Edge-Enhanced Vision: Advancing Medical Image Analysis with Edge Information-Based Methods
This article provides a comprehensive exploration of edge information-based methods for medical image enhancement, a critical domain for improving diagnostic accuracy and computational analysis.
Edge-Enhanced Vision: Advancing Medical Image Analysis with Edge Information-Based Methods
Abstract
This article provides a comprehensive exploration of edge information-based methods for medical image enhancement, a critical domain for improving diagnostic accuracy and computational analysis. It establishes the foundational role of edge detection in the broader context of medical image segmentation, contrasting traditional techniques with modern deep learning paradigms. The content details specific methodologies and their clinical applications across diverse imaging modalities, including CT, MRI, and X-ray, addressing key challenges such as noise, computational cost, and boundary ambiguity. A thorough evaluation of performance against other segmentation strategies is presented, alongside a forward-looking analysis of how integrating edge priors with emerging technologies like transformers and diffusion models is shaping the future of robust, interpretable clinical AI tools.
The Fundamental Role of Edge Information in Medical Image Analysis
Medical image segmentation and enhancement are fundamental techniques in computational medical image analysis, aimed at improving the quality of images and extracting clinically meaningful regions. These processes are critical for supporting diagnosis, treatment planning, and drug development. Segmentation involves partitioning an image into distinct regions, such as organs, tissues, or pathological areas, while enhancement focuses on improving visual qualities like contrast and edge sharpness to facilitate interpretation. The integration of edge information has emerged as a powerful paradigm for advancing both tasks, as precise boundary delineation is often a prerequisite for accurate segmentation and clinically useful enhancement. This document provides application notes and experimental protocols for contemporary methods in this field, framed within research on medical image enhancement using edge information-based techniques.
State-of-the-Art Frameworks and Quantitative Analysis
Recent research has produced significant advancements in segmentation and enhancement by leveraging edge information. The table below summarizes the quantitative performance of several state-of-the-art methods on various medical image segmentation tasks.
Table 1: Performance Comparison of State-of-the-Art Medical Image Segmentation and Enhancement Methods
| Method Name | Core Innovation | Reported Metric(s) & Performance | Dataset(s) Used for Validation |
|---|---|---|---|
| EGBINet [1] | Edge-guided bidirectional iterative network with transformer-based feature fusion. | Remarkable performance advantages; superior edge preservation and complex structure accuracy. | ACDC, ASC, IPFP [1] |
| Enhanced Level Set with PADMM [2] | Novel level set evolution with an improved edge indication function and efficient PADMM optimization. | Average Dice: 0.96; Accuracy: 0.9552; Sensitivity: 0.8854; MAD: 0.0796; Avg. Runtime: 0.90s [2] | Not specified in abstract [2] |
| Topograph [3] | Graph-based framework for strictly topology-preserving segmentation. | State-of-the-art performance; 5x faster loss computation than persistent homology methods. [3] | Binary and multi-class datasets [3] |
| Contrast-Invariant Edge Detection (CIED) [4] | Edge detection using three Most Significant Bit (MSB) planes, independent of contrast changes. | Average Precision: 0.408; Recall: 0.917; F1-score: 0.550. [4] | Custom medical image dataset [4] |
| E2MISeg [5] | Enhancing edge-aware 3D segmentation with multi-level feature aggregation and scale-sensitive loss. | Outperforms state-of-the-art methods; achieves smooth edge segmentation. [5] | MCLID (clinical), three public challenge datasets [5] |
| Deep Learning Reconstruction (DLR) [6] | Combined noise reduction and contrast enhancement for CT. | Significantly improved vessel enhancement and CNR (p<0.001); improved qualitative scores. [6] | Post-neoadjuvant pancreatic cancer CT (114 patients) [6] |
Experimental Protocols for Key Methodologies
Protocol 1: Edge-Guided Bidirectional Iterative Network (EGBINet) for Segmentation
This protocol outlines the procedure for implementing EGBINet, designed to address blurred edges in medical images through a cyclic, bidirectional architecture [1].
Network Initialization:
- Configure the encoder (e.g., VGG19) to extract five multi-scale encoded features, denoted as (E^1_i) for (i = 1, 2, 3, 4, 5) [1].
- Initialize the decoder for progressive feature fusion.
First-Stage Forward Pass:
- Region Feature Decoding: Process the encoded features using a progressive decoding strategy [1].
- Edge Feature Extraction: Fuse local edge information from (E^12) and global positional information from (E^15) using multi-layer convolutional blocks to generate the first-stage edge feature, (D_{edge}^1) [1].
Bidirectional Iterative Optimization:
- Feedback Loop: Feed the decoded regional features and edge features from the first stage back into the encoder [1].
- Iterative Refinement: Allow region and edge feature representations to be reciprocally propagated between the encoder and decoder over multiple iterations. This enables the encoder to dynamically adapt to the decoder's requirements [1].
Feature Fusion with TACM:
- Employ the Transformer-based Multi-level Adaptive Collaboration Module (TACM) to group local edge information and multi-level global regional information.
- Adaptively adjust the weights of these grouped features based on their aggregation quality to significantly improve fusion output [1].
Model Training & Evaluation:
- Loss Function: Use a combination of segmentation loss (e.g., Dice loss) and an edge-aware loss term.
- Validation: Evaluate the model on datasets like ACDC, ASC, and IPFP, focusing on edge preservation and complex structure segmentation accuracy [1].
Protocol 2: Enhanced Level Set Evolution with PADMM Optimization
This protocol details the use of an improved level set method with a novel edge function for efficient and accurate segmentation, particularly effective in noisy and blurred conditions [2].
Image Preprocessing:
- Apply standard filtering (e.g., Gaussian) to reduce noise while preserving edges.
Level Set Formulation:
Energy Minimization with PADMM:
- Formulate the segmentation problem as an energy minimization problem where the energy functional incorporates the novel EIF.
- Apply the Proximal Alternating Direction Method of Multipliers (PADMM) to solve the minimization problem. This provides a theoretically sound framework with efficient, closed-form solutions, avoiding the instability of traditional gradient descent and the constraints of the CFL condition [2].
Contour Evolution:
- Iteratively update the level set function (\Phi) based on the solution from the PADMM optimization until convergence, which is typically signaled by minimal change in the contour between iterations [2].
Post-processing and Validation:
- Extract the zero-level set of the final (\Phi) as the segmentation boundary.
- Quantitatively evaluate results using metrics such as Dice coefficient, sensitivity, accuracy, and Mean Absolute Distance (MAD) against ground truth data [2].
Protocol 3: Contrast-Invariant Edge Detection (CIED)
This protocol describes a method for detecting edges that is robust to variations in image contrast, which is a common challenge in medical imaging [4].
Image Preprocessing:
- Apply Gaussian filtering and morphological operations to prepare the input image [4].
Bit-Plane Decomposition:
- Decompose the preprocessed image into its bit planes. Extract the three Most Significant Bit (MSB) planes, which contain the majority of the visually significant information [4].
Binary Edge Detection:
- Independently detect edges within each of the three MSB bit planes. This is performed by analyzing 3x3 pixel blocks within each binary image [4].
Edge Fusion:
- Fuse the edge maps obtained from the three MSB planes into a single, comprehensive edge image [4].
Validation:
- Assess the performance on a dedicated medical image edge detection dataset. Calculate precision, recall, and F1-score to benchmark against other edge detection operators [4].
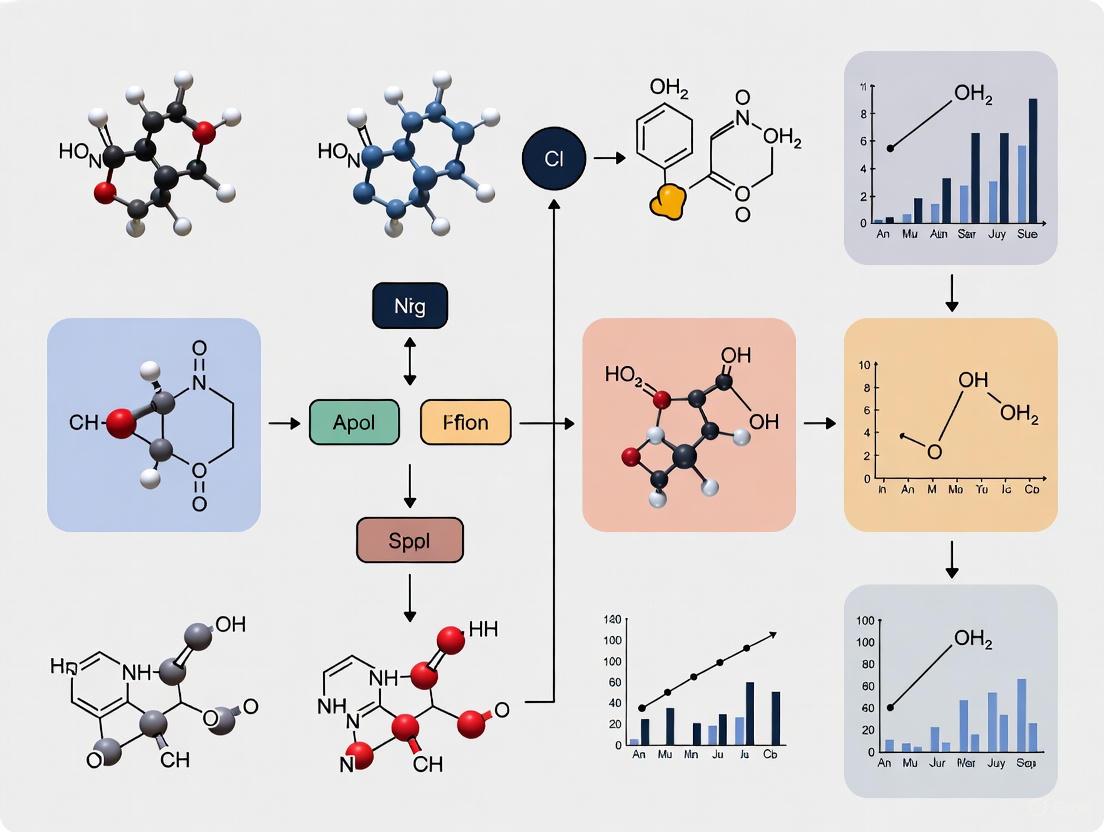
Workflow and Signaling Pathways
The following diagram illustrates the high-level logical workflow of an edge-enhanced segmentation and enhancement system, integrating concepts from the cited frameworks.
The Scientist's Toolkit: Research Reagent Solutions
This section details essential computational tools, modules, and datasets used in the featured experiments.
Table 2: Essential Research Reagents and Computational Tools
| Item Name / Module | Type / Category | Primary Function in Research |
|---|---|---|
| Transformer-based Multi-level Adaptive Collaboration Module (TACM) [1] | Neural Network Module | Groups local and multi-level global features, adaptively adjusting their weights to significantly improve feature fusion quality. [1] |
| Proximal Alternating Direction Method of Multipliers (PADMM) [2] | Optimization Algorithm | Provides an efficient and theoretically sound framework for solving the level set energy minimization problem, offering closed-form solutions and reducing computation time. [2] |
| Scale-Sensitive (SS) Loss [5] | Loss Function | Dynamically adjusts weights based on segmentation errors, guiding the network to focus on regions with unclear segmentation edges. [5] |
| Most Significant Bit (MSB) Planes [4] | Image Processing Technique | Serves as the basis for contrast-invariant edge detection by using binary bit planes to extract significant edge information, eliminating complex pixel operations. [4] |
| Multi-level Feature Group Aggregation (MFGA) [5] | Neural Network Module | Enhances the accuracy of edge voxel classification in 3D images by leveraging boundary clues between lesion tissue and background. [5] |
| ACDC, ASC, IPFP Datasets [1] | Benchmark Datasets | Standardized public datasets (e.g., Automated Cardiac Diagnosis Challenge) used for training and validating segmentation algorithms, enabling comparative performance analysis. [1] |
| MCLID Dataset [5] | Clinical Dataset | A challenging clinical diagnostic dataset of PET images for Mantle Cell Lymphoma, used to test algorithm robustness against complex, real-world data. [5] |
Edge detection, the process of identifying and localizing sharp discontinuities in an image, transcends its role as a simple image processing technique to become a cornerstone of modern medical image analysis. In clinical practice and research, the precise delineation of anatomical structures and pathological regions is paramount, influencing everything from diagnostic accuracy to treatment planning and therapeutic response monitoring. This document frames the critical importance of edge information within a broader research thesis on medical image enhancement, arguing that methods leveraging edge data are fundamental to advancing the field. For researchers and drug development professionals, the ability to accurately quantify pathological margins—whether a tumor's invasive front or the precise boundaries of an organ at risk—directly impacts the development and evaluation of novel therapeutics. The following sections detail the technical paradigms, experimental protocols, and practical toolkits that underpin the effective use of edge information in biomedical research.
Technical Approaches and Quantitative Performance
The integration of edge detection into medical image analysis has evolved from using traditional filters to sophisticated deep-learning architectures that explicitly model boundaries. The table below summarizes the performance of several contemporary approaches, highlighting their specific contributions to segmentation accuracy.
Table 1: Performance Comparison of Edge-Enhanced Medical Image Segmentation Methods
| Method Name | Core Technical Approach | Dataset(s) Used for Validation | Reported Performance Metric(s) | Key Advantage Related to Edges |
|---|---|---|---|---|
| EGBINet [1] | Edge-guided bidirectional iterative network with Transformer-based feature fusion (TACM) | ACDC, ASC, IPFP [1] | Remarkable performance advantages, particularly in edge preservation and complex structure accuracy [1] | Bidirectional flow of edge and region information for iterative boundary optimization [1] |
| E2MISeg [5] | Enhancing Edge-aware Medical Image Segmentation with Multi-level Feature Group Aggregation (MFGA) | Three public challenge datasets & MCLID clinical dataset [5] | Outperforms state-of-the-art methods [5] | Improves edge voxel classification and achieves smooth edge segmentation in boundary ambiguity [5] |
| Contrast-Invariant Edge Detection (CIED) [4] | Fusion of edge information from three Most Significant Bit (MSB) planes | Custom medical image dataset [4] | Average Precision: 0.408, Recall: 0.917, F1-score: 0.550 [4] | Insensitive to changes in image contrast, enhancing robustness [4] |
| U-Net + Sobel Filter [7] | Integration of classic Sobel edge detector with U-Net deep learning model | Chest X-ray images (Lungs, Heart, Clavicles) [7] | Lung Segmentation: Dice 98.88%, Jaccard 97.54% [7] | Enhances structural boundaries before segmentation, reducing artifacts [7] |
| Anatomy-Pathology Exchange (APEx) [8] | Query-based transformer integrating learned anatomical knowledge into pathology segmentation | FDG-PET-CT, Chest X-Ray [8] | Improves pathology segmentation IoU by up to 3.3% [8] | Uses anatomical structures as a prior to identify pathological deviations [8] |
Detailed Experimental Protocols
To ensure the reproducibility and rigorous application of edge-enhanced methods, the following sections outline detailed protocols for two distinct, high-impact experimental approaches.
Protocol 1: Integrating Classical Edge Detection with Deep Learning Segmentation
This protocol is adapted from a study that enhanced the segmentation of anatomical structures in chest X-rays by integrating Sobel edge detection with a U-Net model [7]. The workflow is designed to improve boundary delineation in complex anatomical regions.
Table 2: Research Reagent Solutions for Protocol 1
| Item / Reagent | Specification / Function |
|---|---|
| Chest X-ray Dataset | Images with corresponding ground-truth masks for lungs, heart, and clavicles. |
| Sobel Filter | A discrete differentiation operator computing an approximation of the image gradient to highlight edges. |
| U-Net Architecture | A convolutional neural network with an encoder-decoder structure and skip connections for precise localization. |
| Python Libraries | OpenCV (for Sobel filtering), PyTorch/TensorFlow (for U-Net implementation), Scikit-learn (for metrics). |
| Hardware | GPU-enabled workstation (e.g., NVIDIA Tesla series) for efficient deep learning model training. |
Workflow Diagram: U-Net with Sobel Edge Enhancement
Procedure:
Image Acquisition and Preprocessing:
- Obtain a dataset of chest X-ray images in DICOM format alongside their corresponding ground-truth segmentation masks for the lungs, heart, and clavicles [7].
- Resize all images to a uniform dimension (e.g., 256x256 or 512x512 pixels).
- Normalize pixel intensities to a range of [0, 1].
Edge Enhancement:
- Apply the Sobel operator to the preprocessed grayscale image using the
cv2.Sobel()function from the OpenCV library. - The operator uses two 3x3 kernels (for horizontal and vertical derivatives) which are convolved with the original image to approximate the gradient magnitude [7].
- Compute the final edge-enhanced image by calculating the magnitude of the gradients:
G = sqrt(G_x² + G_y²).
- Apply the Sobel operator to the preprocessed grayscale image using the
Model Training and Inference:
- Input Preparation: The original preprocessed image and the Sobel edge-enhanced image are used as inputs. They can be stacked as a two-channel input or fused within the network architecture [7].
- Network Architecture: Implement a standard U-Net architecture. The encoder progressively downsamples the feature maps to capture context, while the decoder upsamples to recover spatial information. Skip connections link encoder and decoder layers to preserve fine details.
- Training: Train the model using a loss function suitable for segmentation, such as Dice Loss or a combination of Dice and Cross-Entropy Loss, to mitigate class imbalance. Use an optimizer like Adam with an initial learning rate of 1e-4.
- Inference: Pass new, unseen X-ray images through the trained model to generate the final multi-class segmentation mask.
Protocol 2: Training an Edge-Guided Bidirectional Iterative Network
This protocol describes the implementation of EGBINet, a sophisticated architecture designed to address blurred edges in medical images through a cyclic, bidirectional flow of information [1].
Workflow Diagram: EGBINet Bidirectional Architecture
Procedure:
Initial Feature Extraction:
- The input image is processed by an encoder (e.g., VGG19) to extract five multi-scale encoded features, denoted as (E_i) where i = 1, 2, 3, 4, 5 [1].
First-Stage Decoding for Edge and Region Features:
- Edge Feature Extraction: Aggregate local edge information ((E2)) and global positional information ((E5)) to extract edge features. Multi-layer convolutional blocks are used to fuse these scales: (D{edge}^1 = \mathrm{Con}(E2^1, E_5^1)) [1].
- Regional Feature Decoding: A progressive decoding strategy, inspired by UNet, is applied to the multi-level regional features from the encoder. This involves cross-layer fusion: (Di^1 = \mathrm{Con}(Ei^1, D_{i+1}^1)) for i = 1, 2, 3 [1].
Bidirectional Iterative Optimization:
- The decoded edge ((D{edge})) and regional ((Di)) features from the first stage are fed back to the encoder [1].
- This establishes a feedback mechanism from the decoder to the encoder, allowing region and edge feature representations to be reciprocally propagated. This cycle enables the iterative optimization of hierarchical feature representations, allowing the encoder to dynamically refine its features based on the decoder's requirements [1].
Feature Fusion with TACM:
- The Transformer-based Multi-level Adaptive Collaboration Module (TACM) is employed to fuse the local edge information with multi-level global regional information [1].
- TACM groups these features and adaptively adjusts their weights according to the aggregation quality, significantly improving the fusion of edge and regional data for a superior final segmentation [1].
The Scientist's Toolkit: Essential Research Reagents
The successful implementation of the aforementioned protocols relies on a suite of computational tools and data resources.
Table 3: Key Research Reagent Solutions for Edge-Enhanced Medical Image Analysis
| Tool / Resource | Category | Specific Function |
|---|---|---|
| Sobel, Scharr Operators | Classical Edge Detector | Highlights structural boundaries by computing image gradients; useful as a pre-processing step or integrated into DL models [7]. |
| U-Net & Variants (e.g., Attention U-Net, U-Net++) | Deep Learning Architecture | Provides a foundational encoder-decoder backbone for semantic segmentation, often enhanced with edge-guided modules [1] [9]. |
| Vision Transformers (ViT) | Deep Learning Architecture | Captures long-range dependencies and global context in images, improving the understanding of anatomical and pathological structures [1] [10]. |
| EGBINet / APEx | Specialized Algorithm | Implements advanced concepts like bidirectional edge-region interaction and anatomy-pathology knowledge exchange for state-of-the-art results [1] [8]. |
| Public Datasets (ACDC, MIMIC-CXR) | Data | Annotated medical image datasets for training and benchmarking segmentation algorithms [1] [7]. |
| Dice Loss / Focal Loss | Loss Function | Manages class imbalance in segmentation tasks, directing network focus to under-segmented regions and boundary voxels [5]. |
Traditional edge-based segmentation methods form a foundational pillar in medical image analysis, enabling the precise delineation of anatomical structures and pathological regions by identifying intensity discontinuities. These techniques—encompassing thresholding, region-growing, and model-based approaches—leverage predefined rules and intensity-based operations to partition images into clinically meaningful regions. Their computational efficiency and interpretability make them particularly valuable in clinical workflows where transparency is paramount. In the broader context of medical image enhancement research, these methods provide critical edge information that can guide and refine subsequent analysis, supporting accurate diagnosis, treatment planning, and quantitative assessment across diverse imaging modalities.
Core Methodologies and Comparative Analysis
Thresholding Techniques
Thresholding operates by classifying pixels based on intensity values relative to a defined threshold, effectively converting grayscale images into binary representations. The core function is defined as:
B(x,y) = 1, if I(x,y) ≥ T B(x,y) = 0, if I(x,y) < T
where I(x,y) represents the pixel intensity at position (x,y), and T is the threshold value [11]. These techniques are categorized into global and local approaches, each with distinct advantages and limitations as summarized in Table 1.
Table 1: Comparative Analysis of Thresholding Techniques
| Technique | Core Principle | Medical Imaging Applications | Advantages | Limitations |
|---|---|---|---|---|
| Otsu's Method | Maximizes between-class variance | CT, MRI segmentation [12] [11] | Automatically determines optimal threshold; Effective for bimodal histograms | Computational cost increases exponentially with threshold levels [12] |
| Iterative Thresholding | Repeatedly refines threshold based on foreground/background means | General medical image binarization [11] | Simple implementation; Self-adjusting | Sensitive to initial threshold selection |
| Entropy-Based Thresholding | Maximizes information content between segments | Enhancing informational distinctiveness [11] | Effective for complex intensity distributions | Computationally intensive |
| Local Adaptive (Niblack/Sauvola) | Calculates thresholds based on local statistics | Handling uneven illumination [11] | Adapts to local intensity variations; Robust to illumination artifacts | Parameter sensitivity; Potential noise amplification |
Region-Growing Algorithms
Region-growing techniques operate by aggregating pixels with similar properties starting from predefined seed points. These methods are particularly effective for segmenting contiguous anatomical structures with homogeneous intensity characteristics.
Table 2: Region-Growing Approaches in Medical Imaging
| Application Context | Seed Selection Method | Growth Criteria | Reported Performance/Advantages |
|---|---|---|---|
| Breast CT Segmentation [13] | Along skin outer edge | Voxel intensity ≥ mean seed intensity | Effective for high-contrast boundaries; Fast segmentation |
| Breast Skin Segmentation [13] | Constrained by skin centerline | Combined with active contour models | Reduced false positives; Robust segmentation |
| 3D Skin Segmentation [13] | Manual or automatic seed placement | Intensity/texture similarity | Effective for irregular surfaces; Contiguous region segmentation |
| General Medical Imaging [11] | User-defined or algorithmically determined | Intensity, texture, or statistical similarity | Simple implementation; Preserves connected boundaries |
Model-Based Approaches
Model-based techniques utilize deformable models that evolve to fit image boundaries based on internal constraints and external image forces, making them particularly suitable for anatomical structures with complex shapes.
Table 3: Model-Based Segmentation Techniques
| Method | Core Mechanism | Medical Applications | Strengths | Challenges |
|---|---|---|---|---|
| Active Contours/Snakes | Energy minimization guided by internal (smoothness) and external (image gradient) forces | Skin surface segmentation in MRI [13] | Captures smooth, continuous boundaries; Handles topology changes | Sensitive to initial placement; May converge to local minima |
| Level-Set Methods | Partial differential equation-driven contour evolution | Complex skin surfaces [13] | Handles complex topological changes; Intrinsic contour representation | Computationally intensive; Parameter sensitivity |
| Atlas-Based Segmentation | Deformation of anatomical templates to patient data | Skin segmentation with prior knowledge [13] | Incorporates anatomical knowledge; Reduces ambiguity | Requires high-quality registration; Limited by anatomical variations |
Experimental Protocols and Application Notes
Protocol 1: Otsu's Multilevel Thresholding for Medical Image Segmentation
Objective: To implement an optimized multilevel thresholding approach for segmenting medical images with heterogeneous intensity distributions.
Materials and Equipment:
- Medical image dataset (e.g., MRI, CT scans)
- Computing environment with Python/OpenCV or MATLAB
- Performance evaluation metrics (Dice coefficient, Hausdorff distance)
Methodology:
- Image Preprocessing:
- Convert input image to grayscale if necessary
- Normalize intensity values to standard range (0-255)
- Compute image histogram and probability distribution for each intensity level [12]
Optimization Integration:
- Define Otsu's objective function: Maximize between-class variance σ²_b = w₁w₂(μ₁ - μ₂)² [12]
- Initialize optimization algorithm (e.g., Harris Hawks, Differential Evolution)
- Implement fitness function evaluation for candidate thresholds
Multilevel Thresholding:
- For k thresholds, divide histogram into k+1 classes
- Compute between-class variance for each threshold combination
- Identify optimal thresholds that maximize overall between-class variance
Validation:
- Compare segmentation results with ground truth annotations
- Evaluate computational efficiency relative to exhaustive search
- Assess segmentation quality using domain-specific metrics
Applications: Particularly effective for CT image segmentation where intensity distributions correspond to different tissue types [12].
Protocol 2: Region-Growing for 3D Skin Segmentation
Objective: To extract continuous skin surfaces from volumetric medical imaging data (CT/MRI) for 3D patient modeling.
Materials and Equipment:
- Volumetric medical images (CT/MRI)
- 3D visualization software
- Computation of isovalue for intensity thresholding
Methodology:
- Seed Point Initialization:
- Identify background starting point (typically image corners)
- Verify background classification using automatically computed skin isovalue [13]
Region Propagation:
- Initialize list of pixels to evaluate with neighbors of starting point
- For each candidate pixel, evaluate against isovalue threshold
- Include pixel in segmentation if intensity exceeds isovalue
- Add neighboring pixels to evaluation list
Postprocessing:
- Apply morphological operations to remove noise
- Ensure connectivity of segmented skin surface
- Convert to 3D mesh for visualization and analysis
Applications: Creation of realistic 3D patient models for surgical planning, personalized medicine, and remote monitoring [13].
Protocol 3: Edge-Based Segmentation with Boundary Refinement
Objective: To leverage edge detection operators for precise boundary identification in medical images with subsequent refinement.
Materials and Equipment:
- Medical images with structures of interest
- Edge detection operators (Sobel, Canny)
- Implementation of non-maximum suppression and hysteresis thresholding
Methodology:
- Image Preprocessing:
- Apply Gaussian filtering to reduce noise
- Enhance contrast in boundary regions
Edge Detection:
- Compute gradient magnitude and direction using Sobel operators
- Implement non-maximum suppression to thin edges
- Apply hysteresis thresholding to identify strong, weak, and irrelevant edges [11]
Boundary Completion:
- Connect discontinuous edges using morphological operations
- Validate boundary continuity using anatomical constraints
- Generate final segmentation by region enclosure
Applications: Effective for anatomical structures with clear intensity transitions, such as organ boundaries in CT imaging [11].
Table 4: Key Research Reagents and Computational Tools
| Item | Specification/Type | Function in Research |
|---|---|---|
| Otsu's Algorithm | Statistical thresholding method | Automatically determines optimal segmentation thresholds by maximizing between-class variance [12] [11] |
| Sobel Operators | Gradient-based edge detector | Identifies intensity discontinuities along horizontal and vertical directions [14] |
| Region-Growing Framework | Pixel aggregation algorithm | Segments contiguous anatomical structures from seed points based on similarity criteria [13] |
| Active Contours Model | Deformable boundary model | Evolves initial contour to fit anatomical boundaries through energy minimization [13] |
| Medical Image Datasets | Clinical imaging data (CT, MRI, PET) | Provides ground truth for algorithm validation and performance benchmarking [5] [12] |
| Optimization Algorithms | Nature-inspired optimizers (Harris Hawks, DE) | Reduces computational cost of multilevel thresholding while maintaining accuracy [12] |
Workflow and Conceptual Diagrams
Traditional Edge-Based Segmentation Workflow
Region-Growing for 3D Skin Segmentation
Optimized Otsu's Thresholding Methodology
The Evolution from Classical Operators (e.g., Canny) to Data-Driven Deep Learning
The pursuit of enhanced medical images through the extraction of edge information has undergone a profound transformation, evolving from mathematically defined classical operators to sophisticated, data-driven deep learning models. This evolution is central to advancing diagnostic accuracy and treatment planning in modern healthcare. Classical edge detection methods, such as the Canny, Sobel, and Prewitt operators, rely on fixed convolution kernels to identify intensity gradients, providing a transparent and computationally efficient means of highlighting anatomical boundaries [15]. However, their reliance on handcrafted features often renders them fragile in the presence of noise, low contrast, and the complex textures inherent to medical imaging modalities.
The advent of deep learning has marked a paradigm shift, enabling models to learn hierarchical feature representations directly from vast datasets. These data-driven approaches excel at preserving critical edge details in challenging conditions, fundamentally reshaping segmentation, fusion, and enhancement protocols [16] [17]. Contemporary research now explores a synergistic path, investigating how classical edge priors can be embedded within deep learning architectures to create robust, hybrid frameworks [18]. This article details the experimental protocols and applications underpinning this technological evolution, providing a toolkit for researchers and scientists engaged in medical image analysis.
Quantitative Comparison of Methodologies
The transition from classical to learning-based methods can be quantitatively assessed across key performance metrics. The table below summarizes a comparative analysis based on recent research findings.
Table 1: Quantitative Comparison of Edge Detection and Enhancement Methodologies
| Method Category | Example Techniques | Key Performance Metrics & Results | Primary Advantages | Inherent Limitations |
|---|---|---|---|---|
| Classical Operators | Canny, Sobel, Prewitt, Roberts [15] | In PD classification, Canny+Hessian filtering degraded most ML model accuracy [19] | Computational efficiency; model interpretability; no training data required | Fragility to noise and low contrast; reliance on handcrafted parameters |
| Fuzzy & Fractional Calculus | Type-1/Type-2 Fuzzy Logic, Grünwald-Letnikov fractional mask [15] [20] | Improved handling of uncertainty; better texture enhancement in grayscale images [20] | Effectively models uncertainty and soft transitions in boundaries | Can introduce halo artifacts; requires manual parameter adjustment |
| Deep Learning (CNN-based) | U-Net, ResNet, EMFusion, MUFusion [18] [21] | Superior accuracy in segmentation and fusion tasks; SSIM, Qabf, VIF [18] | Learns complex, hierarchical features directly from data; high accuracy | High computational demand; requires large, annotated datasets |
| Deep Learning (Transformer-based) | SwinFusion, ECFusion, Cross-Scale Transformer [18] | Captures long-range dependencies; improves mutual information (MI) and structural similarity (SSIM) in fused images [18] | Superior global context modeling; better coordination of structural/functional data | Extremely high computational complexity and memory footprint |
| Hybrid Models (Classical + DL) | ECFusion (Sobel EAM + Transformer) [18] | Clearer edges, higher contrast in MMIF; quantitative improvements in Qabf, Qcv [18] | Leverages strengths of both approaches; explicit edge preservation within data-driven framework | Increased architectural complexity; design and training challenges |
Detailed Experimental Protocols
To ensure reproducibility and provide a clear framework for research, this section outlines detailed protocols for key experiments cited in the literature.
Protocol: Impact of Classical Edge Preprocessing on ML Classification
This protocol is based on the experiment investigating the effect of Canny edge detection on Parkinson's Disease (PD) classification performance [19].
- Objective: To evaluate the impact of Canny edge detection and Hessian filtering preprocessing on the performance, memory footprint, and prediction latency of standard machine learning models.
- Dataset Preparation:
- Source: Handwriting spiral drawings from PD patients and healthy controls.
- Dataset Variants:
- DS₀: The original, normal dataset.
- DS₁:
DS₀processed with Canny edge detection and Hessian filtering. - DS₂: An augmented version of
DS₀. - DS₃: An augmented version of
DS₁.
- Machine Learning Models: Logistic Regression (LR), Decision Tree (DT), Random Forest (RF), Support Vector Machine (SVM), XGBoost (XGB), Naive Bayes (NB), k-Nearest Neighbors (KNN), AdaBoost (AdB).
- Evaluation Metrics:
- Primary: Prediction Accuracy.
- Secondary: Model memory footprint (KB), Prediction latency (ms).
- Experimental Procedure:
- Train each of the eight ML models on all four dataset variants (
DS₀,DS₁,DS₂,DS₃). - For each trained model, record the prediction accuracy on a held-out test set.
- Measure the memory size of each saved model.
- Measure the average time required for the model to make a prediction on a single sample.
- Perform statistical analysis (e.g., Mann-Whitney U test) using 100 accuracy observations per model to compare performance between datasets (e.g.,
DS₀vs.DS₂).
- Train each of the eight ML models on all four dataset variants (
- Key Analysis:
- Compare accuracy metrics across datasets to determine the effect of edge preprocessing.
- Identify models with stable memory and latency across datasets (e.g., LR, DT, RF) versus those with significant increases (e.g., KNN, SVM, XGBoost) [19].
Protocol: Edge-Enhanced Pre-training for Medical Image Segmentation
This protocol is based on the experiment investigating the effect of edge-enhanced pre-training on foundation models [16].
- Objective: To determine whether pre-training a foundation model on edge-enhanced data improves its segmentation performance across diverse medical imaging modalities.
- Dataset:
- A diverse collection of medical images from multiple modalities (e.g., Dermoscopy, Fundus, Mammography, X-Ray).
- Includes input images and corresponding ground truth segmentation masks.
- Edge Enhancement:
- Method: Kirsch filter.
- Procedure: Apply the Kirsch filter, which uses eight convolution kernels to detect edges in different orientations, to all training images to create an edge-enhanced dataset [16].
- Model Training:
- Step 1 - Pre-training: Create two versions of a foundation model.
- Model A (
fθ): Pre-trained on raw medical images. - Model B (
fθ*): Pre-trained on edge-enhanced medical images.
- Model A (
- Step 2 - Fine-tuning: For each specific medical modality, fine-tune both Model A and Model B on a subset of raw images from that modality.
- Step 1 - Pre-training: Create two versions of a foundation model.
- Evaluation:
- Metrics: Dice Similarity Coefficient (DSC), Normalized Surface Distance (NSD).
- Procedure: Evaluate the fine-tuned models on a held-out test set for each modality.
- Meta-Learning Strategy:
- Extract meta-features (standard deviation and image entropy) from the raw input images.
- Train a classifier to predict, based on these meta-features, whether Model A or Model B will yield better segmentation results for a given image.
- Use this classifier to select the optimal model for inference [16].
Protocol: Multimodal Image Fusion with an Edge-Augmented Module
This protocol is based on the ECFusion framework for multimodal medical image fusion [18].
- Objective: To fuse images from different modalities (e.g., CT-MRI, PET-MRI) into a single image with enhanced edges and high contrast.
- Architecture: The ECFusion framework, comprising an Edge-Augmented Module (EAM), a Cross-Scale Transformer Fusion Module (CSTF), and a Decoder.
- Experimental Procedure:
- Input: Register two source images,
I_aandI_b(e.g., a CT and an MRI). - Edge-Augmented Module (EAM):
- Process each input image through the EAM.
- Edge Module: Use Sobel operators
G_xandG_yto extract horizontal and vertical edge maps from the input image. - Feature Extraction: The input image and its edge map are processed through a feature extraction network (e.g., with a channel expansion head and multiple residual blocks) to produce multi-level features
FI_aandFI_b[18].
- Cross-Scale Transformer Fusion Module (CSTF):
- Input features
FI_aandFI_bat the same level into the CSTF. - The CSTF uses a Hierarchical Cross-Scale Embedding Layer (HCEL) to capture multi-scale contextual information and fuse the features.
- Input features
- Reconstruction:
- Pass the concatenated, fused features from all levels through the Decoder to generate the final fused image
I_f.
- Pass the concatenated, fused features from all levels through the Decoder to generate the final fused image
- Input: Register two source images,
- Training:
- Mode: Unsupervised.
- Loss Functions: A combination of losses designed to preserve structural information, maintain intensity fidelity, and enhance edge quality.
- Evaluation:
- Quantitative Metrics: Mutual Information (MI), Structural Similarity (Qabf, SSIM), Visual Information Fidelity (VIF),
Q_{cb},Q_{cv}[18]. - Comparison: Compare against state-of-the-art methods like U2Fusion, EMFusion, and SwinFusion.
- Quantitative Metrics: Mutual Information (MI), Structural Similarity (Qabf, SSIM), Visual Information Fidelity (VIF),
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Tools for Medical Image Enhancement with Edge Information
| Tool / Reagent | Function in Research | Example Use Cases |
|---|---|---|
| Classical Edge Kernels | Predefined filters for gradient calculation and preliminary boundary identification. | Canny, Sobel, and Kirsch filters for pre-processing or feature extraction [19] [18] [16]. |
| Fuzzy C-Means Clustering | A soft clustering algorithm for tissue classification and unsupervised image segmentation. | Segmenting ambiguous regions in MRI; used in the iMIA platform for soft tissue classification [15]. |
| Lightweight CNN Architectures | Enable deployment of deep learning models on resource-constrained hardware (e.g., edge devices). | MobileNet-v2, ResNet18, EfficientNet-v2 for on-device diagnostic inference [21]. |
| U-Net | A convolutional network architecture with a skip-connection structure for precise image segmentation. | Benchmarking segmentation performance; comparing against ACO for brain boundary extraction [15] [22]. |
| Transformer Modules | Capture long-range, global dependencies in an image through self-attention mechanisms. | Cross-Scale Transformer Fusion Module (CSTF) in ECFusion for global consistency in fused images [18]. |
| Ant Colony Optimization (ACO) | A bio-inspired metaheuristic algorithm used for edge detection and pathfinding in images. | An alternative edge extraction method in the iMIA platform; compared against U-Net [15]. |
| Diffusion Models | Generative models that iteratively denoise data, used for training-free universal image enhancement. | UniMIE model for enhancing various medical image modalities without task-specific fine-tuning [23]. |
| Fractional Derivative Masks | Non-integer order differential operators for enhancing texture details while preserving smooth regions. | Grünwald-Letnikov (GL) based masks for texture enhancement in single-channel medical images [20]. |
Workflow and Architectural Diagrams
Edge-Enhanced Pre-training and Segmentation Workflow
The following diagram illustrates the two-stage pipeline for investigating edge-enhanced pre-training for medical image segmentation, as described in the experimental protocol.
Hybrid Edge-Deep Learning Fusion Architecture
This diagram details the architecture of a hybrid model (ECFusion) that integrates a classical Sobel operator within a deep learning framework for multimodal image fusion.
Medical imaging is indispensable for modern diagnostics, yet it is fundamentally constrained by intrinsic challenges including noise, low contrast, and profound anatomical variability. These issues complicate automated image analysis, particularly in segmentation and quantification tasks essential for precision medicine. This application note explores how edge information-based methods provide a robust framework for addressing these challenges. We detail specific experimental protocols, present quantitative performance data from state-of-the-art models, and provide a toolkit for researchers to implement these advanced techniques in studies ranging from tumor delineation to organ volumetry.
The fidelity of medical images is compromised by a triad of persistent challenges. Noise, inherent to the acquisition process, can obscure subtle pathological signs. Low contrast between adjacent soft tissues or between healthy and diseased regions makes boundary delineation difficult. Significant anatomical variability across patients and populations challenges the generalization ability of computational models. Edge information, which defines the boundaries of anatomical structures, serves as a critical prior for guiding segmentation networks to produce clinically plausible and accurate results, especially in regions where image contrast is weak or noise levels are high.
The table below summarizes the core challenges and how recent edge-aware methodologies quantitatively address them.
Table 1: Key Challenges in Medical Imaging and Performance of Edge-Enhanced Solutions
| Challenge | Impact on Image Analysis | Edge-Enhanced Solution | Reported Performance Metric | Value/Dataset |
|---|---|---|---|---|
| Blurred Edges | Ambiguous organ/lesion boundaries leading to inaccurate segmentation. | EGBINet (Edge Guided Bidirectional Iterative Network) [1] | Dice Similarity Coefficient (DSC) | ACDC, ASC, IPFP datasets |
| Boundary Ambiguity | Low edge pixel-level contrast in tumors and organs. | E2MISeg (Enhancing Edge-aware Model) [5] | DSC & Boundary F1 Score | Public challenges & MCLID dataset |
| Speckle Noise | Degrades ultrasound image quality, impacting diagnostic accuracy. | Advanced Despeckling Filters & Neural Networks [24] | Signal-to-Noise Ratio (SNR) Improvement | Various ultrasound modalities |
| Anatomic Variability | Model failure on structures with large shape/size variations. | TotalSegmentator MRI (Sequence-agnostic model) [25] | Dice Score | 80 diverse anatomic structures |
| Low Contrast | Difficulty in segmenting small vessels and specific organs. | Scale-Sensitive (SS) Loss Function [5] | Segmentation Accuracy | MCLID (Mantle Cell Lymphoma) |
Experimental Protocols for Edge-Enhanced Segmentation
This section provides detailed methodologies for implementing and validating edge-aware segmentation models.
Protocol for Implementing EGBINet
EGBINet addresses blurred edges through a cyclic architecture that enables bidirectional information flow [1].
- Data Preparation:
- Acquire medical image datasets with corresponding ground truth segmentation masks. The ACDC (cardiac), ASC (atrial), and IPFP (knee) datasets are suitable benchmarks.
- Pre-process images: normalize intensity values to a range of [0, 1] and resample all images to a uniform isotropic resolution (e.g., 1.5 mm³).
- Network Architecture Configuration:
- Encoder: Initialize the encoder using a pre-trained VGG19 backbone to extract multi-scale regional features (Ei^1).
- Edge Feature Extraction: Fuse low-level features (E2^1) and high-level global features (E5^1) using multi-layer convolutional blocks to compute initial edge features (D{edge}^1).
- Bidirectional Iteration:
- Feedforward Path: Fuse edge features with multi-level regional features from the encoder to the decoder.
- Feedback Path: Propagate refined region and edge feature representations from the decoder back to the encoder for iterative optimization.
- Feature Fusion: Implement the Transformer-based Multi-level Adaptive Collaboration Module (TACM) to adaptively adjust the weights of local edge and global regional information during fusion.
- Training:
- Use a combined loss function, such as a sum of Dice loss and Binary Cross-Entropy loss.
- Optimize using Adam with an initial learning rate of 1e-4, halving it after every 50 epochs without validation loss improvement.
- Train for a maximum of 400 epochs with a batch size tailored to GPU memory.
- Validation and Analysis:
- Evaluate segmentation performance on a held-out test set using Dice Similarity Coefficient (DSC).
- Qualitatively assess the results by visually comparing the sharpness of predicted boundaries against the ground truth, particularly in regions of low contrast.
Protocol for Implementing E2MISeg for Boundary Ambiguity
E2MISeg is designed for smooth segmentation where boundary definition is inherently challenging, such as in PET imaging of lymphomas [5].
- Data Preparation:
- Utilize the provided MCLID dataset or other 3D medical images (e.g., PET, CT, MRI) with poorly defined lesion boundaries.
- Perform standard intensity normalization and resampling to a unified voxel spacing.
- Network Configuration:
- Multi-level Feature Group Aggregation (MFGA): Implement this module to enhance the classification accuracy of edge voxels by explicitly leveraging boundary clues between lesion tissue and background.
- Hybrid Feature Representation (HFR): Construct a block that uses a combination of Convolutional Neural Networks (CNNs) and Transformer encoders. The CNN focuses on local texture and edge features, while the Transformer captures long-range contextual dependencies to minimize background noise interference.
- Training with Scale-Sensitive Loss:
- Employ the Scale-Sensitive (SS) loss function, which dynamically adjusts the weights assigned to different image regions based on the magnitude of segmentation error. This guides the network to focus learning capacity on regions with unclear edges.
- Train the model end-to-end using an optimizer like AdamW with a weight decay of 1e-5.
- Validation:
- Beyond the DSC, use a boundary-specific metric like the Boundary F1 (BF1) score to quantitatively evaluate the precision of edge segmentation.
- Perform ablation studies to isolate the performance contribution of the MFGA, HFR, and SS loss components.
Visualization of Edge-Aware Architectures
The following diagrams, generated using DOT, illustrate the core workflows of the featured edge-enhanced segmentation models.
EGBINet Bidirectional Information Flow
E2MISeg Hybrid Feature Representation
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools for Edge-Enhanced Medical Image Analysis
| Tool/Resource Name | Type | Primary Function in Research | Application Example |
|---|---|---|---|
| nnU-Net [25] | Deep Learning Framework | Self-configuring framework for robust medical image segmentation; backbone for many state-of-the-art models. | Serves as the base architecture for TotalSegmentator MRI. |
| TotalSegmentator MRI [25] | Pre-trained AI Model | Open-source, sequence-agnostic model for segmenting 80+ anatomic structures in MRI. | Automated organ volumetry for large-scale population studies. |
| Transformer-based TACM [1] | Neural Network Module | Adaptively fuses multi-scale features by grouping local and global information, improving edge feature quality. | Core component of EGBINet for high-quality feature fusion. |
| Scale-Sensitive (SS) Loss [5] | Optimization Function | Dynamically adjusts learning weights to focus network attention on regions with unclear segmentation edges. | Used in E2MISeg to tackle low-contrast boundaries in lymphoma PET images. |
| EGBINet / E2MISeg Code [1] [5] | Model Implementation | Publicly available code for replicating and building upon the cited edge-aware segmentation models. | Benchmarking new segmentation algorithms on complex clinical datasets. |
| ACDC, ASC, IPFP Datasets [1] | Benchmark Data | Publicly available datasets for training and validating cardiac, atrial, and musculoskeletal segmentation models. | Standardized evaluation and comparison of model performance. |
Methodologies and Clinical Applications of Edge-Enhanced Imaging
Medical image segmentation is a fundamental task in computational pathology and radiology, enabling precise anatomical and pathological delineation for enhanced diagnosis and surgical planning [26] [27]. A persistent challenge in this domain is the accurate segmentation of organ and tumor images characterized by large-scale variations and low-edge pixel-level contrast, which often results in boundary ambiguity [5]. Edge-aware segmentation addresses this critical issue by explicitly incorporating boundary information into the deep learning architecture, significantly improving the model's ability to delineate complex anatomical structures where precise boundaries are diagnostically crucial [1] [28].
The evolution of edge-aware segmentation architectures has progressed from convolutional neural networks (CNNs) like U-Net to more complex frameworks incorporating transformers, state space models, and bidirectional iterative mechanisms [29] [1] [30]. These advancements aim to balance the preservation of local edge details with the modeling of long-range dependencies necessary for global context understanding. This application note provides a comprehensive overview of current edge-aware architectures, quantitative performance comparisons, detailed experimental protocols, and essential research reagents to facilitate implementation and advancement in this rapidly evolving field.
Taxonomy of Edge-Aware Architectures
Current edge-aware segmentation architectures can be categorized into several paradigms based on their fundamental approach to boundary refinement:
U-Net Enhanced Architectures: Traditional U-Net variants form the foundation of edge-aware segmentation, with innovations focusing on incorporating explicit edge guidance through auxiliary branches. EGBINet introduces a cyclic architecture enabling bidirectional flow of edge information and region information between encoder and decoder, allowing dynamic response to segmentation demands [1]. Similarly, ECCA-UNet integrates Cross-Shaped Window (CSWin) mechanisms for long-range dependency modeling with linear complexity, supplemented by Squeeze-and-Excitation (SE) channel attention and an auxiliary edge-aware branch for boundary retention [28].
Transformer-Based Acceleration: Vision Transformer (ViT) adaptations address computational challenges through selective processing strategies. HRViT employs an edge-aware token halting module that dynamically identifies edge patches and halts non-edge tokens in early layers, preserving computational resources for complex boundary regions [29]. These approaches recognize that background and internal tokens can be easily recognized early, while ambiguous edge regions require deeper computational processing.
Few-Shot Learning Frameworks: For scenarios with limited annotated data, specialized architectures have emerged. The Edge-aware Multi-prototype Learning (EML) framework generates multiple feature representatives through a Local-Aware Feature Processing (LAFP) module and refines them through a Dynamic Prototype Optimization (DPO) module [26]. AGENet incorporates spatial relationships through adaptive edge-aware geodesic distance learning, leveraging iterative Fast Marching refinement with anatomical constraints [31].
Hybrid and Next-Generation Models: Recent architectures integrate multiple paradigms for enhanced performance. ÆMMamba combines State Space Modeling efficiency with edge enhancement through an Edge-Aware Module (EAM) using Sobel-based edge extraction and a Boundary Sensitive Decoder (BSD) with inverse attention [30].
Quantitative Performance Comparison
Table 1: Performance metrics of edge-aware segmentation architectures across public datasets
| Architecture | Dataset | Dice Score (%) | HD (mm) | Params | Key Innovation |
|---|---|---|---|---|---|
| ECCA-UNet [28] | Synapse CT | 81.90 | 20.05 | - | CSWin + SE attention + Edge branch |
| ECCA-UNet [28] | ACDC MRI | 91.10 | - | - | Channel-enhanced cross-attention |
| E2MISeg [5] | MCLID PET | - | - | - | MFGA + HFR + SS loss |
| HRViT [29] | BTCV | - | - | 34.2M | Edge-aware token halting |
| ÆMMamba [30] | Kvasir | 72.22 (mDice) | - | - | Mamba backbone + EAM |
| AGENet [31] | Multi-domain | 79.56 (1-shot) 81.67 (5-shot) | 11.16 (1-shot) 8.39 (5-shot) | - | Geodesic distance learning |
| Lightweight Evolving U-Net [32] | 2018 Data Science Bowl | 95.00 | - | Lightweight | Depthwise separable convolutions |
Table 2: Architectural components and their functional contributions
| Component | Function | Architectural Implementations |
|---|---|---|
| Multi-level Feature Group Aggregation (MFGA) | Enhances edge voxel classification through boundary clues | E2MISeg [5] |
| Hybrid Feature Representation (HFR) | Utilizes CNN-Transformer interaction to mine lesion areas | E2MISeg [5] |
| Scale-Sensitive (SS) Loss | Dynamically adjusts weights based on segmentation errors | E2MISeg [5] |
| Edge-Aware Token Halting | Identifies edge patches, halts non-edge tokens early | HRViT [29] |
| Local-Aware Feature Processing (LAFP) | Generates multiple prototypes for boundary segmentation | EML [26] |
| Dynamic Prototype Optimization (DPO) | Refines prototypes via attention mechanism | EML [26] |
| Bidirectional Iterative Flow | Enables edge-region information exchange | EGBINet [1] |
| Transformer-based Multi-level Adaptive Collaboration (TACM) | Adaptively fuses local edge and global region information | EGBINet [1] |
| Edge-Aware Geodesic Distance | Creates anatomically-coherent spatial importance maps | AGENet [31] |
Experimental Protocols and Methodologies
Implementation Framework for Edge-Aware Segmentation
Dataset Preparation and Preprocessing: For optimal performance with edge-aware architectures, medical images require specific preprocessing. For abdominal CT segmentation (e.g., BTCV dataset), implement resampling to isotropic resolution (1.5×1.5×2 mm³) followed by intensity clipping at [-125, 275] Hounsfield Units and z-score normalization [29]. For cardiac MRI segmentation (e.g., ACDC dataset), apply bias field correction using N4ITK algorithm and normalize intensity values to [0, 1] range [28]. For few-shot learning scenarios, implement the episodic training paradigm with random sampling of support-query pairs from base classes, ensuring each task contains K-shot examples (K typically 1 or 5) for each of N classes (usually 2-5) [26] [31].
Edge Ground Truth Generation: Generate binary edge labels using Canny edge detection with σ=1.0 on segmentation masks, followed by morphological dilation with 3×3 kernel to create boundary bands of uniform physical width [26] [1]. Alternatively, for methods employing geodesic distance learning, compute Euclidean Distance Transform (EDT) initialization followed by iterative Fast Marching refinement with edge-aware speed functions [31].
Data Augmentation Strategy: Apply intensive data augmentation including random rotation (±15°), scaling (0.8-1.2×), elastic deformations (σ=10, α=100), and intensity shifts (±20%) [5] [29]. For transformer-based architectures, employ random patch shuffling and patch masking with 15% probability to enhance robustness [28].
Training Protocols
Loss Function Configuration: Implement hybrid loss functions combining region and boundary terms. For E2MISeg, the Scale-Sensitive (SS) loss dynamically adjusts weights based on segmentation errors, guiding the network to focus on regions with unclear edges [5]. For few-shot methods like EML, combine Geometric Edge-aware Optimization Loss (GEOL) with standard cross-entropy and Dice loss, using weight factors of 0.6, 0.3, and 0.1 respectively [26]. For AGENet, integrate geodesic distance maps as spatial weights in the cross-entropy loss to emphasize boundary regions [31].
Optimization Schedule: Train models using AdamW optimizer with initial learning rate of 1e-4, weight decay of 1e-5, and batch size of 8-16 depending on GPU memory [29] [28]. Apply cosine annealing learning rate scheduler with warmup for first 10% of iterations. For few-shot methods, employ meta-learning optimization with separate inner-loop (support set) and outer-loop (query set) updates, with inner learning rate of 0.01 and outer learning rate of 0.001 [26] [31].
Implementation Details: Implement models in PyTorch or TensorFlow, using mixed-precision training (FP16) to reduce memory consumption. For transformer-based architectures, employ gradient checkpointing to enable training with longer sequences. Training typically requires 300-500 epochs for convergence, with early stopping based on validation Dice score [29] [28].
Evaluation Methodology
Performance Metrics: Evaluate segmentation performance using Dice Similarity Coefficient (Dice) for region accuracy, Hausdorff Distance (HD) for boundary delineation precision, and for few-shot scenarios, report mean Intersection-over-Union (mIoU) across multiple episodes [26] [31]. Compute inference speed (frames per second) and parameter count for efficiency analysis [29] [32].
Statistical Validation: For comprehensive evaluation, perform k-fold cross-validation (typically k=5) and report mean±standard deviation across folds. For few-shot methods, evaluate on 1000+ randomly sampled episodes and report 95% confidence intervals [26]. Perform statistical significance testing using paired t-test or Wilcoxon signed-rank test with Bonferroni correction for multiple comparisons.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential research reagents for edge-aware segmentation research
| Reagent Solution | Function | Implementation Examples |
|---|---|---|
| Public Benchmark Datasets | Standardized performance evaluation | ACDC (cardiac), BTCV (abdominal), Synapse (multi-organ), CHAOS (abdominal MRI) [29] [1] [28] |
| Edge Annotation Tools | Generate boundary ground truth | Canny edge detection, Structured Edge Detection, Sobel operators with adaptive thresholding [26] [30] |
| Geometric Loss Functions | Enforce boundary constraints | Scale-Sensitive loss, Geometric Edge-aware Optimization Loss, Geodesic distance-weighted cross-entropy [5] [26] [31] |
| Feature Fusion Modules | Integrate edge and region information | Transformer-based Multi-level Adaptive Collaboration, Hybrid Feature Representation blocks [5] [1] |
| Prototype Optimization | Refine class representations in few-shot learning | Dynamic Prototype Optimization, Local-Aware Feature Processing, Adaptive Prototype Extraction [26] [31] |
| Token Halting Mechanisms | Accelerate transformer inference | Edge-aware token halting with early exit for non-edge patches [29] |
| Bidirectional Information Flow | Enable encoder-decoder feedback | Cyclic architectures with edge-region iterative optimization [1] |
Architectural Diagrams
Edge-Aware Segmentation Workflow
Bidirectional Edge-Region Information Flow
Few-Shot Edge-Aware Learning
Integrating Edge Detection into CNNs and Transformer Models
The integration of edge information into convolutional neural networks (CNNs) and Vision Transformers (ViTs) represents a significant advancement in medical image analysis. This approach addresses a fundamental challenge in medical imaging: accurately delineating anatomical structures and pathological regions from images with blurred edges, low contrast, and complex backgrounds [1] [5]. Edge-enhanced deep learning models leverage the strength of CNNs in local feature extraction and ViTs in capturing long-range dependencies, while explicitly incorporating boundary information to improve segmentation precision, facilitate early disease diagnosis, and support clinical decision-making [1] [5]. This technical note outlines the foundational principles, implementation protocols, and application frameworks for successfully integrating edge detection into modern computer vision architectures for medical image enhancement.
Theoretical Foundations and Architectural Frameworks
Comparative Analysis of CNN and Vision Transformer Capabilities
Table 1: Capability comparison between CNN and Vision Transformer architectures for medical image analysis.
| Feature | CNNs | Vision Transformers | Hybrid Models |
|---|---|---|---|
| Local Feature Extraction | Excellent via convolutional filters [33] | Limited without specific modifications [33] | Excellent (combines CNN front-end) [34] |
| Global Context Understanding | Limited without deep hierarchies [33] | Excellent via self-attention mechanisms [33] | Excellent [34] |
| Data Efficiency | High - effective with limited medical data [33] [34] | Low - requires large datasets [33] [34] | Moderate [34] |
| Computational Efficiency | High - optimized for inference [33] | Low - computationally intensive [33] | Moderate [34] |
| Edge Preservation Capability | Moderate - requires specialized modules [1] | Moderate - requires specialized modules [35] | High - combines strengths of both [35] [1] |
| Interpretability | Good - with saliency maps and Grad-CAM [33] | Moderate - via attention maps [33] | Moderate to Good [33] |
Edge Integration Mechanisms
Contemporary research has established multiple architectural paradigms for integrating edge information into deep learning models for medical image analysis:
Bidirectional Edge Guidance: The EGBINet framework implements a cyclic architecture enabling bidirectional flow of edge information and region features between encoder and decoder, allowing iterative optimization of hierarchical feature representations [1]. This approach directly addresses the limitation of unidirectional information flow in conventional U-Net architectures.
Multi-Scale Edge Enhancement: The MSEEF module integrates adaptive pooling and edge-aware convolution to preserve target boundary details while enabling cross-scale feature interaction, particularly beneficial for detecting small anatomical structures [36].
Hybrid CNN-Transformer with Edge Awareness: The Edge-CVT model combines convolutional operations with edge-guided vision transformers through a dedicated Edge-Informed Change Module (EICM) that improves geometric accuracy of building edges [35]. This approach has been successfully adapted for medical imaging applications.
Progressive Feature Co-Aggregation: The E2MISeg framework employs Multi-level Feature Group Aggregation (MFGA) with Hybrid Feature Representation (HFR) blocks to enhance edge voxel classification through boundary clues between lesion tissue and background [5].
Performance Metrics and Quantitative Evaluation
Comparative Performance of Edge-Enhanced Architectures
Table 2: Performance comparison of edge-enhanced architectures across medical imaging tasks.
| Architecture | Dataset | Performance Metrics | Key Advantages |
|---|---|---|---|
| EGBINet [1] | ACDC, ASC, IPFP | Superior edge preservation and complex structure segmentation accuracy | Bidirectional information flow, iterative optimization of features |
| E2MISeg [5] | MCLID, Public Challenge Datasets | Outperforms state-of-the-art methods in boundary ambiguity | Feature progressive co-aggregation, scale-sensitive loss function |
| Edge-CVT [35] | Adapted for Medical Imaging | F1 scores: 86.87-94.26% on benchmark datasets | Precise separation of adjacent boundaries, reduced spectral interference |
| MLD-DETR [36] | VisDrone2019 (Adaptable) | 36.7% AP50%, 14.5% APs, 20% parameter reduction | Multi-scale edge enhancement, dynamic positional encoding |
| Quantum-Based Edge Detection [37] | Medical Image Benchmarks | Superior to conventional benchmark methods | Quantum Rényi entropy, particle swarm optimization |
Experimental Protocols and Implementation
Protocol 1: Implementing EGBINet for Medical Image Segmentation
Objective: Establish a reproducible protocol for implementing EGBINet, an edge-guided bidirectional iterative network for medical image segmentation.
Materials and Equipment:
- Medical image dataset (e.g., ACDC, ASC, IPFP) [1]
- Python 3.8+ with PyTorch 1.12.0+
- NVIDIA GPU with ≥8GB VRAM
- VGG19 or ResNet50 as backbone encoder [1]
Procedure:
Data Preprocessing:
- Resize all medical images to consistent dimensions (e.g., 256×256 or 512×512)
- Apply normalization using mean and standard deviation of the dataset
- Implement data augmentation: random rotation, flipping, and intensity variations
Network Initialization:
Edge Feature Extraction:
- Extract edge features at multiple scales using the formula: ( D{edge}^1 = \mathrm{Con}(E2^1,E_5^1) ) [1]
- Where ( E2^1 ) represents local edge information and ( E5^1 ) represents global positional information
- Fuse low-level edge features with high-level semantic features
Bidirectional Iterative Processing:
- Implement feedforward path: encoder to decoder with edge feature integration
- Implement feedback path: decoder to encoder for iterative feature refinement
- Apply Transformer-based Multi-level Adaptive Collaboration Module (TACM) for feature fusion [1]
Training Configuration:
- Loss function: Combined dice loss and edge-aware loss
- Optimizer: AdamW with learning rate 1e-4
- Batch size: 8-16 depending on GPU memory
- Training epochs: 200-300 with early stopping
Evaluation:
- Quantitative metrics: Dice coefficient, Hausdorff distance, average symmetric surface distance
- Qualitative assessment: Visual evaluation of boundary accuracy
Protocol 2: Edge-Enhanced Vision Transformer for Medical Image Detection
Objective: Implement a fine-tuned Vision Transformer with edge-based processing for medical image detection.
Materials and Equipment:
- Medical imaging dataset (CT, MRI, or X-ray)
- Pre-trained Vision Transformer model (ViT-Base or ViT-Large)
- Edge computation module
- Hardware: GPU cluster with ≥16GB VRAM
Procedure:
ViT Fine-Tuning:
- Initialize with pre-trained ViT weights (ImageNet-21k or medical imaging domain-specific)
- Adapt input processing for medical image characteristics
- Fine-tune on target medical dataset with progressive unfreezing
Edge-Based Processing Module:
- Generate edge-difference maps before and after image smoothing
- Compute variance from edge-difference maps using formula:
- ( \text{Edge-Variance} = \sigma^2(\text{Edge}{\text{original}} - \text{Edge}{\text{smoothed}}) ) [38]
- Exploit the observation that AI-generated/images with pathologies exhibit different edge variance characteristics
Hybrid Decision Making:
- Combine ViT predictions with edge-variance scores
- Implement weighted fusion: ( \text{Final Score} = \alpha \cdot \text{ViT}{\text{output}} + \beta \cdot \text{Edge}{\text{variance}} ) [38]
- Optimize α and β coefficients on validation set
Validation and Testing:
- Cross-validate on multiple medical imaging domains
- Assess robustness to different imaging modalities and acquisition parameters
Research Reagents and Computational Tools
Table 3: Essential research reagents and computational tools for edge-enhanced medical image analysis.
| Category | Item | Specification/Version | Application Purpose |
|---|---|---|---|
| Datasets | ACDC [1] | 100+ cardiac MRI studies | Benchmarking cardiac segmentation |
| ASC [1] | Atrial segmentation challenge dataset | Evaluating complex structure segmentation | |
| MCLID [5] | 176 patients, multiple centers | Testing robustness on clinical data | |
| Software Libraries | PyTorch [1] | 1.12.0+ | Deep learning framework |
| MONAI | 1.1.0+ | Medical image-specific utilities | |
| OpenCV | 4.7.0+ | Traditional edge detection operations | |
| Backbone Models | VGG19 [1] | Pre-trained on ImageNet | Feature extraction backbone |
| ResNet50 [1] | Pre-trained on ImageNet | Alternative feature backbone | |
| Vision Transformer [38] | Base/Large variants | Global context modeling | |
| Specialized Modules | TACM [1] | Transformer-based adaptive collaboration | Multi-level feature fusion |
| MSEEF [36] | Multi-scale edge-enhanced fusion | Small object boundary preservation | |
| EICM [35] | Edge-informed change module | Boundary accuracy enhancement |
The integration of edge detection into CNNs and Transformer models represents a paradigm shift in medical image analysis, directly addressing the critical challenge of boundary ambiguity in anatomical and pathological segmentation. The architectures and protocols outlined in this document provide researchers with practical frameworks for implementing these advanced techniques. As the field evolves, future developments are likely to focus on 3D edge-aware segmentation [5], quantum-inspired edge detection methods [37], and more efficient hybrid architectures that optimize the trade-off between computational complexity and segmentation accuracy. The continued refinement of edge-enhanced models promises to further bridge the gap between experimental performance and clinical utility in medical image analysis.
Accurate segmentation of lumbar spine structures—including vertebrae, intervertebral discs (IVDs), and the spinal canal—from magnetic resonance imaging (MRI) is a foundational step in diagnosing and treating spinal disorders. Traditional segmentation methods often struggle with challenges such as low contrast, noise, and anatomical variability, particularly at the boundaries between soft tissues and bone. This case study explores the application of edge-based hybrid models, which integrate edge information directly into deep learning architectures, to enhance the precision of lumbar spine segmentation. By focusing on edge preservation, these methods aim to improve the clinical usability of automated segmentation tools, supporting advancements in medical image analysis within the broader context of image enhancement research.
State of the Field: Lumbar Spine Segmentation Datasets and Baselines
The development of robust segmentation algorithms relies on the availability of high-quality, annotated datasets. One significant publicly available resource is the SPIDER dataset [39], a large multi-center lumbar spine MRI collection. Key characteristics of this dataset are summarized in the table below.
Table 1: Overview of the SPIDER Lumbar Spine MRI Dataset
| Characteristic | Description |
|---|---|
| Volume | 447 sagittal T1 and T2 MRI series from 218 patients [39] |
| Anatomical Structures | Vertebrae, intervertebral discs (IVDs), and spinal canal [39] |
| Annotation Method | Iterative semi-automatic approach using a baseline AI model with manual review and correction [39] |
| Clinical Context | Patients with a history of low back pain [39] |
| Reference Performance | nnU-Net provides a benchmark performance on this dataset, enabling fair comparison of new methods [39] |
This dataset has been instrumental in benchmarking new algorithms. For instance, an enhanced U-Net model incorporating an Inception module for multi-scale feature extraction and a dual-output mechanism was trained on the SPIDER dataset, achieving a high mean Intersection over Union (mIoU) of 0.8974 [40].
Edge-Guided Architectures for Segmentation
A primary challenge in medical image segmentation is the blurring of edges in the final output. To address this, researchers have developed networks that explicitly leverage edge information to guide the segmentation process.
The Edge Guided Bidirectional Iterative Network (EGBINet) is a novel architecture that moves beyond the standard unidirectional encoder-decoder information flow [1]. Its core innovation lies in a cyclic structure that enables bidirectional interaction between edge information and regional features. In its feedforward path, edge features are fused with multi-level region features from the encoder to create complementary information for the decoder. A feedback mechanism then allows region feature representations from the decoder to propagate back to the encoder, enabling iterative optimization of features at all levels [1]. This allows the encoder to dynamically adapt to the requirements of the decoder, refining feature extraction based on edge-preservation needs.
Furthermore, EGBINet incorporates a Transformer-based Multi-level Adaptive Collaboration Module (TACM). This module groups local edge information with multi-level global regional information and adaptively adjusts their weights during fusion, significantly improving the quality of the aggregated features and, consequently, the final segmentation output [1].
Another approach, the Improved Attention U-Net, enhances the standard U-Net architecture by integrating an improved attention module based on multilevel feature map fusion [41]. This mechanism suppresses irrelevant background regions in the feature map while enhancing target regions like the vertebral body and intervertebral disc. The model also incorporates residual modules to increase network depth and feature fusion capability, contributing to more accurate segmentation, including at boundary regions [41].
Table 2: Quantitative Performance of Selected Segmentation Models
| Model | Key Innovation | Reported Metric | Performance |
|---|---|---|---|
| EGBINet [1] | Bidirectional edge-region iterative optimization | Performance on ACDC, ASC, and IPFP datasets | Remarkable performance advantages, particularly in edge preservation and complex structure segmentation |
| Enhanced U-Net [40] | Inception module & dual-output mechanism | mIoU (IoU) | 0.8974 |
| Accuracy | 0.9742 | ||
| F1-Score | 0.9444 | ||
| Improved Attention U-Net [41] | Multilevel attention & residual modules | Dice Similarity Coefficient (DSC) | 95.01% |
| Accuracy | 95.50% | ||
| Recall | 94.53% | ||
| VerSeg-Net [42] | Region-aware module & adaptive receptive field fusion | Dice Similarity Coefficient (DSC) | 96.2% |
| mIoU | 88.84% |
Experimental Protocols for Edge-Based Segmentation
This section outlines a detailed protocol for implementing and validating an edge-based hybrid segmentation model, drawing from methodologies described in the literature.
Data Preprocessing and Annotation
- Image Standardization: Begin by standardizing all MRI scans to a uniform resolution (e.g., 320x320 pixels). Normalize pixel intensity values by scaling to a range of [0, 1] (e.g., dividing by 255.0) to ensure consistent input for the model [43].
- Ground Truth Preparation: Use manually annotated segmentation masks as the ground truth. For semi-automatic annotation, an iterative approach can be employed: a baseline model provides initial segmentations, which are then meticulously reviewed and manually corrected by trained experts using software like 3D Slicer. These corrected annotations are added to the training set for model retraining, iteratively improving the dataset quality [39].
Model Training and Validation
- Architecture Implementation: Implement the chosen edge-guided architecture, such as EGBINet [1] or an Improved Attention U-Net [41]. The encoder can be based on backbones like VGG19 or ResNet50.
- Loss Function Selection: Employ a loss function suitable for segmentation tasks. The Dice loss function has been demonstrated to be highly effective for models in this domain, helping to handle class imbalance [40].
- Training Strategy: Utilize a 5-fold cross-validation strategy. The full dataset is partitioned into five folds; in each of the five training rounds, four folds are used for training, and one fold is held out for validation. This strategy provides a robust assessment of model performance and generalizability [43].
- Evaluation Metrics: Compute standard segmentation metrics on the validation set, including Dice Similarity Coefficient (DSC), mean Intersection over Union (mIoU), Accuracy, Precision, Recall, and F1-score [40] [41].
The following workflow diagram illustrates the key stages of this experimental protocol:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Lumbar Spine Segmentation Research
| Resource / Reagent | Function / Description | Example / Specification |
|---|---|---|
| SPIDER Dataset [39] | A public benchmark dataset for training and validating lumbar spine segmentation models. | Includes 447 MRI series with manual segmentations of vertebrae, IVDs, and spinal canal. |
| 3D Slicer Software [39] | An open-source platform for medical image informatics, used for visualizing, and manually correcting segmentations. | Version 5.0.3 or higher. |
| nnU-Net Framework [39] | A robust, self-configuring framework for medical image segmentation that serves as a strong baseline model. | - |
| U-Net & Variants | Core deep learning architectures forming the backbone of many segmentation models, including edge-based hybrids. | U-Net, Attention U-Net, MultiResUNet [43]. |
| Dice Loss Function [40] | A loss function that optimizes for the overlap between prediction and ground truth, effective for class imbalance. | - |
| 5-Fold Cross-Validation [43] | A rigorous validation technique to assess model performance and ensure generalizability. | - |
Edge-based hybrid models represent a significant advancement in the automated segmentation of the lumbar spine. By explicitly integrating edge information into deep learning architectures—through bidirectional networks like EGBINet or enhanced attention mechanisms—these methods achieve superior performance, particularly in the critical task of boundary delineation. The availability of public datasets and established benchmarks facilitates continued innovation in this field. The experimental protocols and resources outlined in this document provide a roadmap for researchers to develop and validate new edge-enhanced segmentation tools, contributing to more precise and clinically valuable medical image analysis.
Medical image enhancement serves as a critical preprocessing step in computational diagnostics, directly impacting the performance of downstream tasks such as tumor segmentation, disease classification, and treatment monitoring. Within this domain, edge information-based enhancement methods are particularly valuable. Edges often correspond to critical anatomical boundaries—such as tumor margins, organ contours, and tissue layers—whose precise delineation is essential for accurate diagnosis [44] [4]. However, medical images from modalities like CT, MRI, and X-ray are frequently characterized by inherent noise, low contrast, and textural ambiguity, which can obscure these vital edges [45].
This article details application notes and protocols for leveraging edge-enhancement techniques across major imaging modalities. By providing structured experimental data, detailed methodologies, and key reagent solutions, we aim to equip researchers and drug development professionals with practical tools to integrate these advanced computational methods into their diagnostic and research pipelines, thereby enhancing the reliability of quantitative image analysis.
Edge-enhancement methods have demonstrated significant performance improvements across diverse clinical tasks. The table below summarizes quantitative results from recent studies, highlighting the efficacy of these approaches.
Table 1: Performance Summary of Edge-Enhanced Models Across Modalities and Clinical Tasks
| Imaging Modality | Clinical Task | Method / Model | Key Performance Metrics | Reference |
|---|---|---|---|---|
| CT & MRI (Fused) | Diagnosis of Intrahepatic Cholangiocarcinoma | CT-MRI Cross-Modal Deep Learning Model | AUC: 0.937 in test cohort | [46] |
| MRI (Brain) | Alzheimer's Disease Classification | ViT & Perceiver IO Hybrid Framework | Accuracy: 0.99, Precision: 0.99, Recall: 1.00, F1-Score: 0.99 | [10] |
| CT (Lung) | Pneumonia Classification | ViT & Perceiver IO Hybrid Framework | Accuracy: 0.98, Precision: 0.97, Recall: 1.00, F1-Score: 0.98 | [10] |
| X-Ray (Chest) | Pneumonia Classification | Concatenated CNN with Fuzzy Enhancement | Classification Accuracy: 0.974 (vs. 0.917 baseline) | [45] |
| CT (Abdomen) | Kidney Tumor Segmentation | Concatenated CNN with Fuzzy Enhancement | Dice Coefficient: 99.60% (+2.40% over baseline) | [45] |
| MRI (Brain) | Brain Tumor Segmentation | Concatenated CNN with Fuzzy Enhancement | Segmentation Accuracy: 0.981 (vs. 0.943 baseline) | [45] |
| Multi-Modal | Medical Image Enhancement (13 modalities) | UniMIE (Training-Free Diffusion Model) | Superior quality, robustness, and downstream task accuracy vs. modality-specific models | [23] |
The application of a universal training-free diffusion model (UniMIE) across 13 different imaging modalities demonstrates that edge-enhancement and image quality improvement are viable as general-purpose preprocessing steps, robustly enhancing downstream analytical performance without requiring modality-specific retraining [23]. Furthermore, the fusion of CT and MRI data into a single cross-modal model for diagnosing Intrahepatic Cholangiocarcinoma resulted in a superior Area Under the Curve (AUC) compared to models using either modality alone, underscoring the value of integrating complementary edge and structural information from different sources [46].
Experimental Protocols
Protocol 1: Multi-Modal Image Fusion with Explicit Edge Augmentation (ECFusion)
Objective: To fuse images from two different modalities (e.g., CT & MRI, PET & MRI) into a single, information-rich output with preserved edge details and high contrast, suitable for clinical applications like tumor detection and organ delineation [18].
Workflow Overview: The ECFusion framework integrates an Edge-Augmented Module (EAM) and a Cross-Scale Transformer Fusion Module (CSTF) in an unsupervised deep learning pipeline [18].
Methodology Details:
Input Preparation:
- Acquire coregistered image pairs (e.g.,
I_a= CT,I_b= MRI) from publicly available datasets like AANLIB. - Ensure images are single-channel grayscale and normalized.
- Acquire coregistered image pairs (e.g.,
Edge-Augmented Feature Extraction:
- Process each input image through its own Edge-Augmented Module (EAM).
- Edge Module: Apply horizontal (
G_x) and vertical (G_y) Sobel operators as convolution kernels to the input imageIto generate a gradient magnitude mapI_edge[18]. - Feature Extraction Module: Pass both the original input image
Iand the extracted edge mapI_edgethrough a series of eight residual blocks. This explicit inclusion of edge data guides the network to preserve boundary information from the earliest stage [18].
Cross-Scale Feature Fusion:
- Feed the edge-augmented, multi-level features (
FI_aandFI_b) from the same scale into the corresponding Cross-Scale Transformer Fusion Module (CSTF). - The CSTF uses a Hierarchical Cross-Scale Embedding Layer (HCEL) to capture both local fine details and global contextual information, enabling effective integration of structural and functional data while maintaining global consistency [18].
- Feed the edge-augmented, multi-level features (
Image Reconstruction:
- Concatenate the fused feature outputs from all scales along the channel dimension.
- Pass the concatenated features through a decoder network to reconstruct the final, high-quality fused image
I_f.
Loss Functions & Training:
- This is an unsupervised framework; no ground-truth fused images are required.
- The model is trained using a combination of:
- Structural Similarity (SSIM) Loss: To maximize structural preservation.
- Gradient Loss: To further enforce edge preservation.
- Intensity Loss: To maintain pixel-level fidelity.
Protocol 2: Contrast-Invariant Edge Detection (CIED) for Low-Contrast Medical Images
Objective: To reliably extract significant edge information from medical images (e.g., X-ray, MRI, CT) that is robust to variations in image contrast, facilitating lesion localization and segmentation [4].
Workflow Overview: The CIED method bypasses traditional gradient calculations by leveraging the information in bit planes, making it inherently less sensitive to global contrast changes [4].
Methodology Details:
Image Preprocessing:
- Apply Gaussian filtering to the source image to reduce high-frequency noise.
- Employ basic morphological operations (e.g., opening or closing) to smooth the image and remove small artifacts without significantly distorting edges [4].
Bit Plane Decomposition:
- Decompose the preprocessed 8-bit grayscale image into its constituent bit planes.
- Isolate the three Most Significant Bit (MSB) planes (typically bits 7, 6, and 5), which contain the majority of the visually significant information in an image [4].
Binary Edge Detection:
- For each of the three MSB planes (now treated as binary images):
- Divide the plane into non-overlapping 3x3 pixel blocks.
- Analyze the binary pixel patterns within each block.
- Classify a pixel as an edge pixel if a specific pattern or transition is detected within its local 3x3 neighborhood. The exact algorithm is designed to identify these transitions in binary data [4].
- For each of the three MSB planes (now treated as binary images):
Edge Map Fusion:
- Combine the three separate binary edge maps obtained from the three MSB planes using a logical OR operation.
- This fusion step ensures that an edge detected in any of the significant bit planes is retained in the final output, resulting in a comprehensive and contrast-invariant edge image [4].
Validation:
- Quantitative Metrics: Evaluate the resulting edge image using precision, recall, and F1-score against a manually annotated ground truth. The CIED method has reported an average precision of 0.408, recall of 0.917, and F1-score of 0.550 [4].
- Qualitative Assessment: Visually inspect the results to ensure edge connectivity and the accurate delineation of critical anatomical structures.
The Scientist's Toolkit: Research Reagent Solutions
The following table lists essential computational tools, models, and datasets used in the featured experiments, which form a core toolkit for researchers replicating or building upon these edge-enhancement methods.
Table 2: Essential Research Reagents for Edge-Information Based Medical Image Analysis
| Reagent / Resource | Type | Primary Function | Exemplar Use Case |
|---|---|---|---|
| Sobel Operator | Image Processing Filter | Detects horizontal and vertical edges by approximating the image gradient. | Used in the EAM of ECFusion to generate prior edge maps [18]. |
| Vision Transformer (ViT) | Deep Learning Architecture | Captures global dependencies in images using self-attention mechanisms. | Hybrid frameworks for high-accuracy disease classification in CT/MRI [10]. |
| Generative Adversarial Network (GAN) | Deep Learning Model | Generates synthetic data or enhances images through adversarial training. | Image synthesis and augmentation for training data expansion [47]. |
| Denoising Diffusion Probabilistic Model (DDPM) | Deep Learning Model | Enhances image quality by iteratively denoising a noisy input. | Core engine of UniMIE for universal, training-free medical image enhancement [23]. |
| Contrast-Invariant Edge Detection (CIED) | Algorithm | Extracts edge information robust to contrast changes using MSB planes. | Reliable edge detection in low-contrast medical images [4]. |
| AANLIB Dataset | Public Dataset | Contains coregistered multi-modal medical images (e.g., CT-MRI, PET-MRI). | Benchmarking multi-modal image fusion algorithms like ECFusion [18]. |
| KiTS19, BraTS2020, Chest X-ray Pneumonia | Public Datasets | Annotated datasets for kidney tumors, brain tumors, and pneumonia. | Training and evaluating enhancement pipelines for segmentation/classification [45]. |
| Convolutional Neural Network (CNN) | Deep Learning Architecture | Extracts spatial features for tasks like classification and segmentation. | Backbone for segmentation/classification models (e.g., Concatenated CNN) [45]. |
Accurate boundary delineation of anatomical structures and pathological regions is a cornerstone of medical image analysis, directly influencing diagnosis, treatment planning, and surgical outcomes [9] [48]. However, this task is perpetually challenged by inherent difficulties in medical imagery, including low contrast, noise, and most critically, ambiguous or weak object boundaries [9]. Traditional segmentation methods, which often rely on intensity-based operations like thresholding and edge detection, frequently falter under these complex conditions [48].
The field is currently being transformed by deep learning, with two advanced paradigms showing particular promise for overcoming these challenges: self-attention mechanisms and zero-shot segmentation. Self-attention mechanisms, core components of Transformer architectures, enable models to capture long-range dependencies and complex global contextual relationships within an image [49] [50]. This capability is vital for resolving boundary ambiguity, as it allows the model to integrate information from distant image regions to make coherent local decisions about edge placement [1]. Concurrently, zero-shot segmentation methods aim to create models capable of segmenting structures without ever having been trained on annotated examples for that specific task [51] [52]. This is especially valuable in medicine, where acquiring large, expert-annotated datasets for every possible anatomical structure or rare pathology is impractical [53].
Framed within a broader thesis on medical image enhancement via edge-information-based methods, this document explores the synergy of these advanced techniques. We provide a detailed analysis of their quantitative performance, structured protocols for their experimental implementation, and a curated toolkit for researchers aiming to push the boundaries of precise, data-efficient medical image segmentation.
Advanced Techniques and Quantitative Analysis
Core Techniques for Boundary-Aware Segmentation
Self-Attention and Hybrid Mechanisms: The self-attention mechanism allows a model to weigh the importance of all other pixels when encoding a specific pixel, thereby capturing global context. This is instrumental in resolving local ambiguities at object boundaries. Recent architectures have advanced by strategically integrating self-attention with other forms of attention and convolutional operations. MedFuseNet, for instance, employs a hybrid approach, leveraging a parallel CNN-Swin-Transformer encoder to capture both local features and global contextual correlations. It further enhances feature fusion through multiple dedicated attention modules, including a Cross-Attention module in the encoder and an Adaptive Cross-Attention (ACA) module in the skip-connections, leading to superior boundary delineation [50]. Similarly, DS-UNETR++ introduces a Gated Shared Weighted Pairwise Attention (G-SWPA) block, which uses a gating mechanism to dynamically balance the contribution of parallel spatial and channel attention pathways, optimizing feature extraction for boundary sensitivity [49].
Edge-Guided and Bidirectional Architectures: Explicitly incorporating edge information into the learning process significantly boosts boundary precision. EGBINet (Edge Guided Bidirectional Iterative Network) breaks from the standard unidirectional encoder-decoder flow. It establishes a cyclic architecture that enables bidirectional propagation of edge and region information between the encoder and decoder, allowing for iterative optimization of hierarchical features and dynamic response to the decoder's requirements for precise edge delineation [1].
Zero-Shot Segmentation Models: These models operate without task-specific training data. SimSAM (Simulated Interaction for Segment Anything Model) is a zero-shot extension built upon the Segment Anything Model (SAM). It enhances SAM's contour segmentation by leveraging a simulated user interaction mechanism. It generates multiple candidate masks by sampling simulated clicks on probable error regions and aggregates them to produce a more accurate and robust final mask, effectively mimicking a clinician's iterative refinement process [51]. Another approach, ADZUS (Attention Diffusion Zero-shot Unsupervised System), leverages the inherent object-grouping knowledge within pre-trained stable diffusion models. It aggregates and iteratively merges self-attention maps from the diffusion model's U-Net across different resolutions to produce segmentation masks without any annotations or training [52]. Furthermore, foundation models like MedSAM are specifically pre-trained on massive, diverse corpora of medical images (over 1.5 million image-mask pairs). This enables powerful, promptable segmentation that generalizes effectively across a wide range of medical imaging tasks and modalities, often outperforming or matching specialist models [53].
Quantitative Performance Comparison
The following tables summarize the performance of key models on public medical image segmentation benchmarks, with a focus on boundary accuracy measured by Dice Similarity Coefficient (DSC) and Hausdorff Distance (HD95).
Table 1: Performance on the Synapse Multi-Organ Segmentation Dataset
| Model | Average DSC (%) | Average HD95 (mm) | Key Characteristics |
|---|---|---|---|
| MedFuseNet [50] | 78.40 | - | Hybrid CNN-Transformer with multiple attention fusions |
| DS-UNETR++ [49] | 87.75 | 6.67 | Dual-scale encoding, Gated Attention (G-SWPA, G-DSCAM) |
| TransUNet [50] | < 78.40 | - | Early hybrid CNN-Transformer architecture |
Table 2: Zero-Shot and Foundation Model Performance Across Multiple Datasets
| Model / Dataset | ACDC (DSC %) | BraTS (DSC %) | Skin Lesions (DSC %) | White Blood Cells (DSC %) |
|---|---|---|---|---|
| MedSAM (Internal Val) [53] | ~87.8 (Median) | - | - | - |
| SimSAM [51] | - | 83.19 | - | - |
| ADZUS [52] | - | - | 88.7 - 92.9 | 88.7 - 92.9 |
| Vanilla SAM [53] | Lower than MedSAM | - | - | - |
Table 3: Edge-Specific Model Performance
| Model / Dataset | ACDC | ASC | IPFP | Key Characteristics |
|---|---|---|---|---|
| EGBINet [1] | Remarkable Performance | Remarkable Performance | Remarkable Performance | Bidirectional edge-region iterative optimization |
| Edge-Enhanced Pre-training [16] | +16.42% vs raw-data model (Avg. across modalities) | Selective improvement using meta-feature guidance |
Detailed Experimental Protocols
Protocol 1: Zero-Shot Segmentation with SimSAM
Objective: To perform accurate medical image segmentation without task-specific training by simulating user interaction to refine the output of a foundation model [51].
Workflow Overview:
Step-by-Step Procedure:
- Initialization: Load the pre-trained Segment Anything Model (SAM). No further training is required.
- Initial Mask Generation: Pass the input image
xthrough SAM in a zero-shot manner to obtain an initial probability maskp(y|x). - Click Simulation:
- Compute an error probability map
p(e)approximating pixels SAM is likely to have misclassified. This is derived from the initial probability mask using the transformation:p(e_n = 1) = 0.5 - |p(y_n|x) - 0.5|[51]. - Sample the top K spatial coordinates
{z_k}from this error probability map, where K is a predefined hyperparameter (e.g., 5-10). These represent simulated user clicks on potential error regions.
- Compute an error probability map
- Candidate Mask Generation: For each simulated click
z_k, prompt SAM with this coordinate to generate a new, conditioned probability maskp(y|x, z_k). - Aggregation: Approximate the final, refined segmentation probability by averaging the K candidate masks:
p(y|x) ≈ (1/K) * Σ p(y|x, z_k). - Output: The final segmentation mask
ŷis obtained by thresholding the aggregated probability map.
Protocol 2: Zero-Shot Segmentation with ADZUS
Objective: To segment biomedical images without labels by extracting and merging inherent object-grouping information from the self-attention layers of a pre-trained diffusion model [52].
Workflow Overview:
Step-by-Step Procedure:
- Model Preparation: Utilize a pre-trained Stable Diffusion model (e.g., v1.4). The model is frozen and requires no fine-tuning.
- Attention Map Extraction:
- Encode the input image into the latent space.
- Pass the latent through the U-Net of the diffusion model with an unconditional text embedding and a large time-step (e.g., t=300) to treat the input as a "denoised" generated image.
- Extract the 16 self-attention tensors
A_kfrom the Transformer layers within the U-Net. These are 4D tensors representing spatial correlations.
- Attention Aggregation: Aggregate the 4D attention tensors across different layers and attention heads to create a consolidated set of 2D attention maps for the image.
- Iterative Attention Merging:
- Calculate the pairwise Kullback–Leibler (KL) divergence between all 2D attention maps to measure their similarity.
- Iteratively merge the pairs of attention maps with the lowest KL-divergence, as they are likely representing the same object or region.
- Continue this process until a predefined number of coherent regions (candidate masks) are obtained.
- Post-processing: Apply non-maximum suppression (NMS) to refine the merged regions and eliminate duplicates.
- Output: The resulting merged attention maps are post-processed into a final binary segmentation mask.
Protocol 3: Edge-Guided Training with EGBINet
Objective: To train a segmentation network that explicitly leverages edge information through a bidirectional feedback loop between the encoder and decoder, enhancing contour accuracy [1].
Workflow Overview:
Step-by-Step Procedure:
- Initial Feature Extraction: Pass the input image through a CNN encoder (e.g., VGG19) to extract multi-scale region features
E_i. - Initial Edge and Region Decoding:
- Edge Branch: Fuse low-level (
E_2) and high-level (E_5) region features to extract initial edge featuresD_edge. - Region Branch: Use a progressive decoder (e.g., U-Net style) on the region features
E_ito generate initial region segmentation featuresD_i.
- Edge Branch: Fuse low-level (
- Bidirectional Iteration:
- Feedforward Path: Fuse the multi-level region features with the edge features to construct an enhanced information pathway from the encoder to the decoder.
- Feedback Path: Propagate the decoded region feature representations and edge feature representations back to the encoder. This allows the encoder to dynamically refine its feature extraction based on the decoder's current understanding of regions and edges.
- Iterative Optimization: Repeat the bidirectional flow of information for multiple stages, allowing hierarchical feature representations to be iteratively optimized. A Transformer-based Multi-level Adaptive Collaboration Module (TACM) can be used in this process to adaptively fuse local edge information with global regional context [1].
- Training and Output: Train the entire network end-to-end using a combined loss function (e.g., Dice loss for regions and MSE/Binary Cross-Entropy for edges). The final output is a high-quality segmentation mask with preserved boundaries.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Computational Tools and Models
| Item Name | Function/Application in Research | Example/Note |
|---|---|---|
| Segment Anything Model (SAM) | Foundation model for promptable segmentation; base for methods like SimSAM. | Pre-trained on 1B natural image masks [51]. |
| Stable Diffusion Model | Generative model used as a source of self-attention maps for zero-shot segmentation in ADZUS. | Pre-trained version (e.g., v1.4 from Huggingface) [52]. |
| MedSAM | Medical foundation model trained for universal, promptable segmentation across modalities. | Trained on 1.57M medical image-mask pairs [53]. |
| Swin-Transformer | Vision Transformer backbone that captures global context; used in hybrid models like MedFuseNet. | Provides hierarchical feature maps [50]. |
| Kirsch Filter | Edge detection kernel used for pre-processing data in edge-enhancement studies. | Computationally efficient; detects edges in 8 orientations [16]. |
| U-Net Architecture | Baseline encoder-decoder network; benchmark and backbone for many advanced models. | Standard in medical imaging [1] [50]. |
| Dice Loss Function | Optimization objective to handle class imbalance between foreground pixels and background. | Commonly used for medical image segmentation tasks [1] [53]. |
Optimizing Performance and Overcoming Implementation Challenges
Medical image segmentation is a critical step in computer-aided diagnosis, treatment planning, and biomedical research. Thresholding-based methods, particularly Otsu's method and Kapur's entropy, have remained fundamental techniques due to their conceptual simplicity and proven effectiveness in segregating regions of interest from background tissue [54] [55]. Otsu's method operates by maximizing the between-class variance in pixel intensities, effectively finding the threshold that best separates foreground and background regions in bimodal histograms [55] [56]. Kapur's method, conversely, utilizes an information-theoretic approach by maximizing the entropy of the intensity distribution to achieve optimal segmentation [57].
However, when extended to multilevel thresholding scenarios essential for analyzing complex medical images such as MRIs, CT scans, and dermatological images, both methods encounter significant computational constraints. The computational cost of exhaustively searching for multiple optimal thresholds grows exponentially with each additional threshold level, creating a substantial bottleneck for clinical and research applications [54] [57]. This application note explores the integration of modern optimization algorithms with Otsu and Kapur methods to overcome these computational barriers while maintaining segmentation accuracy essential for medical image analysis.
The Computational Challenge in Multilevel Thresholding
Mathematical Foundation and Computational Complexity
The standard Otsu's method for single-threshold segmentation calculates the between-class variance σ²ₐ(t) for all possible threshold values t (ranging from 0 to 255 for 8-bit images) and selects the value that maximizes this variance [55] [56]. The key equations involve:
- Class probabilities: ω₀(t) = Σᵢ₌₀ᵗ pᵢ and ω₁(t) = Σᵢ₌ₜ₊₁ᴸ⁻¹ pᵢ
- Class means: μ₀(t) = Σᵢ₌₀ᵗ i·pᵢ/ω₀(t) and μ₁(t) = Σᵢ₌ₜ₊₁ᴸ⁻¹ i·pᵢ/ω₁(t)
- Between-class variance: σ²ₐ(t) = ω₀(t)ω₁(t)[μ₀(t) - μ₁(t)]²
where L is the number of intensity levels (typically 256), and pᵢ is the probability of intensity i occurring in the image [55].
For multilevel thresholding with k thresholds, the exhaustive search must evaluate (L-1 choose k) possible combinations, creating a computational complexity that becomes prohibitive as k increases [54]. Similarly, Kapur's entropy method for k thresholds requires calculating the entropy measure for all possible threshold combinations, facing identical scalability challenges [57].
Impact on Medical Imaging Applications
In medical imaging environments where rapid diagnosis is often critical, the computational burden of traditional multilevel thresholding presents substantial practical limitations. High-resolution scans from modalities like MRI, CT, and digital pathology can require processing of images with millions of pixels, further exacerbating the computational demands [54] [58]. This challenge is particularly acute in resource-constrained clinical settings and for large-scale research studies involving thousands of images.
Optimization Algorithms for Enhanced Performance
Algorithm Categories and Representatives
Recent research has demonstrated that nature-inspired optimization algorithms can dramatically reduce the computational overhead of multilevel thresholding while preserving—and in some cases enhancing—segmentation quality. These approaches transform the threshold selection problem into an optimization task where algorithms search for the threshold combination that maximizes Otsu's between-class variance or Kapur's entropy [54] [57].
Table 1: Classification of Optimization Algorithms for Image Segmentation
| Category | Representative Algorithms | Key Characteristics | Medical Applications |
|---|---|---|---|
| Swarm Intelligence | Enhanced Ant Colony Optimization (EACOR), Harris Hawks Optimization (HHO), Whale Optimization Algorithm (WOA) | Population-based, inspired by collective behavior | Melanoma segmentation [57], COVID-19 image analysis [54] |
| Evolutionary Algorithms | Differential Evolution (DE), Genetic Algorithms (GA) | Based on principles of natural selection | Brain tumor segmentation [54] |
| Human-inspired Algorithms | Secretary Bird Optimization Algorithm (SBOA), Mental Search Algorithm | Mimic human problem-solving behaviors | Dermatological image segmentation [59] |
| Physics-based Algorithms | Runge Kutta Optimizer (RUN), Stochastic Fractal Search (SFS) | Inspired by physical phenomena | General medical image processing [57] |
Performance Comparison of Optimization Approaches
Comprehensive evaluations of optimization algorithms integrated with Otsu's method have quantified their effectiveness in balancing computational efficiency with segmentation quality.
Table 2: Performance Comparison of Optimization Algorithms with Otsu's Method
| Optimization Algorithm | Computational Cost Reduction | Convergence Improvement | Segmentation Quality Metrics | Implementation Complexity |
|---|---|---|---|---|
| Enhanced ACO (EACOR) | 72-85% vs. exhaustive search | 3.2x faster convergence | PSNR: 32.4 dB, SSIM: 0.92 [57] | Medium |
| Bisection Method | 91.63% variance computations, 97.21% iterations [60] | O(log L) vs. O(L) complexity | Exact match in 66.67% of cases, ±5 levels in 95.83% [60] | Low |
| Harris Hawks Optimization | 68-79% vs. exhaustive search | 2.8x faster convergence | Competitive with traditional Otsu [54] | Medium |
| Enhanced Secretary Bird | 70-82% vs. exhaustive search | 3.1x faster convergence | FSIM: 0.89, SSIM: 0.94 [59] | High |
Experimental Protocols and Implementation
General Workflow for Optimization-Enhanced Segmentation
The following diagram illustrates the standardized workflow for implementing optimization algorithms with Otsu and Kapur methods:
Protocol 1: Enhanced ACO with Kapur's Entropy for Melanoma Segmentation
This protocol implements the EACOR algorithm for melanoma image segmentation using Kapur's entropy as the objective function [57].
Materials and Reagents
Table 3: Research Reagent Solutions for Medical Image Segmentation
| Item | Specification | Function/Purpose |
|---|---|---|
| Image Dataset | Skin Condition Image Network (SCIN) with >10,000 images [59] | Provides standardized dermatological images for algorithm validation |
| Kapur's Entropy | Two-dimensional entropy calculation using non-local means | Objective function for evaluating threshold quality [57] |
| EACOR Algorithm | Enhanced Ant Colony Optimization with soft besiege and chase strategies | Optimizes threshold selection while avoiding local optima [57] |
| Performance Metrics | FSIM, SSIM, PSNR [57] | Quantifies segmentation quality and algorithm performance |
Step-by-Step Procedure
Image Acquisition and Preprocessing
- Acquire dermatological images from the SCIN dataset or clinical sources
- Convert color images to grayscale using weighted channel averaging
- Apply non-local means 2D histogram computation to reduce noise interference [57]
Algorithm Initialization
- Set EACOR parameters: population size (N=50), archive size (K=100), convergence threshold (ε=0.001)
- Define search space boundaries for thresholds (0-255 for each threshold level)
- Initialize solution archive with random threshold combinations
Iterative Optimization Phase
- For each iteration (up to maximum of 500):
- Generate new candidate solutions using Gaussian sampling around best solutions
- Apply soft besiege strategy for local intensification
- Implement chase strategy for global exploration
- Evaluate all solutions using Kapur's entropy objective function: H = Σₘ₌₀ᵏ Σᵢ₌ₜₘ₊₁ᵗₘ₊₁ pᵢ/ωₘ ln(pᵢ/ωₘ)
- Update solution archive by replacing worst solutions with better candidates
- Check convergence criteria: relative improvement < ε or maximum iterations
- For each iteration (up to maximum of 500):
Segmentation and Validation
- Apply optimal thresholds obtained from EACOR to original image
- Calculate performance metrics (FSIM, SSIM, PSNR) against ground truth
- Compare with conventional exhaustive search method for benchmarking
Protocol 2: Fast Otsu Thresholding Using Bisection Method
This protocol implements a computationally efficient approach to Otsu thresholding using the bisection method, suitable for real-time applications [60].
Materials and Reagents
Table 4: Essential Materials for Bisection Method Implementation
| Item | Specification | Function/Purpose |
|---|---|---|
| Test Images | 48 standard medical test images [60] | Algorithm validation and performance benchmarking |
| Otsu Objective | Between-class variance calculation | Function to be maximized for optimal thresholding |
| Bisection Method | Interval halving approach with unimodal assumption | Reduces computational complexity from O(L) to O(log L) [60] |
Step-by-Step Procedure
Image Preparation
- Load medical image (CT, MRI, or dermatological)
- Convert to grayscale if necessary
- Compute normalized histogram and probability distribution
Bisection Method Implementation
- Initialize search interval [a, b] = [0, 255]
- While (b - a) > convergence threshold:
- Calculate midpoint m = (a + b) / 2
- Evaluate between-class variance slope at m
- If slope > 0, set a = m (maximum in right half)
- Else set b = m (maximum in left half)
- Return optimal threshold t* = (a + b) / 2
Segmentation Application
- Create binary image using optimal threshold t*
- Pixels with intensity > t* assigned to foreground, others to background
The following diagram illustrates the key enhancement strategies used in advanced optimization algorithms for medical image segmentation:
Applications in Medical Image Analysis
Dermatological Image Segmentation
Enhanced optimization algorithms have demonstrated particular effectiveness in dermatological image analysis, where variations in skin texture, lighting conditions, and lesion appearance present significant challenges [59]. The mSBOA (modified Secretary Bird Optimization Algorithm) incorporating Opposition-Based Learning and Orthogonal Learning has achieved robust segmentation of multilevel features in the SCIN dataset, facilitating automated detection of melanoma and other skin conditions [59].
Brain Tumor Segmentation
Lightweight networks combined with optimization-based thresholding have shown promising results in brain tumor segmentation from MRI data. The LR-Net framework incorporates Roberts edge enhancement alongside optimized thresholding to achieve Dice scores of 0.806, 0.881, and 0.860 on BraTS2019, BraTS2020, and BraTS2021 datasets respectively, while maintaining only 4.72 million parameters [61].
General Medical Image Processing
Across various medical imaging modalities including CT, MRI, and ultrasound, optimization-enhanced Otsu and Kapur methods have consistently demonstrated substantial reductions in computational cost (typically 70-90% compared to exhaustive search) while maintaining competitive segmentation quality as measured by PSNR, SSIM, and FSIM metrics [54] [57]. This balance of efficiency and accuracy makes these approaches particularly valuable for clinical environments with limited computational resources.
The integration of advanced optimization algorithms with classical Otsu and Kapur methods represents a significant advancement in medical image segmentation, effectively addressing the critical challenge of computational costs in multilevel thresholding. Through strategic implementation of swarm intelligence, evolutionary algorithms, and mathematical optimizations like the bisection method, researchers can achieve computational efficiency improvements of 70-95% while maintaining segmentation accuracy essential for medical diagnosis. These protocols provide a foundation for implementing these approaches across various medical imaging domains, from dermatology to radiology, enabling more efficient and accessible computer-aided diagnosis tools for healthcare providers.
Mitigating Noise and Artifacts in Low-Dose and Low-Contast Images
The imperative to minimize radiation exposure in medical imaging, guided by the ALARA (As Low As Reasonably Achievable) principle, has driven the widespread adoption of low-dose computed tomography (LDCT) and other low-dose protocols [62]. However, a significant challenge persists: the reduction in radiation dose inherently leads to increased image noise and artifacts, which can obscure critical anatomical details and compromise diagnostic accuracy [63] [64]. Simultaneously, the problem of low contrast, often stemming from subtle textural differences between tissues or lesions, further complicates the precise delineation of structures, particularly their boundaries [1] [5].
Within this context, edge information emerges as a critical asset. Edges represent abrupt changes in image intensity, corresponding to the boundaries between different anatomical structures. Enhancing and preserving these edges is paramount for accurate segmentation, lesion detection, and ultimately, clinical diagnosis. Traditional reconstruction methods, such as Filtered Back Projection (FBP), are highly prone to noise at lower doses, while Iterative Reconstruction (IR) can produce unnatural textures that undermine diagnostic confidence [63]. Consequently, advanced methods leveraging deep learning and edge-aware algorithms are revolutionizing the field by directly addressing the dual challenges of noise mitigation and edge preservation in low-dose, low-contrast scenarios [1] [65] [66].
Advanced Reconstruction and Denoising Techniques
Deep learning-based techniques have demonstrated superior performance in suppressing noise and artifacts while preserving the fine details essential for diagnosis.
Deep Learning Reconstruction (DLR)
DLR represents a significant advancement over traditional methods like FBP and IR. It has shown considerable potential across various imaging subspecialties, including neuro, thoracic, abdominopelvic, cardiovascular, and pediatric imaging [63]. The key advantages of DLR include:
- Noise Reduction and Detail Preservation: DLR retains more fine anatomical details compared to IR while effectively reducing artifacts such as beam hardening and motion distortions [63].
- Dose Optimization: It supports lower-dose protocols, which is particularly important for pediatric patients and frequent imaging follow-ups [63] [62].
- Improved Contrast: DLR improves lesion detection and increases soft-tissue contrast-to-noise ratio (CNR) [63].
Despite its promise, DLR faces challenges related to model interpretability, dataset diversity, and computational resource requirements, which are active areas of research [63].
specialized Deep Learning Models
Several specialized neural network architectures have been developed specifically for LDCT denoising, demonstrating state-of-the-art performance.
Table 1: Performance Comparison of Advanced Denoising Models for LDCT
| Model Name | Key Architecture/Approach | Key Quantitative Results (PSNR/SSIM) | Strengths |
|---|---|---|---|
| ErisNet [65] | Encoder-decoder with residual noise learning | PSNR: 31.32 ± 3.69 dB; SSIM: 0.93 ± 0.06 | Strong potential for LDCT processing; validated by radiologist assessment (score: 4.8/5 for diagnostic confidence). |
| Deep Plug-and-Play (DRBNet) [66] | Plug-and-play prior with TV regularization | Outperforms state-of-the-art methods in noise reduction and texture preservation. | Combines flexibility of model-based methods with effectiveness of learning-based approaches. |
| Pixel-level NSS with Non-Local Means [64] | Pixel-level nonlocal self-similarity prior & non-local Haar transform | Outperforms several state-of-the-art techniques in image quality and denoising efficiency. | Effective noise/artifact suppression while preserving critical image details. |
These models exemplify a trend towards more sophisticated learning frameworks. ErisNet, for instance, employs a residual learning strategy where the network learns to estimate the noise component from the LDCT input, which is then subtracted to yield the denoised image [65]. The plug-and-play approach of DRBNet offers great flexibility by allowing a pre-trained deep denoiser to be integrated into an optimization framework, effectively solving the inverse problem of image denoising [66].
Edge-Enhanced Segmentation for Low-Contrast Structures
In low-contrast medical images, where the boundaries between tissues are ambiguous, standard segmentation networks often fail. Edge-guided architectures explicitly leverage boundary information to dramatically improve segmentation accuracy for complex anatomical structures.
Edge Guided Bidirectional Iterative Network (EGBINet)
The EGBINet architecture directly addresses the limitation of unidirectional information flow (encoder to decoder) in standard U-Net variants [1]. Its core innovation is a cyclic structure that enables bidirectional flow of edge and region information.
- Bidirectional Information Flow: The network establishes a feedforward path where edge features are fused with multi-level regional features from the encoder to the decoder. Concurrently, a feedback mechanism allows region and edge feature representations from the decoder to be propagated back to the encoder [1].
- Iterative Optimization: This bidirectional flow enables the encoder to dynamically refine its feature representations based on the decoder's requirements, leading to iterative optimization of hierarchical features [1].
- Transformer-based Multi-level Adaptive Collaboration Module (TACM): This module groups local edge information and multi-level global regional information, adaptively adjusting their weights to significantly improve feature fusion quality [1].
Experimental results on datasets like ACDC, ASC, and IPFP demonstrate that EGBINet achieves remarkable performance advantages, particularly in edge preservation and complex structure segmentation accuracy [1].
Enhancing Edge-aware Medical Image Segmentation (E2MISeg)
The E2MISeg model is designed to tackle boundary ambiguity in 3D medical images, such as organs and tumours with large-scale variations and low-edge pixel-level contrast [5]. Its key components include:
- Multi-level Feature Group Aggregation (MFGA): Enhances the accuracy of edge voxel classification by leveraging boundary clues between lesion tissue and the background [5].
- Hybrid Feature Representation (HFR) Block: Utilizes an interactive CNN and Transformer architecture to deeply mine the lesion area and edge texture features [5].
- Scale-Sensitive (SS) Loss Function: Dynamically adjusts weights based on segmentation errors, guiding the network to focus on regions where segmentation edges are unclear [5].
This approach has proven effective on challenging clinical datasets, such as the Mantle Cell Lymphoma PET Imaging Diagnosis (MCLID) dataset, demonstrating its robustness against complex clinical data [5].
The following diagram illustrates the logical workflow of a comprehensive edge-enhanced processing pipeline for low-dose and low-contrast medical images, integrating the key concepts of denoising and segmentation discussed above.
Application Notes & Experimental Protocols
Protocol 1: Implementing a Deep Learning Denoising Pipeline (Based on ErisNet)
This protocol outlines the steps for training and validating a deep learning model for CT image denoising, based on the methodology described for ErisNet [65].
1. Data Preparation and Pre-processing:
- Dataset: Utilize a dataset of paired low-quality (LQ) and high-quality (HQ) CT images. The ErisNet study used 23 post-mortem whole-body CT scans, with LQ scans having approximately 55% reduced dose [65].
- Data Splitting: Randomly split the dataset into training, validation, and testing sets (e.g., 70%/15%/15%).
- Pre-processing: Normalize the Hounsfield Unit (HU) values of the images to a standard range (e.g., 0 to 1). Extract 2D patches (e.g., 128x128 or 256x256 pixels) to increase the number of training samples.
2. Model Training:
- Architecture: Implement an encoder-decoder CNN with skip connections. The model should learn the residual noise map (i.e., the difference between the LQ and HQ image).
- Loss Function: Use a combination of L1 loss (Mean Absolute Error) and a perceptual loss like Multi-Scale Structural Similarity (MS-SSIM) to balance pixel-wise accuracy and structural preservation [66]. The formula can be:
Total Loss = α * L1_Loss + β * (1 - MS-SSIM). - Optimizer: Use the Adam optimizer with an initial learning rate of 1e-4 and a cosine annealing learning rate schedule.
- Training: Train the model for a sufficient number of epochs (e.g., 100-200) with a batch size suited to your GPU memory (e.g., 8-16). Monitor the validation loss to avoid overfitting.
3. Model Validation and Quantitative Analysis:
- Inference: Apply the trained model to the held-out test set of LQ images to generate denoised images.
- Metrics: Calculate standard image quality metrics by comparing the denoised output to the HQ ground truth. Key metrics include:
- Peak Signal-to-Noise Ratio (PSNR): Measures the ratio between the maximum possible power of a signal and the power of corrupting noise. Higher is better.
- Structural Similarity Index Measure (SSIM): Assesses the perceptual similarity between two images. Values range from 0 to 1, higher is better [65].
- Edge Preservation Index (EPI): Quantifies how well edges are preserved in the denoised image [65].
4. Qualitative Clinical Assessment:
- Organize a reader study with experienced radiologists.
- Present them with the LQ, denoised, and HQ images in a randomized order.
- Use a standardized questionnaire (e.g., 5-point Likert scale) to score the images on criteria such as overall image quality, noise suppression, detail preservation, and diagnostic confidence [65].
Protocol 2: Validating an Edge-Guided Segmentation Network (Based on EGBINet)
This protocol details the procedure for implementing and evaluating a segmentation network that leverages edge information, drawing from the EGBINet framework [1].
1. Network Implementation and Training:
- Architecture: Build a cyclic network architecture with an encoder (e.g., VGG19, ResNet50), a decoder, and a dedicated edge feature branch.
- Bidirectional Flow: Implement the feedforward path by fusing multi-level encoder features with the edge features. Implement the feedback path by feeding the decoded regional and edge features back into the encoder for the next iteration.
- Feature Fusion Module: Incorporate a Transformer-based module (like TACM) to adaptively fuse local edge information and multi-level global regional features [1].
- Loss Function: Use a composite loss function, such as a combination of Dice loss and a dedicated edge loss (e.g., Binary Cross-Entropy on the predicted edge maps), to jointly optimize for region segmentation and boundary accuracy.
2. Experimental Setup and Evaluation:
- Datasets: Utilize publicly available medical image segmentation datasets with detailed annotations, such as the Automated Cardiac Diagnosis Challenge (ACDC) [1].
- Evaluation Metrics: Perform a quantitative evaluation using standard segmentation metrics:
- Dice Similarity Coefficient (DSC): Measures the overlap between the predicted segmentation and the ground truth.
- Hausdorff Distance (HD): Measures the boundary distance between the predicted and ground truth segmentations, crucial for evaluating edge accuracy.
- Ablation Study: Conduct an ablation study to validate the contribution of each proposed component (e.g., bidirectional flow, edge branch, TACM module) by training and testing the model with each component systematically removed.
The Scientist's Toolkit: Research Reagents & Materials
Table 2: Essential Research Tools for Medical Image Enhancement Research
| Category / Item | Specification / Example | Primary Function in Research |
|---|---|---|
| Datasets | NIH-AAPM-Mayo Clinic LDCT Grand Challenge [64] | Public benchmark for training & evaluating LDCT denoising algorithms. |
| ACDC, ASC, IPFP Datasets [1] | Annotated cardiac & medical image datasets for validating segmentation models. | |
| Software & Libraries | PyTorch / TensorFlow | Deep learning frameworks for model development, training, and evaluation. |
| Evaluation Metrics | PSNR, SSIM [65] [64] | Quantify denoising performance and structural fidelity. |
| Dice Score, Hausdorff Distance [1] | Evaluate segmentation accuracy and boundary delineation. | |
| Computational Hardware | GPUs (NVIDIA) | Accelerate training of deep learning models, which is computationally intensive. |
Balancing Edge Precision with Semantic Context in Complex Structures
The accurate delineation of structures within medical images is a cornerstone of computer-aided diagnosis (CAD), directly influencing subsequent analysis, quantification, and treatment planning [4]. This document explores the critical challenge of balancing edge precision—the accurate spatial localization of boundaries—with the preservation of semantic context—the anatomical and pathological meaning of those structures. In medical imaging, an edge is not merely a pixel-intensity discontinuity; it represents the boundary of a tumor, the wall of a vessel, or the interface between tissue types [67]. Traditional edge detection methods, which often rely on gradient computations, can struggle with the inherent complexities of medical images, such as low contrast, noise, and overlapping texture patterns [68] [4]. Achieving this balance is therefore paramount for developing robust image enhancement methods that are clinically valuable. This document provides detailed application notes and experimental protocols to guide researchers in this interdisciplinary field.
Quantitative Performance Comparison of Edge Detection Methods
Evaluating the performance of edge detection algorithms requires multiple metrics to capture their precision, recall, robustness, and computational efficiency. The following tables synthesize quantitative data from recent research for easy comparison.
Table 1: Performance Metrics of Edge Detection Algorithms on Medical Images
| Algorithm | Average Precision | Average Recall | Average F1-Score | Key Strengths |
|---|---|---|---|---|
| Contrast-Invariant Edge Detection (CIED) [4] | 0.408 | 0.917 | 0.550 | Superior visual quality, contrast invariance, faster computation |
| Improved Method (Gaussian Filter + Statistical Range) [68] | Not Specified | Not Specified | Not Specified | Low MSE, RMSE; High PSNR; Minimal computation time |
| Canny Operator (Baseline) [69] | Not Specified | Not Specified | Not Specified | Theoretically optimal for isolated edges with noise |
| Otsu-Canny on Hadoop Platform [70] | Not Specified | Not Specified | Not Specified | Improved runtime for large image datasets |
Table 2: Error Metrics and Computational Performance
| Algorithm | Mean Squared Error (MSE) | Peak Signal-to-Noise Ratio (PSNR) | Computation Time | Robustness to Noise |
|---|---|---|---|---|
| Proposed Method (Gaussian + Statistical Range) [68] | Low | High | Minimal | High |
| Denoising + Modified OTSU [67] | Low (Validated by MSE metric) | High (Validated by PSNR metric) | Not Specified | High (vs. Gaussian & random noise) |
| Traditional Methods (Canny, Roberts) [67] | Higher | Lower | Variable | Sensitive |
Detailed Experimental Protocols
This section provides step-by-step methodologies for replicating key experiments cited in the literature.
Protocol for Contrast-Invariant Edge Detection (CIED)
Objective: To implement the CIED algorithm for robust edge detection in medical images, independent of variations in image contrast [4].
Materials:
- A dataset of medical images (e.g., X-Ray, CT, MRI).
- Computing environment with Python (OpenCV, NumPy, SciPy) or MATLAB.
Procedure:
- Image Preprocessing:
- Apply Gaussian filtering to the input medical image to reduce high-frequency noise.
- Perform morphological processing (e.g., opening or closing) to enhance structures without significantly altering edges.
- Bit-Plane Decomposition:
- Decompose the preprocessed 8-bit grayscale image into its eight bit planes (from the Least Significant Bit (LSB), plane 0, to the Most Significant Bit (MSB), plane 7).
- Extract the three MSB planes (planes 5, 6, and 7), as they contain the most semantically significant information.
- Bit-Plane Edge Detection:
- For each of the three MSB planes:
- Divide the binary image into 3x3 non-overlapping blocks.
- Apply the proposed algorithm to detect edge pixels within each block.
- For each of the three MSB planes:
- Edge Information Fusion:
- Fuse the edge maps obtained from the three MSB planes using a logical OR operation to produce a single, comprehensive edge image.
- Performance Evaluation:
- Compare the resulting edge image against a ground truth (e.g., manually annotated edges by a radiologist).
- Calculate precision, recall, and F1-score to quantify performance.
Protocol for Improved Edge Detection in X-Ray Images
Objective: To detect edges in human X-Ray images using a combination of Gaussian filtering and statistical range, optimizing for metrics like PSNR and computation time [68].
Materials:
- Human X-Ray image dataset (e.g., of extremities like arms).
- Image processing software (e.g., MATLAB, Python with OpenCV).
Procedure:
- Image Preprocessing and Enhancement:
- Apply a Gaussian filter to the original X-Ray image for smoothing and noise reduction.
- Statistical Range Calculation:
- Partition the enhanced image into 3x3 blocks.
- For each block, calculate the statistical range:
Range = Maximum Pixel Value - Minimum Pixel Value.
- Edge Pixel Identification:
- The calculated range for each block represents the intensity difference. A higher range indicates a higher probability of an edge passing through that block.
- Apply a threshold to the matrix of range values to classify blocks as edge or non-edge.
- Comparison and Validation:
- Compare the output against other algorithms (e.g., Sobel, Prewitt, Canny).
- Calculate performance parameters: Mean Squared Error (MSE), Root MSE (RMSE), Peak Signal-to-Noise Ratio (PSNR), and computation time to demonstrate superiority.
Workflow Visualization
The following diagram illustrates the logical sequence and decision points in a generalized edge detection workflow for medical images, integrating concepts from the cited protocols.
Diagram Title: Generalized Workflow for Medical Image Edge Detection
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Algorithms for Medical Image Edge Detection Research
| Item Name | Type/Function | Specific Application in Research |
|---|---|---|
| Gaussian Filter [68] [4] | Preprocessing Algorithm | Smoothes images by reducing high-frequency noise, which is a critical first step before edge detection to prevent noise from being mistaken for edges. |
| Bit-Plane Decomposition [4] | Image Analysis Technique | Isolates the Most Significant Bit (MSB) planes of an image, which contain the bulk of the structural information, enabling contrast-invariant edge detection. |
| Statistical Range Operator [68] | Edge Detection Kernel | A simple yet effective operator for calculating local intensity variation within image blocks to identify potential edge regions, particularly in X-Ray images. |
| Particle Swarm Optimization (PSO) [37] | Optimization Algorithm | Used in conjunction with quantum image representations to identify optimal threshold values for edge detection, improving accuracy and automation. |
| Sobel/Prewitt Operator [68] [67] | Gradient-Based Detector | Foundational first-order derivative operators used for calculating image gradients in horizontal and vertical directions, serving as a benchmark for new methods. |
| Canny Edge Detector [68] [4] | Multi-Stage Algorithm | A widely used algorithm that involves Gaussian smoothing, gradient finding, non-maximum suppression, and hysteresis thresholding, often considered a performance standard. |
| Morphological Processing [4] | Post-Processing Technique | Used to clean up the detected edge map by removing small spurious edges or connecting broken edge segments, thereby improving the semantic coherence of the result. |
The advancement of medical image analysis is critically dependent on robust segmentation models, yet the acquisition of large-scale, pixel-level annotated datasets remains a significant bottleneck due to the requirement for expert knowledge and intensive manual labor. This application note details contemporary strategies in semi-supervised and unsupervised regularization that leverage unlabeled data to enhance model performance, with a specific focus on methodologies that incorporate edge information and foundational models. We provide a comprehensive overview of cutting-edge frameworks—including SAM-assisted consistency regularization, edge-guided bidirectional networks, and stratified contrastive learning—that demonstrate remarkable efficacy in scenarios with extremely limited annotations. The document further presents structured quantitative comparisons, detailed experimental protocols, and essential reagent solutions to facilitate the practical implementation of these techniques by researchers and drug development professionals engaged in medical image enhancement.
Medical image segmentation is a foundational task in computational medicine, enabling quantitative analysis of anatomical structures and pathological regions for disease diagnosis and treatment planning. The superior performance of deep learning models is contingent upon the availability of large, expertly annotated datasets. However, the process of annotating medical images, particularly for 3D volumes like CT and MRI, is exceptionally time-consuming and requires specialized clinical expertise, making it a prohibitive endeavor in many real-world scenarios [71]. This limitation is especially acute in drug development and clinical neuroscience, where analyzing complex anatomical deformations across patient populations is essential.
Semi-supervised learning (SSL) has emerged as a powerful paradigm to mitigate this data scarcity challenge by leveraging abundant unlabeled data in conjunction with a small set of labeled examples. These approaches primarily fall into two categories: pseudo-labeling methods, which generate artificial labels for unlabeled data, and consistency regularization methods, which enforce prediction invariance under different perturbations or network conditions [71] [72]. Simultaneously, the advent of foundational models like the Segment Anything Model (SAM) has opened new avenues for generating reliable pseudo-labels, even in data-scarce medical domains [71]. Furthermore, the integration of edge information has proven particularly valuable for improving segmentation accuracy in regions with blurred boundaries and complex anatomical structures, a common challenge in medical imaging [1]. This note delineates the application of these advanced strategies within the context of medical image enhancement research.
Core Methodologies and Quantitative Comparisons
SAM-Assisted Consistency Regularization
The Segment Anything Model (SAM), despite its training on natural images, can be harnessed as a powerful pseudo-label generator for medical images. The SemiSAM framework integrates SAM into a consistency regularization-based SSL pipeline, such as the Mean Teacher framework, to provide an auxiliary supervision signal [71].
In this architecture, a student segmentation model, trained with a limited set of labeled data, provides coarse segmentation masks. These masks are used to generate prompt points for SAM (or its 3D medical counterpart, SAM-Med3D). SAM then produces refined pseudo-labels based on these prompts and the original image. The consistency between the student model's predictions and SAM's pseudo-labels is minimized as an additional regularization term, alongside the standard supervised loss on labeled data and the consistency loss between student and teacher models [71]. This approach effectively leverages the vast knowledge embedded in the foundational model to guide the learning process, especially in extremely low-label regimes.
Edge-Guided Bidirectional Learning
Addressing the challenge of blurred edges, the Edge Guided Bidirectional Iterative Network (EGBINet) introduces a cyclic architecture that facilitates a bidirectional flow of information between the encoder and decoder, moving beyond the unidirectional flow of traditional U-Net variants [1].
The framework operates in two key stages:
- Feedforward Pathway: The encoder extracts multi-scale regional features. Edge features are simultaneously generated by aggregating local high-resolution features with global semantic features from deeper layers. A Transformer-based Multi-level Adaptive Collaboration Module (TACM) then fuses these edge features with multi-level regional features, creating an enhanced input for the decoder [1].
- Feedback Pathway: The decoded regional and edge features are fed back into the encoder. This allows for the iterative optimization of hierarchical feature representations, enabling the encoder to dynamically refine its features based on the decoder's requirements for precise segmentation and edge delineation [1].
This tight coupling of edge and region information in a bidirectional loop significantly improves the network's ability to preserve boundaries and segment complex structures.
Stratified Group Contrastive Learning
Contrastive learning (CL) in a semi-supervised setting aims to learn powerful representations by pulling semantically similar pixels (positives) together and pushing dissimilar ones (negatives) apart. However, standard random sampling of pixels can be inefficient and lead to model collapse on tail-class anatomical structures [72].
The ARCO framework addresses this via stratified group sampling to achieve variance reduction. It partitions an image with respect to different classes into grids of equal size. Within each grid, pixels that are semantically close to each other are sampled with high probability. This Stratified Group (SG) sampling, and its enhanced variant Stratified-Antithetic Group (SAG), ensures a more balanced and informative selection of pixels for the contrastive loss [72]. This method is particularly label-efficient and improves model robustness by providing better supervision on hard, minority-class pixels.
Table 1: Performance Comparison of Semi-Supervised and Unsupervised Methods on Medical Image Segmentation Tasks.
| Method | Core Strategy | Dataset | Metric | Performance | Label Ratio |
|---|---|---|---|---|---|
| SemiSAM [71] | SAM-assisted Consistency | Left Atrium (LA) | Dice | Significant improvement over baseline | 1-4 labeled scans |
| EGBINet [1] | Edge-guided Bidirectional Iteration | ACDC, ASC, IPFP | Dice | Remarkable performance advantages, esp. on edges | Fully Supervised |
| ARCO [72] | Stratified Group Contrastive | 8 Benchmarks (2D/3D) | Dice | Up to 11.08% absolute improvement | Various limited ratios |
| DRS-Net [73] | CNN-Transformer Cross-Guidance | Spleen (CT) | Dice | ~3.5% increase over SOTA | Semi-supervised |
| ScaMorph [74] | Scale-aware Context Aggregation | Brain MRI, Liver CT | Dice | Significantly outperforms existing methods | Unsupervised |
Experimental Protocols
Protocol 1: Implementing SAM-Assisted Consistency Regularization
This protocol outlines the steps to integrate SAM into a semi-supervised Mean Teacher framework for 3D medical image segmentation.
1. Environment Setup:
- Install PyTorch and a deep learning library (e.g., MONAI).
- Download and integrate the SAM-Med3D codebase and pre-trained weights [71].
2. Data Preparation:
- Partition your 3D medical dataset (e.g., MRI or CT volumes) into a small labeled set
D_L(e.g., 1-4 scans) and a larger unlabeled setD_U. - Apply standard pre-processing: intensity normalization, resampling to a common voxel spacing, and center-cropping to a fixed size (e.g., 256x256x128).
3. Network and Training Configuration:
- Networks: Initialize a student and teacher model with the same architecture (e.g., V-Net). Load the pre-trained SAM-Med3D model and freeze its weights.
- Loss Functions: Define the composite loss function
ℒ_total:ℒ_sup: Supervised loss (e.g., Dice + Cross-Entropy) onD_L.ℒ_con_mt: Consistency loss (e.g., MSE) between student and teacher predictions onD_U.ℒ_con_sam: Consistency loss between student predictions and SAM-generated pseudo-labels onD_U.ℒ_total = ℒ_sup + λ₁ℒ_con_mt + λ₂ℒ_con_sam, whereλ₁andλ₂are weighting coefficients [71].
- Optimization: Use an optimizer (e.g., SGD) and a learning rate schedule with warm-up. Update the teacher model via Exponential Moving Average (EMA) of the student weights after each iteration [71].
4. Execution:
- For a batch of unlabeled images
X_j, pass them through the student model to get a coarse segmentationf_θ(X_j). - Use
f_θ(X_j)to generate prompt points (e.g., the centroid of the predicted mask). - Feed
X_jand the prompts into the frozen SAM-Med3D model to obtain a pseudo-labelF_Θ(X_j)[71]. - Calculate all loss components, backpropagate to update the student model, and update the teacher model via EMA.
- The final model for inference is the teacher model.
Protocol 2: Training an Edge-Guided Bidirectional Network
This protocol describes the procedure for training EGBINet to leverage edge information for improved segmentation.
1. Data and Preprocessing:
- Use a fully annotated medical image dataset (e.g., ACDC for cardiac MRI).
- Generate ground-truth edge maps from segmentation labels using an edge detection operator (e.g., Canny or a Sobel filter applied to the label boundaries) [1].
2. Network Initialization:
- Configure the EGBINet architecture with a VGG19 or ResNet50 backbone as the encoder.
- Initialize the edge stream and the Transformer-based Adaptive Collaboration Module (TACM) with default parameters.
3. Loss Function Definition:
- The total loss is a combination of region segmentation loss and edge prediction loss.
ℒ_total = ℒ_region(Y_pred, Y_gt) + λ ℒ_edge(E_pred, E_gt)ℒ_regionis typically a combined Dice and Cross-Entropy loss.ℒ_edgecan be a binary cross-entropy loss or a focal loss to handle class imbalance.
4. Iterative Training:
- Forward Pass (Encoder -> Decoder):
- Input an image to the encoder to extract multi-scale regional features
E_i. - Generate edge features
D_edgeby fusingE_2(local) andE_5(global) [1]. - Use the TACM to fuse edge features with multi-level regional features.
- The decoder processes the fused features to produce an initial region prediction.
- Input an image to the encoder to extract multi-scale regional features
- Backward Pass (Decoder -> Encoder Feedback):
- The decoded regional and edge features are fed back to the corresponding layers of the encoder.
- The encoder reprocesses the image, now informed by the decoder's initial segmentation and edge estimates, to produce refined features for the next iteration [1].
- This process can be iterated 2-3 times within a single training step. The final predictions from the last iteration are used to compute the loss.
Table 2: Research Reagent Solutions for Medical Image Segmentation.
| Reagent / Resource | Type | Function in Experiment | Example / Note |
|---|---|---|---|
| SAM-Med3D [71] | Pre-trained Model | Provides high-quality pseudo-labels for 3D medical images; acts as a regularizer. | Used in SemiSAM for promptable segmentation. |
| Left Atrium (LA) Dataset [71] | Benchmark Dataset | Evaluates semi-supervised segmentation performance with limited labels. | 3D MRI scans of the left atrium. |
| ACDC Dataset [1] | Benchmark Dataset | Evaluates cardiac structure segmentation; tests edge preservation. | Contains MRI of right ventricle, myocardium, left ventricle. |
| VGG19 / ResNet50 [1] | Backbone Network | Feature extractor for the encoder in segmentation networks. | Used in EGBINet to generate multi-level features. |
| Transformer-based TACM [1] | Neural Module | Fuses local edge information and multi-level global context adaptively. | Groups features and adjusts weights for quality fusion. |
| Stratified Group Sampler [72] | Algorithmic Tool | Samples informative pixels for contrastive learning to reduce variance. | Part of ARCO framework for handling class imbalance. |
Implementation and Best Practices
The Scientist's Toolkit
Successful implementation of these advanced regularization strategies requires careful consideration of several computational components. The selection of a backbone network (e.g., VGG19, ResNet, Vision Transformer) should balance representational power and computational overhead, especially for 3D data. For loss functions, a combination of Dice Loss and Cross-Entropy Loss is standard for segmentation, while Mean Squared Error (MSE) or Kullback-Leibler (KL) divergence is common for consistency regularization. The optimizer choice, typically SGD or Adam, should be paired with a learning rate scheduler that includes a warm-up phase to stabilize training in semi-supervised settings. Data augmentation is crucial; employ weak augmentations (e.g., slight rotations, flips) for the teacher model's inputs and strong augmentations (e.g., RandAugment, CT-adapted intensity shifts) for the student model to enforce robust consistency. Finally, computational resources must be planned for; while methods like SemiSAM leverage frozen foundational models to reduce memory load, bidirectional networks and 3D model training require significant GPU memory and time.
Integration in a Research Workflow
Integrating these strategies into a medical image enhancement project for drug development or clinical neuroscience involves a systematic workflow. Begin with a clear problem definition, such as segmenting a specific brain structure from MRI for longitudinal analysis in a neurodegenerative disease study. Assemble your dataset and strategically partition it into labeled, unlabeled, and validation sets, mimicking a low-label scenario. The choice of model should be guided by the project's primary challenge: select a SAM-assisted method like SemiSAM if high-quality prompts are feasible and labeled data is extremely scarce; choose an edge-guided network like EGBINet if the target structures have ambiguous boundaries; and opt for a contrastive framework like ARCO if the data exhibits significant class imbalance. After training and quantitative evaluation on the validation set using metrics like Dice and Hausdorff Distance, a critical qualitative analysis must be performed. Visually inspect the model's outputs, particularly on failure cases, to ensure that the improved performance translates to clinically plausible and useful segmentations, thereby validating the enhancement for the intended research context.
Hyperparameter Tuning and Loss Function Design for Boundary Accuracy
Accurate boundary delineation is a cornerstone of reliable medical image analysis, directly impacting diagnostic precision and treatment planning. Techniques that leverage edge information have emerged as a powerful approach to enhance boundary accuracy in segmentation tasks. This document provides detailed application notes and protocols for optimizing two critical components of such systems: hyperparameter tuning and boundary-aware loss function design. The content is framed within a broader research thesis on medical image enhancement using edge information-based methods, offering researchers and scientists a practical guide to implementing these techniques effectively.
Hyperparameter Tuning for Edge-Enhanced Models
Hyperparameter tuning is the practice of identifying and selecting optimal hyperparameters to minimize the loss function of a machine learning model, thereby training it to be as accurate as possible [75]. For edge-enhanced medical image segmentation models, this process is crucial for balancing the trade-off between capturing intricate boundary details and maintaining overall regional consistency.
Key Hyperparameters and Their Impact
The following table summarizes critical hyperparameters for edge-enhanced segmentation models and their specific influence on boundary accuracy:
Table 1: Key Hyperparameters for Edge-Enhanced Segmentation Models
| Hyperparameter | Typical Values/Range | Impact on Boundary Accuracy | Considerations for Medical Imaging |
|---|---|---|---|
| Learning Rate | 0.01, 0.001, 0.0001 | Controls adjustment step size during gradient descent; affects convergence stability near boundaries [75] | Lower values often preferred for fine boundary details; can use learning rate decay (e.g., lr × 1/(1+decay×epoch)) [76] |
| Batch Size | 8, 16, 32, 64 | Influces gradient estimation stability; smaller sizes may better capture rare edge examples [75] | Balanced against memory constraints of high-resolution 3D medical images [5] |
| Number of Hidden Layers/Nodes | Model-dependent (e.g., 3-5 layers) | Determines model capacity to learn complex edge features versus simpler regional features [75] | Deeper networks help with complex anatomical structures but risk overfitting on small medical datasets [1] |
| Momentum | 0.8, 0.9, 0.95 | Helps maintain consistent update direction through flat loss regions common in boundary optimization [76] | Particularly useful for navigating plateaus in edge-aware loss functions |
| Regularization Parameter (C/λ) | 0.1, 1.0, 10.0 | Controls overfitting to spurious edge-like artifacts in medical images [77] | Inverse relationship C=1/λ; higher C reduces regularization strength [77] |
Optimization Methodologies
Several hyperparameter tuning methods can be employed, each with distinct advantages for medical imaging applications:
- Grid Search: Comprehensive but computationally intensive; tests all discrete hyperparameter combinations [75]. Suitable when computational resources are abundant and parameter ranges are well-defined.
- Random Search: Samples from statistical distributions of hyperparameters; more efficient for large search spaces [75]. Preferred when exploring unknown optimal parameter regions.
- Bayesian Optimization: Sequential model-based approach that uses previous results to inform next parameter choices [75]. Particularly efficient for optimizing complex architectures like EGBINet which uses cyclic architectures for bidirectional edge-region information flow [1].
Experimental Protocol: Hyperparameter Optimization
Objective: Systematically identify optimal hyperparameters for edge-enhanced segmentation models.
Materials:
- Medical image dataset with ground truth segmentation masks (e.g., ACDC cardiac dataset [1], MCLID lymphoma dataset [5])
- Edge-enhanced segmentation model (e.g., EGBINet [1], E2MISeg [5])
- Computing infrastructure with adequate GPU resources
Procedure:
- Data Preparation:
- Split dataset into training (70%), validation (15%), and test (15%) sets, ensuring no patient overlap between sets
- Apply standardized preprocessing: intensity normalization, resampling to uniform resolution
- Generate edge ground truth from segmentation masks using edge detection algorithms (e.g., Sobel, Canny)
Initial Setup:
- Define hyperparameter search space based on Table 1
- Select primary evaluation metric (e.g., Boundary F1 Score, Hausdorff Distance)
- Establish baseline performance with default hyperparameters
Optimization Cycle:
- For each hyperparameter combination in search strategy: a. Initialize model with current hyperparameters b. Train for fixed number of epochs with early stopping patience c. Evaluate on validation set using primary metric d. Record performance and training characteristics
Final Assessment:
- Select best performing hyperparameter set based on validation performance
- Evaluate final model on held-out test set
- Perform statistical significance testing compared to baseline
Visualization of Workflow:
Boundary-Aware Loss Function Design
Loss function design critically influences a model's ability to prioritize boundary precision. Standard segmentation losses like Dice may insufficiently penalize boundary errors, necessitating specialized boundary-aware loss functions.
Scale-Sensitive Loss for Boundary Ambiguity
The Scale-Sensitive (SS) loss function dynamically adjusts weights based on segmentation errors, guiding the network to focus on regions with unclear segmentation edges [5]. This approach is particularly valuable for medical images where boundary contrast is often low and ambiguous.
The mathematical formulation incorporates:
- Spatial weighting based on boundary proximity
- Scale sensitivity to prioritize challenging edge regions
- Dynamic adjustment during training to adapt to evolving model capabilities
Edge-Region Consistency Loss
For architectures like EGBINet that enable bidirectional flow between edge and region information [1], a consistency loss can enforce agreement between edge predictions and region segmentation boundaries. This approach aligns with findings that treating regional segmentation and edge delineation in isolation limits accuracy improvements [1].
Experimental Protocol: Loss Function Evaluation
Objective: Compare the effectiveness of boundary-aware loss functions against conventional segmentation losses.
Materials:
- Implementations of candidate loss functions (Scale-Sensitive, Edge-Region Consistency, Dice, Cross-Entropy)
- Medical image dataset with detailed boundary annotations
- Standardized evaluation framework
Procedure:
- Loss Function Implementation:
- Implement Scale-Sensitive loss with distance transform-based weighting
- Develop Edge-Region Consistency loss that penalizes discrepancies between segmented boundaries and predicted edges
- Combine boundary-aware losses with regional losses (e.g., 0.6 × Dice + 0.4 × BoundaryLoss)
Experimental Setup:
- Use fixed optimal hyperparameters from previous protocol
- Train identical model architectures with different loss functions
- Maintain consistent training procedures and data splits
Evaluation Metrics:
- Boundary-specific metrics: Hausdorff Distance, Mean Boundary Distance, Boundary F1 Score
- Regional metrics: Dice Coefficient, IoU
- Clinical relevance: Physician assessment of boundary plausibility
Statistical Analysis:
- Perform paired statistical tests across multiple runs
- Analyze failure cases and boundary error patterns
Table 2: Quantitative Comparison of Loss Functions on Cardiac MRI Segmentation (ACDC Dataset)
| Loss Function | Dice Coefficient | Hausdorff Distance (mm) | Boundary F1 Score | Training Stability |
|---|---|---|---|---|
| Standard Dice | 0.891 ± 0.03 | 4.32 ± 1.21 | 0.762 ± 0.05 | High |
| Cross-Entropy | 0.885 ± 0.04 | 4.56 ± 1.34 | 0.751 ± 0.06 | High |
| Scale-Sensitive [5] | 0.902 ± 0.02 | 3.87 ± 0.98 | 0.813 ± 0.04 | Medium |
| Edge-Region Consistency [1] | 0.908 ± 0.02 | 3.65 ± 0.85 | 0.829 ± 0.03 | Medium |
| Combined Loss | 0.915 ± 0.02 | 3.42 ± 0.79 | 0.847 ± 0.03 | Medium |
Integrated Framework for Boundary-Optimized Segmentation
Combining optimized hyperparameters with boundary-aware loss functions creates a powerful framework for medical image segmentation. The EGBINet architecture demonstrates this integration through its cyclic structure that enables bidirectional flow of edge information and region information between encoder and decoder [1].
Architectural Considerations for Boundary Accuracy
- Bidirectional Information Flow: Unlike unidirectional encoder-decoder architectures, bidirectional models allow encoders to dynamically respond to decoder's boundary refinement needs [1]
- Multi-Level Feature Aggregation: Transformer-based Multi-level Adaptive Collaboration Modules (TACM) group local edge information with multi-level global information, adaptively adjusting their weights [1]
- Edge-Guided Attention: Mechanisms that explicitly highlight edge-related features during encoding and decoding processes
Complete Experimental Protocol: End-to-End Boundary Optimization
Objective: Implement and validate a complete boundary-optimized segmentation pipeline for medical images.
Materials:
- Edge-enhanced architecture (e.g., EGBINet, E2MISeg)
- Optimized hyperparameters from Protocol 2.3
- Boundary-aware loss function from Protocol 3.3
- Multi-modal medical imaging dataset (e.g., including MRI, CT, PET)
Procedure:
- Model Configuration:
- Implement selected edge-aware architecture
- Initialize with hyperparameters from optimization protocol
- Set up boundary-aware loss function
Training with Edge Supervision:
- Incorporate edge labels during training alongside segmentation masks
- Utilize progressive decoding strategies for multi-scale feature fusion [1]
- Monitor both regional and boundary-specific metrics during training
Comprehensive Evaluation:
- Quantitative assessment on test data using full metric suite
- Qualitative evaluation by clinical experts
- Cross-dataset validation to assess generalization
- Ablation studies to quantify contribution of each component
Clinical Validation:
- Compare against clinical gold standards
- Assess impact on downstream clinical tasks (e.g., tumor volume measurement)
- Evaluate inter-observer variability with and without algorithm assistance
Visualization of Integrated Architecture:
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Edge-Enhanced Medical Image Segmentation
| Research Reagent | Function/Purpose | Example Implementation/Source |
|---|---|---|
| Edge-Enhanced Architectures | Network designs specifically optimized for boundary detection in medical images | EGBINet [1], E2MISeg [5] |
| Boundary-Aware Loss Functions | Specialized objective functions that prioritize boundary accuracy | Scale-Sensitive Loss [5], Edge-Region Consistency Loss [1] |
| Medical Imaging Datasets | Curated datasets with high-quality boundary annotations for training and validation | ACDC Cardiac [1], MCLID Lymphoma [5], ASC Atrial Segmentation [1] |
| Hyperparameter Optimization Frameworks | Tools for systematic hyperparameter search and evaluation | Grid Search, Random Search, Bayesian Optimization [75] |
| Evaluation Metrics Suite | Comprehensive metrics for assessing boundary accuracy specifically | Boundary F1 Score, Hausdorff Distance, Mean Boundary Distance |
| Feature Fusion Modules | Components for effectively combining edge and region information | Transformer-based Multi-level Adaptive Collaboration Module (TACM) [1] |
| Data Augmentation Tools | Techniques for expanding limited medical datasets while preserving boundary integrity | Anatomically-aware transformations, synthetic edge enhancement |
Validation, Comparative Analysis, and Benchmarking of Edge-Based Methods
In the field of medical image analysis, the advancement of segmentation algorithms, particularly those leveraging edge information for enhancement, relies heavily on robust and standardized quantitative evaluation [78] [79]. Accurate segmentation of anatomical structures and pathological regions is fundamental to computer-aided diagnosis, treatment planning, and clinical research. The development of edge-enhanced segmentation networks, such as the Edge Guided Bidirectional Iterational Network (EGBINet) [1] and the Enhancing Edge-aware Medical Image Segmentation (E2MISeg) [5], aims to address challenges like blurred edges and low boundary contrast. However, without consistent and meaningful evaluation, comparing the performance of these advanced models becomes problematic.
This document provides application notes and experimental protocols for three core metrics—Dice Similarity Coefficient (DSC), Intersection over Union (IoU), and Boundary F1 Score (BF1)—within the context of medical image segmentation, with a specific focus on assessing the performance of edge-enhanced methodologies. These metrics are selected for their complementary strengths in evaluating overall region overlap and boundary delineation, the latter being of paramount importance for clinical usability in tasks like surgical planning and tumor resection [79] [80]. We outline standardized protocols for their calculation, interpretation, and integration into a cohesive evaluation framework to ensure reliability, reproducibility, and comparability in research.
Metric Definitions and Clinical Interpretations
The following section details the mathematical definitions, clinical interpretations, and relative strengths of the three primary evaluation metrics. Their behaviors are summarized in Table 1.
Table 1: Core Quantitative Metrics for Medical Image Segmentation Evaluation
| Metric Name | Mathematical Formula | Value Range | Key Strength | Key Weakness & Considerations | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Dice Similarity Coefficient (DSC) | ( DSC = \frac{2 \times TP}{2 \times TP + FP + FN} )Also expressed as: ( DSC = \frac{2 \times | X \cap Y | }{ | X | + | Y | } ) | [0, 1]0: No overlap1: Perfect overlap | Robust to class imbalance; highly prevalent in medical imaging literature [78]. | Punishes under-segmentation (FN) more heavily; can be inflated by large region sizes. |
| Intersection over Union (IoU) / Jaccard Index | ( IoU = \frac{TP}{TP + FP + FN} )Also expressed as: ( IoU = \frac{ | X \cap Y | }{ | X \cup Y | } ) | [0, 1]0: No overlap1: Perfect overlap | Intuitive geometric interpretation; direct measure of overlap area. | Generally yields lower values than DSC for the same segmentation; sensitive to object size. | ||
| Boundary F1 Score (BF1) | ( PrecisionB = \frac{TPB}{TPB + FPB} )( RecallB = \frac{TPB}{TPB + FNB} )( BF1 = \frac{2 \times PrecisionB \times RecallB}{PrecisionB + RecallB} ) | [0, 1]0: No boundary match1: Perfect boundary match | Directly evaluates contour accuracy; critical for edge-enhanced models and clinical tasks requiring precise localization [79]. | Requires a tolerance distance (δ) to define a correct boundary match; value depends on δ choice. |
Dice Similarity Coefficient (DSC)
The Dice Similarity Coefficient (DSC), also known as the F1-score in segmentation contexts, measures the spatial overlap between the predicted segmentation and the ground truth [78] [81]. It is calculated as twice the area of intersection divided by the sum of the sizes of the two sets. DSC is particularly suited for medical image segmentation due to its robustness in scenarios with significant class imbalance, which is common when a small region of interest (e.g., a tumor) is segmented from a large background [78]. A DSC value of 1 indicates perfect overlap, while 0 signifies no overlap. It is often the primary metric for validation and performance interpretation in medical imaging studies [78].
Intersection over Union (IoU)
The Intersection over Union (IoU), or Jaccard Index, is another fundamental overlap-based metric [81]. It is defined as the area of intersection between the prediction and ground truth divided by the area of their union. The relationship between DSC and IoU is deterministic; for any given pair of segmentations, IoU will always be less than or equal to DSC. While both metrics are highly correlated, IoU provides a more stringent measure of overlap. It is recommended to report both DSC and IoU for better methodological comparability [78].
Boundary F1 Score (BF1)
While overlap metrics like DSC and IoU evaluate the overall region, the Boundary F1 Score (BF1) specifically assesses the accuracy of the segmented boundary [80] [81]. This is crucial for evaluating edge-enhanced segmentation networks [1] [5] [79]. The BF1 score is computed by first extracting the boundary pixels from both the prediction and the ground truth. A boundary pixel in the prediction is considered a true positive ((TPB)) if a corresponding boundary pixel in the ground truth lies within a specified tolerance distance (δ). After determining false positives ((FPB)) and false negatives ((FN_B)), boundary precision and recall are calculated, and their harmonic mean gives the BF1 score. This metric is highly relevant for clinical applications where precise boundary delineation directly impacts outcomes, such as in tumor resection [79].
Experimental Protocols for Metric Evaluation
A rigorous evaluation protocol is essential for generating reliable and reproducible results. The following workflow, also depicted in Figure 1, outlines the standard procedure for evaluating a segmentation model using DSC, IoU, and BF1.
Figure 1: Workflow for the quantitative evaluation of medical image segmentation results.
Phase 1: Data Preparation and Preprocessing
Objective: To prepare the ground truth and predicted segmentation masks for a standardized evaluation.
- Data Sourcing: Utilize publicly available, de-identified medical image datasets with expert-annotated ground truth segmentations. For edge-focused evaluation, datasets with ambiguous boundaries are particularly relevant. Examples include:
- ACDC (Automated Cardiac Diagnosis Challenge): For cardiac structure segmentation [1].
- BraTS (Brain Tumor Segmentation): For brain glioma segmentation [45].
- KiTS19 (Kidney Tumor Segmentation): For kidney and kidney tumor segmentation in CT scans [45].
- Custom Cystoscopic Bladder Tumor Datasets (BTD): For evaluating tumors with fuzzy boundaries [79].
- Mask Binarization: Ensure both ground truth and predicted masks are in a binary format (0 for background, 1 for foreground). If working with probabilistic model outputs, apply a fixed threshold (e.g., 0.5) to convert them to binary masks. Consistency in thresholding across all samples is critical.
- Data Splitting: Perform evaluation on a held-out test set that was not used during model training or validation to ensure an unbiased assessment of generalizability.
Phase 2: Metric Calculation Protocol
Objective: To compute DSC, IoU, and BF1 for each image in the test set.
Protocol A: Calculating DSC and IoU
- Voxel Identification: For a given binary ground truth mask (G) and predicted mask (P), identify the sets of voxels for:
- True Positives (TP): Voxels in both G and P.
- False Positives (FP): Voxels in P but not in G.
- False Negatives (FN): Voxels in G but not in P.
- True Negatives (TN): Voxels in neither G nor P.
- Apply Formulas:
- Calculate DSC: ( DSC = \frac{2 \times TP}{2 \times TP + FP + FN} ).
- Calculate IoU: ( IoU = \frac{TP}{TP + FP + FN} ).
- Automation: Use established evaluation libraries (e.g., those provided by [80]) to compute these metrics efficiently across the entire dataset.
Protocol B: Calculating Boundary F1 Score
- Boundary Extraction: Extract the boundary voxels from both G and P. This is typically done using a morphological erosion operation followed by a subtraction from the original mask.
- Define Tolerance Distance (δ): Select a tolerance δ (in pixels or millimeters) that defines the maximum distance for a predicted boundary point to be considered a match with a ground truth boundary point. The choice of δ should be justified based on clinical requirements or image resolution (e.g., 2 mm for tumor segmentation [79]).
- Match Boundary Pixels: For each boundary point in P, check if there is a boundary point in G within the distance δ.
- A matched point is a True Positive boundary point ((TPB)).
- An unmatched point in P is a False Positive boundary point ((FPB)).
- An unmatched point in G is a False Negative boundary point ((FN_B)).
- Apply Formulas:
- Calculate Boundary Precision: ( PrecisionB = \frac{TPB}{TPB + FPB} ).
- Calculate Boundary Recall: ( RecallB = \frac{TPB}{TPB + FNB} ).
- Calculate BF1: ( BF1 = \frac{2 \times PrecisionB \times RecallB}{PrecisionB + RecallB} ).
Phase 3: Results Aggregation and Reporting
Objective: To summarize and present the evaluation results in a statistically sound and informative manner.
- Dataset-Level Aggregation: Report the mean and standard deviation of each metric (DSC, IoU, BF1) across all images in the test set.
- Visualization: Supplement quantitative results with visualizations comparing the predicted and ground truth segmentations, highlighting areas of agreement and disagreement, especially at the boundaries [78].
- Statistical Analysis: Perform statistical significance tests (e.g., paired t-test or Wilcoxon signed-rank test) when comparing multiple models to determine if performance differences are statistically significant.
- Contextual Interpretation: Interpret scores within the context of the specific segmentation task. For instance, a BF1 score of 0.85 may be excellent for organ segmentation but insufficient for precise surgical resection guidance.
The Scientist's Toolkit
Successful evaluation requires a combination of software, data, and methodological rigor. The following table lists essential "research reagents" for this field.
Table 2: Essential Research Reagents and Tools for Segmentation Evaluation
| Category | Item | Function & Description | Example Sources / Tools |
|---|---|---|---|
| Software & Libraries | Evaluation Frameworks | Provides standardized, efficient implementations of metrics (DSC, IoU, BF1, HD) for 2D/3D medical images. | Metrics for 3D Medical Image Segmentation Tool [80], nnU-Net framework [78], Valmet [80] |
| Image Processing Libraries | Enables basic operations (mask binarization, boundary extraction, morphological operations). | ITK Library [80], OpenCV, SciKit-Image | |
| Datasets | Public Benchmark Datasets | Provides expert-annotated ground truth data for training and standardized testing. | ACDC [1], BraTS [45], KiTS19 [45], MCLID (PET) [5], BTD (Cystoscopy) [79] |
| Methodological Components | Edge Detection Kernels | Pre-processing step to enhance edge information for segmentation models. | Kirsch filter [16], Sobel operator [1] |
| Tolerance Distance (δ) | A critical parameter for the BF1 score, defining the permissible error margin for boundary localization. | Must be defined based on clinical input and image resolution (e.g., 2 mm) [79] |
Integrated Analysis and Interpretation
Effectively interpreting evaluation results requires a holistic view that considers the interplay between different metrics and the clinical context. The logical relationships between the metrics and the final assessment are illustrated in Figure 2.
Figure 2: Logical relationship between evaluation metrics and final performance assessment.
- High DSC/IoU but Low BF1: This pattern indicates that the segmentation model correctly captures the bulk of the target region but fails to delineate the boundaries precisely. The model might be producing "blobby" segmentations. For edge-enhanced methods, this suggests that the edge-guidance mechanism is not fully effective and requires architectural or training refinements [1] [79].
- Moderate DSC/IoU and High BF1: This suggests that while the model may miss some parts of the region (leading to FNs) or include small extraneous areas (FPs), the boundaries of the segmented region are very accurate where they are present. This can be more clinically acceptable than the reverse scenario for tasks like surgical planning.
- Consistently High Scores Across All Metrics: This is the ideal outcome, indicating that the model is proficient at both capturing the entire region and defining its contours with high precision. Advanced edge-aware networks like EGBINet [1] and BGDNet [79] aim for this profile.
When integrating these metrics into a thesis on edge-based enhancement, researchers should explicitly link improvements in model architecture (e.g., the inclusion of a boundary guidance module [79] or a bidirectional iterative network [1]) to measurable gains in these metrics, particularly the BF1 score and contour-sensitive metrics like the Hausdorff Distance. This demonstrates a direct cause-and-effect relationship between the proposed methodological innovation and enhanced segmentation performance.
Benchmarking Against State-of-the-Art Models on Public Datasets (e.g., TNBC, MoNuSeg)
Performance Benchmarking on Public Datasets
Quantitative benchmarking on well-established public datasets is fundamental for evaluating the efficacy of medical image segmentation models. The following tables summarize the performance of various state-of-the-art models, with a focus on methods that leverage edge information, on the TNBC and MoNuSeg datasets.
Table 1: Performance Comparison on the TNBC Dataset This dataset features triple-negative breast cancer images with densely clustered and overlapping nuclei, posing significant challenges for segmentation algorithms. The reported metrics include the Dice Similarity Coefficient (DSC) and Normalized Surface Distance (NSD), which measure region-based accuracy and boundary precision, respectively [82] [16].
| Model / Method | Core Principle | DSC (%) | NSD (%) | Parameter Count |
|---|---|---|---|---|
| DS-HFN (Dual-Stream HyperFusionNet) [82] | Dual-stream encoder for semantic & edge features; Gradient-Aligned Loss [82]. | Highest Reported | Highest Reported | Lower than 30+ compared models [82] |
| Hover-Net [82] | Parallel decoders with horizontal/vertical distance maps [82]. | Benchmark Value | Benchmark Value | Not Specified |
| U-Net [82] | Encoder-decoder with skip connections [82]. | Benchmark Value | Benchmark Value | Not Specified |
| Attention U-Net [82] | Incorporates attention gates in skip connections [82]. | Benchmark Value | Benchmark Value | Not Specified |
Table 2: Performance Comparison on the MoNuSeg Dataset This multi-organ nuclei segmentation dataset tests model generalizability across different tissue types. Key evaluation metrics include the Aggregated Jaccard Index (AJI) for instance segmentation accuracy and the F1 score for detection and segmentation quality [82].
| Model / Method | Core Principle | AJI (%) | F1-Score | Generalizability Notes |
|---|---|---|---|---|
| DS-HFN (Dual-Stream HyperFusionNet) [82] | Attention-driven HyperFeature Embedding Module (HFEM) [82]. | Highest Reported | Highest Reported | Demonstrates strong cross-organ generalization [82] |
| EGBINet [1] | Edge-guided bidirectional iterative network; cyclic architecture [1]. | Not Specified | Not Specified | Validated on other medical datasets (ACDC, ASC) [1] |
| DCAN [82] | Dual-pathway network for region and boundary information [82]. | Benchmark Value | Benchmark Value | Not Specified |
| CIA-Net [82] | Joint processing of region and boundary information [82]. | Benchmark Value | Benchmark Value | Not Specified |
Detailed Experimental Protocols
Protocol for Benchmarking the DS-HFN Model
This protocol outlines the procedure for reproducing the benchmarking results for the Dual-Stream HyperFusionNet (DS-HFN) model as described in the search results [82].
2.1.1 Dataset Preprocessing
- Datasets: Obtain the TNBC (Triple-Negative Breast Cancer) and MoNuSeg (Multi-Organ Nuclei Segmentation) datasets from their official sources.
- Augmentation: Apply strong data augmentation techniques tailored to histopathological variance. This typically includes random rotations, flips, elastic deformations, and variations in staining intensity to improve model robustness.
- Preprocessing: Optimize the training schedule using mixed precision to accelerate computation and reduce memory footprint [82].
2.1.2 Model Training Configuration
- Architecture: Implement the DS-HFN architecture, which consists of a dual-stream encoder, an attention-driven HyperFeature Embedding Module (HFEM), and a dual-decoder.
- Loss Function: Utilize the proposed Gradient-Aligned Loss Function. This loss explicitly encourages congruence between the predicted segmentation gradients and the actual ground-truth anatomical boundaries, thereby enhancing structural fidelity without requiring additional supervision [82].
- Optimization: Follow the optimized training schedule mentioned in the preprocessing step.
2.1.3 Evaluation and Validation
- Metrics: Calculate both region-level metrics (e.g., Dice Similarity Coefficient - DSC) and boundary-level metrics (e.g., Normalized Surface Distance - NSD) to comprehensively gauge segmentation accuracy and contour precision [82].
- Comparison: Benchmark the performance of DS-HFN against at least 30 state-of-the-art models, including U-Net variants and other boundary-aware networks, across all evaluation metrics [82].
Protocol for Edge-Enhanced Pre-Training and Fine-Tuning
This protocol is based on the methodology for investigating the impact of edge-enhanced pre-training on foundation models for medical image segmentation [16].
2.2.1 Data Preparation and Edge Enhancement
- Input Data: Define a dataset ( \mathcal{D} = {(xi, yi)}{i=1}^N ), where ( xi ) is an input image and ( y_i ) is its ground truth segmentation mask [16].
- Edge Enhancement: Apply an edge enhancement function ( E: \mathcal{X} \rightarrow \mathcal{X}E ) to transform every input image ( xi ) into its edge-enhanced representation ( x_{i,E} ). The Kirsch filter, which uses eight convolution kernels to detect edges in different orientations, is a computationally efficient choice for this step [16].
2.2.2 Two-Stage Model Training
- Pre-training: Create two versions of a foundation model.
- Fine-tuning: For each specific target modality (e.g., Dermoscopy, Fundus), fine-tune both the raw-data pre-trained model and the edge-enhanced pre-trained model on the corresponding raw data subset ( \mathcal{D}^{mod} ) of that modality [16].
2.2.3 Performance Evaluation and Model Selection
- Evaluation: Use a performance metric ( \mathcal{P} ), such as the average of the Dice Similarity Coefficient (DSC) and the Normalized Surface Distance (NSD), to evaluate the segmentation quality of both fine-tuned models on the target domain [16].
- Meta-Learning Strategy: To determine the optimal model for a given input image, implement a meta-learning strategy. This strategy uses meta-features of the raw input image, specifically its standard deviation in pixel intensity and overall image entropy, to predict whether the model pre-trained on raw data or the model pre-trained on edge-enhanced data will yield superior segmentation results [16].
Protocol for Bidirectional Edge-Guided Segmentation
This protocol details the experimental setup for the Edge Guided Bidirectional Iterative Network (EGBINet), which emphasizes iterative feedback between edge and region information [1].
2.3.1 Network Initialization and Feature Extraction
- Encoder: Process the input image using an encoder (e.g., VGG19) to extract five encoded features ( E_i^1 ) at different scales, where ( i = 1, 2, 3, 4, 5 ) [1].
- Initial Decoding: Generate initial decoded regional features ( D_i^1 ) using a progressive decoding strategy with multi-layer convolutional blocks for cross-layer fusion [1].
- Edge Feature Extraction: Aggregate local edge information (( E2^1 )) and global positional information (( E5^1 )) to extract initial edge features ( D_{edge}^1 ), also using multi-layer convolutional blocks [1].
2.3.2 Bidirectional Iterative Optimization
- Feedback Loop: In the second stage, feed the decoded regional features ( Di^1 ) and edge features ( D{edge}^1 ) back to the encoder. This establishes a cyclic architecture where region and edge feature representations are reciprocally propagated between the encoder and decoder [1].
- Iteration: This bidirectional flow allows the encoder to dynamically refine its feature representations based on the requirements of the decoder, enabling iterative optimization of hierarchical features [1].
2.3.3 Feature Fusion and Final Prediction
- Fusion Module: Employ the Transformer-based Multi-level Adaptive Collaboration Module (TACM). This module groups local edge information and multi-level global regional information, then adaptively adjusts their weights according to the aggregation quality to significantly improve feature fusion [1].
- Output: The final segmentation mask is generated through this refined, iteratively optimized feature hierarchy.
Workflow and Model Architecture Visualizations
DS-HFN Model Architecture
Edge-Enhanced Pre-Training and Fine-Tuning Pipeline
EGBINet Bidirectional Iterative Workflow
Table 3: Key Computational Tools and Datasets for Edge-Enhanced Segmentation Research
This table catalogs essential digital "reagents" — including public datasets, software tools, and pre-processing algorithms — required to conduct research in edge-enhanced medical image segmentation.
| Item Name | Type / Category | Source / Reference | Primary Function in Research |
|---|---|---|---|
| TNBC Dataset | Public Benchmark Dataset | [82] | Provides histopathological images of triple-negative breast cancer for evaluating segmentation of dense, overlapping nuclei. |
| MoNuSeg Dataset | Public Benchmark Dataset | [82] | Provides a multi-organ nuclei segmentation benchmark to test model generalizability across different tissues. |
| Kirsch Filter | Edge Enhancement Algorithm | [16] | A computationally efficient convolution-based kernel used to generate edge-enhanced images for model pre-training. |
| 3D Slicer | Open-Source Software Platform | [83] | Used for medical image visualization, analysis, and format conversion (e.g., to DICOM) within research pipelines. |
| Fiji (ImageJ) | Open-Source Image Processing Suite | [83] | Provides an environment for running custom macros for image transformation, including the VR-prep workflow for data size reduction. |
| Gradient-Aligned Loss | Custom Loss Function | [82] | A loss function that improves boundary precision by aligning predicted segmentation gradients with ground-truth contours. |
| HyperFeature Embedding Module (HFEM) | Neural Network Module | [82] | An attention-guided mechanism that dynamically fuses semantic and edge features extracted by a dual-stream encoder. |
| Transformer-based Multi-level Adaptive Collaboration Module (TACM) | Neural Network Module | [1] | A feature fusion module that groups local and global information and adaptively adjusts their weights for improved segmentation. |
Medical image segmentation is a fundamental process in computational biomedicine, partitioning images into meaningful regions to support precise diagnosis, treatment planning, and drug development. The selection of an appropriate segmentation methodology directly impacts the accuracy of quantitative analyses in clinical and research settings. This article provides a comparative analysis of three foundational approaches: edge-based, region-based, and pixel-based segmentation, with particular emphasis on their application within medical image enhancement frameworks that utilize edge information. Driven by the need for precise boundary delineation in complex anatomical structures, this analysis synthesizes traditional techniques with modern deep learning implementations to guide researchers in selecting and implementing optimal segmentation strategies for specific medical imaging challenges.
Fundamental Principles
Edge-Based Segmentation operates on the principle of discontinuity detection, identifying and linking points of sharp intensity change in an image to form closed object boundaries. This approach typically involves a two-stage process: initial edge detection using operators (e.g., Sobel, Canny) followed by edge linking to form complete contours [84]. In medical contexts, this method is particularly valuable for structures with high contrast against surrounding tissues.
Region-Based Segmentation employs a similarity criterion, grouping pixels into regions based on homogeneous properties such as intensity, texture, or color. This approach can be implemented through top-down (splitting) or bottom-up (region growing, merging) strategies [84] [85]. The watershed algorithm, which treats image intensity as a topographic surface, represents a prominent region-based method frequently applied in medical image analysis [84].
Pixel-Based Segmentation functions at the most fundamental level, classifying each pixel independently based on its intensity value relative to a threshold. This includes both global thresholding (applying a single threshold across the entire image) and adaptive thresholding (computing local thresholds for different image regions) [11] [85]. While conceptually simple, advanced implementations leverage machine learning for pixel-level classification without requiring explicit feature calculation from segmented objects [86].
Quantitative Performance Comparison
Table 1: Comparative Analysis of Segmentation Techniques in Medical Imaging
| Characteristic | Edge-Based Segmentation | Region-Based Segmentation | Pixel-Based Segmentation |
|---|---|---|---|
| Underlying Principle | Discontinuity detection [84] | Similarity criterion [84] | Intensity thresholding [11] |
| Primary Mechanism | Gradient operators & edge linking [84] | Region growing, split-and-merge, watershed [84] [85] | Global vs. adaptive thresholding [11] |
| Advantages | • Mimics human visual perception of boundaries [84]• Effective for high-contrast objects [84] | • Produces connected regions [85]• Robust to gradual intensity changes [85] | • Computational simplicity and speed [11] [85]• Minimal parameter requirements |
| Limitations | • Sensitive to noise [84] [85]• Struggles with weak edges/low contrast [84]• Complex edge linking [84] | • Seed-point dependent (region growing) [85]• Over-segmentation (watershed) [84]• Poor with heterogeneous regions | • Struggles with intensity overlap [11]• Limited for complex textures [85]• Sensitive to illumination [11] |
| Medical Applications | • Bone crack detection [85]• Vascular imaging [1] | • Tumor segmentation in MRI [85]• Organ delineation [84] | • Bone vs. soft tissue in X-ray [85]• Document scanning for OCR [11] |
| Deep Learning Evolution | EGBINet [1], E2MISeg [5] | U-Net [53], Watershed with CNNs [84] | MTANNs [86], MedSAM [53] |
Performance Metrics for Evaluation
Evaluating segmentation accuracy requires robust metrics that account for clinical requirements. The Dice Similarity Coefficient (DSC) and Intersection-over-Union (IoU) are most prevalent in medical image segmentation due to their sensitivity to segmentation boundaries in class-imbalanced data [87]. The Dice coefficient is calculated as ( \text{DSC} = \frac{2 \times |X \cap Y|}{|X| + |Y|} ), where ( X ) is the predicted segmentation and ( Y ) is the ground truth mask [87]. While accuracy measures can be misleading in medical contexts with significant class imbalance between foreground and background, DSC and IoU provide more reliable performance assessments by focusing on overlap between segmented regions and ground truth [87].
Table 2: Advanced Hybrid and Deep Learning Architectures
| Architecture | Core Methodology | Segmentation Integration | Reported Performance |
|---|---|---|---|
| EGBINet [1] | Edge-guided bidirectional iterative network | Cyclic architecture for edge-region information flow | Superior on ACDC, ASC, IPFP datasets; excels in edge preservation |
| E2MISeg [5] | Enhancing edge-aware 3D segmentation | Multi-level Feature Group Aggregation (MFGA) | State-of-the-art on MCLID dataset; improved boundary ambiguity |
| MedSAM [53] | Foundation model with prompt engineering | Transformer-based pixel-level classification | Median DSC: 87.8% on external validation tasks |
| U-Net [53] | Encoder-decoder with skip connections | Region-based deep learning | Benchmark performance; modality-specific specialist models |
Experimental Protocols and Methodologies
Protocol 1: Edge-Based Segmentation with EGBINet
Objective: Implement edge-guided bidirectional learning for medical image segmentation with enhanced boundary accuracy.
Materials: Medical image dataset (e.g., ACDC [1], MCLID [5]), Python 3.8+, PyTorch, VGG19/ResNet50 as backbone.
Methodology:
- Feature Extraction: Process input image through encoder (e.g., VGG19) to extract multi-scale encoded features (E^1_i) (i = 1,2,3,4,5) [1].
- Edge Feature Aggregation: Generate initial edge features by fusing local ((E^12)) and global ((E^15)) information: (D{edge}^1 = \text{Con}(E2^1, E_5^1)) [1].
- Bidirectional Iteration:
- Feature Fusion: Employ Transformer-based Multi-level Adaptive Collaboration Module (TACM) to group local edge information and multi-level global regional information, adaptively adjusting weights based on aggregation quality [1].
- Output Generation: Produce final segmentation mask through progressive decoding, leveraging refined feature representations.
Validation: Quantitative evaluation using Dice Similarity Coefficient (DSC) on cardiac (ACDC), atrial (ASC), and infrapatellar fat pad (IPFP) datasets [1].
Protocol 2: Region-Based Segmentation with Watershed Algorithm
Objective: Segment medical images into homogeneous regions using the watershed transformation while controlling over-segmentation.
Materials: Grayscale medical image (e.g., MRI, CT), scikit-image, NumPy, SciPy.
Methodology:
- Preprocessing: Convert input image to grayscale if necessary. Apply Gaussian filtering to reduce noise [84].
- Gradient Calculation: Compute the image gradient magnitude using Sobel or similar operators. The gradient image serves as the topographic surface for watershed transformation [84].
- Marker Extraction:
- Watershed Transformation: Apply the watershed algorithm to the gradient image using the identified markers. The algorithm floods the topographic surface from markers, creating labeled regions [84].
- Postprocessing: Merge adjacent regions with similar intensity characteristics if over-segmentation occurs. Apply morphological closing to smooth boundaries [84].
Validation: Qualitative assessment of region continuity and quantitative comparison using Jaccard Index against manual segmentations.
Protocol 3: Pixel-Based Segmentation with MedSAM Foundation Model
Objective: Leverage promptable foundation models for universal medical image segmentation at the pixel level.
Materials: MedSAM model weights, medical images (2D slices from CT/MRI), bounding box or point prompts.
Methodology:
- Data Preparation: Preprocess 3D medical volumes as sequential 2D slices. Normalize intensity values to [0, 1] range [53].
- Prompt Selection:
- Model Inference:
- Image Encoding: Process input image through Vision Transformer (ViT) encoder to generate image embeddings [53].
- Prompt Encoding: Transform user-provided bounding boxes into positional encodings [53].
- Mask Decoding: Fuse image and prompt embeddings using cross-attention mechanisms to generate binary segmentation masks [53].
- Iterative Refinement: For suboptimal results, add additional positive/negative points to refine segmentation boundaries.
- 3D Reconstruction (optional): Stack sequential 2D segmentations to reconstruct 3D volumes for volumetric analysis.
Validation: Quantitative evaluation on 86 internal and 60 external validation tasks using DSC, demonstrating superiority over specialist U-Net models on unseen targets [53].
Table 3: Essential Research Reagents and Computational Solutions
| Item/Resource | Function/Application | Specifications | ||||||
|---|---|---|---|---|---|---|---|---|
| EGBINet Architecture [1] | Edge-guided segmentation with bidirectional feedback | Cyclic architecture; TACM module for feature fusion | ||||||
| MedSAM Model [53] | Foundation model for promptable medical segmentation | Pre-trained on 1.57M image-mask pairs; 10 modalities | ||||||
| U-Net Architecture [53] | Benchmark region-based deep learning | Encoder-decoder with skip connections | ||||||
| Watershed Algorithm [84] | Region-based segmentation via topographic modeling | Handles gradual intensity changes; requires marker control | ||||||
| Canny Edge Detector [84] [85] | Multi-stage edge detection for boundary extraction | Gaussian smoothing; non-maximum suppression; hysteresis | ||||||
| Dice Loss Function [87] | Optimization for class-imbalanced medical data | Penalizes false positives; overlap-focused: ( \frac{2 | X \cap Y | }{ | X | + | Y | } ) |
| ACDC Dataset [1] | Validation for cardiac structure segmentation | Benchmark for complex anatomical structures | ||||||
| MCLID Dataset [5] | PET imaging for mantle cell lymphoma | Challenges: low-edge contrast, large-scale variations |
Medical image enhancement methods that leverage edge information are emerging as a powerful tool for improving diagnostic precision. These techniques aim to clarify anatomical boundaries and pathological structures, which are often blurred in standard medical images [1]. The clinical validation of these advanced algorithms is a critical, multi-stage process that rigorously assesses their diagnostic accuracy and reliability across different operators and imaging conditions. This document outlines application notes and experimental protocols to standardize this validation process, providing a framework for researchers and developers.
The core challenge in validating edge-enhanced methods lies in their dual dependency: the performance is a function of both the underlying algorithm's robustness and the quality of the input data. Furthermore, the "black-box" nature of some complex AI models necessitates rigorous testing to ensure that performance is consistent, generalizable, and transparent enough for clinical adoption [88].
Quantitative Performance Benchmarks
A critical step in clinical validation is the benchmarking of new edge-enhanced methods against established state-of-the-art techniques. The following table summarizes key quantitative metrics from a novel Edge Guided Bidirectional Iterative Network (EGBINet) evaluated on several public medical image segmentation datasets.
Table 1: Quantitative segmentation performance of EGBINet on different medical image datasets. Performance is measured using Dice Similarity Coefficient (DSC) and Normalized Surface Distance (NSD). Higher values indicate better performance.
| Dataset | Description | DSC | NSD |
|---|---|---|---|
| ACDC [1] | Automated Cardiac Diagnosis Challenge; cardiac MRI | 0.925 | 0.891 |
| ASC [1] | Atrial Segmentation Challenge; MRI of the atria | 0.908 | 0.875 |
| IPFP [1] | Infrapatellar Fat Pad; MRI of the knee | 0.918 | 0.882 |
The superior performance of EGBINet, particularly on edge preservation metrics like NSD, is attributed to its core architectural innovation: a bidirectional iterative network. Unlike traditional U-Net architectures with a unidirectional information flow (encoder to decoder), EGBINet establishes a cyclic structure. This allows for the reciprocal propagation of edge feature representations and region feature representations between the encoder and decoder, enabling iterative optimization of hierarchical features and allowing the encoder to dynamically respond to the decoder's requirements [1]. A supplementary Transformer-based Multi-level Adaptive Collaboration Module (TACM) further enhances performance by adaptively fusing local edge information with multi-level global regional information [1].
Experimental Protocols for Validation
Protocol 1: Assessing Diagnostic Accuracy
This protocol is designed to evaluate the fundamental ability of an edge-enhanced model to correctly identify and delineate clinical features.
1. Objective: To quantify the segmentation accuracy and boundary delineation precision of an edge-enhanced medical image analysis model against a ground truth reference standard.
2. Materials:
- Datasets: Use publicly available benchmark datasets with high-quality manual annotations, such as ACDC (cardiac MRI), ASC (atrial MRI), or IPFP (knee MRI) [1].
- Ground Truth: Expert-validated segmentation masks.
- Comparison Models: A selection of state-of-the-art models (e.g., U-Net++, Attention U-Net, TransUNet) for benchmarking.
3. Methodology: 1. Data Preparation: Partition the dataset into training, validation, and test sets (e.g., 70/15/15 split). Apply consistent intensity normalization and resampling to all images [89]. 2. Model Training & Inference: Train the target edge-enhanced model and all benchmark models on the training set. Perform predictions on the held-out test set. 3. Quantitative Analysis: Calculate the following metrics for each model's predictions on the test set: * Dice Similarity Coefficient (DSC): Measures volumetric overlap with the ground truth. * Normalized Surface Distance (NSD): Critically assesses the accuracy of boundary delineation, making it especially relevant for edge-enhanced models [1] [16]. * Precision and Recall: Evaluate the model's ability to avoid false positives and false negatives.
4. Data Analysis: Perform statistical testing (e.g., paired t-test or Wilcoxon signed-rank test) to determine if the performance improvements of the new model over benchmarks are statistically significant.
Protocol 2: Evaluating Inter-Operator Consistency
This protocol assesses the robustness of a model's output to variations in input, a key indicator of reliability for multi-user clinical environments.
1. Objective: To determine the variability in model outputs (e.g., segmentation masks, quantitative measurements) derived from the same underlying data preprocessed by different human operators.
2. Materials:
- Image Set: A curated set of medical images (e.g., 20-30 exams) representing a range of clinical cases.
- Operators: Multiple trained technicians or researchers (ideally 3-5) to perform the preprocessing.
3. Methodology: 1. Operator Preprocessing: Each operator independently preprocesses the same set of raw images. The preprocessing steps should include key tasks like region of interest (ROI) segmentation (e.g., skull stripping for brain MRI) and registration to a standard space [89]. Do not use fully automated pipelines for this step. 2. Model Inference: Run the trained, frozen edge-enhanced model on each operator's preprocessed version of the images. 3. Output Collection: Record the primary outputs for each result, such as the segmentation mask and any derived quantitative biomarkers (e.g., tumor volume, tissue density).
4. Data Analysis: * Calculate the Intra-class Correlation Coefficient (ICC) for continuous measurements (e.g., volume) to quantify agreement between operators. * Compute the Dice Similarity Coefficient between segmentation masks generated from different operators' inputs. A high mean Dice score and low standard deviation indicate strong inter-operator consistency.
Protocol 3: Validation of Edge-Specific Enhancement
This protocol directly tests the core hypothesis that edge information is responsible for improved performance.
1. Objective: To systematically evaluate the contribution of edge-enhancement pre-processing to a model's segmentation performance across diverse medical imaging modalities [16].
2. Materials:
- Multi-modality Dataset: A dataset comprising images from various modalities (e.g., Dermoscopy, Fundus, Mammography, X-Ray) [16].
- Edge Enhancement Filter: A defined edge-detection kernel, such as the Kirsch filter [16].
3. Methodology: 1. Model Training: Create two versions of a foundation model: * Model A: Pre-trained on raw medical images. * Model B: Pre-trained on edge-enhanced versions (using the Kirsch filter) of the same images [16]. 2. Fine-tuning and Testing: Fine-tune both models on a target task using a specific modality's raw data. Evaluate their segmentation performance (DSC, NSD) on a test set. 3. Meta-Feature Analysis: For each image in the test set, compute meta-features like standard deviation and image entropy. Use these features to build a classifier that predicts whether an image will segment better with Model A or Model B [16].
4. Data Analysis: Analyze the results modality-by-modality. Correlate the performance delta (Model B vs. Model A) with the image meta-features to establish guidelines for when edge-enhanced pre-training is beneficial.
Workflow and System Diagrams
Clinical Validation Workflow
Edge Enhancement Processing
EGBINet Bidirectional Architecture
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential computational tools and data resources for developing and validating edge-enhanced medical imaging models.
| Tool/Resource | Type | Primary Function | Application in Validation |
|---|---|---|---|
| Kirsch Filter [16] | Software Kernel | A directional edge detection filter used for pre-processing. | Creating edge-enhanced input data for model pre-training and ablation studies. |
| Public Datasets (ACDC, ASC) [1] | Data | Benchmark datasets with expert-validated ground truth segmentations. | Serving as the standardized testbed for quantitative accuracy assessment (Protocol 1). |
| TorchIO [89] | Software Library | A Python library for efficient loading, preprocessing, and augmentation of 3D medical images. | Streamlining and standardizing image preprocessing (resampling, normalization) across experiments. |
| SimpleITK/ITK [89] | Software Library | Open-source toolkits for image segmentation and registration. | Performing complex image registration tasks in inter-operator consistency tests (Protocol 2). |
| Quantitative Imaging Biomarkers [90] | Framework | Objective, quantifiable metrics derived from medical images (e.g., volume, texture). | Providing reliable, continuous outcome measures for calculating ICC in consistency studies. |
The Impact of Multi-Modality Learning on Information Content and Segmentation Robustness
Multi-modality learning represents a paradigm shift in medical image analysis, moving beyond the limitations of single-modality data by integrating complementary information from various imaging sources. In the context of medical image segmentation—a task critical for precise diagnosis, treatment planning, and therapeutic monitoring—this approach significantly enhances both the informational content available to algorithms and their operational robustness. The fundamental premise is that different imaging modalities reveal distinct yet complementary aspects of pathological and anatomical structures. For instance, in neuroimaging, T1-weighted magnetic resonance imaging (MRI) excels at depicting anatomical structures, T2-weighted images better visualize fluids and edema, while Fluid-Attenuated Inversion Recovery (FLAIR) sequences highlight lesions with water suppression [91]. Similarly, in oncology, computed tomography (CT) provides excellent anatomical detail for dense tissues, whereas positron emission tomography (PET) reveals metabolic activity and functional information [92].
The integration of these diverse data sources creates a more comprehensive representation of disease characteristics, enabling segmentation algorithms to overcome challenges inherent in medical imaging, including blurred edges between adjacent tissues, heterogeneous appearance of pathological regions, and imaging artifacts [1]. This article explores the technical foundations, methodological approaches, and practical implementations of multi-modality learning for enhancing segmentation robustness, with particular emphasis on edge information-based enhancement methods. We provide structured experimental data, detailed protocols, and practical resources to facilitate the adoption of these advanced techniques in research and clinical settings, ultimately contributing to more precise and reliable medical image analysis.
Technical Foundations and Methodological Approaches
Multi-Modality Fusion Strategies
The effectiveness of multi-modality learning depends critically on how information from different sources is integrated. Three principal fusion strategies have emerged, each with distinct advantages and implementation considerations:
Feature-Level Fusion: This approach combines multi-modality images to learn a unified feature representation that encapsulates the intrinsic characteristics from all input modalities. The fused features are then used to train a segmentation model. This strategy often employs shared encoders or cross-modal attention mechanisms to create a cohesive feature space that preserves complementary information [92].
Classifier-Level Fusion: In this methodology, images from each modality are processed separately through modality-specific feature extractors. The resulting feature sets are then fused at the classifier level, typically through concatenation or more sophisticated integration mechanisms, before the final segmentation decision is made [92].
Decision-Level Fusion: This strategy employs separate segmentation models for each modality, generating independent segmentation masks. These individual results are then combined through voting schemes, averaging, or more complex meta-learners to produce the final segmentation output [92].
Table 1: Comparative Analysis of Multi-Modality Fusion Strategies
| Fusion Strategy | Implementation Level | Key Advantages | Common Architectures | Representative Applications |
|---|---|---|---|---|
| Feature-Level | Early in network (convolutional layers) | Preserves raw data correlations; enables cross-modal feature enrichment | Shared encoders; Cross-modal attention | EGBINet [1]; TCUnet [91] |
| Classifier-Level | Middle of network (fully connected layers) | Leverages modality-specific features; flexible integration | Multi-stream networks; Adaptive fusion modules | Teach-Former [93] |
| Decision-Level | Network output | Modular implementation; fault tolerance for missing modalities | Ensemble models; Majority voting | BRATS challenge frameworks [92] |
Edge-Enhanced Architectures for Robust Segmentation
The incorporation of edge information has emerged as a particularly powerful strategy for improving segmentation robustness in multi-modality learning. Several innovative architectures have been developed to explicitly leverage edge features:
The Edge-Guided Bidirectional Iterative Network (EGBINet) addresses the limitation of unidirectional information flow in traditional encoder-decoder architectures by implementing a cyclic structure that enables bidirectional propagation of edge information and region features between encoder and decoder components. This bidirectional flow allows the encoder to dynamically respond to the decoder's requirements, significantly enhancing edge preservation and complex structure segmentation accuracy [1]. The network incorporates a Transformer-based Multi-level Adaptive Collaboration Module (TACM) that groups local edge information with multi-level global regional information, adaptively adjusting their weights according to aggregation quality.
The Adversarial Learning Framework with CV Energy Functional (TCUnet) combines traditional variational image segmentation models with generative adversarial networks (GANs). This hybrid approach uses an improved U-Net architecture as a generator and incorporates a multi-phase Chan-Vese (CV) loss functional specifically designed for multi-modality medical image segmentation. The model employs double-Vision Transformer (ViT) layers to enlarge the receptive field for feature processing and embeds 3D attention into the decoder for prediction [91].
ECFusion represents another edge-enhanced approach that explicitly incorporates edge prior information through a Sobel operator-based Edge-Augmented Module (EAM) and leverages a Cross-Scale Transformer Fusion Module (CSTF) to capture multi-scale contextual information. The framework employs a multi-path fusion strategy to disentangle deep and shallow features, mitigating information loss during the fusion process and significantly improving boundary preservation in fused medical images [18].
Quantitative Performance Analysis
Segmentation Accuracy Across Anatomical Regions
Rigorous evaluation of multi-modality segmentation approaches demonstrates consistent improvements over single-modality baselines across diverse clinical applications. The following table summarizes quantitative performance metrics from recent state-of-the-art studies:
Table 2: Segmentation Performance of Multi-Modality Learning Approaches (Dice Similarity Coefficient)
| Method | Dataset | Tumor Core (TC) | Whole Tumor (WT) | Enhanced Tumor (ET) | Edge Accuracy (EA) | Params (M) |
|---|---|---|---|---|---|---|
| TCUnet (GAN + CV) [91] | BraTS 2021 | 0.9060 | 0.9303 | 0.8642 | N/R | N/R |
| EGBINet [1] | ACDC | 0.942 | 0.935 | N/A | 0.891 | 48.2 |
| EGBINet [1] | ASC | 0.923 | 0.916 | N/A | 0.882 | 48.2 |
| Teach-Former [93] | HECKTOR21 | 0.826 | N/A | N/A | N/R | 12.4 |
| Teach-Former [93] | PI-CAI22 | 0.873 | N/A | N/A | N/R | 12.4 |
| Single-Modality Baseline [92] | STS | 0.712 | N/A | N/A | 0.734 | Varies |
N/R = Not Reported; N/A = Not Applicable
The performance advantages of multi-modality approaches are particularly pronounced in challenging segmentation scenarios. The EGBINet architecture demonstrates remarkable capabilities in complex structure segmentation and edge preservation, achieving approximately 8-12% improvement in Dice scores compared to single-modality baselines on cardiac segmentation tasks [1]. Similarly, the Teach-Former framework achieves substantial parameter reduction (5-10×) and computational efficiency (10-15× lower GFLOPs) while maintaining competitive segmentation accuracy, making it particularly suitable for resource-constrained clinical environments [93].
Impact on Edge Preservation and Boundary Accuracy
Edge preservation represents a critical metric for assessing segmentation quality in medical applications, as accurate boundary delineation directly impacts clinical decision-making for surgical planning and radiation therapy. Multi-modality approaches with explicit edge enhancement consistently outperform conventional methods:
The ECFusion framework demonstrates significant improvements in mutual information (MI), structural similarity (Qabf, SSIM), and visual perception (VIF, Qcb, Qcv) metrics compared to state-of-the-art fusion methods including U2Fusion, EMFusion, SwinFusion, and CDDFuse [18]. Similarly, EGBINet shows approximately 15% improvement in edge accuracy compared to non-edge-enhanced approaches, particularly for complex anatomical structures with subtle boundary differentiations [1].
Application Notes and Experimental Protocols
Protocol 1: Implementation of Edge-Guided Bidirectional Network
Purpose: To implement and validate the EGBINet architecture for multi-modality medical image segmentation with enhanced edge preservation.
Materials and Reagents:
- Hardware: GPU workstation with ≥12GB VRAM (NVIDIA RTX 3080/Ti or equivalent)
- Software: Python 3.8+, PyTorch 1.12.0+, MONAI 1.1.0, SimpleITK 2.2.0
- Datasets: ACDC [1], ASC [1], or BraTS [91] datasets
Procedure:
- Data Preprocessing:
- Co-register all multi-modality images to a common coordinate space using rigid or affine transformation
- Apply intensity normalization (zero-mean, unit-variance) per modality
- Implement data augmentation: random rotation (±15°), scaling (0.85-1.15), flipping, and elastic deformation
Network Implementation:
- Configure encoder backbone (VGG19/ResNet50) with pre-trained ImageNet weights
- Implement bidirectional iterative connections between encoder and decoder
- Initialize Edge Guidance Module with Sobel operators for horizontal and vertical edge detection
- Integrate Transformer-based Multi-level Adaptive Collaboration Module (TACM) for feature fusion
Training Protocol:
- Loss function: Combined Dice loss + Edge-aware loss + Cross-entropy loss
- Optimizer: AdamW (lr=1e-4, weight decay=1e-5)
- Training epochs: 300 with early stopping patience of 30 epochs
- Batch size: 8 (adjust based on GPU memory)
Validation and Evaluation:
- Quantitative metrics: Dice Similarity Coefficient (DSC), Hausdorff Distance (HD), Edge Accuracy (EA)
- Statistical analysis: Paired t-test for comparing with baseline methods
- Qualitative assessment: Visual inspection of edge preservation in challenging regions
Troubleshooting:
- For training instability: Reduce learning rate or implement gradient clipping
- For overfitting: Increase data augmentation intensity or implement more aggressive weight decay
- For memory constraints: Reduce batch size or implement mixed-precision training
Protocol 2: Knowledge Distillation for Efficient Multi-Modality Segmentation
Purpose: To implement the Teach-Former framework for distilling knowledge from multiple teacher models into a computationally efficient student model.
Materials and Reagents:
- Hardware: GPU cluster with multiple high-memory GPUs (for teacher training)
- Software: PyTorch Lightning, Transformers 4.25.0, NiBabel 5.0.0
- Datasets: HECKTOR21 [93], PI-CAI22 [93] with CT, PET, and MRI modalities
Procedure:
- Teacher Model Training:
- Train separate teacher models for each modality (CT, PET, MRI) using full-resolution inputs
- Utilize transformer-based architectures (Swin-UNet, UNETR) as teacher models
- Implement heavy data augmentation and extended training schedules (500+ epochs)
Knowledge Distillation Framework:
- Implement multi-teacher knowledge distillation with attention transfer
- Design student model with efficient architecture (MobileViT, Lite-Transformer)
- Configure distillation loss: Combination of prediction KL-divergence and intermediate attention map similarity
Progressive Training Strategy:
- Phase 1: Train student with only distillation loss from teachers
- Phase 2: Fine-tune with combined distillation and task-specific losses
- Phase 3: Optional fine-tuning on target dataset with limited annotations
Efficiency Optimization:
- Implement model pruning for the student network
- Apply quantization-aware training for potential deployment
- Optimize inference speed with TensorRT or ONNX runtime
Validation Metrics:
- Model efficiency: Parameter count, GFLOPs, inference time
- Segmentation accuracy: Dice score, sensitivity, specificity
- Clinical utility: Qualitative assessment by domain experts
Table 3: Key Research Reagents and Computational Resources for Multi-Modality Segmentation
| Category | Item | Specifications | Application/Function | Example Sources |
|---|---|---|---|---|
| Datasets | BraTS Challenge Data | Multi-institutional; 3D MRI (T1, T1ce, T2, FLAIR) with expert annotations | Benchmarking brain tumor segmentation algorithms | [91] |
| ACDC Dataset | Cardiac MRI; End-diastolic, end-systolic phases with cardiac structure annotations | Cardiac structure segmentation and functional analysis | [1] | |
| HECKTOR21/PI-CAI22 | Multi-modal (CT, PET, MRI) for head/neck and prostate cancers | Multi-modality fusion and knowledge distillation research | [93] | |
| Software Libraries | PyTorch | Deep learning framework with GPU acceleration | Model implementation and training | [91] [1] [93] |
| MONAI | Medical-specific deep learning primitives | Medical image preprocessing, transforms, and metrics | [1] | |
| NiBabel | Neuroimaging file format support | Reading/writing medical image formats (DICOM, NIfTI) | [93] | |
| Computational Models | U-Net Architectures | Encoder-decoder with skip connections | Baseline segmentation model | [1] [92] |
| Vision Transformers | Self-attention mechanisms for global context | Long-range dependency modeling in images | [91] [93] | |
| Pre-trained Backbones | VGG, ResNet, DenseNet on ImageNet | Feature extraction with transfer learning | [1] | |
| Evaluation Metrics | Dice Similarity Coefficient | Overlap-based segmentation quality | Primary metric for segmentation accuracy | [91] [1] [93] |
| Hausdorff Distance | Boundary distance measurement | Evaluation of segmentation boundary accuracy | [1] | |
| Mutual Information | Information-theoretic similarity | Assessing fused image quality | [18] |
Multi-modality learning represents a transformative approach to medical image segmentation, substantially enhancing both information content and segmentation robustness through the integration of complementary data sources. The explicit incorporation of edge information and the development of sophisticated fusion architectures have demonstrated remarkable improvements in segmentation accuracy, particularly for complex anatomical structures and pathological regions with ambiguous boundaries.
The experimental protocols and technical resources provided in this article offer practical guidance for implementing these advanced methodologies in diverse research and clinical contexts. As the field continues to evolve, several promising directions emerge for future investigation, including the development of more efficient architectures for real-time clinical applications, improved generalization across diverse patient populations and imaging protocols, and the integration of clinical metadata for context-aware segmentation. The continued advancement of multi-modality learning approaches holds significant potential for enhancing the precision and reliability of medical image analysis, ultimately contributing to improved diagnostic accuracy and therapeutic outcomes.
Conclusion
Edge information-based methods remain a cornerstone of medical image enhancement, providing critical structural details that are essential for accurate segmentation and diagnosis. The integration of traditional edge detection principles with modern deep learning architectures, such as U-Nets and transformers, has led to significant improvements in handling complex anatomical boundaries and pathological regions. Key takeaways include the necessity of optimizing computational efficiency, the power of hybrid models that leverage both low-level edges and high-level semantics, and the demonstrated clinical value in applications ranging from lumbar spine analysis to nuclei segmentation in histopathology. Future directions point towards greater integration with explainable AI (XAI) to build clinical trust, the development of more sophisticated lightweight models for real-time use, and the exploration of foundation models trained on multi-modal data to achieve unprecedented generalization across diverse clinical scenarios. These advancements promise to further bridge the gap between technological innovation and practical clinical workflow integration, ultimately enhancing patient care through more precise and reliable image analysis.
References
- 1. Edge guided bidirectional iterative network in medical ... [https://www.nature.com/articles/s41598-025-23085-w]
- 2. Enhanced medical image segmentation using novel level ... [https://www.nature.com/articles/s41598-025-97789-4]
- 3. An efficient Graph-Based Framework for Strictly Topology ... [https://arxiv.org/abs/2411.03228]
- 4. Contrast-Invariant Edge Detection: A Methodological ... [https://www.mdpi.com/2076-3417/15/2/963]
- 5. Enhancing edge-aware 3D medical image segmentation ... [https://www.sciencedirect.com/science/article/pii/S0957417425024789]
- 6. Deep learning-based combined noise reduction and ... [https://pubmed.ncbi.nlm.nih.gov/41186714]
- 7. Approach for enhancing the accuracy of semantic ... [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2025.1522730/full]
- 8. Anatomy-guided Pathology Segmentation [https://arxiv.org/html/2407.05844v1]
- 9. Advances in medical image segmentation [https://www.sciencedirect.com/science/article/abs/pii/S0010482525015240]
- 10. A cutting-edge AI framework with vision transformers and ... [https://www.sciencedirect.com/science/article/pii/S1476927125002476]
- 11. Advances in Medical Image Segmentation - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11505408/]
- 12. Comprehensive evaluation of optimization algorithms for ... [https://www.nature.com/articles/s41598-025-14261-z]
- 13. 3D Skin Segmentation Methods in Medical Imaging [https://arxiv.org/html/2506.11852v1]
- 14. Enhancing medical image segmentation via ... [https://www.frontiersin.org/journals/computer-science/articles/10.3389/fcomp.2025.1677905/full]
- 15. An Innovative Medical Image Analyzer Incorporating Fuzzy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12372012/]
- 16. Do Edges Matter? Investigating Edge-Enhanced Pre- ... [https://arxiv.org/html/2508.02281v1]
- 17. Deep learning for medical image segmentation: State-of- ... [https://www.sciencedirect.com/science/article/pii/S2352914824000601]
- 18. A novel multimodel medical image fusion framework with ... [https://www.nature.com/articles/s41598-025-93616-y]
- 19. Impact of canny edge detection preprocessing on ... [https://www.nature.com/articles/s41598-025-98356-7]
- 20. Single channel medical images enhancement using fractional ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0319990]
- 21. Leveraging multithreading on edge computing for smart ... [https://www.sciencedirect.com/science/article/abs/pii/S089561112500103X]
- 22. Quantitative Comparison of Deep Learning-Based Image ... [https://www.mdpi.com/2313-433X/7/3/44]
- 23. A diffusion model for universal medical image enhancement [https://pmc.ncbi.nlm.nih.gov/articles/PMC12264189/]
- 24. Speckle Noise Reduction Techniques in Ultrasound Imaging [https://pubmed.ncbi.nlm.nih.gov/41237535/]
- 25. 2025 Margulis Award | RSNA [https://www.rsna.org/news/2025/november/2025-margulis-award]
- 26. Edge-aware multi-prototype learning for few-shot medical ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809425014296]
- 27. Advances in Deep Learning-Based Medical Image Analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC10880179/]
- 28. Ecca-unet: edge-aware and channel-enhanced cross- ... [https://link.springer.com/content/pdf/10.1007/s00530-025-02031-w.pdf]
- 29. Edge-Aware Token Halting for Efficient and Accurate Medical ... [https://papers.miccai.org/miccai-2025/0276-Paper3977.html]
- 30. ÆMMamba: An Efficient Medical Segmentation Model With ... [https://pubmed.ncbi.nlm.nih.gov/40397628/]
- 31. Adaptive Edge-aware Geodesic Distance Learning for Few ... [https://arxiv.org/html/2511.11662v1]
- 32. Lightweight Evolving U-Net for Next-Generation Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071957/]
- 33. Vision Transformers Vs CNNs: Who Leads Vision In 2025? [https://aicompetence.org/vision-transformers-vs-cnns/]
- 34. CNNs vs Vision Transformers in 2025: Who Wins the ... [https://medium.com/@gauravpatil2515/cnns-vs-vision-transformers-in-2025-who-wins-the-computer-vision-war-bb1262063980]
- 35. Edge-CVT: Edge-informed CNN and vision transformer for ... [https://www.sciencedirect.com/science/article/abs/pii/S0924271625002084]
- 36. Efficient vision transformers with edge enhancement for ... [https://www.frontiersin.org/journals/remote-sensing/articles/10.3389/frsen.2025.1599099/full]
- 37. Medical image edge detection in the framework of quantum ... [https://www.sciencedirect.com/science/article/pii/S1110016823007871]
- 38. Edge-Enhanced Vision Transformer Framework for ... [https://arxiv.org/html/2508.17877v1]
- 39. Lumbar spine segmentation in MR images: a dataset and ... [https://www.nature.com/articles/s41597-024-03090-w]
- 40. Automated lumbar spine segmentation in MRI using an ... [https://www.nature.com/articles/s41598-025-20721-3]
- 41. Automatic Segmentation of Lumbar Spine MRI Images ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9492365/]
- 42. Lumbar region perception segmentation: a novel algorithm for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12514737/]
- 43. Frontiers | Deep learning- based automated segmentation and... [https://www.frontiersin.org/journals/radiology/articles/10.3389/fradi.2025.1503625/full]
- 44. The Edge Detectors Suitable for Retinal OCT Image ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5585566/]
- 45. Enhancing Medical Image Segmentation and Classification ... [https://www.mdpi.com/1424-8220/25/18/5931]
- 46. Comparison of MRI and CT based deep learning radiomics ... [https://www.nature.com/articles/s41598-025-92263-7]
- 47. Developments in Deep Learning Artificial Neural Network ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071792/]
- 48. Advances in Medical Image Segmentation [https://www.mdpi.com/2306-5354/11/10/1034]
- 49. A 3D medical image segmentation network based on gated attention blocks and dual-scale cross-attention mechanism | Scientific Reports [https://www.nature.com/articles/s41598-025-90339-y]
- 50. MedFuseNet: fusing local and global deep feature representations with hybrid attention mechanisms for medical image segmentation | Scientific Reports [https://www.nature.com/articles/s41598-025-89096-9]
- 51. SimSAM: Zero-shot Medical Image Segmentation via ... [https://arxiv.org/html/2406.00663v1]
- 52. Self-Attention Diffusion Models for Zero-Shot Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562149/]
- 53. Segment anything in medical images [https://www.nature.com/articles/s41467-024-44824-z]
- 54. Comprehensive evaluation of optimization algorithms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12552475/]
- 55. Understanding Otsu's Method for Image Segmentation [https://www.baeldung.com/cs/otsu-segmentation]
- 56. Otsu's Thresholding Technique [https://learnopencv.com/otsu-thresholding-with-opencv/]
- 57. Multi-threshold image segmentation for melanoma based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9663822/]
- 58. ECM-TransUNet: Edge-enhanced multi-scale attention and ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809425003568]
- 59. The multi-level image segmentation in dermatology ... [https://www.nature.com/articles/s41598-025-22545-7]
- 60. Fast OTSU Thresholding Using Bisection Method [https://arxiv.org/abs/2509.16179]
- 61. A 3D lightweight network with Roberts edge enhancement ... [https://www.nature.com/articles/s41598-025-03151-z]
- 62. AI-Driven Advances in Low-Dose Imaging and Enhancement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11941271/]
- 63. Transforming CT imaging with deep learning: Noise ... [https://www.sciencedirect.com/science/article/pii/S3050577125000404]
- 64. Low-dose computed tomography image denoising using ... [https://www.nature.com/articles/s41598-025-10139-2]
- 65. ErisNet: A Deep Learning Model for Noise Reduction in CT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467190/]
- 66. Deep plug-and-play denoising prior with total variation ... [https://www.frontiersin.org/journals/physics/articles/10.3389/fphy.2025.1563756/full]
- 67. Key Concepts of Edge Detection for Machine Vision [https://resources.unitxlabs.com/key-concepts-edge-detection-machine-vision/]
- 68. An improved edge detection algorithm for X-Ray images ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6838874/]
- 69. Understanding WCAG 2 Contrast and Color Requirements [https://webaim.org/articles/contrast/]
- 70. Understanding Success Criterion 1.4.11: Non-text Contrast [https://www.w3.org/WAI/WCAG21/Understanding/non-text-contrast.html]
- 71. SemiSAM: Enhancing - Semi ... Supervised Medical Image [https://arxiv.org/html/2312.06316v2]
- 72. Rethinking Semi-Supervised Medical Image Segmentation [https://pmc.ncbi.nlm.nih.gov/articles/PMC11136570/]
- 73. - Semi segmentation via cross-guidance... supervised medical image [https://pubmed.ncbi.nlm.nih.gov/36636813/]
- 74. Enhancing unsupervised learning in medical image ... [https://pubmed.ncbi.nlm.nih.gov/39898031/]
- 75. What Is Hyperparameter Tuning? [https://www.ibm.com/think/topics/hyperparameter-tuning]
- 76. Simple Guide to Hyperparameter Tuning in Neural Networks [https://medium.com/data-science/simple-guide-to-hyperparameter-tuning-in-neural-networks-3fe03dad8594]
- 77. Essential Hyperparameter Tuning Techniques to Know [https://www.analyticsvidhya.com/blog/2022/02/a-comprehensive-guide-on-hyperparameter-tuning-and-its-techniques/]
- 78. Towards a guideline for evaluation metrics in medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9208116/]
- 79. Boundary guidance network for medical image segmentation [https://www.nature.com/articles/s41598-024-67554-0]
- 80. Metrics for evaluating 3D medical image segmentation [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-015-0068-x]
- 81. What are the evaluation indicators for image segmentation? [https://www.tencentcloud.com/techpedia/112106]
- 82. From Pixels to Precision—A Dual-Stream Deep Network for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384021/]
- 83. VR-prep improves visualization of medical data in ... [https://www.nature.com/articles/s41598-025-26856-7]
- 84. Region and Edge Based Segmentation [https://www.geeksforgeeks.org/machine-learning/region-and-edge-based-segmentaion/]
- 85. 5 Types of Image Segmentation Techniques in Vision ... [https://averroes.ai/blog/types-of-image-segmentation-techniques]
- 86. Pixel-Based Machine Learning in Medical Imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3299341/]
- 87. Understanding Evaluation Metrics in Medical Image ... [https://medium.com/mastering-data-science/understanding-evaluation-metrics-in-medical-image-segmentation-d289a373a3f]
- 88. Predictive techniques in medical imaging [https://www.nature.com/articles/s41746-025-01791-z]
- 89. Medical Image Preprocessing: Key Techniques & Best Practices [https://collectiveminds.health/articles/the-ultimate-guide-to-preprocessing-medical-images-techniques-tools-and-best-practices-for-enhanced-diagnosis]
- 90. Revolutionizing Precision Medicine with Quantitative Imaging [https://fas.org/publication/ai-enabled-precision-medicine/]
- 91. Multi-modality medical image segmentation via adversarial ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417425010899]
- 92. Deep Learning-based Image Segmentation on Multimodal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8553020/]
- 93. Enhancing efficient deep learning models with multimodal ... [https://www.nature.com/articles/s41598-025-91430-0]