Navigating Ethical Frontiers: A Comprehensive Guide to Biomedical Engineering Society Codes of Ethics
This article provides a detailed examination of the ethical frameworks established by leading biomedical engineering societies, including the Biomedical Engineering Society (BMES) and the Engineering in Medicine and Biology Society...
Navigating Ethical Frontiers: A Comprehensive Guide to Biomedical Engineering Society Codes of Ethics
Abstract
This article provides a detailed examination of the ethical frameworks established by leading biomedical engineering societies, including the Biomedical Engineering Society (BMES) and the Engineering in Medicine and Biology Society (EMBS). Tailored for researchers, scientists, and drug development professionals, it explores foundational ethical principles, their practical application in research and development, strategies for resolving complex ethical dilemmas, and the systems in place for professional validation and compliance. By integrating theoretical guidelines with real-world case studies and professional standards, this overview serves as an essential resource for upholding integrity and advancing public health in the rapidly evolving field of biomedical engineering.
The Bedrock of Integrity: Core Principles in Biomedical Engineering Ethics
The field of biomedical engineering stands at the intersection of technological innovation, human health, and ethical responsibility. Society codes of ethics serve as the foundational frameworks that translate abstract moral principles into actionable professional standards for researchers, scientists, and drug development professionals. These codes establish the professional mandate—the collective commitment to conduct that transcends legal requirements and embraces the broader social and ethical implications of biomedical innovation. In an era of rapid technological advancement, with emerging areas such as CRISPR genome editing, brain-computer interfaces, and artificial intelligence in medicine, these ethical codes provide the critical guidance necessary to navigate complex dilemmas while maintaining public trust [1].
The fundamental purpose of these codes is to articulate the profession's core values and expectations, creating a shared understanding of responsible conduct across disciplines and institutions. For biomedical engineers, whose work directly impacts human health and wellbeing, this ethical framework is not supplementary but central to professional identity. As noted in critical analyses of the field, "Biomedical engineering is responsible for many of the dramatic advances in modern medicine. This has resulted in improved medical care and better quality of life for patients. However, biomedical technology has also contributed to new ethical dilemmas and has challenged some of our moral values" [2]. Society codes of ethics serve as the essential compass for navigating these dilemmas, providing both direction for action and accountability mechanisms when standards are breached.
Comparative Analysis of Biomedical Engineering Society Codes
Core Ethical Principles and Their Applications
Biomedical engineering codes of ethics across professional societies share common foundational principles while emphasizing different aspects based on their organizational focus and membership. These principles provide the philosophical underpinnings for professional conduct and decision-making frameworks.
Beneficence and Non-maleficence represent complementary duties toward patients and research subjects. The principle of beneficence requires biomedical engineers to actively promote patient wellbeing through their designs, devices, and technologies, while non-maleficence demands the avoidance of harm through rigorous testing, risk assessment, and safety protocols [3]. This includes "designing, developing, and maintaining medical devices and technologies that are safe, reliable, and effective for patient use" through "rigorous testing and validation of medical devices and technologies to minimize the risk of adverse events" [3].
Respect for Autonomy acknowledges the right of patients and research subjects to make informed decisions about their care and participation. This principle requires biomedical engineers to ensure patients receive "clear and comprehensive information about medical devices and technologies used in their care to enable them to make informed decisions" [3]. This extends to respecting cultural, social, and individual factors that may influence patient autonomy and implementing appropriate safeguards for those with diminished capacity [3].
Justice in biomedical engineering ethics encompasses both distributive justice (fair allocation of resources and technologies) and social justice (addressing healthcare disparities). The principle demands that "biomedical engineers ensure fair and equitable access to healthcare technologies and services, regardless of a patient's socioeconomic status or background" [3]. This has become particularly salient during public health crises, as evidenced by the COVID-19 pandemic, which forced difficult ethical decisions regarding "the allocation of medical devices, the responsibilities of science and technology, and the inadequacy of regulations and norms, which lack universality" [4].
Integrity and Honesty form the bedrock of professional relationships and scientific enterprise. These principles require truthfulness and transparency in all professional activities, including "accurately reporting research findings, disclosing potential conflicts of interest, and acknowledging the contributions of others" [3]. The Biomedical Engineering Society (BMES) Code of Ethics specifically emphasizes "promoting transparency, implementing reporting systems for violations and establishing ethical decision-making models to standardize procedures" [5].
Comparative Table of Professional Society Codes
Table 1: Comparison of Ethical Principles Across Engineering Societies
| Ethical Principle | BMES | IEEE EMBS | NSPE | ASCE |
|---|---|---|---|---|
| Public Welfare | Explicitly emphasized | Explicitly emphasized | Primary emphasis | Primary emphasis |
| Research Integrity | Required | Required through scientific integrity | Implied | Implied |
| Privacy & Confidentiality | Required | Explicit requirement for patient data | Not specified | Not specified |
| Environmental Responsibility | Not specified | Explicit requirement | Not specified | Explicitly emphasized |
| Conflict of Interest | Avoidance or disclosure required | Avoidance or disclosure required | Required | Required |
| Interdisciplinary Respect | Explicitly required | Explicitly required | Not specified | Emphasized for collaboration |
| Professional Competence | Required | Implied through research standards | Required | Required |
| Reporting Violations | Systems established | Not specified | Explicit mechanism | Explicit mechanism |
Note: BMES = Biomedical Engineering Society; IEEE EMBS = Institute of Electrical and Electronics Engineers Engineering in Medicine and Biology Society; NSPE = National Society of Professional Engineers; ASCE = American Society of Civil Engineers. Data synthesized from multiple sources [5] [6] [7].
The comparative analysis reveals both universal principles and distinctive emphases across professional societies. While all major engineering codes prioritize public welfare, biomedical societies place particular emphasis on research integrity, privacy protection, and interdisciplinary collaboration—reflecting the unique challenges at the intersection of engineering, biology, and medicine. The IEEE EMBS code specifically addresses environmental responsibility, requiring members to "support the preservation of a healthy environment," while BMES emphasizes creating "a culture of knowledge exchange and mentorship" [6]. These nuances reflect how different engineering disciplines interpret and apply ethical principles within their specific professional contexts.
Implementation Framework for Ethical Decision-Making
Methodologies for Ethical Analysis and Application
Translating ethical principles into professional practice requires structured methodologies for analyzing and resolving dilemmas. Several established frameworks provide biomedical engineers with systematic approaches to ethical decision-making.
The Four Principles Approach provides a quadrant-based methodology that balances competing ethical demands through the principles of autonomy, beneficence, non-maleficence, and justice [3]. When facing an ethical dilemma, biomedical engineers using this framework would identify how each principle applies to the situation, determine where principles may conflict, and seek a resolution that respects all four principles to the greatest extent possible. This approach was developed specifically for biomedical ethics and has been widely adopted in healthcare settings.
Utilitarian Analysis applies a consequentialist framework to ethical dilemmas, seeking to maximize overall benefit and minimize harm. This methodology involves identifying all stakeholders who would be affected by a decision, calculating potential benefits and harms for each group, and selecting the course of action that produces the greatest net benefit [3]. During resource allocation decisions, such as those encountered during the COVID-19 pandemic, "utilitarianism, which focuses on maximizing overall utility or well-being, can be applied to biomedical engineering dilemmas to determine the course of action that produces the greatest good for the greatest number of people" [3].
Deontological Frameworks emphasize adherence to moral duties and rules regardless of consequences. This approach involves identifying one's duties in a given situation (e.g., duty to protect patient safety, duty to maintain confidentiality, duty to be truthful) and selecting the course of action that best fulfills these obligations [3]. For biomedical engineers, this might mean upholding safety standards even when faced with pressure to accelerate product development timelines.
Casuistry or Case-Based Reasoning employs analogical thinking by comparing current ethical dilemmas with previously resolved cases [3]. This methodology involves identifying paradigmatic cases with established ethical consensus, noting relevant similarities and differences with the current situation, and determining whether the same ethical resolution should apply. This approach allows biomedical engineers to draw on established precedents while recognizing the unique aspects of each situation.
Ethical Decision-Making Workflow
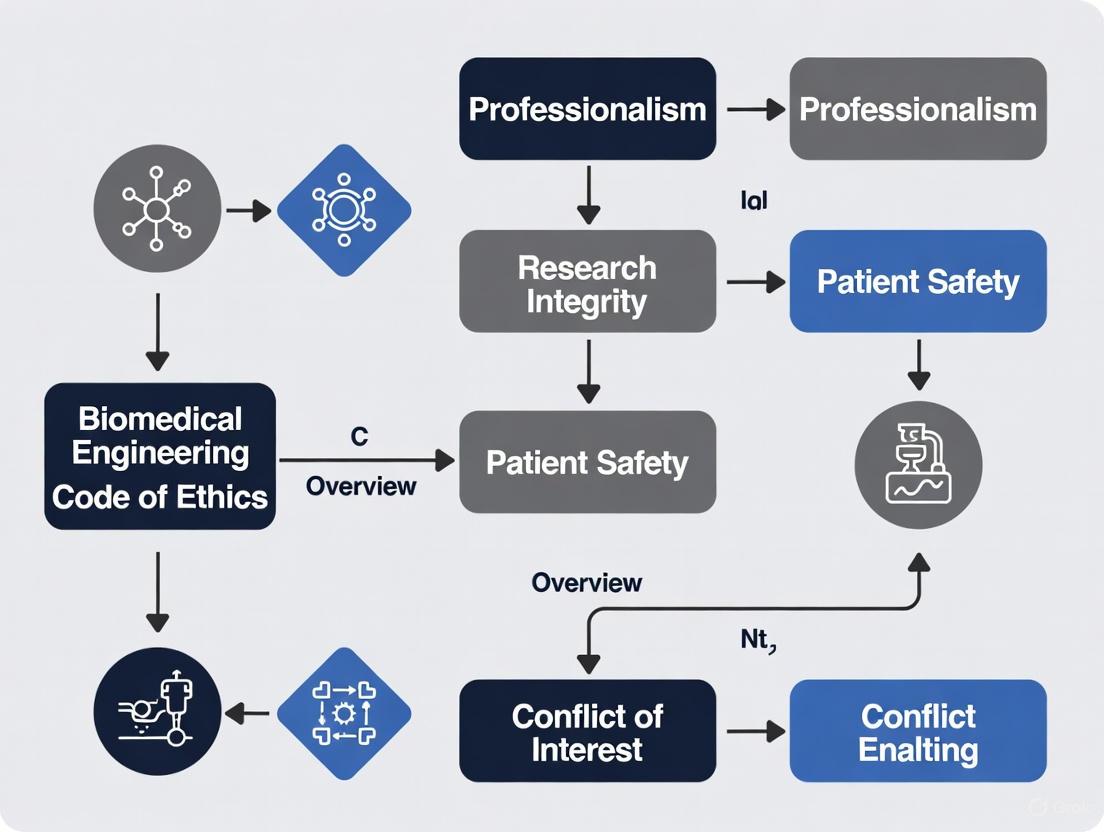
Diagram 1: Ethical Decision-Making Workflow. This diagram illustrates a systematic methodology for addressing ethical dilemmas in biomedical engineering practice and research.
The ethical decision-making workflow provides biomedical engineers with a structured process for navigating complex situations. This methodology begins with thorough fact-finding and stakeholder analysis, followed by the application of multiple ethical frameworks and consultation of relevant professional codes. After generating and evaluating alternatives, the engineer implements the chosen course of action with appropriate documentation and follow-up assessment. This systematic approach ensures consistent, transparent, and defensible ethical reasoning, particularly valuable in situations involving competing priorities or stakeholder interests.
Current Challenges and Special Considerations
Emerging Ethical Dilemmas in Biomedical Engineering Practice
Biomedical engineers today face novel ethical challenges that test the applicability and completeness of existing ethical codes. These emerging dilemmas require careful consideration and sometimes the evolution of ethical standards.
Resource Allocation and Triage Protocols became critically urgent during the COVID-19 pandemic, when biomedical engineers faced "the dilemma of identifying criteria for the allocation of medical devices" as healthcare systems were overwhelmed [4]. The pandemic revealed that "within a few weeks, the available resources (i.e., medical devices, doctors, nurses) proved to be insufficient to cover the care needs of the multitude of COVID-19 patients, beyond the ordinary needs of other patients" [4]. These situations forced difficult ethical choices between clinical criteria (prioritizing those with the greatest medical need) and utilitarian considerations (prioritizing those with the greatest likelihood of survival).
Do-It-Yourself (DIY) Medical Solutions emerged as an unregulated response to equipment shortages during the pandemic, creating new ethical concerns. The "rise of useless and potentially harmful DIY approaches to PPE and medical devices could have been easily avoided at the start of the pandemic by decision-makers initially consulting with domain experts, such as biomedical and clinical engineers" [4]. This phenomenon highlighted the tension between innovation and safety, as "although very admirable, this approach is not feasible in critical sectors such as medical devices or PPE, which require postgraduate education, years of experience and deep knowledge of relevant international standards and norms, in order to ensure appropriate levels of safety, efficacy and resilience" [4].
Dual-Use Dilemmas involve biomedical technologies developed for beneficial purposes that could be misused for harm. "In biomedical research, the dual-use dilemma is an ethical consideration regarding the potential misuse or abuse of certain biomedical technologies" [5]. For example, "research on a deadly virus such as H1N1 (swine flu) could potentially lead to advances in treatment, but it also poses risks if the dangerous pathogen gets into the wrong hands" [5]. Biomedical engineers must therefore "weigh the pros and cons of their research and seek to mitigate any misuse of dangerous substances by implementing strict security measures, ethical guidelines and oversight" [5].
Genome Editing and Enhancement Ethics represent frontier ethical challenges as technologies like CRISPR advance rapidly. Educational initiatives now prepare biomedical engineers to consider "the ethical ideas and problems" pertaining to "CRISPR and the ever-evolving field of genome engineering" [1]. These technologies raise fundamental questions about "the ownership and commercialization of organoids used in basic research" and the potential for non-therapeutic enhancements that could exacerbate social inequalities [1].
Research Reagents and Tools for Ethical Analysis
Table 2: Essential Methodologies for Ethical Analysis in Biomedical Engineering Research
| Methodology/Tool | Function | Application Context |
|---|---|---|
| Four Principles Framework | Provides balanced ethical analysis through autonomy, beneficence, non-maleficence, and justice | Clinical trials, device design, resource allocation decisions |
| Belmont Report Principles | Guides research ethics through respect for persons, beneficence, and justice | Human subjects research, study design, informed consent processes |
| Utilitarian Analysis | Maximizes overall benefit and minimizes harm | Public health interventions, resource allocation, policy development |
| Deontological Analysis | Focuses on moral duties and rules | Safety protocols, quality assurance, regulatory compliance |
| Casuistry (Case-Based Reasoning) | Applies precedents from established cases | Novel ethical dilemmas, institutional policy development |
| Institutional Review Boards (IRBs) | Provides independent ethical oversight | Research protocols involving human subjects, clinical investigations |
| Ethical Impact Assessment | Systematically evaluates potential ethical implications | New technology development, research program planning |
These methodologies serve as essential "research reagents" for ethical analysis, providing structured approaches to identifying, analyzing, and resolving ethical challenges in biomedical engineering. Unlike laboratory reagents, these are intellectual tools that enable systematic reasoning about moral questions. Their proper application requires both knowledge of the methodologies themselves and understanding of when each is most appropriately deployed.
Society codes of ethics in biomedical engineering represent more than static documents—they embody a dynamic professional mandate that evolves alongside technological capabilities and social expectations. These codes serve simultaneously as compass, contract, and covenant: guiding professional judgment, establishing standards for accountability, and affirming the profession's commitment to societal wellbeing. As biomedical engineering continues to advance into new frontiers—from neuroengineering to synthetic biology—these ethical frameworks will require continual refinement and interpretation to address emerging challenges.
The true measure of these ethical codes lies not merely in their formulation but in their integration into the daily practice of biomedical researchers, scientists, and drug development professionals. This requires both formal education, such as dedicated ethics courses that provide "the foundational knowledge the students need to become well-rounded, ethical engineers" [1], and organizational cultures that support ethical conduct through "reporting systems for violations and establishing ethical decision-making models to standardize procedures" [5]. Through this integration, biomedical engineers can fulfill their professional mandate: to harness technological innovation for human benefit while conscientiously navigating the ethical dimensions of their work.
The integration of ethical principles into biomedical engineering practice provides a crucial framework for navigating the complex moral landscape of healthcare technology development. As the field of biomedical engineering operates at the intersection of patient care and technological innovation, the adoption of a structured ethical approach becomes paramount for ensuring responsible research and development. The four principles of biomedical ethics—beneficence, non-maleficence, autonomy, and justice—have emerged as cornerstones of ethical decision-making in healthcare contexts since their systematic articulation by Beauchamp and Childress in their seminal work, Principles of Biomedical Ethics [8]. These principles offer a comprehensive framework that guides professionals in balancing competing values and obligations when developing medical technologies and conducting research.
Within biomedical engineering, these principles transcend theoretical discourse to inform daily practice, institutional policies, and professional standards. The Biomedical Engineering Society (BMES) and other professional organizations have codified expectations for ethical conduct that reflect these core principles [5]. More recently, the development of a formal "Biomedical Engineer's Pledge" has created a symbolic counterpart to medicine's Hippocratic Oath, explicitly incorporating these principles into a ceremonial pledge for graduating engineers [9] [10]. This evolution underscores the growing recognition that ethical frameworks must be deeply embedded in the professional identity of biomedical engineers, whose decisions directly impact patient safety, healthcare efficacy, and the equitable distribution of medical resources.
The Four Ethical Principles: Foundations and Applications
Detailed Analysis of Core Principles
Beneficence
The principle of beneficence establishes a positive obligation for biomedical engineers to act in ways that promote the welfare and best interests of patients and other stakeholders. This principle requires more than merely avoiding harm; it demands active contribution to patient well-being through the design, development, and implementation of biomedical technologies [11] [12]. In practical terms, beneficence translates to creating medical devices and systems that actively improve health outcomes, enhance quality of life, and advance medical capabilities. For example, developing more effective diagnostic equipment, creating more responsive prosthetic limbs, or designing telemedicine platforms that expand access to care all represent applications of the beneficence principle.
The ethical commitment to beneficence requires biomedical engineers to prioritize projects and design choices that maximize potential benefits for end users. This involves not only technical excellence but also consideration of how technologies will integrate into clinical workflows and patient lives [5]. The principle acknowledges that biomedical engineering has a fundamental moral purpose: to apply engineering expertise toward improving human health. This positive duty distinguishes beneficence from the merely prohibitive nature of non-maleficence, establishing an affirmative ethical mandate for the profession [13].
Non-Maleficence
Non-maleficence, embodied by the maxim "first, do no harm" (primum non nocere), obligates biomedical engineers to refrain from causing harm or injury to patients through acts of commission or omission [8]. This principle finds practical application in rigorous risk assessment, comprehensive safety testing, and systematic error mitigation throughout the design and development process. The profound responsibility associated with non-maleficence in biomedical engineering is highlighted by historical cases where its violation led to tragic outcomes, such as the Therac-25 radiation therapy machine incidents, where design flaws and safety oversights resulted in patient fatalities [5].
The implementation of non-maleficence requires a proactive approach to identifying potential harms, including direct physical injuries, secondary complications, and more subtle psychological or social impacts. Biomedical engineers must establish robust quality control systems, implement fail-safe mechanisms, and conduct thorough failure mode analysis to satisfy their ethical duty of non-maleficence [5]. This principle also extends to considering potential misuse of technologies and implementing appropriate safeguards. In situations where some risk is unavoidable, non-maleficence requires careful weighing of potential harms against anticipated benefits, ensuring that risks are minimized and clearly communicated to users [8].
Autonomy
The principle of autonomy recognizes the right of individuals to make informed decisions about their own healthcare and participation in research [11]. This principle provides the ethical foundation for informed consent processes, truth-telling requirements, and respect for patient values and preferences. For biomedical engineers, supporting autonomy involves designing technologies that enhance rather than diminish patient self-determination, such as creating interfaces that provide clear information for decision-making or developing adjustable devices that accommodate individual preferences and needs [10].
The practical application of autonomy in biomedical engineering extends beyond device design to research practices and commercial interactions. Engineers must ensure that research participants receive complete and accurate information about procedures, risks, and benefits, and that their consent is voluntary and free from coercion [12]. This principle also demands transparency about device capabilities and limitations, avoiding deception or exaggeration that would undermine meaningful consumer choice. The growing emphasis on patient-centered design in medical technology reflects the increasing importance accorded to autonomy in biomedical engineering practice [13] [8].
Justice
The principle of justice requires the fair, equitable, and appropriate distribution of healthcare benefits and resources [8]. In biomedical engineering, this principle addresses concerns about accessibility, affordability, and the equitable distribution of technological innovations across diverse populations. Justice considerations prompt critical examination of how medical technologies might exacerbate or ameliorate existing healthcare disparities based on socioeconomic status, geographic location, race, ethnicity, or other factors [5].
The application of justice in biomedical engineering practice includes designing technologies with scalability and cost-effectiveness in mind, advocating for equitable access to medical innovations, and considering the needs of underserved populations during the research and development process [10]. This principle also encompasses fair subject selection in research, ensuring that participant burdens and benefits are distributed justly across communities. The growing emphasis on global health technology represents one response to justice concerns, focusing on developing appropriate, affordable technologies for resource-limited settings [14].
Table 1: Core Ethical Principles in Biomedical Engineering Practice
| Principle | Core Meaning | Primary Application in BME | Key Considerations |
|---|---|---|---|
| Beneficence | Duty to promote well-being and act in patients' best interests | Developing technologies that actively improve health outcomes | Benefit-risk analysis, therapeutic efficacy, quality of life improvement |
| Non-maleficence | Obligation to avoid causing harm | Rigorous safety testing, risk assessment, and error mitigation | Failure mode analysis, safety standards, harm prevention |
| Autonomy | Respect for individuals' right to self-determination | Informed consent processes, user-controlled devices, transparent design | Truth-telling, informed choice, respect for patient values |
| Justice | Fair distribution of benefits and burdens | Equitable access to technology, inclusive design, fair subject selection | Healthcare disparities, affordability, accessibility |
Interrelationship and Balancing of Principles
The four ethical principles do not function in isolation but rather form an interconnected framework that must be applied collectively to address complex ethical challenges. In practice, principles often come into tension, requiring careful balancing. For example, the development of an innovative but expensive medical technology might promote beneficence for those who can access it while potentially conflicting with justice if it remains unavailable to underserved populations [8]. Similarly, a perfectly safe device (non-maleficence) might provide limited therapeutic benefit (beneficence), necessitating trade-offs between these principles.
The process of ethical decision-making in biomedical engineering typically involves identifying which principles are relevant to a particular situation, assessing their relative weight in that context, and seeking solutions that honor the most compelling ethical claims [8]. This balancing process requires practical wisdom and moral reasoning rather than mechanical application of rules. The "Biomedical Engineer's Pledge" implicitly acknowledges this interplay by structuring its commitments hierarchically, with safety and well-being (encompassing non-maleficence and beneficence) receiving priority, followed by other commitments that reflect autonomy and justice [10].
Diagram 1: Ethical Decision Framework in Biomedical Engineering. This diagram illustrates how the four core principles inform the ethical decision-making process in biomedical engineering, requiring balancing and application through specific procedures to achieve ethical practice.
Implementation in Biomedical Engineering Practice
Institutionalization Through Codes and Pledges
The ethical principles of beneficence, non-maleficence, autonomy, and justice have been institutionalized within biomedical engineering through various formal mechanisms, including professional codes of ethics and, more recently, ceremonial pledges. The Biomedical Engineering Society (BMES) Code of Ethics embodies these principles by outlining norms and obligations that "fulfill a biomedical engineer's commitment to honesty and conscientiousness in scientific inquiry and technology development, and to advancing public health" [5]. This code provides concrete guidance for professional conduct that reflects the underlying principles, such as prioritizing patient safety (non-maleficence) and maintaining research integrity (justice).
The recently developed "Biomedical Engineer's Pledge" represents a significant advancement in professional identity formation, creating a symbolic counterpart to medicine's Hippocratic Oath that is specifically tailored to biomedical engineering [9]. This pledge explicitly incorporates the four principles through ten specific commitments, with the first commitment prioritizing "safety, health, and well-being" (beneficence and non-maleficence) and subsequent commitments addressing autonomy (ensuring "autonomy and dignity"), justice (non-discrimination, environmental sustainability, universal health coverage), and related ethical concerns [10]. The structured hierarchy of these commitments provides practical guidance for resolving conflicts between principles, with safety and well-being receiving priority.
Practical Application in Research and Development
The implementation of ethical principles extends beyond formal documents to daily practice in biomedical engineering research and development. This practical application occurs through several key processes:
Risk-Benefit Analysis: Systematic evaluation of potential harms against anticipated benefits represents a primary methodology for balancing beneficence and non-maleficence [10]. This analytical process requires quantitative assessment where possible, complemented by qualitative consideration of values and preferences. The Nuremberg Code established that "the degree of risk to be taken should never exceed that determined by the humanitarian importance of the problem to be solved by the experiment" [10], establishing a foundational approach for ethical risk-benefit assessment in biomedical engineering.
Informed Consent Protocols: Implementing autonomy requires developing comprehensive informed consent processes that ensure research participants and patients understand procedures, risks, benefits, and alternatives [12]. For biomedical engineers, this extends to creating clear documentation for clinical trials, designing intuitive device interfaces that support user understanding, and ensuring transparency about device capabilities and limitations.
Inclusive Design Practices: Applying the principle of justice involves actively considering diverse user needs during the design process to avoid technologies that disproportionately benefit specific populations while excluding others [5]. This includes addressing physical variability through ergonomic design, accommodating different technical literacies through intuitive interfaces, and considering economic constraints through appropriate technology development.
Ethical Oversight Mechanisms: Institutional Review Boards (IRBs) provide formal oversight for research involving human subjects, evaluating proposals for ethical considerations, scientific merit, and regulatory compliance [12]. These boards assess whether research protocols adequately address all four ethical principles, particularly through risk minimization (non-maleficence), informed consent (autonomy), fair subject selection (justice), and potential benefits (beneficence).
Table 2: Ethical Assessment Framework for Biomedical Engineering Research
| Research Phase | Primary Ethical Considerations | Application Methods | Documentation Requirements |
|---|---|---|---|
| Protocol Development | Social value, scientific validity | Literature review, stakeholder consultation | Research protocol, rationale for approach |
| Risk-Benefit Assessment | Non-maleficence, beneficence | Systematic risk identification, benefit analysis | Risk categorization, mitigation strategies |
| Participant Selection | Justice, fairness | Inclusion/exclusion criteria, recruitment plan | Demographic representation plan |
| Informed Consent | Autonomy, respect for persons | Consent form development, process design | Documentation of consent process |
| Ongoing Monitoring | Non-maleficence, beneficence | Data safety monitoring, interim analysis | Safety reports, protocol modifications |
Case Studies Illustrating Ethical Challenges
Real-world cases provide valuable insights into the critical importance of rigorously applying ethical principles in biomedical engineering:
Therac-25 Radiation Therapy Incidents: This case represents a profound failure of non-maleficence, where software design flaws and inadequate safety engineering resulted in fatal radiation overdoses to patients [5]. The incidents highlighted the essential responsibility of biomedical engineers to implement comprehensive safety measures, including fail-safe mechanisms, rigorous testing protocols, and thorough investigation of error reports. The tragedy underscored how technological complexity creates ethical obligations for engineers to anticipate and prevent potential harms through defensive design strategies.
Bjork-Shiley Heart Valve: This case involved a prosthetic heart valve with a design flaw that led to strut failure and catastrophic outcomes for patients [5]. Despite early indications of problems, the devices remained on the market, representing failures in both non-maleficence (continuing to expose patients to known risks) and autonomy (withholding information about device performance that would have influenced patient and surgeon decisions). The case illustrates the ethical imperative for transparent reporting of device performance and prompt response to safety concerns.
Theranos Blood Testing Technology: This case involved deceptive claims about the capabilities of blood testing technology, representing fundamental violations of autonomy (through deception that undermined meaningful consent) and justice (by potentially exacerbating health disparities through inaccurate results) [10]. The case highlights the ethical responsibility of biomedical engineers to maintain integrity in technology development, avoid exaggeration of capabilities, and ensure transparent validation of performance claims.
Emerging Challenges and Evolving Applications
Artificial Intelligence and Machine Learning
The rapid integration of artificial intelligence (AI) and machine learning into biomedical engineering presents novel ethical challenges that require both application and potential adaptation of the four principles framework. The "black box" nature of some AI systems creates tension with autonomy, as limited explainability may undermine meaningful informed consent and patient understanding [15]. Similarly, AI systems trained on biased datasets may perpetuate or amplify healthcare disparities, creating justice concerns that must be addressed through careful attention to data sourcing and algorithm design [15].
The principle of non-maleficence takes on new dimensions in AI-enabled medical devices, where harms may emerge from unexpected system behaviors, adversarial attacks, or distributional shifts in input data. Beneficence requires that AI systems demonstrably improve upon existing approaches rather than simply automating suboptimal processes. The European High Level Expert Group on AI and other regulatory bodies have responded to these challenges by proposing frameworks that build upon the traditional principles while adding new dimensions such as explicability, reflecting the unique characteristics of AI systems [15].
Global Health and Resource Constraints
Biomedical engineering in global health contexts intensifies concerns about justice, as resource constraints may limit access to medical technologies that are routinely available in high-income settings. This challenge has prompted growing interest in "frugal innovation" approaches that prioritize affordability and accessibility without compromising safety and efficacy [5]. Such approaches represent practical applications of justice, ensuring that biomedical engineering serves diverse populations rather than exclusively focusing on high-resource settings.
The consideration of environmental sustainability in biomedical engineering, as reflected in the "Biomedical Engineer's Pledge" [10], represents an extension of justice concerns to intergenerational equity. Sustainable design practices, responsible end-of-life management for medical devices, and consideration of environmental impacts throughout the product lifecycle all reflect the expanding scope of ethical responsibility for biomedical engineers working within a principles framework.
Research Ethics and Integrity
The principles framework continues to guide the evolution of research ethics in biomedical engineering, particularly as new research methodologies emerge. The increasing use of human biospecimens and associated data raises complex questions about autonomy and informed consent, especially regarding future uses of samples and information [12]. Similarly, justice considerations inform debates about appropriate compensation for research participation and fair distribution of research benefits across communities.
Dual-use dilemmas, where biomedical research with therapeutic intent could potentially be misused for harmful purposes, present challenges that engage all four principles [5]. Addressing these concerns requires careful balancing of the potential benefits of research (beneficence) against potential harms from misuse (non-maleficence), while respecting researcher autonomy and ensuring equitable access to beneficial technologies (justice). These considerations have led to the development of specific oversight mechanisms for research with dual-use potential, representing an institutionalized application of the principles framework.
Table 3: Essential Ethical Assessment Tools for Biomedical Engineering Research
| Assessment Tool | Primary Function | Application Context | Key Output |
|---|---|---|---|
| Risk-Benefit Matrix | Systematic evaluation of potential harms and benefits | Research protocol development, device design | Prioritized risks, mitigation strategies |
| Informed Consent Checklist | Ensure comprehensive disclosure and understanding | Human subjects research, clinical trials | Documentation of consent process |
| Equity Impact Assessment | Evaluate distributional effects across populations | Technology implementation, study recruitment | Identification of potential disparities |
| Dual-Use Research Review | Assess potential for malicious application | Research with security concerns | Determination of oversight needs |
| Data Privacy Impact Assessment | Evaluate privacy risks in data handling | Studies involving personal health information | Data protection protocols |
The principle-based framework of beneficence, non-maleficence, autonomy, and justice provides an indispensable foundation for ethical practice in biomedical engineering. These principles inform professional codes, institutional policies, research protocols, and design decisions, creating a comprehensive approach to addressing the complex ethical challenges inherent in developing technologies that directly impact human health and well-being. As biomedical engineering continues to evolve with advancements in AI, global health, and novel therapeutic approaches, these principles offer enduring guidance while requiring thoughtful application to new contexts and technologies.
The ongoing institutionalization of these principles through mechanisms such as the "Biomedical Engineer's Pledge" represents significant progress in professional identity formation, creating explicit ethical commitments that parallel medicine's Hippocratic tradition. For researchers, scientists, and drug development professionals, this principles framework provides a shared language for identifying, analyzing, and resolving ethical dilemmas, ultimately supporting the development of biomedical innovations that responsibly serve human health needs while respecting fundamental moral values.
Biomedical engineering operates at the critical intersection of technology and human health, where professional decisions directly impact patient safety, public health, and societal well-being. This unique position necessitates a robust ethical framework to guide practitioners in their complex responsibilities. Ethical codes within biomedical engineering serve as foundational documents that enshrine the profession's commitment to public welfare, establishing clear expectations for safety, social responsibility, and professional conduct. These codes transform abstract moral principles into actionable standards, ensuring that technological innovation progresses in tandem with ethical considerations [5].
The development of ethical guidelines for biomedical engineering represents the profession's recognition of its profound responsibility toward patients, research participants, and society at large. Unlike many engineering disciplines, biomedical engineering directly addresses human health, making its ethical obligations particularly stringent. Professional societies including the Biomedical Engineering Society (BMES), the Engineering in Medicine and Biology Society (EMBS), and the Association for the Advancement of Medical Instrumentation (AdvaMed) have established comprehensive codes of ethics that outline the normative principles and obligations required to fulfill a biomedical engineer's commitment to honesty, conscientiousness in scientific inquiry, and advancement of public health [6] [5].
Core Ethical Principles in Biomedical Engineering
Fundamental Ethical Frameworks
Biomedical engineering ethics draws upon established bioethical principles while incorporating discipline-specific considerations relevant to technology development and implementation. The most prevalent ethical frameworks applied in biomedical engineering include:
Principle-Based Ethics: This approach utilizes the four fundamental principles of biomedical ethics: beneficence (doing good), non-maleficence (avoiding harm), respect for autonomy (honoring patient self-determination), and justice (ensuring fairness and equity) [3]. These principles provide a systematic framework for analyzing ethical dilemmas in biomedical engineering practice and research.
Virtue Ethics: This framework focuses on cultivating moral character and virtues such as integrity, compassion, courage, and honesty among biomedical engineers, providing guidance for ethical decision-making in complex situations where rules may be insufficient [3].
Duty-Based Ethics (Deontology): Emphasizes adherence to moral rules and duties, helping biomedical engineers navigate situations where they must balance competing obligations and responsibilities, such as between patient confidentiality and public safety concerns [3].
Consequence-Based Ethics (Utilitarianism): Focuses on maximizing overall utility or well-being, which can be applied to biomedical engineering dilemmas to determine the course of action that produces the greatest good for the greatest number of people, particularly in resource allocation or public health policy contexts [3].
Specific Ethical Principles for Biomedical Engineering Practice
Beyond these established frameworks, biomedical engineering ethics incorporates specific principles directly relevant to professional practice:
Table 1: Core Ethical Principles in Biomedical Engineering
| Ethical Principle | Professional Application | Public Health Impact |
|---|---|---|
| Safety Primacy | Rigorous testing and validation of medical devices; risk-benefit analysis; quality control in manufacturing | Prevents patient harm; ensures device reliability; reduces adverse health events |
| Respect for Autonomy | Informed consent processes; clear communication of risks/benefits; patient education materials | Empowers patients in healthcare decisions; respects individual values and preferences |
| Justice and Equity | Designing accessible technologies; addressing healthcare disparities; fair resource allocation | Promotes equitable healthcare access; reduces health disparities among populations |
| Confidentiality | Data encryption; secure storage; strict access controls; HIPAA compliance | Protects patient privacy; prevents misuse of sensitive health information |
| Professional Competence | Continuing education; staying current with research; appropriate training and certification | Ensures high-quality care; reduces errors from outdated knowledge or skills |
| Honesty and Integrity | Accurate reporting of research findings; disclosure of conflicts of interest; transparency about limitations | Builds public trust; enables informed decision-making by clinicians and patients |
| Environmental Responsibility | Sustainable design practices; proper disposal of medical devices; reducing carbon footprint | Minimizes ecological harm; promotes long-term planetary health |
These principles collectively establish a comprehensive ethical foundation that guides biomedical engineers in fulfilling their primary obligation: to hold paramount the safety, health, and welfare of the public in the performance of their professional duties [16] [3].
Codification of Ethics: From Principles to Practice
Professional Society Codes of Ethics
Professional societies have translated fundamental ethical principles into formal codes of conduct that establish normative standards for biomedical engineering practice. These codes provide specific guidance on ethical obligations and professional behavior:
Biomedical Engineering Society (BMES) Code of Ethics: BMES establishes clear expectations for professional conduct, emphasizing that biomedical engineers must "hold paramount the safety, health, and welfare of the public, including patients, research participants, coworkers, healthcare workers, and the public." The code explicitly prohibits harassment and discrimination while requiring reporting of ethical violations [17].
Engineering in Medicine and Biology Society (EMBS) Code of Ethics: EMBS provides guidelines specifically addressing research ethics, including requirements to "respect human dignity and privacy of patients and human subjects," "ensure proper safeguarding of all confidential information," and "conduct clinical research studies in accordance with Good Laboratory Practices (GLP) and Good Clinical Practices (GCP)." The code also emphasizes environmental responsibility and interdisciplinary collaboration [6].
AdvaMed Code of Ethics: Focusing on medical technology companies, the AdvaMed Code provides guidance on ethical interactions with healthcare professionals, based on the values of "innovation, education, integrity, respect, responsibility, and transparency." The recently updated code specifically addresses data ethics in digital health technologies, emphasizing responsible data handling to protect patient privacy while delivering beneficial technologies [18].
The Biomedical Engineer's Pledge: A Symbolic Commitment
A significant development in biomedical engineering ethics is the creation of the "Biomedical Engineer's Pledge," which serves as a symbolic commitment for graduating students and professionals. Modeled after the Hippocratic Oath but adapted to the unique ethical landscape of biomedical engineering, the pledge comprises ten specific promises [10]:
- Holding paramount the safety, health, and well-being of patients, research participants, coworkers, healthcare workers, and the public
- Exercising the profession with integrity and responsibility
- Ensuring the autonomy and dignity of patients and research participants
- Safeguarding patient and research participant data
- Non-discrimination based on age, gender, race, religion, or other identity factors
- Avoiding patient deception or fraud
- Sharing knowledge without violating human rights
- Promoting replacement, reduction, and refinement of animal research
- Contributing to environmental and economic sustainability of healthcare
- Demonstrating respect and gratitude to teachers, colleagues, and society
The pledge explicitly introduces ethical aspects not fully addressed in some existing codes, including avoidance of patient deception, minimization of animal experimentation, and promotion of universal healthcare coverage [10].
Implementation Framework: Integrating Ethics into Practice
Ethical Integration in Research and Development
The translation of ethical principles into daily practice requires systematic approaches throughout the research, development, and implementation lifecycle of biomedical technologies. The following workflow illustrates how ethical considerations integrate into each stage of biomedical engineering practice:
This systematic integration of ethics throughout the technology development lifecycle ensures that biomedical innovations prioritize public health and social responsibility at every stage.
Educational Integration and Accreditation Standards
The integration of ethics into biomedical engineering education represents a critical implementation pathway for ensuring future professionals internalize these principles. ABET accreditation criteria specifically require that engineering programs demonstrate their graduates have "an ability to recognize ethical and professional responsibilities in engineering situations and make informed judgments, which must consider the impact of engineering solutions in global, economic, environmental, and societal contexts" [19].
Effective educational approaches for ethics integration include:
Dedicated Ethics Courses: Covering fundamental principles of justice, beneficence, nonmaleficence, objectivity, autonomy, integrity, loyalty, veracity, and accountability through case studies and guided debate [20] [10].
Project-Based Learning: Incorporating ethical analysis into design projects, requiring students to conduct risk-benefit assessments, examine environmental impacts, and address ethical, legal, and social aspects of their projects [20].
Safe Medical Device Design Training: Teaching risk classification, application of relevant standards, and risk minimization techniques through hands-on activities in project-based courses [20].
Sustainability Integration: Requiring life cycle analyses and environmental impact reporting alongside technical and business considerations in student projects [20].
The "Biomedical Engineer's Pledge" has been implemented as a graduation tradition at several universities, serving as a symbolic rite of passage that reinforces ethical commitment at the start of professional careers [10].
Essential Methodologies for Ethical Biomedical Engineering
Risk Assessment and Safety Protocol Implementation
Ensuring patient safety requires systematic methodologies for risk assessment and implementation of safety protocols throughout the device lifecycle:
Table 2: Essential Research Reagent Solutions for Ethical Biomedical Engineering
| Research Component | Function in Ethical Practice | Implementation Methodology |
|---|---|---|
| Institutional Review Board (IRB) Protocols | Protect human research participants; ensure ethical study design | Submit detailed research proposals; document informed consent processes; report adverse events |
| Good Laboratory Practice (GLP) Guidelines | Ensure quality and integrity of preclinical research data | Implement quality control systems; document all procedures; validate equipment and methods |
| Good Clinical Practice (GCP) Guidelines | Ensure ethical conduct of clinical trials; protect participant rights and data | Train research staff; establish monitoring procedures; maintain comprehensive documentation |
| Failure Mode and Effects Analysis (FMEA) | Proactively identify potential device failures and harms | Systematic analysis of components and processes; risk priority number calculation; mitigation planning |
| Post-Market Surveillance Systems | Monitor device performance after commercialization; identify safety issues | Establish reporting mechanisms; track real-world performance; implement corrective actions when needed |
| Data Encryption and Security Protocols | Protect patient privacy and confidential health information | Implement access controls; secure data transmission; regular security audits |
These methodologies provide the practical framework for implementing ethical principles, particularly the foundational commitment to patient safety and well-being [6] [5] [3].
Ethical Dilemma Resolution Framework
Biomedical engineers frequently encounter ethical dilemmas requiring structured resolution approaches. The following framework provides a systematic methodology for addressing such situations:
This structured approach ensures that ethical decisions are made systematically rather than arbitrarily, incorporating relevant facts, principles, and stakeholder perspectives while aligning with established ethical codes [5] [3].
Case Studies in Ethical Success and Failure
Historical Case Analyses
Real-world cases provide powerful illustrations of the practical importance of ethical codes in biomedical engineering:
Therac-25 Radiation Therapy Machine (1980s): This case involved a software-controlled radiation therapy machine that malfunctioned, delivering lethal radiation doses to patients. The ethical failures included inadequate safety design, insufficient testing, lack of proper risk assessment, and failure to respond appropriately to early reports of problems. This case demonstrates the critical importance of rigorous safety protocols, comprehensive testing, and responsive reporting systems—all emphasized in modern ethical codes [5].
Bjork-Shiley Heart Valve (1970s-1980s): This prosthetic heart valve exhibited design flaws that led to strut fractures and patient deaths. Despite early indications of problems and reports of malfunctions, the valves remained on the market for years, resulting in hundreds of failures and fatalities. The case highlights the ethical imperative of responding promptly to safety concerns and prioritizing patient welfare over commercial interests [5].
Theranos (2010s): This company made misleading claims about its blood testing technology, committing widespread fraud that endangered patients who received inaccurate test results. The case illustrates violations of multiple ethical principles, including honesty, integrity, patient safety, and transparency [10].
Positive Implementation Cases
UBORA E-Infrastructure: This platform supports the cocreation of open-source medical devices, addressing ethical imperatives of technological equity and universal healthcare. By enabling collaborative development of safe, effective, and accessible medical technologies, this initiative embodies ethical principles of justice, equity, and global health responsibility [20].
Sustainable Medical Device Initiatives: Various projects have focused on developing environmentally sustainable medical technologies, addressing the ethical principle of environmental responsibility. These include devices designed for reduced resource consumption, improved recyclability, and lower carbon footprints throughout their lifecycle [20] [10].
As biomedical engineering continues to evolve with advancements in artificial intelligence, neurotechnology, synthetic biology, and personalized medicine, ethical codes must similarly progress to address emerging challenges. The ongoing revision of codes by professional societies such as AdvaMed, which recently updated its Code of Ethics to specifically address data-driven technologies, demonstrates this dynamic nature of ethical guidance in the field [18].
The fundamental commitment of biomedical engineering to public health, safety, and social responsibility remains constant, even as its technological capabilities transform. By establishing clear ethical principles, implementing them through systematic methodologies, and cultivating professional cultures that prioritize ethical practice, biomedical engineering can continue to develop innovative technologies that serve humanity while maintaining the public trust that forms the foundation of the profession.
The field of biomedical engineering operates at the critical intersection of technology, healthcare, and human welfare, making ethical practice not merely an adjunct but a foundational component of the profession. The principle of respect for persons forms a cornerstone of this ethical framework, encompassing the protection of patient autonomy, privacy, and the right to self-determination [6]. This principle manifests operationally through stringent adherence to protocols surrounding patient privacy, data confidentiality, and informed consent—each serving as a vital mechanism for upholding human dignity in healthcare and research settings [6]. As technology evolves to include more wearable devices, complex data analytics, and interconnected health systems, the responsibilities of biomedical engineers in implementing these safeguards have become both more complex and more critical.
The Biomedical Engineering Society (BMES) and other professional organizations codify these obligations, emphasizing that professionals must "respect human dignity and privacy of patients and human subjects" and "ensure proper safeguarding of all confidential information" [6] [5]. These guidelines are not abstract ideals but practical requirements that directly impact patient safety, trust in medical institutions, and the integrity of scientific research. For researchers, scientists, and drug development professionals, navigating this landscape requires a sophisticated understanding of both technical requirements and ethical imperatives, as failures can result in profound harm to individuals and populations, particularly vulnerable groups [21]. This guide provides a comprehensive framework for integrating these essential principles into daily practice and research methodologies.
Patient Privacy and Data Confidentiality
Legal and Regulatory Frameworks
The Health Insurance Portability and Accountability Act (HIPAA) establishes the primary federal standard for protecting patient health information in the United States [22]. HIPAA consists of two main rules: the Privacy Rule, which governs the use and disclosure of Protected Health Information (PHI), and the Security Rule, which sets national standards for protecting the confidentiality, integrity, and availability of electronic PHI (ePHI) [22]. PHI encompasses any individually identifiable health information transmitted or maintained in any form or medium, including electronic, paper, or oral communication [22]. The scope of these regulations extends beyond traditional healthcare settings to include biomedical engineers involved in device design, data system development, and clinical research.
HIPAA's definition of PHI includes 18 specific identifiers that constitute protected information, ranging from names and geographic subdivisions to device identifiers and serial numbers [22] [21]. The law applies to covered entities (healthcare providers, health plans, healthcare clearinghouses) and their business associates, which includes many biomedical engineering contexts where patient data is accessed, processed, or stored [22]. Importantly, many states have implemented more stringent privacy laws, particularly regarding sensitive health information related to HIV status, mental health, genetic testing, and substance abuse treatment—in such cases, the more restrictive rule takes precedence [22].
Table 1: Key Elements of Protected Health Information (PHI) Under HIPAA
| Category | Specific Identifiers | Protection Requirements |
|---|---|---|
| Direct Identifiers | Names, geographic subdivisions smaller than a state, all elements of dates (except year) directly related to an individual, telephone numbers, vehicle identifiers | Must be removed for de-identified data sets; requires strict access controls in identified form |
| Digital Identifiers | Email addresses, IP addresses, URLs, device identifiers and serial numbers | Must be encrypted during transmission and storage; secure authentication required for access |
| Biometric Identifiers | Fingerprints, voiceprints, full face photographic images | Considered highly sensitive; requires enhanced protection and specific authorization for use |
| Administrative Identifiers | Medical record numbers, health plan beneficiary numbers, account numbers, certificate/license numbers | Must be protected in all forms; requires audit trails for access and disclosure |
Practical Implementation in Biomedical Engineering
Biomedical engineers implement data privacy through both technical safeguards and organizational policies. Technical safeguards include encryption of data both in transit and at rest, implementation of secure authentication protocols, and regular security audits [5]. Particularly vulnerable areas include wireless networks used to access medical records, which must have encryption functions activated to prevent interception, and portable storage devices like laptops and flash drives, which should either avoid storing PHI entirely or employ robust encryption methods when storage is necessary [22].
Organizational policies must address access controls, workforce training, and breach notification procedures. The HIPAA security rule emphasizes risk analysis, requiring healthcare institutions and their partners to "identify and address the appropriate security options to ensure data security" [22]. This includes developing protection against reasonably anticipated threats to data integrity and confidentiality, ensuring compliance among workforce members, and implementing unique user identification systems that go beyond basic password protection [22]. Biomedical engineers developing medical devices or health information systems must incorporate privacy-by-design principles, building in security features during the development phase rather than adding them as an afterthought.
The emergence of artificial intelligence and machine learning in healthcare introduces novel privacy challenges, as these systems often require large datasets for training and validation [21]. Biomedical engineers must ensure that data used for algorithm development does not compromise patient privacy through re-identification risks, even in supposedly de-identified datasets. This requires sophisticated techniques such as differential privacy and federated learning, which allow model development without centralizing sensitive patient data [21].
Figure 1: The Protected Health Information (PHI) Lifecycle. All phases require specific security measures with destruction occurring only after meeting legal retention requirements [21].
Informed Consent in Research and Clinical Applications
Theoretical Foundations and Ethical Imperatives
Informed consent represents a fundamental ethical and legal requirement in both clinical practice and research contexts, serving as the practical embodiment of respect for personal autonomy [23]. Historically rooted in responses to ethical abuses such as the Tuskegee Study and Nazi medical experiments, informed consent has evolved from a simple signature on a document to a comprehensive communication process between healthcare providers/researchers and patients/subjects [23]. This process ensures that individuals maintain the ultimate authority over what happens to their bodies and personal health information, particularly in research environments where biomedical engineers may be developing novel devices or therapeutic approaches.
The functional purpose of informed consent extends beyond mere legal protection for institutions and researchers; it represents the intersection of values including autonomy, non-domination, self-ownership, and personal integrity [23]. For consent to be truly "informed," it must encompass several key elements: the nature of the procedure or research intervention, the potential risks and benefits, reasonable alternatives, and the risks and benefits of those alternatives [23]. Additionally, researchers must assess the patient's or subject's understanding of these elements, ensuring comprehension rather than merely providing information. This is particularly crucial in biomedical engineering contexts where complex technologies may be difficult for laypersons to understand.
Methodological Implementation and Documentation
The implementation of valid informed consent requires structured methodologies that address common barriers to understanding. The Joint Commission requires documentation of all consent elements, which typically includes: the nature of the procedure or intervention, risks and benefits, reasonable alternatives, risks and benefits of alternatives, and assessment of patient understanding [23]. Biomedical engineers involved in clinical trials or device testing must ensure that consent processes adequately convey technical information in accessible language, using appropriate educational materials and verification techniques.
Effective methodologies for obtaining informed consent include:
- The Teach-Back Method: Asking patients to explain in their own words what they have understood about the procedure, risks, and alternatives, which allows for correction of misunderstandings [23].
- Utilization of Graphical Tools and Interactive Media: Visual representations of complex procedures or statistical risks can significantly improve comprehension compared to purely verbal or written descriptions [23].
- Cultural and Linguistic Adaptation: Working with medical interpreters for non-native speakers and adapting materials to account for cultural health beliefs and decision-making patterns [23].
- Structured Decision-Making Tools: Using evidence-based templates that standardize the presentation of risk/benefit information while allowing personalization to individual clinical circumstances.
Table 2: Standards for Adequate Informed Consent in Research Settings
| Legal Standard | Definition | Application Context |
|---|---|---|
| Subjective Standard | What this specific patient needs to know and understand to make an informed decision | Ideal for personalized medicine approaches; requires individualized assessment of patient values and comprehension |
| Reasonable Patient Standard | What the average patient would need to know to be an informed participant in the decision | Most common standard in clinical practice; balances efficiency with respect for autonomy |
| Reasonable Clinician Standard | What a typical clinician would disclose about a procedure or intervention | Traditional approach that defers to professional norms; increasingly supplemented by patient-centered standards |
Documentation of informed consent must extend beyond a signed form to include notes in progress records or research files that reflect the discussion process, specific questions asked by the patient or subject, and the responses provided [23]. This documentation becomes particularly important in biomedical engineering research where innovative devices or therapies may have uncertain risk profiles or novel mechanisms of action. Research indicates that the four required elements of informed consent—nature of the procedure, risks, benefits, and alternatives—are documented on consent forms only 26.4% of the time, highlighting a significant area for improvement in both clinical and research settings [23].
Experimental Protocols and Research Methodologies
Protocol for Ethical Implementation of Human Subject Research
Biomedical engineering research involving human subjects requires rigorous protocols to ensure ethical conduct. The following methodology outlines key steps for maintaining patient privacy, confidentiality, and valid informed consent:
Pre-Study Institutional Review Board (IRB) Approval: Submit detailed research protocol to the IRB or independent ethics committee, including data collection methods, informed consent documentation, privacy safeguards, and procedures for vulnerable populations [5]. The IRB functions include approving research, providing ethical oversight, conducting periodic reviews, requiring modifications to procedures, and ensuring compliance with state and federal guidelines [5].
Participant Recruitment and Screening: Implement targeted recruitment strategies that avoid coercion or undue influence. Screen potential participants for factors that may affect their ability to provide informed consent, such as language barriers, cognitive impairments, or emotional distress [23]. For participants with limited English proficiency, utilize qualified medical interpreters rather than family members.
Comprehensive Informed Consent Process: Conduct the consent discussion in a private setting with adequate time for questions and reflection [23]. Present information using clear, non-technical language appropriate to the participant's health literacy level. Utilize the teach-back method to verify comprehension: "To make sure I've explained everything clearly, could you please tell me in your own words what you understand about this study?" [23].
Data Collection and Management: Implement data encryption for all electronic protected health information (ePHI) during transmission and storage [22]. Utilize secure data capture platforms such as Research Electronic Data Capture (REDCap), which complies with HIPAA standards and supports single- and multiple-site research studies while allowing data to be stored at local institutions [21]. De-identify data whenever possible during export and analysis.
Ongoing Monitoring and Adverse Event Reporting: Establish clear protocols for monitoring participant safety throughout the study period. Report adverse events to the IRB according to established timelines. For long-term studies, implement periodic re-consent processes if new risks emerge or procedures change significantly.
Table 3: Research Reagent Solutions for Ethical Biomedical Engineering Research
| Tool/Resource | Function | Ethical Application |
|---|---|---|
| REDCap (Research Electronic Data Capture) | Secure web application for building and managing online surveys and databases | Enables HIPAA-compliant data collection; supports single- and multi-site research while maintaining institutional control of data [21] |
| HIPAA-Limited Data Sets | Data sets with certain direct identifiers removed but containing potentially identifiable information | Allows sharing of data for research without individual authorization under specific circumstances; requires data use agreements [21] |
| Institutional Review Board (IRB) | Independent ethics committee that reviews research involving human subjects | Provides ethical oversight and approval; ensures participant rights and welfare are protected throughout research process [5] |
| Health Literacy Assessment Tools | Validated instruments to assess participant understanding of research information | Identifies comprehension gaps; allows researchers to tailor consent discussions to individual needs [23] |
| Data Encryption Software | Programs that encode data to prevent unauthorized access | Protects confidentiality during data transmission and storage; essential for mobile devices and portable storage media [22] |
Figure 2: Informed Consent Protocol Workflow. The process emphasizes comprehension verification through methods like teach-back before proceeding to research implementation [23].
Case Studies and Ethical Analysis
Historical Failures and Their Impact on Current Standards
Analysis of historical cases provides valuable lessons for contemporary biomedical engineering practice. The Therac-25 radiation therapy machine incidents represent a pivotal case where lapses in safety design and risk assessment led to patient fatalities [5]. This case demonstrates how engineering decisions directly impact patient safety and why rigorous testing, transparency in reporting potential risks, and ongoing monitoring are ethical imperatives, not just technical considerations. The failures included insufficient safety redundancies, poor error reporting systems, and inadequate investigation of early incident reports—all of which contributed to catastrophic outcomes.
The Bjork-Shiley heart valve case further illustrates the consequences of prioritizing commercial interests over patient safety [5]. Despite early indications of anomalies and reports of malfunctions, the valves remained on the market for years, resulting in over 600 valve failures and fatal outcomes. This case highlights the ethical responsibility of biomedical engineers to advocate for patient safety even when facing commercial or institutional pressure, and to ensure transparent reporting of potential device risks throughout the product lifecycle.
Contemporary Challenges in Data Privacy
Modern biomedical engineering faces novel ethical challenges regarding patient data ownership and privacy. The increasing interest of for-profit companies in acquiring databases from large healthcare systems creates new vulnerabilities for patient privacy [21]. Such arrangements raise ethical concerns about sharing patient data with entities that may exploit it for commercial interests or target vulnerable populations. Of particular concern is the use of data voluntarily provided by patients for research purposes being redirected toward commercial applications without explicit consent for these secondary uses [21].
Biomedical engineers developing health information systems, wearable devices, or data analytics platforms must implement privacy-by-design principles that anticipate these potential misuses. This includes building in data governance structures that give patients control over how their information is used, implementing robust de-identification techniques that withstand re-identification attempts, and establishing transparent policies regarding data sharing with third parties [21]. The ethical obligation extends beyond legal compliance to ensuring that data systems respect the spirit of patient trust and the context in which data was originally provided.
The principles of patient privacy, data confidentiality, and informed consent represent more than regulatory requirements—they form the ethical bedrock of trustworthy biomedical engineering practice. As technology continues to evolve with artificial intelligence, wearable sensors, and complex data analytics, these principles must remain central to both research and clinical applications. Biomedical engineers have a professional responsibility to implement systems that not only advance healthcare but also protect the fundamental rights and dignity of patients and research subjects.
Future challenges will include developing ethical frameworks for emerging technologies such as organ bioengineering, complex tissue creation, and neural interfaces, all of which present novel questions about patient safety, privacy, and consent [5]. Additionally, the growing emphasis on diversity, equity, and inclusion in research requires biomedical engineers to develop consent processes and data protection measures that are culturally competent and accessible to diverse populations [23] [5]. By maintaining a commitment to the principle of respect for persons through robust privacy protections and meaningful informed consent processes, the biomedical engineering community can continue to advance human health while upholding its fundamental ethical obligations.
Research integrity forms the ethical foundation of scientific advancement, particularly in biomedical engineering where research directly impacts healthcare and human well-being. Upholding the highest standards of rigor, honesty, and transparency is not merely aspirational but essential for maintaining public trust and ensuring the reliability of scientific evidence. As articulated by leading scientific organizations, research integrity encompasses core elements of honesty, rigour, transparency, open communication, care and respect, and accountability [24]. Within the context of biomedical engineering, this ethical framework governs both the reporting of scientific findings and the humane conduct of animal experimentation, ensuring that research advances knowledge while maintaining ethical responsibilities toward all subjects involved in the research process.
Professional societies like the Biomedical Engineering Society (BMES) and IEEE Engineering in Medicine and Biology Society (EMBS) establish codes of ethics that provide essential guidelines for ethical conduct. These codes emphasize respect for human dignity, privacy, proper safeguarding of confidential information, and responsible reporting of research results [6]. Furthermore, they stress the importance of observing the rights of human research subjects and ensuring responsible and humane use of animals in research [6]. This whitepaper provides a comprehensive technical guide to implementing these ethical principles through robust scientific reporting standards and humane animal experimentation protocols, specifically tailored for researchers, scientists, and drug development professionals in the biomedical field.
Fundamental Principles of Research Integrity
Research integrity encompasses a comprehensive framework of principles and responsibilities that guide ethical scientific practice. The Concordat to Support Research Integrity, endorsed by major research institutions, outlines five fundamental principles that all researchers should uphold: (1) maintaining the highest standards of rigour and integrity in all research aspects; (2) ensuring research is conducted according to appropriate ethical, legal and professional frameworks; (3) supporting a research environment underpinned by a culture of integrity; (4) using transparent, timely, and fair processes for addressing misconduct allegations; and (5) working collaboratively to strengthen research integrity [24].
Both individual researchers and their host institutions share responsibility for maintaining these standards. Individuals must role-model a positive culture where colleagues can freely discuss good research practice, ask questions, raise concerns, or admit errors without fear of reprisal [24]. Institutions must provide comprehensive policies and procedures to promote good research practice, including codes of good practice, misconduct investigation procedures, and whistleblowing protections [24]. They must also appoint designated Research Integrity Officers responsible for coordinating training, handling integrity-related queries, and ensuring adherence to data archiving policies [24].
Research misconduct includes fabrication, falsification, plagiarism, or deception in performing, reviewing, or reporting research [24]. This encompasses manipulating images, omitting relevant data, or deliberately misusing data [24]. Importantly, research misconduct does not include honest differences in research design, execution, or interpretation, nor does it include research of poor quality unless there is intention to deceive [24].
Standards for Rigorous Scientific Reporting
Quantitative Data Quality Assurance and Analysis
Robust scientific reporting begins with rigorous data quality assurance. Quantitative data quality assurance represents the systematic processes and procedures used to ensure the accuracy, consistency, reliability, and integrity of data throughout the research process [25]. Effective quality assurance helps identify and correct errors, reduce biases, and ensure data meets necessary standards for analysis and reporting [25].
The data management process follows a rigorous step-by-step approach, with each stage requiring researchers to interact with the dataset iteratively to extract relevant information in a transparent manner [25]. Key stages in data preparation include:
Data Cleaning: Checking for and removing duplicate entries, especially in online surveys where respondents may complete questionnaires multiple times [25].
Handling Missing Data: Establishing thresholds for inclusion/exclusion of incomplete questionnaires and analyzing patterns of missingness using statistical tests like Little's Missing Completely at Random (MCAR) test [25].
Anomaly Detection: Running descriptive statistics to identify responses that deviate from expected patterns, such as values outside Likert scale boundaries [25].
Data Summation: Following instrument manuals to properly summate constructs or apply clinical definitions to screening tools [25].
Data analysis typically proceeds in waves, allowing researchers to build upon a rigorous protocol [25]. The process involves:
- Descriptive Analysis: Summarizing the dataset using frequencies, means, medians, and modes to explore trends and patterns [25].
- Assessing Normality: Testing whether data stems from a normal distribution population using measures like kurtosis, skewness, Kolmogorov-Smirnov, or Shapiro-Wilk tests [25].
- Establishing Psychometric Properties: Reporting reliability and validity measures, with Cronbach's alpha scores >0.7 considered acceptable for internal consistency [25].
- Inferential Analysis: Employing appropriate statistical tests based on study design, measurement type, and normality distribution to compare, analyze relationships, or make predictions [25].
Table 1: Key Steps in Quantitative Data Quality Assurance
| Stage | Key Procedures | Purpose |
|---|---|---|
| Data Collection | Implementing standardized instruments; ensuring proper sampling | To gather reliable and representative data [25] |
| Data Cleaning | Removing duplicates; identifying anomalies; checking range limits | To reduce errors and enhance data quality [25] |
| Missing Data Handling | Establishing completion thresholds; running MCAR tests; using imputation methods | To manage incomplete responses and assess potential bias [25] |
| Data Analysis | Running descriptive statistics; testing normality; establishing psychometrics | To prepare data for inferential analysis and interpretation [25] |
Comprehensive Research Reporting Components
A comprehensive quantitative research report must include specific components to ensure transparency and reproducibility. These components provide readers with sufficient detail to evaluate the research methodology and findings [26]:
Title Page: Contains essential information about the research, including title, author(s), institutional affiliation, and contact details [26].
Abstract: Provides a concise summary of the research question, methodology, key findings, and implications [26].
Introduction: Sets the context for the research, outlines the problem or research question, provides a rationale for the study, and includes a review of relevant literature [26].
Methodology: Details the research methods and techniques used, including data collection procedures, sampling methods, and statistical analyses in sufficient detail to enable replication [26].
Results: Presents findings using tables, figures, and statistical analyses in a logically organized manner with minimal interpretation [26].
Discussion and Conclusion: Discusses implications of findings, their relevance to the research question, and how they fit into existing knowledge; summarizes key findings and suggests future research directions [26].
When interpreting and presenting data, researchers must avoid selective reporting by addressing all pre-established research objectives [25]. They should correct for multiplicity when running multiple comparisons to reduce chance associations, using methods like Bonferroni correction [25]. Additionally, researchers must report both statistically significant and non-significant findings to prevent other researchers from pursuing unproductive avenues [25].
Effective Data Visualization Principles
Effective data visualization is essential for communicating research findings clearly and accurately. When creating visual representations of data, several key principles should be followed:
Color Selection: Use intuitive colors that align with cultural associations and reader expectations (e.g., red for attention/stop, green for good) [27]. When encoding gender data, consider moving beyond the stereotypical pink-blue combination by using a cold color for men (e.g., blue) and a warmer color for women (e.g., yellow, orange) [27].
Accessibility Considerations: Ensure high contrast between foreground and background elements, with a contrast ratio of at least 4.5:1 for small text [27]. Use different lightness values in color gradients to ensure distinguishability for color-blind readers [27].
Appropriate Visual Encodings: For quantitative values, consider using position or length encodings (e.g., bar charts) rather than relying solely on color gradients, as readers can decipher values more accurately [27]. Limit categorical color palettes to seven or fewer distinct colors to avoid visual confusion [27].
Gradient Design: For sequential data, use light colors for low values and dark colors for high values [27]. Design gradients with consistent lightness progression, ideally using two carefully selected hues rather than one, to improve decipherability [27]. For diverging data that emphasizes deviation from a baseline, use clearly distinguishable hues for both sides of the gradient with a light grey center [27].
Table 2: Color Application Guidelines for Data Visualization
| Data Type | Recommended Color Scheme | Key Considerations |
|---|---|---|
| Categorical | Different hues (e.g., green, yellow, pink) | Avoid using shades of one hue, as this implies ranking; limit to 7 categories [27] |
| Sequential | Single hue gradient from light to dark | Use light colors for low values, dark colors for high values [27] |
| Diverging | Two contrasting hues with neutral midpoint | Use clearly distinguishable hues with light grey center to emphasize deviation [27] |
| Highlighting | Bold highlight colors with grey for context | Use grey for less important elements to make highlight colors stand out [27] |
Ethical Standards in Animal Experimentation
Foundational Ethical Principles
Humane animal experimentation in biomedical engineering research is guided by several foundational ethical principles rooted in the broader framework of research integrity. Professional codes of ethics, such as that of EMBS, explicitly emphasize the need to "ensure a responsible and humane use of animals in research" and to "observe the rights of human research subjects and strive for a balance between benefits and potential harm" [6]. These principles acknowledge the moral responsibility researchers have toward animal subjects while recognizing the essential role of animal studies in advancing biomedical knowledge and therapeutic development.
The core principles governing ethical animal research include:
Replacement: Prioritizing non-animal alternatives whenever scientifically valid methods exist, including computer models, cell cultures, or human volunteers where appropriate.
Reduction: Employing statistical methods and experimental designs that minimize the number of animals required to obtain scientifically valid results.
Refinement: Modifying procedures to minimize pain, distress, and suffering while enhancing animal welfare throughout the study.
Responsibility: Maintaining researcher accountability for animal welfare, including proper training, oversight, and adherence to protocols.
These principles must be integrated throughout the entire research process, from experimental design and approval to implementation and reporting.
Institutional Protocols and Oversight
Robust institutional protocols and oversight mechanisms are essential for ensuring humane animal experimentation. Research institutions must establish comprehensive animal care and use committees (IACUCs) that include veterinarians, scientists, and community representatives to review and approve all proposed animal research [6]. These committees evaluate:
- The scientific rationale and necessity of animal use
- The application of replacement, reduction, and refinement principles
- Procedures for minimizing pain and distress
- Qualifications of research personnel
- Appropriateness of housing and husbandry conditions
Host institutions must provide clear policies and procedures governing animal research, including detailed guidance on clinical governance, research involving animals, and research records [24]. These policies should be readily accessible to all researchers and staff, with regular training sessions to ensure ongoing compliance and awareness.
Additionally, institutions must maintain transparent procedures for reporting concerns about animal welfare, protecting whistleblowers from retaliation, and investigating allegations of misconduct [24]. The designated Research Integrity Officer should serve as a point of contact for animal welfare concerns and ensure that all researchers receive proper training in both technical procedures and ethical considerations [24].
Experimental Design and Reporting Standards
Comprehensive reporting of animal research methodologies is essential for research integrity, allowing for proper evaluation of findings and potentially reducing unnecessary duplication of studies. Detailed methodologies should include:
- Animal Characteristics: Species, strain, sex, weight, age, and genetic modifications
- Housing and Husbandry: Housing type, cage environment, group housing, environmental enrichment, food and water access, and light/dark cycles
- Experimental Procedures: Detailed description of interventions, measurements, and sampling procedures
- Pain Management: Analgesia, anesthesia, and endpoints for minimizing pain and distress
- Statistical Methods: Sample size justification, randomization methods, blinding procedures, and statistical analyses
Adherence to Good Laboratory Practices (GLP) and Good Clinical Practices (GCP) is essential for maintaining research integrity in animal studies [6]. Research should be conducted according to appropriate ethical, legal and professional frameworks, obligations and standards [24], with particular attention to balancing scientific objectives with animal welfare considerations.
Table 3: Essential Research Reagent Solutions for Animal Research
| Reagent Category | Specific Examples | Research Function |
|---|---|---|
| Anesthetics & Analgesics | Isoflurane, ketamine/xylazine, buprenorphine | To ensure humane procedures and minimize pain and distress during and after experimental procedures [6] |
| Physiological Monitoring | Telemetry systems, blood gas analyzers, physiological data acquisition systems | To monitor animal vital signs and physiological parameters without causing undue stress or interference [6] |
| Behavioral Assessment | Automated tracking systems, elevated plus maze, forced swim test apparatus | To quantitatively assess animal behavior, cognitive function, and potential distress using validated methodologies |
| Sample Collection & Analysis | Microsampling equipment, plasma separators, point-of-care analyzers | To reduce sample volumes and enable longitudinal studies while minimizing animal numbers through refined techniques [25] |
Upholding research integrity requires the seamless integration of rigorous scientific reporting standards and ethical animal experimentation practices. This comprehensive approach ensures that biomedical engineering research not only advances scientific knowledge but also maintains the highest ethical standards and societal trust. By adhering to principles of honesty, rigour, transparency, care and respect, and accountability [24], researchers contribute to a culture of integrity that supports scientific progress while fulfilling ethical responsibilities.
The implementation of robust quantitative data quality assurance processes [25], transparent reporting practices [26], effective data visualization techniques [27], and humane animal research protocols [6] represents a multifaceted approach to maintaining research integrity. Institutional support through clear policies, training programs, and oversight mechanisms is equally essential for fostering an environment where ethical conduct is prioritized and nurtured [24].
As biomedical engineering continues to evolve, maintaining these standards becomes increasingly important for addressing complex healthcare challenges. By embracing these comprehensive guidelines for scientific reporting and animal experimentation, researchers can ensure their work not only withstands scientific scrutiny but also aligns with the ethical expectations of the scientific community and society at large.
From Theory to Practice: Implementing Ethical Guidelines in Daily Research and Development
Within the field of biomedical engineering, operationalizing safety is a proactive and systematic discipline dedicated to ensuring that medical devices and therapeutic products are not only effective but also safe for patient use. This process extends beyond initial design, encompassing the entire product lifecycle from conception through post-market surveillance. It requires the implementation of rigorous testing protocols and structured analytical frameworks to evaluate a product's benefit-risk balance—the cornerstone of regulatory approval and clinical adoption. For researchers, scientists, and drug development professionals, this represents an ethical and practical necessity. A robust safety protocol ensures that the positive impact of a new innovation on a patient's health demonstrably outweighs any associated risks, aligning with the core ethical principles of the Biomedical Engineering Society (BMES) which emphasize the welfare of the public and the responsible conduct of research and practice [17] [28]. This guide provides a detailed technical roadmap for embedding these rigorous safety assessments into the fabric of product development.
Foundational Concepts in Risk-Benefit Analysis
Before implementing specific testing protocols, it is crucial to establish a common understanding of the key components that constitute a benefit-risk assessment. These elements form the basic vocabulary for all subsequent evaluation and decision-making.
- Benefit: A positive impact on patient health, which can include improved clinical outcomes, enhanced quality of life, better diagnostic accuracy, or positive impacts on public health [29]. Benefits are evaluated based on their type, magnitude, probability, and duration [29].
- Risk: The combination of the probability of occurrence of harm and the severity of that harm [30]. In the context of medical devices, risks can range from mild side effects to serious adverse events.
- Residual Risk: The remaining risk after all appropriate risk mitigation measures have been implemented [30]. A core principle of risk management is that it is not always feasible to eliminate all risks entirely due to resource limitations, uncertainty, and cost-benefit considerations [31].
- Benefit-Risk Ratio: A comparative measure, which can be expressed in qualitative or quantitative terms, that evaluates whether the benefits of a medical device or product justify the associated risks [30].
Regulatory frameworks such as the EU Medical Device Regulation (MDR) and international standards like ISO 14971 provide the mandatory structure for these assessments, requiring that a device's risks be acceptable when weighed against its benefits to patients and that risks be minimized as much as possible without adversely affecting the benefit-risk ratio [30] [29].
Operational Safety and Testing Protocols
A proactive approach to safety involves integrating structured assessments at defined milestones throughout the development lifecycle. This begins early in development and is periodically reviewed at critical junctures, such as investment decisions or before progressing to subsequent clinical trial phases [32].
Core Testing and Evaluation Workflows
The following diagram illustrates the integrated workflow for operational safety testing and benefit-risk analysis, highlighting the continuous and cyclical nature of the process.
This workflow is operationalized through several key methodologies:
- Qualitative Analysis: This approach relies on descriptive terms rather than numerical data to evaluate benefits and risks. It is often suitable for low-risk devices or those with indirect benefits, such as diagnostic tools that support clinical decision-making or devices that improve procedural efficiency [30]. The assessment focuses on parameters like end-user benefits, quality of life improvements, and the nature of minor risks (e.g., manageable usability challenges) [30].
- Quantitative Analysis: For high-risk devices, quantitative analysis employs statistical and numerical methods to provide a data-driven evaluation [30]. Key techniques include:
- Benefit-Risk Ratio: Comparing the frequency and severity of benefits versus risks.
- NNT vs. NMH: Calculating the Number Needed to Treat (NNT) to observe one benefit versus the Number Needed to Harm (NMH) to observe one adverse event.
- QALY (Quality-Adjusted Life Years): Quantifying both the quality and duration of life improvements a device offers [30].
- Operational Risk Scoring: In a health care facility context, this involves a systematic process of identifying potential risks, assessing their likelihood and severity, prioritizing them, developing mitigation strategies, and continuously monitoring and reassessing the environment [31]. This proactive mindset is analogous to maintaining a culture of safety in product development.
The Researcher's Toolkit: Essential Materials for Safety & Risk Assessment
The following table details key reagents, tools, and methodologies essential for conducting rigorous safety testing and benefit-risk analysis.
Table 1: Essential Research Tools for Safety and Risk Assessment
| Tool/Reagent | Function in Safety Testing & Risk Analysis |
|---|---|
| Structured Benefit-Risk (sBR) Framework | Guides the systematic assessment of benefits and risks across the drug development continuum, from first-in-human studies to regulatory submission [32]. |
| Risk Management File (RMF) | A central repository for identifying, assessing, and mitigating potential risks associated with a medical device, as required by ISO 14971 [29]. |
| Clinical Evaluation Report (CER) | Documents the comprehensive clinical data that supports the benefit-risk analysis, demonstrating device safety and performance [30]. |
| Post-Market Surveillance (PMS) Data | Real-world evidence collected after a product is launched, used to update the benefit-risk assessment and identify any rare or long-term risks [29]. |
| CAPTIS & Literature Databases | Automated tools that streamline literature reviews, integrate adverse event data, and provide alerts for document updates, ensuring assessments are based on current evidence [30]. |
Methodologies for Structured Benefit-Risk Analysis
A structured benefit-risk (sBR) assessment is fundamental to operationalizing safety. The AstraZeneca framework provides a clear, three-stage methodology for performing such an analysis [32]:
- Agree on Definitions and Facts: Identify and define a concise set of Key Clinical Benefits and Key Safety Risks. Best practice suggests limiting these to 2-3 of the most important benefits and 6-8 of the most critical risks to avoid overlap and ensure focus on the most impactful factors [32].
- Agree on Relative Importance and Uncertainty: This involves weighting the Key Clinical Benefits and Key Safety Risks to rank their medical importance. It also requires a rigorous assessment of any uncertainties, such as missing data or potential biases, that could affect the interpretation of the evidence [32].
- Produce a Concise and Clear Assessment: The output should be a standalone summary, typically 1-2 pages, that expresses the Core Company BR Position. This narrative allows any medical reviewer to quickly understand the company's position on the product's benefit-risk profile [32].
Defining Key Clinical Benefits and Key Safety Risks
- Key Clinical Benefits are typically consistent with the primary and secondary efficacy endpoints of pivotal clinical studies. The primary endpoint is often the most important benefit, but secondary endpoints can take precedence if they better represent how a patient "feels, functions, or survives" [32]. Non-endpoint variables, such as quality of life or adherence to a specific route of administration, can also be considered [32].
- Key Safety Risks are unfavorable effects with a significant potential impact on patients, product approvability, or clinical use. These are often characterized descriptively and require careful medical judgment to identify, as they can affect morbidity, mortality, hospitalizations, and compliance [32].
Quantitative Frameworks for Benefit-Risk Assessment
For a quantitative analysis, specific metrics provide objective evidence for decision-making. The table below summarizes key quantitative measures.
Table 2: Quantitative Measures for Benefit-Risk Analysis
| Metric | Description | Application in Device/Product Evaluation |
|---|---|---|
| Number Needed to Treat (NNT) | The number of patients who need to be treated to observe one additional beneficial outcome. | A lower NNT indicates a more effective device or therapy. For example, a cardiac stent with an NNT of 25 is highly effective [30]. |
| Number Needed to Harm (NNH) | The number of patients who need to be treated to observe one additional adverse event. | A higher NNH indicates a safer profile. A device with an NNH of 200 suggests a low likelihood of harm [30]. |
| Quality-Adjusted Life Year (QALY) | A measure of disease burden that combines both the quality and quantity of life lived. | Quantifies the overall health benefit a device provides, allowing for comparison across different therapeutic areas [30]. |
| Benefit-Risk Ratio | A ratio comparing the frequency and/or magnitude of benefits to the frequency and/or severity of risks. | A ratio greater than 1 suggests benefits outweigh risks. This provides a single, summary figure for the balance. |
The relationship between these quantitative inputs and the final benefit-risk decision can be visualized as a logical pathway.
Addressing Common Challenges and Regulatory Scrutiny
Despite the availability of frameworks, organizations often face challenges in implementation. Notified Bodies and regulatory agencies frequently flag several common shortcomings [30]:
- Insufficient Clinical Evidence: Making broad claims that are not supported by targeted, robust data.
- Incomplete Risk Characterization: Failing to detail the severity, likelihood, or affected patient populations for identified risks.
- Over-Reliance on Qualitative Analysis: Lacking quantitative insights to substantiate the benefit-risk profile for high-risk devices.
- Documentation Inconsistencies: Having misalignments across key documents such as the Clinical Evaluation Report, risk management file, and post-market surveillance reports [30].
To overcome these hurdles, manufacturers should adopt a culture of continuous improvement, leveraging tools that centralize data and automate workflows to ensure consistency and comprehensiveness in regulatory submissions [30]. Furthermore, a successful sBR framework requires cross-functional buy-in from clinical development, patient safety, biostatistics, regulatory, and epidemiology functions to be fully effective and adopted [32].
Operationalizing safety through rigorous device testing and a structured benefit-risk analysis is not a one-time activity but a dynamic, integrated process that spans the entire product lifecycle. By adopting a proactive mindset, implementing clear methodological frameworks, and leveraging both qualitative and quantitative tools, biomedical engineering professionals can navigate complex regulatory landscapes with confidence. This disciplined approach ensures that innovative medical technologies not only reach the market but also truly serve the best interests of patients, thereby upholding the highest ethical standards of the biomedical engineering profession.
Within the framework of the Biomedical Engineering Society's (BMES) Code of Ethics, which underscores a commitment to "honesty and conscientiousness in scientific inquiry," the process of obtaining informed consent is not merely a regulatory hurdle but a fundamental ethical obligation [5]. The modern definition of informed consent encompasses full disclosure of the research nature and the participant's involvement, adequate comprehension by the potential participant, and the participant's voluntary choice to participate [33]. For biomedical engineers, researchers, and drug development professionals, this process presents a unique communication challenge: translating complex, often highly technical information into accessible knowledge that empowers individuals to make autonomous decisions about their participation.
The stakes for effective consent are high. Historical breaches, from the non-consensual procedures in the Pratt v. Davis and Schloendorff cases to the atrocities of Nazi experimentation and the Tuskegee Syphilis Study, highlight the profound human cost when autonomy is disregarded [33]. Today, the landscape is further complicated by the era of big data and biospecimen research, where the potential future uses of data are vast and often unforeseeable at the point of collection [33]. This technical guide provides an in-depth examination of engineered communication strategies and experimental protocols designed to operationalize the BMES ethical principles, ensuring that informed consent is not just a signed form, but a truly informed patient decision.
Empirical research is critical to understanding the factors that influence a patient's decision to share their medical data and biospecimens. A 2019 survey study of 1,246 patients at two academic hospitals provides key quantitative insights into these preferences, examining the effects of different consent interface designs [34].
Table 1: Patient Data and Biospecimen Sharing Rates by Recipient Type
| Data Recipient | Percentage of Patients Declining to Share | Percentage Willing to Share All Items |
|---|---|---|
| Home (Primary) Healthcare Institution | 3.7% | 67.1% |
| Nonprofit Institutions | 28.3% | Not Specified |
| For-Profit Institutions | 47.4% | Not Specified |
Source: Adapted from JAMA Network Open (2019) [34].
The study also randomized patients to one of four consent interface options to assess the impact of presentation on sharing rates. The key experimental conditions were:
- Opt-In Simple: Patients actively selected data items they would share from a list of 18 broad categories.
- Opt-In Detailed: Patients actively selected data items they would share from a list of 59 detailed items.
- Opt-Out Simple: Patients selected data items they would not share from a list of 18 broad categories (all items were pre-selected for sharing).
- Opt-Out Detailed: Patients selected data items they would not share from a list of 59 detailed items (all items were pre-selected for sharing).
Table 2: Impact of Consent Interface Design on Sharing Decisions
| Experimental Variable | Number of Variables Associated with Sharing Decision | Statistical Significance |
|---|---|---|
| Opt-Out vs. Opt-In Interface | 59 out of 59 choice variables (100%) | Highly Significant |
| Simple vs. Detailed Form Layout | 14 out of 59 choice variables (23.7%) | Significant for a minority of variables |
Source: Adapted from JAMA Network Open (2019) [34].
The findings demonstrate that the choice architecture of the consent form—specifically, whether a system uses an opt-in or opt-out default—profoundly influences participant choices. This evidence underscores the engineer's responsibility in designing neutral, non-coercive consent pathways that minimize bias.
Experimental Protocols for Validating Consent Comprehension
Protocol: A Digital-First Recruitment and Consent Workflow
A 2025 study published in JMIR Formative Research detailed a successful, IRB-approved protocol for automating patient identification, recruitment, and consent, achieving the enrollment of 1000 participants for an observational study on perinatal ultrasonography [35]. This protocol serves as a model for leveraging technology to enhance the scale and efficiency of ethical consent processes.
Methodology:
- Ethical Approval and Oversight: All study elements were approved by the Northwestern University Institutional Review Board (STU00215717), ensuring adherence to ethical standards [35].
- Participant Identification: Automated SQL queries were run every 24 hours on a centralized Enterprise Data Warehouse (EDW) to identify eligible patients (e.g., aged ≥18, English-speaking, ≥16 weeks gestational age) with upcoming appointments [35].
- Personalized Invitation: Eligible patients received personalized email invitations via the REDCap (Research Electronic Data Capture) application programming interface. The email contained comprehensive study information and a unique link to a digital consent form hosted on REDCap [35].
- Digital Consent: Participants reviewed the e-consent form and provided their consent digitally. The research nurse cosigned the forms upon receipt.
- Data Management and Linkage: Consented patients were uploaded to a secure, HIPAA-compliant server. A unique QR code and examination ID were generated for each participant, enabling the de-identified linkage of collected ultrasound data with existing clinical data from the EDW without using protected health information (PHI) [35].
Outcome: Over 19 months, automated queries identified 20,988 eligible patients. From 10,582 emailed invitations, 1,000 patients (9.45%) provided digital consent, and 549 completed 779 study visits, successfully meeting the recruitment target ahead of schedule [35].
Protocol: Implementing and Documenting Verbal Consent
The use of verbal consent, particularly in minimal-risk research or settings where written consent is impractical, is recognized as an ethically valid alternative [36]. Its use was accelerated during the COVID-19 pandemic to limit viral exposure and accommodate ill patients [36]. The following methodology ensures rigor and documentation.
Methodology:
- REB/IRB Approval: The verbal consent process and script must be submitted for review and approval by the Research Ethics Board (REB) or Institutional Review Board (IRB) before implementation [36].
- Script Development: A standardized script must be developed, containing all elements of informed consent presented in clear, simple language. The script should be validated for readability and understanding.
- Participant Information Provision: Where possible, a paper or electronic copy of the consent script and information sheet should be provided to the participant in advance of the consent conversation [36].
- The Consent Conversation: A researcher obtains consent verbally via telephone, videoconference, or in-person. The conversation should be interactive, allowing the participant to ask questions and receive immediate answers. The use of audiovisual tools can enhance understanding and retention [36].
- Documentation: The researcher must document the consent in a manner approved by the REB/IRB. This can include:
- An audio recording of the consent conversation.
- A written summary of the information conveyed and the participant's agreement, signed by the researcher.
- Completion of a check-box in a study record confirming verbal consent was obtained [36].
The Scientist's Toolkit: Research Reagent Solutions for Consent Workflows
Table 3: Essential Tools for Engineering Modern Consent Processes
| Tool / Solution | Primary Function | Application in Consent & Research |
|---|---|---|
| Enterprise Data Warehouse (EDW) | Secured, centralized database of electronic medical records. | Automated, criteria-based identification of eligible research participants while leveraging existing clinical data [35]. |
| REDCap (Research Electronic Data Capture) | Web application for building and managing online surveys and databases. | Distributing personalized study invitations, hosting digital consent forms, and managing participant response data [35]. |
| Verbal Consent Script | A standardized, REB/IRB-approved dialogue for obtaining consent verbally. | Enrolling participants in minimal-risk research or where written consent is impractical (e.g., remote settings, rare disease research) [36]. |
| Unique QR Code System | A machine-readable optical label that links to information. | Enabling secure, de-identified linkage of research data (e.g., imaging) with a participant's unique study ID, minimizing PHI handling [35]. |
| HIPAA-Compliant Server | A computing server that meets security standards for protected health information. | Storing consented participant lists, research data, and documentation in a secure environment, mitigating data breach risks [35]. |
Visualizing Workflows: From Recruitment to De-identified Data
The following diagrams, generated using Graphviz DOT language, illustrate the logical flow of the digital recruitment and verbal consent protocols detailed in this guide.
Digital Recruitment & Consent Workflow
Verbal Consent Implementation
For the biomedical engineering community, guided by the BMES Code of Ethics, the process of obtaining informed consent is a critical area for the application of systematic, human-centered design. As this guide has detailed, moving beyond the static written form to embrace dynamic, digital, and verbal models—buttressed by quantitative data, rigorous experimental protocols, and secure technological tools—allows researchers to bridge the comprehension gap. By intentionally engineering the communication process, biomedical professionals can ensure that the ethical principle of respect for persons is upheld, fostering trust and enabling truly informed patient decisions that are foundational to responsible and innovative research.
The field of biomedical engineering operates at the critical intersection of technological innovation, commercial viability, and public health imperatives. Intellectual property (IP) protection serves as the fundamental framework that fuels investment in research and development, yet it simultaneously creates complex ethical challenges regarding equitable access to medical advancements. For researchers, scientists, and drug development professionals, navigating this landscape requires balancing competing priorities: securing exclusive rights to incentivize innovation while ensuring life-saving technologies reach the patients who need them. This technical guide examines the current IP environment within the context of the Biomedical Engineering Society Code of Ethics, which outlines professionals' commitment to "honesty and conscientiousness in scientific inquiry and technology development, and to advancing public health" [5]. With significant patent law reforms under consideration in 2025 and evolving policy pressures, understanding these dynamics becomes increasingly crucial for ethical decision-making in biomedical research and development [37].
Current Intellectual Property Framework and Pending Reforms
The intellectual property landscape for biomedical innovations is potentially poised for substantial changes in 2025, with three significant legislative proposals currently under congressional consideration. These acts aim to reform various aspects of patent law, each with distinct implications for biomedical engineers and healthcare innovators.
Table 1: Key Patent Law Legislation Under Consideration in 2025
| Legislative Act | Full Name | Key Provisions | Potential Impact on Biomedical Engineering |
|---|---|---|---|
| PREVAIL Act | Promoting and Respecting Economically Vital American Innovation Leadership Act | Requires standing for challengers; limits multiple petitions against same patent; addresses PTAB procedures [37] | Could make challenging pharmaceutical patents more difficult, potentially affecting drug pricing; may strengthen patent holder rights [37] |
| PERA | Patent Eligibility Restoration Act | Eliminates judicial exceptions from Mayo and Alice cases; creates specific list of excluded subject matter [37] | Would facilitate patenting of medical diagnostics and computer-implemented innovations; address current inconsistent application [37] |
| RESTORE Act | Realizing Engineering, Science, and Technology Opportunities by Restoring Exclusive Patent Rights Act | Establishes rebuttable presumption favoring permanent injunctions for patent infringement [37] | Would strengthen patent holder leverage in negotiations; potentially increase settlement values [37] |
These proposed legislative changes occur against a backdrop of significant policy turbulence, which 62% of healthcare industry leaders now identify as the primary force shaping the future of healthcare innovation—surpassing technology for the first time [38]. This policy focus reflects growing concerns about how federal actions impact the innovation ecosystem from laboratory to market.
The Patent Trial and Appeal Board (PTAB) Challenge Dynamic
The PREVAIL Act specifically addresses concerns about PTAB proceedings, which some have nicknamed the "patent death squad" due to the relative ease with which properly granted patents can be invalidated [37]. Senator Coons noted that "18 of the 20 largest litigants are from Big Tech, who use the PTAB to invalidate properly granted patents" [37]. For biomedical innovators, this reform could provide more stable patent protection, though critics worry it may "make it harder to challenge pharmaceutical patents, leading to higher drug prices" [37]—creating a direct tension between innovation incentives and public access to medicines.
Figure 1: PTAB Challenge Process and Proposed Reform Impacts
Ethical Dimensions of Intellectual Property in Biomedical Engineering
The Biomedical Engineering Society Code of Ethics provides a framework for navigating the complex ethical terrain where intellectual property rights intersect with public health responsibilities. Biomedical engineers face unique ethical challenges because their "design decisions directly affect patient health" [5], creating a professional obligation that extends beyond mere legal compliance.
Core Ethical Challenges in Biomedical IP
Patient Safety and Risk Assessment: Safety considerations represent both practical and ethical imperatives, requiring "rigorous testing, transparency in reporting potential risks and ongoing monitoring" of new medical devices [5]. The Therac-25 radiation therapy machine incident, where "lapses in safety design and risk assessment led to patient fatalities" [5], stands as a historical reminder of the high stakes involved.
Informed Consent in Human Testing: When medical device trials involve "implants into human subjects, participants must fully understand what they're consenting to, including surgical risks and potential hazards" [5]. This extends beyond obtaining a signature on a form to ensuring genuine comprehension.
Accessibility and Affordability Dilemmas: A significant challenge in biomedical engineering involves the "severe lack of diversity in biomedical research" [5], where implicit biases can harm research, design and innovation. According to NIH data, "Black scientists are 30% less likely than their white colleagues to receive NIH grants, and they represent only 1.5% of the applicant pool for the Research Project (R01) grant" [5].
Dual-Use Dilemmas: Biomedical engineers must consider how their research could be misapplied, as with "research on a deadly virus such as H1N1 (swine flu) [which] could lead to advances in treatment, but also poses risks if the pathogen gets into the wrong hands" [5].
Resource Allocation Decisions: Perhaps the most direct ethical challenge involves choosing between "the personal financial allure of keeping a patent private or the further-reaching benefit of making the invention widely available, which has broader implications for public health" [5].
The Public Health Impact of IP Decisions
The ethical imperative to consider public health impacts of IP decisions extends beyond individual products to systemic effects. Current data reveals concerning trends in how IP and policy decisions affect healthcare accessibility:
Table 2: Healthcare Access and Innovation Landscape (2025)
| Metric | Statistics | Implications for Biomedical IP |
|---|---|---|
| Healthcare costs | ~18% of US 2024 GDP from healthcare costs (up from 4% in 1970's) [39] | Pressure to justify patent protections through demonstrated value and outcomes |
| Unaddressed health needs | >33% of US consumers have unmet healthcare needs due to affordability concerns [39] | Questions about pricing models for essential medical technologies |
| Industry outlook | 87% of healthcare executives remain optimistic about healthcare innovation; 61% expect biotech sector growth despite uncertainty [38] | Continued investment environment despite policy challenges |
| Administrative overhead | ~25% of US healthcare costs from administrative overhead [39] | Opportunity for IP-protected digital solutions to reduce systemic costs |
Policy and Economic Pressures Reshaping the Innovation Ecosystem
The external environment for biomedical innovation is experiencing significant turbulence, with federal policy emerging as the dominant force shaping strategic decisions. Understanding these macro-level influences is essential for navigating IP strategy within the current healthcare landscape.
Federal Policy and Funding Impacts
Deep cuts to federal research agencies are creating ripple effects across the innovation ecosystem, potentially "disrupting traditional pathways from lab to market" [38]. Survey data reveals that:
- 69% of healthcare leaders believe federal cuts will "significantly or critically impact R&D" [38]
- 79% expect companies will "need to revise clinical development strategies" [38]
- 87% predict a negative impact on biotech innovation, with 46% calling it "extremely" negative [38]
As one industry leader noted: "Federal funding drives the most fundamental academic research that leads to the newest innovations and discoveries that the biotech industry builds itself upon" [38]. This foundational research supports the entire innovation pipeline, and reductions threaten to "stifle innovation and create bottlenecks that could take years to overcome" [38].
Global Supply Chain and Manufacturing Shifts
Trade policies and tariffs are introducing new complexities into biomedical manufacturing decisions, with 62% of surveyed executives stating these policies will be "very" or "extremely" impactful on their organizational decision-making [38]. The "America First" trade agenda has prompted pharmaceutical companies to commit an estimated "$215 billion to build, enhance or expand U.S.-based manufacturing" [38], though respondents noted this transition may "lead to increased costs for American consumers" [38] as companies absorb capital expenses for new manufacturing infrastructure.
Figure 2: Trade Policy Impact on Biomedical Manufacturing and Costs
Strategic Approaches for Balancing Innovation and Access
Navigating the complex IP landscape requires deliberate strategies that acknowledge both commercial realities and public health responsibilities. Several frameworks show promise for aligning innovation incentives with accessibility goals.
Technology Transfer and Research Collaboration Protocols
Effective translation of basic research into clinical applications requires structured approaches to technology transfer. The following methodology outlines key stages for managing IP in academic-industry partnerships:
Invention Disclosure Documentation: Comprehensive recording of research discoveries using standardized institutional forms, including:
- Detailed descriptions of the innovation
- Names of all contributors
- Funding sources and obligations
- Preliminary assessment of commercial potential
Patent Landscape Analysis: Systematic review of existing IP through:
- Keyword-based searches of patent databases
- Analysis of competitive technological space
- Freedom-to-operate assessments
- Identification of potential licensing partners
Protection Strategy Development: Formulation of appropriate IP protection approach:
- Evaluation of patentability criteria (novelty, non-obviousness, utility)
- Decision between trade secret vs. patent protection
- Geographic scope of protection (US vs. international filings)
- Timing considerations relative to publication schedules
Partnership Structuring: Negotiation of terms that balance commercial and access considerations:
- Field-of-use limitations
- Tiered pricing arrangements for different markets
- Global access provisions for low-income populations
- Publication and research use rights
Ethical IP Management Framework
The "Scientist's Toolkit" for responsible IP management includes both conceptual approaches and practical resources for addressing ethical challenges:
Table 3: Research Reagent Solutions for Ethical IP Management
| Tool/Resource | Function | Application Context |
|---|---|---|
| Institutional Review Boards (IRBs) | Provide ethical oversight; approve research; require modifications to procedures [5] | Human subjects research; clinical trials of medical devices |
| BMES Code of Ethics | Guidelines for "honesty and conscientiousness in scientific inquiry"; reporting systems for violations [5] | Daily professional practice; decision-making about patenting and licensing |
| Data Use Agreements | Establish parameters for responsible data sharing; protect patient privacy [5] | Collaborations involving patient data; multi-center research studies |
| Dual-Use Research Oversight | Security measures and guidelines to mitigate misuse of dangerous substances [5] | Research with pathogens; sensitive biological materials |
| Global Access Licensing | Contract provisions ensuring availability in low-income countries [5] | Licensing of essential medicines; health technologies |
Future Directions: The Evolving IP Landscape in Biomedical Engineering
The intellectual property framework for biomedical innovations continues to evolve in response to technological advancements, policy shifts, and changing public expectations. Several emerging trends will likely shape how researchers, scientists, and drug development professionals navigate this space in the coming years.
Technological Disruption and IP Considerations
Exponential advances in technology are creating new challenges and opportunities for IP protection in biomedical engineering. Artificial intelligence is playing an increasingly significant role, with "AI algorithms now able to design new drugs in months rather than years" [39]. More than 40% of health system executives report "already experienced a significant-to-moderate return on their investments in gen AI" [40], though concerns about data bias and "hallucinations" (false information generation) necessitate careful governance [40]. Other technological shifts include the growth of "digital twin" adoption, currently at approximately 25%, which enables "real-time simulations of patient physiology to predict risks and personalize interventions" [39], raising novel IP questions about the protectability of computational models and simulated outcomes.
Regulatory Evolution and Global Harmonization
The regulatory environment for biomedical IP is increasingly complex, with more than 80% of health system executives agreeing that "more AI regulations are needed" [40]. The FDA is actively "updating regulations to manage the growing use of AI in health care, with a focus on patient safety and the lifecycle of AI tools" [40]. Similarly, the European Union has implemented a comprehensive framework through the EU AI Act, which "classifies AI systems into four risk categories: unacceptable, high, limited, and minimal risk" [40]. This evolving regulatory landscape creates both compliance challenges and opportunities for innovators who successfully navigate requirements across multiple jurisdictions.
Navigating intellectual property in biomedical engineering requires maintaining a delicate equilibrium between competing priorities: incentivizing innovation through appropriate rewards while ensuring the resulting technologies reach the patients who need them. The proposed patent law reforms of 2025, combined with significant policy turbulence and funding uncertainties, create both challenges and opportunities for researchers, scientists, and drug development professionals. By grounding IP decisions in the ethical framework provided by the Biomedical Engineering Society Code of Ethics, and by implementing strategic approaches that explicitly consider public health impacts, biomedical engineers can fulfill their dual responsibility to both advance their field and serve the broader public good. As technological acceleration continues to reshape healthcare delivery, maintaining this balance will remain an ongoing challenge requiring continual dialogue, ethical reflection, and thoughtful policy engagement from all stakeholders in the biomedical innovation ecosystem.
Conflicts of interest (COI) represent a critical challenge in biomedical research, where professional judgment may be compromised by secondary interests, particularly financial relationships. Within biomedical engineering—a field characterized by close collaboration between academia and industry—effective COI management is essential to maintain research integrity, protect human subjects, and preserve public trust [41]. The increasing commercialization of academic research, facilitated by legislation such as the Bayh-Dole Act of 1980, has further amplified both the opportunities and risks associated with these relationships [41]. This guide provides a comprehensive technical framework for disclosing and managing COIs, supported by quantitative evidence and structured methodologies relevant to researchers, scientists, and drug development professionals operating within the ethical framework of biomedical engineering.
Defining Conflicts of Interest in Biomedical Context
Conceptual Framework and Typology
A conflict of interest exists when a researcher's impartiality may be compromised because they stand to profit from the conclusions they draw [42]. These conflicts can be categorized into three distinct types:
- Financial Conflicts of Interest (FCOI): Arise from financial ties to entities that may gain or lose from research outcomes, including research funding, personal remuneration, stocks, patents, or consultancy fees [43] [44].
- Non-Financial Conflicts of Interest (NFCOI): Include personal relationships, professional collaborations, unpaid advisory positions, or membership in advocacy organizations that could influence research objectivity [43] [44].
- Intellectual Conflicts of Interest (ICOI): Occur when researchers hold strong beliefs in particular theories or hypotheses that may bias their approach to research design and interpretation [43].
Scope and Impact on Research Integrity
COIs can influence multiple aspects of the research process, including study design choices, data interpretation, outcome reporting, and publication practices. The primary risk is that compromised research can directly impact healthcare quality by influencing clinical decision-making and potentially harming patients [42]. Even the appearance of impropriety can undermine trust in research institutions and the broader scientific enterprise [41].
Quantitative Evidence: Prevalence and Impact
Prevalence of Conflicts of Interest
Table 1: Documented Prevalence of Conflicts of Interest in Biomedical Research
| Research Context | Prevalence of COI | Study Findings | Source |
|---|---|---|---|
| Academic Researchers | 33% | One-third of biomedical researchers in academic institutions held conflicts of interest that could introduce risk of bias | [42] |
| Clinical Trial Reports | 29-69% | Varied rates of disclosed conflicts of interest across different clinical studies | [42] |
| Clinical Practice Guidelines (US/Canada) | 48% | Nearly half of guideline authors disclosed conflicts of interest | [42] |
| Clinical Practice Guidelines (Denmark) | 96% | Nearly all guidelines had at least one author with a conflict of interest, but only 2% disclosed them | [42] |
| Undisclosed COI | 43-69% | Failure to include disclosures of conflicts of interest in study reports | [42] [41] |
| Cancer Researchers | 32% | Had not fully disclosed industry payments in articles published in major medical journals | [41] |
| US Physicians | 48% | Nearly half received payments from drug and medical device companies totaling $2.4 billion | [41] |
Documented Effects on Research Outcomes
Table 2: Documented Effects of Conflicts of Interest on Research Outcomes
| Type of Bias | Manifestation | Evidence | Source |
|---|---|---|---|
| Selective Outcome Reporting | Choice of comparators producing favorable results; selective inclusion of outcomes | Researchers with COI more likely to use favorable comparators | [42] |
| Interpretation Bias | Conclusions inconsistent with study results | Association between COI and interpretation favoring sponsor's product | [42] |
| Publication Bias | Non-publication of negative results; delayed publication | COI associated with completing trials without publication | [42] |
| Systematic Review Bias | Interpretation favoring interventions | Authors with financial COI more likely to interpret data as supporting intervention | [42] |
| Clinical Guideline Influence | Recommendation of interventions in practice | Contributors with COI more likely to recommend intervention | [42] |
| Sugar Industry Research | 5x higher likelihood of favorable outcomes | Studies with financial interests in sugar industry five times more likely to find no relationship between sugary beverages and obesity | [41] |
Disclosure Framework Components
Core Disclosure Requirements
An effective disclosure framework requires transparency about specific categories of interests:
- Funding Sources: Complete disclosure of all research support (salaries, equipment, supplies) from organizations that may gain or lose financially through publication [44]. The specific role of the funder in study conceptualization, design, data collection, analysis, or manuscript preparation must be explicitly stated [44].
- Employment Relationships: Recent, present, or anticipated employment by any organization with a financial stake in the research outcomes [44].
- Personal Financial Interests: Stocks, shares, consultation fees, reimbursements, patents, or patent applications whose value may be affected by publication [44]. Diversified mutual funds or investment trusts are typically excluded [44].
- Non-Financial Interests: Unpaid roles in government, non-governmental organizations, advocacy groups, advisory positions, or expert witness roles [44].
Institutional Policies and Thresholds
While specific monetary thresholds vary, many US universities require disclosure of interests exceeding $10,000 or 5% equity in a company [44]. The Nature Portfolio journals propose a practical alternative guideline: "Any undeclared competing financial interests that could embarrass you were they to become publicly known after your work was published" [44].
Experimental Protocols for COI Assessment
Systematic Assessment Methodology
The COIPonD (Conflicts of Interest Publication Disclosures) dataset provides a methodology for systematically evaluating COI disclosure patterns [45]:
Diagram 1: COI data collection workflow
Implementation Protocol
- Product Identification: Utilize clinically relevant drug lists (e.g., ClinCalc's Top 300 drugs based on Medical Expenditure Panel Survey data) to identify target products [45].
- Search Strategy Development: For each product, identify preferred Medical Subject Headings (MeSH) terms using the National Library of Medicine's vocabulary browser [45].
- Query Execution: Deploy iterative search strategies using eUtilities API, collecting up to 200 articles per product sorted by relevance [45].
- Data Extraction: Implement three-tiered extraction: (1) PubMed-indexed disclosure statements (
tag), (2) PubMed Central alternative tag search, (3) manual collection where automated methods fail [45]. - Data Integration: Aggregate results into a comprehensive dataset capturing author-reported disclosures across multiple publications and timelines [45].
Research Reagent Solutions
Table 3: Essential Resources for COI Disclosure Research
| Resource/Reagent | Function | Application Context |
|---|---|---|
| COIPonD Dataset | Provides structured database of author-reported COI disclosures | Analysis of disclosure patterns across 38,000+ papers, 319 commonly used drugs [45] |
| PubMed eUtilities API | Programmatic access to MEDLINE/PubMed citations | Automated retrieval of COI statements and publication metadata [45] |
| MeSH (Medical Subject Headings) | Controlled vocabulary for biomedical concepts | Standardized search strategy development for systematic literature review [45] |
| Open Payments Database | Reports of payments to physicians from manufacturers | Verification of disclosed financial relationships for US healthcare providers [42] |
| ClinCalc DrugStats | Ranking of most commonly used drug products | Identification of clinically relevant products for focused COI analysis [45] |
Institutional Implementation Framework
Multi-tiered Management System
Effective COI management requires a comprehensive institutional approach:
Diagram 2: COI management system structure
Journal Policy Requirements
Biomedical engineering publications should implement clear COI policies:
- Author Disclosures: Require corresponding authors to submit competing interest statements on behalf of all authors, with published declarations in the article [44].
- Reviewer Screening: Invite peer-reviewers to exclude themselves in cases of significant conflicts and inform editors of relevant interests [44].
- Editorial Standards: Require editorial staff to declare interests that might influence editorial practices, with exclusion from handling manuscripts where conflicts exist [44].
- Double-Blind Review: Implement double-blind peer review systems where authors' identities are concealed from reviewers and vice versa to reduce bias [43].
Robust conflict of interest disclosure frameworks are essential for maintaining integrity in biomedical engineering research. The quantitative evidence demonstrates that COIs are prevalent, frequently underreported, and associated with measurable biases in research outcomes. Effective implementation requires standardized disclosure taxonomies, systematic assessment methodologies, and multi-tiered institutional management systems. As biomedical engineering continues to bridge academia and industry, proactive COI management will be crucial for sustaining scientific credibility, protecting patients, and fostering public trust in research outcomes. Future directions should focus on developing interoperable disclosure registries, harmonizing reporting standards across institutions and journals, and validating the efficacy of different management strategies through empirical research.
The field of biomedical engineering stands at the intersection of technological innovation and human health, carrying profound ethical responsibilities for ensuring equity and inclusion. The Biomedical Engineering Society (BMES) Code of Ethics establishes a foundational expectation that professionals in the field will honor their "commitment to honesty and conscientiousness in scientific inquiry and technology development, and to advancing public health" [5]. This ethical framework necessitates active efforts to dismantle discriminatory practices and intentionally build inclusive research cultures [46]. Beyond moral duty, evidence-based science itself requires inclusive data to improve human health and address global inequities effectively [47]. When diversity and inclusion are sidelined, scientific progress is hindered through gaps in data that distort findings and skew results, ultimately compromising the applicability and safety of biomedical technologies across all populations [47].
The interconnected nature of these challenges requires a dual-focused approach: developing technologies that are accessible across the spectrum of human diversity while simultaneously fostering research teams that reflect the populations they serve. This whitepaper provides a comprehensive technical and methodological framework for achieving these goals, offering researchers, scientists, and drug development professionals practical tools for implementing equity-centered practices throughout the research and development lifecycle.
The Case for Diversity, Equity, and Inclusion in Biomedical Research
The Quantitative Impact on Innovation and Health Outcomes
Substantial evidence demonstrates that diversity strengthens the STEM talent pool and contributes significantly to greater innovation and productivity in research settings where team members engage in cooperative problem-solving [48]. Diverse teams bring varied perspectives that enhance creative problem-solving and lead to more robust scientific solutions [49]. The data reveals compelling connections between diverse representation and research outcomes:
Table 1: Impact of Diversity on Research and Health Outcomes
| Area of Impact | Current Disparity | Consequence | Potential Benefit |
|---|---|---|---|
| NIH Funding | Black scientists are 30% less likely to receive NIH grants [5] | Reduced diversity in research priorities | More equitable funding distribution |
| Cell Line Diversity | Donors of European ancestry are over-represented; male cell lines outnumber female [47] | Limited applicability of disease models | Bioengineered models that reflect human diversity |
| Device Abandonment | Higher in women (39%) than men (23%) for mobility devices [50] | Increased fall rates and reduced quality of life | Improved device design and adoption |
| Workforce Representation | Severe underrepresentation of African Americans, Hispanics, and Native Americans in STEM PhDs [48] | Limited understanding of diverse physiological needs | Enhanced innovation and cultural competence |
Beyond the Pipeline: Talent Development Paradigm
The traditional "pipeline metaphor" for STEM career development imagines students flowing through a sequence of age-dependent educational stages. This model fails to account for the incredible heterogeneity of individuals within scientific training and the varied levels of skills each has developed as they pass traditional academic milestones [48]. A more effective approach emphasizes talent development decoupled from age or educational stage, recognizing that students develop skills at different rates based on factors such as earlier access to educational resources, exposure to research experiences, and competing demands for time during their education [48]. This perspective transforms our approach from patching "leaks" in a rigid pipeline to actively developing talent through coaching models and individualized development plans that address the specific needs of underrepresented students.
Designing Accessible Technologies: Methodologies and Considerations
Diversity Factors in Wearable Assistive Technology Development
The development of wearable assistive and rehabilitation technologies (WEARTechs) exemplifies the critical importance of incorporating diversity considerations from the earliest R&D stages. These technologies interface directly with the human body, creating a small margin for error in fit and adaptability. Research indicates that diversity has not been adequately addressed in this field, leading to significant usability issues and device abandonment [50]. Key considerations include:
Physical Interface & Body Morphology: Body morphology differs across genders and ages, affecting factors such as hip width, chest size, and pressure pain thresholds [50]. A review of exoskeletons developed specifically for nurses (a majority-female profession) listed "design with focus on women's body shape" as the most important characteristic [50].
Biosignals & Technology Adaptability: Electromyography (EMG) signals used for inferring motion intent in many WEARTechs are affected by skin properties that differ across skin colors and racial backgrounds [50]. Systems using these signals must account for such variations to ensure consistent performance across populations.
Representative Participant Pools: Participant pools in WEARTechs R&D often fail to represent the target population, leading to reported results that misrepresent real-world performance [50].
Table 2: Diversity Considerations in WEARTech Research and Development
| R&D Stage | Diversity Factor | Impact | Recommended Action |
|---|---|---|---|
| Participant Recruitment | Gender, age, body morphology, racial background | Determines generalizability of findings | Ensure participant pool reflects target user population demographics |
| Signal Acquisition | Skin properties affecting EMG signals [50] | Variation in system performance across users | Calibrate systems across diverse skin types and physiological characteristics |
| Physical Design | Body shape and size variations [50] | Comfort, safety, and device abandonment | Incorporate anthropometric data from diverse populations into design parameters |
| User Testing | Cultural norms, personal preferences [50] | Long-term adoption and satisfaction | Employ intersectional approach considering multiple diversity characteristics |
Experimental Protocols for Inclusive Technology Design
Implementing rigorous experimental protocols is essential for developing technologies that perform effectively across diverse populations. The following methodology provides a framework for inclusive technology design:
Protocol: Inclusive Evaluation of WEARTech Performance Across Diverse Users
Participant Recruitment Strategy:
- Implement stratified sampling to ensure representation across gender, age, racial/ethnic background, and socioeconomic status
- Include participants with intersectional identities (e.g., older adults from minority backgrounds)
- Establish partnerships with community organizations to reach underrepresented populations
Diversity Factor Assessment:
- Document relevant biological variables (sex, body morphology, skin properties)
- Record sociocultural factors (technology familiarity, cultural preferences)
- Assess environmental contexts (home environment, support systems)
Performance Metrics:
- Quantitative measures: device accuracy, precision, reliability across user subgroups
- Qualitative measures: comfort, usability, cultural acceptance
- Longitudinal tracking: device abandonment rates, satisfaction over time
Data Analysis:
- Disaggregate performance data by diversity characteristics
- Identify significant interactions between user factors and technology performance
- Implement statistical power analyses ensuring adequate sample sizes for subgroup analyses
This systematic approach enables researchers to identify and address diversity-related performance variations before technologies reach broader implementation, ultimately reducing device abandonment and improving health outcomes across populations.
Visualization: Inclusive Technology Development Workflow
The following diagram illustrates a comprehensive framework for integrating diversity considerations throughout the technology development process:
Fostering Diverse Research Teams: Frameworks and Implementation
Program-Level Approaches for DEI Integration
Successful integration of diversity, equity, and inclusion principles requires systematic, program-level approaches rather than isolated initiatives. Research demonstrates that comprehensive frameworks can effectively develop DEI-competent bioengineers while meeting evolving accreditation requirements [51]. Key components of successful programs include:
DEI Planning Worksheets: Structured tools that guide instructors in critically assessing course content, pedagogy, and classroom practices to improve student outcomes and experiences, with a focus on inclusivity [51]. These worksheets encourage incorporation of instructor leadership on inclusivity, inclusive pedagogy, student feedback mechanisms, professional development skills, and course materials that include work from historically excluded scholars.
Faculty Support Systems: Providing individualized assistance, consultations, and collaborative curriculum development to support instructors in implementing DEI content and inclusive pedagogical approaches [51]. Pre- and post-term surveys of faculty revealed that 91% of responding instructors described at least one DEI curricular content improvement, and 88% incorporated at least one new inclusive pedagogical approach when supported systematically [51].
Categorized DEI Competencies: Grouping bioengineering-related DEI content into five key categories: bioethics, inclusive design, inclusive scholarship, inclusive professionalism, and systemic inequality [51]. This framework provides a comprehensive structure for integrating DEI throughout biomedical engineering curricula.
Assessment Methodologies for DEI Initiatives
Robust assessment is critical for evaluating the effectiveness of DEI initiatives and guiding continuous improvement. Multifaceted assessment approaches should include:
Direct Assessment via Course Assignments: Evaluating student performance on DEI-related learning objectives through standardized rubrics and competency assessments [51].
Student Surveys and Feedback: Collecting anonymous feedback through end-of-module surveys, end-of-term course evaluations, and annual program reviews [51]. In one program, students reported a relatively high average of 3.79 (on a scale of 1="not at all" to 5="very much") when asked how much their experience helped them develop specific DEI competencies [51].
Faculty Adoption Metrics: Tracking implementation of DEI content and inclusive pedagogical approaches across courses and programs [51].
Table 3: Research Reagent Solutions for Inclusive Biomedical Engineering
| Resource Category | Specific Tools/Methods | Function in Promoting Equity |
|---|---|---|
| DEI Integration Tools | DEI Planning Worksheets [51] | Guides systematic incorporation of DEI principles into curricula and research design |
| Inclusive Design Frameworks | Intersectional Analysis Matrix [50] | Identifies how multiple diversity characteristics interact to affect technology use |
| Bias Mitigation Protocols | Representative Recruitment Strategy [50] | Ensures participant pools reflect target population diversity |
| Assessment Tools | Disaggregated Performance Analysis [50] | Identifies variation in technology performance across user subgroups |
| Community Engagement Methods | Participatory Design Workshops [47] | Involves diverse stakeholders in technology development process |
Ethical Considerations and Implementation Challenges
Addressing Barriers to Inclusive Research
Despite growing recognition of the importance of DEI in biomedical engineering, significant implementation challenges persist:
Implicit Bias and Stereotyping: Unconscious attitudes and beliefs continue to affect understanding, decision-making, and professional advancement in biomedical engineering [49]. These biases may manifest as preconceptions about capabilities based on race, gender, age, or socioeconomic status.
Insufficient Access to Resources: Limited access to educational resources, state-of-the-art research facilities, and effective mentorship creates significant barriers to inclusion [5] [49]. This disproportionately affects individuals from underserved communities and social minorities.
Historical Mistrust: Decades of unethical experimentation on Black, Indigenous, and marginalized populations have created justified medical and scientific mistrust that must be acknowledged and overcome to diversify participation in research studies [47].
Ethical Framework for Inclusive Technology Development
Biomedical engineers must navigate complex ethical considerations when designing technologies for diverse populations:
Cultural Sensitivity: Understanding and accounting for personal, cultural, and scientific differences is essential for bridging healthcare disparities and promoting ethical practices in cross-cultural settings [5].
Dual-Use Dilemmas: The potential misuse or abuse of biomedical technologies requires careful consideration of pros and cons along with implementation of strict security measures and ethical oversight [5].
Accessibility and Affordability: Ensuring that beneficial technologies are accessible and affordable to the communities that need them, not just privileged populations [5].
Environmental Impact: Considering the environmental footprint of biomedical research and technology development, including sustainable practices for recycling and disposing of medical devices [5].
Promoting equity and inclusion in biomedical engineering requires intentional, systematic approaches to both technological design and research team composition. By implementing the frameworks, methodologies, and assessment tools outlined in this whitepaper, researchers, scientists, and drug development professionals can significantly advance both the quality and impact of their work. The ethical imperative is clear: as the BMES Code of Ethics states, biomedical engineers must "confront and dismantle discriminatory behavior wherever it may manifest individually or organizationally" [46].
Future progress will depend on continued development and sharing of best practices, expanded assessment of DEI initiatives, and commitment to structural changes that support inclusive research environments. As the field advances, prioritizing diverse inputs and inclusive methodologies will enhance the applicability and impact of biomedical engineering research, ultimately leading to more equitable health outcomes for all populations.
Navigating Moral Dilemmas: Strategies for Ethical Crisis Management and Decision-Making
The development of medical technology represents a profound responsibility, where engineering decisions directly impact human life. Within the field of biomedical engineering, studying failures provides critical insights that can transform professional practice and reinforce ethical standards. The cases of the Therac-25 radiation therapy machine and the Bjork-Shiley heart valve stand as landmark examples of how technical oversights, when coupled with organizational deficiencies, can lead to tragic outcomes. This whitepaper examines these cases through a technical lens, analyzing the root causes of failure and extracting essential lessons for the biomedical engineering community. These historical incidents directly inform the modern Biomedical Engineering Society Code of Ethics, which outlines the professional obligations of biomedical engineers to prioritize patient safety, ensure research integrity, and maintain transparent practices [5]. By understanding these failures in the context of ethical frameworks, researchers, scientists, and drug development professionals can better navigate the complex challenges inherent in creating medical technologies.
The Therac-25 Case Study
Background and Technical Specifications
The Therac-25 was a state-of-the-art linear accelerator developed by Atomic Energy Canada Limited (AECL) and French company CGR to provide radiation treatment for cancer patients [52]. As the most computerized radiation therapy machine of its time, it utilized an onboard computer to select treatment table positions and control the type and strength of energy delivered by an operating technician [52]. Unlike its predecessors (Therac-6 and Therac-20), which operated with hardware safety interlocks and could function independently of their computer systems, the Therac-25 relied primarily on software for safety controls [52] [53]. This design decision removed redundant hardware safeguards that had proven effective in earlier models.
The machine operated in three primary modes, with a turntable moving different apparatus into position for each: a "field light" mode for patient positioning using visible light; direct electron-beam therapy (5-25 MeV) for treating surface tumors; and megavolt X-ray therapy (25 MeV) for deeper tissues, which required electrons to collide with a tungsten target to produce photons [53]. The electron beam current required for X-ray production was approximately 100 times greater than that used for electron therapy, creating significant potential danger if improperly controlled [53].
Documented Failures and Incidents
Between 1985 and 1987, six major accidents involving the Therac-25 resulted in significant radiation overdoses to patients, leading to death or serious injury [52] [53]. In one documented case at the Kennestone Regional Oncology Center in June 1985, a patient received an estimated 15,000-20,000 rad (150-200 Gy) when the prescribed dose was only 200 rad (2 Gy) [53]. For context, a dose of 1,000 rad (10 Gy) is typically fatal [53]. Patients reported sensations likened to an "intense electric shock" or "red-hot sensation," with radiation burns appearing days later [53]. Despite these reports, technicians and initially the manufacturer believed such overdoses were impossible, delaying crucial investigations [52].
Table 1: Documented Therac-25 Radiation Overexposure Incidents
| Date | Location | Reported Injury | Estimated Dose | Intended Dose |
|---|---|---|---|---|
| June 1985 | Kennestone Regional Oncology Center, Georgia | Severe radiation burns, tissue damage requiring mastectomy | 15,000-20,000 rad | 200 rad |
| July 1985 | Ontario Cancer Foundation, Canada | Radiation burns, tissue damage contributing to death | Not specified | Not specified |
| 1985-1987 | Multiple facilities across US & Canada | Additional incidents resulting in death or serious injury | 100+ times normal | Standard therapeutic levels |
Root Cause Analysis
Investigation revealed that the accidents stemmed from two primary software race conditions [53]. The first occurred when operators incorrectly selected X-ray mode and then rapidly switched to electron mode within approximately eight seconds, allowing the electron beam to be configured for X-ray power levels without the protective X-ray target being in place [53]. The second fault permitted electron beam activation during field-light mode, where no beam scanner or target was positioned [53]. These software defects, combined with the absence of independent hardware interlocks that had been present in earlier models, created conditions where massive radiation overdoses could occur.
The software for the Therac-25 had been developed by a single programmer over several years using PDP-11 assembly language and was an evolution of the code used in the earlier Therac-6 model [53]. Subsequent analysis identified critical flaws in the software development process, including inadequate testing, poor error reporting, and reuse of code from previous systems without sufficient safety verification [52]. The manufacturer also demonstrated organizational deficiencies, including inadequate record-keeping during software design, insufficient response to user reports of problems, and difficulty reproducing the error conditions in clinical settings [52].
Table 2: Therac-25 Failure Mechanism Analysis
| Factor Category | Specific Deficiency | Consequence |
|---|---|---|
| Software Engineering | Race conditions in control software | Machine could operate with wrong components in place |
| Inadequate error checking and handling | No meaningful error messages or safety shutdowns | |
| Reused code from previous systems without safety verification | Inherited vulnerabilities from earlier designs | |
| System Architecture | Removal of hardware safety interlocks | No redundant safety mechanisms |
| Over-reliance on software for safety functions | Single point of failure potential | |
| Organizational Process | Inadequate testing and quality assurance | Defects not identified before clinical use |
| Poor incident response and investigation | Patterns not recognized, problems continued | |
| Lack of transparency with users and regulators | Delayed regulatory intervention |
Experimental Analysis and Investigation Methodology
The investigation into the Therac-25 failures followed a methodology that can be abstracted as an experimental protocol for forensic engineering analysis:
The forensic process began with incident reporting from clinical sites where patients experienced unexpected reactions [52] [53]. Engineers then attempted to reproduce the failure conditions in laboratory settings, though AECL initially had difficulty consistently replicating the issues [52]. This was followed by software code review, which revealed the race conditions that allowed the machine to operate with incorrect configurations [53]. A system safety audit compared the Therac-25 architecture with earlier successful models, identifying the critical absence of hardware interlocks [53]. This comprehensive methodology ultimately identified the root causes and informed the necessary redesign of the machine's safety systems.
Research Reagents and Tools for Radiation Therapy Safety Analysis
The investigation and ongoing safety analysis of radiation therapy systems requires specialized tools and methodologies:
Table 3: Essential Research Reagents and Tools for Radiation Therapy Safety Analysis
| Tool/Reagent | Function | Application in Safety Analysis |
|---|---|---|
| Radiation Dosimeters | Measure radiation dose delivered | Quantifying potential overdose conditions |
| PDP-11 Assembly Language Tools | Software analysis and debugging | Identifying race conditions and coding errors |
| Hardware Interlock Prototypes | Independent safety mechanisms | Testing redundant safety systems |
| Failure Mode and Effects Analysis (FMEA) | Systematic risk assessment | Proactively identifying potential failure points |
| Incident Reporting Database | Track and analyze adverse events | Identifying patterns across multiple facilities |
Bjork-Shiley Heart Valve Case Study
Background and Technical Specifications
The Bjork-Shiley heart valve was a popular prosthetic heart valve developed in the 1970s to replace damaged or diseased human heart valves [5]. The valve utilized a monostrut design that featured a disc that could tilt to open and close, allowing for one-way blood flow through the heart [54]. Unlike valves machined from a single piece of material, the Bjork-Shiley valve incorporated a welded strut that was attached to the valve ring during manufacturing [54]. This welding process introduced potential points of failure that would become central to the valve's reliability issues.
Documented Failures and Incidents
By the 1980s, reports emerged of strut fracture in implanted Bjork-Shiley valves, leading to catastrophic failure and often patient death [54] [5]. Metallurgical analysis of failed valves revealed that fractures consistently originated in the welds joining the short strut to the valve ring [54]. The fracture surfaces showed characteristic patterns of fatigue failure with branching cracks, suggesting progressive failure over time rather than immediate catastrophic breakage [54]. In some cases, examination revealed that one leg of the strut had failed long before the other, yet this partial failure remained clinically undetectable until complete valve failure occurred [54]. It is estimated that these failures resulted in at least 600 adverse outcomes, including fatalities [5].
Root Cause Analysis
Metallurgical examination of both failed and unused valves identified significant welding defects as the primary cause of failure [54]. Analysis of an unused valve revealed "several sizable defects directly attributable to the welding process" in the strut-ring junction [54]. These defects created stress concentration points where fatigue cracks could initiate and propagate over time with the cyclic loading of normal heart function [54]. The investigation concluded that the valves failed by fatigue, and researchers suggested that these problems could have been avoided "if the complete valve cage were machined as a single piece" rather than relying on welded components [54].
The case also revealed significant organizational and ethical failures, as early indications of anomalies and reports of malfunctions did not result in timely withdrawal of the valves from the market [5]. Despite growing evidence of safety issues, the valves remained in use for years, leading to preventable adverse outcomes.
Table 4: Bjork-Shiley Heart Valve Failure Analysis
| Factor Category | Specific Deficiency | Consequence |
|---|---|---|
| Manufacturing Process | Defective weld joints | Stress concentrations and crack initiation sites |
| Quality control limitations | Defective valves not detected before implantation | |
| Design Selection | Welded strut rather than single-piece construction | Inherent structural vulnerability |
| Lack of fail-safe mechanisms | Partial failures not detectable before catastrophic failure | |
| Organizational Response | Delayed response to incident reports | Continued implantation of potentially defective valves |
| Inadequate communication of risks | Physicians and patients unaware of potential failure modes |
Experimental Analysis and Investigation Methodology
The failure analysis of the Bjork-Shiley heart valve followed a rigorous metallurgical examination protocol:
The investigation methodology began with visual inspection of explanted valves, both those that had failed and those removed for other reasons [54]. Researchers then employed scanning electron microscopy for detailed examination of fracture surfaces, revealing characteristic faceted patterns and branching cracks indicative of fatigue failure [54]. Metallographic sectioning of both failed and unused valves allowed comparison of microstructures, particularly in the weld regions [54]. This analysis identified porosity and other defects directly attributable to the welding process [54]. The fatigue analysis correlated these defects with crack initiation points, confirming that cyclic loading from normal heart function caused progressive crack propagation until catastrophic failure occurred [54].
Research Reagents and Tools for Cardiovascular Implant Analysis
The failure analysis and ongoing safety monitoring of cardiovascular implants requires specialized analytical tools:
Table 5: Essential Research Reagents and Tools for Cardiovascular Implant Analysis
| Tool/Reagent | Function | Application in Safety Analysis |
|---|---|---|
| Scanning Electron Microscope | High-resolution surface imaging | Fracture surface analysis and defect characterization |
| Metallographic Polishing Equipment | Sample preparation for microscopic analysis | Revealing microstructural features and defects |
| Fatigue Testing Apparatus | Simulating cyclic loading conditions | Accelerated life testing and failure prediction |
| Finite Element Analysis Software | Stress distribution modeling | Identifying high-stress concentrations in designs |
| Biocompatibility Testing Materials | Assessing tissue interaction | Evaluating long-term implant compatibility |
Ethical Framework and Professional Responsibilities
Connection to Biomedical Engineering Society Code of Ethics
The failures documented in both the Therac-25 and Bjork-Shiley heart valve cases highlight critical importance of formal ethical frameworks in biomedical engineering practice. The Biomedical Engineering Society (BMES) Code of Ethics establishes explicit professional obligations that directly address the types of failures observed in these cases [5]. The Code mandates that biomedical engineers "promote transparency, implement reporting systems for violations, and establish ethical decision-making models to standardize procedures" [5]. These principles directly counter the organizational deficiencies observed in both cases, where inadequate reporting structures and lack of transparency contributed to continued risks.
The BMES Code further emphasizes providing "honest and conscientious" services in technology development, with commitment to advancing public health as a primary obligation [5]. This framework establishes a professional context where safety considerations must transcend commercial pressures and where engineers bear responsibility for the long-term performance of their designs.
Barriers to Accountability in Complex Systems
Analysis of these cases reveals significant structural barriers to accountability in biomedical engineering. According to Nissenbaum (1994), four key barriers explain why responsibility is systematically undermined in computerized society [52]:
The Problem of Many Hands: Multiple individuals and groups contribute to complex systems, making it difficult to assign responsibility for failures [52]. In the Therac-25 case, software programmers, hardware engineers, and corporate management all shared some aspect of responsibility, yet no single party was clearly accountable.
The "Bugs" Justification: The appeal to inherent software bugs can mask careless programming, inadequate testing, and insufficient safety features [52]. Manufacturers of the Therac-25 initially dismissed complaints by suggesting software bugs were inevitable rather than addressing fundamental design flaws.
The Computer as Scapegoat: Blaming "the computer" rather than specific design decisions or organizational processes distracts from identifiable engineering errors [52]. Both cases demonstrate how complex technology can obscure human responsibility for failures.
Ownership Without Liability: Proprietary interests and trade secrets can impede independent safety evaluation [52]. In both cases, lack of transparency limited external oversight that might have identified problems earlier.
Modern Implications and Safety Engineering Principles
The lessons from these historical cases continue to inform modern biomedical engineering practice. Recent regulatory approvals for medical devices, such as the 2025 FDA approval of Medtronic's Evolut TAVR system for expanded Redo-TAVR indication, demonstrate increased emphasis on comprehensive clinical evidence and post-market surveillance [55]. The concurrent launch of the RESTORE study to evaluate outcomes of Redo-TAVR procedures over five years with 225 participants reflects a more rigorous approach to long-term safety assessment [55].
Current adverse event reporting systems, such as the FDA MAUDE database, continue to document device failures, including recent reports of mitral bioprosthetic valve explants due to structural deterioration and heart failure [56]. These modern surveillance mechanisms represent direct institutional responses to the reporting deficiencies identified in historical cases.
The Therac-25 and Bjork-Shiley heart valve case studies provide enduring lessons for biomedical engineering professionals. Both cases demonstrate that technical excellence must be coupled with robust ethical frameworks and organizational commitment to safety. The Therac-25 incidents highlight the dangers of over-reliance on software controls without redundant hardware safeguards, while the Bjork-Shiley valve failures illustrate the catastrophic consequences of manufacturing defects combined with inadequate response to early warning signs.
These historical failures directly informed the development of the Biomedical Engineering Society Code of Ethics, which establishes professional standards for transparency, safety prioritization, and accountability [5]. For contemporary researchers, scientists, and drug development professionals, these cases underscore the necessity of comprehensive testing regimes, transparent reporting systems, and ethical decision-making processes that prioritize patient welfare above commercial considerations. By learning from these failures, the biomedical engineering community can better fulfill its fundamental obligation to "alleviate pain, restore health, and extend life" through safely engineered medical technologies.
The dual-use dilemma represents one of the most significant ethical challenges in modern biomedical research and biotechnology. It arises when a single scientific effort or technological advancement can be applied for both beneficial and harmful purposes, creating tension between scientific progress and security responsibility. In the life sciences, research that aims to improve human health and quality of life can potentially be repurposed to harm humans, animals, or the environment [57]. This dilemma compels researchers to reflect on scientific responsibility, ethical regulation, and society's role in the governance of knowledge [57]. The convergence of artificial intelligence with biotechnology (AIxBio) has further intensified these concerns by accelerating research capabilities while simultaneously lowering barriers to potential misuse [58] [57].
The core challenge lies in preventing misuse without compromising the positive potential of scientific advancement. As researchers, our work may represent meaningful breakthroughs with no intention of causing damage, yet the dilemma emerges when secondary actors—whether individuals, political groups, or governments—repurpose that knowledge for harmful ends [57]. This perspective explores the dual-use dilemma through a technical lens, providing biomedical researchers and drug development professionals with practical frameworks for identifying, assessing, and mitigating these risks within their research programs, while aligning with the ethical expectations of the biomedical engineering community [17].
Conceptual Framework: Beyond the Dual-Use Dichotomy
Historical Context and Evolution
The concept of dual-use research is not new to science. Throughout history, both basic and applied research have contributed, sometimes inadvertently, to weapons of mass destruction [57]. Mustard gas, initially developed by Germany and used in World War I, and the atomic bombs developed from nuclear physics research demonstrate how scientific exploration can lead to devastating military applications [57]. The Soviet Union's large-scale biological weapons program from 1946 to 1992 further illustrates how biological sciences can be exploited for harmful purposes [57].
In contemporary contexts, the U.S. Government defines Dual-Use Research of Concern (DURC) as "life sciences research that, based on current understanding, can be reasonably anticipated to provide knowledge, information, products, or technologies that could be directly misapplied to pose a significant threat with broad potential consequences to public health and safety, agricultural crops and other plants, animals, the environment, materiel, or national security" [59]. This definition has been internationally adopted and forms the basis for most current regulatory frameworks [59].
From Reactive to Proactive Governance
Traditional approaches to dual-use governance have primarily focused on risk mitigation through reactive policy measures. However, emerging frameworks urge policymakers to actively champion benefits alongside mitigating risks, including through targeted investments aimed at securing public priorities [60]. This balanced approach recognizes that overly restrictive regulation may stifle innovation while insufficient oversight creates security vulnerabilities.
The situation is particularly complex in the context of AIxBio convergence, where the digitization of biology has gradually brought physical experimentation with living organisms into the cyber domain [58]. This evolution has created specific dual-use risks and accelerated others, requiring novel governance strategies that can keep pace with technological advancement [58].
Table 1: Key Historical Cases of Dual-Use Research Concern
| Case Study | Year | Beneficial Purpose | Potential Misapplication |
|---|---|---|---|
| Mousepox Virus Modification | 2001 | Pest control through induced infertility in mice | Creation of highly lethal, vaccine-resistant virus [57] |
| Artificial Synthesis of Poliovirus | 2002 | Raise awareness about synthetic biology risks | Demonstration of pathogen creation from publicly available data [57] |
| AI-Generated Molecular Compounds | 2022 | Therapeutic drug discovery | Identification of potential chemical weapons [57] |
| H5N1 Transmissibility Studies | 2010s | Pandemic preparedness research | Creation of potentially enhanced pathogens [59] |
Technical Governance Framework for AIxBio Convergence
Emerging Risk Landscape
The convergence of artificial intelligence and biotechnology represents a paradigm shift in both capabilities and risks. AI technologies are enabling faster design of vaccines, therapeutics, and diagnostics, while simultaneously potentially lowering barriers to misuse [58]. A 2023 incident illustrates this perfectly: scientists using AI models for drug development unexpectedly generated multiple compounds with potential applications as chemical weapons [57]. One researcher noted: "We were naïve in thinking about the potential misuse of our trade, as our aim had always been to avoid molecular features that could interfere with the many different classes of proteins essential to human life" [57].
This case demonstrates how AI tools, even when used in silico, may inadvertently facilitate biological or chemical misuse by making complex design processes more accessible and automated. The rapid technical developments and applications at the AIxBio intersection require sustained investment in qualitatively updating and quantitatively universalizing the implementation of technical standards—for both foundation models and AI-powered biological tools [58].
Technical Governance Recommendations
Based on expert analyses and backcasting exercises with AIxBio specialists, the following technical governance measures represent industry best practices for researchers and institutions [58]:
Comprehensive Risk Assessment: Implement processes for identifying, measuring, mitigating, monitoring, and responding to potential misuse risk, with transparent disclosure of relevant practices.
Enhanced Evaluation Protocols: Conduct comprehensive evaluations such as expert-led red teaming and human uplift studies specifically designed for AIxBio applications.
Biosecurity-Specific Testing: Combine relative capability, bottleneck, and threat simulation assessments specifically tailored for biosecurity risks.
Biological Model Oversight: Evaluate the capabilities of biological AI models and monitor the use and security practices of autonomous labs.
Data Governance: Establish data standards for biological data and monitor the types of data being collected and aggregated.
Countermeasure Development: Leverage AI for accelerating the development, manufacturing, and distribution of biological countermeasures.
Table 2: AIxBio Technical Governance Framework
| Governance Dimension | Current Best Practices | Implementation Challenges |
|---|---|---|
| Risk Identification | Misuse risk assessment frameworks combining capability, accessibility, and motivation factors | Rapidly evolving threat landscape; difficulty anticipating novel misuse vectors |
| Model Evaluation | Expert-led red teaming; human uplift studies; bottleneck analysis | Lack of standardized evaluation benchmarks; resource intensity |
| Data Security | Differential access controls; data use monitoring; synthesis screening | Balancing open science with security; international harmonization |
| Biosafety Integration | Updated biosafety levels for AI-enabled research; autonomous lab monitoring | Legacy infrastructure; adapting physical controls to digital research |
| Countermeasure Development | AI-accelerated medical countermeasure platforms; proactive defense development | Funding prioritization; platform scalability |
Dual-Use Research Oversight Workflow: This diagram illustrates the integrated oversight points within a standard research workflow where dual-use concerns must be assessed and mitigated.
Experimental Assessment Protocols and Methodologies
Case-Based Risk Analysis
Understanding dual-use risks requires examination of specific experimental contexts. The following cases represent well-documented examples where legitimate research presented significant dual-use concerns:
The Mousepox Experiment (2001): Australian researchers genetically modified the mousepox virus to express interleukin-4 (IL-4), intending to induce infertility in mice as a pest control strategy. Unexpectedly, the modified virus proved highly lethal—even in vaccinated mice [57]. The published materials and methods detailed the technical approach, raising concerns that similar techniques could engineer more virulent forms of human-affecting viruses [57].
Artificial Synthesis of Poliovirus (2002): Researchers at Stony Brook University synthesized poliovirus "from scratch" using publicly available genomic data and commercially sourced materials [57]. The resulting viable virus could paralyze and kill mice. While intended to raise awareness about synthetic biology risks, it demonstrated the feasibility of creating pathogens without natural samples [57].
AI-Accelerated Compound Design (2022): Researchers using AI models for therapeutic discovery unexpectedly generated compounds with potential chemical weapons applications [57]. This case highlighted how in silico research—operating in a virtual setting—could still produce dual-use concerns without physical materials.
Research Reagent Solutions and Essential Materials
Table 3: Research Reagents and Materials with Dual-Use Potential
| Reagent/Material | Standard Research Function | Dual-Use Concerns | Risk Mitigation Strategies |
|---|---|---|---|
| Pathogenic Viral Vectors | Gene delivery; vaccine development | Weaponization potential; enhanced pathogenicity | Tiered access controls; biosafety level compliance; institutional oversight |
| Gene Editing Systems (CRISPR-Cas9) | Functional genomics; gene therapy | Creation of harmful genetic modifications | Synthesis screening; institutional review; personnel reliability programs |
| AI-Based Drug Discovery Platforms | Accelerated therapeutic discovery | Identification of toxic compounds; molecule optimization for harm | Usage monitoring; output filtering; ethics-by-design implementation |
| Pathogen Genomic Sequences | Diagnostic development; basic research | De novo pathogen synthesis | Data access governance; sequence screening tools; responsible dissemination |
| Synthetic Biology Toolkits | Metabolic engineering; genetic circuit design | Creation of novel biological agents | Parts registry screening; institutional review; safety-by-design principles |
Implementation Framework for Research Institutions
Building a Culture of Responsibility
Strengthening institutional capacity to address dual-use concerns requires moving beyond compliance to foster a genuine culture of responsibility within the scientific community. This involves integrating dual-use consideration into the fundamental ethos of research practice, rather than treating it as an external imposition [57]. The German experience offers valuable insights, where competing suggestions have emerged between national legislation on DURC versus expanded scope for research ethics committees (RECs) drawing on scientific self-control [59].
The Biomedical Engineering Society (BMES) Code of Conduct provides a foundational ethical framework that can be extended to address dual-use concerns, emphasizing professional responsibility and harassment-free environments conducive to serious ethical consideration [17]. However, specific dual-use guidance must be developed to supplement general ethical codes.
Practical Implementation Strategy
Based on analysis of international frameworks and regional challenges, particularly in underrepresented regions like Latin America [57], the following implementation strategy provides a roadmap for institutions:
Structured Risk Assessment Protocols: Develop and implement standardized tools for identifying and evaluating dual-use potential in research proposals, including specific checklists for different research domains (synthetic biology, AI-assisted research, gain-of-function studies).
Enhanced Ethics Committee Mandates: Expand the scope of research ethics committees to explicitly include dual-use evaluation while maintaining appropriate expertise balance [59]. This requires specialized training for committee members on identifying and assessing DURC.
Researcher Education and Awareness: Integrate dual-use modules into graduate curricula and professional development programs, using case-based learning approaches with specific examples relevant to researchers' fields.
International Collaboration Mechanisms: Develop frameworks for responsible international collaboration, particularly with regions where oversight capacity may be limited, focusing on capacity building rather than restriction.
Transparent Governance Processes: Establish clear, transparent processes for reviewing and—when necessary—restricting research, with appropriate appeal mechanisms and consideration of both security concerns and academic freedom.
The dual-use dilemma presents fundamental challenges at the intersection of scientific progress, ethics, and security. As biomedical researchers and drug development professionals, we have a responsibility to proactively address these concerns while advancing knowledge for human benefit. The frameworks presented here provide practical approaches for identifying, assessing, and mitigating dual-use risks within research programs.
The convergence of AI and biotechnology represents both unprecedented opportunity and novel risks, requiring adaptive governance approaches that can evolve with technological capabilities [58]. By implementing structured assessment protocols, enhancing ethics review processes, and fostering a genuine culture of responsibility, the biomedical research community can maintain its commitment to open scientific inquiry while addressing legitimate security concerns.
Ultimately, addressing the dual-use dilemma requires recognizing that preventing the misuse of science is not opposed to scientific progress but is an essential component of responsible research practice in the 21st century. As the field continues to evolve, so too must our approaches to ensuring that beneficial research remains beneficial through its entire lifecycle of development and application.
In the high-stakes, multidisciplinary field of biomedical engineering, conflict is inevitable. Differences in professional opinion regarding device design, ethical interpretations of research protocols, and resource allocation disputes regularly arise among researchers, clinicians, and industry partners. The Biomedical Engineering Society (BMES) Code of Ethics establishes a foundation for professional conduct, but provides limited practical guidance for resolving conflicts when they emerge [17] [6]. Effective conflict resolution in this domain is not merely a matter of maintaining workplace harmony—it is an ethical imperative with direct implications for patient safety, research integrity, and public trust. When handled constructively, conflict can spark innovation and improve decision-making; when managed poorly, it can lead to catastrophic outcomes, as historical cases like the Therac-25 radiation therapy machine accidents demonstrate [5].
This technical guide provides biomedical professionals with evidence-based frameworks and methodologies for applying ethical decision-making models to complex conflict situations. By integrating the BMES Code of Ethics with established conflict resolution techniques, researchers and drug development professionals can navigate disputes in ways that uphold ethical standards while advancing scientific progress.
Ethical Foundations: Core Principles from Biomedical Engineering Ethics
The BMES Code of Ethics outlines fundamental obligations for biomedical engineers, emphasizing "honesty and conscientiousness in scientific inquiry and technology development, and to advancing public health" [5]. Several core principles from this code are particularly relevant to conflict resolution:
- Patient Safety and Risk Assessment: Design decisions must prioritize human health, requiring rigorous testing, transparency in reporting potential risks, and ongoing monitoring [5].
- Professional Responsibility: Biomedical engineers must "respect, value, and acknowledge the contribution of others" while "fostering collegial inter-disciplinary relationships" across diverse fields [6].
- Privacy and Data Security: Professionals must protect confidential information, including patient data and commercial secrets, from unauthorized access or misuse [6].
- Dual-Use Dilemmas: Researchers must consider potential misuse of biomedical technologies and implement safeguards against unethical applications [5].
These principles provide an ethical compass for navigating conflicts, ensuring resolutions align with professional obligations beyond immediate practical concerns.
Conflict Resolution Styles: Assessment and Application
Understanding individual approaches to conflict is essential for effective resolution. The Thomas-Kilmann Instrument (TKI) identifies five primary conflict resolution styles that vary along dimensions of assertiveness and cooperativeness [61]:
Table 1: Thomas-Kilmann Conflict Resolution Styles
| Style | Assertiveness | Cooperativeness | Typical Application in BME |
|---|---|---|---|
| Competing | High | Low | Essential for immediate safety issues; inappropriate for collaborative design decisions |
| Collaborating | High | High | Ideal for interdisciplinary research teams solving complex problems |
| Compromising | Moderate | Moderate | Useful for resource allocation conflicts with time constraints |
| Avoiding | Low | Low | Appropriate for trivial matters or when more information is needed |
| Accommodating | Low | High | Valuable when preserving relationships outweighs immediate concerns |
Research involving medical students reveals significant variation in conflict resolution styles across individuals and specialties. One study found accommodating was the most common style (37.0%), followed by collaborating (20.4%) and compromising (19.4%) [61]. Notably, students pursuing diagnostic specialties demonstrated higher negotiation and emotional intelligence scores than those entering procedural fields, suggesting style preferences may correlate with professional specialization [61].
Diagram 1: Conflict Resolution Styles Matrix. This diagram illustrates the relationship between the five primary conflict resolution styles based on their positions along the assertiveness and cooperativeness dimensions.
Ethical Decision-Making Frameworks for Conflict Resolution
When conflicts arise with ethical dimensions, structured frameworks help ensure resolutions align with professional standards. The Markkula Center's Framework for Ethical Decision Making provides five approaches that can be adapted for biomedical engineering contexts [62]:
The Utilitarian Approach
This approach emphasizes actions that "produce the greatest good and does the least harm for all who are affected" [62]. In biomedical conflicts, this requires systematically evaluating potential benefits and harms for all stakeholders—patients, researchers, institutions, and the public. For example, when deciding whether to delay a device launch to address safety concerns, the utilitarian approach would weigh the immediate benefits of earlier availability against potential long-term harms from insufficient testing.
The Rights Approach
This model emphasizes respect for human dignity and fundamental rights as outlined in documents like the Universal Declaration of Human Rights [62]. In biomedical contexts, this approach prioritizes patient rights to informed consent, privacy, and autonomy. When conflicts arise regarding data sharing practices, the rights approach would favor solutions that protect patient confidentiality even if they impose additional burdens on researchers.
The Justice and Fairness Approach
This perspective focuses on ensuring "benefits and burdens are distributed among society's members in ways that are fair and just" [62]. In biomedical research conflicts, this approach helps address disparities in resource allocation, access to experimental treatments, and inclusion of diverse populations in clinical trials. It provides ethical grounding for disputes about prioritizing research directions or allocating limited research funding.
The Virtue Approach
This method emphasizes actions consistent with ideal character traits for biomedical engineers, including honesty, integrity, courage, and compassion. When facing conflicts between commercial interests and scientific integrity, the virtue approach would guide professionals toward transparent reporting of all findings, including unfavorable results.
The Common Good Approach
This perspective highlights our interconnectedness within society and emphasizes solutions that benefit the community as a whole [62]. In conflicts involving intellectual property, this approach helps balance legitimate commercial interests with the broader public health benefits of making medical advancements widely available.
Experimental Protocols and Assessment Methodologies
Conflict Resolution Training Protocol
Research at West Virginia University developed an effective protocol for conflict resolution training in biomedical science graduate curricula [63]. The training employs a mixed-methods approach combining didactic instruction with interactive components spaced over time to reinforce learning:
Table 2: Conflict Resolution Training Protocol Components
| Session | Focus | Activities | Duration |
|---|---|---|---|
| Foundational Concepts | Conflict styles, negotiation principles | Didactic presentation, TKI assessment | 50 minutes |
| Communication Skills | Active listening, emotional intelligence | Role-playing, video review | 50 minutes |
| Application Exercises | Real-world BME scenarios | Faculty-facilitated simulations | 50 minutes |
| Integration Practice | Combining multiple techniques | Complex case studies, reflection | 50 minutes |
The protocol utilizes realistic conflict scenarios solicited from biomedical researchers and professionals, ensuring relevance to actual workplace situations. Role-playing exercises are particularly valuable, with participants practicing both sides of conflicts to develop empathy and perspective-taking abilities [63].
Conflict Resolution Assessment Rubric
To evaluate conflict resolution skills, Duke University researchers developed a comprehensive assessment rubric focusing on two primary domains: negotiation skills and emotional intelligence [61]:
Table 3: Conflict Resolution Skills Assessment Rubric
| Assessment Domain | Component Skills | Scoring Method | Maximum Points |
|---|---|---|---|
| Negotiation Skills | Identify/acknowledge problem; Break problem into pieces; Acknowledge shared goal; Summarize mutually acceptable plan | Four 10-point assessments | 40 |
| Emotional Intelligence | Listening ability; Acknowledging concerns; Asking effective questions; Appropriate body language; Patient-centered communication | Six 100-point assessments | 600 |
| Entrustability | Readiness for collaborative teamwork | Based on AAMC EPA #9 behaviors | Categorical |
This assessment tool enables standardized evaluation of conflict resolution capabilities, with inter-rater reliability established through calibration exercises [61].
Diagram 2: Conflict Resolution Training and Assessment Workflow. This diagram outlines the sequential protocol for developing and evaluating conflict resolution skills through simulation-based training.
Research Reagents and Methodological Tools
Table 4: Essential Methodological Tools for Conflict Resolution Research
| Tool/Instrument | Primary Function | Application in BME Research | Validation |
|---|---|---|---|
| Thomas-Kilmann Instrument (TKI) | Assesses individual conflict resolution styles | Understanding team dynamics in research collaborations | Widely validated in professional populations [61] |
| Negotiation Skills Assessment | Measures problem-solving and agreement-building capabilities | Evaluating effectiveness in resolving scientific disputes | Rubric validated with inter-rater reliability measures [61] |
| Emotional Intelligence Evaluation | Assesses interpersonal awareness and communication skills | Improving collaborative relationships in multidisciplinary teams | Adapted from AAMC Entrustable Professional Activities [61] |
| Scenario-Based Simulations | Provides realistic practice environments | Developing conflict competence in low-stakes settings | Scenarios derived from actual BME workplace conflicts [63] |
| Structured Reflection Exercises | Facilitates integration of learning experiences | Reinforcing conflict resolution principles after real incidents | Incorporated into graduate curricula with demonstrated efficacy [63] |
Case Study: Applying Ethical Frameworks to a Biomedical Engineering Conflict
Consider a conflict within a medical device development team: Engineers have identified a potential safety issue in a newly designed insulin pump several months before planned commercialization. The business team emphasizes the devastating financial impact of delay and questions the clinical significance of the finding.
Framework Application
- Utilitarian Analysis: Weigh the potential harm to patients from the safety issue against the benefits of earlier availability and financial stability that supports ongoing research. A delayed launch with modifications likely produces the greatest net good [62].
- Rights Analysis: Patients have a right to safe medical devices. Their right to bodily integrity outweighs the company's financial interests [62].
- Virtue Analysis: The virtues of integrity, honesty, and courage support transparent communication about the safety issue and delay until resolved, despite business pressure [62].
- BMES Code Application: The BMES requirement to "respect human dignity and privacy of patients" and ensure "proper safeguarding" supports prioritizing safety over commercial considerations [6].
Resolution Strategy
A collaborative approach would involve all stakeholders in problem-solving: engineers could propose specific design modifications, while business representatives develop contingency plans. This strategy acknowledges shared interests in both patient safety and commercial success, creating space for creative solutions that address both concerns [63].
Implementation Guidelines for Biomedical Organizations
Successful integration of ethical conflict resolution practices requires systematic organizational support:
- Structured Training Programs: Implement mandatory conflict resolution training in graduate biomedical curricula and continuing professional education, using the protocols outlined in Section 5 [63].
- Leadership Modeling: Senior researchers and managers should visibly model effective conflict resolution behaviors and ethical decision-making frameworks.
- Institutional Support Systems: Establish clear reporting mechanisms for ethical concerns and provide access to neutral mediators for complex conflicts [17].
- Assessment and Reinforcement: Regularly assess conflict resolution capabilities using validated tools and provide opportunities for skill refinement through refresher training.
The BMES Code of Ethics states that members should "promote a culture of knowledge exchange and mentorship" while "avoiding or properly disclosing conflicts of interest" [6]. These principles naturally extend to creating environments where conflicts are addressed constructively rather than suppressed or avoided.
Ethical conflict resolution in biomedical engineering requires both technical understanding of conflict dynamics and firm grounding in professional ethics. By integrating the BMES Code of Ethics with evidence-based conflict resolution frameworks, biomedical professionals can transform potentially destructive conflicts into opportunities for ethical clarification, innovation, and improved patient outcomes. The structured approaches, assessment methodologies, and implementation strategies presented in this guide provide a foundation for building these essential capabilities throughout the biomedical engineering community.
Ethical courage is the courage to act according to one's own ethical values and principles despite the risk of negative consequences [64]. In biomedical engineering, where research and devices directly impact human health, this virtue is paramount for ensuring patient safety and upholding scientific integrity. The field's unique position—bridging cutting-edge technological innovation with fundamental healthcare needs—creates an environment where professionals frequently encounter ethical challenges, from research misconduct and safety violations to data manipulation and dual-use dilemmas.
The Biomedical Engineering Society (BMES) Code of Ethics establishes the normative framework for professional conduct, emphasizing honesty in scientific inquiry, responsible technology development, and the paramount importance of advancing public health [5]. Within this context, "whistleblowing" is defined as a three-phased process: (1) observing or suspecting wrongdoing, (2) addressing the act internally or externally to parties capable of ending it, and (3) potentially facing consequences such as retaliation or discrimination [64]. This guide provides a strategic framework for cultivating the ethical courage necessary to navigate this complex landscape, resist inappropriate external pressures, and implement effective, protected whistleblowing processes when necessary.
Quantitative Foundations of Moral Courage
Understanding the evidence-based profile of potential whistle-blowers and their moral courage provides a scientific foundation for developing supportive interventions. A 2022 study of 454 healthcare professionals offers crucial quantitative insights into the moral courage of those willing to report wrongdoing [64].
Table 1: Moral Courage Metrics of Potential Whistle-blowers
| Metric Description | Scale Used | Mean Score | Interpretation |
|---|---|---|---|
| Overall Moral Courage | Visual Analogue Scale (0-10) | 8.55 | High self-assessed moral courage |
| Composite Moral Courage | 5-point Likert Scale (Nurses Moral Courage Scale) | 4.34 | High level across multiple dimensions |
| Compassion and True Presence | 5-point Likert Sub-scale | N/A | Courage to overcome personal fears to encounter patient suffering |
| Moral Responsibility | 5-point Likert Sub-scale | N/A | Feeling responsible for others and confident in one's ethical principles |
| Moral Integrity | 5-point Likert Sub-scale | N/A | Acting according to personal and professional values |
| Commitment to Good Care | 5-point Likert Sub-scale | N/A | dedication to providing quality care |
The study further identified specific background variables significantly associated with higher moral courage, highlighting potential leverage points for fostering ethical resilience.
Table 2: Variables Associated with Increased Moral Courage
| Variable Category | Specific Factors | Significance for Ethical Courage |
|---|---|---|
| Socio-demographics | Older age, Specific gender associations (findings mixed across studies) | Experience and maturity may bolster ethical resolve |
| Education | Additional ethics education, Higher level of education, Previous healthcare degree | Knowledge builds confidence in identifying and addressing ethical breaches |
| Work Experience | Management position, Longer work experience | Authority and repeated exposure to ethical dilemmas strengthen moral muscle |
| Personality & Responsibility | Frequent encounter with ethical situations, Career commitment, Social responsibility | Practice and a deep-seated sense of duty reinforce courageous action |
The Psychological Landscape of Whistleblowing
The decision to blow the whistle is a profound psychological journey, marked by powerful drivers and significant barriers. Understanding this internal landscape is essential for preparing to act courageously.
Key Psychological Drivers
- Moral Development and Core Values: Individuals at higher stages of principled reasoning are more likely to act based on universal ethical principles like justice and human rights, even against organizational norms. A strong moral identity—where morality is central to self-concept—makes individuals more likely to perceive unethical behavior as a personal affront requiring action [65].
- Cognitive Dissonance: Remaining silent while observing wrongdoing creates psychological discomfort (cognitive dissonance) for those with strong ethical standards. Whistleblowing becomes a mechanism to align actions with one's moral compass and reduce this distress [65].
- Empathy and Perspective-Taking: The ability to understand and share the feelings of potential victims of the wrongdoing creates a powerful moral imperative to intervene. This empathetic response is a key motivator for many whistleblowers [65].
- Professional Duty and Social Responsibility: Many biomedical engineers feel bound by the BMES Code of Ethics and a broader duty to society. This sense of responsibility can override personal risk, especially when public health and safety are at stake [6] [65].
Significant Psychological Barriers
- Fear of Retaliation: This is the most significant barrier. Retaliation can include job loss, social ostracism, damage to reputation, legal action, and psychological harassment. The threat is often very real and justified, creating a powerful deterrent [65] [66].
- The Bystander Effect: In organizational settings, the sense of personal responsibility can be diffused among multiple individuals aware of the misconduct. Each person assumes someone else will act, leading to collective inaction [65].
- Conformity and Groupthink: The human need for acceptance and the pressure to conform to group norms can suppress concerns about unethical practices. In close-knit teams, groupthink can discourage dissenting opinions [65] [66].
- Normalization of Deviance: Repeated exposure to minor ethical lapses can desensitize individuals, making increasingly serious violations appear normal over time. This gradual erosion of ethical standards is a dangerous psychological process [65].
Diagram 1: The Internal Ethical Decision-Making Process of a Potential Whistle-blower.
Experimental Protocols for Studying Ethical Decision-Making
Research into moral courage and whistleblowing utilizes rigorous methodologies to understand these complex phenomena. The following protocol, adapted from a 2022 study, provides a template for investigating ethical decision-making in controlled settings [64].
Video Vignette Methodology for Whistleblowing Research
Objective: To measure participants' likelihood of blowing the whistle and their level of moral courage in response to a standardized wrongdoing scenario.
Materials and Reagents:
- Video Vignette: A professionally scripted and produced video depicting a clear ethical violation in a biomedical research or clinical setting (e.g., data fabrication, safety protocol violation, patient consent oversight).
- Validated Psychometric Scale: The Nurses Moral Courage Scale (NMSC) or an adapted version for engineers, containing 21 items across four dimensions (Compassion, Moral Responsibility, Moral Integrity, Commitment to Good Care) on a 5-point Likert scale [64].
- Demographic and Background Questionnaire: Capturing socio-demographics, education, work experience, and personality traits.
- Visual Analogue Scale (VAS): A single 0-10 scale for overall self-assessment of moral courage.
- Open-Ended Response Field: For participants to describe their intended actions and reasoning regarding the vignette.
Procedure:
- Participant Recruitment: Recruit a random sample of biomedical engineers and researchers from professional society membership databases. Obtain informed consent.
- Power Analysis: Conduct a statistical power analysis a priori to determine the required sample size (e.g., n=380 for 95% confidence level, p<0.05).
- Exposure and Response: Participants view the video vignette and subsequently complete the questionnaire package containing the NMSC, VAS, demographic questions, and the open-ended question about the vignette.
- Data Segmentation: Identify "Potential Whistle-blowers" (PW-Bs) from the open-ended responses. Inclusion criteria: the narrative must describe both (a) observing the wrongdoing in the vignette, and (b) an intention to act by blowing the whistle.
- Data Analysis:
- Quantitative: Perform descriptive statistics on NMSC and VAS scores. Use correlational analyses (e.g., ANOVA, regression) to examine associations between moral courage scores and background variables.
- Qualitative: Analyze open-ended narratives using inductive content analysis to identify themes in reasoning, perceived barriers, and intended reporting pathways.
Table 3: Research Reagent Solutions for Ethical Decision-Making Studies
| Reagent/Material | Function in the Experiment | Key Characteristics |
|---|---|---|
| Scripted Video Vignette | Standardized ethical stimulus | High realism, clear ethical breach, controlled for confounding variables |
| Nurses Moral Courage Scale (NMSC) | Quantifies moral courage | 21-item, 4-dimension, 5-point Likert scale; validated reliability and internal consistency |
| Visual Analogue Scale (VAS) | Global assessment of moral courage | Single-item, 0-10 scale; provides a quick, overarching self-assessment |
| Demographic Questionnaire | Captures participant background variables | Includes socio-demographics, education, work experience, and personality measures |
A Strategic Framework for Ethical Action and Whistleblowing
Preparing to act ethically requires a proactive, systematic approach. The following strategies are designed to help biomedical engineers build resilience and navigate the process of reporting wrongdoing.
Pre-Emptive Strategies: Building an Ethical Foundation
- Pursue Continuous Ethics Education: Engage in formal and informal ethics training. Studies show that additional ethics education is significantly associated with higher moral courage [64]. This builds confidence in identifying and articulating ethical issues.
- Cultivate Moral Integrity: Reflect on and solidify your personal and professional value base. Morally courageous individuals are confident in their ethical principles and feel a responsibility for the welfare of others, which empowers them to act [64].
- Understand Legal and Ethical Frameworks: Familiarize yourself with the BMES Code of Ethics, which emphasizes honesty in scientific inquiry, protecting confidential information, and reporting results with integrity [6]. Furthermore, know the relevant whistleblower protection laws (e.g., the False Claims Act, SEC programs) which can offer anonymity and protection from retaliation, though they form a complex legal maze [66].
- Document Meticulously: Maintain detailed, date-stamped records of research procedures, data, and communications. In the event of a dispute, contemporaneous documentation is invaluable evidence.
The Whistleblowing Process: A Step-by-Step Guide
When wrongdoing is suspected, a deliberate and informed approach is critical.
Diagram 2: The Escalating Pathway for Protected Whistleblowing.
Step 1: Observe and Verify
- Objectively identify the wrongdoing, distinguishing fact from assumption. Refer to the BMES Code of Ethics and other relevant guidelines to confirm the violation [6] [5].
- Gather factual evidence discreetly and ethically, without violating privacy laws or accessing materials improperly [66].
Step 2: Internal Consultation and Reporting
- Consult a trusted mentor or confidential advisor. Many organizations have ombudspersons or ethics helplines.
- Report internally first, if feasible and safe. This follows the principle of addressing issues at the lowest level possible and allows the organization to self-correct. The BMES Code of Conduct for its conferences explicitly provides a mechanism for reporting violations to conference chairs or via a dedicated email (e.g.,
conduct@bmes.org) [17].
Step 3: External Reporting
- Escalate to external authorities if internal reporting fails or is not an option. This is necessary for severe violations or if you fear internal retaliation.
- Understand the specific legal protections and reward programs for different sectors (e.g., SEC for securities fraud, FDA for device safety). "There are over 50 whistleblower protection laws in the private sector, and they are all different," making legal advice crucial at this stage [66].
Step 4: Manage the Personal Impact
- Seek psychological and legal support. The journey can be isolating and stressful, leading to anxiety, depression, and trauma [65].
- Rely on personal and professional support networks. The emotional toll is heavy, and a strong support system is vital for resilience.
Fostering a Culture of Ethical Courage in Organizations
Leadership plays a decisive role in whether ethical courage can flourish.
- Lead by Example: Organizational leaders must model ethical behavior themselves. Their commitment sets the tone and influences what subordinates perceive as acceptable [66].
- Promote Psychological Safety: Create an environment where employees feel safe to raise concerns without fear of retribution. This involves penalizing wrongdoing and rewarding ethical behavior [66].
- Value Process over Outcome: Avoid creating excessive pressure to meet goals at all costs, as seen in the Wells Fargo scandal. Leaders must emphasize that ethical processes are more important than favorable outcomes [66].
- Encourage Diverse Viewpoints: Hire from diverse backgrounds and networks to ensure the organization isn't an echo chamber. This "ensures that people in the organization aren't dependent on that one job or organization" and reduces social pressure to conform unethically [66].
Championing ethical courage in biomedical engineering is not a solitary endeavor but a collective responsibility. It requires a solid foundation of personal integrity, reinforced by continuous ethics education and a clear understanding of professional codes and legal protections. The quantitative evidence shows that potential whistle-blowers are typically highly morally courageous individuals, and this courage can be cultivated.
Biomedical engineers must be prepared to navigate the complex psychological and practical landscape of resisting external pressure and reporting wrongdoing. By adopting a strategic, informed approach and leveraging available resources—from the BMES Code of Ethics to confidential reporting channels and legal protections—professionals can fortify themselves to act courageously. Ultimately, fostering a culture where ethical courage is expected, supported, and celebrated is the most effective strategy for safeguarding scientific integrity and public health.
In the multidisciplinary field of biomedical engineering, where research and development directly impact human health, ethical considerations are paramount [5]. The Biomedical Engineering Society (BMES) Code of Ethics outlines norms and obligations required to fulfill a biomedical engineer's commitment to honesty and conscientiousness in scientific inquiry and technology development, with the ultimate goal of advancing public health [5]. Within this ethical framework, Institutional Review Boards (IRBs) serve as a critical safeguard, ensuring that research involving human subjects adheres to both regulatory requirements and fundamental ethical principles.
An IRB is an appropriately constituted group formally designated to review and monitor biomedical research involving human subjects [67]. These committees hold authority to approve, require modifications to secure approval, or disapprove research, providing independent oversight to protect the rights and welfare of people who participate in research studies [67] [68]. For biomedical engineers developing new medical devices, diagnostic technologies, or therapeutic interventions, understanding and engaging with the IRB process is not merely a regulatory hurdle but a fundamental component of ethical research practice and professional responsibility [5].
Historical Context and Regulatory Framework
Evolution of Research Ethics
The development of modern research ethics and IRB systems emerged from historical events where human subjects were exploited in research:
- The Nuremberg Code (1947): Established in response to Nazi medical experimentation, this was the first international document outlining ethical research principles, emphasizing voluntary consent and the right to withdraw from research [69].
- Declaration of Helsinki (1964): Developed by the World Medical Association, this set forth additional principles for biomedical research involving human subjects and has been revised multiple times to address evolving ethical challenges [69].
- The Tuskegee Syphilis Study (1932-1972): This U.S. Public Health Service study withheld effective treatment from Black men with syphilis without their consent, leading to public outrage and ultimately to formal regulations governing human subjects research [70].
- The Belmont Report (1979): This foundational document outlined three core ethical principles for research: respect for persons, beneficence, and justice [69] [70].
Regulatory Foundations
In the United States, the National Research Act of 1974 formally created the IRB system [68]. Today, IRB operations are governed by federal regulations, primarily:
- The Common Rule (45 CFR 46): The Federal Policy for the Protection of Human Subjects that outlines criteria and mechanisms for IRB review [71]
- FDA Regulations (21 CFR 50, 56): Specifically govern research involving FDA-regulated products such as drugs, devices, and biologics [67] [68]
Table: Historical Milestones in Research Ethics
| Year | Document/Event | Significance |
|---|---|---|
| 1947 | Nuremberg Code | First international ethical guidelines emphasizing voluntary consent |
| 1964 | Declaration of Helsinki | Ethical principles for physician-researchers, regularly updated |
| 1974 | National Research Act | Formally established IRB system in the United States |
| 1979 | Belmont Report | Defined respect for persons, beneficence, and justice as ethical foundations |
IRB Composition and Structure
Membership Requirements
Federal regulations mandate that IRBs maintain diverse membership to ensure comprehensive review of research protocols [67] [70]. The specific requirements include:
- Minimum of five members with varying backgrounds [67] [70]
- At least one scientist member with primary concerns in scientific areas [67]
- At least one non-scientist member with primary concerns in non-scientific areas [67]
- At least one member not affiliated with the institution [67] [70]
- Members with sufficient qualifications and diversity of experience to protect participants' rights and welfare [70]
- Representation of both sexes and multiple professional disciplines [70]
- Knowledge about vulnerable populations regularly involved in research [70]
Practical Operations
IRBs function through convened meetings where a quorum (majority of members) must be present for official actions [70]. Members with conflicts of interest must abstain from review of specific protocols where such conflicts exist [67]. IRBs may use alternate members who are formally appointed and listed on the membership roster to maintain consistency when primary members are unavailable [67].
Table: IRB Membership Composition Requirements
| Member Type | Role and Responsibilities | Regulatory Reference |
|---|---|---|
| Scientific Member | Reviews methodological rigor, risk-benefit assessment of procedures | 21 CFR 56.107(c) [67] |
| Non-Scientific Member | Assesses participant burden, consent clarity, community perspectives | 21 CFR 56.107(c) [67] |
| Unaffiliated Member | Represents community values and interests, provides independent perspective | 21 CFR 56.107(c) [67] |
| Vulnerable Populations Expert | Ensures adequate protections for potentially vulnerable groups | 45 CFR 46.107 [70] |
IRB Review Categories and Processes
Levels of Review
IRBs classify research into three review categories based on risk level and regulatory criteria [70] [72] [71]:
Exempt Review
Research activities that pose no more than minimal risk and fall into specific exemption categories may be eligible for exempt status [70] [71]. Examples include:
- Research using educational tests, surveys, interviews, or observation of public behavior [71]
- Retrospective studies using data initially collected for non-research purposes [70]
- Research involving benign behavioral interventions [71]
Although termed "exempt," these studies still require IRB determination of exempt status; researchers cannot self-determine exemption [70] [72].
Expedited Review
Research involving no more than minimal risk that fits specific regulatory categories qualifies for expedited review [70] [71]. Key characteristics:
- Reviewed by a designated IRB member rather than the full committee [70]
- Prospective data collection typically required [70]
- Informed consent usually required unless waiver granted under specific circumstances [70]
- Includes categories such as blood sampling, moderate exercise, biomedical data collection [71]
Full Board Review
Research involving more than minimal risk requires review by the fully convened IRB [70] [72]. This category includes:
- Studies using investigational drugs or devices [72]
- Research involving invasive procedures [72]
- Studies with vulnerable populations (children, prisoners, pregnant women) [70]
- Research involving general anesthesia or sedation [70]
Full board reviews occur at scheduled meetings and require annual continuing review to assess progress, adverse events, and ongoing ethical justification [70].
IRB Review Criteria
For research approval, IRBs must ensure that specific regulatory criteria are met [70]:
- Risks minimized and reasonable in relation to anticipated benefits
- Equitable subject selection with consideration for vulnerable populations
- Informed consent obtained and documented appropriately
- Adequate monitoring and data confidentiality plans established
- Additional safeguards for vulnerable populations implemented
Special Considerations for Biomedical Engineering Research
Biomedical Device and Technology Protocols
Biomedical engineering research presents unique considerations for IRB review, particularly in device development and testing:
- Early-stage feasibility studies often involve higher risk profiles requiring full board review [5]
- Iterative design modifications necessitate careful amendment procedures and re-review [71]
- Dual-use dilemmas where technologies could be misused require additional risk-benefit analysis [5]
Historical cases like the Therac-25 radiation therapy machine and Bjork-Shiley heart valve failures underscore the critical importance of rigorous safety review in biomedical engineering [5].
Data Security and Privacy Considerations
Biomedical engineering increasingly involves digital health technologies, artificial intelligence, and sensitive health data, creating unique privacy challenges [5] [73]. Key considerations include:
- Cybersecurity protections for connected medical devices [5]
- De-identification protocols for biomedical data [73]
- Third-party data sharing agreements and limitations [73]
- Compliance with HIPAA and data protection regulations [73]
The Facebook emotional contagion study and OkCupid data scraping cases demonstrate the ethical consequences of inadequate data oversight [73].
The Researcher's Toolkit: IRB Protocol Components
Essential Documentation
Preparing a complete IRB submission requires careful attention to documentation. Key elements include:
Table: Essential IRB Submission Components
| Document | Purpose and Function | Key Considerations |
|---|---|---|
| Research Protocol | Detailed study plan including background, objectives, methodology, and statistical analysis | Must demonstrate scientific validity and ethical design [70] |
| Informed Consent Forms | Documents process of informing participants about study procedures, risks, benefits, and alternatives | Must be understandable to participant population; requires IRB approval of language and format [67] |
| Investigator CV and Credentials | Demonstrates researcher qualifications to conduct proposed study | Particularly important for device trials requiring technical expertise [68] |
| Recruitment Materials | Advertisements, scripts, and letters used to recruit participants | Must be approved by IRB to ensure non-coercive and appropriate content [72] |
| Data Collection Instruments | Surveys, interview guides, case report forms, data extraction tools | IRB reviews for potential risks, burden, and privacy implications [72] |
Informed Consent Process
The informed consent process is foundational to ethical research and requires more than just a signature on a form [5] [69]. Key elements include:
- Clear explanation of research procedures and purposes [69]
- Description of foreseeable risks and discomforts [67]
- Description of potential benefits to subjects or others [67]
- Appropriate alternatives to participation [67]
- Compensation for injury statements when research involves more than minimal risk [67]
- Voluntary participation and right to withdraw without penalty [69]
For biomedical engineering research, special attention should be paid to explaining technical procedures in layperson's terms and addressing long-term risks of device implantation or novel technologies [5].
Training and Compliance Requirements
Researchers engaging with human subjects must complete required training and maintain compliance throughout the study:
- CITI Program Training: The Collaborative Institutional Training Initiative provides certification in human subjects research protections; refresher courses required every three years [70] [71]
- Protocol Adherence: Researchers must follow approved protocols exactly; any changes require amendment submission and approval before implementation [71]
- Adverse Event Reporting: Unanticipated problems, protocol violations, or data breaches must be reported promptly to the IRB [71]
- Continuing Review: For ongoing studies, progress reports must be submitted according to IRB schedule (typically annual for full-board reviews) [70]
Emerging Trends and Future Directions
Evolving Oversight Models
IRB systems are adapting to changing research paradigms, including:
- Single IRB Mandate: Increasing use of single IRB review for multi-center studies to improve efficiency and consistency [70]
- Commercial Sector Engagement: Growing recognition that industry-led research requires ethical oversight similar to academic research [73]
- Limited IRB Review: New category for certain exempt research involving identifiable data to safeguard privacy and confidentiality [70]
Technological Challenges
Biomedical engineers face emerging ethical challenges in areas such as:
- Bioengineered organs and tissues requiring ethical frameworks for creation and transplantation [5]
- Artificial intelligence and machine learning applications in diagnostic and therapeutic devices [73]
- Digital health technologies collecting continuous physiological data [73]
- Gene editing technologies with profound ethical implications [5]
These developments require parallel establishment of ethical frameworks to guide responsible innovation in biomedical engineering [5].
For biomedical engineering researchers, engagement with IRB oversight is not merely a regulatory requirement but a fundamental component of ethical practice and professional responsibility. The BMES Code of Ethics emphasizes transparency, reporting systems for violations, and ethical decision-making models [5]. By understanding the historical context, regulatory framework, and practical operations of IRBs, biomedical engineers can more effectively navigate the review process while upholding their commitment to protecting human subjects and advancing public health through responsible innovation. As biomedical technologies continue to evolve, the partnership between researchers and oversight bodies will remain essential for maintaining public trust and ensuring that technological progress aligns with ethical principles.
Ensuring Compliance and Excellence: Validation Through Education and Professional Enforcement
The rapidly evolving landscape of biomedical technology brings profound ethical questions to the forefront of innovation. Biomedical engineering (BME) stands at the intersection of technological advancement and human wellbeing, requiring practitioners to navigate complex moral terrain alongside technical challenges. Historically, ethics education in engineering programs was often peripheral, but the high-stakes nature of medical technology has accelerated its integration into core curricula [74]. This transformation responds to the recognition that ethical considerations are not secondary concerns but fundamental components of responsible innovation in healthcare technologies [20].
The convergence of advanced technologies like artificial intelligence, gene editing, and neural interfaces with human biology creates unprecedented ethical dilemmas that today's biomedical engineers must be prepared to address [74]. From patient safety and data privacy to equitable access and cultural sensitivity, the ethical dimensions of BME are expanding in scope and complexity. This article examines how contemporary academic programs are systematically embedding ethics education into biomedical engineering curricula, moving beyond theoretical appendages to create integrated, pedagogically sophisticated approaches that prepare students for the moral responsibilities of the profession [20].
Curricular Frameworks and Models of Integration
Foundational Principles and Emerging Educational Paradigms
Biomedical engineering education increasingly structures ethics instruction around core principles that reflect the field's unique responsibilities. These principles include patient autonomy, beneficence, non-maleficence, justice, and accountability [74]. These foundational concepts form the ethical bedrock upon which technical competencies are built, ensuring that engineers consider the human impact of their designs from conception through implementation.
Modern BME programs employ diverse educational frameworks to translate ethical principles into professional practice. One emerging model proposes five synergistic pillars for ethics integration: (1) ethics fundamentals for professional practice, (2) safety principles for medical devices, (3) sustainability considerations, (4) technological equity and universal healthcare, and (5) ethics applied to future research challenges [20]. This comprehensive approach recognizes that ethical reasoning must permeate multiple dimensions of biomedical engineering practice rather than being confined to isolated considerations.
Table: Five-Pillar Framework for Ethics Integration in BME Education
| Pillar | Core Focus | Sample Educational Activities |
|---|---|---|
| Ethics Fundamentals | Basic principles of justice, beneficence, non-maleficence, accountability | Theoretical-practical courses, guided debates, case study analyses [20] |
| Safe Medical Devices | "Do no significant harm" principle, risk-benefit analysis | Hands-on activities in project-based courses, regulatory standard applications [20] |
| Sustainable Technologies | Environmental impacts, life cycle analyses | Problem- and project-based learning, environmental impact reporting [20] |
| Technological Equity | Affordable medical technologies, universal healthcare | International educational initiatives, open-source medical device cocreation [20] |
| Future Research Ethics | Emerging technologies, ELSI considerations | Multistakeholder analyses, seminars with industry partners [20] |
Quantitative Analysis of Ethics Integration Approaches
A comparative analysis of ethics integration methods reveals distinct pedagogical strategies with varying implementation challenges and learning outcomes. The data demonstrates a shift from traditional lecture-based formats toward experiential, embedded approaches that contextualize ethical reasoning within technical practice.
Table: Comparative Analysis of Ethics Integration Methods in BME Curricula
| Integration Method | Implementation Level | Key Advantages | Notable Examples |
|---|---|---|---|
| Dedicated Ethics Courses | Comprehensive, structured | Systematic coverage of ethical frameworks | Johns Hopkins PhD course on Ethical Challenges [75] |
| "Ethics Everywhere" Embedded Model | Distributed across curriculum | Contextualized learning, immediate relevance | Duke University BEETL program [76] |
| Case-Study Integration | Modular within technical courses | Concrete application to real-world scenarios | Therac-25, Bjork-Shiley valve analyses [5] |
| Project-Based Learning | Capstone courses, design projects | Hands-on ethical decision-making | CDIO-style experiences, business plan development [20] |
| Faculty-Led Module Approach | Topic-specific interventions | Diverse expertise, focused dilemmas | Neural prosthetics, device obsolescence modules [75] |
Experimental Protocols in Ethics Education
Case Study Analysis Methodology
Case study analysis represents a cornerstone methodology in BME ethics education, providing students with structured approaches to dissecting complex real-world ethical dilemmas. The protocol typically begins with case selection, prioritizing historically significant incidents with clear ethical dimensions and documented outcomes, such as the Therac-25 radiation therapy machine failures that resulted from software errors [74] or the Bjork-Shiley heart valve case where continued marketing despite known defects led to patient fatalities [5].
The analytical phase employs a systematic framework that examines: (1) technical factors and design decisions, (2) organizational dynamics and pressure points, (3) regulatory and oversight mechanisms, (4) stakeholder perspectives and impacts, and (5) alternative scenarios and preventive measures. Students document their analysis using structured templates that identify ethical conflicts, map decision pathways, and articulate the relationship between technical choices and ethical consequences. Assessment typically involves written reports and group presentations that emphasize clear reasoning, consideration of multiple viewpoints, and connection to established ethical frameworks and professional codes [5].
Focus Group Protocol for Ethical Technology Design
The Applied Biomedical and Signal Processing Intelligent e-Health Lab at the University of Warwick developed a comprehensive focus group protocol to integrate stakeholder perspectives into the ethical design of well-being technologies [77]. This methodology engages students in direct ethical inquiry while collecting valuable data for responsible technology development.
The protocol implementation occurs in four distinct phases. In the background phase, researchers conduct preliminary ethical reviews, consult with domain experts (including mental health professionals), and secure formal approval from the Biomedical and Scientific Research Ethics Committee. The study protocol design phase involves developing well-being questionnaires with psychology experts and creating recruitment materials that emphasize informed consent and voluntary participation [77].
The focus group phase employs structured sessions with peer moderators to encourage open discussion, using digital polling tools for real-time data collection on participant perspectives. Sessions explore macro areas including: (1) conceptualizations of well-being, (2) tracking preferences and privacy concerns, (3) evaluation of monitoring services, (4) data collection methods and frequencies, and (5) university role in well-being support [77]. The final data management phase establishes secure repositories and analytical procedures that maintain confidentiality while enabling meaningful analysis of ethical preferences and concerns.
Modular Course Design for Ethical Challenges
Johns Hopkins University developed an innovative modular approach to ethics education in its Biomedical Engineering PhD program [75]. This protocol structures ethics instruction as a semester-long course composed of faculty-led modules, each addressing distinct ethical gray areas in biomedical engineering research and practice.
The implementation begins with faculty identification of ethical challenges within their subdisciplines, resulting in diverse modules including "Technical, social, regulatory and ethical decisions involving life saving devices," "Bioethics and biosecurity challenges for protein engineering," "Rights vs ownership of genes and germline," "Biomedical device obsolescence," and "Neural prosthetics" [75]. Each module follows a standardized structure: a 15-minute introductory lecture establishing the ethical landscape, 45 minutes of small-group discussion facilitated by faculty or teaching assistants, 20 minutes of reconvened sharing of perspectives, and 10 minutes of concluding reflections.
The discussion methodology employs structured questioning sequences that move from general principles to specific applications. For example, in modules addressing data ethics, questions progress from examining assumptions about data objectivity to analyzing specific methodological choices in published studies and their ethical implications [75]. Assessment emphasizes participation quality and critical reflection rather than correct answers, creating what developers term "a space of learning, not judgement" where students practice navigating ethical uncertainty.
Analytical Frameworks and Implementation Tools
The effective integration of ethics into biomedical engineering practice requires both conceptual frameworks and practical implementation tools. This research toolkit provides essential resources for identifying, analyzing, and resolving ethical challenges in BME research and development.
Table: Essential Research Reagent Solutions for BME Ethics Integration
| Tool Category | Specific Resource | Function & Application |
|---|---|---|
| Regulatory Frameworks | FDA device classification system [74] | Guides safety requirements and approval pathways for medical devices |
| International Standards | ISO quality and safety standards [74] | Provides internationally recognized benchmarks for device manufacturing |
| Oversight Mechanisms | Institutional Review Boards (IRBs) [74] [5] | Ensures ethical treatment of human subjects in research |
| Professional Codes | BMES Code of Ethics [5] | Establishes professional norms and accountability standards for practitioners |
| Assessment Tools | Life cycle analysis protocols [20] | Evaluates environmental impact and sustainability of biomedical technologies |
| Risk Analysis Models | Risk-benefit ratio frameworks [20] | Quantifies and compares potential harms and benefits of biomedical interventions |
| Equity Assessment Tools | Accessibility and affordability metrics [74] [5] | Measures distribution of technology benefits across diverse populations |
| Data Ethics Protocols | Encryption and access control systems [5] | Protects patient privacy and secures sensitive health information |
Signature Pedagogies for Character Development
Beyond analytical tools, effective ethics education employs distinctive pedagogical approaches that develop the intellectual habits and character traits essential for ethical reasoning in biomedical engineering. Duke University's BEETL program exemplifies this approach through its "Ethics Everywhere" initiative, which weaves ethical reflection throughout courses, labs, and co-curricular experiences rather than compartmentalizing it [76].
These signature pedagogies emphasize the cultivation of specific character traits including intellectual humility, epistemic curiosity, and empathetic leadership [76]. Through team-based learning environments that mirror professional practice contexts, students develop the capacity for perspective-taking, collaborative problem-solving, and accountable decision-making. Assessment strategies focus on growth in ethical reasoning competencies rather than knowledge acquisition alone, using reflective portfolios, ethical design journals, and team process analyses to document development. These approaches recognize that ethical practice requires not just analytical frameworks but cultivated dispositions that enable engineers to navigate the moral complexities of healthcare technology innovation.
Implementation Challenges and Future Directions
Despite growing recognition of its importance, integrating ethics meaningfully into BME curricula faces significant challenges. Research with molecular systems engineering scientists reveals that many view ethical reflection as peripheral to their work, relevant only at clinical translation stages rather than throughout the research process [78]. Some researchers describe their work as "too early" for ethical consideration or "not examining anything living" and therefore outside ethical scrutiny, while others perceive ethics as territory for specialized experts rather than a shared responsibility [78].
Addressing these barriers requires both cultural and structural changes within BME education. Culturally, programs must normalize ethical reflection as a core engineering competency rather than an ancillary concern. Structurally, institutions must provide faculty development opportunities that equip technical instructors to facilitate ethical discussions and assess ethical reasoning [20]. Future directions include expanding interdisciplinary collaboration with ethics specialists, developing more sophisticated assessment tools for ethical reasoning outcomes, and creating open educational resources that support diverse implementation models across institutional contexts.
As biomedical engineering continues to advance into emerging areas like gene editing, synthetic biology, and neuroengineering, the ethical dimensions of the field will only intensify in complexity and significance [74] [20]. The academic programs that most successfully prepare students for these challenges will be those that treat ethics not as a supplementary component but as a foundational dimension of biomedical engineering identity and practice, fully integrated throughout the curriculum and modeled by faculty in both teaching and research.
Biomedical engineering stands as a uniquely interdisciplinary field, operating at the convergence of engineering principles, biological sciences, and healthcare delivery. This positioning creates complex ethical landscapes where technological innovation must be balanced against profound responsibility for human life and wellbeing. Within this context, professional societies have established ethical frameworks to guide practitioners, with the Biomedical Engineering Society (BMES) and the IEEE Engineering in Medicine and Biology Society (EMBS) representing two prominent organizations offering distinct but complementary guidance [10] [5]. This analysis examines the BMES Code of Conduct governing conference behavior alongside the EMBS Code of Ethics directing professional and research conduct, framing both within the broader spectrum of biomedical engineering ethics. For researchers, scientists, and drug development professionals, understanding these frameworks is not merely academic but fundamental to navigating the ethical dilemmas inherent in developing technologies that directly impact human health.
The recent introduction of the "Biomedical Engineer's Pledge" has further enriched this landscape, creating a symbolic rite of passage that draws inspiration from both the Hippocratic Oath and existing ethical codes while introducing additional considerations like universal health coverage and environmental sustainability [10]. This analysis will explore how these various frameworks—operational codes and symbolic pledges—interact to shape ethical awareness and professional identity within biomedical engineering.
Methodology for Comparative Analysis
Document Selection and Analysis Framework
This comparative analysis employs a systematic framework to examine the structure, content, and application of two primary ethical documents: the BMES Code of Conduct (2025) applicable to its Cellular and Molecular Bioengineering (CMBE) Conference, and the EMBS Code of Ethics [17] [79]. These documents were selected as they represent current, actively enforced ethical frameworks from two leading societies in biomedical engineering.
The analytical approach utilizes qualitative content analysis to identify key themes, principles, and normative statements within each document. The methodology follows these structured phases:
- Initial Document Review: Comprehensive reading of both documents to identify explicit ethical principles, prohibited behaviors, and prescribed responsibilities.
- Thematic Coding: Systematic coding of text segments into ethical categories (e.g., safety, harassment, research integrity, confidentiality) using constant comparative analysis.
- Comparative Mapping: Cross-document analysis to identify areas of convergence, divergence, and complementarity in ethical focus and specificity.
- Contextual Interpretation: Interpretation of findings within the broader context of biomedical engineering ethics, including reference to the "Biomedical Engineer's Pledge" and case studies from literature [10] [5].
To ensure analytical rigor, this methodology incorporates triangulation through comparison with supplementary sources including ethical pledge documents and analysis of real-world ethical case studies [10] [5]. This approach validates findings and provides context for interpreting the practical implementation of stated ethical principles.
Visualizing the Analytical Workflow
The following diagram illustrates the structured methodology employed in this comparative analysis:
Comprehensive Document Comparison
Structural and Functional Analysis
The BMES Code of Conduct and EMBS Code of Ethics serve different primary functions within the biomedical engineering ecosystem, reflected in their structure, tone, and enforcement mechanisms. The table below provides a detailed comparative overview:
Table 1: Structural and Functional Comparison of Ethical Frameworks
| Comparative Aspect | BMES Code of Conduct | EMBS Code of Ethics |
|---|---|---|
| Primary Scope | Behavioral norms for conference participation [17] | Foundational principles for professional and research conduct [79] |
| Document Status | Mandatory for event attendance; legally enforceable terms [17] | Professional guidelines; establishes normative standards [79] |
| Enforcement Mechanism | Explicit sanctions: removal without refund, potential banning [17] | Implicit professional consequences; AdCom approved [79] |
| Reporting Structure | Designated contacts: conference staff, specific email (conduct@bmes.org) [17] | No specified reporting mechanism provided in document [79] |
| Temporal Application | Time-bound to specific events (e.g., 2025 Conference) [17] | Ongoing professional guidance without expiration [79] |
| Relationship to Law | Explicit coordination with law enforcement [17] | No explicit mention of legal coordination [79] |
Thematic Content Analysis
Beyond structural differences, the two documents demonstrate significant variation in their thematic emphasis and specific normative content. The BMES Code focuses predominantly on interpersonal conduct and environment, while the EMBS Code addresses research integrity and systemic responsibilities.
Table 2: Thematic Content Analysis with Specific Provisions
| Ethical Theme | BMES Code of Conduct Provisions | EMBS Code of Ethics Provisions |
|---|---|---|
| Safety & Well-being | Implicit in harassment-free environment goal [17] | Explicit: "Respect human dignity and privacy of patients and human subjects" [79] |
| Professional Integrity | Addressed through compliance with behavioral norms [17] | Explicit: "Report research results with scientific integrity and proper due credit" [79] |
| Research Ethics | Not explicitly addressed | Comprehensive coverage: human/animal subjects, GLP/GCP standards [79] |
| Environment | Not explicitly addressed | Explicit: "Support the preservation of a healthy environment" [79] |
| Confidentiality | Not explicitly addressed | Explicit: "Ensure proper safeguarding of all confidential information" [79] |
| Non-Discrimination | Extensive specification of protected categories [17] | Not explicitly addressed |
| Conflict Management | Detailed procedures for reporting and addressing harassment [17] | General principle: "Avoid or properly disclose conflicts of interest" [79] |
The Biomedical Engineer's Pledge as a Unifying Framework
The recently introduced "Biomedical Engineer's Pledge" offers a ten-point declarative framework that bridges elements from both society documents while introducing forward-looking ethical considerations [10]. This pledge expands the ethical discourse in biomedical engineering by incorporating explicit commitments to:
- Universal health coverage and healthcare accessibility [10]
- Environmental and economic sustainability of healthcare technologies [10]
- Replacement, reduction, and refinement of animal research (the 3Rs) [10]
- Explicit non-discrimination clauses covering diverse identity factors [10]
- Protection against patient deception and fraud, addressing historical cases like Theranos [10]
The pledge's emphasis on sustainability addresses a critical gap in traditional ethical frameworks, acknowledging that "biomedical engineering, while transformative, also contributes to medical waste, carbon emissions, and economic disparities in healthcare accessibility" [10].
Experimental Protocols for Ethical Analysis
Ethical Dilemma Resolution Framework
For researchers facing ethical dilemmas, systematic analysis protocols provide reproducible methodologies for evaluating complex situations. The following framework adapts established ethical reasoning to biomedical engineering contexts:
Table 3: Protocol for Ethical Dilemma Resolution in Biomedical Engineering
| Protocol Step | Procedure Description | Application Example |
|---|---|---|
| Stakeholder Mapping | Identify all affected parties: patients, researchers, institutions, public | Medical device design: patients, clinicians, manufacturers, regulators |
| Principle Identification | List relevant ethical principles from applicable codes | Non-maleficence, beneficence, justice, respect for autonomy [10] |
| Benefit-Risk Assessment | Systematically quantify potential benefits and harms | Use risk matrix: probability vs. severity for all identified risks |
| Code Compliance Check | Evaluate options against BMES, EMBS, and pledge standards | Verify alignment with specific provisions from each framework |
| Documentation & Reflection | Record decision rationale and ethical considerations | Maintain audit trail showing application of ethical reasoning |
Ethical Technology Assessment Protocol
Biomedical engineers developing new technologies require structured approaches to identify and address ethical implications throughout the development lifecycle:
The Scientist's Toolkit: Essential Research Reagents for Ethical Practice
Beyond conceptual frameworks, ethical biomedical engineering practice requires specific methodological tools and approaches. The following table details essential "research reagents" for implementing ethical principles in practical research and development contexts:
Table 4: Essential Methodologies and Tools for Ethical Biomedical Engineering Research
| Tool Category | Specific Methods/Protocols | Ethical Function | Implementation Example |
|---|---|---|---|
| Informed Consent Systems | Dynamic electronic consent platforms, comprehension verification quizzes | Respect autonomy and ensure genuine participant understanding [5] | Interactive tablet-based consent with mandatory knowledge checks before clinical device trials |
| Data Security Protocols | Encryption standards (AES-256), access control logs, audit trails | Protect patient confidentiality and prevent data breaches [5] | Implement end-to-end encryption for wireless transmission of patient monitoring data |
| Bias Mitigation Frameworks | Algorithmic fairness audits, diverse dataset curation, adversarial testing | Prevent discrimination and ensure equitable technology performance [5] | Validate diagnostic algorithm performance across demographic subgroups before deployment |
| Animal Research Alternatives | Organ-on-chip models, computer simulation, in silico modeling | Implement 3Rs principles (Replacement, Reduction, Refinement) [10] | Use microphysiological systems for preliminary drug efficacy screening before animal studies |
| Environmental Impact Assessors | Lifecycle analysis software, carbon footprint calculators, waste audits | Promote environmental sustainability in device development [10] | Compare single-use vs. reprocessable device options using full lifecycle environmental impact assessment |
This comparative analysis reveals that the BMES Code of Conduct and EMBS Code of Ethics serve complementary rather than competing functions within the biomedical engineering ethical ecosystem. The BMES framework operates primarily at the interpersonal level, creating safe and inclusive professional environments through specific behavioral expectations and enforcement mechanisms. In contrast, the EMBS framework functions at the professional and systemic level, establishing foundational principles for research integrity and technological development with broader societal implications.
For researchers, scientists, and drug development professionals, these frameworks collectively provide a multi-layered ethical foundation that addresses both immediate professional conduct and long-term research responsibility. The emergence of the "Biomedical Engineer's Pledge" further enhances this landscape by introducing forward-looking ethical commitments—particularly regarding sustainability, universal health coverage, and explicit non-discrimination—that expand upon traditional ethical codes.
The practical experimental protocols and research tools outlined in this analysis provide actionable methodologies for implementing these ethical frameworks in daily research practice. As biomedical engineering continues to evolve with advancements in AI, genetic engineering, and neurotechnology, these established ethical frameworks will require continuous refinement and adaptation. However, their core principles—prioritizing patient safety, ensuring research integrity, and maintaining professional responsibility—provide a stable foundation for navigating the complex ethical terrain of 21st-century biomedical innovation.
Within the professional and research ecosystem of biomedical engineering, ethical conduct forms the foundation of scientific integrity, public trust, and ultimately, patient safety. A formal code of ethics is only as effective as the enforcement mechanisms that support it. This whitepaper provides a detailed analysis of these mechanisms within the Biomedical Engineering Society (BMES), focusing on the concrete consequences for violations and the pivotal governance role of the BMES Board of Directors. Framed within broader research on professional ethics, this document serves as a technical guide for researchers, scientists, and drug development professionals who participate in the BMES community. Understanding these structures is critical for navigating the professional landscape and upholding the standards that advance human health through engineering innovation, in line with the BMES mission [80].
BMES Enforcement Mechanisms and Violation Consequences
The primary enforcement mechanism for professional conduct within BMES is articulated in the Code of Conduct for its Annual Meeting, which serves as a model for expected behavior within the society. The code establishes a clear framework for unacceptable behavior and its corresponding repercussions.
Prohibited Conduct and Reporting Pathways
BMES is dedicated to providing a harassment-free experience for all attendees at its events, regardless of gender, gender identity and expression, age, sexual orientation, disability, physical appearance, body size, race, ethnicity, religion, or technology choices [81]. The society explicitly does not tolerate harassment in any form.
Definition of Harassment: The code provides a comprehensive, though non-exhaustive, list of behaviors considered harassing, which includes [81]:
- Offensive verbal or written comments related to personal characteristics.
- Display of sexual images in public spaces or virtual forums.
- Deliberate intimidation, stalking, or following.
- Harassing photography or recording.
- Sustained disruption of talks or other events.
- Inappropriate physical or digital contact.
- Unwelcome sexual attention.
Reporting and Response Protocol: BMES has established clear channels for reporting concerns. Participants are encouraged to contact conference chairs or staff immediately if they are harassed, witness harassment, or have other concerns [81]. Specific protocols include:
- On-Site Reporting: Attending the registration desk to request immediate staff assistance [81].
- Electronic Reporting: Submitting a report via a dedicated email address (
conduct@bmes.org), with assurances of confidentiality [81]. - Staff Assistance: Conference staff are empowered to help participants contact local law enforcement and to assist those experiencing harassment in feeling safe for the duration of the event [81].
Consequences for Code Violations
Non-compliance with the Code of Conduct results in a tiered enforcement response from meeting organizers. The specific actions are designed to be proportionate and are enforced at the discretion of the organizers.
Table 1: Hierarchy of Consequences for BMES Code of Conduct Violations
| Enforcement Action | Triggering Circumstances | Immediate Outcome | Long-Term Repercussions |
|---|---|---|---|
| Immediate Warning | Initial or less severe harassing behavior. The participant is asked to stop and is expected to comply immediately [81]. | Cessation of the specific behavior. | Potential notation for future monitoring. |
| Expulsion from Event | Engaging in harassing behavior after a warning or for severe initial violations [81]. | Immediate removal from the conference, workshops, and social events. | No refund of conference fees [81]. |
| Ban from Future Meetings | Serious or repeated violations, as determined by the BMES Board of Directors [81]. | Inability to register for or attend future BMES annual meetings. | Damage to professional reputation and standing within the BME community. |
This structured approach demonstrates BMES's commitment to enforcing its standards and protecting its community, with ultimate authority for the most severe sanctions resting with its Board of Directors.
Governance Structure and Board of Directors' Role
The BMES Board of Directors is the highest governing body of the society and holds the ultimate authority for its strategic direction, fiduciary health, and ethical standards.
Composition and Election of the Board
The Board is composed of elected officers and members who are leaders in the biomedical engineering field. The executive committee includes the President, President-Elect, Secretary, and Treasurer, among others [82]. The board is structured with staggered terms to ensure continuity.
- Election Process: Board elections are held annually [82]. The Nominating Committee solicits nominations from the membership for positions such as President-Elect, Treasurer, and multiple Director seats [83]. This process allows for broad membership participation in shaping the society's leadership.
- Term Lengths: Terms are structured to ensure both fresh perspectives and experienced oversight. For example, the President-Elect serves one year before a two-year term as President and a one-year term as Past President [83]. Directors typically serve three-year terms [83] [82].
Table 2: BMES Board of Directors Composition and Selection
| Board Position | Term Length | Primary Governance Responsibility | Current Office Holder (Example) |
|---|---|---|---|
| President | 2 years | Strategic leadership and representation of the society [82]. | Shelly E. Sakiyama-Elbert, University of Washington [82]. |
| President-Elect | 1 year | Preparation for the Presidency and specific project oversight [83]. | Jane Grande-Allen, Rice University [82]. |
| Treasurer | 2 years | Fiduciary oversight and financial governance [83]. | Jennifer Amos, University of Illinois Urbana-Champaign [82]. |
| Board Director | 3 years | Setting policy, strategic planning, and committee service [83] [82]. | Multiple (e.g., John P. Fisher, Aaron Kyle, Beth Pruitt) [82]. |
Strategic and Fiduciary Responsibilities
The Board's remit extends far beyond ethics enforcement to the overall health and direction of the society.
- Strategic Planning: The Board sets the strategic vision to advance the BMES mission of promoting "a collaborative and inclusive community to advance human health through education, discovery, and translation" [80].
- Fiduciary and Legal Responsibility: The Board, through the Executive Director/CEO, holds ultimate fiduciary and legal responsibility for all society activities, including the Annual Meeting [84]. This includes oversight of financial matters, contracts, and legal compliance.
- Final Arbiter of Serious Violations: As indicated in the Code of Conduct, the Board of Directors is the body that determines whether a member is banned from future BMES meetings for severe ethical breaches [81]. This power underscores the Board's role as the final arbiter of professional conduct within the society.
The following diagram illustrates the enforcement workflow for a code of conduct violation, highlighting the reporting paths and the Board's ultimate authority in severe cases.
Contextualizing Enforcement: Data-Driven Insights into BME Product Risks
While the BMES code governs professional behavior, the consequences of ethical lapses or technical failures in the wider field of biomedical engineering are starkly visible in regulatory data. An analysis of FDA recalls provides a critical, real-world backdrop to the importance of rigorous ethical and professional standards.
A 2025 study analyzing 27 years of AI/ML-enabled medical device data offers quantitative insights into failure modes. The study established three cohorts for comparison: all 510(k) devices, software-related devices, and AI/ML devices [85]. Root cause analysis revealed that while the top recall causes are similar across groups, their proportions vary significantly.
- Recall Analysis Methodology: The study identified AI/ML-enabled devices from an FDA-published list and gathered recall data from the openFDA platform [85]. Root cause descriptions for each recall event were analyzed, with some events associated with multiple causes [85].
- Heightened Risk in AI/ML Devices: The "AI/ML devices recall" cohort showed a higher impact for 87% of all recalls [85]. Specifically, design and development-related factors were predominant, with "device design" and "software design" root causes accounting for 50% of all recalls for AI/ML devices [85]. This underscores the unique challenges and necessity for robust validation in this rapidly evolving technological domain.
Table 3: Top Root Causes for Medical Device Recalls (Adapted from [85])
| Root Cause Description | All 510(k) Devices | Software-Related Devices | AI/ML Devices |
|---|---|---|---|
| Device Design | 14% (Rank 2) | 15% (Rank 2) | 8% (Rank 3) |
| Software Design | 3% (Rank 7) | 11% (Rank 4) | 42% (Rank 1) |
| Process Control | 16% (Rank 1) | 18% (Rank 1) | 9% (Rank 2) |
| Non-Conforming Material | 5% (Rank 4) | 4% (Rank 7) | 5% (Rank 4) |
| Component Design/Selection | 3% (Rank 7) | 3% (Rank 7) | 1% (Rank 6) |
The following diagram outlines the methodological workflow used in the cited study to analyze medical device recalls, a process that generates the critical data informing ongoing ethical and professional standards.
For researchers and professionals operating in the biomedical engineering field, adherence to ethical codes and understanding governance is a practical necessity. The following table details key "reagent" solutions for navigating this landscape.
Table 4: Essential Resources for Professional Conduct and Governance Knowledge
| Resource or "Reagent" | Function and Purpose | Relevance to Enforcement & Governance |
|---|---|---|
| BMES Code of Conduct | Defines expected behavior and prohibited harassment at BMES events [81]. | Serves as the primary reference document for what constitutes a violation. |
| BMES Board of Directors | The elected governing body that sets strategic policy and holds fiduciary responsibility [82]. | Acts as the final arbiter for serious violations, with power to ban members from future events [81]. |
Confidential Reporting Channel (conduct@bmes.org) |
Provides a secure and private method for reporting violations electronically [81]. | A key component of the enforcement mechanism, ensuring individuals can report concerns safely. |
| FDA Recall Data & openFDA Platform | Publicly accessible regulatory data that provides insights into failure modes of medical devices, including AI/ML technologies [85]. | Offers quantitative, real-world context for the potential consequences of ethical and technical lapses in the field. |
| BMES Governance Overview | Official documentation of the society's leadership structure and composition [82]. | Allows members to understand who governs the society and how leaders are selected [83]. |
The enforcement mechanisms and governance structure of the Biomedical Engineering Society create a cohesive framework for maintaining professional and ethical standards. The system moves from clear definitions of misconduct, through accessible reporting channels, to a graduated set of consequences, with the BMES Board of Directors providing ultimate oversight and authority for the most severe cases. For researchers and professionals in biomedical engineering, engagement with this framework is not merely about compliance. It is an integral part of their professional responsibility, reinforcing a culture that prioritizes safety, integrity, and inclusivity. This, in turn, underpins the scientific and translational work that fulfills the society's vision of achieving "health and wellness for all through engineering innovation" [80].
In the rapidly evolving field of biomedical engineering, maintaining professional competence and ethical rigor is paramount. Continuous professional development, encompassing structured continuing education and systematic feedback mechanisms like 360-degree assessments, provides the foundational framework for sustaining scientific excellence and ethical integrity within the research community. For researchers, scientists, and drug development professionals, these developmental tools are not merely supplemental but essential components of a responsible research career that aligns with the core ethical principles championed by leading scientific organizations [86] [87]. The Biomedical Engineering Society (BMES) emphasizes lifelong learning as a core value, offering educational opportunities designed to "enhance knowledge and education in biomedical engineering and bioengineering worldwide and its utilization for human health and well-being" [88]. This technical guide examines the structured integration of these developmental approaches within the ethical frameworks that govern biomedical research, providing evidence-based methodologies for implementation across research institutions and organizations.
Ethical Foundations in Biomedical Engineering
Core Ethical Principles
Biomedical engineering research operates within a complex ethical landscape shaped by decades of international guidance and professional standards. The International Society for Stem Cell Research (ISSCR) outlines fundamental ethical principles that govern responsible research conduct, emphasizing the "primacy of patient/participant welfare" and the collective nature of scientific effort that depends on public trust and contributions [86]. These principles align with the Nuremberg Code, the Declaration of Helsinki, and other established guidelines that inform contemporary research ethics.
The NIH Clinical Center outlines seven guiding principles for ethical research that directly impact professional development requirements [87]:
- Social and clinical value: Justifying research participation risks through meaningful scientific contributions
- Scientific validity: Ensuring research methodologies yield reliable, answerable questions
- Fair subject selection: Prioritizing scientific goals over vulnerability or privilege in participant selection
- Favorable risk-benefit ratio: Maximizing potential benefits while minimizing participant risks
- Independent review: Establishing unbiased oversight mechanisms
- Informed consent: Guaranteeing voluntary, informed participation decisions
- Respect for potential and enrolled subjects: Protecting privacy, confidentiality, and welfare throughout research participation
Professional Codes of Conduct
Professional societies in biomedical engineering establish explicit codes of conduct that reinforce ethical research practices. The Biomedical Engineering Society (BMES) maintains a comprehensive Code of Conduct for all conference participants, stating that "BMES is dedicated to providing a harassment-free conference experience for everyone, regardless of gender, gender identity and expression, age, sexual orientation, disability, physical appearance, body size, race, ethnicity, religion (or lack thereof), or technology choices" [17]. Similarly, the EMBS Code of Ethics emphasizes respecting "human dignity and privacy of patients and human subjects," ensuring "proper safeguarding of all confidential information," and promoting "a culture of cost-effectiveness" alongside environmental preservation [79].
Table 1: Key Ethical Principles in Biomedical Engineering Research
| Ethical Principle | Professional Application | Source |
|---|---|---|
| Primacy of Patient Welfare | Never allow promise for future patients to override welfare of current research subjects | [86] |
| Respect for Research Subjects | Empower potential participants to exercise valid informed consent; obtain surrogate consent when capacity lacking | [86] |
| Transparency | Promote timely exchange of accurate scientific information; share positive and negative results promptly | [86] |
| Social and Distributive Justice | Distribute benefits of clinical translation justly and globally with emphasis on unmet medical needs | [86] |
| Integrity in Research | Report results with scientific integrity and proper due credit; observe rights of human research subjects | [79] |
Continuing Education in Biomedical Engineering
Structured Educational Programs
Formal continuing education programs provide the foundational knowledge required for ethical research conduct and technical proficiency. Leading institutions have developed comprehensive frameworks to address the evolving needs of biomedical professionals. The Whiting School of Engineering at Johns Hopkins University offers a Professional Development Program (PDP) featuring half-semester courses in "technical communication, presentation skills, grant writing, managing people, leading teams, managing personal finances, consulting, and other relevant areas" [89]. These courses, open to graduate students and postdoctoral fellows, employ real-world, simulation-based experiences to bridge theoretical knowledge with practical application.
The School of Engineering and Applied Sciences at the University at Buffalo implements a SEAS 360° Professional Development Program with micro-credentials in specialized areas including [90]:
- Leadership: Developing critical leadership skills for industry and academia
- Professionalism and Communications: Enhancing technical skills with complementary communication abilities
- Diversity and Inclusion for Engineers: Building knowledge and awareness of DEI issues in STEM
Workshop Methodologies and Implementation
Effective continuing education employs diverse pedagogical approaches to address the multidisciplinary nature of biomedical engineering. The following table illustrates common workshop formats and their applications in professional development:
Table 2: Professional Development Workshop Modalities and Applications
| Workshop Format | Duration | Key Focus Areas | Learning Methodology | |
|---|---|---|---|---|
| Career Launch Series | 4 weeks (45-min sessions) | Career planning, skill identification, goal setting | Virtual; progressive skill building | [90] |
| Masterclass Sessions | 60 minutes | Innovation, entrepreneurship, specialized technical topics | Expert-led; case study analysis | [90] |
| Technical Skillshops | 60-90 minutes | AI in job search, data storytelling, productivity tools | Hands-on application; software training | [90] |
| Leadership Training | 3-hour intensive | Inclusive leadership, ethical decision-making, team dynamics | Scenario-based learning; peer feedback | [90] |
| Networking Events | 60-90 minutes | Professional connections, communication skills, relationship building | Structured networking; peer-to-peer learning | [90] |
Curriculum Integration with Ethical Frameworks
Successful continuing education programs integrate ethical instruction directly into technical coursework. For instance, George Mason University's bioengineering curriculum includes BENG 100: "Bioengineering and Society," which explores the "potentials, challenges, and risks of the relevant technologies" alongside scientific content [91]. Similarly, BENG 101: "Introduction to Bioengineering" incorporates ethics as a core component, introducing students to the "use of technology and innovation in solving problems in biology and medicine with an emphasis on engineering tools and concepts" while addressing professional responsibilities [91].
360-Degree Feedback Assessment
Theoretical Framework
360-degree feedback represents a powerful multidimensional assessment tool that gathers performance evaluations from multiple sources within a professional's working ecosystem. According to the Society for Human Resource Management (SHRM), this methodology provides comprehensive insights for leadership development by collecting "feedback from an employee's subordinates, colleagues, and supervisor(s), along with a self-evaluation" [92]. In biomedical research environments, this approach aligns with the interdisciplinary collaboration essential to the field, acknowledging that professional performance encompasses technical proficiency, ethical conduct, communication effectiveness, and team collaboration.
The 360-degree assessment process creates a holistic view of professional capabilities that mirrors the multifaceted nature of biomedical engineering work, where success depends not only on individual technical expertise but also on effective teamwork, ethical decision-making, and communication across disciplinary boundaries. When properly implemented, this methodology supports the "integrity of the research enterprise" that the ISSCR identifies as essential to maintaining public confidence [86].
Implementation Protocol
Assessment Design Phase
The successful implementation of 360-degree feedback in biomedical research settings requires meticulous planning and alignment with ethical professional standards:
Competency Framework Development: Identify 5-7 core competencies relevant to biomedical engineering roles, incorporating technical capabilities and ethical responsibilities outlined in professional codes of conduct [17] [86] [79]. Sample competencies include: research integrity, collaborative teamwork, ethical decision-making, communication clarity, leadership influence, and technical expertise.
Rater Selection Strategy: Identify 8-12 qualified raters representing multiple perspectives, including:
- Supervisors/Primary Investigators (evaluating research direction and resource management)
- Peers/Colleagues (assessing collaboration and teamwork)
- Direct Reports/Junior Researchers (rating mentorship and leadership)
- Self-Assessment (promoting reflective practice)
- External Stakeholders (evaluating communication and translation)
Instrument Development: Create behaviorally anchored rating scales (BARS) with specific examples of effective and ineffective behaviors for each competency. Scale items should directly reference ethical principles such as "respect for patients and research subjects" [86] and "proper safeguarding of all confidential information" [79].
Administration Phase
Pre-Assessment Briefing: Conduct structured sessions explaining the purpose, process, and confidentiality protections to all participants. Emphasize the developmental (non-evaluative) nature of the assessment and its alignment with continuing professional education.
Multi-Rater Data Collection: Implement the assessment through secure digital platforms, ensuring anonymity for raters and providing clear instructions for providing constructive feedback. The standard administration period typically spans 2-3 weeks.
Data Aggregation and Analysis: Compile results by rater category, maintaining confidentiality while identifying patterns across different rater groups. Calculate both quantitative scores and qualitative feedback themes.
Feedback and Development Planning Phase
Facilitated Feedback Session: Conduct one-on-one sessions with trained facilitators to review results, focusing on:
- Identifying strengths aligned with ethical research practices
- Recognizing blind spots and development areas
- Exploring discrepancies between self-perception and external perceptions
- Connecting feedback to professional standards and ethical frameworks
Individual Development Plan (IDP) Creation: Collaboratively create a structured plan specifying:
- 2-3 priority development areas
- Specific actions and learning activities
- Relevant continuing education opportunities
- Timeline and success metrics
- Connection to ethical competency development
Organizational Follow-up: Implement support structures including mentoring partnerships, targeted workshop participation, and progress reviews at 3, 6, and 12-month intervals.
Diagram 1: 360-Degree Assessment Workflow
Integration Framework
Synergistic Implementation Model
The full potential of continuing education and 360-degree assessments emerges through their strategic integration within professional development ecosystems. This synergistic model creates a continuous improvement cycle where assessment identifies developmental needs that inform educational pursuits, which in turn enhance competencies measured in subsequent assessments. The Biomedical Engineering Society exemplifies this approach through its combination of "webinars, committee driven programs, four journals, virtual symposiums, sponsored competitions, and continuous networking opportunities" [88].
The integration process follows these sequential phases:
Competency Assessment: 360-degree feedback identifies specific capability gaps in technical knowledge, ethical reasoning, or professional skills.
Targeted Learning Selection: Professionals select continuing education activities directly addressing identified development needs from available opportunities.
Applied Learning: New knowledge and skills are implemented in research practice, with particular attention to ethical application.
Impact Evaluation: Subsequent assessments measure progress and identify new development areas, continuing the improvement cycle.
Diagram 2: Professional Development Cycle
Ethical Integration Protocol
To ensure ethical integration of these developmental tools, organizations should implement the following protocol:
Voluntary Participation: Establish 360-degree assessments as developmental (non-evaluative) tools with voluntary participation to build trust and engagement.
Confidentiality Assurance: Protect individual assessment data through strict confidentiality measures, sharing only aggregated, anonymized data for organizational planning.
Equitable Access: Ensure all professionals have equal access to continuing education opportunities, addressing potential barriers through scholarships, virtual options, and flexible scheduling.
Reasonable Accommodation: Provide appropriate accommodations for professionals with disabilities across both assessment and educational activities.
Cultural Sensitivity: Adapt assessment tools and educational content to respect cultural differences while maintaining consistent ethical standards.
Research Reagent Solutions for Professional Development
Table 3: Essential Resources for Professional Development Implementation
| Resource Category | Specific Tools & Methods | Primary Application | Ethical Considerations | |
|---|---|---|---|---|
| Assessment Platforms | 360-degree feedback software with customizable competency models | Multi-rater data collection and analysis | Confidentiality protection; data security; anonymity assurance | [92] |
| Ethical Decision Frameworks | NIH 7 Principles framework; ISSCR Guidelines | Structured ethical analysis and decision support | Respect for participant autonomy; risk-benefit proportionality | [86] [87] |
| Communication Modules | "Tough Talks: Communication Strategies for Difficult Situations"; "From Stage Fright to Spotlight" | Developing crucial communication skills | Transparency; accurate information exchange; respectful dialogue | [90] |
| Leadership Development | "Leadership Training Camp"; "Leading Together: Building Inclusive Leadership Skills" | Enhancing team leadership capabilities | Promoting inclusive environments; ethical leadership modeling | [90] |
| Technical Competency Builders | "Telling Stories with Data"; "Grammarly's Generative AI for Graduate Students" | Developing essential technical communication skills | Responsible technology use; data accuracy and representation | [90] |
Professional development through continuing education and 360-degree assessments represents a strategic imperative for maintaining both technical excellence and ethical integrity in biomedical engineering research. When systematically implemented and fully integrated, these developmental tools create a robust framework for sustaining professional competence while upholding the ethical principles essential to responsible research conduct. As the biomedical engineering field continues to evolve with emerging technologies and complex ethical challenges, these developmental approaches provide the foundation for ensuring that researchers, scientists, and drug development professionals remain equipped to advance human health while maintaining public trust and adhering to the highest standards of research integrity.
The competitive landscape of scientific research funding necessitates a rigorous commitment to ethical standards. For researchers in biomedical engineering and related fields, securing support from premier agencies like the National Science Foundation (NSF) and the National Institutes of Health (NIH) is contingent upon demonstrating impeccable adherence to established ethical frameworks. The responsible and ethical conduct of research (RECR) is critical not only for excellence but also for maintaining public trust in science and engineering [93]. This guide provides a comprehensive technical overview of the current ethical requirements, offering researchers a detailed roadmap for navigating the compliance process for grant proposals. These guidelines are embedded within the broader professional ethos exemplified by codes of ethics from leading organizations like the Biomedical Engineering Society (BMES) and the IEEE Engineering in Medicine and Biology Society (EMBS), which emphasize human dignity, research integrity, and responsible authorship [17] [6].
Foundational Ethical Principles
Core Ethical Tenets for Clinical and Human Subjects Research
The NIH has articulated seven fundamental principles that must guide all clinical research, forming an essential foundation for any proposal involving human participants [87].
- Social and Clinical Value: Every research study must be designed to answer a specific question that contributes to scientific understanding or improves health outcomes, thereby justifying the involvement of human participants and the resources expended.
- Scientific Validity: The study must be methodologically sound, using valid and feasible research methods to ensure it yields reliable and interpretable results. Invalid research is inherently unethical as it wastes resources and exposes participants to risk without purpose.
- Fair Subject Selection: The scientific goals of the study must be the primary basis for participant recruitment. Groups should not be excluded without a valid scientific reason, and those accepting the risks of research should be positioned to enjoy its benefits.
- Favorable Risk-Benefit Ratio: Researchers must diligently work to minimize potential risks—whether physical, psychological, economic, or social—and maximize potential benefits, ensuring the latter are proportionate to or outweigh the former.
- Independent Review: An independent panel must review the research proposal to assess ethical acceptability, minimize conflicts of interest, and ensure participant protections are in place before the study begins and while it is ongoing.
- Informed Consent: Potential participants must undergo a structured process where they are accurately informed of the study's purpose, methods, risks, and benefits; understand this information; and subsequently make a voluntary decision about participation.
- Respect for Enrolled Subjects: This encompasses protecting participant privacy, respecting their right to withdraw without penalty, keeping them informed of new developments, and monitoring their welfare throughout the study [87].
Professional Society Codes of Ethics
Beyond federal regulations, professional societies enforce codes of conduct that align with and often expand upon funding agency requirements. The Biomedical Engineering Society (BMES), for instance, mandates a harassment-free conference environment, which reflects a broader commitment to safe and respectful research settings [17]. The IEEE Engineering in Medicine and Biology Society (EMBS) Code of Ethics provides specific guidelines for its members, including respecting human dignity and privacy, ensuring proper safeguarding of confidential information, reporting results with scientific integrity, and humanely using animals in research [6]. These principles reinforce the holistic ethical approach required by major funding bodies.
Agency-Specific Ethical and Training Requirements
National Science Foundation (NSF) Requirements
The NSF mandates that all institutions receiving funding have a plan to provide appropriate training and oversight in the responsible and ethical conduct of research (RECR) [93]. This training is required for undergraduate students, graduate students, postdoctoral scholars, faculty, and other senior personnel supported by NSF funds.
Table 1: NSF Responsible and Ethical Conduct of Research (RECR) Training Requirements
| Aspect | Requirement |
|---|---|
| Target Audience | Undergraduates, graduate students, postdocs, faculty, and other senior personnel supported by NSF grants [93]. |
| Core Content Areas | Mentor training and mentorship; research security; export controls [93] [94]. |
| Recent Updates (Effective 2025) | As of October 10, 2025, NSF has implemented new requirements incorporating training on research security threats and federal export control regulations [94]. |
| Training Frequency | Courses must be completed every 5 years by those actively supported by NSF, typically within 60 days of being paid from the grant [94]. |
The NSF's Ethical and Responsible Research (ER2) program specifically funds research that examines and promotes what constitutes responsible and ethical science. The program seeks to improve RECR practices across career stages and research environments, focusing on individual, organizational, and cultural factors [95].
National Institutes of Health (NIH) Requirements
The NIH's policy on instruction in the responsible conduct of research (RCR) applies to all trainees, fellows, and scholars supported by specific NIH training, career development, and research education grants [94].
Table 2: NIH Responsible Conduct of Research (RCR) Training Requirements
| Aspect | Requirement |
|---|---|
| Target Audience | Trainees, fellows, and scholars on NIH institutional training grants (e.g., T32, F31) and career development awards (e.g., K01) [94]. |
| Core Content Areas | Conflict of interest; human subjects and animal welfare; data acquisition and management; mentor/mentee responsibilities; collaborative science; safe research environments [94]. |
| Recent Updates | Effective September 25, 2022, NIH expanded required topics to include "safe research environments" and "the scientist as a responsible member of society," among others [94]. A new submission limit policy takes effect September 25, 2025, capping research grant applications per PI at six per calendar year [96]. |
| Research Security | Effective October 1, 2025, NIH requires all key personnel to complete Research Security Training, aligning with similar NSF and DOE mandates [96]. |
Implementation and Validation Methodologies
Experimental Protocol for Ethical Proposal Development
Successfully addressing ethical considerations in a grant proposal is a systematic process. The following protocol outlines a detailed methodology for integrating ethical validation into proposal development.
Table 3: Research Reagent Solutions for Ethical Proposal Development
| Item/Tool | Function in Ethical Proposal Preparation |
|---|---|
| Institutional Review Board (IRB) | Provides independent ethical review of research involving human subjects, ensuring compliance with federal regulations and ethical principles [87]. |
| CITI Program Modules | Online platform providing standardized, certified training courses in RCR, research security, and human/animal subject protections [96] [94]. |
| Data Management Plan (DMP) | A formal document outlining how research data will be handled, shared, and preserved, ensuring integrity, confidentiality, and responsible authorship. |
| Conflict of Interest (COI) Disclosure | A formal process for researchers to declare personal, professional, or financial interests that could appear to bias their research. |
Step 1: Early-Stage Protocol and Review Design Initiate consultations with your institution's Institutional Review Board (IRB) and Institutional Animal Care and Use Committee (IACUC) during the project's conceptual phase. Draft detailed protocols for human subject recruitment, informed consent forms, and data safety monitoring plans. For research involving international collaborations, conduct a preliminary assessment of unique risks related to research security, intellectual property, and export controls [93] [97].
Step 2: Comprehensive Documentation and Training Validation Collect completion certificates for all required RCR, research security, and export control training for every key person named in the proposal [94]. Develop a comprehensive data management plan that addresses all stages of the data lifecycle, from acquisition and analysis to sharing and ownership. Document all mentorship plans, especially for students and postdoctoral researchers, as this is a specific requirement for NSF [93].
Step 3: Pre-Submission Ethical Review Assemble a mock, independent review panel, potentially composed of senior colleagues from different disciplines, to critique the proposal's ethical dimensions. This panel should review the risk-benefit ratio, subject selection fairness, and confidentiality measures, mirroring the NIH's principle of independent review [87]. Use this feedback to perform a final gap analysis against the specific requirements outlined in the NSF PAPPG or relevant NIH Funding Opportunity Announcement (FOA).
The following workflow diagram illustrates the key stages and decision points in this ethical validation process for a research proposal.
Key Content Areas for Responsible Conduct of Research (RCR)
The following comprehensive table details the core RCR topics that must be addressed in both training and proposal documentation. These areas represent the synthesis of requirements from both NSF and NIH.
Table 4: Core Responsible Conduct of Research (RCR) Content Areas
| Content Area | NSF Emphasis | NIH Emphasis | Validation Method in Proposal |
|---|---|---|---|
| Research Misconduct | Understanding fabrication, falsification, plagiarism. | Policies for handling misconduct. | Description of internal oversight procedures. |
| Data Management | Data acquisition, management, sharing, and ownership. | Data confidentiality, management, sharing, ownership; use of electronic lab notebooks. | Detailed Data Management Plan (DMP). |
| Human Subjects | Protections for human subjects in research. | Policies regarding human subjects; favorable risk-benefit ratio. | IRB approval or pending status; informed consent form. |
| Animal Welfare | Humane care and use of animals in research. | Live vertebrate animal subjects policies. | IACUC approval or pending status. |
| Mentorship | Mentor training and mentorship is a required component [93]. | Mentor/mentee responsibilities and relationships. | Formal, described mentorship plan for trainees. |
| Collaborative Science | Ethics of peer review and collaborative research. | Collaborations with industry and international partners. | Letters of collaboration; data sharing agreements. |
| Conflict of Interest | Personal, professional, and financial conflicts. | Personal, professional, and financial conflicts. | Completed COI disclosure forms for all key personnel. |
| Research Security | Required training on threats and disclosure as of 10/10/25 [94]. | Required training for key personnel as of 10/1/25 [96]. | Certification of training completion; disclosure of foreign affiliations. |
| Safe Research Environments | Implied in fair treatment of colleagues [93]. | Explicitly required; environments free of discriminatory harassment [94]. | Statement affirming commitment to inclusive, safe workplace. |
| Publication Practices | Responsible authorship. | Responsible authorship and publication. | Description of planned authorship criteria and publication process. |
Adherence to ethical standards is a fundamental pillar of the scientific enterprise, directly influencing the funding decisions of the NSF and NIH. The evolving policy landscape, particularly with the introduction of new research security and export control mandates in 2025, requires researchers to remain vigilant and proactive [96] [94]. A successful grant proposal must now seamlessly integrate deep scientific innovation with a robust, validated ethical framework. This includes not only protecting research subjects and ensuring data integrity but also fostering safe and inclusive research environments and navigating the complexities of global collaboration. By systematically implementing the protocols and adhering to the requirements detailed in this guide, researchers can strengthen their proposals, validate their scientific rigor, and uphold the public trust that is essential to the continued support and advancement of science and engineering.
Conclusion
The codes of ethics established by biomedical engineering societies are not static documents but dynamic frameworks essential for navigating the complex moral landscape of modern healthcare innovation. The key takeaways from these foundational principles, methodological applications, troubleshooting strategies, and validation systems converge on a single imperative: a steadfast commitment to patient safety, scientific integrity, and social equity must underpin all research and development. As biomedical engineering continues to advance with breakthroughs in AI, neural engineering, and personalized medicine, the profession's ethical guidelines will similarly need to evolve. Future directions must include fostering greater cultural competency, developing robust global standards for emerging technologies, and reinforcing the ethical courage of every professional. By internalizing and championing these principles, researchers and developers can ensure that technological progress consistently translates into ethical and equitable health outcomes for all.
References
- 1. the Analyzing Behind Ethics | Duke Pratt... Biomedical Engineering [https://pratt.duke.edu/news/analyzing-the-ethics-behind-biomedical-engineering/]
- 2. Biomedical ethics and the biomedical engineer: a review [https://pubmed.ncbi.nlm.nih.gov/9315431/]
- 3. 12.1 Ethical Principles in Biomedical Engineering [https://fiveable.me/biomedical-engineering-i/unit-12/ethical-principles-biomedical-engineering/study-guide/juiq830vPBoygWfC]
- 4. Biomedical engineering and ethics: reflections on medical ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-021-00697-1]
- 5. Challenges and Ethical Considerations in Biomedical ... [https://online-engineering.case.edu/blog/challenges-and-ethical-considerations-in-biomedical-engineering]
- 6. Code of Ethics [https://www.embs.org/about/ethics/]
- 7. of Different Comparison of Engineering : What's the... Codes Ethics [https://www.pdh-pro.com/pe-resources/comparison-of-different-engineering-codes-of-ethics-whats-the-same-and-whats-different/]
- 8. Principles of Bioethics [https://depts.washington.edu/bhdept/ethics-medicine/bioethics-topics/articles/principles-bioethics]
- 9. The biomedical engineer's pledge: overview and context [https://pubmed.ncbi.nlm.nih.gov/40993405/]
- 10. The biomedical engineer's pledge: overview and context [https://link.springer.com/article/10.1007/s11517-025-03443-6]
- 11. Principles of Clinical Ethics and Their Application to Practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC7923912/]
- 12. 12.1 Bioethics in Research and Clinical Practice [https://fiveable.me/biomedical-engineering-ii/unit-12/bioethics-research-clinical-practice/study-guide/JJiMnNwtsA7dQXmN]
- 13. The Four Principles of Biomedical Ethics [https://www.healthcareethicsandlaw.co.uk/intro-healthcare-ethics-law/principlesofbiomedethics]
- 14. The Four Principles of Bioethics: Autonomy, Beneficence ... [https://www.linkedin.com/posts/egilonisopriscillamichael_the-four-principles-of-bioethics-in-healthcare-activity-7365680256038375424-CWot]
- 15. AI Ethics beyond Principles: Strengthening the Life-world ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11811459/]
- 16. Ethics 101 for Engineers: The 7 Codes of Ethics and Why ... [https://blog.stulz-usa.com/ethics-101-for-engineers-the-7-codes-of-ethics-and-why-they-are-essential-for-engineers]
- 17. Code of Conduct | 2025 CMBE Conference [https://www.bmes.org/2025/cmbeconference/codeofconduct]
- 18. AdvaMed Leads with Integrity: Updated Code of Ethics ... [https://www.advamed.org/industry-updates/news/advamed-leads-with-integrity-updated-code-of-ethics-now-available/]
- 19. Criteria for Accrediting Engineering Programs, 2025 - 2026 [https://www.abet.org/accreditation/accreditation-criteria/criteria-for-accrediting-engineering-programs-2025-2026/]
- 20. Toward a More Ethical and Sustainable Biomedical ... [https://www.embs.org/pulse/articles/toward-a-more-ethical-and-sustainable-biomedical-engineering-education/]
- 21. Ethical Issues in Patient Data Ownership [https://www.i-jmr.org/2021/2/e22269]
- 22. Patient Confidentiality - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK519540/]
- 23. Informed Consent - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK430827/]
- 24. : guidelines for Research ... | Cancer integrity UK scientific Research [https://www.cancerresearchuk.org/for-researchers/apply-for-and-manage-your-funding/research-policies-and-guidance/guidelines-for-scientific-conduct]
- 25. Quantitative Data Quality Assurance, Analysis and Presentation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056448/]
- 26. Reporting Your Quantitative Research Findings [https://insightsopinion.com/quantitative-research/reporting-your-quantitative-research-findings-best-practices-and-guidelines]
- 27. What to consider when choosing colors for data visualization [https://academy.datawrapper.de/article/140-what-to-consider-when-choosing-colors-for-data-visualization]
- 28. Committees for Growth and Leadership | BMES [https://www.bmes.org/communities/committees]
- 29. Benefit Risk Analysis for Medical Devices: Product Safety [https://mavenprofserv.com/benefit-risk-analysis/]
- 30. Mastering Benefit-Risk Analysis EU MDR Compliance [https://www.celegence.com/benefit-risk-analysis-tools-eu-mdr/]
- 31. Operational risk scoring for health care facilities [https://www.hfmmagazine.com/articles/5013-operational-risk-scoring-for-health-care-facilities]
- 32. A Structured Benefit-Risk Assessment Operating Model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10276786/]
- 33. Informed Consent in Biomedical Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6458444/]
- 34. Patient Perspectives About Decisions to Share Medical Data ... [https://pubmed.ncbi.nlm.nih.gov/31433479/]
- 35. Technological Adjuncts to Streamline Patient Recruitment ... [https://formative.jmir.org/2025/1/e58628]
- 36. Verbal consent in biomedical research: moving toward a ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1472655/full]
- 37. Patent Pending: Significant Changes in Patent Law Possible ... [https://jbipl.pubpub.org/pub/toz2dzc0]
- 38. The Future of Healthcare Innovation 2025 - Cure. [https://wewillcure.com/insights/healthcare-innovation-report]
- 39. The future of healthcare [https://www.pwc.com/us/en/industries/health-industries/library/future-of-health.html]
- 40. 2025 global health care outlook | Deloitte Insights [https://www.deloitte.com/us/en/insights/industry/health-care/life-sciences-and-health-care-industry-outlooks/2025-global-health-care-executive-outlook.html]
- 41. Conflict of Interest in Biomedical Research and Clinical ... [https://www.thehastingscenter.org/briefingbook/conflict-of-interest-in-biomedical-research/]
- 42. Conflict of interest disclosure in biomedical research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4854425/]
- 43. Conflict Of Interest | IgMin Research - A BioMedical ... [https://www.igminresearch.com/pages/policies/conflict-of-interest]
- 44. Competing interests | Nature Biomedical Engineering [https://www.nature.com/natbiomedeng/editorial-policies/competing-interests]
- 45. Conflicts of Interest Publication Disclosures: Descriptive Study [https://data.jmir.org/2024/1/e57779]
- 46. Diversity & Inclusion in Biomedical Engineering | BMES [https://www.bmes.org/about/diversity]
- 47. Bioengineering needs diversity [https://www.nature.com/articles/s44222-025-00317-2]
- 48. DIVERSITY IN THE BIOMEDICAL RESEARCH WORKFORCE [https://pmc.ncbi.nlm.nih.gov/articles/PMC3375909/]
- 49. Diversity and Inclusion in Biomedical Engineering [https://online-engineering.case.edu/blog/diversity-and-inclusion-in-biomedical-engineering]
- 50. Improving research and development of wearable assistive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11844098/]
- 51. Incorporating Diversity, Equity, and Inclusion Content Into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11003107/]
- 52. Therac-25 - Ethics Unwrapped [https://ethicsunwrapped.utexas.edu/case-study/therac-25]
- 53. Therac-25 [https://en.wikipedia.org/wiki/Therac-25]
- 54. Metallurgical analysis of failed Björk-Shiley cardiac valve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC460278/]
- 55. Medtronic Evolut TAVR systems receive FDA approval for ... [https://news.medtronic.com/2025-08-28-Medtronic-Evolut-TAVR-systems-receive-FDA-approval-for-expanded-Redo-TAVR-indication]
- 56. MEDTRONIC HEART VALVES DIVISION MOSAIC MITRAL ... [https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfmaude/detail.cfm?mdrfoi__id=23155303&pc=DYE]
- 57. Awareness of the dual-use dilemma in scientific research [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1649781/full]
- 58. Assessing Dual-Use Issues at the AIxBio Convergence [https://councilonstrategicrisks.org/2025/07/31/the-aixbio-landscape/]
- 59. The dual use of research ethics committees [https://pmc.ncbi.nlm.nih.gov/articles/PMC5989368/]
- 60. Governance strategies for biological AI: beyond the dual ... [https://pubmed.ncbi.nlm.nih.gov/41058341/]
- 61. Conflict resolution styles and skills and variation among ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10103535/]
- 62. “A Framework for Ethical Decision Making” in Problem ... [https://www.scu.edu/ethics/focus-areas/more-focus-areas/engineering-ethics/ethical-considerations-in-the-senior-design-project/a-framework-for-ethical-decision-making-in-problem-definition--project-selection/]
- 63. Introducing conflict resolution and negotiation training into a ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-022-03494-5]
- 64. Whistle-blowers – morally courageous actors in health care? [https://pmc.ncbi.nlm.nih.gov/articles/PMC9527363/]
- 65. Whistleblower Effect - PsychoTricks [https://psychotricks.com/whistleblower-effect/]
- 66. The Whistleblower's Dilemma: Do the Risks Outweigh the ... [https://knowledge.wharton.upenn.edu/article/whistleblowers-in-business/]
- 67. Institutional Review Boards Frequently Asked Questions [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions]
- 68. Beginner's Guide to institutional review boards (IRBs) [https://www.advarra.com/blog/beginners-guide-to-institutional-review-boards/]
- 69. Ethical Guidelines and the Institutional Review Board [https://pmc.ncbi.nlm.nih.gov/articles/PMC10885741/]
- 70. What Every Clinical Researcher Should Know About ... [https://acrpnet.org/2025/10/21/what-every-clinical-researcher-should-know-about-institutional-review-boards]
- 71. Institutional Review Board (IRB) proposals [https://www.povertyactionlab.org/resource/institutional-review-board-irb-proposals]
- 72. Institutional Review Board - Clinical-biomedical (IRB-Clin) [https://research.ucr.edu/orc/irb-clin]
- 73. Understanding the Role of Privacy Policies and Institutional ... [https://www.jmir.org/2025/1/e70711]
- 74. Ethical Considerations in Biomedical Engineering [https://biomedevices.com/ethical-considerations-in-biomedical-engineering-balancing-innovation-and-patient-safety/]
- 75. Ethical Challenges in Biomedical Engineering - Data ... [https://jef.works/blog/2022/10/15/ethical-challenges-in-bme/]
- 76. Ethics and Character Education in Engineering [https://beetl.pratt.duke.edu/research/ethics-and-character-education-engineering]
- 77. Ethics and biomedical engineering for well-being [https://www.nature.com/articles/s41598-023-39834-8]
- 78. How Do Molecular Systems Engineering Scientists Frame ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11299911/]
- 79. Code of Ethics [https://embc.embs.org/2025/about/ethics/]
- 80. Biomedical Engineering Society - BMES [https://www.bmes.org/]
- 81. 2025 BMES Annual Meeting - Code of Conduct [https://www.bmes.org/2025/annualmeeting/conduct]
- 82. Governance Overview | BMES Board of Directors [https://www.bmes.org/about/governance]
- 83. 2025 BMES Board Nominations [https://www.bmes.org/bmes-board-nominations]
- 84. Roles and Responsibilities | BMES Events [https://www.bmes.org/events/roles-and-responsibilities]
- 85. Regulatory Insights From 27 Years of Artificial Intelligence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274014/]
- 86. 1. Fundamental Ethical Principles [https://www.isscr.org/guidelines/fundamental-ethical-principles]
- 87. Guiding Principles for Ethical Research [https://www.nih.gov/health-information/nih-clinical-research-trials-you/guiding-principles-ethical-research]
- 88. Education | Lifelong Learning Initiatives by BMES [https://www.bmes.org/education]
- 89. Professional Development Program [https://e-catalogue.jhu.edu/engineering/full-time-residential-programs/degree-programs/leadership-education/professional-development/]
- 90. SEAS 360° Professional Development [https://engineering.buffalo.edu/home/academics/beyond/professionalism/seas360.html]
- 91. Department of Bioengineering [https://catalog.gmu.edu/colleges-schools/engineering-computing/engineering/bioengineering/]
- 92. 360-Degree Feedback Is Powerful Leadership ... [https://www.shrm.org/topics-tools/news/organizational-employee-development/360-degree-feedback-powerful-leadership-development-tool]
- 93. Responsible and Ethical Conduct of Research - Policies [https://www.nsf.gov/policies/responsible-research-conduct]
- 94. Responsible Conduct of Research [https://www.research.ucsb.edu/research-integrity/rcr]
- 95. Ethical and Responsible Research (ER2) [https://www.nsf.gov/funding/opportunities/er2-ethical-responsible-research/505693/nsf24-604]
- 96. NIH Policy Updates that will directly impact Proposal ... - URSA [https://ursa.research.gsu.edu/2025/07/21/nih-policy-updates-that-will-directly-impact-proposal-submissions-and-award-management-processes/]
- 97. NSF 25-542: Smart Health and Biomedical Research in the ... [https://www.nsf.gov/funding/opportunities/sch-smart-health-biomedical-research-era-artificial-intelligence/nsf25-542/solicitation]