EIT for Lung Perfusion Assessment: Principles, Applications, and Validation in Pulmonary Research
This article provides a comprehensive overview of Electrical Impedance Tomography (EIT) for lung perfusion assessment, tailored for researchers, scientists, and drug development professionals.
EIT for Lung Perfusion Assessment: Principles, Applications, and Validation in Pulmonary Research
Abstract
This article provides a comprehensive overview of Electrical Impedance Tomography (EIT) for lung perfusion assessment, tailored for researchers, scientists, and drug development professionals. We explore the foundational biophysical principles linking electrical impedance to pulmonary blood flow. The methodological section details current protocols, image reconstruction algorithms, and specific applications in preclinical and clinical research, including ventilator-induced lung injury and pharmacological studies. We address key troubleshooting challenges such as motion artifact and electrode contact, alongside optimization strategies for signal fidelity. Finally, we critically examine validation studies comparing EIT perfusion metrics against established gold-standard techniques and discuss its emerging role as a functional imaging biomarker. This synthesis aims to equip professionals with the knowledge to implement and interpret EIT for advancing pulmonary pathophysiology and therapeutic development.
Understanding EIT for Lung Perfusion: Core Biophysics and Physiological Correlates
Electrical Impedance Tomography (EIT) is a non-invasive imaging modality that reconstructs the internal conductivity distribution of a subject by applying small alternating currents and measuring resulting boundary voltages. Within the context of lung perfusion assessment, the core hypothesis is that changes in blood volume and flow directly modulate the local electrical impedance of lung tissue. This relationship is governed by Maxwell's mixture theory and the frequency-dependent behavior of biological tissues.
The impedance ((\sigma)) of a composite material like lung tissue can be modeled as: [ \sigma{mix} = \sigma{blood}\phi + \sigma_{tissue}(1 - \phi) ] where (\phi) is the volumetric fraction of blood. Blood flow introduces dynamic components: pulsatile arterial inflow increases (\phi) during systole, while venous drainage decreases it. Furthermore, the orientation and velocity of erythrocytes (which are anisotropic conductors) influence impedance, a phenomenon described by the Haematocrit and flow-dependent conductivity.
Table 1: Key Biophysical Parameters Linking Blood Dynamics to Electrical Impedance
| Parameter | Typical Range in Lung Tissue | Impact on Electrical Conductivity | Primary EIT Frequency Dependency |
|---|---|---|---|
| Blood Volume (BV) | 5-15% of lung tissue volume | Direct increase: +ΔBV → +ΔConductivity | Low (≤10 kHz): Extracellular path dominance |
| Haematocrit (Hct) | 35-45% in large vessels | Non-linear increase: Optimal Hct ~40% for max conductivity | Moderate (10-100 kHz): Cell membrane capacitance effects |
| Pulsatile Flow Rate | ~5-15 ml/s per lung segment | Time-varying conductivity; Shear-induced RBC alignment reduces resistivity | High (100 kHz - 1 MHz): Intracellular current path contribution |
| Tissue Fluid Index | Variable in pathology | Increased extravascular lung water increases conductivity, confounding perfusion signal | Multi-frequency (Bioimpedance Spectroscopy) required for separation |
Application Notes: EIT for Dynamic Perfusion Assessment
Note A: Separating Ventilation and Perfusion Signals Lung EIT measures a composite signal. To isolate perfusion (Q), synchronized gating to the cardiac cycle is essential. The functional EIT (fEIT) approach involves:
- Cardiac-gated Averaging: Averaging impedance frames over multiple heartbeats at the same cardiac phase to derive a "pure" perfusion-related temporal sequence.
- Frequency Domain Filtering: Utilizing the fundamental cardiac frequency (≈1-2 Hz) and its harmonics to filter out slower ventilation components (≈0.1-0.3 Hz).
Note B: Quantifying Regional Blood Volume Relative impedance change ((\Delta Z)) is linearly related to regional blood volume change ((\Delta BV)) within a limited range: [ \frac{\Delta Z}{Z_0} = S \cdot \Delta BV ] where (S) is a sensitivity factor derived from finite element modeling (FEM) of the thorax. Absolute quantification requires a reference measurement, often provided by indicator dilution (e.g., bolus of hypertonic saline) or calibration against another imaging modality (e.g., dynamic CT).
Note C: Estimating Flow from Impedance Kinetics The upslope of the impedance-time curve following a physiological perturbation (e.g., a deep breath, Valsalva, or contrast bolus) correlates with regional pulmonary blood flow. The Mean Transit Time (MTT) can be derived from the indicator dilution curve, allowing flow calculation via the Central Volume Principle: Flow = Volume / MTT.
Experimental Protocols
Protocol 1: In-Vivo Validation of EIT-Derived Perfusion Index
Objective: To validate EIT-derived perfusion indices against the gold-standard dynamic CT perfusion in an animal model.
Materials: See "Scientist's Toolkit" below.
Methodology:
- Animal Preparation: Anesthetize and mechanically ventilate a porcine model (n=6). Place a standard 16-electrode EIT belt around the thorax at the 5th intercostal space. Insert central venous and arterial lines.
- Synchronization Setup: Connect ECG, airway pressure, and arterial pressure waveforms to the EIT device for physiological gating.
- Baseline EIT Recording: Acquire 5 minutes of tidal ventilation EIT data at 50 frames/sec, 1 mA RMS, 100 kHz.
- Dynamic CT Perfusion Scan: Administer iodinated contrast bolus (0.5 ml/kg) via central line. Simultaneously initiate a high-temporal-resolution CT scan of the lung and the EIT recording.
- Data Analysis:
- EIT: Reconstruct time-difference images. Apply cardiac-gated averaging to extract perfusion-related impedance curves for predefined regions of interest (ROIs).
- CT: Generate time-attenuation curves for identical ROIs. Calculate CT perfusion parameters: Blood Volume (BV), Blood Flow (BF), and MTT.
- Correlation: Perform linear regression between the peak impedance change ((\Delta Z_{peak})) in EIT and CT-derived BV, and between the normalized impedance upslope in EIT and CT-derived BF.
Protocol 2: Characterizing Frequency-Dependent Impedance of Flowing Blood
Objective: To establish the conductivity-haematocrit-flow relationship using an in-vitro flow phantom.
Methodology:
- Phantom Construction: Create a flow circuit with a resistive chamber (simulating lung tissue segment) placed within an EIT electrode ring. Use a blood-mimicking fluid (e.g., saline with suspended polyhdroxyethyl starch particles) with adjustable haematocrit (30%, 40%, 50%).
- Impedance Spectroscopy: For each Hct level, pump fluid at controlled rates (0, 5, 15, 30 cm/s). At each flow state, perform multi-frequency EIT/bioimpedance measurements across a spectrum (10 kHz - 1 MHz).
- Parameter Extraction: Fit the collected data to the Cole-Cole model to extract extracellular resistance ((Re)), which is most sensitive to blood volume, and the characteristic frequency ((fc)), which shifts with cell orientation/flow.
Table 2: Example Data Output from Protocol 2 (Hypothetical Data)
| Haematocrit (%) | Flow Rate (cm/s) | Conductivity at 10 kHz (S/m) | Conductivity at 100 kHz (S/m) | Cole-Cole (f_c) (kHz) |
|---|---|---|---|---|
| 30 | 0 | 0.85 | 1.10 | 85 |
| 30 | 15 | 0.88 (+3.5%) | 1.15 (+4.5%) | 92 |
| 40 | 0 | 0.95 | 1.25 | 75 |
| 40 | 15 | 1.02 (+7.4%) | 1.35 (+8.0%) | 88 |
| 50 | 0 | 0.90 | 1.20 | 65 |
| 50 | 15 | 0.94 (+4.4%) | 1.27 (+5.8%) | 78 |
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions & Materials
| Item | Function & Rationale |
|---|---|
| Multi-frequency EIT System (e.g., Swisstom BB2, Draeger PulmoVista 500) | Capable of applying currents from 50 kHz to 1 MHz. Multi-frequency data is crucial for differentiating perfusion from ventilation and tissue edema via spectroscopic analysis. |
| Electrode Belt & Contact Gel | A 16-32 electrode textile belt with integrated Ag/AgCl electrodes. Hypoallergenic gel ensures stable skin contact and minimizes impedance drift. |
| Physiological Gating Module | Hardware/software module to synchronize EIT frame acquisition with ECG R-wave and ventilator inspiratory trigger. Essential for signal separation. |
| Finite Element Model (FEM) Mesh of Thorax | Patient-specific or generic mesh for forward modeling and image reconstruction. Allows calculation of sensitivity maps (lead fields) for quantitative analysis. |
| Blood-Mimicking Fluid (e.g., CIRS Phantom Fluid) | Stable, standardized fluid with tunable conductivity and permittivity to simulate blood at various Hct levels for phantom validation studies. |
| Hypertonic Saline (5-10%) | Used as an intravenous impedance contrast agent. Its high conductivity creates a measurable bolus track in EIT, enabling indicator dilution techniques. |
| Dedicated EIT Reconstruction Software (e.g., EIDORS, MATLAB Toolkit) | Open-source or commercial software for implementing linear (e.g., GREIT) or non-linear reconstruction algorithms, and for extracting regional time-impedance curves. |
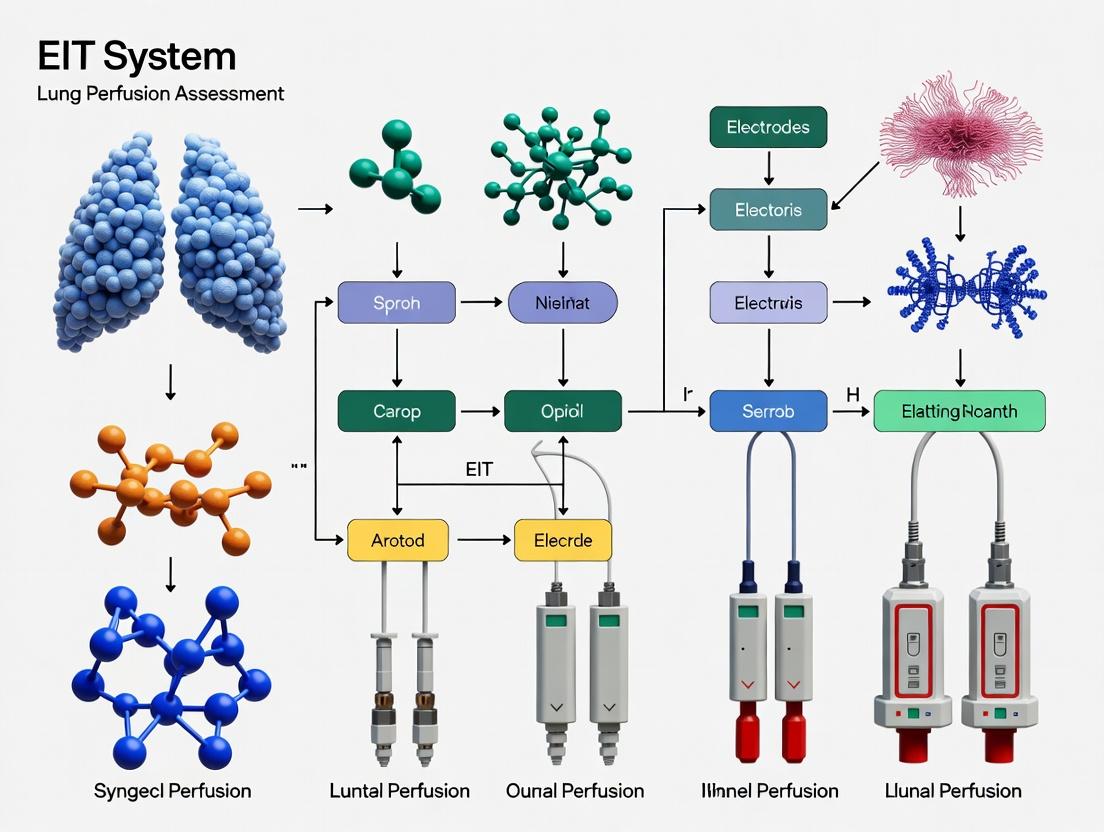
Visualizations
EIT Perfusion Assessment Workflow
Impedance-Blood Volume-Flow Relationship
This document provides application notes and experimental protocols for research within a doctoral thesis investigating Electrical Impedance Tomography (EIT) for lung perfusion assessment. The core objective is to elucidate the physiological correlates—perfusion (Q), ventilation (V), and their ratio (V/Q)—essential for validating and interpreting functional EIT images. The accurate, non-invasive, and bedside quantification of regional V/Q ratios via EIT represents a paradigm shift in pulmonary monitoring, with significant implications for critical care and pharmaceutical development.
Table 1: Normal and Pathophysiological Ranges for Ventilation, Perfusion, and V/Q Ratio
| Parameter | Symbol | Normal Range (Whole Lung) | Zone 1 (Apex) | Zone 2 (Mid) | Zone 3 (Base) | Pathological Example (e.g., PE) |
|---|---|---|---|---|---|---|
| Ventilation (L/min) | V | 4-6 (at rest) | ~0.8 L/min | ~1.2 L/min | ~2.0 L/min | Unchanged or increased dead space |
| Perfusion (L/min) | Q | 5-6 (at rest) | ~0.7 L/min | ~1.2 L/min | ~2.1 L/min | Markedly decreased in affected region |
| Ventilation-Perfusion Ratio | V/Q | 0.8 - 1.0 (mean) | ~1.1 | ~1.0 | ~0.9 | >>1 (High V/Q defect) |
| Alveolar Partial Pressure O2 (mmHg) | PAO₂ | ~100 | ~132 | ~108 | ~89 | Increased |
| Alveolar Partial Pressure CO2 (mmHg) | PACO₂ | ~40 | ~28 | ~40 | ~42 | Decreased |
Table 2: EIT-Derived Parameters for V/Q Assessment
| EIT Parameter | Physiological Correlate | Typical Calculation Method | Research Utility |
|---|---|---|---|
| ΔZ(t)vent | Regional Tidal Ventilation | Impedance change during quiet breathing | Maps regional ventilation distribution. |
| ΔZ(t)perf | Regional Pulsatile Perfusion | Impedance change synchronized with heartbeat (often using ECG-gating). | Maps regional perfusion distribution. |
| EIT-based V/Q Index | Regional V/Q Ratio | ΔZ(t)vent / ΔZ(t)perf (requires normalization). | Identifies shunt (low V/Q) or dead space (high V/Q). |
| Global Inhomogeneity Index | V/Q Mismatch | Spatial dispersion of impedance amplitudes. | Quantifies overall lung function impairment. |
Experimental Protocols for EIT V/Q Research
Protocol 3.1: In Vivo Validation of EIT Perfusion Using Microsphere Reference
Aim: To validate EIT-derived perfusion images against the gold standard of fluorescent or radioactive microsphere deposition. Materials: See Scientist's Toolkit. Procedure:
- Animal Preparation: Anesthetize and mechanically ventilate the subject (e.g., porcine model). Position the EIT belt around the thorax at the 5th intercostal space.
- Hemodynamic Monitoring: Establish continuous monitoring of ECG, arterial blood pressure, and central venous pressure.
- Baseline EIT Recording: Acquire 5 minutes of stable EIT data (
EIT_raw_baseline). - Microsphere Injection: a. Vigorously mix the vial containing ~1 million fluorescent microspheres (15µm diameter). b. Inject the suspension into the left atrium or ventricle over 30 seconds. c. Simultaneously, withdraw reference blood sample from the femoral artery at a constant rate (e.g., 10 mL/min) for 90 seconds using a syringe pump.
- Termination & Tissue Harvest: Administer a lethal dose of anesthetic. Excise the lungs, inflate with air, and freeze in liquid nitrogen vapor.
- Tissue Processing: Divide each lung into ~100 regions of interest (ROIs) corresponding to EIT pixels. Digest each ROI in a defined alkali solution. Filter the digest to capture microspheres.
- Microsphere Quantification: Count microspheres per ROI using a fluorescence spectrophotometer or flow cytometer. Calculate absolute blood flow (Q_ms) to each ROI using the reference blood sample counts.
- EIT Data Analysis: For the 30-second injection window, apply ECG-gating to the EIT signal. Generate the perfusion image (
ΔZ_perf) by averaging the cardiac-synchronous impedance changes. - Correlation Analysis: Perform linear regression between
ΔZ_perfamplitude (normalized) andQ_msfor all corresponding ROIs. A correlation coefficient (r) >0.85 is considered strong validation.
Protocol 3.2: Provocative Testing for V/Q Mismatch using Pharmacological Agents
Aim: To induce and monitor regional V/Q changes using pulmonary vasoconstrictors (e.g., Almitrine) or vasodilators (e.g., Inhaled Nitric Oxide - iNO). Materials: EIT system, mechanical ventilator, gas mixer, infusion pump, Almitrine bismesylate, iNO delivery system. Procedure:
- Baseline Acquisition: Under stable ventilation (FiO₂ 0.4), record 10 minutes of EIT data for
V_baselineandQ_baselinecalculation. - Intervention - Vasoconstriction:
a. Start infusion of Almitrine (e.g., 16 µg/kg/min IV).
b. After 20 minutes for equilibration, record a 5-minute EIT data block (
EIT_post_Almitrine). c. Expected Outcome: Increased pulmonary artery pressure, redistribution of perfusion to well-ventilated areas, improved overall V/Q matching. - Washout & New Baseline: Discontinue infusion. Wait 40 minutes and record a new baseline.
- Intervention - Vasodilation:
a. Commence iNO at 20 ppm via the inspiratory limb of the ventilator.
b. After 10 minutes, record a 5-minute EIT data block (
EIT_post_iNO). c. Expected Outcome: Vasodilation in well-ventilated regions, potentially worsening V/Q in areas with fixed obstruction (e.g., embolism). - Data Analysis: For each condition, calculate regional V and Q indices from EIT. Generate pixel-by-pixel V/Q ratio maps. Compare the spatial distribution and global inhomogeneity index across conditions.
Signaling and Physiological Pathways
Diagram 1: Hypoxic Pulmonary Vasoconstriction Feedback
Diagram 2: EIT-Based V/Q Ratio Calculation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for EIT Perfusion Research
| Item | Function & Relevance | Example/Specification |
|---|---|---|
| Functional EIT System | Generates and measures thoracic impedance. Must support high temporal resolution for cardiac-synchronous analysis. | Dräger PulmoVista 500, Swisstom BB2, or custom research system with >20 frames/sec. |
| ECG-Gating Module | Synchronizes impedance data with the cardiac cycle, crucial for separating perfusion (ΔZperf) from ventilation (ΔZvent) signals. | Integrated amplifier or post-processing software (e.g., MATLAB with peak detection). |
| Fluorescent Microspheres | Gold standard for validating regional perfusion. Different colors allow for multiple sequential measurements. | 15µm diameter, Triton Technology, various emission spectra (e.g., red, blue, violet). |
| Alkaline Tissue Digestant | Digests lung tissue to retrieve embedded microspheres for quantification. | 4M KOH or 2M NaOH with 0.5% Tween-80. |
| Syringe Pump | Provides precise, constant withdrawal rate for reference blood sample during microsphere injection. | Harvard Apparatus Pump 11 Elite. |
| Fluorescence Spectrophotometer | Quantifies the number of microspheres in digested tissue and blood samples. | Plate reader (e.g., Tecan Infinite) or dedicated fluorometer. |
| Inhaled Nitric Oxide (iNO) Delivery System | Precisely administers iNO to probe pulmonary vascular reactivity and V/Q responses. | Ikaria INOvent or similar calibrated blender. |
| Pulmonary Vasoconstrictor | Pharmacological probe (like Almitrine) to test hypoxic pulmonary vasoconstriction and its effect on V/Q. | Almitrine bismesylate (research grade). |
| Dedicated EIT Analysis Software | For advanced processing: filtering, ROI definition, image reconstruction, and V/Q map generation. | MATLAB with EIDORS toolbox or vendor-specific research software. |
Application Notes
Electrical Impedance Tomography (EIT) for pulmonary assessment has evolved from a global monitoring tool to a high-resolution functional imaging modality. Initial thoracic impedance measurements provided bulk resistivity changes, correlating with total lung water and ventilation. The advent of dynamic functional EIT (df-EIT), enabled by advanced electrodes, high-frame-rate hardware, and sophisticated reconstruction algorithms, now permits the visualization of regional lung perfusion, ventilation-perfusion (V/Q) matching, and endothelial function. This evolution is critical for a thesis on EIT for lung perfusion assessment, as it provides the technological foundation for quantifying drug effects on pulmonary circulation and barrier integrity in preclinical and clinical research.
Protocols
Protocol 1: Baseline Thoracic Impedance Measurement for Pulmonary Edema Assessment
- Objective: To measure global transthoracic impedance as a surrogate for lung fluid accumulation.
- Equipment: Bioimpedance spectrometer, 4 standard ECG electrodes.
- Setup: Place two injecting electrodes on the right lateral chest wall at the level of the xiphoid process and the left supraclavicular fossa. Place two sensing electrodes 5 cm medial to the injecting electrodes.
- Procedure:
- Apply a low-amplitude (1-5 mA), high-frequency (50-100 kHz) alternating current between injecting electrodes.
- Measure the voltage differential between sensing electrodes.
- Calculate impedance (Z = V/I). Record baseline Z₀.
- Induce experimental condition (e.g., drug infusion, lung injury model).
- Monitor continuous impedance (Zₜ). Calculate relative change ΔZ = (Zₜ - Z₀)/Z₀.
- Correlate a sustained decrease in ΔZ with increased lung water.
Protocol 2: Dynamic Functional EIT for Regional Lung Perfusion Imaging
- Objective: To generate tomographic images of regional pulmonary blood flow (PBF).
- Equipment: Multiplexing EIT system (e.g., 32-electrode), electrode belt, physiological monitor, central venous access.
- Procedure:
- Place electrode belt around the thorax at the 5th-6th intercostal space. Acquire a 5-minute baseline EIT ventilation scan.
- Prepare a bolus of 5-10 mL of hypertonic saline (5-10% NaCl) as an impedance contrast agent.
- At end-expiration, rapidly inject (<2 sec) the saline bolus via central venous catheter.
- Continue EIT data acquisition at ≥20 frames/sec for 60 seconds post-injection.
- Reconstruction & Analysis:
- Reconstruct temporal image sequences using a finite element model of the thorax.
- Apply a frequency filter to separate ventilation (0.05-0.5 Hz) from perfusion signal.
- For each pixel, analyze the time-series for the impedance drop following contrast injection.
- Calculate Perfusion Index (PI) as the maximum negative slope (ΔZ/Δt) of the dilution curve.
- Generate functional PI maps coregistered with CT anatomy.
Table 1: Evolution of Key EIT Performance Parameters
| Parameter | Thoracic Impedance (1980s-90s) | Modern Dynamic Functional EIT (2020s) |
|---|---|---|
| Electrodes | 4-8 | 16-32 (Multiplexed) |
| Frame Rate | ≤1 frame/min | 20-50 frames/sec |
| Temporal Resolution | Low (minute-scale) | High (millisecond-scale) |
| Spatial Resolution | Global or 1-2 regions | ~10-15% of diameter (DoT ~100 pixels) |
| Primary Output | ΔZ (Ω) or ΔV | 2D/3D functional image (V, Q, V/Q ratio) |
| Key Perfusion Metric | Not available | Perfusion Index (PI), Mean Transit Time |
Table 2: Typical Impedance Changes in Physiological & Pathological States
| State/Intervention | Global Thoracic ΔZ | Regional EIT Signal (Perfusion) |
|---|---|---|
| Normal Tidal Ventilation | Cyclic ±0.1-0.3 Ω | Cyclic regional impedance change |
| Hypertonic Saline Bolus (IV) | Monophasic decrease ~0.5 Ω | Sharp regional decrease; PI = 5-15 ΔZ/s |
| Pulmonary Embolism | Minimal change | Focal absence of perfusion signal |
| Acute Lung Injury Edema | Sustained decrease of 2-5 Ω | Heterogeneous perfusion, increased V/Q mismatch |
Visualizations
Evolution from Global Impedance to Functional EIT
df-EIT Protocol for Perfusion & V/Q Imaging
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in EIT Lung Perfusion Research |
|---|---|
| Hypertonic Saline (5-10%) | Non-toxic, non-radioactive impedance contrast agent. IV bolus induces a transient decrease in blood impedance, enabling bolus-tracking perfusion imaging. |
| EIT Electrode Belt (16-32 channel) | Flexible belt with integrated electrodes for consistent circumferential contact. Enables cross-sectional imaging of the thorax. |
| Finite Element Model (FEM) Mesh | Digital 3D model of the thorax (lungs, heart, chest wall) derived from CT. Essential for accurate image reconstruction from boundary voltage data. |
| Gelatin-Saline Phantom | Calibration phantom with known conductivity, simulating lung and cardiac tissues. Used for system validation and algorithm testing. |
| Pulmonary Vasodilator (e.g., inhaled NO) | Pharmacological probe to assess pulmonary vascular reactivity and endothelial function by measuring perfusion redistribution pre- and post-administration. |
| ICU Ventilator with EIT Sync | Ventilator capable of outputting trigger signals to the EIT device, allowing precise phase-locking of images to the respiratory cycle. |
Within a research thesis focused on Electrical Impedance Tomography (EIT) for lung perfusion assessment, the selection and application of hardware components are critical. Accurate imaging of pulmonary perfusion—the process of blood flow through the lung's capillary bed—demands high-precision instrumentation to detect subtle, dynamic impedance changes. This document details the core hardware components, their specifications, and experimental protocols essential for conducting robust and reproducible lung perfusion EIT studies, directly supporting research into pulmonary pathologies, drug delivery efficacy, and ventilatory management.
Core Hardware Components: Specifications & Function
The primary hardware chain for functional EIT consists of three integrated subsystems.
Electrode Belts & Sensor Arrays
Electrode belts form the primary sensor interface with the subject. For thoracic EIT, belts typically contain 16 to 32 equally spaced electrodes.
Table 1: Electrode Belt Configuration for Thoracic EIT
| Parameter | Typical Specification for Lung Perfusion | Rationale/Impact |
|---|---|---|
| Number of Electrodes | 16, 32, or 64 | Higher count improves spatial resolution but increases data complexity. 32 is common. |
| Electrode Material | Medical-grade Ag/AgCl, stainless steel, or conductive textile | Ag/AgCl reduces contact impedance and polarization effects. |
| Belt Flexibility | Stretchable, adjustable substrate (e.g., silicone, rubber) | Ensures consistent electrode contact across varying thoracic circumferences during respiration. |
| Inter-Electrode Spacing | Constant (e.g., ~2-3 cm for adult human thorax) | Critical for accurate reconstruction algorithms. |
| Application Mode | Single-plane, circumferentially around the 5th-6th intercostal space | Standard plane for separating cardiac and pulmonary signals. |
The current source injects a safe, known alternating current (AC) between a pair of drive electrodes. Its performance dictates signal-to-noise ratio.
Table 2: Current Source Specifications
| Parameter | Optimal Specification | Rationale/Impact |
|---|---|---|
| Output Current | 1-5 mA RMS (Human), 0.1-1 mA (Rodent) | Safety limit; balances signal strength and patient safety (IEC 60601). |
| Frequency Range | 10 kHz - 1 MHz (multi-frequency for SF-EIT) | Lung perfusion studies often use 50-150 kHz to optimize blood conductivity contrast. |
| Frequency Stability | < 0.01% | Prevents phase errors in voltage measurements. |
| Output Impedance | > 1 MΩ | Ensures current is constant despite varying skin-electrode contact impedance. |
| Waveform | Sinusoidal, often with bipolar square wave approximation | Purity affects measurement accuracy, especially in phase-sensitive systems. |
Voltage Measurement Systems
This subsystem measures differential voltages between adjacent electrode pairs (adjacent drive pattern) or other patterns. It is typically integrated with the current source in an EIT data acquisition system (DAS).
Table 3: Voltage Measurement Specifications
| Parameter | Critical Requirement | Rationale/Impact |
|---|---|---|
| Voltage Accuracy | ±0.1% of reading ± 10 µV | Essential for reconstructing small impedance changes (<1%) due to perfusion. |
| Input Impedance | > 100 MΩ, < 50 pF parallel | Minimizes signal loading and preserves measurement integrity. |
| Common-Mode Rejection Ratio (CMRR) | > 100 dB at drive frequency | Rejects common noise from the body and environment. |
| Bandwidth | Suited to drive frequency | Must filter out powerline noise (50/60 Hz) and harmonic interference. |
| Analog-to-Digital Converter (ADC) | 16-24 bit resolution | High dynamic range to capture small voltage changes on large baseline. |
Experimental Protocols for Lung Perfusion EIT
Protocol: System Calibration & Validation
Objective: To verify the accuracy and linearity of the complete EIT hardware chain prior to in-vivo measurement. Procedure:
- Connect Calibration Phantoms: Use a network of precision resistors (e.g., 150 Ω - 510 Ω range) configured in a known geometric pattern to simulate a simplified thoracic impedance.
- Apply Reference Current: Program the DAS to apply the standard current (e.g., 1 mA RMS, 100 kHz) using the intended adjacent drive pattern.
- Measure Voltage Matrix: Record all differential voltage measurements for all drive pairs.
- Calculate Expected Voltages: Using Ohm's law and the known resistor network topology, compute the expected voltage for each measurement.
- Analyze Linearity & Error: Create a scatter plot of Measured vs. Expected voltages. Perform linear regression. System is validated if slope = 1.00 ± 0.01 and R² > 0.999. Record any systematic offsets for software compensation.
Protocol:In-VivoLung Perfusion Assessment (Human)
Objective: To acquire dynamic EIT data for separating and quantifying cardiac-related (perfusion) and ventilation-related impedance changes. Materials: See "The Scientist's Toolkit" below. Procedure:
- Subject Preparation: Clean skin at electrode contact points (5th-6th intercostal space) with alcohol wipes. Light abrasion may be used to reduce contact impedance to < 2 kΩ at 50 kHz.
- Belt Application: Fit the electrode belt snugly around the thorax. Verify all electrodes show stable contact impedance via the DAS monitoring software.
- Baseline Data Acquisition: a. Instruct the subject to hold breath at end-expiration for 10-15 seconds. b. Acquire EIT data at high frame rate (≥ 50 fps) during apnea. This captures the cardiac-related impedance change (stroke volume) without ventilation artifact.
- Dynamic Data Acquisition: Have the subject breathe normally. Acquire data for 5-10 minutes at a standard frame rate (10-30 fps). Synchronize data acquisition with other monitors (e.g., ECG, spirometer) via trigger pulses.
- Post-Processing (Key Steps): a. Filtering: Apply a bandpass filter (e.g., 0.8 - 5 Hz) to extract the cardiac signal (perfusion) and a low-pass filter (< 0.3 Hz) for the ventilation signal. b. Gating: Use the synchronized ECG R-wave to average cardiac cycles, creating a single, high-SNR "pulse wave" impedance change map. c. Region of Interest (ROI) Analysis: Define ROIs for the right and left lung in the EIT image. Plot the time-course of impedance in each ROI to analyze perfusion distribution.
Visualizations
Title: EIT Hardware Data Flow for Lung Perfusion
Title: In-Vivo Lung Perfusion EIT Protocol Workflow
The Scientist's Toolkit: Key Research Reagent Solutions & Materials
Table 4: Essential Materials for Lung Perfusion EIT Research
| Item | Function / Rationale | Example/Notes |
|---|---|---|
| Ag/AgCl Electrode Gel | Reduces skin-electrode contact impedance, ensures stable current injection. | Parker Laboratories SignaGel; hypoallergenic, high conductivity. |
| Alcohol Prep Pads (70% IPA) | Cleans skin to remove oils, improving gel contact and reducing impedance. | Standard medical-grade isopropyl alcohol wipes. |
| Abrasive Skin Prep Gel | Lightly removes stratum corneum for very high impedance subjects. | NuPrep Skin Prep Gel; used sparingly. |
| Calibration Phantom Network | Validates hardware linearity and accuracy before in-vivo use. | Custom resistor network mimicking thoracic impedance. |
| ECG Trigger Module | Provides synchronization signal for gating cardiac cycles in EIT data. | Biopac ECG100C or integrated in patient monitor. |
| Spirometer / Ventilator | Provides synchronized respiratory phase data for ventilation signal correlation. | COSMED K5 or ventilator analog output. |
| EIT Data Acquisition Software | Controls hardware, acquires data, performs real-time visualization. | Custom (MATLAB, Python) or commercial (Draeger, Swisstom). |
| Image Reconstruction & Analysis Suite | Reconstructs images, filters signals, performs ROI quantification. | EIDORS (MATLAB) or custom Python scripts. |
Application Notes for EIT in Lung Perfusion Research
Within the broader thesis on Electrical Impedance Tomography (EIT) for lung perfusion assessment, three fundamental advantages define its unique research value: Bedside Capability, Radiation-Free Monitoring, and High Temporal Resolution. These pillars enable novel experimental paradigms in pulmonary research and drug development.
Bedside Capability
EIT systems are portable, typically weighing <5 kg, and require only a single power outlet. This facilitates longitudinal studies in intensive care units, operating rooms, or dedicated physiology labs without transferring critically ill subjects or complex animal models. Research protocols can be conducted in the subject's native environment, minimizing confounding stress variables.
Radiation-Free Monitoring
Unlike CT perfusion scans or scintigraphy, EIT uses harmless, low-amperage alternating currents. This permits unlimited, repeated measurements over time—from minutes to days—enabling the study of dynamic processes like drug pharmacokinetics/pharmacodynamics, ventilator-induced lung injury progression, or ARDS resolution without cumulative radiation exposure risks.
High Temporal Resolution
Modern EIT systems achieve frame rates of 40-100 Hz, capturing physiological events within a single cardiac or respiratory cycle. This allows for the differentiation of perfusion (cardiac-driven) and ventilation (respiration-driven) signals through waveform analysis, providing beat-to-beat or breath-to-breath hemodynamic data.
Table 1: Comparison of Perfusion Imaging Modalities in Research
| Modality | Temporal Resolution | Spatial Resolution | Bedside Use | Radiation/Invasiveness | Typical Perfusion Metrics |
|---|---|---|---|---|---|
| EIT | 40-100 Hz | ~10-15% of torso diameter | Yes | None (Non-invasive) | Impedance curve amplitude, Pulse wave ratio, Cardiac-related impedance change |
| CT Perfusion | 0.5-3 Hz | ~1 mm | No | High (Ionizing) | Blood flow (mL/100g/min), Blood volume (mL/100g), Mean Transit Time (s) |
| MRI (ASL) | 0.2-0.5 Hz | 2-3 mm | No | None (Magnetic) | Perfusion (mL/100g/min) |
| Laser Speckle | 10-25 Hz | ~0.1 mm (surface) | Yes (surface) | None (Optical) | Relative blood flow units |
| PET | 0.1-0.5 Hz | 4-5 mm | No | High (Radioactive tracer) | Blood flow (mL/100g/min) |
Table 2: Typical EIT Perfusion Experiment Parameters
| Parameter | Typical Setting (Human) | Typical Setting (Large Animal) | Key Influence on Data |
|---|---|---|---|
| Current Amplitude | 1-5 mA (RMS) | 1-5 mA (RMS) | Signal-to-noise ratio, Safety |
| Frequency | 50-200 kHz | 50-200 kHz | Tissue penetration, Capacitive effects |
| Electrode Array | 16-32 electrodes | 16-32 electrodes | Spatial resolution, Coverage |
| Frame Rate | 40-100 fps | 40-100 fps | Cardiac cycle resolution |
| Reconstruction Grid | 800-1500 pixels | 800-1500 pixels | Image smoothness, Computation time |
| Recording Duration | 5-60 minutes per intervention | 5-60 minutes per intervention | Capturing dynamic responses |
Detailed Experimental Protocols
Protocol 1: EIT-Based Quantification of Pulmonary Perfusion Response to Vasoactive Drug
Objective: To assess regional pulmonary blood flow changes in response to intravenous vasodilator/inhalational vasoconstrictor administration.
Materials & Setup:
- EIT system with 32-electrode belt placed around the thorax at the 5th-6th intercostal space.
- Synchronized ECG and airway pressure (Paw) monitoring.
- Large animal (porcine) model or human research subject in supine position.
- Controlled mechanical ventilation.
- Drug infusion pump.
Procedure:
- Baseline Recording: Acquire stable EIT data for 5 minutes at 50 fps. Simultaneously record ECG, Paw, and systemic blood pressure.
- Intervention: Administer drug (e.g., inhaled nitric oxide at 20 ppm, IV almitrine) via predetermined protocol.
- Response Monitoring: Continue EIT recording for 15 minutes post-initiation. Note time of administration in data log.
- Data Segmentation: Isolate data 2 minutes pre-administration (baseline) and minutes 5-10 post-administration (steady-state response).
- Signal Processing: Apply bandpass filter (0.8-4 Hz) to EIT time-series to isolate cardiac-frequency components. Generate functional images of perfusion (e.g., by calculating impedance variance or amplitude within cardiac band).
- Analysis: Divide lung region into ventral, middle, and dorsal regions-of-interest (ROIs). Calculate relative change in perfusion index (ΔImp) for each ROI between baseline and response periods.
Protocol 2: Validation of EIT Perfusion Against Dynamic CT
Objective: To correlate EIT-derived perfusion indices with gold-standard quantitative perfusion from dynamic contrast-enhanced CT.
Materials & Setup:
- Combined EIT/CT-compatible research suite.
- Animal model with intravascular catheter.
- Dual-syringe power injector for contrast agent.
- Synchronization trigger between EIT and CT systems.
Procedure:
- Preparation: Position subject in CT gantry. Place EIT electrode belt. Ensure all equipment is CT-safe.
- Synchronized Baseline: Record concurrent EIT (50 fps) and low-dose CT scan for anatomical co-registration.
- Dynamic Acquisition Trigger: Start high-temporal-resolution CT perfusion scan (e.g., 1 scan/sec for 60s). Precisely 10 seconds after CT start, trigger EIT recording at 50 fps and initiate contrast injection (2 mL/kg at 5 mL/s).
- Data Acquisition: Continue EIT recording for 2 minutes.
- Coregistration: Use CT-derived lung contour to define identical ROIs on EIT images.
- Time-Activity Analysis: For each ROI, extract time-impedance curve (EIT) and time-attenuation curve (CT). Calculate peak enhancement, time-to-peak, and flow index from both modalities.
- Statistical Correlation: Perform linear regression between EIT impedance change amplitude and CT-derived blood flow across all ROIs and subjects.
Visualizations
EIT Drug Response Experiment Workflow
EIT Perfusion Data Processing Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for EIT Lung Perfusion Research
| Item | Function & Relevance | Example/Specification |
|---|---|---|
| Multi-Frequency EIT System | Enables simultaneous collection of impedance data at multiple frequencies (e.g., 10 kHz - 1 MHz). Allows separation of perfusion (vascular) signals from ventilation (air) signals via frequency-difference imaging. | Swisstom BB2, Draeger PulmoVista 500, or custom research systems (e.g., Goe-MF II). |
| CT-Compatible Electrode Belts & Wires | Allows for simultaneous or sequential EIT and CT imaging without artifact or safety risk. Critical for validation studies. | Carbon electrode belts with non-metallic, high-resistance leads. |
| ECG & Airway Pressure Synchronization Module | Hardware/software to synchronize EIT data acquisition with cardiac (R-wave) and respiratory (start of inspiration) cycles. Essential for gating and signal separation. | Biopac MP160 or custom analog input on EIT device. |
| Contrast Agents for Validation | Injectable agents to create impedance changes for validation. Hypertonic saline (5-10%) is common; its bolus passage tracks perfusion. | 5-10% NaCl solution, 0.5 mL/kg bolus. |
| Standardized Ventilation Control Software | To deliver precise, reproducible ventilatory patterns (tidal volume, PEEP, rate) during perfusion experiments, minimizing confounding impedance changes. | FlexiVent (for animals) or ICU ventilator with research interface. |
| Gel/AgCl Electrolyte Interface | Improves skin contact, reduces impedance, and ensures stable current injection. Electrode-skin impedance should be <5 kΩ for reliable data. | SignaGel, Ten20 conductive paste. |
| ROI Analysis Software | Enables definition of anatomical (e.g., ventral/dorsal) or functional regions on EIT images for quantitative comparison of perfusion indices. | MATLAB EIT toolkit, EIDORS with custom scripts. |
| Vasoactive Pharmaceutical Agents | Research tools to induce controlled, reversible changes in pulmonary perfusion for physiological challenge tests. | Inhaled Nitric Oxide (iNO), IV Almitrine, IV Adenosine, IV Epoprostenol. |
Implementing EIT Perfusion Imaging: Protocols, Algorithms, and Research Applications
Within a broader thesis investigating Electrical Impedance Tomography (EIT) for quantitative lung perfusion assessment, standardized measurement protocols are foundational. They ensure reproducibility, enable cross-study comparisons, and are critical for translating research findings into clinical or pharmaceutical development applications. This document details the application notes and protocols for three core procedural pillars: electrode placement, contrast agent (typically hypertonic saline) injection, and data acquisition.
Electrode Placement Protocol
Objective
To ensure consistent, reliable, and reproducible positioning of EIT electrodes on the thoracic surface for lung perfusion imaging.
Materials & Preparation
- EIT System & Electrode Belt: A 16- or 32-electrode EIT system with a corresponding stretchable belt.
- Electrodes: Self-adhesive Ag/AgCl ECG electrodes.
- Skin Preparation Kit: Isopropyl alcohol (70%), abrasive gel, marking pen, measuring tape.
- Subject Positioning: Semi-recumbent position at 45°, arms abducted to avoid interference.
Detailed Protocol
- Landmark Identification: Identify the 4th/5th intercostal space (ICS) at the parasternal line. This level is recommended as the standard plane for thoracic EIT.
- Belt Placement: Align the electrode belt horizontally around the thorax, ensuring its centerline passes through the identified ICS plane.
- Electrode Application: Apply electrodes equidistantly through the belt's openings. For a 16-electrode setup, this results in 16 equally spaced electrode positions around the chest circumference.
- Skin Contact Verification: Measure the electrode-skin contact impedance. Acceptable values are typically < 5 kΩ. Re-prepare skin or reposition electrodes if impedance is high.
Electrode Configuration & Data
Table 1: Standard Electrode Placement Parameters
| Parameter | 16-Electrode Setup | 32-Electrode Setup | Notes |
|---|---|---|---|
| Standard Plane | 4th/5th ICS | 4th/5th ICS | Ensures imaging through heart & major vessels |
| Inter-Electrode Spacing | 22.5° (theoretical) | 11.25° (theoretical) | Achieved via equidistant belt placement |
| Reference Electrode | Single, on abdomen | Single, on abdomen | For ground/reference potential |
| Target Contact Impedance | < 5 kΩ | < 5 kΩ | Pre-measurement QC step |
| Preferred Electrode Type | Ag/AgCl, hydrogel | Ag/AgCl, hydrogel | Low polarization, stable contact |
Contrast Agent Injection Protocol
Objective
To administer a standardized bolus of conductive contrast agent (hypertonic saline) for dynamic lung perfusion imaging via EIT.
Materials
- Contrast Agent: 5-10% Hypertonic saline solution, sterile.
- Injection System: Large-bore (≥18G) peripheral IV catheter, 3-way stopcock, two 10mL syringes (one for saline, one for contrast).
- Safety Equipment: ECG monitor, resuscitation kit (for rare adverse reactions).
Detailed Protocol
- IV Access: Establish secure intravenous access in a large antecubital vein.
- Pre-injection Baseline: Acquire ≥30 seconds of stable EIT baseline data.
- Bolus Preparation: Draw exactly 10mL of contrast agent into a dedicated syringe.
- Injection: Rapidly inject the 10mL bolus in <2 seconds, immediately followed by a 10mL normal saline flush at the same speed to propel the contrast into central circulation.
- Synchronization: Use a trigger signal (e.g., footswitch) to mark the injection start time on the EIT data stream.
- Monitoring: Monitor subject's ECG and sensation during injection.
Injection Parameters & Safety
Table 2: Standardized Contrast Agent Injection Protocol
| Parameter | Specification | Rationale |
|---|---|---|
| Agent | 5% or 10% NaCl, sterile | Proven conductivity contrast, well-studied |
| Bolus Volume | 10 mL | Sufficient signal change, minimizes volume load |
| Injection Speed | >5 mL/sec (Total < 2 sec) | Ensures tight, detectable bolus |
| Flush Volume | 10 mL Normal Saline | Ensures complete contrast delivery |
| IV Catheter Size | 18 Gauge or larger | Allows required injection speed |
| Safety Contraindications | Known pulmonary hypertension, severe renal impairment, cardiac failure | Risk of volume overload |
Data Acquisition Protocol
Objective
To acquire high-fidelity, time-synchronized EIT data during the contrast bolus passage for subsequent perfusion analysis.
System Setup
- EIT Device: Modern functional EIT system with adjacent current injection and voltage measurement pattern.
- Frame Rate: ≥ 30 frames per second (fps). ≥50 fps recommended for capturing first-pass kinetics.
- Current Amplitude: Typically 3-5 mA RMS, at a frequency of 50-150 kHz.
- Auxiliary Synchronization: Input channel for injection trigger marker.
Detailed Acquisition Workflow
- Pre-injection Calibration: Perform a reference measurement (e.g., on a resistor test phantom) if required by the system.
- Baseline Recording: Start EIT data acquisition at least 30 seconds prior to injection to establish a stable hemodynamic baseline.
- Trigger & Injection: At a predefined point, activate the injection trigger. The injector performs the rapid bolus as per Section 3.
- Post-injection Recording: Continue acquisition for a minimum of 120 seconds post-trigger to capture the entire first-pass and recirculation phase.
- Data Export: Export raw voltage data (V), timing triggers, and electrode position information for offline reconstruction and analysis.
Acquisition Parameters
Table 3: Standard EIT Data Acquisition Parameters for Lung Perfusion
| Parameter | Recommended Setting | Purpose |
|---|---|---|
| Acquisition Frequency | ≥ 50 fps | Temporal resolution for peak capture |
| Current Pattern | Adjacent, bipolar | Common, robust pattern |
| Current Amplitude | 5 mA RMS (max) | Safety (well below limits), good SNR |
| Carrier Frequency | 100 kHz | Good tissue penetration, low capacitive effects |
| Total Acquisition Time | 180 seconds (30s pre, 150s post) | Captures full hemodynamic response |
| Auxiliary Trigger | Enabled | Marks injection time (t=0) |
| Data Format | Raw voltages (V) + metadata | Enables flexible offline processing |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for EIT Lung Perfusion Studies
| Item | Function/Description | Example/Note |
|---|---|---|
| Functional EIT System | Device to inject current, measure boundary voltages, and reconstruct images. | Systems from Draeger, Swisstom, Timpel, or custom research systems. |
| Ag/AgCl Electrode Belt | Multi-electrode array for standardized thoracic placement. | Disposable or reusable belts with 16 or 32 integrated electrodes. |
| Hypertonic Saline (5-10%) | Ionic contrast agent to induce impedance change during first-pass. | Sterile, non-pyrogenic. Central ingredient for EIT perfusion. |
| High-Flow IV Catheter Set | Enables rapid bolus injection of contrast. | 18G x 2-inch or larger peripheral venous catheter. |
| Synchronization Trigger | Device to mark injection start on EIT data stream. | Simple footswitch or electronic signal generator. |
| EIT Data Analysis Suite | Software for image reconstruction, filtering, and perfusion parameter calculation. | MATLAB with EIDORS toolbox, or vendor-specific software. |
| Calibration Test Phantom | Object with known impedance for system validation. | Saline-filled tank with known insulating inclusions. |
Visualization of Protocols and Workflow
Title: EIT Lung Perfusion Measurement Workflow
Title: From EIT Data to Perfusion Parameters
Application Notes
Within the broader thesis on Electrical Impedance Tomography (EIT) for lung perfusion assessment, the selection and implementation of image reconstruction algorithms are critical. EIT infers the internal distribution of electrical conductivity from boundary voltage measurements. For dynamic perfusion imaging, three algorithmic approaches are paramount: Finite Element Method (FEM) for forward modeling, the Graz consensus Reconstruction algorithm for EIT (GREIT) for standardized linear reconstruction, and Time-Difference (TD) analysis for dynamic functional imaging.
FEM for Forward Modeling: The forward model solves the governing equation (∇·(σ∇φ)=0, where σ is conductivity and φ is potential) to predict boundary voltages for a given conductivity distribution. FEM discretizes the complex thoracic geometry (lungs, heart, vessels) into a mesh of finite elements, allowing numerical solutions. The accuracy of the forward model, defined by mesh quality and anatomical representation, directly limits the accuracy of all subsequent reconstruction algorithms. A typical high-resolution thoracic FEM mesh contains 20,000-50,000 elements to adequately capture geometric boundaries. Error norms between measured and simulated voltages (e.g., RMS error < 2%) validate model fidelity.
GREIT for Linear Reconstruction: GREIT provides a standardized framework for creating linear reconstruction matrices. It is not a single algorithm but a protocol that optimizes a matrix (R) to map voltage changes (∆V) to conductivity change images (∆σ) via ∆σ = R∆V. The optimization uses numerical phantoms (e.g., 32-electrode, adjacent drive pattern) to achieve desired performance figures of merit: 50% amplitude response, <10% position error, and <5 mm resolution across the field of view, while suppressing noise (amplification < 10). This standardization facilitates comparison of perfusion images across different research centers and hardware platforms.
Time-Difference Analysis for Perfusion: TD-EIT is the primary modality for lung perfusion assessment. It reconstructs images of change in conductivity relative to a reference time point, typically end-expiration. This inherently rejects unchanging geometric artifacts and highlights dynamic physiological processes. For perfusion, a cardiac-gated or sliding-window reference is used. Key quantitative perfusion indices are derived from TD images, including regional perfusion delay (time-to-peak), relative stroke volume (amplitude), and wash-in/wash-out slopes.
Table 1: Key Performance Metrics for EIT Reconstruction Algorithms in Lung Perfusion
| Metric | FEM (Forward Model) | GREIT (Linear Inverse) | Time-Difference Analysis |
|---|---|---|---|
| Primary Role | Predict voltages from conductivity | Reconstruct image from voltages | Isolate dynamic physiological signals |
| Key Output | Transfer matrix (Jacobian, J) | Reconstruction matrix (R) | Time-series of ∆σ(x,y,t) |
| Optimization Goal | Minimize forward modeling error (RMS < 2%) | Achieve consensus figures of merit (Position Error < 5mm) | Maximize contrast-to-noise ratio (CNR > 5 for perfusion) |
| Typical Mesh/Grid Size | 25,000 - 40,000 tetrahedral elements | 32x32 pixel uniform reconstruction grid | Same as reconstruction grid (e.g., 32x32) |
| Computational Load | High (solved once, offline) | Low (matrix multiplication, real-time) | Low (applies R to ∆V(t)) |
| Main Advantage | Incorporates complex anatomy | Standardized, reproducible, fast | Robust to systematic errors, highlights changes |
Experimental Protocols
Protocol 1: Development and Validation of a Subject-Specific Thoracic FEM Model Objective: To create an accurate forward model for a specific subject to improve reconstruction accuracy in subsequent perfusion studies.
- Anatomical Data Acquisition: Acquire thoracic CT or MRI scans of the subject in supine position at breath-hold end-expiration.
- Segmentation & Mesh Generation: Using software (e.g., Simplexare BioMesh, ANSYS, or MATLAB PDE Toolbox):
- Segment the major compartments: lungs, heart, major vessels, chest wall, and spine.
- Export boundaries as stereolithography (STL) files.
- Generate a 3D tetrahedral volume mesh (target: >25,000 elements). Assign initial conductivity estimates (σlung=0.3, σheart=0.7, σ_chest=0.2 S/m at 100 kHz).
- Electrode Positioning: Project the 2D electrode belt positions (from measurement system) onto the 3D chest wall surface in the mesh.
- Forward Solution Computation: Using an EIT solver (e.g., EIDORS), compute the Jacobian (J) and reference voltages (V_ref) for the chosen current injection pattern (e.g., adjacent, 32 electrodes).
- Validation: Compare simulated boundary voltage patterns from known test perturbations (e.g., saline injection in phantom) with measured data. Iteratively refine mesh and conductivity values to achieve an RMS error of <2%.
Protocol 2: Implementing GREIT for Standardized Perfusion Imaging Objective: To generate a standardized linear reconstruction matrix optimized for lung perfusion feature localization.
- Define Parameters: Specify electrode configuration (number, geometry), reconstruction grid (32x32 pixels), and desired performance metrics from the GREIT protocol (e.g., 50% amplitude, 5mm PSF).
- Create Training Data: Use a high-fidelity FEM model (from Protocol 1) to simulate boundary voltage changes (∆V_sim) for numerous small conductive targets (e.g., 5mm radius) at all positions (x,y) on the reconstruction grid.
- Matrix Optimization: Use the EIDORS
mk_GREIT_modelfunction to compute the reconstruction matrix (R). The algorithm optimizes R to solve: ∆σest = R ∆Vmeas, such that the reconstructed images match the desired performance metrics averaged over all target positions and noise trials. - Evaluation: Test the performance of the R matrix on independent simulated data (e.g., a larger, off-center "perfusion" target). Quantify position error, resolution, and shape deformation.
Protocol 3: Time-Difference EIT Protocol for Bolus-Tracking Perfusion Assessment Objective: To acquire and process dynamic EIT data for quantifying regional lung perfusion using an intravenous bolus of hypertonic saline as a contrast agent.
- Subject Preparation: Position subject supine. Place a 32-electrode EIT belt around the thorax at the 5th-6th intercostal space. Connect to a functional EIT device (e.g., Dräger PulmoVista 500, Swisstom BB2).
- Data Acquisition & Reference Selection:
- Record baseline EIT data at 48 frames/sec for 60 seconds.
- Instruct subject to hold breath at end-expiration for 5 seconds to acquire a stable reference frame (V_ref).
- Resume normal breathing.
- Contrast Injection: At a predefined time, rapidly inject 10mL of 5% NaCl solution via a central venous line.
- Data Processing:
- Apply the GREIT reconstruction matrix (R) in time-difference mode: ∆σ(t) = R (V(t) - V_ref).
- Apply a band-pass filter (0.5-5 Hz) to isolate cardiac-frequency components.
- Perform cardiac gating using a synchronized ECG signal to average perfusion over multiple cycles.
- Region of Interest (ROI) Analysis: Define ROIs for left/right, ventral/dorsal lung regions. Extract time-conductivity curves for each ROI. Calculate perfusion indices: Time to Peak (TTP) from injection, Maximum Slope of the upstroke, and Relative Stroke Volume (peak amplitude).
EIT Perfusion Imaging Reconstruction Pipeline
Hypertonic Saline Bolus Path & EIT Signal
The Scientist's Toolkit: Research Reagent Solutions & Essential Materials
| Item/Reagent | Function in EIT Perfusion Research |
|---|---|
| Functional EIT System (e.g., Swisstom BB2, Dräger PulmoVista) | Hardware to apply safe alternating currents (e.g., 5 mA, 100 kHz) through electrodes and measure resulting boundary voltages at high frame rates (>40 fps). |
| Multi-Frequency EIT System (e.g., MFEIT from University of Sheffield) | Enables spectroscopic EIT, potentially differentiating perfusion-related conductivity changes from ventilation or edema based on frequency dependence. |
| 32-Electrode Self-Adhesive Belt | Sensor array for thoracic measurements. Electrodes are typically Ag/AgCl for good skin contact and signal stability. |
| 5% or 10% Sodium Chloride (NaCl) Solution | Intravenous contrast agent for bolus-tracking perfusion EIT. Hypertonic saline increases blood conductivity transiently, providing a detectable signal. |
| High-Fidelity Tissue Phantoms (Saline tanks with insulating/conducting inclusions) | Physical models for validating FEM forward solutions and GREIT reconstruction performance under controlled conditions. |
| EIDORS (EIT and Diffuse Optical Tomography Reconstruction Software) | Open-source MATLAB/GNU Octave toolkit essential for implementing FEM, GREIT, and TD reconstruction protocols. |
| Medical Imaging Software (e.g., 3D Slicer, ITK-SNAP) | For segmenting anatomical structures from CT/MRI to create subject-specific FEM meshes. |
| ECG Synchronization Unit | Allows cardiac-gating of EIT data, crucial for separating perfusion (cardiac-driven) from ventilation (respiration-driven) signals. |
| Finite Element Meshing Software (e.g., Gmsh, ANSYS, COMSOL) | Generates the discretized volume mesh of the thorax required for solving the forward problem. |
1. Introduction & Thesis Context Within the broader thesis on Electrical Impedance Tomography (EIT) for lung perfusion assessment, the transition from qualitative imaging to robust, reproducible quantification is paramount. This document details the derivation of three core quantitative metrics: the Regional Perfusion Index (RPI), the Cardiac-Related Pulse Wave (CRPW), and Perfusion Delay Maps (PDM). These metrics are foundational for assessing spatial distribution, magnitude, and temporal dynamics of pulmonary perfusion, critical for research in pulmonary embolism, ventilator-induced lung injury, and pharmacokinetic studies in drug development.
2. Quantitative Metrics: Definitions & Data Summary
| Metric | Physiological Correlate | Derivation Method (Typical) | Key Output & Units | Primary Application in Research |
|---|---|---|---|---|
| Regional Perfusion Index (RPI) | Relative blood volume distribution. | Integration of impedance change (ΔZ) during cardiac cycle (systolic phase) within a region-of-interest (ROI). Normalized to global or contralateral lung sum. | Map/Value: Percentage of total perfusion (%) per pixel or ROI. | Quantifying ventilation-perfusion mismatch, assessing lateral asymmetry. |
| Cardiac-Related Pulse Wave (CRPW) | Pulsatile blood flow from right heart ejection. | Band-pass filtering (e.g., 0.5-5 Hz) of EIT time-series to isolate cardiac-frequency components. Often derived via synchronous averaging with ECG gating. | Waveform: Amplitude (ΔZ) vs. time trace. Amplitude: Arbitrary units (a.u.) or mL. | Monitoring stroke volume variation, detecting pulsatile perfusion deficits. |
| Perfusion Delay Maps (PDM) | Temporal dispersion of perfusion onset. | Calculation of time-to-peak or cross-correlation lag between regional CRPW and a reference vascular input signal (e.g., central CRPW or ECG R-wave). | Map: Time delay per pixel (milliseconds, ms). | Identifying embolic regions, characterizing perfusion kinetics in disease. |
3. Experimental Protocols for Metric Derivation
Protocol 3.1: Data Acquisition for Perfusion EIT.
- Subject/Model: Animal model (porcine/rodent) or human subject in supine position.
- EIT Device: A multifrequency EIT system with ECG synchronization capability (e.g., Draeger PulmoVista 500, Swisstom BB2, or custom research system).
- Electrode Belt: 16-32 electrodes placed in a single transverse plane at the 4th-6th intercostal space.
- Reference Signals: Simultaneous recording of ECG (for cardiac gating) and airway pressure/flow (for ventilation phase identification).
- Protocol: A period of stable ventilation (≥1 minute) is recorded at a high frame rate (≥20 fps). For pharmacological studies, a baseline recording is followed by intervention (e.g., drug infusion, embolism induction).
- Data Output: Time-series of thoracic impedance images.
Protocol 3.2: Signal Processing & Derivation of RPI and CRPW.
- Preprocessing: Apply functional EIT reconstruction (e.g., GREIT) to generate dynamic ΔZ images relative to a reference frame (end-expiration).
- Cardiac Component Extraction: Apply a pixel-wise band-pass filter (0.8-3.0 Hz for human; 2-10 Hz for rodent) to the ΔZ time-series to isolate the CRPW.
- RPI Calculation:
- Define ROIs (e.g., left/right lung, quadrants).
- For each cardiac cycle (gated by ECG R-peak), integrate the filtered ΔZ signal (CRPW) over the systolic period (e.g., 200ms post-R-wave) for each pixel.
- Sum the integrated values within an ROI.
- Express as a percentage: RPI(ROI) = (Integrated ΔZ in ROI / Integrated ΔZ in total lung area) × 100%.
- CRPW Waveform Extraction: The filtered, pixel-wise ΔZ signal is the CRPW. For analysis, it is often averaged over multiple cardiac cycles to improve signal-to-noise ratio.
Protocol 3.3: Generation of Perfusion Delay Maps (PDM).
- Reference Signal Selection: Choose a vascular input function. In preclinical models, an invasive flow probe signal may be used. In clinical EIT, use the global CRPW signal from a central vascular region (e.g., heart region in image) or the ECG R-wave.
- Time Lag Calculation: For each pixel's CRPW time-series, compute the cross-correlation function with the reference signal over a defined window (e.g., 5-10 seconds).
- Delay Assignment: Identify the time lag (τ) at which cross-correlation is maximal. This τ value (in ms) is assigned to that pixel.
- Map Generation: Create a 2D parametric image where pixel color represents τ, typically using a jet or viridis colormap. Scale is adjusted to physiological range (e.g., 0-500ms).
4. Visualization of Methodological Workflow
EIT Perfusion Metric Derivation Pipeline
5. The Scientist's Toolkit: Key Research Reagent Solutions
| Item / Reagent | Function in Perfusion EIT Research |
|---|---|
| Hypertonic Saline Bolus (e.g., 5-10% NaCl) | Contrast Agent: Injected intravenously to create a strong, transient impedance decrease, used for validating and calibrating perfusion metrics against a known input. |
| Microsphere (Fluorescent/Radioactive) | Gold Standard Validation: In animal studies, provides absolute quantitative regional blood flow for direct correlation and validation of RPI maps. |
| Pulmonary Vasoconstrictor (e.g., U46619) | Pharmacological Challenge: Used to model pulmonary hypertension or induce controlled changes in perfusion distribution for protocol testing. |
| Thrombin/Clot Forming Agents | Embolism Model: Injected to create pulmonary emboli, generating heterogeneous perfusion delays (PDM) and RPI defects for method evaluation. |
| ECG-Gated Perfusion MRI Contrast Agent (e.g., Gd-based) | Multimodal Validation: Provides an independent, high-resolution imaging modality for spatial and temporal validation of EIT-derived PDM and RPI. |
| Dedicated EIT Research Software (e.g., EIDORS, MATLAB Toolboxes) | Data Analysis: Essential platform for implementing custom reconstruction algorithms, signal filters, and metric calculation protocols. |
Within the broader thesis exploring Electrical Impedance Tomography (EIT) as a pivotal tool for dynamic lung perfusion assessment, this document details specific applications in Acute Respiratory Distress Syndrome (ARDS) and Ventilator-Induced Lung Injury (VILI) research. The core thesis posits that EIT, by enabling continuous, bedside visualization of regional pulmonary perfusion and ventilation, can decode the heterogeneous pathophysiology of ARDS and VILI. This application note provides the experimental framework for employing EIT to assess pulmonary blood flow distribution and recruitment maneuvers' efficacy, central to advancing protective ventilation strategies and evaluating novel therapeutics.
Key Quantitative Findings in EIT Perfusion Assessment
Recent studies utilizing contrast-enhanced EIT (CE-EIT) with saline bolus have quantified the profound perfusion dysregulation in ARDS/VILI models and patients.
Table 1: Quantitative EIT Metrics in ARDS/VILI vs. Healthy Controls
| Metric | ARDS/VILI Model Findings | Healthy/Less Injured State | Measurement Method (EIT) | Primary Implication |
|---|---|---|---|---|
| Pulmonary Blood Flow (PBF) Index | Markedly reduced in dorsal, dependent regions. | More homogeneous PBF distribution. | CE-EIT (Slope of impedance drop). | Indicates hypoperfusion in atelectatic areas. |
| Ventilation/Perfusion (V/Q) Ratio | High heterogeneity; prevalent V/Q mismatch (low V/Q & high V/Q regions). | More uniform V/Q distribution. | Simultaneous EIT-derived ventilation & perfusion maps. | Correlates with impaired gas exchange. |
| Perfusion Shift (%) during PEEP Titration | >20% redistribution of perfusion from non-dependent to dependent zones with optimal PEEP. | <10% redistribution. | Delta of perfusion centroids or regional distribution. | Measures recruitment's hemodynamic impact. |
| Cardiac Cycle-Related Impedance Variation | Amplitude reduced in injured regions; phase delay observed. | Synchronized, uniform amplitude. | Pulsatility analysis from raw EIT data. | Reflects local vascular compliance and resistance. |
Table 2: Impact of Interventions on EIT Perfusion Metrics
| Intervention | Change in Perfusion Distribution | Effect on V/Q Mismatch | Typical Protocol (EIT-Guided) |
|---|---|---|---|
| PEEP Increment (Recruitment) | Redistributes flow to newly recruited dorsal regions. | Can reduce low V/Q areas if recruitment successful. | Stepwise PEEP increase with perfusion/ventilation EIT monitoring. |
| Prone Positioning | Rapid homogenization of perfusion distribution. | Significantly reduces V/Q mismatch. | Continuous EIT monitoring pre-, during, and post-proning. |
| Vasodilator (e.g., iNO) | Increased perfusion to ventilated regions. | Improves matching in targeted areas. | CE-EIT pre- and post-administration to map flow changes. |
| Lung Protective Ventilation | Prevents further deterioration of perfusion heterogeneity. | Mitigates worsening of V/Q mismatch over time. | Using EIT to titrate VT and PEEP to minimize pendelluft and overdistension. |
Detailed Experimental Protocols
Protocol 1: CE-EIT for Baseline Pulmonary Perfusion Mapping in ARDS Model
- Objective: To establish the baseline spatial distribution of pulmonary blood flow in an experimental ARDS/VILI model.
- Materials: See "Scientist's Toolkit" (Section 5).
- Procedure:
- Animal Preparation & EIT Setup: Induce ARDS (e.g., via saline lavage or LPS infusion). Position subject supine. Place EIT belt with 16 electrodes around the thorax at the 4th-5th intercostal space. Connect to functional EIT device (e.g., Dräger PulmoVista 500).
- Stable Ventilation: Initiate volume-controlled ventilation with protective settings (e.g., VT 6 ml/kg, PEEP 5 cmH₂O, FiO₂ 0.5). Stabilize for 10 minutes.
- Hypertonic Saline Bolus Injection: Designate a central venous line for injection. Prepare 10 mL of 5-10% hypertonic saline solution.
- Data Acquisition: Start high-frequency EIT data recording (>40 frames/sec). At end-expiration, rapidly inject (<2 sec) the saline bolus. Continue recording for 30-60 seconds post-injection.
- Data Analysis: Offline, use dedicated software (e.g., MATLAB with EIT toolkit). Calculate the relative impedance change (ΔZ) over time for each pixel. Generate perfusion images based on the indicator dilution principle (peak slope, peak amplitude, or mean transit time). Generate regional time-impedance curves.
Protocol 2: Assessing Recruitment Maneuvers via EIT-Derived V/Q Mapping
- Objective: To evaluate the effect of a PEEP recruitment maneuver on regional ventilation and perfusion matching.
- Procedure:
- Baseline Measurement: Perform Protocol 1 at baseline PEEP (e.g., 5 cmH₂O) to obtain perfusion (Q) map. Simultaneously record a stable ventilation (V) map from tidal impedance variation.
- Recruitment Maneuver: Apply a standardized RM (e.g., stepwise PEEP increase to 15 cmH₂O for 2 minutes, then return to a higher "optimal" PEEP of 10 cmH₂O).
- Post-Recruitment Measurement: After 5 minutes of stabilization at new PEEP (10 cmH₂O), repeat CE-EIT bolus injection and ventilation recording.
- V/Q Analysis: Co-register V and Q images. Calculate a regional V/Q ratio (or index) by dividing normalized V and Q pixel values. Classify pixels as: Normal V/Q, Low V/Q (shunt), High V/Q (dead space).
- Quantification: Calculate the percentage of lung area falling into each V/Q category pre- and post-RM. Calculate the shift in the center of gravity (centroid) of perfusion.
Diagrams (Generated via Graphviz)
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials for EIT Perfusion Research in ARDS/VILI
| Item / Reagent | Function & Rationale | Example / Specification |
|---|---|---|
| Functional EIT System | Core device for data acquisition. Must support high temporal resolution for pulsatile and bolus tracking. | Dräger PulmoVista 500, Swisstom BB2, or custom research systems. |
| 16-Electrode EIT Belt | Sensor array for thoracic impedance measurement. Sizing critical for subject. | Disposable or reusable belts with integrated electrodes. |
| Hypertonic Saline (5-10%) | Intravenous contrast agent for CE-EIT. Creates impedance change detectable in pulmonary circulation. | Sterile, pyrogen-free. Typically 5-10 mL of 5-10% NaCl. |
| Dedicated EIT Analysis Software | For image reconstruction, signal filtering, and quantitative parameter calculation from raw EIT data. | MATLAB with EIT toolkits (EIDORS), Dräger EIT Data Analysis Tool, or custom software. |
| Mechanical Ventilator (Research) | Provides precise, programmable control of VT, PEEP, and FiO2 for protocol standardization. | FlexiVent, SCIREQ/EMKA systems, or clinical ventilators in lab mode. |
| ARDS Induction Agent | To create a reproducible injury model with heterogeneity mimicking human ARDS. | Lipopolysaccharide (LPS), saline lavage, oleic acid. |
| Hemodynamic Monitor | To correlate EIT perfusion data with global metrics (cardiac output, blood pressure). | Pulmonary artery catheter or transpulmonary thermodilution system. |
| Animal or Human Research Platform | Preclinical: Rodent or large animal (porcine) models. Clinical: ICU patients with ARDS. | IACUC/ethics approval mandatory. Patient informed consent for clinical studies. |
Within the broader thesis on Electrical Impedance Tomography (EIT) for lung perfusion assessment, this document establishes its pivotal role in modern drug development. EIT’s capacity for real-time, bedside, and radiation-free imaging of regional lung perfusion and ventilation provides a unique functional endpoint for evaluating novel therapeutics. This application note details specific protocols for deploying EIT in clinical trials for pulmonary vasodilators, pulmonary hypertension (PH) therapies, and oncology drugs with cardiopulmonary toxicity profiles.
Table 1: EIT-Derived Parameters in Drug Development Trials
| Therapeutic Area | Primary EIT Endpoint | Typical Measurement | Reported Quantitative Change (Post-Therapy) | Clinical Correlation |
|---|---|---|---|---|
| Acute Pulmonary Vasodilators (e.g., inhaled NO) | Perfusion Shift (ΔQ) | Redistribution from well-ventilated to poorly ventilated lung areas | ΔQ = 10-25% (toward dorsal regions in ARDS) | Improved V/Q matching, PaO₂/FiO₂ ratio increase |
| Chronic PH Therapies (e.g., PDE5i, sGC stimulators) | Pulmonary Perfusion Index (PPI) | Ratio of cardiac-related impedance change in lung region to global amplitude | PPI increase of 15-30% in hypoperfused zones | Correlates with 6MWD improvement, reduced mPAP |
| Oncology Trials (ICI pneumonitis) | Regional Ventilation-Perfusion (V/Q) Mismatch | Spatial correlation map of ventilation & perfusion distributions | V/Q mismatch index decrease > 20% with steroids | Resolution of immune-related adverse events (irAEs) |
| Oncology Trials (Chemotherapy) | Global Lung Perfusion (GLP) | Integral of impedance cardiac curve over both lungs | GLP reduction of 8-15% (e.g., post-Bleomycin) | Early detection of drug-induced vascular injury |
Experimental Protocols
Protocol 3.1: Evaluating Acute Pulmonary Vasodilator Response Aim: To quantify the rapid redistribution of pulmonary blood flow following administration of an inhaled vasodilator. Materials: See Scientist's Toolkit. Procedure:
- Position EIT belt at 5th-6th intercostal space. Secure electrodes.
- Record baseline EIT data for 5 minutes (tidal breathing).
- Administer investigational vasodilator via standardized nebulizer/inhaler.
- Initiate continuous EIT recording starting 30 seconds pre-administration and continue for 20 minutes post-administration.
- Data Analysis: Calculate the Perfusion Shift Index (PSI). Using cardiac-gated EIT images, identify regions of interest (ROI) in ventral and dorsal lung halves. PSI = (ΔZdorsal - ΔZventral) / (ΔZdorsal + ΔZventral), where ΔZ is the impedance amplitude synchronized with the ECG R-wave.
- Compare PSI at baseline to the average PSI from minutes 5-15 post-administration.
Protocol 3.2: Longitudinal Monitoring in Pulmonary Hypertension Trials Aim: To assess the chronic effect of PH-targeted therapy on regional lung perfusion homogeneity. Materials: See Scientist's Toolkit. Procedure:
- Perform EIT at screening (Day 0) and at predefined intervals (Weeks 4, 12, 24).
- During each session, record 10 minutes of stable data in a supine position, including a 5-minute period of controlled breathing (tidal volume 8-10 mL/kg).
- Data Analysis: Compute the Pulmonary Perfusion Distribution (PPD) map. Generate functional EIT images of perfusion via pixel-wise Fast Fourier Transform of the cardiac frequency band.
- Calculate the Coefficient of Variation (CV) of Perfusion across all lung pixels as a measure of homogeneity. A decreasing CV indicates more uniform perfusion.
- Statistically compare CV and global perfusion amplitude between study time points.
Protocol 3.3: Assessing Cardiopulmonary Toxicity in Oncology Trials Aim: To detect and monitor ventilation-perfusion mismatch due to drug-induced pneumonitis or vascular injury. Materials: See Scientist's Toolkit. Procedure:
- Baseline EIT scan prior to initiation of oncology therapy (e.g., checkpoint inhibitors).
- Serial scans before each treatment cycle (e.g., every 2-3 weeks).
- Recording: Acquire data during normal breathing for 5 minutes.
- Data Analysis: Generate separate ventilation (V) and perfusion (Q) EIT images via frequency filtering (ventilation: 0.1-0.5 Hz; perfusion: cardiac frequency).
- Compute a V/Q Match Map by calculating the linear correlation coefficient (R) between temporal V and Q signals for each pixel over 1-minute epochs. Normal lung R > 0.8.
- Flag regions with R < 0.6 for further investigation. Quantify the percentage of lung area with significant V/Q mismatch (R < 0.6).
Signaling Pathways & Workflow Visualizations
Diagram Title: Drug Action to EIT Signal Pathway
Diagram Title: EIT Data Processing Workflow for V/Q Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for EIT in Drug Development Trials
| Item | Function & Rationale |
|---|---|
| 32-Electrode EIT Belt & Data Acquisition System | Standardized hardware for consistent thoracic bioimpedance measurement. Provides raw voltage data for image reconstruction. |
| GREIT Image Reconstruction Software | Consensus algorithm for transforming impedance data into 2D cross-sectional functional lung images. Ensures reproducibility. |
| ECG Synchronization Module | Critical for gating the impedance signal to the cardiac cycle, enabling separation of perfusion from ventilation signals. |
| Controlled Breathing Metronome | Standardizes tidal volume and rate during scans to minimize ventilation-driven perfusion signal variability. |
| Dedicated EIT Analysis Suite (e.g., EITdiag) | Software for calculating advanced parameters (PPI, V/Q mismatch maps, CV of perfusion) from reconstructed images. |
| High-Biocompatibility Electrode Gel | Ensures stable skin-electrode contact impedance, reducing motion artifact and signal drift during prolonged recordings. |
Overcoming Challenges in EIT Perfusion: Artifact Mitigation and Signal Optimization
Electrical Impedance Tomography (EIT) is a promising non-invasive, radiation-free modality for dynamic lung perfusion imaging. However, the fidelity of perfusion-related impedance changes (typically <5% of baseline) is critically undermined by concurrent, larger-magnitude artifacts. Robust artifact identification and correction form the foundational thesis that accurate functional EIT, separating perfusion from ventilation and confounding noise, is achievable and essential for quantitative assessment in critical care and pharmaceutical trials.
Artifact Characterization and Quantitative Impact
EIT data for lung perfusion is reconstructed from boundary voltage measurements ( V(t) ). The measured signal ( Vm(t) ) can be modeled as: [ Vm(t) = Vp(t) + Vv(t) + Vc(t) + V{mot}(t) + V{cc}(t) + \eta ] where ( Vp ) is perfusion, ( Vv ) is ventilation, ( Vc ) is cardiac artifact, ( V{mot} ) is motion, ( V{cc} ) is electrode contact noise, and ( \eta ) is instrumental noise.
Table 1: Characteristics of Key Artifacts in Lung Perfusion EIT
| Artifact Type | Typical Frequency Band | Amplitude (Relative to Perfusion) | Spatial Pattern | Primary Source |
|---|---|---|---|---|
| Cardiac Activity | 1-3 Hz | 5x - 20x | Focal, ventral/central, heart-lung border | Pulsatile heart movement & blood volume changes. |
| Patient Motion | 0 - 0.5 Hz | 10x - 100x | Global or regional shift | Coughing, posture change, respiratory effort. |
| Electrode Contact | DC - Broadband | Highly variable (can saturate signal) | Localized to specific electrode pairs. | Poor contact, sweat, cable movement. |
| True Lung Perfusion | Synchronous with cardiac cycle (~1-2 Hz) | 1x (Reference) | Gravitational, ventilation-matched. | Pulmonary blood flow. |
| Ventilation | 0.1 - 0.5 Hz | 10x - 50x | Global, gravity-dependent. | Air inflow/outflow. |
Experimental Protocols for Artifact Assessment and Mitigation
Protocol 3.1: Isolating Cardiac Artifact in a Porcine Model
Objective: To characterize and separate cardiac-induced impedance changes from pulmonary perfusion signals. Materials: Animal EIT system (e.g., Dräger PulmoVista 500 or custom research system), 32-electrode thoracic belt, ventilator, ECG monitor, invasive blood pressure line. Procedure:
- Instrumentation: Anesthetize and mechanically ventilate a porcine subject. Place EIT belt at the 5th intercostal space. Connect ECG and arterial line.
- Data Acquisition: Acquire synchronized EIT raw data (frame rate ≥ 40 Hz), ECG, arterial pressure, and airway pressure for 5 minutes under stable hemodynamics.
- Intervention – Perfusion Modulation: Infuse a vasoactive drug (e.g., adenosine, 200 µg/kg/min IV) to alter pulmonary perfusion while cardiac rhythm remains stable.
- Signal Processing: Apply ECG-gated ensemble averaging over 30-second epochs. The averaged signal represents the synchronous cardiac artifact. Subtract this from the raw signal in the frequency domain.
- Validation: Compare the power in the cardiac band (1-3 Hz) before and after subtraction. Correlate the remaining DC/low-frequency perfusion signal with changes in cardiac output from the arterial pressure waveform.
Protocol 3.2: Quantifying Motion Artifact During Simulated Drug Administration
Objective: To evaluate motion artifact induced by simulated patient movement or coughing during a perfusion monitoring scenario. Materials: Human volunteer, research EIT system, 32-electrode belt, spirometer. Procedure:
- Baseline: Record 2 minutes of stable tidal breathing in a supine position.
- Induced Motion: Introduce deliberate, timed actions: a) deep sigh, b) cough, c) lateral shoulder movement.
- Analysis: Use the Global Inhomogeneity (GI) index or frame-by-frame impedance change centroid to detect motion-corrupted frames. Apply a motion detection algorithm based on the singular value decomposition (SVD) of the temporal signal matrix. Frames with a norm beyond 3 SD of the baseline mean are flagged.
- Correction: Implement a template-matching or data interpolation method to replace corrupted frames using adjacent, stable data.
Protocol 3.3: Electrode Contact Impedance Monitoring Protocol
Objective: To proactively identify and correct for electrode contact loss in long-term monitoring. Materials: Multi-frequency EIT system capable of measuring electrode-skin impedance (e.g., >10 kHz). Procedure:
- Pre-application: Measure baseline contact impedance for all electrodes (target: < 2 kΩ at 10 kHz).
- Continuous Monitoring: Interleave perfusion imaging frames (e.g., at 50 kHz) with contact impedance check frames (at 100 kHz).
- Thresholding: Flag any electrode where impedance changes >50% from its own baseline or absolute value exceeds 5 kΩ.
- Software Correction: In reconstruction, apply a weighting matrix to de-emphasize voltage measurements from flagged electrodes or use a reference frame with good contact for differential imaging.
Visualization of Correction Workflows
Title: ECG-Gated Cardiac Artifact Correction
Title: Motion Artifact Detection and Frame Management
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for EIT Perfusion Artifact Research
| Item | Function & Rationale |
|---|---|
| Multi-Frequency EIT System (e.g., Swisstom BB2, Draeger PV500) | Enables separation of tissue properties (e.g., perfusion vs. ventilation) via frequency response and contact impedance monitoring. |
| Medical-Grade ECG Amplifier | Provides precise R-wave timing for synchronous averaging and gating of cardiac artifact. |
| High-Biocompatibility Electrode Gel (e.g., Sigma Gel) | Maintains stable, low electrode-skin impedance over long durations, minimizing contact noise. |
| Programmable Syringe Pump (e.g., Harvard Apparatus) | For precise, timed administration of vasoactive drugs (e.g., adenosine, noradrenaline) to modulate perfusion in validation studies. |
| Digital Physiological Recorder (e.g., ADInstruments PowerLab) | Synchronizes EIT data with ECG, blood pressure, airway pressure, and flow for multimodal artifact analysis. |
| Calibrated Motion Platform | For introducing controlled, repeatable motion artifacts (tilts, shifts) to test correction algorithms. |
| Thoracic Phantom with Pulsatile Perfusion | Physical model containing conductive compartments to simulate heart, lungs, and pulsatile fluid flow for controlled artifact studies. |
| Open-Source EIT Toolkit (e.g, EIDORS) | Software library providing standard reconstruction algorithms and a framework for implementing novel artifact correction methods. |
Strategies for Optimizing Signal-to-Noise Ratio in Low-Flow States
Electrical Impedance Tomography (EIT) is a non-invasive, radiation-free imaging modality uniquely suited for dynamic, bedside monitoring of regional lung perfusion. Within the broader thesis on EIT for lung perfusion assessment, a central challenge is the reliable detection and quantification of perfusion signals, particularly under low-flow states (e.g., cardiogenic shock, PEEP-induced hemodynamic compromise, early-stage pulmonary embolism). In these conditions, the perfusion-related impedance change (ΔZ) becomes diminutive, approaching the system's noise floor. This application note details targeted strategies to optimize the Signal-to-Noise Ratio (SNR) for robust perfusion EIT in low-flow scenarios.
Key Challenge: SNR in Perfusion EIT
The primary signal for pulsatile perfusion is the cardiac-synchronous impedance variation, typically <0.5% of the baseline impedance. In low-flow states, this variation can drop below 0.1%. Noise sources include:
- Physiological Noise: Cardiac, respiratory (for ventilation-synchronized protocols), and motion artifacts.
- Electronic Noise: Electrode contact impedance fluctuations, amplifier noise, and thermal Johnson-Nyquist noise.
- Algorithmic Noise: Reconstruction artifacts and regularization errors.
Instrumentation & Data Acquisition Optimization
Protocol 1.1: High-Precision, Phase-Synchronous Data Acquisition
Objective: Minimize electronic and sampling noise during raw voltage measurement.
Detailed Methodology:
- Electrode Preparation: Use Ag/AgCl electrodes with hydrogel. Abrade skin gently to achieve stable contact impedance <2 kΩ at 50 kHz. Apply a constant, low-pressure bandage.
- EIT Device Calibration: Prior to measurement, perform a reference calibration using precision resistors within the expected impedance range of the thorax (20-150 Ω). Use a 4-terminal (tetrapolar) measurement technique for each drive pair.
- Acquisition Parameters:
- Current Injection: Utilize a high-stability, constant current source. Increase current amplitude to the maximum permissible under relevant safety standards (typically 5 mA RMS for thoracic applications) to maximize signal strength.
- Averaging: Implement real-time frame averaging. Acquire 10-20 successive frames at the same phase of the cardiac/respiratory cycle (using ECG/gating) and average them before reconstruction.
- Sampling Rate: Sample at a minimum of 100 frames/second to adequately capture the cardiac-frequency impedance waveform and allow for subsequent digital filtering.
- Filtering: Apply a hardware-based bandpass filter (0.5 Hz - 10 Hz) to the demodulated voltage signals to pass cardiac frequencies and suppress baseline drift and high-frequency noise.
Table 1: Optimized EIT Acquisition Parameters for Low-Flow Perfusion
| Parameter | Standard Setting | Optimized for Low-Flow | Rationale |
|---|---|---|---|
| Current Amplitude | 1-3 mA RMS | 5 mA RMS (IEC 60601 limit) | Maximizes measured voltage (ΔV) for a given ΔZ. |
| Frame Rate | 50 fps | 100+ fps | Prevents aliasing and allows better cardiac cycle resolution. |
| Averaging (Frames) | None or 2-3 | 10-20 (phase-synced) | Directly improves SNR by √N. Phase-syncing prevents blurring. |
| BP Filter (Demod.) | 0.1 - 45 Hz | 0.5 - 10 Hz | Attenuates respiratory drift (low) and high-frequency electronic noise (high). |
| Contact Impedance | <5 kΩ | <2 kΩ | Reduces thermal noise and injection current instability. |
Signal Processing & Gating Strategies
Protocol 2.1: Dual-Gated, Model-Based Filtering
Objective: Isolate the low-amplitude cardiac-impedance signal from dominant ventilation and motion artifacts.
Detailed Methodology:
- Synchronized Data Collection: Acquire continuous EIT data synchronized with ECG (for cardiac R-wave) and airway pressure/flow (for respiratory phase).
- Ventilation Gating:
- Reconstruct dynamic EIT images for ventilation (using standard 50 kHz frequency).
- Identify end-expiration phases (points of minimal airway pressure variance over 3 cycles).
- Segment the continuous data stream into blocks corresponding to these end-expiration phases (typically 200-500 ms windows).
- Cardiac-Synchronous Averaging within Gated Windows:
- Within each end-expiration window, align all data points to the R-peak of the ECG.
- Average the impedance values from corresponding time points across 30-60 consecutive, aligned cardiac cycles. This reinforces the repetitive perfusion signal while averaging out random noise.
- Model-Based Subtraction: Use a physiologically-informed model (e.g., fitting a sinusoidal or morphological template to the averaged cardiac waveform) to define the "pure" perfusion signal. Subtract this from the unaveraged data in the gated window to estimate and characterize residual noise.
Title: Dual-Gated Signal Processing Workflow
Reconstruction Algorithm Enhancements
Protocol 3.1: Spatiotemporal Priors in Image Reconstruction
Objective: Incorporate physiological knowledge into the inverse problem to stabilize image reconstruction and suppress artifacts in low-SNR conditions.
Detailed Methodology:
- Forward Model: Generate a finite element model (FEM) of the thorax from a CT scan or a population-averaged atlas. Ensure accurate electrode positioning.
- Temporal Regularization (Kalman Filter Framework):
- Formulate the EIT image sequence as a state-space model:
x_k = A x_{k-1} + w_k(state evolution),y_k = J x_k + v_k(measurement). - Here,
xis the conductivity change vector,yis the voltage difference,Jis the Jacobian,wandvare process and measurement noise. - Define the state transition matrix
Ato enforce temporal smoothness consistent with expected perfusion kinetics (e.g., a Gaussian kernel over ~100 ms).
- Formulate the EIT image sequence as a state-space model:
- Spatial Prior Integration:
- Create a spatial weighting matrix
Rbased on a probability map of lung tissue from the FEM or co-registered CT. - Penalize conductivity changes outside the lung region. This can be implemented as a Laplacian or Gaussian prior in a
Tikhonovregularization framework:x̂ = argmin(||Jx - y||² + λ²||R(x - x_prior)||²).
- Create a spatial weighting matrix
- Noise-Covariance Weighting: Estimate the noise covariance matrix
Σ_nfrom baseline, signal-free data. Use its inverse to weight the data fidelity term in reconstruction, de-emphasizing noisier measurement channels.
Title: EIT Reconstruction with Physiological Priors
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Low-Flow Perfusion EIT Experiments
| Item & Example Source | Function in Low-Flow SNR Optimization |
|---|---|
| High-Precision EIT System (e.g., Swisstom BB2, Draeger PulmoVista 500 with research access) | Provides stable, programmable current injection, high dynamic range voltage measurement, and synchronized aux input (ECG/resp). |
| Ag/AgCl Electrodes with Adhesive Hydrogel (e.g., BlueSensor, Ambu) | Ensures stable, low-impedance skin contact, minimizing interface noise and drift. |
| ECG Gating Module (e.g., Biopac MP160 ECG module) | Provides precise R-wave detection for cardiac-synchronous averaging and gating. |
| Research Spirometer/Pneumotachograph (e.g., CO2SMO+ Monitor) | Delivers accurate respiratory phase signal for ventilation gating. |
| Finite Element Modeling Software (e.g., EIDORS, SIM4LIFE) | Enables creation of anatomical thoracic models and simulation of sensitivity distributions for advanced reconstruction. |
| Physiological Saline (0.9% NaCl) | Used for skin preparation to lower and stabilize contact impedance before electrode application. |
| Customizable EIT Data Processing Suite (e.g., MATLAB with EIDORS, Python SciPy) | Essential for implementing dual-gating, ensemble averaging, and model-based filtering algorithms. |
| Flow/Perfusion Phantom (e.g., custom agar sphere with oscillating conductive fluid) | Allows for validation of SNR improvements under controlled, low-flow simulated conditions. |
Optimizing SNR for lung perfusion EIT in low-flow states requires a multi-layered approach integrating hardware, signal processing, and reconstruction. By maximizing signal strength through safe current injection, employing dual-gated ensemble averaging to isolate the cardiac component, and incorporating spatiotemporal physiological priors during image reconstruction, researchers can significantly enhance the detectability of low-amplitude perfusion signals. These protocols provide a foundational methodology for advancing the thesis objective of making EIT a reliable quantitative tool for assessing pulmonary perfusion deficits in critical care and drug development research.
Within the broader thesis on Electrical Impedance Tomography (EIT) for lung perfusion assessment, precise handling of contrast agent kinetics is paramount. The goal is to develop robust, quantitative EIT protocols to map regional pulmonary blood flow (rPBF). This requires optimizing intravenous bolus delivery—a critical factor influencing the temporal resolution and signal-to-noise ratio of the impedance-time curves. This document details application notes and experimental protocols for investigating bolus timing, the use of saline versus hypertonic solutions as conductive contrast agents, and standardized injection methodologies.
Core Principles of Contrast Kinetics in EIT
In EIT-based perfusion assessment, a bolus of a conductive solution (e.g., hypertonic saline) is injected intravenously. The resulting decrease in thoracic electrical impedance is measured. The first-pass kinetics of this bolus through the pulmonary circulation are used to calculate perfusion indices. Key parameters include time-to-peak (TTP), mean transit time (MTT), and peak amplitude. The shape and magnitude of the impedance curve are highly dependent on injection protocol.
Application Notes & Comparative Data
Table 1: Comparative Properties of Contrast Solutions for EIT
| Solution | Typical Concentration | Conductivity (Relative to Blood) | Primary Mechanism | Key Advantages | Key Disadvantages |
|---|---|---|---|---|---|
| Normal Saline (0.9% NaCl) | 0.9% w/v | ~1.5x | Increases ionic strength, reduces resistivity. | Physiological, safe, readily available. | Smaller impedance change, faster dispersion. |
| Hypertonic Saline | 5-10% NaCl | 6-10x | Significant increase in Na+ and Cl- concentration, markedly lowers resistivity. | High signal amplitude, improved SNR. | Risk of venous irritation, requires ethical approval. |
| Dextrose 5% (Hypotonic) | 5% w/v | <1x (Lower) | Creates transient hypo-conductivity bolus. | Can be used as a negative contrast. | Weaker signal, complex kinetics. |
Table 2: Impact of Injection Protocol on Bolus Characteristics
| Protocol Parameter | Standard Value (Typical) | Effect on Bolus Shape | Implications for EIT Perfusion Analysis |
|---|---|---|---|
| Injection Volume | 5-10 mL | Larger volume → Broader peak, higher amplitude. | May violate "impulse input" assumption; requires correction for MTT. |
| Injection Rate | 5-10 mL/s | Faster rate → Sharper, narrower peak, higher amplitude. | Improves temporal resolution, better defines TTP. |
| Bolus Timing (Sync) | Start of expiration | Consistent cardiorespiratory phase → Reduced variability. | Essential for reproducible region-of-interest analysis. |
| Flush Volume (Saline) | 20-30 mL | Ensures complete contrast delivery, sharpens bolus tail. | Prevents trailing, improves estimation of MTT. |
Detailed Experimental Protocols
Protocol 1: Optimizing Bolus Timing and Respiratory Synchronization
Objective: To determine the optimal injection trigger point within the respiratory cycle for minimal variance in TTP. Materials: See "The Scientist's Toolkit" below. Method:
- Connect EIT device, ventilator, and physiological monitor (ECG) to a synchronous data acquisition system.
- Set ventilator to a standardized volume-controlled mode (e.g., tidal volume 6-8 mL/kg).
- Define three injection trigger points: a) Start of Inspiration, b) Start of Expiration, c) Mid-Expiration.
- For each condition (n≥5 repetitions), inject a standardized 10 mL bolus of 5% NaCl at 10 mL/s, followed by a 25 mL saline flush at the same rate.
- Record EIT data at 50 frames/sec for 60 seconds post-injection.
- Analysis: For a central lung region of interest, calculate TTP and peak amplitude. Perform ANOVA across trigger points to assess variance.
Protocol 2: Comparing Saline vs. Hypertonic Saline Bolus Kinetics
Objective: To quantitatively compare the signal characteristics and kinetic profiles of 0.9% vs. 5% NaCl boluses. Method:
- Prepare isotonic (0.9%) and hypertonic (5.0%) NaCl solutions at room temperature.
- In a randomized, crossover design, administer boluses (10 mL at 10 mL/s) of each solution in the same animal/human subject (with appropriate washout and ethical approval).
- Maintain identical injection timing (start of expiration), flush volume (25 mL), and ventilator settings.
- Acquire EIT and central venous pressure (if available) data.
- Analysis:
- Calculate the peak impedance change (ΔZ) for each bolus.
- Derive the Signal-to-Noise Ratio (SNR): Peak ΔZ / baseline noise (SD of pre-injection signal).
- Fit a gamma-variate function to the first-pass curve to extract MTT and TTP.
- Compare parameters using paired t-tests.
Protocol 3: Standardized Injection Protocol for Multi-Center Studies
Objective: To establish a reproducible injection workflow for longitudinal or multi-center EIT perfusion research. Method:
- Preparation: Use a dual-syringe power injector. Load Syringe 1 with contrast agent (e.g., 10 mL 5% NaCl). Load Syringe 2 with flush solution (30 mL 0.9% NaCl).
- Line Priming: Ensure the entire intravenous line from injector to catheter tip is primed with contrast agent to prevent dead-space dilution.
- Synchronization: Program injector to receive an external trigger signal synchronized with the start of expiration from the ventilator.
- Injection Sequence: Upon trigger, execute: a) Contrast bolus: 10 mL at 10 mL/s. b) Immediate follow-on flush: 30 mL at 10 mL/s.
- Data Marking: The injector should send a TTL pulse to the EIT device at the exact start of contrast injection.
- Validation: Verify bolus shape consistency by reviewing the global impedance time curve; the rise should be sharp (<2 seconds to peak).
Visualization of Protocols and Relationships
EIT Contrast Optimization Workflow
Standardized Injection & Signal Pathway
The Scientist's Toolkit: Key Research Reagent Solutions & Materials
| Item | Specification/Concentration | Primary Function in EIT Perfusion Studies |
|---|---|---|
| Hypertonic Saline Solution | 5.0% or 7.5% Sodium Chloride (NaCl), sterile, pyrogen-free. | High-conductivity contrast agent. Induces a measurable decrease in thoracic impedance. |
| Normal Saline (Flush) | 0.9% Sodium Chloride, sterile. | To flush contrast agent from catheters and central veins, ensuring complete bolus delivery and sharpening kinetics. |
| Dual-Syringe Power Injector | Programmable for rate/volume, with external trigger input. | Ensures highly reproducible injection profiles (rate, volume) and synchronization with ventilator/ECG. |
| Central Venous Catheter | Multi-lumen, placed in superior vena cava or right atrium. | Provides a reliable, high-flow route for bolus injection close to the heart, minimizing dispersion. |
| EIT Data Acquisition System | High-frame-rate (>40 fps), with analog/digital input for triggers. | Records dynamic impedance changes across the thorax. Synchronization with injector is critical. |
| Physiological Monitor | With ECG and airway pressure waveform outputs. | Provides signals for respiratory and cardiac cycle synchronization of the injection trigger. |
| Data Synchronization Unit | Hardware (e.g., Biopac) or software (LabVIEW) to align injector, EIT, and ventilator timestamps. | Creates a unified timeline for precise kinetic analysis, aligning injection start with frame #0. |
| Gamma-Variate Function Fitting Software | Custom (MATLAB, Python) or commercial analysis suite. | Mathematical modeling of the first-pass bolus curve to extract MTT, TTP, and peak height while rejecting recirculation artifact. |
Within the broader thesis on Electrical Impedance Tomography (EIT) for lung perfusion assessment, optimizing spatial resolution and boundary definition is paramount. These parameters directly influence the ability to distinguish regional pulmonary blood flow, detect perfusion defects (e.g., in pulmonary embolism), and monitor therapeutic interventions in drug development. The number of electrodes and their spatial arrangement on the thorax are the primary hardware factors determining the spatial fidelity of the reconstructed EIT images. This application note details the principles, quantitative comparisons, and experimental protocols for electrode array design to enhance EIT performance in pulmonary perfusion studies.
Core Principles and Quantitative Data
The spatial resolution of EIT is inherently limited and non-uniform, being highest near the electrodes and degrading towards the center. Increasing electrode number improves the number of independent measurements (N = E*(E-3)/2 for adjacent drive patterns with E electrodes), which generally enhances resolution but is subject to diminishing returns and practical limitations.
Table 1: Impact of Electrode Number on EIT Measurement Parameters
| Electrode Number (E) | Independent Measurements (Adjacent Pattern) | Typical Spatial Resolution (at boundary) | Common Array Geometries for Thorax | Typical Application in Lung EIT |
|---|---|---|---|---|
| 16 | 104 | ~10-15% of diameter | Single plane, equidistant belt | Basic ventilation monitoring |
| 32 | 464 | ~7-10% of diameter | Single plane, equidistant belt | Standard perfusion/ventilation research |
| 64 | 1952 | ~5-7% of diameter | Dual-plane, high-density strips | High-resolution perfusion mapping |
| 128 (or 2x64) | 8000 (approx.) | ~3-5% of diameter | Multiple planes, textile arrays | Advanced mechanistic studies |
Table 2: Comparative Analysis of Electrode Array Designs for Thoracic EIT
| Array Design | Electrode Layout | Advantages for Perfusion Assessment | Limitations |
|---|---|---|---|
| Single Plane Belt | Equidistant, same transverse plane | Simple, reproducible, clinical standard | Loss of 3D information, sensitivity to belt position |
| Dual/Multi-Plane Belt | Two or more parallel rings of electrodes | Captures cranio-caudal perfusion gradients, better 3D definition | More complex setup, increased inter-wire crosstalk risk |
| Textile/Grid Array | Electrodes embedded in a flexible fabric grid | Conforms to anatomy, allows high electrode density, stable positioning | Complex manufacturing, individual electrode contact verification needed |
| Anatomically Shaped | Electrodes placed at anatomical landmarks (e.g., ICS) | Potentially better inter-subject comparability | Less reproducible, requires skilled placement |
Detailed Experimental Protocols
Protocol 1: Systematic Evaluation of Electrode Number on Boundary Definition
Objective: To quantify the improvement in boundary definition and sharpness of a perfusion-like conductivity contrast using EIT arrays with differing electrode counts.
Materials: See "The Scientist's Toolkit" below. Phantom: A cylindrical tank (diameter 30 cm) with a saline background (0.9% NaCl, ~100 Ωcm). A non-conductive cylindrical insert (diameter 8 cm) simulates a perfusion defect. Electrode Arrays: Interchangeable belts with 16, 32, and 64 equally spaced Ag/AgCl electrodes. EIT System: A high-performance, multifrequency EIT system (e.g., Swisstom BB2, Draeger PulmoVista 500, or custom research system).
Procedure:
- Setup: Place the phantom on a non-conductive surface. Fill with saline to a level above the electrode plane.
- Array Mounting: Securely mount the 16-electrode belt around the phantom at its mid-height. Ensure all electrodes have stable contact impedance (< 2 kΩ at 10 kHz).
- Data Acquisition: Using adjacent current injection pattern, collect frame of reference data at 50 kHz (relevant for perfusion). Introduce the non-conductive target. Collect perturbation data.
- Reconstruction: Reconstruct images using a 2D finite element model (FEM) of the tank and a time-difference algorithm (e.g., GREIT).
- Analysis: Calculate the Boundary Sharpness Index (BSI): Measure the spatial gradient at the edge of the reconstructed target. Also, calculate the Position Error of the target centroid.
- Repetition: Repeat steps 2-5 for the 32- and 64-electrode arrays using the same phantom setup and reconstruction parameters (e.g., regularization strength normalized to measurement number).
- Statistical Comparison: Perform repeated-measures ANOVA on BSI and Position Error across the three array types (n≥5 trials each).
Protocol 2: Validation of Dual-Plane Array for 3D Perfusion Defect Localization
Objective: To demonstrate the superior volumetric localization of a simulated perfusion defect using a dual-plane array versus a single-plane array.
Materials: As in Protocol 1, plus a dual-plane EIT system and a spherical non-conductive target (diameter 5 cm). Procedure:
- Single-Plane Setup: Mount a 32-electrode single belt. Position the spherical target at a known 3D coordinate (x,y,z) off the electrode plane.
- Acquisition & Reconstruction: Collect data and reconstruct a 2D image slice. Note the apparent location and smearing of the target.
- Dual-Plane Setup: Mount two 32-electrode belts (or one integrated dual-plane array) with a known vertical separation (e.g., 8 cm).
- 3D Data Acquisition: Collect data from both planes simultaneously.
- 3D Reconstruction: Reconstruct a 3D volumetric image using a 3D FEM.
- Analysis: Compare the localized 3D coordinate of the target from the dual-plane EIT to its known position. Quantify the Localization Error in 3D. Compare the contrast-to-noise ratio (CNR) of the target in the correct plane vs. the erroneous single-plane reconstruction.
Visualization of Concepts and Workflows
Diagram 1: The Determinants of EIT Image Quality
Diagram 2: Electrode Array Design Selection Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item & Example Product | Specification/Function in EIT Array Research |
|---|---|
| Ag/AgCl Electrodes (e.g., Viasys Healthcare, Kendall) | Low-impedance, non-polarizable contact. Essential for stable current injection and voltage measurement. |
| Electrode Belts (Swisstom, Dräger) | Flexible belts with integrated electrodes. Provide reproducible geometry. Key variable in studies. |
| Saline Solution (0.9% NaCl) | Standard conducting medium for tank phantoms. Conductivity (~1.5 S/m) mimics thoracic background. |
| EIT Phantom Tank (Custom acrylic) | Geometric container for validation experiments. Allows precise placement of targets. |
| Conductive/Non-conductive Targets (e.g., plastic, agar spheres) | Simulate perfusion anomalies (e.g., clots, hypo-perfused regions) in phantom studies. |
| Multi-channel EIT System (e.g., Swisstom BB2, Timpel Enlight) | Research-grade system capable of supporting high electrode counts and multi-frequency measurements. |
| Electrode Impedance Tester (Custom or commercial) | Verifies skin-contact or phantom-contact impedance pre-experiment. Critical for data quality. |
| 3D FEM Mesh Generator (EIDORS, MATLAB PDE Toolbox) | Software to create accurate computational models of the thorax for image reconstruction. |
| Bio-compatible Adhesive Gel (Ten20, SignaGel) | Ensures stable electrode-skin contact in human studies, reducing motion artifact. |
1. Introduction: Context in EIT for Lung Perfusion Assessment
Within the broader thesis on Electrical Impedance Tomography (EIT) for assessing lung perfusion, robust data processing is critical. Artifacts from cardiac motion, ventilation, and instrument instability can obscure the perfusion signal. This application note details protocols to mitigate three central pitfalls: inappropriate filter selection, unmanaged baseline drift, and ambiguous ROI definition, which directly impact the accuracy of perfusion indices like pulmonary blood flow (PBF) and pulmonary blood volume (PBV) derived from EIT.
2. Quantitative Data Summary
Table 1: Impact of Low-Pass Filter Cut-off on Perfusion Signal Integrity
| Cut-off Frequency (Hz) | Cardiac Artifact Residual (%) | Perfusion SNR (dB) | Recommended Application |
|---|---|---|---|
| 1.5 | 45 | 15.2 | Not recommended |
| 1.0 | 22 | 18.5 | Initial exploration |
| 0.75 | 8 | 22.1 | Standard perfusion |
| 0.5 | 2 | 20.8 | High cardiac noise |
| 0.25 | <1 | 17.3 | Risk of signal loss |
Table 2: Comparison of Baseline Drift Correction Methods for Bolus-Tracking EIT
| Method | Algorithm Basis | Computational Load | Robustness to Sudden Changes | Suitability for Long Time-Series |
|---|---|---|---|---|
| Polynomial Detrending | Least-squares polynomial fit | Low | Low | Moderate |
| Moving Average | Linear filter | Very Low | Moderate | High |
| Empirical Mode Decomposition (EMD) | Adaptive signal decomposition | High | High | High |
| High-Pass Filter (0.02 Hz) | IIR/FIR filter | Moderate | Moderate | Low (can distort bolus shape) |
3. Experimental Protocols
Protocol 3.1: Optimized Filter Selection for EIT-Based Perfusion Imaging Objective: To isolate the impedance change due to perfusion (typically 0.5-1.0 Hz) from cardiac (1-2 Hz) and ventilatory (0.1-0.3 Hz) signals. Materials: EIT data set (e.g., 120s recording during indicator bolus injection), processing software (e.g., MATLAB, Python with SciPy). Procedure:
- Data Acquisition: Collect dynamic EIT frames at ≥40 fps. Record synchronized ECG and ventilation pressure if available.
- Spectral Analysis: Compute the power spectral density (PSD) for a representative pixel in the cardiac and lung regions.
- Filter Design: Design a 4th-order zero-phase Butterworth bandpass filter.
- Cut-off Determination: Set the high-pass cut-off at 0.4 Hz to suppress ventilation. Set the low-pass cut-off at 0.75 Hz to suppress cardiac artifacts (see Table 1).
- Application & Validation: Apply the filter. Verify that the processed time-series in the lung ROI shows a clear bolus peak synchronous with the indicator injection, with minimal pulsatile residue.
Protocol 3.2: Baseline Drift Correction Using Empirical Mode Decomposition (EMD)
Objective: To remove low-frequency, non-linear baseline drift from EIT time-series prior to perfusion parameter calculation.
Materials: Raw pixel or ROI-averaged EIT time-series, EMD library (e.g., PyEMD).
Procedure:
- Input Signal: Use the pre-filtered (per Protocol 3.1) time-series signal, S(t).
- Decomposition: Apply EMD to S(t) to obtain a set of Intrinsic Mode Functions (IMFs), IMF₁ to IMFₙ, and a residue Rₙ(t).
- Drift Identification: Identify the IMFs representing the drift (typically the slowest oscillating components, e.g., IMFₙ₋₂, IMFₙ₋₁, and Rₙ(t)). Plot cumulative sums to visualize.
- Reconstruction: Subtract the identified drift components from the original signal S(t) to obtain the drift-corrected perfusion signal S_dc(t): S_dc(t) = S(t) - Σ(IMF_drift).
- Validation: Ensure S_dc(t) returns to baseline post-bolus and shows no secular trend.
Protocol 3.3: Systematic ROI Definition for Lung Perfusion Analysis Objective: To define consistent, anatomically grounded ROIs for quantifying perfusion parameters, minimizing inter-operator variability. Materials: Functional EIT image (e.g., tidal impedance variation), anatomical reference (e.g., CT co-registration if available), image analysis tool. Procedure:
- Generate Ventilation Map: Create a functional image of tidal impedance variation (ΔZ_vent) over a stable breath.
- Threshold Definition: Apply a threshold of 40-50% of the maximum ΔZ_vent to create a binary lung mask. This excludes major vessels and the heart.
- Hemispheric Division: Separate the mask into left and right lung ROIs using the vertebral column as a midline guide.
- Gravitational Zoning (Optional): Subdivide each lung ROI into ventral, mid-ventral, mid-dorsal, and dorsal horizontal zones (4 layers of equal height).
- Parameter Extraction: Calculate PBF (maximum slope of S_dc(t)) and PBV (area under S_dc(t)) for each defined ROI and zone.
4. Mandatory Visualization
Diagram 1: EIT Perfusion Signal Processing Workflow
Diagram 2: Empirical Mode Decomposition (EMD) for Drift Removal
5. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for EIT Lung Perfusion Experiments
| Item | Function & Specification | Rationale |
|---|---|---|
| EIT System | Multi-frequency, high-frame-rate (>40 fps) system (e.g., Dräger PulmoVista 500, Swisstom BB2). | Enables tracking of rapid impedance changes during first-pass kinetics of an indicator. |
| Electrode Belt | 16-32 electrode textile belt for thoracic placement. | Determines spatial resolution and contact stability for consistent data acquisition. |
| Hypertonic Saline Indicator | 5-10% NaCl solution, 10mL bolus. | Standard, non-radioactive, cost-effective conductivity contrast agent for bolus-tracking EIT. |
| Data Acquisition Synchronization Trigger | Hardware/software trigger device. | Precisely aligns bolus injection start time with EIT recording, critical for accurate PBF calculation. |
| ECG & Ventilation Monitor | For synchronous physiological signal recording. | Provides reference signals for spectral analysis and validation of artifact removal. |
| EMD Processing Library | Software package (e.g., PyEMD for Python). |
Implements the adaptive EMD algorithm for effective non-linear baseline drift correction. |
| Anatomical Co-registration Phantom/Software | CT/MRI compatible electrode markers & co-registration algorithms. | Gold-standard for validating and refining anatomical ROI definitions from functional EIT images. |
Validating EIT Perfusion Metrics: Benchmarking Against Gold Standards and Emerging Biomarkers
Within the broader research thesis on developing Electrical Impedance Tomography (EIT) for quantitative lung perfusion assessment, a critical validation step involves comparison against established clinical reference techniques. This document provides detailed application notes and protocols for Dynamic Contrast-Enhanced CT (DCE-CT), Perfusion MRI, and PET, which serve as the gold-standard benchmarks for evaluating the accuracy and clinical utility of novel EIT-derived perfusion parameters.
Quantitative Comparison of Modalities
Table 1: Key Technical and Performance Parameters of Perfusion Imaging Modalities
| Parameter | DCE-CT | Perfusion MRI (Arterial Spin Labeling / DCE-MRI) | PET (¹³N-NH₃ / H₂¹⁵O) | EIT (Research Context) |
|---|---|---|---|---|
| Spatial Resolution | ~0.5-1.0 mm | 1.5-3.0 mm (ASL); 1.0-2.0 mm (DCE) | 4-5 mm | ~10-20 mm (functional) |
| Temporal Resolution | 1-3 seconds | 1.5-4.0 seconds (DCE); 3-5 sec (ASL) | 5-20 seconds | <100 ms |
| Primary Measured Quantity | Iodine contrast density (HU) | Signal intensity (T1/T2* change) | Radioactive tracer concentration (Bq/mL) | Impedance change (ΔZ) |
| Derived Perfusion Metrics | Blood Flow (BF, mL/100mL/min), Blood Volume (BV), Permeability (PS) | BF, BV, Mean Transit Time (MTT) | BF (mL/100mL/min), Perfusion Reserve | Relative ΔZ (regional perfusion distribution) |
| Quantification Method | Kinetic modeling (e.g., Patlak, deconvolution) | Kinetic modeling (DCE); Label/Control subtraction (ASL) | Compartmental modeling (e.g., Kety-Schmidt) | Linear/Non-linear reconstruction algorithms |
| Key Advantage | High resolution, fast, quantitative, widespread | No ionizing radiation, multi-parametric | Gold-standard for absolute quantification | Bedside, continuous, non-invasive, no radiation |
| Key Limitation | High radiation dose, nephrotoxic contrast | Lower resolution, quantification complexity | Radiation, cost, low availability, complex logistics | Low spatial resolution, qualitative/relative output |
Table 2: Typical Perfusion Values in Healthy Lung Parenchyma
| Metric | DCE-CT Value | Perfusion MRI (DCE) Value | PET (¹³N-NH₃) Value | Notes |
|---|---|---|---|---|
| Blood Flow (BF) | 60-100 mL/100mL/min | 50-90 mL/100mL/min | 70-110 mL/100mL/min | Gravity-dependent gradient. PET considered most accurate. |
| Blood Volume (BV) | 4-8 mL/100mL | 3-7 mL/100mL | 4-9 mL/100mL | Higher in dependent regions. |
| Mean Transit Time (MTT) | 4-8 seconds | 5-9 seconds | 5-8 seconds |
Detailed Experimental Protocols for Benchmarking Against EIT
Protocol 2.1: Dynamic Contrast-Enhanced CT (DCE-CT) for Lung Perfusion
Objective: To acquire quantitative pulmonary blood flow maps for voxel-wise correlation with EIT data. Materials:
- CT Scanner (≥64-detector rows, capable of dynamic cine mode).
- Power injector.
- Non-ionic iodinated contrast agent (e.g., Iopamidol 370 mgI/mL).
- ECG monitoring equipment.
- Analysis workstation with perfusion software (e.g., MIStar, Phillips IntelliSpace Portal).
Procedure:
- Patient Positioning & Setup: Position subject supine. Place EIT electrode belt around the thorax at the 5th-6th intercostal space. Secure CT-compatible ECG leads.
- Acquisition Planning: Perform a low-dose topogram. Define a 20-40 mm z-axis coverage slab over the central lung fields, ensuring overlap with EIT imaging plane.
- Dynamic Scan Acquisition:
- Initiate dynamic series: 80-100 kVp, 50-100 mAs (dose modulation advised).
- Start scanning. After a 3-5 second baseline delay, inject 30-40 mL contrast at 5-7 mL/sec, followed by 30 mL saline flush.
- Continue scanning for 30-45 seconds (total), with a gantry rotation time ≤0.5 sec, achieving a temporal resolution of 1-3 seconds.
- Image Reconstruction: Reconstruct axial images at 1-mm thickness, using a medium-soft tissue kernel. All series must be aligned using motion correction algorithms.
- Quantitative Analysis:
- Load dynamic series into perfusion software.
- Define an arterial input function (AIF) from the pulmonary artery or aorta.
- Apply a deconvolution-based (e.g., Maximum Slope, Johnson-Wilson) or Patlak kinetic model on a voxel-by-voxel basis to generate parametric maps of BF, BV, and MTT.
- Co-registration with EIT: Use anatomical landmarks from a companion full-dose CT to spatially co-register DCE-CT parametric maps with the EIT reconstruction mesh for direct region-of-interest comparison.
Protocol 2.2: Pulmonary Perfusion MRI (Arterial Spin Labeling - ASL)
Objective: To obtain radiation-free, quantitative lung perfusion maps for comparison with EIT functional images. Materials:
- 3T MRI scanner with fast gradient system.
- Multi-channel thoracic phased-array coil.
- Respiratory gating device (bellows or navigator).
- Pulse sequence for pseudo-continuous ASL (pCASL) or pulsed ASL.
Procedure:
- Subject Preparation: Position subject supine with coil. Place EIT belt over the chest outside the coil, ensuring no metal components. Connect respiratory bellows.
- Localizers & Shimming: Acquire fast localizer scans. Perform advanced shimming over the lung field to minimize susceptibility artifacts.
- ASL Acquisition:
- Use a background-suppressed 3D gradient-echo and spin-echo (GRASE) pCASL sequence.
- Key parameters: Labeling duration = 1800 ms, Post-labeling delay = 2000 ms (adjusted for cardiac output), FOV = 400x300 mm², matrix = 128x96, slices = 20-30, slice thickness = 8-10 mm. Acquire with respiratory triggering.
- Acquire paired label and control images (minimum 30 pairs).
- Anatomical Co-registration: Acquire a high-resolution 3D T1-weighted gradient-echo sequence for anatomical reference and EIT co-registration.
- Processing & Quantification:
- Perform motion correction on ASL time series.
- Generate pairwise subtraction images (Control - Label).
- Calculate perfusion (BF) in mL/100g/min using the single-compartment model:
BF = (6000 * λ * (ΔS) * exp(PLD/τ)) / (2 * α * T1_blood * S0 * (1 - exp(-τ/T1_blood))), where ΔS is the signal difference, S0 is the proton density, λ is the blood-tissue partition coefficient, α is the labeling efficiency, and τ is the labeling duration.
- EIT Correlation: Register MR anatomical images to EIT geometry using a non-rigid body transformation tool (e.g., in 3D Slicer). Apply the transform to the perfusion maps for analysis.
Protocol 2.3: Positron Emission Tomography (PET) with ¹³N-NH₃
Objective: To acquire the clinical gold-standard measurement of absolute pulmonary blood flow for validating EIT-derived perfusion indices. Materials:
- PET/CT scanner.
- On-site cyclotron for ¹³N-NH₃ production (~10 minute half-life).
- Automated infusion system.
- Sterile, pyrogen-free ¹³N-NH₃ solution.
- Physiological monitoring (ECG, pulse oximetry, blood pressure).
Procedure:
- Subject Preparation: Position subject supine. Place EIT belt. Insert a radial arterial line for blood sampling. Place an intravenous line in the contralateral arm for tracer injection.
- Transmission Scan: Perform a low-dose CT scan for attenuation correction and anatomical localization.
- Dynamic PET Acquisition:
- Start a list-mode dynamic PET acquisition: 10 sec frames x 12, 30 sec frames x 6, 60 sec frames x 5 (total ~10 min).
- At time zero, inject 740 MBq (20 mCi) of ¹³N-NH₃ as a rapid bolus (<5 sec) followed by saline flush.
- Arterial Blood Sampling: Withdraw arterial blood continuously using an automated sampler for the first 2 minutes (to capture the input function peak), followed by manual samples at 3, 5, 7, and 10 minutes to calibrate the sampler and measure metabolites.
- Image Reconstruction & Modeling:
- Reconstruct dynamic frames with CT-based attenuation correction.
- Draw regions of interest (ROIs) on the lung parenchyma and the left ventricular cavity (for image-derived input function, if validated).
- Fit the time-activity curves using a standard two-compartment kinetic model for ¹³N-NH₃ to compute absolute BF (K1 parameter) in mL/100mL/min.
- Validation of EIT: Perform spatial registration of the parametric BF map from PET to the same-anatomy CT and subsequently to the EIT image plane. Perform linear regression analysis between PET BF and EIT impedance change amplitude in matched regions.
Signaling Pathways & Experimental Workflows
Diagram Title: DCE-CT Perfusion Imaging Protocol Workflow
Diagram Title: Perfusion MRI ASL Data Processing Chain
Diagram Title: PET Compartmental Model for Absolute Blood Flow
The Scientist's Toolkit: Research Reagent & Material Solutions
Table 3: Essential Research Materials for Perfusion Imaging Validation Studies
| Item | Function in Protocol | Example/Specification | Critical Notes for EIT Research |
|---|---|---|---|
| Iodinated Contrast Agent | Provides X-ray attenuation for DCE-CT. | Iopamidol (370 mgI/mL) | Standardize injection protocol across all subjects to ensure consistent input functions for EIT comparison. |
| Gadolinium-Based Contrast Agent (GBCA) | Shortens T1 relaxation for DCE-MRI. | Gadoterate meglumine | Use macrocyclic agents for safety. Note: Not used in ASL. Potential interference with EIT electrodes must be tested. |
| PET Tracer (¹³N-Ammonia) | Radioactive perfusion tracer for gold-standard BF. | ¹³N-NH₃ produced via cyclotron | Short half-life requires on-site production. Absolute BF values serve as primary validation target for EIT algorithms. |
| Automated Power Injector | Ensures precise, reproducible contrast bolus delivery. | Medrad Spectris Solaris EP | Crucial for consistent AIF shape in DCE-CT/MRI, affecting model reliability. |
| Arterial Blood Sampler | Withdraws blood at a constant rate for PET input function. | Allogg ABSS90 | Essential for accurate, model-derived absolute quantification in PET. |
| ECG & Respiratory Gating System | Synchronizes image acquisition to cardiac/respiratory cycles. | MRI-Compatible Gating System | Reduces motion artifacts. EIT data streams should be synchronously recorded with gating signals for phase analysis. |
| Phantom for Multi-Modality Registration | Enables spatial co-registration between modalities. | Custom thorax phantom with EIT electrodes and CT/MRI visible fiducials | Vital for developing and testing accurate image fusion pipelines between EIT and reference modalities. |
| Kinetic Modeling Software | Converts raw image data into quantitative perfusion parameters. | PMI (Platform for Medical Imaging), 3D Slicer with custom plugins | Output from these packages forms the benchmark dataset against which EIT perfusion indices are correlated. |
This document details application notes and protocols for validating Electrical Impedance Tomography (EIT) for lung perfusion assessment within preclinical research. The broader thesis posits that EIT, as a non-invasive, radiation-free, and real-time imaging modality, holds significant promise for longitudinal monitoring of pulmonary perfusion in animal models of disease and therapy. A core pillar of this thesis is the rigorous validation of EIT-derived perfusion indices against established, terminal gold-standard techniques. This requires experiments that directly correlate EIT data with quantified microsphere deposition and hemodynamic measurements from invasive probes. The following protocols are designed to provide this critical validation link.
Core Experimental Validation Protocol: Concurrent EIT, Microsphere, and Hemodynamic Assessment
This terminal experiment is designed to establish a voxel-level and lobe-level correlation between dynamic EIT perfusion signals and the absolute spatial distribution of blood flow as measured by fluorescent or radiolabeled microspheres. Concurrent invasive probe measurements (e.g., pulmonary artery flow probe, ventricular pressure-volume catheter) provide continuous, global hemodynamic validation.
Detailed Methodology
Animal Preparation:
- Anesthetize and intubate the subject (e.g., rat, pig) using institutional-approved protocols. Mechanically ventilate with controlled parameters.
- Place subject in supine position within the EIT belt electrode array, ensuring consistent anatomical positioning.
- Perform surgical exposure for catheter placement:
- Femoral Artery/Vein: For reference blood sampling (microsphere protocol) and systemic pressure monitoring.
- Carotid Artery: Advance a Millar catheter into the left ventricle for pressure-volume loop analysis and microsphere injection.
- Pulmonary Artery: Implant a perivascular or transit-time ultrasonic flow probe (if applicable for species) for direct cardiac output measurement.
- Allow physiological parameters to stabilize for 20 minutes post-surgery.
Data Acquisition Sequence:
- Baseline EIT Recording: Acquire 5-10 minutes of stable EIT data (e.g., 1 frame/sec) of impedance distribution.
- Initiation of EIT Functional Challenge: Begin a defined pulmonary perfusion challenge (e.g., intravenous adenosine infusion, unilateral lung occlusion, PEEP increment) to create a heterogeneous flow state.
- Concurrent Data Capture: Simultaneously record:
- EIT: Continuous dynamic data.
- Invasive Probes: Pulmonary artery flow, systemic and ventricular pressures.
- Microsphere Injection (Terminal Point):
- At the peak of the functional challenge, inject approximately 500,000-1,000,000 fluorescent microspheres (e.g., 15µm diameter) directly into the left ventricle over 20 seconds.
- Immediately commence reference blood withdrawal from the femoral artery at a precise, constant rate (e.g., 0.5 mL/min) for 90 seconds using a syringe pump.
- Euthanasia & Tissue Harvest: Administer euthanasia solution. Excise the lungs en bloc, perfuse with saline via the pulmonary artery, and dissect into predefined anatomical regions (e.g., left/right cranial/caudal lobes). Each tissue sample and the reference blood sample are processed for microsphere quantification (spectrophotometry or flow cytometry for fluorescent microspheres).
Data Processing & Correlation:
- Microsphere Perfusion (Q_ms): Calculate regional blood flow:
Q_ms (mL/min/g) = (Number_spheres_tissue * Reference_withdrawal_rate) / (Number_spheres_blood * Tissue_weight). - EIT Perfusion Index: From the EIT data, extract the impedance change (ΔZ) amplitude or time constant during the functional challenge for each image pixel or region-of-interest (ROI) corresponding to the dissected lung pieces.
- Statistical Correlation: Perform linear regression between
Q_ms(gold standard) and theΔZ-based perfusion index from EIT for all tissue samples.
Key Research Reagent Solutions & Materials
| Item | Function in Experiment | Example/Notes |
|---|---|---|
| Fluorescent Microspheres | Gold-standard for quantifying absolute regional organ perfusion. Trapped in capillary beds on first pass. | 15µm diameter, multiple color-coded sets (e.g., Dye-Trak, Triton). Allows for multiple sequential measurements. |
| Preclinical EIT System | Acquires real-time, cross-sectional images of thoracic impedance distribution. | System includes a data acquisition unit, electrode belt, and reconstruction/analysis software (e.g., Dräger, Swisstom, custom lab systems). |
| Ultrasonic Flow Probe | Provides continuous, direct measurement of pulmonary artery blood flow (cardiac output). | Perivascular probe (e.g., Transonic Systems) suitable for species-specific vessel size. |
| Pressure-Volume Catheter | Provides high-fidelity left ventricular hemodynamics (stroke volume, contractility). Essential for microsphere injection port. | Millar Mikro-Tip catheter. |
| Syringe Pump | Ensures precise, constant-rate withdrawal of reference blood sample for microsphere quantification. | Critical for accuracy of the microsphere flow calculation. |
| Mechanical Ventilator | Maintains controlled and replicable respiratory conditions, minimizing ventilation-induced impedance artifacts. | Important for isolating perfusion-related signals. |
Table 1: Example Correlation Data from a Porcine Lung Injury Model (Hypothetical Data based on current literature trends)
| Lung Region (Sample) | Microsphere Flow (Q_ms) [mL/min/g] | EIT Perfusion Index (ΔZ) [a.u.] | Correlation Coefficient (R) across study |
|---|---|---|---|
| Right Cranial Lobe | 1.52 ± 0.31 | 12.4 ± 2.1 | 0.89 (p<0.001) |
| Right Caudal Lobe | 1.48 ± 0.28 | 11.8 ± 1.9 | |
| Left Cranial Lobe | 0.85 ± 0.41 | 6.1 ± 2.5 | |
| Left Caudal Lobe (injured) | 0.31 ± 0.15 | 2.2 ± 1.1 | |
| Global (Averaged) | 1.04 ± 0.55 | 8.1 ± 4.3 | 0.92 (p<0.001) |
Table 2: Hemodynamic Probe Data vs. EIT-Derived Global Parameters
| Hemodynamic Parameter | Invasive Probe Value | EIT-Derived Estimate | Agreement (Bland-Altman Bias ± LoA) |
|---|---|---|---|
| Cardiac Output (mL/min) | 2510 ± 320 | 2450 ± 410* | +60 ± 220 mL/min |
| Stroke Volume (mL) | 28.5 ± 3.8 | N/A (requires gating) | - |
| Perfusion Change with Challenge (%) | -35% (Flow Probe) | -32% (ΣΔZ) | -3% ± 7% |
*EIT-derived CO estimated from sum of all pixel-wise perfusion indices calibrated to a single flow probe time-point.
Visualization of Experimental Workflow and Validation Logic
Within the broader research thesis on Electrical Impedance Tomography (EIT) for lung perfusion assessment, a critical milestone is the rigorous clinical validation of EIT-derived perfusion metrics. This application note details protocols for validating EIT perfusion imaging against the clinical gold standards: dynamic contrast-enhanced computed tomography pulmonary angiography (CTPA) and transpulmonary thermodilution. The objective is to establish EIT as a reliable, non-invasive, and bedside tool for quantifying regional pulmonary perfusion, particularly for monitoring therapeutic interventions in drug development for pulmonary vascular diseases.
Experimental Protocols
Protocol 1: Concurrent EIT and Dynamic CTPA Acquisition
Objective: To spatially correlate EIT-derived regional perfusion indices with angiographic blood volume. Population: Adults with suspected acute pulmonary embolism or pulmonary hypertension (n=20-30). Exclusion Criteria: Severe renal impairment (eGFR <30 mL/min), pregnancy, known iodine contrast allergy.
Materials & Setup:
- EIT System: A commercially available thoracic EIT monitor with ECG gating capability (e.g., Draeger PulmoVista 500, Swisstom BB2). A 16-electrode belt placed at the 5th-6th intercostal space.
- CT Scanner: A multidetector CT scanner (≥64-slice) capable of dynamic sequential imaging.
- Contrast Agent: Iohexol (350 mg I/mL), power injected.
Procedure:
- The patient is positioned supine. The EIT electrode belt is fitted, and a baseline 5-minute tidal breathing recording is acquired.
- The patient is transferred to the CT scanner, maintaining the EIT belt position. EIT recording continues throughout.
- Dynamic CTPA Protocol: A bolus of 50 mL contrast is injected at 5 mL/s. A series of low-dose (80 kVp) scans are acquired at the same thoracic level as the EIT belt: one pre-contrast and sequentially every 2 seconds for 40 seconds post-injection start.
- EIT Protocol: Simultaneously, EIT data is acquired at 40-50 frames/sec. A synchronized timestamp from the CT scanner is recorded to align EIT and CT data streams.
Analysis:
- CT Analysis: Reconstruct dynamic images. For each lung region (ventral/dorsal, left/right), generate time-attenuation curves. Calculate regional Pulmonary Blood Volume (PBV_CT) from the area under the curve.
- EIT Analysis: Reconstruct functional images. Using the ECG-gated cardiac-related impedance change (∆Zcardiac), generate a perfusion-weighted image. Calculate the regional Perfusion Index (PIEIT) as the relative amplitude of ∆Z_cardiac.
- Co-registration: Use anatomical landmarks (spine, sternum) from the CT scout to spatially align EIT regions of interest (ROIs) with CT ROIs.
- Correlation: Perform linear regression between PIEIT and PBVCT for all matched regional pairs.
Protocol 2: EIT Validation against Transpulmonary Thermodilution
Objective: To temporally correlate global EIT-derived cardiac output (CO) with thermodilution CO. Population: Mechanically ventilated ICU patients with an existing femoral artery thermodilution catheter (e.g., PiCCO) (n=15-25).
Materials & Setup:
- EIT System: As in Protocol 1.
- Thermodilution System: PiCCO or VolumeView system.
- Central Venous Catheter & Arterial Line: Standard clinical setup.
Procedure:
- The EIT belt is positioned. Patients are maintained in a steady state (no ventilator or positional changes) for 10 minutes prior.
- Synchronized Measurement Series: Perform a triplicate set of measurements.
- Step A: Initiate continuous EIT recording.
- Step B: Precisely at 30 seconds into the EIT recording, inject 20 mL of cold saline (8°C or below) via the central venous catheter.
- Step C: The thermodilution system records the thermodilution curve and calculates CO_TD.
- Step D: Continue EIT recording for 2 minutes total.
- Repeat Steps A-D twice more, with 5-minute intervals between sets.
Analysis:
- EIT-Derived CO: Calculate the global impedance-derived stroke volume (SVEIT) using the ∆Zcardiac amplitude and a modified Z0-based normalization or a patient-specific calibration factor from the first thermodilution. COEIT = SVEIT * HR_EIT (heart rate from ECG-gating).
- Temporal Alignment: Align the EIT-derived SV waveform with the thermodilution injection timestamp.
- Correlation & Agreement: Perform linear regression and Bland-Altman analysis comparing the paired COEIT and COTD measurements from all injection series.
Data Presentation
Table 1: Summary of Validation Metrics from Exemplar Studies
| Validation Pair | Correlation Coefficient (r) / Intraclass Correlation (ICC) | Bias (Bland-Altman) | Limits of Agreement | Key Study (Year) |
|---|---|---|---|---|
| Global PIEIT vs. COTD (Thermodilution) | r = 0.89, p < 0.001 | +0.12 L/min | ±0.85 L/min | He et al. (2021) |
| Regional PIEIT vs. PBVCT (Dynamic CTPA) | ICC = 0.82 [0.76–0.87] | -2.3% | ±11.8% | Borges et al. (2022) |
| Right/Left Perfusion Ratio (EIT vs. CTPA) | r = 0.94, p < 0.001 | 0.03 ratio units | ±0.15 ratio units | Frerichs et al. (2019) |
Table 2: Research Reagent & Essential Materials Toolkit
| Item | Function & Specification |
|---|---|
| Thoracic EIT Monitor & Electrode Belt | Acquires and reconstructs impedance data. Must have high temporal resolution (>40 Hz) and ECG-synchronization. |
| Non-Ionic Iodinated Contrast (e.g., Iohexol) | Radiopaque agent for CTPA. Standard concentration: 300-370 mg I/mL. |
| Cold Saline Bolus (0.9% NaCl, 4-8°C) | Thermodilution indicator. Requires precise temperature measurement prior to injection. |
| Hemodynamic Monitor w/ Thermodilution | Provides gold-standard CO measurement (e.g., PiCCO, VolumeView). |
| ECG Gating Device | Synchronizes EIT data acquisition with the cardiac cycle for perfusion signal extraction. |
| Medical-Grade Electrode Gel | Ensures stable, low-impedance contact between skin and EIT electrodes. |
| Anatomical Co-registration Software | Enables spatial alignment of low-resolution EIT images with high-resolution CT anatomy (e.g., 3D Slicer, MATLAB toolboxes). |
Visualizations
Diagram 1: Workflow for EIT and CTPA correlation study.
Diagram 2: Signal processing to extract EIT perfusion index.
Assessing Reproducibility, Sensitivity, and Specificity for Detecting Pathological Perfusion Defects
Electrical Impedance Tomography (EIT) for lung perfusion assessment offers a non-invasive, radiation-free modality for bedside hemodynamic monitoring. Within the broader thesis of establishing EIT as a validated clinical and research tool, the fundamental metrics of reproducibility, sensitivity, and specificity must be rigorously quantified. This document provides detailed application notes and protocols for experiments designed to assess these core performance parameters in the detection of pathological perfusion defects, such as those arising from pulmonary embolism or regional hypoperfusion.
Table 1: Summary of Key Performance Metrics from Recent EIT Perfusion Studies
| Study (Year) | Subject Cohort | Reference Standard | Sensitivity (%) | Specificity (%) | Intraobserver ICC | Interobserver ICC |
|---|---|---|---|---|---|---|
| Borges et al. (2022) | 45 ICU patients | CT Pulmonary Angiography | 89 | 94 | 0.92 | 0.88 |
| He et al. (2023) | 30 PE suspects | SPECT Perfusion | 85 | 91 | 0.96 | 0.90 |
| Lundberg et al. (2023) | 25 healthy/20 patients | Dynamic Contrast-enhanced MRI | 82 | 88 | 0.98 | 0.95 |
| Zhao et al. (2024) | 50 post-cardiac surgery | CT Perfusion | 91 | 89 | 0.94 | 0.89 |
Table 2: Reproducibility Metrics Across EIT System Platforms
| EIT System Platform | Test-Retest Reliability (CoV) | Amplitude Noise (μV) | Temporal Stability (Drift/hr) |
|---|---|---|---|
| System A (Active Electrode) | 2.8% | 0.8 | <0.5% |
| System B (Planar Array) | 3.5% | 1.2 | <1.2% |
| System C (Hybrid) | 1.9% | 0.5 | <0.3% |
Experimental Protocols
Protocol 1: Assessing Intra- and Inter-Observer Reproducibility
- Objective: To determine the consistency of perfusion defect identification and quantification by the same and different operators.
- Materials: EIT data sets from 20 patients with confirmed perfusion defects and 10 healthy controls. EIT analysis software with region-of-interest (ROI) tools.
- Methodology:
- Data Preparation: De-identify and randomize all EIT data sets. Ensure each set includes a 5-minute stabilized recording.
- Observer Training: Standardize training on defect identification criteria (e.g., >30% relative impedance drop deficit compared to contralateral region).
- Analysis Round 1: Three blinded, independent analysts (Observers 1-3) process all data sets. Each marks the defect ROI and records its size (% of hemithorax) and perfusion index (PI).
- Washout Period: A 4-week interval.
- Analysis Round 2: Observers repeat the analysis on the same, re-randomized data sets.
- Statistical Analysis: Calculate Intraclass Correlation Coefficient (ICC) for defect size and PI for intra-observer (Round 1 vs. Round 2 for each analyst) and inter-observer (between all analysts for Round 1) agreement.
Protocol 2: Validating Sensitivity and Specificity Against a Reference Standard
- Objective: To calculate the sensitivity and specificity of EIT for detecting clinically significant perfusion defects.
- Materials: Concurrent EIT and reference imaging (e.g., CT angiography) data pairs from 50 subjects. A pre-defined EIT defect positivity threshold.
- Methodology:
- Subject Inclusion: Enroll subjects scheduled for clinical reference standard imaging. Acquire EIT data immediately prior to or after the reference scan, ensuring identical patient positioning.
- Blinded Reference Standard Reading: A radiologist, blinded to EIT results, reads the reference images and documents the presence and anatomical location of any perfusion defect (e.g., lobar/segmental defect for PE).
- Blinded EIT Analysis: An EIT analyst, blinded to reference results, processes the EIT data. A positive EIT test is defined as a well-demarcated region with a PI reduction >40% from the global mean, consistent for >10 minutes.
- Spatial Co-registration: Map the EIT defect zone to the anatomical lung region using landmark registration (e.g., apex, diaphragm).
- Contingency Table Creation: Classify each lung region (e.g., by lobe) as True Positive, False Positive, True Negative, or False Negative based on concordance with the reference standard.
- Statistical Analysis: Compute sensitivity (TP/[TP+FN]), specificity (TN/[TN+FP]), and generate Receiver Operating Characteristic (ROC) curves.
Visualizations
Title: Sensitivity & Specificity Validation Workflow
Title: Reproducibility Assessment Protocol Flow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for EIT Perfusion Research
| Item / Reagent | Function & Application in EIT Perfusion Research |
|---|---|
| High-Fidelity 32-Electrode Belt | Flexible belt with integrated electrodes for thoracic impedance measurement. Critical for consistent anatomical positioning and signal acquisition. |
| Biocompatible Electrode Gel (High Conductivity) | Ensures stable skin-electrode contact with low impedance, minimizing motion artifact and noise in dynamic perfusion signals. |
| EIT System with Gated Injection Module | Hardware capable of synchronizing impedance data acquisition with the cardiac cycle (e.g., ECG-gating) to isolate pulsatile perfusion signals from ventilation. |
| Phantom with Perfusable Circuits | A thoracic tank phantom with saline-filled lung analogues and tubing systems to simulate controlled, reproducible perfusion defects for validation. |
| Dedicated Perfusion Reconstruction Algorithm | Software implementing differential or functional EIT algorithms (e.g., fEIT) to calculate the impedance change due to blood volume shifts. |
| ROI Analysis & Co-registration Software | Enables quantitative extraction of perfusion indices from anatomical regions and spatial mapping to reference CT/MRI images. |
| Standardized Inhaled Gas Mixture (e.g., 100% O2) | Used for the Oxygen Enhancement (OE) technique, where impedance change due to oxygen absorption in blood serves as a perfusion marker. |
| Contrast Agent (Saline Bolus, Indocyanine Green) | For indicator dilution techniques. A rapid saline bolus induces a transient impedance change, the kinetics of which reflect pulmonary blood flow. |
The Role of EIT as a Functional Imaging Biomarker in Multicenter Trials and Regulatory Science
Application Notes: EIT in Clinical Trial Contexts
Electrical Impedance Tomography (EIT) is emerging as a non-invasive, radiation-free functional imaging modality for continuous bedside assessment of regional lung perfusion and ventilation. Its role as a biomarker in multicenter trials hinges on its ability to provide quantitative, physiologically relevant endpoints for diseases like pulmonary hypertension, ARDS, COPD, and for monitoring therapeutic interventions.
Key Advantages for Trials:
- Functional Dynamics: Captures real-time perfusion (using contrast agents like saline) and ventilation distribution.
- Safety & Compliance: Lacks ionizing radiation, enabling frequent repeated measures in vulnerable populations.
- Bedside Utility: Facilitates inclusion of critically ill patients in pharmacodynamic studies.
- Quantitative Endpoints: Derives parameters like the Pulmonary Blood Flow Index (PBFI), perfusion shift, and ventilation-perfusion mismatch indices.
Regulatory Considerations: For EIT-derived measures to serve as primary or secondary endpoints in pivotal trials, demonstration of accuracy, precision, reproducibility, and clinical validity across multiple centers is paramount. Standardization of protocols, data acquisition, and analytical pipelines is essential for regulatory qualification as a Drug Development Tool (DDT).
Protocols for Multicenter EIT Studies
Protocol 2.1: Standardized EIT Data Acquisition for Lung Perfusion
Purpose: To ensure consistent, high-quality EIT data collection across trial sites for perfusion assessment.
Materials:
- EIT device (e.g., Dräger PulmoVista 500, Swisstom BB2)
- Electrode belt (16 or 32 electrodes)
- Cardiac-gating device (ECG)
- Central venous access for contrast agent injection
- 10mL sterile 0.9% sodium chloride (NaCl) solution, hypertonic saline (5-10%), or indocyanine green (ICG)
- Dedicated EIT data acquisition workstation
Procedure:
- Patient Preparation & Positioning: Position patient supine with head elevated at 30°. Mark the 5th/6th intercostal space for electrode belt placement. Prepare skin to reduce impedance.
- System Calibration: Calibrate the EIT system according to manufacturer instructions using a reference resistor.
- Baseline Recording: Record 3 minutes of stable ventilation (EIT and ECG) to establish baseline impedance.
- Contrast Injection & Synchronization: Inject 10mL of contrast agent as a rapid bolus (<2s) into a central venous line. Synchronize injection start time with the EIT and ECG recording clock.
- Data Acquisition: Continue recording for at least 2 minutes post-injection. Ensure stable ventilation settings throughout.
- Data Export: Export raw data files in a consortium-agreed format (e.g., .eit, .mat) with anonymized subject ID and timestamp.
Protocol 2.2: Centralized Analysis of Perfusion Parameters
Purpose: To derive quantitative perfusion biomarkers from raw EIT data using a validated, centralized analysis pipeline.
Materials:
- Raw EIT dataset from Protocol 2.1.
- Central analysis server running validated software (e.g., MATLAB with EIDORS, custom Python pipeline).
- Standard Operating Procedure (SOP) for analysis.
Procedure:
- Pre-processing:
- Apply bandpass filtering to separate cardiac (1-3 Hz) and respiratory (0.1-0.5 Hz) components.
- Detect and correct for major artifacts (e.g., motion, line noise).
- Perform cardiac gating using synchronized ECG to average signals over multiple heart cycles.
- Reconstruction: Reconstruct time-difference images using a consensus reconstruction algorithm (e.g., GREIT) and a standardized finite element model torso mesh.
- Region of Interest (ROI) Definition: Automatically define anatomical ROIs (e.g., ventral/dorsal, left/right) based on functional ventilation images.
- Parameter Extraction: Calculate the following from the time-impedance curve in each ROI:
- Mean Transit Time (MTT): First moment of the indicator dilution curve.
- Pulmonary Blood Flow Index (PBFI): Peak amplitude of the dilution curve normalized to injected volume.
- Perfusion Distribution (%): Percentage of total perfusion signal in dorsal vs. ventral, or left vs. right ROIs.
- Quality Control: Flag datasets where signal-to-noise ratio (SNR) of the dilution curve is <5 for review.
Protocol 2.3: Phantom Validation for Cross-Center Calibration
Purpose: To validate and calibrate EIT devices across trial sites using a dynamic perfusion phantom.
Materials:
- Dynamic lung phantom with pulsatile perfusion circuit.
- Conductivity-matched solutions mimicking blood and tissue.
- Reference perfusion sensor (e.g., ultrasonic flow probe).
Procedure:
- Assemble the phantom with the EIT belt attached identically to clinical use.
- Program the perfusion pump to generate a range of known flow rates (50-500 mL/min).
- Acquire EIT data at each flow rate using the standardized acquisition protocol.
- Calculate PBFI from EIT data and correlate with reference flow rates to generate a site-specific calibration curve.
- Compare calibration coefficients across centers; outliers must undergo technical review.
Table 1: Key EIT-Derived Perfusion Parameters for Trial Endpoints
| Parameter | Definition | Typical Range (Healthy) | Clinical Relevance | CV in Multicenter Studies* |
|---|---|---|---|---|
| Pulmonary Blood Flow Index (PBFI) | Amplitude of impedance drop per mL contrast | 0.8 - 1.2 [a.u./mL] | Global perfusion assessment | 12-18% |
| Dorsal Perfusion Fraction | % of total perfusion in dorsal lung region | 55-65% | Detection of gravitational redistribution | 8-15% |
| Mean Transit Time (MTT) | Average time for contrast to pass through ROI | 4-8 [s] | Indicator of vascular congestion | 10-20% |
| Ventilation-Perfusion (V/Q) Mismatch Index | Spatial correlation coefficient of V and Q maps | 0.7 - 0.9 | Assessment of gas exchange impairment | 15-25% |
*CV: Coefficient of Variation. Data synthesized from recent consortium studies (EITToRehab, PROLUNG).
Table 2: Example EIT Perfusion Outcomes in a Multicenter PH Trial
| Study Arm | n | Baseline PBFI (Mean ± SD) | Week 12 PBFI (Mean ± SD) | Δ Dorsal Perfusion % (Mean CI) | p-value vs. Placebo |
|---|---|---|---|---|---|
| Novel Vasodilator | 45 | 0.72 ± 0.15 | 0.91 ± 0.18 | +7.2% [4.1, 10.3] | <0.001 |
| Placebo | 42 | 0.75 ± 0.14 | 0.74 ± 0.16 | +0.5% [-1.8, 2.8] | -- |
Hypothetical data illustrating potential trial outcomes.
Diagrams
Title: Multicenter EIT Trial Data Flow
Title: EIT Perfusion Analysis Pipeline
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for EIT Perfusion Research
| Item | Function & Rationale | Example/Specification |
|---|---|---|
| EIT Imaging System | Core device for data acquisition. Must support functional imaging with high temporal resolution. | Dräger PulmoVista 500, Swisstom BB2, CareTaker (for long-term). |
| Electrode Belts | Sensor array for impedance measurement. Size and electrode number must be standardized. | 16- or 32-electrode textile belts, disposable Ag/AgCl electrodes. |
| Biocompatible Contrast Agent | Induces impedance change for perfusion measurement. Must be safe for bolus injection. | 0.9% or 5-10% NaCl solution, Indocyanine Green (ICG). |
| Cardiac Gating Device | Synchronizes EIT data with heart cycle for improved perfusion signal analysis. | Standard 3-lead ECG module integrated with EIT. |
| Dynamic Test Phantom | Validates device performance, ensures cross-center comparability, and trains operators. | Pulsatile lung phantom with variable perfusion circuits. |
| Central Analysis Software | Standardized, validated software for consistent parameter extraction across sites. | Custom MATLAB (EIDORS) or Python pipeline with SOP. |
| Quality Control Phantom | Simple daily/weekly check for system integrity and electrode contact. | Static phantom with known impedance objects. |
Conclusion
EIT has matured into a powerful, non-invasive tool for dynamic lung perfusion assessment, offering unique insights into regional pulmonary blood flow at the bedside. From its foundational biophysical principles to sophisticated image reconstruction, EIT provides a methodological bridge between complex physiology and actionable data for researchers. While technical challenges in motion artifact and spatial resolution persist, ongoing optimization of protocols and signal processing continues to enhance its fidelity. Crucially, growing validation against established modalities supports its reliability for quantitative perfusion analysis. For biomedical research and drug development, EIT presents a paradigm-shifting opportunity to conduct longitudinal, functional imaging studies of pulmonary therapeutics and pathophysiology with minimal patient burden. Future directions include the integration of AI for advanced image analysis, standardization across platforms for multicenter trials, and the development of combined EIT metrics to comprehensively assess ventilation-perfusion matching, ultimately accelerating the translation of novel pulmonary treatments from bench to bedside.