upon implantation. |
| Drug Release Kinetics | ||
| Cumulative Drug Release | % Released = (M𝓉 / M∞) × 100% M𝓉: drug released at time 𝓉 M∞: total loaded drug [28] [29] | Quantifies release profile. A burst release followed by sustained release is often targeted for therapies. |
| Hydrogel Swelling | ||
| Equilibrium Swelling Ratio (ESR) | ESR = (Wₛ - W𝒹) / W𝒹 Wₛ: weight of swollen gel W𝒹: weight of dry gel [27] | Induces water content and porosity. Affects nutrient diffusion, cell infiltration, and release kinetics. |
| Material Cytocompatibility | ||
| Cell Viability (via MTT/XTT assay) | % Viability = (ODsample / ODcontrol) × 100% [31] | Fundamental requirement. Ensures the biomaterial and its degradation products are non-toxic to cells. |
Smart biomaterials responsive to temperature, pH, and magnetic fields are fundamentally altering the landscape of tissue engineering and regenerative medicine. By transitioning from static implants to dynamic systems that interact intelligently with their biological environment, these materials enable sophisticated applications such as self-fitting implants, spatially and temporally controlled drug delivery, and tissue scaffolds that provide active mechanical cues. The convergence of these materials with 4D printing technologies is particularly powerful, allowing for the fabrication of complex, patient-specific constructs that evolve over time within the body [30] [25].
Despite the remarkable progress, challenges remain in the clinical translation of these systems. The long-term biocompatibility and degradation profiles of some synthetic smart polymers require further investigation [30] [31]. There is also a need to enhance the precision and sensitivity of the responsive mechanisms to finer physiological changes. Future research directions will likely focus on developing multi-responsive materials that can react to a combination of cues in a logical sequence, much like natural biological processes [26]. Furthermore, the integration of bioinstructive capabilities, such as the presentation of specific cell-adhesive ligands or the controlled release of multiple growth factors, will create truly next-generation biomaterials that not only respond to the body but also actively guide and instruct the regenerative process [32] [31]. As the field matures, the role of smart biomaterials is poised to expand, driving innovations in personalized medicine and advanced therapies for tissue regeneration.
Engineering Tissues: Fabrication Techniques and Target Applications
Within the field of tissue engineering, biomaterials are not merely passive structural elements; they are dynamic frameworks that actively orchestrate tissue repair and regeneration. The scaffold, a foundational component, serves as a three-dimensional (3D) analog of the native extracellular matrix (ECM), providing mechanical support and critical biochemical and biophysical cues that direct cell behavior, including adhesion, migration, proliferation, and differentiation [3]. The fabrication technique employed directly determines the scaffold's architectural features—such as porosity, pore size, interconnectivity, and surface topography—which are key determinants of its regenerative performance [33] [34]. This technical guide examines three pivotal scaffold fabrication methods—electrospinning, gas foaming, and particulate leaching—detailing their methodologies, material considerations, and the characteristics of the resulting constructs, thereby framing their essential role within the broader context of biomaterials research for tissue engineering.
Core Fabrication Techniques and Methodologies
Electrospinning
Electrospinning is a versatile technique for producing fibrous scaffolds with a high surface-to-volume ratio that closely mimics the nanoscale architecture of the native ECM [34]. The process involves applying a high voltage to a polymer solution, which creates a charged jet that is drawn toward a grounded collector. As the jet travels, the solvent evaporates, depositing solid, sub-micron to nanoscale fibers that accumulate into a non-woven mat.
- Standard Workflow and Limitations: A conventional setup uses a solid, stationary collector, which often results in densely packed fibers with small pore sizes, typically less than 10 µm [34]. While excellent for cell attachment on the surface, this dense architecture significantly hinders cell infiltration and 3D tissue ingrowth, limiting its application to mostly two-dimensional (2D) cell culture models [34].
- Advanced Modifications to Enhance Cell Infiltration: To overcome these limitations, several modified electrospinning techniques have been developed, as summarized in Table 1.
Table 1: Advanced Electrospinning Techniques for Enhanced Cell Infiltration
| Technique | Core Principle | Key Outcome/Advantage | Exemplary Material(s) |
|---|---|---|---|
| Micro/Nano Fiber Hybrid [34] | Simultaneous electrospinning of microfibers (creating large pores) and nanofibers (promoting cell adhesion). | Creates a hierarchical structure; microfibers provide a framework for cell migration, while nanofibers enhance cell-scaffold interaction. | Poly(ɛ-caprolactone) (PCL) |
| Electrospinning with Salt Leaching [34] | Incorporation of salt particles (e.g., 90–106 µm) into the fiber-deposition process, followed by their dissolution post-fabrication. | Generates large, interconnected pores (up to ~200 µm) and delaminated layers within the scaffold, facilitating deep cell penetration. | PCL; Hyaluronic acid/Collagen |
| Cryogenic Electrospinning [34] | Electrospinning onto a low-temperature collector, causing moisture to freeze into ice crystals that act as a porogen. The crystals are later removed via freeze-drying. | Allows precise control over pore size (10–500 µm) and high porosity, enabling the creation of thick, 3D-like scaffolds. | Polylactic acid (PLA); Silk Fibroin (SF) |
| Gas Foaming [35] | Post-treatment of an electrospun mat with a gas-foaming agent (e.g., NaBH₄), which generates in-situ gas bubbles that puff the dense mat into a 3D structure. | Transforms 2D mats into low-density, fluffy 3D scaffolds with large pore areas and high porosity, excellent for cell infiltration. | PLCL/SF crosslinked with Hyaluronic Acid |
The following workflow diagram illustrates the key steps in creating a 3D gas-foamed electrospun scaffold, a method proven to enhance cartilage regeneration [35]:
Gas Foaming
The gas foaming technique is used to create highly porous, 3D structures from pre-formed polymer mats, particularly those derived from electrospinning. Its primary advantage is the ability to create 3D scaffolds without the use of organic solvents, which could be cytotoxic.
- Detailed Experimental Protocol (Based on 3DHAS Scaffold for Cartilage Regeneration) [35]:
- Scaffold Precursor Fabrication: A 2D nanofibrous mat is first fabricated using a Dynamic Liquid Support (DLS) electrospinning system. The material used is a blend of poly(l-lactide-co-ε-caprolactone) (PLCL) and silk fibroin (SF).
- Cross-linking: The electrospun mat is cross-linked with hyaluronic acid (HA) to improve its biomechanical properties and bioactivity.
- Gas Foaming Reaction: The cross-linked mat is submerged in an aqueous sodium borohydride (NaBH₄) solution. The chemical decomposition of NaBH₄ (NaBH₄ + 2H₂O → NaBO₂ + 4H₂↑) generates hydrogen gas in situ. The trapped gas bubbles within the polymer matrix cause the dense mat to expand volumetrically into a fluffy, porous 3D structure.
- Freeze-Drying: The gas-foamed scaffold is subsequently frozen and lyophilized to remove water and permanently set the porous architecture.
- Resulting Scaffold Properties: Scaffolds produced via this method exhibit low density, large pore area, high porosity, excellent water absorption capacity, and mechanical stability, while preserving beneficial nanotopographical cues from the original electrospun fibers [35].
Particulate Leaching (Salt Leaching)
Particulate leaching is a straightforward and widely used method to introduce controlled porosity into scaffolds. The pore size and overall porosity can be precisely tuned by the size and volume of the porogen particles used.
- Standard Protocol:
- Mixing: A polymer solution is thoroughly mixed with insoluble porogen particles, typically salt (e.g., sodium chloride) or sugar, of a specific sieved size.
- Casting: The polymer-porogen composite is cast into a mold and the solvent is allowed to evaporate, leaving a solid composite.
- Leaching: The solid composite is immersed in a solvent (e.g., water) that dissolves the porogen particles but not the polymer. This process leaves behind a porous network where the porogen particles were located.
- Integrated Electrospinning-Particulate Leaching Protocol [34]:
- Integration: Salt particles (e.g., 90–106 µm in diameter) are introduced at intervals into the Taylor Cone during the electrospinning process using a sheath surrounding the needle. This results in a uniform fiber network with a well-distributed salt particles.
- Fiber Collection & Leaching: The fibers and salt are collected, and the scaffold is subsequently placed in water to leach out the salt.
- Outcome: This hybrid method creates electrospun scaffolds with improved porosity and large, interconnected pores, which have been shown to support cell infiltration depths of up to 4 mm [34].
3D Printing as a Complementary Advanced Technique
While not the focus of this guide, 3D printing (additive manufacturing) is a pivotal technology that enables unparalleled control over scaffold macro- and micro-architecture. It allows for the fabrication of scaffolds with patient-specific geometries and perfectly controlled, reproducible pore arrangements [33] [15]. For example, beta-tricalcium phosphate (β-TCP) scaffolds can be 3D-printed with exact pore sizes (e.g., 500 µm vs. 1000 µm) to systematically study the effect of pore size on osteogenic differentiation under dynamic culture conditions [33]. Similarly, composites like PLGA/nHA/GO can be printed using low-temperature 3D printing to create scaffolds with optimal pore size and microtopography for bone regeneration [15].
Performance Comparison and Quantitative Data
The choice of fabrication technique directly impacts the scaffold's physical properties, which in turn dictate its biological performance. Table 2 consolidates quantitative data from the cited research, providing a direct comparison of key parameters.
Table 2: Comparative Performance of Scaffolds from Different Fabrication Techniques
| Fabrication Technique | Material | Porosity / Pore Size | Mechanical Properties | Cell Infiltration / Biological Performance |
|---|---|---|---|---|
| 3D Printed β-TCP [33] | Beta-Tricalcium Phosphate | Precisely defined 500 µm and 1000 µm pores | Lower mechanical strength in 1000 µm group | Superior osteogenic differentiation in 1000 µm group under perfusion; homogeneous cell distribution |
| Gas Foamed Electrospinning [35] | PLCL/SF crosslinked with HA | High porosity, large pore area | Stable mechanical properties | Excellent cellular infiltration and chondrification; promoted articular cartilage regeneration in rabbits |
| Electrospinning + Salt Leaching [34] | PCL | ~200 µm | Not specified | ~4 mm infiltrated depth with 70% cell coverage after 3 weeks (CFK2 cells) |
| Cryogenic Electrospinning [34] | PLA | 10–500 µm (adjustable) | Not specified | Fibroblasts penetrated 50 µm-thick scaffold under static culture; good infiltration in vivo after 56 days |
| 3D Printed Composite [15] | PLGA/nHA/GO | Optimal pore size and microtopography | Enhanced mechanical properties | Improved BMSC adhesion and proliferation, indicating good biocompatibility |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for Scaffold Fabrication and Evaluation
| Item | Function / Relevance | Example from Research |
|---|---|---|
| Poly(ɛ-caprolactone) (PCL) | A biodegradable, synthetic polymer widely used in electrospinning and hybrid scaffold fabrication due to its excellent processability. | Used in electrospinning with salt leaching and micro/nano fiber hybrid scaffolds [34]. |
| Beta-Tricalcium Phosphate (β-TCP) | A bioceramic known for its osteoconductivity and resorbability; used for bone tissue engineering scaffolds, often via 3D printing. | Fabricated into 500 µm and 1000 µm pore size scaffolds to study osteogenesis [33]. |
| PLGA / nHA / GO Composite | A composite material where PLGA is a structural polymer, nHA mimics bone mineral, and GO can enhance mechanical properties. | Used in low-temperature 3D printing to create scaffolds for bone defect repair [15]. |
| Hyaluronic Acid (HA) | A natural glycosaminoglycan found in ECM; used as a bioactive component to improve biocompatibility and promote chondrogenesis. | Cross-linked into PLCL/SF gas-foamed scaffolds for cartilage regeneration [35]. |
| Sodium Borohydride (NaBH₄) | A chemical foaming agent that decomposes in water to generate hydrogen gas for the gas foaming process. | Used to expand 2D electrospun mats into 3D porous scaffolds [35]. |
| Bone Marrow Mesenchymal Stem Cells (BMSCs) | A primary cell type commonly used for in vitro biocompatibility and osteogenic/chondrogenic differentiation assays. | Co-cultured with scaffolds to evaluate cell adhesion, proliferation, and differentiation potential [33] [15]. |
The strategic selection and refinement of scaffold fabrication techniques are paramount to advancing the field of tissue engineering. As demonstrated, methods like electrospinning, gas foaming, and particulate leaching—individually or in combination—enable the creation of biomaterial scaffolds with tailored architectural and mechanical properties. The ongoing innovation in these fabrication protocols is directly aligned with the core objective of biomaterials research: to engineer synthetic microenvironments that not only provide structural support but also actively recapitulate the dynamic and instructive nature of the native ECM. By precisely controlling parameters such as pore size, interconnectivity, and topography, researchers can develop next-generation scaffolds that guide cellular processes and vascularization more effectively, thereby bridging the gap between laboratory research and successful clinical translation in regenerative medicine.
In tissue engineering, biomaterials have evolved from passive structural elements into active, instructive components that direct biological responses. These materials—engineered to interact with biological systems—provide the essential scaffolding that supports cell adhesion, proliferation, and differentiation, thereby enabling the fabrication of functional tissues [36]. The emergence of 3D bioprinting technology has further elevated the importance of biomaterials, as they form the "bioinks" that are deposited layer-by-layer to create complex, three-dimensional tissue constructs [37]. This advancement represents a significant leap beyond traditional two-dimensional cell cultures, allowing for the creation of tissue models that more accurately mimic the native tissue microenvironment through direct cell-cell signaling and cell-matrix interactions [36].
The limitations of conventional monolayer cultures and animal models in predicting human physiological responses have accelerated the development of these advanced in vitro models [38]. However, the field has faced significant challenges, particularly the historical reliance on tumor-derived extracellular matrices like Matrigel, which pose concerns due to their xenogeneic nature and variable composition [38]. This has driven innovation in biomaterial design, leading to the creation of sophisticated, well-defined alternatives that offer greater control over mechanical properties, biodegradation kinetics, and bioactivity [36]. The progression to 4D bioprinting introduces an additional temporal dimension, where smart biomaterials enable printed constructs to change their shape or functionality over time in response to specific stimuli, creating dynamic biological structures that better simulate the adaptive nature of living tissues [39] [40].
Table 1: Key Biomaterial Classes in Bioprinting and Their Characteristics
| Material Class | Representative Examples | Key Properties | Primary Applications |
|---|---|---|---|
| Natural Polymers | Collagen, gelatin, alginate, chitosan, hyaluronic acid [36] [41] | Innate biocompatibility, biological recognition, enzymatic degradation | Hydrogels for cell encapsulation, soft tissue models |
| Synthetic Polymers | PLA, PCL, PGA, PEG [42] [41] | Tunable mechanical properties, controlled degradation, reproducible manufacturing | Customizable scaffolds, load-bearing structures |
| Composite Materials | GelMA with heparin [39], PCL with ceramics [41] | Combined advantages of multiple materials, enhanced functionality | Vascularized constructs, bone tissue engineering |
| Smart Materials | Shape memory polymers, moisture-responsive hydrogels [39] [40] | Stimuli-responsive (temperature, pH, light), dynamic shape change | 4D bioprinting, self-assembling structures |
The State of 3D Bioprinting: Technologies and Biomaterial Interfaces
Fundamental Bioprinting Technologies
3D bioprinting employs additive manufacturing principles to process living cells and biomaterials into structured tissue constructs. The technology encompasses several core approaches, each with distinct mechanisms for bioink deposition and solidification. Extrusion-based bioprinting, one of the most prevalent techniques, utilizes pneumatic or mechanical pressure to continuously deposit bioink filaments in a layer-by-layer fashion [41]. This method accommodates high cell densities and a wide range of material viscosities, making it suitable for creating dense tissue constructs. Inkjet-based bioprinting operates by ejecting discrete droplets of low-viscosity bioinks through thermal or piezoelectric actuators, offering high printing speeds and resolution but limited to lower cell concentrations [37]. Stereolithography (SLA) and digital light processing (DLP) techniques employ focused light patterns to selectively photocrosslink light-sensitive bioinks in a vat, achieving excellent resolution and structural complexity [41]. Laser-assisted bioprinting uses laser pulses to transfer bioink from a donor layer to a substrate, providing high resolution and viability but with more complex instrumentation [37].
The success of these bioprinting modalities hinges on their integration with advanced biomaterials that meet stringent biological and mechanical requirements. Printable biomaterials must demonstrate appropriate viscosity for deposition, structural integrity post-printing, and biocompatibility to support cell viability and function [36]. Furthermore, these materials increasingly incorporate bioactive cues to guide specific cellular responses, moving beyond passive scaffolding to active tissue induction.
Advanced Biomaterial Formulations for 3D Bioprinting
Innovations in biomaterial science have produced sophisticated bioinks that address the competing demands of printability, mechanical stability, and biological functionality. Hybrid and composite bioinks have emerged as particularly promising strategies, combining the advantageous properties of multiple materials. For instance, methacrylated gelatin (GelMA) has gained widespread adoption due to its tunable physical properties via light-initiated crosslinking and presence of cell-adhesive motifs [39]. In one application, researchers developed porous shape memory cryogel microspheres (CMS) from GelMA that supported vascularized bone tissue formation when loaded with human bone marrow stromal cells (hBMSCs) and human umbilical vein endothelial cells (HUVECs) [39].
Decellularized extracellular matrix (dECM) bioinks represent another advanced approach, retaining the complex biochemical composition of native tissues while eliminating cellular components that could trigger immune responses [42]. These materials provide tissue-specific cues that enhance differentiation and functional maturation of embedded cells. Similarly, composite approaches blending natural and synthetic components enable the creation of scaffolds that offer both biological recognition and mechanical robustness. For example, incorporating chitosan into polylactic acid (PLA) scaffolds has been shown to enhance cell adhesion and alkaline phosphatase activity while modulating degradation rates [39].
Table 2: Global 3D Bioprinting Market Overview and Projections
| Metric | 2024 Value | 2025 Value | 2029 Projection | CAGR (2025-2029) |
|---|---|---|---|---|
| Market Size | $1.86 billion [37] | $2.21 billion [37] | $5.11 billion [37] | 23.3% [37] |
| Tissue Engineering Market | $4.8 billion [43] | $5.4 billion [43] | $9.8 billion (by 2030) [43] | 12.8% (2025-2030) [43] |
| Dominant Product Segment | Scaffolds [43] | - | - | - |
| Leading Region | North America [37] [43] | - | - | - |
Core 4D Bioprinting Concept: This diagram illustrates the fundamental principle of 4D bioprinting, where stimuli-responsive biomaterials enable the creation of dynamic tissue constructs that change their shape, properties, or functionality over time when exposed to specific external triggers.
The Emergence of 4D Bioprinting: Dynamic Biomaterials
Principles and Mechanisms of 4D Bioprinting
4D bioprinting represents a paradigm shift from static to dynamic tissue fabrication by incorporating the dimension of time into printed constructs [39]. This advanced approach utilizes smart biomaterials that undergo predetermined transformations in response to specific external stimuli, enabling the creation of structures that evolve their shape, properties, or functionality post-printing [40]. The fourth dimension—time—allows these biofabricated structures to adapt, self-assemble, or change in response to environmental cues such as temperature, moisture, pH, or light [39]. The transformation mechanisms in 4D printing can be achieved through various approaches, including the use of single smart materials that alter their configuration when stimulated, or bilayer structures composed of materials with differing properties that respond inhomogeneously to stimuli, creating bending or folding motions [39].
The core elements of 4D printing technology encompass five essential components: the printing technique itself, the additive manufacturing medium (bioinks), the specific stimulus, the interaction mechanism between stimulus and material, and sophisticated modeling approaches to predict and control the dynamic behavior [39]. Mathematical modeling is particularly crucial for forecasting shape evolution after printing and preventing structural collisions during self-assembly processes. This modeling includes solving both forward problems (predicting the final shape based on material properties and stimulus characteristics) and inverse problems (determining the necessary material structure or print paths to achieve a desired shape transformation) [39].
Classes of Smart Biomaterials in 4D Bioprinting
The functionality of 4D bioprinting systems depends fundamentally on the smart biomaterials employed, which can be categorized based on their responsiveness to different stimuli:
Moisture-responsive hydrogels represent one of the most prominent material classes, consisting of cross-linked polymer networks that can swell up to 200% of their original volume upon water exposure due to their hydrophilic nature [39]. This moisture sensitivity enables significant expansion, folding, stretching, and bending transformations, making them ideal for creating dynamic micro-actuators and reversible origami structures. These hydrogels also support the encapsulation of bioactive compounds that facilitate cell proliferation and differentiation. Commonly used polymers in this category include poly(ethylene glycol) (PEG), poly(N-isopropylacrylamide) (PNIPAM), collagen, gelatin, and alginate [39]. A notable application demonstrated by Jiang et al. involves collagen scaffolds that return to their original shape upon moisture exposure while promoting chondrocyte adhesion and growth [39].
Thermoresponsive shape memory polymers and elastomers constitute another important category, capable of changing their shape in response to temperature variations [39] [40]. These materials can be programmed to "remember" a permanent shape and transition from a temporary deformed state back to this original configuration when heated above a specific transition temperature. This property is particularly valuable for creating minimally invasive medical devices and implants that can be inserted in a compact form and then expand to their functional shape at body temperature [40].
Other stimuli-responsive materials include pH-sensitive polymers that undergo conformational changes in different acidity environments, and light-responsive materials that can be precisely controlled using specific wavelengths [39]. These diverse smart material systems enable the temporal programming of tissue constructs, allowing them to evolve their structure and functionality to better mimic the dynamic nature of native tissues.
Experimental Protocols and Methodologies
Protocol 1: Bioprinting Vascularized Bone Tissue Constructs
This protocol outlines the methodology for creating vascularized bone tissue using methacrylated gelatin (GelMA)-based cryogel microspheres (CMS), adapted from Yuan et al. [39].
Materials and Reagents:
- Methacrylated gelatin (GelMA)
- Photoinitiator (e.g., LAP or Irgacure 2959)
- Human bone marrow stromal cells (hBMSCs)
- Human umbilical vein endothelial cells (HUVECs)
- Osteogenic differentiation medium (ascorbic acid, β-glycerophosphate, dexamethasone)
- Endothelial cell growth medium
- Sterile phosphate-buffered saline (PBS)
- Crosslinking solution (e.g., CaCl₂ for ionic crosslinking)
Equipment:
- Digital light processing (DLP) or stereolithography (SLA) bioprinter
- UV light source (wavelength 320-400 nm, intensity 5-20 mW/cm²)
- Laminar flow hood for sterile procedures
- Cell culture incubator (37°C, 5% CO₂)
- Centrifuge
- Vacuum degassing system
Procedure:
- Bioink Preparation: Prepare 10% (w/v) GelMA solution in sterile PBS containing 0.5% (w/v) photoinitiator. Gently mix at 37°C until fully dissolved, then vacuum degas to remove air bubbles.
- Cell Preparation: Culture and expand hBMSCs and HUVECs separately. Harvest cells at 80-90% confluence using standard trypsinization. Centrifuge at 300 × g for 5 minutes and resuspend in appropriate medium. Adjust cell density to 5 × 10^6 cells/mL for hBMSCs and 3 × 10^6 cells/mL for HUVECs.
- Bioink Cell Loading: Mix cell suspensions with GelMA bioink to achieve final concentrations of 1 × 10^6 cells/mL for hBMSCs and 5 × 10^5 cells/mL for HUVECs. Maintain bioink temperature at 20-24°C during printing to ensure optimal viscosity.
- Bioprinting Parameters: Using a DLP bioprinter, set layer thickness to 100 μm and exposure time to 15-30 seconds per layer based on calibration tests. Print the construct according to the digital model with incorporated microchannel networks (150-300 μm diameter).
- Post-printing Crosslinking: After printing, immerse constructs in CaCl₂ solution (2% w/v) for 5 minutes for additional ionic crosslinking, then rinse with PBS.
- Culture and Differentiation: Transfer constructs to osteogenic medium for hBMSCs differentiation. For coculture systems, use a 1:1 mixture of osteogenic and endothelial growth media. Change media every 2-3 days for up to 4 weeks.
- Analysis: Assess osteogenic differentiation by alkaline phosphatase activity (day 7-14), calcium deposition (Alizarin Red staining, day 21-28), and expression of osteogenic markers (RUNX2, OPN, OCN) via RT-qPCR. Evaluate vascular network formation by CD31 immunostaining and confocal microscopy.
Protocol 2: 4D Bioprinting of Temperature-Responsive Bilayer Constructs
This protocol describes the fabrication of a temperature-responsive bilayer structure capable of shape-changing behavior, utilizing combinations of smart materials [39] [40].
Materials and Reagents:
- Shape memory polymer (e.g., PCL-based or PLA-based)
- Thermoresponsive hydrogel (e.g., PNIPAM or Pluronic F127)
- Photoinitiator for crosslinking
- Cell culture medium if printing with cells
- Dulbecco's Modified Eagle Medium (DMEM)
Equipment:
- Multi-material extrusion bioprinter with temperature-controlled printheads
- Heated print bed
- UV crosslinking system (for photopolymerizable materials)
- Environmental chamber for controlled temperature conditioning
- Sterile petri dishes or multi-well plates
Procedure:
- Material Preparation:
- Layer A (Active): Prepare thermoresponsive hydrogel (e.g., 20% PNIPAM) with 0.5% photoinitiator. Heat to 4°C to ensure complete dissolution and degas under vacuum.
- Layer B (Passive): Prepare shape memory polymer (e.g., PCL) by heating to 70-80°C until molten. For photopolymerizable versions, add 1% photoinitiator.
Printing Process:
- Set printhead temperatures: 4°C for Layer A (hydrogel) and 70°C for Layer B (SMP).
- Set build plate temperature to 20°C.
- Program printing path to create a bilayer structure with specific geometric patterns.
- Print Layer A first with nozzle diameter 0.2-0.4 mm, pressure 20-40 kPa, printing speed 5-10 mm/s.
- Print Layer B directly onto Layer A with nozzle diameter 0.2-0.4 mm, pressure 30-50 kPa, printing speed 10-15 mm/s.
- Apply UV light (365 nm, 10 mW/cm² for 60 seconds) after each layer if using photopolymerizable materials.
Shape Programming:
- Heat the printed structure to 50°C (above transition temperature of SMP).
- Mechanically deform to temporary shape while maintaining temperature.
- Cool to 20°C while maintaining deformation.
- Release mechanical force.
Shape Recovery:
- Immerse construct in warm medium (37°C) or transfer to 37°C incubator.
- Observe and record shape transformation over time (typically 5-30 minutes).
- For quantitative analysis, track angular changes or linear dimensions at 10-second intervals.
Characterization:
- Measure shape recovery ratio: Rr(t) = (εm - εt(t)) / (εm - εp) × 100%, where εm is maximum strain, εt(t) is strain at time t, and εp is permanent strain.
- Evaluate cell viability if printed with cells using Live/Dead staining at 24, 48, and 72 hours post-recovery.
4D Bioprinting Workflow: This diagram outlines the key stages in the 4D bioprinting process, from initial bioink formulation through the final maturation and analysis of the dynamic tissue construct, highlighting the critical post-printing phase where shape transformation occurs.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Advanced Bioprinting Applications
| Reagent/Material | Function | Example Applications | Key Considerations |
|---|---|---|---|
| Methacrylated Gelatin (GelMA) | Photocrosslinkable hydrogel providing cell-adhesive motifs [39] | Vascularized bone tissue, soft tissue models | Degree of methacrylation controls mechanical properties and degradation rate |
| Poly(ethylene glycol) Diacrylate (PEGDA) | Synthetic hydrogel with tunable mechanical properties [42] | Drug delivery systems, neural tissue engineering | Bioinert unless functionalized with cell-adhesive peptides |
| Decellularized ECM (dECM) | Tissue-specific biochemical cues [42] | Organ-specific models, enhanced differentiation | Source tissue affects composition; must verify removal of cellular antigens |
| Shape Memory Polymers (PCL, PLA) | Enable 4D shape transformation upon stimulation [40] | Self-fitting implants, vascular grafts | Transition temperature must be optimized for physiological compatibility |
| Alginate | Ionic-crosslinkable polysaccharide for rapid gelation [36] | Cell encapsulation, wound healing | Limited cell adhesion without modification with RGD peptides |
| Hyaluronic Acid Methacrylate (HAMA) | ECM-derived glycosaminoglycan for hydrogel formation [42] | Cartilage engineering, stem cell niches | Molecular weight affects physical properties and biological activity |
| Tricalcium Phosphate/Hydroxyapatite | Mineral components for osteoconductivity [41] | Bone tissue engineering, orthopedic implants | Ratio and crystal structure influence resorption rates and bone formation |
| LAP Photoinitiator | Visible light photoinitiator for cell-friendly crosslinking [37] | Volumetric bioprinting, high-resolution structures | Superior cytocompatibility compared to traditional UV initiators |
Current Challenges and Future Perspectives
Despite significant advancements, several substantial challenges impede the widespread clinical translation of 3D and 4D bioprinting technologies. Vascularization remains a primary obstacle, as establishing functional vascular networks within bioprinted constructs is essential for nutrient delivery and waste removal in thick tissues [41]. Current approaches include incorporating angiogenic factors, creating sacrificial channels that can be evacuated to form perfusable networks, and designing multi-material constructs that support endothelial cell self-assembly into capillary structures [41]. Scalability presents another significant challenge, as maintaining cell viability and structural integrity becomes increasingly difficult with larger tissue volumes and longer printing times [41]. This limitation currently restricts clinical application to thinner tissues like skin or smaller implants.
The regulatory landscape for bioprinted tissues and organs remains complex, with the FDA and other regulatory bodies still developing appropriate frameworks for these advanced therapeutic products [44]. The classification of these products—as biologics, medical devices, or combination products—affects the approval pathway and requirements. As of 2025, only four cell-based tissue engineering therapies have received FDA approval, highlighting the stringent regulatory hurdles [44]. Key considerations include ensuring consistent cell potency, characterizing cellular heterogeneity, and validating manufacturing processes according to current Good Manufacturing Practices (cGMP) [44].
Future advancements in bioprinting will likely be driven by several converging technologies. The integration of artificial intelligence with bioprinting processes enables predictive modeling of tissue behavior, optimization of biomaterial compositions, and generation of complex tissue designs that would be difficult to create manually [41]. Multi-material printing capabilities continue to advance, allowing the creation of heterogeneous tissues with precise spatial arrangements of different cell types and biomaterials that better mimic native tissue complexity [41]. Nanotechnology integration offers opportunities to enhance material properties and incorporate additional functionality, such as conductive nanomaterials for neural or cardiac tissues that require electrical signaling [42] [41].
The trajectory of bioprinting points toward increasingly sophisticated tissue models for drug screening, disease modeling, and ultimately, clinical transplantation. As biomaterials evolve from passive scaffolds to active, instructive microenvironments, and as 3D printing advances to 4D dynamic systems, the field moves closer to its ultimate goal: the faithful recreation of functional human tissues and organs for therapeutic applications. The convergence of material science, biology, and engineering will continue to drive this exciting field forward, potentially transforming the future of regenerative medicine and drug development.
Bone tissue engineering represents a paradigm shift in addressing large bone defects caused by trauma, tumor resection, infection, and degenerative diseases [45]. With approximately 2.2 million bone graft procedures performed annually worldwide, the limitations of conventional treatments—autografts and allografts—have accelerated the development of advanced biomaterials as the foundation for regenerative strategies [46]. Biomaterials for bone tissue engineering must fulfill three fundamental requirements: osteoconduction (providing a scaffold that supports bone cell adhesion, proliferation, and extracellular matrix formation), osteoinduction (inducing stem cell differentiation toward osteogenic lineage), and osteogenesis (facilitating new bone formation) [45] [47].
Ceramics and composites have emerged as particularly promising biomaterial classes due to their ability to mimic the natural bone mineral phase while offering tunable physicochemical properties [45] [48]. This technical guide examines the current state of ceramic and composite biomaterials for osteoconductive bone tissue engineering, with emphasis on material properties, biological mechanisms, experimental methodologies, and translational applications relevant to researchers and drug development professionals.
Core Principles: Osteoconduction and Material Requirements
Osteoconduction refers to the ability of a biomaterial to support the attachment, proliferation, and migration of osteogenic cells along its surface or through its three-dimensional structure, ultimately guiding new bone formation [45] [47]. Effective osteoconductive biomaterials must meet specific criteria to function successfully in bone regeneration applications.
The biological sequence of osteoconduction involves: (1) protein adsorption from blood and tissue fluids onto the material surface immediately upon implantation; (2) osteoprogenitor cell recruitment and attachment; (3) cell proliferation and migration through the scaffold architecture; (4) extracellular matrix deposition and mineralization; (5) scaffold integration with host bone tissue [45] [46]. The material properties that govern these processes include surface chemistry, topography, porosity, and mechanical compatibility with native bone tissue.
Table 1: Critical Material Properties for Optimal Osteoconduction
| Property | Optimal Range | Biological Significance |
|---|---|---|
| Porosity | 50-90% | Enables cell migration, vascular invasion, nutrient/waste exchange [45] |
| Pore Size | 100-500 μm | Facilitates osteoblast infiltration, matrix deposition, and capillary formation [45] |
| Surface Roughness | Micron to submicron scale | Enhances protein adsorption and cell adhesion through increased surface area [45] |
| Compressive Strength | 2-12 MPa (cancellous bone range) | Provides structural support while matching bone mechanical properties [49] |
The microstructure of scaffolds plays a crucial role in bone regeneration, with three-dimensional porous structures containing interconnected and open porosity accelerating the healing process by ensuring adequate oxygen and nutrient diffusion, waste product elimination, and providing space for cell proliferation and vascularization [45].
Ceramic Biomaterials for Osteoconduction
Calcium Phosphate Ceramics
Calcium phosphate (CaP) ceramics constitute the most extensively investigated class of osteoconductive biomaterials due to their chemical similarity to the mineral phase of natural bone [45]. The predominant CaP ceramics include:
- Hydroxyapatite (HA) - Ca~10~(PO~4~)~6~(OH)~2~: Characterized by excellent biocompatibility and bioactivity but relatively slow degradation rates [45] [49]
- β-Tricalcium Phosphate (β-TCP) - Ca~3~(PO~4~)~2~: Exhibits faster resorption compared to HA and can be actively remodeled by osteoclasts [46]
- Biphasic Calcium Phosphates (BCP): Combinations of HA and β-TCP that balance stability and resorption [45]
Table 2: Comparative Properties of Principal Calcium Phosphate Ceramics
| Ceramic Type | Ca/P Ratio | Compressive Strength (MPa) | Degradation Rate | Osteoconductivity |
|---|---|---|---|---|
| Hydroxyapatite (HA) | 1.67 | 5-12 | Very slow | Excellent |
| β-Tricalcium Phosphate (β-TCP) | 1.50 | 2-10 | Moderate to fast | Excellent |
| Biphasic Calcium Phosphate (BCP) | 1.55-1.65 | 4-11 | Tunable | Excellent |
The mechanism of HA osteoconduction involves the formation of a biological apatite layer on its surface through ionic exchange with the physiological environment, which facilitates the adsorption of bone-specific proteins and promotes osteoblast adhesion [45]. β-TCP undergoes dissolution-reprecipitation processes that release calcium and phosphate ions, stimulating osteogenic differentiation of mesenchymal stem cells and enhancing bone matrix mineralization [46].
Silicate-Based Ceramics
Calcium silicate ceramics have gained prominence due to their enhanced bioactivity and ability to release silicon ions, which stimulate osteogenesis at the molecular level [48]. Recent developments have focused on zirconium-containing silicates such as baghdadite (Ca~3~ZrSi~2~O~9~), which demonstrates an optimal balance of bioactivity and mechanical stability [48]. The incorporation of zirconium ions into the silicate structure reduces degradation rates while maintaining biocompatibility, addressing a significant limitation of pure calcium silicate ceramics [48].
Composite Scaffolds: Enhancing Functionality
Composite materials combine ceramic components with polymers or other materials to create systems with synergistic properties that overcome the limitations of single-phase biomaterials [49] [50]. The strategic combination of materials enables tuning of mechanical properties, degradation profiles, and biological responses.
Polymer-Ceramic Composites
The integration of ceramics with natural or synthetic polymers represents the most prevalent approach to composite scaffold development:
- Natural Polymer-Based Composites: Chitosan, collagen, and alginate combined with HA or β-TCP provide biomimetic environments that enhance cell-material interactions [50]. Chitosan-based composites leverage the polymer's structural similarity to glycosaminoglycans found in native extracellular matrix while benefiting from the osteoconductivity of ceramic fillers [50].
- Synthetic Polymer-Based Composites: Polycaprolactone (PCL), polylactic acid (PLA), and poly(lactic-co-glycolic acid) (PLGA) offer controlled degradation kinetics and processability. PCL-ceramic composites have demonstrated exceptional potential, with studies showing that PCL with 20% β-TCP provides optimal mechanical support while maintaining flexibility for surgical handling [49].
Table 3: Characterization of PCL-Ceramic Composite Scaffolds
| Composite Formulation | Tensile Strength (MPa) | Elongation at Break (%) | Cell Viability (%) | Key Applications |
|---|---|---|---|---|
| PCL + 10% HA | 8.5 ± 0.7 | 210 ± 15 | 98.2 ± 3.1 | Cranial defects, non-load bearing |
| PCL + 20% HA | 11.2 ± 0.9 | 185 ± 12 | 97.5 ± 2.8 | Maxillofacial reconstruction |
| PCL + 10% β-TCP | 9.1 ± 0.8 | 205 ± 14 | 99.1 ± 2.5 | Spinal fusion, dental defects |
| PCL + 20% β-TCP | 12.8 ± 1.1 | 165 ± 11 | 98.3 ± 3.2 | Long bone defects, load-sharing |
Bioactive Composite Mechanisms
The osteoconductive efficacy of composite scaffolds arises from multiple synergistic mechanisms. Ceramic components release calcium, phosphate, and silicate ions that stimulate osteogenic differentiation through activation of specific signaling pathways, including Wnt/β-catenin and BMP/Smad [46] [48]. The polymer matrix provides mechanical integrity and can be functionalized with bioactive molecules to further enhance biological activity [50]. Surface topography and chemistry of composites direct cell behavior through integrin-mediated adhesion and activation of focal adhesion kinase (FAK) signaling [45].
Experimental Protocols and Methodologies
Scaffold Fabrication and Characterization
Melt-Extrusion 3D Printing Protocol:
- Materials Preparation: Blend PCL pellets with ceramic powders (HA or β-TCP) at 10-20% w/w concentration. Dry mixtures at 60°C for 24 hours to remove moisture [49]
- Extrusion Parameters: Nozzle diameter: 200-400 μm; Printing temperature: 90-120°C; Platform temperature: 40-60°C; Pressure: 4-6 bar; Printing speed: 5-10 mm/s [49]
- Post-Processing: Anneal printed scaffolds at 60°C for 2 hours to relieve internal stresses
- Characterization: Assess morphological properties via scanning electron microscopy (SEM), mechanical properties by tensile/compression testing, and thermal stability through thermogravimetric analysis (TGA) [49]
Sol-Gel Synthesis of Doped Ceramics (for baghdadite and other silicate ceramics):
- Precursor Preparation: Combine tetraethyl orthosilicate (TEOS), calcium nitrate tetrahydrate, and zirconium propoxide in stoichiometric ratios. For Ag-doped formulations, add silver nitrate (2-6 mol%) to impart antibacterial properties [48]
- Hydrolysis and Condensation: Maintain pH at 2-3 using nitric acid; age gel for 24 hours at 60°C
- Calcination: Heat treatment at 800-1300°C for 2 hours to crystallize the ceramic phase
- Characterization: Phase analysis via X-ray diffraction (XRD); functional groups by Raman spectroscopy; morphology and elemental composition by SEM-EDS [48]
In Vitro Biological Evaluation
Cell Seeding and Culture:
- Cell Types: Human bone marrow mesenchymal stem cells (hBMSCs), primary osteoblasts, or cell lines (MG-63, SAOS-2) [49] [48]
- Seeding Density: 5,000-50,000 cells/cm² depending on scaffold porosity
- Culture Medium: α-MEM supplemented with 10% FBS, 50 μg/mL ascorbic acid, 10 mM β-glycerophosphate, and 10 nM dexamethasone for osteogenic differentiation [48]
Osteogenic Differentiation Assessment:
- Alkaline Phosphatase (ALP) Activity: Quantify at 7-14 days using p-nitrophenyl phosphate substrate; normalize to total protein content [48]
- Mineralization Analysis: Stain with Alizarin Red S at 21-28 days; quantify by spectrophotometry after cetylpyridinium chloride extraction [46]
- Gene Expression Profiling: Extract RNA at predetermined intervals; analyze osteogenic markers (Runx2, Osterix, Osteocalcin, Collagen I) via RT-qPCR [46] [48]
Biological Mechanisms and Signaling Pathways
The osteoconductive properties of ceramic and composite biomaterials are mediated through specific biological mechanisms that direct cellular responses at the molecular level.
Osteogenic Differentiation Pathways
Ceramic biomaterials promote osteogenic differentiation primarily through ion release and surface topography. Calcium ions activate the calcium-sensing receptor (CaSR), triggering downstream signaling that enhances osteoblast differentiation and function [46]. Silicon ions released from silicate ceramics upregulate osteogenic gene expression through activation of the MAPK/ERK pathway [48]. Additionally, material surface characteristics influence integrin binding and activation of focal adhesion kinase (FAK) signaling, which converges on osteogenic transcription factors including Runx2 and Osterix [45] [46].
Osteoimmunomodulation
Recent advances have revealed the critical role of immune response modulation in bone regeneration, a concept termed osteoimmunomodulation [50]. Ceramic composites can influence macrophage polarization from pro-inflammatory M1 phenotype to pro-healing M2 phenotype, creating a favorable environment for bone regeneration [46] [50]. β-TCP coatings have been shown to activate CaSR pathways in macrophages, promoting M2 polarization and subsequent upregulation of BMP-2 expression, which enhances osteogenic differentiation of MSCs [46]. Chitosan-based composites modulate macrophage behavior through NF-κB and STAT signaling pathways, further supporting regenerative responses [50].
The Scientist's Toolkit: Essential Research Materials
Table 4: Key Research Reagents for Ceramic-Composite Bone Tissue Engineering
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Base Polymers | Polycaprolactone (PCL), Polylactic acid (PLA), Chitosan, Collagen | Structural matrix providing mechanical support and processability [49] [50] |
| Ceramic Components | Hydroxyapatite (nano/micro), β-TCP, Baghdadite, Bioglass | Osteoconductive fillers that enhance bioactivity and bone bonding [49] [48] |
| Crosslinking Agents | Genipin, Glutaraldehyde, Carbodiimide (EDC) | Improve mechanical stability and control degradation kinetics [50] |
| Bioactive Factors | BMP-2, TGF-β1, VEGF, Magnesium ions | Osteoinductive signals that enhance cellular differentiation and angiogenesis [50] |
| Characterization Tools | SEM-EDS, XRD, FTIR, Mechanical Testers | Material physicochemical and structural analysis [49] [48] |
| Cell Culture Reagents | hBMSCs, Osteoblast Cell Lines, Osteogenic Media Supplements | In vitro biological performance assessment [49] [48] |
Ceramic and composite biomaterials have established a fundamental role in bone tissue engineering by providing osteoconductive frameworks that guide the regenerative process. The continued evolution of these materials focuses on enhancing biofunctionality through strategic material combinations, structural design, and biofactor incorporation. Emerging trends include the development of smart biomaterials with responsive properties, 4D printing technologies that create dynamic scaffolds, and multifunctional systems that combine osteoconduction with antibacterial properties through ionic doping [48] [51]. The integration of AI-driven design approaches promises to accelerate the development of optimized scaffold architectures tailored to specific clinical applications [52] [51]. As research progresses, ceramic-composite biomaterials are poised to advance from structural templates to biologically instructive systems that actively orchestrate the bone regeneration process.
Articular cartilage, a smooth and elastic connective tissue, is essential for load-bearing and friction reduction within synovial joints [53]. The osteochondral unit is a complex, multi-tissue structure that includes articular cartilage, a calcified cartilage layer, and the subchondral bone [53] [54]. A critical feature of this interface is its gradient architecture, which facilitates the transition of mechanical loads between the viscoelastic cartilage and the stiff subchondral bone [54]. Unlike other tissues, articular cartilage is avascular, aneural, and alymphatic, which severely limits its intrinsic capacity for self-repair [55] [53] [56]. When injury occurs, particularly when it extends into the subchondral bone, the body's healing response often results in the formation of mechanically inferior fibrocartilage rather than hyaline cartilage, leading to an unfavorable prognosis and potential progression to osteoarthritis (OA) [57] [56].
Within the context of tissue engineering research, biomaterials are not merely passive scaffolds. Their role has evolved to become the cornerstone of regenerative strategies, actively directing biological responses to replicate this complex interface. This whitepaper delves into the design principles, material innovations, and experimental methodologies that are paving the way for the next generation of biomaterial-based solutions for osteochondral repair.
Design Principles for Bionic Scaffolds
The design of an ideal bionic scaffold for osteochondral repair is governed by a set of interdependent principles aimed at recapitulating the native tissue's biological and mechanical environment [55].
Core Properties of an Ideal Scaffold
- Biocompatibility and Biodegradability: The scaffold must interact with local tissue safely without inducing hazardous effects or significant immune reactions [55] [53]. Its degradation kinetics should be synchronized with the rate of new tissue formation, and the degradation products must be non-toxic [55].
- Mechanical and Structural Properties: The scaffold must provide immediate mechanical support, bearing physiological loads to prevent collapse. Its compressive modulus should ideally match that of native cartilage (0.02–1.16 MPa in the superficial zone and 6.44–7.75 MPa in the deep zone) [55]. Porosity is another critical factor; it must be sufficient to facilitate cell migration, proliferation, and nutrient flow, yet not so large as to compromise mechanical integrity [55].
- Bioactivity and Functionality: Beyond structural support, scaffolds must actively promote regeneration. This is achieved by functioning as a delivery vehicle for bioactive factors (e.g., growth factors), cells (e.g., chondrocytes, stem cells), drugs, or extracellular vesicles that modulate the immune microenvironment and direct cellular processes toward chondrogenesis and osteogenesis [55] [53].
Strategic Approaches to Repair
Research has coalesced around three primary strategic approaches for cartilage repair, each with a distinct role for biomaterials [53]:
- Regeneration: This strategy uses tissue engineering constructs—combining scaffolds, cells, and bioactive factors—to stimulate the body's own repair mechanisms to regenerate new, functional tissue [53].
- Substitution: In cases of severe defect, this approach employs biomimetic materials that emulate the architecture and function of the biological system to replace the damaged tissue, often using multi-layered or gradient materials [53].
- Immunization: Given that cartilage defects are frequently associated with inflammatory conditions like OA, this strategy focuses on using biomaterials to deliver immunomodulatory agents (e.g., anti-inflammatory drugs, PRP, exosomes) to control the local immune environment and facilitate regeneration [53].
Biomaterial Innovations in Scaffold Design
A wide array of natural, synthetic, and composite materials is being explored to meet the demanding requirements of osteochondral scaffolds.
Natural Component-Based Scaffolds
Natural polymers are favored for their innate bioactivity and biocompatibility.
- Collagen & Hyaluronic Acid (HA): As natural components of the extracellular matrix (ECM), they support cell adhesion and proliferation. For example, a type I collagen-HA hydrogel has been shown to regenerate hyaline-like cartilage without additional cellular components [55]. HA also provides significant tensile strength to tissue [56].
- Gelatin: Derived from collagen, gelatin is less immunogenic but possesses poor mechanical properties, necessitating crosslinking or combination with other polymers (e.g., pullulan) to enhance its stability and bioactivity [55].
- Silk Fibroin: Valued for its excellent mechanical strength, slow degradation rate, and ability to maintain the chondrocyte phenotype, it directs the formation of cartilage-specific proteins [55].
- Chitosan: An analog of chitin, it offers biocompatibility, biodegradability, antibacterial properties, and can be molded into various geometries. Some chitosan-based scaffolds are already in clinical use [55].
Synthetic and Composite Polymer Scaffolds
Synthetic polymers provide superior control over mechanical properties and degradation rates.
- Polyesters: Materials such as polylactic acid (PLA), polyglycolic acid (PGA), and polycaprolactone (PCL) are widely used. For instance, PCL-PEG scaffolds exhibit excellent cell adhesion, migration, and proliferation, promoting cartilage healing in vivo [56]. Incorporating graphene into PCL scaffolds has been shown to significantly enhance the healing of large osteochondral defects [56].
- Hydrogels: These highly tunable, hydrophilic networks are particularly promising for cartilage regeneration. Advanced stratified structural hydrogels are designed to emulate the zonal architecture of native cartilage, while stimuli-responsive "smart" hydrogels can react to environmental changes (e.g., pH, inflammation) to release therapeutic agents on demand [58].
Table 1: Key Biomaterials for Osteochondral Tissue Engineering
| Material Category | Key Materials | Advantages | Limitations/Considerations |
|---|---|---|---|
| Natural Polymers | Collagen, Hyaluronic Acid, Gelatin, Chitosan, Silk Fibroin | Innate biocompatibility, bioactivity, inherent cell-binding motifs. | Batch-to-batch variability, potential immunogenicity, generally weaker mechanical properties. |
| Synthetic Polymers | PLA, PGA, PCL, PLGA | Tunable mechanical properties & degradation kinetics, high reproducibility. | Lack of bioactivity, potential for acidic degradation products that may cause inflammation. |
| Ceramics | Hydroxyapatite (HAp) | Excellent osteoconductivity, mimics mineral phase of bone, promotes integration with subchondral bone. | Brittle, poor resorbability, primarily used in the bone region of osteochondral scaffolds. |
| Composite Scaffolds | e.g., HAp/PLGA, Collagen/HA, PCL/Graphene | Combine advantages of multiple materials; can create mechanical and biochemical gradients. | Design and manufacturing complexity. |
Advanced Manufacturing and Engineering Strategies
Mimicking the osteochondral interface requires sophisticated manufacturing techniques that can replicate its graded structure.
3D Bioprinting and Additive Manufacturing
3D bioprinting is an additive manufacturing technology that enables the fabrication of patient-specific constructs with precise control over geometry and composition [54]. The process typically involves medical imaging (CT/MRI), computer-aided design (CAD) modeling, and the selection of appropriate bioinks (cell-laden materials) [54]. The primary challenge lies in creating a scaffold that replicates the sub-millimeter gradient in mechanical and chemical properties found at the natural interface [54]. A prominent strategy involves the fabrication of multi-phasic or gradient scaffolds, where the cartilage region is composed of a hydrogel or polymer that supports chondrogenesis, while the bone region is a stiffer, ceramic-reinforced composite that encourages osteogenesis [53] [54]. For example, a hybrid scaffold of HAp, PLGA, and bovine cartilage matrix has been successfully designed to mimic the natural osteochondral structure [54].
Incorporating Biologically Active Components
To transform a structural scaffold into a regenerative implant, the incorporation of bioactive components is essential.
- Cells: Chondrocytes are the primary seed cells, but their use is limited by availability. Mesenchymal Stem Cells (MSCs), derived from bone marrow (BMSCs) or adipose tissue (ADSCs), are a popular alternative due to their multipotency [53] [59]. Induced Pluripotent Stem Cells (iPSCs) represent a groundbreaking cell source, as they can be differentiated into cartilaginous particles (iPSC-CP) with a hyaline-like matrix, offering a potentially unlimited cell supply [59].
- Bioactive Factors: Growth factors are critical for directing cell fate. Transforming Growth Factor-beta (TGF-β) is a potent inducer of chondrogenesis, while Bone Morphogenetic Proteins (BMPs) and Insulin-like Growth Factor (IGF) play key roles in bone and cartilage metabolism [53].
- Extracellular Vesicles (EVs): As cell-free therapeutics, EVs (including exosomes) have garnered significant attention. They carry miRNAs, proteins, and other bioactive molecules that can modulate inflammation, enhance chondrocyte proliferation, and promote matrix synthesis without the risks associated with whole-cell transplantation [57].
Detailed Experimental Protocol: A Case Study in Hybrid Implant Engineering
The following protocol is adapted from a proof-of-concept study investigating a hybrid implant for osteochondral repair in a rat model [59]. This methodology exemplifies the integration of multiple advanced strategies.
Protocol: Evaluation of a Hybrid MSC/iPSC-CP Implant
Objective: To assess the efficacy of a hybrid implant, comprising human iPSC-derived cartilaginous particles (iPSC-CP) wrapped in a tissue-engineered construct (TEC) of human MSCs, for biphasic osteochondral repair.
Materials and Reagents:
- Cells: Human synovial MSCs, human iPSCs.
- Scaffold Components: Tissue culture plastics, standard MSC growth media, iPSC differentiation media.
- Characterization Reagents: Cell viability stains (e.g., Live/Dead assay), antibodies for fibronectin and vitronectin, primers or antibodies for IL-1β, MMP-13, VEGF.
- Animal Model: Immunocompromised rats (e.g., nude rats) to permit the study of human cells.
- Histology: Safranin-O/Fast Green stain, antibodies for Collagen Type II (Col II) and Collagen Type X (Col X).
Methodology:
- Construct Fabrication:
- iPSC-CP Generation: Differentiate human iPSCs into cartilaginous particles using a defined protocol over several weeks to form hyaline-like matrix [59].
- TEC Production: Culture human MSCs to confluence, allowing them to synthesize their own ECM and form a scaffold-free, adhesive sheet-like construct [59].
- Hybrid Implant Assembly: Manually wrap the iPSC-CP within the MSC-based TEC to form the final hybrid implant [59].
- Control Groups: Prepare control groups including:
iPSC-CP/fdTEC: iPSC-CP wrapped in a freeze-dried/rehydrated TEC (fdTEC) containing no living MSCs.iPSC-CP only: iPSC-CP implanted alone.Untreated defect: Empty defect control.
In Vitro Characterization:
- Cell Viability: Perform Live/Dead staining on TEC and fdTEC to confirm the absence of live cells in the fdTEC.
- Matrix Composition: Immunostain TEC and fdTEC for key adhesive proteins like fibronectin and vitronectin to verify matrix integrity.
- Inflammatory Marker Screening: Use RT-PCR or ELISA to ensure no pre-implantation expression of IL-1β, MMP-13, or VEGF in the TEC, fdTEC, or iPSC-CP.
In Vivo Implantation and Analysis:
- Surgery: Create a critical-sized osteochondral defect in the trochlear groove of the rat femur. Implant the constructs into the defects according to the experimental groups (n≥5).
- Engraftment Assessment (4 weeks): Sacrifice a subset of animals and histologically evaluate the engraftment rate of the implants and their bonding to adjacent cartilage.
- Long-Term Repair (12 & 24 weeks): Evaluate the remaining animals for:
- Tissue Morphology & Composition: Histological staining with Safranin-O (for proteoglycans) and immunostaining for Col II (hyaline cartilage marker) and Col X (calcified cartilage marker).
- Subchondral Bone Restoration: Analyze histological sections for the regeneration of the subchondral bone plate and the formation of a tidemark.
- Histological Scoring: Use a modified O'Driscoll scoring system to quantitatively assess the quality of the repaired tissue.
Key Workflow Diagram: The following diagram outlines the experimental workflow for creating and testing the hybrid implant.
Diagram Title: Hybrid Implant Experimental Workflow
Key Findings and Interpretation
The cited study demonstrated that the presence of live MSCs within the TEC was critical for successful biphasic osteochondral repair [59]. While the iPSC-CP/fdTEC control provided initial fixation and supported cartilaginous tissue, only the iPSC-CP/TEC group with live MSCs achieved complete integration and regeneration of the subchondral bone, including the formation of a tidemark and calcified cartilage zone [59]. This underscores that the MSC component does not merely provide an adhesive function but actively facilitates the regenerative process, potentially through paracrine signaling that enhances angiogenesis and remodeling [59].
The Researcher's Toolkit: Essential Reagents and Materials
Table 2: Essential Research Reagents for Osteochondral Tissue Engineering
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Multipotent primary cell source for chondrogenic and osteogenic differentiation. | Bone Marrow-derived MSCs (BMSCs), Adipose-derived MSCs (ADSCs), Synovial MSCs [53] [59]. |
| Induced Pluripotent Stem Cells (iPSCs) | Pluripotent cell source capable of generating large quantities of differentiated cells, such as chondrocytes. | Human iPSC-derived cartilaginous particles (iPSC-CP) [59]. |
| Chondrogenic Growth Factors | Direct stem cell differentiation towards a chondrogenic lineage and promote cartilage matrix synthesis. | Transforming Growth Factor-beta (TGF-β), Bone Morphogenetic Proteins (BMPs) [53]. |
| Natural Polymer Bioinks | Base material for 3D bioprinting and hydrogel formation; provide biocompatibility and bioactivity. | Collagen (Type I/II), Hyaluronic Acid (HA), Gelatin, Chitosan, Alginate [55] [54]. |
| Synthetic Polymer Bioinks | Provide structural integrity, tunable mechanical properties, and printability for 3D bioprinting. | Polylactic Acid (PLA), Polycaprolactone (PCL), Polyethylene Glycol (PEG) [56] [54]. |
| Ceramic Particles | Incorporated into the bone region of scaffolds to provide osteoconductivity and mimic bone mineral. | Hydroxyapatite (HAp) [54]. |
| Extracellular Vesicles (EVs) | Cell-free therapeutic agents that modulate inflammation and promote regeneration via cargo delivery. | Exosomes derived from MSCs [53] [57]. |
| Histological Stains | Visualize and assess the composition and quality of engineered tissues. | Safranin-O (for proteoglycans), Collagen Type II Immunostaining (for hyaline cartilage) [59]. |
The field of osteochondral repair is moving beyond simple structural replacement towards the creation of biologically active, biomimetic interfaces. The convergence of advanced biomaterials, cutting-edge manufacturing like 3D bioprinting, and innovative biological components (MSCs, iPSCs, EVs) is driving this progress. Future advancements will likely hinge on combinatorial strategies that integrate smart biomaterials with controlled release mechanisms for genes and drugs, all guided by patient-specific data [57]. While challenges in scaling up manufacturing, securing regulatory approval, and demonstrating long-term efficacy in large clinical trials remain, the trajectory is clear. Biomaterials are the foundational enablers in tissue engineering, providing the necessary instructions and environment to orchestrate the regeneration of the complex osteochondral interface, offering hope for a definitive solution to a debilitating clinical problem.
The extracellular matrix (ECM) represents a highly sophisticated biological framework that transcends its conventional role as a passive structural scaffold. Comprising a dynamic network of proteins, glycosaminoglycans, and signaling molecules, the ECM actively orchestrates fundamental cellular processes—including adhesion, migration, proliferation, and differentiation—through integrated biomechanical and biochemical cues [3]. This regulatory capacity arises from its tissue-specific composition and architecture, making it indispensable for physiological homeostasis and a critical blueprint for biomaterial design in regenerative medicine [3]. The rising global burden of chronic wounds, degenerative diseases, and organ failure has intensified the demand for advanced therapeutic strategies that address the limitations of conventional treatments [3].
Within this context, biomaterials research has evolved from providing mere structural support to creating bioactive environments that actively guide regenerative processes. ECM-based scaffolds and drug-loaded hydrogels exemplify this paradigm shift, offering increasingly sophisticated platforms for wound management. Chronic wounds affect millions globally, with the worldwide estimated prevalence ranging between 1.47 and 2.2 per 1,000 population, creating substantial healthcare burdens [60]. In the UK alone, a 2017/2018 cohort study showed an estimated 3.8 million skin wound patients treated by the NHS, with more than 1.5 million suffering from chronic wounds including diabetic foot ulcers, venous leg ulcers, and pressure ulcers [60]. The global wound care market is expected to reach over $29.6 billion by 2030, having produced about $22.25 billion in 2023, with advanced wound dressings representing the largest and fastest-growing segment [61].
This technical review examines the foundational principles, design strategies, and experimental methodologies for ECM-based scaffolds and drug-loaded hydrogels, framing their development within the broader thesis that successful tissue engineering requires biomaterials that recapitulate the dynamic reciprocity of native tissue microenvironments.
Extracellular Matrix Fundamentals in Wound Healing
Structural and Biochemical Composition
The ECM constitutes a sophisticated three-dimensional supramolecular assembly that confers both biomechanical support and biochemical regulation to resident cells and tissues [62]. As the endogenous biological scaffold that envelops and interconnects cellular populations, the ECM serves critical functions beyond structural maintenance, orchestrating cellular behaviors fundamental to embryonic development, tissue homeostasis, wound healing, and regenerative processes [62]. The ECM comprises a highly organized assemblage of macromolecules, principally categorized into fibrillar proteins, glycosaminoglycans (GAGs), proteoglycans, and matricellular glycoproteins [62].
Collagens form the primary structural framework of the ECM, representing approximately 30% of total mammalian protein and providing essential tensile strength [62]. Different collagen types serve specialized functions: Type I predominates in skin, tendons, and bone; Type II characterizes cartilage; and Type IV creates the meshwork structure of basement membranes [62]. Working alongside collagen, elastin and elastic fibers provide resilience and elastic recoil, particularly in mechanically active tissues such as blood vessels, lungs, and skin [62]. This collagen–elastin partnership enables tissues to withstand cyclic mechanical stress while preserving structural integrity.
Glycosaminoglycans contribute to ECM function through their unique chemical properties. These linear, negatively charged polysaccharides interact with water and ions to generate osmotic pressure, providing compressive resistance and tissue hydration [62]. Key GAGs—including hyaluronan, chondroitin sulfate, heparan sulfate, keratan sulfate, and dermatan sulfate—regulate cellular migration, proliferation, and morphogenesis [62]. Related proteoglycans, which consist of GAG chains attached to core proteins, control matrix hydration, establish permeability barriers, and serve as reservoirs for growth factors and cytokines [62].
Dynamic ECM Remodeling in Wound Healing
ECM remodeling is a dynamic, tightly regulated process essential for wound healing, involving degradation of the provisional matrix and deposition of new ECM components critical for tissue restoration [3]. Shortly after injury, a fibrin-rich provisional matrix forms, offering structural support and enabling cellular infiltration that initiates repair [3]. This matrix also modulates the inflammatory response by recruiting fibroblasts and endothelial cells [3].
Matrix metalloproteinases (MMPs) become pivotal during the remodeling phase by degrading the provisional matrix and facilitating fibroblast migration and ECM synthesis [3]. MMPs ensure a balanced transition from matrix degradation to new ECM formation, which is essential for effective healing [3]. A hallmark of this phase is the replacement of type III collagen with type I collagen, enhancing tissue tensile strength and restoring structural integrity [3]. The following diagram illustrates this dynamic remodeling process:
Figure 1: ECM Remodeling Process in Wound Healing
Furthermore, remodeling involves upregulation of matricellular proteins like fibronectin and tenascin-C, which modulate cell-ECM interactions and influence cell behavior, including adhesion, migration, and differentiation [3]. Precise regulation of ECM turnover is crucial; dysregulation can lead to pathological scarring, such as hypertrophic scars or keloids [3].
Integrin-Mediated Signaling Pathways
Integrins serve as fundamental mediators of bidirectional communication between cells and their ECM microenvironment, playing indispensable roles in tissue repair and regeneration. These transmembrane receptors, composed of α and β subunits, recognize specific ECM components including collagen, fibronectin, and laminin, thereby orchestrating essential cellular processes such as adhesion, migration, proliferation, and survival [3]. The activation of integrin signaling initiates with ECM ligand binding, which induces conformational changes that promote receptor clustering and the assembly of focal adhesion complexes [3]. These specialized structures serve as mechanical and biochemical signaling hubs, recruiting adaptor proteins including talin, vinculin, and paxillin to bridge the connection between integrins and the actin cytoskeleton [3].
Central to this signaling network is the focal adhesion kinase (FAK) pathway, which, upon activation at Tyr397, recruits Src family kinases to regulate cytoskeletal dynamics and promote cell migration [3]. Parallel MAPK/ERK pathway activation regulates gene expression for proliferation and differentiation, while the PI3K/Akt pathway promotes cell survival in stressful, injured tissue microenvironments [3]. The following diagram illustrates these critical signaling pathways:
Figure 2: Integrin-Mediated Signaling in Wound Repair
ECM-Based Scaffolds: Design and Fabrication
Scaffold Categories and Properties
ECM-inspired biomaterials have emerged as a significant advancement in the field of tissue engineering, presenting promising approaches for the repair and regeneration of damaged tissues [3]. These biomaterials are engineered to replicate both the structural and biochemical characteristics of the natural ECM, providing an optimal environment conducive to cellular activities critical for healing [3]. ECM-based platforms utilized in tissue engineering can be classified into three main categories, depending on the source of the utilized monomers: natural, synthetic, and hybrid [63].
Natural scaffolds are typically derived from biological sources and closely replicate the composition of native ECMs, hence preserving the structural integrity and biochemical cues essential for mediating cellular functions [63]. Synthetic scaffolds composed of artificially synthesized (lab-engineered) polymers enable precise control of mechanical properties, including strength, stiffness, elasticity, and porosity [63]. Hybrid composites are designed to integrate both natural ECM components alongside synthetic materials, merging the bioactivity of biological components with the mechanical strength of synthetic ones, thereby offering a promising remedy for various tissue engineering and regenerative medicine applications [63].
Table 1: Comparative Analysis of ECM-Based Scaffold Types
| Parameter | Natural Scaffolds | Synthetic Scaffolds | Hybrid Scaffolds |
|---|---|---|---|
| Bioactivity | High (preserves native biochemical cues) | Low (unless functionalized) | Intermediate to high |
| Mechanical Control | Limited (tissue-dependent) | High (precise tunability) | Adjustable |
| Immunogenicity | Variable (depends on decellularization) | Low | Can be optimized |
| Degradation Rate | Variable (enzyme-dependent) | Controllable | Design-dependent |
| Fabrication Reproducibility | Low (batch variability) | High | Intermediate |
| Structural Complexity | Limited | High (advanced manufacturing) | High |
| Cost | High | Low to moderate | Moderate to high |
| Regulatory Pathway | Complex (biological product) | Established | Complex |
| Clinical Translation | Multiple approved products [62] | Extensive history | Emerging |
Decellularization Techniques for ECM Scaffolds
Decellularized ECM (dECM) scaffolds preserve native tissue structure and biochemical cues while minimizing immune responses, creating biomimetic templates that promote cell integration and tissue remodeling [62]. Decellularization is a critical bioprocessing technique for creating acellular extracellular matrix (ECM) scaffolds that selectively remove immunogenic cellular components while preserving the native ECM's structural architecture and bioactive composition [62]. Achieving this delicate balance presents significant technical challenges, as protocols must be tailored to tissue-specific characteristics, including cellular density, vascular architecture, and biomechanical properties [62].
Decellularization can be achieved through various methods, which can be applied individually or in combination to optimize the removal of the cellular material. These techniques can be classified into three main categories: chemical, enzymatic, and physical, each presenting unique advantages and disadvantages [63]. The following workflow illustrates a comprehensive decellularization protocol:
Figure 3: Comprehensive Decellularization Protocol
Chemical methods utilize detergents that function as amphiphilic agents that disrupt molecular interactions by solubilizing cell membranes and breaking hydrophobic-hydrophilic bonds [62]. These compounds, classified as ionic, non-ionic, or zwitterionic, remove immunogenic material by dissociating lipid membranes and separating DNA from proteins. Ionic detergents such as sodium dodecyl sulfate (SDS), sodium deoxycholate (SDC), and Triton X-100 are particularly effective at disrupting nuclear and cytoplasmic membranes through their targeting of lipid and protein interactions [62]. However, ionic detergents present significant limitations: they can damage ECM proteins and bioactive molecules, while their strong binding to matrix components makes complete removal difficult and may result in cytotoxic effects on subsequently seeded cells [62].
Enzymatic methods typically employ nucleases (DNases and RNases) to degrade nucleic acid residues following cell membrane disruption by chemical or physical methods. Trypsin and other proteases may also be used to dissociate cells from the ECM, though their application requires careful control to prevent excessive damage to ECM proteins and adhesive motifs [63].
Physical methods include freeze-thaw cycles, mechanical pressure, and perfusion systems that physically disrupt cell membranes and facilitate the removal of cellular debris. Freeze-thaw cycles cause ice crystal formation that ruptures cells, while perfusion-based techniques have been widely used for whole-organ decellularization, enabling the generation of bioartificial constructs for complex organs such as the heart, lung, kidney, and liver [63].
Quality Assessment of dECM Scaffolds
Rigorous quality assessment is essential for ensuring the safety and efficacy of dECM scaffolds. Key evaluation criteria include:
- DNA quantification: Residual DNA content should be <50 ng per mg of dry weight to minimize immunogenic potential [62]
- ECM composition analysis: Preservation of key structural proteins (collagens, elastin) and GAGs through biochemical assays and immunohistochemistry [62]
- Ultrastructural assessment: Evaluation of ECM architecture and porosity via scanning electron microscopy [63]
- Biomechanical testing: Assessment of tensile strength, compressive modulus, and viscoelastic properties [62]
- Sterility testing: Validation of absence of microbial contamination [62]
- In vitro biocompatibility: Evaluation of cell adhesion, proliferation, and viability using relevant cell types [62]
- In vivo performance: Assessment of host integration, vascularization, and immune response in appropriate animal models [62]
Drug-Loaded Hydrogels: Design Principles and Delivery Strategies
Hydrogel Classification and Synthesis Strategies
Hydrogels are water-swollen three-dimensional (3D) networks formed of polymers, small molecules, or colloidal particles, either chemically or physically cross-linked [27]. Within their water-expanded and internal connecting structure, hydrogels are appealing substances for precise therapeutic agent release due to their ability to encapsulate biologically active compounds, such as clinical drugs, proteins, or genes [27]. Their increasing interest as drug delivery systems (DDS) is attributed to their biomimetic properties [27].
Hydrogel synthesis strategies are categorized into physically and chemically crosslinked polymer networks [27]. The classification, properties, and applications of different hydrogel types are summarized in the table below:
Table 2: Hydrogel Classification Systems and Characteristics
| Classification Basis | Hydrogel Types | Key Characteristics | Applications |
|---|---|---|---|
| Origin | Natural (collagen, hyaluronic acid, chitosan) | Biocompatible, biodegradable, bioactive | Wound healing, tissue regeneration |
| Synthetic (PEG, Pluronic, Poloxamer) | Tunable mechanics, reproducible | Controlled drug delivery, diagnostics | |
| Hybrid | Combines advantages of both | Advanced tissue engineering | |
| Cross-linking Method | Physical (hydrogen bonding, ionic, hydrophobic) | Reversible, injectable, self-healing | Minimally invasive delivery |
| Chemical (covalent bonds) | High stability, mechanical strength | Long-term implants | |
| Stimuli Response | Temperature-sensitive | Gelation at body temperature | Injectable depots |
| pH-sensitive | Swelling/deswelling with pH changes | Targeted drug delivery | |
| Enzyme-responsive | Degradation by specific enzymes | Disease-specific release | |
| Polymer Composition | Homopolymer | Single monomer type | Basic drug carrier |
| Copolymer | Multiple monomer types | Multi-functional systems | |
| Interpenetrating network | Two independent networks | Enhanced mechanical properties |
Physically crosslinked hydrogels are typically constructed from colloidal factors, micelles, particles, and proteins, as well as secondary forces, including hydrogen bonds, electrostatic forces, supramolecular forces, stereo-complexing, and hydrophobic self-assembly [27]. In general, they are formed through spontaneous self-assembly and stacking processes. The repeated units rely on compact stacking to form a continuous network structure, raising higher solid contents versus chemically crosslinked hydrogels [27].
Chemically crosslinked hydrogels are constructed by covalent bonds between polymer chains, providing greater stability, better resistance to hydrolysis, and longer degradation than the physical ones [27]. They exhibit excellent mechanical properties and enhanced stability under physiological conditions. The construction of polymeric covalent networks can be achieved through a one-step reaction of their own functional groups, often referred to as "click" chemistry, which represents a subtype of reactions characterized by high efficiency, excellent specificity, biological orthogonality, and mild reaction conditions [27].
Smart Hydrogels for Controlled Drug Delivery
Stimuli-responsive hydrogels are known as a subtype of smart biomaterials, where external triggering factors such as reactive oxygen species (ROS), pH, temperature, electric, sonic, and magnetism, photo, and biomolecules initiate changes in the hydrogel structure or drug release profile [27]. The uniqueness of these hydrogels lies in their nonlinear feedback [27]. The use of smart hydrogels in drug delivery systems can reduce dosing frequency, maintain the therapeutic concentration required in a single dose, adjust release behavior order, and minimize drug side effects by preventing drug accumulation in non-target tissues [27].
The following diagram illustrates the conceptual design of a smart hydrogel drug delivery system:
Figure 4: Smart Hydrogel Drug Release Mechanism
Temperature-responsive hydrogels undergo sol-gel transitions in response to temperature changes. A well-known synthesized block copolymer is poly(ethylene glycol)-b-poly(propylene oxide)-b-poly(ethylene glycol), commonly marketed as Pluronic or Poloxamer [27]. The gelation of Pluronic hydrogel occurs when the concentration and temperature surpasses the critical threshold, resulting from the tight accumulation of micelles [27].
pH-sensitive hydrogels contain ionizable functional groups that protonate or deprotonate in response to environmental pH changes. These hydrogels are particularly valuable for wound healing applications, as chronic wounds often exhibit elevated pH levels (7.2-8.9 compared to normal skin pH of 5.4-6.4) [27].
Enzyme-responsive hydrogels are designed to degrade specifically in the presence of enzymes overexpressed in wound environments, such as matrix metalloproteinases (MMPs) and elastase [27]. This enables targeted drug release precisely at the wound site while minimizing systemic exposure.
Hydrogel Drug Loading and Release Mechanisms
Drug loading into hydrogels can be achieved through various methods, including:
- Physical encapsulation: Drugs are mixed with polymer solutions before crosslinking [64]
- Covalent conjugation: Therapeutic agents are chemically bonded to the polymer backbone [64]
- Affinity-based systems: Drugs interact with binding motifs within the hydrogel network [64]
- Nanoparticle incorporation: Drug-loaded nanocarriers are embedded within the hydrogel matrix [27]
Drug release from hydrogels is governed by multiple mechanisms, including diffusion, hydrogel swelling, chemical degradation, and environmental responsiveness [64]. The release kinetics can be tuned by modifying crosslinking density, polymer composition, and incorporating specific responsive elements [64].
Experimental Protocols and Methodologies
Protocol: Decellularization of Dermal Tissue
This protocol describes the preparation of acellular dermal matrix (ADM) scaffolds for wound healing applications, adapted from established methodologies [63] [62].
Materials:
- Human or porcine dermal tissue samples
- Sodium dodecyl sulfate (SDS) solution (0.1-1.0%)
- Triton X-100 solution (1-2%)
- DNase solution (100-200 U/mL) and RNase solution (10-50 U/mL)
- Phosphate-buffered saline (PBS)
- Peracetic acid solution (0.1%) for sterilization
- Equipment: Biological safety cabinet, orbital shaker, sterile surgical instruments
Procedure:
Tissue Preparation
- Obtain full-thickness skin samples and remove adipose tissue
- Cut into 0.5 cm × 0.5 cm pieces using a dermatome
- Rinse with distilled water and PBS containing antibiotics
Chemical Decellularization
- Incubate tissue in 1% SDS solution for 24-48 hours on an orbital shaker (50 rpm) at room temperature
- Replace SDS solution every 12 hours
- Rinse with distilled water for 1 hour
Enzymatic Treatment
- Transfer tissue to 1% Triton X-100 solution for 24 hours at room temperature with agitation
- Rinse with PBS for 2 hours with multiple solution changes
- Incubate in DNase/RNase solution for 6-8 hours at 37°C
Washing and Sterilization
- Wash with distilled water for 24 hours with frequent changes
- Sterilize with 0.1% peracetic acid for 2 hours
- Rinse extensively with PBS (minimum 3 days with daily changes)
Storage
- Store at 4°C in PBS with antibiotics or lyophilize for long-term storage
Quality Control:
- Confirm decellularization by H&E staining (no visible nuclear material)
- Quantify DNA content (<50 ng/mg dry tissue weight)
- Assess ECM preservation through histology (collagen, elastin, GAGs)
- Evaluate mechanical properties compared to native tissue
Protocol: Fabrication of Drug-Loaded Hybrid Hydrogel
This protocol describes the preparation of a hybrid hydrogel incorporating both natural and synthetic polymers for controlled drug delivery in wound applications [64] [27].
Materials:
- Gelatin methacryloyl (GelMA)
- Poly(ethylene glycol) diacrylate (PEGDA)
- Photoinitiator (Irgacure 2959 or lithium phenyl-2,4,6-trimethylbenzoylphosphinate)
- Therapeutic agent (antibiotic, growth factor, or anti-inflammatory drug)
- UV light source (wavelength 315-400 nm, intensity 5-20 mW/cm²)
Procedure:
Polymer Solution Preparation
- Dissolve GelMA (5-15% w/v) in PBS at 37°C
- Add PEGDA (2-10% w/v) to the GelMA solution
- Incorporate photoinitiator (0.05-0.2% w/v)
Drug Incorporation
- Add therapeutic agent to the polymer solution at desired concentration
- For growth factors, add just before crosslinking to maintain bioactivity
- Mix gently to avoid bubble formation
Crosslinking
- Transfer solution to mold or apply directly to wound site
- Expose to UV light (365 nm, 5-15 mW/cm²) for 30-180 seconds
- Adjust exposure time based on hydrogel thickness
Characterization
- Assess mechanical properties via rheometry
- Evaluate swelling ratio gravimetrically
- Determine drug encapsulation efficiency via HPLC or ELISA
- Perform in vitro release studies in PBS at 37°C
Modifications for Specific Applications:
- For infected wounds: Incorporate broad-spectrum antibiotics (e.g., vancomycin, gentamicin)
- For diabetic wounds: Include angiogenic growth factors (VEGF, FGF-2)
- For inflammatory conditions: Load anti-inflammatory agents (dexamethasone, IL-10)
Protocol: In Vitro Assessment of Bioactivity
This protocol describes the evaluation of cellular responses to ECM-based scaffolds and drug-loaded hydrogels [62] [3].
Materials:
- Relevant cell types (fibroblasts, keratinocytes, endothelial cells)
- Cell culture media and supplements
- Test scaffolds/hydrogels and appropriate controls
- Live/dead viability assay kit
- DNA quantification kit
- Materials for immunohistochemistry
Procedure:
Cell Seeding
- Sterilize scaffolds (if not pre-sterilized) using ethylene oxide or peracetic acid
- Pre-wet scaffolds in culture media for 24 hours
- Seed cells at appropriate density (typically 50,000-500,000 cells/cm²)
- Allow cell attachment for 2-4 hours before adding additional media
Viability and Proliferation Assessment
- Perform live/dead staining at predetermined time points (days 1, 3, 7)
- Quantify metabolic activity using MTT or Alamar Blue assays
- Measure DNA content for proliferation assessment
Cell Morphology and Integration
- Fix samples and process for histology (H&E staining)
- Perform immunohistochemistry for cell-specific markers (cytokeratin for keratinocytes, vWF for endothelial cells)
- Assess cell infiltration into scaffolds through confocal microscopy
Gene Expression Analysis
- Extract RNA from cell-scaffold constructs
- Perform RT-qPCR for markers of differentiation, ECM production, and inflammation
Functional Assays
- For angiogenesis studies: tube formation assay with endothelial cells
- For re-epithelialization: keratinocyte migration assay
- For ECM remodeling: MMP activity assays
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for ECM and Hydrogel Studies
| Reagent Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Decellularization Agents | Sodium dodecyl sulfate (SDS) | Ionic detergent for cell lysis | Can damage ECM structure; optimize concentration |
| Triton X-100 | Non-ionic detergent for membrane disruption | Milder than SDS but less efficient | |
| DNase/RNase solutions | Nucleic acid degradation | Required after detergent treatment | |
| Natural Polymers | Collagen Type I | Base material for hydrogels and scaffolds | Source affects properties (bovine, porcine, recombinant) |
| Gelatin methacryloyl (GelMA) | Photocrosslinkable hydrogel | Degree of functionalization affects mechanics | |
| Hyaluronic acid | Glycosaminoglycan for hydrogel fabrication | Can be modified with methacrylate or other groups | |
| Synthetic Polymers | Poly(ethylene glycol) (PEG) | Base for synthetic hydrogels | Molecular weight affects mesh size and diffusion |
| Pluronic F-127 | Thermoresponsive hydrogel | Reverse thermal gelation at ~15-20% concentration | |
| Crosslinking Agents | Irgacure 2959 | Photoinitiator for UV crosslinking | Cytotoxicity concerns at high concentrations |
| Genipin | Natural chemical crosslinker | Lower cytotoxicity than glutaraldehyde | |
| EDC/NHS | Carbodiimide chemistry for amide bond formation | Zero-length crosslinker | |
| Characterization Reagents | Picrosirius Red | Collagen staining | Birefringence under polarized light indicates organization |
| Alcian Blue | GAG staining | Quantitative with dye extraction | |
| Live/Dead viability kit | Cell viability assessment | Calcein AM (live) and ethidium homodimer-1 (dead) | |
| Therapeutic Agents | VEGF, FGF, EGF | Growth factors for enhanced healing | Short half-life requires stabilization strategies |
| Vancomycin, Gentamicin | Antibiotics for infected wounds | Release kinetics dependent on hydrogel properties | |
| Dexamethasone | Anti-inflammatory agent | Controlled release modulates immune response |
ECM-based scaffolds and drug-loaded hydrogels represent two complementary approaches within the broader biomaterials paradigm for advanced wound healing. While ECM scaffolds provide a biomimetic structural and biochemical template that recapitulates native tissue microenvironments, drug-loaded hydrogels offer dynamic, responsive delivery systems capable of modulating the wound healing process through precise spatiotemporal control of therapeutic agents.
The future of wound healing biomaterials lies in the convergence of these technologies—developing ECM-inspired hydrogels that combine the bioactivity of natural matrices with the tunable properties and drug delivery capabilities of advanced polymer systems. As research continues to unravel the complexities of wound microenvironment and cellular responses, next-generation biomaterials will likely incorporate increasingly sophisticated feedback mechanisms, enabling truly intelligent wound management systems that actively respond to and guide the healing process.
Successful translation of these technologies will require continued interdisciplinary collaboration between materials scientists, biologists, and clinicians, with a focus on addressing the remaining challenges in immunogenicity, vascularization, mechanical matching, and regulatory approval. Through such integrated approaches, biomaterials research will continue to advance toward the ultimate goal of restoring not just tissue structure, but complete form and function.
The field of tissue engineering aims to provide biological substitutes that restore, maintain, or improve tissue function, addressing the critical challenges of organ failure and tissue loss [65]. The integration of advanced biological components—stem cells, growth factors, and exosomes—within engineered biomaterials represents a transformative approach in regenerative medicine. These elements work synergistically to direct cellular behavior, promote tissue formation, and modulate the healing microenvironment [65] [61]. Biomaterials serve as artificial extracellular matrices (ECM), providing not only structural support but also critical biochemical and biophysical cues that regulate stem cell development for regeneration [65] [66]. This technical guide examines the core principles, experimental methodologies, and integrative strategies for effectively combining these biological components within biomaterial systems, framed within the context of their role in advancing tissue engineering research.
Stem Cells in Tissue Engineering
Stem Cell Types and Characteristics
Stem cells possess the unique capabilities of self-renewal and differentiation into multiple cell lineages, making them cornerstone biological components in regenerative medicine [61] [66]. The table below summarizes the key stem cell types used in tissue engineering applications.
Table 1: Characteristics of Major Stem Cell Types in Tissue Engineering
| Stem Cell Type | Origin | Differentiation Potential | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Embryonic Stem Cells (ESCs) | Inner cell mass of blastocyst [66] | Pluripotent (all germ layers) [66] | High differentiation capacity | Ethical concerns, tumorigenic risk (teratomas) [65] [66] |
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed somatic cells [66] | Pluripotent (all germ layers) [66] | Autologous potential, avoids ethical issues | Retained epigenetic memory, tumorigenic risk [66] |
| Mesenchymal Stromal Cells (MSCs) | Bone marrow, adipose, umbilical cord [61] [67] | Multipotent (osteogenic, chondrogenic, adipogenic) [66] | Immunomodulatory properties, paracrine signaling | Debate on true multipotency in vivo, donor age-dependent effects [66] [67] |
| Endothelial Colony-Forming Cells (ECFCs) | Vascular endothelium [66] | Primarily endothelial lineage [66] | Strong angiogenic potential | Limited direct osteogenic potential [67] |
Biomaterial-Guided Stem Cell Fate
Biomaterials serve as artificial stem cell niches that provide mechanical, chemical, and topological cues to direct stem cell fate decisions including self-renewal, differentiation, or quiescence [65]. The "bottom-up" biomaterial design approach prioritizes understanding fundamental stem cell biological needs before engineering cell-instructive materials, creating dynamic microenvironments that enhance differentiation fidelity and functional integration [66]. Key biomaterial properties that guide stem cell behavior include:
- Mechanical Properties: Material stiffness can direct lineage-specific differentiation [65] [68].
- Topographical Features: Nanofibrous scaffolds mimicking collagen structure enhance cell-matrix interactions [65].
- Degradation Characteristics: Biodegradation rates should match tissue formation kinetics [65] [69].
- Chemical Composition: Surface chemistry and functional groups influence cell adhesion and signaling [65] [67].
Growth Factors: Controlled Delivery and Signaling
Key Growth Factors in Tissue Regeneration
Growth factors are signaling proteins that regulate fundamental cellular processes including proliferation, migration, and differentiation. Their spatiotemporal presentation is critical for effective tissue regeneration [70]. The table below summarizes major growth factors used in tissue engineering applications.
Table 2: Key Growth Factors and Their Functions in Tissue Engineering
| Growth Factor | Abbreviation | Primary Functions | Target Cells | Applications |
|---|---|---|---|---|
| Bone Morphogenetic Protein 2 | BMP-2 | Osteogenic differentiation, bone formation [70] [67] | MSCs, osteoprogenitors | Bone regeneration [70] |
| Fibroblast Growth Factor 2 | FGF-2 | Angiogenesis, cell proliferation [61] [70] [67] | Endothelial cells, fibroblasts | Angiogenesis, wound healing [61] [70] |
| Vascular Endothelial Growth Factor | VEGF | Blood vessel formation, endothelial cell migration [61] [67] | Endothelial cells | Vascularization, bone regeneration [61] [67] |
| Transforming Growth Factor Beta | TGF-β | ECM production, chondrogenesis, immunomodulation [61] [67] | Fibroblasts, MSCs | Cartilage formation, fibrosis regulation [61] |
Experimental Protocol: Growth Factor Delivery from PLGA Microparticles
Objective: To investigate spatiotemporal effects of controlled growth factor delivery on cell differentiation and tissue formation [70].
Materials:
- PLGA (Poly(lactic-co-glycolic acid)): FDA-approved biodegradable polymer for controlled release [65] [70]
- Recombinant Human Growth Factors: BMP-2 and FGF-2 [70]
- Water-in-Oil-in-Water (W/O/W) Double Emulsion Solvent Evaporation System
- Ex vivo Chick Embryonic Bone Model: Organ culture system [70]
Methodology:
- Microparticle Fabrication:
- Prepare PLGA solution in dichloromethane
- Create primary water-in-oil emulsion by sonicating growth factor aqueous solution with PLGA organic solution
- Form double emulsion by adding primary emulsion to polyvinyl alcohol solution and homogenizing
- Stir overnight for solvent evaporation and particle hardening
- Wash and lyophilize microparticles [70]
Growth Factor Loading:
- Resuspend purified growth factors in buffer solution
- Add to aqueous phase during primary emulsion formation
- Optimize loading efficiency through encapsulation parameters [70]
Release Kinetics Profiling:
- Incubate growth factor-loaded microparticles in phosphate-buffered saline at 37°C
- Collect supernatant at predetermined time points
- Quantify growth factor concentration using ELISA
- Fit data to release kinetics models (Higuchi, Korsmeyer-Peppas) [70]
Biological Assessment:
- Apply microparticles to ex vivo chick embryonic bone model
- Culture for 7-14 days with regular medium changes
- Analyze cell morphology, collagen deposition, and gene expression (osteogenic/chondrogenic markers) [70]
Key Parameters for Success:
- Growth factor presentation rate must be carefully regulated to achieve morphological changes and patterned collagen deposition [70]
- BMP-2 and FGF-2 exhibit distinct, growth factor-dependent response profiles [70]
Exosomes: Cell-Free Regenerative Therapeutics
Exosome Biogenesis and Composition
Exosomes are nanosized (30-150 nm), lipid bilayer-enclosed extracellular vesicles that play critical roles in intercellular communication by transferring proteins, lipids, RNAs, and other bioactive molecules between cells [71] [67]. They are formed through the endocytic pathway via multivesicular bodies (MVBs) and released upon fusion of MVBs with the plasma membrane [71].
Exosomes offer significant advantages as therapeutic carriers, including:
- Biocompatibility and low immunogenicity [71]
- Protection of cargo from enzymatic degradation [71]
- Capacity to cross biological barriers [71]
- Natural targeting capabilities through surface receptors [71]
Experimental Protocol: Engineering and Assessing Exosomes for Bone Regeneration
Objective: To isolate, engineer, and evaluate the efficacy of MSC-derived exosomes for bone regeneration applications [71] [67].
Materials:
- Mesenchymal Stromal Cells: Bone marrow, adipose, or umbilical cord-derived [67]
- Isolation Reagents: Differential ultracentrifugation buffers, size exclusion chromatography columns, or tangential flow filtration systems [67]
- Characterization Antibodies: CD9, CD63, CD81 for positive markers; calnexin, GM130 for negative markers [67]
- Biomaterial Scaffolds: Hydrogel-ceramic composites, electrospun nanofibers, 3D-printed scaffolds [67]
- Osteogenic Differentiation Media: Ascorbic acid, β-glycerophosphate, dexamethasone [71]
Methodology:
- Exosome Isolation and Purification:
- Cell Culture: Culture MSCs to 70-80% confluence in exosome-depleted media
- Conditioned Media Collection: Collect media after 48 hours and centrifuge at 2,000 × g to remove cells and debris
- Ultracentrifugation: Centrifuge supernatant at 100,000 × g for 70 minutes to pellet exosomes
- Purification: Resuspend pellets in PBS and purify using size-exclusion chromatography
- Storage: Store at -80°C in small aliquots to prevent freeze-thaw degradation [71] [67]
Exosome Engineering and Loading:
- Preconditioning: Treat parent MSCs with osteogenic induction media or hypoxic conditions (1-3% O₂) to enhance osteogenic cargo
- Surface Functionalization: Modify exosome surface with targeting peptides (e.g., RGD, BMP-2 mimetic peptides) using click chemistry
- Cargo Loading:
Biomaterial-Assisted Exosome Delivery:
- Scaffold Fabrication: Prepare 3D porous scaffolds using appropriate techniques (electrospinning, 3D printing, phase separation)
- Exosome Incorporation:
In Vitro and In Vivo Assessment:
- Osteogenic Differentiation: Treat MSCs with exosomes and evaluate alkaline phosphatase activity, mineralization (Alizarin Red), and osteogenic markers (RUNX2, OCN, OPN)
- Angiogenic Potential: Assess tube formation in endothelial cell cultures
- In Vivo Bone Regeneration: Implement critical-sized defect models (calvarial, femoral) with radiographic, histological, and biomechanical analyses [71] [67]
Integrated Biomaterial Strategies
Biomaterial Platforms for Biological Component Integration
The true potential of biological components in tissue engineering is realized through their integration with advanced biomaterial platforms that provide structural support and biochemical signaling in a coordinated manner. Key biomaterial strategies include:
Nanofibrous Scaffolds via Phase Separation:
- Thermally induced phase separation (TIPS) creates 3D nanofibrous structures mimicking native collagen architecture [65]
- Synthetic (PLLA, PLGA, PCL) and natural (gelatin) polymers can be processed into high-porosity (up to 98%) scaffolds [65]
- Nanofiber dimensions (50-500 nm) similar to collagen fibers enhance cell-matrix interactions [65]
Hydrogel Systems:
- Tunable physical and chemical properties that can evolve in time and space [65]
- Enable encapsulation of cells, growth factors, and exosomes [65] [61]
- Facilitate spatially-controlled distribution of bio-stimuli [65]
3D Bioprinting and Biofabrication:
- Precise spatial patterning of multiple biological components [61] [69]
- Creation of complex tissue architectures with region-specific properties [69]
- Emerging 4D/5D bioprinting allows for temporal evolution of printed constructs [69]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Integrated Tissue Engineering
| Reagent/Material | Function | Examples/Specifications |
|---|---|---|
| PLGA | Biodegradable scaffold material & controlled release vehicle [65] [70] | Varying LA:GA ratios (50:50, 75:25, 85:15) for tunable degradation [65] |
| PLLA | Nanofibrous scaffold fabrication via phase separation [65] | High molecular weight grades for optimal fiber formation [65] |
| Recombinant Growth Factors | Signaling induction for differentiation & angiogenesis [70] [67] | BMP-2, FGF-2, VEGF; carrier-free for biomaterial incorporation [70] [67] |
| MSC Culture Media | Expansion and maintenance of mesenchymal stromal cells [61] [67] | α-MEM/DMEM, FBS/exosome-depleted FBS, growth supplements [61] |
| Exosome Isolation Kits | Purification of extracellular vesicles from conditioned media [71] [67] | Ultracentrifugation-based, size-exclusion chromatography, polymer precipitation [67] |
| Osteogenic Differentiation Media | Induction of bone-forming phenotype [71] [67] | Ascorbic acid, β-glycerophosphate, dexamethasone [71] |
| Hydrogel Precursors | 3D cell encapsulation & growth factor delivery [65] [69] | Alginate, chitosan, PEG-based, collagen, hyaluronic acid [65] |
| Decellularized ECM | Bioactive scaffolds with native tissue composition [69] | Liver, heart, cartilage-derived; powder or hydrogel form [69] |
The integration of stem cells, growth factors, and exosomes within engineered biomaterials represents the forefront of tissue engineering research. Biomaterials serve as more than passive scaffolds—they are dynamic, instructive microenvironments that spatially and temporally control the presentation of biological signals to direct tissue regeneration [65] [66]. The continued advancement of this field requires interdisciplinary collaboration across materials science, cell biology, and clinical medicine to address persistent challenges in scalability, standardization, and clinical translation [69]. Future directions will likely focus on intelligent biomaterial systems responsive to environmental cues, precision engineering of biological components for enhanced targeting and functionality, and the integration of emerging technologies such as artificial intelligence for biomaterial design [32] [69]. As these technologies mature, the integrated approach of combining biological components with advanced biomaterials holds tremendous promise for developing effective regenerative therapies that address the significant burden of tissue and organ deficiencies worldwide.
Navigating Challenges: Immunogenicity, Manufacturing, and Regulatory Hurdles
Addressing Immunogenicity and Foreign Body Responses
The success of biomaterials in tissue engineering is fundamentally governed by their interaction with the host immune system. Far from being a passive scaffold, a biomaterial is an active participant in a complex biological dialogue, initiating a cascade of events that determines the ultimate outcome of the regenerative process. Two of the most critical challenges in this dialogue are immunogenicity—the ability of a material to provoke an undesirable immune reaction—and the foreign body response (FBR)—a specific, chronic inflammatory and fibrotic reaction to implanted materials [72] [73]. The FBR can severely impair the performance and longevity of implants, often leading to failure through the formation of a dense, collagenous fibrous capsule that isolates the implant from the surrounding tissue [72] [74]. This technical guide delves into the mechanisms underlying these responses and outlines advanced biomaterial strategies to modulate them, thereby paving the way for more effective and durable tissue-engineered therapies.
Core Mechanisms: Unraveling the Molecular and Cellular Dialogue
The Phases of the Foreign Body Response
The FBR is an inevitable host reaction to implanted materials, marked by a tightly orchestrated but often detrimental sequence of phases [72] [73]:
- Protein Adsorption: Within seconds of implantation, blood and tissue proteins adsorb onto the biomaterial surface, forming a provisional matrix that dictates subsequent cell interactions.
- Acute Inflammation: Tissue injury from implantation recruits innate immune cells, primarily neutrophils and pro-inflammatory (M1) macrophages, to the site within the first 24-48 hours [75] [76].
- Chronic Inflammation and Foreign Body Giant Cell (FBGC) Formation: If the acute response fails to degrade or phagocytose the material, it progresses to a chronic phase. Macrophages undergo fusion to form FBGCs, a hallmark of the FBR, which persist at the material-tissue interface and secrete reactive oxygen species and degradative enzymes [72].
- Fibrous Capsule Formation: The persistent inflammatory milieu activates fibroblasts, leading to the deposition of a dense, collagen-rich extracellular matrix that walls off the implant. This fibrous capsule can functionally isolate the implant, leading to device failure, as seen in capsular contracture of silicone breast implants or impaired drug release from subcutaneous delivery systems [73] [74].
The following diagram illustrates the key cellular events in this process:
Figure 1: The Phased Progression of the Foreign Body Response (FBR). The process begins with instantaneous protein adsorption, progresses through acute and chronic inflammatory phases characterized by specific immune cells, and culminates in fibrous encapsulation, which can lead to device failure [72] [73].
Key Molecular Signaling and Immunogenicity
The cellular events of the FBR are driven by a dynamic network of molecular signaling pathways. Transcriptome analyses of tissue surrounding silicone implants have identified critical hub genes and pathways [73]:
- Hub Genes: Key upregulated genes include Fos, Spp1, Fn1, Ctgf, Mmp9, and Ccl2. These genes are involved in fibroblast proliferation, extracellular matrix (ECM) organization, and immune cell recruitment.
- Critical Transcription Factors (TFs): TFs such as FOS, IRF4, and SPI1 have been identified as potential master regulators of the FBR gene network [73].
- Signaling Pathways: Silicone implant-induced FBR involves several key pathways, including cytokine-cytokine receptor interaction, the PI3K-Akt signaling pathway, the IL-17 signaling pathway, ECM-receptor interaction, and phagosome activation [73].
Immunogenicity can be triggered by the material itself or leachable components, leading to hypersensitivity (allergic) reactions. These are primarily Type I (IgE-mediated) or Type IV (T-cell mediated delayed-type) hypersensitivity, as defined in regulatory guidance [77].
Quantitative Data: Measuring the Immune Response
The assessment of immunogenicity and FBR relies on quantifying specific molecular, cellular, and tissue-level outcomes. The tables below summarize key quantitative findings and methods from recent research.
Table 1: Key Hub Genes and Transcription Factors in the Foreign Body Response (based on a silicone implant model in rats) [73]
| Gene Symbol | Protein Name | Log2 Fold Change (Approx.) | Primary Function in FBR |
|---|---|---|---|
| Fos | Proto-oncogene c-FOS | > 2.0 | A transcription factor; regulates cell proliferation, differentiation, and transformation. |
| Spp1 | Osteopontin | > 4.0 | Chemotactic for macrophages; involved in cell adhesion and ECM remodeling. |
| Mmp9 | Matrix Metallopeptidase 9 | > 3.0 | Degrades ECM components (collagen IV, V); facilitates cell migration. |
| Ccl2 | C-C Motif Chemokine Ligand 2 | > 3.0 | Recruits monocytes/macrophages to the site of inflammation. |
| Fn1 | Fibronectin 1 | > 2.5 | Key ECM protein; supports cell adhesion, growth, and migration. |
| Ctgf | Connective Tissue Growth Factor | > 3.0 | Promotes fibroblast proliferation and ECM deposition. |
| Itgax | CD11c | > 2.0 | Marker for dendritic cells and a subset of macrophages. |
Table 2: Impact of FBR on Drug Release from Implantable Systems [74]
| Parameter | Small Molecule (Islatravir, 293 Da) | Large Protein (IgG, 150 kDa) |
|---|---|---|
| Study Model | Reservoir-based drug delivery devices (PMMA, Nylon, PLA) in rats. | |
| Acute FBR Phase | No significant change in plasma levels. | Transient modulation of release (e.g., from PMMA implants). |
| Chronic FBR Phase | Consistent plasma levels across materials; no significant impact from fibrous capsule. | Diffusivity increased over time, correlating with reduced collagen density in the capsule. |
| Key Finding | Fibrotic encapsulation does not significantly impact steady-state release. | Acute FBR can temporarily affect the release of larger molecules. |
Experimental Protocols: Profiling the Foreign Body Response
A detailed methodology for investigating the FBR at a molecular level is crucial for developing new strategies to mitigate it. The following protocol, adapted from a study on silicone implants, provides a comprehensive workflow [73].
Protocol: Transcriptomic Analysis of the FBR in a Rodent Model
Objective: To identify key genes, transcription factors, and signaling pathways involved in the foreign body response to a subcutaneous implant.
Materials and Reagents:
- Animals: Male Sprague-Dawley rats (e.g., 6-week-old).
- Implant Material: Customized silicone sheet (e.g., 1.0 cm diameter).
- Reagents: RNAlater solution, 10% neutral buffered formalin, TRIzol reagent.
- Antibodies: For immunofluorescence (e.g., anti-CD68 for macrophages, anti-α-SMA for myofibroblasts).
- Kit: NEBNext Ultra RNA Library Prep Kit for Illumina.
Procedure:
Implantation Surgery:
- Anesthetize rats according to approved institutional animal care protocols.
- Surgically implant the sterile silicone sheet subcutaneously (e.g., in the scalp). A sham-operated group serves as the control.
- Allow the FBR to develop for a predetermined period (e.g., 30 days).
Tissue Collection:
- Euthanize the animals and dissect out the implant with the surrounding fibrous capsule and tissue.
- Divide each sample: one part is stored in RNAlater at -20°C for RNA sequencing, and the other is fixed in formalin and paraffin-embedded for histology.
Histological and Immunofluorescence Analysis:
- Section paraffin-embedded tissues (5-7 μm thickness).
- Perform H&E staining to assess general capsule morphology and thickness.
- Conduct immunofluorescence staining for specific cell types:
- Use anti-CD68 to identify total macrophages.
- Use anti-α-SMA to identify activated myofibroblasts.
- Use anti-iNOS for M1 and anti-CD206 for M2 macrophage polarization.
- Visualize and quantify fluorescence using confocal microscopy.
RNA Extraction and Sequencing:
- Homogenize the RNAlater-preserved tissue samples.
- Extract total RNA using a standard method (e.g., TRIzol).
- Assess RNA integrity (RIN > 8.0 is recommended).
- Construct sequencing libraries from 2 μg of total RNA per sample using the NEBNext Ultra RNA Library Prep Kit.
- Perform high-throughput sequencing on an Illumina platform (e.g., HiSeq 4000) to generate 150 bp paired-end reads.
Bioinformatic Analysis:
- Quality Control: Filter raw reads to remove adapters and low-quality bases.
- Alignment: Map high-quality clean reads to the reference genome (e.g., Ensembl Rnor 6.0.87) using HISAT2.
- Quantification: Calculate gene expression levels (e.g., FPKM) and obtain read counts using HTSeq.
- Differential Expression: Identify DEmRNAs (Differentially Expressed mRNAs) using DESeq2 with thresholds of |log2FC| ≥ 1.5 and adjusted p-value (q) < 0.05.
- Functional Enrichment: Perform GO (Gene Ontology) and KEGG (Kyoto Encyclopedia of Genes and Genomes) pathway analysis on DEmRNAs using Metascape.
- Network Analysis: Construct a Protein-Protein Interaction (PPI) network from DEmRNAs and identify hub genes and key modules using CytoScape and its plugins (e.g., MCODE). Decipher TF-mRNA regulatory relationships.
The workflow for this experimental protocol and the subsequent bioinformatic analysis is summarized below:
Figure 2: Experimental Workflow for Transcriptomic Analysis of FBR. The process integrates in vivo implantation with downstream molecular and computational analyses to identify key drivers of the foreign body response [73]. IF: Immunofluorescence; IHC: Immunohistochemistry.
Biomaterial Strategies to Modulate Immune Responses
The ultimate goal of understanding FBR mechanisms is to inform the rational design of biomaterials that can mitigate adverse reactions and promote integration. Advanced immunomodulatory biomaterials employ several key strategies [75] [76]:
- Surface Modification and Biofunctionalization: Engineering the material's surface topography, chemistry, and charge to control protein adsorption and direct immune cell behavior. This includes coating materials with native ECM components like collagen or hyaluronic acid to present a "self" signal [78] [79].
- Delivery of Bioactive Cues: Incorporating immunomodulatory factors (e.g., cytokines, growth factors) into the biomaterial to guide local immune responses. For example, releasing IL-4 or IL-13 can promote macrophages toward a pro-regenerative M2 phenotype [75] [80].
- Leveraging Material Properties: The physical and chemical properties of the biomaterial itself (e.g., stiffness, elasticity, degradation rate) are potent regulators of immune cell activity. Stiffer materials often promote a pro-fibrotic response, while softer substrates may reduce it [75] [76].
- Use of "Smart" and Responsive Systems: Developing materials that respond to the local microenvironment (e.g., pH, enzyme activity) to release their therapeutic payload in a feedback-controlled manner [75].
The strategic application of these principles is leading to a new generation of "immunoinstructive" biomaterials that can dynamically interact with the host immune system to foster regeneration rather than rejection.
The Scientist's Toolkit: Key Reagents and Models
Table 3: Essential Research Reagents and Models for Investigating Immunogenicity and FBR
| Category / Item | Specific Examples | Function/Application in Research |
|---|---|---|
| In Vivo Models | Sprague-Dawley rat subcutaneous implant model [73] | Gold-standard for studying the temporal progression of FBR and fibrous capsule formation. |
| Histological Stains | Hematoxylin & Eosin (H&E), Masson's Trichrome | H&E for general morphology; Trichrome for visualizing collagen deposition in the fibrous capsule. |
| Immunostaining Markers | CD68 (pan-macrophage), iNOS (M1 macrophage), CD206 (M2 macrophage), α-SMA (myofibroblasts) [73] | Identifying and quantifying key cellular players in the FBR and assessing macrophage polarization. |
| RNA Sequencing Kit | NEBNext Ultra RNA Library Prep Kit for Illumina [73] | Preparing high-quality sequencing libraries from tissue RNA for transcriptome analysis. |
| Bioinformatic Tools | HISAT2 (alignment), DESeq2 (differential expression), Metascape (GO/KEGG analysis), CytoScape (network analysis) [73] | A computational pipeline for analyzing RNA-seq data to find hub genes and pathways. |
| Engineered Polymers | Polylactic acid (PLA), Polyethylene glycol (PEG), Elastin-like Polypeptides (ELPs) [80] [79] | Versatile, tunable biomaterials for creating controlled-release systems and 3D scaffolds with defined properties. |
| Natural Biomaterials | Chitosan, Hyaluronic Acid, Alginate, Decellularized ECM [75] [79] | Inherently bioactive materials that can mimic the native ECM and promote favorable immune responses. |
Within the broader context of the role of biomaterials in tissue engineering research, achieving a mechanical match with native tissues represents a fundamental design principle critical for clinical success. The field of functional tissue engineering has emerged to address the specific challenges in repairing tissues that serve biomechanical functions, recognizing that mechanobiological interactions between cells and scaffolds critically influence cell behavior even in non-structural organs [81]. Physical factors within the cellular microenvironment—including ECM stiffness, interstitial flows, and mechanical gradients—collectively drive emergent tissue behaviors that cannot be replicated in conventional two-dimensional culture systems [82]. When engineered constructs possess mechanical properties mismatched to the target tissue, consequences can include impaired integration, altered cell differentiation, pathological remodeling, and ultimately functional failure of the implant [83].
The paradigm of "mechanobiomaterials" represents a recent shift toward proactively programming biological functionalities of biomaterials by leveraging mechanics–geometry–biofunction relationships [84]. This approach acknowledges that mechanical stimuli play critical roles in mediating tissue repair and regeneration, and that rational design of material properties can direct desired cellular responses. Furthermore, the global tissue engineering market, projected to grow at a CAGR of 12.8% through 2030, underscores the economic and clinical imperative to address such fundamental design challenges [85]. This technical guide provides a comprehensive framework for understanding, measuring, and achieving mechanical matching in tissue engineering applications, with specific methodologies and design principles for researchers and drug development professionals.
Fundamental Principles of Mechanical Matching
Biomechanical Properties of Native Tissues
The initial step in achieving mechanical match involves thorough characterization of the biomechanical properties of native tissues across multiple geometric scales. These measurements should encompass tissues through various stages of development, injury, disease, repair, and aging to establish appropriate design parameters [81]. Biomechanical properties can be categorized as either structural properties, which reflect the overall functional requirements of a tissue or organ and include the influence of morphological parameters, or material properties, which represent the intrinsic characteristics of the tissue independent of size and shape [81].
Understanding the mechanical "thresholds" that normal tissues encounter for different in vivo activities is essential for developing appropriate design criteria for tissue repairs and replacements. For instance, in the musculoskeletal system, significant advances have been made in measuring and modeling the range and history of stresses and strains placed on tissues such as tendons/ligaments and articular cartilage [81]. These measurements establish the boundaries of expected usage and help develop "safety factors" for tissue-engineered implants [81].
Table 1: Key Mechanical Properties of Native Tissues for Characterization
| Property Category | Specific Parameters | Measurement Techniques | Representative Tissues |
|---|---|---|---|
| Structural Properties | Ultimate tensile strength, Compressive stiffness, Failure strain, Creep behavior | Uniaxial tension/compression, Dynamic mechanical analysis | Tendon, ligament, bone |
| Material Properties | Elastic modulus, Shear modulus, Poisson's ratio, Viscoelastic parameters | Atomic force microscopy, Rheology, Nanoindentation | Cartilage, blood vessels, skin |
| Time-Dependent Behavior | Stress relaxation, Creep, Hysteresis | Cyclical loading, Stress-relaxation tests | Intervertebral disc, meniscus |
| Hydration-Dependent Properties | Permeability, Swelling pressure, Porosity | Confined compression, Permeability tests | Cornea, articular cartilage |
Consequences of Mechanical Mismatch
Mechanical mismatch between engineered constructs and native tissues can lead to several failure modes. At the cellular level, substrate stiffness and mechanical properties directly influence cell differentiation, migration, and ECM production through mechanotransduction pathways [84] [82]. For example, insufficient stiffness in bone grafts can lead to inadequate osteogenic differentiation, while excessive stiffness in soft tissue implants can promote fibrotic encapsulation [83].
At the tissue level, stress shielding occurs when implants bear a disproportionate share of mechanical loads, potentially leading to native tissue atrophy. Conversely, insufficient load-bearing capacity can result in implant failure under physiological stresses. The mechanical environment also significantly influences tissue growth and remodeling through both cellular and acellular mechanisms, with mismatched implants often leading to pathological adaptation rather than functional integration [81].
Quantitative Analysis of Native Tissue Mechanical Environments
In Vivo Measurement and Modeling
Establishing design parameters for tissue-engineered constructs requires detailed knowledge of the mechanical environment that normal and repaired tissues experience during various in vivo activities. Significant advances have been made in this area through combinations of novel imaging methods with theoretical modeling [81]. For example, studies have combined motion capture with computational modeling to determine the in vivo strains experienced by tendons and ligaments during physiological activities [81].
In the cardiovascular system, researchers have combined medical imaging with computational fluid dynamics to extend knowledge of flow- and pressure-induced stresses in blood vessels and heart valves [81]. These approaches have been further developed to study repair tissues, which likely experience altered mechanical environments due to either changes in patient activity or fundamental differences in the mechanical properties of the implant compared to native tissues [81].
Table 2: Representative Mechanical Properties of Native Human Tissues
| Tissue Type | Elastic Modulus | Ultimate Tensile Strength | Failure Strain | Key Mechanical Function |
|---|---|---|---|---|
| Articular Cartilage | 0.5 - 1.5 MPa (compressive) | 10-20 MPa (tensile) | 100-150% | Weight-bearing, low friction |
| Tendon/Ligament | 200-1500 MPa | 50-100 MPa | 10-15% | Force transmission, joint stability |
| Cortical Bone | 15-20 GPa | 100-150 MPa | 1-3% | Structural support, protection |
| Skin | 5-40 MPa | 5-30 MPa | 35-115% | Barrier, mechanical protection |
| Blood Vessels | 0.1-10 MPa (circumferential) | 0.5-5 MPa | 40-80% | Pressure containment, flow regulation |
| Skeletal Muscle | 0.1-0.5 MPa (passive) | 0.1-0.5 MPa | 50-100% | Force generation, movement |
Experimental Protocols for Mechanical Characterization
Protocol 1: Uniaxial Tensile Testing of Soft Biological Tissues
- Sample Preparation: Harvest fresh tissue samples and machine into standardized dog-bone shapes with uniform gauge regions. Maintain hydration with physiological saline throughout preparation.
- Dimension Measurement: Precisely measure cross-sectional dimensions using non-contact optical methods or digital calipers. Record length, width, and thickness at multiple points.
- Mounting: Carefully mount samples in mechanical testing grips, ensuring proper alignment to avoid shear forces or stress concentrations. Use pneumatic or friction grips with appropriate surface treatments.
- Preconditioning: Apply 10-15 cycles of low-load cyclic loading (1-2% strain) to establish a reproducible mechanical state and assess sample integrity.
- Testing: Conduct tensile testing at a strain rate representative of physiological conditions (typically 0.1-1% strain per second). Record force and displacement data until complete failure.
- Data Analysis: Calculate engineering stress (force/original area) and engineering strain (displacement/original length). Determine elastic modulus from the linear region of the stress-strain curve, ultimate tensile strength, and failure strain.
Protocol 2: Atomic Force Microscopy (AFM) for Nanomechanical Mapping
- Sample Preparation: Embed tissue samples in optimal cutting temperature (OCT) compound and section to 10-20μm thickness using a cryostat. Mount sections on glass slides.
- Cantilever Selection: Choose appropriate cantilevers with known spring constants (typically 0.01-0.1 N/m for soft tissues) and attach colloidal probes of defined diameter (2-5μm).
- Calibration: Perform thermal tune method to determine exact spring constant and sensitivity of the photodetector.
- Measurement: Acquire force-volume maps by performing approach-retract cycles at multiple points across a defined grid (typically 16×16 to 64×64 points).
- Data Processing: Fit the approach portion of force curves with appropriate contact mechanics models (Hertz, Sneddon, or JKR models) to calculate elastic modulus at each point.
- Spatial Analysis: Generate stiffness maps and correlate with histological features or other imaging modalities.
Biomaterial Strategies for Achieving Mechanical Match
Material Selection and Design Approaches
Advanced biomaterial strategies focus on replicating both the structural and biochemical characteristics of natural ECM to provide an optimal environment for cellular activities critical for healing [83]. The design principles underlying ECM-inspired biomaterials emphasize precise replication of the architecture, composition, and mechanical properties characteristic of the native ECM [83]. Common material categories include:
Decellularized ECM (dECM) Biomaterials: These materials are produced from donor tissues through processes that remove cellular components while preserving structural proteins and bioactive molecules [82]. dECM biomaterials can be processed into various forms including injectable hydrogels, electrospun scaffolds, and 3D-bioprinted constructs [82]. The mechanical properties of dECM materials can be modulated through concentration adjustments, crosslinking strategies, and combination with synthetic polymers [82].
Synthetic Hydrogels: Materials such as polyethylene glycol (PEG), polyacrylamide, and polyvinyl alcohol offer highly tunable mechanical properties through control of polymer concentration, crosslinking density, and network architecture [83]. These systems provide defined environments where mechanical variables can be precisely controlled independent of biochemical cues.
Composite Materials: Combining natural and synthetic components enables creation of materials with optimized mechanical properties and bioactivity. For example, incorporating dECM particles into synthetic polymer networks can enhance biological activity while maintaining mechanical integrity [82].
Table 3: Biomaterial Classes for Mechanical Matching
| Biomaterial Class | Representative Materials | Tunable Mechanical Parameters | Fabrication Techniques | Tissue Applications |
|---|---|---|---|---|
| Naturally Derived | Collagen, fibrin, hyaluronic acid | Concentration, Crosslinking density, Fiber orientation | Solvent casting, Freeze-drying, Electrospinning | Skin, cartilage, vascular grafts |
| Synthetic Polymers | PLGA, PCL, PEG | Molecular weight, Crystallinity, Porosity | 3D printing, Electrospinning, Phase separation | Bone, ligament, dental |
| ECM-Based | Decellularized tissues, ECM hydrogels | Source tissue, Decellularization method, Concentration | Decellularization, Solubilization, Bioprinting | Cardiac, liver, lung |
| Composite Systems | Polymer-ceramic, Natural-synthetic blends | Phase distribution, Interface bonding, Relative composition | Co-electrospinning, Sequential deposition, In situ precipitation | Osteochondral, dentin-pulp |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Mechanical Matching Studies
| Reagent Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Hydrogel Forming Materials | Methacrylated gelatin (GelMA), Polyethylene glycol diacrylate (PEGDA) | Tunable 3D culture systems with controlled mechanical properties | Photoinitiator concentration and cytotoxicity must be optimized |
| Crosslinking Agents | Genipin, Microbial transglutaminase, NHS-ester compounds | Modulate stiffness and degradation rate without cytotoxicity | Crosslinking efficiency and kinetics affect final properties |
| Mechanosensing Reporters | FRET-based tension sensors, YAP/TAZ antibodies, Paxillin-GFP | Visualize and quantify cellular mechanosensing | Require appropriate controls for expression levels and localization |
| dECM Sources | Urinary bladder matrix (UBM), Small intestinal submucosa (SIS) | Tissue-specific biological and mechanical cues | Batch-to-batch variability requires careful characterization |
| Bioreactor Systems | Uniaxial strain systems, Perfusion bioreactors, Compression chambers | Apply physiologically relevant mechanical stimulation | Strain uniformity and mass transfer must be validated |
Mechanobiology and Signaling Pathways
The mechanical properties of biomaterials influence cellular behavior through the process of mechanotransduction, where physical cues are converted into biochemical signals. Central to this process are integrin-mediated adhesions that connect the extracellular matrix to the intracellular cytoskeleton [83]. The following diagram illustrates the key signaling pathways involved in cellular mechanotransduction:
Diagram 1: Cellular Mechanotransduction Signaling Pathways. This diagram illustrates how mechanical cues from the ECM are transmitted via integrin-mediated signaling to regulate gene expression and cell behavior.
Integrin signaling initiates with ECM ligand binding, which induces conformational changes that promote receptor clustering and assembly of focal adhesion complexes [83]. These specialized structures serve as mechanical and biochemical signaling hubs, recruiting adaptor proteins including talin, vinculin, and paxillin to bridge the connection between integrins and the actin cytoskeleton [83]. The formation of focal adhesions triggers activation of multiple downstream signaling pathways:
FAK/Src Pathway: FAK activation at Tyr397 recruits Src family kinases, forming a dual kinase complex that regulates cytoskeletal dynamics and promotes cell migration [83].
MAPK/ERK Pathway: Regulates gene expression for proliferation and differentiation in response to mechanical stimuli [83].
PI3K/Akt Pathway: Promotes cell survival in stressful mechanical environments [83].
YAP/TAZ Pathway: Mechanical tension on the actin cytoskeleton regulates the nuclear localization of YAP and TAZ transcriptional coactivators, which control genes involved in proliferation and stemness [84].
The mechanical properties of the ECM exert profound influence on integrin signaling dynamics. Substrate stiffness, topography, and ligand density collectively modulate the spatial organization and activation state of integrin clusters [83]. This mechanosensitive regulation has inspired innovative biomaterial design strategies aimed at recapitulating key aspects of native ECM signaling.
Experimental Workflow for Biomaterial Mechanical Optimization
The following diagram outlines a systematic approach for developing and optimizing biomaterials with tailored mechanical properties for specific tissue engineering applications:
Diagram 2: Biomaterial Mechanical Optimization Workflow. This systematic approach ensures rational design of biomaterials with mechanical properties matched to specific tissue engineering applications.
Computational Modeling Approaches
Computational models play an increasingly important role in optimizing material properties and geometry for mechanical matching [84]. These approaches include:
Finite Element Analysis (FEA): Enables prediction of stress and strain distributions in complex tissue-engineered constructs under physiological loading conditions. FEA can identify potential failure points and guide material selection and architectural design.
Multiscale Modeling: Connects phenomena across different length scales, from molecular interactions to tissue-level mechanics, providing insights into structure-function relationships.
Growth and Remodeling Models: Predict how engineered tissues will adapt and remodel in response to mechanical stimuli after implantation, informing design criteria for long-term functionality.
Achieving mechanical match with native tissues remains a critical challenge in tissue engineering, with significant implications for clinical success. The emerging field of mechanobiomaterials represents a paradigm shift toward proactive programming of biological functionalities by leveraging mechanics–geometry–biofunction relationships [84]. Future advances will likely include four key areas:
First, advanced manufacturing technologies such as 3D bioprinting with multi-material capabilities will enable creation of constructs with spatially graded mechanical properties that better mimic tissue interfaces [83] [82]. Second, stimuli-responsive biomaterials that dynamically adjust their mechanical properties in response to local tissue environment or external triggers will provide enhanced integration and remodeling capacity [83].
Third, improved computational models that incorporate machine learning and artificial intelligence strategies will accelerate the design and optimization of biomaterials with tailored mechanical properties [82]. Finally, standardized testing methodologies that better recapitulate the complex mechanical environment of native tissues will enable more accurate prediction of in vivo performance [81].
As the field continues to mature, consideration of mechanical matching principles in the biomaterial design process will hopefully improve the safety, efficacy, and overall success of engineered tissue replacements [81]. By integrating insights from mechanobiology with advanced material design and fabrication technologies, researchers can develop next-generation biomaterials that truly recapitulate the mechanical functionality of native tissues.
In the field of tissue engineering, the successful development of functional tissue constructs hinges on solving a fundamental biological challenge: establishing adequate vascular networks to supply nutrients and oxygen while removing metabolic waste. The absence of integrated vasculature represents a primary reason for the failure of many engineered tissue grafts upon implantation [86]. This limitation becomes critically apparent when considering that the diffusion limit of oxygen in biological tissues restricts the size of avascular constructs to approximately 100-200 micrometers [86]. Beyond this threshold, cells in the core of the construct experience hypoxia, nutrient deprivation, and eventual apoptosis, leading to graft failure [86].
Biomaterials serve as the foundational scaffold in addressing this vascularization challenge, providing not only three-dimensional structural support but also biological cues that guide and promote the formation of functional vascular networks. The role of biomaterials extends beyond passive structural templates to active participants in biological processes, influencing cellular behavior through their chemical composition, physical architecture, and biofunctionalization [87] [88]. Within the context of tissue engineering research, advanced biomaterials are being engineered to mimic native extracellular matrix properties, deliver pro-angiogenic factors in a controlled manner, and create microenvironments conducive to vascular ingrowth and maturation.
The clinical imperative for solving the vascularization challenge is substantial. While thin, avascular tissues like skin and cartilage have achieved some clinical success, the engineering of complex, metabolically active tissues requires functional perfusion systems [86]. For any reconstruction tissue or organ exceeding 400μm in size, vascularization becomes essential to meet cellular metabolic demands [88]. This technical guide explores the multifaceted strategies being employed to overcome the vascularization challenge, with particular emphasis on the evolving role of biomaterials in enabling these approaches.
Physiological Fundamentals of Vascularization
The Biological Basis of Blood Vessel Formation
Vascularization in physiological systems occurs through three principal mechanisms: vasculogenesis, angiogenesis, and arteriogenesis [86]. Vasculogenesis involves the differentiation of angioblasts or mesodermal progenitor cells and the subsequent de novo formation of blood vessels, a process once thought to be restricted to embryonic development but now recognized to occur in adults through circulating endothelial progenitor cells. Angiogenesis describes the sprouting of new capillaries from pre-existing vasculature, while arteriogenesis refers to the shear stress-induced remodeling that forms larger arteries [86].
The process of sprouting angiogenesis is particularly relevant to tissue engineering applications. This complex, multi-step biological event begins with the secretion of protein水解 enzymes that degrade the basement membrane, allowing endothelial cells to invade the extracellular matrix rich in type I collagen and elastic protein [89]. Specialized endothelial tip cells extend numerous filopodia to explore microenvironmental cues, while following endothelial stalk cells proliferate to form the nascent vessel with high permeability [89]. Subsequent maturation involves basement membrane deposition, pericyte recruitment, and eventual vascular stabilization and remodeling into a hierarchical network [89].
Critical Signaling Pathways in Angiogenesis
Table 1: Key Signaling Pathways in Vascular Development and Homeostasis
| Signaling Pathway | Key Components | Biological Functions | Therapeutic Applications |
|---|---|---|---|
| VEGF-VEGFR | VEGF-A, VEGFR-1/2 | Endothelial cell proliferation, migration, permeability; lumen formation | VEGF delivery via biomaterials to initiate angiogenesis |
| FGF Signaling | bFGF, FGF-1/2, FGFR | Endothelial cell proliferation, migration; ECM remodeling | Sustained FGF release from hydrogels for vessel maturation |
| Angiopoietin-Tie | Ang-1/2, Tie-1/2 | Vessel stabilization, maturation, pericyte recruitment | Ang-1 delivery to enhance vessel stability in engineered tissues |
| Hypoxia-Induced | HIF-1α, VEGF-α, SDF-1 | Upregulation of angiogenic factors in response to low oxygen | Biomaterial strategies to mimic hypoxic conditions for vascular induction |
| Notch Signaling | Dll4, Notch1 | Endothelial tip/stalk cell specification, branching regulation | Controlling branching density in engineered vascular networks |
The VEGF signaling pathway serves as the master regulator of angiogenesis, with VEGF activating receptor tyrosine kinases on endothelial cells to promote proliferation, migration, and survival, while also increasing vascular permeability [89]. This pathway is complemented by FGF signaling, which contributes to endothelial cell proliferation and extracellular matrix remodeling [89]. The Angiopoietin-Tie system plays a crucial role in later stages of vascular maturation, with Ang-1 promoting vessel stabilization through pericyte recruitment and enhanced endothelial cell-cell junctions [89].
Hypoxia serves as a potent physiological inducer of angiogenesis through the HIF-1α pathway. Under low oxygen conditions, HIF-1α accumulates and translocates to the nucleus, where it activates transcription of numerous pro-angiogenic genes including VEGF-α, angiopoietin-2, and SDF-1 [87]. This natural response to oxygen deprivation provides important insights for designing biomaterials that can mimic hypoxic signaling to initiate vascularization in engineered tissues.
Biomaterial Strategies for Enhanced Vascularization
Material Composition and Origin
The selection of base biomaterials fundamentally influences their vascularization potential. Both natural and synthetic polymers offer distinct advantages and limitations for promoting vascular ingrowth.
Table 2: Biomaterials for Vascularization Applications
| Material Class | Examples | Advantages for Vascularization | Limitations | Key Applications |
|---|---|---|---|---|
| Natural Polymers | Collagen, fibrin, hyaluronic acid, silk fibroin, ADM | Innate bioactivity, cellular recognition sites, enzymatic degradation | Batch-to-batch variability, limited mechanical control | Collagen: cell adhesion, ECM deposition, angiogenesis [87]; Silk fibroin: promotes MSC differentiation to VECs [87] |
| Synthetic Polymers | PEG, PCL, PLA, PLGA, polyurethane | Tunable mechanical properties, controlled degradation, reproducible manufacture | Lack of cellular recognition sites, potentially inflammatory degradation products | Requires chemical modification (e.g., RGD peptides) to enhance bioactivity [87] |
| Heparin-Mimetic Materials | Sulfonated polysaccharides, sulfonated HA, chitosan | Growth factor stabilization and presentation, enhanced endothelial cell adhesion | Optimization of sulfonation degree needed, potential cytotoxicity | Sulfonated HA hydrogels significantly enhance vascularization in skin wounds [90] |
| Hydrogels | GelMA, polysaccharide-peptide hybrids | ECM-mimetic properties, tunable physical properties, injectability | Limited mechanical strength for load-bearing applications | GelMA sustains VEGF release, promotes endothelial migration [89] |
Natural biomaterials derived from extracellular matrix components provide inherent biological cues that support vascularization. Decellularized porcine adipose-derived extracellular matrix (ADM) creates a microenvironment that induces vascular endothelial cell proliferation, differentiation, and migration, while its interwoven fiber arrangement facilitates capillary crawling and formation of dermal vascular networks [87]. Similarly, collagen—a major component of native ECM—participates in the adhesion of wound repair-related cells (fibroblasts, keratinocytes, vascular endothelial cells), ECM deposition, and angiogenesis [87]. Hyaluronic acid modulates inflammation levels while stimulating vascular endothelial cell recruitment and proliferation, thereby promoting neovascular formation in full-thickness defects [87].
Synthetic biomaterials offer superior control over mechanical properties and degradation kinetics but typically require modification to enhance their bioactivity. Common approaches include incorporating cell-adhesive peptides (e.g., RGD sequences), immobilizing growth factors, or creating composite materials that combine the tunability of synthetic polymers with the bioactivity of natural components [87]. The emergence of heparin-mimetic biomaterials represents a significant advancement, as these materials recapitulate heparin's ability to bind and stabilize angiogenic growth factors like VEGF and bFGF while avoiding its anticoagulant properties [90]. By incorporating sulfonate or sulfate groups onto polymer backbones, these materials protect growth factors from proteolytic degradation and present them to endothelial cell receptors, thereby enhancing and prolonging their bioactivity [90].
Structural Design Parameters
The structural characteristics of biomaterial scaffolds profoundly influence their vascularization potential. Key parameters include porosity, pore size, interconnectivity, and microarchitectural features.
Porosity and pore size directly affect nutrient diffusion, cellular infiltration, and vascular ingrowth. Research indicates that scaffold porosity should ideally exceed 90% to facilitate cell proliferation and migration [87]. The optimal pore size depends on the specific application, with studies suggesting that smaller pores (<200μm) promote denser capillary networks, while larger pores (>275μm) facilitate the formation of larger vascular structures [87]. For instance, polymer scaffolds with large pore sizes (275-400μm) and high interconnectivity promote rapid and extensive vascularization in full-thickness skin defects [87].
Microarchitecture can guide vascular organization through surface patterning and channel incorporation. Techniques such as photolithography have been used to create gelatin-polycaprolactone/silk fibroin composite films with micro-patterns (linear, grid, planar), where linear patterns not only guide directional growth of wound repair cells and neovascularization but also upregulate angiogenesis-related markers and α-smooth muscle actin at both gene and protein levels [87]. The creation of hollow channels that mimic pre-vascular structures provides physical guidance for vascular growth, enhancing oxygen and nutrient transport while facilitating cell migration [87]. Innovative approaches like 3D printing of caramelized sucrose as a sacrificial template enable fabrication of constructs with fully interconnected, perfusable vascular channels [87].
Experimental Approaches and Methodologies
Biomaterial-Mediated Growth Factor Delivery
The controlled delivery of angiogenic growth factors represents one of the most extensively studied approaches for enhancing vascularization. Experimental protocols typically involve encapsulating growth factors within biomaterial matrices to protect them from degradation and provide sustained release.
Standard Protocol for VEGF-Loaded GelMA Hydrogel Preparation:
- GelMA Synthesis: React gelatin with methacrylic anhydride (0.1-0.2 mL/g gelatin) in PBS at 50°C for 2-3 hours, followed by dialysis against distilled water for 5-7 days and lyophilization.
- Photoinitiator Solution: Prepare 0.5% (w/v) lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) in PBS.
- Hydrogel Precursor: Dissolve GelMA (10-15% w/v) in the LAP solution containing VEGF (50-100 ng/mL).
- Crosslinking: Transfer solution to mold, expose to UV light (365 nm, 5-10 mW/cm²) for 30-60 seconds to form hydrogel.
- In Vivo Application: Apply hydrogel directly to wound sites; assess vascularization at 7, 14, and 21 days post-implantation [89].
Advanced delivery systems incorporate responsive elements to achieve spatiotemporal control over growth factor release. For example, reactive oxygen species (ROS)-responsive FGF21/metformin injectable hydrogels simultaneously clear ROS and upregulate angiopoietin-1 expression to recruit endothelial progenitor cells, creating a regenerative microenvironment that enhances diabetic wound healing [89].
Cell-Based Vascularization Strategies
Cell-based approaches leverage the innate capacity of endothelial cells and their precursors to self-assemble into vascular networks. These strategies typically involve seeding scaffolds with single cell types or co-cultures that promote vascular maturation.
Protocol for Generating Vascularized Organoids via Co-culture:
- hPSC Maintenance: Culture human pluripotent stem cells (hPSCs) in mTeSR1 medium on Matrigel-coated plates.
- Brain Organoid Differentiation: Transfer hPSC aggregates to neural induction medium containing SMAD inhibitors (dorsomorphin, SB431542) for 10-12 days with gentle agitation.
- Endothelial Cell Differentiation: Differentiate hPSCs in parallel to endothelial progenitor cells using Wnt activation and supplementation with BMP4, VEGF, and FGF2.
- Co-culture Assembly: Re-embed day 34 brain organoids in polymerization Matrigel containing endothelial progenitor cells.
- Maturation: Culture for 3-5 weeks with periodic medium changes; validate vascular structures using CD31 immunostaining and perfusion assays [91].
Alternative approaches employ genetic engineering to induce endothelial differentiation within organoids. One innovative method involves generating human cortical organoids from hESCs genetically modified to ectopically express the endothelial transcription factor ETV2 in a specific proportion (20% of cells) [91]. This approach yields vascular-like structures that express endothelial markers, support oxygen and nutrient transport, reduce cell death, promote neuronal maturation, and exhibit blood-brain barrier characteristics including tight junctions, nutrient transporters, and increased transendothelial electrical resistance [91].
Figure 1: Vascularized Brain Organoid Co-culture Workflow
In Vivo Vascularization Models
Preclinical models are essential for evaluating the functional capacity of vascularized constructs. The mouse hindlimb ischemia model and dorsal skinfold chamber are commonly used for this purpose, but organoid transplantation models provide particularly valuable insights.
Protocol for Brain Organoid Transplantation and Vascularization Assessment:
- Organoid Preparation: Culture GFP-labeled hESC-derived brain organoids for 40-50 days until they display clear embryonic body boundaries, radially arranged neuroepithelium, and defined buds.
- Surgical Transplantation: Anesthetize immunodeficient adult NOD-SCID mice, create cranial window by making cavity in retrosplenial cortex, implant organoid, and seal with coverslip and adhesive.
- Vascularization Monitoring: Use in vivo two-photon imaging at 7, 14, and 28 days post-transplantation to observe host-derived vascular invasion.
- Functional Assessment: Perform extracellular recordings combined with optogenetics to verify functional synaptic connections between transplant and host brain.
- Histological Analysis: Process brain sections for immunohistochemistry using endothelial markers (CD31, von Willebrand factor) to quantify vascular density and network complexity [91].
This approach demonstrates that host vessels begin invading transplants within 7-10 days, with extensive vascular network formation by day 14, achieving a vascularization success rate of 85.4±6.4% [91]. The resulting vascularization not only significantly improves organoid survival but also promotes progressive neuronal differentiation and maturation, glial generation, microglial integration, and axonal extension to multiple host brain regions [91].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Vascularization Studies
| Reagent Category | Specific Examples | Function/Application | Experimental Considerations |
|---|---|---|---|
| Growth Factors | VEGF-A, bFGF, FGF-2, Ang-1 | Endothelial proliferation, migration, tube formation, vessel stabilization | Short half-life requires stabilization strategies (e.g., heparin-binding) |
| Biomaterial Polymers | GelMA, collagen, fibrin, silk fibroin, PEG | 3D scaffold formation, structural support, mechanical cues | Modulus should match target tissue (typically 0.5-5 kPa for soft tissues) |
| Crosslinking Systems | LAP photoinitiator, genipin, transglutaminase | Hydrogel formation, mechanical stabilization | Crosslinking density affects porosity, nutrient diffusion, and degradation |
| Cell Markers | CD31, vWF, VE-cadherin, α-SMA | Endothelial cell identification, pericyte coverage | Species-specific antibody validation required for animal models |
| Signaling Modulators | SB431542, LDN193189, Y-27632 | TGF-β inhibition, BMP inhibition, ROCK inhibition | Concentration optimization critical to avoid cytotoxicity |
| Assessment Tools | dextran perfusion, two-photon microscopy, lectin staining | Vascular functionality, network visualization | Multiple complementary methods needed for comprehensive assessment |
Emerging Technologies and Future Directions
Advanced Biofabrication Strategies
Convergence of biomaterials with advanced manufacturing technologies is creating new opportunities for engineering complex vascular networks. 3D bioprinting enables precise spatial patterning of multiple cell types and biomaterials to create hierarchical structures that mimic native vascular organization. Sacrificial printing approaches—exemplified by the use of carbohydrate glasses (e.g., caramelized sucrose) as fugitive inks—allow creation of intricate, perfusable channel networks within volumetric tissue constructs [87]. Similarly, microfluidic device integration with organoid culture systems (organ-on-a-chip platforms) provides controlled fluid flow and mechanical stimulation that enhance vascular maturation and function [91].
Figure 2: Biofabrication Technologies for Vascularization
Smart Biomaterials and Stimuli-Responsive Systems
Next-generation biomaterials are being engineered with increasingly sophisticated biological functionalities. Stimuli-responsive biomaterials that release angiogenic factors in response to specific environmental cues (e.g., matrix metalloproteinases, reactive oxygen species, pH changes) enable more precise spatiotemporal control over vascularization processes [89]. For instance, researchers have developed a metformin/copper-loaded polydopamine nanoparticle composite hydrogel with dual ROS-scavenging and copper ion-releasing capabilities that simultaneously addresses oxidative stress, provides antibacterial activity (>85% antibacterial rate), recruits fibroblasts and vascular endothelial cells, and promotes vascular regeneration [89].
The emerging frontier of immunomodulatory biomaterials recognizes that the host immune response plays a critical role in determining vascularization outcomes. Scaffolds that selectively polarize macrophages toward pro-regenerative (M2) phenotypes create a favorable microenvironment for vascular growth [92]. For example, porcine ADM has been shown to guide M2 macrophage recruitment, generating a series of growth factors that promote rat wound vascular regeneration [87]. Similarly, magnesium ions in hydrogels mediate M2 macrophage reprogramming through neurovascular coupling mechanisms, providing an immunomodulatory microenvironment conducive to diabetic wound repair [89].
The vascularization challenge remains a central focus in tissue engineering research, with biomaterials serving as critical enabling technology for overcoming diffusion limitations and establishing functional perfusion networks. Strategic combinations of material composition, structural design, biological signaling, and advanced fabrication are yielding increasingly sophisticated solutions that better recapitulate native vascular biology. As biomaterials continue to evolve from passive scaffolds to active participants in regenerative processes, their capacity to guide and support vascularization will undoubtedly expand. The convergence of these biomaterial strategies with emerging technologies in 3D bioprinting, microfluidics, and stem cell biology promises to accelerate progress toward the ultimate goal of engineering complex, vascularized tissues for clinical application.
The development of biomaterials for tissue engineering represents a frontier in regenerative medicine, aiming to overcome the critical limitations of donor organ shortages and suboptimal healing outcomes. Within this field, decellularized extracellular matrix (dECM) has emerged as a premier biological scaffold, prized for its innate biocompatibility and preservation of tissue-specific biochemical and structural cues. The central challenge, however, lies in the preparation of these scaffolds: the processes of decellularization and sterilization must achieve the complete removal of immunogenic cellular material while simultaneously preserving the delicate bioactivity of the ECM. This technical review provides an in-depth analysis of current methods, evaluating their efficacy in removing cellular components and their impact on the structural integrity, mechanical properties, and bioactive potential of the resulting scaffold. Furthermore, it situates this technical balancing act within the broader thesis of biomaterials research, wherein the ultimate goal is to engineer a microenvironment that not only supports but actively orchestrates tissue regeneration.
The extracellular matrix (ECM) is a dynamic, complex network of structural and functional proteins, glycosaminoglycans, and signaling molecules that provides not only architectural support but also critical biochemical and biomechanical cues for cellular behavior [3]. Decellularized ECM scaffolds harness this innate biological wisdom by removing cellular antigens that trigger immune rejection while aiming to preserve the native ECM's composition and three-dimensional architecture [93] [94]. This makes dECM an ideal biomaterial, as it provides a tissue-specific microenvironment that supports cell adhesion, proliferation, differentiation, and ultimately, functional tissue regeneration [94] [95].
The efficacy of any decellularization protocol is judged by two paramount, and often competing, objectives: efficacy and bioactivity. Efficacy entails the complete removal of cellular components (e.g., nuclei, mitochondria) and genetic material (DNA, RNA) to levels deemed non-immunogenic ( [93] [96]). Bioactivity refers to the preservation of the ECM's native composition, including key proteins like collagens, glycosaminoglycans (GAGs), growth factors, and the intricate ultrastructure that defines its mechanical properties and signaling capabilities [94] [3]). The process of sterilization adds another layer of complexity, as techniques must eradicate microbial life without compromising the scaffold's bioactivity or introducing cytotoxic residues [93]. Achieving this balance is the cornerstone of producing clinically viable dECM scaffolds for tissue engineering.
Decellularization Methods: Mechanisms and Impacts
Decellularization techniques can be broadly categorized into physical, chemical, and enzymatic methods. The choice and combination of these methods are highly dependent on the source tissue's properties, such as density, thickness, and lipid content [93] [95].
Physical Methods
Physical methods primarily function by lysing cell membranes through mechanical force or energy input.
- Thermal Shock (Freeze-Thaw): This method involves rapid freezing (e.g., -80°C) and thawing (e.g., 37°C) of tissues. The formation of intracellular ice crystals pierces and destroys cell membranes [93]. While effective for cell lysis and relatively gentle on ECM mechanical properties, it is insufficient for complete decellularization on its own, as it leaves behind significant cellular debris and DNA. It is therefore almost always used as an initial step followed by chemical or enzymatic treatments to wash away the remnants [93].
- High Hydrostatic Pressure (HHP): HHP applies pressurized water (e.g., 980 MPa) to tissues, disrupting cell membranes and altering cellular ultrastructure [93]. It can significantly reduce decellularization time but may induce ice crystal formation that damages the ECM unless controlled with colloidal agents like dextran [93].
- Supercritical Fluids: Utilizing fluids like carbon dioxide (CO₂) at pressures and temperatures above their critical point, this method offers rapid penetration and removal of cellular components without requiring extensive rinsing. Its low viscosity and high diffusivity make it a promising technology for complex organs [93].
Chemical and Enzymatic Methods
These methods employ chemical agents and enzymes to solubilize and remove cellular components.
- Ionic Detergents (e.g., Sodium Dodecyl Sulfate - SDS): SDS is a highly effective anionic detergent that robustly disrupts lipid-lipid and lipid-protein interactions, leading to efficient nuclear removal and decellularization of dense tissues [93] [94]. However, it is also the most damaging to ECM structure, causing significant loss of GAGs and growth factors, and can be difficult to rinse out completely, leading to potential cytotoxicity [94] [95].
- Non-Ionic Detergents (e.g., Triton X-100): Triton X-100 is milder than SDS and effectively solubilizes lipid bilayers. It is less disruptive to collagen structure but is often ineffective at removing nuclear material alone, necessitating combination with other methods [94].
- Acids and Bases: Chemical treatments using acids (e.g., peracetic acid) or bases (e.g., sodium hydroxide) can efficiently remove cells by denaturing proteins and nucleic acids. While biocompatible at low concentrations, they can have a pronounced negative impact on ECM constituents and their structure, making them more suitable for thin tissues [94].
- Enzymes (e.g., Trypsin, Nucleases): Trypsin cleaves peptide bonds, disrupting cell-cell and cell-ECM adhesions. Nucleases (DNases, RNases) are specifically used to digest residual genetic material following cell lysis, which is crucial for reducing immunogenicity [94] [96]. Enzymatic treatments must be carefully controlled, as prolonged exposure can damage ECM proteins like collagen and fibronectin [96].
Table 1: Comparative Analysis of Common Decellularization Methods
| Method | Mechanism of Action | Key Advantages | Key Disadvantages & Impact on Bioactivity |
|---|---|---|---|
| Thermal Shock | Intracellular ice crystal formation lyses cells [93]. | Preserves mechanical properties; minimal ECM disruption [93]. | Incomplete; leaves >88% DNA; requires secondary methods [93]. |
| High Hydrostatic Pressure | High pressure disrupts cell membranes [93]. | Fast; retains ECM structure and immunocompatibility [93]. | Risk of ice crystal damage to ECM; requires additives [93]. |
| Ionic Detergents (SDS) | Disrupts phospholipid bilayers and protein interactions [94]. | Highly effective for dense tissues and nuclear removal [93] [94]. | Damages collagen & GAGs; hard to rinse; cytotoxic residues [94] [95]. |
| Non-Ionic Detergents (Triton X-100) | Solubilizes lipid membranes [94]. | Milder on ECM structure; good for lipid removal [94]. | Poor nuclear removal; may require cytotoxic co-agents [94]. |
| Trypsin | Proteolytic enzyme cleaves adhesion proteins [94]. | Effective at disrupting cell-ECM attachments [94]. | Prolonged exposure damages ECM proteins (collagen, fibronectin) [96]. |
The following workflow diagram illustrates the decision-making process for selecting and applying these decellularization methods.
Sterilization Techniques for dECM Scaffolds
Sterilization is a critical and non-negotiable step for clinical application. However, the same properties that make dECM bioactive—native proteins and growth factors—also make it susceptible to damage from harsh sterilization processes.
- Gamma Irradiation: A widely used physical sterilization method that damages microbial DNA. While effective, the required doses can cause fragmentation of collagen fibers and a significant loss of mechanical strength and growth factor bioactivity [93].
- Chemical Sterilants (e.g., Ethylene Oxide - ETO, Peracetic Acid): ETO is a gas that alkylates microbial DNA and proteins. Its main drawback is the potential for cytotoxic residues to remain within the scaffold, which can elicit adverse host responses [93]. Peracetic acid is effective and leaves non-toxic byproducts but can oxidize and damage ECM components if not carefully controlled [94].
- Electron Beam (E-Beam) Sterilization: Similar in principle to gamma irradiation, E-beam is a faster process but with less material penetration. It is increasingly used in sensitive applications, including food and biomedical product sterilization, due to its controllability [97].
The choice of sterilization must be validated for each specific dECM scaffold type, as the trade-off between sterility assurance and bioactivity preservation is a delicate one.
Evaluating Decellularization Efficacy and Bioactivity
Rigorous quality control is essential to ensure that the dual goals of decellularization have been met. The consensus is that effective decellularization requires a residual DNA content of less than 50 ng per mg of dry scaffold weight and the absence of visible nuclear material in tissue sections stained with DAPI or H&E [93] [96].
Beyond cellular removal, the preservation of bioactivity is assessed through multiple lenses:
- Biochemical Composition: Quantification of retained ECM components, such as total collagen (e.g., hydroxyproline assay) and sulfated GAGs (e.g., DMMB assay), is crucial [93] [94].
- Ultrastructural Integrity: Scanning Electron Microscopy (SEM) is used to visualize the 3D architecture of the ECM, confirming the preservation of porous networks and collagen fibril organization [95].
- Mechanical Properties: Tensile and compressive testing ensures that the mechanical integrity of the scaffold matches that of the native tissue, which is critical for guiding cell behavior and withstanding in vivo forces [55] [3].
- In Vitro Biocompatibility: Scaffolds are seeded with relevant cells (e.g., fibroblasts, stem cells) to assess cell viability, adhesion, proliferation, and migration. Successful recellularization is a strong indicator of retained bioactivity [95].
- In Vivo Biocompatibility: Implantation in animal models allows for the assessment of the host immune response. A well-decellularized and sterilized scaffold should integrate with host tissue, support vascularization, and provoke only a minimal, transient inflammatory response rather than a classic foreign body reaction [95] [98].
The Cellular Interface: How Bioactive dECM Orchestrates Regeneration
The success of a dECM scaffold hinges on its dynamic interaction with host and seeded cells. This interaction is largely mediated by integrins, transmembrane receptors that bind to specific ligands within the ECM, such as the RGD (Arginine-Glycine-Aspartic acid) peptide sequence found in fibronectin and other proteins [3]. Upon binding, integrins cluster and form focal adhesions, which act as mechanical and biochemical signaling hubs. This triggers the activation of key intracellular pathways, including:
- Focal Adhesion Kinase (FAK)/Src Pathway: Regulates cytoskeletal dynamics and cell migration [3].
- MAPK/ERK Pathway: Influences gene expression related to cell proliferation and differentiation [3].
- PI3K/Akt Pathway: Promotes cell survival [3].
This integrin-mediated signaling, combined with the presentation of preserved growth factors (e.g., VEGF, TGF-β), creates a microenvironmental niche that directs cellular fate and promotes functional tissue regeneration. The following diagram illustrates this critical signaling cascade.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagents for Decellularization and Analysis
| Reagent / Material | Function in Research | Key Considerations |
|---|---|---|
| Sodium Dodecyl Sulfate (SDS) | Ionic detergent for effective cell lysis and nuclear removal from dense tissues [93] [94]. | Concentration and exposure time must be optimized to minimize ECM damage and ensure complete rinsing to avoid cytotoxicity [95]. |
| Triton X-100 | Non-ionic detergent for lipid removal and delipidation, often used in sequence with SDS [93] [98]. | Less effective at removing nuclear material alone; often used in combination with other agents [94]. |
| DNase/RNase | Enzymatic degradation of residual DNA and RNA to reduce immunogenicity after cell lysis [94] [96]. | Essential follow-up treatment; requires specific ionic conditions (e.g., Mg²⁺) for optimal activity. |
| Peracetic Acid | Chemical sterilization and disinfection agent; also aids in decellularization [94]. | Effective with low-toxicity byproducts (water, acetic acid), but can oxidize and damage ECM if misused [94]. |
| RGD Peptide | Synthetic peptide containing Arg-Gly-Asp sequence used to biofunctionalize scaffolds to enhance cell adhesion [3] [98]. | Can be conjugated to scaffolds (e.g., via dopamine coating) to improve integrin binding and cellular interaction [98]. |
The journey of a tissue or organ from its native state to a implantable, bioinstructive dECM scaffold is a testament to the sophistication of modern biomaterials science. The core challenge—balancing the efficacy of decellularization and sterilization with the preservation of bioactivity—is not merely a technical hurdle but a fundamental consideration in the design of regenerative therapies. The optimal protocol is never a one-size-fits-all solution; it is a carefully calibrated process tailored to the specific tissue and its intended clinical application. As research advances, the integration of novel technologies like supercritical fluids, advanced biofunctionalization with peptides and growth factors, and precision sterilization will further enhance our ability to create off-the-shelf scaffolds that truly mimic the native ECM. Within the broader thesis of biomaterials, decellularized scaffolds stand as a powerful example of leveraging biology's own blueprint to engineer microenvironments that guide the complex process of healing and regeneration, thereby pushing the boundaries of what is possible in tissue engineering and regenerative medicine.
Scalability and Cost-Effectiveness in Manufacturing
The field of tissue engineering (TE) aims to create biological substitutes to restore, maintain, or improve tissue function, representing a pivotal advancement in regenerative medicine and personalized healthcare [99]. While much research focuses on biological performance and novel material discovery, the translation of these innovations into clinically available therapies hinges overwhelmingly on scalability and cost-effectiveness in manufacturing. The role of biomaterials extends beyond mere biocompatibility; they must be processable using manufacturing technologies that can reliably produce complex structures at relevant scales. Manufacturing scalability ensures that tissue engineering products can transition from promising laboratory prototypes to widely available clinical solutions, addressing the needs of a global patient population. Simultaneously, cost-effectiveness determines the economic viability and healthcare system accessibility of these advanced therapies. This technical guide examines the core manufacturing paradigms, quantitative performance metrics, and experimental methodologies that underpin scalable and cost-effective production of biomaterial-based tissue engineering constructs, providing researchers with the practical framework necessary to advance the field toward widespread clinical impact.
Biomaterial Manufacturing Techniques: Scalability and Economic Analysis
The selection of appropriate manufacturing techniques is fundamental to balancing technical requirements with production scalability and cost considerations. Several manufacturing platforms have emerged as particularly promising for tissue engineering applications, each with distinct advantages and limitations regarding scalability and cost-effectiveness.
Additive Manufacturing in Tissue Engineering
Additive manufacturing (AM), particularly material extrusion-based techniques, has revolutionized the approach to fabricating complex tissue engineering scaffolds by offering unprecedented design freedom, personalization capabilities, and reduced material waste compared to traditional manufacturing methods [100]. According to market analysis, the 3D printing healthcare market is projected to grow at a compound annual growth rate (CAGR) of 18.6% between 2024 and 2032, rising from $2.9 billion in 2023 to $13.8 billion by 2032, reflecting the significant commercial and clinical adoption of these technologies [100].
Material extrusion encompasses several specific techniques suitable for different biomaterial classes and application requirements:
Fused Filament Fabrication (FFF): Utilizes thermoplastic filaments which are heated and extruded through a nozzle. Well-suited for medical-grade polymers like PLA and PEEK, FFF offers moderate resolution at low equipment costs, making it accessible for prototyping and small-scale production [100].
Direct Ink Writing (DIW): Extrudes shear-thinning bioinks or pastes at room temperature or with mild heating, preserving the bioactivity of incorporated biological factors. DIW enables the incorporation of high biomaterial concentrations and cell-laden printing but requires post-processing for many materials [100].
Direct Pellet Extrusion (DPE): Extrudes raw polymer pellets directly, eliminating the filament production step and significantly reducing material costs, especially for high-performance polymers. DPE systems typically feature larger nozzles suitable for larger scaffold constructions [100].
Electrospinning and Alternative Manufacturing Approaches
Beyond material extrusion, electrospinning represents a highly versatile manufacturing technique for producing nanofibrous scaffolds that closely mimic the native extracellular matrix (ECM). Recent advances have incorporated artificial intelligence and machine learning to enhance process control and predictability. For instance, artificial neural networks (ANNs) have demonstrated promising accuracy in predicting polyethylene nanofiber diameter with an average error of just 2.29%, significantly streamlining parameter optimization and reducing material waste during process development [101].
Additional manufacturing approaches include:
- Cell Sheet Engineering: Creates scaffold-free tissues by harvesting intact cell layers from temperature-responsive culture surfaces.
- Microfluidics: Enables precise patterning of cells and biomaterials with high resolution for complex tissue architectures.
- Decellularization: Utilizes natural tissue scaffolds that preserve complex ECM composition and bioactivity.
Table 1: Technical and Economic Comparison of Biomaterial Manufacturing Techniques for Tissue Engineering
| Manufacturing Technique | Typical Resolution | Scalability Potential | Equipment Cost | Material Utilization Efficiency | Suitable Biomaterials |
|---|---|---|---|---|---|
| Fused Filament Fabrication (FFF) | 100-300 μm | Medium-High | Low | High (Near-net-shape) | Thermoplastics (PLA, PEEK) |
| Direct Ink Writing (DIW) | 50-500 μm | Medium | Medium | High | Hydrogels, Ceramic Pastes, Bioinks |
| Direct Pellet Extrusion (DPE) | 200-1000 μm | High | Medium | Very High (Raw material) | Thermoplastic Pellets |
| Electrospinning | 0.1-5 μm | Low-Medium | Low-Medium | Medium (Solution-based) | Polymer Solutions, Composites |
| Bioprinting | 10-300 μm | Low | High | Medium | Cell-laden Hydrogels, Bioinks |
Quantitative Performance Metrics and Benchmarking
Objective evaluation of manufacturing performance requires standardized metrics that enable direct comparison across different technologies and material systems. The following quantitative data provides critical benchmarking parameters for assessing scalability and cost-effectiveness.
Production Metrics and Economic Indicators
Bibliometric analysis of tendon tissue engineering, as a representative tissue engineering subfield, reveals a consistent upward trajectory in annual publications, following the cubic function: y = 0.83944 + 4.41499x - 1.16772x² + 0.07371x³ (R² = 0.999) for cumulative publications from 1991-2023 [68]. This substantial and accelerating research investment underscores the growing importance of the field and the concomitant need for scalable manufacturing solutions.
The United States (571 publications) and China (550 publications) lead in research output for tendon tissue engineering, followed by the UK (166), Italy (118), and Germany (113) [68]. This geographic distribution highlights the global research effort and the need for manufacturing approaches that can be implemented across different healthcare systems and regulatory environments.
Table 2: Performance Comparison of Material Extrusion Techniques for Biomedical Applications
| Performance Parameter | Fused Filament Fabrication (FFF) | Direct Ink Writing (DIW) | Direct Pellet Extrusion (DPE) | Bioprinting |
|---|---|---|---|---|
| Layer Height | 100-300 μm | 50-500 μm | 200-1000 μm | 10-300 μm |
| Nozzle Diameter | ~0.4 mm | 0.1-1 mm | 0.5-2 mm | 0.1-0.5 mm |
| Dimensional Accuracy | ±0.1-0.2 mm | ±0.05-0.2 mm | ±0.2-0.5 mm | ±0.01-0.1 mm |
| Mechanical Anisotropy | Significant (Weak interlayer adhesion) | Moderate | Significant | Highly variable |
| Production Speed | Medium | Slow-Medium | High | Very Slow |
| Relative Cost per Unit Volume | Low | Medium-High | Very Low | High |
Experimental Protocols for Scalable Manufacturing
Robust experimental methodologies are essential for developing, optimizing, and validating scalable manufacturing processes for tissue engineering applications. The following protocols provide standardized approaches for key manufacturing processes.
Protocol 1: Artificial Neural Network Optimization for Electrospinning Parameters
Purpose: To streamline the optimization of electrospinning parameters for nanofiber production using machine learning, reducing traditional trial-and-error approaches [101].
Materials and Equipment:
- Electrospinning apparatus with controlled voltage, flow rate, and collector distance
- Polymer solution of interest (e.g., polyethylene)
- Data set of electrospinning parameters and resulting fiber diameters (minimum 100 records recommended)
- Artificial neural network software platform (Python with TensorFlow/PyTorch, MATLAB)
Procedure:
- Data Collection: Compile a comprehensive dataset of electrospinning parameters including solution concentration, viscosity, applied voltage, flow rate, collector distance, and corresponding fiber diameters from literature or controlled experiments.
- Network Architecture Design: Configure a feedforward neural network with 3-5 hidden layers, using linear activation functions for input/output layers and nonlinear functions (e.g., ReLU, sigmoid) for hidden layers.
- Data Partitioning: Split the dataset into training (70%), validation (15%), and testing (15%) subsets, ensuring representative distribution across parameter spaces.
- Model Training: Train the ANN using backpropagation algorithm, monitoring validation error to prevent overfitting.
- Model Validation: Test trained model against laboratory measurements, calculating mean absolute percentage error (MAPE). The study by Solis-Rios et al. achieved an average error of 2.29% using this approach [101].
- Parameter Optimization: Use the validated model to predict optimal electrospinning parameters for target fiber diameters, verifying with limited experimental trials.
Scalability Assessment: This approach reduces optimization time by up to 65% compared to conventional one-factor-at-a-time methodologies, with particular efficiency gains when applied to new material systems.
Protocol 2: Multi-Material Scaffold Fabrication via Hybrid Extrusion
Purpose: To manufacture complex, multi-material tissue engineering scaffolds that mimic the heterogeneous composition of native tissues using a hybrid extrusion approach [100].
Materials and Equipment:
- Dual-extrusion additive manufacturing system with independent temperature control
- Biomedical-grade thermoplastic filaments (PLA, PCL, PLGA) or pellet forms
- Compatible hydrogel bioink (alginate, gelatin methacryloyl, collagen)
- Crosslinking system (UV light, ionic solution) for hydrogels
- CAD software with multi-material support (e.g., nTopology, SolidWorks)
Procedure:
- Scaffold Design: Create a digital model of the scaffold with defined regions for different materials, incorporating porous architectures (300-500 μm pore size) and anatomical geometry.
- Material Preparation: Dry thermoplastic materials to remove moisture (60°C vacuum oven, ≥4 hours). Prepare bioink according to standardized protocols and maintain at appropriate temperature.
- Machine Setup: Calibrate separate extrusion systems for thermoplastics (high temperature, 160-220°C depending on material) and hydrogels (room temperature or cooled).
- Integrated Printing: Program toolpaths to deposit structural thermoplastic elements followed by hydrogel incorporation into designated regions, minimizing cross-contamination.
- Post-Processing: Apply appropriate crosslinking method for hydrogel components (UV exposure, ionic crosslinking). Sterilize using method appropriate for material combination (ethanol, gamma irradiation).
- Quality Control: Assess dimensional accuracy against digital model (±0.2 mm tolerance), interlayer bonding integrity, and material interface stability.
Economic Analysis: Hybrid systems increase initial equipment costs by 30-50% but reduce overall production time for complex constructs by 40-60% compared to sequential manufacturing approaches.
Protocol 3: Mechanical and Biological Performance Validation
Purpose: To comprehensively evaluate manufactured scaffolds against functional requirements for target tissue application.
Materials and Equipment:
- Universal mechanical testing system
- Cell culture facilities and appropriate cell lines
- Sterile culture media and reagents
- Scanning electron microscope
- Biochemical assay kits (DNA content, metabolic activity, tissue-specific markers)
Procedure:
- Structural Characterization: Image scaffold microstructure using SEM, quantifying pore size, fiber diameter, and interconnectivity using image analysis software.
- Mechanical Testing: Conduct uniaxial compression/tension testing at physiological strain rates, measuring modulus, strength, and failure strain. Test multiple orientations to quantify anisotropy.
- In Vitro Biological Evaluation:
- Seed scaffolds at appropriate cell density (e.g., 50,000-100,000 cells/cm³)
- Assess cell viability (Live/Dead staining), proliferation (DNA content), and metabolic activity (AlamarBlue, MTT) at days 1, 3, 7, and 14
- Evaluate tissue-specific matrix production (histology, immunohistochemistry, biochemical assays)
- For tendon applications, assess collagen I/III ratio; for bone, measure calcium deposition
- Degradation Profiling: Monitor mass loss and mechanical property changes in physiological solution over 4-12 weeks, measuring pH changes and degradation products.
Scalability Correlation: Establish correlation between small-scale (≤1 cm³) and large-scale (≥10 cm³) construct properties to validate scalability of manufacturing parameters.
Visualization of Manufacturing Workflows
The following diagrams illustrate key processes and decision pathways in scalable manufacturing of tissue engineering constructs, created using DOT language with the specified color palette.
Diagram 1: Biomaterial Manufacturing Pathway. This workflow illustrates the decision pathway for selecting and scaling biomaterial manufacturing techniques in tissue engineering.
Diagram 2: Iterative Scaffold Design Process. This diagram shows the iterative development cycle for tissue engineering scaffolds, integrating clinical requirements with manufacturing constraints.
Research Reagent Solutions for Manufacturing Innovation
The following reagents, materials, and technologies represent essential components for advancing scalable manufacturing in tissue engineering research.
Table 3: Essential Research Reagents and Materials for Scalable Manufacturing
| Reagent/Material | Function/Application | Scalability Consideration | Cost Impact |
|---|---|---|---|
| Polylactic Acid (PLA) | Bioabsorbable thermoplastic for FFF; temporary implants and scaffolds | High scalability from established supply chains; easy processing | Low cost; derived from renewable resources (sugarcane, corn starch) |
| Polyether Ether Ketone (PEEK) | High-performance thermoplastic for load-bearing implants | Requires high-temperature processing; limited by equipment capabilities | High material cost offset by durability and longevity in implants |
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable hydrogel for DIW and bioprinting | Crosslinking time impacts production throughput; batch-to-batch variability | Medium cost; versatile mechanical properties through concentration control |
| Peptide Amphiphiles | Self-assembling nanofibers for injectable scaffolds | Eliminates manufacturing equipment through self-assembly | High synthesis cost but reduced processing requirements |
| Cerium Oxide Nanoparticles (CeO2NPs) | Antioxidant additive for wound healing scaffolds | Easily incorporated into multiple material systems; enhances functionality | Moderate cost with significant biological benefit (ROS scavenging) |
| Exopolysaccharides (from Geobacillus sp.) | Drug delivery matrix from cost-effective lignocellulosic biomass | Utilizes sustainable, low-cost feedstocks; simple film formation | Very low cost; utilizes extremophile bacterial synthesis |
| Ti-Mo-Cu Alloys | Metallic biomaterials with enhanced corrosion resistance | Compatible with powder-based AM processes; improved biocompatibility | Higher initial cost than conventional alloys but improved long-term performance |
Current Challenges and Future Directions
Despite significant advances, several technical challenges continue to limit the scalability and cost-effectiveness of biomaterial manufacturing for tissue engineering. Key persistent challenges include:
- Anisotropic Mechanical Properties: Layer-by-layer fabrication in material extrusion creates directional weakness, particularly in the Z-axis, limiting application in load-bearing tissues [100].
- Biocompatibility and Sterilization: Many manufacturing processes compromise material biocompatibility through high temperatures, harsh solvents, or radiation sterilization, requiring careful optimization [100].
- Vascularization Integration: Manufacturing perfusable vascular networks within thick tissues remains a significant limitation for nutrient and oxygen transport [99] [101].
- Process Monitoring and Control: Inconsistent output quality due to inadequate real-time monitoring systems increases rejection rates and costs [100].
Future advancements will likely focus on several promising directions:
- Artificial Intelligence and Machine Learning: AI-driven design optimization and real-time defect detection using convolutional neural networks (CNN) and artificial neural networks (ANN) will enhance process reliability and reduce waste [101] [100].
- Hybrid Manufacturing Approaches: Combining multiple manufacturing technologies (e.g., FFF for structural elements with DIW for biological components) will enable more complex, functional tissue constructs [100].
- Sustainable Biomaterial Sources: Increasing utilization of biologically derived materials from sustainable sources, such as exopolysaccharides from lignocellulosic biomass, will improve cost-effectiveness and environmental compatibility [101].
- Closed-Loop Control Systems: Integration of in-process monitoring with automated parameter adjustment will ensure consistent quality and reduce manual intervention in scaled production [100].
- Standardized Characterization Protocols: Development of universally accepted benchmarking methods will enable direct comparison across studies and facilitate technology transfer to industrial partners.
The continued convergence of biomaterial science with advanced manufacturing technologies holds the potential to overcome current limitations, ultimately enabling the widespread clinical adoption of tissue engineering therapies that are both biologically functional and economically viable.
The development and commercialization of biomaterials and tissue engineering products are governed by a complex regulatory landscape designed to ensure safety and efficacy while fostering innovation. In the United States, the Food and Drug Administration (FDA) serves as the primary regulatory body for these advanced therapies, operating under the Center for Biologics Evaluation and Research (CBER) for most regenerative medicine products [102]. The regulatory pathway for these products is significantly influenced by their classification as biological products, medical devices, or combination products, depending on their primary mode of action [44]. Understanding this framework is crucial for researchers and developers aiming to translate laboratory innovations into clinically available therapies that can address the growing global burden of chronic wounds, degenerative diseases, and organ failure [3].
The 21st Century Cures Act, enacted in 2016, established new regulatory designations specifically for regenerative medicine therapies, including the Regenerative Medicine Advanced Therapy (RMAT) designation, which aims to expedite the development and review of products for serious conditions [102]. This evolving regulatory environment reflects the unique challenges and opportunities presented by biomaterials and tissue engineering, particularly as these technologies increasingly incorporate complex elements such as decellularized extracellular matrix (ECM), synthetic polymers, and cellular components [3] [103]. For researchers operating within the context of biomaterials development, navigating this pathway requires careful planning from the earliest stages of product design through to post-market surveillance.
FDA Regulatory Pathways and Designations
Product Classification and Oversight
The FDA classifies regenerative medicine products based on their composition and intended function, which determines the applicable regulatory requirements. Human cells, tissues, and cellular and tissue-based products (HCT/Ps) are regulated under Section 361 of the Public Health Service Act if they meet specific criteria, including minimal manipulation and homologous use [44]. Products that exceed these criteria typically require licensing under Section 351 and are subject to more rigorous premarket review. Biomaterials and tissue-engineered constructs often fall into the latter category, particularly when they combine scaffolds with cellular components or undergo significant processing. Since 2023, the Office of Therapeutic Products (OTP) within CBER has been responsible for evaluating new cell and gene therapy products, including many tissue-engineered constructs [44].
Table 1: FDA Centers and Product Jurisdictions for Biomaterials and Tissue Engineering
| FDA Center | Product Types | Key Regulations |
|---|---|---|
| CBER/Office of Therapeutic Products (OTP) | Cellular therapies, gene therapies, combination products with cellular components | PHS Act Section 351, FD&C Act, 21 CFR Part 1271 |
| Center for Devices and Radiological Health (CDRH) | Biomaterial scaffolds without cellular components, medical devices for tissue collection or processing | FD&C Act, 510(k), Premarket Approval (PMA) |
| Combination Products | Biomaterials integrated with cells or active biological components | 21 CFR Part 4 |
Expedited Programs for Regenerative Medicine
To accelerate the availability of promising therapies, the FDA offers several expedited programs. The RMAT designation, created under the 21st Century Cures Act, is available for regenerative medicine therapies intended to treat, modify, reverse, or cure a serious condition [102]. To qualify, preliminary clinical evidence must indicate the potential to address unmet medical needs. The benefits of RMAT designation are substantial and include opportunities for more frequent interactions with FDA throughout the development process, potential eligibility for accelerated approval based on surrogate or intermediate endpoints, and flexibility in review structure [102].
Other expedited programs that may be relevant to biomaterials and tissue engineering products include Fast Track designation and Breakthrough Device designation, depending on the product's characteristics and intended use. These pathways recognize the unique challenges in developing regenerative medicine products and aim to provide sponsors with enhanced regulatory clarity while maintaining appropriate safety standards. As of 2025, the FDA continues to refine its guidance on these programs, with a draft guidance document on "Expedited Programs for Regenerative Medicine Therapies for Serious Conditions" currently available for comment [102].
Table 2: FDA Expedited Programs Applicable to Biomaterials and Tissue Engineering
| Program | Legal Authority | Eligibility Criteria | Key Benefits |
|---|---|---|---|
| RMAT Designation | FD&C Act Section 506(g) | Regenerative medicine therapy for serious condition; preliminary clinical evidence | Frequent FDA interactions, potential for accelerated approval |
| Fast Track | FD&C Act Section 506(b) | Therapy for serious condition; addresses unmet medical need | Rolling BLA review, more frequent communication |
| Breakthrough Device | FD&C Act Section 515B | Device that provides more effective treatment/diagnosis | Priority review, interactive review process |
Biomaterial-Specific Considerations for Regulatory Submissions
Extracellular Matrix and Decellularized Tissues
Decellularized ECM scaffolds represent one of the most successfully translated classes of biomaterials in regenerative medicine, with millions of patients treated for applications including breast reconstruction, wound care, and hernia repair [103]. The regulatory pathway for these materials requires careful attention to decellularization protocols, residual DNA quantification, and preservation of native ECM components that facilitate constructive remodeling. Effective decellularization must remove cellular debris while maintaining the structural, biochemical, and biomechanical properties of the native ECM [103]. Common challenges include immunogenicity from residual cellular material and batch-to-batch variability, which must be controlled through standardized manufacturing processes.
The clinical success of ECM scaffolds has been linked to their ability to provide both structural support and bioactive signals during tissue repair. As noted in recent research, "degradation products of the ECM are released into the local milieu and influence the host innate immune response, which in turn affects downstream downstream remodeling outcomes" [103]. This biological activity positions many ECM-based products as combination products rather than simple medical devices, complicating their regulatory pathway. Furthermore, the mechanical properties of ECM scaffolds can decay upon implantation, requiring careful characterization of degradation profiles and structural performance over time [103].
Synthetic and Composite Biomaterials
Synthetic polymers and composite materials offer advantages in terms of tunable properties and manufacturing reproducibility but face distinct regulatory challenges. These include demonstrating biocompatibility through standardized testing (ISO 10993), characterizing degradation products, and establishing batch consistency [3]. For biomaterials designed to actively direct cellular behavior through integrated signaling molecules or specific structural features, regulators require robust evidence of the proposed mechanism of action and its relationship to clinical outcomes.
Advanced manufacturing technologies such as 3D bioprinting introduce additional regulatory considerations, including the validation of printing processes, bioink composition, and the stability of printed constructs [3]. The FDA's emerging regulatory framework for additive manufacturing of medical devices provides some guidance, but applications in tissue engineering often push beyond established boundaries, particularly when incorporating living cells during the manufacturing process. For all biomaterials, the Chemistry, Manufacturing, and Controls (CMC) section of regulatory submissions must comprehensively describe the material sourcing, manufacturing process, quality control measures, and release specifications [44].
Experimental Characterization for Regulatory Submissions
In Vitro Assessment of Biomaterial-Host Interactions
Comprehensive in vitro characterization provides the foundation for regulatory submissions and informs the design of subsequent preclinical studies. Key assays must evaluate cell-biomaterial interactions, integration with host tissues, and the biological activity of the product. For biomaterials designed to replicate ECM functions, this includes assessment of integrin-mediated signaling pathways that coordinate cellular responses during tissue repair [3].
Experimental Protocol: Integrin Signaling Activation Assay
- Cell Seeding: Plate human mesenchymal stem cells (hMSCs) at 10,000 cells/cm² on test biomaterials and control surfaces (tissue culture plastic, commercial ECM coatings).
- Immunofluorescence Staining: At 24, 48, and 72 hours, fix cells and stain for integrin subunits (β1, αv, α5), focal adhesion kinase (FAK), and phosphorylated FAK (Tyr397).
- Image Analysis: Quantify focal adhesion size, number, and distribution using high-content imaging and analysis software.
- Western Blotting: Analyze activation of downstream signaling pathways (MAPK/ERK, PI3K/Akt) at same time points.
- Functional Assessment: Correlate signaling activation with cell behaviors (migration, proliferation, differentiation) using time-lapse microscopy and proliferation assays.
This integrated approach provides mechanistic evidence of how biomaterials engage with cellular machinery to promote regenerative outcomes, addressing FDA requirements for understanding product mechanism of action [3].
Diagram: Integrin-Mediated Signaling Pathway in Biomaterial-Tissue Integration. This pathway illustrates how ECM components in biomaterials engage cellular machinery to drive regenerative outcomes.
Preclinical Evaluation in Animal Models
Preclinical studies in appropriate animal models are essential for evaluating the safety and bioactivity of biomaterials and tissue-engineered products. These studies should assess biocompatibility, integration with host tissues, degradation profile, and functional efficacy in disease-relevant models. The FDA emphasizes the 3Rs principle (Replacement, Reduction, Refinement) in animal study design and requires justification of the selected model's relevance to the intended human application.
Experimental Protocol: Subcutaneous Implantation for Biocompatibility
- Implant Preparation: Sterilize test biomaterials (1cm diameter discs) and pre-wet in physiological solution.
- Animal Model: Utilize immunocompetent rodents (e.g., Sprague-Dawley rats, n=8 per group) following IACUC approval.
- Surgical Implantation: Create subcutaneous pockets via dorsal incision and insert one implant per pocket, with closure in layers.
- Time Points: Euthanize animals at 1, 4, and 12 weeks post-implantation for analysis.
- Histological Analysis: Explain, section, and stain implants with host tissue interface (H&E, Masson's Trichrome, immunohistochemistry for macrophages [CD68], T-cells [CD3]).
- Scoring System: Apply semi-quantitative scoring for inflammatory response, vascularization, fibrotic capsule formation, and tissue integration.
This standardized approach generates comprehensive data on host-biomaterial interactions that directly support regulatory submissions for both devices and biologic products [3] [103].
Manufacturing and Quality Control Requirements
Cell Manufacturing for Tissue-Engineered Products
For tissue-engineered products incorporating cellular components, the cell manufacturing process represents a critical determinant of product safety and efficacy. Current FDA-approved, cell-based tissue-engineered products mainly consist of avascular tissues with relatively simple form and function, reflecting the challenges in manufacturing more complex constructs [44]. Key considerations include maintaining cellular identity and potency during expansion, controlling cellular heterogeneity, and ensuring batch-to-batch consistency.
The FDA defines potency as "the specific ability or capacity of the product, as indicated by appropriate laboratory tests or by adequately controlled clinical data obtained through the administration of the product in the manner intended, to effect a given result" [44]. Potency assays must be developed that quantitatively measure the biological activity relevant to the product's proposed mechanism of action, and these assays must be applied throughout product development and manufacturing. For biomaterials supporting cellular components, this may require novel assay systems that account for the material's influence on cell behavior.
Diagram: Cell Manufacturing Workflow for Tissue-Engineered Products. This process highlights critical stages where quality control ensures regulatory compliance.
Biomaterial Manufacturing and Characterization
Biomaterials manufacturing must adhere to Current Good Manufacturing Practices (CGMP) with rigorous quality control systems in place. For naturally derived materials such as decellularized tissues, this includes careful sourcing of raw materials, validation of decellularization efficiency, and monitoring of potential contaminants. Synthetic biomaterials require control over polymer synthesis, purification, and material properties. All biomaterials intended for clinical use must undergo comprehensive characterization of their physical, chemical, and biological properties.
Table 3: Essential Characterization Methods for Biomaterials
| Property Category | Test Methods | Regulatory Purpose |
|---|---|---|
| Physical Properties | Scanning electron microscopy, tensile testing, porosity measurement, swelling ratio | Demonstrate structural integrity and appropriate mechanical properties |
| Chemical Composition | FTIR, NMR, mass spectrometry, elemental analysis | Verify composition and identify potential contaminants |
| Biological Safety | ISO 10993 biocompatibility series (cytotoxicity, sensitization, implantation) | Ensure biological safety per international standards |
| Sterility | Sterility testing, bacterial endotoxin testing, bioburden monitoring | Prevent microbial contamination |
Research Reagent Solutions for Regulatory Studies
The following table outlines essential research reagents and their applications in generating robust data for regulatory submissions. These tools enable comprehensive characterization of biomaterials and their interactions with biological systems.
Table 4: Essential Research Reagent Solutions for Biomaterials Characterization
| Reagent Category | Specific Examples | Research Application | Regulatory Relevance |
|---|---|---|---|
| ECM Component Antibodies | Anti-collagen I, III, IV; anti-fibronectin; anti-laminin | Histological characterization of biomaterial composition and host tissue integration | Verification of material composition and degradation |
| Cell Surface Marker Antibodies | Anti-integrin subunits (β1, αv, α5); CD31 (endothelial cells); CD90 (mesenchymal cells) | Analysis of cell-biomaterial interactions and cellular phenotype | Demonstration of appropriate host response |
| Signaling Pathway Markers | Phospho-specific FAK (Tyr397), ERK1/2 (Thr202/Tyr204), Akt (Ser473) | Evaluation of intracellular signaling activation | Mechanistic evidence of bioactivity |
| Extracellular Matrix Hydrogels | Matrigel (basement membrane extract); collagen type I hydrogels; fibrin gels | 3D culture models for in vitro validation | Preclinical screening of biomaterial performance |
| Decellularization Reagents | SDS, Triton X-100, sodium deoxycholate, DNase I | Preparation of ECM scaffolds from native tissues | Standardization of manufacturing processes |
| Biocompatibility Assay Kits | MTT/XTT cell viability, LDH cytotoxicity, IL-1β/IL-6 ELISA | Assessment of material safety and inflammatory potential | Safety data required for all submissions |
Successfully navigating the regulatory pathway for biomaterials and tissue engineering products requires strategic planning from the earliest stages of development. The evolving regulatory landscape, particularly with programs such as RMAT designation, offers opportunities to accelerate development of promising therapies for serious conditions [102]. However, these expedited pathways still require robust scientific evidence of safety and efficacy, with particular attention to mechanistic studies, manufacturing quality, and appropriate preclinical models [3] [44].
For researchers in biomaterials and tissue engineering, integration of regulatory considerations into the fundamental research approach enhances both scientific rigor and translational potential. This includes designing studies that not only demonstrate therapeutic potential but also address specific regulatory requirements for product characterization, mechanism of action, and quality control. As the field advances with increasingly complex products such as vascularized engineered tissues and 3D-bioprinted constructs, ongoing dialogue between researchers and regulators through formal mechanisms such as the Q-Submission process will be essential to align innovation with regulatory standards [44]. Through this integrated approach, the field can continue to deliver transformative therapies while ensuring patient safety and product efficacy.
From Bench to Bedside: Clinical and Commercial Validation of Biomaterial Strategies
This technical analysis examines three prominent biomaterial-based products—Apligraf, Grafix, and decellularized extracellular matrix (ECM) scaffolds—within the framework of tissue engineering research. As the field shifts from synthetic material replacement to biologically active strategies that harness the body's innate regenerative capacity, these products exemplify the critical role of biomaterials as inductive niches. The analysis covers their design principles, mechanisms of action, clinical performance data, and underlying molecular pathways. Detailed experimental methodologies and key research reagents are provided to facilitate scientific replication and advancement. The evidence underscores that biomaterials which recapitulate native ECM composition, structure, and bioactivity are pivotal for directing cellular processes and achieving functional tissue restoration.
Biomaterials in tissue engineering have evolved from inert structural supports to dynamic, bioactive systems that actively orchestrate regeneration. This paradigm shift is centered on the extracellular matrix (ECM)—a sophisticated supramolecular assembly that provides structural support while concurrently delivering biomechanical and biochemical cues that direct cellular behavior [62] [3]. The ECM's composition of collagens, glycosaminoglycans (GAGs), proteoglycans, and glycoproteins forms a natural scaffold that regulates cell adhesion, migration, proliferation, and differentiation through integrin-mediated signaling and controlled release of growth factors [62].
Clinically approved products successful in regenerating tissues increasingly mimic key aspects of the native ECM. They can be broadly categorized as:
- Cellularized constructs containing living allogeneic cells that actively contribute to healing.
- Acellular scaffolds derived from human or animal tissues that provide an inductive template for host cell infiltration and tissue remodeling.
This review provides a technical analysis of two cellularized, FDA-approved products—Apligraf and Grafix—and the diverse class of decellularized ECM scaffolds, examining their design, efficacy, and role in advancing tissue engineering.
Product Analysis and Clinical Performance
Apligraf: A Bilayered Living Cell Construct
Apligraf is a bilayered, living skin substitute approved for treating venous leg ulcers (VLUs) and diabetic foot ulcers (DFUs). It is designed to closely mimic human skin [104].
- Design and Composition: The product features a dermal layer populated with living human allogeneic fibroblasts embedded in a bovine type I collagen matrix, and an epidermal layer formed by living human allogeneic keratinocytes [104] [105]. It metabolically active, supplying growth factors and cytokines to the wound bed.
- Mechanism of Action: Apligraf acts as a temporary biological dressing that provides the necessary cells, structural matrix, and signaling molecules to "reset" the hostile microenvironment of a chronic wound. It is known to modulate protease activity, suppress inflammation, and stimulate angiogenesis and re-epithelialization [105].
- Clinical and Economic Outcomes: Apligraf has the distinction of being backed by randomized controlled trials (RCTs) that led to its FDA approval for both VLUs and DFUs [104]. Table 1 summarizes key quantitative outcomes from clinical and real-world evidence.
Table 1: Clinical Performance Data for Apligraf and Grafix
| Product | Indication | Study Design | Primary Outcome (Complete Closure) | Key Comparative Results |
|---|---|---|---|---|
| Apligraf | Diabetic Foot Ulcers (DFUs) | Randomized Controlled Trial [104] | N/A | Significant improvement in wound closure vs. standard care [104]. |
| Apligraf | Venous Leg Ulcers (VLUs) | Randomized Controlled Trial [104] | N/A | Significant improvement in wound closure vs. standard care [104]. |
| Apligraf | DFUs & VLUs | Real-World Evidence [104] | N/A | Closes more wounds faster than standard care [104]. |
| Grafix | Diabetic Foot Ulcers | Randomized Controlled Trial [106] | 62% of patients | Vs. 21% in standard care group (p<0.0001); 191% relative improvement [106]. |
Grafix: A Human Placental Membrane Allograft
Grafix is a cryopreserved, cellular placental membrane allograft derived from human amniotic and chorionic tissues. It is regulated as a human cell and tissue product (HCT/P) [106].
- Design and Composition: Grafix retains the native ECM structure and bioactive components of the placental membrane, including endogenous growth factors (e.g., TGF-β, VEGF, FGF) and living cells such as mesenchymal stem cells (MSCs), fibroblasts, and epithelial cells [106].
- Mechanism of Action: As a fresh tissue allograft, its living cells are metabolically active upon implantation. The product delivers a potent mix of bioactive factors and progenitor cells that directly modulate the wound environment by reducing inflammation, promoting angiogenesis, and recruiting host stem and progenitor cells to the site of injury.
- Clinical Outcomes: Grafix demonstrated overwhelming efficacy in a landmark multicenter, randomized controlled trial for DFUs, meeting pre-specified stopping rules at an interim analysis. The data, shown in Table 1, revealed a significantly higher rate of complete wound closure compared to conventional treatment [106].
Decellularized ECM Scaffolds: Native Biomimetic Platforms
Decellularized ECM (dECM) scaffolds represent a broad class of acellular biomaterials derived from tissues like dermis, pericardium, small intestinal submucosa (SIS), and peripheral nerve [62] [107].
- Design and Composition: The core principle is the use of physical, chemical, and enzymatic treatments to remove immunogenic cellular material from a donor tissue while preserving the native ECM's structural and functional proteins, GAGs, and bound growth factors [62]. The resulting scaffold is tissue-specific in its biochemical composition and microarchitecture.
- Mechanism of Action: dECM scaffolds serve as a biomimetic, resorbable template that facilitates constructive remodeling. They guide host cell infiltration, promote stem cell recruitment and differentiation, and modulate the host immune response towards a pro-regenerative phenotype [62] [108]. Their mechanical properties and degradation profile provide mechanical support until new tissue forms.
- Clinical Applications and Products: A 2020 report identified 76 commercially available skin substitute products, a significant portion of which are acellular dECMs [107]. These are used clinically for skin, cardiovascular, rotator cuff, hernia, and peripheral nerve repairs [62]. Commercially available human-derived acellular dermal matrices include products like AlloPatch, DermACELL, and GraftJacket [107].
Experimental Protocols and Methodologies
Protocol for In Vivo Engineering of ECM Scaffolds with Microchannels
An innovative protocol for creating engineered ECM scaffolds with instructive parallel microchannels (ECM-C) demonstrates the advanced design of biomimetic materials [108].
- Template Fabrication: Fabricate a sacrificial template (membranous or tubular) composed of aligned polycaprolactone (PCL) microfibers (diameter ~142 μm) using established methods like electrospinning or melt-spinning.
- Subcutaneous Implantation: Surgically implant the PCL template into a subcutaneous pocket in a rodent model (e.g., rat). Allow it to remain implanted for a defined period (e.g., 4 weeks) for cellularization and tissue in-growth into the inter-fiber space.
- In Vivo Tissue Formation: During the implantation period, host cells (primarily α-SMA-positive fibroblasts) infiltrate the template and synthesize a collagen-rich, new ECM that occupies the space between the microfibers.
- Template Removal and Decellularization:
- Explant the cellularized composite structure.
- Remove the PCL sacrificial template by leaching with organic solvents (e.g., acetone, chloroform), confirmed by gel permeation chromatography.
- Decellularize the remaining native ECM scaffold using a combination of ionic detergents (e.g., SDS) and nucleases (DNase/RNase) to remove cellular DNA. Validate decellularization by DAPI staining and quantifying residual DNA content (<50 ng/mg dry weight).
The resulting ECM-C scaffold retains aligned collagen fibers and parallel microchannels, supporting guided cell migration and enhanced vascularization in vivo [108].
Protocol for Evaluating Scaffold-Cell Interactions In Vitro
To assess the bioactivity and guidance capacity of engineered scaffolds like ECM-C, the following in vitro cell culture assay can be employed [108].
- Scaffold Sterilization and Seeding: Sterilize the acellular scaffold (e.g., ECM-C vs. a control scaffold without microchannels). Seed relevant cell types (e.g., skeletal muscle L6 cells, Schwann RSC96 cells, vascular smooth muscle A10 cells) onto the scaffold surface at a defined density.
- Cell Culture and Fixation: Culture the cell-scaffold constructs under standard conditions for 1, 3, and 7 days.
- Analysis of Cell Behavior:
- Morphology and Alignment: At each time point, fix constructs and perform immunofluorescence staining (e.g., Phalloidin for F-actin, DAPI for nuclei). Use fluorescence microscopy to visualize and quantify cell alignment and nuclear elongation (circularity index) along the microchannels.
- Migration Tracking: Use live-cell imaging to track individual cell trajectories over time. Calculate metrics like Euclidean distance migrated and migration velocity.
- Proliferation Assay: Use a colorimetric assay (e.g., CCK-8) at 1, 3, and 7 days to measure metabolic activity as a proxy for cell proliferation, comparing test scaffolds to controls.
Molecular Mechanisms and Signaling Pathways
The therapeutic efficacy of these biomaterials is mediated through specific molecular interactions with host cells, primarily via integrin-mediated signaling and growth factor activation.
Diagram 1: Integrin-Mediated Signaling Pathway Activated by ECM Scaffolds. This diagram illustrates how ECM components engage integrin receptors, triggering downstream signaling cascades that regulate key cellular processes in tissue regeneration [3].
The signaling cascade begins when ECM ligands (e.g., collagen, fibronectin) from the scaffold bind to integrin receptors on the cell surface [3]. This binding induces conformational changes and clustering of integrins, leading to the assembly of focal adhesion complexes that recruit adapter proteins like talin, vinculin, and paxillin [3]. The formation of these complexes activates Focal Adhesion Kinase (FAK), which autophosphorylates at Tyr397 and recruits Src family kinases [3]. FAK/Src activation initiates three key downstream pathways:
- The MAPK/ERK pathway, which regulates gene expression driving cell proliferation and differentiation.
- The PI3K/Akt pathway, which promotes cell survival in the stressful wound microenvironment.
- Direct regulation of cytoskeletal reorganization, which is essential for cell migration and invasion into the scaffold [3].
This coordinated signaling, modulated by the mechanical properties and biochemical composition of the biomaterial, ensures a directed cellular response for functional tissue repair.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Reagents for ECM Scaffold Research and Development
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| Decellularization Agents | Remove cellular content from native tissues to create acellular ECM scaffolds [62]. | Ionic detergents (SDS), Non-ionic detergents (Triton X-100), Acids/Bases (Peracetic Acid), Enzymes (Trypsin, Nucleases) [62]. |
| Polymeric Template Materials | Serve as sacrificial scaffolds for in vivo or in vitro ECM deposition [108]. | Polycaprolactone (PCL), Polylactic Acid (PLA), Polyglycolic Acid (PGA). PCL microfibers used in engineered ECM-C scaffolds [108]. |
| Cell Culture Assays | Evaluate scaffold biocompatibility, bioactivity, and capacity to guide cell behavior [108]. | CCK-8 assay (proliferation), Live-cell tracking (migration), Phalloidin/DAPI staining (morphology/alignment) [108]. |
| Histological Stains | Characterize ECM composition and structure in native and engineered scaffolds. | Sirius Red (Collagen), Alcian Blue (GAGs), Verhoeff-Van Gieson (Elastin), H&E (general structure) [108]. |
| Analytical Tools for Characterization | Quantify scaffold properties and decellularization efficacy. | DNA quantification kits, Gel Permeation Chromatography (polymer removal), Micro-CT (3D porosity & structure), SEM/TEM (ultrastructure) [62] [108]. |
Apligraf, Grafix, and decellularized ECM scaffolds exemplify the transformative role of biomaterials in modern tissue engineering. They demonstrate that successful regeneration is not merely a matter of providing a physical substrate, but of delivering a sophisticated biological interface that actively communicates with the host. Through their tissue-specific ECM composition, structural cues, and presentation of bioactive signals, these products modulate the wound microenvironment, guide cellular processes through defined molecular pathways, and ultimately enable the restoration of functional tissue. Future advancements will hinge on further refining our ability to engineer biomaterials with spatiotemporal control over these cues, pushing the frontiers of regenerative medicine toward truly predictive and patient-specific healing.
The strategic selection of biomaterials is a cornerstone of tissue engineering, aiming to develop biological substitutes that restore, maintain, or improve tissue function [109]. Within this paradigm, scaffolds serve as the foundational three-dimensional templates that mimic the native extracellular matrix (ECM), providing critical structural support and biochemical cues for tissue development [110]. Two principal scaffolding strategies have emerged: the use of acellular scaffolds, which are implanted without cells to recruit the host's endogenous cells, and cell-seeded constructs, which are pre-populated with specific cell types in vitro prior to implantation [109]. The choice between these approaches significantly influences the regenerative pathway, immunological response, and ultimate clinical success. This analysis provides a comprehensive technical comparison of these strategies, examining their fundamental principles, key applications, and the experimental frameworks essential for their evaluation, thereby elucidating their distinct roles within the broader context of biomaterial research.
Fundamental Principles and Scaffold Characteristics
Core Definitions and Working Mechanisms
Acellular Scaffolds: These are biomaterial frameworks, often derived from decellularized tissues, that are implanted without any cellular components. Their primary mode of action is host-mediated regeneration. Once implanted, they act as instructive matrices that recruit endogenous stem cells and progenitor cells from the surrounding tissue [62] [3]. The efficacy of acellular scaffolds hinges on their preservation of the native ECM's biochemical and biomechanical cues—such as collagen, glycosaminoglycans (GAGs), and growth factors—which guide the infiltrating host cells to proliferate and differentiate, ultimately leading to tissue-specific regeneration and integration with the host architecture [62] [111].
Cell-Seeded Constructs: This approach involves the in vitro seeding and often cultivation of specific therapeutic cells (e.g., stem cells, chondrocytes) onto a scaffold before implantation [109]. The mechanism is delivery-based regeneration, where the construct delivers both a structural scaffold and a living cellular component directly to the defect site [112] [113]. These pre-seeded cells can immediately begin producing new ECM and interacting with the host environment, potentially accelerating the initial stages of healing. The scaffold's role is to provide a supportive microenvironment that maintains cell viability, promotes cell adhesion, and can direct specific cell differentiation pathways, even before implantation [113] [110].
Comparative Analysis of Scaffold Attributes
The choice between acellular and cell-seeded strategies involves balancing a complex set of parameters, from immunological risk to clinical practicality.
Table 1: Key Characteristics of Acellular vs. Cell-Seeded Constructs
| Characteristic | Acellular Scaffolds | Cell-Seeded Constructs |
|---|---|---|
| Mechanism of Action | Host-mediated cell recruitment and infiltration [62] [3] | Delivery of pre-seeded, functional cells [112] |
| Immunogenic Potential | Lower (if decellularization is effective) [62] | Higher (risk of immune rejection of donor cells) [109] |
| Regulatory Pathway | Generally simpler (Class III medical device) [62] | More complex (combination product) [112] |
| Manufacturing & Storage | Off-the-shelf availability; standard storage [62] | Requires cell culture facilities; limited shelf-life [112] [109] |
| Clinical Translation | Faster, more straightforward translation [62] | Logistically complex and costly [112] |
| Key Advantage | Avoids cell sourcing and expansion challenges [62] | Provides controlled, active cellular component [113] |
| Primary Limitation | Dependent on patient's own healing capacity [62] | Risk of cell death, dedifferentiation, or rejection [109] |
Experimental Methodologies for Evaluation
Rigorous evaluation is critical for comparing the efficacy of these two strategies. The following protocols outline standard methodologies for constructing and analyzing these scaffolds.
Protocol 1: Fabrication and In Vitro Evaluation of a Decellularized ECM (dECM) Scaffold
This protocol details the creation and initial testing of an acellular scaffold derived from native tissue.
A. Tissue Decellularization
- Source Tissue Acquisition: Obtain fresh allogeneic or xenogeneic tissue (e.g., porcine meniscus, ovine femoral patella).
- Physical Processing: Subject the tissue to multiple freeze-thaw cycles (e.g., -121°C for 20 minutes, then liquid nitrogen) to lyse cells [114].
- Chemical Treatment: Agitate the tissue fragments in a solution of 1% Triton X-100 for 8-16 hours to solubilize and remove cellular membranes and nuclear material [62] [114].
- Washing: Rinse extensively with distilled water for multiple cycles (e.g., 24 rounds) to eliminate all detergent residues, which could cause cytotoxicity [114].
B. Scaffold Quality Assessment
- DNA Quantification: Measure residual DNA content. Effective decellularization should result in less than 50 ng DNA per mg of tissue dry weight and the absence of visible nuclear material in DAPI-stained sections [62].
- ECM Composition Analysis: Use biochemical assays and immunohistochemistry to confirm the retention of essential ECM components such as collagens (Type I, II, IV), elastin, and GAGs [62] [113].
- Sterilization: Treat the scaffold with 0.1% peracetic acid (PAA), which also provides antimicrobial activity, or use gamma irradiation [62].
C. In Vitro Cell Seeding and Biocompatibility
- Cell Seeding: Seed human fibroblasts or mesenchymal stem cells (MSCs) onto the sterilized dECM scaffold at a density of 1x10^6 cells/scaffold. Incubate for 2 hours to allow for cell attachment [114].
- Viability and Proliferation: Culture the cell-scaffold construct and assess cell viability at days 1, 3, and 7 using a live/dead assay kit. Quantify metabolic activity with an AlamarBlue or MTT assay [113].
- Cell Morphology and Infiltration: Fix the construct at day 7, process for scanning electron microscopy (SEM), and stain with phalloidin (for actin) to visualize cell adhesion, spreading, and migration into the scaffold pores [113].
Protocol 2: Development and Functional Testing of a Cell-Seeded Construct
This protocol describes the process of creating a construct with a specific cell source and evaluating its functional properties.
A. Cell Source Selection and Expansion
- Cell Isolation: Choose a relevant cell source. For meniscus repair, isolate articular chondrocytes from joint cartilage or adipose-derived stem cells (ADSCs) from lipoaspirate using collagenase digestion [113].
- Cell Culture: Expand cells in standard culture flasks using appropriate medium (e.g., DMEM-low glucose for USCs) supplemented with fetal bovine serum and antibiotics until sufficient cell numbers are achieved [114].
B. Dynamic Cell Seeding on a Synthetic Scaffold
- Scaffold Preparation: Use a synthetic, biocompatible scaffold such as an electrospun Poly (lactide-co-caprolactone) (PLLA-CL) nanofiber yarn mesh [113].
- Seeding with Biological Glue: To enhance attachment, pre-coat the scaffold with a biological glue like fibronectin or fibrin by dipping or perfusing the scaffold with the protein solution [112].
- Rotational Seeding: Pipette a concentrated cell suspension (e.g., 5 million cells/mL) into the lumen of a tubular scaffold or onto its surface. Place the scaffold in a rotational bioreactor system, rotating at low speed (e.g., 10-20 rpm) for 12-24 hours. This method increases seeding efficiency and uniformity compared to static seeding [112].
C. In Vitro Functional Maturation
- Construct Culture: Maintain the cell-scaffold construct in a differentiation medium (e.g., chondrogenic medium for chondrocytes) for up to 21 days in a bioreactor that provides mechanical stimulation if appropriate.
- Gene Expression Analysis: After the culture period, extract total RNA from the construct. Perform quantitative real-time PCR (qRT-PCR) to measure the expression of tissue-specific genes (e.g., for cartilage: SOX9, COL2A1, ACAN; for bone: Runx2, ALP, COL1A1) [113] [114].
- Biomechanical Testing: Assess the functional maturity of the engineered tissue by determining the tensile and compressive mechanical properties using a uniaxial testing system. Compare the values to those of native tissue [113].
The following workflow diagram synthesizes the experimental pathways for developing and evaluating both types of constructs, from initial material processing to final analysis.
Analytical Tools and Key Data Interpretation
A side-by-side comparison of quantitative outcomes is essential for evaluating the performance of acellular and cell-seeded strategies in specific tissue engineering contexts.
Table 2: Representative Experimental Data from Key Studies
| Evaluation Parameter | Acellular Scaffold (Meniscus dECM) | Cell-Seeded Construct (Chondrocytes on Nanofiber Yarn) | Cell-Seeded Construct (ADSCs on Nanofiber Yarn) |
|---|---|---|---|
| Primary Cell Type | Host-derived fibroblasts & progenitors [62] | Articular chondrocytes [113] | Adipose-derived stem cells [113] |
| Seeding Efficiency | Not Applicable (N/A) | >90% (with dynamic seeding) [112] | >90% (with dynamic seeding) [112] |
| Chondrogenic Matrix (GAG) Production | Moderate (host-dependent) [62] | High (mature cartilage-like tissue) [113] | Low (fibroblastic differentiation) [113] |
| Collagen Deposition | Type I/III (remodeling phase) [3] | Moderate, Type II dominant [113] | High, Type I dominant [113] |
| Tensile Strength | Matches native tissue post-remodeling [62] | Lower | Higher [113] |
| Key Molecular Markers | MMPs, TGF-β [3] | SOX9, COL2A1 [113] | RUNX2, COL1A1 [113] [114] |
Data Interpretation:
- The data underscores a fundamental trade-off: chondrocytes on scaffolds excel at forming chondrogenic (cartilage-like) tissues, making them ideal for repairing the inner, avascular region of the meniscus [113]. In contrast, ADSCs, even without specific growth factor induction, predominantly undergo a fibroblastic differentiation, producing abundant collagen I and resulting in constructs with superior tensile strength, which may be beneficial for the outer, fibrous region of the meniscus [113].
- This highlights that the "optimal" strategy is highly application-dependent. The acellular scaffold's performance is highly dependent on the host's innate ability to recruit the appropriate mix of cells to regenerate both tissue phenotypes [62] [113].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the described protocols requires a suite of specialized reagents and materials.
Table 3: Essential Reagents and Materials for Scaffold Research
| Item | Function/Application | Specific Examples |
|---|---|---|
| Decellularization Agents | Removal of cellular material to create acellular scaffolds. | Triton X-100, Sodium Dodecyl Sulfate (SDS), Peracetic Acid (PAA) [62] [114] |
| Natural Polymer Scaffolds | Provide biocompatible and bioactive substrates. | Decellularized ECM (dECM), Collagen, Fibrin, Hyaluronic Acid [109] [3] |
| Synthetic Polymer Scaffolds | Offer tunable mechanical properties and degradation rates. | Poly(lactide-co-caprolactone) (PLLA-CL), Poly(ε-caprolactone) (PCL), Polylactic Acid (PLA) [113] [110] |
| Biological Glues / Coatings | Enhance cell attachment and survival on scaffolds. | Fibronectin, Fibrin, Laminin, Platelet-Rich Fibrin (PRF) [112] [114] |
| Cell Sources | Provide the living component for cell-seeded constructs. | Articular Chondrocytes, Bone Marrow MSCs (BMSCs), Adipose-derived Stem Cells (ADSCs), Umbilical Cord Stem Cells (USCs) [113] [114] |
| Bioreactors | Enable dynamic cell seeding and provide mechanical stimulation during culture. | Rotational Bioreactors, Vacuum Seeding Devices [112] |
The comparative analysis between acellular scaffolds and cell-seeded constructs reveals that neither strategy is universally superior; rather, they serve complementary roles within the tissue engineering arsenal. Acellular scaffolds offer a streamlined, off-the-shelf solution with a lower regulatory burden, making them ideal for applications where the host tissue possesses a robust innate healing capacity and the primary need is a conductive and instructive matrix [62] [111]. In contrast, cell-seeded constructs represent a more complex but powerful approach for regenerating tissues with limited self-repair capability or for orchestrating specific, multi-lineage regenerative programs from the outset [113] [109]. The future of the field lies in smart, integrated strategies that may combine the initial use of acellular scaffolds with subsequent cell therapies, or the development of "primed" acellular scaffolds that are biofunctionalized with specific cytokines to direct host cell fate. As biomaterial science advances, the distinction may blur, leading to a new generation of intelligent constructs that dynamically interact with the host environment to achieve optimal tissue regeneration.
The development of advanced biomaterials for tissue engineering represents a frontier in regenerative medicine, aiming to overcome the limitations of native tissue repair. Within this context, in vivo models are indispensable for bridging the gap between in vitro innovation and clinical application. These models provide the complex physiological environment necessary to evaluate how biomaterial scaffolds influence biological processes such as cell integration, vascularization, and immune response [3]. The selection of an appropriate animal model is therefore a critical strategic decision, directly impacting the reliability and translational potential of data on biomaterial safety, biocompatibility, and functional efficacy [115]. This guide details the key metrics and methodologies for evaluating biomaterials in preclinical models of bone and soft tissue regeneration, providing a framework for researchers to generate robust, actionable data.
In Vivo Models for Soft Tissue Regeneration
Tendon tissue, with its low cellularity and vascularity, presents a significant regenerative challenge. The native healing process often results in biomechanically inferior scar tissue rather than functional regeneration, creating a compelling case for biomaterial interventions [115].
Animal Model Selection for Tendon Research
Selecting the right animal model is contingent upon the research hypothesis, desired outcomes, and translational goals. The following table summarizes the common models used in tendon research.
Table 1: Animal Models for Tendon Regeneration Research
| Model Category | Examples | Advantages | Disadvantages & Considerations |
|---|---|---|---|
| Small Animal Models | Mice, Rats | - Cost-effective & easier handling [115]- High-throughput experimentation [115]- Availability of transgenic lines for genetic studies [115] | - Small size limits clinically relevant surgical repair [115]- Lack genetic variability of human populations [115] |
| Intermediate Models | Rabbits | - Tendon size/structure closer to humans [115]- Better for surgical intervention studies [115] | - Higher maintenance costs than rodents [115]- More vulnerable to injury [115] |
| Large Animal Models | Horses, Sheep, Goats, Dogs | - Close anatomical/functional match to human tendons [115]- Essential for preclinical studies of surgical techniques/devices [115] | - High costs and ethical considerations [115]- Quadrupedal locomotion creates biomechanical differences [115] |
Key Metrics for Evaluating Tendon Regeneration
The efficacy of a biomaterial for tendon repair is assessed through a combination of histological, biomechanical, and functional outcomes.
Table 2: Key Outcome Metrics for Tendon Regeneration
| Metric Category | Specific Outcome Measures | Technical Methodologies |
|---|---|---|
| Histological & Morphological | - Collagen fiber organization and alignment [115]- Transition from Type III to Type I collagen [115]- Cellularity and vascularity [115]- Assessment of scar tissue formation [115] | - Histological staining (e.g., H&E, Masson's Trichrome, Picrosirius Red) [115]- Polarized light microscopy for collagen birefringence [115]- Immunohistochemistry for collagen types [115] |
| Biomechanical | - Ultimate tensile strength [115]- Load-to-failure [115] |
- Uniaxial tensile testing [115] |
| Functional Recovery | - Gait analysis [115]- Joint mobility and range of motion [115]- Return to normal weight-bearing [115] | - Video-based motion capture systems [115]- Force plate analysis [115] |
Experimental Protocol: Rodent Achilles Tendon Repair
Objective: To evaluate the in vivo efficacy of a novel 3D-bioprinted biomaterial scaffold for Achilles tendon repair in a rat model. Biomaterial Implant: AI-optimized PCL/PEG scaffold, sterilized via ethylene oxide [115]. Surgical Procedure:
- Anesthesia & Preparation: Anesthetize adult Sprague-Dawley rats (n=10/group) using an approved regimen (e.g., ketamine/xylazine). Shave and antiseptically prepare the hindlimb.
- Tendon Exposure & Transection: Make a longitudinal skin incision posterior to the ankle. Bluntly dissect to expose the Achilles tendon. Create a full-thickness, transverse defect (e.g., 3mm gap).
- Scaffold Implantation: Suture the experimental biomaterial scaffold into the defect using a non-absorbable suture (e.g., 6-0 Prolene) in a modified Kessler pattern. The control group receives a sham surgery with suture repair only.
- Closure: Close the surgical site in layers. Post-Operative Care: Administer analgesia for 72 hours. Allow unrestricted cage activity. Monitor for signs of infection or distress. Endpoint Analysis: At 4, 8, and 12 weeks post-op, harvest tendons for histological (n=5/group) and biomechanical (n=5/group) analysis as detailed in Table 2.
In Vivo Models for Bone Regeneration
Bone possesses a remarkable innate capacity for regeneration. However, critical-sized defects, resulting from trauma, tumor resection, or disease, require biomaterial-based strategies to heal [116]. These "smart bone implants" are designed to provide osteoconduction, osteoinduction, and potentially deliver biological cues for neurogenic bone repair [116].
Animal Models and Key Metrics in Bone Research
The principles of animal model selection for bone research parallel those for tendon, with size, cost, and anatomical similarity being key drivers. Large animal models like sheep are often used for final preclinical testing due to their similar bone size and weight-bearing mechanics [115]. The key metrics, however, are specific to bone biology.
Table 3: Key Outcome Metrics for Bone Regeneration
| Metric Category | Specific Outcome Measures | Technical Methodologies |
|---|---|---|
| Radiological & Imaging | - Bone mineral density (BMD)- New bone volume (BV/TV)- Trabecular number and thickness- Rate of defect bridging | - Micro-Computed Tomography (μCT)- Longitudinal X-ray radiography- Dynamic histomorphometry via fluorochrome labels |
| Histological | - Osteointegration (implant-bone contact)- Osteoconduction (bone growth into scaffold)- Presence of osteoblasts/osteoclasts- Evidence of inflammatory response | - Undecalcified histology (e.g., methylmethacrylate embedding)- Staining (e.g., Toluidine Blue, Van Gieson)- TRAP staining for osteoclasts |
| Biomechanical | - Compressive/torsional strength |
- Mechanical testing machines for compression/torsion- Push-out test jigs- Finite element analysis (FEA) correlated with μCT data |
The Biomaterial-Tissue Interface: Key Signaling Pathways
The success of a biomaterial is dictated by its interaction with the host tissue at the cellular and molecular level. Biomaterials engineered to recapitulate aspects of the native extracellular matrix (ECM) can actively orchestrate repair by engaging specific signaling pathways [3].
Integrin-Mediated Signaling for Cell Survival and Proliferation
ECM-inspired biomaterials promote cell adhesion through integrin binding, initiating critical signaling cascades that direct cell fate during regeneration [3].
ECM Remodeling in Wound Healing
Successful regeneration requires not only new tissue formation but also the coordinated remodeling of the wound matrix into mature, functional tissue. Biomaterials can be designed to modulate this process [3].
The Scientist's Toolkit: Essential Research Reagents
The following table details key materials and reagents critical for conducting in vivo evaluations of biomaterials for tissue regeneration.
Table 4: Essential Research Reagents for In Vivo Regeneration Studies
| Reagent / Material | Function & Application | Key Characteristics |
|---|---|---|
| ECM-Based Hydrogels (e.g., Collagen, Hyaluronic Acid) | Provide a biomimetic, naturally derived scaffold for 3D cell culture and in vivo implantation; support cell adhesion and infiltration [3]. | Biocompatible, bioactive, and often enzymatically degradable; can be derived from allogeneic or xenogeneic sources. |
| Synthetic Polymers (e.g., PLGA, PCL, PEG) | Serve as versatile, tunable scaffolds for tissue engineering; allow control over degradation rate, mechanics, and architecture [3]. | Reproducible and scalable; mechanical properties can be tailored; lack innate bioactivity unless functionalized. |
| Bioceramics (e.g., Hydroxyapatite, β-Tricalcium Phosphate) | Used primarily for bone regeneration; provide osteoconductivity and closely match the mineral composition of native bone [3]. | Excellent biocompatibility and compression strength; brittle; degradation rates vary. |
| RGD Peptide | A critical bioactive motif used to functionalize biomaterials; promotes cell adhesion by binding to integrin receptors on the cell surface [3]. | Enhances the bioactivity of otherwise inert synthetic polymers; directly engages integrin-mediated signaling pathways. |
| Matrix Metalloproteinase (MMP) Substrates | Peptide sequences crosslinked into biomaterials that are cleaved by specific MMPs; create enzyme-responsive scaffolds that degrade in sync with tissue remodeling [3]. | Allows for cell-driven, localized degradation of the biomaterial, facilitating new tissue ingrowth. |
Biomaterials are substances that have been engineered to take a form which, alone or as part of a complex system, is used to direct, by control of interactions with components of living systems, the course of any therapeutic or diagnostic procedure [117]. Within tissue engineering, a field dedicated to creating biological substitutes to restore or enhance tissue and organ function, biomaterials provide the essential structural and biochemical scaffold that supports cell growth and tissue formation [118]. The integration of biomaterials with stem cells and bioactive molecules represents a cornerstone of regenerative medicine, offering solutions to the critical global shortage of donor organs and the limitations of conventional treatments for damaged tissues [119] [118]. This whitepaper examines the global market dynamics and growth projections of this field, framing them within the essential role biomaterials play in advancing tissue engineering research and clinical applications. The analysis is intended to provide researchers, scientists, and drug development professionals with a detailed technical and commercial perspective on this rapidly evolving sector.
The tissue engineering and biomaterials markets are experiencing robust growth, driven by an increasing demand for regenerative medicine, rising prevalence of chronic diseases, and significant technological advancements [119] [120]. The convergence of these factors is creating a vibrant commercial and research landscape.
Tissue Engineering Market Size and Growth
The global tissue engineering market is characterized by strong expansion, though reported figures vary between sources due to differing segment definitions and methodologies. The market is propelled by the growing burden of chronic diseases and traumatic injuries, which in turn drives the demand for regenerative solutions [121] [122].
Table 1: Global Tissue Engineering Market Projections
| Source | Market Size (Base Year) | Projected Market Size | Forecast Period | CAGR |
|---|---|---|---|---|
| BCC Research [119] [118] | $5.4 billion (2025) | $9.8 billion (2030) | 2025-2030 | 12.8% |
| Towards Healthcare [122] | $22.29 billion (2025) | $74.53 billion (2034) | 2025-2034 | 14.35% |
| Intel Market Research [121] | $34.56 billion (2024) | $120.57 billion (2032) | 2024-2032 | 20.0% |
Biomaterials Market Size and Growth
The broader biomaterials market, which supplies the foundational materials for tissue engineering, is also on a significant growth trajectory. This growth is fueled by advancements in material science and expanding applications across healthcare [120] [52].
Table 2: Global Biomaterials Market Projections
| Source | Market Size (Base Year) | Projected Market Size | Forecast Period | CAGR |
|---|---|---|---|---|
| Precedence Research [52] | $192.43 billion (2025) | $523.75 billion (2034) | 2025-2034 | 11.82% |
| Coherent Market Insights [120] | $208.23 billion (2025) | $577.93 billion (2032) | 2025-2032 | 15.8% |
Key Market Dynamics
Primary Growth Drivers
- Rising Demand for Regenerative Medicine: The increasing need for regenerative medicine is driven by an aging global population, rising cases of chronic diseases, and a critical shortage of donor organs. Tissue engineering provides promising alternatives, thereby fueling demand for advanced biomaterial solutions [119] [122].
- Technological Advancements: The field is rapidly evolving with innovations in 3D bioprinting, smart biomaterials, organ-on-a-chip models, and the integration of artificial intelligence (AI). AI, in particular, is accelerating biomaterial discovery, optimizing scaffold architecture, and enabling predictive modeling of tissue behavior, which significantly reduces R&D cycles and costs [119] [118] [52].
- Increased Funding and Research Activity: Venture capital investment is providing crucial support for startups and biotech firms, enabling research, product development, and commercialization [119]. Furthermore, expanding research activities are leading to more regulatory approvals and a faster translation of laboratory discoveries into clinical applications [119] [118].
Major Challenges and Restraints
- High Treatment Costs and Complex Regulatory Pathways: The high cost associated with tissue-engineered products can limit patient access and market penetration. Additionally, the market is subject to strict regulatory oversight and complex approval pathways, which can be time-consuming and costly, potentially delaying product commercialization [119] [118] [52].
- Technical Challenges in Scaffold Fabrication: Creating scaffolds with the ideal parameters to mimic a native tissue microenvironment remains technically demanding. Key challenges include controlling the internal pore structure, porosity, and pore connectivity, while also ensuring the process is economically viable for clinical translation. Residual organic solvents from scaffold fabrication can also cause cell harm [122].
Emerging Opportunities
- Expansion into Emerging Economies: Countries in the Asia-Pacific region, such as China and India, present significant growth potential due to their expanding healthcare infrastructure, supportive government policies, and rising healthcare awareness [118] [120].
- Development of "Smart" Biomaterials: The advent of smart polymers and hydrogels that can respond to environmental stimuli (e.g., pH, temperature) offers new possibilities for creating dynamic, four-dimensional (4D) tissue constructs. These materials could provide solutions to current limitations in scaffold technology [122].
Market Segmentation and Regional Analysis
Segmentation by Product, Material, and Application
The tissue engineering market can be segmented in several ways, each highlighting the central role of biomaterials.
Table 3: Key Market Segments and Dominant Categories
| Segmentation Axis | Dominant Segment | Key Insights |
|---|---|---|
| Product | Scaffolds [119] [122] | Scaffolds provide the critical structural support for cell adhesion and subsequent tissue formation. They are often composed of polymeric biomaterials. |
| Material | Synthetic Materials [122] | Synthetic biodegradable polymers (e.g., polyesters, polyurethane) are widely used due to their immune system safety, controllable structure, and flexible processing. |
| Application | Orthopedic & Musculoskeletal Disorders [119] [120] [122] | This segment is the largest, driven by the high prevalence of bone and joint disorders. The focus is on 3D scaffolds that offer structural support for new bone formation. |
Geographical Landscape
The market exhibits distinct regional patterns, with North America currently leading but the Asia-Pacific region emerging as the fastest-growing market.
- North America: This region is the largest market for both tissue engineering and biomaterials, a position attributed to its well-established medical device industry, significant R&D infrastructure, high healthcare expenditures, and favorable government policies [119] [120] [52]. The United States is the primary contributor within this region.
- Asia-Pacific: This region is expected to be the fastest-growing, driven by improving healthcare facilities, a large patient population, rising rates of chronic diseases, and increasing government support for healthcare innovations and local manufacturing [120] [122]. Japan is noted as a pioneer in technology development within the region [122].
- Europe: The European market shows steady growth, characterized by a focus on quality healthcare, an aging population, and innovations in nanostructured and bio-inspired materials. Growth is supported by strong industry-research linkages and R&D funding [120] [122].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and reagents used in contemporary tissue engineering research, with a specific emphasis on biomaterials and their functions.
Table 4: Essential Research Reagents and Biomaterials in Tissue Engineering
| Reagent/Material | Function in Research | Technical Notes & Alternatives |
|---|---|---|
| Scaffolds | Provides a 3D structural support for cell adhesion, proliferation, and tissue in-growth. Directs tissue formation. | Can be biological (e.g., collagen) or synthetic (e.g., PCL, PLGA). A key goal is to mimic the native extracellular matrix (ECM) [122]. |
| Hydrogels | Water-swollen polymer networks used as scaffolds, especially for soft tissue engineering and organoid culture. Can be tuned for mechanical properties. | Used as a promising Matrigel alternative. Can be synthetic or derived from natural polymers (e.g., alginate, PEG) to avoid immunogenicity [38]. |
| Matrigel | Tumor-derived ECM commonly used for organoid culture. Provides a complex mixture of proteins and growth factors. | Presents challenges for clinical translation due to its xenogeneic nature, variable composition, and potential immunogenicity [38]. |
| Growth Factors & Cytokines | Bioactive molecules (e.g., BMPs, VEGF, TGF-β) that guide cell differentiation, proliferation, and tissue-specific maturation. | Often integrated into scaffolds for controlled release. Critical for establishing complex organoid structures and functions. |
| Synthetic Biodegradable Polymers | (e.g., PCL, PLGA, PGS) Used to fabricate scaffolds with controlled degradation rates, mechanical properties, and minimal immune response. | Aliphatic polyesters are most common. They offer a more controlled structure and processing flexibility compared to natural materials [122]. |
| Cell Sources | (e.g., Stem cells, primary cells) The living component that proliferates and differentiates to form new tissue within the scaffold. | Mesenchymal stem cells (MSCs) are widely used. The choice depends on the target tissue and application (research vs. clinical). |
Experimental Protocol: Developing Biomaterial-Based Liver Organoids
This protocol provides a detailed methodology for creating liver organoids using defined biomaterial-based hydrogels, addressing the limitations of conventional Matrigel [38].
Background and Principle
Liver organoids are three-dimensional, in vitro models that mimic key functional characteristics of the liver, making them valuable for disease modeling, drug screening, and regenerative medicine. Traditional culture methods rely on Matrigel, a tumor-derived extracellular matrix, which poses challenges for clinical translation due to its xenogeneic nature and batch-to-batch variability. This protocol outlines a method to support liver organoid growth, expansion, and differentiation using a chemically defined, synthetic hydrogel, thereby enhancing reproducibility and potential for therapeutic application [38].
Materials and Reagents
- Human Liver Progenitor Cells (e.g., primary hepatoblasts or iPSC-derived hepatic progenitors).
- Synthetic Hydrogel Precursor Solution: (e.g., Poly(ethylene glycol) (PEG)-based macromers with protease-sensitive crosslinking peptides and adhesion ligands like RGD).
- Hepatocyte Culture Medium: Advanced DMEM/F12 supplemented with:
- Growth Factors: HGF (10-50 ng/mL), EGF (50-100 ng/mL), FGF (10-50 ng/mL).
- Other Supplements: B-27 (1X), N-2 (1X), Nicotinamide (10 mM), L-glutamine (1X).
- Antibiotics: Penicillin-Streptomycin (1%).
- Differentiation Medium: Hepatocyte Culture Medium without EGF/FGF, supplemented with Oncostatin M (20-50 ng/mL) and Dexamethasone (0.1-1 µM).
- Sterile Phosphate Buffered Saline (PBS).
- Cell Dissociation Enzyme: (e.g., TrypLE Express or Accutase).
- Tissue Culture Plates (24-well or 48-well).
Step-by-Step Procedure
Hydrogel Preparation and Seeding: a. Prepare the hydrogel precursor solution according to the manufacturer's instructions. This typically involves dissolving the macromers in a sterile buffer. b. Mix the cell suspension (1-5 x 10⁴ cells per hydrogel) with the precursor solution on ice to ensure even distribution. The final hydrogel composition should be tailored to mimic liver stiffness (typically in the 1-5 kPa range). c. Pipet the cell-polymer mixture into the wells of a pre-warmed tissue culture plate. d. Incubate the plate at 37°C for 15-30 minutes to induce gelation and form the 3D cell-hydrogel construct.
Culture and Expansion: a. After gelation, carefully overlay each hydrogel with pre-warmed Hepatocyte Culture Medium. b. Culture the constructs in a humidified incubator at 37°C with 5% CO₂. c. Replace the culture medium every 2-3 days. Observe under a microscope for the formation of spherical, cystic organoid structures within the hydrogel, which typically begins within 3-7 days.
Organoid Differentiation and Maturation: a. Once organoids reach a desired size (typically after 7-10 days of expansion), carefully aspirate the expansion medium. b. Replace it with Differentiation Medium to promote hepatic maturation. c. Continue culture for an additional 10-14 days, changing the differentiation medium every 2-3 days.
Harvesting and Analysis: a. To harvest organoids for analysis, carefully aspirate the medium and wash the hydrogel with PBS. b. Add a cell dissociation enzyme or a hydrogel-specific degrading solution (e.g., a protease for peptide-crosslinked gels) to dissolve the matrix and release the organoids. c. Collect the organoids by centrifugation and proceed with downstream applications.
Downstream Applications and Functional Assessment
- Histological and Immunofluorescence Analysis: Fix, embed, and section organoids for staining with liver-specific markers (e.g., Albumin, HNF4α, CYP450 enzymes).
- Functional Assays:
- Albumin/Urea Secretion: Quantify secretion levels into the culture medium using ELISA or colorimetric kits.
- CYP450 Activity: Measure metabolism of specific substrates (e.g., Luciferin-IPA for CYP3A4).
- Glycogen Storage: Assess using Periodic acid-Schiff (PAS) staining.
- Gene Expression Analysis: Extract RNA from organoids and perform qRT-PCR to evaluate the expression of hepatic genes.
- Drug Toxicity Screening: Expose mature organoids to drug candidates and measure cell viability (e.g., with ATP-based assays) and functional impairment.
Technological Advancements and Future Outlook
The future of tissue engineering is intrinsically linked to innovations in biomaterials science. Several key technologies are poised to drive the next wave of growth and clinical application.
- 3D Bioprinting: This technology allows for the precise spatial deposition of cells, biomaterials, and growth factors (bioinks) to create complex, patient-specific tissue constructs. The flexibility and precision of 3D printing are making it a leading technology in the biomaterials market, enabling the creation of intricate scaffolds that were previously impossible to fabricate [118] [120].
- Artificial Intelligence (AI) and Machine Learning: AI is revolutionizing biomaterial discovery and design. It accelerates R&D by predicting material properties, optimizing scaffold architecture for specific tissues, and modeling tissue behavior. Explainable AI (XAI) is also increasing confidence in these predictive models among researchers and clinicians [119] [52].
- Advanced "Smart" Biomaterials: The next generation of biomaterials includes programmable hydrogels and nanocomposites that can dynamically respond to physiological stimuli (e.g., pH, mechanical stress). These 4D materials, which change over time, are critical for creating more authentic tissue models and implants that better integrate with the host [120] [122]. The development of biomaterials that simultaneously possess shape memory and self-healing properties is an area of active research [122].
The convergence of these technologies with a deeper understanding of biology is set to further solidify the central role of biomaterials in bridging the gap between laboratory research and clinical translation in tissue engineering.
Within the field of tissue engineering, biomaterials serve as the foundational scaffold that guides the regeneration of damaged tissues and organs. These materials, whether derived from nature or synthesized in a lab, are designed to interface with biological systems to direct healing processes by mimicking the native extracellular matrix (ECM)—the dynamic network of proteins and glycosaminoglycans that orchestrates cellular behavior through biomechanical and biochemical cues [3] [83]. The choice between synthetic and natural biomaterials carries profound implications for clinical outcomes, influencing everything from initial biocompatibility and immune response to the long-term functional integration of the engineered tissue [123] [124]. This whitepaper provides a structured, technical comparison of these material classes, equipping researchers and drug development professionals with the data and methodologies needed to inform their therapeutic strategies.
Table 1: Core Characteristics of Biomaterial Classes
| Feature | Natural Biomaterials | Synthetic Biomaterials |
|---|---|---|
| General Definition | Substances derived from biological sources (animals, plants, microorganisms) [125]. | Artificially produced polymers created in laboratories, often from petroleum-derived monomers [125]. |
| Key Examples | Collagen, chitosan, alginate, hyaluronic acid, gelatin, fibrin [126] [125] [124]. | Polylactic acid (PLA), Polyglycolic acid (PGA), Polycaprolactone (PCL), Polyethylene glycol (PEG) [123] [127]. |
| Inherent Bioactivity | High; contain innate cell-adhesion motifs (e.g., RGD sequences) and interact with cells via integrin signaling [3] [124]. | Typically inert; bioactivity must be engineered through surface modification or biofunctionalization [3] [83]. |
| Immune Response | Generally low chronic immunogenicity, but risk of adverse reactions exists and varies by source and purity [123] [124]. | Can be designed to minimize immune recognition, but may provoke foreign body reactions [123]. |
| Primary Clinical Strengths | Excellent biocompatibility, biomimicry, and inherent biodegradability [124]. | Tunable mechanical properties, predictable degradation kinetics, and high batch-to-batch consistency [123] [125]. |
| Primary Clinical Limitations | Poor mechanical strength, unpredictable degradation rates, and potential risk of immunogenicity [124]. | Lack of inherent bioactivity, potential for chronic inflammation, and biocompatibility challenges [123]. |
Material Properties and Direct Clinical Implications
The fundamental properties of a biomaterial directly dictate its performance in a clinical setting, influencing the success of tissue integration, repair, and long-term function.
Biological Recognition and Signaling
Natural biomaterials, such as collagen and fibronectin, are intrinsically recognized by cells because they present native binding sites for integrin receptors [3] [83]. This engagement initiates crucial downstream signaling pathways—including FAK, MAPK/ERK, and PI3K/Akt—that collectively regulate cell adhesion, migration, proliferation, and survival, thereby accelerating the healing process [3] [83]. In contrast, synthetic polymers like PEG and PLA are biologically inert. To make them interactive, they must be functionalized with bioactive peptides (e.g., RGD) or other ECM-derived motifs to elicit desired cellular responses [3].
Figure 1: Integrin-Mediated Signaling Pathway. Natural ECM components binding to integrin receptors trigger key pathways (FAK, MAPK/ERK, PI3K/Akt) that regulate essential cellular processes for tissue repair [3] [83].
Mechanical and Structural Properties
Synthetic biomaterials excel in their tunable mechanical properties. Researchers can precisely engineer polymers like PCL and PLA to match the stiffness and strength of the target tissue, which is critical for load-bearing applications such as bone regeneration [123] [127]. Furthermore, their degradation profiles can be controlled through polymer chemistry to last from weeks to years [123]. Natural biomaterials, however, often suffer from poor mechanical strength and relatively uncontrollable decomposition, which can limit their use in applications requiring significant structural support [124]. Their mechanical properties are inherently linked to their biological source and processing method.
Immunogenicity and Safety Profiles
While natural polymers are generally biocompatible and resemble the human ECM, they can carry a risk of eliciting immune responses, particularly if residual cellular components remain from their animal or human sources [123] [124]. Rigorous decellularization and purification protocols are essential to mitigate this risk. Synthetic biomaterials, being free from biological contaminants, offer an advantage in this regard. However, their degradation byproducts can sometimes cause local acidosis or inflammatory reactions, as seen with some polyesters [123]. The global biomaterials market, valued in the billions, reflects the high demand for materials that successfully balance efficacy with safety [123].
Table 2: Quantitative Comparison of Key Biomaterial Properties
| Property | Natural Biomaterials (e.g., Collagen) | Synthetic Biomaterials (e.g., PCL, PLA) |
|---|---|---|
| Tensile Strength | Low to Moderate (highly variable) [124] | High and Tunable [123] |
| Degradation Rate | Weeks to Months (enzyme-dependent, less predictable) [124] | Months to Years (highly controllable via chemistry) [123] |
| Elastic Modulus | Can be engineered to range from soft (e.g., ~0.1-1 kPa for brain-mimetic hydrogels) to stiff [3] | Highly tunable across a wide range, including stiff materials for bone (e.g., GPa range for certain composites) [3] [123] |
| Batch-to-Batch Consistency | Low (varies with source and isolation process) [124] | High (precisely controlled synthesis) [123] [125] |
| Market Impact (Material Type Leader) | N/A | Polycaprolactone (PCL) segment led the synthetic tissue engineering market in 2024 [127] |
Experimental Protocols for In Vitro Evaluation
Robust preclinical evaluation is critical for predicting clinical performance. The following protocols outline standard methodologies for assessing biomaterial-cell interactions.
Protocol: Evaluation of Cell Adhesion and Viability on 2D Scaffolds
This protocol assesses the initial cytocompatibility of a biomaterial film or surface.
Material Preparation and Sterilization:
- For synthetic polymers (e.g., PLLA), dissolve in an appropriate organic solvent (e.g., chloroform) and cast into a sterile culture plate to form a thin film. Sterilize under UV light for 1 hour per side [123].
- For natural polymers (e.g., collagen), coat the culture plate with a sterile solution and allow it to gel. Crosslink if necessary. Sterilize under UV light for 30 minutes [124].
Cell Seeding:
- Trypsinize and count relevant cells (e.g., human dermal fibroblasts, HDFs). Seed cells onto the material surfaces and control surfaces (e.g., tissue culture plastic) at a density of 10,000 cells/cm² in complete medium.
Adhesion Assay (After 4-24 Hours):
- Gently wash surfaces with PBS to remove non-adherent cells.
- Fix cells with 4% paraformaldehyde for 15 minutes.
- Permeabilize with 0.1% Triton X-100 and stain actin cytoskeleton with phalloidin (e.g., conjugated to Alexa Fluor 488) and nuclei with DAPI.
- Image using fluorescence or confocal microscopy. Quantify adhered cells by counting nuclei in multiple fields of view.
Viability/Proliferation Assay (Over 1, 3, 7 Days):
- Use a standard MTS or MTT assay. At each time point, add the reagent to the culture medium and incubate for 2-4 hours.
- Measure the absorbance of the formed formazan product at 490 nm. Plot the absorbance over time as an indicator of metabolic activity and cell proliferation.
Protocol: Assessing 3D Scaffold Integration and Remodeling
This protocol evaluates how cells migrate within and remodel a 3D porous scaffold, a closer mimic of the in vivo environment.
Scaffold Fabrication and Seeding:
- Use porous 3D scaffolds fabricated via methods like electrospinning (for synthetic polymers like PCL) or freeze-drying (for natural polymers like chitosan) [126] [123].
- Sterilize scaffolds (e.g., ethanol immersion followed by UV irradiation).
- Seed scaffolds with cells using a dynamic seeding method (e.g., on an orbital shaker) or by injecting a high-density cell suspension into the scaffold to ensure deep penetration.
Culture and Analysis:
- Culture cell-scaffold constructs in vitro for up to 4 weeks, refreshing the medium every 2-3 days.
- Histological Analysis (At endpoint): Fix constructs, paraffin-embed, section, and stain with Hematoxylin and Eosin (H&E) to visualize cell distribution and general morphology. Perform Masson's Trichrome staining to identify newly deposited collagen (stains blue) [83].
- Gene Expression Analysis (qRT-PCR): Lyse a portion of the construct to extract RNA. Analyze the expression of genes critical for tissue remodeling, such as:
- Collagen Type I (COL1A1) and Collagen Type III (COL3A1): Indicators of ECM synthesis.
- Matrix Metalloproteinases (MMPs, e.g., MMP1, MMP2) and their inhibitors (TIMPs): Indicators of ECM degradation and turnover balance [83].
Figure 2: 3D Scaffold Evaluation Workflow. A standard protocol for assessing cell-scaffold constructs involves fabrication, sterilization, long-term culture, and multi-faceted endpoint analysis to evaluate integration and remodeling [126] [83].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful experimentation in biomaterials research requires a suite of reliable reagents and materials. The following table details key items for the protocols described above.
Table 3: Essential Reagents for Biomaterial-Cell Interaction Studies
| Reagent/Material | Function/Description | Example Application in Protocols |
|---|---|---|
| Polycaprolactone (PCL) | A synthetic, biodegradable polyester with high strength and slow degradation rate; a common material for electrospun scaffolds [123] [127]. | Fabrication of 3D porous scaffolds for bone tissue engineering [127]. |
| Type I Collagen | The most abundant protein in mammalian ECM; forms fibrils that support cell attachment and migration [124]. | Coating of 2D surfaces or forming 3D hydrogels for in vitro cell culture models. |
| Phalloidin (Fluorescent Conjugate) | A toxin that binds with high affinity to filamentous actin (F-actin), used to visualize the cell cytoskeleton [3]. | Staining of adhered cells in the 2D adhesion assay to observe cell spreading and morphology. |
| DAPI (4',6-Diamidino-2-Phenylindole) | A fluorescent stain that binds strongly to adenine-thymine regions in DNA, used to label cell nuclei. | Counterstaining in fluorescence microscopy to identify and count all cells in a field. |
| MTS Assay Reagent | A colorimetric assay used to quantify metabolic activity; viable cells reduce MTS to a colored formazan product. | Measuring cell proliferation and viability on material surfaces over time. |
| Masson's Trichrome Stain | A three-color staining protocol that differentiates collagen (blue/green), nuclei (black), and cytoplasm/muscle (red) [83]. | Visualizing and quantifying the deposition of new collagen matrix within 3D scaffolds. |
| qRT-PCR Reagents | Kits and primers for quantitative reverse transcription polymerase chain reaction, used to measure gene expression levels. | Analyzing the expression of ECM-related genes (COL1A1, MMPs) in cells cultured within 3D scaffolds. |
Clinical Translation and Market Landscape
The journey from laboratory research to clinical application reveals distinct pathways and challenges for natural and synthetic biomaterials. The global synthetic tissue engineering market is projected to grow from USD 1.72 billion in 2025 to USD 5.61 billion by 2034, reflecting a strong compound annual growth rate (CAGR) of 14.14% [127]. This growth is largely driven by the tunability and scalability of synthetic polymers. By material type, the polycaprolactone (PCL) segment holds the largest market share due to its biodegradability and high strength, while the hydrogels segment is expected to grow the fastest, mimicking the ECM for soft tissue applications [127].
Natural biomaterials have already achieved significant clinical success in products like Apligraf (a bilayered skin substitute using bovine collagen and neonatal cells) and Grafix (a placental membrane) [128]. However, synthetic materials are gaining traction in complex applications, with innovations like 3D-bioprinted scaffolds and shape-memory polyurethanes showing great promise for creating patient-specific implants and smart wound dressings [127]. A persistent challenge for both classes, which impedes clinical outcomes, is achieving neovascularization—the formation of new blood vessels within the construct to deliver oxygen and nutrients essential for cell survival in thick tissue engineered grafts [127]. Future advancements will likely focus on creating hybrid materials that combine the strengths of both synthetic and natural polymers to overcome these limitations.
The integration of three-dimensional (3D) printing and advanced biomaterials is revolutionizing the development of personalized implants, marking a paradigm shift in patient care within regenerative medicine. This technological synergy enables the fabrication of patient-specific, bioabsorbable constructs that overcome the volume, contour, and donor-site limitations of traditional reconstruction methods [129]. The fundamental advancement lies in the ability to create implants that precisely mimic the natural extracellular matrix (ECM), providing both structural support and bioactive cues that actively orchestrate cellular processes including adhesion, migration, proliferation, and differentiation [3]. As a library, NLM provides access to scientific literature. Inclusion in an NLM database does not imply endorsement of, or agreement with, the contents by NLM or the National Institutes of Health.
The paradigm of personalized care through additive manufacturing represents a significant departure from conventional, standardized implants. By leveraging medical imaging data and computer-aided design (CAD), researchers and clinicians can now design and manufacture implants tailored to an individual's unique anatomical specifications [130]. This customization extends beyond mere physical dimensions to encompass tunable mechanical properties, degradation profiles, and biofunctionalization—attributes critically controlled by the selection and engineering of appropriate biomaterials [131] [3]. The resulting implants demonstrate enhanced biocompatibility and integration, ultimately leading to improved clinical outcomes and patient satisfaction.
Biomaterial Selection and Properties for 3D-Printed Implants
Criteria for Biomaterial Selection
The success of a 3D-printed implant is fundamentally governed by the properties of its constituent biomaterials. An ideal biomaterial must satisfy multiple criteria: biocompatibility to avoid provoking adverse immune responses, appropriate biodegradation rates synchronized with tissue regeneration, and mechanical properties matching the target native tissue to prevent stress shielding or mechanical failure [131] [130]. Furthermore, the material must be amenable to specific 3D printing techniques, requiring properties such as suitable viscosity, rheology, and curing dynamics [130].
Different clinical applications demand distinct material properties. For orthopedic or dental implants, materials with high mechanical stiffness and prolonged degradation rates are essential. In contrast, for soft tissue applications such as breast reconstruction or visceral organ repair, materials with flexibility and more rapid degradation profiles are preferable [131]. The biomaterials used in 3D printing are broadly classified into four categories: metals, ceramics, polymers, and composites, each offering distinct advantages and limitations for regenerative applications [131].
Major Biomaterial Classes and Their Characteristics
Table 1: Major Biomaterial Classes Used in 3D Printing for Medical Implants
| Biomaterial Class | Specific Examples | Key Advantages | Disadvantages | Primary Applications |
|---|---|---|---|---|
| Polymers [129] [131] | Poly-lactic acid (PLA), Polycaprolactone (PCL), Poly-lactic-co-glycolic acid (PLGA), Poly-4-hydroxybutyrate (P4HB) | Biodegradable, biocompatible, easily moldable, suitable mechanical strength | Can be leachable in body fluids, hard to sterilize | Orthopedic and dental implants, tissue engineering scaffolds, drug delivery systems |
| Metals & Alloys [131] | Titanium, Cobalt-Chrome alloy, Gold, Platinum | High material strength, easy to fabricate and sterilize | Corrosive potential, excessive elastic modulus, aseptic loosening risk | Orthopedic implants, screws, pins, and plates |
| Ceramics [131] | Calcium phosphate salts (e.g., Hydroxyapatite), Glass, Aluminum/Titanium Oxides | High material strength, excellent biocompatibility, corrosion resistance | Difficult to mold, excessive elastic modulus | Bioactive orthopedic implants, dental implants |
| Composites [131] | Carbon fiber reinforced bone cement, Dental filling composites | Excellent mechanical properties, corrosive resistant | Expensive, laborious manufacturing methods | Porous orthopedic implants, dental fillings |
Synthetic biodegradable polymers like PCL, PLA, and PLGA are particularly prominent in tissue engineering research due to their tunable degradation rates and mechanical properties. For instance, in breast reconstruction, 3D-printed chambers made from P4HB and PLA have supported up to 140% volume gain in large-animal models by providing a scaffold for vascularized fat flap integration [129]. The mechanical properties of these scaffolds, with elastic moduli ranging from 5–80 MPa, can be engineered to be compatible with native breast tissue, promoting more natural regeneration and reducing complications such as capsular contracture [129].
Technical Protocols and Methodologies
Workflow for Fabricating a Personalized, ECM-Mimicking Scaffold
The fabrication of a personalized implant is a multi-stage process that integrates imaging, computational design, and advanced manufacturing.
Table 2: Key Experimental Protocol for Personalized Scaffold Fabrication
| Step | Protocol Description | Key Parameters & Considerations |
|---|---|---|
| 1. Imaging & 3D Model Creation [130] | Acquire high-resolution medical images (e.g., CT, MRI) of the patient's defect site. Use segmentation software to create a digital 3D model of the target anatomy. | Image resolution, segmentation accuracy, file format (e.g., DICOM). |
| 2. CAD Model Generation [130] | Convert the anatomical model into a CAD file. Design the internal porous architecture (e.g., pore size, connectivity) to facilitate vascularization and cell migration. | Pore size (typically 100-400 μm), porosity percentage, mechanical stress simulation. |
| 3. STL File Generation & Slicing [130] | Export the CAD model as an STL (stereolithography) file. Use slicing software to convert the 3D model into 2D layered instructions (G-code) for the printer. | Layer thickness, print path optimization, support structure design. |
| 4. Biomaterial Preparation & Biofunctionalization [3] | Select and prepare the polymer (e.g., PCL, PLGA). Optionally functionalize with bioactive cues (e.g., RGD peptides, growth factors) to enhance bioactivity. | Solvent choice, peptide concentration, growth factor loading efficiency. |
| 5. 3D Printing [129] [130] | Fabricate the scaffold using the appropriate technique (e.g., Fused Deposition Modeling for PCL). Maintain sterile conditions if possible. | Nozzle temperature, print speed, pressure, environmental control. |
| 6. Post-Processing [130] | Remove support structures. Apply final sterilizations (e.g., ethylene oxide, gamma irradiation). Conduct quality control checks. | Sterilization method compatibility with biomaterial and bioagents, dimensional accuracy. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Biomaterial and Tissue Engineering Research
| Reagent/Material Solution | Function and Role in Research |
|---|---|
| Polycaprolactone (PCL) [129] [131] | A biodegradable polyester providing structural integrity to scaffolds; known for its slow degradation rate and excellent viscoelastic properties suitable for FDM printing. |
| RGD Peptide Sequences [3] | Short peptide chains (Arginine-Glycine-Aspartic acid) used to biofunctionalize scaffold surfaces; promote cell adhesion by mimicking ECM ligands for integrin receptors. |
| Type I Collagen [3] | A major natural component of the ECM; used in hydrogels or coatings to enhance scaffold biocompatibility and provide a native-like environment for cells. |
| Fused Deposition Modeling (FDM) Printer [131] [130] | An extrusion-based 3D printing system that melts and deposits thermoplastic filaments layer-by-layer; widely used for prototyping and creating porous scaffolds from polymers like PCL and PLA. |
| Matrix Metalloproteinase (MMP) Sensitive Peptides [3] | Peptides crosslinked into hydrogels that are degraded by cell-secreted MMPs; facilitate cell-mediated scaffold remodeling and invasion, mimicking dynamic ECM processes. |
Biomaterial-Cell Interaction and Underlying Biological Mechanisms
The therapeutic efficacy of 3D-printed implants is largely governed by their interaction with host cells, primarily mediated through integrin-mediated signaling pathways. Integrins, transmembrane receptors composed of α and β subunits, bind to specific ECM components—or biomaterials engineered to mimic them—such as collagen, fibronectin, and laminin [3]. This binding initiates the assembly of focal adhesion complexes, which serve as mechanical and biochemical signaling hubs, recruiting adaptor proteins like talin, vinculin, and paxillin [3].
The engagement of integrins triggers the activation of key downstream signaling pathways:
- Focal Adhesion Kinase (FAK) Pathway: Activated FAK regulates cytoskeletal dynamics and promotes cell migration, a critical step in tissue integration [3].
- MAPK/ERK Pathway: This pathway regulates gene expression related to cell proliferation and differentiation, driving the expansion and specialization of cells infiltrating the implant [3].
- PI3K/Akt Pathway: This pathway promotes cell survival, which is crucial in the stressful microenvironment of an injured tissue [3].
The mechanical properties of the scaffold—including stiffness, topography, and ligand density—profoundly influence this integrin signaling and subsequent cellular responses, a concept known as mechanotransduction [3]. Furthermore, successful long-term integration requires dynamic ECM remodeling, a balanced process of degradation and synthesis orchestrated by enzymes like matrix metalloproteinases (MMPs). A key hallmark of effective remodeling is the replacement of early, type III collagen with stronger, type I collagen, which enhances tissue tensile strength [3].
Diagram 1: Integrin-Mediated Signaling for Tissue Regeneration. This diagram illustrates how a biomaterial scaffold engages integrin receptors, triggering focal adhesion formation and activating key downstream pathways (FAK, MAPK/ERK, PI3K/Akt) that collectively regulate cellular processes essential for successful tissue regeneration and implant integration [3].
Clinical Translation and Future Perspectives
The translation of 3D-printed biomaterials from laboratory research to clinical application has demonstrated both promising outcomes and significant challenges. Early-phase clinical studies, particularly in breast reconstruction, have shown the biocompatibility and potential for adipose regeneration using custom 3D-printed, bioabsorbable chambers [129]. However, clinical results have been more modest than pre-clinical successes; the best human series achieved only sub-mastectomy volumes and reported issues such as high seroma rates, highlighting the translational gap [129]. The regulatory pathway for these complex, patient-specific devices also remains an area of uncertainty that requires further development [129] [130].
Future progress in the field hinges on several key factors. There is a pressing need for standardized large-animal protocols and head-to-head polymer comparisons to rigorously evaluate biomaterial performance [129]. Innovations such as 4D printing (where printed objects change shape over time under physiological stimuli) and the use of nanobiomaterials are on the horizon, promising even greater control over the implant-tissue interface [130]. Furthermore, bridging the gap between engineering and biology is crucial. This involves moving beyond structural mimicry to creating implants that actively participate in and orchestrate regeneration through controlled immune modulation and spatiotemporal delivery of bioactive factors [3] [132].
Diagram 2: Workflow for Personalized Implant Fabrication. This chart outlines the multi-stage process for creating and implementing a personalized 3D-printed implant, from initial medical imaging and computational design to biomaterial selection, fabrication, and final surgical implantation, culminating in in-vivo remodeling [129] [130].
The rise of personalized implants through 3D printing represents a transformative advancement in patient care, fundamentally rooted in the sophisticated application of biomaterials within tissue engineering research. The ability to design and manufacture patient-specific constructs that mimic the structural and biochemical complexity of the native ECM enables superior aesthetic and functional outcomes, moving beyond the limitations of traditional, standardized implants [129] [3]. While challenges in material biocompatibility, long-term degradation profiles, and regulatory pathways remain, the trajectory of progress is clear [129] [130].
The future of this field lies in the continued interdisciplinary collaboration among material scientists, biologists, engineers, and clinicians. By deepening our understanding of biomaterial-cell interactions and harnessing innovations in biofabrication, the next generation of 3D-printed implants will not only provide passive structural support but will actively orchestrate the regenerative process. This promises to redefine standards of care across surgical specialties, ultimately delivering on the promise of truly personalized and regenerative medicine.
Conclusion
Biomaterials are the cornerstone of tissue engineering, evolving from passive scaffolds to dynamic, bioactive systems that actively direct tissue regeneration. The integration of advanced manufacturing like 3D/4D printing, smart polymers, and stem cell biology is pushing the field beyond structural mimicry toward true biological control. Despite significant progress, challenges in immunomodulation, vascularization, and manufacturing scalability remain central to future research. The successful clinical translation of ECM-based products and the robust market growth signal a promising future. The next decade will likely be defined by fully personalized, off-the-shelf engineered tissues that address organ shortage and chronic diseases, fundamentally transforming patient outcomes in regenerative medicine.
References
- 1. Technology Overview of Biomaterials in Life Sciences [https://boydbiomedical.com/knowledge-center/articles/technology-overview-of-biomaterials-in-life-sciences]
- 2. 10 Top Innovative Tissue Engineering Companies in 2026 ... [https://www.scispot.com/blog/top-innovative-tissue-engineering-startups]
- 3. Biomaterials in tissue repair and regeneration: key insights ... [https://www.frontiersin.org/journals/medical-technology/articles/10.3389/fmedt.2025.1565810/full]
- 4. Biocompatibility Evolves: Phenomenology to Toxicology to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8221530/]
- 5. Biocompatibility - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/biocompatibility]
- 6. Advancements in Alginate-Derived Biomaterials for Tissue ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224725009724]
- 7. Advancements in Chitosan and Cellulose Nanoparticles for ... [https://pubmed.ncbi.nlm.nih.gov/40903632/]
- 8. Pushing the limits of bacterial cellulose for biomedicine [https://www.sciencedirect.com/science/article/pii/S0141813025072587]
- 9. Applications of recombinant type III collagen in tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502140/]
- 10. Research Progress of Sodium Alginate-Based Hydrogels in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469324/]
- 11. The role of collagen and collagen I/III ratio in pathological ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1679625/full]
- 12. Advances and Challenges in Polymer-Based Scaffolds for ... [https://www.mdpi.com/2073-4360/16/23/3303]
- 13. Advances in PCL, PLA, and PLGA-Based Technologies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566892/]
- 14. Material and biological characterization of 3D knitted ... [https://jbioleng.biomedcentral.com/articles/10.1186/s13036-025-00504-0]
- 15. Fabrication and evaluation of 3D printed PLGA/nHA/GO ... [https://www.nature.com/articles/s41598-025-96099-z]
- 16. Characteristics of 3D-Printed Polycaprolactone Tracheal ... [https://pubmed.ncbi.nlm.nih.gov/40828233/]
- 17. Three-Dimensional Printed Porous PLA Scaffolds with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298061/]
- 18. Calcium Phosphates for Bone Tissue Regeneration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610340/]
- 19. Calcium phosphates for biomedical applications [https://www.sciencedirect.com/science/article/pii/S0366317517300444]
- 20. Meta-analysis of the effects of calcium phosphate bone ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1553822/full]
- 21. Bioactive Glasses: Advancing Skin Tissue Repair through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11751205/]
- 22. Biomedical Applications of Titanium Alloys [https://pmc.ncbi.nlm.nih.gov/articles/PMC10780041/]
- 23. Novel Titanium Alloys for Tissue Engineering [https://www.intechopen.com/chapters/88063]
- 24. Titanium-Based alloys and composites for orthopedic ... [https://www.sciencedirect.com/science/article/pii/S0264127524002235]
- 25. Exploring 4D printing of smart materials for regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12412672/]
- 26. Bioresponsive matrices in drug delivery [https://jbioleng.biomedcentral.com/articles/10.1186/1754-1611-4-15]
- 27. Smart hydrogels for in situ tissue drug delivery [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-025-01166-2]
- 28. pH-Sensitive stimulus-responsive nanocarriers for targeted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4945487/]
- 29. pH-Responsive Polymer Nanomaterials for Tumor Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC8980858/]
- 30. Stimuli-responsive smart materials for biomedical ... [https://www.sciencedirect.com/science/article/abs/pii/S0927796X25002049]
- 31. Biomaterials and Tissue Engineering in Neurosurgery [https://www.mdpi.com/2673-6284/14/3/65]
- 32. Artificial intelligence for design strategies of tissue ... [https://www.sciencedirect.com/science/article/pii/S2667325825004832]
- 33. Advancing Scaffold Architecture for Bone Tissue Engineering [https://pmc.ncbi.nlm.nih.gov/articles/PMC12470323/]
- 34. Enhancing cell infiltration of electrospun fibrous scaffolds in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5883964/]
- 35. Three-dimensional porous gas-foamed electrospun ... [https://www.sciencedirect.com/science/article/abs/pii/S0021979721009413]
- 36. Current Standing and Future Potential of 3D Bioprinting ... [https://scifiniti.com/3105-0387/2/2025.0015]
- 37. Market Report 3 - D and Markets Bioprinting 2025 Research [https://www.researchandmarkets.com/reports/5752056/3d-bioprinting-market-report]
- 38. Current advances and prospects in biomaterials-guided ... [https://www.sciencedirect.com/science/article/pii/S2666138125000131]
- 39. Frontiers | Exploring the 4 linked bio-smart materials in... D printing [https://www.frontiersin.org/journals/dental-medicine/articles/10.3389/fdmed.2025.1558382/full]
- 40. Advancements and Applications of 4 in Biomedical... D Bioprinting [https://link.springer.com/article/10.1007/s10118-025-3259-0]
- 41. Recent breakthroughs in 3D bioprinting: A look at trends ... [https://pharmaphorum.com/rd/recent-breakthroughs-3d-bioprinting-look-trends-and-challenges]
- 42. Biomaterials and Tissue Engineering in Neurosurgery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452776/]
- 43. Tissue Engineering and Regeneration Market Set to Surge ... [https://www.bccresearch.com/pressroom/hlc/tissue-engineering-and-regeneration-market-set-to-surge-at-128-cagr?srsltid=AfmBOoqG6j1zSnuO3IyahvE6FNLvZZAbvtsHEcOdwOce1lk_e0GyHp4E]
- 44. Cell manufacturing for cell-based tissue engineering [https://www.frontiersin.org/journals/chemical-engineering/articles/10.3389/fceng.2025.1637075/full]
- 45. Osteoconductive and Osteoinductive Surface Modifications of Biomaterials for Bone Regeneration: A Concise Review [https://www.mdpi.com/2079-6412/10/10/971]
- 46. Enhancing Bone Repair with β-TCP-Based Composite Scaffolds [https://pmc.ncbi.nlm.nih.gov/articles/PMC12273726/]
- 47. An Osteoconductive, Osteoinductive, and Osteogenic Tissue-Engineered Product for Trauma and Orthopaedic Surgery: How Far Are We? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3205731/]
- 48. Processing and characterization of Ca3ZrSi2O9 ceramics ... [https://www.sciencedirect.com/science/article/abs/pii/S0925838825066630]
- 49. Development of Bioceramic Bone-Inspired Scaffolds ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565026/]
- 50. Chitosan-based composite scaffolds for bone tissue ... [https://www.sciencedirect.com/science/article/abs/pii/S2352492825024602]
- 51. Trend Overview 2025: Key Developments in Biomedical ... [https://biomedgrid.com/fulltext/volume25/trend-overview-2025-key-developments-in-biomedical-science-research.003320.php]
- 52. Biomaterials Market Size to Hit USD 523.75 Billion by 2034 [https://www.precedenceresearch.com/biomaterials-market]
- 53. Articular cartilage repair biomaterials: strategies and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10806349/]
- 54. 3D Printing for Bone-Cartilage Interface Regeneration [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.828921/full]
- 55. Recent advances in bionic scaffolds for cartilage tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289700/]
- 56. Tissue engineering strategies hold promise for the repair ... [https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-024-01260-w]
- 57. Cartilage Repair in 2025: Hope, Hype, or Horizon? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536974/]
- 58. Advancements in hydrogel design for articular cartilage ... [https://www.sciencedirect.com/science/article/pii/S2452199X2400392X]
- 59. Repair of osteochondral defects: efficacy of a tissue- ... [https://www.nature.com/articles/s41536-023-00335-x]
- 60. Innovative hydrogels in cutaneous wound healing [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1454903/full]
- 61. Cell-engineered technologies for wound healing and ... [https://www.nature.com/articles/s44385-025-00042-w]
- 62. Acellular Extracellular Matrix Scaffolds in Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565388/]
- 63. Design and Applications of Extracellular Matrix Scaffolds in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293650/]
- 64. Hydrogel Conjugation: Engineering of Hydrogels for Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300585/]
- 65. and Stem Biomaterials for Cells - PMC Tissue Engineering [https://pmc.ncbi.nlm.nih.gov/articles/PMC3596493/]
- 66. Bottom-up Biomaterial strategies for creating tailored stem ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1581292/full]
- 67. Exosome-based therapeutics in bone regeneration [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512519/]
- 68. Historical evolution, hotspots, and trends in tendon tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12144915/]
- 69. Editorial: Tissue engineering and regenerative medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC11949865/]
- 70. Localized Growth Factor Delivery from Microparticles ... [https://pubmed.ncbi.nlm.nih.gov/40816552/]
- 71. and Engineering -assisted exosomes as... biomaterial exosomes [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03275-x]
- 72. Molecular Signaling in Biomaterial-induced Foreign Body ... [https://pubmed.ncbi.nlm.nih.gov/40981767/]
- 73. Deciphering Key Foreign Body Reaction-Related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8958039/]
- 74. The effect of the foreign body response on drug elution from ... [https://pubmed.ncbi.nlm.nih.gov/39824001/]
- 75. Advanced biomaterials in immune modulation: The future ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325008099]
- 76. Research Progress on Biomaterials with Immunomodulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12412535/]
- 77. Immunotoxicity Testing Guidance May 1999 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/immunotoxicity-testing-guidance]
- 78. Tissue Engineering: Understanding the Role of Biomaterials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6502738/]
- 79. Biomimetic natural biomaterials for tissue engineering and ... [https://mmrjournal.biomedcentral.com/articles/10.1186/s40779-023-00448-w]
- 80. Biomaterials Strategies for Generating Therapeutic Immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5606982/]
- 81. Biomechanics and mechanobiology in functional tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4051419/]
- 82. Native Tissue - an overview [https://www.sciencedirect.com/topics/engineering/native-tissue]
- 83. Biomaterials in tissue repair and regeneration: key insights ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394198/]
- 84. Mechanobiomaterials: Harnessing mechanobiology ... [https://www.sciencedirect.com/science/article/pii/S2949907024000421]
- 85. Tissue Engineering and Regeneration Market Set to Surge ... [https://www.bccresearch.com/pressroom/hlc/tissue-engineering-and-regeneration-market-set-to-surge-at-128-cagr?srsltid=AfmBOorenz1EypI3KiegCHBVrq_cgCffOzqU401kCcIl7dp9L_TNQ7FG]
- 86. Oxygen and nutrient delivery in tissue engineering [https://pmc.ncbi.nlm.nih.gov/articles/PMC6852121/]
- 87. 生物材料促进创面血管化的研究进展 [https://pmc.ncbi.nlm.nih.gov/articles/PMC11630115/]
- 88. 6、血管组织工程中的生物材料与支架构建原创 [https://blog.csdn.net/tomato/article/details/151887802]
- 89. Research advances on hydrogels for promoting wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11965802/]
- 90. 模擬肝素生物材料助力血管新生開創再生醫學新篇章 [https://geneonline.news/%E6%A8%A1%E6%93%AC%E8%82%9D%E7%B4%A0%E7%94%9F%E7%89%A9%E6%9D%90%E6%96%99%E5%8A%A9%E5%8A%9B%E8%A1%80%E7%AE%A1%E6%96%B0%E7%94%9F%E9%96%8B%E5%89%B5%E5%86%8D%E7%94%9F%E9%86%AB%E5%AD%B8%E6%96%B0%E7%AF%87/]
- 91. 【协和医学杂志】血管化脑类器官的技术进展与应用前景 [https://www.medsci.cn/article/show_article.do?id=ff3b8e080498]
- 92. 东华大学何创龙教授团队:骨组织工程的血管化和神经支配 [https://wap.sciencenet.cn/blog-3529677-1445749.html]
- 93. Application of decellularization methods for scaffold ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1621641/full]
- 94. Bioactive scaffolds for tissue engineering: A review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11875452/]
- 95. The effect of decellularization processes on the immune ... [https://www.sciencedirect.com/science/article/abs/pii/S0040816625004173]
- 96. Decellularization in Tissue and Regenerative Medicine... Engineering [https://pubmed.ncbi.nlm.nih.gov/35547166/]
- 97. How to Validate Advanced Techniques for Food Sterility Testing in... [https://ebeammachine.com/how-to-validate-advanced-techniques-for-food-sterility-testing-in-2025/]
- 98. Biocompatibility of decellularized spinach leaves [https://www.nature.com/articles/s44385-025-00028-8]
- 99. Convergence of tissue engineering and sustainable development goals | Biotechnology for Sustainable Materials | Full Text [https://biotechsustainablematerials.biomedcentral.com/articles/10.1186/s44316-024-00021-y]
- 100. Material Extrusion Techniques for Biomedical Applications: Biomaterials and Their Performance - A Review - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S2352492825022196]
- 101. Editorial for the Special Issue on Biomaterials, Biodevices and Tissue Engineering - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11122819/]
- 102. Expedited Programs for Regenerative Medicine Therapies ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/expedited-programs-regenerative-medicine-therapies-serious-conditions-0]
- 103. Advances, challenges, and future directions in the clinical ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X24001698]
- 104. Evidence and Outcomes | Apligraf [https://www.apligraf.com/evidence-outcomes/]
- 105. Engineered Biopolymeric Scaffolds for Chronic Wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4975021/]
- 106. Osiris Therapeutics, Inc. Release: Grafix® Demonstrates ... [https://www.biospace.com/osiris-therapeutics-inc-release-grafix-and-0174-demonstrates-overwhelming-efficacy-in-landmark-stem-cell-study-for-the-treatment-of-diabetic-foot-ulc]
- 107. Comparison of Skin Substitutes for Acute and Chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8432988/]
- 108. In vivo engineered extracellular matrix scaffolds with ... [https://www.nature.com/articles/s41467-019-12545-3]
- 109. Scaffolding in tissue engineering: general approaches and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2587658/]
- 110. Design Challenges in Polymeric Scaffolds for Tissue ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.617141/full]
- 111. Acellular Scaffolds as Innovative Biomaterial Platforms for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8440725/]
- 112. Cell-Seeding Techniques in Vascular Tissue Engineering - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2946885/]
- 113. A comparative study on various cell sources for ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1128762/full]
- 114. Evaluation the Impressionability of Acellular Scaffolds in ... [https://brieflands.com/journals/ans/articles/147989]
- 115. Tendon regeneration deserves better: focused review on In ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12062838/]
- 116. Advancement in smart bone implants: the latest ... [https://www.sciencedirect.com/science/article/pii/S2452199X25001914]
- 117. Guide for authors - Biomaterials - ISSN 0142-9612 [https://www.sciencedirect.com/journal/biomaterials/publish/guide-for-authors]
- 118. Tissue Engineering and Regeneration Technology Global [https://www.globenewswire.com/news-release/2025/09/04/3144286/28124/en/Tissue-Engineering-and-Regeneration-Technology-Global-Market-Report-2025-2026-2030-Focus-on-ESG-Technological-Advancements-and-Competitive-Landscape.html]
- 119. Tissue Engineering and Regeneration Market Set to Surge ... [https://www.bccresearch.com/pressroom/hlc/tissue-engineering-and-regeneration-market-set-to-surge-at-128-cagr?srsltid=AfmBOooE4NSVMNht4RqFeBqjqzmjIZ1HGP-dmKpzhjbNM23pfd55Y5Z4]
- 120. Biomaterials Market Trends, Share and Forecast, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/biomaterials-market]
- 121. Global Tissue Engineering Market Outlook 2025-2032 [https://www.intelmarketresearch.com/global-tissue-engineering-forecast-market-20496]
- 122. Tissue Engineering Market Size 2023 - 2034 [https://www.towardshealthcare.com/insights/tissue-engineering-market-sizing]
- 123. Advances in Biodegradable Polymers and Biomaterials for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10488517/]
- 124. Advances of naturally derived biomedical polymers in ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2024.1469183/full]
- 125. Natural and Synthetic Polymers for Biomedical ... [https://www.mdpi.com/2073-4360/16/8/1159]
- 126. Natural and Synthetic Biomaterials, Structural Matrices ... [https://www.sciencedirect.com/science/article/pii/S2950575525000516]
- 127. Synthetic Tissue Engineering Market 2025 to 2034 Driven ... [https://www.towardshealthcare.com/insights/synthetic-tissue-engineering-market-sizing]
- 128. A review of regenerative medicine and tissue engineering with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12176865/]
- 129. State of Research on Tissue Engineering with 3D Printing for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524455/]
- 130. 3D printed biomaterials: From fabrication techniques to ... [https://www.sciencedirect.com/science/article/pii/S001430572400867X]
- 131. Novel Biomaterials Used in Medical 3D Printing Techniques [https://pmc.ncbi.nlm.nih.gov/articles/PMC5872103/]
- 132. 2025 Biomaterials and Tissue Engineering Conference GRC [https://www.grc.org/biomaterials-and-tissue-engineering-conference/2025/]