Cultivating Adaptive Expertise in Biomedical Engineering Education: Strategies for Navigating Complex Healthcare Challenges
This article explores the critical role of adaptive expertise in preparing biomedical engineers and drug development professionals for the unpredictable and rapidly evolving healthcare landscape.
Cultivating Adaptive Expertise in Biomedical Engineering Education: Strategies for Navigating Complex Healthcare Challenges
Abstract
This article explores the critical role of adaptive expertise in preparing biomedical engineers and drug development professionals for the unpredictable and rapidly evolving healthcare landscape. Moving beyond routine problem-solving, adaptive expertise enables professionals to innovate and apply knowledge effectively in novel situations. We examine the foundational theory distinguishing adaptive from routine expertise, present effective educational methodologies including transdisciplinary and experiential learning, address implementation challenges, and review validation frameworks. By synthesizing current research and practical applications, this work provides a comprehensive guide for educators and institutions aiming to foster the next generation of agile and innovative biomedical experts capable of addressing complex healthcare challenges from device development to therapeutic innovation.
Beyond Routine Expertise: Defining the Conceptual Framework for Adaptive Learning in Biomedicine
In the demanding and rapidly evolving field of biomedical engineering, the nature of expertise itself is a critical factor in innovation and problem-solving. Traditionally, expertise has been associated with high efficiency and accuracy in performing well-practiced tasks. However, a more nuanced understanding distinguishes between routine expertise and adaptive expertise, two fundamentally different approaches to professional challenges [1]. Routine expertise enables professionals to execute established procedures with speed and accuracy, making it essential for standardized laboratory protocols and quality control processes. In contrast, adaptive expertise empowers individuals to respond effectively to novel situations, devise innovative solutions, and apply their knowledge in unprecedented circumstances [1]. For biomedical engineers working at the intersection of biology, medicine, and engineering, where unexpected challenges in drug development or medical device design are common, cultivating adaptive expertise is increasingly recognized as essential for navigating the field's inherent complexities and driving forward translational research.
Theoretical Framework: The Pillars of Adaptive Expertise
The concept of adaptive expertise was first formally introduced by Hatano and Inagaki, who conceptualized it as existing on a continuum with routine expertise at the opposite pole [1]. While both types of expertise are founded on a deep knowledge base within a specific domain, they differ markedly in the structure of that knowledge and the approaches taken to problem-solving.
Foundational Characteristics
- Efficiency and Innovation: Adaptive expertise can be understood as the optimal balance between two dimensions: efficiency, the ability to fluently apply domain knowledge to familiar problems, and innovation, the capacity to devise solutions for new scenarios where no precedents exist [1]. This balance creates what has been termed the "optimal adaptability corridor" [1].
- Anchored Adaptability: Effective adaptiveness does not mean abandoning structure. It rests on a backbone of well-practiced, efficient routines for core tasks, which frees up the cognitive capacity necessary to notice subtle cues, interpret complex situations, and make appropriate adjustments. This has been powerfully described as "anchored adaptability"—where solid routines provide the anchor that enables meaningful flexibility [2].
- Knowledge Organization: A key differentiator between adaptive and routine experts lies not necessarily in the amount of knowledge they possess, but in its organization [2] [1]. Adaptive experts organize their knowledge around deep functional principles rather than just surface-level procedures. This enables them to recognize how and when to apply their knowledge in novel situations, facilitating what is known as analogical reasoning [1].
Core Dimensions and Cognitive Underpinnings
Three principal dimensions are widely used to describe and measure adaptive expertise: domain-specific skills, metacognitive skills, and innovative skills [1]. The interplay between these dimensions is supported by specific cognitive processes.
Table: Core Dimensions of Adaptive Expertise
| Dimension | Description | Manifestation in Biomedical Engineering |
|---|---|---|
| Domain-Specific Skills | Declarative ("knowing that"), procedural ("knowing how"), and conditional ("knowing when and where") knowledge [1]. | Understanding not just how to operate a bioreactor, but the biochemical principles governing its function and when to modify parameters. |
| Metacognitive Skills | "Thinking about thinking"; the ability to self-assess one's knowledge, identify gaps, and monitor problem-solving strategies [1]. | A researcher evaluating whether their current statistical knowledge is adequate to analyze a novel, complex dataset. |
| Innovative Skills | The ability to transcend established routines, reconceptualize problems, and develop novel methodologies [1]. | Designing a new drug delivery scaffold that bypasses limitations of existing materials. |
The development and application of these dimensions are influenced by cognitive load theory. Our working memory, where conscious information processing occurs, has severe limitations in capacity [3] [4]. Adaptive experts, through extensive practice and deep understanding, consolidate knowledge into schemas stored in long-term memory. These schemas can be retrieved and applied with minimal cognitive effort, freeing up working memory capacity to handle the novel aspects of a problem [4]. This efficient management of intrinsic cognitive load (the inherent difficulty of the material), reduction of extraneous cognitive load (load imposed by poor presentation or distractions), and optimization of germane cognitive load (load devoted to schema formation) is a hallmark of adaptive expertise [3].
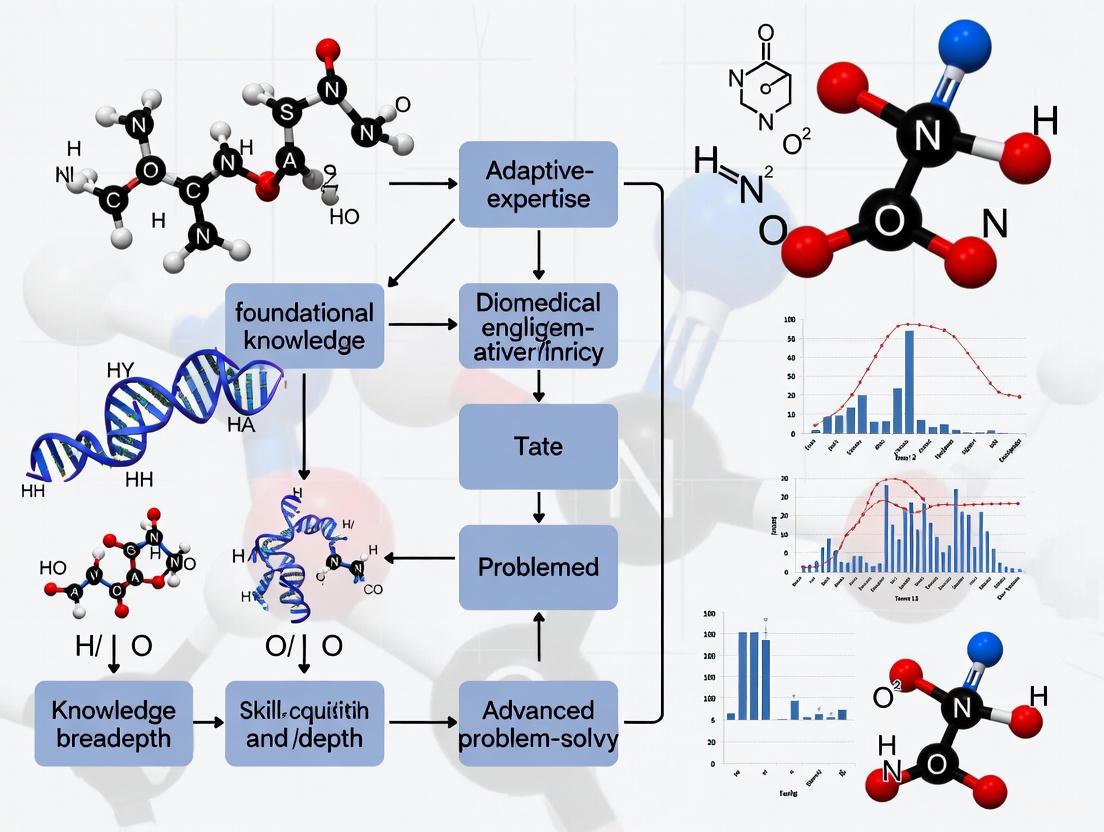
Diagram 1: Cognitive architecture of adaptive expertise, showing how efficient schemas free up working memory for innovation.
Quantitative Assessment and Research Findings
Measuring adaptive expertise requires robust methodological approaches. A common method involves the use of self-reported assessment tools, like the one developed by Carbonell et al. (2016), which probe the different dimensions of the construct [1].
Key Experimental Protocol: Survey-Based Assessment
A recent descriptive, cross-sectional study provides a clear protocol for investigating adaptive expertise among health professions educators (HPEs), a group analogous to biomedical engineering educators in their complex, knowledge-rich environment [1].
- Objective: To investigate how the adaptive expertise of HPEs influenced perceived work performance during the non-standard situation of the COVID-19 pandemic and to examine relationships between adaptive expertise and academic ranking/work experience.
- Population: The study sampled HPEs (lecturers to full professors) from a university.
- Tool: A self-reported survey tool based on the adaptive expertise framework by Carbonell et al. (2016) was used. Participants also answered questions about their perception of work performance, amount of work done, and teaching quality.
- Analysis: The researchers used statistical methods like the Kaiser-Meyer-Olkin (KMO) measure and Bartlett’s Test of Sphericity to ensure sample adequacy. They then analyzed scores for correlations with other variables like academic rank and perceived performance.
Quantitative Results and Correlations
The study yielded insightful quantitative results, summarized in the table below [1].
Table: Correlates of Adaptive Expertise in a Study of Health Professions Educators
| Variable | Correlation with Adaptive Expertise Score | Statistical Significance (p-value) |
|---|---|---|
| Perceived Work Performance | Positive Correlation (r = 0.41) | p < 0.05 |
| Academic Ranking | Positive Correlation (r = 0.42) | p < 0.05 |
| Work Experience | No Significant Correlation | Not Significant |
| Age of Educator | No Significant Correlation | Not Significant |
The average adaptive expertise score on a 5-point scale was 4.18 ± 0.57, indicating a generally high self-assessment. The findings were particularly revealing: the positive correlation with work performance underscores the practical impact of adaptive expertise, while the correlation with academic rank suggests it is a form of 'mastery' recognized in career advancement. Most importantly, the lack of correlation with age and experience indicates that adaptive expertise is not automatically acquired with seniority but must be deliberately developed [1].
A Framework for Cultivating Adaptive Expertise in Education
Based on the theoretical and empirical evidence, a coherent framework for developing adaptive expertise can be proposed, particularly relevant for biomedical engineering education. This framework posits that adaptive expertise is underpinned by four interconnected facets: the ability to Understand, Do, Decide, and Improve [2].
Diagram 2: Four-facet framework for developing adaptive expertise, illustrating core interconnected capacities.
- Understand: This involves building conceptual knowledge organized around core principles and problems of the field (e.g., "Ensure biocompatibility," "Optimize drug release kinetics") rather than as a rigid list of techniques. This organization makes knowledge more accessible and applicable in new situations [2].
- Do: Tactical knowledge must be supported by technical capability. Learners need a repertoire of techniques that they can practice to a level of high efficiency, freeing cognitive resources for adaptation. As stated in one source, "What is tactically desirable must be technically possible" [2].
- Decide: This facet is driven by situation-sensitive mental models—deeply understood representations of how a system behaves under different conditions. These models allow experts to notice critical cues, interpret their significance, predict potential outcomes, and decide on the best course of action [2].
- Improve: The final facet is an adaptive mindset, characterized by cognitive flexibility and the pursuit of the "best thing" rather than just a "best fit." This involves viewing one's role as requiring continuous improvement, holding problem framings lightly, forming multiple hypotheses, and being prepared to reformulate approaches based on evidence [2].
Research Reagent Solutions: Tools for Investigating Expertise
Studying adaptive expertise in the context of biomedical engineering education requires a toolkit of methodological "reagents." The following table details key tools and their functions based on the cited research.
Table: Research Reagent Solutions for Studying Adaptive Expertise
| Research Tool / Concept | Function in Investigation |
|---|---|
| Self-Report Assessment (e.g., Carbonell et al. tool) | Quantifies an individual's self-perceived level of adaptive expertise across its core dimensions (domain-specific, metacognitive, innovative skills) [1]. |
| Work Performance Metrics | Provides a correlative measure to validate the impact of adaptive expertise on tangible outcomes like teaching quality, research output, or project success [1]. |
| Cognitive Load Assessment | Measures the intrinsic, extraneous, and germane cognitive loads experienced by learners during tasks, indicating efficiency of knowledge structure and problem-solving approach [3] [4]. |
| Problem-Solving Protocols (Think-Aloud) | Uncovers the underlying mental models and decision-making processes of individuals when faced with novel problems, distinguishing adaptive from routine approaches [1]. |
| Analysis of Work Products | Evaluates the creativity, efficiency, and appropriateness of solutions generated by individuals or teams in response to standard and novel challenge problems. |
Implications for Biomedical Engineering Education and Research
The distinction between adaptive and routine expertise has profound implications for how biomedical engineers are trained and how research teams are structured and developed. For education, moving beyond a curriculum that primarily transmits static knowledge and procedural skills is necessary. Instructional design should aim to reduce extraneous cognitive load while challenging students to build deep conceptual understanding and flexible mental models [4]. This can be achieved through pedagogical approaches like problem-based learning with variable contexts, analyzing complex case studies, and engaging in deliberate reflection on both successful and unsuccessful problem-solving attempts.
For the professional development of researchers and drug development professionals, the findings suggest that organizations should invest in creating "Situation Sensitive" environments [2]. These environments focus on building a common understanding of first principles, provide coaching and rehearsal to build efficient routines, and frame professional development as continuous, contextual problem-solving rather than the simple application of "best practices." This approach, combined with an awareness of the cognitive principles that underpin expertise, can foster the adaptive capacity necessary to overcome the unprecedented challenges in biomedical engineering and therapeutic development.
The field of biomedical engineering (BME) is experiencing unprecedented transformation driven by technological advancements, increasingly complex human health challenges, and the globalization of the workforce [5]. This evolution demands a fundamental shift in the competencies required of BME professionals, moving beyond traditional technical expertise toward adaptive skills that enable flexibility, innovation, and effective problem-solving in novel situations. The theoretical framework of adaptive expertise provides a crucial lens for understanding how biomedical engineers can navigate this rapidly changing landscape, developing the capacity to apply knowledge flexibly and generate innovative solutions when faced with unusual circumstances or unprecedented challenges [6] [1].
Within health professions education research, adaptive expertise is increasingly recognized as essential for professionals who must solve novel problems and handle ambiguous, complex medical situations [6]. This perspective applies equally to biomedical engineering, where graduates must confront evolving health-related challenges that demand both specialized knowledge and the ability to rapidly acquire additional skills as needed. This whitepaper examines the critical need for adaptive skills in biomedical engineering through analyzing industry demands, educational challenges, and evidence-based frameworks for cultivating adaptive expertise.
Theoretical Framework: Understanding Adaptive Expertise
Adaptive expertise was first conceptualized by Hatano and Inagaki (1986) as a contrast to routine expertise [1] [7]. While routine expertise represents the knowledge and skills that enable efficiency in familiar situations, adaptive expertise encompasses the capability to apply flexible problem-solving approaches and generate novel solutions when unusual circumstances occur [6]. This conceptual distinction is particularly relevant for biomedical engineering, where professionals must balance efficient execution of established procedures with innovation in developing new technologies and approaches.
Dimensions of Adaptive Expertise
Research has identified several critical dimensions that characterize adaptive expertise and distinguish it from routine expertise:
- Domain-specific knowledge: Adaptive experts possess deep conceptual understanding that is organized, abstracted, and consolidated independently of situational contexts, enabling application across various scenarios [1]
- Metacognitive skills: The ability to "think about thinking" allows adaptive experts to assess their knowledge, identify gaps, and strategically apply knowledge in unfamiliar contexts [1]
- Innovation capabilities: Adaptive experts transcend established routines to develop novel solutions, balancing efficiency with creative problem-solving [1]
- Cognitive flexibility: This enables professionals to approach problems from multiple perspectives and adapt strategies as challenges evolve [7]
In healthcare-related fields, adaptive performance is increasingly understood as the visible outcome of adaptive expertise, triggered by contextual changes in tasks or environments [6]. This performance dimension is particularly relevant for biomedical engineers working at the intersection of technology, biology, and medicine, where contextual changes are constant.
Drivers Demanding Adaptive Skills in Biomedical Engineering
Technological Acceleration and Disruption
Biomedical engineering is being transformed by breakthrough technologies including AI-driven protein folding prediction, miRNA-based therapies, mRNA vaccines, CRISPR gene-editing, digital PCR, nanopore sequencing, and single-cell analysis technologies [8]. These innovations emerge at a pace that traditional curricula struggle to match, creating a conspicuous gap between fundamental principles taught in programs and the advanced technologies driving the field forward [8]. This technological volatility requires biomedical engineers to continually adapt to new tools, methodologies, and conceptual frameworks throughout their careers.
The integration of artificial intelligence and machine learning into biomedical engineering practice exemplifies this trend. These technologies are changing how engineering problems are solved across domains including medical imaging, drug discovery, and diagnostic tool development [5]. As noted in industry perspectives from recent Biomedical Engineering Education Summits, critical thinking when analyzing data and adapting to new tools has become increasingly essential, particularly in light of AI advancements and the use of large datasets in BME industry [5].
Increasing Complexity of Health Challenges
Biomedical engineers now address health challenges of unprecedented complexity, often involving interconnected biological systems, multi-scale phenomena, and diverse patient populations. An aging global population, consequences of the COVID-19 pandemic, and novel treatment modalities have collectively created urgent needs for more sophisticated diagnostic tools and therapeutic interventions [8]. These complex challenges resist routine solutions and demand adaptive approaches that integrate knowledge across disciplines and stakeholder perspectives.
The COVID-19 pandemic particularly highlighted the need for adaptive expertise, as professionals across healthcare and related fields were forced to rapidly develop creative, alternative modes of operation when standard practices were disrupted [1]. This disruption extended to biomedical engineering education and practice, requiring rapid adaptation to new constraints and requirements.
Interdisciplinary Work Environments
Biomedical engineering is inherently interdisciplinary, integrating principles from traditional engineering, biological sciences, and medicine [8]. This interdisciplinary nature has intensified as health challenges increasingly require collaboration between specialists from diverse fields. Industry surveys reveal that professional skills including communication, collaboration, and teamwork have grown in importance for BME graduates, with employers emphasizing their critical role in enabling effective work in cross-disciplinary contexts [5].
Table 1: Evolution of Industry Skill Priorities for BME Graduates (2019-2024)
| Skill Category | 2019 Ranking | 2024 Ranking | Significance of Change |
|---|---|---|---|
| Communication Skills | 2nd (Interpersonal)5th (Writing)6th (Technical Presentation) | 1st | Increased emphasis on communicating technical work to diverse audiences |
| Problem-solving | 1st | 3rd | Shift from top priority to still important but secondary to professional skills |
| Teamwork/Collaboration | 4th | 2nd | Recognition of essential role in interdisciplinary work environments |
| Programming/Data Science | Not in top rankings | 4th | Emerging importance due to AI and large dataset utilization |
Measuring Adaptive Expertise in Biomedical Contexts
Current Measurement Instruments and Methodologies
A scoping review of measurement instruments for adaptive expertise and adaptive performance in healthcare contexts reveals a growing but limited set of assessment tools [6]. The review identified 19 measurement instruments across 17 articles, only three of which were specifically developed for the healthcare domain. These instruments were categorized into six types, with a noted dominance of self-evaluation and job requirement instruments, while other methods such as design scenarios, mixed-methods instruments, and collegial verbalization remain underrepresented [6].
The instruments vary significantly in their conceptualization, operationalization, and quality of validity and reliability evidence. This measurement challenge is particularly relevant for biomedical engineering education research, as it highlights the need for domain-specific instruments with strong psychometric properties [6].
Relationship Between Adaptive Expertise and Professional Outcomes
Research conducted with health professions educators during the COVID-19 pandemic provides empirical evidence linking adaptive expertise to professional effectiveness. A study of 40 health professions educators found statistically significant correlations between scores of adaptive expertise and both perceived work performance (r = 0.41, p < 0.05) and academic ranking (r = 0.42, p < 0.05) [1]. Interestingly, adaptive expertise scores were not associated with work experience or age, suggesting that adaptive expertise is not automatically acquired with seniority but must be deliberately developed [1].
Table 2: Adaptive Expertise Measurement in Health Professions Education
| Study Aspect | Findings | Implications for BME |
|---|---|---|
| Sample Size | 40 HPEs from University of Twente | Limited generalizability but suggestive for related fields |
| Average AE Score | 4.18 ± 0.57 on 1-5 scale | Establishes baseline for comparison |
| Key Dimensions | Domain and innovative skills as principal distinct dimensions | Highlights areas for targeted development |
| Correlation with Experience | No significant relationship | Challenges assumption that expertise develops automatically with time |
| Correlation with Performance | Significant positive relationship (r = 0.41, p < 0.05) | Supports investment in adaptive skills development |
Educational Frameworks for Developing Adaptive Expertise
The NICE Strategy for Biomedical Engineering Education
The NICE strategy represents an integrated approach to addressing biomedical engineering education challenges through four interconnected components [8]:
New Frontier: This component focuses on exposing students to cutting-edge advancements through recent research articles and artificial intelligence tools such as DeepSeek, ChatGPT, and Kimi to assist with literature search, summarization, and concept clarification [8].
Integrity: Using case studies of both successful scientists and fraudulent cases (e.g., Theranos), students develop ethical reasoning and understand the implications of their work on patient health and society [8].
Critical and Creative Thinking: Through analysis of creative ideas and generation of novel solutions, students develop the cognitive flexibility essential for adaptive expertise. Activities include peer review exercises and case-based discussions of real-world biomedical engineering challenges [8].
Engagement: Involving clinical doctors and industry professionals in teaching provides students with practical context and exposes them to real-world constraints and requirements. This situated learning approach helps develop the conditional knowledge ("knowing when and where") that characterizes adaptive expertise [8].
Implementing Adaptive Expertise Development
Research suggests that adaptive expertise develops through specific types of learning experiences and environments. Key factors that influence its development include [7]:
- Task variety and complexity: Exposure to diverse problems with varying levels of complexity
- Metacognitive prompting: Activities that encourage reflection on problem-solving strategies
- Feedback quality: Timely, specific feedback focused on deeper understanding
- Learning climate: Environments that tolerate mistakes and encourage experimentation
For biomedical engineering education, this implies a shift from traditional lecture-based approaches to experiential, problem-based learning that presents students with novel, ill-structured challenges resembling real-world biomedical engineering contexts.
Research Reagents and Methodological Tools
Table 3: Essential Research Reagents and Tools for Adaptive Expertise Research
| Reagent/Tool | Function in Research | Application Context |
|---|---|---|
| Carbonell et al. Adaptive Expertise Instrument | Self-reported measure of adaptive expertise dimensions | Quantifying adaptive expertise levels in educational interventions |
| Domain-specific knowledge assessments | Measuring depth and organization of technical knowledge | Evaluating conceptual understanding versus rote memorization |
| Think-aloud protocols | Capturing metacognitive processes during problem-solving | Studying differences in problem-solving approaches between routine and adaptive experts |
| Design scenarios | Presenting novel engineering challenges for response analysis | Assessing innovation and flexibility in applied contexts |
| AI-assisted learning tools (ChatGPT, DeepSeek) | Supporting literature review and concept mastery | Developing independent learning skills for navigating rapidly evolving fields |
The critical need for adaptive skills in biomedical engineering stems from fundamental changes in the field itself—its accelerating technological base, increasingly complex problems, and highly interdisciplinary nature. The theoretical framework of adaptive expertise provides valuable insights into how biomedical engineers can be prepared to navigate this evolving landscape, emphasizing the importance of deep conceptual understanding, metacognitive skills, and innovative capabilities alongside technical proficiency.
Educational approaches such as the NICE strategy demonstrate how adaptive expertise can be cultivated through intentional curriculum design that balances technical knowledge with professional skills, ethical reasoning, and real-world engagement. As the field continues to evolve, developing and validating reliable measurement instruments for adaptive expertise will be crucial for advancing educational research and practice in biomedical engineering.
For researchers, scientists, and drug development professionals, embracing this adaptive mindset is not merely beneficial but essential for driving innovation and addressing the complex health challenges of our time. The institutions that will lead the future of biomedical engineering are those that recognize this imperative and deliberately create environments where adaptive expertise can flourish.
This whitepaper examines the three core dimensions of adaptive expertise development in biomedical engineering education: domain-specific knowledge, metacognition, and innovation capacity. Through analysis of contemporary educational frameworks and empirical studies, we demonstrate how the strategic integration of these dimensions prepares biomedical engineering professionals for complex challenges in drug development and medical technology innovation. The NICE (New frontier, Integrity, Critical and creative thinking, Engagement) strategy provides a foundational model for cultivating these competencies, with evidence showing significant improvements in student outcomes across multiple institutions. We present quantitative data from implementation studies, detailed experimental protocols for educational interventions, and visualization of key conceptual relationships to guide researchers and educators in developing more effective training paradigms for the biomedical workforce.
Biomedical engineering stands at the intersection of rapid technological advancement and pressing healthcare needs, distinguished from traditional disciplines by its highly interdisciplinary nature and focus on practical solutions translatable to clinical applications [9]. The convergence of an aging global population, post-pandemic challenges, and novel treatment modalities has created unprecedented demand for sophisticated diagnostic tools and therapeutic technologies [9]. This landscape requires professionals who possess not only technical knowledge but also the adaptive expertise to apply this knowledge flexibly in novel situations and evolving contexts.
Adaptive expertise refers to the ability to use knowledge and experience to learn in unanticipated situations, contrasting with routine expertise that applies knowledge appropriately to solve routine problems [10]. In biomedical engineering, this adaptability is crucial because the regulatory environment and knowledge base are likely to change significantly over the course of a professional's career [10]. Research indicates that adaptive expertise can be systematically cultivated through educational approaches that simultaneously develop domain-specific knowledge, metacognitive skills, and innovation capacities [11].
Domain-Specific Knowledge: Building the Foundational Framework
Domain-specific knowledge in biomedical engineering encompasses both fundamental principles and awareness of cutting-edge advancements. Current biomedical engineering curricula often emphasize foundational principles while lacking coverage of emerging technologies, creating a significant curriculum gap [9]. This gap is particularly problematic given recent field revolutions including AI-driven protein folding prediction, miRNA-based therapies, mRNA vaccines, CRISPR gene-editing, digital PCR, nanopore sequencing, and single-cell analysis technologies [9].
The "New Frontier" Approach to Domain Knowledge
The NICE educational strategy addresses this challenge through its "New Frontier" component, which immerses students in recent research literature and emerging technologies [9]. In implementation, students are required to read research articles published within the past two years, summarize related articles, and present findings orally. Artificial intelligence tools including DeepSeek, ChatGPT, and Kimi are integrated to assist with literature search, summarization, and concept clarification [9].
Table 1: Quantitative Outcomes of New Frontier Implementation (3-Year Period)
| Metric | Pre-Implementation | Year 1 | Year 2 | Year 3 |
|---|---|---|---|---|
| Student Satisfaction | 72% | 85% | 88% | 91% |
| Industry Readiness Score | 68% | 79% | 82% | 86% |
| Technical Knowledge Retention | 70% | 81% | 85% | 87% |
Experimental Protocol: Current Literature Integration
Objective: Enhance students' familiarity with emerging technologies and research methodologies in biomedical engineering.
Materials:
- Access to scientific databases (PubMed, IEEE Xplore, Web of Science)
- AI-based research tools (DeepSeek, ChatGPT, Kimi)
- Structured presentation templates
- Peer evaluation rubrics
Procedure:
- Students select a recent research article (published within last 24 months) relevant to course topics
- Using AI tools, students identify 4-6 related articles and generate summaries
- Students create critical analyses highlighting methodological strengths/limitations
- Oral presentations (15 minutes) delivered to peer audience
- Peer reviewers evaluate presentations using standardized rubrics
- Instructors provide feedback on technical accuracy and critical analysis depth
Assessment: Pre- and post-tests measuring knowledge of emerging technologies; industry partner evaluations of technical presentations; longitudinal tracking of publication literacy.
Metacognition: The Core of Self-Directed Learning and Professional Growth
Metacognition, often described as "thinking about thinking," involves the regulation of one's cognitive activities in learning processes [12]. It encompasses both knowledge of cognition (knowing about persons, tasks, and strategies) and regulation of cognition (planning, monitoring, controlling, and evaluating activities) [12]. In biomedical engineering education, metacognitive skills enable students to become self-directed learners who can assess task demands, evaluate their knowledge and skills, plan approaches, monitor progress, and adjust strategies as needed [12].
Concept Mapping as a Metacognitive Tool
Concept mapping serves as an effective metacognition tool in biomedical engineering education. Research shows that concept mapping helps students organize knowledge systematically, describe connections between concepts, create visual representations of relationships, verbalize their understanding, and evaluate their strengths and weaknesses [12]. The process involves diagramming mental connections between concepts, which promotes deeper understanding and reveals "muddiest points" where students struggle most.
Table 2: Concept Mapping Implementation Outcomes in Biomedical Engineering Courses
| Parameter | In-Person Instruction (2019) | Online Instruction (2021) |
|---|---|---|
| Completion Rate | 59.30% | 47.67% |
| Performance Improvement (p-value) | > 0.05 (not significant) | > 0.05 (not significant) |
| Student Perception of Usefulness | 78% | 78% |
| Willingness to Apply in Other Courses | 84% | 84% |
| Effect Size | 0.29 | 0.33 |
The MENTOR Framework for Metacognitive Development
The MENTOR (MEtacognition-driveN self-evoluTion framework for uncOvering and mitigating implicit Risks) framework represents an advanced approach to developing metacognitive capabilities, originally developed for LLMs but with applicability to biomedical engineering education [13]. This framework employs metacognitive strategies including perspective-taking (evaluating responses from diverse viewpoints) and consequential thinking (assessing potential real-world impacts) to enhance critical self-assessment [13].
Diagram Title: MENTOR Metacognitive Framework
Experimental Protocol: Concept Mapping Intervention
Objective: Develop metacognitive skills through visual knowledge representation and reflection.
Materials:
- Concept mapping software (CmapTools, MindMeister, or physical materials)
- Structured reflection prompts
- Peer feedback forms
- Metacognitive awareness inventory
Procedure:
- Introduction to concept mapping principles and examples
- Identification of core concepts and relationships for specific biomedical engineering topics
- Individual concept map creation (weeks 8-10 of course)
- Paired explanations and peer feedback sessions
- Revision of concept maps based on feedback
- Completion of structured reflection prompts addressing:
- Knowledge organization strategies
- Connection identification processes
- Challenge recognition in concept relationships
- Self-assessment of understanding
Assessment: Pre- and post-intervention metacognitive awareness inventories; concept map complexity scores; qualitative analysis of reflection responses; longitudinal tracking of problem-solving approaches.
Innovation: Cultivating Creative Capacity in Biomedical Engineering
Innovation in biomedical engineering education requires fostering both critical and creative thinking as complementary processes [9]. Critical thinking provides the analytical framework to evaluate and refine creative ideas, while creative thinking pushes boundaries by generating novel solutions [9]. Traditional educational models often prioritize rote learning and compliance, but a shift toward fostering innovation capacity is necessary to prepare students for the dynamic biomedical landscape.
Engagement with Clinical and Industrial Contexts
The "Engagement" component of the NICE strategy addresses the need for practical innovation experience by actively involving clinical doctors and industry professionals in teaching and student product development projects [9]. This approach bridges the gap between academia and industry, providing students with hands-on experience in identifying unmet clinical needs and translating them into viable product designs.
Interdisciplinary Collaboration Framework
Innovation in biomedical engineering increasingly requires interdisciplinary collaboration between medical experts and engineers. Research indicates that making disciplinary perspectives explicit significantly enhances collaboration effectiveness [14]. A structured framework for analyzing disciplinary perspectives includes examining:
- Epistemic Questions: What constitutes knowledge in the discipline?
- Teleological Questions: What are the primary goals of the discipline?
- Methodological Questions: What methods are valued for knowledge production?
- Ontological Questions: What are the fundamental entities of study?
Diagram Title: Interdisciplinary Innovation Framework
Experimental Protocol: Clinical Product Innovation Project
Objective: Develop innovation skills through authentic product development experiences.
Materials:
- Clinical need identification templates
- Industry mentor guidance protocols
- Prototyping resources (3D printers, simulation software)
- Design review presentation templates
Procedure:
- Student teams (3-5 members) formed with mixed backgrounds
- Clinical immersion sessions to identify unmet needs through:
- Observation of clinical procedures
- Interviews with healthcare providers
- Analysis of workflow inefficiencies
- Ideation sessions to generate potential solutions
- Regular consultation with industry mentors on:
- Technical feasibility
- Regulatory considerations
- Manufacturing constraints
- Business model alignment
- Prototype development and iteration
- Final design reviews with clinical and industry panels
Assessment: Prototype functionality scores; clinical impact potential ratings; innovation novelty evaluations; business viability assessments; longitudinal tracking of patent applications and technology commercialization.
Integration and Assessment: Measuring Development Across Dimensions
The comprehensive development of domain-specific knowledge, metacognition, and innovation capacity requires integrated assessment strategies. Research from Northwestern University's Engineering Education Research Center demonstrates the importance of measuring computational adaptive expertise in design and innovation contexts [11]. Their framework evaluates both efficiency (routine expertise) and innovation (adaptive expertise) across multiple dimensions.
Table 3: Integrated Assessment Framework for Adaptive Expertise Development
| Dimension | Assessment Methods | Performance Indicators | Benchmark Targets |
|---|---|---|---|
| Domain Knowledge | Pre/post content tests; Literature analysis assignments; Technical presentation evaluations | Accuracy scores; Depth of critical analysis; Knowledge application accuracy | >85% content mastery; Industry-rated presentation competence >4.0/5.0 |
| Metacognition | Concept mapping complexity; Reflection journal quality; Self-regulated learning strategies inventory | Connection diversity; Insight depth; Strategy adaptation frequency | >3.5/5.0 metacognitive awareness; >80% strategy diversification |
| Innovation | Project novelty ratings; Clinical impact potential; Interdisciplinary collaboration effectiveness | Solution originality; Need specificity; Perspective integration quality | >4.0/5.0 innovation rating; >90% interdisciplinary communication competence |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Research Reagent Solutions for Biomedical Engineering Education and Research
| Reagent/Tool | Function | Application Context |
|---|---|---|
| AI Research Assistants (ChatGPT, DeepSeek, Kimi) | Literature search, summarization, and concept clarification | New Frontier implementation; Research methodology development |
| Concept Mapping Software | Visual knowledge representation and connection identification | Metacognitive skill development; Conceptual relationship clarification |
| Interdisciplinary Perspective Framework | Systematic analysis of disciplinary approaches and assumptions | Innovation projects; Cross-functional team collaboration |
| Static-Dynamic Hybrid Rule Pool | Structured guidance with adaptive learning capabilities | Ethical decision-making; Regulatory compliance training |
| Activation Steering Mechanisms | Direct modulation of reasoning processes during task execution | Metacognitive strategy implementation; Complex problem-solving |
| 1-(4-Hydroxy-2-methoxyphenyl)-3-(4-hydroxy-3-prenylphenyl) | 1-(4-hydroxy-2-methoxyphenyl)-3-(4-hydroxy-3-prenylphenyl)propane | High-purity 1-(4-hydroxy-2-methoxyphenyl)-3-(4-hydroxy-3-prenylphenyl)propane for research. For Research Use Only. Not for human or veterinary use. |
| N-Boc-15-aminopentadecanoic acid | N-Boc-15-aminopentadecanoic Acid|RUO | N-Boc-15-aminopentadecanoic acid is a specialty fatty acid derivative for research use only (RUO). Explore its applications in chemical synthesis. |
The integration of domain-specific knowledge, metacognition, and innovation represents the cornerstone of adaptive expertise development in biomedical engineering education. The NICE strategy provides a validated framework for simultaneously addressing these dimensions, with empirical evidence demonstrating significant improvements in student outcomes across multiple metrics. The experimental protocols and assessment strategies outlined in this whitepaper offer practical approaches for implementing these educational innovations across diverse institutional contexts.
As biomedical engineering continues to evolve in response to technological advancements and healthcare challenges, the cultivation of adaptive expertise becomes increasingly critical. Educational programs that strategically integrate domain-specific knowledge, metacognitive development, and innovation capacity will best prepare the next generation of biomedical engineers to develop transformative solutions to medicine's most pressing problems. Future research should focus on longitudinal tracking of career outcomes and refinement of assessment methodologies to further validate and enhance these educational approaches.
The Optimal Adaptability Corridor represents a critical framework for expert development in biomedical engineering, describing the dynamic balance between two essential dimensions: efficiency in applying established knowledge to solve routine problems, and innovation in generating novel solutions for unprecedented challenges. This concept, rooted in the adaptive expertise theory first introduced by Hatano and Inagaki, has gained renewed urgency in healthcare education as biomedical engineers face rapidly evolving technologies and complex patient care challenges that demand both procedural fluency and conceptual understanding [1] [15]. Within biomedical engineering education, this framework provides a theoretical foundation for preparing professionals who can not only execute standard protocols with precision but also invent new approaches when confronting novel diagnostic, therapeutic, or rehabilitation challenges.
The COVID-19 pandemic served as a stark demonstration of this imperative, where health professions educators were forced to abruptly shift educational paradigms and develop creative alternatives to traditional training methods [1]. Those with higher adaptive expertise demonstrated significantly better work performance during this disrupted period, highlighting the practical significance of this balance for maintaining educational continuity and quality [1]. Furthermore, research has revealed that adaptive expertise correlates positively with academic ranking but not automatically with age or seniority, suggesting it represents a specialized 'mastery' that must be deliberately cultivated rather than passively acquired through experience [1].
Theoretical Foundations of Adaptive Expertise
Distinguishing Adaptive and Routine Expertise
Adaptive expertise fundamentally differs from routine expertise along critical dimensions of knowledge representation and application. While routine experts demonstrate speed and accuracy in solving problems that fit well-established patterns, they often struggle when faced with novel situations where tasks, methods, or desired outcomes are not previously known [1] [15]. In contrast, adaptive experts respond to novel or unexpected situations more effectively, efficiently, and innovatively by drawing on their conceptual understanding to generate context-appropriate solutions [1].
The key distinction lies in their knowledge representation and cognitive flexibility. Adaptive experts possess knowledge characterized by organization, abstraction, and consolidation that is largely independent of situational contexts (de-contextualization) [1]. This enables them to apply known solutions to new situations more easily through analogical reasoning using their organized knowledge base [1]. Whereas routine expertise focuses primarily on procedural fluency ("knowing how"), adaptive expertise emphasizes both procedural fluency and conceptual understanding ("knowing why"), which permits adaptation to variability in novel and uncertain clinical and research situations [15].
Core Dimensions of Adaptive Expertise
Research has identified several interconnected dimensions that constitute adaptive expertise in practice:
Domain-Specific Skills: Encompassing declarative knowledge (knowing that), procedural knowledge (knowing how), and conditional knowledge (knowing when and where) [1]. Unlike novices, adaptive experts display distinctive knowledge representation in terms of extent, organization, abstraction, and consolidation, which significantly influences their problem-solving capabilities [1].
Innovative Skills: The capacity to transcend established routines and reconsider fundamental ideas, practices, and values to facilitate change [1]. This dimension involves recognizing how previously acquired knowledge can be adapted to novel circumstances, indicating that the knowledge used in innovation processes is both nuanced and complex [1].
Metacognitive Skills: The ability to "think about thinking" – to self-assess one's expertise, knowledge, learning, and problem-solving abilities [1]. While some debate exists about whether metacognitive skills definitively distinguish adaptive from routine expertise, they remain valuable for strategic learning and application of knowledge in unfamiliar contexts [1].
Table 1: Core Dimensions of Adaptive Expertise
| Dimension | Key Characteristics | Role in Adaptive Expertise |
|---|---|---|
| Domain-Specific Skills | Declarative, procedural, and conditional knowledge; de-contextualized knowledge representation | Provides foundational knowledge base organized for flexible application |
| Innovative Skills | Ability to transcend routines, reconceptualize problems, generate novel solutions | Enables creation of new approaches when standard solutions fail |
| Metacognitive Skills | Self-assessment, reflection, recognition of knowledge gaps | Supports continuous learning and strategic application of knowledge |
Measuring Adaptive Expertise in Biomedical Engineering Education
Current Measurement Instruments and Methodologies
A 2025 scoping review of measurement instruments for adaptive expertise and adaptive performance in healthcare professionals revealed 19 distinct instruments, only three of which were specifically developed for the healthcare domain [16]. These instruments can be categorized into six types: self-evaluation instruments, job requirement instruments, knowledge assessment instruments, design scenarios, mixed-methods instruments, and collegial verbalization approaches [16]. The review found a predominance of self-evaluation and job requirement instruments, while other methods such as design scenarios and mixed-methods approaches remain underrepresented despite their potential value [16].
The quality of these instruments varies significantly, with substantial differences in the nature and volume of evidence supporting their validity, reliability, and fairness according to the Standards for Educational and Psychological Testing [16]. This measurement challenge is compounded by the relationship between adaptive expertise (the internal knowledge and skills) and adaptive performance (the visible outcome of adaptive expertise), with the latter being triggered by contextual changes in tasks or environments [16].
Quantitative Assessment of Adaptive Expertise
Recent research provides quantitative insights into adaptive expertise development and its correlates. A 2024 study of health professions educators found an average adaptive expertise score of 4.18 ± 0.57 on a 5-point scale, with domain-specific and innovative skills emerging as the principal distinct dimensions [1]. Statistical analysis revealed significant correlations between adaptive expertise scores and both perceived work performance (r = 0.41, p < 0.05) and academic ranking (r = 0.42, p < 0.05) [1]. Notably, no significant associations were found between adaptive expertise scores and work experience or age, reinforcing that adaptive expertise is not automatically acquired with seniority but must be deliberately developed [1].
Table 2: Correlates of Adaptive Expertise in Health Professions Educators
| Variable | Correlation with Adaptive Expertise | Statistical Significance | Practical Implications |
|---|---|---|---|
| Work Performance | r = 0.41 | p < 0.05 | Higher adaptive expertise associates with better performance in altered environments |
| Academic Ranking | r = 0.42 | p < 0.05 | Professors show higher adaptive expertise than other ranks |
| Work Experience | No significant correlation | p > 0.05 | Expertise not automatically gained through experience alone |
| Age | No significant correlation | p > 0.05 | Not a simple function of age or maturity |
The Optimal Adaptability Corridor: Balancing Efficiency and Innovation
Conceptual Framework and Visual Representation
The Optimal Adaptability Corridor represents the target zone where professionals maintain an effective balance between efficiency and innovation. This balance enables them to apply known solutions efficiently when appropriate while also possessing the conceptual understanding and cognitive flexibility to innovate when facing novel challenges [15]. The corridor metaphor suggests there are boundaries – too much focus on efficiency leads to rigid, routine expertise, while excessive innovation without efficient implementation can lead to inconsistent outcomes.
The following diagram illustrates the conceptual relationship between key components of adaptive expertise development within the Optimal Adaptability Corridor:
Operationalizing the Balance in Educational Settings
In biomedical engineering education, maintaining the Optimal Adaptability Corridor requires deliberate pedagogical approaches that target both efficiency and innovation dimensions simultaneously. Research indicates that adaptive expertise is best developed through educational experiences that include: (a) explicit integration of clinical signs and symptoms with underlying mechanisms (asking or telling "why"), (b) exposure to meaningful variation (asking "what if" questions), and (c) leveraging struggle and discovery in learning followed by immediate feedback and consolidation [15].
This balanced approach stands in contrast to traditional biomedical engineering education that often overemphasizes efficiency and routine performance. The 5th Biomedical Engineering Educational Summit highlighted the critical need for interdisciplinary knowledge combining principles of engineering, physical sciences, and biological sciences, with an emphasis on teaching techniques that empower students with both technical prowess and critical thinking skills vital to this multifaceted discipline [17].
Implementing Adaptive Expertise Development in Biomedical Engineering Education
Curricular Strategies and Methodologies
Effective development of adaptive expertise in biomedical engineering requires implementing specific evidence-based educational strategies:
Cognitive Integration: Developing deep conceptual knowledge through explicit integration of clinical applications with underlying engineering and biological principles [15]. This approach prepares learners to deal with complexity and continue learning in future practice by understanding not just procedures but why specific approaches work.
Variation Exposure: Systematically introducing meaningful variability in problem-solving contexts through "what if" scenarios that require students to adapt solutions to changing parameters, mirroring real-world biomedical engineering challenges [15].
Struggle and Discovery: Creating controlled challenges that push students beyond routine application of formulas, followed by immediate feedback and consolidation activities [15]. This approach leverages productive failure as a mechanism for developing innovative capacity.
Interdisciplinary Collaboration: Facilitating teamwork across engineering, clinical, and biological disciplines to emulate the interprofessional networks required in modern healthcare settings [17]. The Biomedical Engineering Educational Summit emphasizes this as essential for addressing complex healthcare challenges.
Experimental Protocols for Developing Adaptive Expertise
Research-validated protocols for cultivating adaptive expertise in biomedical engineering education include:
Protocol 1: Conceptual Explanation Integration Objective: Develop dual understanding of both procedures and underlying mechanisms. Methodology: For each biomedical engineering problem solved, require students to provide both the technical solution and a detailed explanation of why the solution works, referencing fundamental principles from multiple disciplines (engineering, biology, clinical practice). Assessment: Evaluate solutions based on both technical accuracy and depth of conceptual explanation.
Protocol 2: Progressive Variation Training Objective: Build flexibility in applying knowledge to novel situations. Methodology: Present a core biomedical engineering challenge followed by a series of progressively modified scenarios with altered constraints, resources, or objectives. Require students to adapt their initial solution without complete re-learning. Assessment: Measure efficiency in initial solution and innovation in adapted solutions.
Protocol 3: Multi-perspective Problem-Framing Objective: Develop capacity to view challenges from multiple stakeholder perspectives. Methodology: Present complex biomedical problems requiring students to generate and evaluate solutions from at least three different perspectives (e.g., clinical practitioner, patient, medical device regulator, hospital administrator). Assessment: Evaluate breadth of solution options generated and capacity to articulate trade-offs across perspectives.
Research Reagent Solutions for Studying Adaptive Expertise
Table 3: Essential Methodological Tools for Adaptive Expertise Research
| Research Instrument | Primary Function | Application Context |
|---|---|---|
| Self-Evaluation Scales | Measures self-reported adaptive expertise tendencies | Initial assessment of baseline adaptive capabilities |
| Design Scenario Assessments | Presents novel problems requiring innovative solutions | Evaluation of innovation capacity under constrained conditions |
| Knowledge Assessment Tools | Measures depth and organization of conceptual knowledge | Determining cognitive foundations for adaptive performance |
| Mixed-Methods Instruments | Combines quantitative and qualitative assessment approaches | Comprehensive evaluation of adaptive expertise development |
| Collegial Verbalization Protocols | Records problem-solving discussions with colleagues | Assessment of collaborative adaptation capabilities |
Implications for Biomedical Engineering Competency Frameworks
The integration of adaptive expertise into biomedical engineering education has significant implications for competency frameworks and assessment methodologies. The CanMEDS physician competency framework has recognized the need to better incorporate adaptive expertise, with proposals for the 2025 framework including new competencies specifically addressing the balance between efficient application of known solutions and innovative generation of new approaches during patient care [15].
Similar revisions are needed in biomedical engineering competency standards to explicitly include:
- Capacity to recognize need for flexible knowledge application when facing novelty, uncertainty, and ambiguity in biomedical contexts
- Skill in approaching daily problem-solving as learning opportunities to create new knowledge embedded in practice
- Ability to integrate multiple perspectives from engineering, clinical, and biological disciplines to adaptively respond to biomedical challenges
These competencies align with the broader movement in healthcare education to prepare professionals for future learning, ensuring they can effectively address novel challenges that emerge throughout their careers from rapid technological advancements and evolving healthcare needs [17] [15].
The Optimal Adaptability Corridor provides a powerful framework for reimagining biomedical engineering education to better prepare professionals for the complex, unpredictable challenges of modern healthcare environments. By deliberately balancing efficiency and innovation through evidence-based educational strategies, educators can develop a new generation of biomedical engineers capable of both executing established procedures with precision and generating novel solutions when confronting unprecedented challenges.
Future research should focus on validating biomedical-engineering-specific assessment instruments, developing standardized metrics for tracking progress within the Optimal Adaptability Corridor, and creating targeted interventions for students struggling with either the efficiency or innovation dimensions of adaptive expertise. As biomedical technology continues its rapid advancement, this balanced approach to expertise development will become increasingly essential for ensuring that biomedical engineering education keeps pace with the evolving needs of healthcare delivery and innovation.
In biomedical engineering, adaptive expertise represents a sophisticated model of professional competence that enables experts to respond successfully to novel, complex, and uncertain situations [18] [15]. Unlike routine experts who primarily apply established procedures efficiently, adaptive experts balance efficiency with innovation, allowing them to generate novel solutions when existing knowledge proves insufficient [15] [1]. This balance is particularly critical in biomedical engineering, where professionals routinely confront problems at the interface of engineering, biology, and medicine that lack predetermined solutions [19] [5].
The foundational research of Hatano and Inagaki (1986) established adaptive expertise as a distinct form of competence characterized by the ability to apply knowledge flexibly across varying contexts [18] [1]. In biomedical engineering contexts, this translates to professionals who can not only implement existing protocols and technologies but also reformulate problems, integrate knowledge across disciplinary boundaries, and develop innovative approaches to emerging challenges in medical technology and healthcare [19] [20] [5]. This paper explores the cognitive structures and knowledge representation strategies that enable such adaptive performance, with particular emphasis on implications for biomedical engineering education and practice.
Theoretical Framework: Core Dimensions of Adaptive Expertise
Efficiency-Innovation Balance
Adaptive expertise is characterized by a dynamic balance between efficient application of existing knowledge and innovative generation of new solutions [15]. This balance enables biomedical engineers to execute established procedures with precision while remaining capable of innovating when confronted with novel problems or changing circumstances [21].
Table: Characteristics of Adaptive vs. Routine Expertise in Biomedical Contexts
| Dimension | Adaptive Expertise | Routine Expertise |
|---|---|---|
| Problem Approach | Creates new solutions for novel problems | Applies known solutions to familiar problems |
| Knowledge Structure | Flexible, conceptually organized | Rigid, procedure-based |
| Response to Novelty | Innovates and adapts | Struggles or attempts to force-fit known solutions |
| Error Handling | Treats unexpected outcomes as learning opportunities | Views deviations as failures |
| Biomedical Example | Modifies diagnostic protocol for unusual patient presentation | Strictly adheres to standard protocols regardless of fit |
Conceptual Foundations
Adaptive experts in biomedical engineering demonstrate deep conceptual understanding that enables them to adapt to variability in novel and uncertain situations [15]. This conceptual foundation allows them to understand not just what to do but why certain approaches are appropriate, permitting adaptation when standard solutions prove insufficient [15]. This deep understanding is facilitated by cognitive structures that organize knowledge in ways that emphasize conceptual relationships over surface-level features [1].
Knowledge Representation in Adaptive Expertise
Structural Characteristics of Expert Knowledge
Adaptive experts develop knowledge representations characterized by hierarchical organization, abstract conceptualization, and decontextualization of principles [1]. These structures enable flexible application of knowledge across diverse biomedical contexts:
Hierarchical Organization: Knowledge is organized around fundamental principles rather than surface features, allowing adaptive experts to recognize deep similarities between seemingly dissimilar problems [1].
Abstract Representation: Concepts are represented at theoretical levels that facilitate transfer across contexts, enabling biomedical engineers to apply engineering principles to biological systems despite surface-level differences [1] [20].
Causal Interconnectedness: Knowledge elements are richly interconnected through causal relationships, allowing adaptive experts to mentally simulate outcomes and generate novel solutions [1].
Metacognitive Components
Metacognition—"thinking about thinking"—plays a crucial role in adaptive expertise by enabling professionals to monitor their own understanding, identify knowledge gaps, and strategically deploy cognitive resources [1]. While some debate exists about whether metacognitive skills definitively distinguish adaptive from routine expertise, they undeniably support professionals in recognizing when familiar approaches are insufficient and new learning is required [1].
Experimental Approaches to Studying Knowledge Structures
Methodologies for Investigating Expert Knowledge
Research on adaptive expertise employs diverse methodologies to elucidate how experts structure their understanding:
Table: Experimental Methods for Studying Knowledge Representation
| Methodology | Application | Key Metrics | Biomedical Engineering Example |
|---|---|---|---|
| Think-Aloud Protocols | Tracing problem-solving processes | Verbalized reasoning steps, hypothesis generation | Recording experts' thoughts while designing medical devices |
| Concept Mapping | Revealing knowledge organization | Node connections, hierarchical structure, cross-links | Mapping relationships between engineering principles and biological systems |
| Comparative Case Analysis | Contrasting expert-novice differences | Problem framing, solution pathways, innovation | Comparing approaches to diagnostic technology development |
| Longitudinal Assessment | Tracking expertise development | Knowledge fluency, adaptive transfer, innovation frequency | Studying BME students throughout studio-based curriculum |
Protocol: Studio-Based Learning Assessment
The Cornell University BME Department implemented a studio-based pedagogical approach to develop adaptive expertise, using the following assessment protocol [19]:
Data Collection Instruments:
- Studio artifacts (completed worksheets documenting problem-solving processes)
- Post-studio student reflections on their learning experiences
- End-of-semester surveys with Likert-scale and open-ended questions
Analytical Framework:
- Mixed-methods approach combining quantitative and qualitative analysis
- Thematic coding of open-ended responses to identify trends
- Performance indicator rubrics to assess problem-solving proficiency
- Analysis of collaborative patterns using Google Slides/Documents platforms
Key Outcome Measures:
- Ability to formulate mathematical equations for biological systems
- Iterative refinement of solutions through repetitive practice
- Collaborative problem-solving behaviors
- Development of engineering identity
This methodology revealed that embedding studio-based learning throughout the engineering curriculum—rather than as standalone courses—offered a transformative approach to developing engaged and adaptable biomedical engineers [19].
Interdisciplinary Integration in Biomedical Contexts
Disciplinary Perspectives Framework
Biomedical engineering inherently requires integration of knowledge across multiple disciplines, creating unique challenges for knowledge representation. Adaptive expertise in this field involves recognizing and navigating different disciplinary perspectives—the distinct ways experts from various fields approach problems based on their training and epistemological frameworks [20].
A framework developed to make these perspectives explicit includes analyzing [20]:
- Epistemological commitments: What counts as knowledge in different disciplines
- Characteristic methods: Preferred approaches to investigation and validation
- Conceptual frameworks: Foundational theories and models
- Success criteria: How solutions are evaluated within each discipline
Knowledge Integration Processes
Adaptive experts employ distinctive processes for integrating knowledge across disciplinary boundaries:
Educational Implications and Development Strategies
Cultivating Adaptive Expertise in BME Education
Research indicates that adaptive expertise does not automatically develop with experience alone but requires deliberate educational approaches [1]. Effective strategies include:
Studio-Based Learning: Embedding iterative problem-solving with immediate feedback throughout the curriculum, not just in capstone courses [19]
Work-Based Learning: Providing experiences with challenging, ill-structured real-world problems in safe learning environments [18]
Cognitive Integration: Explicitly connecting clinical signs and symptoms with underlying engineering and biological mechanisms [15]
Variation Exposure: Presenting problems with meaningful variation to develop flexible application of principles [15]
The NICE Strategy for BME Education
The NICE strategy represents a comprehensive approach to developing adaptive expertise in biomedical engineering education [22]:
- New Frontier: Engaging students with cutting-edge research and emerging technologies using AI tools for literature analysis
- Integrity: Case-based learning examining both successful scientific endeavors and ethical failures like the Theranos case
- Critical and Creative Thinking: Peer review exercises and case discussions requiring analysis from multiple perspectives
- Engagement: Direct involvement with clinical doctors and industry partners in product development projects
This approach aligns with constructivist learning principles and problem-based learning methodologies, creating the variation and challenge necessary for developing adaptive expertise [22].
Research Reagent Solutions: Tools for Investigating Knowledge Structures
Table: Key Methodological Approaches for Studying Knowledge Representation
| Research Approach | Primary Function | Application Context | Key Considerations |
|---|---|---|---|
| Concept Mapping Software | Visualizing knowledge structures | Identifying organizational patterns in expert vs. novice knowledge | Requires training for consistent application; analysis can be time-intensive |
| Verbal Protocol Analysis | Capturing real-time problem-solving processes | Studying reasoning patterns during biomedical design tasks | May alter natural thinking processes; complex to code and analyze |
| Eye-Tracking Systems | Identifying information attention patterns | Tracing expert-novice differences in interpreting medical data | Requires specialized equipment; data richness necessitates sophisticated analysis |
| fMRI and Neuroimaging | Revealing neural correlates of expertise | Studying brain activity during innovative problem-solving | High cost limits sample sizes; inferring cognitive processes from activation patterns |
| Longitudinal Assessment Tools | Tracking expertise development over time | Evaluating educational interventions in BME programs | Requires sustained participant engagement; challenging to control confounding variables |
Adaptive expertise in biomedical engineering emerges from distinctive knowledge representation structures that enable professionals to balance efficient application of existing knowledge with innovative generation of new solutions. These cognitive structures are characterized by hierarchical organization, abstract representation, causal interconnectedness, and well-developed metacognitive awareness. The development of such expertise requires educational approaches that systematically foster conceptual understanding alongside procedural fluency, while creating opportunities for interdisciplinary integration and iterative problem-solving with authentic challenges.
Future research should further elucidate the specific mechanisms through which biomedical engineers restructure their knowledge throughout professional development, and how educational experiences can optimally support this process. Particularly as the field confronts increasingly complex challenges at the interface of engineering, biology, and medicine, fostering adaptive expertise becomes essential to preparing biomedical engineers who can not only implement existing solutions but also generate novel approaches to emerging healthcare challenges.
Educational Innovations: Implementing Adaptive Learning Strategies in BME Curricula
Biomedical engineering (BME) sits at the intersection of engineering, biology, and medicine, preparing graduates to tackle urgent healthcare challenges through innovations in medical technologies, diagnostics, and AI-powered tools [23]. The growing demand for more efficient, timely, and safer health services, together with insufficient resources, has created unprecedented pressure on health systems worldwide, generating new opportunities to improve and optimize healthcare services from a transdisciplinary perspective [24]. This approach transcends traditional academic disciplinary boundaries, drawing from diverse fields like biology, engineering, computer science, data analytics, and even social sciences to address multifaceted healthcare challenges [25]. Unlike multidisciplinary or interdisciplinary approaches that maintain disciplinary boundaries while collaborating, transdisciplinarity involves transcending these boundaries to create entirely new approaches and frameworks for solving complex problems [25].
This whitepaper frames transdisciplinary education within the broader context of adaptive expertise development in biomedical engineering education research. Adaptive expertise refers to the ability to use knowledge and experience in a domain to learn in unanticipated situations, differing from routine expertise which involves appropriately using knowledge to solve routine problems [10] [26]. This framework is directly applicable in the context of design and innovation given the emphasis on how one develops adaptiveness in learning and how to apply knowledge fluidly when faced with novel, ambiguous situations characteristic of healthcare challenges [26]. The very nature of design requires one to recognize how prior knowledge might apply under new circumstances, making adaptive expertise particularly relevant for biomedical engineers who must navigate rapidly evolving technological landscapes and complex healthcare systems [10].
Theoretical Foundations: Connecting Transdisciplinarity and Adaptive Expertise
The Conceptual Framework
The relationship between transdisciplinary education and adaptive expertise development forms a reinforcing cycle that prepares biomedical engineers for complex, real-world challenges. Transdisciplinary learning experiences, particularly those grounded in experiential learning models, provide the ideal context for developing adaptive expertise by regularly placing students in situations where they must integrate and apply knowledge from diverse domains to novel problems.
Table 1: Core Dimensions of Transdisciplinary Education in BME
| Dimension | Traditional Approach | Transdisciplinary Approach | Adaptive Expertise Development |
|---|---|---|---|
| Knowledge Structure | Siloed disciplines with clear boundaries | Integrated knowledge ecosystems | Promotes cross-boundary thinking and knowledge fluidity |
| Problem-Framing | Well-defined problems within single disciplines | Ill-structured, complex real-world problems | Enhances ability to define problems in novel contexts |
| Solution Pathways | Standardized methods and approaches | Innovative, co-created solutions | Fosters innovative thinking and methodological flexibility |
| Stakeholder Engagement | Limited to disciplinary experts | Active collaboration with clinicians, patients, engineers, biologists | Develops communication skills across diverse perspectives |
| Assessment | Discipline-specific knowledge recall | Ability to integrate and apply knowledge in novel situations | Measures transfer of learning to unfamiliar domains |
This framework is supported by Kolb's experiential learning cycle, which provides a foundation for designing transdisciplinary learning experiences. The cycle consists of four stages: concrete experience (engaging in a hands-on activity), reflective observation (reviewing what happened), abstract conceptualization (drawing conclusions and forming generalizations), and active experimentation (applying learning to new situations) [24]. This iterative process naturally cultivates adaptive expertise by continually challenging students to modify their approaches based on reflection and conceptualization [24] [26].
Visualizing the Transdisciplinary Learning Framework
The following diagram illustrates the continuous cycle of transdisciplinary learning and adaptive expertise development:
Methodological Approaches: Implementing Transdisciplinary Education
Experiential Learning in Healthcare Contexts
A significant implementation of transdisciplinary education involves creating relevant learning experiences for biomedical engineering students to expand their knowledge and skills in improving and optimizing hospital and healthcare processes [24]. In one documented approach, healthcare processes were translated into specific learning experiences using the Analysis, Design, Development, Implementation, and Evaluation (ADDIE) model [24]. This model systematically identified the learning context, new concepts and skills to be developed, stages of the student's learning journey, required resources, and assessment methods.
The learning journey was structured around Kolb's experiential learning cycle in a 16-week elective course on hospital management for last-year biomedical engineering undergraduate students [24]. Students engaged in analyzing and redesigning healthcare operations for improvement and optimization using tools drawn from industrial engineering, which expanded their traditional professional role. The fieldwork occurred in two large hospitals and a university medical service, where students observed relevant healthcare processes, identified problems, and defined improvement and deployment plans [24].
Table 2: Experimental Protocol for Transdisciplinary Healthcare Optimization Course
| Phase | Duration | Activities | Tools & Methods | Stakeholders Involved |
|---|---|---|---|---|
| Context Analysis | Weeks 1-3 | Hospital immersion, process mapping, problem identification | Observational studies, stakeholder interviews, value stream mapping | Clinical engineers, physicians, nurses, administrators |
| Solution Design | Weeks 4-8 | Brainstorming interventions, prototyping solutions, feasibility analysis | Root cause analysis, simulation modeling, lean principles | Industrial engineers, systems analysts, clinical staff |
| Implementation Planning | Weeks 9-12 | Developing deployment strategies, contingency planning, metrics definition | Project management tools, change management models, performance dashboards | Hospital administrators, quality improvement teams |
| Evaluation & Reflection | Weeks 13-16 | Piloting solutions, measuring outcomes, reflective practice | Statistical analysis, cost-benefit assessment, portfolio development | Patients, clinical teams, engineering faculty |
Adaptive Expertise Assessment Protocols
Measuring the development of adaptive expertise requires specialized assessment strategies that go beyond traditional knowledge recall. Research based on the How People Learn (HPL) framework has demonstrated effective methods for cultivating and assessing adaptive expertise in biomedical engineering education [10].
In one experimental protocol, undergraduate bioengineering students learned about ethics for stem cell research using the HPL method of instruction, which was compared to a control group that learned through a standard lecture sequence [10]. Both groups learned the factual material equally well, but the HPL group demonstrated superior adaptive expertise when presented with novel ethical dilemmas, showing greater preparedness to act adaptively in unfamiliar situations [10].
The key methodological components for developing adaptive expertise include:
- Problem-based learning with increasingly complex and ill-structured problems
- Deliberate practice with varied cases that require different solution approaches
- Metacognitive scaffolding that prompts students to reflect on their problem-solving strategies
- Formative feedback focused on reasoning processes rather than just solutions
- Assessment transfers that evaluate application of knowledge to novel contexts [10] [26]
Case Studies and Applications
Real-World Implementations and Outcomes
Several institutions have successfully implemented transdisciplinary educational approaches with documented outcomes. Cornell's Meinig School of Biomedical Engineering has embarked on a comprehensive curriculum redesign that embeds design thinking, active learning, and flipped classroom models throughout their programs [23]. Their initiatives include restructuring introductory courses, experiential learning seminar sequences, and senior design capstones, supported by modular online content that now serves over 175 students annually across programs [23]. These efforts also include clinical immersion experiences and partnerships with other universities, creating authentic transdisciplinary learning environments.
In another implementation, physician-scientist Dr. Wilbur Lam exemplifies transdisciplinary practice by merging pediatrics, biomedical engineering, and innovation to advance patient care [27]. His work includes developing a non-invasive smartphone application for anemia patients that uses image-based algorithms to determine hemoglobin levels by analyzing pictures of fingernails [27]. This innovation required deep integration of clinical knowledge, biomedical sensing, software engineering, and user-centered design—a truly transdisciplinary endeavor that has translated into tangible patient benefits.
Research Reagent Solutions: Transdisciplinary Toolkit
Table 3: Essential Research Reagents for Transdisciplinary BME Education
| Reagent Category | Specific Examples | Function in Transdisciplinary Research |
|---|---|---|
| Computational Modeling Tools | MATLAB, COMSOL, ANSYS | Simulate biological and engineering systems; enable in-silico testing of hypotheses and device designs |
| Cell Culture Systems | Endothelial cell cultures, microfluidic cell platforms | Study cell interactions in controlled microenvironments; bridge biology with engineering principles |
| Clinical Data Platforms | Electronic Health Records (EHR), medical imaging archives | Provide real-world clinical context; enable data-driven healthcare solutions |
| Prototyping Technologies | 3D bioprinters, microfabrication equipment | Create physical prototypes of medical devices; iterate designs based on biological constraints |
| Sensor Integration Systems | Arduino, Raspberry Pi, LabVIEW | Develop custom sensing solutions for physiological monitoring; bridge hardware and software |
| Data Analysis Frameworks | Python, R, TensorFlow | Process complex biological and clinical datasets; implement machine learning algorithms |
| 1,1-Dibromo-3,3-dichloroacetone | 1,1-Dibromo-3,3-dichloroacetone, CAS:62874-83-3, MF:C3H2Br2Cl2O, MW:284.76 g/mol | Chemical Reagent |
| Oleaside A | Oleaside A, MF:C30H44O7, MW:516.7 g/mol | Chemical Reagent |
Implementation Challenges and Solutions
Despite the clear benefits, implementing transdisciplinary education faces significant challenges. These include the complexity of biomedical systems, diversity of topics in biomedical engineering, difficulties in curriculum development, need for dedicated teaching facilities and additional resources, challenges in student assessment, communication barriers between disciplines, faculty hiring difficulties, and accreditation alignment issues [25].
Specific implementation challenges and mitigation strategies include:
Resource Intensity: Transdisciplinary education requires significant resources and faculty with diverse backgrounds. Solution: Create transdisciplinary hubs that leverage combined strengths of multiple institutions and departments [25].
Curriculum Integration: Balancing core disciplinary competencies with transdisciplinary integration. Solution: Implement a phased approach where foundational years focus on core disciplines while advanced years incorporate transdisciplinary projects [25].
Assessment Complexity: Traditional assessment methods may not capture transdisciplinary learning outcomes. Solution: Develop innovative assessment techniques focused on adaptive expertise and transfer of learning [10].
Faculty Development: Existing faculty may lack transdisciplinary training. Solution: Provide professional development opportunities and create team-teaching models that combine expertise from multiple departments [24].
The transformation toward transdisciplinary education, while challenging, presents an opportunity for institutions to collaborate and share resources rather than being seen as an insurmountable obstacle [25]. As the field continues to evolve, the traditional disciplinary education of biomedical engineering may prove inadequate for preparing students to address future healthcare challenges that inherently cross disciplinary boundaries [25].
Visualizing the Transdisciplinary Innovation Workflow
The following diagram maps the workflow for transdisciplinary innovation in biomedical engineering, from problem identification to solution implementation:
Transdisciplinary education represents a paradigm shift in biomedical engineering education, moving beyond the multi and interdisciplinary approaches that have characterized the field historically. When framed within the context of adaptive expertise development, transdisciplinary learning experiences prepare students not merely to solve known problems efficiently, but to adapt and innovate when confronting novel, complex challenges at the intersections of engineering, biology, and clinical practice [25] [10] [26].
The future of biomedical engineering education will likely see increased emphasis on concepts such as non-invasive monitoring of physiological signals, wearable technologies, point-of-care diagnostics, and home-based healthcare solutions [27]. These emerging areas inherently require transdisciplinary approaches that integrate engineering innovation with deep clinical understanding and biological insights. Furthermore, as artificial intelligence and machine learning continue to transform healthcare, biomedical engineers will need to bridge these technological capabilities with clinical workflows and ethical considerations [23].
While implementation challenges remain, the evidence suggests that transdisciplinary approaches hold significant promise for advancing biomedical engineering education and preparing the next generation of innovators to tackle complex healthcare challenges [24] [25]. By deliberately designing educational experiences that transcend traditional disciplinary boundaries and foster adaptive expertise, educators can equip biomedical engineering students with the skills, mindsets, and approaches needed to make meaningful contributions to 21st-century healthcare.
The evolving challenges in healthcare demand a new kind of engineer—one who is not only technically proficient but also capable of innovating in the face of novel, complex problems. Adaptive expertise is the framework that enables professionals to respond to novel or unexpected situations more effectively, efficiently, and innovatively than routine experts, who may struggle when faced with unfamiliar challenges [1]. In Biomedical Engineering (BME) education, the development of adaptive expertise is paramount for preparing graduates to tackle urgent, real-world healthcare challenges [23].
Clinical immersion and simulation are powerful pedagogical tools for bridging the gap between theoretical knowledge and practical application. These experiences expose students to the authentic, often ambiguous, clinical environment, forcing them to move beyond routine problem-solving. By engaging directly with clinicians and patients, students learn to identify unmet needs, understand complex clinical workflows, and appreciate the human-centric nature of medical technology design [28] [29]. This process cultivates the essential components of adaptive expertise: deep conceptual understanding, cognitive flexibility, and innovative problem-solving skills [26].
Theoretical Foundation: The Pillars of Adaptive Expertise
Adaptive expertise is conceptualized not as a single skill, but as a multi-faceted construct. Its development is crucial for navigating the non-standardized and rapidly changing landscape of clinical medicine and healthcare technology.
Core Dimensions of Adaptive Expertise
Research has identified several key dimensions that distinguish adaptive experts from routine experts [1]:
- Domain-Specific Skills: This encompasses more than just factual knowledge (
knowing that). It includes procedural knowledge (knowing how) and conditional knowledge (knowing when and why). Adaptive experts organize their knowledge in abstract, de-contextualized structures, allowing for flexible application in new situations [1]. - Innovative Skills: This dimension involves the ability to transcend established routines and devise novel solutions when no precedents exist. It requires a balance between efficiency in known tasks and the innovation necessary for unfamiliar challenges [1] [26].
- Metacognitive Skills: Often described as 'thinking about thinking,' this is the capacity for self-assessment. It allows individuals to understand the limits of their knowledge, monitor their learning, and strategically apply their skills in unfamiliar contexts [1].
A 2024 study among health professions educators found that domain and innovative skills are the principal distinct dimensions of adaptive expertise. The research revealed a statistically significant correlation between adaptive expertise scores and work performance (r = 0.41, p < 0.05), underscoring its practical importance. Furthermore, it demonstrated that adaptive expertise is not automatically acquired with seniority, but must be deliberately developed [1].
Table 1: Contrasting Routine and Adaptive Expertise
| Feature | Routine Expert | Adaptive Expert |
|---|---|---|
| Knowledge Application | Efficient in well-known contexts | Flexible and fluid in novel situations |
| Problem-Solving | Relies on established procedures | Innovates and develops new methods |
| Knowledge Structure | Context-bound | Abstract and de-contextualized |
| Response to Change | May struggle | Adapts and overcomes uncertainty |
The Role of Design and Innovation
The process of engineering design is inherently novel and ambiguous, making it an ideal venue for fostering adaptive expertise. Every design project requires individuals to recognize how prior knowledge might apply under new circumstances [26]. Clinical immersion embeds students in this process, requiring them to:
- Frame ill-structured problems where the task, method, and desired outcome are not known in advance.
- Engage in analogical reasoning, applying organized knowledge bases to new clinical scenarios.
- Develop knowledge fluency, enabling them to transfer and apply learning fluidly from the classroom to the clinical setting [26].
Implementing Clinical Immersion for Adaptive Learning
Structured clinical immersion programs are being integrated into BME curricula through various models, from intensive summer programs to semester-long courses. These programs are designed to move students along the spectrum from routine to adaptive expertise.
Program Structures and Models
Successful clinical immersion programs share key elements that promote adaptive learning. An analysis of multiple programs identified five interconnected, essential components [29]:
- Immersion Partner Collaboration: Strong commitment from clinical partners and faculty is vital for success.
- Team-Based Immersion Experiences: Students work in transdisciplinary teams, often including industrial design or other majors.
- Needs-Finding Emphasis: The primary focus is on observing and identifying unmet clinical needs, not jumping to solutions.
- Team-Based Engineering Design: Immersion is linked to the design process, often within a capstone course.
- Immersion Assessment and Evaluation: Robust methods are used to evaluate student learning and program effectiveness [29].
Programs like the one at Rice University, the Co-Production Healthcare Innovation Program (CHIP), employ an eight-week full-time immersive model where students observe complex clinical environments at partner hospitals to identify unmet healthcare needs and explore solutions with a human-centered approach [28]. Alternatively, the "Needs Identification in Healthcare" course described in the research is a semester-long technical elective that combines classroom lectures with 4-5 clinical immersion days throughout the semester, allowing students to engage with the clinical environment while simultaneously learning the theoretical frameworks for needs-finding [29].
The Clinical Immersion Workflow: From Observation to Innovation
The following diagram illustrates the core iterative process that students undergo during clinical immersion, which is designed to cultivate adaptive expertise by challenging them to navigate ambiguity and reframe problems.
Figure 1: The Clinical Immersion Learning Cycle
This workflow is fundamentally different from traditional, linear engineering education. As one program director notes, "I encourage them not to only ask, 'How can I solve this problem?' but also, 'How does this affect the patients and their experience?'" [28]. This shift in questioning is a hallmark of adaptive, human-centered design thinking.
Quantitative Assessment of Immersion Programs
The effectiveness of clinical immersion is measured through both quantitative and qualitative means. The data below summarizes assessment findings from recent research, highlighting the positive impact on key learning outcomes.
Table 2: Assessment Metrics and Outcomes from BME Clinical Immersion Programs
| Assessment Focus | Methodology | Key Findings |
|---|---|---|
| Adaptive Expertise Development | Self-reported survey on adaptive expertise dimensions (5-point scale) [1] | Average adaptive expertise score of 4.18 ± 0.57, correlating with work performance (r=0.41, p<0.05) [1]. |
| Program Impact on Student Learning | Quantitative and qualitative surveys on problem-solving, communication, and teamwork [29] | High student appreciation for the experience; self-reported increased knowledge in needs identification, team-based problem-solving, and confidence [29]. |
| Human-Centered Design Skills | Analysis of student reflections and project outcomes [28] | Students demonstrated a shift towards humanistic perspectives, focusing on the root causes of problems and patient experience [28]. |
| Impact on Career Trajectory | Student self-reporting on perspective and career path influence [28] | Students reported transformative experiences and perspective shifts influencing their future work in bioengineering [28]. |
Implementing a successful clinical immersion program requires careful planning and specific resources. The following table details key components necessary for establishing and running these educational experiences, drawing from documented programs and funding guidelines.
Table 3: Essential Resources for Clinical Immersion Programs
| Resource Category | Specific Items/Functions | Purpose in Clinical Immersion |
|---|---|---|
| Funding & Financial Support | NIBIB R25 grants (e.g., up to $40,000/year with clinical immersion) [30] | Supports parts, supplies, prototyping, student summer salaries, and program coordination. |
| Clinical Partnership Framework | Agreements with VA hospitals, military hospitals, children's hospitals [28] [29] | Provides access to clinical environments, patients, and clinician mentors for authentic immersion. |
| Prototyping & Technical Support | Machine shop access, 3D printers, prototyping budgets [30] | Enables students to create physical models and prototypes of potential solutions identified during immersion. |
| Educational Frameworks | Stanford Biodesign process, Contextual Inquiry methods [29] | Provides structured methodologies for needs-finding, observation, and needs statement development. |
| Stakeholder Engagement Tools | Interview guides, patient interaction protocols, clinical etiquette training [29] | Facilitates effective and respectful communication with clinicians, patients, and other stakeholders. |
Clinical immersion and simulation represent a paradigm shift in biomedical engineering education, moving beyond the transmission of static knowledge towards the deliberate cultivation of adaptive expertise. By immersing students in the complex, often messy reality of clinical practice, these experiences foster the cognitive flexibility, innovative capacity, and metacognitive skills essential for tackling unforeseen healthcare challenges.
The evidence shows that adaptive expertise is not a byproduct of traditional lecture-based learning or even general experience; it must be intentionally developed through pedagogical designs that present students with novel problems and require them to engage in deep, conceptual thinking [1]. Clinical immersion is such a design. It forces students to reframe problems, not just solve them, and to integrate technical knowledge with human-centered empathy [28].
As the field advances, the continued refinement and assessment of these immersive experiences will be critical. The future of biomedical innovation depends on engineers who are not just routine technicians but adaptive innovators, capable of bridging theory and practice to develop technologies that truly meet the needs of patients and clinicians.
Biomedical engineering is a highly interdisciplinary field characterized by the pursuit of innovative engineering solutions for clinical applications. Over the past decade, this field has witnessed remarkable growth, driven by an aging global population, the consequences of the COVID-19 pandemic, and the advent of novel treatment modalities that have created an urgent need for more sophisticated diagnostic tools [31]. However, traditional educational models have struggled to keep pace with these rapid advancements, creating significant gaps between academic preparation and real-world demands.
Current biomedical engineering curricula often overemphasize fundamental principles while lacking coverage of emerging technologies such as AI-driven protein folding prediction, miRNA-based therapies, mRNA vaccines, CRISPR gene-editing technology, digital PCR, nanopore sequencing, and single-cell analysis technologies [31]. This curriculum gap leaves graduates underprepared for either advanced research or industrial careers. Additionally, challenges persist in ethical training, development of critical thinking skills, and practical clinical integration [31].
The NICE strategy represents a comprehensive educational framework designed to address these multi-faceted challenges through four interconnected components: New frontier, Integrity, Critical and creative thinking, and Engagement. Implemented in the "Medical Diagnostic Frontier Technology and Innovation Applications" course for senior undergraduate students, this approach has demonstrated significant success in preparing students for the complex demands of the biomedical engineering landscape [31].
Theoretical Foundations: The NICE Framework and Adaptive Expertise
The Conceptual Framework of NICE
The NICE strategy is built upon a structured framework that aligns with contemporary educational theories, particularly those related to adaptive expertise development. Adaptive expertise enables professionals to respond to novel situations more effectively and innovatively than routine experts, who may excel in standard situations but struggle with novel problems [1]. This distinction is particularly crucial in biomedical engineering, where professionals continually face evolving technological and clinical challenges.
The theoretical foundations of the NICE strategy are deeply rooted in established pedagogical frameworks. The "engagement" and "critical thinking" components align with constructivist learning principles, emphasizing active knowledge construction through hands-on projects and collaborative problem-solving [31]. This approach mirrors Kolb's experiential learning cycle, where students engage in concrete experiences, reflective observation, abstract conceptualization, and active experimentation. The case-based methodology for teaching integrity and critical thinking reflects problem-based learning (PBL), fostering ethical reasoning and analytical skills through immersion in real-world dilemmas [31].
Adaptive vs. Routine Expertise in Biomedical Engineering
Table 1: Comparison of Routine Expertise and Adaptive Expertise
| Dimension | Routine Expertise | Adaptive Expertise |
|---|---|---|
| Knowledge Application | Efficient execution of well-established procedures | Flexible application and adaptation of knowledge to novel situations |
| Problem-Solving Approach | Relies on previous experience with similar problems | Develops innovative solutions for unprecedented challenges |
| Knowledge Structure | Context-dependent knowledge organization | De-contextualized, abstract knowledge representation |
| Metacognitive Skills | Limited self-assessment capabilities | Strong ability to self-assess knowledge and identify gaps |
| Response to Change | Struggles with unexpected situations | Adapts quickly to new requirements and constraints |
Adaptive expertise represents a set of skills or dispositions, influenced by cognitive, motivational, and personality factors, that enables individuals to devise and implement new solutions effectively through a deep conceptual understanding of the problem's nature and context [1]. In contrast to routine experts who demonstrate speed and accuracy in solving familiar problems, adaptive experts exhibit cognitive flexibility and superior problem-solving skills when confronting novel situations [1].
Research has demonstrated significant correlations between adaptive expertise scores and work performance (r = 0.41, p < 0.05) as well as academic ranking (r = 0.42, p < 0.05) among health professions educators [1]. Interestingly, adaptive expertise scores were not associated with work experience or age, suggesting that adaptive expertise is not automatically acquired with seniority but must be developed deliberately through targeted educational approaches [1].
Diagram 1: Theoretical framework linking educational challenges to adaptive expertise development through the NICE strategy
Core Components of the NICE Strategy: Methodology and Implementation
New Frontier (N): Engaging with Emerging Technologies
The "New Frontier" component addresses the critical gap in exposure to cutting-edge advancements in biomedical engineering. This element focuses on immersing students in the latest technological developments from both academia and industry while sensitizing them to unmet clinical needs [31].
Implementation Methodology:
- Current Literature Analysis: Students are required to read and analyze research articles published within the past two years, ensuring exposure to the most recent developments in the field. Following reading, students summarize related articles and present findings orally in class to develop literature review, critical analysis, and communication skills [31].
- AI Tool Integration: Recognizing that undergraduate students often struggle with searching for and understanding scientific publications, the strategy incorporates AI-based tools including DeepSeek, ChatGPT, and Kimi. These tools assist students in literature search, summarization, and clarification of complex concepts [31].
- Emerging Technology Modules: Specific modules focus on revolutionary technologies such as AI-driven protein folding prediction, miRNA-based therapies, mRNA vaccines, CRISPR gene-editing, digital PCR, nanopore sequencing, and single-cell analysis technologies that have been successfully commercialized [31].
Integrity (I): Foundations of Ethical Practice
The "Integrity" component serves as the ethical core of the NICE strategy, recognizing that biomedical engineering graduates will likely engage in research and development of methods and products for human use, where maintaining the highest standards of integrity is non-negotiable [31].
Implementation Methodology:
- Case-Study Approach: Integrity is taught through analysis of both positive and negative real-world examples. Positive cases include experiences of renowned scientists and faculty members who demonstrate innovation, perseverance, and hard work in scientific research [31].
- Positive Exemplars: Stories of international collaborations such as the Human Genome Project are presented to illustrate the cooperative spirit in scientific research, demonstrating how global teams work toward common goals [31].
- Negative Case Analysis: The Theranos fraud case is thoroughly analyzed to demonstrate unethical practices such as false claims about diagnostic test accuracy. This serves to clearly demarcate boundaries of acceptable behavior in biomedical research and development [31].
- Ethical Frameworks: Students receive training on ethical considerations including patient privacy, proper use of medical data, and social responsibility, preparing them for complex ethical dilemmas in their careers [31].
Critical and Creative Thinking (C): Developing Analytical Capabilities
The "Critical and Creative Thinking" component addresses the essential complementary processes of analysis and innovation. Critical thinking provides the analytical framework needed to evaluate and refine creative ideas, while creative thinking pushes boundaries by generating novel solutions [31].
Implementation Methodology:
- Case-Based Discussions: Students engage with real-world cases related to biomedical engineering, such as the development of a new drug or ethical implications of a new medical device. They analyze these cases from multiple perspectives including technical, ethical, social, and economic aspects [31].
- Peer Review Integration: During individual oral presentations, students present content from selected research papers while providing their own insights, judgments, and critiques. Other students function as peer reviewers, evaluating presentations based on predefined criteria such as clarity, depth of analysis, and validity of conclusions [31].
- Creative Problem-Solving Sessions: Structured sessions challenge students to generate novel solutions to complex biomedical engineering problems, emphasizing analogical reasoning and application of knowledge across different contexts [31].
Engagement (E): Clinical and Industrial Integration
The "Engagement" component addresses the critical lack of practical integration in traditional biomedical engineering curricula by actively involving students in clinical and industrial settings, providing hands-on experience that enhances technical skills and builds professional networks [31].
Implementation Methodology:
- Expert Instruction: Clinical doctors and company R&D directors are invited to teach product development sections of the course, bringing real-world experience and industry-specific knowledge [31].
- Industry-Sponsored Projects: Companies provide objectives for student group projects, where teams of three to five students develop design and development plans for novel clinical products [31].
- Clinical Need Identification: Students conduct interviews with clinical doctors to identify unmet clinical needs, then work with industrial mentors to translate these needs into viable product designs [31].
- Interdisciplinary Collaboration: Mirroring successful approaches from other institutions, engineering students partner with nursing students in clinical settings, exposing them to simulation scenarios and real-world clinical environments to identify unmet needs and propose engineering solutions [32].
Diagram 2: Implementation methodology for the four components of the NICE strategy
Quantitative Outcomes and Efficacy Measures
Educational Outcome Assessment
Table 2: Quantitative Assessment of NICE Strategy Implementation Outcomes
| Evaluation Metric | Pre-Implementation Baseline | Post-Implementation Results | Change Measure |
|---|---|---|---|
| Student Satisfaction | Not reported | Significant improvement | Positive trend over 3-year period [31] |
| Knowledge of Emerging Technologies | Limited to textbook content | Enhanced understanding of AI, CRISPR, mRNA technologies | Qualitative improvement [31] |
| Ethical Decision-Making | Theoretical understanding | Case-based application skills | Enhanced practical application [31] |
| Critical Thinking Skills | Traditional problem-solving | Innovative solution generation | Improved analytical capabilities [31] |
| Industry Preparedness | Limited clinical exposure | Practical product development experience | Significant enhancement [31] |
Implementation of the NICE strategy in the "Medical Diagnostic Frontier Technology and Innovation Applications" course has demonstrated substantial positive impacts based on comparison of student performance before and after course reform over a three-year period [31]. While specific numerical data requires consultation of original sources, the results have been remarkably positive across multiple dimensions of student learning and professional development [31].
The program has served more than 200 students over the past five years, providing a substantial sample size for evaluating effectiveness [31]. The strategy's success aligns with research on adaptive expertise, which shows that targeted educational approaches can significantly enhance professionals' abilities to handle novel situations and unexpected challenges in their field [1].
Adaptive Expertise Development Metrics
Research on adaptive expertise in health professions education provides valuable metrics for assessing the development of these crucial skills. In a study of health professions educators, the average adaptive expertise score was 4.18 ± 0.57 on a scale from 1 (low) to 5 (high), with professors showing higher adaptive expertise scores than other ranks [1]. The domain and innovative skills were identified as the principal distinct dimensions of adaptive expertise among health professions educators [1].
The correlation between adaptive expertise scores and perceived work performance (r = 0.41, p < 0.05) demonstrates the tangible impact of these skills on professional effectiveness [1]. This relationship underscores the value of educational approaches like the NICE strategy that specifically target the development of adaptive expertise rather than relying on knowledge acquisition alone.
Experimental Protocols and Implementation Guidelines
Protocol 1: AI-Enhanced Literature Analysis
Objective: Develop students' ability to engage with cutting-edge research using artificial intelligence tools.
Materials and Methods:
- AI Tools: Provide access to DeepSeek, ChatGPT, and Kimi for literature search and analysis
- Current Literature: Identify research articles published within the past two years relevant to course materials
- Analysis Framework: Develop structured templates for article summarization and critique
Procedure:
- Students select 3-5 related research articles on emerging biomedical technologies
- Use AI tools to assist in initial literature search and identification of relevant publications
- Apply AI summarization features to gain initial understanding of complex articles
- Conduct deep reading and analysis without AI assistance to develop critical understanding
- Prepare structured summaries highlighting research objectives, methodology, results, and limitations
- Present findings orally in class, emphasizing personal insights and critiques
- Engage in peer review sessions using predefined evaluation criteria
Assessment: Evaluate based on depth of analysis, quality of insights, effectiveness of AI tool use, and communication clarity.
Protocol 2: Clinical Need Identification and Product Design
Objective: Develop students' ability to identify unmet clinical needs and translate them into engineering solutions.
Materials and Methods:
- Clinical Access: Arrange visits to clinical settings including surgery suites, emergency departments, and therapy clinics
- Industry Mentors: Engage company R&D directors to provide guidance and feedback
- Project Framework: Develop structured protocols for need identification and solution development
Procedure:
- Form interdisciplinary teams of 3-5 students including both engineering and nursing students when possible
- Conduct clinical observations with specific focus on workflow challenges and technology limitations
- Interview clinical practitioners regarding unmet needs and potential improvements
- Identify three specific unmet needs with potential for engineering solutions
- Conduct feasibility analysis considering technical, regulatory, and economic factors
- Select one need for further development based on impact and feasibility
- Develop detailed product design and development plan
- Present proposed solution to industry mentors and clinical practitioners for feedback
Assessment: Evaluate based on clinical relevance of identified needs, feasibility of proposed solution, quality of design plan, and effectiveness of interdisciplinary collaboration.
Table 3: Research Reagent Solutions for Biomedical Engineering Education
| Resource Category | Specific Examples | Function in Educational Context |
|---|---|---|
| AI Literature Tools | DeepSeek, ChatGPT, Kimi | Assist students in literature search, summarization, and clarification of complex concepts in emerging technologies [31] |
| Simulation Equipment | Nursing mannequins, clinical scenario equipment | Provide realistic clinical environments for identifying technological challenges and developing improvement strategies [32] |
| Case Study Materials | Theranos fraud documentation, Human Genome Project records, ethical dilemma scenarios | Facilitate analysis of both positive and negative examples to develop ethical reasoning and integrity [31] |
| Clinical Access | Hospital partnerships, clinical observation opportunities, surgeon collaborations | Enable direct exposure to real-world clinical settings and unmet medical needs [31] [32] |
| Industry Connections | Company R&D directors, product development mentors, industry project sponsors | Provide practical guidance on product development processes and industry requirements [31] |
| Assessment Tools | Adaptive expertise measurement instruments, critical thinking evaluation rubrics | Quantify development of adaptive expertise and critical thinking capabilities [1] |
The NICE strategy represents a comprehensive educational framework that effectively addresses the critical gaps in traditional biomedical engineering education. By systematically integrating New frontier exploration, Integrity development, Critical and creative thinking cultivation, and practical Engagement, this approach successfully bridges the divide between academic preparation and real-world professional demands.
The strategy's effectiveness is demonstrated through improved student outcomes across multiple dimensions, including enhanced understanding of emerging technologies, stronger ethical reasoning capabilities, superior critical thinking skills, and better preparation for industrial and clinical environments [31]. These improvements directly contribute to the development of adaptive expertise - the ability to effectively confront novel situations and generate innovative solutions that is increasingly essential in the rapidly evolving field of biomedical engineering [1].
For researchers, scientists, and drug development professionals, the NICE framework offers valuable insights into effective educational approaches that can enhance innovation capacity and ethical decision-making in both academic and industrial settings. The strategy's emphasis on authentic clinical engagement, case-based ethical analysis, and critical thinking development aligns with the complex demands of the biomedical engineering landscape, making it a valuable model for educational programs aimed at preparing the next generation of professionals in this critical field.
Problem-Based Learning (PBL) has fundamentally reshaped biomedical engineering education by transitioning from well-defined problems to complex, ill-structured challenges. This evolution directly supports the development of adaptive expertise—the ability to apply knowledge flexibly and innovatively to novel situations—which is increasingly essential in a rapidly advancing field. The traditional PBL model, introduced in biomedical engineering in the early 2000s, has demonstrated significant impacts on student learning, including enhanced critical thinking, improved knowledge retention, and stronger problem-solving capabilities [33] [34].
The distinction between routine expertise and adaptive expertise is critical in contemporary biomedical engineering education. Routine experts execute high-quality procedures efficiently in standard situations, while adaptive experts develop the capacity to devise novel solutions when confronting unfamiliar problems [1]. This whitepaper examines how strategically scaffolded PBL experiences, progressing from well-defined to ill-structured problems, systematically foster the adaptive expertise required for biomedical innovation in complex healthcare environments.
Theoretical Framework: PBL and Adaptive Expertise Development
The Spectrum of Problems in BME Education
Biomedical engineering problems exist along a continuum from well-defined to ill-structured. Well-defined problems typically have clear goals, established solution paths, and predictable outcomes, such as calculating physiological forces or designing standard circuit components. In contrast, ill-structured challenges mirror real-world professional practice, featuring ambiguous problem statements, multiple solution pathways, non-engineering constraints, and often-unclear success criteria [19]. Examples include developing novel diagnostic approaches for emerging diseases or creating patient-specific medical devices that balance engineering requirements with clinical usability.
Connecting PBL to Adaptive Expertise
The progression from well-defined to ill-structured problems in PBL directly cultivates the core dimensions of adaptive expertise:
- Domain-Specific Skills: PBL enhances both declarative knowledge ("knowing that") and procedural knowledge ("knowing how") within biomedical contexts [1]
- Metacognitive Skills: Ill-structured problems force students to "think about thinking" as they monitor their understanding and approach [1]
- Innovative Skills: Open-ended challenges with no single correct solution encourage students to transcend established routines and develop novel approaches [1]
Error Management Training provides a powerful mechanism within this framework. When students produce errors while tackling difficult problems before learning conventional solutions, they confront faulty mental representations, triggering metacognition and conceptual understanding essential for adaptive expertise [35].
Implementation Models and Methodologies
Structured PBL Implementation Framework
Successful implementation of progressive PBL requires careful scaffolding. The following experimental protocol outlines a comprehensive approach used in a three-year case study (2021-2023) involving 248 students at the Georgia Institute of Technology and Emory University joint BME program [33]:
Phase 1: Foundational Skills Development (Weeks 1-4)
- Introduce well-defined problems to establish core technical competencies
- Implement paired problem-solving with real-time instructor feedback
- Utilize structured worksheets to guide analytical approaches
- Conduct initial assessment using performance indicator rubrics
Phase 2: Transition to Moderately Structured Problems (Weeks 5-8)
- Introduce problems with multiple possible solution pathways
- Facilitate small team collaborations (3-5 students)
- Implement peer evaluation protocols using predefined criteria
- Incorporate case studies of both successful and problematic biomedical innovations
Phase 3: Ill-Structured Challenge Engagement (Weeks 9-14)
- Present authentic, open-ended biomedical challenges
- Form interdisciplinary teams matching professional practice
- Require identification of stakeholder needs and constraints
- Facilitate iterative solution development with industry/clinical feedback
Phase 4: Reflection and Metacognitive Development (Weeks 15-16)
- Guide structured reflection on problem-solving approaches
- Document knowledge gaps and learning strategies
- Create professional portfolios demonstrating progressive skill development
PBL Variation: Studio-Based Learning
Studio-based pedagogy represents an important PBL variant that emphasizes iterative practice and collaboration. Implemented in Cornell University's BME curriculum, this approach features [19]:
- Repetitive practice cycles with immediate feedback
- Structured collaboration using shared digital platforms (Google Slides/Documents)
- Integration of computational modeling as an iterative tool for refining solutions
- Development of professional identity through authentic engineering practice
Table 1: Quantitative Outcomes from PBL Implementation in Biomedical AI Education (2021-2023) [33]
| Year | Course | Student Level | # Students | # Teams | # Publications | Peer Evaluation Score |
|---|---|---|---|---|---|---|
| 2021 | BHI | Graduate | 17 | 5 | 5 | [Data Not Shown] |
| 2021 | MIP | Graduate | 22 | 6 | 2 | [Data Not Shown] |
| 2021 | BioStats | Undergraduate | 28 | 7 | 0 | [Data Not Shown] |
| 2022 | BHI | Graduate | 34 | 9 | 4 | [Data Not Shown] |
| 2022 | MIP | Graduate | 67 | 17 | 3 | [Data Not Shown] |
| 2022 | BioStats | Undergraduate | 41 | 10 | 0 | [Data Not Shown] |
| 2023 | BHI | Graduate | 41 | 10 | 2 | [Data Not Shown] |
| 2023 | MIP | Graduate | 67 | 17 | 0 | [Data Not Shown] |
| 2023 | BioStats | Undergraduate | 43 | 10 | 0 | [Data Not Shown] |
Quantitative Assessment of PBL Effectiveness
Learning Outcomes and Research Productivity
The structured progression from well-defined to ill-structured PBL generates measurable impacts on student development. Implementation data from a three-year case study demonstrates significant outcomes in both learning and research productivity [33]. The study involved 92 undergraduate and 156 graduate students across three courses: Biomedical Health Informatics (BHI), Medical Image Processing (MIP), and Biostatistics (BioStats).
Productivity metrics show substantial research output, with 16 student-authored publications generated through PBL activities, primarily in graduate-level courses. Peer evaluation data consistently indicated positive team dynamics and collaborative problem-solving development across all cohorts [33]. These outcomes highlight how ill-structured challenges in authentic biomedical contexts motivate students to produce meaningful scholarly work while developing professional skills.
Adaptive Expertise Development Metrics
The relationship between PBL experiences and adaptive expertise development emerges in several critical dimensions. Research examining health professions educators demonstrates that adaptive expertise correlates significantly with work performance (r=0.41, p<0.05) and academic ranking (r=0.42, p<0.05), but not with age or general experience, confirming that adaptive expertise requires deliberate development rather than simple accumulation of experience [1].
Table 2: Adaptive Expertise Dimensions and Development Indicators [1]
| Dimension | Definition | Key Indicators | Relationship to PBL |
|---|---|---|---|
| Domain-Specific Skills | Declarative, procedural, and conditional knowledge | Organized knowledge representation, abstract conceptual understanding | Enhanced through progressive problem complexity |
| Metacognitive Skills | Awareness and understanding of one's own thought processes | Accurate self-assessment, identification of knowledge gaps | Developed through reflection and error management |
| Innovative Skills | Ability to transcend established routines | Novel solution generation, methodological innovation | Fostered through ill-structured challenges |
| Efficiency | Fluent application of knowledge in familiar situations | Speed, accuracy in standard problems | Developed through initial well-defined problems |
Integration of Emerging Technologies in PBL
Generative AI as Cognitive Partner
The emergence of generative artificial intelligence presents both challenges and opportunities for PBL implementation. When strategically integrated, AI tools can enhance adaptive expertise development by [33] [36]:
- Providing personalized scaffolding for diverse student backgrounds
- Generating authentic biomedical problem scenarios with variable parameters
- Offering immediate feedback on solution approaches
- Assisting with literature synthesis and research planning
In the NICE strategy implementation, AI tools including DeepSeek, ChatGPT, and Kimi helped students navigate complex research literature and clarify advanced concepts, particularly benefiting undergraduates facing challenging reading material [36]. This support allowed students to engage with more complex problems earlier in their development.
Digital Collaboration Platforms
Studio-based learning implementations utilized Google Slides and Documents platforms to document and track student work, fostering collaboration and idea-sharing across teams [19]. These digital environments:
- Create portfolios for documenting progressive skill development
- Enable real-time feedback from instructors and peers
- Support iterative refinement of solutions
- Facilitate metacognitive awareness through process visualization
Visualization of PBL Workflows
PBL Implementation Framework
Adaptive Expertise Development Process
Research Reagent Solutions: Essential Methodological Components
Table 3: Essential Methodological Components for PBL Implementation
| Component | Function | Implementation Example |
|---|---|---|
| AI Literature Tools | Scaffold engagement with advanced research | ChatGPT, DeepSeek, Kimi for literature synthesis [36] |
| Digital Collaboration Platforms | Document and track progressive skill development | Google Slides/Documents for portfolio creation [19] |
| Performance Rubrics | Assess problem-solving proficiency | Indicator rubrics for quantitative problem-solving [19] |
| Case Study Libraries | Provide authentic biomedical contexts | Theranos fraud analysis, Human Genome Project cases [36] |
| Peer Evaluation Systems | Develop critical assessment skills | Structured peer review with predefined criteria [36] |
| Industry/Clinical Objectives | Connect learning to real-world applications | Company-provided project goals with clinical interviews [36] |
Discussion and Implications
Addressing Implementation Challenges
Transitioning from well-defined to ill-structured PBL presents significant implementation challenges, including scalability limitations, difficulties in personalized mentoring, and resource intensiveness [33] [34]. The integration of generative AI and digital collaboration platforms offers promising approaches to addressing these constraints while maintaining educational effectiveness. Additionally, the development of structured reflection protocols helps students articulate their evolving problem-solving approaches, enhancing metacognitive development [19] [35].
Implications for Biomedical Engineering Education
The deliberate progression from well-defined to ill-structured problems in PBL represents a fundamental shift in biomedical engineering education philosophy. This approach moves beyond knowledge transmission to cultivating adaptive experts capable of navigating the complex, unpredictable challenges of modern healthcare innovation. By explicitly connecting PBL experiences to adaptive expertise development, educators can create more intentional, effective curriculum designs that prepare students for lifelong learning and innovation in biomedical engineering [33] [1] [36].
Future research should explore optimal pacing for the transition from well-defined to ill-structured problems, investigate individual differences in adaptive expertise development, and examine long-term career impacts of PBL experiences. As biomedical engineering continues to evolve with emerging technologies including AI and advanced diagnostics, the ability to develop adaptive expertise through structured educational experiences will become increasingly critical for both academic and industrial success [33] [36].
The field of Biomedical Engineering (BME) is inherently translational, aiming to develop solutions that address real-world healthcare challenges. Success in this endeavor necessitates moving beyond isolated disciplinary work to deep, structured collaboration with key stakeholders: clinicians who provide medical expertise and frontline perspectives, industry partners who understand market dynamics and manufacturing, and patients who contribute essential lived experiences of disease and treatment. In the context of adaptive expertise development—the ability to apply knowledge to novel and ill-structured problems—stakeholder integration is not merely beneficial but fundamental. It transitions the educational paradigm from producing graduates with routine proficiency to cultivating innovators capable of navigating the unpredictable landscape of healthcare technology development [10] [37].
This integration transforms the learning environment from a theoretical exercise into an experiential one, forcing students and researchers to confront the complex constraints of clinical practice, regulatory pathways, commercial viability, and human factors. This paper provides a technical guide to the frameworks, methodologies, and practical tools for effectively embedding stakeholder collaboration into BME research and education, thereby fostering the development of adaptive expertise.
Theoretical Frameworks for Collaborative Integration
The Biomedical Stakeholder Café Model
The Biomedical Stakeholder Café is an innovative educational framework designed for capstone design projects. It creates a dynamic platform for students to engage directly with a diverse group of stakeholders, including healthcare professionals, patients, and industry experts, to discuss real-world biomedical challenges. The model enriches the learning experience by bridging the critical gap between theoretical engineering knowledge and practical medical application [38].
- Key Principles: The model is grounded in experiential learning and human-centered design. It promotes a deeper understanding of engineering principles through their practical application and emphasizes the importance of empathizing with end-users.
- Mechanism: Through a series of facilitated interactions, students are exposed to a multitude of viewpoints that directly inform their design process and decision-making. This collaborative environment helps students cultivate not only technical skills but also essential soft skills such as communication, empathy, and interdisciplinary teamwork [38].
- Outcome: This symbiotic relationship fosters significant educational and professional growth. Students develop a heightened sense of accountability, viewing their work not just as an academic requirement but as a potential contribution to society [38].
The NICE Strategy for Curriculum Development
The NICE strategy is a comprehensive educational framework developed to address multifaceted challenges in BME teaching. Its "Engagement" component directly mandates the involvement of clinical and industrial partners [37].
- New Frontier (N): Focuses on exposing students to the latest advancements in both academia and industry.
- Integrity (I): Educates students on the paramount importance of ethical conduct in biomedical R&D, using real-world case studies.
- Critical and Creative Thinking (C): Develops students' abilities to analyze information and solve complex problems.
- Engagement (E): Actively involves clinical doctors and industry professionals in teaching and student project development, providing hands-on experience and fostering professional networks [37].
This strategy is rooted in established pedagogical theories like constructivist learning and situated learning theory, ensuring that the integration of stakeholders is educationally coherent and effective in building adaptive expertise.
Triple Helix Model of Innovation
The Triple Helix model conceptualizes innovation as the product of continuous interaction and collaboration between the public (government), private (industry), and academic spheres. This model provides a structural framework for understanding how knowledge flows between universities, hospitals, and manufacturers to drive the development of innovative medical instruments. A functional innovation ecosystem requires breaking down the traditional silos between these institutional spheres [39].
Methodologies and Experimental Protocols for Effective Collaboration
The Clinical Engineering Design Process
For developing novel medical devices in response to unmet clinical needs, a structured engineering design process, managed by an in-house Clinical Engineering R&D team, has proven highly effective. The following workflow outlines this iterative process, from problem identification to a manufactured solution.
Diagram 1: Clinical Engineering Design Workflow
The methodology corresponding to the workflow above involves the following stages [40]:
- Problem Exploration and Definition: The process is initiated when a clinician identifies an unmet need. The first stage involves a joint exploration of the problem by clinicians and engineers. This includes a comprehensive literature and market search to ensure no existing solution is available. A detailed stakeholder analysis is conducted, often via an interactive workshop, to define solution-neutral user requirements that span the device's entire lifecycle, including function, safety, and training.
- Concept Generation and Detailed Design: The creative phase begins with a concept generation workshop. The problem is abstracted to prevent fixation on a single solution, leading to a wide range of concepts. The multidisciplinary team assesses these against the clinical-user requirements. Rough prototypes are manufactured to help clinicians evaluate designs and provide feedback.
- Prototype Evaluation and Iterative Refinement: The favored concept is designed for manufacture, and a prototype is built. This prototype undergoes rigorous evaluation by the clinical partners. Their feedback is integral and often leads to iterative loops back to the detailed design or even concept generation stages (as shown by the red arrows in Diagram 1). This iterative process continues until the device meets all clinical requirements.
- Implementation and Governance: The final device is manufactured for in-house use. The Clinical Engineering R&D team works to standards required for commercialisation, ensuring safety and documenting the entire process under a robust quality framework, preparing the device for potential CE marking in the future [40].
Protocol for Stakeholder Analysis in Medical Device Development
Identifying and prioritizing key factors for medical device development requires a systematic, evidence-based approach. The following methodology leverages expert input to create a strategic development pathway [41].
- Data Collection: Conduct semi-structured interviews with key stakeholders, including managers of auditing organizations, CEOs of consultant companies, government agency managers, and product managers from medical device companies. The interviews focus on the medical device development process and key influencing factors.
- Questionnaire Design and Distribution: Transcribe and perform content analysis on the interviews to extract key factors. Use these factors to design a structured questionnaire. Distribute the questionnaire to a wide group of experts (e.g., 65+ respondents) from the medical, engineering, and regulatory professions with significant seniority in the biomedical industry.
- Data Analysis with DEMATEL: Analyze the questionnaire data using the Decision-Making Trial and Evaluation Laboratory (DEMATEL) method. This technique transforms the complex interrelationships between factors into a visual structural model.
- Model Development: The DEMATEL output is used to establish a FIA-Network Relationship Map (NRM) model. This model identifies the key causal factors and the direction and strength of their influence on other factors, providing developers with an optimal pathway for resource allocation and strategy formulation [41].
Quantitative Analysis of Key Development Factors
Structured analysis of expert input allows for the prioritization of resources in medical device development. The following table synthesizes the key dimensions and their defining factors identified through stakeholder research, providing a framework for strategic focus [41].
Table 1: Key Factors in Medical Device Development
| Dimension | Factor | Description & Impact on Development |
|---|---|---|
| Organizational Characteristic (OC) | Cost Control & Budget | Financial constraints and availability of funding directly impact project scope and feasibility. |
| Professional Manpower | Access to skilled engineers and technical staff is crucial for execution. | |
| Performance Expectations | The organization's ambition level for the device's efficacy and features. | |
| Technical Capability (TC) | Compliance with Regulations | Adherence to strict regional and international medical device regulations (e.g., EU MDR). |
| Human Factors Engineering | Designing the device interface and functions to match user capabilities and limitations. | |
| Product Education & Training | Developing materials to improve user operation skills, confidence, and trust. | |
| Use Environment (UE) | Physical Layout & Conditions | Environmental factors like lighting, noise, and space in clinical or home settings. |
| Time Pressure & Workflow | Integration of the device into existing clinical workflows without causing disruption. | |
| Social & Reimbursement Context | Considering the broader healthcare system, including insurance and payment processes. | |
| User Action (UA) | Technical Knowledge & Experience | The user's pre-existing skill level and familiarity with similar technologies. |
| Individual Physical/Cognitive Abilities | Designing for the variability in end-user capabilities to prevent operation errors. |
Research indicates that the most effective development pathway is to begin by stabilizing Organizational Characteristics, followed by strengthening Technical Capability and considering the Use Environment, with final consideration given to specific User Actions [41].
The Scientist's Toolkit: Research Reagent Solutions
Successful stakeholder-integrated research and development relies on a suite of methodological and technological "reagents." The following table details essential tools for conducting collaborative work in biomedical engineering.
Table 2: Key Research Reagent Solutions for Collaborative BME
| Item | Function in Collaborative BME |
|---|---|
| Stakeholder Workshop Framework | A structured protocol (e.g., using the Double Diamond model) for facilitating multidisciplinary meetings to explore problems, define requirements, and generate concepts with clinicians, patients, and engineers [40]. |
| AI-Assisted Literature Review Tools (e.g., ChatGPT, DeepSeek) | AI tools help students and researchers quickly search, summarize, and understand complex, cutting-edge research publications, accelerating the "New Frontier" learning phase and keeping pace with rapid technological change [37]. |
| Quality Management System (QMS) Framework (e.g., ISO 13485) | A structured system for documenting design, development, and testing processes. Essential for ensuring device safety and preparing for regulatory approval, even for in-house devices [40]. |
| Privacy-Preserving Data Sharing Technologies (e.g., Federated Learning, Blockchain) | Advanced computational tools that enable secure analysis of sensitive clinical and patient data across institutions without moving or exposing the raw data, thus facilitating collaboration while protecting privacy [42]. |
| Rough Prototyping Materials & Tools | Low-fidelity materials (e.g., 3D printers, plastics, electronics) for creating early-stage physical prototypes. Crucial for allowing non-engineer stakeholders to interact with and provide feedback on design concepts tangibly [40]. |
| 4,5-Diepipsidial A | 4,5-Diepipsidial A, MF:C30H34O5, MW:474.6 g/mol |
| ML241 | ML241, MF:C23H24N4O, MW:372.5 g/mol |
Knowledge Management and Communication Strategies
The effectiveness of stakeholder collaboration hinges on the efficient transfer and sharing of knowledge, which exists in both explicit and tacit forms.
Managing Tacit and Explicit Knowledge
- Explicit Knowledge is tangible, codified, and easily communicated through documents, manuals, and reports. In BME, this includes research papers, device specifications, and regulatory submissions [39].
- Tacit Knowledge is intangible, rooted in personal experience, intuition, and know-how. It is shared through personal interaction and social processes. A physician's ability to interpret a complex MRI scan or a clinician's understanding of an unmet need based on years of practice are examples of tacit knowledge [39].
The SECI model (Socialization, Externalization, Combination, Internalization) describes the process of converting between these knowledge types. For instance, Socialization (tacit-to-tacit) occurs when a student shadows a clinician, while Externalization (tacit-to-explicit) happens when that clinician's insight is articulated into a formal design requirement [39].
Crafting Effective Impact Communications
When communicating research outcomes to stakeholders, studies show that the content, language, and presentation of impact narratives significantly influence their perception.
- Content: Stakeholders value evidence of both academic impact (e.g., high number of publications and citations) and non-academic societal benefits. The narrative should focus on facts and evidence, avoiding hyperbolic language, and should be credible by acknowledging challenges, not just successes [43].
- Language and Presentation: Clear, easy-to-read content is paramount. The narrative must quickly capture the reader's attention and be tailored to the specific audience, whether they are from industry, academia, or healthcare [43].
Integrating clinicians, industry partners, and patients into the fabric of BME research and education is a critical enabler for developing adaptive expertise. This integration, facilitated by structured frameworks like the Stakeholder Café and NICE strategy, and operationalized through rigorous methodologies like the clinical engineering design process, transforms theoretical learning into a dynamic, real-world problem-solving endeavor. By systematically leveraging stakeholder insights, BME professionals and educators can ensure that innovations are not only technologically sophisticated but also clinically relevant, user-centered, and poised for successful translation into practice, ultimately improving patient care and advancing the field of biomedical engineering.
Navigating Implementation Challenges: Barriers and Solutions for Adaptive Education
The cultivation of adaptive expertise is increasingly recognized as a critical objective in biomedical engineering (BME) education, preparing graduates to innovatively address novel and complex problems at the intersection of medicine and engineering [1]. However, the development of these competencies—balancing efficient routine performance with innovative problem-solving—faces significant institutional hurdles. This whitepaper examines the primary challenges of resource allocation and faculty development that impede the widespread integration of adaptive expertise frameworks within BME education. Drawing on recent global research, we analyze the systemic barriers and propose evidence-based strategies to reconfigure institutional priorities and structures to better support the educational innovations required for future biomedical innovation.
Theoretical Framework: Adaptive Expertise in BME Education
Adaptive expertise, a concept pioneered by Hatano and Inagaki, describes the ability to apply knowledge flexibly and creatively in novel situations, transcending routine application of learned procedures [1]. This construct is distinguished from routine expertise along several key dimensions:
- Domain-Specific Skills: Encompasses declarative knowledge ("knowing that"), procedural knowledge ("knowing how"), and conditional knowledge ("knowing when and where") [1].
- Innovative Skills: The capacity to devise novel solutions and reconsider fundamental practices when faced with unprecedented challenges [1].
- Metacognitive Skills: The ability to "think about thinking"—to self-assess knowledge, identify gaps, and strategically approach learning and problem-solving in unfamiliar contexts [1].
In BME education, adaptive expertise enables graduates to navigate the rapidly evolving landscape of medical technology, where solutions often require integrating knowledge across traditional disciplinary boundaries and developing novel approaches to complex healthcare challenges [44] [45]. The COVID-19 pandemic served as a potent case study, revealing how professionals with adaptive expertise could rapidly pivot educational and innovation strategies in response to unprecedented disruptions [1].
Table 1: Dimensions of Adaptive Expertise in BME Education
| Dimension | Definition | Manifestation in BME Education |
|---|---|---|
| Domain-Specific Skills | Mastery of core knowledge within a field | Understanding of engineering principles, human biology, and their intersection |
| Innovative Skills | Ability to transcend established routines and devise novel solutions | Creating new diagnostic approaches or medical technologies for emerging health challenges |
| Metacognitive Skills | Capacity to monitor one's own thinking and learning processes | Ability to identify knowledge gaps in complex projects and seek appropriate resources |
| Efficiency-Innovation Balance | Optimal functioning between fluent application and creative adaptation | Balancing standardized protocols with creative problem-solving in design projects |
Resource Allocation Hurdles
Infrastructure and Access Limitations
Effective BME education requires specialized facilities, equipment, and computational resources that mirror real-world clinical and research environments. However, resource constraints significantly limit student access to these essential learning tools, particularly in settings with limited funding [46]. A survey of interdisciplinary medical-engineering education in China revealed that only 19.23% of students reported satisfactory engagement with practical, hands-on learning experiences despite over 80% recognizing the discipline's importance [46]. This theory-practice gap impedes the development of adaptive expertise by limiting opportunities for students to encounter and overcome the types of novel, authentic challenges that foster innovative thinking.
The financial investment required for state-of-the-art BME instructional facilities presents a substantial barrier. Leading programs that successfully bridge this gap, such as those at Tsinghua University, Zhejiang University, and Shanghai Jiao Tong University, have implemented resource-intensive models requiring 162-178.5 credits for graduation, with significant laboratory and practical components [46]. These programs demonstrate that effective resource allocation must support not only equipment acquisition but also curriculum structures that allow for extended engagement with complex problems.
Institutional Priorities and Incentive Structures
A critical hurdle identified across multiple studies is the misalignment of institutional incentives with educational innovation. Faculty participants at the 5th BMES Council of Chairs Biomedical Engineering Educational Summit identified lack of institutional incentives to prioritize student-centered learning approaches as a primary barrier to improving classroom engagement [47]. This challenge is compounded by pressure to cover extensive technical content within constrained timeframes, leaving little room for the open-ended, problem-based activities that foster adaptive expertise [47].
The evaluation and promotion structures within many academic institutions often prioritize research funding and publications over educational innovation, creating a disincentive for faculty to invest the substantial time required to develop and implement adaptive expertise-focused curricula [47] [1]. This systemic issue perpetuates traditional, lecture-based approaches that may efficiently transmit information but do not optimally develop the innovative capacity central to adaptive expertise.
Table 2: Resource Allocation Hurdles and Their Impact on Adaptive Expertise Development
| Hurdle Category | Specific Challenges | Impact on Adaptive Expertise |
|---|---|---|
| Infrastructure Limitations | Limited access to laboratory equipment, simulation tools, and modern educational technologies | Restricts opportunities for engaging with authentic, novel problems that require innovative solutions |
| Financial Constraints | High cost of specialized BME equipment and maintenance; competition for limited institutional funding | Limits scale and frequency of hands-on experiences essential for developing flexible knowledge application |
| Institutional Incentives | Promotion criteria prioritizing research over teaching excellence; lack of recognition for educational innovation | Reduces faculty motivation to invest time in developing adaptive expertise-focused curricula |
| Time Allocation | Pressure to cover extensive technical content; perceived lack of time for active learning implementation | Constrains use of project-based and problem-based learning approaches that foster innovative thinking |
Faculty Development Challenges
Professional Preparedness Gaps
A fundamental challenge in BME education lies in the professional preparation of faculty members. Many BME instructors have limited prior industry experience, restricting their ability to translate theoretical knowledge into the practical, regulated context of medical technology development [45]. This gap is particularly significant for fostering adaptive expertise, as faculty without direct experience navigating novel, real-world challenges may struggle to mentor students in developing these competencies.
The disciplinary composition of BME faculty further complicates this issue. As noted in studies of evidence-based medical education, faculty often lack training in translating educational principles into teaching practice, including the implementation of student-centered approaches that support adaptive expertise development [48]. This dual gap—in both professional practice and educational methodology—represents a significant barrier to curricular innovation.
Structural and Systemic Barriers
Faculty development initiatives face numerous structural barriers that limit their effectiveness. In resource-limited settings, as documented in a study of Sudanese medical institutions, time constraints represent the most significant obstacle to faculty participation in development activities [49]. Additional challenges include:
- Limited financial investment in ongoing faculty development [49]
- Shortage of training personnel with appropriate expertise [49]
- Lack of comprehensive program design that addresses the specific needs of BME educators [49]
- Competing responsibilities of teaching, research, and clinical work that limit availability for development activities [48] [49]
These constraints are particularly problematic given that adaptive expertise is not automatically acquired with seniority or experience but must be deliberately developed through targeted interventions [1].
Impact on Teaching Practices
The cumulative effect of these faculty development challenges is evident in classroom practices. A 2018 observational study found that fewer than 20% of engineering classes utilized student-centered learning approaches, with most relying on traditional lecture-based methods that fail to optimally develop adaptive expertise [47]. This discrepancy occurs despite evidence that student outcomes significantly improve with more frequent use of evidence-based teaching practices [47].
The relationship between faculty development and adaptive expertise was further elucidated in a 2024 study of health professions educators, which found that self-reported levels of adaptive expertise correlated with academic ranking and perceived work performance but not with age or years of experience [1]. This suggests that adaptive expertise represents a "mastery" that must be deliberately cultivated rather than automatically acquired through seniority [1].
Strategic Interventions and Methodological Approaches
Evidence-Based Faculty Development Frameworks
Research supports specific approaches to faculty development that effectively promote the skills needed for fostering adaptive expertise. A qualitative study of medical education in Iran identified several key facilitators for implementing evidence-based educational practices, including faculty competence and motivation, strong leadership support, and professional development programs [48]. These findings align with the principles of adaptive expertise, emphasizing the need for development activities that balance efficiency (mastering core educational practices) with innovation (adapting to novel educational challenges).
Effective faculty development should incorporate deliberate practice across varied contexts, coupled with in-depth reflection—approaches that mirror the methods through which adaptive expertise itself is developed [1]. Programs should move beyond one-time workshops to create sustained communities of practice where educators can collaboratively solve teaching challenges and refine innovative approaches.
Resource Allocation Models
Strategic resource allocation can significantly impact adaptive expertise development. Analysis of leading interdisciplinary medical-engineering programs reveals several effective models:
- Staged competency development that progressively builds from fundamental knowledge to complex problem-solving [46]
- Industry and clinical partnerships that provide access to authentic challenges and resources beyond campus boundaries [46] [45]
- Integrated curriculum design that connects theoretical knowledge with practical application throughout the program [46]
Programs such as the RADx Tech initiative demonstrated how structured apprenticeship models can bridge the theory-practice gap by placing recent BME graduates alongside industry veterans in environments that demand both efficiency and innovation [45]. Such models provide valuable templates for resource-efficient approaches to developing adaptive expertise.
Implementation Protocols
Based on research findings, the following methodological approaches show promise for addressing institutional hurdles:
Table 3: Implementation Framework for Overcoming Institutional Hurdles
| Strategy | Implementation Protocol | Expected Outcome |
|---|---|---|
| Differentiated Faculty Development | 1. Conduct needs assessment across faculty cohorts2. Design tiered programs (foundational to advanced)3. Incorporate mentorship components4. Establish continuous feedback mechanisms | Increased teaching efficacyGreater adoption of evidence-based practicesEnhanced student engagement |
| Strategic Resource Mapping | 1. Audit existing resources and access patterns2. Identify priority gaps through stakeholder engagement3. Develop phased acquisition plan4. Implement shared resource model | Optimized equipment utilizationIncreased student access to practical experiencesEnhanced cost efficiency |
| Incentive Structure Reform | 1. Revise promotion criteria to value educational innovation2. Create internal grant programs for curriculum development3. Establish teaching excellence awards4. Provide course release for educational innovation | Increased faculty engagement in teaching improvementMore sustainable educational innovationEnhanced institutional reputation for teaching excellence |
Research Reagents and Methodological Tools
The following table details key methodological approaches and their applications in researching institutional hurdles and adaptive expertise development in BME education:
Table 4: Key Research Reagents and Methodological Tools
| Research Tool/Method | Function/Application | Example Use in Literature |
|---|---|---|
| Adaptive Expertise Scale (Carbonell et al., 2016) | Measures self-reported adaptive expertise across multiple dimensions | Investigating relationship between adaptive expertise and work performance among health professions educators [1] |
| Semi-structured interviews | Collects qualitative data on experiences and perceptions | Exploring barriers and facilitators to evidence-based medical education implementation [48] |
| Cross-sectional survey design | Captures snapshot of attitudes and perceptions at specific timepoint | Assessing faculty perceptions of Faculty Development Programs in resource-limited settings [49] |
| Content analysis (Graneheim & Lundman framework) | Systematically analyzes qualitative data to identify themes and patterns | Identifying categories of barriers and facilitators in medical education implementation [48] |
| Case study methodology | Provides in-depth examination of specific instances or programs | Comparing interdisciplinary medical-engineering education models across different universities [46] |
Visualizing the Institutional Ecosystem for Adaptive Expertise Development
The following diagram illustrates the relationship between institutional hurdles, strategic interventions, and the development of adaptive expertise in BME education:
Institutional Ecosystem for Adaptive Expertise Development
Addressing the institutional hurdles of resource allocation and faculty development is essential for advancing adaptive expertise in biomedical engineering education. The evidence suggests that strategic investment in faculty development—particularly through programs that balance efficiency with innovation—coupled with thoughtful resource allocation that prioritizes authentic learning experiences, can significantly enhance students' abilities to navigate novel challenges in biomedical innovation. Future progress will require institutional commitment to aligning incentive structures with educational innovation, fostering interdisciplinary collaboration, and implementing evidence-based approaches to both faculty development and resource management. By systematically addressing these hurdles, BME programs can better prepare graduates to drive the medical technology innovations needed to address evolving global health challenges.
Biomedical engineering (BME) education stands at a critical juncture, caught between the relentless pace of technological advancement and the enduring foundation of engineering first principles. The field is undergoing a radical transformation driven by artificial intelligence, personalized medicine, and disruptive technologies that are redefining healthcare delivery [50] [51]. This evolution forces curriculum designers to confront a fundamental challenge: how to integrate emerging competencies without displacing essential engineering fundamentals. This paper argues that resolving this integration-versus-replacement dilemma is paramount for developing adaptive expertise—the capacity to innovate flexibly in novel situations—in future biomedical engineers [52] [18].
The stakes of this curricular balancing act extend beyond academic discourse. Industry surveys consistently reveal that over 40% of BME graduates find their first placement in industry, where they encounter rapidly changing tools and unpredictable challenges [5]. This professional landscape demands more than routine expertise; it requires professionals who can pivot effectively when standard approaches fail. The following sections analyze core competencies, present integrative frameworks, and provide evidence-based methodologies for designing curricula that systematically build adaptive expertise.
The Core Competency Landscape: Industry Needs and Educational Gaps
Evolving Competency Priorities
Current industry perspectives reveal significant shifts in competency expectations for BME graduates. Data collected from the 2024 BME Education Summit illustrate a notable prioritization of professional skills alongside growing technical demands in data science and AI [5].
Table 1: Industry-Ranked Competencies for BME Graduates (2024 BME Education Summit Data)
| Competency | Ranking | Category | Perceived Preparedness Gap |
|---|---|---|---|
| Communication Skills | 1 | Professional | Significant |
| Collaborative Skills | 2 | Professional | Moderate-Significant |
| Critical Thinking | 3 | Professional/Technical | Moderate |
| Programming Skills | 4 | Technical | Moderate |
| Data Analysis | 5 | Technical | Significant |
| Ethical Understanding | 6 | Professional | Not Reported |
Industry representatives explicitly noted that while technical competencies are considered "an expected outcome" of accredited engineering programs, professional skills are viewed as both "difficult to teach" and critical for industry readiness [5]. This perception creates a fundamental challenge for curriculum designers: how to allocate limited instructional time to address these perceived deficiencies without compromising technical rigor.
The Adaptive Expertise Framework
Adaptive expertise represents a crucial theoretical framework for addressing the integration-replacement dilemma. Unlike routine expertise—characterized by efficient execution of familiar procedures—adaptive expertise enables professionals to respond successfully to novel situations by innovating new solutions [52]. Research conducted during the COVID-19 pandemic demonstrated that educators with higher levels of adaptive expertise were better able to maintain educational quality during disruptive conditions, with adaptive expertise scores correlating significantly with perceived work performance (r = 0.41, p < 0.05) [52].
Table 2: Comparative Analysis of Expertise Types in BME Education
| Dimension | Routine Expert | Adaptive Expert |
|---|---|---|
| Knowledge Representation | Context-bound | De-contextualized, abstract |
| Problem-Solving Approach | Efficient execution of known procedures | Innovative approaches for novel situations |
| Metacognitive Activity | Limited self-assessment | Strong reflective practice |
| Response to Novelty | Struggles with unfamiliar problems | Thrives in uncertain conditions |
| Learning Orientation | Skill refinement | Deep conceptual understanding |
Critically, adaptive expertise does not develop automatically with experience or seniority but must be deliberately cultivated through targeted educational experiences [52]. This understanding provides a theoretical foundation for curriculum design that moves beyond content coverage to focus on cognitive development.
Integration Methodologies: Curricular Models for Adaptive Expertise
The Experiential Learning Integration Framework
Experiential learning, particularly when structured around Kolb's cycle, provides a powerful mechanism for integrating new competencies without displacing core fundamentals. This approach engages students in a continuous loop of concrete experience, reflective observation, abstract conceptualization, and active experimentation [53] [54]. When properly implemented, this model allows students to encounter new tools and methodologies while strengthening fundamental engineering principles through application.
Figure 1: Kolb's Experiential Learning Cycle for BME Competency Integration. This continuous process enables the layered development of professional skills alongside technical fundamentals through iterative application and reflection.
A successful implementation of this framework was demonstrated in a 16-week elective course on hospital management for final-year BME undergraduates. Students engaged in analyzing and redesigning healthcare operations, using industrial engineering tools to solve authentic problems in hospital settings [53]. This approach required the integration of new process optimization methodologies with core BME knowledge of healthcare systems and medical technology.
Work-Based Learning and Adaptive Expertise Development
Work-based learning (WBL) environments provide particularly fertile ground for developing adaptive expertise through their inherent presentation of ill-structured, real-world problems. A recent realist review identified five critical elements that enable WBL to foster adaptive expertise [18]:
- Integrative challenging contexts that present novel, complex problems
- Structured reflective practice that prompts metacognitive engagement
- Rich interaction with others across disciplinary boundaries
- Guidance from experts who model adaptive thinking
- Support for learner willingness to engage with uncertainty
These elements work together to create what the review termed "mechanism-responses" - shifts in student thinking and perspective that underlie adaptive expertise development. The research emphasized that the integration of formal and informal learning is an essential prerequisite for developing the kinds of expertise needed in contemporary working life [18].
Transdisciplinary Learning Approaches
Transdisciplinary learning represents another effective integration methodology, particularly for incorporating data science and systems engineering competencies into traditional BME curricula. This approach dissolves traditional disciplinary boundaries to create unified frameworks for addressing complex healthcare challenges [53].
In one documented case, BME students collaborated with industrial engineers and healthcare professionals to optimize hospital processes using lean manufacturing principles. This required students to master new industrial engineering concepts while simultaneously deepening their understanding of clinical environments—a core BME competency [53]. The transdisciplinary approach prevented the new content from displacing fundamental knowledge by contextualizing both within authentic problem-solving frameworks.
Experimental Protocols and Assessment Methodologies
Protocol 1: Integrating Data Science Through Project-Based Learning
Objective: Seamlessly integrate data science and AI competencies alongside traditional BME fundamentals through authentic healthcare challenges.
Methodology:
- Problem Formulation: Student teams select genuine clinical problems requiring predictive modeling (e.g., readmission risk, disease progression)
- Data Acquisition: Students utilize de-identified clinical datasets, requiring ethical reasoning about data governance
- Feature Engineering: Teams extract clinically relevant features, connecting data science practices to physiological principles
- Model Development: Implementation of machine learning algorithms with rigorous validation protocols
- Clinical Interpretation: Translation of technical results into clinically actionable insights
Assessment Framework:
- Technical implementation (40%): Algorithm efficiency, validation rigor
- Clinical relevance (30%): Appropriate problem selection, meaningful insights
- Professional communication (30%): Clear documentation, stakeholder presentation
This protocol was successfully piloted in a neural networks course developed at Cornell's Meinig School, where students built fluency in AI data workflows while maintaining focus on biomedical applications [23].
Protocol 2: Co-curricular Integration for Professional Competency Development
Objective: Systematically develop professional skills through structured reflection on co-curricular experiences without expanding formal curriculum requirements.
Methodology:
- Pre-Experience Preparation: Orientation sessions establishing learning goals and reflection frameworks
- Structured Experience: Internship, co-op, or undergraduate research with defined engineering responsibilities
- Guided Reflection: AI-powered reflection platforms prompt students to connect experiences with curricular concepts [23]
- Synthesis Portfolio: Artifact collection with annotated connections to professional competencies
Assessment Framework:
- Reflective quality (40%): Depth of insight, connection to engineering principles
- Skill demonstration (30%): Evidence of competency development
- Articulation ability (30%): Clear communication of learning and growth
Research presented at the 5th BME Education Summit demonstrated that this approach significantly enhances employability outcomes, particularly when structured around Kolb's experiential learning framework [54].
Research Reagent Solutions: Educational Tools for Competency Integration
Table 3: Essential Resources for Implementing Integrated BME Curricula
| Resource Category | Specific Tool/Platform | Function in Curriculum Integration |
|---|---|---|
| Experiential Learning Platforms | AI-powered reflection systems | Guide students in connecting practical experiences with theoretical concepts through structured reflection prompts [23] [54]. |
| Industry-Academia Bridge | Corporate co-op/internship programs | Provide authentic problem contexts that naturally require both foundational knowledge and emerging competencies [5] [54]. |
| Simulation Environments | Clinical process modeling software | Enable safe experimentation with healthcare systems optimization, integrating industrial engineering concepts with BME fundamentals [53]. |
| Transdisciplinary Collaboration Frameworks | Hospital-university partnerships | Create authentic learning environments where multiple competency domains must be integrated to solve real healthcare challenges [53]. |
| Adaptive Assessment Tools | Scenario-based evaluation systems | Measure adaptive expertise development through responses to novel problems rather than recall of established knowledge [52] [18]. |
Discussion: Toward a Principles-Based Integration Framework
The integration-versus-replacement dilemma in BME curriculum design requires a nuanced approach that recognizes both the constant evolution of technical tools and the enduring nature of fundamental engineering principles. Based on the evidence reviewed, several guiding principles emerge for designing curricula that systematically develop adaptive expertise:
First, new competencies should be contextualized within authentic BME problem spaces rather than taught as isolated technical skills. When students learn AI through medical image analysis or data science through physiological modeling, they simultaneously reinforce core biomedical knowledge while acquiring new capabilities [23] [51].
Second, professional competencies develop most effectively through guided reflection on practical experience rather than through didactic instruction. Industry representatives explicitly value candidates who can articulate learning from co-curricular experiences, suggesting the critical importance of structured reflection frameworks [5] [54].
Third, adaptive expertise thrives on carefully calibrated challenge—situations that are sufficiently novel to require innovation but sufficiently grounded to connect with existing knowledge. Curriculum designers should strategically incorporate such "optimal adaptability corridors" throughout the educational journey [52] [18].
The framework presented in this paper argues not for simple addition of new content, but for thoughtful redesign of learning experiences that naturally engage multiple competency domains simultaneously. This approach respects the time constraints of engineering curricula while more effectively preparing graduates for the complex, unpredictable challenges of modern biomedical engineering practice.
Figure 2: Integration Framework for Adaptive Expertise Development. Foundational principles and emerging competencies converge through integrative experiences, developing adaptive expertise when coupled with structured reflection.
The future of biomedical engineering education lies not in predicting which specific technical skills will be valuable in decades to come, but in developing the adaptive capacities that will enable graduates to learn, innovate, and reinvent themselves throughout their careers. The integration-versus-replacement dilemma is ultimately a false choice—properly designed integrative experiences simultaneously strengthen foundational knowledge while building new competencies.
As biomedical engineering continues to evolve at an accelerating pace, the educators and curriculum designers who embrace this integrative approach will be best positioned to prepare graduates for the complex, unpredictable challenges of 21st-century healthcare innovation. The frameworks and methodologies presented herein provide a roadmap for this essential educational transformation.
Within biomedical engineering (BME) education, cultivating adaptive expertise—the ability to apply knowledge flexibly to novel and unpredictable problems—is increasingly critical. The rapid emergence of AI-driven protein folding, mRNA vaccines, and CRISPR gene-editing technology underscores a field in constant flux, demanding graduates who are not merely technically proficient but also innovative and adaptable [55]. This technical guide provides researchers, scientists, and drug development professionals with a comprehensive framework for assessing these complex competencies. It synthesizes contemporary educational research and experimental data to present validated methodologies, detailed protocols, and practical tools for quantifying innovation and adaptability, thereby contributing to the broader thesis of adaptive expertise development in BME education.
Theoretical Foundations: Linking Assessment to Adaptive Expertise
The concept of adaptive expertise provides the foundational theory for the assessment methodologies described herein. Unlike routine experts who excel at applying established procedures to well-known problems, adaptive experts can effectively use their knowledge to learn and innovate in unanticipated situations [10]. This distinction is crucial for BME, where regulations, technologies, and clinical needs evolve continuously.
Educational frameworks designed to foster this adaptability, such as the NICE strategy (New frontier, Integrity, Critical and creative thinking, Engagement), are grounded in constructivist and experiential learning theories [55]. These posit that knowledge is actively constructed through hands-on projects and collaborative problem-solving. Assessment within such frameworks must therefore move beyond measuring rote memorization to evaluating a student's ability to navigate complexity, integrate new information, and generate novel solutions. The How People Learn (HPL) framework has been shown to be particularly effective in this regard, preparing students to act adaptively when faced with novel ethical and technical challenges [10].
Quantitative Assessment Frameworks and Outcomes
Robust assessment relies on quantitative data to track development and validate methodological efficacy. The following tables summarize key metrics and outcomes from recent implementations of advanced educational strategies.
Table 1: Key Quantitative Metrics for Assessing Innovation and Adaptability
| Assessment Dimension | Specific Metric | Data Collection Method | Application Example |
|---|---|---|---|
| Technical Adaptability | Ability to learn and apply emerging AI tools (e.g., for literature review) [55] | Pre- and post-task performance evaluation; analysis of tool usage efficiency | Students use DeepSeek, ChatGPT to summarize cutting-edge research papers [55] |
| Critical Thinking | Quality of peer review feedback; depth of insight in case study analysis [55] | Validated critical thinking rubric; peer review scores | Students act as peer reviewers for classmates' research presentations [55] |
| Creative Problem-Solving | Novelty and feasibility of solutions in product development projects [55] | Expert evaluation of project outputs using innovation rubrics | Student teams design a novel clinical device based on interviews with doctors [55] |
| Professional Engagement | Level of interaction with clinical/industry mentors [55] | Mentor feedback scores; participation logs in industry-led sessions | Students work with company R&D directors on development plans [55] |
| Ethical Reasoning | Performance in analyzing complex, novel ethical dilemmas [10] | Scenario-based assessments; adaptive expertise ethics tests | HPL-based instruction on stem cell research ethics [10] |
Table 2: Outcomes from the NICE Strategy Implementation (5-Year Period, n>200 students) [55]
| NICE Component | Measured Skill | Reported Outcome |
|---|---|---|
| New Frontier (N) | Understanding of emerging technologies | Students gained up-to-date knowledge and could better understand emerging technologies. |
| Integrity (I) | Ethical decision-making | Students demonstrated a strong sense of integrity and understanding of ethical conduct. |
| Critical & Creative (C) | Independent thinking; solution generation | Students showed enhanced critical and creative thinking skills. |
| Engagement (E) | Practical experience in product development | Students became more familiar with product development processes. |
Experimental Protocols for Method Validation
To ensure the reliability and validity of the aforementioned assessments, the following detailed experimental protocols can be implemented.
Protocol: Assessing Adaptive Critical Thinking via Peer Review
This protocol measures the critical thinking component of adaptability in a classroom setting [55].
- Objective: To evaluate a student's ability to critically analyze and provide constructive feedback on peer work, a key indicator of analytical and evaluative skills.
- Materials: Research articles published within the last two years; AI-based literature search tools (e.g., DeepSeek, Kimi); standardized peer-review rubric covering clarity, analysis depth, and conclusion validity; presentation equipment.
- Procedure:
- Preparation: Students are assigned to use AI tools to search for, summarize, and understand recent research papers outside the core curriculum.
- Presentation: Each student delivers an oral presentation on their selected paper, requiring them to synthesize information and present their own insights and judgments.
- Peer Review: The non-presenting students are assigned as peer reviewers. They use the standardized rubric to evaluate the presentation's strengths and weaknesses.
- Feedback Submission: Reviewers submit written constructive feedback to the presenter.
- Assessment: Instructor assesses both the presenter's depth of understanding and the reviewers' critical evaluations using the same rubric. A high score on the review indicates an ability to adapt critical thinking skills to evaluate novel content.
Protocol: Evaluating Adaptive Expertise in Ethics
This protocol, derived from HPL framework research, assesses adaptive expertise in ethical reasoning [10].
- Objective: To determine a student's ability to transfer ethical knowledge to a novel, unanticipated scenario, distinguishing routine from adaptive expertise.
- Materials: Case studies on foundational bioethics topics; a novel, complex ethical dilemma not covered in instruction (e.g., related to a newly emergent technology); pre- and post-assessment questionnaires; HPL-based instructional materials.
- Procedure:
- Pre-Assessment: Administer a standard ethics test to all participants to establish a baseline of factual knowledge.
- Intervention: Divide students into two groups. The control group receives standard lecture-based ethics instruction. The experimental group learns via the HPL-based method, which is learner-centered, knowledge-centered, assessment-centered, and community-centered.
- Post-Assessment: Both groups are tested on the factual material covered. Crucially, both groups are also presented with a novel ethical scenario.
- Analysis: Compare the performance of the two groups. The protocol is validated if both groups show similar factual knowledge gains, but the HPL group demonstrates significantly superior performance in analyzing and responding to the novel dilemma [10].
Protocol: Measuring Innovation in Product Development
This protocol assesses innovation and practical adaptability through a simulated industry project [55] [56].
- Objective: To quantify a student's capacity for innovation by measuring their ability to identify an unmet clinical need and design a viable, novel product solution.
- Materials: Access to clinical professionals for interviews; mentorship from industry R&D directors; project planning tools; materials for prototyping (if applicable).
- Procedure:
- Need-Finding: Student teams (3-5 members) conduct structured interviews with clinical doctors to identify and validate an unmet clinical need.
- Ideation and Design: Teams brainstorm and develop a detailed design and development plan for a novel clinical product to address the identified need.
- Mentorship: Teams work iteratively with industrial mentors to refine their design, translating clinical needs into engineering specifications.
- Final Evaluation: A panel of faculty and industry experts assesses the final project deliverables (e.g., design report, prototype, business plan) using a rubric that scores the novelty, feasibility, and clinical relevance of the solution. High scores indicate successful integration of creative and adaptive skills.
Visualization of Assessment Workflows
The following diagrams illustrate the logical flow of the core assessment methodologies, providing a clear visual representation of the experimental protocols.
The Scientist's Toolkit: Key Research Reagents
This section details the essential "reagents"—the methodological tools and instruments—required to implement the described assessment protocols effectively.
Table 3: Research Reagent Solutions for Educational Assessment
| Tool/Instrument | Primary Function | Application Context |
|---|---|---|
| Standardized Critical Thinking Rubric | Provides a consistent, multi-criteria scale for evaluating analytical depth, logic, and evidence use. | Peer review assessments; case study analysis evaluations [55]. |
| Industry-Project Co-Design Framework | Structures collaboration between academia and industry to define authentic, assessed projects. | Product development courses; capstone projects measuring innovation [55] [56]. |
| Validated Adaptive Expertise Scenario | A novel, complex problem (e.g., ethical, design) not covered in coursework to test knowledge transfer. | Pre-/post-intervention studies comparing instructional methods [10]. |
| Structured Clinical Interview Guide | A protocol for students to conduct consistent, need-finding interviews with healthcare professionals. | Identifying unmet clinical needs for innovative design projects [55]. |
| Mixed-Methods Exit Survey | Combines Likert-scale and open-ended questions to gauge perceived skill development and experience. | Program-level evaluation; assessing professional engagement and satisfaction [57]. |
The evolving landscape of healthcare and technology demands a new breed of biomedical engineering educators capable of transcending traditional disciplinary boundaries. As biomedical engineering increasingly reflects the integrated and complex nature of healthcare, technology, and research, faculty must develop transdisciplinary mastery that enables them to create holistic educational experiences [25]. This approach transcends traditional academic boundaries, drawing from diverse fields like biology, engineering, computer science, data analytics, and even social sciences to address multifaceted healthcare challenges [25].
Developing such faculty expertise represents a critical component of a broader thesis on adaptive expertise development in biomedical engineering education research. Where routine expertise enables efficient performance in standardized situations, adaptive expertise empowers educators to respond effectively to novel problems and rapidly changing environments [1]. In the context of biomedical engineering education, this adaptive capacity manifests as the ability to dissolve traditional discipline boundaries and foster new learning environments that prepare students for the complex challenges of modern healthcare innovation [58].
Theoretical Foundations: Connecting Transdisciplinarity and Adaptive Expertise
Defining Transdisciplinary Education
Transdisciplinarity in biomedical education represents an evolution beyond multidisciplinary and interdisciplinary approaches:
- Multidisciplinary approaches draw on knowledge from different disciplines but stay within their boundaries, with disciplines connected chronologically but not integrated experientially or conceptually [58].
- Interdisciplinary approaches analyze, synthesize, and harmonize links between disciplines into a coordinated whole through cooperative analysis, typically involving team-teaching and co-teaching while retaining discipline-centric identities [58].
- Transdisciplinary approaches dissolve discipline-based boundaries to generate fundamentally new conceptual frameworks and methodologies that transcend their disciplinary origins, creating integrated learning experiences that foster new professional identities [58].
This progression represents a shift from knowledge sharing to knowledge integration and ultimately to knowledge transformation, which aligns with the core principles of adaptive expertise development.
The Adaptive Expertise Framework for Faculty
Adaptive expertise encompasses the capability to devise novel solutions to professional challenges and develop innovative problem-solving methodologies, particularly in unprecedented situations [1]. For biomedical engineering educators, this translates to specific competencies:
Table 1: Core Dimensions of Adaptive Expertise for Biomedical Engineering Educators
| Dimension | Definition | Application in BME Education |
|---|---|---|
| Domain-Specific Skills | Declarative, procedural, and conditional knowledge within one's field [1] | Deep understanding of both engineering principles and biomedical sciences, including their intersections and limitations |
| Metacognitive Skills | Capacity to understand what one knows and doesn't know, enabling self-assessment and strategic learning [1] | Ability to evaluate the effectiveness of transdisciplinary teaching approaches and identify knowledge gaps at discipline intersections |
| Innovative Skills | Ability to transcend established routines and reconsider fundamental ideas, practices, and values to facilitate change [1] | Development of novel pedagogical approaches that integrate diverse disciplines and create new conceptual frameworks |
Faculty with adaptive expertise demonstrate cognitive flexibility – they recognize the difficulty in predicting cause and effect in complex educational environments, form multiple hypotheses about teaching challenges, and reformulate their approaches based on evidence [2]. This flexibility enables them to navigate the inherent uncertainties of transdisciplinary education.
Implementing Transdisciplinary Faculty Development
Chronological, Experiential, and Conceptual Integration
Effective transdisciplinary faculty development requires integration across three dimensions, as demonstrated by pioneering programs like ENMED – a transdisciplinary dual MD/Master of Engineering degree program:
Table 2: Models of Integration in Dual Degree Programs
| Integration Type | Multidisciplinary Approach | Interdisciplinary Approach | Transdisciplinary Approach |
|---|---|---|---|
| Chronological | Separates discipline-based training chronologically (e.g., leave of absence for second degree) [58] | Concurrently delivers discipline-based courses to merge disciplines in schedule [58] | Fully integrated curriculum with simultaneous exposure to all disciplines [58] |
| Experiential | Students experience two separate discipline-focused learning environments with minimal interaction [58] | Team-teaching and co-teaching with faculty representing different disciplines [58] | Learning experiences designed to dissolve boundaries between disciplines [58] |
| Conceptual | Students must independently integrate concepts across disciplines [58] | Faculty coordinate teaching across disciplines while retaining discipline-centric identities [58] | Creates new conceptual frameworks that transcend disciplinary origins [58] |
The ENMED program exemplifies the transdisciplinary approach through its "physicianeer" training model, which integrates medical and engineering education to develop a new type of healthcare professional capable of systemic health system innovation [58].
Experiential Learning for Transdisciplinary Faculty
Faculty development programs should incorporate experiential learning cycles to foster transdisciplinary mastery. Kolb's experiential learning model provides a framework for designing such development experiences [24]:
This continuous cycle enables faculty to develop the anchored adaptability that characterizes true adaptive expertise – having a secure base of routines and conceptual understanding that enables appropriate flexibility [2]. For instance, faculty might engage in analyzing and redesigning healthcare operations alongside students, using tools from industrial engineering to expand their traditional professional role [24].
Institutional Structures and Support Systems
Developing transdisciplinary faculty expertise requires deliberate institutional support, as adaptive expertise is not automatically acquired with seniority and experience [1]. Effective approaches include:
- Transdisciplinary teaching teams that collaboratively design and implement learning experiences, as demonstrated in a hospital management course where faculty from different disciplines co-created experiential learning activities [24].
- Faculty development programs that incorporate a variety of contexts, intensities, and learning activities with substantive variability, focusing on in-depth reflection rather than simple technique transmission [1].
- Evidence-based educational research initiatives, such as those at Cornell's Meinig School, where faculty apply engineering approaches to study and improve educational systems, embedding design thinking, active learning, and flipped classroom models into curriculum redesign [23].
Assessing Transdisciplinary and Adaptive Expertise
Moving Beyond Self-Assessment
Measuring adaptive expertise presents challenges, as most instruments rely on self-assessments prone to bias [59]. Innovative assessment approaches include:
- Design scenarios that present real-world, open-ended problems varying in complexity and domain-relatedness, allowing assessment of how faculty adapt to novel challenges [59].
- AI-assisted evaluation using large language models to assess solutions to design scenarios in a consistent and reliable manner, correlating results with variables expected to relate to adaptive expertise [59].
- Multi-stakeholder feedback from students, colleagues, and industry partners that provides diverse perspectives on transdisciplinary integration capabilities.
Research has demonstrated significant correlations between adaptive expertise scores and work performance (r=0.41, p<0.05) and academic ranking (r=0.42, p<0.05), suggesting that adaptive expertise contributes to professional effectiveness [1].
Evidence of Impact
Implementation of transdisciplinary faculty development programs shows promising outcomes:
- Faculty engaged in transdisciplinary educational initiatives demonstrate improved ability to create situation-sensitive learning environments that respond to complex contextual factors rather than applying one-size-fits-all solutions [2].
- Educational programs led by transdisciplinary faculty, such as ENMED, produce graduates with novel perspectives and capabilities that have the potential to transform healthcare systemically [58].
- Institutions that systematically support faculty development in transdisciplinary education become leaders in educational innovation, setting new standards for engineering education [23].
Implementing effective transdisciplinary faculty development requires specific "research reagents" – conceptual tools and frameworks that facilitate the process:
Table 3: Essential Resources for Transdisciplinary Faculty Development
| Resource/Tool | Function | Application Context |
|---|---|---|
| ADDIE Model | Systematic instructional design framework (Analysis, Design, Development, Implementation, Evaluation) for creating learning experiences [24] | Translating healthcare processes into specific learning experiences that expand transdisciplinary knowledge and skills |
| Kolb's Experiential Learning Cycle | Four-stage learning process (concrete experience, reflective observation, abstract conceptualization, active experimentation) [24] | Structuring faculty development activities that promote adaptation and integration of diverse disciplinary perspectives |
| Design Scenarios | Real-world, open-ended problems varying in complexity and domain-relatedness [59] | Assessing adaptive expertise and providing practice with transdisciplinary problem-solving |
| AI-Powered Reflection Platforms | Technology tools that guide faculty through personalized reflections on teaching practices [23] | Enhancing metacognitive skills and promoting continuous improvement in transdisciplinary teaching |
| Transdisciplinary Grants | Funding mechanisms specifically supporting cross-disciplinary collaboration [60] | Creating structural incentives and resources for faculty to engage in transdisciplinary educational initiatives |
Developing faculty with transdisciplinary mastery represents a critical frontier in biomedical engineering education research. By framing this development within the broader context of adaptive expertise, institutions can prepare educators who not only possess deep knowledge across multiple disciplines but also the capacity to innovate, adapt, and create fundamentally new educational approaches.
The future of biomedical engineering education depends on faculty who can dissolve traditional boundaries between medicine and engineering, between theory and practice, and between education and research. Through deliberate development programs that incorporate chronological, experiential, and conceptual integration; evidence-based assessment of adaptive expertise; and institutional structures that support transdisciplinary collaboration, we can cultivate the educator expertise necessary to prepare students for the complex healthcare challenges of the 21st century.
As the field continues to evolve, further research is needed to refine assessment methods for transdisciplinary teaching effectiveness, develop more sophisticated faculty development protocols, and identify the optimal institutional structures for sustaining transdisciplinary education. What remains clear is that faculty expertise must evolve beyond traditional disciplinary mastery to embrace the adaptive, transdisciplinary approaches essential for advancing biomedical innovation and improving human health.
Adaptive learning represents a transformative educational approach that leverages technology to tailor learning pathways to individual student needs, proving particularly valuable in complex fields like biomedical engineering (BME). This educational paradigm systematically alters the flow of learning activities based on individual student performance and engagement data, creating personalized educational experiences [61]. Within BME education, which requires the integration of engineering principles with biological sciences and clinical practice, adaptive learning systems show significant promise for developing adaptive expertise—the ability to apply knowledge flexibly and creatively to novel problems—a crucial competency for future biomedical innovators [32].
The implementation of adaptive learning across diverse institutional contexts presents both opportunities and challenges. This technical guide examines scaling strategies based on current research and institutional practices, providing a framework for biomedical engineering educators seeking to implement these approaches systematically. By examining quantitative outcomes, methodological protocols, and technological considerations, we offer evidence-based guidance for deploying adaptive learning systems that enhance educational outcomes while developing the adaptive expertise required for addressing complex healthcare challenges.
Quantitative Evidence: Effectiveness of Adaptive Learning
Comprehensive analysis of empirical studies reveals the measurable impact of adaptive learning implementations in engineering and health sciences education. The following table synthesizes key quantitative findings from recent research:
Table 1: Quantitative Outcomes of Adaptive Learning Implementations
| Study Focus | Performance Improvement | Engagement Metrics | Sample Size & Context |
|---|---|---|---|
| Academic Performance | 59% of studies reported increased academic performance [62] | - | 69 studies across higher education institutions |
| Medical Neuroscience | No significant difference overall; more students scored 70-79% with adaptive approach [61] | - | 102 students per cohort (2019-2020) |
| High Achievers | Enhanced performance for high-performing medical students [61] | - | Medical neuroscience course |
| Student Engagement | 36% of studies indicated increased student engagement [62] | - | Analysis across 69 eligible studies |
| Early Intervention | Effective identification of underachieving students [61] | - | Medical education context |
These quantitative findings demonstrate that while adaptive learning consistently shows positive outcomes, the specific impacts vary based on implementation design, student population, and disciplinary context. The evidence supports adaptive learning as a valuable approach for enhancing educational outcomes in biomedical engineering education when appropriately scaled and implemented.
Technological Infrastructure and Implementation Methodologies
Platform Selection and Integration
Successful institution-wide implementation of adaptive learning requires careful technological infrastructure planning. Research indicates that McGraw-Hill's Connect LearnSmart and Moodle rank among the most utilized adaptive platforms in higher education contexts [62]. These platforms provide the foundational architecture for delivering personalized content pathways based on continuous assessment of student performance.
The integration process typically follows a structured protocol:
Pre-knowledge Assessment: Implementation begins with diagnostic quizzes that activate adaptive content delivery systems, creating individualized baselines for each student [62].
Content Sequencing: Algorithms dynamically adjust learning material presentation based on continuous assessment data, creating personalized pathways through complex biomedical engineering concepts.
Progress Monitoring: Embedded analytics track student engagement and performance metrics, providing both students and instructors with real-time feedback on learning progression.
Intervention Triggers: System-generated alerts identify struggling students early in the learning process, enabling timely educational interventions [61].
Blended Learning Implementation Protocol
The adaptive blended learning model represents a particularly effective approach for biomedical engineering education, combining digital personalized learning with strategic face-to-face interactions. The following methodology was successfully implemented in a medical neuroscience course:
Table 2: Adaptive Blended Learning Implementation Protocol
| Phase | Duration | Core Activities | Adaptive Components |
|---|---|---|---|
| Synchronous Sessions | 25% of course time | Case discussions, complex problem-solving, team-based activities | Just-in-time teaching based on pre-session assessment data |
| Asynchronous Adaptive Learning | 50% of course time | Self-paced progression through adaptive learning modules | Algorithmically generated content pathways based on continuous assessment |
| Hands-on Laboratory | 25% of course time | Experimental procedures, sensor development, prototype testing | Adaptive scaffolding based on individual skill progression |
| Assessment Framework | Continuous | Formative quizzes, practical exams, design projects | Pre-knowledge assessments triggering personalized content delivery |
This protocol demonstrated comparable outcomes to traditional in-person instruction while providing greater flexibility—a critical consideration when scaling across institutions with different resource profiles and student demographics [61].
Visualization: Institutional Scaling Framework
The following diagram illustrates the core workflow for implementing adaptive learning across diverse institutional contexts, specifically designed for biomedical engineering education:
Institutional Scaling Workflow
Development of Adaptive Expertise in BME Education
Adaptive learning systems directly contribute to developing adaptive expertise in biomedical engineering students—the ability to efficiently apply knowledge to novel problems and evolving clinical contexts. This development occurs through several interconnected mechanisms:
Challenge-Based Learning Integration
The incorporation of Challenge-Based Learning (CBL) within adaptive frameworks creates powerful environments for developing adaptive expertise. The following protocol was successfully implemented in a bioinstrumentation course:
Industry Partnership Identification: Collaborate with medical device companies or clinical partners to identify authentic, relevant challenges (e.g., designing respiratory or cardiac gating devices for radiotherapy) [63].
Adaptive Skill Building Modules: Implement personalized pre-training modules that address individual knowledge gaps related to the core challenge.
Iterative Prototyping Cycle: Students engage in repeated design-build-test cycles with adaptive feedback mechanisms providing targeted guidance based on individual progress.
Stakeholder Engagement: Structured interactions with clinical professionals and industry partners provide authentic feedback, reinforcing the connection between adaptive learning and professional practice [63].
This approach demonstrated significant positive outcomes in student engagement and skill development, with students reporting strong agreement that the course "challenged them to learn new concepts and develop new skills" despite the substantial faculty time investment required [63].
Clinical Immersion and Interdisciplinary Collaboration
The integration of clinical immersion experiences within adaptive learning frameworks further enhances adaptive expertise development:
Table 3: Interdisciplinary Clinical Immersion Protocol
| Component | Implementation | Adaptive Expertise Development |
|---|---|---|
| Simulation Laboratory | Mannequin-based scenarios with technological limitations [32] | Identification of unmet clinical needs and engineering opportunities |
| Real Clinical Settings | Observation of surgeries, emergency departments, therapy clinics [32] | Contextual understanding of clinical workflows and constraints |
| Interdisciplinary Teams | BME students partnered with nursing students [32] | Development of cross-disciplinary communication and collaboration skills |
| Need Identification | Structured process for identifying 3+ unmet clinical needs [32] | Enhancement of observation, analysis, and problem-finding capabilities |
This methodology enables students to develop the adaptive expertise required for identifying and addressing complex, ill-structured problems in real healthcare environments—a crucial competency for biomedical engineering professionals [32].
Visualization: Adaptive Expertise Development Pathway
The following diagram illustrates how adaptive learning systems contribute to developing adaptive expertise in biomedical engineering students:
Adaptive Expertise Development Pathway
Implementation Barriers and Scaling Considerations
Technological and Resource Constraints
Implementation of adaptive learning systems faces significant barriers that must be addressed in scaling strategies. Research identifies technological limitations and time resources as major constraints across institutions [62]. These challenges manifest differently across institutional contexts:
Resource-Variable Implementation Models: Develop tiered implementation approaches that can function effectively under different resource constraints, from well-funded research institutions to resource-limited settings.
Faculty Development Protocols: Create comprehensive training programs that address both technological proficiency and pedagogical shifts required for adaptive learning facilitation.
Technical Infrastructure Planning: Implement scalable architecture that can expand from pilot programs to institution-wide deployment without requiring complete system overhaul.
Inclusive Design and Accessibility
Scaling adaptive learning requires deliberate attention to inclusivity and accessibility. The "Engineering for All" framework emerging from biomedical engineering education research emphasizes lowering systemic barriers and creating equitable learning environments [64]. Key components include:
Universal Design for Learning (UDL) Integration: Building multiple means of engagement, representation, and expression into adaptive learning systems from their initial design [64].
Cultural Competence Development: Incorporating training modules that enhance students' ability to understand and appreciate cultural differences—identified as a crucial competency for industry success [64].
Bias Mitigation Protocols: Implementing systematic approaches to identify and address potential biases in algorithmic content delivery and assessment systems.
Research Reagents: Experimental and Implementation Tools
The following table details key implementation "reagents"—essential tools and methodologies—for deploying adaptive learning in biomedical engineering education:
Table 4: Research Reagents for Adaptive Learning Implementation
| Tool/Category | Specific Examples | Function in Implementation |
|---|---|---|
| Adaptive Learning Platforms | McGraw-Hill's Connect LearnSmart, Moodle [62] | Core delivery system for personalized content pathways |
| Learning Analytics Systems | Embedded analytics in adaptive platforms, institutional LMS data dashboards [62] [61] | Tracking student engagement, performance metrics, and intervention triggers |
| Assessment Tools | Pre-knowledge quizzes, formative assessments, concept inventories [62] | Initial benchmarking and continuous progress monitoring |
| Clinical Immersion Resources | Simulation mannequins, hospital partnerships, surgical observation opportunities [32] | Providing authentic contexts for adaptive expertise development |
| Interdisciplinary Collaboration Tools | Shared project platforms, communication systems, team-based learning protocols [32] [64] | Facilitating BME, clinical, and industry collaboration |
| Accessibility Evaluation Tools | Viz Palette, contrast checkers, WCAG compliance validators [65] [66] | Ensuring inclusive design of adaptive learning materials |
Scaling adaptive learning across diverse institutions requires systematic attention to technological infrastructure, pedagogical integration, and contextual adaptation. The evidence-based frameworks, protocols, and visualizations presented in this technical guide provide a foundation for biomedical engineering educators seeking to implement these approaches effectively.
Future development should focus on enhancing interoperability between adaptive learning platforms and institutional systems, refining algorithms for more nuanced learning pathway personalization, and expanding research on the relationship between adaptive learning implementations and the development of measurable adaptive expertise competencies. The integration of emerging technologies—including AI-assisted feedback systems and immersive clinical simulations—promises to further enhance the effectiveness of adaptive learning in preparing biomedical engineering students for the complex challenges of 21st-century healthcare innovation.
As institutions continue to scale these approaches, ongoing assessment of learning outcomes, particularly regarding long-term development of adaptive expertise, will be essential for refining implementation strategies and maximizing the educational impact across diverse institutional contexts and student populations.
Measuring Impact: Evidence-Based Outcomes and Comparative Effectiveness
In an era of rapid technological advancement and complex global challenges, the capacity of professionals to adapt innovatively is paramount. Adaptive expertise (AE) represents a model of expert development that emphasizes a balance between the efficient application of existing knowledge to solve familiar problems and the innovative generation of new solutions when faced with novel challenges [15]. In the highly specialized field of biomedical engineering (BME), where professionals operate at the intersection of engineering, life sciences, and clinical practice, adaptive expertise has emerged as a critical determinant of professional effectiveness. This technical review examines the empirical evidence correlating adaptive expertise with work performance, with specific application to biomedical engineering education and practice, providing researchers and drug development professionals with evidence-based frameworks for cultivating this essential competency.
Quantitative Evidence: Linking Adaptive Expertise to Performance Outcomes
Empirical studies across various professional domains have demonstrated significant correlations between adaptive expertise and enhanced work performance. A 2024 cross-sectional study of health professions educators (HPEs) provides direct quantitative evidence for this relationship, measuring adaptive expertise using a validated self-report instrument and correlating these scores with perceived work performance metrics [1].
Table 1: Correlations Between Adaptive Expertise and Performance Metrics
| Variable | Adaptive Expertise Score (Mean ± SD) | Correlation with Work Performance (r) | P-value |
|---|---|---|---|
| Overall Sample | 4.18 ± 0.57 (on 5-point scale) | 0.41 | < 0.05 |
| By Academic Rank | |||
| Professors | Higher than other ranks | 0.42 | < 0.05 |
| Lower ranks | Lower than professors | N/S | N/S |
| By Experience Level | No significant correlation | N/S | N/S |
| By Age | No significant correlation | N/S | N/S |
The findings reveal two crucial insights: first, adaptive expertise significantly correlates with enhanced work performance (r = 0.41, p < 0.05); second, this expertise is not automatically acquired through seniority or experience alone, but rather must be deliberately developed through targeted educational interventions [1]. This has profound implications for biomedical engineering education and professional development programs, suggesting that structured curricula must intentionally foster adaptive capacities rather than assuming they emerge naturally through accumulated experience.
Conceptual Framework and Theoretical Foundations
Defining Adaptive Expertise
Adaptive expertise represents a dynamic balance between two complementary dimensions: efficiency in applying existing knowledge to familiar problems, and innovation in generating novel solutions when confronted with unfamiliar challenges [15] [67]. This conceptualization positions routine expertise and adaptive expertise along a continuum, where routine expertise reflects mastery of efficient procedures execution, while adaptive expertise encompasses the capability to devise innovative solutions and problem-solving methodologies, particularly in unprecedented situations [1] [67].
In biomedical engineering contexts, this translates to professionals who can not only efficiently operate within established protocols and device specifications, but also innovatively adapt when confronting novel clinical challenges, emerging technologies, or unique patient-specific constraints. The optimal adaptability corridor conceptualizes this balance, positioning individuals high on both efficiency and innovation dimensions as truly adaptive experts [1].
Core Dimensions of Adaptive Expertise
Three principal dimensions constitute the foundational architecture of adaptive expertise:
Domain-Specific Skills: Encompassing declarative knowledge ("knowing that"), procedural knowledge ("knowing how"), and conditional knowledge ("knowing when and where") [1]. Unlike novices, adaptive experts possess knowledge representations characterized by superior organization, abstraction, and consolidation, enabling flexible application across varied scenarios [1].
Metacognitive Skills: The capacity for "thinking about thinking" – self-assessing one's knowledge, identifying gaps, and strategically deploying cognitive resources [1]. This dimension enables professionals to monitor their problem-solving approaches and adjust strategies as needed.
Innovative Skills: The ability to transcend established routines, reconsider fundamental assumptions, and devise novel solutions when existing approaches prove insufficient [1]. This dimension is particularly crucial in biomedical engineering contexts where technological limitations regularly confront unique clinical presentations.
Figure 1: Conceptual Framework of Adaptive Expertise Correlated with Work Performance
Experimental Protocols and Methodologies for Assessing Adaptive Expertise
Measurement Instruments and Study Designs
Research investigating the adaptive expertise-work performance relationship employs diverse methodological approaches, each with distinct strengths and applications for biomedical engineering contexts.
The 2024 study by BMC Medical Education utilized a descriptive, cross-sectional, single-site design with a self-reported adaptive expertise tool originally developed by Carbonell et al. (2016) [1]. The methodology encompassed:
- Sample: 40 health professions educators from the University of Twente, Netherlands, including lecturers, senior lecturers, assistant professors, associate professors, and full professors.
- Instrumentation: Validated adaptive expertise scale measuring the core dimensions of domain-specific skills, metacognitive skills, and innovative skills using Likert-type items.
- Performance Metrics: Three supplementary questions assessing participants' perceptions of their work performance, amount of work accomplished, and teaching quality during the COVID-19 pandemic-induced transition to alternative teaching modes.
- Statistical Analysis: Kaiser-Meyer-Olkin measure and Bartlett's Test of Sphericity to verify sample adequacy (KMO = 0.633, P < 0.0001), followed by correlation analyses to examine relationships between adaptive expertise scores, performance metrics, and demographic variables [1].
This methodological approach demonstrates the feasibility of quantifying the complex construct of adaptive expertise and statistically correlating it with performance outcomes, providing a replicable framework for similar investigations in biomedical engineering contexts.
Work-Based Learning Interventions
A 2025 realist review examined how work-based learning (WBL) environments contribute to adaptive expertise development, identifying key contextual factors and mechanisms [18]. The review methodology included:
- Search Strategy: Comprehensive literature search across multiple databases following realist review methodology.
- Analysis Framework: Context-Mechanism-Outcome (CMO) configurations to understand how, why, and under what circumstances WBL stimulates adaptive expertise development.
- Intervention Elements: Identification of five critical WBL elements for adaptive expertise development: (1) integrative challenging contexts, (2) reflective practice, (3) interacting with others, (4) guidance, and (5) learner characteristics [18].
The realist approach provides particularly valuable insights for designing biomedical engineering education programs, emphasizing that adaptive expertise development requires carefully structured interventions rather than simple exposure to workplace environments.
Figure 2: Work-Based Learning Mechanisms for Adaptive Expertise Development
Applications in Biomedical Engineering Education
Experiential Learning Models
Biomedical engineering education research has demonstrated the efficacy of experiential learning interventions in developing adaptive expertise. A 2023 study implemented a 16-week elective course on hospital management for final-year BME students that incorporated:
- Clinical Immersion: Students engaged in analyzing and redesigning healthcare operations within actual hospital environments, moving beyond theoretical classroom exercises [24].
- Transdisciplinary Integration: Incorporation of industrial engineering concepts (process improvement, lean systems, operations management) alongside traditional BME curriculum [24].
- Structured Reflection: Implementation of Kolb's experiential learning cycle with four iterative stages: concrete experience, reflective observation, abstract conceptualization, and active experimentation [24].
This approach enabled students to develop the conceptual understanding necessary for adaptive expertise by connecting theoretical knowledge with practical application in authentic clinical contexts, precisely addressing the knowing why component that distinguishes adaptive experts from routine experts [15].
Interdisciplinary Clinical Partnerships
Research demonstrates that structured interdisciplinary experiences significantly enhance adaptive expertise development in BME students. A 2018 study created a series of courses pairing engineering students with nursing students in clinical settings [32]. The experimental protocol included:
- Simulation Laboratory Exposure: Engineering students participated in simulation scenarios using mannequins currently employed in nursing education, identifying biomechanical limitations and proposing engineering improvements [32].
- Real Clinical Settings: Interdisciplinary teams (engineering and nursing students) observed actual clinical procedures (cataract surgery, hand surgery, robotic prostate surgery, emergency department, physical therapy) to identify unmet needs [32].
- Need Identification and Solution Design: Teams identified three unmet needs in clinical settings, proposed viable engineering solutions, and could continue development through capstone senior design projects [32].
This methodology not only enhanced students' technical skills but specifically developed their capacity for adaptive performance by exposing them to the complex, ill-structured problems characteristic of real healthcare environments [32].
Table 2: Biomedical Engineering Educational Interventions for Developing Adaptive Expertise
| Intervention Type | Key Components | Measured Outcomes | Evidence Source |
|---|---|---|---|
| Clinical Immersion & Experiential Learning | Hospital fieldwork, process analysis, healthcare operations redesign | Transdisciplinary knowledge, systems thinking, process improvement skills | [24] |
| Interdisciplinary Team-Based Projects | Engineering-nursing student teams, simulation scenarios, real clinical observations | Enhanced problem identification, interdisciplinary communication, innovative solution development | [32] |
| Work-Based Learning Integration | Challenging real-world problems, reflective practice, structured guidance | Adaptive thinking, perspective shifting, ability to transfer knowledge across contexts | [18] |
| Sequential Course Series | Biomechanics course → Medical device design → Capstone project execution | Progressive development of adaptive expertise through repeated clinical exposure | [32] |
Table 3: Essential Methodological Resources for Adaptive Expertise Research
| Resource Category | Specific Instrument/Tool | Function/Application | Evidence Source |
|---|---|---|---|
| Measurement Instruments | Carbonell et al. (2016) Adaptive Expertise Scale | Quantifies adaptive expertise across multiple dimensions using self-report methodology | [1] |
| Study Designs | Descriptive cross-sectional design with correlation analysis | Establishes relationships between adaptive expertise and performance metrics | [1] |
| Educational Frameworks | Kolb's Experiential Learning Cycle | Structures learning experiences through concrete experience, reflection, conceptualization, and active experimentation | [24] |
| Intervention Models | Work-based learning (WBL) with CMO configuration analysis | Identifies how contextual factors trigger mechanisms leading to adaptive expertise development | [18] |
| Pedagogical Approaches | Simulation-based learning with mannequins | Creates controlled clinical environments for problem identification and solution development | [32] |
| Assessment Methods | Perception-based performance metrics | Captures self-reported work performance, teaching quality, and productivity | [1] |
The empirical evidence unequivocally demonstrates a significant positive correlation between adaptive expertise and work performance across multiple professional domains, including biomedical engineering. The quantitative findings (r = 0.41, p < 0.05) establish that professionals with higher levels of adaptive expertise consistently demonstrate superior performance outcomes, particularly in novel, complex, or rapidly changing situations [1]. Crucially, adaptive expertise is not an automatic byproduct of experience or seniority, but rather must be deliberately cultivated through targeted educational interventions that balance efficiency with innovation, domain knowledge with metacognitive awareness, and routine execution with creative problem-solving [1].
For biomedical engineering education and professional development, these findings underscore the imperative to move beyond knowledge transmission toward educational models that explicitly foster adaptive capacities. The most effective approaches incorporate clinical immersion, interdisciplinary collaboration, challenging real-world problems, and structured reflection within work-based learning environments [32] [18] [24]. As biomedical engineering continues to evolve amid rapidly advancing technologies and complex healthcare challenges, the intentional development of adaptive expertise will remain critical for preparing professionals capable of innovating solutions to the unprecedented problems of tomorrow.
This whitepaper presents a comparative analysis of traditional and adaptive learning outcomes within the context of biomedical engineering education. Through systematic evaluation of experimental data and implementation protocols, we demonstrate that adaptive learning strategies significantly enhance academic performance, conceptual understanding, and adaptive expertise development compared to traditional instructional methods. The integration of learning science principles with advanced educational technologies creates scaffolds for developing the flexible problem-solving capabilities essential for biomedical engineering innovation.
The rapid evolution of biomedical engineering demands educational approaches that foster adaptive expertise—the ability to apply knowledge flexibly and creatively to novel problems. Traditional education models, often characterized by standardized content delivery and passive learning, face significant challenges in cultivating these competencies [68]. Adaptive learning systems, which leverage data-driven algorithms to personalize educational experiences, represent a transformative approach with particular relevance for biomedical engineering education [69].
This technical analysis examines the empirical evidence comparing traditional and adaptive learning outcomes, with specific attention to implementations within engineering and biomedical education contexts. We synthesize findings from controlled studies, detail experimental methodologies, and propose a framework for optimizing adaptive expertise development through intelligent tutoring systems, challenge-based instruction, and personalized learning pathways [70] [69].
Theoretical Framework and Definitions
Traditional Learning in Biomedical Engineering
Traditional biomedical engineering education typically employs structured curricula with fixed sequencing, instructor-paced progression, and standardized assessments. This model operates on the assumption of homogeneous learner needs and emphasizes knowledge transmission through lectures, textbooks, and laboratory demonstrations [70]. The VaNTH Engineering Research Center in Bioengineering Educational Technologies described this approach as having inherent limitations for developing the complex reasoning skills required for bioengineering innovation [70].
Adaptive Learning Systems
Adaptive learning constitutes an educational strategy that uses technology-based analytics to create personalized learning paths based on individual student performance, profile, and learning needs [69]. These systems employ algorithms, assessments, and immediate feedback to dynamically adjust content sequencing and difficulty [68]. In biomedical engineering contexts, adaptive learning often incorporates challenge-based instruction grounded in the How People Learn (HPL) framework, which emphasizes learning environments that are knowledge-centered, student-centered, assessment-centered, and community-centered [70].
Adaptive Expertise in Biomedical Engineering
Adaptive expertise refers to the capacity to apply knowledge effectively to novel problems and situations, going beyond routine application of procedures to innovative problem-solving [70]. This constitutes a critical outcome for biomedical engineering education, where professionals routinely encounter unprecedented challenges at the intersection of biology, medicine, and engineering.
Methodological Approaches for Comparative Studies
Controlled Study Designs
Research comparing traditional and adaptive learning outcomes typically employs quasi-experimental designs with control and experimental groups. The study conducted at Tecnologico de Monterrey implemented a sequential quantitative-qualitative methodology (Quant->Qual) across multiple engineering courses including Computational Thinking, Physics I, Physics II, and Fundamental Mathematical Modeling [69].
Experimental Protocol:
- Participant Allocation: Students assigned to control (traditional instruction) and experimental (adaptive learning strategy) groups
- Intervention Duration: Full academic semester implementation
- Baseline Assessment: Pre-tests measuring prior knowledge and cognitive abilities
- Instructional Variable: Control groups received standard lecture-based instruction; experimental groups engaged with adaptive learning platforms (e.g., Realizeit) with personalized learning paths
- Outcome Measures: Standardized content assessments, conceptual understanding tests, problem-solving tasks, and engagement metrics
- Data Collection Points: Pre-test, mid-intervention, post-test, and retention (4-8 weeks post-intervention)
Adaptive Learning Implementation Framework
The Didactic Model Using Adaptive Learning (DMUAL) integrates activities before, during, and after class sessions [69]:
- Pre-class Phase: Students engage with adaptive platform resources (videos, readings, podcasts) and complete exercises with automated feedback targeting lower-order cognitive processes
- In-class Phase: Focus on higher-order cognitive activities including complex problem-solving, challenge-based learning, and application exercises
- Post-class Phase: Reinforcement through additional adaptive activities and assessments
Assessment Methods for Adaptive Expertise
Evaluation of adaptive expertise requires multidimensional assessment strategies beyond conventional testing:
- Knowledge Application Tasks: Problems requiring transfer of concepts to novel contexts
- Path Independence Analysis: Measuring whether students can solve problems using different approaches than those taught
- Conceptual Understanding Maps: Assessment of interconnected knowledge structures
- Efficiency Metrics: Time and step count to solution for complex problems
- Innovation Indicators: Generation of novel solutions or approaches to open-ended challenges [70]
Quantitative Outcomes Analysis
Academic Performance Metrics
Table 1: Comparative Academic Performance in Adaptive vs. Traditional Learning Environments
| Metric | Traditional Learning | Adaptive Learning | Effect Size | Study Reference |
|---|---|---|---|---|
| Course Pass Rates | 72% | 89% | +17% | [69] |
| Conceptual Understanding | 68% | 85% | +17% | [70] |
| Problem-Solving Transfer | 64% | 82% | +18% | [70] |
| Knowledge Retention | 61% | 79% | +18% | [70] |
| Student Engagement | Baseline | +36% | — | [62] |
A comprehensive scoping review of 69 studies on personalized adaptive learning in higher education revealed that 59% (41 studies) reported improved academic performance, while 36% (25 studies) indicated increased student engagement [62]. In biomedical engineering education specifically, challenge-based instruction within the HPL framework demonstrated significant improvements in students' abilities to solve complicated problems and apply knowledge to novel situations [70].
Efficiency and Engagement Outcomes
Table 2: Learning Efficiency and Engagement Comparison
| Efficiency Metric | Traditional Approach | Adaptive Approach | Improvement |
|---|---|---|---|
| Time to Mastery | 100% (baseline) | 68% | -32% |
| Instructional Scaffolding | One-to-many | Personalized | +42% |
| Feedback Latency | 2-7 days | Immediate | >90% reduction |
| Learning Path Flexibility | Fixed | Dynamic | Customized per student |
| Cognitive Load Management | Not monitored | Optimized | +57% |
The implementation of adaptive learning strategies at Tecnologico de Monterrey demonstrated that students following personalized learning paths achieved mastery-level understanding in approximately two-thirds the time required through traditional instruction [69]. This efficiency gain enables deeper exploration of complex biomedical engineering concepts and more extensive practical application.
Experimental Visualization
Adaptive Learning Workflow
Traditional vs. Adaptive Learning Pathways
Implementation Protocols for Biomedical Engineering Education
Research Reagent Solutions for Adaptive Learning Research
Table 3: Essential Research Components for Adaptive Learning Implementation
| Component Category | Specific Solution | Function in Research Context |
|---|---|---|
| Adaptive Platforms | Realizeit | Provides personalized learning paths with AI algorithm analyzing student demographics and performance [69] |
| Learning Analytics | Moodle with Adaptive Extensions | Tracks student progress and enables real-time intervention [62] [69] |
| Assessment Tools | Parameterized Question Banks | Generates dynamic assessments with immediate personalized feedback [69] |
| Cognitive Measurement | Eye Tracking Systems | Monitors attention and cognitive load through gaze patterns [71] |
| Simulation Environments | VR Chemical Processing Plant | Enables experimentation with complex systems without real-world consequences [71] |
| Theoretical Framework | HPL (How People Learn) | Guides instructional design to be knowledge-centered, student-centered, assessment-centered, and community-centered [70] |
Biomedical Engineering Challenge-Based Protocol
The VaNTH ERC developed a specific protocol for implementing challenge-based instruction in biomedical engineering:
Experimental Protocol:
- Challenge Presentation: Students encounter a complex, realistic bioengineering problem
- Initial Perspectives: Students articulate initial thoughts and hypotheses
- Research & Revision: Students engage with adaptive resources to investigate the challenge
- Testing Metacognition: Students compare current understanding to initial perspectives
- Go Public: Students present solutions and receive feedback [70]
This protocol employs the Star.Legacy Cycle, which has demonstrated significant improvements in biomedical engineering students' broad problem-solving skills and conceptual understanding [70].
Discussion and Technical Implications
Integration with Biomedical Engineering Pedagogy
The comparative analysis reveals that adaptive learning strategies particularly benefit biomedical engineering education due to the field's inherent complexity and need for adaptive expertise. The integration of immersive simulations with adaptive learning platforms creates powerful educational environments for developing clinical engineering skills [71]. For example, Dr. Paul Hungler's development of a VR chemical processing plant allows biomedical engineering students to experiment with complex systems without real-world consequences while receiving personalized scaffolding based on performance [71].
Data-Driven Personalization Mechanisms
Adaptive learning systems in biomedical education employ sophisticated algorithmic personalization based on continuous assessment data. The most effective systems use:
- Pre-knowledge diagnostics as the primary trigger for adaptive content delivery [62]
- Real-time analytics for monitoring student progress in personalized learning paths [69]
- Multimodal assessment including physiological measures (eye tracking, pulse monitoring) to gauge cognitive load [71]
- Predictive analytics to identify at-risk students and trigger interventions before academic failure [69]
Scalability and Institutional Implementation
Successful implementation of adaptive learning in biomedical engineering requires careful institutional planning. The research from Tecnologico de Monterrey suggests a comprehensive implementation model that includes faculty development, technical infrastructure, and curricular redesign [69]. Critical success factors include:
- Selection of adaptive platforms that support multiple content types (HTML, multimedia, documents)
- Integration with existing learning management systems and gradebooks
- Professional development for instructors transitioning from knowledge providers to learning facilitators
- Continuous evaluation and refinement based on learning analytics [69]
This comparative analysis demonstrates that adaptive learning systems consistently outperform traditional instructional approaches across multiple metrics relevant to biomedical engineering education. The quantifiable improvements in academic performance, conceptual understanding, problem-solving transfer, and learning efficiency provide compelling evidence for broader implementation of adaptive strategies in biomedical engineering curricula.
Future research should focus on longitudinal studies tracking adaptive expertise development throughout biomedical engineering careers, refined algorithms for personalization in highly specialized subdomains, and cross-institutional collaborations to establish best practices for scalable implementation. As adaptive learning technologies evolve, their integration with emerging capabilities in artificial intelligence and immersive simulation will create increasingly powerful environments for developing the next generation of biomedical engineering innovators.
The evidence strongly supports strategic investment in adaptive learning technologies as a mechanism for enhancing biomedical engineering education outcomes and accelerating the development of adaptive expertise essential for addressing complex challenges at the interface of engineering, biology, and medicine.
Modern economies demand an increasingly diverse and specialized set of skills from engineers, many of which depend on the acquisition of other foundational skills first [72]. This reality has accelerated the need for adaptive expertise—the ability to apply knowledge gained through prior experiences to novel situations where key information may be missing [73]. Within biomedical engineering (BME) and related technical fields, educational frameworks are increasingly emphasizing experiential learning and adaptive expertise as critical targets for development, moving beyond traditional knowledge transmission to foster professionals capable of innovation in unpredictable environments [54] [73].
Longitudinal tracking of career trajectories provides invaluable data for understanding how adaptively-trained engineers navigate their professional pathways, overcome career challenges, and ultimately contribute to technological advancement. This whitepaper synthesizes current research on skill dependency structures, analyzes methodological approaches for tracking career outcomes, and presents evidence-based frameworks for cultivating adaptive expertise in engineering education, with particular relevance to biomedical engineering and drug development professionals.
Theoretical Framework: Skill Dependencies and Career Pathways
The Nested Structure of Human Capital
Recent research analyzing US survey data and skill requirements has revealed a nested structure within skill portfolios, where directional dependencies create hierarchical relationships between foundational and specialized capabilities [72]. This structure is characterized by:
- Asymmetrical conditional probabilities where specialized skills typically depend on broader foundational skills
- Skill generality continuum ranging from general (applicable across many occupations) to specific (required by few specialized roles)
- Sequential acquisition patterns where advanced, specific skills build upon fundamental ones
This nested architecture explains why cognitive and technical skills—particularly those deeply embedded within dependency networks—along with managerial and social skills tend to command higher returns in the labor market [72].
Adaptive Expertise as an Educational Target
Adaptive expertise represents a critical dimension beyond technical proficiency, defined as the ability to apply knowledge to novel situations where key information is missing [73]. This contrasts with routine expertise, characterized by efficient performance in familiar tasks without the flexibility for novel problem-solving. Educational researchers have attempted to measure adaptive expertise through various methods including interviews, think-aloud protocols, and assignment-specific classroom assessments [73].
Table 1: Dimensions of Adaptive Expertise in Engineering
| Dimension | Routine Expertise | Adaptive Expertise |
|---|---|---|
| Knowledge Application | Application to familiar problems | Application to novel situations |
| Problem-Solving Approach | Efficient, standardized procedures | Flexible, innovative strategies |
| Response to Uncertainty | Reliance on established protocols | Tolerance for ambiguity and experimentation |
| Learning Orientation | Knowledge accumulation | Conceptual understanding and adaptation |
Methodological Approaches for Longitudinal Tracking
Tracking career trajectories requires robust methodological approaches capable of capturing professional development across extended timescales. Current research utilizes several data sources:
- Large-scale occupational surveys: The US Bureau of Labor Statistics provides detailed job requirement data, including skill importance and required proficiency levels across nearly a thousand occupations [72].
- Longitudinal resume analysis: Studies have analyzed millions of job transitions to identify patterns in skill acquisition and career progression [72].
- Synthetic birth cohorts: Tracking groups of individuals from early education through career establishment [72].
- Alumni assessment surveys: Systematic tracking of graduates' career trajectories and skill utilization [74] [54].
Skill Dependency Mapping
Research by Hosseinioun et al. demonstrates how skill dependencies can be quantified through analysis of occupational survey data [72]. Their methodology involves:
- Skill Level Assessment: Rating skill importance (1-5 scale) and required proficiency levels (0-7 scale) for each occupation
- Generality Classification: Categorizing skills as general (median level 3.34), intermediate (2.37), or specific (0.87) based on distribution across occupations
- Conditional Probability Analysis: Calculating the probability that one skill is required given the presence of another skill
- Network-Based Metrics: Applying measures like local reaching centrality and nestedness contributions to quantify skill relationships
This approach allows researchers to move beyond simple skill inventories to model the directed dependency network of human capital development.
Experimental Protocols for Tracking Adaptive Expertise
Educational Intervention Studies
Several research protocols have emerged for studying the development of adaptive expertise in engineering contexts:
Protocol 1: Biomedical Engineering Design Assessment
- Objective: Measure adaptive expertise development through novel design challenges
- Methodology: Present undergraduates with design scenarios from cardiologists' concerns about implantable defibrillators to assess approach to novel design challenges [73]
- Analysis: Qualitative assessment of problem-framing strategies, solution innovation, and application of fundamental principles
- Validation: Comparison between entry-level and senior students to measure developmental trajectories
Protocol 2: Longitudinal Biodesign Internship Tracking
- Program Structure: Three-semester sequence (junior year fall, spring, and summer) integrating clinical immersion, needs finding, and prototyping [75]
- Participant Selection: Academic record evaluation, extracurricular activities, performance in design components, faculty recommendations, and personal statements [75]
- Data Collection Points: Baseline assessment, post-clinical immersion, project completion, senior design performance, and post-graduation tracking
- Metrics: Technical skill application, innovation outcomes (patents, publications), career pathway selection, and long-term professional impact
Quantitative Assessment Instruments
Research instruments have been developed specifically to measure dimensions of adaptive expertise:
Engineering Creativity and Propensity for Innovation Index (ECPII)
- Constructs Measured: Engineering fluency, flexibility, disciplined imagination, originality, and design thinking [74]
- Format: 37-item instrument with 6-point Likert scale and scenario-based problem-solving items
- Validation: Application across multiple ERCs and engineering programs with demonstrated psychometric properties [74]
Adaptive Expertise Survey
- Target Populations: Freshmen, senior, and faculty engineering populations [73]
- Complementary Methods: Interviews conducted in conjunction with survey administration
- Application: Analysis of manifest adaptive behaviors in undergraduate engineering students
Table 2: Longitudinal Tracking Metrics for Adaptive Expertise
| Assessment Category | Specific Metrics | Data Collection Methods |
|---|---|---|
| Technical Skill Development | Skill generality profile, Dependency structure alignment, Proficiency progression | Skill inventories, Occupational surveys, Performance assessments |
| Innovation Capability | Patent production, Publications, Design competition outcomes, Novel solution generation | Portfolio analysis, Project documentation, Expert evaluation |
| Career Trajectory | Job transitions, Wage progression, Promotion velocity, Field mobility | Resume analysis, Employment surveys, Interviews |
| Problem-Solving Approach | Solution flexibility, Novel situation adaptation, Knowledge transfer efficiency | Think-aloud protocols, Design scenarios, Workplace observation |
Analysis of Adaptive Expertise Development Programs
Experiential Learning Integration
Evidence from biomedical engineering programs demonstrates the impact of integrated experiential learning on adaptive expertise development:
Clinical Immersion Model [32]
- Structure: Interdisciplinary courses pairing engineering students with nursing students for clinical observation and needs identification
- Protocol: Simulation-based training followed by real-world clinical setting visits
- Outcomes: Enhanced identification of unmet clinical needs, improved interdisciplinary communication, and development of viable engineering solutions addressing authentic healthcare challenges
Kolb's Experiential Learning Theory Application [54]
- Framework: Four-stage cycle of concrete experience, reflective observation, abstract conceptualization, and active experimentation
- Implementation: Structured reflection activities connecting co-curricular experiences to academic concepts
- Impact: Deeper learning integration and enhanced skill transfer to novel situations
Impact of Co-Curricular Experiences
Survey data from the 5th BME Educational Summit reveals participation patterns in co-curricular activities across institution types [54]:
Table 3: Co-Curricular Participation by Institution Type
| Institution Type | Undergraduate Research | Internships | Co-op Programs | Clinical Experiences |
|---|---|---|---|---|
| R1 Universities (n=49) | 60% | 36% | 12% | <10% |
| R2 Universities (n=11) | 37% | 48% | 36% | <10% |
| Predominantly Undergraduate (n=13) | 34% | 48% | 36% | <10% |
Data indicates that these valuable experiential learning activities are often not fully integrated into academic programs, with limited assessment of learning outcomes and structured reflection [54]. This represents a significant opportunity for enhancing adaptive expertise development through improved pedagogical design.
Career Outcomes and Trajectory Analysis
Skill Alignment and Economic Returns
Longitudinal analysis reveals that skills more aligned with the nested dependency structure command higher wage premiums, require longer education, and are less likely to be automated [72]. Key findings include:
- Structural Alignment Premium: Skills fitting the nested dependency structure correlate with 15-25% wage increases compared to similarly complex but less integrated skills
- Career Progression Patterns: Analysis of 70 million job transitions shows human capital development follows structured pathways where foundational skills enable acquisition of specialized, higher-value capabilities
- Automation Resilience: Nested skills demonstrate significantly lower susceptibility to automation displacement, with specific skills showing 30-50% higher retention rates
Demographic Variations in Career Pathways
Research indicates significant disparities in career trajectories across demographic groups:
Gendered STEM Pathways [76]
- Finding: Women and men show different STEM career attainment trajectories, with women particularly underrepresented in mathematical, engineering, physical, and computer science (MEPCS) occupations
- Pattern: Women in life, ecological, health and medical sciences (LEHMS) were more likely to follow a "no leak pipeline" compared to other STEM domains
- Workforce Dynamics: Though small, women's MEPCS workforce expanded to nearly twice its size from age 13 to 25, while the LEHMS workforce shrank to less than a third of its size among both men and women
These disparities in career pathways contribute to long-term wage penalties and illustrate how the nested structure of human capital can either create or inhibit mobility opportunities across demographic groups [72].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Methodological Tools for Career Trajectory Research
| Research Tool | Function | Application Context |
|---|---|---|
| Skill Generality Classification Algorithm | Quantifies skill applicability breadth across occupations | Analysis of occupational survey data to distinguish general, intermediate, and specific skills [72] |
| Conditional Probability Dependency Mapping | Identifies directional relationships between skill pairs | Construction of skill dependency networks from co-requirement patterns [72] |
| Engineering Creativity and Propensity for Innovation Index (ECPII) | Measures innovation-related constructs in engineering contexts | Assessment of creativity, flexibility, and design thinking in educational interventions [74] |
| Adaptive Expertise Survey Instrument | Evaluates ability to apply knowledge to novel situations | Tracking development of adaptive capabilities across educational progression [73] |
| Longitudinal Resume Analysis Pipeline | Processes large-scale career transition data | Identification of skill acquisition sequences and career pathway patterns [72] |
| Clinical Immersion Assessment Protocol | Evaluates needs identification and solution generation in healthcare contexts | Measuring adaptive expertise application in biomedical engineering education [75] [32] |
Longitudinal tracking of adaptively-trained engineers reveals the critical importance of structured skill dependencies in human capital development and career advancement [72]. The nested architecture of skills creates pathways where foundational capabilities enable acquisition of specialized, higher-value expertise—a structure that has become more pronounced over the past two decades [72].
For educational researchers and program designers, these findings highlight the necessity of:
- Intentional curriculum sequencing that mirrors natural skill dependencies
- Enhanced integration of co-curricular experiences through pedagogical frameworks like Kolb's ELT [54]
- Systematic assessment of adaptive expertise development beyond technical knowledge acquisition
- Targeted interventions to address demographic disparities in career trajectories
The development of adaptive expertise represents a crucial frontier in engineering education, particularly in rapidly evolving fields like biomedical engineering and drug development. By understanding and leveraging the structural relationships between skills, educational programs can more effectively prepare engineers for the complex, novel challenges they will face throughout their careers. Future research should focus on refining assessment methodologies, expanding longitudinal tracking initiatives, and developing educational interventions that explicitly target the development of adaptive capabilities alongside technical proficiency.
This whitepaper synthesizes current industry and clinical stakeholder perspectives on the preparedness of biomedical engineering (BME) graduates. Within the broader thesis of adaptive expertise development, findings reveal a critical evolution in competency expectations. While a strong technical foundation remains essential, stakeholders increasingly prioritize professional competencies—such as communication, collaboration, and critical thinking—deemed vital for navigating rapid technological advancements and interdisciplinary work environments. This analysis validates the need for educational frameworks that cultivate these adaptive skills, detailing specific competency gaps, experimental protocols for curriculum intervention, and actionable strategies for aligning academic preparation with the evolving demands of the biomedical field.
Biomedical engineering is a rapidly evolving field, characterized by technological breakthroughs, increasing complexity of human health challenges, and a globalized workforce [5]. A key indicator of BME program success is a graduate's readiness to contribute meaningfully to industry roles, with over 40% of undergraduate graduates finding their first placement in this sector [5]. The emergence of major technological innovations, including artificial intelligence (AI) and machine learning, has transformed how engineering problems are solved, necessitating a shift in the competencies required of graduates [5]. This document explores the specific competencies prioritized by industry and clinical stakeholders, framing these findings within the context of adaptive expertise development. Adaptive expertise refers to the ability to apply knowledge flexibly and creatively to novel problems, a capacity essential for lifelong contribution in a dynamic field like BME.
Quantitative Analysis of Stakeholder Perspectives
Data collected from industry and academic stakeholders highlight a significant shift in the perceived importance of professional versus technical competencies.
Table 1: Evolution of Key Competency Priorities from 2019 to 2024 BME Education Summits [5]
| Competency | Ranking in 2019 Summit | Ranking in 2024 Summit | Shift in Emphasis |
|---|---|---|---|
| Communication Skills | Ranked 2nd (Interpersonal), 5th (Writing), 6th (Technical Presentation) | Ranked 1st | Increased Priority |
| Problem-Solving/Critical Thinking | Ranked 1st | Ranked 3rd | Decreased Priority Relative to Professional Skills |
| Teamwork/Collaboration | Ranked 4th | Ranked 2nd | Increased Priority |
| Programming/Data Science | Not in Top Rankings | Ranked 4th | Newly Emphasized |
Table 2: Quantitative Findings from a Pilot Study on BME Student Competencies [77]
| Competency Domain | Assessment Method | Key Finding | Cronbach's Alpha (Reliability) |
|---|---|---|---|
| Theoretical Knowledge | Structured questionnaire (30 students) | Strong theoretical foundation | 0.739 - 0.932 (High Consistency) |
| Practical Skills | Structured questionnaire (30 students) | Need for enhanced hands-on training | 0.739 - 0.932 (High Consistency) |
| Industry Alignment | Analysis across six domains (theory, operation, safety, etc.) | Gap between academic preparation and industry expectations | N/A |
Experimental Protocols for Curriculum Development and Validation
To address identified competency gaps, researchers and educators have developed and implemented targeted educational interventions. The following protocols provide validated methodologies for cultivating adaptive expertise.
Protocol: The NICE Strategy for Comprehensive BME Education
The NICE strategy is a multi-faceted educational approach designed to address challenges in BME teaching, including curriculum gaps, ethical considerations, and lack of practical integration [78].
- 1. Objective: To provide a well-rounded learning experience that equips BME students with up-to-date knowledge, critical and creative thinking skills, a strong sense of integrity, and practical experience.
- 2. Materials and Setup:
- Course Structure: Implement the strategy within a dedicated course (e.g., "Medical Diagnostic Frontier Technology and Innovation Applications").
- AI Tools: Provide access to AI-based tools (e.g., DeepSeek, ChatGPT, Kimi) to assist with literature search and summarization.
- Stakeholder Network: Establish a network of clinical doctors and industry R&D directors to participate in teaching and mentoring.
- 3. Procedure - Component Implementation:
- New Frontier (N):
- Assign students to research articles published within the last two years.
- Students summarize articles and present findings orally in class.
- Utilize AI tools to overcome difficulties in searching for and understanding complex publications.
- Integrity (I):
- Adopt a case-study-based approach.
- Present positive examples (e.g., renowned scientists, successful faculty) to illustrate innovation and perseverance.
- Analyze negative cases (e.g., Theranos fraud) to demarcate ethical boundaries.
- Critical and Creative Thinking (C):
- Engage students in case-based discussions on real-world BME dilemmas (e.g., new drug development, medical device ethics).
- Require students to provide their own insights and critiques during oral presentations.
- Assign peers as reviewers to evaluate presentations based on clarity, depth of analysis, and validity of conclusions.
- Engagement (E):
- Invite clinical and industry experts to teach product development sections.
- Form student groups (3-5 members) to develop a design plan for a novel clinical product.
- Task students with interviewing clinical doctors to identify unmet needs and working with industrial mentors to translate needs into a viable product design.
- New Frontier (N):
- 4. Analysis and Validation:
- Compare student performance and satisfaction surveys from before and after the implementation of the NICE strategy.
- Track student outcomes over a multi-year period to assess long-term impact on professional development [78].
Protocol: Team-Based Design with Clinical Immersion
This protocol, aligned with funding initiatives from the National Institute of Biomedical Imaging and Bioengineering (NIBIB), focuses on hands-on, clinically relevant design experiences [30].
- 1. Objective: To prepare future engineers who can address the mission of leading the development and accelerating the translation of biomedical technologies through team-based design and clinical immersion.
- 2. Materials and Setup:
- Design Course: Establish or enhance a team-based design course within an undergraduate BME program.
- Clinical Partnerships: Forge relationships with local hospitals or clinical environments.
- Funding: Secure funding for parts, supplies, prototyping, and student salaries during immersion periods.
- 3. Procedure:
- Needs Identification: Involve students in the needs assessment and project identification process within a clinical setting, rather than assigning predetermined projects.
- Clinical Immersion: Engage students in a full-time, 6- to 10-week program in a hospital or clinical environment.
- Clinical Mentorship: Conduct immersion under the supervision of clinical mentor(s), with rotations across various hospital departments.
- Project Development: The primary purpose is observation, acquiring clinical communication skills, and identifying unmet needs that can be addressed in subsequent biomedical design projects.
- 4. Analysis and Validation:
- Evaluate the effectiveness of the educational practice through surveys and assessment tools, which may be characterized as human subjects research and require IRB review [30].
- Assess the number and quality of unmet needs identified and the subsequent design projects generated.
The Scientist's Toolkit: Research Reagent Solutions for Educational Validation
Table 3: Essential Materials for BME Education Research and Validation
| Item | Function in Educational Research |
|---|---|
| Structured Competency Questionnaires | Validated instruments to reliably assess student competencies across multiple domains (e.g., theory, operation, safety, servicing) [77]. |
| AI-Assisted Research Tools (e.g., DeepSeek, ChatGPT) | To help students navigate and understand complex, current research literature, thereby accelerating the "New Frontier" learning component [78]. |
| Clinical Immersion Framework | A structured 6-10 week program facilitating student observation and need identification in clinical settings, crucial for authentic project development [30]. |
| Industry Project Partnerships | Collaborative agreements with companies to provide real-world objectives for student capstone projects, bridging the gap between academia and industry [78]. |
| Ethical Case Studies Library | A curated collection of real-world cases (e.g., Theranos, Human Genome Project) to facilitate the teaching of integrity and ethical reasoning [78]. |
Visualizing the Clinical Immersion and Design Workflow
The following diagram details the workflow for integrating clinical immersion with team-based design, a critical protocol for fostering adaptive expertise and addressing stakeholder-identified gaps in practical skills.
Discussion and Synthesis
Synthesis of stakeholder perspectives reveals a clear mandate for BME education that prioritizes the development of adaptive expertise. The data indicates that while technical competencies are an expected outcome of accredited programs, the "difficult-to-teach" professional skills are now the primary differentiators for industry readiness [5]. The experimental protocols detailed herein—the NICE strategy and team-based clinical immersion—provide validated, actionable frameworks for embedding these competencies into the curriculum. Furthermore, the strong emphasis on data science skills, coupled with ethical understanding, underscores the need for curricula that interconnect technical and professional learning, preparing graduates to contribute in an ethically and socially responsible manner amidst the field's rapid evolution [5] [78].
Adaptive expertise represents a critical form of mastery for biomedical engineering professionals, enabling them to navigate the field's rapidly evolving challenges. Unlike routine expertise that emphasizes efficiency in familiar situations, adaptive expertise integrates this efficiency with the capacity to innovate when confronting novel problems in complex, dynamic environments such as medical technology development, clinical implementation, and interdisciplinary healthcare research [79]. This conceptual framework, originally pioneered by educational psychologists, has gained significant traction in health professions education and is now recognized as essential for biomedical engineering graduates facing technological disruptions from AI, novel therapeutic modalities, and increasingly complex healthcare systems [67] [5].
The distinction between routine and adaptive expertise is particularly salient for biomedical engineering, where professionals must balance established procedures with the generation of novel solutions for unique clinical needs. Where routine experts excel at performing highly practiced tasks quickly and flawlessly, adaptive experts possess the underlying conceptual understanding to deconstruct unfamiliar problems and develop context-specific solutions [79]. This adaptability is increasingly crucial as biomedical engineers confront problems that don't fit standard models, such as developing personalized medical devices, creating novel diagnostic platforms for emerging diseases, or integrating artificial intelligence into clinical decision-making [80] [5].
Conceptual Foundations and Definitions
Adaptive expertise is fundamentally characterized by a balance between two dimensions: efficiency in applying existing knowledge to solve familiar problems, and innovation in generating new solutions when confronted with novelty, uncertainty, and ambiguity [15]. This dual nature distinguishes it from routine expertise, which primarily demonstrates efficiency within known parameters but may struggle when faced with significantly new situations [67]. The concept, first introduced by Hatano and Inagaki in 1986, positions adaptive expertise as complementary to routine expertise, with both being essential for professional effectiveness in biomedical engineering [6] [67].
A critical aspect of adaptive expertise is the relationship between adaptive expertise (the underlying knowledge and cognitive capacities) and adaptive performance (the visible expression of these capacities when triggered by change or novelty) [6] [67]. This distinction is important for assessment, as adaptive expertise represents the latent capability while adaptive performance manifests as observable behaviors in response to novel challenges. The scope of "change" that triggers adaptive performance exists on a continuum from situations that are merely "new for the learner" to those that are "new for everyone in the whole world" [67].
Table 1: Core Dimensions of Adaptive Expertise
| Dimension | Routine Expertise Emphasis | Adaptive Expertise Emphasis |
|---|---|---|
| Knowledge Application | Efficient execution of known procedures | Flexible use of knowledge across contexts |
| Problem-Solving Approach | Applying pre-existing solutions | Generating novel solutions through conceptual understanding |
| Response to Novelty | May struggle with significant novelty | Engages productively with unfamiliar problems |
| Learning Orientation | Focus on mastery of existing knowledge | Emphasis on continuous learning and knowledge creation |
| Error Handling | Views errors as failures | Views errors as learning opportunities |
The theoretical foundations of adaptive expertise emphasize cognitive integration—the deep, conceptual knowledge developed through connecting clinical and biomedical sciences [15]. This integrated understanding enables professionals to adapt to variability in novel clinical and engineering situations by understanding not just what to do but why certain approaches work, allowing them to generate appropriate solutions even when standard protocols are insufficient [15]. This conceptual depth permits what has been termed "preparation for future learning" (PFL)—the capacity to learn and generate new knowledge continuously throughout one's career [15].
Measurement Instruments and Assessment Frameworks
A comprehensive scoping review of measurement instruments for adaptive expertise and adaptive performance identified 19 distinct assessment tools, only three of which were specifically developed for the healthcare domain [6]. These instruments can be categorized into six primary types: (1) self-evaluation instruments, (2) job requirement instruments, (3) knowledge and problem-solving tasks, (4) design scenarios, (5) mixed-methods approaches, and (6) collegial verbalization protocols [6]. The review revealed a predominance of self-evaluation and job requirement instruments, with other methods such as design scenarios and mixed-methods approaches being underrepresented despite their potential value [6].
The instruments varied significantly in their operationalization of adaptive expertise and adaptive performance, with underlying conceptualizations ranging from a focus on cognitive flexibility and problem-solving innovation to behavioral adaptation in changing work situations [6]. This variation highlights the conceptual complexity of adaptive expertise and the importance of selecting assessment tools that align with the specific aspects of adaptability one aims to measure—whether for formative development purposes, summative evaluation, or research on expertise development.
Table 2: Categories of Adaptive Expertise Assessment Instruments
| Instrument Category | Description | Common Applications | Key Characteristics |
|---|---|---|---|
| Self-Evaluation Instruments | Questionnaires assessing self-perceived adaptive capabilities | Healthcare education, professional development | Efficient to administer; subject to self-assessment biases |
| Job Requirement Instruments | Assessments of adaptive performance requirements in specific roles | Workforce development, human resources | Focused on workplace application; context-dependent |
| Knowledge and Problem-Solving Tasks | Performance-based assessments measuring conceptual understanding | Educational research, cognitive science | Objective performance metrics; may lack ecological validity |
| Design Scenarios | Ill-structured problems requiring innovative solutions | Engineering education, design fields | Authentic to professional practice; resource-intensive to score |
| Mixed-Methods Approaches | Combination of quantitative and qualitative assessment methods | Comprehensive program evaluation | Rich data; complex analysis requirements |
| Collegial Verbalization | Analysis of verbal protocols during problem-solving | Cognitive task analysis, expertise research | Provides process insights; requires specialized analysis |
Quality Assessment of Instruments
According to the Standards for Educational and Psychological Testing, the fundamental quality criteria for assessment instruments are validity (evidence supporting test score interpretations), reliability (consistency of scores), and fairness (equitable treatment of all test-takers) [6]. The scoping review evaluated the amount of evidence supporting these quality criteria across the identified instruments and found considerable variation [6]. Only a limited number of instruments demonstrated robust evidence for both validity and reliability, with instruments specifically developed for healthcare settings generally requiring further validation and reliability testing [6].
The analysis of operationalizations across instruments led to the identification of 13 thematic subscales that provide clarity on how adaptive expertise and performance are conceptualized in practice [6]. These themes include cognitive flexibility, problem-solving innovation, handling emergencies, interpersonal adaptability, creative solution generation, dealing with uncertain situations, learning orientation, and several others [6]. This categorization offers researchers and educators a clearer framework for selecting or developing instruments that target specific aspects of adaptive expertise relevant to their context.
Implementation and Methodological Protocols
Assessment Implementation Framework
Implementing adaptive expertise assessment requires careful methodological consideration. The following workflow outlines a comprehensive approach to assessing adaptive expertise in biomedical engineering education contexts:
Experimental Protocols for Assessing Adaptive Expertise
Protocol 1: Design Scenario Assessment
Purpose: To evaluate adaptive expertise through performance on ill-structured problems that simulate real-world biomedical engineering challenges. Materials: Case materials describing unmet clinical needs, prototyping resources, data analysis tools. Procedure:
- Present participants with a novel clinical problem lacking established solutions (e.g., designing a low-cost diagnostic device for resource-limited settings)
- Allow 3-5 hours for problem analysis, solution generation, and prototype planning
- Record all ideation processes, solution attempts, and pivot points
- Conduct structured post-task interviews exploring reasoning processes Metrics: Solution novelty, feasibility, conceptual understanding demonstrated, number of distinct approaches generated, effectiveness of iterative improvements [6] [80].
Protocol 2: Longitudinal Interprofessional Collaboration Assessment
Purpose: To measure adaptive expertise development through extended team-based projects with clinical partners. Materials: Project guidelines, clinical access protocols, interdisciplinary team resources. Procedure:
- Form interdisciplinary teams (engineering students, nursing students, clinical mentors)
- Assign design challenge addressing authentic clinical needs
- Implement weekly progress assessments with reflective components
- Conduct midpoint and final design reviews with clinical and industry experts
- Administer pre-post assessments of design self-efficacy and collaborative competencies Metrics: Design confidence growth, collaborative competency development, clinical need translation quality, final solution innovation [81].
Protocol 3: Cognitive Integration Assessment
Purpose: To evaluate deep conceptual understanding connecting biomedical sciences with engineering principles. Materials: Clinical case scenarios, concept mapping tools, explanation prompts. Procedure:
- Present complex clinical cases with ambiguous presentation
- Ask participants to explain underlying mechanisms connecting clinical signs to biological principles
- Require justification of engineering approach based on mechanistic understanding
- Analyze responses for conceptual depth and integration across knowledge domains Metrics: Accuracy of mechanistic explanations, number of cross-domain connections, appropriateness of engineering solutions based on biological understanding [15].
Table 3: Research Reagent Solutions for Adaptive Expertise Assessment
| Assessment Tool | Function | Application Context |
|---|---|---|
| Ill-Structured Problem Scenarios | Presents open-ended challenges with multiple solution pathways | Design assessment, clinical problem-solving evaluation |
| Reflective Practice Platforms | Guides structured reflection on problem-solving processes | Development of metacognitive skills, formative assessment |
| Interprofessional Collaboration Rubrics | Measures teamwork across disciplinary boundaries | Assessment of collaborative adaptive performance |
| Concept Mapping Tools | Visualizes knowledge structures and connections | Evaluation of cognitive integration across domains |
| Simulation Environments | Recreates authentic clinical and engineering challenges | Performance assessment in near-authentic contexts |
| Structured Interview Protocols | Elicits reasoning processes and conceptual understanding | Qualitative assessment of adaptive expertise components |
Applications in Biomedical Engineering Education
Curriculum Integration and Development
Biomedical engineering programs have implemented various strategies to develop and assess adaptive expertise. The Meinig School at Cornell University has embedded design-centered learning throughout its curriculum, restructuring introductory courses, experiential learning seminars, and senior capstone design projects to emphasize design thinking, active learning, and flipped classroom models [23]. This approach intentionally creates the cognitive challenges and variation necessary to develop adaptive capabilities rather than just routine proficiency.
The NICE (New Frontier, Integrity, Critical and Creative Thinking, Engagement) strategy represents another systematic approach to fostering adaptive expertise in biomedical engineering education [80]. This framework addresses multiple dimensions of adaptability:
- New Frontier: Students study recent research and emerging technologies, developing capacity to rapidly acquire new knowledge
- Integrity: Case studies of ethical challenges prepare students for novel ethical dilemmas they may encounter
- Critical and Creative Thinking: Analysis of creative ideas and generation of novel solutions builds innovation capabilities
- Engagement: Direct interaction with clinical and industry partners provides authentic contexts for adaptation [80]
These educational approaches align with evidence that adaptive expertise development requires cognitive integration of knowledge across domains, exposure to meaningful variation in problems, and opportunities to engage in productive struggle followed by timely feedback [15].
Assessment in Interprofessional Contexts
The integration of nursing students into biomedical engineering capstone design courses at the University of Pittsburgh provides a compelling model for assessing adaptive expertise in interprofessional contexts [81]. This five-year interdisciplinary partnership demonstrated significant benefits for both engineering and nursing students, including increased design confidence and enhanced interprofessional collaborative competencies [81]. The partnership employed multiple assessment methods, including pre-post design self-efficacy surveys, retrospective pre-post interprofessional collaborative competency assessments, and qualitative interviews to capture developmental trajectories [81].
This approach exemplifies how adaptive expertise assessment can capture growth in both technical adaptability (applying engineering principles to novel clinical problems) and collaborative adaptability (adjusting communication and teamwork approaches across disciplinary boundaries). Biomedical engineering students reported that nursing students' clinical knowledge and perspectives provided valuable insights for identifying and addressing unmet clinical needs, creating the novel problem-solving contexts that trigger adaptive performance [81].
Future Directions and Implementation Challenges
Addressing Measurement Limitations
Current assessment of adaptive expertise faces several significant challenges. Traditional evaluation methods often prioritize efficiency and procedural accuracy, thereby rewarding routine performance over conceptual flexibility and innovation [79]. Effective assessment requires tasks that introduce complexity, ambiguity, and non-standard constraints, forcing examinees to rely on deep conceptual understanding rather than automated solutions [79]. This often necessitates qualitative assessment methods, such as think-aloud protocols or detailed analysis of solution justifications, which are more resource-intensive than standardize testing [6] [79].
Future development of assessment frameworks should address the current underrepresentation of certain instrument types, particularly design scenarios and mixed-methods approaches, which show promise for capturing the innovative aspects of adaptive expertise [6]. There is also a need for greater integration of neurocognitive measures that can provide insights into the neural mechanisms underlying adaptive performance, potentially offering more objective indicators of cognitive flexibility and conceptual innovation.
Domain-Specific Adaptations for Biomedical Engineering
The biomedical engineering field presents unique challenges for adaptive expertise assessment due to its highly interdisciplinary nature and the critical consequences of engineering decisions in healthcare contexts [80] [5]. Future assessment frameworks must address domain-specific aspects of adaptability, including:
- Regulatory navigation: Adapting solutions to meet evolving regulatory requirements
- Clinical translation: Modifying technologies based on clinical feedback and real-world constraints
- Ethical innovation: Generating novel solutions while maintaining ethical standards with patient safety implications
- Interdisciplinary communication: Adapting communication approaches across engineering, clinical, and business contexts
The rapid evolution of biomedical technologies, particularly in areas such as AI-driven diagnostics, CRISPR gene editing, and personalized medicine, necessitates assessment approaches that can capture professionals' capacity to adapt to technologies that emerge after their formal education [80] [5]. This requires focusing assessment not just on current knowledge but on preparation for future learning and the ability to rapidly acquire and apply new knowledge in novel contexts [15].
As biomedical engineering continues to evolve, the development of robust, domain-specific assessment frameworks for adaptive expertise will be essential for ensuring graduates can navigate the complex, unpredictable challenges at the intersection of engineering, biology, and medicine. These frameworks must balance methodological rigor with practical feasibility, providing meaningful insights for educational improvement while acknowledging the multifaceted nature of adaptive expertise in biomedical contexts.
Conclusion
The development of adaptive expertise represents a paradigm shift in biomedical engineering education, essential for preparing professionals who can navigate the complexities of modern healthcare innovation and drug development. The synthesis of evidence reveals that adaptive expertise—characterized by deep conceptual understanding, cognitive flexibility, and innovative problem-solving—is not automatically acquired through traditional education but must be deliberately cultivated through transdisciplinary curricula, clinical immersion, and experiential learning. While implementation challenges exist, from resource allocation to assessment methodologies, the demonstrated correlation between adaptive expertise and enhanced work performance underscores its critical value. Future directions must include developing standardized assessment frameworks, expanding faculty development programs, and creating institutional policies that support transdisciplinary collaboration. For biomedical and clinical research, embracing these educational approaches will yield a generation of professionals equipped to address unprecedented challenges in therapeutic development, medical device innovation, and healthcare system optimization, ultimately accelerating the translation of engineering breakthroughs into clinical applications that improve patient outcomes.
References
- 1. Relationship of adaptive expertise of health professions ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-05838-9]
- 2. Under the hood of Adaptive Expertise - by Sarah Cottinghatt [https://cognitivecoaching.substack.com/p/adaptive-expertise-what-it-is-and]
- 3. Cognitive Load Theory [https://thedecisionlab.com/reference-guide/psychology/cognitive-load-theory]
- 4. Cognitive Load Theory and its application in the classroom [https://my.chartered.college/impact_article/cognitive-load-theory-and-its-application-in-the-classroom/]
- 5. A Future-Focused Lens to Equipping Biomedical ... [https://link.springer.com/article/10.1007/s43683-025-00186-6]
- 6. a scoping review of measurement instruments - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572040/]
- 7. Review How experts deal with novel situations [https://www.sciencedirect.com/science/article/abs/pii/S1747938X14000116]
- 8. Biomedical engineering teaching: challenges and the ... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0003/html?srsltid=AfmBOorrOJvBF6UsJ7tibZGE6DP0agTEnOj-KN5HXeeK1XCIPH28gHyv]
- 9. Biomedical engineering teaching: challenges and the ... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0003/html?srsltid=AfmBOoo7RMcxVt0Tkn_zcOiZTAXlsJRij0FbJBxJ2jKH7KVM183pYXAv]
- 10. Teaching for adaptive expertise in biomedical engineering ... [https://pubmed.ncbi.nlm.nih.gov/15915863/]
- 11. Research & Projects - McCormick School of Engineering [https://www.mccormick.northwestern.edu/research/engineering-education-research-center/research-projects/]
- 12. Concept Mapping as a Metacognition Tool in a Problem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8923101/]
- 13. MENTOR: A Metacognition-Driven Self-Evolution ... [https://arxiv.org/html/2511.07107v1]
- 14. Understanding disciplinary perspectives: a framework to ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-05913-1]
- 15. Adaptive Expertise in CanMEDS 2025 - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10042796/]
- 16. a scoping review of measurement instruments [https://link.springer.com/article/10.1007/s10459-025-10413-y]
- 17. Advancing Biomedical Engineering Education: Summit ... [https://bioengineer.org/advancing-biomedical-engineering-education-summit-highlights-revealed/]
- 18. Adaptive Expertise Development during Work-Based ... [https://link.springer.com/article/10.1007/s12186-025-09366-5]
- 19. Embedding Studio-Based Learning in the Biomedical ... [https://link.springer.com/article/10.1007/s43683-025-00195-5]
- 20. Understanding disciplinary perspectives: a framework to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11401306/]
- 21. Adaptive Behaviors of Experts in Following Standard Protocol ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3540446/]
- 22. Biomedical engineering teaching: challenges and the ... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0003/html?srsltid=AfmBOoq1uiF2ax6r2Xal2sDKXdsiOOwRAzjgwCSNKUvh1WUqUNm3MTlm]
- 23. Meinig School leads innovation in engineering education [https://www.engineering.cornell.edu/bme/2025/09/12/revolutionizing-how-we-teach-meinig-school-leads-innovation-in-engineering-education/]
- 24. Transdisciplinary experiential learning in biomedical ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-023-04171-x]
- 25. The future of biomedical engineering education is ... [https://link.springer.com/article/10.1007/s13246-024-01442-9]
- 26. Adaptive Expertise and Knowledge Fluency in Design ... [https://www.cambridge.org/core/books/cambridge-handbook-of-engineering-education-research/adaptive-expertise-and-knowledge-fluency-in-design-and-innovation/1F1025C606A58A41C2370AE57AB8C090]
- 27. Biomedical engineering and interdisciplinary research in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271602/]
- 28. Bioengineering students tackle health care disparities ... [https://news.rice.edu/news/2025/bioengineering-students-tackle-health-care-disparities-through-clinical-immersion-program]
- 29. Exploring Student Experiences in a Transdisciplinary ... [https://link.springer.com/article/10.1007/s43683-025-00201-w]
- 30. Team-Based Design in Biomedical Engineering Education ... [https://www.nibib.nih.gov/programs/division-interdisciplinary-training-didt/team-based-design-biomedical-engineering-education-r25]
- 31. Biomedical engineering teaching: challenges and the ... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0003/html?srsltid=AfmBOoqm-0B1ry5H8ZzSjZ7fRzF4RHhOETxj92XaHklb1vt-67JdAdd9]
- 32. Improving Biomedical Engineering Education Through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6056190/]
- 33. Advancing Problem - Based in Learning in... Biomedical Engineering [https://arxiv.org/html/2503.16558v1]
- 34. - Problem in Biomechanics: Advantages, Challenges... Based Learning [https://pubmed.ncbi.nlm.nih.gov/27210616/]
- 35. Embracing Errors to Develop Adaptive Expertise [https://icenet.blog/2022/04/26/exploration-before-explanation-embracing-errors-to-develop-adaptive-expertise/]
- 36. Biomedical engineering teaching: challenges and the ... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0003/html?srsltid=AfmBOoopTMqGefjL73vLQUg4gLjTVdJUrOYOGyJzBB2cVwZnJ2klDw_4]
- 37. Biomedical engineering teaching: challenges and the ... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0003/html?srsltid=AfmBOoqTAGVodMf1EyiC_Rd_M_-fxFnS_6WRQeeCFYIV3StDV_f56o2L]
- 38. Revamping Biomedical Education Through Stakeholder ... [https://bioengineer.org/revamping-biomedical-education-through-stakeholder-engagement/]
- 39. A Model of Knowledge Sharing in Biomedical Engineering [https://www.businesschemistry.org/article/a-model-of-knowledge-sharing-in-biomedical-engineering-challenges-and-requirements/]
- 40. Collaboration for clinical innovation: a nursing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7932479/]
- 41. Strategies for Medical Device Development: User and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10241585/]
- 42. A Collaborative Data Sharing Platform to Accelerate ... [https://www.mdpi.com/2306-5354/12/9/938]
- 43. Identifying stakeholder preferences for communicating impact ... [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-024-11664-y]
- 44. Characterizing Computational Adaptive Expertise [https://peer.asee.org/characterizing-computational-adaptive-expertise]
- 45. Biomedical Engineering Professional Skills Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC8115220/]
- 46. Innovative strategies for interdisciplinary medical-engin... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0005/html?srsltid=AfmBOoprjCqqoLar2qbvtFqoztmhv0AMFfeu79EycjXf0DLxYxTvRtrt]
- 47. Identifying and Overcoming Barriers to Classroom ... [https://link.springer.com/article/10.1007/s43683-025-00176-8]
- 48. a study within the context of medical education in Iran - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613663/]
- 49. Exploring faculty development initiatives in medical education ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-025-07848-7]
- 50. Emerging Trends in Biomedical Engineering [https://online-engineering.case.edu/blog/emerging-trends-in-biomedical-engineering]
- 51. Trend Overview 2025: Key Developments in Biomedical ... [https://biomedgrid.com/fulltext/volume25/trend-overview-2025-key-developments-in-biomedical-science-research.003320.php]
- 52. Relationship of adaptive expertise of health professions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11316990/]
- 53. Transdisciplinary experiential learning in biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10069080/]
- 54. Integration of Co-Curricular Experiential Learning in BME ... [https://link.springer.com/article/10.1007/s43683-025-00183-9]
- 55. Biomedical engineering teaching: challenges and the ... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0003/html?srsltid=AfmBOorNrx3FHtcHUJullNaebZYBcCSg8OdD44jZHzHIZeHkdoKRCqLm]
- 56. Developing Industry-Ready Engineers | Biomedical ... [https://link.springer.com/article/10.1007/s43683-025-00171-z]
- 57. Datawiz-IN: fostering representative innovation in health data ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-025-07298-1]
- 58. A transdisciplinary dual degree curriculum yields novel and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11906449/]
- 59. Towards unbiased assessment of adaptive expertise [https://teaching-and-learning-collection.sites.uu.nl/project/towards-unbiased-assessment-of-adaptive-expertise/]
- 60. Master of Engineering - School of Biomedical Engineering [https://www.engr.colostate.edu/sbme/graduate-programs/master-of-engineering/]
- 61. An Adaptive Blended Learning Model for the Implementation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8239699/]
- 62. Personalized adaptive learning in higher education: A ... [https://www.sciencedirect.com/science/article/pii/S2405844024156617]
- 63. Implementing a challenge-based learning experience in a ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-05462-7]
- 64. Creating Inclusive Environments to Support Learning and ... [https://link.springer.com/article/10.1007/s43683-025-00189-3]
- 65. How we designed an accessible color palette from scratch [https://medium.com/wttj-tech/how-we-designed-an-accessible-color-palette-from-scratch-f29ec603bd7f]
- 66. Best Color Palettes for Scientific Figures and Data ... [https://www.simplifiedsciencepublishing.com/resources/best-color-palettes-for-scientific-figures-and-data-visualizations]
- 67. Professionals' adaptive expertise and adaptive performance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9859848/]
- 68. An Academic Viewpoint (2025) on the Integration of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12020443/]
- 69. Improving the learning-teaching process through adaptive ... [https://slejournal.springeropen.com/articles/10.1186/s40561-024-00314-9]
- 70. Challenge-based instruction in biomedical engineering [https://www.sciencedirect.com/science/article/abs/pii/S1350453305001062]
- 71. Dr. Paul Hungler's Vision for Smarter, Faster Learning [https://www.queensu.ca/connected-minds/adaptive-learning-paul-hungler]
- 72. Skill dependencies uncover nested human capital - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12018457/]
- 73. Measuring Adaptive Expertise in Engineering Education [https://www.semanticscholar.org/paper/Measuring-Adaptive-Expertise-in-Engineering-Pierrakos-Anderson/9bc863d6cd67ecfdd67354fbf47fdd7dc50e8591]
- 74. Appendix 4.6: Assessment and Evaluation examples [http://erc-assoc.org/best-practices/appendix-46-assessment-and-evaluation-examples]
- 75. A Longitudinal and Interdisciplinary Biodesign Internship ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383801/]
- 76. Not a pipeline but a highway: Men's and women's STEM ... [https://www.sciencedirect.com/science/article/pii/S0001879124001088]
- 77. Improving Industry Readiness: Insights from a Pilot Study of ... [https://hrmars.com/ijarbss/article/view/24909/Improving-Industry-Readiness-Insights-from-a-Pilot-Study-of-Biomedical-Engineering-Program]
- 78. Biomedical engineering teaching: challenges and the ... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0003/html?srsltid=AfmBOoqQZ0Ku6G2F7sHLlu72nUVmJgBA_mBnFUuAFj5IFRY1aHmEXOsq]
- 79. Adaptive Expertise: Skills for a Changing World [https://psychepedia.arabpsychology.com/trm/adaptive-expertise-skills-for-a-changing-world/]
- 80. Biomedical engineering teaching: challenges and the ... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0003/html?srsltid=AfmBOopoYz-gJZhAyfCUWNd8gmDP4TtbEFumF0MF_6CXLwr_i-cpVF95]
- 81. Top 34 Biomedical engineering education papers ... [https://scispace.com/journals/biomedical-engineering-education-1r79ubw6/2025]