Foundations of Medical Imaging Engineering and Physics: From Core Principles to AI-Driven Frontiers
This article provides a comprehensive exploration of the engineering and physical principles underpinning modern medical imaging.
Foundations of Medical Imaging Engineering and Physics: From Core Principles to AI-Driven Frontiers
Abstract
This article provides a comprehensive exploration of the engineering and physical principles underpinning modern medical imaging. Tailored for researchers, scientists, and drug development professionals, it spans from the foundational concepts of established modalities like CT, MRI, and PET to the cutting-edge integration of artificial intelligence. The content systematically addresses the fundamental physics of image formation, methodological advances in imaging applications, critical challenges in optimization and interpretability, and rigorous frameworks for model validation. By synthesizing these core intents, this resource aims to equip professionals with the knowledge to leverage advanced imaging in research and clinical translation, ultimately accelerating diagnostic and therapeutic innovation.
Core Principles and the Evolution of Medical Imaging Modalities
The field of medical imaging engineering relies on fundamental physical principles to visualize internal body structures for clinical analysis and research. These modalities can be broadly categorized based on their underlying physical mechanisms, which dictate their applications, strengths, and limitations in both clinical and research settings. From high-energy ionizing radiation used in X-rays to the magnetic properties of atomic nuclei harnessed in Magnetic Resonance Imaging (MRI), each modality provides unique windows into human physiology and pathology. Understanding the physics of image formation is crucial for developing new imaging techniques, improving diagnostic accuracy, and advancing pharmaceutical research through quantitative biomarker development. This technical guide examines the core physical principles, signal formation mechanisms, and quantitative aspects of major medical imaging modalities, providing researchers with a foundation for selecting appropriate imaging methodologies for specific investigational needs.
Core Imaging Modalities: Physical Principles and Mechanisms
X-ray Imaging Physics
X-ray imaging formation relies on the differential attenuation of high-energy photons as they pass through tissues of varying densities. When X-rays, typically produced in a vacuum tube through the acceleration of electrons from a cathode to a metal anode target, interact with biological tissues, several physical processes occur. The photoelectric effect predominates in dense materials like bone, where X-ray photons are completely absorbed, ejecting inner-shell electrons from atoms. Compton scattering occurs when X-ray photons collide with outer-shell electrons, transferring only part of their energy and scattering in different directions. The varying degrees of these interactions across different tissues create the contrast observed in projection radiography. The transmitted X-ray pattern, representing the sum of attenuation along each path, is captured by detectors to form a two-dimensional image. In computed tomography (CT), this process is extended through rotational acquisition, enabling mathematical reconstruction of three-dimensional attenuation maps via filtered back projection or iterative reconstruction algorithms.
Magnetic Resonance Imaging Physics
Magnetic Resonance Imaging (MRI) utilizes the quantum mechanical property of nuclear spin, exploiting the magnetic moments of specific atomic nuclei when placed in a strong external magnetic field [1]. In clinical and research MRI, hydrogen atoms (1H) are most frequently used due to their natural abundance in biological organisms, particularly in water and fat molecules [1]. When placed in a strong external magnetic field (B0), the magnetic moments of protons align to be either parallel (lower energy state) or anti-parallel (higher energy state) to the direction of the field, creating a small net magnetization vector along the axis of the B0 field [1].
A radio frequency (RF) pulse is applied at the specific Larmor frequency, which is determined by the particle's gyro-magnetic ratio and the strength of the magnetic field [1]. This RF pulse excites protons from the parallel to anti-parallel alignment, tipping the net magnetization vector away from its equilibrium position [1]. Following the RF pulse, the protons undergo two distinct relaxation processes: longitudinal relaxation (T1) and transverse relaxation (T2) [1]. T1 relaxation represents the recovery of longitudinal magnetization along the B0 direction as protons return to their equilibrium state, while T2 relaxation represents the loss of phase coherence in the transverse plane [1]. In practical MRI, the observed signal decay occurs with a time constant T2*, which is always shorter than T2 due to inhomogeneities in the static magnetic field [1].
Spatial encoding in MRI is achieved through the application of magnetic field gradients that vary linearly across space, allowing the selective excitation of specific slices and the encoding of spatial information into the frequency and phase of the signal [1]. The resulting signal is collected in k-space (the spatial frequency domain), and images are reconstructed through a two-dimensional or three-dimensional Fourier transform [1]. By varying the timing parameters of the RF and gradient pulse sequences (repetition time TR and echo time TE), different tissue contrasts can be generated based on their relaxation properties [1].
Table 1: Fundamental Physical Principles of Major Medical Imaging Modalities
| Modality | Signal Origin | Energy Source | Key Physical Interactions | Spatial Encoding Method |
|---|---|---|---|---|
| X-ray/CT | Photon Transmission | Ionizing Radiation (X-rays) | Photoelectric Effect, Compton Scattering | Differential Attenuation, Projection Geometry |
| MRI | Nuclear Spin Resonance | Static Magnetic Field + Radiofrequency Pulses | Precession, T1/T2 Relaxation | Magnetic Field Gradients (Frequency/Phase Encoding) |
| Photoacoustic Imaging | Acoustic Wave Generation | Pulsed Laser Light | Thermoelastic Expansion | Time-of-Flight Ultrasound Detection |
Emerging Modalities: Photoacoustic Imaging
Photoacoustic imaging represents a hybrid modality that combines optical excitation with acoustic detection, leveraging the photoacoustic effect where pulsed laser light induces thermoelastic expansion in tissues, generating ultrasonic waves [2]. This approach provides high-resolution functional and molecular information from deep within biological tissues by exploiting the strong optical contrast of hemoglobin, lipids, and other chromophores while maintaining the penetration depth and resolution of ultrasound [2]. The technique is particularly valuable for imaging vascular networks, oxygen saturation, and molecular targets through exogenous contrast agents, with growing applications in cancer detection, brain functional imaging, and monitoring of therapeutic responses [2]. The physics of signal formation involves optical energy absorption, subsequent thermal expansion, and broadband ultrasound emission, with spatial localization achieved through time-of-flight measurements of the generated acoustic waves using ultrasonic transducer arrays.
Quantitative Imaging and Performance Evaluation
Task-Based Assessment of Image Quality
The rigorous assessment of medical image quality requires specification of both the clinical or research task and the observer (human or computer algorithm) [3]. Tasks are broadly divided into classification (e.g., tumor detection) and estimation (e.g., measurement of physiological parameters) [3]. For classification tasks performed by human observers, performance is typically assessed through psychophysical studies and receiver operating characteristic (ROC) analysis, with scalar figures of merit such as detectability index or area under the ROC curve used to compare imaging systems [3]. For estimation tasks typically performed by computer algorithms (often with human intervention), performance is expressed in terms of the bias and variance of the estimate, which may be combined into a mean-square error as a scalar figure of merit [3].
The Gold Standard Problem in Quantitative Imaging
A fundamental challenge in objective assessment of medical imaging systems is the frequent lack of a believable gold standard for the true state of the patient [3]. Researchers have often evaluated estimation methods by plotting results against those from another established method, effectively using one set of estimates as a pseudo-gold standard [3]. Regression analysis and Bland-Altman plots are commonly used for such comparisons, but both approaches have significant limitations [3]. The correlation coefficient (r) in regression analysis depends not only on the agreement between methods but also on the variance of the true parameter across subjects, making interpretation potentially misleading [3]. Bland-Altman analysis, which plots differences between methods against their means, employs an arbitrary definition of agreement (95% of estimates within two standard deviations of the mean difference) that does not indicate which method performs better [3].
Maximum-Likelihood Approach for Modality Comparison
A maximum-likelihood method has been developed to evaluate and compare different estimation methods without a gold standard, with specific application to cardiac ejection fraction estimation [3]. This approach models the relationship between the true parameter value (Θp) and its estimate from modality m (θpm) using a linear model with slope am, intercept bm, and normally distributed noise term εpm with variance σm² [3]. The likelihood function is derived under assumptions that the true parameter value does not vary across modalities for a given patient and is statistically independent across patients, while the linear model parameters are characteristic of the modality and independent of the patient [3]. This framework enables estimation of the bias and variance for each modality without designating any modality as intrinsically superior, allowing objective performance ranking of imaging systems for estimation tasks [3].
Table 2: Figures of Merit for Medical Imaging System Performance Evaluation
| Task Type | Performance Metric | Definition | Application Context |
|---|---|---|---|
| Classification | Area Under ROC Curve (AUC) | Probability that a randomly chosen positive case is ranked higher than a negative case | Tumor detection, diagnostic accuracy studies |
| Estimation | Bias | Difference between expected estimate and true parameter value | Quantitative parameter measurement (e.g., ejection fraction) |
| Estimation | Variance | Measure of estimate variability around its mean value | Measurement reproducibility, precision assessment |
| Estimation | Mean-Square Error (MSE) | Average squared difference between estimates and true values | Combined accuracy and precision assessment |
Experimental Protocols and Methodologies
Maximum-Likelihood Modality Comparison Protocol
The maximum-likelihood approach for comparing imaging modalities without a gold standard involves a specific experimental and computational protocol [3]. For a study with P patients and M modalities, the following steps are implemented:
Data Collection: Each patient undergoes imaging with all M modalities, with care taken to minimize changes in the underlying physiological state between scans.
Parameter Estimation: For each modality and patient, the quantitative parameter of interest (e.g., ejection fraction) is extracted using the appropriate algorithm for that modality.
Likelihood Function Formulation: The joint probability of the estimated parameters given the linear model parameters ({am, bm, σm²}) is expressed by integrating over the unknown true parameter values (Θp) and assuming statistical independence across patients [3].
Parameter Estimation: The linear model parameters (am, bm, σm²) that maximize the likelihood function are determined through numerical optimization techniques.
Performance Comparison: The estimated parameters for each modality (slope, intercept, and variance) are compared to assess relative accuracy (deviation of am from 1 and bm from 0) and precision (σm²).
This methodology enables researchers to objectively rank the performance of different imaging systems for estimation tasks without requiring an infallible gold standard, addressing a fundamental limitation in medical imaging validation [3].
Standardized Reporting: Node-RADS Criteria
For lymph node assessment in oncology, the Node Reporting and Data System (Node-RADS) provides a standardized methodology for classifying the degree of suspicion of lymph node involvement [4]. This system combines established imaging findings into a structured scoring approach with two primary categories: "size" and "configuration" [4]. The size criterion categorizes lymph nodes as "normal" (short-axis diameter <10 mm, with specific exceptions), "enlarged" (between normal and bulk definitions), or "bulk" (longest diameter ≥30 mm) [4]. The configuration score is derived from the sum of numerical values assigned to three sub-categories: "texture" (internal structure), "border" (evaluating possible extranodal extension), and "shape" (geometric form and fatty hilum preservation) [4]. These scores are combined to assign a final Node-RADS assessment category between 1 ("very low likelihood") and 5 ("very high likelihood") of malignant involvement, enhancing consistency in reporting across radiologists and institutions [4].
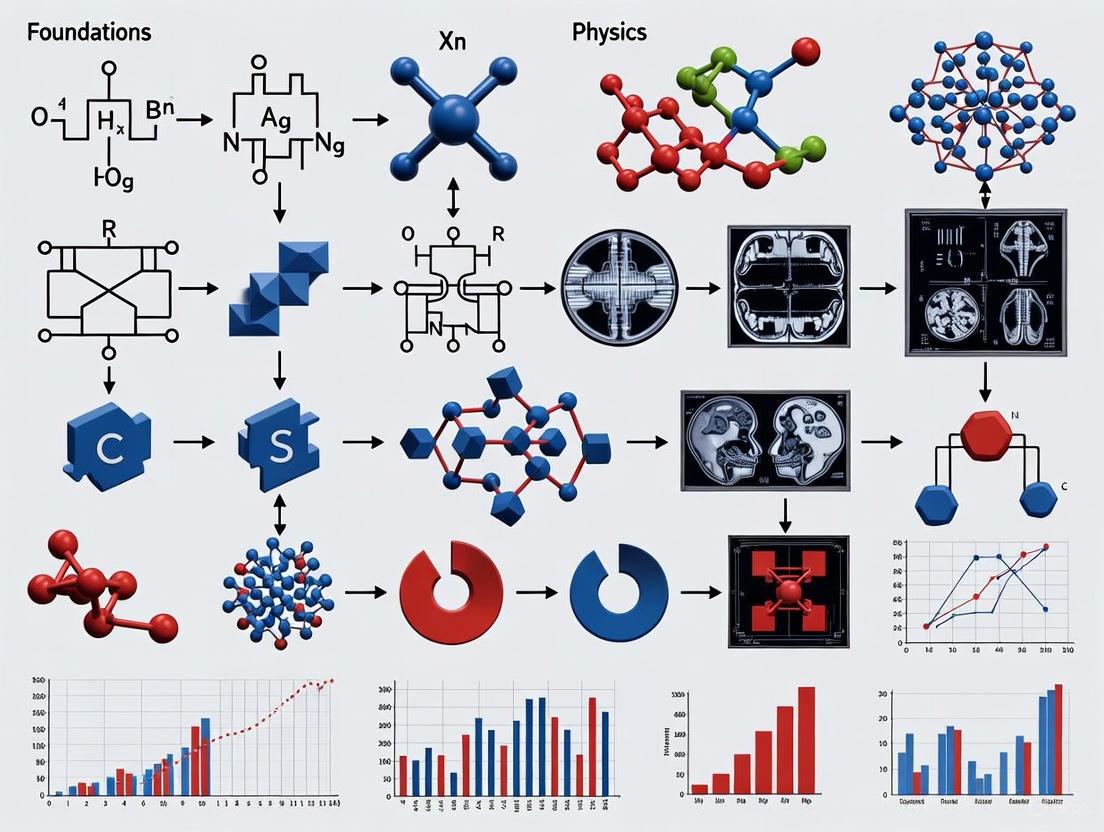
Visualization of Medical Imaging Physics Concepts
MRI Signal Formation and Detection Workflow
The following diagram illustrates the sequential physical processes involved in MRI signal formation, detection, and image reconstruction:
Node-RADS Classification Algorithm
The Node-RADS system provides a standardized methodology for lymph node assessment in oncology imaging, as visualized in the following decision workflow:
Research Reagent Solutions for Medical Imaging
Table 3: Essential Research Reagents and Materials for Medical Imaging Experiments
| Reagent/Material | Function/Application | Example Use Cases |
|---|---|---|
| Gadolinium-Based Contrast Agents | Paramagnetic contrast enhancement; shortens T1 relaxation time | Cerebral perfusion studies, tumor vascularity assessment, blood-brain barrier integrity evaluation [1] |
| Iron Oxide Nanoparticles | Superparamagnetic contrast; causes T2* shortening | Liver lesion characterization, cellular tracking, macrophage imaging [1] |
| Radiofrequency Coils | Signal transmission and reception; affects signal-to-noise ratio | High-resolution anatomical imaging, specialized applications (e.g., cardiac, neuro, musculoskeletal) [1] |
| Magnetic Field Gradients | Spatial encoding of MR signal; determines spatial resolution and image geometry | Slice selection, frequency encoding, phase encoding in MRI [1] |
| Photoacoustic Contrast Agents | Enhanced optical absorption for photoacoustic signal generation | Molecular imaging, targeted cancer detection, vascular mapping [2] |
| Computational Phantoms | Simulation of anatomical structures and physical processes | Imaging system validation, algorithm development, dose optimization |
The field of medical imaging represents one of the most transformative progressions in modern healthcare, fundamentally altering the diagnosis and treatment of human disease. This evolution from simple two-dimensional plane films to sophisticated hybrid and three-dimensional imaging systems exemplifies the convergence of engineering innovation and medical physics research. The journey began with Wilhelm Conrad Roentgen's seminal discovery of X-rays in 1895, which provided the first non-invasive window into the living human body [5] [6]. This breakthrough initiated a technological revolution that would eventually incorporate computed tomography, magnetic resonance imaging, and molecular imaging, each building upon foundational principles of physics and engineering.
Medical imaging engineering has progressed through distinct phases, each marked by increasing diagnostic capability. The initial era of projection radiography provided valuable but limited anatomical information, compressing three-dimensional structures into two-dimensional representations. The development of computed tomography (CT) in the 1970s addressed this limitation by enabling cross-sectional imaging, while magnetic resonance imaging (MRI) later provided unprecedented soft-tissue contrast without ionizing radiation [6] [7]. The contemporary era is defined by hybrid imaging systems that combine anatomical and functional information, and by advanced 3D visualization techniques that transform raw data into volumetric representations [8] [9]. These advancements have created a new paradigm in patient management, allowing clinicians to monitor molecular processes, anatomical changes, and treatment response with increasing precision. This whitepaper examines the historical progression, technical foundations, and future directions of medical imaging systems within the context of engineering and physics research.
The Era of Plane Film: Projection Radiography
The discovery of X-rays by Wilhelm Conrad Roentgen in 1895 marked the genesis of medical imaging, earning him the first Nobel Prize in Physics in 1901 [5] [9]. This foundational technology, initially termed "X-ray radiography" or "plane film," utilized electromagnetic radiation to project internal structures onto a photographic plate, creating a two-dimensional shadowgram of the body's composition [5]. The initial applications focused predominantly on skeletal imaging, allowing physicians to identify fractures, locate foreign objects, and diagnose bone pathologies without surgical intervention [6]. The technology rapidly became standard in medical practice, with fluoroscopy later enhancing its utility by providing real-time moving images [5] [7].
Despite its revolutionary impact, plane film radiography suffered from significant limitations inherent to its design. The technique compressed complex three-dimensional anatomy into a single two-dimensional plane, causing superposition of structures and complicating diagnostic interpretation [10]. Tissues with similar radiodensities, particularly soft tissues, provided poor contrast, limiting the assessment of organs, muscles, and vasculature [5]. Furthermore, the inability to precisely quantify the spatial relationships and dimensions of internal structures restricted its use for complex diagnostic and surgical planning purposes. These constraints drove the scientific community to pursue imaging technologies that could overcome the limitations of projective geometry and provide true dimensional information, setting the stage for the development of cross-sectional and three-dimensional imaging modalities.
Technological Revolutions: From Cross-Sectional to 3D Imaging
Computed Tomography (CT)
The invention of computed tomography in the 1970s by Godfrey Hounsfield represented a quantum leap in imaging technology, effectively ending the reign of plain film as the primary morphological tool [5] [6]. Unlike projection radiography, CT acquired multiple X-ray measurements from different angles around the body and used computational algorithms to reconstruct cross-sectional images [5]. This approach eliminated the problem of structural superposition, allowing clear visualization of internal organs, soft tissues, and pathological lesions. The original CT systems required several minutes for data acquisition, but technological advances led to progressively faster scan times, with modern multi-slice CT scanners capable of acquiring entire body volumes in seconds [5].
The fundamental engineering principle underlying CT is the reconstruction of internal structures from their projections. The mathematical foundation for this process was established by Johann Radon in 1917 with the Radon transform, which proved that a two-dimensional object could be uniquely reconstructed from an infinite set of its projections [5]. In practice, CT scanners implement this principle using a rotating X-ray source and detector array that measure attenuation profiles across the patient. These raw data are then processed using filtered back projection or iterative reconstruction algorithms to generate tomographic images [5]. The transition from analog to digital imaging further enhanced CT capabilities, improving image quality, processing efficiency, and enabling three-dimensional reconstructions through techniques like multiplanar reformation and volume rendering [7] [10].
Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging emerged in the 1980s as an alternative imaging modality that did not rely on ionizing radiation [6] [7]. Instead, MRI utilizes powerful magnetic fields and radiofrequency pulses to manipulate the spin of hydrogen nuclei in water and fat molecules, detecting the resulting signals to construct images with exceptional soft-tissue contrast [6]. This capability made MRI particularly valuable for neurological, musculoskeletal, and oncological applications where differentiation between similar tissues is crucial [10]. The development of functional MRI (fMRI) further expanded its utility by mapping brain activity through associated hemodynamic changes [10].
From a physics perspective, MRI exploits the quantum mechanical property of nuclear spin. When placed in a strong magnetic field, hydrogen nuclei align with or against the field, creating a net magnetization vector. Application of radiofrequency pulses at the resonant frequency excites these nuclei, causing them to emit signals as they return to equilibrium. Spatial encoding is achieved through magnetic field gradients, which create a one-to-one relationship between position and resonance frequency [10]. The engineering complexity of MRI systems lies in generating highly uniform and stable magnetic fields, precisely controlling gradient pulses, and detecting faint radiofrequency signals. Continued innovations in pulse sequences, parallel imaging, and high-field systems have consistently improved image quality, acquisition speed, and diagnostic capability.
Table 1: Evolution of Key Medical Imaging Modalities
| Modality | Decade Introduced | Physical Principle | Primary Clinical Applications |
|---|---|---|---|
| X-ray | 1890s | Ionizing radiation attenuation | Bone fractures, dental imaging, chest imaging |
| Ultrasound | 1950s | Reflection of high-frequency sound waves | Obstetrics, abdominal imaging, cardiac imaging |
| CT | 1970s | Computer-reconstructed X-ray attenuation | Trauma, cancer staging, vascular imaging |
| MRI | 1980s | Nuclear magnetic resonance of hydrogen atoms | Neurological disorders, musculoskeletal imaging, oncology |
| PET | 1970s (clinical 1990s) | Detection of positron-emitting radiotracers | Oncology, neurology, cardiology |
| SPECT | 1960s (clinical 1980s) | Detection of gamma-emitting radiotracers | Cardiology, bone scans, thyroid imaging |
Three-Dimensional Reconstruction and Visualization
The transition from two-dimensional slices to true three-dimensional imaging represents another milestone in medical imaging engineering. 3D medical imaging involves creating volumetric representations of internal structures, typically derived from multiple 2D image slices or projections [10]. This process has transformed diagnostic interpretation, surgical planning, and medical education by providing comprehensive views of anatomical relationships [10].
Several technical approaches enable 3D visualization in clinical practice. Volume rendering converts 2D data (such as CT or MRI slices) into a 3D volume, with each voxel assigned specific color and opacity based on its density or other properties [10]. Surface rendering involves extracting the surfaces of structures of interest from 2D data to create a 3D mesh, particularly useful for visualizing organ shape and size [10]. Multiplanar reconstruction reformats 2D image data into different planes, allowing creation of 3D images viewable from various angles [10]. Recent advances in computational photography have also enabled 3D reconstruction from multiple 2D images using photogrammetric techniques, though these are more applicable to external structures [11].
The development of 3D ultrasound created three-dimensional images of internal structures, while 4D ultrasound added the dimension of real-time imaging, allowing physicians to observe the movement of organs and systems [10]. In obstetrics, this technology revolutionized fetal imaging by enabling clinicians to assess development and identify abnormalities more effectively [10].
Hybrid Imaging Systems: The Convergence of Anatomy and Function
The Concept of Anato-Metabolic Imaging
Hybrid imaging represents the logical convergence of anatomical and functional imaging modalities, addressing the fundamental limitation of standalone systems that provide either structure or function but rarely both [8] [9]. The term "anato-metabolic imaging" describes this integration of anatomical and biological information, ideally acquired within a single examination [8] [9]. This approach recognizes that serious diseases often originate from molecular and physiological changes that may precede macroscopic anatomical alterations [8].
The clinical implementation of hybrid imaging began with software-based image fusion, which involved sophisticated co-registration of images from separate systems [8] [9]. While feasible for relatively rigid structures like the brain, accurate alignment throughout the body proved challenging due to the numerous degrees of freedom involved [8]. This limitation drove the development of "hardware fusion" – integrated systems that combined complementary imaging modalities within a single gantry [8] [9]. These hybrid systems, particularly PET/CT and SPECT/CT, revolutionized diagnostic imaging by providing inherently co-registered structural and functional information [8].
SPECT/CT and PET/CT Systems
The first combined SPECT/CT system was conceptualized in 1987 and realized commercially a decade later [9]. These systems integrated single photon emission computed tomography with computed tomography, initially using low-resolution CT for anatomical localization and attenuation correction [8]. Subsequent generations incorporated fully diagnostic CT systems with fast-rotation detectors capable of simultaneous acquisition of 16 or 64 detector rows [9]. This evolution significantly improved diagnostic performance, particularly in oncology, cardiology, and bone imaging [8] [9].
PET/CT development followed a similar trajectory, with the first prototype proposed in 1984 and the first whole-body system introduced in the late 1990s [9]. The combination of positron emission tomography's exceptional sensitivity for detecting metabolic activity with CT's detailed anatomical reference created a powerful tool for cancer staging, treatment monitoring, and neurological applications [9]. The success of PET/CT stems from several factors: logistical efficiency of a combined examination, superior diagnostic information from complementary data streams, and the ability to use CT data for attenuation correction of PET images [9].
PET/MR Systems
The combination of positron emission tomography with magnetic resonance imaging represents the most technologically advanced hybrid imaging platform [9]. Unlike PET/CT, PET/MR integration presented significant engineering challenges due to the incompatibility of conventional PET photomultiplier tubes with strong magnetic fields [9]. Two primary solutions emerged: spatially separated systems with active shielding of photomultiplier tubes, and integrated systems utilizing solid-state photodetectors (avalanche photodiodes or silicon photomultipliers) that function within magnetic fields [9].
PET/MR offers several advantages over PET/CT, including superior soft-tissue contrast, reduced ionizing radiation exposure (particularly beneficial for pediatric and longitudinal studies), and simultaneous rather than sequential data acquisition [9]. This simultaneity enables true temporal correlation of functional and morphological information, opening new possibilities for dynamic studies of physiological processes [9]. The multiparametric assessment capability of PET/MR, combining metabolic information from PET with various MR sequences (diffusion, perfusion, spectroscopy), provides a comprehensive biomarker platform for drug development and personalized medicine [9].
Table 2: Comparison of Hybrid Imaging Systems
| System Type | Key Technical Features | Primary Clinical Applications | Advantages |
|---|---|---|---|
| SPECT/CT | Gamma camera + 1-64 slice CT; Attenuation correction using CT data [8] [9] | Thyroid cancer, bone scans, parathyroid imaging, cardiac perfusion [8] | Wide range of established radiopharmaceuticals; improved anatomical localization over SPECT alone [8] |
| PET/CT | PET detector + multislice CT; Time-of-flight capability; CT-based attenuation correction [9] | Oncology staging/restaging, treatment response assessment, neurological disorders [9] | Logistically efficient; superior diagnostic accuracy; quantitative capabilities [9] |
| PET/MR | Silicon photomultipliers or APDs for MR compatibility; simultaneous acquisition [9] | Pediatric oncology, neurological disorders, musculoskeletal tumors, research applications [9] | Superior soft-tissue contrast; reduced radiation dose; multiparametric assessment [9] |
Experimental Protocols and Methodologies
3D Reconstruction Pipeline
The generation of three-dimensional models from two-dimensional image data follows a structured computational pipeline with distinct processing stages. Recent research has optimized this pipeline through specific modifications: (1) setting a minimum triangulation angle of 3° to improve geometric stability, (2) minimizing overall re-projection error by simultaneously optimizing all camera poses and 3D points in the bundle adjustment step, and (3) using a tiling buffer size of 1024 × 1024 pixels to generate detailed 3D models of complex objects [11]. This optimized approach has demonstrated robustness even with lower-quality input images, maintaining output quality while improving processing efficiency [11].
The technical workflow begins with feature detection and matching, where distinctive keypoints are identified across multiple images and correspondences are established [11]. The structure from motion step then estimates camera parameters and sparse 3D geometry [11]. Multi-view stereo algorithms subsequently generate dense point clouds, which are transformed into meshes through surface reconstruction [11]. The final stage involves texture mapping to apply photorealistic properties to the 3D model [11]. For medical applications using CT or MRI data, the pipeline typically employs volume rendering techniques that assign optical properties to voxels based on their intensity values, followed by ray casting to generate the final 3D visualization [10].
The Scientist's Toolkit: Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Hybrid Imaging
| Item | Function | Application Examples |
|---|---|---|
| ^99mTc-labeled compounds (e.g., ^99mTc-sestamibi, ^99mTc-MDP) | Single photon emitting radiotracer for SPECT imaging [5] [8] | Myocardial perfusion imaging (^99mTc-sestamibi) [8]; Bone scintigraphy (^99mTc-MDP) [8] |
| ^18F-FDG (Fluorodeoxyglucose) | Positron-emitting glucose analog for PET imaging [8] | Oncology (assessment of glucose metabolism in tumors) [8]; Neurology (epilepsy focus localization) |
| ^111In-pentetreotide | Gamma-emitting radiopharmaceutical targeting somatostatin receptors [8] | Neuroendocrine tumor imaging [8] |
| ^123I and ^131I | Gamma-emitting radioisotopes of iodine [8] | Thyroid cancer imaging and therapy [8] |
| Gadolinium-based contrast agents | Paramagnetic contrast agent for MRI | Contrast-enhanced MR angiography; tumor characterization |
| Iodinated contrast agents | X-ray attenuation enhancement for CT | Angiography; tissue perfusion studies |
| Silicon Photomultipliers (SiPMs) | Solid-state photodetectors for radiation detection [9] | PET detector components in PET/MR systems [9] |
| Quercetin 7-O-(6''-O-malonyl)-beta-D-glucoside | Quercetin 7-O-(6''-O-malonyl)-beta-D-glucoside, MF:C24H22O15, MW:550.4 g/mol | Chemical Reagent |
| 6',7'-Dihydroxybergamottin acetonide | 6',7'-Dihydroxybergamottin acetonide, MF:C24H28O6, MW:412.5 g/mol | Chemical Reagent |
Future Directions and Emerging Technologies
The future of medical imaging engineering is advancing along multiple innovative fronts, with artificial intelligence serving as a particularly transformative force. AI and machine learning algorithms are increasingly integrated throughout the imaging pipeline, from image acquisition and reconstruction to analysis and interpretation [2] [10]. Foundation AI models, with their scalability and broad applicability, possess transformative potential for medical imaging applications including automated image analysis, report generation, and data synthesis [2]. The MONAI (Medical Open Network for AI) framework represents a significant open-source initiative supporting these developments, with next-generation capabilities focusing on generative AI for image simulation and vision-language models for medical image co-pilots [2].
Hybrid imaging continues to evolve with emerging modalities like photoacoustic imaging, which combines optical and ultrasound technologies to provide high-resolution functional and molecular information from deep within biological tissues [2]. This technique shows particular promise for cancer detection, vascular imaging, and functional brain imaging [2]. Computational imaging approaches are also advancing, with techniques like lensless holographic microscopy offering sub-micrometer resolution from single holograms and computational miniature mesoscopes enabling single-shot 3D fluorescence imaging across wide fields of view [12].
The integration of imaging with augmented and virtual reality represents another frontier, creating immersive environments for surgical planning, medical education, and patient engagement [10]. These technologies leverage detailed 3D models derived from medical image data to provide intuitive visualizations of complex anatomy and pathology. Additionally, ongoing developments in detector technology, such as solid-state detectors and organ-specific system designs, continue to push the boundaries of spatial resolution, sensitivity, and quantitative accuracy in medical imaging [9]. These innovations collectively promise to enhance the role of imaging as a biomarker in drug development, enabling more precise assessment of therapeutic efficacy and accelerating the development of new treatments.
The historical progression from plane film to hybrid and 3D imaging systems demonstrates remarkable innovation in applying physics and engineering principles to medical challenges. Each technological advancement – from Roentgen's initial discovery to modern integrated PET/MR systems – has expanded our ability to visualize and understand human anatomy and physiology. This evolution has transformed medical imaging from a simple diagnostic tool to an indispensable technology supporting personalized medicine, drug development, and fundamental biological research.
The current era of hybrid and 3D imaging represents not an endpoint but a platform for future innovation. The convergence of artificial intelligence with advanced imaging technologies, development of novel contrast mechanisms and radiotracers, and creation of increasingly sophisticated visualization methods promise to further enhance our capability to investigate and treat human disease. For researchers, scientists, and drug development professionals, these advancements offer powerful tools for quantifying disease progression, evaluating treatment response, and understanding pathological processes at molecular and systemic levels. The continued collaboration between imaging scientists, clinical researchers, and industry partners will ensure that medical imaging remains at the forefront of medical innovation, building upon its rich history to create an even more impactful future.
Medical imaging is a cornerstone of modern healthcare and biomedical research, providing non-invasive windows into the human body. This technical guide provides an in-depth analysis of five fundamental imaging modalities—Computed Tomography (CT), Magnetic Resonance Imaging (MRI), Positron Emission Tomography (PET), Single-Photon Emission Computed Tomography (SPECT), and Ultrasound—within the context of imaging engineering and physics research. Each modality exploits different physical principles to generate contrast, yielding complementary information about anatomical structure, physiological function, and molecular processes. Understanding these core principles, technical capabilities, and limitations is essential for researchers developing novel imaging technologies, contrast agents, and computational methods, as well as for professionals applying these tools in drug development and clinical translation. This review synthesizes the fundamental engineering physics, current technological advancements, and experimental methodologies that define the state-of-the-art in medical imaging research.
Core Physical Principles and Technical Specifications
The diagnostic utility of each imaging modality is determined by its underlying physical principles and engineering implementation. The interaction of different energy forms with biological tissues creates contrast mechanisms that are captured and reconstructed into diagnostic images.
Fundamental Physics of Image Formation
Computed Tomography (CT) uses X-rays, which are a form of ionizing electromagnetic radiation. As X-rays pass through tissue, their attenuation is governed primarily by the photoelectric effect and Compton scattering [13]. The differential attenuation of these rays through tissues of varying density and atomic composition forms the basis of CT image contrast. The resulting attenuation data from multiple projections are reconstructed using algorithms like filtered back projection or iterative reconstruction to generate cross-sectional images representing tissue density in Hounsfield Units (HU) [14].
Magnetic Resonance Imaging (MRI) leverages the quantum mechanical properties of hydrogen nuclei (primarily in water and fat molecules) when placed in a strong magnetic field. When exposed to radiofrequency pulses at their resonant frequency, these protons absorb energy and transition to higher energy states. The subsequent return to equilibrium (relaxation) emits radiofrequency signals that are detected by receiver coils. The timing of pulse sequences (repetition time TR, echo time TE) weights the signal toward different tissue properties: proton density, T1 relaxation time (spin-lattice), or T2 relaxation time (spin-spin) [15] [14].
Positron Emission Tomography (PET) detects pairs of gamma photons produced indirectly by a positron-emitting radionuclide (tracer) introduced into the body. When a positron is emitted, it annihilates with an electron, producing two 511 keV gamma photons traveling in approximately opposite directions [16] [17]. Coincidence detection of these photon pairs by a ring of detectors allows localization of the tracer's concentration. The resulting images represent the spatial distribution of biochemical and physiological processes.
Single-Photon Emission Computed Tomography (SPECT) also uses gamma-ray-emitting radioactive tracers. Unlike PET, SPECT radionuclides decay directly, emitting single gamma photons [17]. These photons are detected by gamma cameras, typically equipped with collimators to determine the direction of incoming photons. Tomographic images are reconstructed from multiple 2D projections acquired at different angles, showing the 3D distribution of the radiopharmaceutical [16].
Ultrasound utilizes high-frequency sound waves (typically 1-20 MHz) generated by piezoelectric transducers. As these acoustic waves travel through tissues, they are reflected, refracted, scattered, and absorbed at interfaces between tissues with different acoustic impedances [14]. The reflected echoes detected by the transducer provide information about the depth and nature of tissue boundaries. Different modes (B-mode, Doppler, M-mode) process this echo information to create structural or functional images.
Table 1: Quantitative Technical Comparison of Imaging Modalities
| Parameter | CT | MRI | PET | SPECT | Ultrasound |
|---|---|---|---|---|---|
| Spatial Resolution | 0.2-0.5 mm [18] | 0.2-1.0 mm [18] | 4-6 mm [17] | 7-15 mm [17] | 0.1-2.0 mm (depth-dependent) [19] |
| Temporal Resolution | <1 sec | 50 ms - several min | 10 sec - several min | several min | 10-100 ms (real-time) |
| Penetration Depth | Unlimited (whole body) | Unlimited (whole body) | Unlimited (whole body) | Unlimited (whole body) | Centimeter range (depth/frequency trade-off) |
| Primary Contrast Mechanism | Electron Density, Atomic Number | Proton Density, T1/T2 Relaxation, Flow | Radiotracer Concentration | Radiotracer Concentration | Acoustic Impedance, Motion |
| Radiation Exposure | Yes (Ionizing) | No (Non-ionizing) | Yes (Ionizing) | Yes (Ionizing) | No (Non-ionizing) |
Advanced Engineering Implementations
Technological innovations continue to enhance the capabilities of each modality. Dual-Energy CT (DECT) utilizes two different X-ray energy spectra (e.g., 80 kVp and 140 kVp) to acquire datasets simultaneously. The differential attenuation of materials at these energies enables material decomposition, allowing generation of virtual non-contrast images, iodine maps, and virtual monoenergetic reconstructions [13]. Photon-Counting CT (PCCT), an emerging technology, uses energy-resolving detectors that count individual photons and sort them into energy bins, offering superior spatial resolution, noise reduction, and spectral imaging capabilities [13].
In MRI, the development of high-field systems (3T, 7T) increases signal-to-noise ratio, while advanced sequences like diffusion-weighted imaging (DWI), arterial spin labeling (ASL), and magnetic resonance spectroscopy (MRS) provide unique functional and metabolic information. Contrast-enhanced techniques rely on paramagnetic gadolinium-based contrast agents (GBCAs), which alter the relaxation times of surrounding water protons [15]. These are classified as extracellular, blood-pool, or hepatobiliary agents, each with specific pharmacokinetics and indications [15].
Hybrid imaging systems, such as PET/CT, PET/MRI, and SPECT/CT, combine the functional data from nuclear medicine with the anatomical detail of CT or MRI. This integration allows precise localization of metabolic activity and improves diagnostic accuracy [16]. Fusion imaging in ultrasound similarly overlays real-time ultrasound data with pre-acquired CT or MRI datasets, providing enhanced guidance for interventions and biopsies [19].
Research Applications & Experimental Protocols
The selection of an imaging modality in research is dictated by the specific biological question, required resolution, and the nature of the contrast mechanism being probed.
Protocol 1: Tumor Phenotyping with DECT
DECT enables quantitative tissue characterization beyond conventional CT.
- Objective: To differentiate intra-tumoral hemorrhage from iodine contrast staining in a neuro-oncology model.
- Experimental Workflow:
- Animal Model: Employ an orthotopic or transgenic brain tumor model.
- Image Acquisition: Acquire DECT data using a dual-source scanner (e.g., Source 1: 80 kVp, Source 2: 140 kVp) immediately after administration of an iodinated contrast agent.
- Post-processing: Reconstruct virtual monoenergetic images (VMI) at 40-70 keV and material-specific images (iodine and calcium maps) using a three-material decomposition algorithm [13].
- Data Analysis: Measure iodine concentration (mg/mL) within the lesion on iodine maps. On VMI, regions of iodine uptake will show higher attenuation at lower keV, while hemorrhage will not.
- Validation: Correlate DECT findings with post-mortem histology (Perls' Prussian blue for iron in hemorrhage).
Protocol 2: Target Engagement Study with PET
PET is the gold standard for quantitative in vivo assessment of target engagement in drug development.
- Objective: To quantify the occupancy of a novel dopamine D2 receptor antagonist in a non-human primate model.
- Experimental Workflow:
- Radiotracer: Use a specific D2 receptor ligand like [11C]Raclopride.
- Baseline Scan: Perform a 60-minute dynamic PET scan following IV bolus injection of [11C]Raclopride. Acquire arterial blood samples for input function generation.
- Intervention: Administer the candidate therapeutic compound at a predetermined dose.
- Post-Dose Scan: Repeat the dynamic PET scan at the time of expected peak plasma concentration of the therapeutic.
- Kinetic Modeling: Analyze dynamic data using a reference tissue model (e.g., simplified reference tissue model, SRTM) or compartmental modeling with the arterial input function to estimate binding potential (BP~ND~) in the striatum at baseline and post-dose [17].
- Data Analysis: Calculate receptor occupancy as:
Occupancy (%) = [1 - (BP~ND~ post-dose / BP~ND~ baseline)] * 100.
Protocol 3: Liver Fibrosis Staging with Ultrasound Elastography
This protocol assesses tissue mechanical properties, a biomarker for chronic liver disease.
- Objective: To non-invasively stage liver fibrosis in a pre-clinical model of steatohepatitis.
- Experimental Workflow:
- Animal Preparation: Anesthetize and shave the abdomen for adequate transducer contact.
- System Setup: Use an ultrasound system equipped with a shear wave elastography (SWE) module and a curved array transducer.
- Image Acquisition: Position the transducer in an intercostal view to visualize the right liver lobe. Activate the SWE mode and acquire a cine-loop of the liver while holding the transducer steady.
- Quantification: Place a region of interest (ROI) within the homogeneous color-coded elastography box in the liver parenchyma, avoiding large vessels. Record the mean Young's modulus value (in kilopascals, kPa) from multiple measurements [20].
- Validation: Compare ultrasound-derived stiffness measurements with the histopathological Metavir score from liver biopsy.
Diagram 1: Generic research imaging workflow.
The Scientist's Toolkit: Research Reagents & Materials
The fidelity of imaging experiments is critically dependent on the reagents and materials used to generate contrast and ensure experimental validity.
Table 2: Essential Research Reagents and Materials
| Item | Primary Function | Exemplars & Research Context |
|---|---|---|
| Iodinated Contrast Media | Increases X-ray attenuation in vasculature and perfused tissues for CT angiography and perfusion studies. | Iohexol, Iopamidol. Used in DECT to generate iodine maps for quantifying tumor vascularity [13]. |
| Gadolinium-Based Contrast Agents (GBCAs) | Shortens T1 relaxation time, enhancing signal on T1-weighted MRI. | Gadoteridol (macrocyclic, non-ionic). Used for CNS and whole-body contrast-enhanced MRI to delineate pathology [15]. |
| PET Radionuclides & Ligands | Serves as a positron emitter for labeling molecules to track biological processes. | [¹¹C]Raclopride (half-life ~20 min) for neuroreceptor imaging; [¹â¸F]FDG (half-life ~110 min) for glucose metabolism [16] [17]. |
| SPECT Radionuclides & Ligands | Gamma emitter for labeling molecules, allowing longer imaging windows than PET. | Technetium-99m (half-life ~6 hrs), often bound to HMPAO for cerebral blood flow; Indium-111 for labeling antibodies [16] [17]. |
| Anthropomorphic Phantoms | Mimics human tissue properties for validating image quality, dosimetry, and reconstruction algorithms. | 3D-Printed Phantoms. Custom-fabricated using materials tuned to mimic CT Hounsfield Units or MRI relaxation times of various tissues [18]. |
| High-Frequency Ultrasound Probes | Increases spatial resolution for imaging superficial structures in preclinical research. | >20 MHz Transducers. Provide cellular-level resolution for dermatological, ophthalmic, and vascular small-animal imaging [19] [20]. |
| 21,24-Epoxycycloartane-3,25-diol | 21,24-Epoxycycloartane-3,25-diol, MF:C30H50O3, MW:458.7 g/mol | Chemical Reagent |
| 20S,24R-Epoxydammar-12,25-diol-3-one | 20S,24R-Epoxydammar-12,25-diol-3-one, MF:C30H50O4, MW:474.7 g/mol | Chemical Reagent |
Emerging Frontiers & Engineering Challenges
The field of medical imaging is rapidly evolving, driven by engineering innovations and computational advancements.
Artificial Intelligence (AI) and Quantitative Imaging: AI is transforming image reconstruction, denoising, segmentation, and diagnostic interpretation [21] [20]. Deep learning models can automatically detect tumors in breast ultrasound and segment fetal anatomy in obstetric scans [20]. However, challenges such as the "black box" problem, model generalizability across diverse populations, and "alert fatigue" among radiologists need to be addressed through rigorous validation and evolving regulatory frameworks like the EU AI Act [21].
3D Printing of Physical Phantoms: Additive manufacturing enables the creation of sophisticated, patient-specific phantoms for validating imaging protocols and reconstruction algorithms [18]. Current limitations include printer resolution and the limited library of materials that accurately mimic all tissue properties (e.g., simultaneously replicating density, speed of sound, and attenuation) [18].
Miniaturization and Point-of-Care Systems: The proliferation of portable and handheld devices, particularly in ultrasound (POCUS), is democratizing access to diagnostic imaging [19] [20]. These devices empower clinicians in emergency, critical care, and low-resource settings but raise important questions regarding quality assurance and operator training.
Therapeutic Integration: Imaging is increasingly guiding therapy. Techniques like High-Intensity Focused Ultrasound (HIFU) and histotripsy use focused ultrasound energy for non-invasive tumor ablation [20]. Furthermore, focused ultrasound can transiently open the blood-brain barrier, enabling targeted drug delivery to the brain [20].
Diagram 2: Key drivers in imaging technology.
CT, MRI, PET, SPECT, and Ultrasound form a powerful, complementary arsenal in the medical imaging engineering landscape. Each modality, grounded in distinct physical principles, offers unique advantages for probing anatomical, functional, and molecular phenomena in biomedical research. The ongoing convergence of these technologies with artificial intelligence, material science, and miniaturization is pushing the boundaries of diagnostic sensitivity and specificity. For researchers and drug development professionals, a deep understanding of the engineering physics, experimental protocols, and emerging capabilities of these modalities is paramount for designing robust studies, interpreting complex data, and driving the next wave of innovation in personalized medicine. The future of medical imaging lies in the intelligent integration of these multimodal data streams to provide a holistic, quantitative view of health and disease.
Radiation is a fundamental physical phenomenon that plays a critical role in medical imaging, therapeutic applications, and scientific research. Understanding the mechanisms by which radiation interacts with biological tissues is paramount for optimizing diagnostic techniques, developing effective radiation therapies, and ensuring safety for both patients and healthcare professionals. This technical guide provides an in-depth examination of radiation-tissue interactions, focusing on the biological consequences at molecular, cellular, and systemic levels, while framing these concepts within the foundations of medical imaging engineering and physics research. The content is structured to serve researchers, scientists, and drug development professionals who require a comprehensive synthesis of current knowledge, experimental methodologies, and safety frameworks governing radiation use in biomedical contexts.
Radiation is broadly categorized as either ionizing or non-ionizing, based on its ability to displace electrons from atoms and molecules [22] [23]. Ionizing radiation, which includes X-rays, gamma rays, and particulate radiation (alpha, beta particles), carries sufficient energy to ionize biological molecules directly. Non-ionizing radiation, encompassing ultraviolet (UV) radiation, visible light, infrared, microwaves, and radio waves, typically lacks this ionization energy but can still excite atoms and molecules, leading to various biological effects [22]. The energy deposition characteristics of ionizing radiation are described by its linear energy transfer (LET), which classifies radiation as either high-LET (densely ionizing, such as alpha particles and neutrons) or low-LET (sparsely ionizing, such as X-rays and gamma rays) [22]. This distinction is crucial as high-LET radiation causes more complex and challenging-to-repair cellular damage per unit dose compared to low-LET radiation [22].
Fundamental Mechanisms of Radiation-Tissue Interaction
Physical Energy Deposition and Direct Effects
The interaction of ionizing radiation with biological matter occurs through discrete energy deposition events. In aqueous systems, these events are classified based on the energy deposited: spurs (<100 eV, ~4 nm diameter), blobs (100-500 eV, ~7 nm diameter), and short tracks (>500 eV) [22]. These classifications help model the initial non-homogeneous distribution of radiation-induced chemical products within biological systems. The direct effect of radiation occurs when energy is deposited directly in critical biomolecular targets, particularly DNA, resulting in ionization and molecular breakage. This direct interaction breaks chemical bonds and can cause various types of DNA lesions, including single-strand breaks (SSBs), double-strand breaks (DSBs), base damage, and DNA-protein cross-links [22].
Table 1: Classification of Radiation Types and Their Key Characteristics
| Radiation Type | Ionizing/Non-Ionizing | LET Category | Primary Sources | Penetration Ability |
|---|---|---|---|---|
| Alpha particles | Ionizing | High | Radon decay, radioactive elements | Low (stopped by skin or paper) |
| Beta particles | Ionizing | Low to Medium | Radioactive decay | Moderate (stopped by thin aluminum) |
| X-rays | Ionizing | Low | Medical imaging, X-ray tubes | High |
| Gamma rays | Ionizing | Low | Nuclear decay, radiotherapy | Very high |
| Neutrons | Ionizing | High | Nuclear reactors, particle accelerators | Very high |
| Ultraviolet (UV) | Non-ionizing (borderline) | N/A | Sunlight, UV lamps | Low (mostly epidermal) |
| Visible light | Non-ionizing | N/A | Sunlight, artificial lighting | Moderate (superficial) |
| Radiofrequency | Non-ionizing | N/A | Communication devices | High |
Indirect Effects and Radical-Mediated Damage
In biological systems composed primarily of water, the indirect effect of radiation plays a significant role in cellular damage. When ionizing radiation interacts with water molecules, it leads to radiolysis, generating highly reactive species including hydroxyl radicals (OH•), hydrogen atoms (H•), and hydrated electrons (eâ»aq) [22] [23]. These reactive products, particularly hydroxyl radicals, can diffuse to critical cellular targets and damage DNA, proteins, and lipids. Approximately two-thirds of the biological damage from low-LET radiation is attributed to these indirect effects [23]. The presence of oxygen in tissues can fix radiation damage by forming peroxy radicals, making well-oxygenated cells generally more radiosensitive than hypoxic cells—a phenomenon with significant implications for radiotherapy of tumors with poor vasculature.
The diagram below illustrates the fundamental pathways of radiation-induced biological damage:
Molecular and Cellular Responses to Radiation
DNA Damage and Repair Mechanisms
DNA represents the most critical target for radiation-induced biological damage due to its central role in cellular function and inheritance. Ionizing radiation creates various types of DNA lesions, with double-strand breaks (DSBs) being particularly significant because of their lethality and potential for mis-repair, which can lead to chromosomal aberrations such as translocations and dicentrics [22]. The complexity of DNA damage depends on radiation quality, with high-LET radiation producing more complex, clustered lesions that are challenging for cellular repair systems to process correctly [22]. Recent research has revealed that ionizing radiation also induces alterations in the three-dimensional (3D) architecture of the genome, affecting topologically associating domains (TADs) in an ATM-dependent manner, which influences DNA repair efficiency and gene regulation [22].
Beyond DNA damage, radiation induces significant alterations to RNA molecules, including strand breaks and oxidative modifications [22]. Damage to protein-coding RNAs and non-coding RNAs can disrupt protein synthesis and gene expression regulation. Specific techniques, such as adding poly(A) tails to broken RNA termini for RT-PCR detection, have been developed to study radiation-induced RNA damage [22]. Long non-coding RNAs (lncRNAs) have emerged as crucial regulators of biological processes affected by radiation, with approximately 70% of the human genome being transcribed into RNA while only 2-2.5% codes for proteins, suggesting extensive regulatory networks potentially disrupted by radiation exposure [22].
Cellular Response Pathways and Fate Decisions
Following radiation-induced damage, cells activate complex response networks that determine their fate. The diagram below illustrates the key cellular decision-making pathways after radiation exposure:
Cells exhibit different sensitivity to radiation based on their proliferation status, differentiation state, and tissue of origin. Rapidly dividing cells, such as those in bone marrow and the gastrointestinal system, are particularly vulnerable to radiation damage [23]. At low doses (below 0.2-0.3 Gy for low-LET radiation), some cell types exhibit hyper-radiosensitivity (HRS), where they demonstrate increased radiosensitivity compared to what would be predicted from higher-dose responses [24]. This phenomenon may occur because lower radiation doses fail to activate full DNA damage repair mechanisms efficiently. Additionally, exposure to low radiation doses can sometimes induce an adaptive response, where pre-exposure to low doses protects cells against subsequent higher-dose exposure, potentially through priming of DNA repair and antioxidant systems [24].
Non-Targeted Effects and Bystander Signaling
Radiation effects are not limited to directly irradiated cells. Non-targeted effects, including bystander effects and genomic instability in the progeny of irradiated cells, contribute significantly to the overall biological response [24]. Bystander effects refer to biological responses observed in cells that were not directly traversed by radiation but received signals from irradiated neighboring cells. These effects are mediated through two primary mechanisms: secretion of soluble factors by irradiated cells and direct signaling through cell-to-cell junctions [24]. The radiation-induced bystander effect (RIBE) has the greatest influence on DSB induction at doses up to 10 mGy and follows a super-linear relationship with dose [24]. Additionally, radiation-induced genomic instability (RIGI) manifests as a delayed appearance of de novo chromosomal aberrations, gene mutations, and reproductive cell death in the progeny of irradiated cells many generations after the initial exposure [24].
Quantitative Radiation Dosimetry and Safety Standards
Dosimetry Metrics and Reference Levels
Accurate radiation dosimetry is essential for quantifying exposure, assessing biological risks, and implementing protective measures. The fundamental dosimetric quantities include absorbed dose (energy deposited per unit mass, measured in milligrays, mGy), equivalent dose (accounting for radiation type effectiveness, measured in millisieverts, mSv), and effective dose (sum of organ-weighted equivalent doses, measured in mSv) [25]. For computed tomography (CT) imaging, specific standardized metrics have been established, including CTDIvol (volume CT dose index) and DLP (dose-length product) [26]. Regulatory bodies have established reference levels and pass/fail criteria for various imaging protocols to ensure patient safety while maintaining diagnostic image quality.
Table 2: ACR CT Dose Reference Levels and Pass/Fail Criteria [26]
| Examination Type | Phantom Size | Reference Level CTDIvol (mGy) | Pass/Fail Criteria CTDIvol (mGy) |
|---|---|---|---|
| Adult Head | 16 cm | 75 | 80 |
| Adult Abdomen | 32 cm | 25 | 30 |
| Pediatric Head (1-year-old) | 16 cm | 35 | 40 |
| Pediatric Abdomen (40-50 lb) | 16 cm | 15 | 20 |
| Pediatric Abdomen (40-50 lb) | 32 cm | 7.5 | 10 |
Radiation Protection Principles and Safety Implementation
Radiation protection follows three fundamental principles: justification (ensuring the benefits outweigh the risks), optimization (keeping doses As Low As Reasonably Achievable, known as the ALARA principle), and dose limitation (applying dose limits to occupational exposure) [25]. For medical staff working with radiation, practical protection strategies include minimizing exposure duration, maximizing distance from the source (following the inverse square law), and employing appropriate shielding [25]. Personal protective equipment (PPE) for radiation includes lead aprons (typically 0.25-0.5 mm lead equivalence), thyroid shields, and leaded eyeglasses, which can reduce eye lens exposure by up to 90% [25]. Regular use of dosimeters for monitoring cumulative radiation exposure is essential for at-risk healthcare personnel, though compliance remains challenging, with studies indicating that up to 50% of physicians do not wear or incorrectly wear dosimeters [25].
Experimental Methodologies for Studying Radiation Effects
In Vitro and In Vivo Radiation Biology Techniques
The study of radiation effects on biological systems employs diverse experimental approaches spanning molecular, cellular, tissue, and whole-organism levels. Standardized protocols have been developed for quantifying specific radiation-induced lesions, such as double-strand breaks, using techniques like the γ-H2AX foci formation assay detected through flow cytometry or fluorescence microscopy [22]. For RNA damage assessment, researchers have established methods to detect strand breaks using RT-PCR with poly(A) tail addition to broken RNA termini [22]. Advanced spectroscopic techniques, including Fourier transform infrared (FT-IR) and Raman micro-spectroscopy, have been fruitfully employed to monitor radiation-induced biochemical changes in cells and tissues non-destructively [24]. These vibrational spectroscopies provide detailed information about molecular alterations in proteins, lipids, and nucleic acids following radiation exposure.
Recent systems biology approaches have integrated multi-omics data to elucidate complex radiation response networks. A 2025 study employed heterogeneous gene regulatory network analysis combining miRNA and gene expression profiles from human peripheral blood lymphocytes exposed to acute 2Gy gamma-ray irradiation [27]. This approach identified 179 key molecules (23 transcription factors, 10 miRNAs, and 146 genes) and 5 key modules associated with radiation response, providing insights into regulatory networks governing processes such as cell cycle regulation, cytidine deamination, cell differentiation, viral carcinogenesis, and apoptosis [27]. Such integrative methodologies offer comprehensive perspectives on the molecular mechanisms of radiation action beyond single-marker studies.
Table 3: Essential Research Reagents and Methods for Radiation Biology Studies
| Research Tool Category | Specific Examples | Primary Applications | Technical Considerations |
|---|---|---|---|
| DNA Damage Detection | γ-H2AX antibody, Comet assay, PCR-based break detection | Quantifying DSBs, SSBs, and other DNA lesions | Sensitivity varies by method; γ-H2AX is DSB-specific |
| RNA Damage Assessment | Poly(A) tailing RT-PCR, RNA sequencing | Detecting RNA strand breaks and oxidative damage | Specialized protocols needed for damaged RNA |
| Vibrational Spectroscopy | FT-IR, Raman micro-spectroscopy | Non-destructive biomolecular analysis of cells/tissues | Requires specialized instrumentation and data analysis |
| Cell Viability Assays | Clonogenic survival, MTT, apoptosis assays | Measuring reproductive death and cell survival | Clonogenic assay is gold standard for survival |
| Omics Technologies | Transcriptomics, miRNA profiling, network analysis | Systems-level understanding of radiation response | Bioinformatics expertise required for data interpretation |
| Radiation Sources | Clinical linear accelerators, gamma irradiators, X-ray units | Delivering precise radiation doses to biological samples | Dose calibration and quality assurance critical |
Experimental Workflow for Comprehensive Radiation Studies
The diagram below illustrates a systematic research workflow for investigating radiation effects using integrated experimental approaches:
Emerging Concepts and Therapeutic Applications
Nanotechnology and Radiation Medicine
Nanotechnology offers innovative approaches to enhance the efficacy of radiation therapy while mitigating damaging effects on normal tissues. Nanoparticles can serve as radiosensitizers when incorporated into tumor cells, increasing the local radiation dose through various physical mechanisms, including enhanced energy deposition and generation of additional secondary electrons [22]. High-atomic number (high-Z) nanomaterials, such as gold nanoparticles, exhibit enhanced absorption of X-rays compared to soft tissues, making them promising agents for dose localization in tumor targets. Additionally, nanotechnology-based platforms are being developed for targeted delivery of radioprotective agents to normal tissues, potentially reducing side effects during radiotherapy [22]. These approaches aim to overcome radioresistance in certain tumor types by interfering with DNA repair pathways or targeting hypoxic regions within tumors.
Radiation Modifiers and Drug Development
Research into chemical compounds that modify radiation response represents an active area of therapeutic development. Natural products, including polyphenols, flavonoids, and alkaloids, demonstrate promising radioprotective effects by scavenging reactive oxygen species and enhancing DNA repair mechanisms [28]. Conversely, radiosensitizers such as chemotherapeutic agents (e.g., cisplatin) can enhance radiation-induced damage in tumor cells, particularly when combined with inhibitors of DNA repair pathways like poly(ADP-ribose) polymerase (PARP) inhibitors [28]. A 2025 network pharmacology study identified several potential therapeutic compounds for alleviating radiation-induced damage, including small molecules like Navitoclax and Traditional Chinese Medicine ingredients such as Genistin and Saikosaponin D, which may target specific radiation-response pathways identified through systems biology approaches [27].
The field of radiation-tissue interaction continues to evolve with emerging technologies and methodologies. Advanced imaging techniques, artificial intelligence applications in treatment planning and response assessment, and novel targeted radionuclide therapies are expanding the therapeutic window for radiation-based treatments. Future research directions include refining personalized approaches based on individual radiation sensitivity profiles, developing more sophisticated normal tissue protection strategies, and integrating multi-omics data to predict treatment outcomes and long-term effects. These advances, grounded in fundamental understanding of radiation physics and biology, promise to enhance both the safety and efficacy of radiation applications in medicine and beyond.
The field of radiology has long been a fertile ground for the application of artificial intelligence (AI), primarily utilizing deep learning for specific, narrow tasks such as nodule detection or organ segmentation. These traditional models, while effective, are characterized by their limited scope and requirement for vast amounts of high-quality, manually labeled data for each distinct task [29]. The recent emergence of foundation models (FMs) represents a significant paradigm shift, moving beyond conventional, narrowly focused AI systems toward versatile base models that serve as adaptable starting points for numerous downstream applications [29] [30]. These large-scale AI models are pre-trained on massive, diverse datasets and can be efficiently adapted to various tasks with minimal fine-tuning, offering radiology unprecedented capabilities for multimodal integration, improved generalizability, and greater adaptability across the complex landscape of medical imaging [29].
This shift is particularly consequential for medical imaging engineering and physics, as FMs fundamentally alter how we approach image analysis, interpretation, and integration with other data modalities. The transformer architecture, with its attention mechanism that effectively captures long-range dependencies and contextual relationships within data, has become the technical backbone enabling this transition [29]. For researchers and drug development professionals, this evolution opens new frontiers in precision medicine, enabling more sophisticated analysis of imaging biomarkers, drug response monitoring, and integrative diagnostics that combine imaging with clinical, laboratory, and genomic data [29].
Fundamental Concepts and Technical Architecture
Core Architectural Principles
Foundation models distinguish themselves through several transformative technical characteristics. Unlike traditional AI models engineered for single tasks, FMs are developed through large-scale pre-training using self-supervised learning, allowing them to learn rich data representations by solving pretext tasks such as predicting masked portions of an image or text [29]. This pre-training phase leverages unstructured, unlabeled, or weakly labeled data, significantly reducing the dependency on costly, expert-annotated datasets that have traditionally bottlenecked medical AI development [29].
A defining capability of FMs is their strong transfer learning through efficient fine-tuning. The general knowledge acquired during resource-intensive pre-training can be effectively utilized for new, specific tasks with minimal task-specific data. This facilitates few-shot learning (using only a small number of task-specific examples) and even zero-shot learning (using no examples), where models adapt with substantially less specific data than conventional approaches demand [29]. For instance, an FM pre-trained via self-supervised learning on large chest X-ray datasets may be fine-tuned for rib fracture detection using only dozens of cases, whereas a conventional model might require thousands to achieve comparable performance [29].
Multimodal Integration Framework
For radiology, a development of particular importance is the capacity of FMs to be multimodal, processing and integrating diverse data types including images (X-rays, CT, MRI), text (reports, EHR documents), and potentially more [29]. The technical architecture enabling this integration involves several sophisticated components:
- Modality-specific encoders: These components compress high-dimensional inputs (such as CT scans or text reports) into lower-dimensional embeddings, capturing essential features like tissue density, anatomical structures, and radiological terms [29].
- Cross-modal alignment: Techniques like contrastive learning are employed during pre-training, where the model learns to associate matching image-report pairs by adjusting weights so their embeddings are pulled closer together in a conceptual "shared space" [29].
- Fusion modules: After individual encoders process their respective inputs, fusion mechanisms like cross-attention dynamically weigh the relevance of different parts of one modality based on the content of another [29].
- Decoders: These components transform the fused representations into desired outputs, which could range from generating text reports to segmenting relevant image regions [29].
The Transformer Backbone
The transformer architecture serves as the fundamental backbone for most foundation models, originally revolutionizing natural language processing and subsequently adapting for vision and multimodal scenarios [29]. Its central innovation—the attention mechanism—enables the model to focus on specific elements of the input sequence, effectively capturing long-range dependencies and contextual relationships within data [29]. This capability proves particularly valuable in radiology contexts, where pathological findings often depend on understanding complex anatomical relationships across multiple image slices or combining visual patterns with clinical context from reports.
Experimental Methodologies and Validation Frameworks
Pre-training Approaches for Radiology FMs
The development of radiology-specific foundation models employs several sophisticated methodological approaches, each with distinct experimental protocols:
Masked Autoencoding: This methodology involves randomly masking portions of medical images during training and tasking the model with predicting the missing parts [30]. This self-supervised approach forces the model to learn robust representations of anatomical structures and pathological patterns without requiring labeled data. The experimental protocol typically involves dividing images into patches, masking a significant proportion (often 60-80%), and training the model to reconstruct the original content through iterative optimization.
Contrastive Learning: This approach trains models to learn consistent numerical characterizations of images despite alterations to their content [30]. The experimental design creates positive pairs (different augmentations of the same image) and negative pairs (different images), with the model trained to minimize distance between positive pairs while maximizing distance between negative pairs in the embedding space. This technique proves particularly effective for learning invariances to irrelevant variations in medical images while preserving sensitivity to clinically significant findings.
Report-Image Alignment: Models are trained to associate specific image findings with corresponding radiological descriptions [30]. This methodology typically uses a dual-encoder architecture, with one network processing images and another processing text, trained using contrastive objectives to align matching image-report pairs in a shared embedding space. This approach enables the model to learn clinically meaningful representations grounded in radiological expertise.
Benchmarking and Evaluation Metrics
Rigorous evaluation of foundation models requires multifaceted assessment strategies beyond traditional performance metrics:
Table 1: Comprehensive Evaluation Framework for Radiology Foundation Models
| Evaluation Dimension | Key Metrics | Assessment Method |
|---|---|---|
| Diagnostic Accuracy | AUC-ROC, Sensitivity, Specificity, Precision | Retrospective validation on curated datasets with expert annotations |
| Generalizability | Performance degradation across institutions, scanner types, patient demographics | Cross-site validation using datasets from multiple healthcare systems |
| Multimodal Integration | Cross-modal retrieval accuracy, Report generation quality | Task-specific evaluation of image-to-text and text-to-image alignment |
| Robustness | Performance under distribution shift, Adversarial robustness | Stress testing with corrupted data, out-of-distribution samples |
| Fairness | Performance disparities across demographic groups | Subgroup analysis by age, gender, race, socioeconomic status |
Implementation Workflows
The transition from narrow AI to foundation models introduces new operational workflows for research and clinical implementation:
Applications and Performance in Radiology
Transformative Applications
Foundation models enable transformative applications across the radiology workflow, significantly expanding capabilities beyond traditional narrow AI:
Automated Report Generation and Augmentation: FMs can generate preliminary radiology reports based on image findings, with the potential to enhance radiologist productivity and reduce reporting turnaround times [29]. Advanced models can create findings-specific descriptions while maintaining nuanced clinical context, though challenges remain in ensuring accuracy and mitigating hallucination of non-existent findings.
Multimodal Integrative Diagnostics: By simultaneously processing images, textual reports, laboratory results, and clinical history, FMs can provide comprehensive diagnostic assessments that account for the full clinical picture [29]. This capability aligns particularly well with precision medicine initiatives, where treatment decisions increasingly depend on synthesizing diverse data sources.
Cross-lingual Report Translation: The natural language capabilities of FMs enable accurate translation of radiology reports between languages while preserving clinical meaning and terminology precision [29]. This facilitates international collaboration, medical tourism, and care for diverse patient populations.
Synthetic Data Generation: FMs can generate high-quality synthetic medical images for training and validation purposes, helping address data scarcity for rare conditions while maintaining patient privacy [29]. This application proves particularly valuable for drug development research, where collecting sufficient imaging data for clinical trials can be challenging.
Quantitative Performance Assessment
Empirical studies demonstrate the substantial performance advantages of foundation models compared to traditional approaches:
Table 2: Performance Comparison: Foundation Models vs. Traditional AI in Radiology Applications
| Application Domain | Traditional AI Performance | Foundation Model Performance | Data Efficiency Advantage |
|---|---|---|---|
| Chest X-ray Abnormality Detection | AUC: 0.87-0.92 (task-specific models) | AUC: 0.93-0.96 (multimodal FMs) | 5-10x reduction in labeled data requirements |
| CT Report Generation | BLEU-1: 0.32-0.38 (template-based) | BLEU-1: 0.41-0.47 (FM-based) | Zero-shot capability for unseen findings |
| Multimodal Disease Classification | Accuracy: 76-82% (image-only models) | Accuracy: 85-89% (multimodal FMs) | Effective cross-modal inference |
| Rare Condition Identification | Sensitivity: 0.45-0.60 (low-prevalence classes) | Sensitivity: 0.65-0.78 (few-shot FM adaptation) | Viable detection with 10-100 examples |
The performance advantages are particularly pronounced in scenarios with limited labeled data, where FMs demonstrate remarkable few-shot and zero-shot learning capabilities [29]. This data efficiency has significant implications for medical imaging research and drug development, where obtaining expert annotations represents a major bottleneck.
Technical Implementation and Research Toolkit
Successful development and implementation of foundation models in radiology requires sophisticated technical infrastructure and methodological components:
Table 3: Essential Research Toolkit for Radiology Foundation Models
| Component Category | Specific Solutions | Function and Application |
|---|---|---|
| Model Architectures | Vision Transformers (ViT), Multimodal Transformers, Adaptors | Backbone networks for processing images, text, and clinical data |
| Pre-training Strategies | Masked Autoencoding, Contrastive Learning, Cross-modal Alignment | Self-supervised objectives for learning representations without labels |
| Data Resources | Multimodal datasets (images with reports), Public benchmarks (MIMIC-CXR, CheXpert) | Training and validation data with necessary scale and diversity |
| Validation Frameworks | Domain-specific benchmarks (RadImageNet), Fairness assessment tools | Standardized evaluation protocols for clinical reliability |
| Computational Infrastructure | High-performance GPU clusters, Distributed training frameworks | Hardware and software for training large-scale models |
| Ecdysterone 20,22-monoacetonide | Ecdysterone 20,22-monoacetonide, MF:C30H48O7, MW:520.7 g/mol | Chemical Reagent |
| 1,10:4,5-Diepoxy-7(11)-germacren-8-one | 1,10:4,5-Diepoxy-7(11)-germacren-8-one, MF:C15H22O3, MW:250.33 g/mol | Chemical Reagent |
Technical Implementation Considerations
The architectural decisions for implementing foundation models in radiology involve several critical considerations that impact model capability and clinical utility:
Challenges and Future Directions
Critical Challenges in Clinical Translation
Despite their transformative potential, foundation models face several substantial challenges that must be addressed for successful clinical integration:
Interpretability and Transparency: The inherent complexity and opacity of FM decision-making processes present significant barriers to clinical adoption [29] [30]. Radiologists and clinicians require understandable rationale for AI-generated findings to maintain appropriate oversight and trust. Developing effective explanation interfaces that highlight relevant image regions and contextual factors remains an active research challenge.
Hallucination and Stochasticity: FMs can generate plausible but incorrect outputs, including hallucinated findings in generated reports or spurious detection of non-existent pathologies [29]. Managing this stochasticity and ensuring deterministic performance for critical findings is essential for clinical safety. Current research focuses on confidence calibration, uncertainty quantification, and output verification mechanisms.
Data Privacy and Security: The extensive data requirements for FM development raise significant concerns regarding patient privacy and data protection [29]. Federated learning approaches, differential privacy, and synthetic data generation offer promising pathways to mitigate these concerns while maintaining model performance.
Regulatory and Validation Complexity: The adaptable nature of FMs challenges traditional medical device regulatory frameworks designed for fixed-functionality software [30]. Establishing appropriate validation protocols for models that can be continuously adapted or prompt-engineered for new tasks requires novel regulatory science approaches.
Promising Research Directions
Several emerging research directions show particular promise for advancing foundation models in radiology:
Federated Foundation Models: Approaches that enable model development across institutions without centralizing sensitive patient data address critical privacy concerns while maintaining performance [30]. These methodologies are particularly relevant for rare conditions where data aggregation across multiple centers is necessary to achieve statistical power.
Causal Representation Learning: Incorporating causal reasoning capabilities into FMs could enhance their robustness to distribution shifts and improve generalization across patient populations and imaging protocols [31]. This direction aligns with the need for models that maintain performance as imaging technology evolves.
Human-AI Collaboration Frameworks: Developing specialized interaction paradigms that leverage FM capabilities while maintaining appropriate radiologist oversight represents a critical direction for clinical translation [30]. These frameworks aim to augment rather than replace radiologist expertise, particularly for tedious screening tasks or complex multimodality integration.
Lifelong Learning Systems: Creating mechanisms for continuous model adaptation and validation in clinical practice addresses the challenge of model degradation over time [30]. Such systems would enable FMs to evolve with changing clinical practices, patient populations, and imaging technology while maintaining safety and performance standards.
The paradigm shift from narrow AI to versatile foundation models represents a fundamental transformation in how artificial intelligence is conceived, developed, and applied in radiology. These models offer unprecedented capabilities for multimodal integration, data-efficient adaptation, and comprehensive diagnostic support that aligns with the complex reality of clinical practice. For medical imaging engineering and physics research, this shift opens new frontiers in image analysis, biomarker development, and integrative diagnostics that could significantly accelerate precision medicine and therapeutic development.
However, realizing this potential requires addressing substantial technical and translational challenges, including ensuring model transparency, managing stochasticity, protecting patient privacy, and establishing appropriate regulatory frameworks. The international collaborative effort between clinical radiologists, medical physicists, AI researchers, and industry partners will be essential to navigate these challenges responsibly. As foundation models continue to evolve, their thoughtful integration into radiology practice holds the promise of enhancing diagnostic accuracy, expanding access to expertise, and ultimately improving patient care through more precise, personalized imaging assessment.
Advanced Applications and Workflow Integration in Research and Diagnostics
In the field of medical imaging engineering and physics research, the paradigm is shifting from unimodal to multimodal analysis. Traditional unimodal models, which operate on a single data type like only images or only text, fail to capture the comprehensive auxiliary information essential for holistic clinical decision-making [32]. Multimodal data fusion addresses this limitation by systematically integrating complementary biological and clinical data sources such as medical imaging, electronic health records (EHRs), genomic data, and laboratory results [33]. This approach provides a multidimensional perspective of patient health, enhancing the diagnosis, treatment, and management of various medical conditions. The foundational principle is that data from different modalities—text, image, speech, video—carry complementary information about diverse aspects of a task, object, or event [32]. Solving a problem using a multimodal approach provides a more complete understanding, mirroring how clinicians reason by combining visual, numerical, and narrative information to arrive at a medical conclusion [34].
The work in medical physics and engineering is bifurcated: one strand focuses on developing next-generation imaging techniques, such as hyperpolarized magnetic resonance imaging, applying quantum mechanics to extract molecular information not commonly present in existing modalities. The other strand refines and coregisters existing imaging and treatment modalities to make them clinically useful [35]. Multimodal fusion sits at the crossroads of these endeavors, providing the computational framework to integrate these advanced, physics-driven measurements with routine clinical data.
Core Fusion Architectures: From Theory to Implementation
The technical core of multimodal integration lies in its fusion algorithms. These architectures define how information from different modalities is combined, with the choice of architecture significantly impacting the model's ability to learn cross-modal interactions and its performance on clinical tasks.
Table 1: Comparison of Multimodal Fusion Approaches in Healthcare AI
| Fusion Approach | Description | Advantages | Limitations | Example Applications |
|---|---|---|---|---|
| Early Fusion | Raw inputs from different modalities are integrated before feature extraction [34]. | Captures raw-level, fine-grained interactions between modalities [34]. | Difficult to harmonize different data formats and scales; less commonly used in healthcare [34]. | Integrating MRI scans with pixel-aligned segmentation maps and structured data [34]. |
| Intermediate Fusion | Each modality is encoded into embeddings (feature vectors), which are fused before the final prediction layer [34]. | Learns complex interactions between modalities, leading to better accuracy and generalization [34]. | Requires carefully aligned data; can be computationally demanding [34]. | Concatenating image features from CNNs with text embeddings from ClinicalBERT [34]. |
| Late Fusion | Each modality is processed separately; outputs or decisions are combined at the very end using ensemble methods [34]. | Highly flexible, works with missing data, easier to implement [34]. | Limited cross-modal interaction, as integration happens only at the decision level [34]. | Combining predictions from an image model and a separate text model with weighted averaging [34]. |
| Specialized Architectures | Domain-specific models like Graph Neural Networks (GNNs) and Vision-Language models [34]. | Tailored to specific healthcare tasks, supports advanced applications like drug response prediction [34]. | Often still experimental; requires specialized, labeled datasets [34]. | GNNs for modeling relationships between clinical variables and biological pathways [34]. |
The evolution of fusion techniques has moved from simple methods like canonical correlation analysis (CCA) and concatenation to more sophisticated models based on attention mechanisms and transformer networks. These advanced models are crucial as they reduce the semantic gap between different modalities and better preserve their intrinsic correlations [32]. For instance, transformer-based architectures, originally developed for natural language processing (NLP), have shown remarkable success in learning these cross-modal relationships in a unified manner.
A Generic Workflow for Multimodal Fusion
The following diagram illustrates a standard pipeline for developing a multimodal AI system, from data collection to final decision support, incorporating the different fusion points.
Applications and Experimental Protocols in Clinical Research
Multimodal fusion has demonstrated transformative potential across various clinical domains, most notably in oncology and ophthalmology, where its application enhances tumor characterization, personalizes treatment, and aids in early diagnosis [33].
Application in Oncology: Enhanced Tumor Characterization and Treatment
In oncology, the integration of multimodal data enables more precise tumor characterization and personalized treatment plans [33]. For instance, pathological images and omics data are commonly fused for accurate tumor classification. Dedicated feature extractors, such as a trained CNN for images and a deep neural network for genomic data, are used. The resulting multimodal features are integrated via a fusion model to predict molecular subtypes of cancer with high accuracy [33]. This approach can be extended to pan-cancer studies.
Experimental Protocol: Predicting Immunotherapy Response A seminal study by Chen et al. demonstrated a multimodal model for predicting response to anti-human epidermal growth factor receptor 2 (HER2) therapy [33]. The methodology can be broken down as follows:
Data Acquisition: Collect multimodal patient data, including:
- Radiology Images: Standard-of-care CT or MRI scans.
- Pathology Slides: Digitized histopathology slides (e.g., H&E stains).
- Clinical Variables: Patient history, lab values, and performance status.
Feature Extraction:
- Imaging Features: Extract quantitative radiomic features (shape, texture, intensity) from regions of interest (ROIs) in the radiology scans using a pre-defined radiomics software platform.
- Pathology Features: Use a pre-trained CNN (e.g., ResNet) to extract deep feature embeddings from the digitized whole-slide images.
- Clinical Features: Encode structured clinical variables into a numerical vector.
Data Fusion and Model Training:
- Fuse the extracted radiomic, pathologic, and clinical feature vectors into a unified multimodal representation.
- Train a classifier (e.g., a deep neural network or random forest) on this fused dataset to predict the binary outcome of therapy response (Responder vs. Non-Responder). Use patient outcomes as ground truth labels.
Validation: Evaluate the model on a held-out test set using the Area Under the Receiver Operating Characteristic Curve (AUC). The model by Chen et al. achieved an AUC of 0.91, significantly outperforming single-modality models [33].
Table 2: Essential Research Reagents and Computational Tools for Multimodal Oncology Experiments
| Item / Reagent Solution | Function in Experimental Protocol |
|---|---|
| Digitized Histopathology Slides | Provides high-resolution tissue morphology data for feature extraction via Convolutional Neural Networks (CNNs) [33]. |
| Pre-trained CNN Models (e.g., VGGNet, ResNET) | Serves as a feature extractor for imaging data, converting pixels into meaningful, high-level feature representations [32] [33]. |
| Radiomics Software Platform | Enables the extraction of quantitative, hand-crafted features from medical images like CT and MRI scans [33]. |
| Clinical Data Encoder | Transforms structured clinical variables (e.g., lab results, patient demographics) into a numerical format suitable for machine learning models [34]. |
| Multimodal Fusion Framework | The software architecture (e.g., in Python/PyTorch) that implements the fusion strategy (early, intermediate, late) and the final predictive classifier [34]. |
Technical Implementation and Workflow
Building upon the experimental protocol, the following diagram details the computational workflow for a multimodal predictive model, from data input to performance validation.
Challenges and Future Directions in Medical Physics Research
Despite its promising potential, the widespread clinical deployment of multimodal data fusion faces several significant challenges rooted in data, computation, and model interpretability.
- Data Standardization and Heterogeneity: The sheer volume and heterogeneity of multimodal data require sophisticated methodologies. Data from different sources (EHRs, imaging archives, genomic databases) have unique formats and require tailored preprocessing, making standardization a major hurdle [33] [34].
- Computational Bottlenecks: Model training and deployment face computational bottlenecks, especially when processing large-scale multimodal datasets with complex fusion architectures like transformers [33].
- Model Interpretability: For clinical adoption, it is critical that models provide clinically meaningful explanations for their predictions. Enhancing interpretability using techniques like Shapley value analysis and attention visualization is an active area of research to build physician trust [33] [34].
- Handling Data Incompleteness: Real-world clinical datasets are often incomplete. Developing robust methods, such as learnable placeholder embeddings and imputation techniques, to handle missing modalities is essential for real-world robustness [34].
The future of multimodal fusion in medical physics and engineering is poised to be shaped by the development of large-scale multimodal models (LMMs). Models like Med-PaLM M demonstrate this trend; a generalist model that can process text, medical images, and genomic data with a single set of model weights, matching or outperforming specialist models across diverse biomedical tasks [34]. Furthermore, the integration of advanced imaging modalities from physics research, such as hyperpolarized MR and multispectral imaging, will provide even richer datasets for fusion, promising to further revolutionize personalized healthcare [35] [33].
The integration of artificial intelligence with diffusion-weighted magnetic resonance imaging (DW-MRI) is catalyzing a paradigm shift in the field of quantitative neuroimaging. While Fractional Anisotropy (FA) has served as a cornerstone metric for assessing white matter microstructure, emerging AI methodologies are now unlocking a new generation of biomarkers that extend far beyond this single parameter. This whitepaper examines the technical foundations, validation frameworks, and clinical applications of these advanced AI-powered biomarkers, with particular emphasis on their growing importance in accelerating therapeutic development and advancing precision medicine in neurological disorders.
Diffusion-weighted MRI has established itself as a fundamental modality for probing tissue microstructure in vivo by measuring the random, thermal motion of water molecules [36]. The technique leverages the pulsed gradient spin echo sequence, where signal attenuation is quantitatively described by the Stejskal-Tanner equation:
[ S(b) = S_0 e^{-bD} ]
where (S(b)) is the signal intensity with diffusion weighting, (S_0) is the signal without diffusion weighting, (b) is the diffusion weighting factor (b-value), and (D) is the diffusion coefficient [36] [37]. In biological tissues, where barriers impede free water diffusion, this becomes the Apparent Diffusion Coefficient (ADC).
Diffusion Tensor Imaging (DTI) expanded this framework to characterize anisotropic diffusion, modeling water diffusion as a 3×3 tensor from which key parameters like Fractional Anisotropy (FA) could be derived [36]. FA quantitatively represents the degree of directional preference of water diffusion, ranging from 0 (perfectly isotropic) to 1 (perfectly anisotropic), and has become one of the most widely used metrics for assessing white matter integrity in both research and clinical settings [38].
However, the DTI model embodies significant simplifications that limit its biological specificity. The assumption of a single, Gaussian diffusion compartment fails to capture the complex microstructural environment of cerebral tissue, where axons, glial cells, and other structures create multiple diffusion compartments [36]. This limitation has driven the development of advanced models and, more recently, the application of artificial intelligence to extract more nuanced, clinically relevant information from diffusion data.
The Limitations of Conventional Fractional Anisotropy
Despite its widespread adoption, FA possesses several inherent limitations as a quantitative biomarker. As a scalar metric, FA reduces the complex directional information of the diffusion tensor to a single value, discarding potentially valuable orientation data. Furthermore, FA is non-specific; changes in FA can result from various microstructural alterations including changes in axonal density, myelination, fiber coherence, or even edema and inflammation [36]. This lack of pathological specificity severely limits its utility in characterizing complex neurological diseases or monitoring targeted therapeutic interventions.
From a practical standpoint, acquiring high-fidelity FA maps traditionally requires lengthy acquisition sequences with multiple diffusion-encoding directions to reliably estimate the diffusion tensor, often taking several minutes per subject [39] [40]. This extended acquisition time increases vulnerability to motion artifacts and limits clinical throughput, particularly in patient populations with limited capacity to remain still.
Table 1: Key Limitations of Conventional Fractional Anisotropy
| Limitation Category | Specific Challenge | Impact on Biomarker Utility |
|---|---|---|
| Biological Specificity | Non-specific to underlying pathology | Cannot distinguish between different disease processes (e.g., inflammation vs. neurodegeneration) |
| Technical Constraints | Requires multiple diffusion directions for accurate tensor estimation | Lengthy acquisition times increasing motion sensitivity and reducing clinical feasibility |
| Modeling Limitations | Assumes single Gaussian compartment | Oversimplifies complex tissue architecture containing multiple restricted compartments |
| Analytical Complexity | Scalar metric discards directional information | Limited capacity to characterize complex fiber architectures and crossing pathways |
AI-Enhanced Acquisition and Reconstruction
Deep learning (DL) approaches are fundamentally addressing the acquisition speed limitations of conventional DW-MRI. A prominent research direction involves using neural networks to generate high-quality FA maps from significantly reduced input data, effectively accelerating acquisition times.
Experimental Protocol: Evaluating DL-FA with Reduced Inputs
A critical investigation by Gaviraghi et al. systematically evaluated the performance and clinical sensitivity of DL networks trained to calculate FA maps using different numbers of input DW volumes [39] [40]. The methodology provides a template for validating such AI-accelerated biomarkers:
- Training Dataset: Networks were trained on the Human Connectome Project (HCP) dataset, which provides high-resolution data with many DW volumes, enabling the generation of high-fidelity "ground truth" FA maps.
- Network Architectures: Separate DL networks were developed and trained using only 4, 7, or 10 (the previously established "one-minute FA") DW volumes as input.
- Generalization Testing: To assess real-world applicability, the trained networks were tested on two external clinical datasets acquired on different scanners with different protocols from the training data, featuring patients with Multiple Sclerosis and Temporal Lobe Epilepsy.
- Performance Metrics: Quantitative comparison of FA values against ground truth and, crucially, assessment of clinical sensitivity—the ability to detect statistically significant differences between patient groups and controls.
The findings revealed a critical limitation: while networks trained with only 4 or 7 DW volumes could produce FA maps with values matching the ground truth on HCP test data, they lost pathological sensitivity on the external clinical datasets, failing to consistently differentiate patient groups [39] [40]. In contrast, the "one-minute FA" network using 10 inputs maintained clinical sensitivity, establishing a practical lower bound for reliable data reduction using this specific approach. This underscores that technical performance on clean test data does not guarantee retained clinical utility, especially when models are applied to heterogeneous clinical data from different scanners and populations.
AI-Powered FA Reconstruction Workflow
Beyond FA: AI-Driven Microstructural Biomarkers
AI is enabling a move beyond the diffusion tensor model to extract more biologically specific parameters from diffusion data. These approaches typically leverage multi-shell acquisition data and relate the complex diffusion signal to microstructural features.
Advanced Biophysical Models
Multi-compartment models such as NODDI (Neurite Orientation Dispersion and Density Imaging) and CHARMED (Composite Hindered and Restricted Model of Diffusion) provide estimates of specific microstructural properties including axonal density, orientation dispersion, and axonal diameter [36]. However, these models traditionally require long acquisitions and complex, often unstable fitting procedures. DL approaches can stabilize these estimations, reduce scan time by predicting parameters from undersampled data, and enhance reproducibility.
Direct Feature Learning from Diffusion Data
Instead of relying on predefined biophysical models, some AI approaches learn relevant features directly from the raw or preprocessed diffusion data using convolutional neural networks (CNNs) or recurrent neural networks (RNNs). These models can identify complex, multi-scale patterns in the data that may not be captured by conventional model-based parameters, potentially discovering novel imaging signatures of disease.
Validation and Generalization in Clinical Applications
The transition of AI-powered biomarkers from research tools to clinical and drug development applications requires rigorous validation focused on generalizability and clinical utility.
The Multi-Stage Validation Pathway
For an AI-derived biomarker to be considered "fit-for-purpose" in drug development, it must undergo a structured validation process analogous to that established for traditional imaging biomarkers [41] [42]. This pathway, adapted for AI-specific challenges, is visualized below:
AI Biomarker Validation Pathway
Application in Drug Development: A Strategic Framework
Imaging biomarkers, including those derived from advanced DW-MRI, play increasingly critical roles across the drug development continuum [41] [43] [42]. They provide objective, quantifiable measures for:
- Target Engagement: Verifying that a drug interacts with its intended biological target in the human brain.
- Proof-of-Concept: Providing early evidence of biological activity in human subjects.
- Patient Stratification: Identifying patient subgroups most likely to respond to treatment.
- Treatment Response Monitoring: Objectively quantifying changes in tissue microstructure in response to therapy.
Table 2: Roles of Advanced DW-MRI Biomarkers in Drug Development
| Development Stage | Biomarker Application | AI-Enhanced Value |
|---|---|---|
| Target Discovery | Identifying novel pathological pathways and therapeutic targets | Unsupervised learning to discover novel imaging signatures linked to molecular pathways |
| Early Phase Trials | Establishing target engagement and proof-of-concept | Increased sensitivity to detect subtle, early biological effects; reduced sample size requirements |
| Phase II/III Trials | Patient enrichment/stratification; efficacy monitoring | Multi-parametric biomarkers for precise patient selection; reduced acquisition times for improved feasibility |
| Clinical Practice | Treatment response monitoring and personalized management | Automated, reproducible analysis enabling longitudinal tracking of individual patients |
The case of neuropsychiatric disorders illustrates this potential. In schizophrenia research, where developing treatments for cognitive and negative symptoms remains a major challenge, pharmacological neuroimaging using advanced biomarkers may provide critical response biomarkers for early decision-making, particularly in proof-of-concept studies leveraging challenge models in healthy volunteers [43].
The Scientist's Toolkit: Essential Research Reagents
The development and validation of AI-powered DW-MRI biomarkers requires a specific set of data, computational tools, and validation frameworks.
Table 3: Essential Research Reagents for AI-Driven DW-MRI Biomarker Development
| Tool Category | Specific Resource | Function and Importance |
|---|---|---|
| Reference Datasets | Human Connectome Project (HCP) data | Provides high-quality, multi-shell diffusion data with extensive sampling for training and benchmarking [39] [40] |
| Clinical Validation Cohorts | Well-characterized patient cohorts (e.g., MS, epilepsy, neurodegenerative diseases) | Enables assessment of clinical sensitivity and generalizability to real-world populations [39] |
| Deep Learning Frameworks | TensorFlow, PyTorch with medical imaging extensions (e.g., MONAI) | Provides flexible environment for developing and training custom network architectures for diffusion data |
| Diffusion MRI Processing Libraries | FSL, MRtrix3, Dipy | Enable standard preprocessing (eddy current correction, registration) and conventional parameter mapping for comparison [38] |
| Computational Hardware | High-performance GPUs (e.g., NVIDIA A100, H100) | Accelerates training of complex models on large-scale neuroimaging datasets |
| Isomucronulatol 7-O-glucoside | Isomucronulatol 7-O-glucoside, MF:C23H28O10, MW:464.5 g/mol | Chemical Reagent |
| Antitrypanosomal agent 16 | Antitrypanosomal agent 16, MF:C12H8BrN3O3, MW:322.11 g/mol | Chemical Reagent |
AI-powered quantitative biomarkers represent a significant advancement beyond Fractional Anisotropy in DW-MRI, offering enhanced biological specificity, reduced acquisition times, and discovery of novel disease signatures. However, their successful translation into clinical research and drug development hinges on addressing critical challenges related to generalizability, validation, and regulatory qualification. As these technologies mature, they hold immense promise for transforming how we develop and evaluate therapies for neurological and psychiatric disorders, ultimately accelerating the delivery of effective treatments to patients. The future will likely see increased integration of multi-modal data—combining advanced diffusion metrics with other imaging modalities, genomic data, and digital health technologies—to create comprehensive, individualized portraits of brain health and treatment response.
Automated Machine Learning (AutoML) for Accessible Medical Image Analysis
Automated Machine Learning (AutoML) represents a transformative shift in biomedical research, aiming to automate the end-to-end process of applying machine learning (ML) to real-world problems. Within medical imaging, a field deeply rooted in the physical principles of image acquisition and the engineering challenges of signal processing, AutoML is emerging as a critical tool for democratizing advanced image analysis. By automating complex tasks such as data preprocessing, feature engineering, model selection, and hyperparameter tuning, AutoML reduces the extensive expertise and resources traditionally required to develop effective ML models, thereby accelerating the deployment of AI solutions in clinical and research settings [44].
The integration of AutoML into the medical imaging workflow aligns with the core objectives of imaging engineering: to enhance diagnostic accuracy, improve operational efficiency, and derive reproducible, quantitative insights from complex image data. This technical guide explores the foundations of AutoML, its specific applications in medical image analysis, and provides a detailed examination of experimental protocols and key resources, providing researchers and drug development professionals with a framework for its practical implementation.
Technical Foundations of AutoML in Medical Imaging
AutoML systems are designed to automate the multi-stage pipeline of building a machine learning model. In the context of medical imaging, this involves several critical steps that must respect the unique characteristics of medical image data.
The AutoML Pipeline
A typical AutoML pipeline for medical image analysis involves a sequence of automated decisions, from data preparation to model deployment. The automation covers key stages that would otherwise require significant manual intervention from data scientists and domain experts.
Diagram 1: The automated machine learning pipeline for medical image analysis, showing the sequential stages from raw data to deployed model.
Core Automation Strategies
AutoML frameworks employ sophisticated strategies to navigate the complex space of possible ML pipelines. Neural Architecture Search (NAS) represents a foundational advancement, using reinforcement learning or evolutionary algorithms to automatically design optimal neural network architectures for specific tasks and datasets [45]. This is particularly valuable in medical imaging, where the optimal network architecture may vary significantly across imaging modalities and clinical questions.
Complementing NAS, hyperparameter optimization methods such as Bayesian optimization efficiently search the high-dimensional space of model parameters. This automation is crucial for researchers without deep ML expertise, as it systematically identifies configurations that would be difficult to discover manually. Furthermore, meta-learning leverages knowledge from previous ML tasks on similar datasets to accelerate and improve the automation process on new medical imaging problems, effectively transferring learned experience across domains [45].
AutoML Applications in Medical Image Analysis
The application of AutoML in medical imaging spans various modalities and clinical tasks, with particular strength in areas where standardized, quantitative analysis can augment clinical expertise.
Primary Application Areas
- Diagnostic Prediction and Detection: AutoML systems are increasingly deployed to identify pathological findings from medical images, such as detecting tumors, hemorrhages, or other abnormalities. These systems can serve as triage tools or secondary readers, potentially reducing interpretation time and increasing diagnostic consistency [44].
- Image Segmentation: This represents one of the most successful applications of AutoML in medical imaging. Automated segmentation of organs, lesions, and other anatomical structures is crucial for quantitative analysis, treatment planning, and monitoring disease progression. AutoML frameworks excel at adapting segmentation models to specific datasets and imaging protocols without manual re-engineering [46].
- Treatment Response Assessment: By automating the extraction of quantitative imaging biomarkers from serial scans, AutoML can help objectively assess how a disease is responding to therapy. This is particularly relevant in oncology drug development, where precise measurement of tumor changes is critical for evaluating treatment efficacy [44].
Data Types and Learning Paradigms
AutoML applications in medicine most frequently utilize structured numeric data (e.g., extracted radiomic features, patient demographics) and image data from modalities like CT, MRI, and ultrasound [44]. The dominant learning paradigm is supervised learning, where models are trained on images with corresponding expert annotations (e.g., radiologist-derived segmentations or diagnoses). This reliance on high-quality labeled data presents both a challenge and an opportunity for the field, driving interest in semi-supervised and self-supervised approaches that can leverage the vast quantities of unlabeled medical images available in clinical archives.
Experimental Protocols and Performance Evaluation
Rigorous evaluation is essential for validating AutoML frameworks in the clinically sensitive domain of medical imaging. The following section details a representative experimental protocol for benchmarking AutoML performance in an abdominal organ segmentation task, a common prerequisite for radiation therapy planning and surgical navigation.
Experimental Methodology
A recent study provided a comprehensive evaluation of AutoML frameworks for abdominal organ segmentation in CT images, offering a robust template for experimental design [46].
Dataset:
- Source: Abdominal Multi-Organ Segmentation (AMOS) 2022 Grand Challenge dataset [46].
- Content: 500 CT scans with voxel-level annotations for 15 abdominal organs (spleen, kidneys, gallbladder, esophagus, stomach, aorta, postcava, adrenal glands, duodenum, bladder, prostate/uterus) [46].
- Data Splits: 122 scans for training, 72 scans for hold-out validation. The test set consisted of 30 cases for qualitative expert evaluation [46].
Frameworks Benchmarked:
- AutoML Frameworks: nnU-Net, Auto3DSeg (from MONAI) [46].
- Non-AutoML Baseline: SwinUNETR (a state-of-the-art transformer-based model) [46].
Training Protocol:
- Each framework was trained on the same 122 training images.
- A consistent 5-fold cross-validation scheme was applied to minimize training cohort bias.
- Bilateral organs (e.g., left/right kidney) were combined into single labels to leverage left-right flip data augmentation [46].
Evaluation Metrics:
- Quantitative: Dice Similarity Coefficient (DSC), Surface DSC (sDSC), and 95th Percentile Hausdorff Distance (HD95) were calculated on the hold-out validation set [46].
- Qualitative: Three physicians performed a blinded evaluation of 30 auto-contoured test cases, providing ratings on a Likert scale to assess clinical viability and preference [46].
Diagram 2: Experimental workflow for benchmarking AutoML frameworks, showing data partitioning, model training, and multi-faceted evaluation.
Quantitative Performance Results
The benchmarking study demonstrated superior performance of AutoML frameworks over the state-of-the-art non-AutoML approach across multiple metrics. The table below summarizes the key quantitative findings.
Table 1: Performance Comparison of AutoML vs. Non-AutoML Frameworks for Abdominal Organ Segmentation on CT [46]
| Framework | Type | Average DSC | Average sDSC | Average HD95 | Statistical Significance (vs. SwinUNETR) |
|---|---|---|---|---|---|
| nnU-Net | AutoML | 0.924 | 0.938 | 4.26 | All OARs (P > 0.05) in all metrics |
| Auto3DSeg | AutoML | 0.902 | 0.919 | 8.76 | 13/13 OARs (P > 0.05) in DSC & sDSC; 12/13 OARs (P > 0.05) in HD95 |
| SwinUNETR | Non-AutoML | 0.837 | 0.844 | 13.93 | (Baseline) |
DSC: Dice Similarity Coefficient; sDSC: Surface Dice Similarity Coefficient; HD95: 95th Percentile Hausdorff Distance (in mm); OAR: Organs at Risk
The quantitative results show a clear performance advantage for AutoML methods. nnU-Net achieved the highest scores across all three metrics, indicating superior segmentation overlap (DSC), boundary accuracy (sDSC), and worst-case surface error (HD95). The statistical analysis confirms that these improvements are significant for nearly all organs when compared to the non-AutoML SwinUNETR model [46].
Qualitative Clinical Evaluation
The blinded assessment by physicians provided crucial insight into the clinical viability of the AutoML-generated segmentations. The qualitative evaluation used a Likert scale, where higher scores indicate greater clinical acceptability.
Table 2: Physician Preference Scores from Blinded Evaluation of Auto-Generated Segmentations [46]
| Framework | Median Likert Score | Qualitative Preference |
|---|---|---|
| nnU-Net | 4.57 | Highest |
| Auto3DSeg | 4.49 | Intermediate |
| SwinUNETR | (Not reported) | Lowest |
The physician evaluation corroborated the quantitative findings, with nnU-Net receiving the highest median Likert score (4.57). Furthermore, in a direct comparison, nnU-Net was qualitatively preferred over Auto3DSeg with a statistically significant difference (P=0.0027) [46]. This underscores that the performance advantages of AutoML frameworks are not just numerical but are perceptible and meaningful to clinical experts, a critical consideration for integration into real-world workflows.
Implementation Toolkit for Researchers
For researchers and drug development professionals embarking on AutoML projects for medical image analysis, a specific set of tools and resources is essential. The following table details key components of the research reagent solutions required for such work.
Table 3: Essential Research Reagent Solutions for AutoML in Medical Image Analysis
| Item / Resource | Type | Primary Function | Examples |
|---|---|---|---|
| AutoML Frameworks | Software | Provides end-to-end automation for building ML models, handling preprocessing, architecture search, and hyperparameter tuning. | nnU-Net, Auto3DSeg (MONAI) [46] |
| Public Image Datasets | Data | Serves as benchmark for training and validating models; essential for reproducibility and comparative studies. | AMOS22 CT Dataset [46] |
| Evaluation Metrics | Analytical Tool | Quantifies model performance from technical (algorithmic) and clinical (anatomical) perspectives. | Dice Similarity Coefficient (DSC), Surface DSC, Hausdorff Distance (HD95) [46] |
| Clinical Evaluation Protocol | Methodology | Assesses the real-world clinical utility and acceptability of the model's output by domain experts. | Blinded reader studies with Likert-scale scoring [46] |
| High-Performance Computing | Infrastructure | Accelerates the computationally intensive model training and hyperparameter optimization processes. | Cloud-based AutoML platforms (e.g., Google Cloud AutoML, Amazon SageMaker) [45] |
| 1,3-Dihydroxy-2-methoxyxanthone | 1,3-Dihydroxy-2-methoxyxanthone, CAS:87339-74-0, MF:C14H10O5, MW:258.23 g/mol | Chemical Reagent | Bench Chemicals |
Challenges and Future Directions
Despite its promise, the implementation of AutoML in medical imaging faces several significant challenges. Data quality and availability remain paramount, as AutoML models require large, well-annotated datasets for optimal performance, which are often difficult and expensive to curate in medicine [44]. Furthermore, the "black-box" nature of some automated models can hinder clinical adoption, creating an urgent need for the integration of Explainable AI (XAI) techniques within AutoML pipelines to build trust and facilitate model interpretation by clinicians and regulatory bodies [44].
Future progress in the field will likely focus on developing more data-efficient AutoML methods that can perform well with limited annotated examples, a common scenario in medical imaging. There is also a growing emphasis on creating interoperable and standardized AutoML tools that can seamlessly integrate into existing clinical PACS (Picture Archiving and Communication System) and radiology workflow management systems, thereby minimizing disruption and maximizing utility [44] [47]. As these technical and operational challenges are addressed, AutoML is poised to become an indispensable component of the medical imaging research and clinical toolkit.
Specialized medical imaging forms the engineering backbone of precision medicine, enabling the transition from generalized diagnostic approaches to highly individualized patient management. In precision medicine, medical decisions, treatments, and practices are tailored to individual patient subgroups based on their unique genetic, environmental, and experiential characteristics rather than applying a one-size-fits-all model [48]. Advanced imaging modalities provide the non-invasive, quantitative data essential for this deep phenotyping, with imaging physics and engineering principles directly enabling the extraction of clinically actionable information.
The foundational role of imaging extends across medical specialties, including cardiology, oncology, and neurology, where techniques such as computed tomography (CT), echocardiography, and magnetic resonance imaging (MRI) generate critical data for personalized risk assessment, therapeutic monitoring, and outcome prediction. This technical guide examines the engineering principles, quantitative assessment methodologies, and experimental protocols underpinning specialized imaging's contributions to precision medicine, providing researchers and drug development professionals with a framework for implementing these approaches in translational research.
Quantitative Imaging Biomarkers in Precision Medicine
Quantitative image analysis transforms pixel data into objective biomarkers that enable precise disease characterization and monitoring. These biomarkers provide reproducible, computationally-derived metrics that surpass qualitative visual assessment, forming the data backbone of precision medicine applications.
Core Image Quality Metrics for Quantitative Analysis
Robust quantitative imaging requires rigorous assessment of image quality, particularly when implementing reduced-dose protocols or novel reconstruction algorithms. The metrics listed in Table 1 provide a comprehensive framework for evaluating image quality differences between scanning protocols or equipment [49].
Table 1: Quantitative Metrics for Medical Image Quality Assessment
| Metric | Abbreviation | Technical Description | Measurement Range | Clinical Interpretation |
|---|---|---|---|---|
| Dice Similarity Coefficient | DSC | Measures spatial overlap between segmented volumes | 0 (no overlap) to 1 (complete overlap) | Values >0.7 indicate satisfactory segmentation agreement |
| Structural Similarity Index | SSIM | Measures luminance, contrast, and structure/texture information | -1 (no similarity) to 1 (identical) | Models human perceptual image quality assessment |
| Hausdorff Distance | HD | Measures boundary mismatch between shapes | 0 (identical) to larger values (dissimilar) | Quantifies maximum segmentation error at organ boundaries |
| Gradient Magnitude Similarity Deviation | GMSD | Measures variation in similarity of gradient maps | Lower values indicate better quality | Assesses edge preservation and structural integrity |
| Weighted Spectral Distance | WESD | Assesses shape dissimilarity between volumes | 0 (identical) to 1 (no similarity) | Comprehensive shape dissimilarity metric |
These metrics enable rigorous comparison of imaging protocols, such as evaluating whether reduced-dose CT scans maintain diagnostic utility compared to standard-dose acquisitions [49]. For example, one study demonstrated no significant image quality degradation in reduced-dose CT protocols using these quantitative measures, supporting their clinical implementation for specific diagnostic tasks [49].
Research Reagent Solutions for Imaging Experiments
Table 2: Essential Research Reagents and Materials for Imaging Experiments
| Reagent/Material | Function in Imaging Research | Application Examples |
|---|---|---|
| Iterative Reconstruction Algorithms (SAFIRE) | Reduces image noise while preserving structures | Mitigates noise in reduced-dose CT (from 240 to 150 mA) [49] |
| Virtual Non-Contrast (VNC) Processing | Generates synthetic non-contrast images from contrast-enhanced scans | Eliminates dedicated non-contrast phase in CT protocols, reducing radiation [49] |
| Semiautomated Segmentation Software (Amira, 3D-Slicer) | Enables precise organ and tissue delineation | Heart, liver, spleen segmentation for volumetric analysis [49] |
| Affine Image Registration | Creates one-to-one voxel mapping between different scans | Unbiased comparison of standard-dose and reduced-dose CT images [49] |
| Hounsfield Unit (HU) Thresholding | Segments specific tissue types based on attenuation values | Fat (-190 to -30 HU) and bone tissue segmentation [49] |
Cardiology Applications
Precision Cardio-Oncology Imaging
Cardio-oncology represents a critical intersection where specialized imaging detects cardiovascular complications of cancer therapies, particularly important as cancer survivor populations grow. Cardiovascular disease is the leading cause of non-cancer morbidity and mortality in most cancer survivors, with cancer patients facing a 2–6 times higher cardiovascular mortality risk than the general population [48].
Echocardiography forms the frontline imaging modality in cardio-oncology, with left ventricular ejection fraction (LVEF) and global longitudinal strain (GLS) serving as primary indices for monitoring cancer therapy-related cardiac dysfunction (CTRCD) [48]. These metrics enable early detection of subclinical myocardial injury, allowing for timely intervention and potential modification of cancer treatment regimens.
Artificial intelligence integration is revolutionizing cardiac imaging in precision cardio-oncology. Machine learning algorithms process large cardiac imaging datasets to identify patterns predictive of cardiovascular complications, moving beyond traditional risk stratification [48]. As evidenced by the American Heart Association's Precision Medicine Platform, these AI-driven approaches facilitate more personalized cardiovascular risk assessment and management for cancer patients [48].
Experimental Protocol: Quantitative CT Image Comparison
Objective: To determine whether reducing radiation dose impairs CT image quality for quantitative clinical tasks in cardio-oncology assessment.
Methodology:
- Patient Cohort: Retrospective review of 50 patients (22 male, 28 female; mean age 46.5 years) who underwent both standard-dose and reduced-dose CT scanning [49]
- Scan Parameters: Reduced-dose CT implemented via tube current reduction from 240 to 150 mA with iterative reconstruction (SAFIRE, strength 2/5) to mitigate noise [49]
- Image Registration: Affine registration of standard-dose precontrast CT to virtual non-contrast reduced-dose scans to establish one-to-one voxel mapping [49]
- Tissue Segmentation:
- Quality Assessment: Calculate DSC, SSIM, HD, WESD, and GMSD for all segmented tissues/organs [49]
- Statistical Analysis: Pearson correlation for organ morphometry; Welch 2-sample t-test for density distribution; Kendall Tau for inter-reader agreement [49]
Figure 1: Experimental workflow for quantitative CT image quality assessment in cardio-oncology applications.
Oncology Applications
Precision Oncology Imaging
In oncology, specialized imaging enables molecular profiling and tumor characterization that guides targeted therapies. Precision oncology utilizes molecular profiling of tumors to identify targetable alterations, revolutionizing cancer care by enabling therapies targeted to specific molecular alterations [48]. Platforms such as Tempus, Genomoncology, and Missionbio leverage imaging-derived data to identify genetic susceptibility to specific cancer treatments, significantly improving survivorship for many cancer types [48].
Quantitative imaging biomarkers derived from CT, MRI, and PET provide critical information about tumor morphology, metabolism, and perfusion characteristics. These imaging-derived metrics complement genomic data for comprehensive tumor profiling, enabling monitoring of treatment response and detection of resistance mechanisms.
Radiomics represents an advanced approach where extensive quantitative features are extracted from medical images, converting routine clinical images into mineable data [48]. These high-dimensional data sets, when analyzed with machine learning algorithms, can identify tumor patterns imperceptible to the human eye, predicting treatment response and patient outcomes.
Radiation Dose Optimization in Oncology CT
Radiation dose reduction while maintaining diagnostic image quality represents a significant engineering challenge in oncology imaging. Table 3 compares imaging parameters between standard-dose and reduced-dose CT protocols, demonstrating approaches to minimize radiation exposure without compromising quantitative image information.
Table 3: CT Protocol Parameters for Dose Reduction in Oncology Imaging
| Parameter | Reduced-Dose Protocol (VNC) | Standard-Dose Protocol | Reduction Percentage |
|---|---|---|---|
| Average CT Dose Index | 8.59 ± 2.72 mGy | 17.46 ± 9.58 mGy | 50.8% |
| Dose Length Product (DLP) | 577.28 ± 199.12 mGy·cm | 1212.81 ± 684.52 mGy·cm | 52.4% |
| Average Exposure | 105.83 ± 36.73 mAs | 245.94 ± 124.35 mAs | 57.0% |
| Size-Specific Dose Estimates (SSDE) | 20.08 ± 4.56 mGy | 55.80 ± 19.83 mGy | 64.0% |
| Scan Length | 64.92 ± 4.45 cm | 65.95 ± 5.50 cm | Not significant |
The data demonstrate that significant dose reduction (approximately 50-64% across various metrics) can be achieved while maintaining diagnostic quality for quantitative tasks [49]. This optimization is particularly relevant in oncology, where patients often require repeated imaging studies for treatment monitoring and surveillance.
Neurology Applications
Advanced Neurological Imaging
While the provided search results focus primarily on cardiology and oncology applications, specialized imaging in neurology similarly enables precision medicine approaches through quantitative assessment of brain structure and function. Advanced MRI techniques, including diffusion tensor imaging, functional MRI, and perfusion imaging, provide biomarkers for neurological disorders such as Alzheimer's disease, multiple sclerosis, and brain tumors.
The principles of quantitative image quality assessment detailed in Section 2.1 similarly apply to neurological imaging, where metrics such as structural similarity and segmentation accuracy are essential for tracking disease progression and treatment response.
Artificial Intelligence in Neurological Imaging
Artificial intelligence applications in neurological imaging mirror developments in cardiology and oncology, with machine learning algorithms analyzing complex imaging data to identify subtle patterns associated with specific neurological disorders. These approaches enable early diagnosis, prognosis prediction, and treatment monitoring for precision neurology.
Integration of Artificial Intelligence and Machine Learning
Artificial intelligence serves as a transformative technology across all specialized imaging domains, enhancing the precision and predictive power of medical image analysis. In cardio-oncology, AI processes large cardiac imaging datasets to identify patterns predictive of cardiovascular complications from cancer therapies [48]. Similar approaches apply to neurological and oncological imaging, where AI algorithms detect subtle patterns beyond human visual perception.
The implementation of AI in precision medicine poses challenges regarding data security, privacy, potential biases, and ensuring diverse and equitable access [50]. If existing healthcare biases remain unaddressed, they may be propagated by AI systems that rely on existing data sets, potentially disadvantaging patients from lower socioeconomic status and racial/ethnic minorities [48].
Figure 2: AI and machine learning integration pathway for precision medicine imaging.
Future Directions and Implementation Challenges
The evolution of specialized imaging in precision medicine faces several technical and implementation challenges. Ensuring equitable access to advanced imaging technologies remains a concern, as racial and ethnic minorities, particularly African Americans, demonstrate higher incidence of cancer therapy-related cardiotoxicity yet may experience limited access to specialized cardio-oncology care [48].
The digital divide in access to precision medicine technologies must be addressed through conscious effort and system design. Historically, individuals of low socioeconomic status, ethnic/racial minorities, and rural residents experience disparities in both access to care and inclusion in data sets used to train AI algorithms [48]. Without proactive measures, existing healthcare biases may be amplified by AI-powered systems, potentially worsening health disparities.
Technical challenges include standardization of imaging protocols across institutions, validation of quantitative biomarkers for specific clinical contexts, and integration of imaging data with other diagnostic modalities including genomics and proteomics. Future developments will likely focus on multi-parametric imaging approaches that combine structural, functional, and molecular information for comprehensive patient characterization.
Collaborative networks such as the global cardio-oncology registry (G-COR) demonstrate how international consortiums can assess regional and international patterns of treatment, clinical and socioeconomic barriers, and their impact on outcomes [48]. Similar approaches could benefit neurological and general oncology imaging, enabling large-scale data collection necessary for robust AI algorithm development and validation.
Medical physicists play a crucial role in advancing specialized imaging for precision medicine, ensuring that every diagnostic scan and radiation dose is executed with accuracy, safety, and compassion [51]. Their work bridges scientific discovery with clinical care, ensuring that patients benefit from the most advanced and reliable medical technologies.
The disparity in access to medical imaging between urban and rural populations represents one of the most pressing challenges in global healthcare delivery. Over four billion medical imaging procedures are performed globally each year, yet residents of rural and underserved areas face significant barriers to accessing these critical diagnostic services [52]. This inequity stems from a complex interplay of factors including geographical isolation, limited healthcare infrastructure, shortages of specialized personnel, and the substantial costs associated with traditional stationary imaging systems [53] [54].
The emergence of point-of-care (POC) and portable imaging technologies represents a paradigm shift in medical imaging engineering, offering the potential to transform healthcare delivery by bringing advanced diagnostic capabilities directly to patient bedsides, remote clinics, and community settings [52]. These technological innovations are fundamentally redefining the architecture of healthcare systems by decentralizing imaging services and enabling rapid diagnostic assessment at the point of clinical need. For researchers and engineers in medical imaging physics, this shift presents unique technical challenges and opportunities for innovation in miniaturization, power efficiency, artificial intelligence integration, and network connectivity.
This whitepaper examines the engineering principles, implementation frameworks, and clinical validation methodologies for portable imaging technologies, with particular focus on their application in bridging healthcare access gaps. By synthesizing current research and emerging trends, we provide a technical foundation for future innovation in this critically important field.
Technical Landscape of Portable Imaging Modalities
Portable imaging systems have evolved significantly through innovations in transducer design, low-power electronics, and computational imaging techniques. The current generation of devices spans multiple imaging modalities, each with distinct engineering trade-offs and clinical applications suited to resource-limited environments.
Table 1: Technical Specifications of Portable Imaging Modalities
| Imaging Modality | Portable Form Factors | Key Technical Innovations | Representative Systems | Clinical Applications in Rural Settings |
|---|---|---|---|---|
| Ultrasound | Handheld devices, compact cart-based systems, wireless probes | Miniature transducer arrays, AI-guided acquisition, cloud connectivity | GE Vscan Air SL, Prognosys Prorad Atlas | Abscess identification, obstetric assessment, cardiac function [52] [55] |
| X-ray | Lightweight, battery-powered, foldable systems | High-frequency generators, digital detectors, AI-enhanced CAD | United Imaging digital mobile X-ray | Tuberculosis screening, pneumonia, fracture assessment [52] |
| CT | Mobile trailers, compact scanners | Photon counting detectors, laminated lead shielding, noise reduction algorithms | Neurologica OmniTom Elite | Stroke diagnosis, traumatic brain injury, pneumonia [52] |
| MRI | Ultra-low-field portable systems | AI-reconstructed images, battery operation, iPad Pro control | Hyperfine Swoop system | Brain injury, stroke, ventriculomegaly [52] |
Physics Principles and Engineering Constraints
The development of effective portable imaging systems requires careful balancing of fundamental physics constraints with clinical performance requirements. For ultrasound, the piezoelectric effect (or silicon chip transducers in newer devices) generates high-frequency sound waves that penetrate tissue and create images based on reflected signals [56]. Key physics principles governing image quality include:
- Frequency and Resolution Trade-offs: Higher frequency transducers (5-10 MHz) provide superior spatial resolution but limited tissue penetration, while lower frequencies (2.5-3.5 MHz) offer deeper penetration at reduced resolution [56].
- Acoustic Impedance and Artifacts: The impedance mismatch between tissue interfaces (Z = density × propagation speed) determines reflection coefficients and artifact generation [56].
- Attenuation Characteristics: Signal loss varies significantly between tissue types (0.18 dB/cm/MHz for blood vs. 15 dB/cm/MHz for bone), impacting penetration depth and image quality [56].
For CT and MRI systems, portability introduces additional engineering challenges related to magnetic field stability (MRI), X-ray source power requirements (CT), and radiation shielding. Novel approaches such as Hyperfine's ultra-low-field MRI (0.064T) demonstrate how alternative design parameters can yield clinically useful images despite significant reductions in traditional performance metrics [52].
Implementation Framework: Engineering Deployable Systems
System Architecture and Workflow Integration
Successful deployment of portable imaging technologies in rural settings requires holistic system architecture that extends beyond the imaging hardware itself. The technical workflow encompasses image acquisition, data transmission, interpretation, and clinical integration.
Technical Requirements and Validation Protocols
Implementing portable imaging systems requires rigorous validation against clinical requirements specific to rural practice environments. The following technical assessment framework ensures systems meet necessary performance standards while remaining operable within resource constraints.
Table 2: Technical Validation Protocol for Portable Imaging Systems
| Validation Domain | Test Methodology | Performance Metrics | Acceptance Criteria |
|---|---|---|---|
| Image Quality | Phantom imaging (tissue-mimicking) | Spatial resolution, contrast-to-noise ratio, uniformity | Detectable targets: ≥5 line pairs/cm (US), ≥0.5 mm (CT), ≥3 mm (MRI) |
| Operational Reliability | Simulated field use cycle testing | Mean time between failures, boot-up time, battery life | ≥99% uptime, <2 minute boot time, ≥4 hours battery |
| Connectivity Performance | Network stress testing | Data transmission speed, latency, offline functionality | Functional with bandwidth <1 Mbps, latency <500ms |
| Environmental Tolerance | Thermal, humidity, vibration testing | Operational temperature range, shock resistance | 5-40°C, 10-90% humidity, withstand 0.5m drop |
Research Reagent Solutions for Field Validation
Field validation of portable imaging technologies requires specialized tools and phantoms to ensure consistent performance assessment across diverse environments. The following research toolkit enables quantitative evaluation of system performance under realistic conditions.
Table 3: Essential Research Toolkit for Field Validation Studies
| Research Tool | Technical Specifications | Validation Application | Representative Examples |
|---|---|---|---|
| Tissue-Mimicking Phantoms | Acoustic properties matching human tissue (Z = 1.5-1.7 × 10^6 kg/m²s), stable thermal characteristics | Ultrasound image quality quantification, accuracy of measurement calipers | Gammex 403GS, CIRS Model 040GSE |
| Geometric Resolution Phantoms | Precise spatial targets (0.1-5.0 mm), high-contrast materials | Spatial resolution measurement, linearity assessment, distortion analysis | Leeds Test Objects, USP Phantom |
| Connectivity Simulators | Bandwidth throttling (0.5-10 Mbps), variable latency injection (100-1000ms), packet loss emulation (0-10%) | Network performance under constrained conditions, data integrity verification | iPerf3, NetEm, WANem |
| Portable Power Analyzers | Current/voltage monitoring, battery capacity verification, efficiency calculation | Power consumption profiling, battery life validation, efficiency optimization | Yokogawa WT500, Fluke 438-II |
Technical Challenges and Engineering Solutions
Physical and Operational Constraints
Portable imaging systems face significant engineering challenges that must be addressed through innovative design solutions:
- Power Management: Limited battery capacity necessitates sophisticated power gating architectures, low-power electronics, and alternative energy sources such as solar panels for extended operation in off-grid settings [54].
- Environmental Hardening: Operation in extreme temperatures, humidity, and dusty conditions requires conformal coatings, ruggedized enclosures (IP54 rating or higher), and shock-resistant mechanical designs [54].
- Limited Physical Space: Compact scanner designs such as narrower bore diameters in portable MRI systems (55-60cm vs. 70cm standard) can induce patient anxiety and limit anatomical access, requiring innovative patient positioning solutions and in-bore entertainment systems to improve patient tolerance [52].
Data Security and Network Infrastructure
The transmission of medical images from remote locations presents significant cybersecurity challenges that require robust encryption protocols (AES-256), secure authentication mechanisms, and compliance with healthcare data privacy regulations such as HIPAA and GDPR [52]. Systems must maintain functionality during network outages through local caching and synchronized database replication when connectivity is restored.
Emerging Innovations and Research Directions
Artificial Intelligence Integration
AI technologies are transforming portable imaging through multiple mechanisms:
- Image Enhancement and Reconstruction: Deep learning algorithms compensate for reduced signal-to-noise ratios in miniaturized systems, enabling diagnostic-quality images from lower-cost hardware [57]. For example, AI-based reconstruction techniques allow portable MRI systems to produce clinically useful images despite significantly reduced magnetic field strength [52].
- Automated Interpretation: Computer-aided detection (CAD) algorithms provide decision support for non-specialist operators, with the World Health Organization endorsing CAD for tuberculosis detection on portable chest X-rays in resource-limited settings [52].
- Workflow Optimization: AI-powered triage tools incorporate risk stratification algorithms to prioritize critical cases in radiology worklists, reducing time-to-diagnosis for urgent conditions [52].
Advanced Materials and Transducer Technologies
Next-generation portable imaging systems leverage novel materials to enhance performance while reducing size, weight, and power requirements:
- Photon-Counting Detectors: CT systems incorporating cadmium telluride or cadmium zinc telluride direct conversion detectors provide superior spatial resolution and reduced electronic noise compared to traditional scintillator-based systems [52].
- CMUT Transducers: Capacitive micromachined ultrasound transducers fabricated using silicon micromachining techniques enable broader bandwidth, improved sensitivity, and lower manufacturing costs compared to piezoelectric elements [56].
- Composite Materials: Carbon fiber composites and engineered polymers reduce weight while maintaining structural stability and radiation shielding properties in mobile CT and X-ray systems [52].
Portable and point-of-care imaging technologies represent a convergence of medical imaging physics, materials science, artificial intelligence, and network engineering that collectively enable the transformation of healthcare delivery in rural and underserved areas. The technical challenges inherent in designing systems for resource-limited environments—including power constraints, environmental factors, and network limitations—drive innovation in engineering approaches that ultimately benefit all clinical settings.
For researchers and engineers in medical imaging, this field presents abundant opportunities for impactful work in miniaturization, computational imaging, adaptive acquisition techniques, and validation methodologies. As these technologies continue to evolve, their integration into connected healthcare ecosystems promises to fundamentally redefine medical imaging as a distributed, accessible resource rather than a centralized, limited commodity—ensuring that advanced diagnostic capabilities reach all populations regardless of geographical or economic barriers.
Addressing Key Challenges in Image Quality, AI Interpretability, and Data Security
The integration of artificial intelligence (AI) into medical imaging has revolutionized diagnostic capabilities, enabling the detection of pathological changes that are often imperceptible to the human eye [58]. Deep learning models, particularly convolutional neural networks (CNNs), have demonstrated remarkable performance in tasks ranging from diabetic retinopathy screening to lung cancer detection [59] [58]. However, this unprecedented capability comes with a fundamental trade-off: as models become more powerful, they simultaneously become more opaque, creating what researchers term the interpretability–performance paradox [58]. The clinical implications of this increasing model opacity are profound. Healthcare providers operating under the fundamental principle of primum non nocere (first, do no harm) must understand not just what an AI system predicts but how and why it reaches specific conclusions [58]. This paper examines two prominent approaches to addressing this challenge: the established Gradient-weighted Class Activation Mapping (Grad-CAM) method and the emerging Pixel-Level Interpretability (PLI) model, analyzing their technical foundations, performance characteristics, and practical implications for medical imaging research and clinical deployment.
Technical Foundations: From Heatmaps to Pixel-Level Explanations
Gradient-weighted Class Activation Mapping (Grad-CAM)
Grad-CAM is a model-specific technique for interpreting and visualizing deep learning models, particularly CNNs [60]. It enhances transparency by highlighting the most influential regions in an image that contribute to the model's decision. The technique leverages gradients from the target class score relative to the last convolutional layer, identifying key neurons that impact predictions [60]. For instance, if a model classifies an image as containing a tumor, Grad-CAM can reveal whether features like specific tissue structures or boundaries influenced this classification.
While Grad-CAM provides visually intuitive explanations and is widely adopted due to its simplicity and CNN-specific design, it exhibits critical limitations. The explanations it generates are often coarse and lack the pixel-level granularity required to detect subtle pathological changes in medical images [59] [58]. This method produces generalized heatmaps that highlight broad regions of interest but fails to provide the precise localization needed for detailed clinical analysis of fine-grained anatomical features.
Pixel-Level Interpretability (PLI) Model
The Pixel-Level Interpretability (PLI) model represents a novel framework designed to address critical limitations in medical imaging diagnostics by enhancing model transparency and diagnostic accuracy [59]. PLI is a hybrid convolutional–fuzzy system that integrates CNN-Generated Class Activation Maps with fuzzy logic to enhance diagnostic accuracy and interpretability by providing fine-grained, pixel-level visualizations of AI predictions [59].
Unlike Grad-CAM's coarse heatmaps, PLI generates detailed heatmaps that visualize critical regions in medical images for diagnosis at the pixel level [59]. These heatmaps mark regions with the highest influence on classification outcomes, taking values from 0.1 to 1, and allow clinicians to correlate model predictions directly with precise anatomical features [59]. This granular approach ensures the precise localization of diagnostic features, empowering clinicians with actionable insights that align with their expectations and foster trust in AI-assisted diagnostics [59].
Figure 1: PLI Model Workflow - Integration of CNN feature extraction with fuzzy logic inference for pixel-level interpretability.
Comparative Performance Analysis: Quantitative Metrics
Diagnostic Performance and Computational Efficiency
Rigorous evaluation comparing PLI against Grad-CAM reveals significant differences across multiple performance dimensions. The PLI model demonstrates superior performance in both diagnostic accuracy and computational efficiency when analyzed on standardized medical imaging datasets, particularly using COVID-19 chest radiographs [59] [61].
Table 1: Performance Comparison Between PLI and Grad-CAM in Medical Image Classification
| Metric | PLI | Grad-CAM | Improvement (PLI over Grad-CAM) | Observation |
|---|---|---|---|---|
| Accuracy | 92.0% | 87.5% | 4% (p=0.003) | PLI shows statistically significant improvement [61] |
| Precision | 91.9% | 88.6% | 3.3% (p=0.008) | Better precision with significant reduction in false positives [61] |
| Recall | 91.9% | 86.0% | 5.9% (p=0.001) | Significantly better sensitivity in detecting infected regions [61] |
| F1-Score | 91.9% | 87.2% | 4.7% | More consistent performance across precision and recall [61] |
| Structural Similarity (SSIM) | Higher | Lower | Significant | PLI produces more structurally similar explanations [59] |
| Mean Squared Error (MSE) | Lower | Higher | Significant | PLI demonstrates reduced error in localization [59] |
| Average Inference Time | 0.75s | 1.45s | 48% faster (p=0.001) | Significantly better computational efficiency [61] |
Beyond these quantitative metrics, studies evaluating explanation fidelity across medical imaging modalities reveal important patterns. A systematic review and meta-analysis of 67 studies showed that Grad-CAM achieved a fidelity score of 0.54 (95% CI: 0.51–0.57) across all modalities, significantly lower than LIME's 0.81 (95% CI: 0.78–0.84) [58]. This fidelity measurement, which quantifies how well explanations represent the actual decision-making process of the underlying model, highlights fundamental limitations in gradient-based attention methods like Grad-CAM.
Clinical Utility and Localization Precision
From a clinical perspective, radiologists have expressed very high confidence in PLI for precise localization of subtle features, which is critical for early disease detection [61]. In comparative evaluations, PLI was ranked superior for focusing on smaller, specific regions, enabling detection of micro-level anomalies [61]. In contrast, Grad-CAM's broader heatmaps sometimes hindered fine detail observation, providing general overviews but lacking the precision required for high-stakes diagnostic tasks [61].
Expert validation confirms PLI's ability to provide precise, actionable insights, establishing high trust in clinical decision-making, particularly for subtle anomaly detection where Grad-CAM showed limitations [59] [61]. This alignment with clinical expectations is further enhanced through PLI's integration of fuzzy logic, which enhances both visual and numerical explanations to deliver interpretable outputs that resonate with practitioner reasoning processes [59].
Table 2: Characteristics and Clinical Applications of Interpretability Methods
| Characteristic | PLI | Grad-CAM |
|---|---|---|
| Interpretability Level | Pixel-level | Region-level |
| Granularity | Fine-grained, precise localization | Coarse, generalized areas |
| Architecture | Hybrid convolutional-fuzzy system | Gradient-based visualization |
| Clinical Alignment | High - aligns with clinical expectations | Moderate - provides general overviews |
| Primary Medical Applications | Subtle anomaly detection, early disease identification | Initial screening, general abnormality localization |
| Computational Demand | Higher due to pixel-by-pixel processing | Lower but less detailed |
| Implementation Complexity | Higher - requires fuzzy logic integration | Lower - widely implemented in libraries |
Experimental Protocols and Methodologies
PLI Model Implementation Framework
The implementation of Pixel-Level Interpretability models follows a structured experimental protocol to ensure robustness and reproducibility. The methodology typically leverages established convolutional neural network architectures like VGG19 and utilizes multiple publicly available medical imaging datasets for comprehensive validation [59]. For COVID-19 chest radiograph analysis, the process incorporated over 1000 labeled images across three distinct datasets, which were preprocessed through resizing, normalization, and augmentation to ensure robustness and generalizability [59].
The experimental workflow involves several critical phases. Initially, the base CNN architecture is trained on the target medical imaging task. Subsequently, the PLI framework integrates fuzzy logic systems with CNN-generated feature maps, converting pixel intensities into fuzzy membership values for nuanced, pixel-level interpretability and precise diagnostic classification [59] [61]. This fuzzification process enables the model to handle uncertainty and partial membership in decision boundaries, more closely mirroring clinical reasoning.
Evaluation metrics focus on multiple dimensions including interpretability quality, structural similarity index (SSIM), diagnostic precision, mean squared error (MSE), and computational efficiency [59]. Comparative analyses against baseline methods like Grad-CAM are conducted using rigorous statistical testing to determine significance, with results demonstrating PLI's superior performance across these measured dimensions [59].
Grad-CAM Experimental Implementation
Grad-CAM implementations for medical imaging typically employ transfer learning approaches, fine-tuning pre-trained CNN architectures on medical datasets. For example, one study investigating high-altitude pulmonary edema (HAPE) diagnosis utilized VGG19 and MobileNetV2 architectures pre-trained on the ARXIVV5_CHESTXRAY database containing 3,923 images before fine-tuning on HAPE-specific datasets [62].
The standard Grad-CAM protocol involves:
- Model Training: Developing a classification model using CNN architectures (VGG19, ResNet, MobileNet)
- Gradient Extraction: Computing gradients of the target class score relative to the feature maps of the last convolutional layer
- Heatmap Generation: Combining these gradients with forward-activated feature maps to produce weighted localization maps
- Visualization: Overlaying the resulting heatmaps on original images to highlight influential regions
In practice, Grad-CAM has demonstrated strong performance in binary classification tasks, with one study reporting an AUC of 0.950 for edema detection [62]. However, its performance notably degrades for fine-grained differentiation tasks, such as distinguishing intermediate severity grades of pulmonary edema, where sensitivities for intermediate classes dropped to 0.16 and 0.37 compared to 0.91 for normal and 0.88 for severe cases [62]. This limitation underscores Grad-CAM's challenges with granular medical diagnostic tasks requiring precise differentiation.
Table 3: Key Research Reagents and Computational Resources for Interpretability Experiments
| Resource | Type | Function/Application | Example Specifications |
|---|---|---|---|
| VGG19 Architecture | Software/Model | Base CNN for feature extraction | Pre-trained on ImageNet, adapted for medical images [59] [62] |
| Grad-CAM Implementation | Software Library | Generating baseline explanation heatmaps | Standard implementation in frameworks like PyTorch Captum or TensorFlow TF-Explain [60] |
| Fuzzy Logic Toolkit | Software Library | Implementing fuzzy inference systems | MATLAB Fuzzy Logic Toolbox or Python scikit-fuzzy [59] |
| Medical Imaging Datasets | Data | Model training and validation | COVID-19 chest radiographs [59], HAPE X-rays [62], brain MRI [63] |
| GPU Computing Resources | Hardware | Accelerating model training and inference | NVIDIA RTX series (e.g., RTX 3070 with 8GB VRAM) [62] |
| Image Segmentation Models | Software/Model | Preprocessing and ROI isolation | DeepLabV3_ResNet50 for lung field segmentation [62] |
| Data Augmentation Pipelines | Software | Enhancing dataset diversity and size | Random horizontal flipping, rotation (±10°), brightness/contrast adjustment [62] |
Implementation Workflow: From Data to Interpretable Results
Figure 2: Experimental Protocol Workflow - End-to-end pipeline for developing interpretable AI models in medical imaging.
The implementation workflow for developing interpretable AI models in medical imaging follows a systematic, multi-phase approach. The Data Preparation Phase involves collecting diverse medical imaging datasets, applying preprocessing techniques like resizing and normalization, implementing data augmentation to enhance generalizability, and expert annotation for ground truth establishment [59] [62]. The Model Development Phase encompasses selecting appropriate architectures (VGG19, MobileNet_V2, etc.), training models using transfer learning where beneficial, and rigorous validation using techniques like k-fold cross-validation [62]. The Interpretability Phase involves generating explanations using either PLI or Grad-CAM approaches, quantitatively evaluating explanation quality using metrics like SSIM and fidelity measures, and conducting clinical validation with expert radiologists to assess practical utility [59] [58].
The comparative analysis between Pixel-Level Interpretability (PLI) and Grad-CAM models reveals a significant evolution in approach to the "black box" problem in medical AI. While Grad-CAM has served as an important step toward interpretability by providing visual explanations and highlighting influential regions, its limitations in granularity and precision constrain its utility in clinical settings requiring fine-grained diagnostic insights [59] [58] [61]. The emerging PLI framework, with its hybrid convolutional–fuzzy architecture and pixel-level explanatory capabilities, represents a promising direction for bridging the gap between AI performance and clinical utility [59].
Future research directions should focus on several critical areas. First, reducing the computational demands of pixel-level approaches will be essential for real-time clinical applications [59] [61]. Second, developing standardized evaluation frameworks for interpretability methods across diverse medical imaging modalities remains an open challenge [58]. Third, addressing dataset dependency issues through more robust generalization techniques will be crucial for widespread clinical adoption [59] [62]. Finally, integrating domain knowledge more explicitly into interpretability frameworks may enhance their alignment with clinical reasoning patterns [59] [63].
As the field progresses, the ultimate goal remains the development of AI systems that not only achieve high diagnostic accuracy but also enhance clinical understanding and trust through transparent, interpretable decision-making processes that resonate with medical expertise and practice.
Balancing Algorithmic Efficiency with Diagnostic Accuracy
The integration of artificial intelligence (AI) into medical imaging represents a paradigm shift in diagnostic medicine, creating a fundamental tension between the pursuit of maximal algorithmic efficiency and the imperative of uncompromised diagnostic accuracy. This balance is not merely a technical consideration but a core requirement in medical imaging engineering and physics research, where decisions directly impact patient outcomes. The emergence of both task-specific AI models and more generalized foundation models has created a complex ecosystem where researchers must make strategic decisions about model architecture, training methodologies, and integration strategies [64]. This technical guide examines the current state of this balance across multiple imaging modalities and clinical specialties, providing a structured framework for evaluating and implementing AI solutions that meet the rigorous demands of medical research and clinical practice.
Foundations of AI in Medical Imaging
From Task-Specific Models to Foundation Models
Medical image analysis has evolved from traditional task-specific models to more versatile foundation models. Task-specific models are designed for specialized applications such as segmentation, classification, enhancement, and registration of medical images. These models typically rely on supervised learning and demonstrate strong performance on focused tasks, achieving metrics such as Dice scores of 0.85 for brain tumor segmentation on MRI and accuracy of 95.4% for breast cancer classification on histology images [64]. However, their limitation lies in narrow generalization capabilities and dependency on large, annotated datasets for each specific task.
Foundation models (FMs) represent a transformative approach by leveraging large-scale pre-training on extensive, diverse datasets using self-supervised learning objectives. Unlike task-specific models, FMs learn general-purpose visual features that can be adapted to multiple downstream tasks with minimal additional supervision [65]. The core advantage of FMs lies in their ability to address the fundamental challenge of labeled data scarcity in medical imaging by pre-training on large unlabeled datasets to learn rich, general representations that capture broad patterns and features [65]. This approach significantly reduces dependency on large annotated datasets while often outperforming traditional methods due to the depth and generality of their pre-trained knowledge.
Technical Architectures and Implementation
The architectural foundations of modern medical imaging AI span convolutional neural networks (CNNs), vision transformers (ViTs), and hybrid approaches. CNNs maintain relevance due to their inductive biases for locality and translation invariance, making them particularly efficient for tasks where local patterns such as edges and textures are crucial [65]. ResNet and ConvNeXt remain popular CNN-based architectures for foundation models.
Vision transformers have emerged as powerful alternatives, processing images as sequences of patches and using self-attention mechanisms to capture both local and global dependencies [65]. The hybrid CNN-ViT architecture represents a promising middle ground, leveraging CNN's efficiency in local feature extraction with ViT's strength in modeling long-range dependencies. This approach has demonstrated significant success in areas such as thoracic imaging, where it boosted diagnostic accuracy for chest diseases including tuberculosis and pneumonia [66].
Table 1: Performance Comparison of AI Architectures in Medical Imaging
| Architecture | Representative Models | Strengths | Clinical Validation Examples |
|---|---|---|---|
| CNN-Based | ResNet, ConvNeXt | Efficient with limited data, strong local feature extraction | Liver segmentation in CT/MRI (Dice score: 0.85) [66] |
| Vision Transformer | ViT, UNeXt | Global context capture, strong scaling capabilities | Left ventricle segmentation in echocardiography [66] |
| Hybrid (CNN-ViT) | CNN-ViT frameworks | Balanced local-global feature integration | Multi-class classification of chest diseases [66] |
| Foundation Models | MedSAM, specialized FMs | Cross-task transfer, few-shot learning | Universal medical image segmentation [64] |
Experimental Frameworks and Methodologies
Evaluation Metrics and Performance Assessment
Rigorous evaluation of AI models in medical imaging requires multidimensional assessment across both efficiency and accuracy metrics. Standard accuracy metrics include sensitivity, specificity, area under the curve (AUC), and task-specific measures such as Dice similarity coefficient for segmentation tasks. Efficiency metrics encompass computational requirements, inference time, memory footprint, and scalability.
In hepatocellular carcinoma (HCC) screening studies, the UniMatch model for lesion detection achieved a sensitivity of 0.941 and specificity of 0.833, while the LivNet classification model attained a sensitivity of 0.891 and specificity of 0.783 at a threshold optimized for recall rate balance [67]. These metrics provide the foundation for evaluating the clinical utility of AI systems, but must be considered alongside efficiency measures such as the 54.5% reduction in radiologist workload achieved through optimized human-AI collaboration strategies [67].
Human-AI Integration Strategies
The integration strategy between AI systems and human expertise significantly impacts both diagnostic accuracy and workflow efficiency. Research in HCC screening has identified four primary interaction strategies with distinct performance characteristics:
- Strategy 1: Fully automated AI analysis without radiologist intervention
- Strategy 2: AI analysis with radiologist review of positive cases
- Strategy 3: Radiologist analysis with AI review of negative cases
- Strategy 4: Combined AI initial detection with radiologist evaluation of negative cases in both detection and classification phases
Strategy 4 has demonstrated optimal balance, achieving non-inferior sensitivity (0.956 vs. 0.991) and superior specificity (0.787 vs. 0.698) compared to the original algorithm while reducing radiologist workload by 54.5% [67]. This approach represents a successful model of human-AI collaboration that enhances clinical outcomes while minimizing system burden.
Diagram 1: Optimal HCC Screening Workflow (Strategy 4)
Quantitative Performance Analysis Across Specialties
Cross-Domain Application Performance
The balance between efficiency and accuracy manifests differently across medical specialties and imaging modalities. In oncology, AI models have demonstrated remarkable precision in tumor detection and characterization. For liver cancer, U-Net-based models provide explainable segmentation for hepatocellular carcinoma cases in CT and MRI scans, while multiphase CT analysis with AI differentiation between hepatocellular carcinoma and intrahepatic cholangiocarcinoma shows strong performance and interobserver agreement [66]. In prostate cancer, Random Forest models applied to mp-MRI data and radiomic features can predict lymph node involvement, aiding preoperative planning [66].
Beyond oncology, cardiology applications include deep learning models for detecting critical conditions such as Stanford type A and B aortic dissections in CTA scans, where rapid diagnosis is essential [66]. UNeXt-based segmentation algorithms automatically delineate the left ventricle in transesophageal echocardiography images, enhancing precision of cardiac assessments [66]. Neurological applications include AI-driven analysis of hand-drawn spirals for early Parkinson's disease detection, identifying subtle changes crucial for early intervention [66].
Table 2: Performance Metrics of AI Applications Across Medical Specialties
| Clinical Area | AI Application | Performance Metrics | Clinical Impact |
|---|---|---|---|
| Liver Oncology | U-Net segmentation for HCC | Robust segmentation in CT/MRI | Improved treatment planning [66] |
| Dermatology | YOLOv8 + SAM hybrid model | Automated lesion detection/segmentation | Early skin cancer identification [66] |
| Prostate Oncology | Random Forest on mp-MRI | Prediction of lymph node involvement | Informed surgical planning [66] |
| Cardiology | Deep learning on CTA | Detection of aortic dissections | Reduced diagnostic delay [66] |
| Neurology | Spiral drawing analysis | Early Parkinson's detection | Earlier intervention opportunity [66] |
| Dental Radiology | YOLOv10 on panoramic X-rays | Automatic tooth detection | Efficient pediatric dental care [66] |
Workflow Efficiency and Clinical Impact
The integration of AI into medical imaging extends beyond diagnostic accuracy to encompass significant workflow efficiencies. In HCC screening, the optimal human-AI collaboration strategy reduced radiologist workload by 54.5% while maintaining high sensitivity (0.956) and improving specificity (0.787) compared to traditional approaches [67]. This reduction in workload translates to practical clinical benefits including reduced radiologist fatigue, increased throughput, and potentially decreased healthcare costs.
Additionally, AI implementation affects recall rates and false positive rates, with significant implications for patient anxiety and system burden. In HCC screening, AI-enhanced strategies reduced false positive rates from 0.302 in the original algorithm to as low as 0.131 in Strategy 3, while maintaining diagnostic sensitivity [67]. This reduction in false positives minimizes unnecessary patient anxiety and prevents overtreatment, demonstrating how properly balanced AI systems can improve both clinical outcomes and patient experience.
Implementation Framework
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of AI in medical imaging requires specialized computational tools and frameworks that constitute the modern researcher's toolkit:
Table 3: Essential Research Reagent Solutions for AI in Medical Imaging
| Tool Category | Specific Solutions | Function | Application Context |
|---|---|---|---|
| Segmentation Models | U-Net, SAM, MedSAM | Organ/tumor delineation | Liver segmentation in CT/MRI [66] |
| Detection Frameworks | YOLOv8, YOLOv10 | Automated lesion detection | Skin lesion detection, tooth numbering [66] |
| Classification Models | Random Forest, CNN-ViT hybrids | Disease classification | Liver lesion classification, chest disease identification [66] |
| Foundation Models | Vision-Language Models | Generalized representation | Report generation, outcome prediction [68] |
| Data Harmonization | Federated learning frameworks | Multi-institutional collaboration | Renal tumor segmentation [68] |
Technical Implementation Considerations
Implementing AI systems in medical imaging requires careful attention to several technical considerations. Data governance and privacy must be addressed through appropriate security measures and compliance with healthcare regulations [66]. Model robustness demands rigorous testing across diverse patient populations and imaging devices to ensure generalizability. Computational efficiency must be balanced against performance requirements, particularly for real-time applications in interventional procedures.
The choice between task-specific and foundation models represents a fundamental strategic decision. While foundation models offer broader applicability and reduced dependency on labeled data, task-specific models often achieve superior performance on narrow domains and remain integrated into nearly all medical image analyses [64]. The relationship between these approaches is complementary rather than competitive, with each addressing different aspects of the clinical workflow.
Diagram 2: Model Selection Decision Framework
The balance between algorithmic efficiency and diagnostic accuracy in medical imaging represents a dynamic frontier where engineering principles meet clinical imperatives. The evidence demonstrates that strategic implementation of AI, particularly through optimized human-AI collaboration frameworks, can simultaneously enhance diagnostic performance and workflow efficiency. The complementary relationship between task-specific models and foundation models offers researchers a diverse toolkit for addressing varied clinical challenges across imaging modalities and medical specialties. As the field evolves, the integration of multimodal data, development of more sophisticated foundation models, and refinement of human-AI collaboration strategies will continue to push the boundaries of what is possible in medical imaging research and clinical practice. The fundamental principle remains constant: technological advancement must serve the ultimate goal of improving patient outcomes through more accurate, efficient, and accessible diagnostic capabilities.
Ensuring Data Privacy and HIPAA Compliance in Cloud-Based AI Systems
The field of medical imaging engineering and physics research is undergoing a profound transformation driven by artificial intelligence (AI). These advanced computational methods, particularly when deployed in cloud environments, offer unprecedented capabilities for quantitative image analysis, pattern recognition in high-dimensional data, and predictive biomarker discovery. However, the integration of AI into research and clinical workflows introduces significant data privacy challenges, as imaging data constitutes protected health information (PHI) under the Health Insurance Portability and Accountability Act (HIPAA). Medical imaging researchers and developers operate within a complex regulatory landscape where technical innovation must be balanced with rigorous privacy protections. The fundamental challenge lies in leveraging large-scale imaging datasets for AI model development and validation while ensuring cryptographic privacy guarantees for patient data. This technical guide examines the architectural frameworks, experimental protocols, and compliance validation methodologies essential for building HIPAA-compliant cloud AI systems within medical imaging research, addressing both current standards and emerging 2025 regulatory requirements.
Regulatory Framework: HIPAA and Evolving 2025 Requirements
Core HIPAA-HITECH Provisions for Imaging Research
HIPAA establishes the foundational framework for protecting patient health information, with several key provisions directly impacting medical imaging research:
- Protected Health Information (PHI) Definition: In medical imaging contexts, PHI includes not only standard patient demographics but also the imaging data itself (pixel data in DICOM files), associated metadata (DICOM headers), imaging reports, and derived quantitative biomarkers that could identify an individual [69].
- Security Rule Safeguards: HIPAA mandates implementation of specific safeguards for systems handling electronic PHI (ePHI), which directly applies to cloud-based AI processing pipelines for medical images [70]:
- Technical Safeguards: Access controls, audit controls, integrity controls, transmission security
- Administrative Safeguards: Security management processes, workforce training, evaluation
- Physical Safeguards: Facility access controls, workstation security, device controls
- Business Associate Agreements (BAAs): Research institutions must establish BAAs with cloud service providers, software vendors, and any third parties handling imaging data in AI workflows, making them directly liable for compliance [71].
Key 2025 Regulatory Updates and Implications
Recent regulatory developments significantly impact how medical imaging researchers must approach AI system design:
Table: Key 2025 HIPAA Updates Affecting Medical Imaging AI Research
| Regulatory Change | Technical Requirement | Research Impact |
|---|---|---|
| Reduced Breach Notification Timeline | 30-day notification window (down from 60 days) | Accelerated incident response capabilities required in AI pipelines [72] |
| Enhanced Interoperability Rules | FHIR (Fast Healthcare Interoperability Resources) standards for data exchange | Standardized APIs for imaging data sharing between research systems [72] |
| Expanded Cybersecurity Mandates | Multi-factor authentication (MFA) for all ePHI access points | Enhanced access controls for researcher portals and computational environments [72] |
| Business Associate Oversight | Annual security audits for all business associates | Regular compliance validation for cloud AI vendors and annotation services [71] |
| Zero Trust Framework Implementation | Mandatory "never trust, always verify" architecture | Micro-segmentation of imaging data storage from AI processing workloads [72] |
The HITECH Act extension to cloud services means that medical imaging AI platforms must implement stringent data protection measures, with particular attention to how imaging data is processed, stored, and transmitted during AI training and inference operations [69]. Furthermore, proposed updates to the HIPAA Security Rule would require more rigorous vendor oversight and technical inventories of systems handling ePHI, directly impacting multi-institutional imaging research collaborations [71].
Technical Architecture for Compliant Medical Imaging AI
Confidential Computing with Trusted Execution Environments
Confidential computing represents a paradigm shift in secure data processing, particularly valuable for medical imaging AI workloads. Trusted Execution Environments (TEEs) enable computation on encrypted imaging data without exposing it to the cloud infrastructure, operating system, or other tenants [69]. This hardware-enforced isolation provides:
- Memory Encryption: Continuous encryption of imaging data during AI processing in CPU and GPU memory
- Remote Attestation: Cryptographic verification that AI code is running in a genuine TEE before releasing data
- Hardware-enforced Access Controls: Prevention of unauthorized access even with administrative privileges
For medical imaging research, TEEs enable privacy-preserving federated learning where AI models can be trained across multiple institutions without sharing raw imaging data, addressing a significant barrier to large-scale medical AI development.
End-to-End Secure Imaging AI Pipeline Architecture
A comprehensive architecture for HIPAA-compliant medical imaging AI systems incorporates multiple security layers throughout the data lifecycle:
Diagram: End-to-End Secure Medical Imaging AI Pipeline with TEE Protection
This architecture implements defense-in-depth strategies specifically designed for medical imaging AI workloads:
Ingestion Layer Security: Automated de-identification pipelines using services like Amazon Comprehend Medical specifically configured to handle DICOM metadata and burned-in pixel data [73]. This layer must address the unique characteristics of medical images, including single-channel grayscale images with intensity values of 0-10,000, secondary captures, and annotations [73].
Confidential AI Processing: TEE-protected environments for both model training and inference, ensuring that imaging data remains encrypted during the entire AI processing lifecycle. Implementation requires specialized hardware with GPU TEE capabilities for computationally intensive imaging algorithms [69].
Continuous Compliance Monitoring: Tamper-proof audit logs that record all access to imaging data, integrated with automated compliance checking against HIPAA requirements. This includes monitoring for anomalous access patterns that might indicate unauthorized use or potential breaches [70].
2025-Specific Security Controls for Imaging AI
Based on emerging 2025 requirements, medical imaging AI systems must implement several specific technical controls:
Table: Mandatory 2025 Security Controls for Medical Imaging AI Systems
| Security Control | Technical Implementation | HIPAA Reference |
|---|---|---|
| Multi-Factor Authentication | Phishing-resistant MFA (FIDO2/WebAuthn) for all researcher access | §164.312(d) [72] |
| Zero Trust Architecture | Microsegmentation of imaging data, least-privilege access enforcement | §164.308(a)(4) [72] |
| Data Loss Prevention (DLP) | Content-aware protection blocking unauthorized exfiltration of DICOM data | §164.312(e)(1) [71] |
| Encryption in Transit | TLS 1.3 for all data transfers, including PACS communications | §164.312(e)(2)(i) [70] |
| Encryption at Rest | AES-256 encryption for DICOM storage with customer-managed keys | §164.312(a)(2)(iv) [70] |
| Encryption in Use | TEE memory encryption during AI processing of images | §164.312(a)(2)(iv) [69] |
Implementation of these controls requires careful integration with existing imaging research workflows, including PACS systems, AI training pipelines, and data annotation platforms.
Experimental Protocols for Validation and Testing
PHI De-identification Efficacy Testing
Medical imaging researchers must establish rigorous experimental protocols to validate the effectiveness of PHI removal from DICOM files:
Protocol: Comprehensive DICOM De-identification Testing
- Test Dataset Curation: Assemble a representative dataset of 1,000+ DICOM studies spanning multiple modalities (CT, MRI, PET, X-ray), manufacturers, and institutions, containing known PHI in both header fields and burned-in image data [73].
- PHI Injection: Augment clean datasets with synthetic PHI in multiple locations:
- DICOM header fields (PatientName, PatientID, StudyDate)
- Burned-in text overlays with varying fonts, sizes, and orientations
- Private DICOM tags used by specific manufacturers
- Processing and Validation: Process datasets through the de-identification pipeline, then verify completeness of PHI removal using:
- Automated DICOM header validation scripts
- Computer vision analysis for text detection in images
- Manual sampling by trained reviewers
This protocol should demonstrate >99% PHI detection and removal efficacy across all PHI categories to meet HIPAA Safe Harbor requirements [73].
AI Model Performance Validation in TEE Environments
When deploying AI models in confidential computing environments, researchers must validate that performance remains consistent with standard environments:
Protocol: TEE AI Performance Benchmarking
- Model Selection: Choose representative medical imaging AI models spanning different architectures (CNNs, Transformers, UNet variants) and clinical tasks (segmentation, classification, detection).
- Baseline Establishment: Measure baseline performance metrics (Dice similarity, AUC, inference latency) for each model in a standard cloud environment using standardized imaging datasets.
- TEE Performance Assessment: Execute identical evaluation protocols in TEE environments, measuring:
- Algorithmic performance metrics on validation datasets
- Computational performance (throughput, latency, memory usage)
- Resource utilization and scaling characteristics
- Statistical Analysis: Perform paired statistical testing to identify any significant performance differences between environments, with particular attention to floating-point precision effects in encrypted computation.
Security Control Validation Testing
Rigorous security testing is essential to validate the implementation of privacy controls:
Protocol: Penetration Testing for Medical Imaging AI Systems
- Infrastructure Testing: External penetration testing of all exposed APIs and interfaces, with special attention to DICOM web services and AI model endpoints.
- Data Exfiltration Attempts: Simulated attacks attempting to access imaging data through:
- Side-channel attacks on multi-tenant infrastructure
- Memory inspection attacks on running AI processes
- Model inversion attacks to reconstruct training data
- Access Control Bypass: Attempted privilege escalation and unauthorized access to restricted imaging datasets.
- Compliance Validation: Verification that all security controls meet 2025 HIPAA requirements, including audit logging completeness, encryption implementations, and breach response capabilities [70].
The Scientist's Toolkit: Research Reagents for Compliant Imaging AI
Medical imaging researchers require specialized tools and services to implement compliant AI systems. The following table details essential "research reagents" for building HIPAA-compliant imaging AI pipelines:
Table: Essential Research Reagents for HIPAA-Compliant Medical Imaging AI
| Tool/Category | Specific Examples | Research Function | Compliance Role |
|---|---|---|---|
| Confidential Computing Platforms | Phala Cloud TEE, NVIDIA GPU TEE, Intel SGX | Hardware-enforced encrypted computation during AI training/inference | Ensures PHI protection during processing (§164.312(a)(2)(iv)) [69] |
| Medical Image De-identification Tools | AWS Comprehend Medical, Custom DICOM anonymizers | PHI detection/removal from DICOM headers and burned-in text | Enables Safe Harbor de-identification for research datasets [73] |
| Secure ML Operations Platforms | SageMaker with HIPAA compliance, Azure ML with TEE | End-to-end ML pipeline management with built-in security controls | Implements required audit controls and access restrictions (§164.312(b)) [73] |
| Data Loss Prevention (DLP) Systems | Netskope, Symantec DLP | Monitoring and prevention of unauthorized PHI exfiltration | Provides breach prevention and detection capabilities (§164.308(a)(1)(ii)(D)) [71] |
| Audit & Attestation Services | Phala Trust Center, Custom attestation verifiers | Cryptographic verification of TEE integrity and compliance | Demonstrates ongoing compliance through verification (§164.316(b)(1)) [69] |
| FHIR-Compatible APIs | SMART on FHIR, HAPI FHIR | Standards-based interoperability for imaging data exchange | Supports 2025 interoperability requirements for data sharing [72] |
Compliance Verification and Audit Preparedness
Automated Compliance Monitoring Framework
Maintaining continuous HIPAA compliance requires automated monitoring and evidence collection:
Diagram: Automated HIPAA Compliance Monitoring Framework for Imaging AI
Audit Preparedness Documentation
Research institutions must maintain comprehensive documentation for HIPAA audits, including:
- Risk Analysis Documentation: Formal risk assessment addressing specific threats to medical imaging AI systems, including model inversion attacks, membership inference attacks, and training data extraction vulnerabilities [71].
- Business Associate Inventory: Complete inventory of all third-party vendors with access to imaging data, including signed BAAs and records of their security compliance validation [71].
- Incident Response Plan: Documented procedures for responding to security incidents involving imaging data, aligned with the 30-day breach notification requirement [72].
- Workforce Training Records: Documentation of HIPAA security training specifically tailored for researchers working with medical imaging AI systems [70].
For medical imaging engineering and physics research, ensuring HIPAA compliance in cloud-based AI systems is not merely a regulatory obligation but a fundamental requirement for ethical research conduct. The technical architectures, experimental protocols, and compliance frameworks presented in this guide provide a foundation for developing AI systems that both advance scientific understanding and maintain robust patient privacy protections. As regulatory requirements continue to evolve, particularly with the 2025 HIPAA updates, researchers must adopt a privacy-by-design approach that integrates security controls throughout the AI development lifecycle. By implementing confidential computing technologies, establishing rigorous validation protocols, and maintaining comprehensive compliance documentation, the medical imaging research community can harness the power of AI while maintaining the trust of patients and research participants essential to advancing human health.
Strategies for Mitigating Bias and Ensuring Fairness in AI Model Training
The integration of Artificial Intelligence (AI) into medical imaging represents a paradigm shift in diagnostic medicine, offering unprecedented opportunities for enhancing diagnostic accuracy, workflow efficiency, and patient outcomes [74]. However, these systems can systematically and unfairly perform worse for certain populations, potentially violating core bioethical principles: justice, autonomy, beneficence, and non-maleficence [74]. The field of medical imaging, where AI systems are increasingly being adopted, is no exception to this risk [74]. A growing body of evidence shows that AI models for analyzing medical images can exhibit disparate performance across sub-groups defined by protected attributes such as race, ethnicity, sex, gender, age, and socioeconomic status [74] [75]. For instance, models for diagnosing diabetic retinopathy have shown a substantial gap in diagnostic accuracy (73% vs. 60.5%) for light-skinned versus dark-skinned individuals, and cardiac MRI segmentation models have demonstrated lower performance metrics for Black patients [74]. This whitepaper provides an in-depth technical guide to the strategies for mitigating bias and ensuring fairness throughout the AI model training pipeline, with a specific focus on the context of medical imaging engineering and physics research.
Defining Fairness in the Medical Context
Establishing a criterion for algorithmic fairness is complex, as a one-size-fits-all definition does not exist, especially in healthcare [74]. Fairness can be evaluated using a multitude of metrics, which generally fall into several categories, as detailed in Table 1. The choice of metric is critical and must be guided by the clinical context. For example, demographic parity, which requires equal rates of positive predictions across groups, is often unsuitable for disease diagnosis because it ignores legitimate differences in disease prevalence between sub-groups [74]. In such cases, equal opportunity, which requires equal true positive rates, or equalized odds, which requires equality of both true positive and false positive rates, are often more appropriate fairness criteria [74] [76].
Table 1: Common Fairness Definitions and Metrics in AI
| Category | Metric Name | Technical Definition | Clinical Applicability |
|---|---|---|---|
| Group Fairness | Demographic Parity | Prediction outcomes are independent of protected attributes. | Often inappropriate for disease diagnosis where prevalence varies. |
| Equal Opportunity | Equality of True Positive Rates across groups. | Suitable when ensuring equal detection rates for a condition is critical. | |
| Equalized Odds | Equality of both True Positive Rates and False Positive Rates across groups. | A stricter criterion for non-discriminatory diagnostic performance. | |
| Performance-based | Predictive Parity | Equality of Positive Predictive Value across groups. | Ensures that a positive prediction is equally reliable for all groups. |
| Calibration | Equality between predicted probability and actual outcome rate across groups. | Ensures risk scores are equally meaningful for all patients. | |
| Individual Fairness | Similarity-based | Similar individuals receive similar predictions, regardless of group. | Mathematically defined similarity measures are challenging to establish. |
| Counterfactual Fairness | Prediction remains unchanged after altering a protected attribute. | A strong causal criterion, but computationally complex. |
Effective bias mitigation begins with a thorough understanding of its potential sources. In medical imaging, bias can be introduced at every stage of the AI lifecycle, from data collection to clinical deployment [75]. The fundamental sources can be categorized into three primary areas, as visualized in the workflow below.
Figure 1: Workflow of Bias Sources in Medical Imaging AI
Data and Study Design (â‘ )
This is a predominant source of bias. Representation and sampling bias occurs when training databases do not match the demographics of the target population, leading to lower performance for underrepresented groups [74] [75]. Annotation bias arises from systematic errors introduced by human annotators (e.g., radiologists), often reflecting their subjective experience and cognitive biases [75]. Aggregation bias occurs when false conclusions about individuals are made based on inappropriately combining distinct populations into a single model [75]. Temporal bias emerges from changes in medical imaging technology, protocols, or patient demographics over time, creating a discrepancy between development and deployment data [75].
Modeling (â‘¡)
The choices made during model development can amplify or mitigate bias. The selection of model architecture, loss function, optimizer, and hyperparameters can significantly influence how a model learns and potentially codifies biases present in the data [74] [75]. For instance, a model optimized solely for overall accuracy may sacrifice performance on minority subgroups to maximize gains on the majority group.
Deployment and People (â‘¢)
Human and systemic factors introduce critical biases. Automation bias is the tendency for clinicians to over-rely on AI outputs, potentially overlooking contradictory findings [75]. Confirmation bias can lead users to interpret AI results in a way that confirms their pre-existing beliefs [75]. Feedback loop bias can occur when a model continues to learn from its own predictions, reinforcing and amplifying initial biases over time [75]. Furthermore, underlying structural and institutional biases, such as unequal access to healthcare, can be baked into the data and are exceptionally challenging to rectify [74].
Technical Strategies for Bias Mitigation
Bias mitigation strategies can be applied at three main stages of the model development pipeline: pre-processing, in-processing, and post-processing. The following workflow provides a structured overview of these techniques.
Figure 2: Technical Workflow for Bias Mitigation
Pre-Processing Techniques
These methods aim to modify the training data to remove underlying biases before model training.
- Data Augmentation and Collection: The most straightforward strategy is to collect more representative data to address underrepresentation [77]. When this is infeasible due to cost, privacy, or low disease prevalence, data augmentation can be used. This includes generating synthetic data for underrepresented groups using generative methods, which has proven effective in reducing disparity in diagnostic accuracy for diabetic retinopathy between skin tones [74] [77].
- Resampling and Reweighting: Resampling involves over-sampling the underrepresented groups or under-sampling the overrepresented groups to create a balanced dataset. Alternatively, reweighting assigns different weights to examples from different groups during loss calculation to align their influence with the target population distribution [76].
In-Processing Techniques
These techniques involve modifying the training algorithm itself to incentivize fairer behavior.
- Adversarial Debiasing: This approach uses an adversarial framework with two models: a primary model trained to perform the main task (e.g., disease classification), and an adversarial model trained to predict the protected attribute (e.g., race) from the primary model's features. The primary model is trained to maximize performance on the task while minimizing the adversary's ability to predict the protected attribute, thereby learning feature representations that are invariant to that attribute [74]. This method has been shown to reduce biases in skin lesion classification [74].
- Fairness-Aware Loss Functions: Standard loss functions like log loss can be replaced with fairness-aware alternatives. The TensorFlow Model Remediation library provides two key techniques [77]:
- MinDiff: This technique adds a penalty to the standard loss function that directly minimizes the difference in prediction distributions (e.g., the distribution of output scores) between two defined subgroups. This aims to balance errors across these groups [77].
- Counterfactual Logit Pairing (CLP): CLP encourages individual fairness by penalizing the model if it produces different predictions for a pair of examples that are identical in all features except for a sensitive attribute. This ensures that predictions are not based solely on sensitive attributes [77].
Post-Processing Techniques
These methods adjust model outputs after training to improve fairness.
- Threshold Optimization: This involves setting different decision thresholds for different subgroups to equalize metrics like true positive rates or false positive rates, thereby satisfying criteria like equal opportunity [76]. This is a simple but effective method that does not require retraining the model.
- Calibration by Group: Models can be calibrated post-hoc to ensure that a predicted probability of 70% corresponds to a 70% likelihood of the event across all sub-groups, addressing miscalibration bias [74].
Table 2: Experimental Protocols for Key Mitigation Strategies
| Technique | Core Methodology | Key Hyperparameters | Evaluation Protocol |
|---|---|---|---|
| Adversarial Debiasing | Jointly train predictor and adversary networks with competing objectives. | Adversary loss weight, learning rate ratio, adversary architecture. | Compare subgroup performance (AUC, F1) before/after debiasing; measure adversary's accuracy (lower is better). |
| MinDiff | Add a regularization term (MMD/Wasserstein) to loss that penalizes distribution differences between groups. | MinDiff weight, distribution distance metric, definition of subgroups. | Audit and compare disparities in performance metrics (e.g., FPR, FNR) and score distributions across groups. |
| Counterfactual Logit Pairing (CLP) | Penalize loss for differences in logits between counterfactual pairs of examples. | CLP weight, method for generating/selecting counterfactual pairs. | Measure Individual Fairness: Check that similar patients (differing only in sensitive attribute) receive similar predictions. |
| Reweighting | Assign instance-specific weights during training to balance group representation. | Weighting scheme (e.g., inverse propensity). | Evaluate performance on minority groups; check for overall performance degradation. |
Implementing the aforementioned strategies requires a suite of software tools and libraries. For medical imaging researchers, the following table details essential "research reagents" for fairness experimentation.
Table 3: Essential Tools for Fairness Research in Medical Imaging AI
| Tool / Resource | Type | Primary Function | Application in Medical Imaging |
|---|---|---|---|
| TensorFlow Model Remediation | Software Library | Provides implementations of MinDiff, CLP, and other bias mitigation techniques. | Integrate fairness constraints directly into TensorFlow-based image analysis models during training. |
| AI Fairness 360 (AIF360) | Software Library (IBM) | A comprehensive open-source toolkit with 70+ fairness metrics and 10+ mitigation algorithms. | For auditing models with multiple fairness definitions and comparing efficacy of various pre-, in-, and post-processing methods. |
| Public Medical Datasets (e.g., MIMIC, CheXpert) | Data Resource | Publicly available, often multi-modal clinical datasets, sometimes with demographic metadata. | Serve as benchmarks for developing and testing fairness methods; enable reproducibility and comparison across studies. |
| Fairness Metrics (e.g., disparate impact, equal opportunity difference) | Analytical Tool | Quantitative measures to audit and evaluate model fairness. | Required for model validation and reporting in scientific publications. Tracking multiple metrics is recommended. |
Challenges and Future Directions
Despite the availability of these techniques, significant challenges remain. A major disconnect persists between technical solutions and clinical applications [76]. There is a scarcity of AI fairness research in many medical domains, a narrow focus on a limited set of bias-relevant attributes (often only age, sex, and race), and a dominance of group fairness metrics that may not capture important individual-level inequities [76]. Furthermore, there is limited integration of a "clinician-in-the-loop" to help define what constitutes fairness in a specific clinical context [76].
Future research must focus on bridging these gaps. This includes:
- Expanding Research: Conducting fairness studies across a wider range of medical specialties and using diverse data types (e.g., text, signal) [76].
- Context-Aware Fairness: Moving beyond purely statistical definitions of fairness to incorporate clinical context and ethical principles, ensuring that mitigation strategies align with the goal of promoting health equity [74] [76].
- Multi-Stakeholder Collaboration: Building interdisciplinary teams that include medical physicists, clinicians, ethicists, and AI engineers to define fairness constraints and evaluate the real-world impact of mitigated models [74] [78].
Ensuring fairness in AI models for medical imaging is not a single-step intervention but a continuous process that must be integrated throughout the entire AI lifecycle. It requires a vigilant, multi-faceted approach that combines technical mitigation strategies—applied at the pre-processing, in-processing, and post-processing stages—with a deep understanding of the clinical context and the underlying sources of bias. As the field of medical imaging continues to embrace AI, a proactive commitment to identifying, auditing, and mitigating bias is not merely a technical necessity but an ethical obligation for researchers, engineers, and clinicians alike. By adopting the strategies outlined in this whitepaper, the medical imaging community can steer the development of AI tools toward a more equitable and just future for all patient populations.
The field of radiology stands at a pivotal moment, facing a fundamental paradox: while diagnostic imaging volumes grow annually, a global shortage of radiologists threatens to compromise timely healthcare delivery [79]. Artificial intelligence promises to bridge this gap, not by replacing radiologists, but by augmenting their capabilities through seamless workflow integration. The critical challenge has shifted from developing accurate algorithms to implementing AI tools that work unobtrusively within existing clinical environments [80]. Research indicates that when AI is bolted on without considering workflow integration, it can actually increase radiologist workload instead of reducing it. Conversely, properly integrated AI becomes a "co-traveler in the interpretive process," working quietly in the background to enhance efficiency without demanding additional attention or clicks from already-overburdened clinicians [80]. This whitepaper examines the technical foundations, implementation methodologies, and future directions for optimizing radiology workflows through seamless AI integration, framed within the broader context of medical imaging engineering and physics research.
Technical Foundations: Standards and Interoperability
The seamless integration of AI into radiology workflows depends critically on interoperability standards that enable diverse systems to communicate effectively. These standards form the technical backbone that allows AI applications to connect with picture archiving and communication systems (PACS), radiology information systems (RIS), and electronic health records (EHR) without disrupting established workflows.
Core Interoperability Standards
The Radiological Society of North America (RSNA) has demonstrated that seamless AI integration relies on a specific set of interoperability standards [81]:
- IHE AI Results: Defines how AI-generated results are stored, retrieved, and displayed within clinical systems
- IHE AI Workflow for Imaging: Specifies methods to request, manage, perform, and monitor imaging AI algorithms throughout the diagnostic process
- Interactive Multimedia Reporting: Provides mechanisms to enhance radiology reports with hyperlinks to specific images or findings described in the report text
- RadElement Common Data Elements (CDEs): Offers standardized methods for representing observations made during radiologic diagnosis
- HL7 FHIRcast: Enables synchronization of clinical applications (EHR, PACS, reporting systems, AI tools) to a common study or patient context
Emerging Protocols and Architectures
Beyond established standards, emerging protocols show significant promise for advancing AI integration. Model Context Protocol (MCP) operates as a "universal connector" that enables AI systems to share context and operate together more effectively [79]. Unlike conventional agents that operate independently, MCP establishes a shared context layer where each AI agent can reference prior interactions, patient context, and diagnostic findings. This creates more cohesive, multi-agent reasoning similar to collaboration among clinical specialists. By structuring and versioning contextual inputs, MCP also establishes a verifiable reasoning chain so that every output can be traced back to its originating data, facilitating compliance, auditability, and governance in regulated healthcare environments [79].
Modular, service-oriented architectures are being designed specifically for integration with protocols like MCP. These frameworks combine three foundational elements: imaging framework services that provide access, rendering, and interaction capabilities for medical images; imaging cockpits that create dynamic workspaces for data selection, filtering, and application lifecycle management; and imaging developer resources that help developers prototype imaging workflows efficiently while aligning with regulatory and quality standards [79].
Quantitative Evidence: Measuring AI's Impact
The integration of AI into radiology workflows demonstrates quantifiable benefits across multiple dimensions, from diagnostic efficiency to clinical outcomes. The table below summarizes key performance metrics from recent implementations and studies.
Table 1: Quantitative Benefits of AI Integration in Radiology Workflows
| Application Area | Performance Metric | Baseline | With AI Integration | Data Source |
|---|---|---|---|---|
| Chest X-ray Triage | Result delivery time | Not specified | As little as 2 minutes | [80] |
| Liver Disease Risk Prediction | Concordance index for mortality prediction | eCTP Score: 0.64 | Imaging AI Model: 0.72-0.73 | [82] |
| Pediatric Radiation Dose | Radiation dose reduction | Standard dosing | 36-70% reduction (up to 95%) | [83] |
| Brain Tumour Classification | Diagnostic time | 20-30 minutes | Under 150 seconds | [83] |
| Future Decompensation Prediction | Concordance index (no decompensation at baseline) | eCTP Score: 0.67 | Imaging AI Model: 0.79-0.80 | [82] |
Workflow Efficiency Metrics
Beyond the specific applications highlighted in Table 1, workflow efficiency gains manifest in more generalized metrics. Research indicates that poorly integrated AI forces radiologists to lose more than an hour during a typical shift to excessive clicking and application switching [80]. Seamlessly integrated AI, by contrast, reclaims this time by embedding functionality directly into existing diagnostic viewers and worklists. This approach automatically prioritizes abnormal cases and reduces turnaround times, translating directly into improved patient care through faster clinical decision-making [80].
Predictive Performance Enhancement
Quantitative imaging biomarkers extracted through AI demonstrate significant improvements in predictive performance for clinical outcomes. In a study of 4,614 patients with liver disease, automatically derived imaging biomarkers alone outperformed the electronic Child-Turcotte-Pugh (eCTP) Score for predicting overall mortality (Concordance index of 0.72 vs. 0.64) [82]. The combined model achieved even better performance (Concordance index 0.73), demonstrating that imaging features provide complementary prognostic information to classic health data. For predicting future decompensation in patients without baseline hepatic decompensation (n=4,452), the improvement was even more substantial (Concordance index 0.80 for combined model vs. 0.67 for eCTP Score alone) [82].
Implementation Methodology: From Concept to Clinical Practice
Successful AI integration requires a systematic approach that addresses technical, clinical, and human factors. The following experimental protocol outlines a comprehensive methodology for implementing and validating AI integration in radiology workflows.
Experimental Protocol: AI Workflow Integration
Objective: To quantitatively assess the impact of seamlessly integrated AI tools on radiology workflow efficiency, diagnostic accuracy, and user satisfaction.
Materials and Setup:
- Imaging Infrastructure: PACS/RIS with DICOM standard compliance
- AI Integration Framework: Standards-based platform (IHE AI Results, IHE AI Workflow, HL7 FHIRcast)
- Evaluation Workstations: Diagnostic review stations with integrated AI capabilities
- Data Collection System: Automated logging of interaction timestamps, user actions, and case processing times
Methodology:
- Baseline Assessment Phase (4 weeks):
- Record current workflow metrics without AI assistance
- Document time per case, click counts, application switching frequency
- Establish baseline diagnostic accuracy and report turnaround times
AI Integration Phase (8 weeks):
- Implement AI tools using interoperability standards (IHE AI Profiles, FHIRcast)
- Configure system to present AI results within primary diagnostic viewer
- Enable automated case prioritization based on AI findings
- Provide training sessions with emphasis on trust-building through explainable AI
Validation and Optimization Phase (4 weeks):
- Collect quantitative metrics on workflow efficiency
- Administer user satisfaction surveys addressing system usability and perceived workload
- Conduct structured interviews to identify integration challenges and optimization opportunities
Data Analysis:
- Compare pre- and post-implementation metrics using paired statistical tests
- Correlate quantitative efficiency gains with qualitative user feedback
- Perform subgroup analysis by radiologist experience level and specialty domain
Table 2: Research Reagent Solutions for AI Integration Studies
| Reagent Category | Specific Solution | Function in Research Context |
|---|---|---|
| Interoperability Standards | IHE AI Results, IHE AI Workflow, HL7 FHIRcast | Enable seamless communication between AI applications and clinical systems |
| Quantitative Imaging Platforms | Analytic Morphomics Platform | Automates extraction of imaging biomarkers from CT scans for risk prediction |
| AI Integration Frameworks | GE HealthCare's Imaging Framework | Modular, service-oriented architecture for connecting AI agents to imaging tools |
| Protocol Integration | Model Context Protocol (MCP) | Serves as universal connector enabling AI systems to share context effectively |
| Visualization & Analysis | CT Cardiac Suite | Provides cardiac-specific algorithms and post-scan analysis capabilities |
Integration Architecture Visualization
The following diagram illustrates the information flow within a radiology practice with AI tools seamlessly integrated using interoperability standards, representing both current implementations and future architectures:
This architecture demonstrates how AI integration spans the entire radiology workflow, from pre-interpretive tasks through to post-interpretive follow-up planning. The visualization highlights the continuous feedback loops that enable system learning and optimization over time, with AI acting as an embedded component rather than a separate application.
Future Directions: Agentic AI and Quantitative Imaging
The next evolutionary phase in radiology AI integration moves beyond single-task algorithms toward comprehensive workflow orchestration through agentic AI and quantitative imaging biomarkers.
The Shift to Agentic AI Systems
While the first wave of AI in radiology focused primarily on the interpretive moment—helping radiologists read images faster and more accurately—the next wave addresses the extensive pre- and post-interpretive work that consumes significant radiologist time [80]. Agentic AI systems represent a paradigm shift from single-task algorithms to collaborative AI agents that orchestrate complex workflows. Research concepts demonstrate how agentic AI built on protocols like MCP can coordinate multiple specialized AI agents to complete multi-step diagnostic tasks through natural-language commands [79]. For example, a command to "perform a coronary review" might orchestrate agents that access imaging data, apply rendering modes, call cardiac-specific algorithms, and prepare preliminary findings—all through a single voice-driven instruction [79].
These agentic systems aim to create more adaptive, context-aware imaging workflows where patient demographics, prior studies, and imaging metadata persist across workflow stages, reducing redundancy and ensuring continuity [79]. Each AI action is logged with parameters and timestamps, producing immutable audit trails that strengthen governance and traceability. The fundamental objective is to lift the burden of work radiologists were never meant to do, allowing them to focus on their specialized training in the interpretive moment [80].
Quantitative Imaging Infrastructure
A critical foundation for advanced AI integration is the development of robust quantitative imaging (QI) infrastructure. Current medical imaging suffers from two fundamental shortcomings that inhibit AI applications: lack of standardization across manufacturers and imaging protocols, and a reliance on qualitative (subjective) measurements despite technological capabilities for quantitative (objective) measurements [84]. The growing field of quantitative imaging addresses these limitations by providing accurate, precise quantitative-image-based metrics that are consistent across different imaging devices and over time [84].
A proposed Quantitative Imaging Infrastructure would establish a metrology standards framework encompassing protocol development, quality assurance methodology, quantitative imaging biomarker profiles, and AI/ML validation [84]. This infrastructure would transform medical imaging from subjective interpretation to objective measurement, potentially eliminating the need for invasive biopsies in some cases and providing valuable objective information before even expert radiologist qualitative assessment [84]. Such standardization enables the development of more reliable AI systems and facilitates the emergence of quantitative imaging biomarkers that can predict treatment response and disease progression.
Future Architecture: Agentic AI Ecosystem
The following diagram illustrates the architecture of future agentic AI systems, showing how multiple specialized AI agents collaborate through a shared context protocol to support radiologists throughout the entire workflow:
This future architecture illustrates how agentic AI systems will coordinate multiple specialized agents through a shared context protocol, enabling comprehensive workflow support that anticipates needs, surfaces relevant information at the right moment, and guides radiologist attention to the most urgent cases or findings [79] [80].
The seamless integration of AI into radiology workflows represents a fundamental transformation in healthcare delivery, enabled by interoperability standards, modular architectures, and evolving agentic systems. The optimal AI future in radiology is not one of replacement but of augmentation—where AI functions so seamlessly that it becomes barely noticeable, working quietly in the background to handle routine tasks and administrative burdens [80]. This approach allows radiologists to focus on their core competencies in image interpretation, complex decision-making, and patient communication.
Successful implementation requires addressing both technological and human factors, including trust-building through explainable AI, careful attention to workflow integration, and maintaining appropriate clinical oversight. As radiology continues its digital transformation, those who actively shape AI integration—designing systems that align with clinical needs and workflow realities—will be best positioned to harness its potential for improving patient care, enhancing professional satisfaction, and addressing the growing demands on medical imaging services [85]. The future of radiology belongs not to AI alone, but to radiologists who effectively leverage its capabilities to enhance their practice and improve patient outcomes.
Benchmarking Performance and Rigorous Validation of Imaging Technologies
This whitepaper presents a technical comparative analysis of two distinct artificial intelligence (AI) platforms, H2O.ai Driverless AI and Amazon Rekognition, within the specialized context of medical imaging engineering and physics research. The study evaluates how these platforms' underlying architectures, data processing methodologies, and model deployment paradigms address the unique challenges of medical image analysis, including the need for high-dimensional feature engineering, robust model interpretability, and seamless clinical workflow integration. By framing this analysis against the rigorous requirements of drug development and biomedical research, this guide provides researchers and scientists with a foundational understanding for selecting and implementing automated machine learning (AutoML) solutions that ensure both scientific validity and regulatory compliance.
The integration of artificial intelligence into medical imaging represents a paradigm shift in how researchers approach image-based biomarker discovery, treatment response monitoring, and automated diagnostic support. Automated machine learning (AutoML) platforms have emerged as critical tools for accelerating this integration, democratizing AI development for researchers who are domain experts in medicine or physics but may lack deep specialization in data science [86]. The global AI spending is projected to reach $337 billion in 2025, highlighting the growing emphasis on AI for research transformation [87].
This analysis focuses on two technologically distinct approaches to AI in imaging: H2O.ai Driverless AI, an enterprise AutoML platform that automates the end-to-end machine learning lifecycle for custom model development, and Amazon Rekognition, a specialized, pre-trained computer vision service offering API-based image and video analysis [86] [88]. The core thesis examines how these differing philosophies—general-purpose AutoML versus specialized, pre-built computer vision services—serve the foundational requirements of medical imaging research, where data governance, model explainability, and clinical validation are paramount.
Platform Architectures and Technical Foundations
H2O.ai Driverless AI Architecture
H2O Driverless AI employs a automated machine learning (AutoML) architecture designed to systematize the data science lifecycle. Its core innovation lies in using AI to automate key steps such as data visualization, feature engineering, model development, and validation [86]. The platform is built upon a Kubernetes-based infrastructure, providing compatibility across cloud and on-premise environments, which is crucial for healthcare institutions with strict data sovereignty requirements [89].
- AI Engine Management: The platform operates within the H2O AI Cloud (HAIC) ecosystem, where Enterprise Steam manages AI engines like Driverless AI on Kubernetes and Hadoop clusters, providing security, resource control, and multi-tenancy for research organizations [89].
- Model Deployment and MLOps: Through H2O MLOps, researchers can export experiments and import models into a shared environment for collaboration, management, deployment, and monitoring. This component supports Bring Your Own Model (BYOM) features for integrating third-party Python models [89].
- Authentication and Data Security: HAIC uses OpenID Connect (OIDC) with Keycloak as its reference implementation, ensuring all platform services use the same identity management. This enterprise-grade security framework is essential for handling protected health information (PHI) [89].
Amazon Rekognition Architecture
Amazon Rekognition is a fully managed, proprietary computer vision service operating on a serverless architecture. Unlike the customizable approach of Driverless AI, it provides pre-trained models accessible via API calls, requiring no infrastructure management [88] [90]. Its architecture is specifically optimized for scalable image and video analysis.
- Serverless Microservices: The service operates on AWS infrastructure, automatically scaling to analyze millions of images or video streams within seconds. This fully managed approach eliminates the need for researchers to provision hardware or manage ML infrastructure [88].
- Face Liveness Detection System: For security-critical applications, the architecture incorporates a sophisticated liveness detection flow. This involves creating a unique session ID, real-time video streaming and analysis, and returning a confidence score to determine if the user is live, with all session data expiring after 3 minutes for security [91].
- Integration with AWS Ecosystem: Rekognition is designed for seamless integration with other AWS services like Amazon S3 for data storage, AWS Lambda for serverless computing, and Amazon Kinesis Video Streams for real-time video analysis [90].
Architectural Comparison for Medical Imaging
Table 1: Core Architectural Comparison
| Architectural Feature | H2O.ai Driverless AI | Amazon Rekognition |
|---|---|---|
| Deployment Model | Kubernetes-based; Cloud, on-premise, or hybrid [89] | Fully managed AWS service; Serverless [88] |
| Primary Interface | Web GUI and Python Client [86] | RESTful API [88] |
| Data Sovereignty | Flexible; supports air-gapped environments [89] | AWS cloud regions; limited on-premise options |
| Computational Scaling | Automated on CPUs/GPUs within cluster [86] | AWS-managed auto-scaling |
| Authentication | OpenID Connect (OIDC) with Keycloak [89] | AWS Identity and Access Management (IAM) |
Diagram 1: Contrasting Architectural Workflows for Medical Imaging Analysis
Core Technical Capabilities Comparison
Machine Learning Approach and Customization
The fundamental distinction between these platforms lies in their machine learning approach. H2O Driverless AI embodies a "build-your-own" paradigm, while Amazon Rekognition operates on a "pre-built" model philosophy.
H2O Driverless AI utilizes automated machine learning to create custom models tailored to specific datasets. Its core capability includes automatic feature engineering that transforms raw data into meaningful values machine learning algorithms can consume [86]. The platform employs a unique evolutionary competition approach that finds the best combination of features, algorithms, and tuning parameters for each specific use case [92]. This approach is particularly valuable for medical imaging applications where radiomic features, texture analysis, and shape characteristics require specialized engineering.
Amazon Rekognition provides pre-trained computer vision models accessible via API. The service includes capabilities for object and scene detection, facial analysis, content moderation, and custom labels [88]. The Custom Labels feature does allow for some model customization using transfer learning, enabling researchers to detect specific objects with as few as 10 images per class [88]. However, this offers substantially less flexibility compared to the full model customization available in Driverless AI.
Model Interpretability and Explainability
Model interpretability is non-negotiable in medical applications where clinical decision-making requires understanding the "why" behind model predictions.
H2O Driverless AI provides robust Machine Learning Interpretability (MLI) capabilities, including:
- K-LIME and LIME-SUP for local explanations
- Shapley values for feature importance attribution
- Partial Dependence Plots and Individual Conditional Expectation (ICE) plots
- Automated model documentation (AutoDoc) for regulatory compliance [92]
- Disparate impact analysis for detecting model bias [92]
Amazon Rekognition returns confidence scores and bounding boxes for detections but offers limited inherent explainability for why particular determinations were made [88]. Researchers receive identification results without detailed feature attribution or model decision rationale, which presents challenges for clinical validation and regulatory approval.
Performance and Scalability
Table 2: Quantitative Performance Characteristics
| Performance Metric | H2O.ai Driverless AI | Amazon Rekognition |
|---|---|---|
| Training Data Requirements | Custom models require substantial labeled datasets [86] | Custom Labels can train with as few as 10 images per class [88] |
| Compute Infrastructure | GPU acceleration (up to 30x speedup); CPUs/GPUs in cluster [86] | Fully managed by AWS; no infrastructure management |
| Processing Speed | Minutes to hours for model development [92] | Seconds for image analysis; minutes for video [88] |
| Scalability | Vertical and horizontal scaling within Kubernetes cluster [89] | Automatic scaling to millions of images; serverless |
| Latency for Inference | Low-latency scoring pipelines (Java/Python) [92] | API-based with consistent response times |
Experimental Framework for Medical Imaging Evaluation
Methodology for Platform Assessment
To evaluate these platforms for medical imaging research, we propose a structured experimental protocol focusing on three core imaging modalities: X-ray (2D), MRI (3D), and whole-slide imaging (WSI) for digital pathology.
Dataset Preparation and Curation
- Data Sourcing: Utilize publicly available medical imaging datasets (e.g., NIH ChestX-ray14, TCGA, BraTS) representing diverse clinical conditions and imaging modalities.
- Data Annotation: Establish ground truth annotations through consensus reading by at least three board-certified radiologists/pathologists, with inter-reader variability quantification.
- Data Partitioning: Implement stratified splitting (70% training, 15% validation, 15% test) maintaining class distribution across sets, with patient-level separation to prevent data leakage.
Experimental Protocol for H2O Driverless AI
- Environment Configuration: Deploy Driverless AI on Kubernetes cluster with NVIDIA GPU support for accelerated computation [86].
- Data Ingestion: Import DICOM and whole-slide image patches through H2O's data connectors, supporting formats including PNG, JPEG, and TIFF.
- Feature Engineering Configuration: Enable automatic feature engineering with genetic algorithms to evolve optimal radiomic feature transformations [92].
- Model Training: Execute experiments with interpretability settings (5/5) and fairness constraints, using time-series validation for longitudinal studies.
- Model Interpretation: Generate MLI reports with Shapley values, partial dependence plots, and reason codes for individual predictions [92].
- Deployment: Export models as Java POJOs or MOJOs for integration into clinical research platforms with REST API endpoints.
Experimental Protocol for Amazon Rekognition
- AWS Service Setup: Configure Amazon Rekognition through AWS Console or programmatically via AWS SDK, establishing IAM roles with least-privilege access.
- Data Storage: Upload de-identified DICOM-converted JPEG images to Amazon S3 buckets with server-side encryption enabled.
- Custom Labels Project: For specialized detection tasks (e.g., tumor identification), create Custom Labels project with training and test datasets.
- Model Training: Initiate transfer learning with Rekognition Custom Labels, utilizing pre-trained computer vision models as foundation.
- Inference: Execute batch analysis for stored images or real-time analysis for clinical applications via Rekognition API calls.
- Result Extraction: Process JSON responses containing bounding boxes, confidence scores, and label associations for research analysis.
Diagram 2: Medical Imaging Research Evaluation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Components for Medical Imaging AI
| Research Component | Function in Medical Imaging Research | Platform Implementation |
|---|---|---|
| Radiomic Feature Extractors | Quantifies textural, shape, and intensity-based patterns in medical images | H2O Driverless AI: Automated feature engineering with custom recipes [86] |
| DICOM Converters | Transforms standard medical imaging format to AI-compatible formats | Both Platforms: Pre-processing step to JPEG/PNG for analysis |
| Data Annotation Interfaces | Enables expert labeling of medical images for ground truth establishment | External tools required; labels used for Custom Labels (Rekognition) or full model training (Driverless AI) |
| Model Interpretability Suites | Provides explanations for model decisions critical clinical validation | H2O Driverless AI: Built-in MLI with Shapley, LIME, surrogate models [92] |
| Statistical Validation Packages | Assesses model performance, confidence intervals, clinical significance | Both Platforms: External statistical analysis required (R, Python) |
| HIPAA-Compliant Storage | Secures protected health information (PHI) during research | H2O: On-premise or cloud with encryption [89]; AWS: S3 with server-side encryption [88] |
Discussion: Implications for Medical Imaging Research
Platform Selection Framework for Research Use Cases
The choice between H2O Driverless AI and Amazon Rekognition depends fundamentally on the research objectives, data characteristics, and clinical integration requirements. Our analysis indicates three primary scenarios:
Scenario 1: Novel Biomarker Discovery For research aimed at discovering new imaging biomarkers or developing novel quantitative imaging signatures, H2O Driverless AI provides the necessary flexibility. Its automated feature engineering can identify complex, non-intuitive patterns in high-dimensional imaging data that may correlate with clinical outcomes [92]. This capability is particularly valuable for radiomics research where the relationship between texture features and underlying pathophysiology is being investigated.
Scenario 2: Operational Workflow Automation For tasks involving well-established visual findings (e.g., fracture detection, instrument counting, or gross pathology screening), Amazon Rekognition offers rapid implementation. The Custom Labels feature enables quick adaptation to specific imaging findings without requiring massive datasets [88]. This approach suits quality control applications in radiology departments or high-volume screening environments.
Scenario 3: Multi-Modal Data Integration Medical imaging research increasingly integrates images with clinical, genomic, and laboratory data. H2O Driverless AI excels at modeling complex interactions across these diverse data types within its automated machine learning framework [86]. This capability enables researchers to develop comprehensive models that combine imaging features with electronic health record data for more accurate predictive modeling.
Regulatory and Compliance Considerations
For drug development professionals and clinical researchers, regulatory compliance is a fundamental concern. H2O Driverless AI provides extensive model documentation capabilities (AutoDoc) and interpretability features that facilitate preparation of submissions to regulatory bodies like the FDA [92]. The platform's support for on-premise and air-gapped deployments addresses data sovereignty requirements for protected health information [89].
Amazon Rekognition operates under AWS's shared responsibility model, where AWS manages security of the cloud while customers remain responsible for security in the cloud [88]. Researchers must implement appropriate data de-identification procedures and ensure proper configuration of IAM roles and S3 bucket policies to maintain HIPAA compliance when using the service for medical imaging research.
This comparative analysis demonstrates that H2O Driverless AI and Amazon Rekognition represent fundamentally different approaches to implementing AI in medical imaging research. H2O Driverless AI serves as a comprehensive AutoML platform for researchers developing custom, interpretable models for novel discovery, with robust support for the end-to-end machine learning lifecycle. Amazon Rekognition provides a specialized, API-driven approach for applying pre-trained computer vision capabilities to medical images, with faster implementation but less customization and inherent explainability.
The selection between these platforms should be guided by specific research goals: Driverless AI for investigations requiring custom model development, deep interpretability, and integration of imaging with multi-modal data; Rekognition for applications that align well with its pre-trained capabilities and where rapid deployment is prioritized. As medical imaging AI continues to evolve, both platforms contribute to the foundational infrastructure enabling more reproducible, scalable, and clinically relevant imaging research for drug development and precision medicine. Future work should include rigorous validation studies comparing these platforms' performance on standardized medical imaging tasks across diverse clinical domains.
The integration of Artificial Intelligence (AI), particularly large language models (LLMs) and generative AI, into medical imaging and drug development introduces two fundamental challenges that threaten the reliability and safety of these systems: stochasticity and hallucination. Stochasticity, the inherent randomness in AI model outputs, complicates the reproduction of results and undermines statistical reliability. Hallucination, wherein models generate confident but fabricated information, presents a direct risk to diagnostic accuracy and patient safety [93] [94]. In medical imaging, these challenges are not merely academic; they represent a multi-billion-dollar risk and a critical barrier to clinical trust [93] [95]. This whitepaper provides an in-depth technical guide for researchers and scientists on validation frameworks designed to mitigate these risks. It is framed within the broader context of medical imaging engineering and physics, which offers a principled approach to constraining AI behavior through physical laws and domain knowledge [96], thereby advancing the foundations of robust and trustworthy AI for healthcare.
Defining the Problem: Stochasticity and Hallucination in Medical AI
AI Hallucinations: A Multi-Layered Risk
An AI hallucination occurs when a model generates information that is plausible-sounding and syntactically correct but is factually inaccurate or entirely fabricated [93] [97]. Unlike humans, who can express uncertainty, LLMs are often designed to always provide an answer, even from a position of ignorance [93]. The consequences in medical fields are severe, ranging from eroded user trust and operational disruptions to significant legal liabilities in regulated environments [97].
A conceptual framework from communication research usefully analyzes hallucinations through a supply-and-demand lens [94]. On the supply side, the generation of hallucinations stems from multi-layered technical vulnerabilities, illustrated by a Swiss cheese model where risks align across several layers [94]:
- Training Data: Models are trained on datasets that can contain biases, omissions, or inconsistencies. A degenerative "AI-on-AI" feedback loop, or "model collapse," can occur when AI-generated inaccuracies pollute future training data, compounding the problem [94].
- Training Process: The process of training LLMs is largely opaque, making it difficult to trace or audit why a specific output was produced [94].
- Downstream Gatekeeping: Practical constraints like budget, volume, and context-sensitivity can limit the effectiveness of human or automated oversight designed to filter out subtle hallucinations before deployment [94].
Stochasticity in Model Outputs
Stochasticity refers to the non-deterministic nature of many AI models, where the same input can produce different outputs. This behavior arises from the probabilistic methods used for text generation (e.g., sampling techniques like top-k or nucleus sampling). While this can foster creativity, it is a significant liability in medical applications where consistency and reproducibility are paramount. Stochasticity exacerbates the hallucination risk by making it difficult to consistently reproduce and validate model outputs, thereby complicating the entire validation lifecycle.
Technical Validation Frameworks and Mitigation Strategies
A robust validation framework must move beyond traditional accuracy metrics to address the unique challenges of stochasticity and hallucination. This requires a multi-faceted strategy combining evaluation, observability, and grounding in domain knowledge.
Rethinking Model Evaluation
Traditional benchmarks that reward simple accuracy create a perverse incentive for models to guess rather than express uncertainty [97]. A more effective evaluation paradigm for high-stakes fields includes:
- Penalizing Confident Errors: Scoring systems should penalize incorrect answers given with high confidence more severely than abstentions or expressions of uncertainty [97].
- Rewarding Uncertainty Awareness: Models should receive partial credit for appropriately indicating doubt or requesting clarification, reflecting a more scientifically honest posture [97].
- Agent-Level Evaluation: Instead of evaluating a model in isolation, it should be assessed in context—considering user intent, domain, and scenario. This provides a more accurate picture of real-world reliability [97].
Table 1: Key Metrics for a Modern AI Validation Framework
| Metric Category | Specific Metric | Description and Rationale |
|---|---|---|
| Factuality & Integrity | Hallucination Rate | Measures the proportion of outputs containing fabricated or unsupported information. |
| Faithfulness | Assesses if the generated answer sticks to the provided source information. | |
| Reasoning & Efficiency | Task Success Rate | Tracks whether the AI agent successfully completes the intended goal. |
| Step Utility | Evaluates if each step in a multi-step reasoning process contributes meaningfully to progress. | |
| Uncertainty Calibration | Self-Aware Failure Rate | Measures how often the system appropriately refuses or defers answers when it should. |
| Operational Performance | Cost per Successful Task | A scalability metric linking financial cost to reliable outcomes. |
| Latency Percentiles | Ensures that response times meet clinical workflow requirements. |
Advanced Technical Mitigations
1. Physics-Informed Machine Learning (PIML) For medical imaging, PIML offers a transformative solution by integrating fundamental physical laws—such as partial differential equations governing electromagnetic interactions in MRI or acoustic wave propagation in ultrasound—directly into the learning process [96]. This approach constrains the solution space, reducing the model's tendency to hallucinate by anchoring it to physically plausible outcomes. PIML enhances interpretability and reduces dependency on massive, annotated datasets, which are often scarce in medical domains [96]. For instance, in MRI reconstruction, physics-informed methods incorporate k-space consistency, which significantly reduces artifacts and improves image quality without requiring exponentially more data [96].
2. Advanced Prompt Management and Retrieval-Augmented Generation (RAG) Systematic prompt engineering, versioning, and regression testing are essential for minimizing ambiguity that can lead to hallucinations [97]. Retrieval-Augmented Generation (RAG) is a critical technique that grounds the model's responses by first retrieving information from authoritative, up-to-date knowledge bases (e.g., medical journals or clinical guidelines) before generating a response [94]. However, RAG systems face their own challenges, including conflicting sources and "poisoned" retrievals, which must be managed through careful data curation [94].
3. Real-Time Observability and Human-in-the-Loop Pipelines Continuous monitoring of model outputs in production is a best practice. Observability platforms track interactions, flag anomalies, and provide actionable insights to prevent hallucinations before they impact users [97]. For critical or high-stakes scenarios, integrating scalable human evaluation pipelines ensures that nuanced errors are caught before deployment, creating a essential feedback loop for model improvement [97].
Experimental Protocols for Validation
To empirically validate an AI model against stochasticity and hallucination risks, researchers should implement the following detailed experimental protocols.
Protocol: Quantifying Hallucination Rate in Medical Text Generation
Objective: To measure the propensity of a model to fabricate information when answering questions on medical topics.
Methodology:
- Test Suite Curation: Construct a benchmark dataset of questions derived from established medical sources with verified, consensus-driven answers. This dataset should span topics with varying levels of knowledge consolidation (e.g., well-established facts vs. emerging research) [94].
- Model Querying: Present each question to the model under standardized conditions, using a fixed random seed to control for stochasticity where possible. A sufficient number of iterations (e.g., n>100 per question) should be performed to account for output variance.
- Output Analysis: Analyze responses against the ground truth. Categorize errors, specifically identifying:
- Fabrications: Instances of entirely invented information.
- Citation Hallucinations: Invented or incorrect references to academic literature [94].
- Contradictions: Outputs that internally or externally contradict established knowledge.
- Metric Calculation: Calculate the Hallucination Rate as the proportion of responses containing one or more categories of fabricated information.
Protocol: Evaluating Physics-Informed Constraints in Image Reconstruction
Objective: To assess the effectiveness of PIML in improving reconstruction accuracy and reducing artifacts in a low-data regime, relevant to rare disease studies.
Methodology:
- Dataset Preparation: Use a limited dataset of medical images (e.g., n<100 MRI scans). Artificially degrade the image quality or simulate sparse data conditions.
- Model Training:
- Control Group: Train a standard deep learning model (e.g., a U-Net) on the limited dataset.
- Intervention Group: Train a Physics-Informed Neural Network (PINN) on the same dataset, incorporating a relevant physical loss term (e.g., enforcing consistency with the Fourier transform in MRI physics) [96].
- Evaluation and Metrics:
- Quantitative: Calculate Peak Signal-to-Noise Ratio (PSNR) and Structural Similarity Index (SSIM) between the reconstructed and ground-truth images.
- Qualitative: Expert radiologists should perform a blinded assessment of output images for clinical usability and the presence of hallucinated artifacts.
- Statistical Analysis: Compare the performance metrics between the control and intervention groups using statistical tests (e.g., t-test) to confirm the significance of the PIML approach.
Table 2: The Scientist's Toolkit: Essential Research Reagents and Resources
| Tool or Resource | Category | Function in Validation |
|---|---|---|
| Benchmark Datasets (e.g., MIMIC, The Cancer Imaging Archive) | Data | Provides standardized, real-world data for training and evaluating model performance on clinically relevant tasks. |
| Physics-Informed Neural Network (PINN) Frameworks | Software Library | Enables the integration of physical laws (PDEs) as soft constraints in the model's loss function, reducing hallucinations [96]. |
| Retrieval-Augmented Generation (RAG) Pipeline | Software Architecture | Grounds model responses in verified, external knowledge bases to prevent factual hallucinations [94]. |
| WebAIM Contrast Checker / Colour Contrast Analyser (CCA) | Accessibility Tool | Ensures that any visual outputs (e.g., charts, UI components) meet WCAG contrast standards, which is critical for users with low vision [98] [99] [100]. |
| Agent-Level Evaluation Platform | Evaluation Software | Facilitates the testing of AI systems in context, measuring complex metrics like task success and self-aware failure rates [97]. |
| Multisociety AI Syllabus (AAPM, ACR, RSNA, SIIM) | Educational Framework | Defines critical competencies for users, purchasers, and developers of AI in radiology, providing a checklist for responsible implementation [101]. |
The path to trustworthy AI in medical imaging and drug development requires a fundamental shift in how we validate our models. Moving beyond simple accuracy metrics to frameworks that actively combat stochasticity and hallucination is not optional—it is a scientific and ethical imperative. By embracing agent-level evaluation, integrating physical and domain knowledge through PIML, implementing robust grounding techniques like RAG, and establishing continuous monitoring with human oversight, researchers can build more reliable, transparent, and safe AI systems. The frameworks and protocols outlined in this whitepaper provide a foundation for this endeavor, aligning technical innovation with the rigorous standards demanded by medical physics and engineering. The future of AI in healthcare depends on our ability to not only enhance model capabilities but also to concretely bound their failures.
The integration of artificial intelligence (AI) into diagnostic medicine necessitates robust, standardized metrics to evaluate model performance reliably. Within medical imaging engineering and physics research, selecting appropriate validation metrics is paramount, as they must align with clinical goals and ensure patient safety [102]. Technical validation provides objective evidence that software correctly processes input data and generates outputs with appropriate accuracy and reproducibility [103]. This guide details three critical categories of performance metrics—the F1-Score for classification, the Structural Similarity Index (SSIM) for image synthesis, and localization precision for segmentation—providing a foundational framework for researchers and drug development professionals to assess the efficacy and clinical utility of diagnostic AI tools.
F1-Score: A Balanced Metric for Diagnostic Classification
The F1-Score is a fundamental metric for evaluating classification models, particularly in scenarios involving imbalanced datasets common in medical diagnostics, such as disease screening [104] [105]. It harmonically balances two crucial concepts: precision and recall (sensitivity) [104].
Calculation and Interpretation
The F1-Score is calculated as the harmonic mean of precision and recall: F1 = 2 × (Precision × Recall) / (Precision + Recall) [104] [105].
This formula yields a value between 0 and 1, where scores closer to 1 indicate superior model performance in correctly identifying positive cases while minimizing false alarms and missed cases [104]. In clinical practice, a high F1-Score signifies a model that effectively balances the need to avoid unnecessary stress and costs from false positives (low precision) with the need to prevent dangerous delays in treatment from false negatives (low recall) [104] [105].
Experimental Protocol for Classification Task Evaluation
Evaluating an AI model's classification performance, such as distinguishing malignant from benign lung nodules in CT scans, involves a standard protocol [106]:
- Dataset Preparation: A dataset of medical images is split into training, validation, and test sets. The test set must be independent of the data used for algorithm development to ensure an unbiased evaluation [102].
- Model Training & Prediction: The model is trained on the training set, and its final predictions (e.g., malignant or benign) are generated for the test set.
- Confusion Matrix Construction: Predictions are compared against ground truth labels to populate a confusion matrix, tallying True Positives (TP), False Positives (FP), True Negatives (TN), and False Negatives (FN) [102].
- Metric Calculation: Precision, Recall, and subsequently the F1-Score are calculated from the confusion matrix counts [105].
The following workflow diagram illustrates this experimental process for classification tasks:
Table 1: Key Classification Metrics Derived from the Confusion Matrix
| Metric | Formula | Clinical Interpretation |
|---|---|---|
| Precision (PPV) | TP / (TP + FP) | The proportion of positive predictions that are truly positive. High precision reduces false alarms and unnecessary follow-ups [102]. |
| Recall (Sensitivity) | TP / (TP + FN) | The proportion of actual positive cases that are correctly identified. High recall reduces missed diagnoses [102] [105]. |
| F1-Score | 2 × (Precision × Recall) / (Precision + Recall) | The harmonic mean of precision and recall. Provides a single balanced measure when both false positives and false negatives are critical [104] [105]. |
| Specificity | TN / (TN + FP) | The proportion of actual negative cases that are correctly identified. Essential for "ruling in" diseases [102] [105]. |
SSIM: Evaluating Image Synthesis and Reconstruction Fidelity
The Structural Similarity Index Measure (SSIM) is a reference-based metric extensively used to assess the perceptual quality of synthetic medical images, such as those generated by super-resolution models or image-to-image translation networks [103] [106]. Unlike pixel-wise metrics (e.g., PSNR), SSIM evaluates the structural similarity between a generated image and a reference image, which is often more aligned with human perception [103].
Advanced SSIM Applications and Methodologies
Recent research has advanced beyond basic SSIM application. For instance, the S3IMFusion method for multi-modal medical image fusion introduces a stochastic structural similarity loss [107]. This approach involves:
- Generating a random sorting index based on source images.
- Mixing and rearranging pixel features between fused and source images according to this index.
- Computing the structural similarity loss by averaging losses between pixel blocks of the rearranged images [107].
This method ensures the fusion result preserves globally correlated complementary features from source images, addressing a limitation of conventional loss functions that overlook non-local features [107].
Experimental Protocol for Image Synthesis Validation
A rigorous protocol for validating super-resolution or image-to-image translation models using SSIM involves both synthetic and real-world evaluation [106]:
- Model Training & Inference: Train the SR model (e.g., SwinIR, EDSR) on paired low-resolution and high-resolution images. Use the model to generate synthetic high-resolution images for the test set [106].
- Reference-Based Assessment: Calculate SSIM between each synthetic image and its corresponding ground-truth high-resolution reference image.
- Statistical Reporting: Report the average SSIM across the entire test set. It is crucial to accompany SSIM with task-specific downstream evaluations, as high SSIM does not guarantee improved diagnostic performance [103] [106].
Table 2: Common Image Quality and Similarity Metrics in Medical Imaging
| Metric | Type | Description | Key Considerations |
|---|---|---|---|
| SSIM | Reference | Measures perceptual structural similarity between two images [103]. | Sensitive to structural distortions but can underestimate blurriness; not a standalone validator [103]. |
| PSNR | Reference | Measures the fidelity of a reconstructed image based on the peak signal-to-noise ratio [106]. | Can be insensitive to clinically relevant perceptual distortions [103]. |
| FSIM | Reference | Focuses on low-level features like phase congruency and gradient magnitude [106]. | Provides additional insights beyond SSIM and PSNR. |
| Non-Reference Metrics | No-Reference | Estimates quality (e.g., blurriness, noisiness) without a ground-truth image [103]. | Essential for real-world use when a reference image is unavailable. |
Localization Precision: Metrics for Segmentation and Detection
Localization precision quantifies an AI model's ability to accurately identify the spatial position and boundaries of anatomical structures or pathologies. This is critical for tasks like tumor segmentation, lesion detection, and organ delineation [102].
Overlap and Distance Metrics
For segmentation tasks, the Dice Similarity Coefficient (DSC) and Intersection over Union (IoU), also known as the Jaccard index, are standard overlap metrics [102]. Both range from 0 (no overlap) to 1 (perfect overlap). However, these volume-sensitive metrics can favor larger, spherical objects. Therefore, the European Society of Medical Imaging Informatics recommends reporting DSC alongside boundary-specific metrics like the Normalized Surface Distance for a more comprehensive assessment [102]. The Hausdorff distance is another boundary metric, though it is sensitive to outliers, so reporting the 95th or 99th percentile is advised over the maximum distance [102].
For object detection, localization is often evaluated using IoU with bounding boxes. A predicted bounding box is considered a true positive if its IoU with the ground-truth box exceeds a set threshold (e.g., 0.5) [102]. Performance is then summarized using the mean Average Precision (mAP) [102].
Experimental Protocol for Segmentation Evaluation
Evaluating the localization precision of a segmentation model, such as a U-Net for tumor volumetry, follows a structured protocol:
- Inference: The trained model generates a pixel-wise segmentation mask for each image in the test set.
- Comparison to Ground Truth: The predicted mask is compared to the expert-annotated ground truth mask.
- Voxel-Level Counting: The number of True Positive (TP), False Positive (FP), and False Negative (FN) voxels is counted.
- Metric Calculation: The Dice coefficient is calculated as DSC = 2TP / (2TP + FP + FN). Surface distances are computed between the boundaries of the predicted and ground-truth segmentations [102].
Table 3: Key Metrics for Evaluating Localization Precision
| Metric | Scope | Formula / Principle | Clinical Relevance |
|---|---|---|---|
| Dice Coefficient (DSC) | Segmentation | DSC = 2TP / (2TP + FP + FN) [102] | Measures volumetric overlap. Essential for assessing tumor volume or organ segmentation accuracy. |
| Intersection over Union (IoU) | Segmentation / Detection | IoU = TP / (TP + FP + FN) [102] | Similar to DSC, provides a slightly more pessimistic measure of overlap. |
| Normalized Surface Distance | Segmentation | Average distance between the surfaces of predicted and ground-truth volumes [102]. | Critical for evaluating boundary accuracy in applications like surgical planning or radiotherapy targeting. |
| mean Average Precision (mAP) | Detection | Mean of average precision values over all classes and IoU thresholds [102]. | Comprehensive measure for multi-object detection tasks (e.g., detecting multiple lesions). |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Computational Tools for AI Metric Evaluation
| Item Name | Function / Description | Example Use in Evaluation |
|---|---|---|
| Curated Medical Image Datasets | Paired datasets (e.g., low-resolution & high-resolution images, source images & fusion targets) for model training and validation. | Used to train and test super-resolution or image fusion models like SwinIR or S3IMFusion [107] [106]. |
| Expert-Annotated Ground Truth | Pixel-wise segmentation masks or bounding boxes created by clinical experts. | Serves as the reference standard for calculating segmentation (DSC) and detection (mAP) metrics [102]. |
| Whole Slide Images (WSIs) with Multi-Omics Data | Large, high-resolution digital pathology images matched with genomic data. | Used for training and validating multi-modal AI platforms like EXAONE Path 2.0 for predicting gene mutations from images [108] [109]. |
| Synthetic Image Distortion Tools | Software to apply controlled distortions (e.g., blur, noise, MR artifacts) to reference images. | Allows for systematic analysis of metric sensitivity to specific image distortions and artifacts [103]. |
| Benchmarking Frameworks (e.g., Scikit-learn) | Open-source libraries providing standardized implementations of metrics like F1-Score, precision, and recall. | Ensures reproducible and consistent calculation of classification metrics across different studies [105]. |
Interoperability, the ability of different health information systems to access, exchange, and use data cohesively, forms the foundational infrastructure supporting modern medical imaging engineering and physics research. For researchers, scientists, and drug development professionals, interoperable systems enable the large-scale, multi-institutional data exchange necessary for validating imaging biomarkers, developing artificial intelligence (AI) algorithms, and conducting robust clinical trials. The Office of the National Coordinator for Health Information Technology (ONC) leads and coordinates these interoperability activities nationwide through technical initiatives, standards development, and health IT certification programs [110]. Without effective interoperability standards, the translation of innovative imaging physics research from laboratory environments into clinical practice and therapeutic development pipelines remains fragmented and inefficient, ultimately hindering scientific progress and patient care advancement.
Core Interoperability Standards and Regulatory Frameworks
Foundational Standards and Data Elements
The technical architecture for healthcare interoperability relies on standardized data formats and application programming interfaces (APIs) that ensure consistent interpretation of exchanged information across diverse systems.
Table 1: Core Data Standards for Medical Imaging and Research Interoperability
| Standard Name | Governing Body | Primary Function | Relevance to Imaging Research |
|---|---|---|---|
| U.S. Core Data for Interoperability (USCDI) | ONC | Defines standardized set of health data classes & elements for exchange [110] | Includes clinical notes, imaging results; essential for structured research datasets |
| Fast Healthcare Interoperability Resources (FHIR) | HL7 | Modern API standard for exchanging healthcare information electronically [111] | Enables integration of imaging data with clinical information for multimodal analysis |
| DICOM (Digital Imaging and Communications in Medicine) | NEMA | Standard for handling, storing, printing, and transmitting medical imaging information | Fundamental for imaging physics research across modalities (MRI, CT, PET, etc.) |
| Trusted Exchange Framework and Common Agreement (TEFCA) | ONC | Establishes universal governance, policy, and technical foundation for nationwide interoperability [110] | Facilitates multi-institutional research data sharing while maintaining security |
The USCDI provides a critical foundation for research interoperability by establishing a consistent set of data elements that must be accessible for exchange. For imaging physics researchers, this standardization enables the aggregation of structured datasets combining imaging data with clinical context, including allergies, laboratory results, and medications [110]. This structured approach is essential for developing and validating AI models that correlate imaging findings with clinical outcomes, a key focus area in advanced imaging research laboratories [68].
Regulatory Enforcement and Certification
Recent regulatory developments have significantly strengthened interoperability requirements through both enforcement mechanisms and certification programs. In September 2025, the HHS Office of Inspector General and ONC announced that enforcement of federal information blocking regulations would be a "top priority" [111]. These regulations prohibit healthcare "actors"—including developers of certified health IT, health information exchanges/networks, and healthcare providers—from practices likely to interfere with legally permissible access, exchange, or use of electronic health information (EHI).
The ONC Health IT Certification Program establishes a voluntary framework that ensures technologies are developed with interoperability in mind [110]. Certified systems must demonstrate capabilities including standards-based data exchange through FHIR APIs and compliance with USCDI requirements. For research environments, utilizing certified health IT provides assurance that data exported from clinical systems will conform to predictable standards and formats, reducing preprocessing overhead and facilitating replication of findings across institutions.
Implementation Frameworks and Modern Initiatives
The Trusted Exchange Framework and Common Agreement (TEFCA)
TEFCA establishes a universal governance, policy, and technical foundation for nationwide interoperability, simplifying connectivity for organizations to securely exchange information [110]. This framework is particularly valuable for multi-center imaging research studies, which require standardized mechanisms for sharing imaging data, clinical information, and analysis results across participating institutions while maintaining data security and patient privacy.
CMS Health Technology Ecosystem
In July 2025, the Centers for Medicare & Medicaid Services (CMS) announced the "Health Technology Ecosystem," a voluntary private sector initiative encouraging interoperability through a shared CMS Interoperability Framework [111]. This ecosystem encompasses five participant categories:
- CMS Aligned Networks: Data networks meeting CMS Framework criteria
- Healthcare Providers: Connecting to CMS Aligned Networks
- EHR Systems: Connecting to CMS Aligned Networks
- Payers: Connecting to CMS Aligned Networks
- Patient-Facing Applications: Leveraging CMS Aligned Networks
The initiative emphasizes FHIR API implementation adhering to the U.S. Core FHIR implementation guide and USCDI version 3 (or later) [111]. For medical imaging researchers, this ecosystem promises improved access to real-world clinical and imaging data at scale, facilitating more robust research datasets and accelerated translational pathways for imaging biomarkers and AI technologies.
CMS Ecosystem Structure
Interoperability in Medical Imaging Research Environments
Integration with Imaging Physics Research Workflows
In advanced imaging research settings, interoperability standards enable the seamless flow of data between clinical imaging systems and research analysis platforms. The AI Medical Imaging Lab at the University of Colorado Anschutz exemplifies this integration, developing "foundation and vision-language models that align images with radiology reports and clinical data" [68]. This research requires robust interoperability between Picture Archiving and Communication Systems (PACS), EHR data, and computational analysis environments.
Table 2: Research Reagent Solutions for Interoperable Imaging Research
| Solution Component | Function in Research Workflow | Implementation Example |
|---|---|---|
| FHIR API Interfaces | Extract clinical data from EHR systems for correlation with imaging features | Retrieving laboratory values, medications, and outcomes for AI model training |
| DICOM Standard | Ensure consistent image data format across different scanner manufacturers and institutions | Multi-center trials using MRI, CT, or PET data from multiple vendor platforms |
| TEFCA-Compatible Networks | Enable secure data sharing between collaborating institutions while maintaining privacy | Sharing de-identified imaging data between academic medical centers for validation studies |
| syngo.via/teamplay Integration | Connect AI analysis tools with clinical imaging platforms for translational research [68] | Implementing research AI algorithms for evaluation within clinical reading workflows |
| USCDI-Structured Data | Provide standardized clinical elements for algorithm development and validation | Using structured allergy data to exclude contrast-enhanced imaging studies for analysis |
Experimental Protocol for Multi-Center Imaging Research
For researchers designing interoperability-dependent studies, the following protocol provides a methodological framework for ensuring consistent data exchange:
Protocol Title: Standardized Methodology for Multi-Center Medical Imaging Research Using Interoperability Standards
Objective: To establish a reproducible framework for acquiring, exchanging, and analyzing medical imaging data across multiple institutions while maintaining data quality and consistency.
Materials and Methods:
- Data Acquisition Standards:
- Configure all participating imaging systems to export data in DICOM format with consistent metadata tags
- Implement automated de-identification procedures compliant with HIPAA standards
- Utilize structured reporting templates based on USCDI elements for clinical data annotation [110]
Data Exchange Mechanism:
- Establish TEFCA-aligned or CMS Aligned Network connections between participating institutions [111]
- Implement FHIR APIs for extraction of clinical data from EHR systems
- Utilize secure file transfer protocols with encryption for imaging data exchange
Data Harmonization Process:
- Apply computational methods for cross-site data harmonization to mitigate scanner-specific variations
- Implement quality control checks for data completeness and format compliance
- Use standardized terminologies (SNOMED CT, LOINC) for clinical data annotation
Analysis Implementation:
- Deploy containerized analysis algorithms to ensure consistent execution across sites
- Utilize federated learning approaches when data sharing restrictions apply [68]
- Implement version control for all analytical pipelines to ensure reproducibility
Validation Metrics:
- Data completeness across all required USCDI elements
- Successful interoperability rate between systems
- Quantitative imaging biomarker consistency across platforms
- Algorithm performance maintenance across institutional datasets
Recent Developments and Future Directions
Enhanced Certification Criteria
The August 2025 final rule from CMS and ONC established new health IT certification criteria for "real-time prescription benefit checks and electronic prior authorization" [111]. These criteria, available for health IT developers beginning October 1, 2025, will become part of the minimum "Base EHR" capabilities required for Certified EHR Technology (CEHRT) by January 1, 2028. For imaging researchers, these advancements facilitate more efficient correlation of imaging utilization patterns with therapeutic interventions and outcomes.
Artificial Intelligence and Advanced Interoperability
The integration of artificial intelligence with interoperable health data represents a frontier in medical imaging research. The AI Medical Imaging Lab emphasizes "foundation and vision-language models that integrate images, radiology text, and clinical variables to power automated reporting, lesion detection/segmentation, longitudinal response assessment, and risk prediction" [68]. These approaches require sophisticated interoperability between imaging data, unstructured radiology reports, and structured clinical information—advances made possible through standards like FHIR and USCDI.
AI Research Data Flow
Information Blocking Enforcement and Research Implications
The September 2025 HHS enforcement alert regarding information blocking regulations signals increased scrutiny of practices that may impede appropriate data exchange [111]. For researchers, this enforcement priority may facilitate improved access to legacy datasets and reduced administrative barriers to data sharing for research purposes. However, researchers must also ensure their own data management practices comply with these regulations, particularly when working with controlled datasets or developing data sharing platforms.
Interoperability standards provide the essential infrastructure enabling advanced medical imaging physics research in an increasingly data-driven healthcare environment. The evolving framework of technical standards, implementation specifications, and regulatory requirements establishes a foundation for reproducible, scalable, and collaborative research across institutional boundaries. For researchers developing novel imaging technologies, AI algorithms, or therapeutic assessment biomarkers, understanding and leveraging these interoperability frameworks is no longer optional—it is fundamental to conducting rigorous scientific investigation that can successfully translate from laboratory environments to clinical practice. As interoperability continues to evolve through initiatives like TEFCA and the CMS Health Technology Ecosystem, researchers who strategically incorporate these standards into their methodological approaches will be positioned to lead the next generation of medical imaging innovation.
Benchmarking through competitive challenges represents a cornerstone of progress in the field of medical imaging engineering and physics research. These organized competitions provide structured frameworks for evaluating and comparing the performance of emerging algorithms against standardized datasets and well-defined metrics. The International Symposium on Biomedical Imaging (ISBI) has established itself as a premier venue for such challenges, catalyzing innovation across diverse imaging modalities and clinical applications. Within the broader thesis of medical imaging research, these challenges function as critical validation mechanisms, transitioning theoretical algorithms into clinically viable solutions by addressing real-world constraints such as data scarcity, computational efficiency, and generalizability across heterogeneous clinical environments.
The ISBI 2025 challenges continue this tradition by focusing on pressing clinical needs where advanced computational methods can yield significant diagnostic and prognostic improvements. These challenges embody the interdisciplinary nature of modern medical imaging research, integrating principles from physics-based image acquisition, engineering-oriented algorithm development, and clinically grounded validation methodologies. This whitepaper provides a comprehensive technical analysis of these challenges, extracting methodological insights and benchmarking approaches that inform the foundational principles of medical imaging research.
Core ISBI 2025 Challenges: Objectives and Biomedical Significance
The ISBI 2025 challenges address clinically significant problems across multiple imaging domains, each presenting unique benchmarking considerations within medical imaging research. These challenges were meticulously designed to advance both algorithmic capabilities and clinical applicability.
Table 1: Overview of Core ISBI 2025 Challenges
| Challenge Name | Primary Technical Objective | Clinical/ Biological Significance | Key Innovation Focus |
|---|---|---|---|
| Fuse My Cells Challenge [112] | Predict fused 3D microscopy images from limited 2D views using deep learning | Extends live imaging duration; reduces photon damage to biological samples | 3D image-to-image fusion; computational compensation for physical acquisition limitations |
| Pap Smear Cell Classification [112] | Develop algorithms for classification of cervical cell images from Pap smears | Early detection of pre-cancerous conditions; improves cervical cancer screening accuracy | Handling data variability; reducing false positives/negatives in cancer detection |
| Semi-Supervised Cervical Segmentation [112] | Leverage labeled and unlabeled data for ultrasound cervical segmentation | Predicts spontaneous preterm labor; enables early intervention strategies | Semi-supervised learning for medical image analysis; reducing annotation burden |
| Glioma-MDC 2025 [112] | Detect and classify mitotic figures in glioma tissue samples | Indicators of tumor aggressiveness; enhances brain tumor grading and prognostication | Automation of manual pathological counting; generalization to abnormal mitotic figures |
| Beyond FA [112] | Identify diffusion MRI metrics beyond Fractional Anisotropy for white matter integrity | Improves specificity in pathological interpretation; establishes more reliable biomarkers | Crowdsourcing biomarker development; analyzing sensitivity to hidden data variability |
The "Fuse My Cells" challenge addresses fundamental limitations in multi-view microscopy, where traditional fusion requires multiple sample exposures that cause photon damage [112]. This challenge innovates by predicting fused 3D representations from limited views, thus operating at the intersection of acquisition physics and computational reconstruction. Similarly, the "Beyond FA" challenge confronts the limitations of standard Fractional Anisotropy metrics in diffusion MRI by crowdsourcing the development of more specific biomarkers, acknowledging that physical measurement constraints often necessitate computational compensation [112].
The "Glioma-MDC 2025" challenge highlights the critical role of quantitative analysis in digital pathology, where automating the detection of mitotic figures—a key indicator of cellular proliferation—addresses both inter-observer variability and diagnostic efficiency challenges in neuropathology [112]. This exemplifies how benchmarking advances both engineering and clinical practice simultaneously.
Methodological Approaches and Experimental Protocols
Data Curation and Annotation Standards
A critical foundation of any benchmarking effort lies in its data curation strategy. The ISBI 2025 challenges employ diverse but methodologically rigorous approaches to dataset development:
- Multi-institutional data collection: Several challenges, including the semi-supervised cervical segmentation challenge, incorporate data from multiple clinical sites to ensure demographic and acquisition diversity [112]. This approach directly tests algorithm generalizability across different populations and equipment specifications.
- Expert annotation protocols: The Pap Smear challenge employs a multi-stage annotation process where initial labels generated by medical trainees undergo verification by senior specialists with over ten years of experience [112]. This hierarchical validation ensures label quality while acknowledging the resource-intensive nature of medical image annotation.
- Standardized pre-processing: The ChestDR subset within the MedFMC benchmark converts original DICOM files to 12-bit PNG format while preserving original image sizes, maintaining critical bit-depth information crucial for diagnostic interpretation [113].
Algorithmic Frameworks and Evaluation Metrics
The methodological approaches benchmarked in these challenges span contemporary machine learning paradigms, each with distinct experimental considerations:
Table 2: Algorithmic Frameworks and Evaluation Methodologies
| Technical Approach | Implementation in ISBI 2025 Challenges | Advantages | Limitations |
|---|---|---|---|
| Foundation Models with PEFT | LoRA and BitFit for COVID-19 outcome prediction from chest X-rays [114] | Reduces computational resources; maintains pre-trained knowledge | Performance degradation under severe class imbalance |
| Semi-supervised Learning | Leveraging unlabeled ultrasound data for cervical segmentation [112] | Reduces annotation burden; utilizes readily available unlabeled data | Requires specialized architecture design; potential error propagation |
| Full Fine-tuning (CNNs) | ImageNet pre-trained CNNs adapted for medical imaging tasks [114] | Robust performance on small, imbalanced datasets | Requires more labeled data; potential overfitting |
| Failure Detection Methods | Pairwise Dice score between ensemble predictions for segmentation quality control [115] | Simple implementation; robust to distribution shifts | Requires multiple model inferences; computational overhead |
The benchmarking study by Ruffini et al. provides particularly insightful methodological guidance, demonstrating that no single fine-tuning strategy proves universally optimal across data regimes [114]. Their systematic comparison reveals that while CNNs with full fine-tuning perform robustly on small, imbalanced datasets, foundation models with parameter-efficient fine-tuning (PEFT) methods like LoRA and BitFit achieve competitive results on larger datasets, highlighting the context-dependent nature of algorithm selection.
Experimental Workflow for Benchmarking Medical Imaging Algorithms
The following diagram illustrates the comprehensive experimental workflow common to rigorous benchmarking in medical imaging challenges, integrating both technical and clinical validation components:
Benchmarking Metrics and Performance Evaluation
Quantitative Evaluation Frameworks
Robust evaluation constitutes the foundation of meaningful benchmarking in medical imaging challenges. The ISBI 2025 ecosystem employs multifaceted metrics tailored to clinical relevance and statistical rigor:
- Handling Class Imbalance: The benchmarking of foundation models for COVID-19 prognosis employs Matthews Correlation Coefficient (MCC) and Precision-Recall AUC (PR-AUC), which provide more informative performance assessments on imbalanced datasets compared to traditional accuracy metrics [114].
- Segmentation Quality Control: The comprehensive failure detection benchmarking study advocates for risk-coverage analysis as a holistic evaluation approach, with the pairwise Dice score between ensemble predictions emerging as a simple yet robust baseline for failure detection in medical image segmentation [115].
- Cross-validation Protocols: The MedFMC benchmark employs rigorous evaluation with metrics computed as an average of ten individual runs of the same testing process to ensure statistical reliability [113].
Comprehensive Benchmarking Metrics Table
Table 3: Metrics for Benchmarking Medical Imaging Algorithms
| Metric Category | Specific Metrics | Optimal Use Cases | Interpretation Guidelines |
|---|---|---|---|
| Classification Performance | Matthews Correlation Coefficient (MCC), Precision-Recall AUC [114] | Imbalanced medical datasets; rare disease detection | MCC > 0.7 indicates strong model; PR-AUC more informative than ROC-AUC for imbalance |
| Segmentation Accuracy | Dice Similarity Coefficient, Pairwise Dice for failure detection [115] | Anatomical structure segmentation; treatment planning | Dice > 0.7 clinically acceptable; > 0.9 excellent |
| Generalization Assessment | Performance drop on external validation sets [116] | Multi-institutional evaluations; domain shift measurement | Drop < 10% indicates good generalization |
| Failure Detection | Area Under the Risk-Coverage Curve (AURC) [115] | Quality control in automated segmentation | Higher AURC indicates better failure identification |
| Bias and Fairness | Performance disparities across patient subgroups [117] | Evaluating model equity across demographics | < 10% difference between subgroups recommended |
Confidence Aggregation in Failure Detection
The benchmarking of failure detection methods reveals critical insights into quality assurance for medical image segmentation. The following diagram illustrates the role of confidence aggregation in identifying potential segmentation failures:
Research Reagents and Computational Tools
The experimental frameworks employed in ISBI 2025 challenges rely on carefully curated resources and computational tools that constitute the essential "reagents" for reproducible medical imaging research:
Table 4: Essential Research Resources for Medical Imaging Benchmarking
| Resource Category | Specific Tools/Datasets | Primary Function | Access Considerations |
|---|---|---|---|
| Benchmark Datasets | MedFMC (22,349 images across 5 tasks) [113] | Standardized evaluation of generalizability across diverse clinical tasks | Publicly accessible; includes multiple modalities and annotation types |
| Out-of-Distribution Detection Benchmarks | OpenMIBOOD [116] | Evaluation of model robustness to distribution shifts | Framework available on GitHub; some datasets require formal access requests |
| Fairness Assessment Platforms | FairMedFM [117] | Comprehensive bias evaluation across patient subgroups | Integrates 17 datasets; explores 20 foundation models |
| Evaluation Codebases | OpenMIBOOD evaluation scripts [116] | Reproducible implementation of evaluation metrics | Open-source; supports extendible functionalities |
| Foundation Models | CLIP, DINO, Vision Transformers [113] | Pre-trained backbones for parameter-efficient adaptation | Various pre-training datasets and architectures |
The ISBI 2025 challenges represent the evolving frontier of benchmarking methodologies in medical imaging engineering and physics research. Several strategic directions emerge from analyzing these coordinated efforts:
First, there is a clear transition from isolated task-specific optimization toward the development of generalizable foundation models capable of adaptation across multiple clinical domains. The Foundation Model Challenge for Ultrasound Image Analysis announced for ISBI 2026 exemplifies this direction, focusing on models that generalize across diverse ultrasound imaging tasks and anatomical regions [118]. This aligns with the broader thesis that medical imaging research must balance domain-specific precision with architectural flexibility.
Second, increasing emphasis on real-world clinical constraints marks a maturation of the field. Challenges such as CXR-LT 2026 explicitly address long-tailed multi-label classification with imbalanced disease prevalence and cross-institutional distribution shifts [118], moving beyond clean laboratory conditions to the messy realities of clinical practice.
Finally, the systematic attention to failure detection, uncertainty quantification, and fairness assessment represents a crucial evolution in benchmarking comprehensiveness. The integration of these considerations reflects the growing recognition that mere average-case performance is insufficient for clinical deployment, where worst-case reliability and equitable performance across patient populations constitute essential requirements.
These collective efforts underscore that rigorous, multifaceted benchmarking remains indispensable for translating engineering innovations into clinically impactful solutions, ensuring that advances in medical imaging algorithms genuinely address the complex challenges of modern healthcare.
Conclusion
The field of medical imaging is undergoing a profound transformation, driven by the convergence of advanced physics, sophisticated engineering, and powerful artificial intelligence. The journey from understanding core physical principles to deploying multimodal foundation models illustrates a clear trajectory toward more personalized, precise, and accessible diagnostics. While significant challenges remain—particularly in model transparency, data privacy, and robust validation—the ongoing developments in explainable AI, portable imaging, and rigorous benchmarking provide a clear path forward. For researchers and drug development professionals, these advances offer unprecedented tools for discovery and translation. The future will likely see deeper integration of AI into the fabric of medical imaging, the rise of more generalizable and data-efficient models, and a stronger emphasis on ethically sound and clinically actionable systems, ultimately shaping a new era in precision medicine and patient care.
References
- 1. Physics of magnetic resonance imaging - Wikipedia [https://en.wikipedia.org/wiki/Physics_of_magnetic_resonance_imaging]
- 2. Workshops [https://biomedicalimaging.org/2025/workshops/]
- 3. Objective Comparison of Quantitative Imaging Modalities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3150581/]
- 4. Introducing the Node Reporting and Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8270876/]
- 5. Modern Diagnostic Imaging Technique Applications and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9192206/]
- 6. The Evolution of Medical Imaging [https://lakezurichopenmri.com/evolution-of-medical-imaging/]
- 7. The Evolution of Diagnostic Imaging: A Journey Through ... [https://www.glmi.com/blog/the-evolution-of-diagnostic-imaging-a-journey-through-time]
- 8. hybrid imaging technologies and SPECT/CT - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3288981/]
- 9. Hybrid Imaging: Instrumentation and Data Processing [https://www.frontiersin.org/journals/physics/articles/10.3389/fphy.2018.00047/full]
- 10. A Dive into the World of 3D Medical Imaging [https://openmedscience.com/a-dive-into-the-world-of-3d-medical-imaging/]
- 11. Improved 3D reconstruction pipeline for enhancing the ... [https://www.nature.com/articles/s41598-025-18318-x]
- 12. Three-Dimensional Imaging, Visualization, and Display 2025 [https://spie.org/Publications/Proceedings/Volume/13465]
- 13. Dual Energy CT Physics—A Primer for the Emergency ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10364985/]
- 14. Scattered Radiation and Contrast [http://www.sprawls.org/resources/IMGCHAR/module/]
- 15. Gadolinium Magnetic Resonance Imaging - StatPearls - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK482487/]
- 16. Radiopharmaceuticals for PET and SPECT Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC9103893/]
- 17. SPECT vs PET | Fastest Clinical Research Organization [https://www.tracercro.com/resources/blogs/spect-vs-pet-in-drug-development/]
- 18. Recent advances on the development of phantoms using 3D printing... [https://pubmed.ncbi.nlm.nih.gov/29933508/]
- 19. Innovative Medical Imaging for 2025 - Acertara [https://acertaralabs.com/5-new-ultrasound-capabilities-innovative-medical-imaging-for-2025/]
- 20. Ultrasound Technology in AI Medical Imaging [https://openmedscience.com/the-future-of-ultrasound-imaging-key-developments-shaping-2025-and-beyond/]
- 21. Predictive techniques in medical imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC12218343/]
- 22. Multiple radiations and its effect on biological system [https://pmc.ncbi.nlm.nih.gov/articles/PMC11995768/]
- 23. What Really Happens? The Impact of Radiation Inside ... [https://www.versantphysics.com/2025/01/31/what-really-happens-the-impact-of-radiation-inside-the-body/]
- 24. Effects Induced in Human Cells and Tissues by Low Doses ... [https://www.mdpi.com/2673-592X/5/2/10]
- 25. Radiation Safety and Protection - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK557499/]
- 26. Radiation Dosimetry: CT (Revised 6-4-2025) [https://accreditationsupport.acr.org/support/solutions/articles/11000056198-radiation-dosimetry-ct-revised-6-4-2025-]
- 27. Exploring molecular and modular insights into space ... [https://www.nature.com/articles/s41526-025-00508-6]
- 28. Impact of ionizing radiation and low-energy electrons on ... [https://www.sciencedirect.com/science/article/pii/S1687157X25000459]
- 29. Foundation models for radiology [https://dirjournal.org/articles/foundation-models-for-radiology-fundamentals-applications-opportunities-challenges-risks-and-prospects/dir.2025.253445]
- 30. Foundation models for radiology—the position of the AI for ... [https://insightsimaging.springeropen.com/articles/10.1186/s13244-025-02056-9]
- 31. Accurate predictions on small data with a tabular ... [https://www.nature.com/articles/s41586-024-08328-6]
- 32. Multimodal fusion techniques: Review, data representation ... [https://www.sciencedirect.com/science/article/abs/pii/S0925231225014997]
- 33. Multimodal Integration in Health Care: Development With ... [https://www.jmir.org/2025/1/e76557]
- 34. Multimodal AI in Healthcare: Use Cases with Examples [https://research.aimultiple.com/multimodal-ai-in-healthcare/]
- 35. Imaging & Medical Physics [https://physics.duke.edu/research/imaging-and-medical-physics]
- 36. The physical and biological basis of quantitative parameters derived... [https://qims.amegroups.org/article/view/1315/1771]
- 37. Diffusion weighted magnetic resonance imaging and its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4426106/]
- 38. Diffusion tensor imaging and tractwise fractional statistics... anisotropy [https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/1475-925X-6-42]
- 39. Finding the limits of deep learning clinical sensitivity with fractional ... [https://pubmed.ncbi.nlm.nih.gov/38933144/]
- 40. To Reduce or Not to Reduce Input Data? Finding the Limits of... :: SSRN [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4713167]
- 41. Empowering drug development - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10014695/]
- 42. What is an imaging biomarker? An important tool in drug ... [https://antarosmedical.com/blog/what-is-an-imaging-biomarker-an-important-tool-in-drug-development/]
- 43. Neuroimaging Biomarkers for Drug Discovery and ... [https://www.sciencedirect.com/science/article/pii/S0006322324000362]
- 44. Automated Machine Learning in medical research [https://www.sciencedirect.com/science/article/abs/pii/S0933365725002374]
- 45. Understanding the Rise of Automated Machine Learning [https://www.mdpi.com/2078-2489/16/11/994]
- 46. Assessing Quantitative Performance and Expert Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462693/]
- 47. Master Radiology Workflow Optimization [https://curogram.com/blog/mastering-radiology-workflow-optimization-medical-imaging]
- 48. Cardio oncology: Digital innovations, precision medicine ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2022.951551/full]
- 49. Quantitative Image Quality Comparison of Reduced [https://pmc.ncbi.nlm.nih.gov/articles/PMC5573232/]
- 50. Artificial Intelligence to Enhance Precision Medicine in Cardio ... [https://professional.heart.org/en/science-news/artificial-intelligence-to-enhance-precision-medicine-in-cardio-oncology]
- 51. International Day of Medical Physics 2025 [https://oncodaily.com/insight/medical-physics-2025]
- 52. Rise of mobile medical imaging to revolutionise healthcare [https://www.worldhealthexpo.com/insights/medical-technology/rise-of-mobile-medical-imaging-to-revolutionise-healthcare]
- 53. Rural Areas Face Imaging Obstacles on the Road to Health ... [https://www.rsna.org/news/2021/june/rural-radiology-equity]
- 54. Bringing imaging to the people: Enhancing access and ... [https://www.sciencedirect.com/science/article/abs/pii/S1939865424004466]
- 55. Point-of-Care Ultrasound: A Practical Guide for Primary Care [https://www.aafp.org/pubs/fpm/issues/2020/1100/p33.html]
- 56. Basic Principles of Ultrasound Physics and Artifacts Made ... [https://www.pocus101.com/basic-principles-of-ultrasound-physics-and-artifacts-made-easy/]
- 57. Industry Day [https://biomedicalimaging.org/2025/industry-day/]
- 58. A Comprehensive Framework for Accountable AI in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383817/]
- 59. Advancing AI Interpretability in Medical Imaging [https://www.mdpi.com/2504-4990/7/1/12]
- 60. Grad-CAM (Gradient-weighted Class Activation Mapping) [https://www.sciencedirect.com/science/article/abs/pii/S0010482525015537]
- 61. A Comparative Analysis of Pixel-Level Interpretability and ... [https://ownyourai.com/advancing-ai-interpretability-in-medical-imaging-a-comparative-analysis-of-pixel-level-interpretability-and-grad-cam-models/]
- 62. Assessment of a Grad-CAM interpretable deep learning model ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-025-03256-5]
- 63. Explainable AI in medical imaging: an interpretable and ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1535478/full]
- 64. Artificial intelligence in medical imaging: From task-specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11925424/]
- 65. Foundation Models in Medical Imaging - A Review and ... [https://arxiv.org/html/2506.09095v1]
- 66. Revolutionizing Medical Imaging: The Transformative Role of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191749/]
- 67. AI enhanced diagnostic accuracy and workload reduction ... [https://www.nature.com/articles/s41746-025-01892-9]
- 68. AI Medical Imaging Lab [https://medschool.cuanschutz.edu/radiology/research/labs/ai-medical-imaging-lab]
- 69. HIPAA-Compliant Medical AI with TEE [https://phala.com/learn/HIPAA-Compliant-Medical-AI]
- 70. 2025 HIPAA IT Compliance Guide [https://www.atlantic.net/hipaa-data-centers/hipaa-compliant-it-infrastructure-guide/]
- 71. HIPAA Compliance in the Age of AI: Safeguarding ePHI for ... [https://research.cgu.edu/icdc/2025/07/26/hipaa-compliance/]
- 72. New 2025 HIPAA Regulations: Key Changes & How to ... [https://www.hipaavault.com/resources/2025-hipaa-new-regulations/]
- 73. Accelerating Clinical Imaging Intelligence with HIPAA ... [https://caylent.com/blog/accelerating-clinical-imaging-intelligence-with-hipaa-compliant-ai-solutions]
- 74. Addressing fairness in artificial intelligence for medical ... [https://www.nature.com/articles/s41467-022-32186-3]
- 75. Bias in artificial intelligence for medical imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC11880872/]
- 76. A scoping review and evidence gap analysis of clinical AI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12167363/]
- 77. Fairness: Mitigating | Machine Learning | Google for Developers bias [https://developers.google.com/machine-learning/crash-course/fairness/mitigating-bias]
- 78. FAIMI | Fairness of AI in Medical Imaging [https://faimi-workshop.github.io/]
- 79. Reinventing radiology imaging workflows with agentic AI [https://research.gehealthcare.com/patient-care-pathways/reinventing-radiology-imaging-workflows-with-agentic-ai-jb35459xx/]
- 80. The future of AI in radiology is the AI you barely notice - Blog [https://www.philips.com/a-w/about/news/archive/blogs/innovation-matters/2025/the-future-of-ai-in-radiology-is-the-ai-you-barely-notice]
- 81. Radiology Reimagined: AI, innovation and interoperability ... [https://www.rsna.org/artificial-intelligence/radiology-reimagined-ai]
- 82. Incorporation of quantitative imaging data using artificial ... [https://pubmed.ncbi.nlm.nih.gov/38156985/]
- 83. The 2025 guide to clinical-ready tools [Using AI for X-ray] [https://www.azmed.co/news-post/ai-in-radiology-the-2025-guide-to-clinical-ready-tools-using-ai-for-x-ray]
- 84. Revolutionizing Precision Medicine with Quantitative Imaging [https://fas.org/publication/ai-enabled-precision-medicine/]
- 85. Role Of AI In Medical Imaging [https://www.rsna.org/news/2025/january/role-of-ai-in-medical-imaging]
- 86. H2O Driverless AI [https://h2o.ai/platform/ai-cloud/make/h2o-driverless-ai/]
- 87. Top AI Platforms to Drive Business Growth in 2025 [https://www.curotec.com/insights/leading-ai-platforms/]
- 88. Amazon Rekognition [https://aws.amazon.com/rekognition/]
- 89. Architecture | H2O AI Cloud | Docs [https://docs.h2o.ai/haic-documentation/overview/architecture]
- 90. Amazon Rekognition Video [https://aws.amazon.com/rekognition/video-features/]
- 91. Architecture and Sequence Diagrams - Amazon Rekognition [https://docs.aws.amazon.com/rekognition/latest/dg/face-liveness-diagrams.html]
- 92. H2O Driverless AI [https://h2o.ai/resources/product-brief/h2o-driverless-ai/]
- 93. The AI Problem in Hallucination | by Chaos To Clarity | Medium 2025 [https://medium.com/@sonal.sadafal/the-ai-hallucination-problem-in-2025-af49057c7cfc]
- 94. New sources of inaccuracy? A conceptual framework for studying AI ... [https://misinforeview.hks.harvard.edu/article/new-sources-of-inaccuracy-a-conceptual-framework-for-studying-ai-hallucinations/]
- 95. Exploring the potential of generative artificial intelligence in ... [https://www.sciencedirect.com/science/article/pii/S258975002500072X]
- 96. Physics-informed machine learning for advancing ... [https://link.springer.com/article/10.1007/s10462-025-11303-w]
- 97. in AI : Causes, Impact, and... - DEV Community Hallucinations 2025 [https://dev.to/navyashipsit/ai-hallucinations-in-2025-causes-impact-and-solutions-for-trustworthy-ai-4mga]
- 98. Making Color Usage Accessible [https://www.section508.gov/create/making-color-usage-accessible/]
- 99. Color Contrast Accessibility: Complete WCAG 2025 Guide ... [https://www.allaccessible.org/blog/color-contrast-accessibility-wcag-guide-2025]
- 100. Contrast Checker [https://webaim.org/resources/contrastchecker/]
- 101. AAPM, ACR, RSNA, and SIIM Announce Joint Effort to ... [https://www.rsna.org/media/press/i/2607]
- 102. ESR Essentials: common performance metrics in AI ... [https://link.springer.com/article/10.1007/s00330-025-11890-w]
- 103. Similarity and quality metrics for MR image-to- ... [https://www.nature.com/articles/s41598-025-87358-0]
- 104. Analyzing the F1 Score: A Comprehensive Metric for ... [https://www.simbo.ai/blog/analyzing-the-f1-score-a-comprehensive-metric-for-assessing-ai-model-effectiveness-in-healthcare-3890496/]
- 105. F1 Score for Model Evaluation: Calculation, Interpretation & ... [https://futureagi.com/blogs/f1-score-evaluating-classifiers-2025]
- 106. Evaluating Super-Resolution Models in Biomedical Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027580/]
- 107. A stochastic structural similarity guided approach for multi- ... [https://www.nature.com/articles/s41598-025-93662-6]
- 108. LG Debuts Next-Generation Precision Medical AI [https://www.prnewswire.com/news-releases/lg-debuts-next-generation-precision-medical-ai-302502425.html]
- 109. LG Debuts Next-Generation Precision Medical AI [https://ai-techpark.com/lg-debuts-next-generation-precision-medical-ai/]
- 110. Interoperability [https://www.healthit.gov/topic/interoperability]
- 111. HHS Announces New and Renewed Efforts to Promote ... [https://www.ropesgray.com/en/insights/alerts/2025/09/hhs-announces-new-and-renewed-efforts-to-promote-health-information-sharing-and-interoperability]
- 112. Challenges [https://biomedicalimaging.org/2025/challenges/]
- 113. A Real-world Dataset and Benchmark For Foundation ... [https://www.nature.com/articles/s41597-023-02460-0]
- 114. Benchmarking Foundation Models and Parameter-Efficient ... [https://arxiv.org/abs/2506.18434]
- 115. Comparative benchmarking of failure detection methods in medical ... [https://pubmed.ncbi.nlm.nih.gov/39657400/]
- 116. GitHub - remic-othr/OpenMIBOOD: Medical for... Imaging Benchmarks [https://github.com/remic-othr/OpenMIBOOD]
- 117. FairMedFM: Fairness Benchmarking for Medical Imaging ... [https://proceedings.neurips.cc/paper_files/paper/2024/hash/c9826b9ea5e1b49b256329934a578d83-Abstract-Datasets_and_Benchmarks_Track.html]
- 118. Challenges – ISBI 2026 [https://biomedicalimaging.org/2026/challenges/]