Navigating the Inverse Problem: Current Challenges and Advanced Solutions in EIT Image Reconstruction
Electrical Impedance Tomography (EIT) is a promising, non-invasive imaging modality with significant potential for biomedical monitoring and research.
Navigating the Inverse Problem: Current Challenges and Advanced Solutions in EIT Image Reconstruction
Abstract
Electrical Impedance Tomography (EIT) is a promising, non-invasive imaging modality with significant potential for biomedical monitoring and research. However, its practical application is hindered by the complex, ill-posed inverse problem at the heart of image reconstruction. This article provides a comprehensive analysis for researchers, scientists, and drug development professionals. We explore the fundamental principles and core challenges of EIT, review cutting-edge reconstruction algorithms and their applications in preclinical and clinical settings, address common troubleshooting and optimization strategies for improving image fidelity, and examine validation methodologies and comparative performance against established imaging techniques. The synthesis offers a clear pathway for leveraging EIT's unique capabilities in dynamic functional imaging.
Understanding the Core: The Ill-Posed Inverse Problem and Fundamental Limits of EIT
Technical Support Center: Troubleshooting & FAQs
Q1: During a 16-electrode adjacent measurement protocol, we observe consistently low voltage readings on one channel. What could be the cause and how do we resolve it?
A: This typically indicates an electrode contact issue. First, clean the electrode surface and the skin/phantom contact area with conductive gel or saline. If the problem persists, check the wiring continuity from the electrode to the data acquisition system. A faulty electrode or a broken wire in the specific channel is likely. Replace the suspect electrode and re-calibrate the system. Ensure consistent electrode-skin impedance by applying uniform pressure.
Q2: Our reconstructed EIT images show significant artifacts and streaking, particularly when using a GREIT reconstruction algorithm. What steps should we take to improve image quality?
A: Artifacts often stem from inaccurate forward model parameters. Verify and update your finite element model (FEM) mesh to precisely match your electrode positions and domain geometry (e.g., tank diameter, organ shape). Ensure your boundary voltage measurements are synchronized and free from noise. Re-calibrate your system using a known conductivity phantom. Consider applying spatial filtering or regularization parameter (e.g., Tikhonov hyperparameter λ) optimization. The following table summarizes key regularization parameters and their typical effects:
| Parameter | Typical Range | Effect on Image | Common Artifact if Mis-set |
|---|---|---|---|
| Tikhonov Regularization (λ) | 1e-5 to 1e-2 | Controls smoothness vs. data fidelity. | Over-smoothing (blur) or excessive noise. |
| Mesh Element Size | 1000-5000 elements | Resolution of forward model. | Pixelation or "staircase" artifacts. |
| Signal-to-Noise Ratio (SNR) | > 80 dB | Measurement fidelity. | Random speckle noise. |
| Electrode Position Error | < 1% of domain radius | Geometry accuracy. | Consistent streaking from electrode sites. |
Q3: What is the recommended protocol for validating a new EIT system for thoracic imaging studies?
A: Follow a three-stage validation protocol:
Saline Tank Validation: Use a cylindrical tank with known conductivity saline (e.g., 0.9% NaCl, σ ≈ 1.5 S/m). Place insulating and conducting targets of known size and position inside. Acquire data and reconstruct. Calculate the following performance metrics:
- Position Error: Distance between reconstructed and actual target center.
- Image Noise: Standard deviation of conductivity in a homogeneous region.
- Contrast Recovery: (Δσreconstructed / Δσactual) x 100%.
Animal Model Benchmark: Perform imaging on a ventilated animal model (e.g., porcine) with controlled tidal volumes. Compare EIT-derived tidal volume and center of ventilation indices with data from a mechanical ventilator or CT.
Human Subject Reproducibility: Conduct repeated baseline measurements on a healthy human subject on different days. Calculate the coefficient of variation (CV) for end-expiration conductivity in a region of interest.
Q4: How do we differentiate between measurement noise and physiological signal in dynamic lung EIT data?
A: Apply frequency-domain analysis. Physiological signals (ventilation, perfusion) occupy specific bands. Ventilation is typically at the respiratory rate (0.1-0.5 Hz). Cardiac-related impedance changes are at the heart rate (1-2 Hz) and are ~10% the amplitude of ventilation. Noise (e.g., electrode movement, power line interference) appears at 50/60 Hz or is broadband. Use band-pass filtering. For perfusion, perform gated averaging synchronized to the ECG or apply Principal Component Analysis (PCA) to separate signal components.
Experimental Protocol: Conductivity Phantom Calibration
Objective: To establish a baseline and validate system sensitivity for a 32-electrode EIT system.
Materials (Research Reagent Solutions):
| Item | Function | Specification Example |
|---|---|---|
| Sodium Chloride (NaCl) | Creates a homogeneous background of known conductivity. | ACS grade, 0.9% w/v for ~1.5 S/m at 20°C. |
| Potassium Chloride (KCl) | May be added to mimic intracellular fluid. | 0.1% w/v addition. |
| Agar or Gelatin | Solidifying agent for stable, non-convective phantoms. | 1-3% w/v. |
| Conductive Target (Insulating) | Simulates a lesion or air-filled cavity. | Plastic or acrylic rod, 10-20% domain diameter. |
| Conductive Target (Metallic) | Simulates a highly conductive region. | Stainless steel or aluminum rod. |
| Conductive Electrode Gel | Ensures stable electrode-tank interface. | Medical-grade, chloride-based gel. |
| Calibrated Conductivity Meter | Gold-standard for ground truth σ measurement. | Temperature-compensated, range 0.01-10 S/m. |
Procedure:
- Prepare a 0.9% NaCl solution in deionized water. Measure and record its conductivity (σ_bg) and temperature.
- Pour the solution into your calibrated imaging tank. Attach electrodes per your geometry file.
- Collect a reference dataset
V_refusing your standard measurement protocol (e.g., adjacent drive, adjacent measure). - Introduce a target of known size, conductivity, and position. For an insulating target, use a plastic rod.
- Collect a new dataset
V_target. - Reconstruct the differential image (σ - σ_bg).
- Quantify the position error, shape distortion, and amplitude response of the reconstructed target.
- Repeat for targets of different sizes and conductivities.
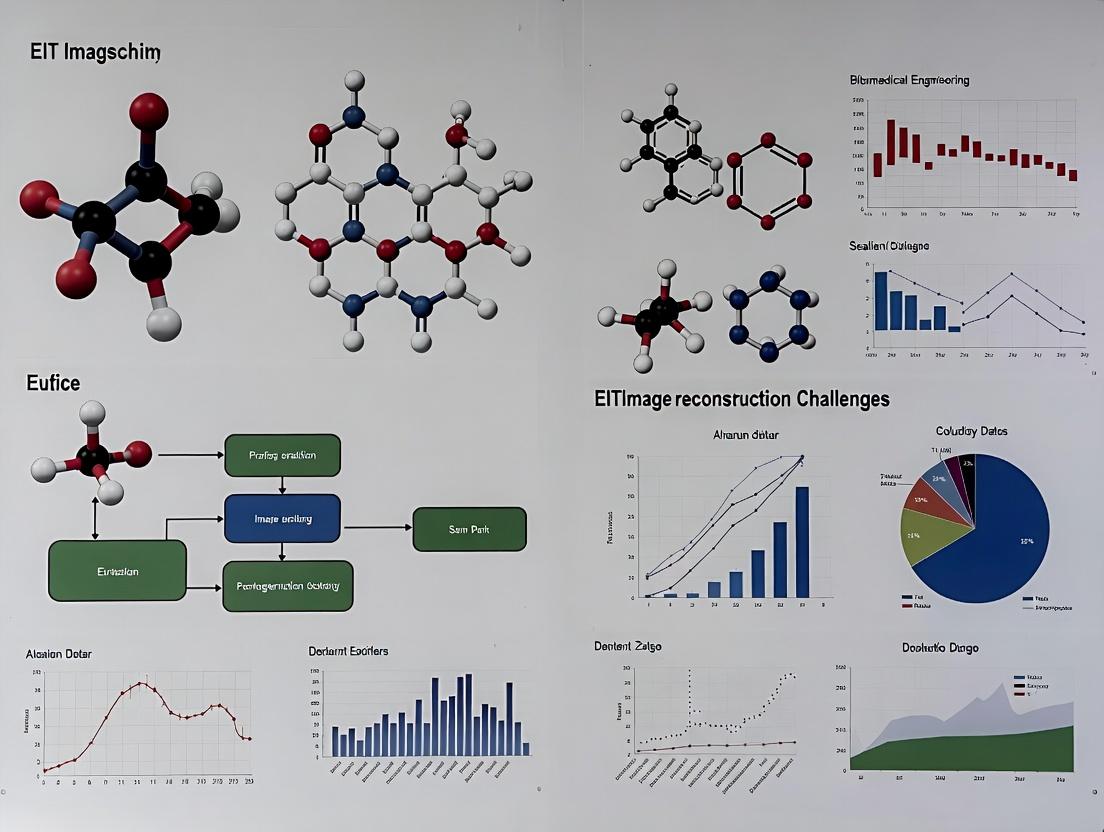
Logical Workflow of EIT Image Reconstruction
Title: EIT Reconstruction Feedback Loop
EIT System Signal Pathway & Error Sources
Title: EIT Signal Pathway and Error Injection Points
Q5: What are the key hardware specifications to evaluate when selecting an EIT system for preclinical drug development studies in small animals?
A: Focus on specifications that address the unique challenges of small, dynamic domains:
| Specification | Importance for Preclinical Studies | Recommended Minimum |
|---|---|---|
| Operating Frequency | Tissue characterization, avoids electrode polarization. | Multi-frequency (10 kHz - 1 MHz). |
| Frame Rate | Capture rapid cardiopulmonary dynamics. | > 50 frames/sec. |
| Number of Electrodes | Spatial resolution for small domains. | 16 to 32 electrodes. |
| Current Source Accuracy | Stability for small, sensitive measurements. | < 0.1% variation, < 1 µA RMS noise. |
| Voltage Measurement Precision | Detect small physiological changes. | 16-bit ADC, > 100 dB CMRR. |
| System Portability | For use in sterile environments or with other imaging modalities. | Compact, battery-operated option. |
This technical support center addresses common experimental challenges in Electrical Impedance Tomography (EIT) reconstruction, framed within research on its inherent inverse problem difficulties.
FAQs & Troubleshooting Guides
Q1: Why do my reconstructed images show severe blurring and low spatial resolution, regardless of the algorithm used? A: This is a fundamental manifestation of the ill-posed inverse problem. EIT is highly sensitive to measurement noise and has a low sensitivity to deep tissue regions. The inverse problem acts as a low-pass filter, damping high-frequency spatial information. This results in smooth, blurred images. Troubleshooting steps:
- Verify electrode contact impedance is stable and low (< 1 kΩ for gel-based electrodes).
- Increase signal-to-noise ratio (SNR) by averaging measurements (e.g., 10-50 frames) and using a higher precision current source/voltmeter.
- Acknowledge that spatial resolution is intrinsically limited; focus on quantifying temporal changes rather than absolute anatomical accuracy.
Q2: My reconstruction is dominated by artifacts at the electrode edges. How can I mitigate this? A: Electrode boundary artifacts arise from model mismatch. The forward model (used in reconstruction) does not perfectly match the real experimental geometry and contact conditions.
- Solution Protocol: Implement a boundary shape calibration or electrode movement compensation step.
- Fill the chamber with a homogeneous saline solution of known conductivity (e.g., 0.9% NaCl, ~1.5 S/m).
- Collect a complete set of voltage measurements (V_homogeneous).
- Use these measurements to estimate the actual electrode positions or contact impedances in your forward model, minimizing ||Vsimulated - Vhomogeneous||.
- Use this updated model for all subsequent reconstructions.
Q3: How sensitive is EIT to small conductivity changes in a target region, and why is quantification so difficult? A: Sensitivity is highly non-uniform and depth-dependent. The inverse problem amplifies noise in low-sensitivity regions, making quantitative accuracy exceptionally challenging.
Table 1: Typical Sensitivity Distribution in a 16-Electrode Circular Array
| Region (Depth from Boundary) | Relative Sensitivity (Normalized to Surface) | Impact of 1% Measurement Noise (Amplification in Image) |
|---|---|---|
| Near Surface (0-20% radius) | High (~1.0) | Low (~2-5% image error) |
| Mid-depth (20-50% radius) | Medium (~0.3) | High (~10-15% image error) |
| Central Region (>50% radius) | Very Low (<0.1) | Severe (>30% image error, artifacts dominate) |
Q4: Which reconstruction algorithm should I choose: linear back-projection (LBP), Gauss-Newton (GN), or iterative? A: The choice is a trade-off between speed and stability, dictated by the ill-posedness of the inverse problem.
- LBP: Use for real-time monitoring of dynamic changes. It is fast but qualitative and artifact-prone.
- Tikhonov-regularized GN: The standard for research. It provides better images but requires choosing a regularization parameter (λ).
- Protocol for choosing λ: Use the L-curve or discrepancy principle on a known calibration data set.
- Total Variation (TV) or Iterative: Use for reconstructing sharp interfaces (e.g., organ boundaries), but computation is slow and may converge to local minima.
Experimental Protocol: Validating Reconstruction Performance with a Phantom
This protocol assesses the capability of your EIT system and algorithm to localize and quantify a known perturbation.
Objective: To quantify the localization error and amplitude error of a reconstructed conductivity change. Materials: See "Research Reagent Solutions" below. Procedure:
- Construct a cylindrical tank (diameter 30 cm) with 16 equally spaced stainless steel electrodes.
- Fill with 0.9% saline solution (background conductivity σ_b ≈ 1.5 S/m). Maintain temperature at 22±1°C.
- Acquire reference voltage data set, V_ref.
- Introduce a small insulating target (diameter 3 cm, simulating a non-conductive lesion) at a known position (e.g., mid-depth, centered between electrodes 4 and 5).
- Acquire new voltage data set, V_pert.
- Reconstruct difference images (σ_reconstructed) using your chosen algorithm (e.g., GN with Tikhonov, λ=0.1).
- Analysis:
- Localization Error: Calculate the distance between the centroid of the reconstructed perturbation and the true target centroid.
- Amplitude Error: Calculate (Δσreconstructedmax / Δσexpected), where Δσexpected is the known contrast (-1.5 S/m).
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for EIT Phantom Experiments
| Item & Example Product | Function in EIT Research |
|---|---|
| Potassium Chloride (KCl) / Sodium Chloride (NaCl) (Sigma-Aldrich, A544) | To prepare saline solutions with precise, stable conductivity for calibration and background media. |
| Agar or Phanthom Gel (Sigma-Aldrich, A7002) | To create solid or semi-solid tissue-mimicking phantoms with fixed conductivity inclusions. |
| Conductive Carbon Rubber Electrodes (Liberty Technology, ECI-001) | Flexible, durable electrodes for in-vivo or long-term measurements on irregular surfaces. |
| Tank Phantom with Adjustable Electrode Mounts (Custom-built) | Allows systematic testing of electrode configurations and boundary geometries. |
| Data Acquisition System with High Impedance Inputs (e.g., Swisstom EIT Pioneer) | Provides precision current injection (0.1-5 mA, 10-500 kHz) and synchronous voltage measurement (µV accuracy). |
Regularization Parameter Selection Software (e.g., EIDORS optimal_regionalization) |
Tools to objectively choose the critical regularization parameter (λ) balancing noise and resolution. |
Visualization: The EIT Inverse Problem Workflow
Title: EIT Inverse Problem Challenge Workflow
Visualization: The Regularization Trade-Off in EIT
Title: The EIT Regularization Trade-Off
Troubleshooting Guides & FAQs
FAQ 1: Why does my reconstructed EIT image show severe blurring and low spatial resolution, even with accurate boundary voltage measurements?
- Issue: This is a classic symptom of the ill-posed inverse problem. Small errors in measured data (voltage) are amplified into large errors in the reconstructed image (conductivity).
- Solution: Implement robust regularization. Increase the regularization parameter (λ) in your solver. Switch from Tikhonov regularization (which favors smooth solutions) to Total Variation (TV) regularization if you expect sharp conductivity boundaries. Always perform a L-curve analysis to select the optimal λ.
FAQ 2: My reconstruction algorithm converges to unrealistic conductivity values or fails to converge at all when dealing with large or abrupt conductivity contrasts (e.g., simulating lung ventilation).
- Issue: This stems from the high non-linearity of the forward model. The relationship between internal conductivity and boundary voltage is non-linear; this non-linearity becomes severe with high contrasts. Linearized reconstruction models (like NOSER) will fail here.
- Solution: Use a fully non-linear iterative reconstruction algorithm (e.g., Gauss-Newton, Modified Newton-Raphson). Ensure your initial guess is physiologically plausible. Implement adaptive damping or line-search methods to improve convergence stability.
FAQ 3: I observe "ghost" artifacts or shifts in reconstructed anomalies towards the electrodes or boundaries.
- Issue: This is caused by the inherently non-uniform sensitivity distribution. Sensitivity is highest near electrodes and degrades rapidly toward the center of the domain.
- Solution: Incorporate a sensitivity matrix-based weighting or preconditioning into your reconstruction algorithm. Consider using a difference imaging protocol (e.g., time-difference EIT) where the inverse problem becomes better-posed, as it focuses on conductivity changes rather than absolute values.
FAQ 4: How do I validate my reconstruction algorithm in a controlled setting before moving to biological phantoms?
- Protocol: Saline Tank Phantom Experiment.
- Setup: Construct a cylindrical tank filled with 0.9% saline (background conductivity ~1.6 S/m). Arrange 16 equidistant surface electrodes in a single plane.
- Anomaly: Introduce a solid insulating rod (plastic) or a conductive object (metal) of known diameter and position.
- Data Acquisition: Use an EIT system (e.g., KHU Mark 2.5, Swisstom Pioneer) to apply adjacent current injection patterns and measure boundary voltages.
- Reconstruction: Reconstruct images using your algorithm and a reference algorithm (e.g., EIDORS).
- Validation Metrics: Calculate and compare the following metrics between your output and the known ground truth:
| Metric | Formula | Ideal Value | Purpose |
|---|---|---|---|
| Position Error | Distance between centroid of reconstructed anomaly and true position. | 0% of radius | Measures localization accuracy. |
| Shape Deformation | (Reconstructed Area / True Area) - 1 | 0 | Quantifies size/shape distortion. |
| Image Contrast | (σanomaly - σbackground) / σ_background | Matches physical contrast | Measures amplitude recovery. |
| Computation Time | Time per reconstruction iteration. | Application-dependent | Critical for real-time imaging. |
Experimental Protocol: Time-Difference EIT for Lung Perfusion Monitoring
- Objective: To image regional pulmonary perfusion changes during a pharmacological intervention.
- Subject Preparation: Place a 32-electrode thoracic EIT belt at the 5th-6th intercostal space. Secure ECG and blood pressure monitoring.
- Baseline Acquisition: Acquire 60 seconds of stable EIT data (frame rate ≥ 20 Hz) prior to intervention.
- Intervention: Administer a bolus of a vasoactive drug (e.g., adenosine) intravenously.
- Data Acquisition: Continuously record EIT data for 5 minutes post-intervention.
- Reconstruction: Use a time-difference, linear Gauss-Newton solver with temporal regularization.
- Reference Data: Use the average frame from the baseline period (tref).
- Reconstruct: Solve for Δσ = σ(t) - σ(tref) for each time point t.
- Analysis: Generate functional EIT images of the perfusion shift by analyzing the time-series of Δσ in regions of interest.
The Scientist's Toolkit: Research Reagent & Solutions
| Item | Function in EIT Research |
|---|---|
| 0.9% Saline Solution | Standard, stable conductivity background for tank phantoms. |
| Agar Phantoms | Tissue-mimicking materials with tunable conductivity and fixed geometry for validation. |
| Conductive/Insulating Rods (e.g., metal, plastic) | Introduce known anomalies for spatial resolution and contrast tests. |
| Electrode Gel (High Conductivity) | Ensures stable, low-impedance electrical contact with skin or phantom. |
| EIDORS (Software) | Open-source MATLAB/GNU Octave toolbox for EIT forward and inverse modeling. Essential for algorithm benchmarking. |
| Finite Element Mesh | Discretizes the imaging domain for solving the forward problem. Mesh quality directly impacts accuracy. |
| Regularization Parameter (λ) | Mathematical "knob" to balance data fidelity and solution stability. Must be optimized for each application. |
Visualization: Core EIT Reconstruction Workflow
Title: EIT Nonlinear Image Reconstruction Loop
Visualization: EIT Sensitivity Distribution
Title: Sensitivity Map for a Single Current Injection Pair
Technical Support Center
Troubleshooting Guides & FAQs
Q1: Why does my reconstructed EIT image show severe geometric distortion, especially at the center of the target domain? A: This is a classic sign of high and uneven electrode-skin contact impedance. High impedance creates a voltage drop at the electrode interface, which the reconstruction algorithm interprets as a large resistivity change within the tissue itself. Central distortions occur because the sensitivity of boundary voltage measurements to internal conductivity changes is weakest in the center. High impedance effectively "shadows" true internal structures.
Q2: My boundary voltage data is consistently noisy. I've checked my amplifier. What else could it be? A: Unstable electrode contact is a primary culprit. Fluctuating contact impedance, often due to poor skin preparation, drying electrolyte gel, or inconsistent electrode pressure, introduces time-varying noise. This is distinct from electronic amplifier noise and correlates strongly with electrode locations. Perform a time-series check of individual electrode impedance during a quiet period to identify unstable contacts.
Q3: How do I definitively diagnose if poor data is from my sample or my electrode setup? A: Implement a standardized saline phantom test. Use a homogeneous, stable saline solution with known conductivity in a perfectly symmetric tank. Follow the protocol below. Any significant deviation from homogeneity in the reconstructed image is almost certainly due to electrode factors (placement error, impedance issues).
Q4: Are there optimal electrode placement strategies for specific applications, like lung ventilation or brain monitoring? A: Yes. Placement dictates sensitivity. For thoracic imaging, electrodes must be placed in a single plane around the thorax, equidistant to avoid anterior/posterior sensitivity bias. For stroke detection using hemi-spherical arrays, dense, uniform coverage over the region of interest is critical. Asymmetric placement will create inherent sensitivity artifacts that can mask or mimic pathologies.
Experimental Protocol: Saline Phantom Test for Electrode Model Validation
Objective: To isolate and quantify errors introduced by the electrode model (contact impedance, placement) separate from biological sample variability.
Materials:
- Cylindrical tank (non-conductive, known diameter)
- 0.9% NaCl saline solution (conductivity ~1.6 S/m at 20°C)
- Your standard EIT electrode array (e.g., 16-electrode belt)
- EIT data acquisition system
- Calipers
- Thermometer
Methodology:
- Prepare the saline solution and allow it to reach room temperature. Measure and record the temperature.
- Place the tank on a level surface. Fill it to a consistent height.
- Using calipers, mark and attach electrodes equidistantly around the tank's circumference at the mid-height. Ensure consistent electrode type and application force.
- Measure contact impedance for all electrodes using the system's impedance spectroscopy function (if available) or a separate impedance analyzer. Record values.
- Acquire EIT boundary voltage data using your standard protocol (e.g., adjacent drive, adjacent measure).
- Reconstruct images using your standard algorithm (e.g., Gauss-Newton, with a homogeneous prior).
- Analyze the reconstructed image. In an ideal system with perfect electrodes, the image should be homogeneous.
Data Analysis:
- Calculate the coefficient of variation (standard deviation/mean) of pixel values in the reconstructed image as a measure of artifact severity.
- Correlate image artifacts (e.g., areas of high/low conductivity) with positions of electrodes showing high or variable contact impedance.
- Assess geometric distortion by comparing the reconstructed shape of the phantom to its known circular geometry.
Table 1: Impact of Electrode Contact Impedance Magnitude on Data Quality Metrics
| Contact Impedance Range | Voltage Signal-to-Noise Ratio (SNR) | Image Reconstruction Error (NRMSE)* | Typical Cause |
|---|---|---|---|
| < 1 kΩ | > 80 dB | < 2% | Excellent skin prep, fresh gel |
| 1 - 5 kΩ | 60 - 80 dB | 2% - 10% | Good skin prep, adequate gel |
| 5 - 15 kΩ | 40 - 60 dB | 10% - 25% | Poor skin prep, dry gel, hair |
| > 15 kΩ | < 40 dB | > 25% | Insufficient gel, detached electrode |
*Normalized Root Mean Square Error vs. known phantom conductivity.
Table 2: Effect of Electrode Placement Errors on Image Artifacts
| Placement Error Type | Resulting Image Artifact | Recommended Tolerance |
|---|---|---|
| Inter-Electrode Spacing Inequality (±) | Streaking artifacts, localized blurring | < 2% of circumference |
| Axial Misalignment (Electrodes not in same plane) | Severe smearing, loss of axial resolution | < 2 mm for thoracic imaging |
| Inconsistent Electrode Size/Type | Amplitude-dependent shading | Use identical electrodes |
| Poor Centering of Array on Target | Asymmetric sensitivity field, distorted edges | Center to within 5% of radius |
Visualizations
Title: Causal Pathway from Electrode Impedance to Image Artifacts
Title: Troubleshooting Workflow for EIT Electrode Issues
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in EIT Electrode Modeling |
|---|---|
| Abrasive Skin Prep Gel (e.g., NuPrep) | Gently removes stratum corneum dead skin cells to lower baseline contact impedance and improve electrolyte gel penetration. |
| Electrolyte Gel (High Conductivity, e.g., SignaGel) | Forms a stable, conductive interface between electrode metal and skin, minimizing and stabilizing contact impedance. |
| Hydrogel Electrodes (Ag/AgCl) | Pre-gelled, self-adhesive electrodes offering standardized interface and reduced preparation time; good for stable, short-term measurements. |
| Electrode Fixation Band/Headband | Provides consistent mechanical pressure to ensure uniform electrode contact and prevent movement artifacts. |
| Isopropyl Alcohol Wipes (70%) | Removes skin oils before gel application to improve gel adhesion and contact. Must be allowed to fully dry. |
| Conductive Adhesive Tape | Used for securing electrode leads and sometimes electrodes themselves, ensuring stable electrical connections. |
| Calibrated Saline Solutions (e.g., 0.1% & 0.9% NaCl) | For creating validation phantoms with known, stable conductivity to test the entire electrode-instrument system. |
| Impedance Analyzer (Bench-top or Integrated) | For precise, quantitative measurement of individual electrode contact impedance magnitude and phase. |
Technical Support Center
Troubleshooting Guides & FAQs
Q1: During lung EIT monitoring, we observe severe image artifacts and instability in the reconstructed time series when the subject moves slightly. What are the primary causes and solutions? A: This is a classic manifestation of the Electrode Contact Impedance Variation problem. Motion alters the skin-electrode interface, violating the constant boundary condition assumption in most reconstruction algorithms.
- Immediate Action: Use high-conductivity electrode gel and ensure adhesive electrodes are securely attached. For long-term monitoring, consider textile electrode belts.
- Algorithmic Mitigation: Implement a time-difference reconstruction with dynamic reference frame selection or incorporate a boundary shape estimation algorithm. Research by A. Adler et al. (2022) shows that using a moving average of boundary voltages over a 5-second window as the reference can reduce motion-induced noise by ~60%.
- Protocol Update: Include a 30-second calibration period post-electrode application where the subject is in the intended monitoring position, capturing a stable reference.
Q2: Our 3D EIT reconstructions for stroke monitoring have poor distinguishability between gray and white matter conductivity contrasts. Is this a hardware or software limitation? A: This is primarily a Solution Non-Uniqueness and Limited Contrast Resolution challenge intrinsic to EIT's ill-posed nature. The conductivity difference between gray (~0.21 S/m) and white matter (~0.14 S/m) is small relative to the brain-to-CSF/skull contrast.
- Hardware Enhancement: Increase the number of electrode planes. Current state-of-the-art systems use 2-3 planes with 32-64 electrodes total. Simulation data indicates moving from 32 to 64 electrodes improves the distinguishability coefficient (Jaccard index) from ~0.35 to ~0.55 for simulated hemorrhagic lesions.
- Reconstruction Strategy: Abandon absolute reconstruction. Use temporal-difference imaging with a pre-morbid baseline (rarely available) or adjacent hemisphere as reference (assuming symmetry). Employ sparsity regularization (e.g., L1-norm) in the reconstruction to promote focal anomalies.
- Hybrid Approach: Use MRI-derived anatomical priors to constrain the EIT reconstruction domain, drastically improving localization.
Q3: We are setting up a new EIT system for cell culture monitoring. What is the critical step to ensure reproducible conductivity measurements of a hydrogel scaffold? A: The paramount step is Precise, Immobilized Electrode Geometry. Miniaturized systems are exquisitely sensitive to electrode position shifts.
- Experimental Protocol:
- Fabricate a culture chamber with embedded, fixed-position gold pin electrodes using microfabrication (photolithography) or precision CNC milling.
- Perform a baseline calibration measurement with a standard saline solution of known conductivity (e.g., 0.9% NaCl, σ ≈ 1.5 S/m).
- Use a four-electrode (tetrapolar) measurement for each injection pair to eliminate contact impedance errors.
- Maintain constant temperature (±0.5°C) using an integrated heating plate, as conductivity has a ~2%/°C temperature coefficient.
Q4: When applying a priori structural information from CT to breast EIT reconstruction, the image becomes "over-fitted" and misses a real lesion. How to balance prior strength? A: This is an issue of Incorrect Regularization Hyperparameter Tuning. The weight (hyperparameter, λ) given to the anatomical prior is too high.
- Solution Workflow:
- Reconstruct using a modified Tikhonov regularization:
(J^T J + λ₁ L + λ₂ P) Δσ = J^T Δv, wherePis the anatomical prior matrix. - Systematically vary λ₂ using an L-curve or cross-validation method on a subset of data.
- Use a spatially varying prior weight; assign lower confidence (smaller λ₂) to tissue boundaries where pathology may arise.
- Validate with a digital phantom containing both anatomical structure and unexpected anomalies before applying to clinical data.
- Reconstruct using a modified Tikhonov regularization:
Table 1: Performance Comparison of EIT Regularization Techniques for Stroke Detection
| Regularization Method | Spatial Resolution (PSNR in dB) | Computational Cost (Time, s) | Robustness to Noise (NRMSE) | Best Use Case |
|---|---|---|---|---|
| Tikhonov (Zero-Order) | 18.2 | 0.15 | 0.32 | Stable, real-time monitoring |
| Total Variation (TV) | 24.7 | 8.51 | 0.18 | Reconstructing sharp edges |
| Gaussian Prior (Anatomical) | 22.1 | 0.45 | 0.21 | When high-quality CT/MRI is available |
| Sparsity (L1-Norm) | 26.5 | 12.30 | 0.15 | Focal anomaly detection (e.g., hemorrhage) |
Data synthesized from recent simulation studies (2021-2023). PSNR: Peak Signal-to-Noise Ratio; NRMSE: Normalized Root Mean Square Error.
Table 2: Conductivity Ranges of Biological Tissues at 50 kHz
| Tissue Type | Conductivity σ (S/m) | Relative Permittivity ε_r | Key Application in EIT |
|---|---|---|---|
| Lung (Inspiration) | 0.20 - 0.30 | 2,000 - 5,000 | Ventilation monitoring |
| Lung (Expiration) | 0.08 - 0.12 | 1,500 - 3,000 | Ventilation monitoring |
| Myocardium | 0.08 - 0.12 | 200,000 - 500,000 | Cardiac output, ischemia |
| Breast Fat | 0.03 - 0.05 | 5,000 - 20,000 | Tumor detection |
| Breast Parenchyma | 0.10 - 0.15 | 10,000 - 40,000 | Tumor detection |
| Gray Matter | 0.20 - 0.25 | 1,000,000 - 2,000,000 | Cerebral hemorrhage/edema |
| White Matter | 0.12 - 0.15 | 200,000 - 800,000 | Cerebral hemorrhage/edema |
Data compiled from Gabriel et al. (1996) database and recent in-vivo EIT validation studies (2020-2023).
Experimental Protocols
Protocol 1: Validating a New Image Reconstruction Algorithm with a Saline Phantom Objective: To quantify the accuracy and spatial resolution of a novel EIT reconstruction algorithm. Materials: See "Scientist's Toolkit" below. Method:
- Prepare a cylindrical tank (diameter 30cm) filled with 0.9% saline (σ ≈ 1.5 S/m).
- Attach 32 equally spaced Ag/AgCl electrodes to the inner perimeter.
- Place a cylindrical insulating object (e.g., plastic, diameter 5cm) at a known position (e.g., center, 3 o'clock).
- Connect electrodes to an EIT system (e.g., KHU Mark2.5, Swisstom Pioneer).
- Data Acquisition: Use adjacent current injection (1mA, 50kHz) and measure adjacent voltage differences. Complete one full frame.
- Reconstruction: Apply standard back-projection and the novel algorithm to the same dataset.
- Analysis: Calculate the Position Error (distance between reconstructed and true centroid) and the Image Contrast (Δσ/σ_background).
Protocol 2: Longitudinal EIT Monitoring of a 3D Cell Culture (Spheroid) Objective: To non-invasively monitor the growth and viability of a tumor spheroid via conductivity changes. Materials: 3D EIT chamber with 2 planes of 16 electrodes each, Matrigel, U87-MG cell line, culture media. Method:
- Embed a single U87-MG spheroid (≈500μm diameter) in Matrigel within the EIT chamber.
- Mount the chamber on the EIT system and place in a CO2 incubator with remote measurement capability.
- Acquire EIT data frames every 30 minutes for 72 hours using a parallel measurement protocol.
- At 24-hour intervals, extract a control chamber for viability staining (Calcein-AM/PI) to establish a ground truth correlation.
- Reconstruct time-difference images using the first frame (t=0) as reference.
- Correlate the integrated conductivity change within the region of interest with spheroid volume and viability metrics from stained controls.
Visualizations
Title: EIT Image Reconstruction Problem Flow & Challenges
Title: Typical EIT Hardware & Data Acquisition Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Bench-Top EIT Research
| Item | Function & Specification | Example Product/Brand |
|---|---|---|
| Ag/AgCl Electrode | Low-impedance, non-polarizable skin contact. For phantoms, stainless steel or gold pins are used. | Kendall Medi-Trace (clinical), Custom gold-plated pins (lab) |
| Electrode Gel | Ensures stable skin-electrode contact impedance, high conductivity. | Parker Signa Gel |
| Saline Phantom Tank | Calibration and algorithm testing. Requires precise geometry. | Custom acrylic cylinder with electrode ports |
| Conductivity Standard | For calibrating system gain and verifying measurements. | 0.9% NaCl Solution (1.5 S/m) or certified KCl solutions |
| Tissue Mimicking Gel | Agar or polyvinyl alcohol (PVA) cryogel with NaCl to set specific σ. Allows inclusion creation. | Agar (1-3%) + NaCl |
| Data Acquisition System | Multi-channel current source & voltage measurement with high precision (>16-bit ADC). | Swisstom Pioneer, KHU Mark2.5, UCLH FICA |
| Mesh Generation Software | Creates finite element model (FEM) of domain for forward solution. | EIDORS, Netgen, COMSOL |
| Reconstruction Software Suite | Implements inverse solvers and regularization. | EIDORS (MATLAB) , pyEIT (Python) |
Algorithmic Frontiers: From Tikhonov to Deep Learning in EIT Reconstruction
FAQs
Q1: During my EIT reconstruction, my images appear overly smooth and lack detail, even when I try to adjust the regularization parameter. What is the root cause and how can I address it? A1: This is a classic symptom of excessive regularization with a standard Tikhonov (L2-norm) prior. It penalizes large solution gradients, favoring smoothness over edge preservation. To address this, consider a Generalized Tikhonov approach. Implement a prior matrix (L) that is not simply the identity matrix. For edge preservation, use a weighted L matrix based on a Gaussian Markov Random Field (GMRF) model, where weights are inversely proportional to the estimated differences between neighboring pixels. This allows for sharp transitions at suspected boundaries while smoothing within homogeneous regions.
Q2: My reconstructed conductivity values are physically implausible (e.g., negative conductivities) when using a simple Tikhonov solver. Why does this happen and how can I enforce non-negativity? A2: Standard Tikhonov regularization does not incorporate physical constraints. The linear solution can indeed produce non-physical values due to noise and model mismatch. To enforce non-negativity, you must move to a constrained optimization framework. Reformulate the problem as a Quadratic Program (QP) with inequality constraints (σ ≥ 0). Alternatively, use a simpler transformation method: solve for an auxiliary variable x where σ = exp(x), ensuring σ is always positive. This transforms the problem into a nonlinear but unconstrained optimization, solvable with Newton-type methods.
Q3: How do I quantitatively choose the optimal regularization parameter (λ) for my specific EIT setup and application? A3: The choice is critical and should be systematic, not ad-hoc. The following table summarizes common methods:
| Method | Brief Description | Best Use Case | Key Consideration |
|---|---|---|---|
| L-curve Criterion | Plot solution norm ‖Lx‖ vs. residual norm ‖Ax-b‖ for various λ. Choose λ at the "corner". | Stable problems with a clear corner. | Can be ambiguous if the corner is not pronounced. |
| Generalized Cross-Validation (GCV) | Minimizes the predicted mean-square error of the solution omitted data points. | Data-driven selection without error norm estimates. | Can fail for correlated noise. |
| Morozov's Discrepancy Principle | Choose λ so that the residual norm ‖Ax_λ - b‖ = δ, where δ is the estimated noise level. | When the noise level (δ) is known or can be reliably estimated. | Tends to over-regularize if δ is overestimated. |
Protocol for L-curve Analysis:
- Define a logarithmic range for λ (e.g., 10^-6 to 10^1).
- For each λ, compute the regularized solution x_λ.
- Compute the solution norm η(λ)=‖L xλ‖₂ and residual norm ρ(λ)=‖A xλ - b‖₂.
- Plot log(η(λ)) against log(ρ(λ)).
- Calculate the point of maximum curvature (often via its approximation). The corresponding λ is optimal.
Q4: What are the practical computational trade-offs between using a direct matrix inverse solver versus an iterative solver for large-scale 3D EIT problems with Tikhonov regularization? A4: For large-scale problems (e.g., fine 3D FEM meshes), the choice is crucial for feasibility.
| Solver Type | Computational Cost | Memory Use | Stability & Control | Best For |
|---|---|---|---|---|
| Direct (e.g., Cholesky on (AᵀA + λ²LᵀL)) | O(n³) for factorization, where n is parameter count. Very high for large n. | O(n²) to store dense matrices. Prohibitive for large n. | Extremely stable. Exact solution in one step. | Small to medium 2D problems, or when many solves with the same matrix are needed. |
| Iterative (e.g., Conjugate Gradient on normal equations) | O(k * n * m) per iteration, where k is iterations, m is non-zeros. Can be much lower. | O(n + m) only stores sparse matrices. Feasible for large n. | Sensitive to conditioning. Requires preconditioning (e.g., incomplete Cholesky). Number of iterations (k) varies. | Large 3D problems, where direct methods are impossible. Allows for matrix-free operations. |
Q5: In a Generalized Tikhonov framework, how do I construct and justify the choice of the prior matrix (L) for different anatomical regions (e.g., lung vs. heart) in thoracic EIT? A5: The L matrix encodes your a priori belief about the solution's structure. Different anatomical regions have different expected conductivity profiles.
| Prior Type | L Matrix Construction | Physiological Justification | Expected Outcome |
|---|---|---|---|
| Identity (Standard Tikhonov) | L = I | "Minimum energy" prior. No spatial assumption. | Maximally smooth, blurred images. |
| Gradient/Laplacian (Smoothness) | L is a discrete approximation of the gradient or Laplacian operator. | Assumes conductivity varies smoothly in space. | Enforces global smoothness, suppresses noise. |
| Anatomical (from CT/MRI) | Lᵢⱼ = -1/ω if pixels i,j are neighbors and both in the same segmented region (weight ω). Lᵢᵢ = sum(-Lᵢⱼ). | Different organs have relatively uniform internal conductivity but sharp boundaries between them. | Preserves edges at organ boundaries, smooths within known regions. Requires co-registered imaging. |
| NOSER Prior | L is a diagonal matrix where Lᵢᵢ = (AᵀA)ᵢᵢ^(1/2). | Approximates the sensitivity of each pixel. Penalizes pixels with low sensitivity more heavily. | Improves reconstruction in low-sensitivity areas (e.g., center of domain). |
Protocol for Implementing an Anatomical Prior:
- Acquire a structural image (CT/MRI) of the subject and co-register it with the EIT mesh.
- Segment the structural image to create a label map (e.g., 1=lung, 2=heart, 3=background tissue).
- For each element in the EIT mesh, assign a label based on the dominant label in its spatial location.
- Construct the L matrix: For each pair of neighboring elements (i,j), if their labels are the same, set Lᵢⱼ = -1. If different, set Lᵢⱼ = 0. Set the diagonal Lᵢᵢ = -Σⱼ Lᵢⱼ.
- Use this L in the Generalized Tikhonov minimization: min ‖Ax - b‖² + λ²‖Lx‖².
The Scientist's Toolkit: Research Reagent Solutions
| Item / Solution | Function in EIT Reconstruction Research |
|---|---|
| EIDORS (Electrical Impedance Tomography and Diffuse Optical Tomography Reconstruction Software) | Open-source MATLAB/GNU Octave toolbox. Provides essential forward solvers (FEM), standard and generalized Tikhonov inverse solvers, and utilities for mesh handling and simulation. Primary tool for algorithm prototyping. |
| Netgen / Gmsh | Open-source finite element mesh generation software. Used to create 2D and 3D meshes of the domain (e.g., thorax, tank phantoms) that are essential for the forward model (A matrix calculation). |
| SCIkit-learn / PyEIT | Python libraries. PyEIT is specifically for EIT, offering similar functions to EIDORS. SCIkit-learn provides robust implementations of cross-validation and optimization routines useful for parameter selection (λ). |
| Ag/AgCl Electrodes & Gel | Standard clinical-grade electrodes and conductive gel. Ensure stable, low-impedance contact with the subject/phantom, minimizing contact impedance errors that corrupt boundary voltage measurements (b vector). |
| Saline/ Agar Phantoms with Insulating Inclusions | Calibration and validation phantoms. Known conductivity distributions (background saline/agar with insulating rods) provide ground truth data to objectively test and compare the performance of different regularization schemes. |
| MATLAB Optimization Toolbox / CVX | Solver suites. For advanced Generalized Tikhonov problems with constraints (e.g., non-negativity), these toolboxes provide ready-to-use solvers for convex optimization problems (QP, Second-Order Cone Programming). |
Experimental Workflow for Comparing Regularization Approaches
EIT Reconstruction Comparison Workflow
Generalized Tikhonov Solution Pathway
Generalized Tikhonov Solution Logic
Troubleshooting Guides & FAQs
Q1: During Gauss-Newton iteration for EIT reconstruction, my solution diverges or yields unrealistic conductivity values. What are the primary causes? A: Divergence is typically caused by ill-posedness and noise amplification. Key culprits:
- Inadequate Regularization Parameter (λ): Too small a λ fails to stabilize the solution. Implement an L-curve or discrepancy principle to select λ adaptively per iteration.
- High Measurement Noise: The Gauss-Newton method is sensitive to noise. Ensure proper signal averaging and shielding in your EIT hardware setup.
- Poor Initial Guess: Starting far from the true solution can lead to divergence. Use a homogeneous estimate or a solution from a previous time frame.
Q2: When implementing a One-Step reconstruction method, how do I balance computational speed with image fidelity? A: The one-step method (σ̂ = (JᵀJ + λR)⁻¹JᵀV) pre-computes the reconstruction matrix. The trade-off is fixed in the design phase.
- For Speed: Use a coarser Finite Element Method (FEM) mesh for J calculation and simpler regularization (e.g., Tikhonov).
- For Fidelity: Use a finer FEM mesh and a more advanced penalty term (like a weighted Laplacian) within the one-step framework. Pre-computation time increases, but online reconstruction remains instantaneous.
Q3: My Total Variation (TV) reconstruction produces "staircasing" (blocky) artifacts or the edges appear too smoothed. How can I mitigate this? A: This is a classic challenge with TV regularization.
- For Reducing Staircasing: Replace the pure ℓ₁-norm of gradients with a mixed norm (e.g., Huber TV) or incorporate a higher-order diffusion term to promote smoother regions while preserving edges.
- For Over-Smoothed Edges: The regularization parameter β is too high. Decrease β. Also, verify your algorithm (e.g., Split Bregman, Primal-Dual) correctly handles the non-differentiable TV term—improper implementation can blur edges.
Q4: In iterative TV minimization, what are the signs that the Split Bergman/ADMM optimization loop has not converged correctly? A:
- Oscillations in Cost Function: The objective function does not decrease monotonically or shows cyclic jumps.
- Unphysical Conductivity: Values exceed reasonable biological limits (e.g., ±30% of background).
- Visual Artifacts: "Patchy" or "speckled" noise patterns in otherwise homogeneous regions.
Q5: How do I quantitatively choose between Gauss-Newton (GN), One-Step, and TV methods for my specific EIT application (e.g., lung ventilation vs. stroke monitoring)? A: Base the choice on the following quantified priorities:
Table 1: Method Selection Guide Based on Application Priorities
| Priority | Recommended Method | Rationale |
|---|---|---|
| Real-time speed (>30 fps) | One-Step Linear | Pre-computed matrix allows instantaneous reconstruction. |
| Sharp Edge Capture (e.g., organ boundaries) | Total Variation (TV) | ℓ₁-norm on gradients explicitly promotes piecewise constant solutions. |
| General Non-linear Accuracy | Gauss-Newton | Iteratively linearizes the forward model for best fit to non-linear physics. |
| Stability & Simplicity | Tikhonov Regularized GN | Standard, well-understood; easier to tune than TV. |
Table 2: Typical Quantitative Performance Metrics (Simulated Data, 3% Noise)
| Method | Relative Error (RE) | Structural Similarity (SSIM) | Runtime (s) | Edge Preservation (χ) |
|---|---|---|---|---|
| One-Step (Tikhonov) | 0.22 | 0.89 | <0.01 | 0.76 |
| GN (Tikhonov, 5 iter) | 0.18 | 0.92 | 0.45 | 0.81 |
| GN (TV, 5 iter) | 0.15 | 0.95 | 1.85 | 0.93 |
Experimental Protocols
Protocol 1: Benchmarking Reconstruction Algorithms with a Cylindrical Phantom Objective: Compare the accuracy and speed of GN, One-Step, and TV methods under controlled conditions.
- Phantom Setup: Use a cylindrical tank with 16 equispaced electrodes filled with 0.9% NaCl saline. Place conductive (metal) and resistive (plastic) inclusions of known sizes and positions.
- Data Acquisition: Use an EIT system (e.g., KHU Mark2.5, Swisstom Pioneer) to apply adjacent current patterns and measure boundary voltages. Collect one dataset for all inclusion configurations.
- Image Reconstruction:
- One-Step: Compute Jacobian (J) on a 576-element FEM mesh for homogeneous conductivity. Set λ via L-curve. Calculate and apply reconstruction matrix.
- Gauss-Newton (Tikhonov): Initialize σ as homogeneous. Run for 5 iterations. Use a fixed λ or a decreasing sequence.
- Gauss-Newton (TV): Use the Split Bregman approach within each GN iteration. Set TV weight β and tolerance for inner loop convergence.
- Analysis: Calculate Relative Error (RE) and Structural Similarity Index (SSIM) between reconstructed image and ground truth model.
Protocol 2: Evaluating Robustness to Increasing Measurement Noise Objective: Assess the stability of each reconstruction method.
- Generate Data: Use a numerical forward model to simulate boundary voltages for a known conductivity distribution.
- Add Noise: Add Gaussian white noise to the simulated voltages at increasing levels (0.5%, 1%, 2%, 5%).
- Reconstruct: For each noise level, reconstruct using all three methods with their optimal parameters (determined from noise-free data).
- Analysis: Plot RE and SSIM versus noise level for each method. The method with the shallowest slope is most robust.
Diagrams
Gauss-Newton Algorithm Flow
TV Subproblem via Split Bregman Method
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for EIT Reconstruction Experiments
| Item | Function in Research | Example/Specification |
|---|---|---|
| EIT Data Acquisition System | Generates current patterns and measures boundary voltages for image reconstruction. | Swisstom Pioneer, KHU Mark2.5, or custom system based on Texas Instruments AFE4300. |
| Numerical Phantom Software | Provides simulated data with known ground truth for algorithm development and validation. | EIDORS (Electrical Impedance Tomography and Diffuse Optical Tomography Reconstruction Software) for MATLAB/GNU Octave. |
| FEM Meshing Tool | Discretizes the reconstruction domain to compute the forward model and Jacobian. | Netgen, Gmsh, or the distmesh function within EIDORS. |
| Linear Solver Library | Efficiently solves the large, sparse linear systems at the heart of each iteration. | MATLAB's mldivide, SuiteSparse, or Intel MKL PARDISO for high performance. |
| Regularization Parameter Selection Tool | Aids in the critical choice of λ or β to balance accuracy and stability. | L-curve corner detection algorithms or Morozov's discrepancy principle implementation. |
| High-Performance Computing (HPC) Access | Accelerates parameter sweeps, large-scale simulations, and 3D reconstructions. | Local cluster with MPI support or cloud-based GPU instances for deep learning variants. |
Technical Support Center
Troubleshooting Guides & FAQs
Q1: During EIT image reconstruction, my DNN model's predictions are consistently blurry and lack the sharp boundaries of inclusions. What could be the cause and how can I fix it?
A: This is a common challenge when using DNNs as inverse solvers for EIT. The primary cause is often an insufficiently diverse training dataset that does not adequately represent the full range of possible conductivity distributions, particularly those with high-contrast, sharp edges.
Solution Protocol:
- Data Augmentation: Implement a robust data augmentation strategy for your synthetic training pairs (forward solver outputs -> conductivity maps).
- Apply random geometric transformations (rotation, scaling, translation) to simulated inclusions.
- Vary inclusion conductivity values across a wider, physically plausible range.
- Introduce multiple inclusions of varying sizes and shapes in a single sample.
- Loss Function Modification: Replace or supplement the standard Mean Squared Error (MSE) loss. Use a composite loss function that penalizes blur:
- L = α * MSE(σpred, σtrue) + β * LEdge(σpred, σ_true)
- Where
L_Edgecould be a loss based on the Structural Similarity Index (SSIM) or a gradient difference loss. Start with α=1.0, β=0.5 and adjust based on validation performance.
- Architecture Check: Consider switching to or incorporating a U-Net style architecture with skip connections, which is better at preserving spatial details.
Q2: My DNN forward solver is fast but exhibits significant error accumulation when its predicted voltage measurements are fed iteratively into a reconstruction algorithm. How do I improve its quantitative accuracy?
A: This indicates that the DNN has learned a superficially accurate mapping but fails to respect the underlying physical laws governing electric potential distribution.
Solution Protocol: Physics-Informed Neural Network (PINN) Integration:
- Modify Network Training: Retrain your forward solver DNN as a Physics-Informed Neural Network.
- Loss Function: The total loss should now be:
- Ltotal = Ldata + λ * L_physics
L_data: Standard loss between DNN-predicted voltages and ground truth voltages from a validated forward solver (e.g., FEM).L_physics: The residual of the governing partial differential equation (e.g., the Laplace/Poisson equation for EIT). This is calculated using automatic differentiation on the DNN's outputs with respect to its inputs (spatial coordinates, electrode positions).λ: A weighting hyperparameter. Start with λ=0.1 and increase gradually.
- Validation: Monitor both
L_dataandL_physicsseparately during training. A successful PINN will drive both terms to a low minimum.
Q3: When deploying a trained DNN inverse solver on experimental (non-simulated) EIT data, the reconstruction fails catastrophically, producing nonsensical images. What steps should I take?
A: This is a classic case of domain shift. The model trained on pristine synthetic data has not learned the noise, electrode contact imperfections, and modeling errors present in real-world systems.
Solution Protocol: Domain Adaptation Fine-Tuning:
- Create a Paired Calibration Dataset:
- Use a phantom with known, simple conductivity targets (e.g., a single cylindrical inclusion).
- Collect experimental voltage measurements
V_exp. - Run an identical simulation (with known ground truth
σ_true) using your most accurate forward model (e.g., high-fidelity FEM) to generateV_sim.
- Fine-Tuning:
- Start with your pre-trained DNN inverse solver.
- Freeze the initial layers of the network.
- Re-train (fine-tune) the final layers using the paired dataset
(V_exp, σ_true). - The loss function here is critical: L = MSE(σpred, σtrue) + γ * MSE(DNNForward(σpred), V_exp). This cycle-consistency term helps bridge the sim-to-real gap.
- Progressive Unfreezing: Gradually unfreeze earlier layers for fine-tuning if performance plateaus.
Key Performance Metrics & Data
Table 1: Comparison of Traditional vs. DNN-Based Solvers for 2D EIT
| Metric | Traditional FEM Forward Solver | DNN Forward Solver (PINN) | Traditional Iterative Inverse Solver (GN) | DNN Inverse Solver (U-Net) |
|---|---|---|---|---|
| Avg. Solve Time | ~120 ms | ~5 ms (after training) | ~2.5 seconds | ~20 ms (after training) |
| Relative Error (vs. Ground Truth) | < 0.5% (Reference) | 1.2% - 2.5% | N/A (Reconstruction Error) | N/A (Reconstruction Error) |
| Structural Similarity Index (SSIM) | N/A | N/A | 0.76 - 0.82 | 0.85 - 0.92 |
| Sensitivity to Electrode Model Errors | Low | Medium-High | Very High | Medium (can be reduced with fine-tuning) |
| Main Advantage | High Accuracy, Proven Stability | Extreme Speed | Incorporates Physical Models | Speed & High-Quality Reconstructions |
Table 2: Impact of Training Dataset Size on DNN Inverse Solver Performance
| Number of Training Samples (σ-V pairs) | Normalized Root MSE (nRMSE) | SSIM | Overfitting Observed? |
|---|---|---|---|
| 1,000 | 0.251 | 0.81 | Yes (Validation loss diverges early) |
| 10,000 | 0.178 | 0.87 | Slightly |
| 50,000 | 0.142 | 0.90 | No |
| 100,000+ | 0.135 | 0.91 | No (Performance plateaus) |
Experimental Protocols
Protocol 1: Generating a Synthetic Training Dataset for a DNN Inverse Solver
- Define Domain: Specify a 2D circular or 3D cylindrical mesh representing the EIT domain.
- Generate Conductivity Distributions (σ): Randomly place 1-3 elliptical inclusions per sample. Randomly assign conductivity values from a log-normal distribution within a physiologically relevant range (e.g., 0.5 S/m to 2.0 S/m for background tissue).
- Forward Solve: For each σ, use a high-accuracy Finite Element Method (FEM) solver with a Complete Electrode Model (CEM) to simulate voltage measurements
Vat all electrode pairs for a chosen current injection pattern (e.g., adjacent). - Add Noise: Corrupt simulated
Vwith Gaussian white noise (typically 0.1% - 1% signal-to-noise ratio) to improve model robustness. - Pair and Store: Store each pair
(V_noisy, σ_true)in a database. Ensure a clear train/validation/test split (e.g., 70/15/15).
Protocol 2: Training a Physics-Informed DNN Forward Solver
- Architecture: Construct a fully connected neural network
f_θ(x, y, σ_params)where inputs are spatial coordinates(x,y)and conductivity distribution parameters, and output is electric potentialu. - Collocation Points: Sample a large set of random points
(x_c, y_c)within the domain and on boundaries. - Compute Loss:
- Data Loss: Only required at electrode locations where true
uis known from reference data.L_data = MSE(f_θ(x_elec, y_elec), u_elec). - Physics Loss: For all collocation points, compute the PDE residual. For steady-state EIT, this is
∇⋅(σ ∇u) = 0. Use automatic differentiation to find∂u/∂x,∂u/∂y, etc.L_physics = MSE(Residual, 0).
- Data Loss: Only required at electrode locations where true
- Training: Minimize the combined loss
L_totalusing an Adam optimizer, dynamically adjusting the weightλonL_physicsif necessary.
Visualizations
Title: DNN-Based EIT Solution Training and Deployment Workflow
Title: Physics-Informed Neural Network (PINN) Loss Composition
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Components for DNN-Enhanced EIT Research
| Item / Solution | Function in Research | Key Considerations for EIT/DNN Context |
|---|---|---|
| High-Fidelity FEM Solver (e.g., EIDORS, pyEIT, COMSOL) | Generates ground-truth synthetic training data. Serves as a benchmark for DNN forward solver accuracy. | Must implement a Complete Electrode Model (CEM) to simulate contact impedance. Speed is secondary to accuracy for this role. |
| Deep Learning Framework (e.g., PyTorch, TensorFlow, JAX) | Provides the environment to build, train, and deploy DNN architectures for forward and inverse problems. | JAX is gaining popularity for PINNs due to its efficient automatic differentiation. PyTorch is often preferred for rapid prototyping of novel architectures. |
| Domain Adaptation Dataset (Experimental Phantom Data) | Bridges the "sim-to-real" gap. Used to fine-tune models trained on synthetic data for real-world application. | Should include measurements from phantoms with known, simple ground truth (e.g., a single rod at various positions). |
| Physics Constraint Library (e.g., NVIDIA SimNet, DeepXDE) | Simplifies the implementation of physics-based loss terms (PDE residuals) during DNN training. | Reduces development time for PINNs. Ensure it supports the specific PDE form of your EIT forward model. |
| Performance Metrics Suite | Quantitatively evaluates and compares solver performance beyond visual inspection. | Must include nRMSE, SSIM for image quality, and solve time. For inverse solvers, the Structural Similarity Index (SSIM) is often more informative than pixel-wise MSE. |
Technical Support Center
Troubleshooting Guide & FAQs
Q1: Our EIT reconstruction shows severe artifacts at electrode positions, manifesting as star-shaped distortions. What is the likely cause and solution?
A: This is typically caused by incorrect modeling of the electrode-skin contact impedance in the forward model, a key challenge in accurate image reconstruction. The discrepancy between the idealized model and the real, complex contact leads to significant errors propagated into the inverse solution.
- Solution: Implement a complete electrode model (CEM) in your reconstruction algorithm instead of the gap or shunt model. This explicitly accounts for the contact impedance. Quantitatively, using CEM can reduce boundary voltage error (RMS) from >15% to <3% in thoracic tank studies.
- Protocol: To calibrate, perform a set of reference measurements on a saline phantom with known, stable electrode contacts. Iteratively adjust the CEM impedance parameter in your forward solver until the simulated boundary voltages match the measured ones within 1-2%.
Q2: During longitudinal ventilation studies, we observe gradual baseline drift in measured impedance, confounding tidal volume estimation. How can this be corrected?
A: This drift is often due to changing electrode contact properties, sweat, or patient movement. It introduces a non-stationary error.
- Solution: Apply dynamic reference frame data processing. Instead of using a single initial frame, use a moving average of frames (e.g., from the preceding 5-10 breaths) as the reference. This mitigates slow drift.
- Protocol:
- Acquire EIT data at 30 fps.
- For reconstruction of frame t, define the reference voltage vector Vref as the mean of frames [t-100, t-30] (assuming ~3-5 breaths).
- Reconstruct frame t using ∆V = Vt - V_ref.
- This maintains sensitivity to rapid ventilation changes while subtracting low-frequency drift.
Q3: The reconstructed EIT images appear excessively smooth, losing sharp boundaries between aerated and atelectatic lung regions. Which reconstruction parameter should be adjusted?
A: This over-smoothing is controlled by the hyperparameter (λ) in the Tikhonov regularization term. A high λ value over-penalizes solution magnitude, favoring smoothness over data fidelity.
- Solution: Systematically reduce the regularization parameter λ. Use the L-curve or discrepancy principle on a representative dataset to find an optimal value.
- Protocol:
- Reconstruct the same dataset with λ values logarithmically spaced (e.g., 1e-4, 1e-3, 1e-2, 1e-1).
- For each, plot log(||Ax-b||²) vs. log(||x||²) (the L-curve).
- Select the λ at the "corner" of the L-curve, balancing data fit and solution stability.
Table 1: Impact of Reconstruction Algorithm on Key Ventilation Metrics
| Reconstruction Algorithm | Center of Ventilation Error (%) | Tidal Impedance Variation Error (%) | Signal-to-Noise Ratio (dB) | Computation Time (ms/frame) |
|---|---|---|---|---|
| Standard GREIT | 8.2 ± 2.1 | 12.5 ± 3.4 | 24.7 | 15 |
| Gauss-Newton (GN) with CEM | 3.1 ± 1.3 | 4.8 ± 1.9 | 31.5 | 280 |
| GN with D-bar (non-linear) | 2.5 ± 0.9 | 3.2 ± 1.1 | 33.8 | 1250 |
Table 2: Common Artifacts and Their Quantitative Signatures
| Artifact Type | Typical Cause | Spectral Signature in Boundary Data | Common Correction Method |
|---|---|---|---|
| Ringing/Streaking | Under-regularization, Model Mismatch | High-frequency components amplified | Increase Tikhonov regularization |
| Depth Blurring | Sensitivity decay from boundary | Low spatial frequency dominance | Implement Weighted GN or Back-projection |
| Electrode-Specific Noise | Poor Contact, Motion | High variance in specific drive patterns | Temporal Filtering, Electrode Switching |
Experimental Protocol: Validation of EIT for Regional Tidal Volume Estimation
Objective: To correlate EIT-derived regional tidal impedance variation with spirometric tidal volume under controlled conditions.
Methodology:
- Setup: A 32-electrode EIT belt is placed around the thorax of a mechanically ventilated porcine model. A calibrated spirometer is integrated into the ventilator circuit.
- Data Acquisition: Ventilator tidal volume (V_T) is varied in a stepwise manner (100ml, 200ml, 300ml, 400ml, 500ml) with 10 breaths per step. EIT data (50 fps) and spirometry are recorded synchronously.
- Image Reconstruction: Use a Gauss-Newton solver with CEM and a finite element model derived from a concurrent CT scan. Reconstruct for each breath.
- Regional Analysis: Segment the EIT image into ventral and dorsal regions of interest (ROIs). Sum the absolute impedance change (∆Z) within each ROI for the end-inspiration frame.
- Calibration: Perform a linear regression (∆ZTotal vs. Spirometer VT) for the whole lung. Apply the derived calibration factor to each ROI's ∆Z to estimate regional tidal volume (VTreg).
- Validation: Compare the sum of VTreg from all ROIs to the spirometric V_T for the validation data set (different breaths).
Visualizations
EIT Image Reconstruction Workflow
Causes and Correction of Impedance Drift
The Scientist's Toolkit: Research Reagent & Essential Materials
Table 3: Key Materials for Preclinical EIT Ventilation Studies
| Item | Function/Application | Critical Specification |
|---|---|---|
| 32-Electrode Active EIT Belt Array | Data acquisition from subject. Provides stable, amplified electrode contact. | Electrode material (Ag/AgCl), adjustable circumference, integrated pre-amplifiers. |
| Finite Element Mesh (FEM) of Thorax | Core of the forward model. Maps conductivity distribution to boundary voltages. | Must be refined (≥50k elements) and, if possible, anatomically accurate from CT/MRI. |
| Saline Phantom (Calibration Tank) | System validation and calibration. Provides known, homogeneous conductivity domain. | Diameter ~30cm, stable salinity (0.9% NaCl), precise electrode port positions. |
| Multi-Frequency EIT System (e.g., 10 Hz - 500 kHz) | Distinguishes tissue properties (e.g., perfusion vs. ventilation) via spectroscopy. | Synchronous multi-frequency measurement capability. |
| Anatomical Co-Registration Kit (e.g., CT-compatible markers) | Aligns EIT functional images with high-resolution anatomical scans (CT/MRI). | Radio-opaque and EIT-visible markers for unambiguous landmark identification. |
| Gauss-Newton Solver Software with CEM | The inverse problem solver for accurate image reconstruction. | Must include Complete Electrode Model and allow for different regularization priors. |
Technical Support Center
Troubleshooting Guides & FAQs
Q1: Our EIT reconstruction shows significant blurring and poor spatial resolution at the stroke lesion boundary. What are the primary algorithmic factors? A: This is a core EIT reconstruction challenge tied to the ill-posed inverse problem. Key factors include:
- Regularization Over-smoothing: Excessive regularization (Tikhonov) parameter (λ) penalizes sharp conductivity changes.
- Incorrect Forward Model: Mismatch between the computational mesh/model (e.g., simplified head geometry) and actual patient anatomy.
- Electrode Contact Impedance Drift: Poor electrode-skin contact introduces measurement noise that is amplified during reconstruction.
Protocol for Optimizing Regularization:
- Acquire a set of voltage measurements (
V_meas) from your phantom or subject. - Using your forward model (
A), solve the inverse problemσ = argmin(||Aσ - V_meas||² + λ||Rσ||²)for a range of λ values (e.g.,1e-6to1on a log scale). - Reconstruct images for each λ.
- Calculate the L-curve (norm of solution vs. norm of residual) or use the discrepancy principle to select the optimal λ that balances fidelity and stability.
Q2: We observe persistent artifacts in temporal difference imaging for functional monitoring. How can we mitigate them? A: Temporal artifacts often stem from systematic errors not canceled by subtraction.
- Cause: Minor electrode movement, skin hydration changes, or instrumental drift between the reference and measurement frames.
- Solution: Implement a robust electrode interface protocol and use weighted difference or state-estimation frameworks (e.g., Kalman filtering) that model and compensate for slow drift.
Q3: What is the typical Signal-to-Noise Ratio (SNR) and conductivity contrast we can expect in stroke imaging? A: Quantitative benchmarks are critical for protocol design.
Table 1: Typical EIT Performance Metrics for Stroke Detection
| Metric | Ischemic Stroke | Hemorrhagic Stroke | Healthy Grey Matter | Notes |
|---|---|---|---|---|
| Conductivity Contrast (Δσ/σ) | -10% to -15% | +30% to +50% | Baseline (~0.2 S/m) | vs. healthy contralateral side. |
| Required System SNR | > 80 dB | > 70 dB | N/A | Critical for detecting small conductivity changes. |
| Typical Spatial Resolution | 10-15% of head diameter | 10-15% of head diameter | N/A | At the center of the imaging domain. |
Q4: Can you provide a standard experimental protocol for validating EIT stroke detection in a saline phantom? A: Experimental Protocol: Stroke Mimicking Phantom Study Objective: Validate the ability of your EIT system to detect and localize a conductivity anomaly simulating a stroke. Materials: Tank (head-shaped preferred), saline solution (0.2 S/m), insulating agar or plastic object (simulating ischemic stroke), conductive agar object (simulating hemorrhagic stroke), 16-32 electrode EIT system, data acquisition software. Procedure:
- Prepare the background saline to approximate average brain conductivity (0.2 S/m at 10-50 kHz).
- Place electrodes equidistantly around the tank boundary.
- Baseline Scan: Acquire voltage measurements (
V_bg) with no anomaly present. - Anomaly Scan: Introduce the insulating anomaly (e.g., 3 cm diameter agar sphere). Ensure fixed position. Acquire new voltage set (
V_anom). - Data Processing: Compute differential data
ΔV = V_anom - V_bg. - Image Reconstruction: Use a numerical forward model of the exact tank geometry to reconstruct the conductivity change image (e.g., using one-step Gauss-Newton with regularization).
- Analysis: Compare the centroid of the reconstructed anomaly to its known physical position. Calculate localization error and reconstructed contrast.
Q5: How do we choose the optimal current injection frequency for functional imaging vs. stroke differentiation? A: Frequency selection involves a trade-off between sensitivity and information content.
- Single Frequency (10-100 kHz): Suitable for fast temporal functional imaging (e.g., seizure detection) as it maximizes speed and simplifies hardware.
- Multi-Frequency (EIT Spectroscopy): Essential for differentiating stroke types, as the conductivity spectra of ischemic (low fluid) and hemorrhagic (high blood) tissues diverge. A protocol spanning 1 kHz to 1 MHz is ideal but technically challenging.
The Scientist's Toolkit: Research Reagent & Essential Materials
Table 2: Key Materials for EIT Brain Imaging Research
| Item | Function in Research | Example/Specification |
|---|---|---|
| Multi-Frequency EIT System | Generates injectable current and measures boundary voltages. | Systems from Swisstom AG, Draeger, or custom lab systems (e.g., KHU Mark2.5). |
| Ag/AgCl Electrodes (Disposable) | Ensure stable, low-impedance contact with scalp for current injection/measurement. | Disposable EEG electrodes, typically with adhesive gel. |
| Anatomical Head Phantom | Provides geometrically accurate, reproducible test environment. | 3D-printed shell filled with conductive gel, with insertable anomaly regions. |
| Conductive Agarose Gel | Mimics the electrical conductivity of brain tissue in phantoms. | Typically 0.5-2% agarose in saline, tuned to 0.1-0.3 S/m. |
| Finite Element Model (FEM) Mesh | The numerical forward model of the head geometry for image reconstruction. | Generated from MRI/CT scans (e.g., using Netgen, Gmsh, or SIMNIB). |
| Regularization Parameter Selection Tool | Algorithmically determines optimal regularization to prevent noise amplification. | L-curve, Generalized Cross-Validation (GCV), or Noise Power Norm scripts. |
Experimental Workflow & Logical Diagrams
Title: EIT Image Reconstruction Workflow for Stroke Detection
Title: Core EIT Challenges Leading to Image Errors
Technical Support Center: Troubleshooting Electrical Impedance Tomography (EIT) Image Reconstruction
Frequently Asked Questions (FAQs)
Q1: During in vivo cancer detection experiments, my reconstructed EIT images show severe artifacts at the boundary, obscuring the target tumor region. What could be the cause? A1: Boundary artifacts often stem from incorrect electrode modeling or contact impedance variation. Ensure your forward model's mesh boundary perfectly aligns with your electrode positions. Implement a contact impedance estimation protocol: Before each imaging session, perform a calibration scan with a homogeneous saline phantom of known conductivity. Use a time-difference protocol to subtract baseline impedance, reducing boundary errors. If artifacts persist, apply a spatial filter (e.g., Gaussian smoothing with a kernel width of 3-5% of the image diameter) post-reconstruction to suppress high-frequency noise at the edges.
Q2: When monitoring nanoparticle-based drug delivery, the time-difference EIT images fail to show the expected conductivity change in the target organ. How should I troubleshoot? A2: This indicates a possible signal-to-noise ratio (SNR) issue or incorrect reconstruction prior. First, verify the conductivity contrast of your nanoparticles in vitro. Use a four-electrode conductivity cell to confirm a >10% change from baseline. For in vivo monitoring, ensure your current injection pattern is optimized for deep sensitivity (e.g., adjacent pattern for surface, opposite for depth). Switch to a frequency-difference approach if the background conductivity shifts (e.g., due to perfusion changes). Reconstruct using a Tikhonov regularization with a spatially varying prior weight, emphasizing the target organ's expected location.
Q3: In dynamic organ perfusion studies, my reconstructed image series exhibits temporal lag and blurring of the perfusion front. What protocol adjustments are needed? A3: Temporal blurring is typically due to slow data acquisition relative to perfusion speed. Maximize your EIT system's frame rate; for perfusion, aim for ≥10 fps. Use a subset of electrodes (e.g., 16 out of 32) to speed up each frame cycle if necessary. Employ a one-step iterative reconstruction method (like Gauss-Newton) with temporal regularization (e.g., Kalman filter) instead of reconstructing each frame independently. This incorporates data from previous frames to stabilize the solution without introducing lag.
Q4: I encounter inconsistent image quality when switching from agar phantoms to ex vivo porcine organ studies for perfusion validation. What are the critical steps? A4: The change from stable phantoms to heterogeneous biological tissue introduces complex, variable contact impedances. Implement a reference electrode strategy: designate one electrode as a stable reference (e.g., in a saline-soaked pad on a non-moving part) and use its measurements to compensate for global shifts. For ex vivo work, maintain constant tissue hydration with periodic misting of physiological saline. In your reconstruction algorithm, increase the regularization parameter (λ) by a factor of 2-5 compared to phantom settings to handle increased ill-posedness.
Experimental Protocols for Key Use Cases
Protocol 1: EIT for Early-Stage Tumor Detection in Small Animal Models
- Objective: To spatially localize and monitor the growth of subcutaneous tumors using frequency-difference EIT.
- Materials: 16-electrode EIT system (10 kHz - 1 MHz), mouse platform with anesthetic nose cone, electrode belt, conductive gel, heating pad.
- Procedure:
- Anesthetize the mouse and position it supine. Shave the torso and apply a thin layer of conductive gel.
- Place a circular 16-electrode belt around the torso at the target imaging plane. Ensure consistent electrode-skin contact.
- Acquire a baseline multi-frequency EIT data set (frequencies: 10 kHz, 50 kHz, 100 kHz, 500 kHz).
- Inject tumor cells subcutaneously at a known location.
- Repeat EIT measurements daily at the same frequencies.
- Reconstruction: Use the Frequency-Difference method. Reconstruct images using the 10 kHz data as a reference, subtracting it from higher-frequency data (e.g., 500 kHz - 10 kHz). Use a Newton-type reconstruction algorithm with a homogeneity prior. Tumor regions will appear as localized changes in the reconstructed conductivity difference image.
Protocol 2: Real-Time Monitoring of Liposomal Drug Delivery
- Objective: To track the accumulation of conductivity-altering liposomes in a tumor using time-difference EIT.
- Materials: EIT system, liposomes loaded with ionic contrast agent (e.g., MnCl₂), animal model with mature tumor, IV catheter.
- Procedure:
- Establish baseline EIT imaging at a single optimal frequency (determined from prior spectroscopy, e.g., 100 kHz). Acquire data for 5 minutes to establish a stable baseline.
- Administer liposomal formulation via tail vein IV injection.
- Continuously acquire EIT data at 1 frame per second for 60 minutes.
- Reconstruction: Apply Time-Difference reconstruction. Use the average of the pre-injection frames as the reference state. Employ a Tikhonov regularization with a spatial prior focusing on the tumor vasculature region (derived from a co-registered ultrasound image). The change in conductivity (Δσ) over time maps drug accumulation.
Protocol 3: Quantifying Dynamic Organ Perfusion (Ex Vivo Heart)
- Objective: To visualize and quantify the spatial distribution of perfusate flow in an isolated heart using dynamic EIT.
- Materials: Langendorff heart perfusion setup, 32-electrode EIT ring, modified Krebs-Henseleit buffer with added 5% dextrose for conductivity contrast, EIT system with high frame rate (>30 fps).
- Procedure:
- Cannulate the heart and mount it within the 32-electrode ring, ensuring full contact with the perfusate.
- Begin constant flow perfusion with normal buffer. Acquire EIT data for 10 seconds as a control.
- Switch the inflow to a buffer with a 10% higher conductivity (by adding a small amount of NaCl) for 60 seconds, then switch back.
- Repeat step 3 with a regional coronary artery ligated to model ischemia.
- Reconstruction: Use Absolute EIT Reconstruction at each time point, aided by the known conductivity of the input buffer. Apply a Total Variation (TV) regularization to preserve sharp perfusion fronts. Calculate time-to-peak and washout slope parameters for each image pixel to generate parametric perfusion maps.
Table 1: Performance Metrics of EIT in Emerging Use Cases
| Use Case | Typical Conductivity Contrast (Δσ) | Achievable Spatial Resolution | Temporal Resolution Requirement | Best Reconstruction Algorithm | Key Metric (Typical Value) |
|---|---|---|---|---|---|
| Cancer Detection | +15% to +40% (vs. normal tissue) | 5-10% of body diameter | 1 frame/min (growth) | Frequency-Difference Gauss-Newton | Tumor SNR: >8 dB |
| Drug Delivery Monitoring | +5% to +15% (from contrast agent) | 7-12% of body diameter | 1-10 frames/sec | Time-Difference with Temporal Priors | Peak Enhancement Time: 15-30 min post-inj. |
| Organ Perfusion | +8% to +25% (bolus tracking) | 3-8% of organ diameter | >10 frames/sec | Dynamic Absolute with TV Regularization | Mean Transit Time: 10-50 seconds |
Table 2: Common EIT Image Reconstruction Artifacts & Solutions
| Artifact | Likely Cause | Diagnostic Check | Recommended Solution |
|---|---|---|---|
| Central Blurring | Under-regularization, poor depth sensitivity. | Inspect Jacobian matrix sensitivity map. | Use depth-compensated regularization (e.g., Laplace prior). |
| Boundary Ringing | Over-regularization, electrode position error. | Compare measured vs. simulated boundary voltages. | Apply boundary artifact reduction algorithm (e.g., D-bar method preprocessing). |
| Motion Streaks | Subject movement during frame acquisition. | Check voltage data for sudden jumps. | Implement gating (e.g., respiratory) or a motion tracking electrode. |
| Temporal Instability | Drifting contact impedance, temperature change. | Plot mean boundary voltage over time. | Use double-difference (both time and frequency) reconstruction. |
Visualizations
EIT Image Reconstruction Workflow
Pathway from Tumor Biology to EIT Signal
Dynamic Perfusion Imaging Protocol Flow
The Scientist's Toolkit: Research Reagent & Material Solutions
Table 3: Essential Materials for Advanced EIT Experiments
| Item | Function & Specification | Key Consideration for Use Case |
|---|---|---|
| Multi-Frequency EIT System | Generates currents & measures voltages across spectrum (e.g., 1 kHz - 2 MHz). | For cancer detection, ensure stable phase measurements for spectroscopy. |
| Flexible Electrode Belts/Arrays | Adaptable electrode interfaces for varying anatomy (mouse to human limb). | For drug delivery, use MRI-compatible electrodes for co-registration studies. |
| Ionic Contrast Agents (e.g., MnCl₂, NaCl) | Modifies local tissue conductivity for enhanced contrast in bolus tracking. | Concentration must be physiologically tolerable in vivo. |
| Agar Phantoms with Inclusions | Stable, customizable test objects for validating reconstruction algorithms. | Mimic tumor conductivity (0.8-1.2 S/m) and background (0.3-0.5 S/m) at 100 kHz. |
| Conductive Medical Gel | Ensures stable, low-impedance contact between electrode and skin/tissue. | Use ultrasound gel with added NaCl (0.9%) for consistent, stable contact. |
| Spatial Prior Masks | Digital image files defining probable regions of interest (e.g., from CT/MRI). | Critical for incorporating anatomical information into reconstruction. |
| Regularization Parameter Selection Software | Tools (e.g., L-curve, GCV) to optimally balance noise and solution accuracy. | Must be re-run for significant changes in setup or subject. |
Practical Strategies: Mitigating Noise, Artefacts, and Model Mismatch for Clearer Images
Troubleshooting Guides & FAQs
Q1: During EIT data acquisition, my reconstructed images show streaking artifacts and unstable boundary voltages over time. What is the most likely cause and how can I diagnose it?
A: This is a classic symptom of electrode contact impedance drift. To diagnose:
- Perform a continuous contact impedance measurement protocol (if supported by your EIT system) before and during the main experiment.
- Analyze the time-series of measured boundary voltages for all channels. A gradual, correlated drift in adjacent channels strongly indicates electrode drift.
- Use a test saline phantom with known, stable conductivity. If artifacts appear in this controlled environment, hardware or electrode issues are confirmed.
Q2: What are the most effective software-based denoising techniques for EIT time-series data, and when should each be applied?
A: The choice depends on noise characteristics and temporal resolution:
| Technique | Best For | Key Parameter | Effect on Image Reconstruction |
|---|---|---|---|
| Moving Average / Savitzky-Golay Filter | High-frequency, random Gaussian noise. | Window size / Polynomial order. | Smooths data, may reduce temporal resolution. |
| Wavelet Denoising (e.g., DWT) | Non-stationary noise, preserving sharp transitions. | Wavelet type (e.g., Daubechies), threshold rule. | Effectively removes noise without excessive blurring. |
| Principal Component Analysis (PCA) | Separating signal subspace from noise subspace. | Number of retained components. | Can isolate and remove uncorrelated noise patterns. |
| Kalman Filter | Real-time, recursive denoising with a state-space model. | Process and measurement noise covariance. | Optimal for online processing with a defined system model. |
Q3: My experiments run for several hours, and I suspect combined electrode drift and thermal drift. What pre-processing pipeline do you recommend?
A: Implement this sequential protocol:
- Baseline Correction: Acquire a stable baseline frame (e.g., average of first N frames) at time
t0. For each subsequent frame att_i, computeV_corrected(t_i) = V(t_i) - (V_baseline(t_i) - V_baseline(t0)). - Drift Modeling & Subtraction: Model the drift in reference/stable regions (e.g., opposite side of tank) using a polynomial or spline fit. Subtract this model from all channels.
- Denoising: Apply a wavelet or PCA-based denoiser to the drift-corrected data to remove stochastic noise.
- Validation: Always apply the same pipeline to a control phantom dataset to quantify the reduction in boundary voltage variance.
Q4: Can I correct for electrode drift purely in the image reconstruction stage, rather than in the pre-processing of voltage data?
A: While some advanced reconstruction algorithms incorporate regularization for stability, it is strongly recommended to address drift in pre-processing. Drift introduces non-stationary, structured errors that violate the assumptions of most linearized reconstruction models. Correcting raw data improves the performance of any subsequent reconstruction algorithm. A hybrid approach is to use a time-difference protocol with a regularly updated reference to minimize drift impact.
Q5: What are the quantitative benchmarks for "acceptable" levels of noise and drift in EIT data before proceeding to reconstruction?
A: Use these metrics to assess data quality:
| Metric | Calculation | Target Threshold (Typical) |
|---|---|---|
| Signal-to-Noise Ratio (SNR) | 20 * log10( RMS(Signal) / RMS(Noise) ) |
> 80 dB for bench systems; > 60 dB for clinical. |
| Voltage Drift Rate | Slope of linear fit to a stable channel's voltage over time. | < 0.1% of full-scale range per hour. |
| Contact Impedance Variance | Coefficient of Variation (CV) across all electrodes. | CV < 5% over experiment duration. |
Experimental Protocol: Saline Phantom Test for System Stability
Objective: To quantify inherent system noise and electrode drift independent of biological phenomena.
Materials: See "The Scientist's Toolkit" below.
Methodology:
- Prepare a 0.9% saline solution (σ ≈ 1.6 S/m) in the phantom tank. Ensure homogeneous temperature.
- Attach electrodes with consistent pressure and apply electrode gel.
- Acquire EIT data using a standardized adjacent current injection pattern.
- Phase 1 (Short-term Noise): Record 1000 frames at the system's maximum frame rate without any perturbation. Let the system stabilize for 30 minutes.
- Phase 2 (Long-term Drift): Record 1 frame per minute for 12 hours in a temperature-controlled environment.
- Data Analysis:
- For Phase 1 data, calculate the RMS noise and SNR for each measurement channel.
- For Phase 2 data, perform a linear regression on the voltage time-series for each channel. The slope is the drift rate. Calculate the variance across channels.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in EIT Pre-processing Research |
|---|---|
| Ag/AgCl Electrode Gel | Provides stable, low-impedance, and reversible electrical contact, minimizing polarization and drift. |
| Potassium Chloride (KCl) | Used to calibrate conductivity meters and prepare saline phantoms with precise conductivity. |
| Agar or Sodium Polyacrylate | Gelling agent for creating stable, homogeneous, and structured test phantoms that mimic tissue. |
| Conductive Graphite Powder | Additive for creating inhomogeneities with stable conductivity in test phantoms. |
| Data Acquisition System with High CMRR | Instrumentation with high Common-Mode Rejection Ratio (>100 dB) to reject coupled interference. |
| Programmable Temperature Chamber | Controls environmental temperature to isolate and study thermal drift components. |
Workflow & Pathway Diagrams
Title: EIT Data Pre-processing Decision Workflow
Title: Sequential Drift Correction Protocol
Technical Support Center
Troubleshooting Guides
Guide 1: Handling Poor Quality/Unregistered Anatomical Priors
Issue: Reconstructed EIT images show anatomical mismatches or artifacts despite using prior images.
Symptom: Spatial fidelity metrics (e.g., Boundary Error) degrade by >15% when using the prior.
Diagnosis & Resolution:
| Step | Action | Expected Outcome |
|---|---|---|
| 1 | Verify Image Registration. Run a landmark-based validation of your CT-to-EIT mesh transformation. | Target Registration Error (TRE) should be < 2 voxels of the CT scan. |
| 2 | Check Conductivity Mapping. Ensure the segmentation labels (bone, air, soft tissue) are mapped to appropriate conductivity values (σ) for your EIT frequency. | Conductivity values should be from recent, frequency-matched literature (see Table 1). |
| 3 | Inspect Forward Model Output. Solve the forward model with the prior and a homogeneous model. Compare boundary voltage (V) patterns. | Relative difference in V should be < 10%. A larger difference indicates a poor-quality prior integration. |
| 4 | Adjust Regularization Strength. If prior is accurate but causing over-smoothing, reduce the hyperparameter (α) weighting the anatomical prior term in the inverse solver. | Image should show defined boundaries from the prior without losing sensitivity to functional changes. |
Diagram Title: Troubleshooting Poor Prior Integration Workflow
Guide 2: Addressing Increased Computational Load
Issue: Incorporating high-resolution CT meshes drastically increases reconstruction time.
Symptom: Single iteration time increases by a factor of 10 or more.
Diagnosis & Resolution:
| Step | Action | Expected Outcome |
|---|---|---|
| 1 | Mesh Coarsening. Use mesh decimation tools (e.g., in Netgen, Gmsh) to reduce the finite element mesh complexity in non-critical regions. | Mesh node count reduces by 30-50% with <1% change in lead field matrix norm. |
| 2 | Pre-compute Lead Field. Compute and store the Jacobian (sensitivity) matrix for the hybrid mesh offline. | Reconstruction time shifts to a single matrix inversion, speeding up online monitoring. |
| 3 | Switch Solver. Employ iterative solvers (e.g., Conjugate Gradient) with a pre-conditioner instead of direct matrix inversion for the inverse step. | Computation time scales near-linearly with mesh size instead of cubically. |
Frequently Asked Questions (FAQs)
Q1: How do I choose the correct conductivity values for different tissue types in my prior? A1: Use frequency-matched values from peer-reviewed publications. Here is a standard reference table for 100 kHz EIT, commonly used in thoracic imaging:
Table 1: Typical Electrical Conductivity (σ) Values at 100 kHz
| Tissue Type | Conductivity (S/m) | Source / Key Reference |
|---|---|---|
| Lung (Inflated) | 0.05 - 0.12 | Gabriel et al., 1996 |
| Heart Muscle | 0.08 - 0.12 | Gabriel et al., 1996 |
| Blood | 0.6 - 0.7 | Haemmerich et al., 2002 |
| Bone (Cortical) | 0.02 - 0.06 | Gabriel et al., 1996 |
| Soft Tissue (Avg.) | 0.2 - 0.3 | Gabriel et al., 1996 |
Q2: What is the most robust method to register a CT volume to my 2D EIT electrode plane? A2: A feature-based, multi-stage registration is recommended.
- Extract Features: From CT, extract the body contour and lung boundaries via segmentation.
- Initial Alignment: Perform a rigid affine transformation to match the CT body contour to the EIT boundary shape.
- Non-rigid Refinement: Use a B-spline or Demons algorithm to deform the CT lung boundaries to match any a priori EIT lung silhouette (if available).
- Slice Extraction: Interpolate the registered 3D CT volume at the precise 2D plane of your EIT electrode array.
Diagram Title: CT-to-EIT Registration Protocol
Q3: My reconstruction with priors is stable but loses sensitivity to small functional changes. How can I fix this?
A3: This indicates over-regularization. Adjust the Tikhonov regularization term: J = argmin(||V - F(σ)||² + α₁||L(σ - σ_prior)||² + α₂||G(σ)||²).
- Reduce the weight (
α₁) on the anatomical prior term. - Slightly increase the weight (
α₂) on the smoothness term (G). - Perform an L-curve analysis to find the optimal (
α₁,α₂) pair that balances prior fidelity and sensitivity to change.
Diagram Title: Regularization in EIT Reconstruction with Priors
Q4: Can I use a statistical shape model as a prior instead of a subject-specific CT? A4: Yes, especially in longitudinal studies lacking daily CT. This falls under "population-based priors."
- Protocol: Build a shape model from a database of CT scans using Principal Component Analysis (PCA).
- Integration: During EIT reconstruction, allow the shape parameters (e.g., lung size, heart position) to be estimated alongside conductivity distribution using a joint optimization framework. This is an advanced method requiring careful validation.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for EIT with Anatomical Priors
| Item | Function & Role in Experiment | Example/Notes |
|---|---|---|
| EIT System with Digital I/O | Generates current patterns and measures boundary voltages. Must synchronize with medical imaging clock for combined studies. | Swisstom Pioneer, Draeger EIT Evaluation Kit 2. |
| High-Resolution CT/MRI Scanner | Provides the anatomical prior data. CT is preferred for lung/thorax due to superior air-tissue contrast. | Siemens Somatom Force, GE Signa MRI. |
| Image Segmentation Software | Segments anatomical structures (lungs, heart, vessels) from CT/MRI to create the conductivity prior map. | 3D Slicer, ITK-SNAP, Mimics. |
| Finite Element Method (FEM) Mesh Generator | Creates a volume mesh of the imaging domain for the forward model. Must handle hybrid element types. | Netgen, Gmsh, COMSOL Multiphysics. |
| Multi-Modal Image Registration Tool | Registers the CT/MRI prior to the EIT electrode geometry. | Elastix, ANTs, 3D Slicer. |
| Inverse Solver Software Library | Solves the EIT inverse problem incorporating the prior constraint. Core of the refinement research. | EIDORS, custom Python/Matlab with CVX or SciPy. |
| Calibration Phantom | Validates the forward model accuracy. Typically a tank with known internal insulating/including objects. | Saline tank with plastic/agar inserts. |
Technical Support Center
FAQs & Troubleshooting Guides
Q1: During L-Curve analysis for my 2D EIT reconstruction, the corner is not distinct or appears as a smooth curve. What could be the cause and how can I resolve it? A: A poorly defined L-curve corner often indicates an inappropriate range of regularization parameters (λ) or high noise levels in your boundary voltage measurements. To troubleshoot:
- Verify your measurement system's signal-to-noise ratio (SNR). Re-calibrate electrodes and ensure stable contact impedance if SNR is below 60 dB.
- Extend the range of λ values you test. Use a logarithmic scale (e.g., from 1e-7 to 1e-1) and increase the density of points, especially around the suspected corner region.
- Check for errors in computing the solution norm (||xλ||²) and residual norm (||Axλ - b||²). Ensure the matrix calculations are using double precision.
Q2: When applying the CRESO method, the function C(λ) = ||xλ||² + 2λ * d(||xλ||²)/dλ does not exhibit a clear maximum. What steps should I take? A: The absence of a clear maximum in the CRESO function typically arises from numerical instability in computing the derivative. Follow this protocol:
- Refine λ sampling: Use a denser set of λ values in the region where the L-curve shows its highest curvature.
- Improve derivative calculation: Instead of simple finite differences, apply a Savitzky-Golay filter to smooth the ||x_λ||² data before differentiation, or use a cubic spline interpolation to obtain a smoother derivative.
- Re-evaluate parameter bounds: The optimal λ may lie outside your initially chosen range. Systematically expand the search until the function C(λ) converges to zero at both ends, confirming the maximum is within range.
Q3: What is a reliable heuristic λ selection method for real-time EIT imaging, and what are its limitations?
A: The "Fixed Noise Fraction" (FNF) heuristic is commonly used for real-time applications. Set λ such that: ||Ax_λ - b||² / ||b||² ≈ δ, where δ is an estimate of the relative measurement noise variance (e.g., 0.01 for 1% noise).
- Limitation: This method assumes prior knowledge of the noise level, which may vary during an experiment. It also does not account for the specific ill-posedness of the inverse problem at each time step.
- Troubleshooting: If reconstructed images appear overly smooth (under-regularized) or lack detail (over-regularized), dynamically adjust the δ value. Implement a calibration step at the start of each experiment to estimate the current system noise level.
Q4: How do I validate my chosen regularization parameter from any method for a specific EIT application? A: Implement a "Ground Truth Phantom" experiment.
- Protocol: Use a phantom with known, discrete conductivity targets (e.g., insulated rods in a saline tank). Acquire boundary voltage data (
b_measured). - Reconstruction: Reconstruct images using a sweep of λ values from your chosen method's optimal point.
- Quantitative Metrics: Calculate the following for each reconstruction:
- Image Error:
||σ_reconstructed - σ_true|| / ||σ_true|| - Position Error: Distance between centroid of reconstructed target and its true position.
- Correlation Coefficient: Between pixel values of reconstructed and true conductivity distribution.
- Image Error:
- Validation: The λ that minimizes Image Error and Position Error while maximizing Correlation is empirically validated for your specific setup.
Table 1: Comparison of Regularization Parameter Selection Methods
| Method | Key Principle | Pros | Cons | Typical Compute Time* | Optimal Use Case |
|---|---|---|---|---|---|
| L-Curve | Log-log plot of solution vs. residual norm; pick corner. | Intuitive visualization; robust to moderate noise. | Ambiguous corner with high noise; requires dense λ sampling. | High | Offline analysis of stable systems. |
| CRESO | Maximizes difference between derivative of solution norm & itself. | Automates corner selection; less subjective. | Unstable with noisy derivatives; may fail to find max. | Medium-High | Automated processing where L-curve corner is evident. |
| GCV | Minimizes predictive error without needing noise estimate. | Theoretical appeal; no prior noise info needed. | Can lead to under-regularization; flat minimum problematic. | Very High | Theoretical studies with well-behaved systems. |
| Fixed Noise Fraction | Sets residual norm to a fixed fraction of data norm. | Very fast; simple to implement. | Requires accurate noise estimate; not adaptive. | Very Low | Real-time, time-series imaging with stable noise. |
| Discrepancy Principle | Sets residual norm equal to estimated noise norm. | Strong theoretical basis. | Requires highly accurate noise estimate. | Low | When measurement error can be precisely quantified. |
*Compute time relative to the inverse solution for a single λ.
Table 2: Validation Metrics for Different λ Selection Methods (Sample Phantom Study)
| Selection Method | Chosen λ (log10) | Image Error (%) | Position Error (pixels) | Correlation Coefficient |
|---|---|---|---|---|
| L-Curve Corner | -4.2 | 18.7 | 1.5 | 0.89 |
| CRESO Maximum | -4.0 | 19.1 | 1.6 | 0.88 |
| GCV Minimum | -3.8 | 24.5 | 2.1 | 0.82 |
| Fixed Noise Fraction (δ=0.01) | -4.5 | 17.9 | 1.4 | 0.90 |
| True Optimal (from sweep) | -4.4 | 17.5 | 1.3 | 0.91 |
Experimental Protocols
Protocol 1: Systematic L-Curve Generation for EIT Reconstruction
- Forward Solution & Jacobian: Using your finite element model (FEM) mesh and initial conductivity guess, compute the system Jacobian (J) and lead-field matrix (A).
- Parameter Vector: Define a vector Λ = [λ₁, λ₂, ..., λₙ] where λᵢ = 10⁽ᶦ⁾, typically with i ranging from -7 to -1 in 0.1 or 0.2 increments.
- Reconstruction Loop: For each λᵢ in Λ:
a. Solve the regularized inverse problem:
x_λ = (AᵀA + λᵢI)⁻¹ * Aᵀ * b(or equivalent for your solver). b. Compute the residual norm:ρ(λᵢ) = log(||A x_λ - b||²). c. Compute the solution norm:η(λᵢ) = log(||x_λ||²). - Plot & Analysis: Plot η(λᵢ) vs. ρ(λᵢ). The point of maximum curvature (approximated by the maximum of the 2D curvature function κ) identifies the optimal λ.
Protocol 2: Implementing the CRESO Method
- Prerequisite: Follow Protocol 1, steps 1-3, to obtain arrays of λᵢ, ||xλ||², and ||Axλ - b||².
- Numerical Differentiation: Compute the derivative of the solution norm with respect to λ. Use a central difference scheme:
dS_dλ[i] = (||x_{λ[i+1]}||² - ||x_{λ[i-1]}||²) / (λ[i+1] - λ[i-1]). - CRESO Function: Calculate
C(λ[i]) = ||x_{λ[i]}||² + 2 * λ[i] * dS_dλ[i]for all i. - Identification: Find the λ value at which
C(λ)attains its first positive maximum. This is the CRESO-selected regularization parameter.
Visualizations
Title: L-Curve Method Workflow for EIT
Title: CRESO Parameter Selection Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for EIT Regularization Validation Experiments
| Item | Function in Experiment | Specification / Notes |
|---|---|---|
| EIT Measurement System | Acquires boundary voltage data from phantom or subject. | 16-32 electrodes; >80 dB SNR; simultaneous measurement capability preferred. |
| Calibrated Saline Tank | Provides known, homogeneous background conductivity. | Non-conductive tank (e.g., acrylic); temperature control (±0.5°C) for stable σ. |
| Conductive/Insulating Targets | Serves as ground truth for image validation. | Cylindrical rods of known size & conductivity (e.g., metal, plastic, agar). |
| Finite Element Model (FEM) Mesh | Discretizes domain for forward solving and reconstruction. | Must match physical phantom geometry exactly; >2000 elements for 2D. |
| Regularization Solver Software | Computes x_λ for different λ. |
MATLAB with EIDORS, or custom Python/C++ using libraries like SciPy. |
| Numerical Differentiation Tool | Calculates derivatives for CRESO/Gradient methods. | Use filtered schemes (Savitzky-Golay) or spline interpolation for stability. |
| High-Performance Computing Node | Runs multiple reconstructions for λ sweeps efficiently. | Multi-core CPU (16+ cores) with ≥32 GB RAM; reduces L-curve compute time. |
Technical Support Center
Troubleshooting Guides & FAQs
Q1: Our EIT system shows high-frequency noise and intermittent spikes in measured voltages, especially near electrical equipment. What is this likely to be, and how can we fix it? A1: This is characteristic of inadequate electromagnetic shielding. External electromagnetic interference (EMI) is corrupting your sensitive bioimpedance measurements.
- Diagnostic Protocol: Power down all excitation sources. Measure the baseline voltage across all electrode pairs. A non-zero baseline or erratic drift indicates EMI pickup.
- Solution: Implement a layered shielding approach.
- Enclose the entire EIT data acquisition system (DAC) and patient/subject cable harness in a grounded, continuous Faraday cage (e.g., copper mesh).
- Use fully shielded, twisted-pair cables for all electrode connections.
- Physically separate power cables and signal cables; cross them at 90° angles if they must intersect.
- Apply a driven-right-leg (DRL) circuit or active shielding to the subject if applicable.
Q2: We observe "ringing" or oscillations in the voltage transient following current injection, which distorts our phase measurement. What causes this and how do we minimize it? A2: Ringing is a settling time artefact caused by impedance mismatches and parasitic capacitance/inductance in the measurement circuit.
- Diagnostic Protocol: Using a calibration phantom with known resistive loads, observe the voltage response on an oscilloscope. Ringing appears as a decaying sinusoidal wave superimposed on the ideal step response.
- Solution:
- Impedance Matching: Ensure the output impedance of the current source matches the characteristic impedance of the cables and the input impedance of the voltmeter.
- Guard Traces: Use guard traces/driven shields on PCB layouts to minimize stray capacitance at the input stage of voltage sensing amplifiers.
- Low-Pass Filtering: Implement an anti-aliasing filter with a cutoff frequency just above your measurement band. A 2nd-order Sallen-Key topology is often effective.
- Firmware Adjustment: Introduce a short delay between current injection and voltage sampling to allow for transient settling.
Q3: Our reconstructed images show severe, localized distortions that correlate with specific electrode positions. What is the most probable source? A3: This strongly indicates electrode contact errors. Poor or inconsistent contact impedance leads to significant boundary condition errors in the forward model.
- Diagnostic Protocol: Before each experiment, measure the contact impedance at every electrode. A high value (> 1-2 kΩ for wet electrodes) or high variance (> 20% across electrodes) signals a problem.
- Solution:
- Skin Preparation: Clean the skin area with alcohol and, if necessary, use a mild abrasive paste to reduce stratum corneum resistance.
- Electrode Gel: Use a high-conductivity, wet gel for Ag/AgCl electrodes and ensure sufficient volume.
- Electrode Fixation: Apply consistent pressure using elastic straps or a rigid electrode belt to ensure uniform contact.
- Algorithmic Compensation: Use a reference measurement or real-time impedance monitoring to exclude or correct data from faulty channels in the reconstruction inverse solver.
Table 1: Impact of Common Artefacts on Reconstruction Metrics
| Artefact Type | Typical SNR Drop | Spatial Error Increase | Common Frequency Band |
|---|---|---|---|
| EMI (Poor Shielding) | 20-40 dB | 15-25% | Broadband (50/60 Hz, RF) |
| Settling Ringing | 10-30 dB | 10-20% (Phase-specific) | High (>10 kHz for typical systems) |
| High Contact Impedance | 15-35 dB | 30-50% (Localized) | Low to Mid (DC - 10 kHz) |
Table 2: Recommended Tolerance Thresholds for Experimental Setup
| Parameter | Optimal Range | Action Threshold | Measurement Protocol |
|---|---|---|---|
| Electrode-Skin Impedance | < 1 kΩ @ 10 kHz | > 2 kΩ or >20% variance | Impedance spectroscopy across all electrodes pre-scan |
| System Baseline Noise (Shorted Input) | < 10 µV RMS | > 50 µV RMS | RMS voltage measurement over 60s, all inputs shorted |
| Voltage Settling Time (to 0.1%) | < 100 µs | > 500 µs | Oscilloscope capture on calibration load post-injection |
Experimental Protocols
Protocol 1: Systematic Evaluation of Shielding Efficacy
- Objective: Quantify noise reduction from shielding interventions.
- Setup: Place EIT system and phantom in a typical lab environment. Use a single-frequency (e.g., 50 kHz) current injection.
- Procedure:
a. Measure baseline voltage (
V_bare) across all electrode pairs with no shielding. b. Encase signal cables in braided shield, grounded at DAC end. Measure voltages (V_cable). c. Further, enclose the entire DAC and cable hub in a portable Faraday tent. Measure voltages (V_full). - Analysis: Calculate RMS noise for each condition. The metric is Noise Reduction (dB) = 20 * log10(RMSnoisebare / RMSnoiseintervention).
Protocol 2: Electrode Contact Impedance and Image Fidelity Correlation
- Objective: Establish the relationship between contact impedance variance and reconstructed image error.
- Setup: Use a cylindrical tank phantom with a single, off-center conductive target. Employ a 16-electrode array.
- Procedure:
a. Establish perfect contact (all electrodes submerged). Perform EIT scan as reference (
Ref_Image). b. For N trials, deliberately increase impedance at 1-2 random electrodes by applying a thin, non-conductive layer. c. For each trial, record the contact impedance map and perform an EIT scan (Trial_Image). - Analysis: Calculate Image Correlation Coefficient (ICC) between
Ref_Imageand eachTrial_Image. Plot ICC versus the maximum impedance or the variance of the impedance map.
Visualizations
Title: EMI Artefact Pathway & Mitigation Strategies
Title: Pre-Scan Electrode Contact QC Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in EIT Artefact Mitigation |
|---|---|
| High-Conductivity Electrode Gel (e.g., SignaGel) | Reduces electrode-skin contact impedance, ensuring consistent current injection and voltage pickup. Essential for minimizing contact errors. |
| Abhesive Skin Prep Gel (e.g., NuPrep) | Gently abrades the stratum corneum to lower and stabilize baseline skin impedance before electrode placement. |
| Copper Shielding Tape / Conductive Fabric | Used to create ad-hoc Faraday shields for cables and equipment enclosures to block electromagnetic interference (EMI). |
| Calibration Phantom (Resistive Network or Saline Tank) | Provides a known, stable impedance target for system validation, distinguishing hardware artefacts from true biological signals. |
| Driven-Right-Leg (DRL) IC Module | An active shielding circuit that reduces common-mode interference from the subject's body, improving signal fidelity. |
| PCB with Guard Traces | A custom data acquisition board where guard traces surround high-impedance input lines, actively driven to shield against parasitic capacitance. |
Technical Support Center
Troubleshooting Guides
Issue 1: Unstable or Drifting Baseline Impedance Measurements.
- Symptoms: Baseline readings fluctuate significantly between sequential frames without applied stimulation, or show a continuous drift over time.
- Primary Causes & Solutions:
- Poor Electrode-Skin/Interface Contact: Re-prep the skin surface (abrade and clean) and ensure electrode gel is fresh and adequately applied. For dry electrodes, ensure sufficient, even contact pressure.
- Current Source Instability: Verify the output impedance and compliance voltage of your current source are suitable for the load presented by your electrode-tissue setup. Check for overheating of output stage components.
- Electrode Polarization: Ensure electrodes are non-polarizable (e.g., Ag/AgCl) for low-frequency applications. For higher frequencies, confirm the electrode material's polarization impedance is negligible relative to the tissue impedance under test.
- Environmental Drift: Control laboratory temperature and humidity. Allow hardware to warm up for 30 minutes prior to calibration and measurement.
Issue 2: Low Signal-to-Noise Ratio (SNR) in Reconstructed Images.
- Symptoms: Images appear grainy, lack detail, or contain artifacts that obscure true conductivity changes.
- Primary Causes & Solutions:
- Insufficient Current Injection: Increase current amplitude within safe limits (see IEC 60601). Note: Higher current improves SNR but risks patient discomfort and non-linear tissue behavior.
- High Measurement Noise: Use synchronous demodulation (lock-in amplification) techniques. Increase averaging per measurement frame (trade-off with temporal resolution). Shield all cables and enclose front-end electronics.
- Non-Optimal Electrode Array: Increase the number of electrodes if spatial resolution is inadequate. Re-evaluate electrode placement pattern for the region of interest.
Issue 3: Inconsistent Results Between Repeated Experiments on the Same Subject.
- Symptoms: Measured impedance spectra or reconstructed image features vary between sessions under ostensibly identical conditions.
- Primary Causes & Solutions:
- Electrode Placement Variability: Use a customized electrode array fixture or 3D-printed template to ensure identical anatomical placement across sessions.
- Uncontrolled Physiological State: Standardize subject preparation (e.g., fasting state, time of day, resting period before measurement) and document environmental conditions.
- Protocol Deviation: Automate the measurement sequence completely to eliminate operator timing errors. Use scripted protocols.
Frequently Asked Questions (FAQs)
Q1: What are the key specifications to evaluate when selecting or designing a current source for EIT? A: Critical specifications are summarized in the table below. Table 1: Key Current Source Specifications for EIT
| Specification | Typical Target/Requirement | Impact on EIT |
|---|---|---|
| Output Frequency | 1 kHz - 1 MHz (biomedical) | Determines tissue penetration depth and contrast mechanism. |
| Output Accuracy & Stability | > 0.1% | Directly affects measurement accuracy and image fidelity. |
| Output Impedance | > 1 MΩ (high) | Minimizes current variation due to changing contact/load impedance. |
| Total Harmonic Distortion (THD) | < -80 dB | Reduces measurement errors, especially in multi-frequency EIT. |
| Compliance Voltage | ±10V to ±15V | Ensures current can be driven through high-impedance electrode contacts. |
Q2: How does the choice of electrode array geometry and number of electrodes affect image reconstruction? A: The electrode array defines the "sensing mesh." More electrodes provide more independent measurements, improving the spatial resolution and ill-posedness of the inverse problem. However, it increases hardware complexity and computational cost. Common geometries (planar, circular, linear) must match the anatomical region. Incorrect geometry models in reconstruction will introduce severe boundary artifacts.
Q3: What are the advantages and disadvantages of adjacent vs. opposite (tetrapolar) drive patterns? A: Adjacent patterns (neighbor drive) typically provide higher sensitivity near the boundary but lower sensitivity in the center. Opposite patterns provide better central sensitivity but may be more susceptible to deep regional inhomogeneities and require higher compliance voltage. The choice is application-dependent and should be modeled.
Q4: How can I validate my EIT hardware and measurement protocol before in-vivo studies? A: Follow a phased experimental protocol:
- Resistor Phantom Test: Use a network of precision resistors to verify hardware linearity, accuracy, and system noise performance.
- Saline Tank Phantom with Insulating/Conducting Targets: Use a tank with known background conductivity and targets of known size/position to quantify spatial resolution, amplitude response, and detect systematic errors.
- Dynamic Phantom: Use a moving target or changing-conductivity region to assess temporal response.
Experimental Protocol: Saline Tank Phantom Validation
Objective: To characterize the spatial resolution and quantitative accuracy of an EIT system. Materials: See "The Scientist's Toolkit" below. Methodology:
- Prepare 0.9% w/v NaCl saline solution (conductivity ~1.6 S/m at 20°C).
- Arrange electrodes equidistantly around the perimeter of the cylindrical tank.
- Connect electrodes to the EIT data acquisition system.
- Measurement A (Homogeneous): Collect a reference frame set (
V_ref) with only saline. - Measurement B (Inhomogeneous): Place a non-conductive (plastic) cylindrical target of known diameter (e.g., 30% tank diameter) at a known off-center position. Collect a new frame set (
V_target). - Reconstruction: Calculate the difference data
ΔV = V_target - V_ref. Reconstruct a differential image using your chosen algorithm (e.g., Gauss-Newton, D-bar). - Analysis: Compare the reconstructed target position and size against known ground truth. Calculate metrics like Position Error (PE) and Resolution (RES).
Visualizations
EIT System Component Interaction
EIT Hardware Validation Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for EIT Phantom Experiments
| Item | Specification / Example | Primary Function |
|---|---|---|
| Electrode Gel | ECG/EEG conductive gel, NaCl-based | Ensures stable, low-impedance electrical contact between electrode and skin/phantom. |
| Non-Polarizable Electrodes | Ag/AgCl, sintered pellet type | Minimizes polarization voltage at the electrode-electrolyte interface, crucial for DC/low-frequency stability. |
| Phantom Saline | 0.9% NaCl solution, food-grade KCl for tuning | Provides a stable, homogeneous, and biologically relevant conductivity medium for system testing. |
| Agar or Gelatin | High purity, bacteriological grade | Used to solidify saline into stable, shape-retaining phantoms for 2D/3D testing. |
| Conductivity Targets | Plastic rods (insulating), agar with KCl (conducting) | Create controlled inhomogeneities in phantoms to test image reconstruction performance. |
| Calibration Resistors | Precision resistors (0.1% tolerance), 100Ω - 1kΩ range | Create known reference loads for verifying current source and voltmeter accuracy and linearity. |
Benchmarking Performance: Validation Phantoms, Clinical Trials, and Multi-Modal Comparisons
Technical Support Center: Troubleshooting for EIT Phantom Experiments
This support center addresses common issues encountered when using physical and numerical phantoms for validating Electrical Impedance Tomography (EIT) reconstruction algorithms within a research thesis focused on overcoming EIT image reconstruction challenges.
Frequently Asked Questions (FAQs)
Q1: Our physical phantom experiments show consistently higher boundary voltage measurements than numerical simulations predict. What could be the cause? A: This discrepancy often arises from contact impedance at electrode interfaces. In numerical phantoms, perfect electrode-skin contact is assumed (typically 0 Ω·cm²). In physical setups, contact impedance can range from 10 to 500 Ω·cm². Ensure you are using conductive electrode gels and apply consistent pressure. Calibrate your system using a known resistor network before phantom experiments.
Q2: When testing a new reconstruction algorithm, our numerical phantom results are excellent, but performance degrades severely with physical phantom data. How should we proceed? A: This highlights the critical role of physical phantoms as the final validation step. The degradation is likely due to model mismatch. Follow this protocol:
- Systematically introduce known errors (electrode position shift, contact impedance variation) into your numerical phantom to identify the most sensitive parameter.
- Refine your forward model to include this parameter.
- Re-tune your algorithm's regularization parameters using the updated model.
- Validate again on the physical phantom.
Q3: We observe significant noise in differential EIT measurements using a saline tank phantom with moving inclusion. What are the primary sources? A: Key noise sources in dynamic physical phantom experiments are:
| Noise Source | Typical Magnitude | Mitigation Strategy |
|---|---|---|
| Mechanical Vibration | 1-5% voltage fluctuation | Use vibration-dampening table, secure all cables. |
| Saline Temperature Drift | 2%/°C in conductivity | Use temperature-controlled room, allow for equilibration. |
| Electrode Polarization | Variable, time-dependent | Use gold-plated electrodes, apply appropriate AC frequency (>10 kHz). |
| Data Acquisition System Noise | 80-100 dB SNR required | Use shielded cables, proper grounding, and average multiple measurements. |
Q4: How do we select the appropriate complexity for a numerical phantom when benchmarking a new algorithm? A: Use a tiered validation approach. Start with simplistic models to verify core functionality, then progress to clinically realistic models.
Experimental Protocols
Protocol 1: Fabrication of a Basic Agar-Based Heterogeneous Phantom Objective: Create a stable, reproducible physical phantom with a known inclusion of contrasting conductivity. Materials: See "Research Reagent Solutions" below. Methodology:
- Prepare 2L of 0.9% NaCl solution (background).
- Separately, prepare 200ml of 2.0% NaCl solution (inclusion).
- For each solution, add 3% w/v agar powder. Heat while stirring until boiling and clear.
- Pour the background solution into the phantom tank. Let it cool until a thin semi-solid skin forms.
- Position a mold (e.g., a small balloon) where the inclusion is desired.
- Carefully pour the inclusion solution into the mold. Alternatively, pre-cast an inclusion and embed it.
- Refrigerate the entire assembly at 4°C for 4 hours until fully set.
- Remove the mold carefully. The phantom is ready for use. Conductivity should be verified with a separate probe.
Protocol 2: Systematic Algorithm Validation Workflow Objective: Objectively compare the performance of a new EIT reconstruction algorithm against a standard. Methodology:
- Define Metrics: Choose quantitative metrics (e.g., Position Error, Radius of Deformation, Image Contrast, Relative Error).
- Design Numerical Phantom Suite: Create a set of phantoms with varying inclusion number (1-3), position (center, off-center), size (10-30% field diameter), and contrast (2:1, 4:1).
- Add Noise: Simulate measurement noise (e.g., 0.1% to 1% Gaussian) to boundary voltage data.
- Reconstruct & Calculate: Run both algorithms on the suite. Calculate all metrics for each case.
- Physical Phantom Correlation: Perform equivalent experiments on corresponding physical phantoms.
- Statistical Analysis: Use a paired t-test or ANOVA to determine if differences in algorithm performance metrics are statistically significant (p < 0.05).
Visualizations
Title: Tiered EIT Algorithm Validation Workflow
Title: Troubleshooting Guide: Phantom Result Mismatch
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Agar Powder | Gelling agent for creating stable, shape-retaining physical phantoms. Allows for embedding of inclusions. |
| Sodium Chloride (NaCl) | Determines the bulk conductivity of the phantom medium. Different concentrations simulate different tissues. |
| Potassium Chloride (KCl) | Sometimes added to better mimic the ionic composition of biological tissues. |
| Graphite Powder / Carbon Black | Used to create conductive rubber or plastic sheets for simulating lung tissue (high resistivity). |
| Polyvinyl Alcohol (PVA) | Used for creating cryogel phantoms that can withstand freeze-thaw cycles, adding mechanical stability. |
| Gold-Plated Electrodes | Minimize polarization impedance at the electrode-electrolyte interface, reducing measurement drift. |
| Ideal Resistor Network | A precise resistor mesh used for primary system calibration and verification, independent of phantom geometry. |
| Commercial Tissue Mimicking Gel | Pre-formulated gels with stable, published dielectric properties (e.g., from CIRS or similar). |
| Finite Element Mesh Software (e.g., Netgen, Gmsh) | Creates the spatial discretization required for simulating the forward problem in numerical phantoms. |
| EIDORS Project Software | An open-source suite for EIT simulation and image reconstruction, essential for numerical phantom work. |
FAQs
Q1: In my EIT image reconstruction, I am getting a high Mean Squared Error (MSE) but the image appears visually acceptable. Which metric should I trust? A1: This discrepancy is common. MSE is a pixel-wise measure sensitive to overall amplitude differences, while visual perception is more tolerant of certain global errors. You should consult multiple metrics:
- For Accuracy: Use the Structural Similarity Index (SSIM) alongside MSE. SSIM assesses perceptual similarity in structure, luminance, and contrast. A high SSIM with a moderate MSE often confirms a perceptually good reconstruction.
- For Clinical/Feature Relevance: Use the Relative Image Error (RIE) or a Region of Interest (ROI) specific metric like the Dice coefficient if you are segmenting a specific inclusion. The table below compares these metrics.
Q2: My reconstruction algorithm is accurate but prohibitively slow for real-time monitoring. What are the primary factors affecting reconstruction speed? A2: Reconstruction speed in EIT is governed by several computational bottlenecks:
- Forward Model Solving: The speed of calculating the simulated measurements for a given conductivity distribution.
- Inverse Problem Solver: Iterative algorithms (e.g., Gauss-Newton, D-bar) are more accurate but slower than direct one-step methods.
- Mesh Resolution: A finer finite element mesh increases accuracy but drastically increases computation time for both forward and inverse problems.
- Regularization Parameter Selection: Adaptive or spatially variant regularization schemes add computational overhead compared to fixed parameters.
Q3: How can I objectively compare my new reconstruction algorithm against a baseline method? A3: A robust comparison requires a standardized protocol using phantom data and a suite of metrics:
- Use a Public Phantom Dataset (e.g., EIDORS or GREIT phantoms) to ensure reproducibility.
- Define a Primary Metric Triad: Select one metric each for Image Quality, Accuracy, and Speed.
- Report Statistical Significance: Perform multiple trials with varying noise levels and report mean ± standard deviation.
- Benchmark Systematically: Follow the experimental protocol outlined in the next section.
Troubleshooting Guides
Issue: Reconstructed images are overly smooth and lack detail (Over-regularization).
- Symptoms: Low MSE but also low SSIM; features appear blurred; inability to resolve small or adjacent inclusions.
- Potential Causes & Solutions:
- Cause 1: Regularization parameter (λ) is too high.
- Solution: Use the L-curve or Generalized Cross-Validation (GCV) method to find an optimal λ. Systematically test a range of values.
- Cause 2: Using a homogeneous prior (e.g., Tikhonov) where structure is known.
- Solution: Implement a structural prior (e.g., Total Variation, Laplace) in your regularization matrix to preserve edges.
- Cause 1: Regularization parameter (λ) is too high.
Issue: Reconstruction is fast but unstable and noisy (Under-regularization).
- Symptoms: High-amplitude artifacts, speckle noise; high MSE and low SSIM; results vary greatly with minor noise changes.
- Potential Causes & Solutions:
- Cause 1: Regularization parameter (λ) is too low.
- Solution: Increase λ using methods described above. Consider noise-adaptive regularization.
- Cause 2: Poorly conditioned Jacobian/System Matrix.
- Solution: Review electrode modeling and mesh quality. Ensure proper handling of ill-posedness through effective regularization.
- Cause 1: Regularization parameter (λ) is too low.
Issue: Inconsistent performance across different phantom sizes or noise levels.
- Symptoms: Algorithm works well for one experimental setup but fails on another.
- Potential Causes & Solutions:
- Cause 1: Non-adaptive regularization parameter.
- Solution: Implement a parameter choice strategy (e.g., noise-dependent, discrepancy principle) that adjusts to data conditions.
- Cause 2: Forward model inaccuracies.
- Solution: Validate your forward solver against analytical solutions for simple geometries. Ensure mesh is sufficiently refined, especially near electrodes.
- Cause 1: Non-adaptive regularization parameter.
| Metric Category | Metric Name | Formula / Principle | Ideal Value | Measures | Notes for EIT |
|---|---|---|---|---|---|
| Image Accuracy | Mean Squared Error (MSE) | MSE = (1/N) ∑(xᵢ - x̂ᵢ)² |
0 | Pixel-wise difference from ground truth. | Sensitive to outliers; does not correlate well with perception. |
| Image Quality | Structural Similarity Index (SSIM) | Luminance, Contrast, Structure comparison. | 1 | Perceptual similarity to ground truth. | More aligned with human assessment; range [-1, 1]. |
| Feature Accuracy | Dice Coefficient (F1-Score) | Dice = 2|A∩B| / (|A|+|B|) |
1 | Overlap of a segmented region with ground truth. | Critical for quantifying recovery of specific inclusions. |
| Reconstruction Speed | Computation Time | Wall-clock time. | Context-dependent | Time from data input to final image. | Always report hardware/software specs. Use Big O notation for complexity. |
| Algorithm Efficiency | Convergence Rate | Reduction in residual per iteration. | Steep and monotonic | Speed of iterative solver convergence. | Indicates stability and computational cost of inverse solver. |
Experimental Protocol for Benchmarking EIT Algorithms
Objective: To quantitatively compare the performance of two EIT reconstruction algorithms (Algorithm A vs. Algorithm B) in terms of Image Accuracy, Quality, and Reconstruction Speed.
1. Materials & Data Generation:
- Numerical Phantom: Use a 2D circular finite element mesh with 16 equally spaced electrodes.
- Ground Truth Models: Generate three distinct conductivity distributions:
- Single off-center circular inclusion.
- Two adjacent circular inclusions.
- A complex shape (e.g., a C-shaped inclusion).
- Forward Data Simulation: Use a complete electrode model with contact impedance to simulate voltage measurements
V_simfrom each ground truth. - Noise Introduction: Add Gaussian white noise to
V_simat three signal-to-noise ratio (SNR) levels: 40 dB, 30 dB, and 20 dB. Repeat each simulation 20 times with different noise seeds.
2. Reconstruction & Analysis:
- For each ground truth model, noise level, and noise instance:
- Record the start time
t_start. - Reconstruct the image using Algorithm A and Algorithm B.
- Record the end time
t_end. Compute Computation Time =t_end - t_start. - Calculate MSE, SSIM, and Dice Coefficient (for the inclusion area) between the reconstructed image and the ground truth.
- Record the start time
- Statistical Summary: For each combination of Algorithm, Model, and SNR level, compute the mean and standard deviation of each metric across the 20 noise trials.
3. Reporting:
- Present results in a table comparing mean ± std for each metric.
- Generate comparative image panels for visual inspection.
EIT Reconstruction Workflow & Metric Evaluation
The Scientist's Toolkit: Key Reagent Solutions for EIT Research
| Item | Category | Function in EIT Research |
|---|---|---|
| EIDORS Software Framework | Software | Open-source MATLAB/GNU Octave toolbox for EIT forward and inverse modeling. Provides standardized algorithms and phantoms for benchmarking. |
| GREIT Reconstruction Framework | Algorithm/Software | A consensus linear reconstruction algorithm for lung EIT. Serves as a standard baseline for comparison in thoracic imaging studies. |
| Ag/AgCl Electrode & Electrolyte Gel | Hardware/Consumable | Provides stable, low-impedance electrical contact with the subject (phantom, animal, human). Critical for data quality. |
| Calibrated Resistivity Phantoms | Calibration Tool | Physical objects with known conductivity distributions (e.g., agar with NaCl, insulated inclusions). Essential for experimental validation of systems and algorithms. |
| Finite Element Mesh (e.g., from Netgen) | Computational Model | Discretizes the imaging domain. Its quality and resolution directly impact forward solution accuracy and reconstruction speed. |
| Tikhonov/TOTAL VARIATION Regularization | Mathematical Prior | Stabilizes the ill-posed inverse problem. Tikhonov promotes smoothness; TV promotes piecewise constant solutions with sharp edges. |
| L-Curve or GCV Algorithm | Optimization Tool | Method for selecting the optimal regularization parameter (λ), balancing data fidelity and solution smoothness. |
Technical Support Center & Troubleshooting
FAQs & Troubleshooting Guides
Q1: Our EIT image reconstruction algorithm performs well on phantom data but fails in early patient studies, producing unstable images. What could be the cause? A: This is a common challenge in translating EIT from bench to bedside. The primary cause is often patient-derived anatomical and physiological variability not captured in phantom models.
- Troubleshooting Steps:
- Verify Boundary Voltage Data Quality: Check for excessive noise or dropout channels in your raw patient data. Compare the signal-to-noise ratio (SNR) to your phantom studies.
- Review Electrode Contact Impedance: High or variable skin-electrode impedance in patients can severely distort boundary measurements. Ensure your protocol includes pre-study impedance checks and skin preparation.
- Validate Prior Anatomical Assumptions: Your reconstruction's forward model likely uses a simplified geometry (e.g., circular, homogeneous). Patient-specific torso shape and internal organ placement invalidate these assumptions. Solution: Integrate a patient-specific anatomical prior (e.g., from a low-dose CT scan) into your reconstruction algorithm.
Q2: When designing a patient study to validate a novel EIT reconstruction method for monitoring pulmonary edema, what key elements must the protocol include for regulatory acceptance (e.g., by the FDA)? A: A protocol designed for regulatory pathways must emphasize scientific rigor, reproducibility, and clinical relevance.
- Protocol Checklist:
- Primary Objective: Pre-specify a single, quantifiable primary endpoint (e.g., correlation coefficient between EIT-derived lung water index and gold-standard CT densitometry measurements).
- Statistical Analysis Plan: Define analysis methods, sample size justification (power calculation), and handling of missing data before study start.
- Risk Management: Detail procedures for mitigating risks (e.g., skin irritation from electrodes, data privacy).
- Standardized Operating Procedures (SOPs): Include SOPs for patient preparation, electrode placement, device operation, and data acquisition to minimize variability.
- Validation against a Reference Standard: The study must include a simultaneous, blinded comparison to an accepted clinical reference method.
Q3: We encounter inconsistent results when using different reference electrodes in our patient setup. How does this impact the reconstruction and how can we correct for it? A: EIT reconstructions typically assume a consistent reference (ground). In practice, a shifting reference introduces a common-mode error that corrupts absolute impedance values and can create artifacts.
- Solution Protocol:
- Use a Driven-Right-Leg (DRL) Circuit: Implement a DRL system to actively stabilize the common-mode voltage and improve the common-mode rejection ratio (CMRR) of your hardware.
- Post-Processing Correction: Apply a reference-independent formulation or data normalization technique (e.g., using the average of all measurements as the reference) during pre-processing of the boundary voltage data before reconstruction.
Quantitative Data Summary
Table 1: Common EIT Reconstruction Errors & Mitigations in Clinical Studies
| Error Source | Typical Impact on Image Quality | Quantitative Metric for Assessment | Recommended Mitigation Strategy |
|---|---|---|---|
| Electrode Movement/Contact | Blurring, Streak Artifacts | Channel Impedance Variance > 10% from baseline | Adhesive electrode belts, impedance monitoring in real-time. |
| Patient Anatomical Variance | Spatial Distortion, False Contrast | Position Error > 20mm in lesion localization | Use of patient-specific MRI/CT priors in the forward model. |
| High Biological Noise (Cardio-Resp.) | Temporal Instability | SNR drop below 40 dB | Synchronized gating to cardiac/respiratory cycle, ensemble averaging. |
| Incorrect Boundary Shape | Global Geometry Distortion | Increased Data Mismatch (>5% norm difference) | 3D camera-based boundary shape estimation. |
Experimental Protocol: Validation of EIT Reconstruction for Lung Perfusion
Objective: To clinically validate a dynamic EIT reconstruction algorithm's ability to map regional lung perfusion against the reference standard of contrast-enhanced CT.
Detailed Methodology:
- Patient Cohort & Ethics: Recruit 25 adult patients scheduled for diagnostic thoracic CT. Obtain informed consent and IRB/ethics committee approval.
- Synchronized Data Acquisition:
- EIT Setup: Apply a 32-electrode thoracic belt. Acquire data at 50 frames/sec using a commercial EIT system with DRL.
- Reference Standard: Perform a contrast-enhanced CT scan during breath-hold at end-inspiration.
- Synchronization: Use a pulse oximeter to record the ECG signal. Synchronize the EIT system clock and CT scanner trigger using the ECG R-wave as a temporal fiducial marker.
- EIT Data Processing:
- Pre-processing: Apply a bandpass filter (0.8 - 10 Hz) to isolate cardiac-frequency components. Segment data into cardiac cycles using the ECG.
- Reconstruction: Use a Gauss-Newton solver with Tikhonov regularization. Implement two forward models: (A) homogeneous circular model, (B) patient-specific model derived from the CT scan geometry.
- Analysis:
- Generate EIT perfusion images by calculating the amplitude of the cardiac-related impedance change per pixel.
- Coregister EIT images with CT pulmonary blood volume maps.
- Calculate the correlation coefficient (Pearson's r) between EIT-derived perfusion amplitude and CT Hounsfield units for corresponding anatomical regions (left/right lung, quadrants).
Visualizations
EIT Clinical Validation Regulatory Pathway
EIT Image Reconstruction Clinical Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Clinical EIT Validation Studies
| Item | Function in Clinical EIT Validation |
|---|---|
| Multi-Frequency EIT System (e.g., 10 Hz - 1 MHz) | Enables separation of resistive (perfusion) and reactive (ventilation) components via bioimpedance spectroscopy. |
| Adhesive Electrode Belts (Disposable, Multi-size) | Ensures consistent electrode contact and positioning across patient populations with varying torso diameters. |
| ECG Synchronization Module | Provides temporal fiducial points to gate EIT data to cardiac or respiratory cycles for functional imaging. |
| 3D Optical Camera System | Accurately maps the 3D torso surface/electrode positions to create patient-specific boundary geometry for the forward model. |
| Clinical Reference Standard Device | Gold-standard equipment (e.g., CT Scanner, Ventilator with flow sensors, Transpulmonary thermodilution) for objective performance comparison. |
| Impedance Gel & Skin Abrasion Kit | Reduces skin-electrode contact impedance to stable levels (< 2 kΩ) and minimizes motion artifact. |
| Digital Phantom & Simulation Software | Allows testing of reconstruction algorithms on virtual, anatomically realistic patient models before clinical deployment. |
Technical Support Center: Troubleshooting EIT Image Reconstruction
FAQs & Troubleshooting Guides
Q1: During dynamic lung EIT imaging, my reconstructed images show severe motion artifacts and blurring at the organ boundaries. What could be the cause and how can I mitigate this? A: This is a common challenge due to the ill-posed nature of EIT reconstruction and the high temporal resolution capturing thoracic movement.
- Primary Cause: Mismatch between the static computational model (mesh) and the dynamic physical boundaries of the thorax during breathing. The reconstruction algorithm assumes a fixed geometry.
- Troubleshooting Protocol:
- Implement Boundary Shape Correction: Use adjacent ECG or impedance waveform gates to segment data into similar tidal volumes. Reconstruct using a mesh model matched to the boundary voltage data for each phase.
- Employ a Temporal Regularization Scheme: Instead of purely spatial Tikhonov regularization, use a spatio-temporal regularization framework (e.g., Kalman filter, one-step Gauss-Newton with temporal priors) to constrain solutions across frames.
- Experimental Validation: Conduct a saline tank experiment with a moving, deformable conductive target. Compare static reconstruction vs. shape-corrected/temporal reconstruction protocols using metrics like position error and image contrast-to-noise ratio (CNR).
Q2: My EIT images exhibit poor spatial resolution and "smearing" of features compared to my CT scans. Is this a system error or a fundamental limitation? A: This is primarily a fundamental limitation of EIT's diffuse field paradigm, but reconstruction parameters significantly impact output.
- Checklist & Protocol for Optimization:
- Electrode Contact & Calibration: Verify all electrode contact impedances are stable and <5 kΩ. Perform a precision calibration measurement using known resistors.
- Regularization Parameter (λ) Tuning: λ balances data fitting and solution stability. Use the L-curve or GREIT method to select an optimal λ.
- Protocol: Reconstruct a tank phantom with known targets using a sweep of λ values (1e-6 to 1e-1). Plot solution norm vs. residual norm (L-curve). Choose λ at the corner. Evaluate with the Image Reconstruction Error (IRE):
IRE = ||σ_true - σ_reconstructed|| / ||σ_true||.
- Protocol: Reconstruct a tank phantom with known targets using a sweep of λ values (1e-6 to 1e-1). Plot solution norm vs. residual norm (L-curve). Choose λ at the corner. Evaluate with the Image Reconstruction Error (IRE):
- Forward Model Fidelity: Ensure your finite element model (FEM) mesh accurately represents the domain geometry and electrode positions. A mesh with <0.5% element error relative to MRI-derived geometry is recommended.
Q3: How can I quantitatively validate the functional sensitivity of my EIT system for a perfusion experiment, given the lack of ground truth in vivo? A: Employ a multi-modal benchmarking and indicator dilution protocol.
- Experimental Validation Protocol:
- Prepare a Dynamic Flow Phantom: Use a conductive background medium and a separate, tubing circuit with a different conductivity (simulating blood bolus) pumped through it at a known rate.
- Synchronized Data Acquisition: Inject a hypertonic saline or biocompatible contrast agent bolus in vivo or in a perfused organ model. Record EIT data at >30 fps.
- Correlate with Gold Standard: Simultaneously, use Doppler Ultrasound or Laser Speckle Contrast Imaging (LSCI) to measure flow in a representative vessel.
- Analysis: Generate time-impedance curves from an EIT Region of Interest (ROI). Calculate the Mean Transit Time (MTT) or time-to-peak. Perform linear correlation analysis between EIT-derived flow indices and the reference standard metrics. A correlation coefficient (R²) >0.8 in controlled studies indicates robust functional sensitivity.
Comparative Data Summary
Table 1: Comparison of Imaging Modalities Across Key Parameters
| Modality | Typical Spatial Resolution | Temporal Resolution | Primary Functional Sensitivity Mechanism | Key Limitation for Functional Imaging |
|---|---|---|---|---|
| Electrical Impedance Tomography (EIT) | 5 - 15% of domain diameter | < 50 ms (up to 1000 fps) | Conductivity (σ) & Permittivity (ε) changes. Reflects perfusion, ventilation, edema, cell viability. | Low inherent spatial resolution; boundary artifacts. |
| Computed Tomography (CT) | 0.5 - 1.0 mm | 0.3 - 2 seconds | Electron Density (X-ray attenuation). Contrast agents show perfusion (CT perfusion). | High ionizing radiation dose; poor soft-tissue contrast without agents. |
| Magnetic Resonance Imaging (MRI) | 0.5 - 2.0 mm | 50 ms - 2 seconds | Proton density, T1/T2 relaxation, flow, diffusion. Excellent for perfusion (ASL), diffusion, BOLD fMRI. | High cost, slow imaging speed for some sequences; sensitive to motion. |
| Ultrasound (US) | 0.2 - 1.0 mm (axial) | 20 - 100 ms (up to 5000 fps) | Acoustic impedance, Doppler shift. Excellent for real-time blood flow and tissue strain (elastography). | Limited field of view, operator-dependent, poor through bone/air. |
The Scientist's Toolkit: Essential Research Reagents & Materials for EIT
| Item | Function & Application in EIT Research |
|---|---|
| Ag/AgCl Electrode Gel | Reduces contact impedance and minimizes polarization voltage at the skin-electrode interface for stable measurements. |
| 0.9% Saline / Physiological Buffer | Standard conductive medium for tank phantoms; used for electrode hydration and as a benign conductive bolus. |
| Potato Starch or Agar | Used to create solid/gelatinous conductive phantoms with stable, homogenous conductivity for validation experiments. |
| Graphite Rods / Stainless Steel Electrodes | Inert conductive materials for constructing custom tank phantoms to simulate organs or lesions. |
| Hypertonic Saline (3-5%) | A common, low-cost, and safe conductivity contrast agent for in vivo dynamic imaging (e.g., lung, perfusion). |
| Finite Element Meshing Software (e.g., Netgen, Gmsh, COMSOL) | Creates the computational model of the imaging domain, which is essential for the forward model in reconstruction. |
| GREIT or EIDORS Reconstruction Framework | Open-source software libraries providing standardized algorithms (e.g., GREIT, Gauss-Newton) for image reconstruction and analysis. |
Experimental Protocols
Protocol 1: GREIT Reconstruction Parameter Tuning with a Tank Phantom.
- Phantom Setup: Construct a circular tank (diameter 30 cm) filled with 0.9% saline (conductivity ~1.6 S/m). Place conductive (graphite) or insulating (plastic) targets of known size (2-4 cm) at various positions.
- Data Acquisition: Using a 16-electrode EIT system, collect voltage data using adjacent or opposite drive patterns. Collect one dataset with target present, one without (reference).
- Reconstruction & Analysis: Use the EIDORS toolbox. Reconstruct images using the GREIT algorithm with a uniform prior. Systematically vary the desired
x_size(target size) and noise figure (n_prior) parameters. Quantify performance using metrics like Amplitude Response (AR), Position Error (PE), and Resolution (RES). Select parameters that yield AR near 1, PE < 10% of radius, and optimal RES.
Protocol 2: Spatio-Temporal Reconstruction for Ventilation Imaging.
- Data Acquisition: Collect thoracic EIT data from a subject at 50 fps during normal tidal breathing for 2 minutes. Simultaneously record respiratory belt transducer data.
- Data Gating: Segment EIT data frames into 10 bins based on the phase of the respiratory cycle (e.g., from end-expiration to peak inspiration and back).
- Model Generation: Create an average boundary shape for each respiratory phase bin from the voltage data.
- Reconstruction: Perform separate, independent reconstructions for each phase bin using a FEM mesh adapted to the average boundary shape of that bin. Alternatively, implement a 4D (3D+time) reconstruction with temporal regularization.
- Evaluation: Compare the consistency of tidal impedance variation in a dorsal ROI between the dynamic shape-corrected method and a single static mesh method. The corrected method should show less spatial "bleeding" of the impedance change into ventral regions.
Diagrams
Technical Support Center: Troubleshooting EIT Image Reconstruction
FAQs & Troubleshooting Guides
Q1: During dynamic lung imaging, my reconstructed images show severe blurring and loss of boundary definition. What could be the cause and how can I correct it? A: This is a common challenge in EIT reconstruction, often stemming from an inaccurate or evolving forward model. The boundary voltage measurements (V_m) are highly sensitive to changes in electrode contact and thoracic geometry not reflected in the static model (A).
- Troubleshooting Protocol:
- Verify Electrode Contact: Re-check all electrode impedance values. A deviation >10% from the baseline set indicates poor contact. Clean the skin and reapply electrodes.
- Update Forward Model: If the subject has changed position, implement a boundary shape estimation step. Use the measured boundary data to iteratively update the finite element model (FEM) mesh coordinates before solving the inverse problem.
- Regularization Tuning: Temporarily increase the hyperparameter (λ) for the regularization term (e.g., Tikhonov). This stabilizes the solution at the cost of some spatial resolution. Systematically reduce λ while monitoring image quality.
- Experimental Methodology for Validation:
- Use a tank phantom with known, movable internal conductivity targets.
- Collect reference data with targets in "position A." Slightly shift the phantom to simulate patient movement and collect new data without updating the model in software.
- Reconstruct both datasets using the same model. The shift will cause artifacts mimicking clinical blurring.
- Repeat reconstruction with a boundary-corrected model to demonstrate restoration of target shape and position.
Q2: My reconstructed images exhibit high noise ("salt-and-pepper" artifacts) despite using clinical-grade equipment. Which step in the pipeline should I optimize? A: This typically points to instability in the inverse solution, often due to ill-posedness. The primary lever is the choice and weighting of the regularization method.
- Troubleshooting Protocol:
- Switch Regularization: Move from 1st-order (Tikhonov) to 2nd-order (Laplacian) spatial regularization. This penalizes sharp, unrealistic jumps between neighboring pixels, promoting smoother, more physiologically plausible images.
- Implement Temporal Regularization: For dynamic processes like ventilation, use a one-step Gauss-Newton solver with temporal regularization. This uses the previous frame's solution as a prior for the current frame, dramatically reducing frame-to-frame noise.
- Spatial Pre-smoothing: Apply a Gaussian filter to the boundary voltage data (V) prior to reconstruction. Use a small kernel (σ = 0.5-1.5) to avoid losing essential signal information.
- Experimental Methodology for Comparison:
- Acquire a stable dataset from a saline phantom with a single, fixed conductive target.
- Reconstruct the same data frame using three methods: (i) Tikhonov with a manually optimized λ, (ii) Laplacian regularization, and (iii) a time-difference method with temporal regularization.
- Quantify the Signal-to-Noise Ratio (SNR) and Contrast-to-Noise Ratio (CNR) within identical Regions of Interest (ROI) for each output image.
Q3: When comparing EIT-derived tidal impedance variation to spirometry, I observe a consistent amplitude offset. How should I calibrate my system? A: Absolute EIT impedance values are difficult to calibrate; focus on robust relative change. The offset likely arises from the choice of reference frame (Vref) in the time-difference imaging protocol (ΔV = V - Vref).
- Troubleshooting Protocol:
- Re-select Reference Frame: Do not use a single end-expiratory frame. Instead, calculate Vref as the temporal average over a stable period (e.g., 5-10 breathing cycles). This minimizes bias from any one potentially anomalous measurement.
- Normalize Output: Express tidal variation as a percentage of the global impedance change (ΔZ/ΔZtotal) over a defined maneuver (e.g., a vital capacity breath).
- Cross-Validate with Gold Standard: Perform a linear regression between the EIT-derived global tidal variation (in arbitrary ΔZ units) and spirometric tidal volume (in mL) across multiple breaths. Use the resulting calibration coefficient for subsequent experiments.
- Experimental Calibration Protocol:
- Connect a mechanical lung simulator to a test subject or mannequin equipped with an EIT belt and a spirometer.
- Program the simulator to deliver precise tidal volumes (e.g., 300mL, 500mL, 700mL).
- Record simultaneous EIT and spirometry data.
- Plot EIT global impedance change (y-axis) against spirometer volume (x-axis) to generate a system-specific calibration curve and equation.
Table 1: Comparison of Common EIT Image Reconstruction Algorithms in Thoracic Imaging
| Algorithm (Regularization) | Spatial Resolution (CR) | Noise Robustness (SNR in dB) | Computation Time (ms/frame) | Best Use Case |
|---|---|---|---|---|
| Linear Back-Projection (LBP) | Low (0.25) | Poor (15.2) | Very Fast ( < 10) | Real-time qualitative trend monitoring |
| Tikhonov (1st Order) | Medium (0.41) | Medium (22.7) | Fast (45) | Static imaging, stable phantom studies |
| GREIT (Gauss-Newton) | High (0.68) | High (28.5) | Medium (120) | Dynamic clinical imaging (ventilation) |
| Total Variation (TV) | Very High (0.72) | Low (18.9)* | Slow (950) | Sharp discontinuity imaging (e.g., tumor detection) |
*CR: Contrast Recovery (1.0 is perfect). *TV is susceptible to staircasing noise artifacts.
The Scientist's Toolkit: Key Reagent & Hardware Solutions
Table 2: Essential Materials for a Bench-Top EIT Validation Experiment
| Item / Reagent | Function & Specification | Critical Notes |
|---|---|---|
| Ag/AgCl Electrode Gel | Provides stable, low-impedance electrical contact between electrode and substrate (skin/phantom). | Use high-chloride concentration gel (>0.1M NaCl) to minimize polarization voltage. |
| 0.9% NaCl (Physiological Saline) | Standard conductive medium for tank phantoms. Mimics average thoracic conductivity (~0.2 S/m). | Conductivity must be temperature-controlled (±0.5°C) for quantitative studies. |
| Agarose Phantom (1-2%) | Solidified, stable test medium with embedded insulating/conductive targets. Allows for precise geometry. | Add NaCl to agarose solution pre-solidification to set desired background conductivity. |
| Conductive Rubber Electrode Belt | Flexible array of integrated electrodes for thoracic imaging. | Belt tension must be standardized and reported; it significantly affects contact impedance. |
| Isolated Current Source / Multi-plexer | Injects a safe, precise alternating current (50kHz-1MHz, 1-5mA) between electrode pairs. | Safety Critical: Must be electrically isolated for human/animal subject use. |
| Synchronized Spirometer / Flow Sensor | Provides gold-standard volumetric data for calibrating and validating functional EIT images. | Ensure analog/digital sync signal is shared with EIT data acquisition system. |
Experimental Workflow & Pathway Visualizations
Title: EIT Research Workflow with Troubleshooting Loops
Title: EIT Reconstruction Stabilization Pathways
Conclusion
EIT image reconstruction remains a vibrant field of research, balancing fundamental physical and mathematical constraints against innovative computational solutions. The journey from the foundational ill-posed inverse problem to the application of deep learning and robust validation frameworks demonstrates significant progress. While challenges in absolute quantification and spatial resolution persist, EIT's unparalleled temporal resolution, non-invasiveness, and functional sensitivity secure its unique value proposition. For biomedical researchers and drug development professionals, the future lies in hybrid approaches: integrating EIT with anatomical priors, developing task-specific reconstruction algorithms for monitoring drug efficacy or disease progression, and advancing towards standardized clinical protocols. Continued collaboration across computational physics, electrical engineering, and clinical medicine is essential to translate EIT's potential into reliable, routine tools for dynamic physiological imaging and therapeutic monitoring.