Poly(2-Hydroxyethyl Methacrylate) Hydrogels: From Foundational Material to Advanced Drug-Eluting Contact Lens Applications
This comprehensive review explores the enduring role of poly(2-hydroxyethyl methacrylate) (PHEMA) hydrogels in contact lens applications, with a specific focus on the evolving frontier of ophthalmic drug delivery.
Poly(2-Hydroxyethyl Methacrylate) Hydrogels: From Foundational Material to Advanced Drug-Eluting Contact Lens Applications
Abstract
This comprehensive review explores the enduring role of poly(2-hydroxyethyl methacrylate) (PHEMA) hydrogels in contact lens applications, with a specific focus on the evolving frontier of ophthalmic drug delivery. It covers the foundational chemistry and intrinsic properties of PHEMA that established it as a benchmark material. The article details advanced methodological approaches for fabricating and functionalizing PHEMA-based lenses, including the integration of natural biomaterials to overcome inherent limitations in drug loading and release kinetics. A critical analysis addresses key challenges such as low oxygen permeability and uncontrolled drug release, presenting optimization strategies like copolymerization and surface modifications. Finally, the review provides a comparative validation of PHEMA against modern silicone hydrogels and emerging natural biomaterials, contextualizing its unique value proposition for researchers and drug development professionals working on therapeutic ophthalmic devices.
The PHEMA Foundation: Chemistry, Properties, and Historical Significance in Contact Lenses
Chemical Structure and Fundamental Properties of PHEMA Hydrogels
Poly(2-hydroxyethyl methacrylate), or pHEMA, is a foundational synthetic polymer that revolutionized eye care with the development of the first soft corneal contact lens [1]. Its unique molecular structure, comprising a hydrophobic carbon backbone with hydrophilic hydroxyl-functionalized side chains, enables the formation of hydrogels—three-dimensional, cross-linked networks capable of absorbing significant amounts of water while maintaining structural integrity [2]. This balance of properties, including biocompatibility, optical clarity, and mechanical stability, has established pHEMA as a dominant material in the traditional contact lens market and a critical component in biomedical research [3] [2]. Within the context of contact lens applications, ongoing research focuses on enhancing pHEMA's inherent characteristics, such as improving surface wettability, mechanical strength, and functionality for sustained drug delivery, to address limitations like dry eye syndrome and protein deposition [1]. This document outlines the fundamental properties and provides detailed experimental protocols for the synthesis and characterization of pHEMA-based hydrogels, serving as a guide for researchers and scientists in the field.
Fundamental Properties and Performance Data
The performance of pHEMA hydrogels in contact lens applications is governed by a set of key physicochemical properties. These include water content, which influences comfort and oxygen permeability; mechanical properties, which affect durability and handling; and optical transparency, which is critical for vision. The following tables summarize quantitative data for these properties across different pHEMA-based formulations, providing a basis for comparison and material selection.
Table 1: Physicochemical Properties of pHEMA Hydrogels with Different Crosslinkers
| Crosslinking Agent | Equilibrium Water Content (EWC%) | Tensile Stress (MPa) | Young's Modulus (MPa) | Onset Decomposition Temperature (°C) | Citation |
|---|---|---|---|---|---|
| TEGDA (Triethylene glycol dimethacrylate) | ~31% | Highest value reported | Best at low water content | 280 | [4] |
| HDODA (1,6-hexanediol diacrylate) | ~37% | - | - | 275 | [4] |
| EGDMA (Ethylene glycol dimethacrylate) | - | - | - | ~190 | [4] |
| mHA-β-CD (Methacrylated hyaluronan-β-cyclodextrin) | ~60% | Good mechanical properties reported | - | - | [1] |
| Standard pHEMA (Reference) | ~30% | - | - | - | [1] |
Table 2: Functional Performance of Modified pHEMA Hydrogels
| Hydrogel Material | Key Functional Property | Performance Outcome | Citation |
|---|---|---|---|
| p(HEMA-co-mHA-β-CD) | Surface Hydrophilicity (Water Contact Angle) | Reduced to ~50°-60° vs. ~80° for standard pHEMA | [1] |
| p(HEMA-co-mHA-β-CD) | Tear Protein Deposition | Enhanced resistance to Bovine Serum Albumin (BSA) and Lysozyme | [1] |
| p(HEMA-co-mHA-β-CD) | Drug Release (Puerarin) | Sustained release over 90 hours; release kinetics fit to Korsmeyer-Peppas model | [1] |
| pHEMA-gr-PVP | Surface Hardness & Heat Resistance | Increased with higher PVP content in initial composition | [5] |
| pHEMA-gr-PVP | Elasticity (Swollen State) | Increased with higher PVP content | [5] |
Experimental Protocols
Protocol 1: Synthesis of p(HEMA-co-mHA-β-CD) Hydrogel
This protocol describes the synthesis of an advanced pHEMA copolymer using methacrylated hyaluronic acid functionalized with β-cyclodextrin (mHA-β-CD) as a macromolecular crosslinker. This formulation aims to enhance hydrophilicity, mechanical strength, and sustained drug delivery capability [1].
- Objective: To synthesize a pHEMA-based copolymer hydrogel with high water content, good mechanical properties, and sustained drug release functionality.
- Principle: The rigid, hydrophilic mHA-β-CD macromer acts as a functional crosslinker, copolymerizing with HEMA monomers via free radical polymerization to form a robust network. β-cyclodextrin's ability to form inclusion complexes with drug molecules enables sustained release [1].
Experimental Workflow: Synthesis of p(HEMA-co-mHA-β-CD) Hydrogel
Materials:
- HEMA (2-hydroxyethyl methacrylate): Primary monomer. Must be purified and distilled under vacuum before use to remove inhibitors [1] [5].
- mHA-β-CD (Methacrylated hyaluronan-β-cyclodextrin): Functional macromolecular crosslinker. Synthesized in a multi-step process prior to hydrogel synthesis [1].
- APS (Ammonium Persulfate): Initiator for free radical polymerization [1].
- Deionized Water: Solvent for polymerization and hydration.
Procedure:
- Monomer Solution Preparation: Dissolve the synthesized mHA-β-CD macromer in HEMA monomer. The ratio of mHA-β-CD to HEMA determines the final crosslinking density and properties [1].
- Initiation: Add ammonium persulfate (APS) to the monomer solution to initiate the polymerization reaction.
- Polymerization: Pour the solution into a suitable mold (e.g., a contact lens mold) and allow the free radical polymerization to proceed to completion, forming a solid polymer network.
- Post-processing: Remove the synthesized hydrogel from the mold and hydrate it in deionized water or a buffered saline solution. Rinse extensively to remove any unreacted monomers, initiator, or soluble oligomers [1] [5].
Characterization Methods:
- Nuclear Magnetic Resonance (NMR): Verify the chemical structure and composition of the mHA-β-CD derivative and the final copolymer [1].
- Equilibrium Water Content (EWC): Measure the water absorption capacity using the formula:
EWC% = [(W_s - W_d) / W_s] * 100, where Ws is the swollen hydrogel weight and Wd is the dry hydrogel weight [1] [4]. - Water Contact Angle: Assess surface wettability using a goniometer. A lower angle indicates higher hydrophilicity [1].
- Tensile Testing: Determine mechanical properties (tensile strength, elongation at break) using a universal testing machine [1] [4].
- UV-Vis Spectroscopy: Evaluate optical transparency in the visible light range [1].
- Drug Release Kinetics: Conduct in vitro release studies using Franz diffusion cells or similar apparatus, with the release data often modeled using the Korsmeyer-Peppas equation [1] [6].
Protocol 2: Synthesis of pHEMA-gr-PVP Graft Copolymer Hydrogel
This protocol details the synthesis of a pHEMA hydrogel grafted with polyvinylpyrrolidone (PVP) using an iron(II) sulfate initiation system. This method produces macroporous hydrogels at room temperature and in the presence of air, simplifying the process [5].
- Objective: To synthesize a grafted pHEMA-PVP copolymer hydrogel with a macroporous structure and tunable sorption-mechanical properties.
- Principle: Polymerization of HEMA in the presence of PVP, initiated by Fe²⁺ ions, results in a grafted, cross-linked copolymer network. PVP acts as a pore-forming agent and modifies the hydration and mechanical characteristics of the resulting hydrogel [5].
Experimental Workflow: Synthesis of pHEMA-gr-PVP Hydrogel
Materials:
- HEMA (2-hydroxyethyl methacrylate): Primary monomer. Must be purified and distilled under vacuum [5].
- PVP (Polyvinylpyrrolidone), M_w ~28,000: Grafting polymer. Should be dried at 338 K in a vacuum before use.
- Iron(II) Sulfate (FeSO₄): Initiation catalyst.
- Deionized Water: For hydration and rinsing.
Procedure:
- Solution A (Fe²⁺): Dissolve 0.05% by weight of FeSO₄ in approximately one-third of the total required HEMA monomer.
- Solution B (PVP): Dissolve the desired amount of PVP (typically 10-40 parts per 100 parts HEMA) in the remaining two-thirds of HEMA.
- Mixing: Combine Solution A and Solution B to form a homogeneous mixture without insoluble agglomerates.
- Polymerization: Cast the mixture into a polymerization mold. The polymerization will proceed at room temperature, in air, over 0.3 to 1.5 hours, depending on the formulation.
- Hydration and Purification: Rinse the polymerized product extensively in distilled water to remove unreacted HEMA and, crucially, any PVP that was not grafted onto the polymer network [5].
Characterization Methods:
- Fourier-Transform Infrared Spectroscopy (FTIR): Confirm the formation of the graft copolymer and the presence of PVP [5].
- Scanning Electron Microscopy (SEM): Visualize the macroporous structure (pore sizes of 10–30 μm) [5].
- Thermogravimetric Analysis (TGA) / Differential Thermal Analysis (DTA): Evaluate thermal stability and decomposition profile [4] [5].
- Sorption-Diffusion Studies: Measure water uptake capacity and kinetics [5].
- Mechanical Testing: Assess tensile strength and elasticity of the swollen hydrogel [5].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for pHEMA Hydrogel Research
| Reagent | Function / Role in Research | Key Consideration |
|---|---|---|
| HEMA Monomer | The primary building block for forming the polymer backbone. | Requires purification (distillation) to remove inhibitors like MEHQ for reproducible polymerization [5]. |
| EGDMA / TEGDA / HDODA | Small molecular crosslinkers that control the mesh size and density of the polymer network. | Type and concentration directly and significantly impact mechanical strength, water content, and transparency [1] [4]. |
| PVP (Polyvinylpyrrolidone) | A hydrophilic polymer used as a grafting agent to modify water content, elasticity, and surface properties. | The amount of PVP that is successfully grafted (vs. washed away) determines the final material properties [5]. |
| Methacrylated Hyaluronic Acid (mHA) | A rigid, hydrophilic macromer used as a co-monomer and crosslinker to enhance mechanical strength and hydrophilicity. | The degree of methacrylation controls its reactivity and integration into the pHEMA network [1]. |
| β-Cyclodextrin (β-CD) | A functional additive that provides host-guest interaction sites within the hydrogel, enabling sustained drug delivery. | Must be chemically bonded to the polymer network (e.g., via mHA) to prevent leaching and enable effective drug encapsulation [1]. |
| Ammonium Persulfate (APS) | A common thermal initiator for free radical polymerization reactions. | Concentration affects the polymerization rate and the molecular weight of the resulting polymer chains. |
| Iron(II) Sulfate (FeSO₄) | An initiation catalyst for room-temperature polymerization, particularly useful in graft copolymerization with PVP. | Allows for rapid polymerization in air, simplifying the process [5]. |
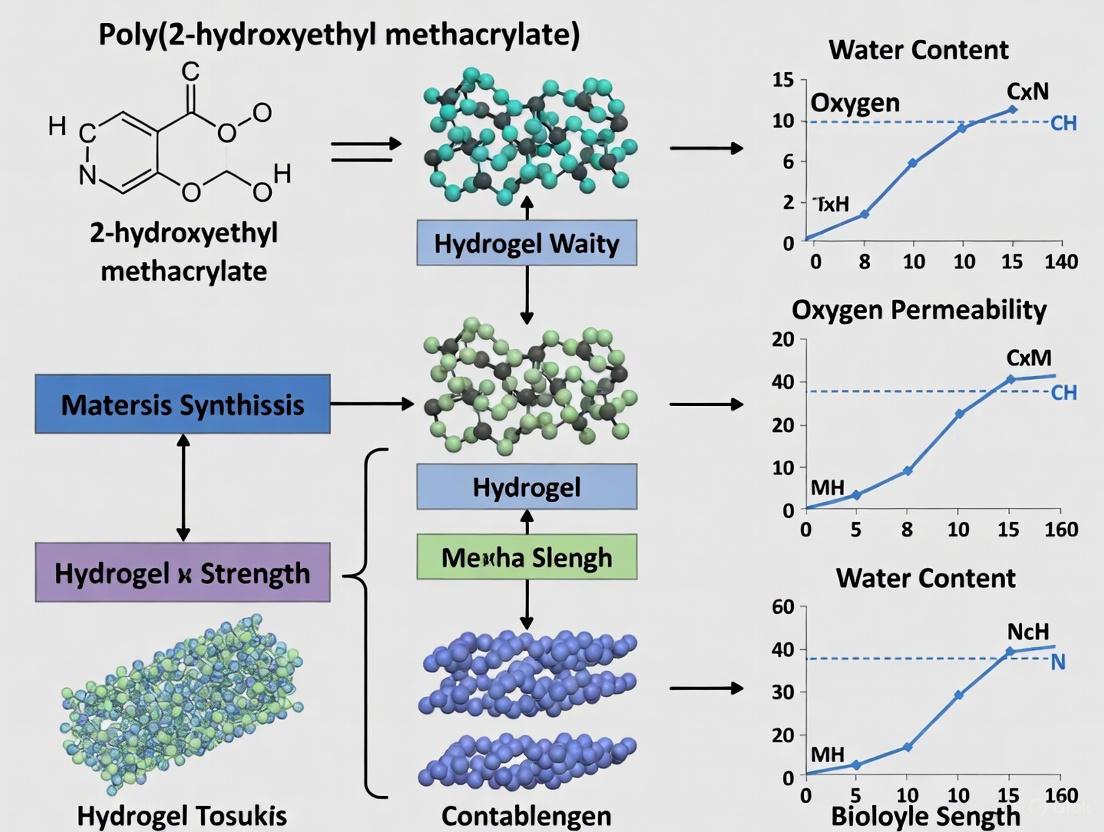
Structure-Property Relationships in pHEMA Hydrogels
The properties of a pHEMA hydrogel are not intrinsic but are directly engineered through its chemical composition and synthesis conditions. The following diagram illustrates the logical relationship between key structural modifications and the resulting physicochemical properties.
Structure-Property Relationships in Modified pHEMA Hydrogels
Historical Context and Scientific Breakthrough
The invention of soft contact lenses represents a convergence of material science and biomedical engineering, pioneered by the Czech chemist Otto Wichterle. Born in 1913, Wichterle preferred a life in science over a career in his family's business [7]. His research trajectory changed during a train ride in 1952, where a conversation with an official from the Ministry of Health sparked his interest in biological plastics [7]. This encounter initiated Wichterle's lifelong journey into hydrogel development.
By 1952, Wichterle and his colleague Drahoslav Lím began intensive research on biocompatible plastics [8]. Within just six months, they successfully synthesized a hydrophilic gel known as poly(2-hydroxyethyl methacrylate) or pHEMA [7] [9]. This material exhibited unique properties ideal for biological applications: it was flexible, oxygen permeable, and optically clear [7]. The researchers recognized that pHEMA's capacity to absorb up to 40% water while maintaining suitable mechanical properties and transparency made it potentially suitable for ocular applications [8].
Despite this promising discovery, Wichterle faced significant institutional challenges. The Ministry of Health in Czechoslovakia rejected his proposal for developing contact lenses from pHEMA [7]. Political purges led to his removal from the Institute of Chemical Technology in 1958, forcing him to continue research domestically [7] [8]. By 1961, with budget cuts ceasing hydrogel investigations at the Institute of Macromolecular Chemistry, Wichterle was forced to resolve lens production issues at his home [7].
The pivotal breakthrough occurred in late 1961 when Wichterle succeeded in producing the first four hydrogel contact lenses on a home-made apparatus built using a children's building kit (Merkur), a bicycle dynamo, and a bell transformer [8]. On Christmas afternoon, with his wife Linda's assistance, he produced lenses using a centrifugal casting procedure on his kitchen table [8]. Although these initial lenses had incorrect optical power, they demonstrated exceptional comfort, validating pHEMA's suitability for ocular use [8].
Fundamental Properties of pHEMA Hydrogels
pHEMA belongs to a class of synthetic hydrogels characterized by highly hydrophilic polymeric networks. The material's molecular structure enables unique physicochemical properties that make it ideal for contact lens applications and other biomedical uses.
Physicochemical Characteristics
pHEMA is a biocompatible, non-biodegradable, and optically transparent hydrophilic polymer [9]. In its dry state, pHEMA exists as a hard and brittle material, but upon swelling with water or biological fluids, it becomes flexible and soft while maintaining optical clarity [9]. This transition occurs due to the hydrophilic pendant groups in its chemical structure that facilitate water absorption.
The typical glass transition temperature (Tg) of pHEMA ranges between 358–393 K, with a density of 1.15–1.34 g mL⁻¹ [9]. The polymer demonstrates resistance to crack propagation, leading to high load-bearing ability despite its hydrogel nature [9]. The mechanical (tensile strength and Young's modulus) and optical (light transmission) properties, oxygen permeability, and water absorption of pHEMA-based hydrogels can be modified through different polymerization techniques, copolymerization, and varying cross-linking rates [9].
pHEMA in Biomedical Applications
Beyond contact lenses, pHEMA's unique properties have enabled diverse biomedical applications:
- Bone Tissue Regeneration: pHEMA/hydroxyapatite biocomposites exhibit elastomeric properties but require degradable cross-linkers for practical application [9]
- Wound Healing: pHEMA-based dressings provide transparency and biocompatibility, though they have limitations in exudate absorbability [9]
- Drug Delivery Systems: pHEMA serves as a carrier for controlled drug release, with applications in cancer therapy and ocular drug delivery [9] [10]
- Blood-Contacting Devices: Recent research incorporates degradable cross-linkers and graphene-based materials to enhance mechanical properties while maintaining hemocompatibility [11]
Table 1: Advantages and Limitations of pHEMA in Biomedical Applications
| Application | Advantages | Disadvantages | References |
|---|---|---|---|
| Contact Lenses | Inexpensive, biocompatible, abundant copolymer possibilities | Protein deposition issues | [9] |
| Bone Tissue Generation | Biocompatibility, excellent adhesion-promoting to other polymers, elastomeric properties | Non-degradable, requiring cross-linker | [9] |
| Wound Healing | Transparency, biocompatibility | Low exudate absorbability, non-degradable, requiring cross-linker | [9] |
| Cancer Therapy | Stimuli-responsive, inexpensive, easily combined with different polymers and drugs | Non-degradable, requiring cross-linker | [9] |
Evolution of pHEMA-Based Contact Lens Manufacturing
Initial Production Challenges
Wichterle's early attempts at lens manufacturing in 1957 involved producing approximately 100 soft lenses from closed polystyrene molds [7]. However, these initial efforts faced significant technical challenges: material contraction during polymerization caused edges to split and tear during removal from molds [7]. Each imperfect lens required manual finishing with a fingernail file, highlighting the need for a more sophisticated manufacturing approach [7].
The development of centrifugal casting in 1961 represented the critical innovation that enabled viable lens production [8]. This process utilized pHEMA's unique properties under rotational forces, allowing precise lens formation with consistent optical qualities and edge integrity.
Manufacturing Workflow: Historical to Contemporary
The original manufacturing process developed by Wichterle has evolved into sophisticated modern protocols. The following workflow diagrams capture both historical and contemporary approaches to pHEMA hydrogel contact lens production.
Advanced Material Formulations
Contemporary research continues to enhance pHEMA's properties for improved contact lens performance. Recent innovations include:
- Enhanced Mechanical Properties: pHEMA hydrogels fabricated in water/ionic liquid mixtures achieve elongation at break up to 705% and tensile strength up to 173 kPa at swollen equilibrium states while maintaining high transparency [12]
- Antimicrobial Strategies: Incorporation of silver nanoparticles, antibiotics, and antimicrobial agents to protect against microbial keratitis [9]
- Drug-Eluting Systems: Development of pHEMA-based lenses for controlled ocular drug delivery with zero-order release kinetics [10]
Table 2: Quantitative Properties of Advanced pHEMA Hydrogels
| Property | Standard pHEMA | Enhanced pHEMA [12] | Measurement Conditions |
|---|---|---|---|
| Tensile Strength | ~50-100 kPa | Up to 173 kPa | Swollen equilibrium state |
| Elongation at Break | ~200-400% | Up to 705% | Swollen equilibrium state |
| Light Transmittance | >90% | >90% | Visible spectrum |
| Water Content | 38-42% | 38-42% | Equilibrium in saline |
| Oxygen Permeability (Dk) | 8-12 barrers | 8-12 barrers | 35°C |
Experimental Protocols
Protocol 1: Synthesis of pHEMA Hydrogels for Contact Lens Applications
Principle: pHEMA hydrogels are formed through free radical polymerization of HEMA monomer in the presence of a cross-linking agent, creating a three-dimensional network that swells in water [9] [2].
Materials:
- 2-hydroxyethyl methacrylate (HEMA) monomer
- Ethylene glycol dimethacrylate (EGDMA) cross-linker
- Photoinitiator (e.g., Irgacure 2959)
- Deionized water
- Nitrogen gas for degassing
- UV light source (305 nm)
Procedure:
- Solution Preparation: Combine HEMA (11.6 mL) with EGDMA (44 μL) in deionized water (8.6 mL) [10]
- Initiation: Add photoinitiator (100 μL of 0.1 g/mL in DMSO) to the monomer solution [10]
- Degassing: Purge the solution with nitrogen gas for 40 minutes to remove oxygen which inhibits polymerization [10]
- Molding: Transfer 160 μL of solution into a 100-μm-deep cylindrical rubber mold (16 mm diameter) [10]
- Polymerization: Cover with a glass slide and polymerize with 305-nm UV light for 60 minutes in a nitrogen environment [10]
- Hydration: Carefully remove the polymerized hydrogel and hydrate in sterile saline solution for 24 hours
- Characterization: Evaluate physical properties including water content, transparency, and mechanical strength
Technical Notes:
- Monomer to cross-linker ratio significantly affects mechanical properties and swelling behavior [9]
- For enhanced mechanical properties, consider polymerization in water/ionic liquid mixtures (e.g., 1-butyl-3-methylimidazolium chloride) [12]
- Sterilization methods (autoclave, gamma irradiation) may affect hydrogel properties and require validation
Protocol 2: Fabrication of Drug-Eluting pHEMA Contact Lenses
Principle: This protocol describes creating a drug-eluting contact lens using a dual polymer system with a PLGA drug core coated with pHEMA, enabling sustained drug release [10].
Materials:
- PLGA (65% lactic acid, 35% glycolic acid; 118-kDa or 18-kDa molecular mass)
- Therapeutic agent (e.g., ciprofloxacin, fluorescein)
- Ethyl acetate
- HEMA monomer and cross-linker components (as in Protocol 1)
- Teflon casting wells
- Lyophilizer
Procedure: A. Drug-Polymer Film Fabrication:
- Dissolve PLGA in ethyl acetate (15 mL) [10]
- Add drug compound (e.g., 20 mg ciprofloxacin) and mix to form uniform suspension [10]
- Pour suspension into Teflon well and evaporate ethyl acetate overnight in fume hood [10]
- Lyophilize for 48 hours to remove residual solvent [10]
- Punch rings with 14-mm outer diameter and 5-mm central aperture from drug-PLGA film [10]
B. pHEMA Coating:
- Prepare pHEMA solution as described in Protocol 1 [10]
- Polymerize a thin bottom pHEMA layer in mold using UV light [10]
- Manually press drug-PLGA film onto the dried pHEMA gel [10]
- Add additional pHEMA solution to fully encapsulate the drug-polymer film [10]
- Complete polymerization with UV light for 60 minutes [10]
C. Drug Release Characterization:
- Conduct release studies in phosphate-buffered saline at 37°C with continuous shaking [10]
- Sample release medium at predetermined intervals and analyze drug concentration
- Verify antimicrobial efficacy of released compounds using appropriate assays [10]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents for pHEMA Hydrogel Contact Lens Research
| Reagent/Material | Function | Research Considerations | References |
|---|---|---|---|
| HEMA Monomer | Primary building block for hydrogel formation | Purify to remove inhibitors; toxic in monomer form but safe when polymerized | [9] [10] |
| EGDMA Cross-linker | Creates 3D network structure; controls mesh size | Concentration affects mechanical properties and swelling ratio | [10] |
| Irgacure 2959 | Photoinitiator for UV polymerization | Concentration affects polymerization rate and final properties | [10] |
| PLGA (65:35 LA:GA) | Biodegradable polymer for drug-eluting systems | Molecular weight (18-118 kDa) controls drug release kinetics | [10] |
| Ionic Liquids (BmimCl) | Enhances mechanical properties | Creates denser, more homogeneous microstructure in pHEMA | [12] |
| Hydroxyapatite | Ceramic component for composite hydrogels | Enhances bioactivity for bone tissue applications | [9] |
| Antimicrobial Agents | Prevents microbial colonization | Silver nanoparticles, antibiotics reduce infection risk | [9] |
Contemporary Applications and Future Perspectives
Advanced Contact Lens Technologies
Modern contact lens technology continues to build upon Wichterle's pHEMA foundation with several key advancements:
- Multifocal Designs: Latest innovations include daily disposable multifocal contact lenses incorporating blue light filtration (OptiBlue Light Filter), tear film stabilization (TearStable Technology), and blink-stabilized designs [13]
- Myopia Management: Increasing focus on contact lenses for childhood myopia control, with research supporting their efficacy in slowing myopia progression [14]
- Smart Lens Technologies: Development of electronics-free contact lenses capable of monitoring intraocular pressure in real-world conditions (miLens) [14]
Integration of Artificial Intelligence
The field of contact lens management is increasingly incorporating artificial intelligence to enhance clinical outcomes:
- AI-Driven Diagnostics: Machine learning algorithms analyze ocular images for precise fitting and complication detection [15]
- Predictive Modeling: AI tools anticipate patient needs and potential complications, enabling proactive care [15]
- Digital Patient Management: Hybrid care platforms combine in-person visits with remote monitoring to improve patient adherence and retention [15]
Future Research Directions
The future of pHEMA hydrogels in contact lens applications includes several promising research avenues:
- Enhanced Material Properties: Continued development of pHEMA composites with improved oxygen permeability, mechanical strength, and surface wettability [2] [12]
- Personalized Medicine: Lens customization based on individual ocular parameters and therapeutic needs [15]
- Extended Drug Delivery: Advancement of drug-eluting systems capable of sustained release over weeks to months [10]
- Biointegrated Sensors: Development of diagnostic contact lenses capable of monitoring physiological parameters and disease markers [14]
The legacy of Otto Wichterle's invention continues to drive innovation in ocular biomaterials, with pHEMA remaining a foundational polymer for both current applications and future breakthroughs in contact lens technology. The integration of material science, pharmaceutical technology, and digital health platforms promises to further enhance the functionality and therapeutic potential of pHEMA-based contact lenses in the coming decades.
Quantitative Material Properties of PHEMA Hydrogels
The utility of poly(2-hydroxyethyl methacrylate) (PHEMA) hydrogels in contact lens applications is quantified by a set of critical physical, mechanical, and optical properties. These characteristics, derived from its polymer network structure, directly dictate its performance and comfort as an ophthalmic biomaterial [16].
Table 1: Key Properties of PHEMA Hydrogels for Contact Lens Applications
| Property | Typical Range/Value | Functional Significance in Contact Lenses |
|---|---|---|
| Water Content | 20% to 80% [16] | Enhances oxygen permeability and wearer comfort; mimics the hydrated ocular surface. |
| Tensile Strength | 0.12 - 0.2 MPa [16] | Provides sufficient mechanical integrity to withstand handling and eyelid forces during blinking. |
| Young's Modulus | 0.4 - 1.8 MPa [16] | Imparts softness and flexibility, ensuring comfort on the sensitive corneal tissue. |
| Oxygen Permeability | Correlates with water content [16] | Facilitates corneal oxygenation during wear, which is critical for ocular health. |
| Optical Clarity | High transparency [2] | Ensures unimpaired vision, a fundamental requirement for any optical device. |
Experimental Protocols
Protocol: Synthesis of PHEMA Hydrogels via Bulk Polymerization
This protocol describes the synthesis of PHEMA hydrogels through free radical polymerization, adapted from foundational research on polymerization kinetics [17].
Research Reagent Solutions
- Monomer: 2-hydroxyethyl methacrylate (HEMA). Function: Primary building block of the polymer network. Must be purified by passing through an inhibitor-remover column prior to use [17].
- Crosslinking Agent: Ethylene glycol dimethacrylate (EGDMA) or poly(ethylene glycol) diacrylate (PEGDA). Function: Creates covalent bridges between polymer chains, forming a three-dimensional network that provides mechanical stability and controls swelling [18] [16].
- Initiator: Benzoyl peroxide (BPO) for thermal initiation. Function: Generates free radicals upon heating to initiate the polymerization reaction [17].
- Photoinitiator (Alternative): 1-hydroxycyclohexyl phenyl ketone (HCHPK). Function: Generates free radicals upon exposure to UV light for photopolymerization [18].
Procedure
- Monomer Purification: Pass HEMA monomer through an inhibitor-remover packed column at least twice to remove the hydroquinone monomethyl ether (MEHQ) stabilizer [17].
- Reaction Mixture Preparation: In a glass vial, combine purified HEMA (e.g., 9.5 mL), crosslinking agent (e.g., EGDMA at 0.1-4 mol%), and thermal initiator (e.g., BPO at 0.03 mol/L). Mix thoroughly until a homogeneous solution is obtained [17] [18].
- Degassing (Optional but Recommended): Sparge the mixture with an inert gas (e.g., nitrogen or argon) for 10-15 minutes to remove dissolved oxygen, which can inhibit free radical polymerization.
- Casting and Sealing: Pipette the reaction mixture into an appropriate mold (e.g., a glass mold with a silicone gasket to define thickness). Seal the mold to prevent solvent evaporation and oxygen ingress.
- Polymerization: Place the sealed mold in an oven or thermal chamber. Cure isothermally at a temperature between 52°C and 82°C for a duration sufficient to achieve high conversion (e.g., several hours). The reaction is highly exothermic, particularly during the autoacceleration phase [17].
- Post-Processing: After polymerization, carefully demold the PHEMA hydrogel. Wash the hydrogel extensively in distilled water or an appropriate solvent to remove any unreacted monomers, initiator residues, and sol fraction. Change the washing solution multiple times over 24-48 hours [18].
- Hydration and Storage: Equilibrate the purified hydrogel in a sterile saline solution or buffered solution. Store the hydrated hydrogel in a sealed container at 4°C.
Diagram 1: PHEMA hydrogel synthesis workflow.
Protocol: Characterization of Swelling Behavior and Hydration
Understanding the water uptake capacity and kinetics is essential for predicting hydrogel comfort and oxygen transmissibility [19] [18].
Procedure
- Sample Preparation: Synthesize PHEMA hydrogels as described in Protocol 2.1. Cut into standardized discs (e.g., 10 mm diameter) and dry in a vacuum oven at 50°C until constant weight is achieved (Wd).
- Equilibrium Swelling: Immerse the dried hydrogel discs in a large volume of phosphate-buffered saline (PBS) at a physiological temperature (e.g., 34°C to simulate ocular surface temperature). Allow the hydrogels to swell until equilibrium is reached (typically 24-48 hours).
- Weighing: Remove the hydrogel from the PBS at predetermined time intervals, gently blot with lint-free tissue to remove surface water, and immediately weigh (Ws). Return the hydrogel to the PBS after each measurement until the weight stabilizes.
- Calculation: Calculate the equilibrium water content (EWC) using the formula:
- EWC (%) = [(Ws - Wd) / Ws] × 100
Table 2: Swelling and Mechanical Characterization Methods
| Characterization Method | Measured Parameters | Application in PHEMA Hydrogel Analysis |
|---|---|---|
| Gravimetric Swelling Analysis | Equilibrium Water Content (EWC), Swelling Kinetics | Quantifies hydration capacity and rate, directly related to oxygen permeability and comfort [18]. |
| Rheology | Storage Modulus (G'), Loss Modulus (G''), Mesh Size (ξ) | Determines mechanical stability (G' ~10 kPa suitable for dermal use), viscoelasticity, and network structure which influences drug diffusion [19]. |
| Differential Scanning Calorimetry (DSC) | Polymerization Rate, Conversion, Reaction Enthalpy | Monitors polymerization kinetics, determines degree of monomer conversion, and studies thermal transitions [17]. |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for PHEMA Hydrogel Research
| Reagent/Chemical | Function in Research | Key Consideration |
|---|---|---|
| 2-Hydroxyethyl Methacrylate (HEMA) | Primary monomer for constructing the hydrogel polymer network. | Requires purification to remove polymerization inhibitors (e.g., MEHQ) before use for reproducible kinetics [17]. |
| Poly(Ethylene Glycol) Diacrylate (PEGDA) | A biocompatible crosslinker that defines the network's mesh size and mechanical properties. | The molecular weight and concentration allow tuning of hydrogel stiffness and permeability [18]. |
| Benzoyl Peroxide (BPO) | Thermal free-radical initiator for polymerization. | Must be purified via recrystallization for consistent initiation rates and reaction kinetics [17]. |
| 1-Hydroxycyclohexyl Phenyl Ketone | UV-photoinitiator for light-induced polymerization, enabling spatial control. | Enables rapid curing and fabrication of complex geometries at room temperature [18]. |
| Ethylene Glycol Dimethacrylate (EGDMA) | A common crosslinking agent used to control the hydrogel's swelling and mechanical strength. | The concentration significantly affects the final water content and modulus of the lens material [16]. |
Diagram 2: From reagents to functional lens properties.
Poly(2-hydroxyethyl methacrylate), or PHEMA, is a foundational synthetic hydrogel in contact lens research, prized for its biocompatibility, soft consistency, and high water content [20] [17] [21]. However, its application is constrained by two intrinsic limitations: insufficient oxygen permeability for extended wear and a limited, often uncontrolled, drug loading capacity. This application note details these material limitations and provides validated experimental protocols for their quantification, providing researchers with the methodologies needed to advance the design of next-generation ophthalmic materials.
Oxygen Permeability Barriers in PHEMA Hydrogels
The Fundamental Limitation
In conventional hydrogels like PHEMA, oxygen is primarily transported through the aqueous phase of the material [22]. This mechanism imposes a fundamental upper limit on oxygen permeability (Dk), as the Dk value of pure water is approximately 80 Barrer [23]. PHEMA-based contact lenses typically contain up to only 38% water by mass, which further restricts their oxygen transmissibility [20]. This low permeability can cause the lens to act as a barrier, potentially leading to corneal hypoxia, a condition associated with corneal swelling, red eyes, and other pathological changes [23] [22] [21].
Table 1: Oxygen Permeability and Water Content of Hydrogel Materials
| Material Type | Typical Water Content (%) | Oxygen Permeability (Dk, Barrer or Fatt units) | Primary Oxygen Transport Pathway |
|---|---|---|---|
| PHEMA Homopolymer | ~38% [20] | Below 60 [22] | Water phase [22] |
| Non-Silicone Hydrogel (DMAA-based) | 75-81% [22] | Up to 73.9 [22] | Water phase [22] |
| Silicone Hydrogel (SiHy) | Varies | >100 (can exceed 140) [23] [22] | Hydrophobic silicone phase [23] [22] |
| Pure Water | 100% | ~80 [23] | N/A |
Experimental Protocol: Coulometric Measurement of Oxygen Permeability
Principle: The coulometric method determines oxygen permeability and diffusivity by measuring the flux of oxygen through a hydrogel membrane under a controlled pressure gradient [23].
Materials & Reagents:
- Test Hydrogel Samples: PHEMA sheets or lenses of uniform thickness.
- Coulometric Permeability Cell: Consisting of two chambers separated by the test sample.
- Gas Flow System: For delivering humidified nitrogen (carrier gas) and oxygen (test gas).
- Oxygen Sensor: A coulometric sensor to detect the oxygen flux.
- Data Acquisition System: To record the transient flux response.
Procedure:
- Sample Preparation: Hydrate the PHEMA hydrogel samples in a saline solution until equilibrium swelling is achieved. Precisely measure and record the sample thickness.
- Cell Assembly: Mount the hydrated sample securely in the permeability cell, ensuring no edge leaks.
- Gas Humidification: Bubble both the carrier (N₂) and test (O₂) gases through a water bath to humidify them, preventing sample dehydration during testing.
- Flux Measurement: Expose one side of the sample to humidified O₂ while the other side is purged with humidified N₂, which carries any permeating oxygen to the sensor.
- Data Recording: Record the oxygen flux as a function of time until a steady state is reached.
- Data Analysis: Fit the transient flux data to a mathematical model (e.g., a solution to Fick's law) to calculate the oxygen diffusivity (D) and solubility (k). The oxygen permeability (P) is then calculated as the product: ( P = D \times k ) [23].
Drug Loading Capacity and Release Control
The Challenge of Uncontrolled Release
While PHEMA hydrogels can absorb aqueous drug solutions, a significant limitation is the rapid, uncontrolled release of the loaded therapeutic agent [24]. Simple impregnation methods often lead to a burst release, where a large portion of the drug is released within a short period. This fails to sustain therapeutic concentrations over a clinically useful duration, such as a full day of wear [24]. The primary mechanism for drug transport is diffusion through the water-filled pores of the hydrogel, which, without strategic modification, offers little resistance to rapid drug elution.
Table 2: Key Properties of PHEMA Affecting Drug Loading and Release
| Property | Impact on Drug Delivery | Typical Value / Characteristic for PHEMA |
|---|---|---|
| Water Content | Determines loading capacity for hydrophilic drugs; higher content can weaken polymer network [24]. | ~38% by mass [20]. |
| Polymer Network Mesh Size | Controls diffusion rate of drugs; determined by crosslink density [24]. | Adjustable via crosslinker concentration [17] [25]. |
| Glass Transition Temperature (Tg) | Reflects polymer chain mobility; a stable Tg indicates drug loading does not compromise matrix integrity [24]. | ~425 K (simulated) [20]; remains stable with drug impregnation [24]. |
| Transparency | Essential for functionality; must not be impaired by drug or loading method [24]. | High transparency (up to 99.91% transmittance in similar hydrogels) [22]. |
Experimental Protocol: In-Situ Polymerization for Drug-Loaded PHEMA
Principle: This protocol involves polymerizing HEMA in the presence of a drug and a crosslinker to create a hydrogel matrix where the drug is entrapped within the polymer network, offering more controlled release than post-polymerization soaking.
Materials & Reagents:
- Monomer: 2-hydroxyethyl methacrylate (HEMA).
- Crosslinker: Ethylene glycol dimethacrylate (EGDMA).
- Initiator: UV initiator (e.g., Irgacure 1173) or thermal initiator (e.g., Benzoyl Peroxide, BPO).
- Solvent/Diluent: Deionized water.
- Therapeutic Agent: Drug of choice (e.g., Timolol maleate for glaucoma).
- Molds: Customized lenses or slab molds.
- UV Chamber: For photopolymerization (if using a UV initiator).
Procedure:
- Inhibitor Removal: Pass HEMA monomer through an inhibitor-remover column to ensure efficient polymerization [25].
- Reaction Mixture Preparation: Combine the purified HEMA, deionized water, EGDMA crosslinker, initiator, and the target drug. A typical formulation by weight is 63% HEMA, 35% water, 1% EGDMA, and 1% initiator [25]. Stir the mixture until clear.
- Molding and Polymerization: Pour the solution into pre-designed molds. For UV polymerization, expose the molds to UV light (e.g., 365 nm, 100 W) for 10 minutes [25]. For thermal polymerization, place the molds in an oven at a temperature suitable for the initiator (e.g., 52-82°C for BPO) [17].
- Post-Processing and Hydration: Carefully demold the polymerized drug-loaded hydrogel. Hydrate the lenses in a buffered saline solution to remove any unreacted monomers and to achieve equilibrium swelling before release testing.
- Drug Release Kinetics: Immerse the hydrated drug-loaded lens in a known volume of release medium (e.g., phosphate-buffered saline) under constant agitation. Periodically withdraw samples from the medium and analyze the drug concentration using a validated method (e.g., HPLC or UV-Vis spectroscopy) to construct a release profile over time.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PHEMA Hydrogel Research
| Reagent/Material | Function in Research | Example & Notes |
|---|---|---|
| HEMA Monomer | Primary building block of the hydrogel polymer network. | Requires removal of inhibitor (e.g., monomethyl ether hydroquinone) prior to polymerization [25]. |
| Crosslinker (e.g., EGDMA) | Creates covalent bridges between polymer chains, controlling mesh size and mechanical strength. | Concentration and chain length (e.g., 1-EGDMA, 23-EGDMA) significantly impact oxygen permeability and water content [22] [25]. |
| Polymerization Initiator | Generates free radicals to initiate the chain-growth polymerization reaction. | UV Initiator (Irgacure 1173): For photopolymerization [25]. Thermal Initiator (BPO): For thermal polymerization [17]. |
| Hydrophilic Comonomer (e.g., NVP) | Increases the water content of the PHEMA matrix. | N-Vinylpyrrolidone (NVP) is common; forms P(VP-co-HEMA) copolymers with water content up to 60% [20]. |
| Silicone Monomer (e.g., TRIS, mPDMS) | Enhances oxygen permeability by creating a separate oxygen-transport phase. | Used in silicone hydrogels; inherently hydrophobic and can phase-separate [23]. |
| Model Drug Compounds | For testing drug loading and release profiles. | Timolol maleate (glaucoma) and acetazolamide are used in impregnation studies [24]. |
Advanced Fabrication and Functionalization of PHEMA for Therapeutic Applications
Synthesis and Manufacturing Techniques for PHEMA Hydrogel Lenses
Poly(2-hydroxyethyl methacrylate) (pHEMA) hydrogels have been a cornerstone of contact lens technology since their initial development by Wichterle and Lim in the 1960s [1]. These cross-linked, three-dimensional polymeric networks revolutionized vision correction by offering a biocompatible, oxygen-permeable, and transparent material that could be comfortably worn on the eye [21]. Despite their long-standing use, traditional pHEMA hydrogels face significant limitations including relatively low oxygen permeability, susceptibility to tear protein deposition, and limited functionality for therapeutic applications [1] [26].
Recent research has focused on developing advanced copolymerization strategies and surface modification techniques to address these challenges while maintaining the favorable biocompatibility of pHEMA [27]. This Application Note details contemporary synthesis methodologies and manufacturing protocols for fabricating both conventional and next-generation pHEMA-based hydrogel contact lenses, with particular emphasis on functionalized materials offering improved hydrophilicity, mechanical properties, and sustained drug delivery capabilities for ophthalmic applications.
Fundamental Synthesis Protocols
Conventional pHEMA Hydrogel Synthesis
The synthesis of standard pHEMA hydrogels follows a well-established protocol of free radical polymerization using 2-hydroxyethyl methacrylate (HEMA) monomer with a small molecular crosslinker [1].
Protocol: Basic pHEMA Hydrogel Formation
Reagents Required:
- 2-hydroxyethyl methacrylate (HEMA) monomer
- Crosslinking agent: ethylene glycol dimethacrylate (EGDMA)
- Photoinitiator: 2,2-dimethoxy-2-phenylacetophenone (DMPA) or thermal initiator
- Solvent: Deionized water
- Inhibitor remover beads (if HEMA contains inhibitor)
Procedure:
- Inhibitor Removal: If the HEMA monomer contains monomethyl ether hydroquinone as an inhibitor, pass 30 mL of HEMA through 10 mg of inhibitor remover beads with stirring for approximately 3 minutes. Filter the solution to remove the beads [25].
- Solution Preparation: Combine the purified HEMA (63% w/w) with deionized water (35% w/w), EGDMA crosslinker (1% w/w), and the photoinitiator DMPA (1% w/w). Stir the mixture until it becomes clear and homogeneous [25].
- Molding: Pour the solution into appropriate molds designed for the desired contact lens geometry. For laboratory-scale prototyping, this can involve sandwiching between glass slides with controlled spacers or using custom-fabricated concave molds.
- Polymerization: Expose the molded solution to ultraviolet radiation (365 nm center wavelength, 100 W) for 10 minutes to initiate photopolymerization. Thermal initiation using ammonium persulfate (APS) is a common alternative [1] [25].
- Post-Processing: Carefully demold the polymerized hydrogel. The resulting lens must be hydrated in a saline solution and subjected to rigorous extraction and washing processes to remove any unreacted monomers, initiators, or solvent residues, which is critical for ensuring biocompatibility [28].
Synthesis of Functionalized p(HEMA-co-mHA-β-CD) Hydrogel
To overcome the limitations of conventional pHEMA, a functional copolymer incorporating methacrylated hyaluronan-β-cyclodextrin (mHA-β-CD) has been developed [1].
Protocol: Synthesis of mHA-β-CD Comonomer and Copolymerization
Reagents Required:
- Sodium hyaluronan (HA)
- β-cyclodextrin (β-CD)
- Methacrylic anhydride (MA)
- 1,6-hexanediamine (HDA)
- p-toluenesulfonyl chloride (p-TsCl)
- Coupling agents: 1-(3-Dimethylaminopropyl)-3-ethylcarbodiimide hydrochloride (EDC•HCl) and N-hydroxysuccinimide (NHS)
Procedure:
- Synthesis of mHA-β-CD Derivative:
- Activation of β-CD: React β-CD with p-TsCl to form mono-tosyl-β-CD (M-6-O-Ts-β-CD).
- Amination: Substitute the tosyl group with 1,6-hexanediamine (HDA) to create β-CD-HDA.
- Methacrylation of HA: React HA with methacrylic anhydride to form methacrylated hyaluronic acid (mHA).
- Conjugation: Covalently link the amine groups of β-CD-HDA to the carboxyl groups of mHA using EDC•HCl and NHS as coupling agents, resulting in the mHA-β-CD macromer [1].
- Copolymerization:
- Combine the synthesized mHA-β-CD macromer with HEMA monomer in aqueous solution.
- Use ammonium persulfate (APS) as an initiator for the free radical copolymerization.
- The mHA-β-CD acts as a multifunctional hydrophilic comonomer and macromolecular crosslinker, forming a robust p(HEMA-co-mHA-β-CD) hydrogel network without the need for additional small-molecule crosslinkers like EGDMA [1].
- Synthesis of mHA-β-CD Derivative:
Diagram 1: Experimental workflow for the synthesis of pHEMA-based hydrogels, highlighting key stages from monomer preparation to final characterization.
Material Characterization and Performance Data
The evaluation of synthesized hydrogel lenses involves a comprehensive analysis of their physical, optical, and biological properties to ensure they meet the stringent requirements for ophthalmic use.
Table 1: Comparative Properties of Conventional and Advanced pHEMA-based Hydrogels
| Property | Conventional pHEMA | p(HEMA-co-mHA-β-CD) [1] | pHEMA/β-CD-crHA [26] | Test Method/Aonditions |
|---|---|---|---|---|
| Water Contact Angle (°) | ~80 [1] | 53.8 - 64.5 | ~60 | Static water contact angle measurement |
| Equilibrium Water Content (%) | ~30 [1] | 44.5 - 52.9 | ~55 | Gravimetric analysis after hydration |
| Tensile Strength (MPa) | Baseline | 0.18 - 0.39 | - | Universal testing machine |
| Elongation at Break (%) | Baseline | 112.3 - 185.8 | - | Universal testing machine |
| Light Transmittance (%) | >90 (at 550 nm) [27] | >90 (at 550 nm) | >90 | UV-Vis spectrophotometer |
| Lysozyme Deposition (μg/lens) | High | Significantly Reduced | Significantly Reduced | SDS-PAGE or direct quantification |
| Oxygen Permeability (Dk) | Low | Improved | Improved | Polarographic method |
Table 2: Formulation and Function of Key Research Reagent Solutions
| Reagent | Function/Role in Synthesis | Typical Concentration | Critical Notes |
|---|---|---|---|
| 2-Hydroxyethyl methacrylate (HEMA) | Primary monomer; forms hydrogel backbone | 63% (w/w) in standard recipe [25] | Requires inhibitor removal prior to polymerization |
| Ethylene glycol dimethacrylate (EGDMA) | Small molecular crosslinker; controls network density | 1% (w/w) [25] | Concentration inversely related to equilibrium water content |
| Ammonium Persulfate (APS) | Thermal initiator for free radical polymerization | Varies | Common for bulk polymerization; requires purification post-synthesis |
| 2,2-dimethoxy-2-phenylacetophenone (DMPA) | Photoinitiator for UV-induced polymerization | 1% (w/w) [25] | Enables rapid curing at room temperature |
| Methacrylated Hyaluronan (mHA) | Rigid, hydrophilic comonomer; improves mechanics & wettability | Varies by desired property | Provides active carboxyl and hydroxyl groups for further modification |
| β-Cyclodextrin (β-CD) | Functional additive; enables sustained drug delivery via host-guest complexes | Varies by desired property | Hydrophobic cavity encapsulates drugs; must be covalently bonded to prevent leaching |
Advanced Manufacturing and Surface Engineering
Surface Patterning via Replica Molding
Nanostructuring the lens surface can significantly influence its interaction with ocular tissues and proteins.
Protocol: Replica Mold Nanopatterning of pHEMA Surfaces [27]
Reagents/Materials:
- Silicon wafer with native oxide layer
- pHEMA hydrogel precursor solution
- Focused Ion Beam (FIB) system
Procedure:
- Fabrication of Master Mold: Use a Focused Ion Beam (FIB) to mill an array of nanoscale holes (e.g., tens of nanometers deep) into a silicon wafer, creating a negative pattern of the desired surface features.
- Replica Molding: Pour the standard pHEMA precursor solution onto the fabricated silicon stamp mold.
- Polymerization: Carry out photopolymerization under UV light to cure the hydrogel, thereby transferring the nanopattern from the mold to the hydrogel surface.
- Demolding: Carefully peel the fully polymerized and patterned hydrogel from the mold. The resulting hydrogel surface features randomly distributed nanopillars, which have been shown to potentially suppress the upregulation of cytoskeleton proteins in cells, offering a strategy to prevent conditions like secondary cataracts in intraocular lenses [27].
Interpenetrating Networks and Combination with Silicone
For applications requiring very high oxygen permeability, pHEMA can be combined with silicone-based polymers to form interpenetrating networks (IPNs) or copolymer systems [29].
Table 3: Properties of a Silicone-Hydrogel Combining PDMS and pHEMA-based Polymers [29]
| Property | Trend with Increasing Silicone Content | Impact on Lens Performance |
|---|---|---|
| Oxygen Permeability (Dk) | Increases | Reduces risk of corneal hypoxia, supports extended wear |
| Equilibrium Water Content | Decreases | Can affect comfort and hydration; requires balance |
| Water Contact Angle | Increases (more hydrophobic) | May reduce wettability; necessitates surface treatments |
| Young's Modulus | Decreases | Softer lens, potentially improving comfort |
| Protein Deposition | Varies with hydrophilicity | Lysozyme deposition increases with hydrophilicity of the final formulation |
Diagram 2: Logical relationship between inherent limitations of conventional pHEMA and the advanced material strategies developed to address them, leading to improved functional outcomes.
The synthesis and manufacturing of pHEMA hydrogel lenses have evolved significantly from the basic cross-linked networks first introduced decades ago. The protocols detailed herein—ranging from conventional polymerization to advanced functionalization with mHA-β-CD, and from surface nanopatterning to the formation of silicone IPNs—provide a robust toolkit for researchers and material scientists. These strategies directly address the historical limitations of pHEMA, enabling the creation of next-generation contact lenses with superior comfort, enhanced resistance to protein deposition, and advanced capabilities such as sustained drug delivery. The quantitative data presented confirms that these advanced materials meet the critical optical, mechanical, and biological requirements for successful ophthalmic application, paving the way for their use in both corrective and therapeutic vision care.
The efficacy of conventional ophthalmic treatments, such as eye drops, is significantly limited by physiological barriers and rapid clearance mechanisms, resulting in less than 5% drug bioavailability [30]. Poly(2-hydroxyethyl methacrylate) (PHEMA) hydrogels, a cornerstone material in contact lens fabrication, provide an ideal platform for innovative ocular drug delivery systems. This application note details three primary drug loading methodologies—soaking, molecular imprinting, and physical encapsulation—framed within ongoing thesis research on enhancing PHEMA hydrogel functionality. These methods are engineered to overcome bioavailability challenges by enabling sustained, controlled release of therapeutics directly to the ocular surface, thereby improving treatment outcomes for conditions like glaucoma, dry eye syndrome, and post-surgical inflammation [31] [30] [32].
Performance Comparison of Drug Loading Techniques
The table below summarizes the key characteristics, advantages, and limitations of the three primary drug loading methods as applied to PHEMA-based hydrogels.
Table 1: Comparative Analysis of Drug Loading Techniques for PHEMA Hydrogels
| Loading Method | Mechanism of Action | Sustained Release Duration | Key Advantages | Inherent Limitations |
|---|---|---|---|---|
| Soaking | Passive diffusion of drug molecules from a solution into the hydrogel matrix [33]. | Hours to a few days [34]. | Simple, cost-effective, compatible with commercial lenses [34]. | Limited control, typically exhibits high initial burst release, lower loading capacity [35] [32]. |
| Molecular Imprinting | Creation of specific molecular cavities within the polymer network that exhibit high affinity for a target drug molecule [35] [36]. | Several days to weeks [37]. | High loading capacity, programmable and sustained release, reduces initial burst effect [35] [36]. | Complex fabrication, requires optimization of functional monomer and cross-linker ratios [35] [36]. |
| Physical Encapsulation | Entrapment of drug within a polymeric barrier or nanoparticle dispersed in the hydrogel [31] [30]. | Days to weeks [31] [34]. | Excellent sustained release, protects drug stability, can be combined with other methods [31] [30]. | Potential impact on lens transparency and mechanical properties, complex manufacturing [31] [30]. |
Experimental Protocols
Protocol 1: Drug Loading via the Soaking Method
The soaking method is a straightforward approach to passively load drugs into pre-formed PHEMA contact lenses.
Table 2: Key Reagents for Soaking and Molecular Imprinting
| Reagent Name | Function/Application |
|---|---|
| Senofilcon A or Hilafilcon B Lenses | Pre-formed commercial hydrogel lenses used as substrates for drug loading [33]. |
| Vitamin C (Ascorbic Acid) | A model hydrophilic drug compound for studying loading and release kinetics [33]. |
| Simulated Lacrimal Fluid (SLF) | A pH 7.5 solution mimicking the ionic composition of tears, used for in vitro release studies [36]. |
| N-Vinyl Pyrrolidone (NVP) | A functional monomer used in molecular imprinting to create hydrogen bonds with target drug molecules [35]. |
| Ethylene Glycol Dimethacrylate (EGDMA) | A cross-linking agent that creates a stable three-dimensional network in imprinted hydrogels [35] [36]. |
| Methacrylic Acid (MAA) | A functional monomer that provides ionic interaction sites for drugs containing amino groups [36]. |
Procedure:
- Preparation of Drug Solution: Dissolve the target drug (e.g., Vitamin C, timolol) in a suitable solvent, typically deionized water or a buffer, to a known concentration (e.g., 5 mg/mL for moxifloxacin) [31] [33].
- Lens Immersion: Fully immerse the pre-hydrated or dry PHEMA-based hydrogel lenses in the drug solution. Ensure the lenses are completely submerged and free of air bubbles.
- Loading Incubation: Allow the lenses to soak for a predetermined period (e.g., 24-72 hours) at a controlled temperature (e.g., 25°C or 37°C) with gentle agitation to reach equilibrium saturation [33] [34].
- Post-Loading Rinse: After incubation, remove the lenses from the solution and gently rinse them with a small volume of DI water to remove surface-adhered drug crystals.
- Storage: The drug-loaded lenses can be stored in a sealed vial with a small amount of saline or buffer to maintain hydration before use or release testing [33].
Protocol 2: Drug Loading via Molecular Imprinting
Molecular imprinting creates a macromolecular "memory" within the PHEMA matrix for sustained and targeted release. The following workflow details the fabrication process.
Procedure:
- Computational Screening (Optional but Recommended): Use computational modeling (e.g., molecular dynamics) to screen functional monomers (e.g., NVP, MAA) for their binding affinity with the template drug molecule (e.g., naringenin, valacyclovir) [35] [36].
- Polymerization Mixture Preparation: Prepare a mixture containing:
- Polymerization: Cast the mixture into contact lens molds and initiate free radical polymerization under controlled temperature or UV irradiation [35].
- Template Extraction: After polymerization, immerse the formed hydrogels in a suitable solvent (e.g., ethanol:water mixture) to leach out the template drug molecules. This process leaves behind specific molecular cavities complementary in size, shape, and functional groups to the drug [35] [36].
- Validation: The success of imprinting is validated by comparing the drug loading and sustained release profiles of imprinted lenses against non-imprinted control lenses.
Protocol 3: Drug Loading via Physical Encapsulation
Physical encapsulation relies on creating diffusion barriers within the hydrogel to control drug release.
Table 3: Key Reagents for Physical Encapsulation
| Reagent Name | Function/Application |
|---|---|
| Poly(lactic-co-glycolic) acid (PLGA) | A biodegradable polymer used to form a drug-loaded film that acts as a sustained-release barrier [31]. |
| Vitamin E (Tocopherol) | A hydrophobic additive that creates nanoscale barriers within the hydrogel to slow drug diffusion [31] [34]. |
| Ethylcellulose | A polymer used to form drug-loaded nanoparticles that are subsequently incorporated into the hydrogel matrix [34]. |
| Gold Nanoparticles (GNPs) | Nanocarriers that can be loaded with drugs (e.g., timolol) to enhance accumulation in target tissues [34]. |
| Dexamethasone | A corticosteroid drug model used in encapsulation studies for sustained anti-inflammatory delivery [31]. |
Procedure:
- Barrier Creation: This can be achieved through several strategies:
- Vitamin E Aggregation: Soak pre-formed lenses in a vitamin E-ethanol solution, allowing vitamin E aggregates to form within the polymer matrix and create a hydrophobic diffusion barrier [34].
- Drug-Polymer Film Encapsulation: Mix the drug (e.g., dexamethasone) with a barrier polymer like PLGA. This mixture is then encapsulated as a discrete film within the peripheral region of a methafilcon hydrogel lens during manufacturing, leaving the optical zone clear [31].
- Nanoparticle Incorporation: Pre-load the drug into nanoparticles (e.g., gold nanoparticles, ethylcellulose nanoparticles). These nanoparticles are then dispersed within the HEMA monomer mixture before polymerization [34].
- Lens Fabrication: If the encapsulation occurs during manufacturing (as with film or nanoparticle methods), proceed with standard lens polymerization and curing processes.
- Release Testing: The sustained release capability is evaluated by monitoring drug elution into a medium like SLF over days or weeks, demonstrating significantly extended duration compared to unencapsulated systems [31] [34].
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for PHEMA Hydrogel Drug Delivery
| Reagent Solution | Function in Research |
|---|---|
| Simulated Lacrimal Fluid (SLF) | Serves as a physiologically relevant medium for conducting in vitro drug release studies to predict in vivo performance [36]. |
| Methacrylic Acid (MAA) Monomer | An ionic functional monomer used in molecular imprinting to create electrostatic interactions with basic drug molecules (e.g., valacyclovir) [36]. |
| N-Vinyl Pyrrolidone (NVP) Monomer | A non-ionic functional monomer used in molecular imprinting to form hydrogen bonds with drug molecules, enhancing loading and sustaining release [35]. |
| Ethylene Glycol Dimethacrylate (EGDMA) | A cross-linking agent crucial for imparting mechanical stability to the hydrogel and fixing the molecularly imprinted cavities within the polymer network [35] [36]. |
| Vitamin E (α-Tocopherol) Ethanol Solution | Used to create a hydrophobic diffusion barrier within the hydrogel, dramatically extending the release duration of both hydrophilic and hydrophobic drugs [34]. |
Poly(2-hydroxyethyl methacrylate), or pHEMA, is a cornerstone synthetic polymer in the development of biomedical hydrogels, most notably in commercial soft contact lenses, owing to its excellent biocompatibility, optical transparency, and high water absorption capacity [9]. However, for advanced applications such as ocular drug delivery, its inherent limitations—including low drug loading capacity, uncontrolled release profiles, and non-degradability—pose significant challenges [38] [9]. The integration of natural biomaterials presents a powerful strategy to overcome these constraints and enhance the functionality of pHEMA-based systems.
Natural biopolymers such as chitosan, gelatin, and hyaluronic acid offer distinct advantages, including inherent biodegradability, high biocompatibility, and the presence of functional groups that facilitate chemical modification and controlled drug release [38] [39]. Integrating these biopolymers with pHEMA creates composite hydrogels that synergize the robust mechanical properties of the synthetic polymer with the enhanced biofunctionality of natural materials [38] [30]. This document provides detailed application notes and experimental protocols for the development and characterization of these advanced composite materials, framed within the context of ophthalmic drug delivery systems.
Natural Biomaterials for pHEMA Enhancement: Properties and Rationale
The selection of an appropriate natural biomaterial is critical for tailoring the properties of the final pHEMA composite. Below is a summary of the key natural polymers used for enhancing pHEMA.
Table 1: Key Characteristics of Natural Biomaterials for pHEMA Composites
| Natural Biomaterial | Source | Key Functional Groups | Primary Role in pHEMA Composite | Key Advantages |
|---|---|---|---|---|
| Chitosan [38] [39] | Chitin (shellfish) | Amino (-NH₂), Hydroxyl (-OH) | Drug release modulation, Antimicrobial activity | Mucoadhesiveness, biodegradability, intrinsic antibacterial properties. |
| Gelatin [38] [39] | Collagen (animal) | Amino (-NH₂), Carboxyl (-COOH) | Cell adhesion, Mechanical reinforcement | Excellent cell adhesion properties (RGD sequences), thermoresponsive gelation. |
| Hyaluronic Acid (HA) [38] [40] | Bacterial fermentation / Animal tissues | Carboxyl (-COOH), Hydroxyl (-OH) | Hydration, Bioactivity, Drug delivery | High water retention, CD44 receptor targeting, ECM mimicry, biodegradability. |
Synthesis and Fabrication Protocols
Composite hydrogels can be fabricated through several methods, with the choice of method significantly impacting the final material's architecture and properties. The following workflows and protocols outline common approaches.
Composite Fabrication Workflows
Detailed Experimental Protocols
Protocol 1: Synthesis of pHEMA-Gelatin Methacrylate (GelMA) Interpenetrating Network (IPN)
This protocol is adapted from a study fabricating a pHEMA conduit containing a GelMA-HA IPN for nerve regeneration, demonstrating its applicability for creating complex composite structures [41].
- Objective: To create a robust, degradable IPN hydrogel combining pHEMA's mechanical strength with GelMA's bioactivity.
Materials:
- Monomers: 2-hydroxyethyl methacrylate (HEMA)
- Cross-linkers: Ethylene glycol dimethacrylate (EGDMA) for pHEMA; Methacrylic anhydride for GelMA modification
- Initiator: Irgacure 2959 (for UV initiation) or Ammonium persulfate (APS) / Tetramethylethylenediamine (TEMED) (for thermal initiation)
- Natural Polymer: Gelatin (Type A from porcine skin)
- Solvent: Phosphate Buffered Saline (PBS) or deionized water
Procedure:
- Synthesis of GelMA:
- Dissolve gelatin (10% w/v) in PBS at 50°C under constant stirring.
- Slowly add methacrylic anhydride (0.1-0.2 mL per gram of gelatin) to the solution and react for 2-3 hours at 50°C.
- Terminate the reaction by diluting with warm PBS and dialyze against distilled water for 5-7 days to remove impurities and unreacted reagents.
- Lyophilize the purified product to obtain porous GelMA foam. Confirm the degree of methacrylation (can be >90% [41]) via ¹H-NMR.
- Preparation of Pre-polymer Solution:
- Prepare the pHEMA pre-polymer solution by mixing HEMA monomer (56% v/v final concentration [41]), EGDMA cross-linker (0.1-1% v/v), and photo-initiator Irgacure 2959 (0.5% w/v) in a solvent.
- Separately, dissolve the synthesized GelMA (e.g., 5-10% w/v) in PBS containing a photo-initiator at 40°C.
- Fabrication of IPN:
- Mix the pHEMA and GelMA pre-polymer solutions thoroughly.
- Pour the mixture into a polydimethylsiloxane (PDMS) mold designed with the desired contact lens geometry.
- Expose the mold to UV light (e.g., 365 nm, 5-10 mW/cm²) for 30-60 minutes to concurrently polymerize both networks, forming the IPN.
- Post-processing:
- Carefully demold the hydrogel and wash extensively in distilled water or ethanol to remove any unreacted monomers.
- Store the final pHEMA-GelMA IPN in sterile PBS until further use.
- Synthesis of GelMA:
Protocol 2: Coating pHEMA Lenses with Chitosan
This method offers a simpler approach to functionalizing pre-formed pHEMA lenses, significantly altering surface properties without modifying the bulk [38].
- Objective: To impart mucoadhesive and antimicrobial properties to a commercial pHEMA contact lens via a chitosan coating.
Materials:
- Pre-polymerized pHEMA lenses (commercial or lab-made)
- Chitosan (medium molecular weight, >75% deacetylated)
- Acetic acid solution (1% v/v)
- NaOH solution (0.1 M)
- Orbital shaker
Procedure:
- Chitosan Solution Preparation: Dissolve chitosan (1-2% w/v) in an aqueous acetic acid solution (1% v/v). Stir overnight until a clear, homogeneous solution is obtained.
- Lens Pre-treatment: Equilibrate clean pHEMA lenses in distilled water or a mild buffer to hydrate them fully.
- Coating Process: Immerse the hydrated pHEMA lenses in the chitosan solution. Place the container on an orbital shaker set to a low speed (e.g., 50 rpm) for a predetermined time (e.g., 24 hours) to allow for polymer adsorption.
- Cross-linking and Washing: After coating, rinse the lenses gently with distilled water to remove loosely adsorbed chitosan. To stabilize the coating, immerse the lenses in a 0.1 M NaOH solution for 30 minutes to induce physical cross-linking.
- Final Rinsing and Storage: Rinse the coated lenses thoroughly with distilled water until the eluent reaches a neutral pH. Store the lenses in sterile saline solution.
Characterization and Performance Data
Rigorous characterization is essential to validate the success of composite fabrication and assess performance for drug delivery applications.
Material Characterization Workflow
Quantitative Characterization Data
The integration of natural polymers measurably alters the physicochemical properties of pHEMA, as summarized below.
Table 2: Performance Characteristics of pHEMA-Natural Biomaterial Composites
| Composite Type | Drug Loading Method / Agent | Key Findings | Reference |
|---|---|---|---|
| pHEMA-Chitosan Coating | Soaking / Various ophthalmic drugs | Extended drug release duration; Significant increase in bioavailability from ~5% (eye drops) to ~50%. | [38] |
| pHEMA-GelMA-HA IPN | N/A (Structural study) | Tunable degradation profile: Pure HA degraded in ~3 weeks, pure GelMA in >5 weeks. IPN properties can be adjusted by component ratios. | [41] |
| General Natural Polymer-based Lenses | Molecular Imprinting, Soaking, Vitamin E nano-barriers | Achieved sustained drug release over days to weeks, overcoming the initial burst release of pure pHEMA. | [38] [30] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Developing pHEMA-Natural Biomaterial Composites
| Reagent / Material | Function | Example & Notes |
|---|---|---|
| HEMA Monomer | Primary building block for the synthetic hydrogel network. | 2-Hydroxyethyl methacrylate. Purify to remove inhibitors before polymerization. |
| Methacrylic Anhydride | Introduces polymerizable methacrylate groups onto natural polymers (e.g., for GelMA, HA-MA). | Enables covalent cross-linking of natural polymers within the pHEMA network. |
| EDC (1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide) | Carbodiimide cross-linker for forming amide bonds between carboxyl and amine groups. | Commonly used for conjugating HA (COOH) to chitosan (NH₂) or for grafting. [40] |
| Irgacure 2959 | UV photo-initiator for free radical polymerization. | Ideal for biocompatible applications; requires UV light at ~365 nm for activation. |
| APS/TEMED | Thermal redox initiator system for free radical polymerization. | Ammonium Persulfate (APS) and Tetramethylethylenediamine (TEMED); used for polymerization at room or physiological temperature. |
| Ethylene Glycol Dimethacrylate (EGDMA) | Cross-linking agent for pHEMA, controls mesh size and mechanical strength. | Use at low concentrations (typically 0.1-1% v/v relative to monomer). |
Application Notes for Ophthalmic Drug Delivery
The primary application driving the development of these advanced composites is their use as drug-eluting contact lenses.
Controlled Release Mechanisms: The release kinetics from these composites can be engineered through several mechanisms:
- Diffusion Control: Governed by the mesh size of the hydrogel network, which is tuned by cross-linking density and the presence of the natural polymer.
- Degradation-Mediated Release: For composites containing degradable polymers like GelMA or HA, drug release is coupled to the hydrolysis or enzymatic degradation of the polymer chains, enabling programmable, long-term release [30] [41].
- Ionic/Specific Interactions: Charged drugs can interact ionically with chitosan (cationic) or hyaluronic acid (anionic), providing an additional mechanism to sustain release [38].
Overcoming Commercial Limitations: These composites directly address the critical limitations of commercial contact lenses for drug delivery, which include low drug loading capacity and uncontrolled release kinetics (typically a large initial burst followed by rapid depletion) [38]. The natural biomaterials significantly enhance loading capacity and provide sustained, controlled release, improving therapeutic efficacy and patient compliance.
Future Perspectives and Challenges: While research is promising, the translation of these composite lenses to commercial products faces challenges. These include scaling up manufacturing with high reproducibility, ensuring long-term stability of the drug and material, and navigating the complex regulatory pathway for drug-device combination products [38] [30]. Future research is likely to focus on "smart" stimuli-responsive systems and further personalization of therapy.
PHEMA as a Platform for Sustained and Controlled Ophthalmic Drug Delivery
Poly(2-hydroxyethyl methacrylate), or pHEMA, hydrogels have emerged as a leading biomaterial platform for sustained and controlled ophthalmic drug delivery. This application note details the fundamental properties of pHEMA that make it suitable for contact lens-based drug delivery, provides quantitative data on drug release kinetics for various therapeutic agents, and outlines standardized experimental protocols for researchers developing ophthalmic drug delivery systems. By integrating drug delivery functionality directly into contact lens materials, pHEMA-based systems address critical limitations of conventional eye drops, including poor bioavailability and rapid precorneal clearance, thereby enabling more efficient and patient-friendly ocular therapies.
Poly(2-hydroxyethyl methacrylate) is a synthetic hydrogel that has revolutionized ophthalmic applications since its development by Wichterle and Lim in 1960 [42]. Its unique properties—including excellent biocompatibility, transparency, mechanical stability, and ability to absorb and retain significant amounts of water—make it particularly suitable for contact lens applications and drug delivery systems [43]. The three-dimensional cross-linked network structure of pHEMA allows for the encapsulation of therapeutic agents and their subsequent controlled release onto the ocular surface, addressing fundamental challenges in ocular pharmacology [42].
Conventional ophthalmic formulations like eye drops suffer from extremely low bioavailability (typically less than 5%) due to rapid precorneal loss through tear drainage and nasolacrimal removal [44]. By serving as a drug-reservoir in direct contact with the eye, pHEMA-based contact lenses can significantly extend drug residence time and improve corneal penetration, thereby enhancing therapeutic efficacy while reducing systemic side effects [45]. This application note provides a comprehensive framework for utilizing pHEMA as a platform for sustained and controlled ophthalmic drug delivery, with specific protocols and data to support research and development activities.
Key Properties and Advantages of pHEMA
Fundamental Material Characteristics
pHEMA possesses several intrinsic properties that make it ideal for ophthalmic drug delivery applications:
Biocompatibility and Safety: pHEMA elicits minimal immunological response and demonstrates excellent tissue compatibility, as evidenced by its long history of safe use in contact lenses [43]. In vivo safety evaluations in rabbit models showed no ocular irritation or pathological changes during 7-day wearing periods [45].
Optical Properties: pHEMA hydrogels maintain high optical transmittance (>90%), ensuring unimpaired vision when used as drug-eluting contact lenses [45] [27].
Hydration and Stability: pHEMA can absorb 38-42% water by weight while maintaining dimensional stability, creating an aqueous environment suitable for hydrating water-soluble ophthalmic drugs [43] [21].
Tunable Physicochemical Properties: The cross-linking density, polymer molecular weight, and composition can be modified to control mesh size, swelling behavior, and drug release kinetics [46] [42].
Functional Advantages for Drug Delivery
The functional benefits of pHEMA for ophthalmic drug delivery include:
Extended Release Profiles: pHEMA matrices enable sustained drug release over periods ranging from hours to days, compared to minutes with conventional eye drops [45] [44].
Enhanced Bioavailability: By maintaining therapeutic drug levels at the corneal surface, pHEMA systems significantly improve drug bioavailability [45].
Multi-Functional Capability: pHEMA can be engineered to provide additional functionalities such as UV-blocking [45] and antioxidant activity [45].
Stimuli-Responsive Formulations: Incorporation of pH-sensitive monomers like 2-(dimethylamino) ethyl methacrylate (DMAEMA) enables intelligent drug release triggered by specific ocular conditions [46].
Quantitative Drug Release Profiles from pHEMA Systems
The following tables summarize experimental data for various drug-loaded pHEMA systems, demonstrating the range of release profiles achievable through material engineering.
Table 1: Controlled Release Kinetics of Ophthalmic Drugs from pHEMA Hydrogels
| Therapeutic Agent | Drug Class | Release Duration | Cumulative Release | Key Release Parameters | Reference |
|---|---|---|---|---|---|
| Levofloxacin | Antibiotic | 120 hours | 84.2% | Zero-order kinetics | [45] |
| Pilocarpine Nitrate | Miotic | 24 hours | ~70% | Cross-linking dependent | [44] |
| Cytarabine (ara-C) | Anticancer | Initial linear phase | Fickian diffusion | Temperature dependent | [47] |
| Tetrahydrozoline | Vasoconstrictor | 12 hours | Variable | Molecular weight dependent | [46] |
Table 2: Influence of Drug Molecular Weight on Release from pHEMA Hydrogels
| Drug Molecule | Molecular Weight (g/mol) | Release Rate | Hydrogel Composition | Key Finding | Reference |
|---|---|---|---|---|---|
| Tetrahydrozoline | 236.74 | Highest | HEMA-EGDMA | Inverse correlation between drug molecular weight and release rate | [46] |
| Naphazoline | 246.73 | High | HEMA-EGDMA | Release kinetics influenced by hydrogen bonding | [46] |
| Dorzolamide | 324.44 | Moderate | HEMA-PEGDMA | Molecular weight affects diffusion through hydrogel mesh | [46] |
| Timolol Maleate | 432.51 | Slowest | HEMA-TEGDMA | Higher molecular weight drugs show sustained release profiles | [46] |
Table 3: Antibacterial and Antioxidant Performance of Functional pHEMA Lenses
| Functional Component | Bacterial Strain | Efficacy | Antioxidant Performance | Application | Reference |
|---|---|---|---|---|---|
| Levofloxacin-loaded hCe NPs | S. aureus ATCC29213 | 89.8% inhibition | 78.4% ROS scavenging in 60 min | Bacterial keratitis | [45] |
| Levofloxacin-loaded hCe NPs | E. coli ATCC25922 | 94.2% inhibition | Enhanced antioxidant protection | Ocular infection | [45] |
Experimental Protocols
Protocol 1: Fabrication of Drug-Loaded pHEMA Hydrogels for Ophthalmic Application
Principle: This protocol describes the preparation of pHEMA hydrogels loaded with ophthalmic drugs using thermally-initiated free radical polymerization, producing matrices suitable for sustained drug release [46] [44].
Materials:
- 2-hydroxyethyl methacrylate (HEMA)
- Ethylene glycol dimethacrylate (EGDMA) crosslinker
- Ammonium persulfate (APS) initiator
- N,N,N',N'-tetramethylethylenediamine (TEMED) catalyst
- Target drug (e.g., levofloxacin, pilocarpine, timolol)
- Ethylene glycol solvent
- Phosphate buffered saline (PBS, pH 7.4)
Procedure:
- Preparation of Precursor Solutions:
- Solution A: Dissolve APS initiator (0.5% w/w) in ethylene glycol with stirring for 10 minutes at room temperature.
- Solution B: Mix HEMA monomer (95% w/w), drug (2-5% w/w), EGDMA crosslinker (2% w/w), and TEMED catalyst (0.5% w/w) for 10 minutes at room temperature.
Imprinting and Polymerization:
- Allow Solution B to imprint for 24 hours at 5.0°C to facilitate molecular interactions between drug and monomer.
- Combine Solutions A and B, mix for 10 minutes at room temperature.
- Pour the mixture into polypropylene molds designed with contact lens curvature.
- Cover molds and polymerize at 5.0°C for 24 hours.
Post-Polymerization Processing:
- Carefully demold the polymerized hydrogels.
- Wash hydrogels in PBS solution for 24 hours to remove unreacted monomers and extractable drugs.
- Sterilize using low-temperature ethylene oxide gas or UV irradiation.
- Store in sterile PBS at 4°C until use.
Quality Control:
- Verify hydrogel dimensions and thickness using digital calipers.
- Confirm optical transmittance >90% using UV-Vis spectrophotometry.
- Assess surface morphology and integrity by scanning electron microscopy.
Protocol 2: In Vitro Drug Release Kinetics Assessment
Principle: This protocol standardizes the quantification of drug release profiles from pHEMA hydrogels under physiological conditions, enabling prediction of in vivo performance [46] [44].
Materials:
- Drug-loaded pHEMA hydrogels (5×5 mm discs, 1.5 mm thickness)
- Phosphate buffered saline (PBS, pH 7.4) with 0.01% sodium azide
- Water bath shaker maintained at 37°C
- UV-Vis spectrophotometer with appropriate cuvettes
- Calibration standards of pure drug in PBS
Procedure:
- Experimental Setup:
- Place individual drug-loaded hydrogel discs in containers with 10 mL PBS release medium.
- Maintain containers in water bath shaker at 37°C with constant agitation at 50 rpm.
- Protect from light to prevent drug photodegradation.
Sampling and Measurement:
- At predetermined time intervals (1, 2, 4, 6, 8, 12, 24, 48, 72, 120 hours), withdraw 2 mL of release medium for analysis.
- Replace with equal volume of fresh pre-warmed PBS to maintain sink conditions.
- Analyze drug concentration in withdrawn samples using UV-Vis spectrophotometry at predetermined λmax for each drug.
- Construct calibration curve using standard solutions (0.1-100 μg/mL) for quantification.
Data Analysis:
- Calculate cumulative drug release using standard formulas.
- Plot cumulative release versus time to determine release profile.
- Fit data to mathematical models (zero-order, first-order, Higuchi, Korsmeyer-Peppas) to determine release mechanisms.
- Determine diffusion coefficients from initial linear portion of release curves.
Troubleshooting:
- If release rates are too rapid: Increase cross-linking density or decrease drug loading.
- If release rates are too slow: Decrease cross-linking density or increase drug loading.
- If burst effect is observed: Implement pre-washing step or modify impregnation method.
Visualization of pHEMA Drug Delivery Mechanisms
Diagram 1: Drug release mechanisms from pHEMA hydrogels involve multiple concurrent processes including hydration, diffusion through the polymer mesh, swelling-induced release, and specific molecular interactions between drug and polymer chains. These mechanisms can be engineered to achieve desired release profiles for various ophthalmic applications.
Diagram 2: Standardized workflow for developing drug-loaded pHEMA hydrogels for ophthalmic applications, highlighting critical preparation, polymerization, and evaluation stages with quality control checkpoints to ensure reproducible performance.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for pHEMA Hydrogel Formulation
| Reagent/Category | Specific Examples | Function/Purpose | Application Notes |
|---|---|---|---|
| Primary Monomers | 2-hydroxyethyl methacrylate (HEMA) | Primary building block of hydrogel network | Distill under vacuum before use to remove inhibitors [44] |
| Crosslinkers | Ethylene glycol dimethacrylate (EGDMA), PEGDMA, TEGDMA | Creates 3D network structure; controls mesh size | Concentration determines release kinetics and mechanical properties [46] |
| Initiators | Ammonium persulfate (APS), 2,2-dimethoxy-2-phenyl acetophenone (DMPA) | Initiates free radical polymerization | Thermal (APS) or photoinitiation (DMPA) options available [27] [46] |
| Catalysts | N,N,N',N'-tetramethylethylenediamine (TEMED) | Accelerates polymerization reaction | Use controlled concentrations for reproducible kinetics [46] |
| Functional Monomers | 2-(dimethylamino) ethyl methacrylate (DMAEMA) | Provides pH-responsive behavior | Protonation at ocular pH triggers swelling and drug release [46] |
| Ophthalmic Drugs | Levofloxacin, pilocarpine, timolol, tetrahydrozoline | Therapeutic agents for ocular conditions | Molecular weight significantly influences release kinetics [45] [46] [44] |
| Nanoparticles | Hollow ceria nanoparticles (hCe NPs) | Provides antioxidant functionality; enhances drug loading | Enables dual-functionality (drug delivery + ROS scavenging) [45] |
Advanced Engineering Strategies
Surface Modification and Nanostructuring
Surface engineering of pHEMA hydrogels enables enhanced functionality and performance:
Nanopatterning: Replica molding techniques create nanostructured surfaces (nanopillars) that can suppress cytoskeleton protein upregulation, potentially preventing secondary cataracts in intraocular lenses [27].
Antimicrobial Strategies: Incorporation of silver nanoparticles, antibiotics, or antimicrobial agents protects against microbial infections at implantation sites [43].
Wettability Enhancement: Plasma treatments or built-in wetting agents improve surface hydrophilicity, crucial for comfort in contact lens applications [48].
Stimuli-Responsive Formulations
Smart pHEMA hydrogels can be engineered to respond to specific ocular conditions:
pH-Sensitive Systems: Incorporation of ionic monomers enables swelling and drug release triggered by pH changes in diseased states [46] [42].
Diffusion-Controlled Systems: Standard pHEMA formulations provide predominantly diffusion-controlled release following Fickian or non-Fickian kinetics [49] [46].
Molecular Imprinting: Creating specific binding pockets for target molecules through molecular imprinting enhances drug loading and controls release kinetics [46].
pHEMA hydrogels represent a versatile and effective platform for sustained and controlled ophthalmic drug delivery, addressing critical limitations of conventional eye drop therapies. Through strategic material design and engineering, researchers can precisely control drug release profiles, enhance therapeutic efficacy, and incorporate additional functionalities such as antioxidant protection and antimicrobial activity.
Future development directions include more sophisticated stimuli-responsive systems, advanced nanostructuring techniques for enhanced biointegration, and multi-drug delivery platforms for combination therapies. The continued innovation in pHEMA-based drug delivery systems holds significant promise for addressing challenging ocular diseases and improving patient compliance through reduced dosing frequency and enhanced therapeutic outcomes.
As research advances, pHEMA platforms are expected to evolve beyond simple sustained release to become truly intelligent drug delivery systems capable of responding to specific pathological conditions and providing personalized therapeutic profiles for optimal patient care.
Overcoming PHEMA's Limitations: Strategies for Enhanced Performance and Drug Delivery
Poly(2-hydroxyethyl methacrylate) (pHEMA) hydrogels, since their inception by Wichterle and Lim, have formed the cornerstone of soft contact lens technology due to their excellent biocompatibility, optical transparency, and favorable wettability [9]. However, a significant limitation of pure pHEMA hydrogels is their inherent low oxygen permeability (Dk), which is dependent on water content as oxygen primarily permeates through the aqueous phase of the hydrogel [50]. The cornea is an avascular tissue that relies on atmospheric oxygen for its metabolic needs. Extended lens wear with low Dk materials can induce corneal hypoxia, leading to complications such as corneal swelling, discomfort, and limbal injection [50]. This application note details two primary material science strategies—copolymerization and silicone hybridization—employed to enhance the oxygen permeability of pHEMA-based contact lenses, thereby supporting the development of advanced ocular devices.
Quantitative Analysis of Contact Lens Material Properties
The evolution of contact lens materials demonstrates a clear trajectory toward higher oxygen permeability, as summarized in Table 1.
Table 1: Properties of Different Contact Lens Material Classes
| Material Class | Representative Materials | Oxygen Permeability (Dk) | Key Characteristics | Primary Limitations |
|---|---|---|---|---|
| Hard (Non-Permeable) | Poly(methyl methacrylate) (PMMA) | None [50] | Rigid, excellent optics [50] | Very low oxygen transmission, discomfort [50] |
| Rigid Gas Permeable (RGP) | Siloxanyl-containing methacrylates, Fluoroalkyl methacrylates [50] | +++ [50] | High Dk, durable [50] | Rigidity, potential for discomfort, surface fouling [50] |
| Traditional Hydrogel | pHEMA, pHEMA-co-NVPy, pHEMA-co-MAA [50] [9] | + to ++ [50] | ~40% water content, soft, comfortable [50] | Low to moderate Dk, dependent on water content [50] |
| Silicone Hydrogel | TRIS, SiMA, H-PDMS copolymers with HEMA/NVPy [50] [51] | ++++ [50] (Up to 6x higher than traditional hydrogels [51]) | High Dk independent of water content, extended wear capability [50] [51] | Hydrophobicity, high modulus, lipid deposition [50] |
Silicone hydrogel materials, which celebrate over two decades of commercial success, now dominate the market due to their superior oxygen transmissibility [51]. Modern versions achieve Dk/t values exceeding 100, with some advanced materials reaching 200+ [51].
Strategic Approach 1: Copolymerization with Hydrophilic Monomers
Copolymerization involves the chemical incorporation of hydrophilic co-monomers into the pHEMA network to increase the hydrogel's water content, thereby enhancing oxygen transport through the aqueous phase.
Protocol: Copolymerization of pHEMA with N-Vinylpyrrolidone (NVPy) for Enhanced Hydration
Principle: NVPy is a highly hydrophilic monomer that, when copolymerized with HEMA, increases the overall water content of the resulting hydrogel, facilitating higher oxygen diffusion [50].
Materials:
- Monomer Mixture: 2-Hydroxyethyl methacrylate (HEMA), N-Vinylpyrrolidone (NVPy).
- Cross-linker: Ethylene glycol dimethacrylate (EGDMA).
- Initiator: Azobis(isobutyronitrile) (AIBN).
- Solvent: Deionized water or ethanol.
- Equipment: Three-neck reaction flask, magnetic stirrer, heating mantle, nitrogen gas inlet, and polypropylene mold plates.
Procedure:
- Monomer Feed Preparation: In a beaker, mix HEMA (80% w/w) and NVPy (20% w/w). Add EGDMA (0.5-1% w/w relative to total monomers) and AIBN (0.1% w/w) to the monomer mixture. Stir until homogenous.
- Degassing: Transfer the solution to the reaction flask. Sparge the mixture with nitrogen gas for 15-20 minutes to remove dissolved oxygen, which inhibits free-radical polymerization.
- Polymerization: Place the flask in a heating mantle at 70°C under a continuous nitrogen atmosphere with constant stirring. Allow the reaction to proceed for 12-24 hours.
- Casting & Curing: Pour the degassed, pre-polymerized mixture into polypropylene mold plates designed for contact lens curvature.
- Post-Processing: Carefully demold the cured hydrogel lenses. Hydrate them in deionized water for 24 hours, with periodic water changes, to remove any unreacted monomers and oligomers.
- Characterization: Determine the equilibrium water content (EWC) gravimetrically. Measure oxygen permeability (Dk) using a coulometric sensor method per relevant standards (e.g., ASTM F1927) [52].
Logical Workflow for Copolymerization Strategy
The following diagram outlines the logical decision-making and experimental workflow for developing a copolymerized hydrogel contact lens.
Strategic Approach 2: Silicone Hybrid Hydrogels
The silicone hybrid approach represents a paradigm shift by incorporating siloxane-containing monomers that possess high oxygen solubility, enabling oxygen transmission through both the aqueous and polymer phases [50].
Protocol: Fabrication of pHEMA-Silicone (TRIS) Hybrid Hydrogels
Principle: Methacrylate-functionalized siloxanes like Tris(trimethylsiloxy)silylpropyl methacrylate (TRIS) are copolymerized with HEMA. The siloxane (Si-O-Si) backbone provides a high-oxygen-solubility pathway, while hydrophilic components maintain bulk hydration and comfort [50].
Materials:
- Silicone Monomer: Tris(trimethylsiloxy)silylpropyl methacrylate (TRIS).
- Hydrophilic Monomers: HEMA, N-Vinylpyrrolidone (NVPy).
- Cross-linker: Ethylene glycol dimethacrylate (EGDMA).
- Initiator: Azobis(isobutyronitrile (AIBN).
- Compatibilizer/Solvent: Isopropanol or a similar solvent to ensure monomer homogeneity.
- Equipment: Ultrasonic bath, three-neck reaction flask, nitrogen inlet, heating mantle, and lens casting molds.
Procedure:
- Monomer Mixture Preparation: Combine TRIS (30% w/w), HEMA (65% w/w), and NVPy (5% w/w) in a flask. Add EGDMA (1% w/w) and AIBN (0.1% w/w). To overcome the poor compatibility of TRIS with hydrophilic monomers, add isopropanol (20% v/w of total monomers) and sonicate the mixture for 30 minutes to achieve a homogeneous solution [50].
- Degassing and Polymerization: Sparge the mixture with nitrogen gas for 20 minutes. Heat the reaction flask to 70°C under a nitrogen blanket for 18-24 hours to complete the bulk polymerization.
- Molding and Curing: Transfer the mixture to appropriate contact lens molds and cure in an oven.
- Extraction and Hydration: Demold the lenses and perform a solvent extraction step using isopropanol to remove unreacted monomers, followed by a gradual solvent exchange to deionized water to prevent excessive swelling and stress cracking.
- Surface Treatment (Critical Step): The polymerized lens will have a hydrophobic surface due to surface-oriented siloxane groups. To render it hydrophilic, perform a surface treatment via radio-frequency (RF) plasma oxidation or an extracted coating process. This step creates a permanent, hydrophilic surface that is compatible with the tear film [50].
- Characterization: Evaluate oxygen permeability (Dk). Assess surface wettability via contact angle goniometry. Measure the elastic modulus to ensure it remains within a comfortable range for the ocular surface.
Material Pathway in Silicone Hydrogel Formation
The diagram below illustrates the key components and their functional integration in a silicone hydrogel material.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Advanced Contact Lens Hydrogel Development
| Reagent / Material | Function in Research & Development | Typical Use Case |
|---|---|---|
| HEMA (2-Hydroxyethyl methacrylate) | Primary backbone monomer; forms the base hydrogel, providing biocompatibility and hydration [9]. | Fundamental component in both traditional and advanced copolymer hydrogels. |
| TRIS (3-[tris(trimethylsiloxy)silyl]propyl methacrylate) | Silicone-based monomer; imparts high oxygen permeability via its siloxane groups [50]. | Critical for formulating silicone hydrogel materials for extended wear. |
| N-Vinylpyrrolidone (NVPy) | Hydrophilic comonomer; increases the water content of the hydrogel to boost oxygen dissolution and diffusion [50]. | Used in copolymerization strategies to enhance Dk in water-pathway hydrogels. |
| Poly(ethylene glycol) methacrylate (PEGMA) | Hydrophilic/compatibilizing agent; improves hydrophilicity and can resist protein adsorption [50]. | Used as a comonomer to enhance surface wettability and comfort. |
| Ethylene Glycol Dimethacrylate (EGDMA) | Cross-linking agent; creates a three-dimensional polymer network, governing mechanical strength and swelling [9]. | Essential in nearly all hydrogel formulations to control matrix structure. |
| Azobis(isobutyronitrile) (AIBN) | Thermal free-radical initiator; decomposes upon heating to generate radicals that initiate the polymerization chain reaction [50]. | Standard initiator for thermal curing of methacrylate-based systems. |
The challenge of low oxygen permeability in pHEMA hydrogels has been successfully addressed through sophisticated material science strategies. The copolymerization approach enhances oxygen transmission by maximizing the aqueous pathway, while the silicone hybrid approach establishes a parallel, high-capacity solubility pathway through siloxane moieties. The latter has proven particularly transformative, enabling safe extended wear. Future developments will likely focus on next-generation biomimetic surfaces, smarter drug-eluting capabilities, and the refinement of biodegradable polymer systems for therapeutic applications [51] [30]. The protocols and analyses provided herein offer a foundational framework for ongoing research and development in the field of advanced ocular biomaterials.
Controlling Drug Release Kinetics to Prevent Burst Release and Prolong Efficacy
Poly(2-hydroxyethyl methacrylate) (pHEMA) hydrogels are a cornerstone material for therapeutic contact lenses due to their high biocompatibility, optical transparency, and favorable oxygen permeability. A significant challenge in utilizing these systems for ophthalmic drug delivery is overcoming rapid, uncontrolled burst release of therapeutics, which leads to suboptimal bioavailability and potential side effects. Consequently, designing pHEMA-based platforms that provide sustained, controlled drug release is a critical focus of ophthalmic research. This Application Note details established and emerging strategies to finely tune drug release kinetics from pHEMA hydrogel contact lenses, providing structured experimental protocols and data to guide researchers in prolonging therapeutic efficacy.
Key Strategies for Controlling Release Kinetics
Several effective methodologies have been developed to mitigate burst release and extend drug release duration from pHEMA hydrogels. The following sections and Table 1 summarize the primary approaches.
Table 1: Strategies for Controlling Drug Release from pHEMA Hydrogel Contact Lenses
| Strategy | Mechanism of Action | Impact on Release Duration | Key Considerations |
|---|---|---|---|
| Vitamin E (α-Tocopherol) Loading | Creates hydrophobic diffusion barriers within the hydrogel mesh, hindering drug diffusion [53] [34]. | Extends release of timolol from hours to 7-9 days [34]. | Does not significantly alter water content or lens size [53]; requires ethanol for loading [53]. |
| Molecular Imprinting | Creates specific, complementary binding sites for the drug molecule within the polymer network, enhancing affinity and retarding diffusion [34]. | Provides sustained release for 8-10 hours; increased drug absorption (e.g., 12 mg/g dry hydrogel) [34]. | Functional monomer ratio and crosslinking density are critical for optimal performance [34]. |
| Sandwich Hydrogel Lenses with Microchambers | Encapsulates drug within a polymer film (e.g., Polylactic Acid) sandwiched between pHEMA layers, creating a reservoir for zero-order release kinetics [54]. | Provides sustained and controlled release over several days [54]. | Maintains a clear central visual aperture; complex fabrication process [54]. |
| Nanoparticle Incorporation | Drug-loaded nanoparticles (e.g., ethyl cellulose) dispersed within the hydrogel act as secondary reservoirs, slowing drug release [34]. | Can deliver medication for up to a week [34]. | Nanoparticle composition and distribution are key to controlling release profile. |
The logical relationship between the choice of strategy and the resulting drug release profile is summarized in the diagram below.
Experimental Protocols
Protocol: Drug Loading via Vitamin E Diffusion Barrier
This protocol outlines the process for creating a hydrophobic vitamin E barrier within pHEMA hydrogels to prolong the release of hydrophilic drugs like timolol [53] [34].
Research Reagent Solutions & Essential Materials:
Table 2: Key Reagents for Vitamin E Loading Protocol
| Item | Function/Description | Exemplary Source |
|---|---|---|
| pHEMA Hydrogel Lenses | Base material for the drug delivery system. | Commercially available or synthesized in-house [53]. |
| Vitamin E (α-Tocopherol) | Forms hydrophobic aggregates that act as a diffusion barrier. | Sigma-Aldrich [53]. |
| Anhydrous Ethanol | Solvent for dissolving vitamin E and facilitating its infusion into the hydrogel. | Sigma-Aldrich [53]. |
| Drug of Interest (e.g., Timolol Maleate) | The therapeutic agent to be delivered. | Sigma-Aldrich or pharmaceutical supplier [53]. |
| Phosphate Buffered Saline (PBS) | Release medium for in vitro testing, simulating physiological pH (7.4). | Sigma-Aldrich [53]. |
Procedure:
- Vitamin E/EtOH Solution Preparation: Prepare a solution of vitamin E in anhydrous ethanol. Concentrations ranging from 0 to 0.28 M can be tested to optimize the release profile [53].
- Hydrogel Loading: Immerse dry pHEMA hydrogel lenses in 1.5 mL of the vitamin E-ethanol solution. Allow the infusion to proceed for 24 hours at room temperature [53].
- Washing and Drying: After loading, remove the lenses and rinse them gently with ethanol and then deionized water to remove excess vitamin E from the surface. Dry the lenses at room temperature overnight [53].
- Drug Loading (Simultaneous Method): Add the target drug (e.g., 0.5 mg timolol) directly to the vitamin E-ethanol solution in step 1 to load the drug and vitamin simultaneously [53].
- Drug Loading (Sequential Method): Alternatively, soak the vitamin E-loaded lens from step 3 in a 1.5 mL aqueous PBS solution containing the drug (0.5 mg timolol) for 24 hours [53].
- Final Preparation: After drug loading, wash the lenses and dry them overnight to remove residual ethanol prior to release tests [53].
Protocol: Fabrication of Sandwich Hydrogel Lenses with Microchambers
This protocol describes creating a structured contact lens where a drug-loaded polylactic acid (PLA) microchamber film is encapsulated between two layers of pHEMA hydrogel [54].
Research Reagent Solutions & Essential Materials:
- pHEMA Monomer Solution: HEMA monomer, ethylene glycol dimethacrylate (EGDMA) crosslinker, and a photoinitiator (e.g., Irgacure 2959) [54].
- Polylactic Acid (PLA): Biodegradable polymer for fabricating the microchamber film [54].
- Drug: e.g., Dexamethasone powder, milled to a fine particle size [54].
- PDMS Kit: (e.g., Sylgard 184) for creating soft lithography stamps [54].
- Chloroform: Solvent for PLA [54].
Procedure:
- Microchamber Fabrication:
- Create a patterned PDMS stamp via soft lithography.
- Dip the stamp into a 2% (w/v) PLA solution in chloroform and allow the solvent to evaporate, forming a thin polymer layer.
- Distribute milled drug powder evenly over the patterned PLA-coated stamp.
- Seal the microchambers by pressing a flat PDMS stamp coated with a thicker, sticky PLA layer onto the patterned stamp.
- Detach the stamps to obtain a free-standing microchamber film. Use a biopsy punch to create a doughnut shape, clearing a central 5 mm diameter aperture to preserve the visual axis [54].
- Sandwich Lens Fabrication:
- Pour 350 μL of pHEMA monomer solution into a custom female contact lens mold.
- Polymerize the first pHEMA layer under a 305 nm UV lamp for 50 minutes.
- Lightly press the doughnut-shaped microchamber film onto the polymerized pHEMA layer.
- Add another 350 μL of monomer solution over the film and perform a second UV polymerization for 50 minutes [54].
- Post-processing: Carefully demold the composite sandwich lens and wash thoroughly in deionized water to remove any unreacted monomers [54].
The workflow for this multi-step fabrication process is illustrated below.
Data Analysis and Release Kinetics
In VitroDrug Release Testing
A standardized release test is crucial for comparing the performance of different formulations.
Procedure:
- Place each drug-loaded lens into a vial containing 3 mL of fresh PBS buffer (pH 7.4) maintained at 37°C to simulate physiological conditions [53].
- Agitate the vials at a constant rate using an orbital shaker.
- At predetermined time intervals (e.g., every 30 minutes initially, then less frequently), withdraw a small aliquot of the release medium and replace it with fresh PBS to maintain sink conditions.
- Analyze the drug concentration in the aliquots using an appropriate analytical technique (e.g., UV-Vis spectroscopy at λ = 294 nm for timolol) [53].
- Construct a cumulative drug release profile over time.
Modeling Release Kinetics
To characterize the release mechanism, experimental data should be fitted to mathematical models. The Higuchi model is often well-suited for drug release from matrix systems, indicating a diffusion-controlled process [55]. The model is expressed as: ( Qt = kH \cdot \sqrt{t} ) where ( Qt ) is the amount of drug released at time ( t ), and ( kH ) is the Higuchi release rate constant.
The strategic modification of pHEMA hydrogels is essential for developing effective ocular drug delivery systems that prevent burst release and provide prolonged therapy. Techniques such as incorporating vitamin E barriers, molecular imprinting, and designing advanced sandwich lenses with microchambers offer robust and tunable control over release kinetics. The protocols and data presented herein provide a foundation for researchers to design, fabricate, and characterize the next generation of therapeutic contact lenses, ultimately aiming to improve patient compliance and treatment outcomes for chronic ocular diseases.
Surface Modification and Coatings to Improve Wettability and Reduce Protein Adsorption
Within the context of developing advanced poly(2-hydroxyethyl methacrylate) (PHEMA) hydrogels for contact lens applications, controlling the interface between the material and the ocular environment is paramount. Surface modification and coatings are critical technologies for enhancing the clinical performance of contact lenses by improving their wettability and reducing protein adsorption [56] [57]. Unmodified soft contact lens surfaces, particularly those based on PHEMA and its copolymers, are prone to rapid coating by tear film components, including proteins, lipids, and mucins [58]. This deposition can lead to diminished visual acuity, dryness, discomfort, and inflammatory complications [58]. Furthermore, the intrinsic surface properties of some lens materials, especially silicone hydrogels which contain hydrophobic siloxane domains, can result in poor wettability, compromising patient comfort and lens efficacy [59] [60]. This application note details established and emerging surface modification protocols designed to address these challenges, thereby extending lens functionality and improving user experience.
Key Surface Modification Strategies
Several chemical strategies have been developed to engineer the surface properties of hydrogel contact lenses. The primary goals are to create a durable, hydrophilic surface that resists the non-specific adsorption of proteins and lipids. The table below summarizes the primary functions and outcomes of three prominent approaches.
Table 1: Key Surface Modification Strategies for Hydrogel Contact Lenses
| Strategy | Primary Function | Key Outcome | Representative Materials/Agents |
|---|---|---|---|
| Silanization [56] | Chemical grafting of organosilane compounds to the polymer surface. | Creates a surface that adsorbs less lysozyme; alters wettability. | Methyltrimethoxysilane, Ethyltrimethoxysilane, Phenyltrimethoxysilane |
| Plasma Surface Treatment [59] [61] | Application of a plasma-generated, thin, hydrophilic coating to the lens surface. | Forms a visually distinct, silicate-containing film with a mosaic pattern; significantly improves hydrophilicity. | Silicon Oxides (from organosilicon precursors) |
| Polyphenolic Co-Deposition [60] | Aqueous-based, mussel-inspired coating that adheres to various substrates. | Imparts extreme hydrophilicity and lipid repellency; process is industry-friendly and rapid (15 min). | Dopamine, Tannic Acid, Chitosan derivatives, Polyethyleneimine (PEI) |
Quantitative Comparison of Performance Data
Evaluating the efficacy of surface modifications requires quantitative measurement of protein adsorption and wettability. The following tables consolidate key performance metrics from the literature for unmodified and modified lens surfaces.
Table 2: Protein Adsorption on Modified and Unmodified Lens Materials
| Lens Material / Surface Treatment | Protein Studied | Amount Adsorbed | Key Findings on Protein State | Source |
|---|---|---|---|---|
| PHEMA/MAA (Untreated) | Lysozyme | High | Adsorbs thirty times more lysozyme than PHEMA lenses. | [57] |
| PHEMA/MAA (Silanized) | Lysozyme | Less than untreated | Adsorbs less lysozyme than the untreated lenses. | [56] |
| PHEMA (Lathe cut) | Lysozyme | ~2x PHEMA spin cast | Fabrication process influences adsorption behavior. | [57] |
| etafilcon A (Group IV) | Lysozyme | Highest among groups | Lysozyme accumulated rapidly, plateaued at day 7; deposited lysozyme exhibited the greatest activity. | [58] |
| lotrafilcon A & B (Plasma) | Lysozyme | Low | Similar deposition pattern to PMMA; lysozyme exhibited low activity. | [58] |
Table 3: Wettability and Lipid Repellency Performance
| Lens Material / Surface Treatment | Test Method | Performance Outcome | Source |
|---|---|---|---|
| Silicone Hydrogel (Polyphenolic Coating) | Static Contact Angle | Exhibited extreme hydrophilicity. | [60] |
| Silicone Hydrogel (Polyphenolic Coating) | Lipid Adhesion (Oleic Acid) | Demonstrated significant lipid repellency. | [60] |
| Silicone Hydrogel (Plasma Coating) | Hydration & Wettability | The process creates a stable, hydrophilic coating post-hydration and heat sterilization. | [59] |
Detailed Experimental Protocols
Protocol: Silanization of PHEMA-based Hydrogels
This protocol describes the surface reaction of PHEMA and PHEMA-methacrylic acid (MAA) copolymers with alkoxysilanes to create a surface that reduces lysozyme adsorption [56].
4.1.1 Research Reagent Solutions
Table 4: Essential Reagents for Silanization
| Reagent | Function |
|---|---|
| PHEMA or PHEMA/MAA contact lenses | Substrate for modification |
| Methyltrimethoxysilane, Ethyltrimethoxysilane, or Phenyltrimethoxysilane | Silanizing agent that reacts with surface groups |
| Anhydrous solvent (e.g., Toluene) | Reaction medium to prevent premature hydrolysis of alkoxysilane |
| Inert atmosphere (e.g., N₂ gas) | Prevents moisture contamination |
4.1.2 Procedure
- Preparation: Place the dry PHEMA or PHEMA/MAA contact lenses in a reaction vessel. Purging the vessel with an inert gas such as nitrogen is recommended to control moisture.
- Reaction Mixture: Prepare a 5-10% (v/v) solution of the chosen alkoxysilane (e.g., phenyltrimethoxysilane) in an anhydrous solvent.
- Silanization: Add the reaction mixture to the lenses, ensuring complete immersion. React for 2-6 hours at a controlled temperature (e.g., 60-80°C) with constant agitation.
- Washing: After the reaction, thoroughly wash the lenses with the same anhydrous solvent to remove any unreacted silane, followed by a series of rinses with ethanol and deionized water.
- Curing & Hydrolysis: Allow the silanized lenses to cure, during which any remaining methoxy groups will hydrolyze in ambient moisture, forming a cross-linked siloxane network on the surface.
- Characterization: Analyze the modified surface using Attenuated Total Reflectance-Fourier Transform Infrared (ATR-FTIR) spectroscopy to confirm the presence of siloxane bonds (peaks at ~1000-1100 cm⁻¹) [56].
Silanization Experimental Workflow
Protocol: Plasma Surface Treatment for Silicone Hydrogels
This protocol outlines a plasma treatment process to deposit a stable, hydrophilic silicate coating on silicone hydrogel lenses, enhancing their wettability [59] [61].
4.2.1 Research Reagent Solutions
Table 5: Essential Reagents for Plasma Treatment
| Reagent/Equipment | Function |
|---|---|
| Silicone Hydrogel Lenses | Substrate for coating |
| Organosilicon precursor (e.g., silane) | Plasma gas source for forming silicate film |
| Plasma reactor chamber | Controlled environment for plasma generation and deposition |
| Inert carrier gas (e.g., Argon) | Creates and sustains the plasma |
4.2.2 Procedure
- Lens Loading: Place the clean, dry silicone hydrogel lenses in a plasma reactor chamber.
- System Evacuation: Evacuate the chamber to a low base pressure (e.g., 10⁻² to 10⁻³ Torr) to remove atmospheric contaminants.
- Gas Introduction: Introduce a controlled flow of an organosilicon precursor vapor (e.g., a silane) and an inert carrier gas into the chamber.
- Plasma Ignition & Deposition: Apply radio-frequency (RF) power (e.g., 50-200 W) to generate a plasma. Maintain the process for a specific time (e.g., 1-10 minutes) to allow for the deposition of a thin, silicate-containing film on the lens surface. The resulting surface, when imaged by Atomic Force Microscopy (AFM), often shows a mosaic pattern of plate-like projections surrounded by cracks [59] [61].
- Post-Treatment Processing: Following plasma treatment, subject the lenses to standard hydration and heat sterilization processes. This step is critical for stabilizing the coating and making it visually distinct [59].
Protocol: Dopamine-Assisted Polyphenolic Co-Deposition
This protocol describes a rapid, industry-friendly dip-coating process to create a super-hydrophilic and lipid-repellent surface on hydrophobic silicone hydrogel lenses [60].
4.3.1 Research Reagent Solutions
Table 6: Essential Reagents for Polyphenolic Co-Deposition
| Reagent | Function |
|---|---|
| Dry Silicone Hydrogel Lens | Substrate for modification |
| Polyethyleneimine (PEI), branched | Promotes superficial reaction; primer layer |
| Dopamine hydrochloride | Molecular anchor; polymerizes to form polydopamine |
| Tannic Acid | Bulky, less-colored phenolic compound for co-deposition |
| TmCs-MOI (Chitosan derivative) | Hydrophilic macromolecule to enhance wettability |
| Sodium meta-periodate (NaIO₄) | Oxidant for rapid polymerization and cross-linking |
| Bicine buffer with NaCl | Reaction buffer system |
4.3.2 Procedure
- Preparation of Coating Solutions: Prepare separate stock solutions of PEI in deionized water, TmCs-MOI in bicine/NaCl buffer (pH 5.2), NaIO₄ in deionized water, and a phenolic solution of dopamine and tannic acid in the bicine/NaCl buffer. Sonicate all solutions for 5 minutes prior to use [60].
- PEI Pretreatment: Fill the lens container holding the dry lens with the PEI solution. Let it adsorb for a defined period (e.g., 9 minutes) to create a priming layer on the hydrophobic surface.
- Coating Solution Formation: In a separate reservoir, mix the TmCs-MOI solution with the oxidant (NaIO₄) solution and let it oxidize for 9 minutes. Then, add the phenolic (dopamine/tannic acid) solution to this mixture.
- Co-Deposition: Replace the PEI solution in the lens container with the final coating solution from Step 3. Allow the reaction to proceed for 5 minutes.
- Termination and Packaging: Remove the coating solution, rinse the lens thoroughly with saline, and package the lens in its primary packaging solution for final autoclaving [60].
The entire coating process is designed to be completed within 15 minutes.
Polyphenolic Co-deposition Workflow
Characterization Methods for Modified Surfaces
Rigorous characterization is essential to validate the efficacy and stability of surface modifications.
- Protein Adsorption Analysis: Use ATR-FTIR spectroscopy to directly quantify and study the conformation of proteins like lysozyme adsorbed on lens surfaces [56] [57]. For quantitative tracking, incubate lenses in a solution containing ¹²⁵I-labeled lysozyme and measure deposition over time using a Gamma Counter [58]. To assess the biological activity and conformational state of the deposited protein, use activity assays (e.g., lysoplate or enzymatic activity) on extracted proteins [58].
- Wettability Assessment: Measure the static contact angle using a small volume (e.g., 2 µL) of saline solution on the lens surface. A lower contact angle indicates higher hydrophilicity [60].
- Surface Topography and Chemistry: Employ Atomic Force Microscopy (AFM) to image the nanoscale surface morphology, such as the mosaic pattern characteristic of some plasma coatings [59] [61]. Perform X-ray Photoelectron Spectroscopy (XPS) to determine the elemental composition and chemical states of the top few nanometers of the coating [60].
- Lipid Repellency Testing: Qualitatively assess lipid adhesion by exposing coated lenses to dyed (e.g., Sudan Red) lipids like oleic acid or cottonseed oil, followed by rinsing and visual inspection under a microscope [60].
- Biocompatibility Testing: Conduct cytotoxicity testing per ISO 10993-5 standards (e.g., colony formation assay with V79 cells) to ensure the coating does not leach toxic compounds [60].
Surface modification is an indispensable tool for advancing the performance of PHEMA-based and silicone hydrogel contact lenses. Techniques such as silanization, plasma treatment, and innovative bio-inspired co-depositions provide robust and scalable solutions to the persistent challenges of protein fouling and poor wettability. The protocols outlined in this application note provide researchers with detailed methodologies to implement these strategies, while the accompanying characterization frameworks ensure that the performance of modified surfaces can be quantitatively validated. By integrating these surface engineering approaches, next-generation contact lenses can achieve enhanced comfort, improved clinical performance, and greater patient satisfaction.
Balancing Hydration, Modulus, and Comfort for Extended Wearability
Poly(2-hydroxyethyl methacrylate) (pHEMA) hydrogels have served as a foundational biomaterial for soft contact lenses since their inception, prized for their inherent biocompatibility and favorable optical properties [16]. A primary, ongoing challenge in the field is the optimization of the interrelated triumvirate of hydration, modulus, and comfort to achieve extended wearability. While pHEMA provides an excellent base, its traditional formulations present limitations, including relatively low oxygen permeability that is dependent on water content, and a propensity for protein and lipid deposition that can compromise comfort and safety over time [1]. This document provides detailed application notes and experimental protocols for researchers aiming to develop advanced pHEMA-based hydrogel materials that successfully balance these critical parameters for next-generation contact lens applications.
Quantitative Material Properties of Contact Lens Hydrogels
The performance of a contact lens material is governed by a set of key physicochemical properties. The table below summarizes critical parameters for traditional pHEMA, its common copolymers, and modern silicone hydrogels, which serve as benchmarks for next-generation pHEMA materials.
Table 1: Key Properties of Hydrogel and Silicone Hydrogel Contact Lens Materials
| Material (USAN) | Brand Name Examples | Water Content (%) | Oxygen Permeability (Dk) | Oxygen Transmissibility (Dk/t)† | Modulus (MPa) | Key Material Features |
|---|---|---|---|---|---|---|
| pHEMA (Traditional) | Various generic lenses | 38 - 40 [62] [63] | ~8 Barrer [63] | Low (modeled <24) [63] | 0.4 - 1.8 [16] | Baseline material; biocompatible [16] |
| pHEMA-co-NVP/MAA | Acuvue Moist (etafilcon A) | 58 - 75 [51] [63] | Up to ~35 Barrer [63] | Varies with thickness | Softer than pHEMA [1] | High-water hydrogels |
| Delefilcon A (SiHy) | Dailies Total1 [64] | 33 (core) to >80 (surface) [63] | Not specified | 156 [63] | Not specified | Water gradient technology |
| Lotrafilcon B (SiHy) | Air Optix for Astigmatism [64] | 33 [63] | 110 [63] | 138 [51] | Not specified | High Dk, deposit resistant [51] |
| Senofilcon A (SiHy) | Acuvue Oasys [64] | 38 [63] | 103 [63] | Not specified | 0.60 [63] | PVB internal wetting agent |
| Comfilcon A (SiHy) | Biofinity [64] | 48 [63] | 128 [63] | Not specified | 0.75 [63] | No surface coating |
†Dk/t values are often provided for a -3.00 D lens. Minimum recommended Dk/t for daily wear is 24 [63].
Key Property Interrelationships and Experimental Characterization
The Hydration-Oxygen-Modulus Paradigm
In traditional hydrogel materials like pHEMA, oxygen permeability (Dk) is directly linked to water content, as oxygen dissolves in and diffuses through the water phase of the polymer [63]. This creates a fundamental trade-off: increasing water content to improve Dk can compromise mechanical strength, making the lens fragile and difficult to handle [62]. Furthermore, the type of water within the hydrogel matrix is crucial. Water can be tightly bound to hydrophilic groups or exist as free molecules within polymer spaces; it is primarily the free water that facilitates oxygen transport [62]. A material with a high percentage of free water may dehydrate more quickly, leading to discomfort and optical instability [62].
The advent of silicone hydrogel (SiHy) materials broke this paradigm by using silicone, a highly oxygen-permeable phase, to transmit oxygen independently of the material's water content [63]. This allows SiHys to achieve very high Dk values even with moderate water content (e.g., lotrafilcon B with 33% water and a Dk of 110 Barrer) [63]. However, early SiHy materials introduced new challenges, as the silicone phase is inherently hydrophobic and can have a high modulus (stiffness), leading to mechanical complications like superior limbic keratoconjunctivitis [62]. Subsequent generations of SiHys have focused on lowering the modulus and incorporating internal wetting agents (e.g., polyvinylpyrrolidone, PVP) to improve surface wettability and comfort [62] [63]. For pHEMA-based materials to compete, innovative approaches that enhance oxygen transmissibility without relying solely on water content, while maintaining a low modulus, are required.
Advanced pHEMA Composite Formulations
Recent research has focused on modifying pHEMA to overcome its limitations. One promising strategy involves creating copolymers with rigid, hydrophilic polysaccharides. For instance, the synthesis of poly(2-hydroxyethyl methacrylate-co-methacrylated hyaluronan-β-cyclodextrin) [p(HEMA-co-mHA-β-CD)] has been reported to yield hydrogels with superior properties [1].
Table 2: Properties of Advanced pHEMA-co-mHA-β-CD Hydrogels vs. Traditional pHEMA
| Property | Traditional pHEMA | p(HEMA-co-mHA-β-CD) Hydrogel |
|---|---|---|
| Water Contact Angle | ~80° (Poor hydrophilicity) [1] | ~60° (High hydrophilicity) [1] |
| Equilibrium Water Content | ~30% (Low) [1] | Up to ~42% (Enhanced) [1] |
| Tensile Strength | 0.12 - 0.20 MPa [16] | ~0.29 MPa (Good mechanical strength) [1] |
| Tear Protein Deposition | Prone due to hydrophobic interactions [1] | Significant resistance to BSA and lysozyme [1] |
| Drug Delivery | Low drug loading, fast release [1] | Sustained release of puerarin over 120+ hours [1] |
This composite approach enhances hydrophilicity and mechanical strength simultaneously by incorporating the rigid helical structure of methacrylated hyaluronic acid (mHA). The β-cyclodextrin (β-CD) moieties provide cavities for drug encapsulation, enabling sustained drug delivery capabilities, which is a significant advancement over traditional pHEMA [1].
Experimental Protocols
Protocol: Synthesis of p(HEMA-co-mHA-β-CD) Hydrogel
This protocol outlines the synthesis of an advanced pHEMA-based copolymer hydrogel with enhanced wettability, mechanical strength, and drug-loading capacity [1].
Research Reagent Solutions & Essential Materials
| Reagent/Material | Function/Explanation |
|---|---|
| 2-Hydroxyethyl methacrylate (HEMA) | Primary monomer for forming the pHEMA network [1]. |
| Methacrylated Hyaluronic Acid-β-Cyclodextrin (mHA-β-CD) | Macromolecular crosslinker; enhances hydrophilicity, mechanical strength, and provides drug-binding sites [1]. |
| Ammonium Persulfate (APS) | Free radical initiator for the polymerization reaction [1]. |
| Phosphate Buffered Saline (PBS), pH 7.4 | Simulates the ionic strength and pH of the tear fluid for swelling and drug release studies [1]. |
| Bovine Serum Albumin (BSA) & Lysozyme | Model tear proteins for testing protein deposition resistance [1]. |
Procedure:
- Reaction Setup: In a glass vial, combine HEMA monomer and the synthesized mHA-β-CD macromer in a chosen mass ratio (e.g., 98:2 HEMA to mHA-β-CD). Add APS initiator at 1.0 wt% relative to the total monomers.
- Polymerization: Purge the reaction mixture with nitrogen gas for 5-10 minutes to remove oxygen, which can inhibit free radical polymerization. Seal the vial and place it in a water bath at 60°C for 24 hours to complete the polymerization and crosslinking reaction.
- Hydrogel Extraction: Carefully break the vial to remove the synthesized hydrogel rod.
- Equilibration and Purification: Immerse the hydrogel in a large excess of deionized water for 48 hours, changing the water every 12 hours. This step removes any unreacted monomers and initiator residues.
- Swelling Measurement: After purification, blot the hydrogel surface with a lint-free wipe to remove surface water and immediately weigh it to obtain the wet weight (Ww). Then, lyophilize the hydrogel and weigh it to obtain the dry weight (Wd). Calculate the Equilibrium Water Content (EWC) as: EWC (%) = [(Ww - Wd) / W_w] × 100.
Protocol: In-vitro Characterization of Hydrogel Properties
A. Protein Deposition Resistance Assay
- Sample Preparation: Prepare hydrogel discs of standard size (e.g., 10 mm diameter) and equilibrate them in PBS.
- Protein Incubation: Immerse each hydrogel disc in 2 mL of a protein solution (e.g., 4 mg/mL BSA and 2 mg/mL lysozyme in PBS) and incubate at 37°C for 12 hours under gentle agitation.
- Quantification: After incubation, remove the discs and gently rinse with PBS. Elute the deposited proteins from the disc surface using a 2% sodium dodecyl sulfate (SDS) solution. Quantify the protein concentration in the eluent using a standard protein assay, such as the Bicinchoninic Acid (BCA) assay [1].
B. Sustained Drug Release Profiling
- Drug Loading: Soak the purified and dried hydrogel discs in a concentrated drug solution (e.g., 1 mg/mL puerarin or levofloxacin in PBS) for 48 hours to allow for passive drug loading via absorption and inclusion complex formation with β-CD.
- Release Study: Transfer the drug-loaded discs into a vial containing a known volume of fresh PBS as the release medium (e.g., 10 mL). Place the vial in an incubator shaker at 37°C.
- Sampling and Analysis: At predetermined time intervals, withdraw a small aliquot of the release medium (e.g., 1 mL) and replace it with an equal volume of fresh PBS to maintain sink conditions. Analyze the drug concentration in the aliquot using UV-Vis spectrophotometry or HPLC. Plot the cumulative drug release (%) versus time to generate the release profile [1].
Visualization of Material Design and Evaluation Workflow
The following diagram illustrates the logical workflow for the design, synthesis, and evaluation of advanced pHEMA-based contact lens materials.
The Scientist's Toolkit: Key Reagents for pHEMA Hydrogel Research
Table 3: Essential Research Reagents for Advanced pHEMA Hydrogel Development
| Category / Reagent | Specific Examples | Function in Research & Development |
|---|---|---|
| Base Monomers | 2-Hydroxyethyl methacrylate (HEMA) | Primary building block for the hydrogel polymer network [1]. |
| Hydrophilic Comonomers | N-Vinyl-2-pyrrolidone (NVP), Methacrylic Acid (MAA) | Increase the water content and ionic character of the hydrogel [1] [65]. |
| Polymer Crosslinkers | Ethylene glycol dimethacrylate (EGDMA) | Creates crosslinks between polymer chains, determining mechanical strength and mesh size [1]. |
| Functional Biopolymers | Methacrylated Hyaluronic Acid (mHA), Chitosan | Enhance biocompatibility, wettability, and mechanical properties; can impart antimicrobial or wound-healing properties [1] [65]. |
| Drug Complexation Agents | β-Cyclodextrin (β-CD) | Provides hydrophobic cavities for forming inclusion complexes with drugs, enabling sustained release profiles [1]. |
| Polymerization Initiators | Ammonium Persulfate (APS) | Generates free radicals to initiate the chain-growth polymerization reaction [1]. |
| Model Tear Components | Bovine Serum Albumin (BSA), Lysozyme, Mucin | Used in in-vitro assays to test protein deposition and model the interaction of the lens with the tear film [1]. |
| Characterization Standards | Phosphate Buffered Saline (PBS), FDA-approved cytocompatibility kits | Provide standardized conditions for swelling, drug release, and cytotoxicity testing (e.g., ISO 10993-5) [1]. |
PHEMA in the Modern Landscape: Benchmarking Against Silicone Hydrogels and Natural Biomaterials
Within the context of a broader thesis on poly(2-hydroxyethyl methacrylate) (PHEMA) hydrogels for contact lens applications, this document provides a rigorous performance benchmarking of traditional PHEMA-based lenses against modern silicone hydrogel (SiHy) lenses. For researchers and drug development professionals, the transition from PHEMA to SiHy materials represents a significant paradigm shift in ocular biomaterial science, driven by the critical need to overcome the fundamental limitation of PHEMA: its low oxygen permeability [63] [62]. This application note synthesizes current data to deliver a direct, quantitative comparison of key material properties, provides detailed experimental protocols for their evaluation, and visualizes the core technological advancements.
The foundational principle of this comparison lies in the distinct mechanisms of oxygen transport. In conventional PHEMA hydrogels, oxygen permeability (Dk) is directly proportional to water content, as oxygen dissolves in and diffuses through the aqueous phase of the polymer, leading to a maximum Dk of approximately 35 Barrer [63]. SiHy materials, in contrast, incorporate siloxane phases that provide a high-capacity pathway for oxygen independent of water content, enabling Dk values that can exceed 100 Barrer [63] [66]. This report details the implications of this and other material differences on lens performance and ocular health.
Material Properties & Performance Benchmarking
The following tables summarize the core properties of PHEMA and SiHy lens materials, providing a quantitative basis for comparison.
Table 1: Fundamental Material Properties and Composition
| Property | PHEMA (Conventional Hydrogel) | Silicone Hydrogel (SiHy) |
|---|---|---|
| Primary Component(s) | Poly(2-hydroxyethyl methacrylate) [3] | Siloxane-based macromers (e.g., TRIS) co-polymerized with hydrophilic monomers [62] |
| Oxygen Permeability (Dk) Mechanism | Through water phase; increases with water content [63] | Through silicone phase; high Dk even at low water content [63] [66] |
| Typical Water Content | 38% - 80% [66] | Typically lower than hydrogels (~20% - 60%) [63] [66] |
| Inherent Surface Properties | Hydrophilic [3] | Inherently hydrophobic, requires surface modifications or internal wetting agents [62] |
| Representative USAN Names | Etafilcon A, Nelfilcon A [63] | Lotrafilcon A, Balafilcon A, Senofilcon A, Comfilcon A [63] |
Table 2: Key Performance and Clinical Characteristics
| Characteristic | PHEMA (Conventional Hydrogel) | Silicone Hydrogel (SiHy) | Impact & Clinical Significance |
|---|---|---|---|
| Oxygen Permeability (Dk) | Low (e.g., ~8-35 Barrer) [63] | High (e.g., >100 Barrer) [66] | SiHy lenses drastically reduce corneal hypoxia, associated complications (edema, neovascularization), and are suitable for extended wear [63] [66]. |
| Elastic Modulus (Stiffness) | Low and flexible [62] | Higher, especially in 1st generation [62] | A higher modulus can improve handling but may increase mechanical interaction with the palpebral conjunctiva, potentially contributing to papillary conjunctivitis (CLPC) [62]. |
| Deposit Type | Primarily protein [62] | Primarily lipids [62] | Silicone's lipophilicity attracts lipids; care systems must be compatible. Newer generations incorporate wetting agents to combat this [62]. |
| Wettability | Good, inherent hydrophilicity [3] | Requires surface treatment (e.g., plasma) or internal wetting agents (e.g., PVP) [62] | Wettability is critical for comfort and tear film stability; advanced SiHy designs have significantly improved surface wettability [63] [62]. |
| Optical Clarity | High [3] | High; phase separation is engineered to be smaller than the wavelength of light [62] | Both material families provide excellent vision correction when properly manufactured. |
Evolution of Silicone Hydrogel Materials
The development of SiHy lenses has progressed through distinct generations aimed at mitigating the limitations of early materials:
- First Generation (e.g., Lotrafilcon A, Balafilcon A): Featured very high Dk but a high modulus and required surface treatments to manage hydrophobicity [62].
- Second Generation (e.g., Galyfilcon A, Senofilcon A): Incorporated long-chain polymeric internal wetting agents like polyvinylpyrrolidone (PVP), which migrates to the surface to maintain wettability, and offered a lower modulus for improved comfort [62].
- Third Generation (e.g., Comfilcon A, Enfilcon A): Utilized siloxane macromers with inherently hydrophilic ends, creating a more homogeneous and wettable bulk material without the need for surface treatments [62].
The Scientist's Toolkit: Key Reagents & Materials
Table 3: Essential Research Reagents and Materials for Hydrogel Lens Evaluation
| Reagent / Material | Function / Application in Research |
|---|---|
| 2-Hydroxyethyl Methacrylate (HEMA) | The foundational monomer for synthesizing PHEMA-based hydrogels [18]. |
| Siloxane Macromers (e.g., TRIS) | Key monomers that provide the high oxygen permeability in SiHy formulations [62]. |
| Ethylene Glycol Dimethacrylate (EGDMA) | A common crosslinking agent used to create the polymer network in both PHEMA and SiHy hydrogels [26]. |
| Polyvinylpyrrolidone (PVP) | Used as an internal wetting agent in many SiHy materials to enhance surface hydrophilicity and comfort [62]. |
| Hyaluronic Acid (HA) / β-Cyclodextrin (β-CD) | Functional additives studied for creating advanced drug-delivering hydrogels with improved biocompatibility and sustained release profiles [26]. |
| Polyethylene Glycol Diacrylate (PEGDA) | A crosslinker often used in research for creating interpenetrating polymer networks (IPNs) or for advanced manufacturing like 3D printing [18]. |
| Franz Diffusion Cells | Standard apparatus for conducting in vitro drug release studies from hydrogel matrices [18]. |
| Tensile Tester | Instrument for measuring mechanical properties, including elastic modulus and tensile strength [26]. |
Detailed Experimental Protocols
Protocol: In Vitro Oxygen Permeability (Dk) Measurement
Objective: To accurately determine the oxygen permeability (Dk) of hydrogel contact lens materials.
Background: The Dk value is a critical parameter predicting the oxygen transmissibility (Dk/t) of a lens. The polarographic method is a standard technique.
Materials & Equipment:
- Oxygen Permeability System (e.g., according to ISO 9913-1 standard)
- Test lenses (hydrated in saline for at least 24 hours)
- Temperature-controlled chamber
- Saline solution (0.9% NaCl)
Procedure:
- Calibration: Calibrate the instrument according to the manufacturer's instructions using reference materials of known Dk values.
- Lens Preparation: Hydrate the test lenses in saline at the specified temperature (typically 35°C) for a minimum of 24 hours to achieve equilibrium.
- Mounting: Carefully mount the hydrated lens in the test chamber, ensuring it is properly positioned to create a seal without damaging the lens. The lens separates the chamber into an oxygen-rich (anterior) and an oxygen-depleted (posterior) side.
- Measurement:
- The electrode on the posterior side measures the flux of oxygen molecules diffusing through the lens material.
- Record the steady-state current generated by the oxygen flux. This current is proportional to the rate of oxygen transmission.
- Calculation: The Dk value is calculated by the system software based on the measured current, the partial pressure difference of oxygen across the lens, and the lens thickness (t). The oxygen transmissibility is given by Dk/t.
- Replication: Perform measurements on a minimum of n=5 lenses from at least two different manufacturing batches to ensure statistical significance.
Protocol: Drug Loading and Release Kinetics
Objective: To evaluate the potential of a hydrogel contact lens as a sustained drug delivery platform.
Background: Hydrogels can be loaded with therapeutic agents for targeted ocular delivery, significantly improving bioavailability compared to eye drops [26] [30].
Materials & Equipment:
- Test lenses (PHEMA and SiHy)
- Drug of interest (e.g., Dexamethasone, Timolol)
- Phosphate Buffered Saline (PBS), pH 7.4
- Franz Diffusion Cells
- UV-Vis Spectrophotometer or HPLC system
- Analytical balance
Procedure:
- Drug Loading:
- Soak Method: Immerse pre-hydrated lenses in a concentrated drug solution (e.g., 1-5 mg/mL) for a predetermined time (e.g., 24-72 hours) at room temperature with gentle agitation [26].
- Alternative Methods: For more controlled loading, molecular imprinting or the incorporation of drug-laden nanoparticles or cyclodextrin complexes can be employed [26] [30].
- Release Study Setup:
- Place the drug-loaded lens in the donor chamber of a Franz diffusion cell.
- Fill the receptor chamber with PBS (pH 7.4), maintained at 35°C with continuous stirring to simulate physiological conditions and ensure sink conditions.
- Sampling:
- At predetermined time intervals (e.g., 1, 2, 4, 8, 24 hours), withdraw a small aliquot (e.g., 200 µL) from the receptor chamber.
- Immediately replace the withdrawn volume with fresh, pre-warmed PBS to maintain a constant volume.
- Analysis:
- Analyze the drug concentration in each sample using a validated UV-Vis spectrophotometric method or HPLC.
- Plot the cumulative amount of drug released per unit area (µg/cm²) versus time to generate the release profile.
- Kinetic Modeling: Fit the release data to various mathematical models (e.g., Zero-order, Higuchi, Korsmeyer-Peppas) to determine the underlying drug release mechanism.
The workflow for the synthesis, functionalization, and characterization of advanced contact lens materials is summarized in the following diagram:
Advanced Applications & Future Directions
The benchmarking of PHEMA and SiHy materials provides a foundation for developing next-generation therapeutic and diagnostic lenses.
- Drug-Eluting Contact Lenses (DECLs): SiHy materials, and particularly PHEMA-based IPNs, are excellent candidates for sustained drug delivery. Strategies like cyclodextrin-drug inclusion complexes [26] or interpenetrating networks (IPNs) [18] allow for programmable release kinetics, overcoming the "burst release" of simple soak-loaded lenses.
- Microfluidic Contact Lenses: Emerging fabrication techniques, such as soft lithography and 3D printing, enable the integration of microfluidic channels into contact lenses [67]. These platforms hold immense promise for continuous, non-invasive monitoring of biomarkers (e.g., glucose, IOP) and highly controlled drug delivery [67].
- Biodegradable Lenses: A frontier in ocular drug delivery is the development of biodegradable polymers that offer controlled drug release and eliminate the need for lens removal, presenting a new paradigm for post-surgical or chronic disease treatment [30].
The fundamental relationship between material composition, oxygen permeability, and water content is the core differentiator between these lens types, as illustrated below:
Comparative Analysis of Drug Delivery Efficacy in PHEMA and Natural Biomaterial-Based Lenses
Within the broader research on poly(2-hydroxyethyl methacrylate) (pHEMA) hydrogels for contact lens applications, a critical advancement is their use as ocular drug delivery systems (DDS). Conventional eye drops are highly inefficient, with less than 5% of the administered dose reaching intraocular tissues due to protective ocular barriers and rapid clearance [30] [68]. Drug-eluting contact lenses (DECLs) present a promising alternative by providing sustained, localized delivery, which can significantly improve drug bioavailability and patient compliance [30] [69]. Among the various materials investigated for DECLs, synthetic pHEMA and natural biomaterials represent two major categories with distinct properties and performance characteristics. This application note provides a comparative analysis of their drug delivery efficacy, supported by experimental data and detailed protocols for researchers and drug development professionals.
Material Properties and Drug Delivery Mechanisms
The efficacy of a contact lens as a drug delivery vehicle is fundamentally governed by the physicochemical properties of its constituent material. pHEMA and natural biomaterials exhibit fundamentally different structures, which directly influence their interaction with water, drugs, and the ocular surface.
pHEMA Hydrogels: pHEMA is a synthetic polymer that forms a hydrogel capable of absorbing approximately 40% water in its equilibrium-swollen state [70]. Its network structure provides a balance of hydrophilicity and mechanical strength, making it a longstanding material for contact lenses [21] [70]. As a drug carrier, pHEMA typically functions as a reservoir matrix, where drug molecules are dispersed throughout the polymer network and released via diffusion through the water-swollen gel [53]. Release kinetics can be modified by incorporating functional comonomers or creating diffusion barriers with lipophilic molecules like Vitamin E [53].
Natural Biomaterials: This category includes polymers such as chitosan, alginate, hyaluronic acid, gelatin, collagen, and silk fibroin [71] [69]. These materials are characterized by their innate biocompatibility, biodegradability, low immunogenicity, and often, bioactivity [71]. Unlike simple diffusion-based systems, many natural polymer-based lenses can be engineered for controlled degradation, where drug release is coupled to the breakdown of the polymer matrix itself [30] [69]. This allows for more programmable release profiles and eliminates the need for lens removal after therapy [30].
Table 1: Key Characteristics of pHEMA and Natural Biomaterials for DECLs
| Characteristic | pHEMA Hydrogels | Natural Biomaterials |
|---|---|---|
| Origin | Synthetic | Natural (animal, plant, fungal, bacterial) |
| Primary Drug Release Mechanism | Diffusion-based | Diffusion combined with degradation-controlled release |
| Biodegradability | Typically non-degradable | Degradable with tunable kinetics |
| Key Advantages | Well-established synthesis, good mechanical properties, optical clarity | High biocompatibility, inherent bioactivity, sustainable sourcing |
| Key Challenges | Limited drug-loading capacity, uncontrolled release profiles, protein adsorption [71] | Batch-to-batch variability, scalability of production, long-term stability [71] |
Comparative Drug Delivery Performance
Quantitative data from recent studies highlight the differences in performance between pHEMA-based and natural biomaterial-based lenses. Key metrics include drug loading capacity, release duration, and therapeutic outcomes in model systems.
Table 2: Comparative Drug Delivery Performance of Different Lens Materials
| Lens Material / System | Loaded Agent(s) | Key Performance Findings | Reference |
|---|---|---|---|
| pHEMA (Vitamin E modified) | Timolol, Brimonidine | Drug loading increased by 19.1% and 18.7% respectively; no significant extension of release duration. | [53] |
| pHEMA (hCe nanoparticles) | Levofloxacin (LEV) | Controlled LEV release (84.2% within 120 h); enhanced antioxidant activity; treated bacterial keratitis in vivo in 7 days. | [45] |
| Chitosan-based Lenses | Various (model drugs) | High biocompatibility and mucoadhesiveness; potential for sustained and targeted release. | [71] [69] |
| Alginate-based Lenses | Various (model drugs) | Favorable wettability and patient comfort; drug release profiles can be tuned via cross-linking density. | [71] |
| Gelatin-based Lenses | Various (model drugs) | High drug-loading capacity; release kinetics linked to hydrogel swelling and biodegradation. | [71] [69] |
The data demonstrates that while pHEMA lenses can be effectively enhanced with additives to improve loading or impart multiple functionalities, natural biomaterials offer inherent advantages for creating more sophisticated, biodegradable drug delivery platforms.
Experimental Protocols
To ensure reproducibility in the development and testing of DECLs, the following standardized protocols are provided.
Protocol 1: Fabrication of pHEMA-based Drug-Eluting Lenses
This protocol outlines the synthesis of basic pHEMA hydrogel contact lenses and the subsequent loading of a therapeutic agent [53].
Research Reagent Solutions:
- Backbone Monomer: 2-hydroxyethyl methacrylate (HEMA)
- Crosslinker: Ethylene glycol dimethacrylate (EGDMA)
- Functional Co-monomers: Glycidyl methacrylate (GMA), N-vinyl-2-pyrrolidone (NVP)
- Initiator: Azobisisobutyronitrile (AIBN)
- Solvent: Ethanol or Phosphate Buffered Saline (PBS)
- Therapeutic Agent: Drug of choice (e.g., Timolol, Brimonidine, Levofloxacin)
Procedure:
- Monomer Solution Preparation: Prepare a mixture of 92% (w/w) HEMA and 8% (w/w) of a combination of crosslinker and functional co-monomers (e.g., EGDMA, GMA, NVP).
- Initiator Addition: Add AIBN initiator (typically 0.1-1% w/w of the total monomer weight) and mix thoroughly until fully dissolved.
- Molding and Curing: Pipette the monomer solution into custom contact lens molds.
- Thermal Polymerization: Place the molds in an oven and cure using a two-stage thermal cycle: 1 hour at 70°C followed by 1 hour at 110°C.
- Hydration and Leaching: After polymerization, carefully demold the lenses and immerse them in deionized water for one week to remove any unreacted monomers and residues. Change the water daily.
- Drug Loading via Soaking: Immerse the clean, hydrated lenses in a solution of the drug in PBS or ethanol (e.g., 0.5 mg/mL for Timolol) for 24 hours at room temperature.
- Finishing: Remove the lenses from the loading solution, rinse gently with deionized water to remove surface-adsorbed drug, and store in a sterile saline solution until use.
Protocol 2: In Vitro Drug Release Kinetics Testing
This protocol describes a standard method to characterize the drug release profile from DECLs [53].
Research Reagent Solutions:
- Release Medium: Phosphate Buffered Saline (PBS, pH 7.4)
- Analysis Instrument: UV-Vis Spectrophotometer or HPLC system
Procedure:
- Setup: Place each drug-loaded lens into a separate vial containing 3.0 mL of fresh, pre-warmed PBS (pH 7.4). Seal the vials to prevent evaporation.
- Incubation: Maintain the vials in a shaking incubator at 34±1°C (simulating ocular surface temperature) with constant, gentle agitation.
- Sampling: At predetermined time intervals (e.g., 30 min, 1, 2, 4, 8, 24, 48, 72 hours), completely withdraw the entire release medium and replace it with an equal volume of fresh, pre-warmed PBS.
- Analysis: Analyze the concentration of the drug in the collected samples using a validated analytical method (e.g., UV-Vis spectrophotometry at λ_max of the drug).
- Data Processing: Calculate the cumulative amount of drug released at each time point and plot the release profile. Model the data using appropriate kinetic models (e.g., Higuchi, Korsmeyer-Peppas) to understand the release mechanism.
Workflow Diagram
The following diagram illustrates the logical workflow for the development and evaluation of drug-eluting contact lenses, integrating both pHEMA and natural biomaterial pathways.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key materials and their functions for developing and testing DECLs based on pHEMA and natural biomaterials.
Table 3: Essential Research Reagents for DECL Development
| Reagent / Material | Function in DECL Research |
|---|---|
| 2-hydroxyethyl methacrylate (HEMA) | Primary monomer for synthesizing pHEMA hydrogel matrices [53]. |
| Chitosan | Natural biopolymer used to fabricate biodegradable lenses with inherent mucoadhesive properties [71] [69]. |
| Alginate | Natural biopolymer used for its biocompatibility and tunable gelling properties [71] [69]. |
| Ethylene glycol dimethacrylate (EGDMA) | Crosslinking agent that provides mechanical stability to pHEMA hydrogels [53]. |
| Vitamin E (α-Tocopherol) | Lipophilic additive used as a diffusion barrier in pHEMA lenses to enhance drug loading and prolong release [53]. |
| Hollow Ceria Nanoparticles (hCe NPs) | Functional nanomaterial embedded in hydrogels to provide antioxidant activity and modulate drug release [45]. |
| Azobisisobutyronitrile (AIBN) | Thermal initiator for radical polymerization of pHEMA hydrogels [53]. |
| Timolol Maleate | Model hydrophilic beta-blocker drug used for testing DECL performance in glaucoma research [53]. |
| Levofloxacin | Broad-spectrum antibiotic used for developing DECLs targeting bacterial keratitis [45]. |
Market Position and Current Commercial Applications of PHEMA-Based Lenses
Poly(2-hydroxyethyl methacrylate), or pHEMA, is a biocompatible, optically transparent, hydrophilic, and non-degradable polymer that forms a hydrogel upon water absorption [9] [72]. Invented by Otto Wichterle and Drahoslav Lim in 1960, it revolutionized vision correction by enabling the development of modern soft contact lenses [9] [73]. Its unique properties—including high oxygen permeability, flexibility in the hydrated state, and excellent biocompatibility—make it a foundational material in ophthalmic applications [9]. While pure pHEMA lacks inherent antimicrobial properties, its structure allows for extensive modification and functionalization, facilitating its use in advanced therapeutic and diagnostic applications [9] [72]. This document details the current commercial landscape and provides detailed experimental protocols for researching pHEMA-based lens technologies.
Market Position and Commercial Landscape
The pHEMA-based lens market is a robust and evolving sector within the broader ophthalmic industry. Its position is characterized by established use in vision correction and a rapid expansion into therapeutic and diagnostic applications.
Current Market Size and Segments
The smart contact lenses market, wherein pHEMA is a leading material, was valued at approximately USD 329.5 million in 2022 and is projected to grow at a compound annual growth rate (CAGR) of 15.2%, reaching around USD 1.39 billion by 2032 [74]. Within this market, pHEMA held a dominant share of over 33% in 2022 by material type, signifying its critical importance and widespread adoption [74].
Table 1: Smart Contact Lenses Market Overview by Key Segment (2022)
| Segment | Leading Category | Market Value / Share (2022) | Key Growth Driver |
|---|---|---|---|
| Material | Poly (2-Hydroxyethyl methacrylate) (pHEMA) | >33% market share [74] | High biocompatibility and optimal oxygen permeability [74] |
| Type | Daily-wear soft lenses | ~USD 155.8 million [74] | Superior comfort and convenience; reduced infection risk [74] |
| Application | Intraocular Pressure (IOP) Monitoring | ~USD 205.7 million [74] | Critical need for continuous glaucoma management [74] |
| Usability | Disposable Lenses | ~USD 228.5 million [74] | Hygiene, convenience, and avoidance of cleaning routines [74] |
| End-use | Hospitals | ~USD 189.0 million [74] | Adoption for post-surgical care and chronic disease monitoring [74] |
Key Commercial Applications
pHEMA-based lenses have transcended their initial role in passive vision correction. Current commercial applications focus on active therapeutic and diagnostic functions:
- Ocular Drug Delivery: A major research and commercial frontier involves using pHEMA hydrogels as sustained-release drug delivery systems [9] [53]. This application addresses the limitations of traditional eye drops, which suffer from low bioavailability (<5%) and rapid clearance [45]. Commercial and research efforts focus on lenses for delivering antibiotics, glaucoma medications (e.g., timolol, brimonidine), and other ophthalmic therapeutics [45] [53].
- Continuous Health Monitoring: Smart contact lenses made with pHEMA are being developed for non-invasive, continuous monitoring of physiological biomarkers. The most advanced application is intraocular pressure (IOP) monitoring for glaucoma management, a segment valued at over USD 205 million in 2022 [74]. Research is also underway for continuous glucose monitoring in tears for diabetic patients [74].
- Vision Correction and Cosmetic Applications: This remains the largest volume application. pHEMA-based daily-wear soft lenses dominate this segment due to their comfort and biocompatibility [74]. The market is characterized by innovation in copolymer formulations to enhance water content, oxygen permeability, and surface wettability [73] [75].
Detailed Experimental Protocols and Application Notes
This section provides detailed methodologies for key experiments and formulations in pHEMA-based lens research, supporting the development of next-generation applications.
Protocol: Fabrication of a Dual-Functional Drug-Eluting pHEMA Contact Lens
This protocol details the synthesis of antibiotic-loaded pHEMA contact lenses fortified with hollow ceria nanoparticles (hCe NPs) for combined ocular drug delivery and antioxidant protection, as demonstrated in recent research [45].
3.1.1 Research Reagent Solutions
Table 2: Essential Materials for Dual-Functional pHEMA Lens
| Reagent / Material | Function / Explanation |
|---|---|
| 2-hydroxyethyl methacrylate (HEMA) | Primary monomer for forming the pHEMA hydrogel network [45]. |
| Hollow Ceria Nanoparticles (hCe NPs) | Reactive Oxygen Species (ROS) scavengers; provide antioxidant protection and act as a nanocarrier for drugs [45]. |
| Levofloxacin (LEV) | A broad-spectrum antibiotic drug for treating bacterial keratitis [45]. |
| Ethylene glycol dimethacrylate (EGDMA) | Cross-linking agent to create a stable, three-dimensional polymer network [45] [53]. |
| Ammonium persulfate (APS) | Free-radical initiator to start the polymerization reaction [1]. |
3.1.2 Experimental Workflow
The following diagram illustrates the multi-step synthesis process for creating dual-functional LEV@hCe-pHEMA contact lenses:
3.1.3 Step-by-Step Procedure
- Drug-Loaded Nanoparticle Preparation: Pre-synthesized hollow ceria nanoparticles (hCe NPs) are immersed in a concentrated solution of levofloxacin (LEV) under gentle agitation for 24 hours to allow for drug diffusion into the hollow cores and adsorption onto the nanoparticle surfaces. The resulting LEV@hCe NPs are collected and purified [45].
- Monomer Mixture Preparation: The LEV@hCe NPs are uniformly dispersed in the HEMA monomer. A cross-linker (e.g., EGDMA, typically 0.5-1% v/v) and a polymerization initiator (e.g., Azobisisobutyronitrile, AIBN) are added to the mixture. The solution is thoroughly mixed and degassed to remove dissolved oxygen which can inhibit free-radical polymerization [45] [53].
- Molding and Polymerization: The prepared mixture is pipetted into contact lens molds designed to achieve the desired final lens geometry. The molds are placed in an oven and cured in a stepped heating profile (e.g., 1-2 hours at 70°C, followed by 1 hour at 110°C) to complete the polymerization [45] [53].
- Post-Polymerization Processing: The polymerized lenses are demolded and immersed in deionized water or phosphate-buffered saline (PBS) for at least one week. This hydrates the lenses, forming the soft hydrogel, and leaches out any unreacted monomers or initiator residues [53].
- Characterization and Quality Control:
- Drug Release Kinetics: Place the hydrated lens in a known volume of release medium (e.g., PBS at 37°C). Monitor the drug concentration in the medium over time (e.g., via UV-Vis spectroscopy). The dual-functional lens demonstrated sustained release of LEV (84.2% over 120 hours) [45].
- Antioxidant Activity: Assess ROS scavenging potential using a standard assay like DPPH or by measuring the degradation of hydrogen peroxide. The LEV@hCe-pHEMA lenses showed 78.4% ROS scavenging within 60 minutes [45].
- Biocompatibility: Perform in vitro cytotoxicity tests (e.g., using human corneal epithelial cells) according to ISO 10993-5. The hCe-pHEMA lenses showed excellent biocompatibility with >95% cell viability [45]. In vivo safety in rabbit models also confirmed no ocular irritation over a 7-day wearing period [45].
Protocol: Enhancing Drug Delivery via Vitamin Loading in pHEMA Lenses
This protocol describes a method to increase the drug loading capacity of pHEMA-hydrogel contact lenses by co-loading with lipophilic vitamins (E or A), which act as diffusion barriers and drug reservoirs [53].
3.2.1 Experimental Workflow
The diagram below outlines the sequential and simultaneous loading methods for creating vitamin-enhanced, drug-loaded pHEMA lenses:
3.2.2 Step-by-Step Procedure
- Lens Preparation: Use synthesized or commercially available pHEMA-based hydrogel contact lenses. Ensure lenses are in a dry state to maximize the uptake of the vitamin solution [53].
- Vitamin Loading:
- Prepare a concentrated solution of vitamin E (α-tocopherol) or vitamin A (retinol) in absolute ethanol. Typical concentrations range from 0 to 0.28 M [53].
- Immerse the dry pHEMA lenses in the vitamin-ethanol solution for 24 hours at room temperature.
- Remove the lenses and wash them briefly with ethanol and deionized water to remove excess surface vitamin.
- Dry the vitamin-loaded lenses at room temperature overnight. Note that this process did not significantly alter the water content or size of the lenses [53].
- Drug Loading (Two Methods):
- Sequential Loading: Soak the vitamin-preloaded lens in an aqueous PBS solution containing the hydrophilic drug (e.g., timolol, brimonidine, or a drug surrogate like Alexa Fluor 488 dye) for 24 hours [53].
- Simultaneous Loading: Soak a dry, virgin lens in an ethanol solution containing both the vitamin and the drug for 24 hours [53].
- In Vitro Drug Release Test:
- Place the loaded lens in a vial containing 3 mL of fresh PBS buffer (pH = 7.4) as the release medium. Maintain at a constant temperature (e.g., 37°C).
- At predetermined time intervals, measure the concentration of the released drug in the PBS buffer using an appropriate analytical method (e.g., UV-Vis spectrophotometry at λ_max of 294 nm for timolol). Replenish the release medium to maintain sink conditions [53].
- Expected Outcome: Vitamin E loading significantly increased the loading of timolol and brimonidine by 19.1% and 18.7%, respectively, though it did not drastically extend the release duration [53].
Protocol: Synthesis of a High-Performance p(HEMA-co-mHA-β-CD) Copolymer Hydrogel
This protocol outlines the creation of an advanced pHEMA copolymer designed to overcome inherent limitations of traditional pHEMA, such as poor hydrophilicity and uncontrolled drug release [1].
3.3.1 Key Functional Modifications
Table 3: Key Reagents for Advanced pHEMA Copolymer
| Reagent | Function / Explanation |
|---|---|
| Methacrylated Hyaluronic Acid (mHA) | A rigid, hydrophilic comonomer that enhances hydrophilicity, resists protein deposition, and improves mechanical strength without extra cross-linkers [1]. |
| β-cyclodextrin (β-CD) | A cyclic oligosaccharide grafted onto mHA. Its hydrophobic cavity forms inclusion complexes with drugs, dramatically improving drug loading and enabling sustained release [1]. |
| Methacrylated Hyaluronan-β-cyclodextrin (mHA-β-CD) | The final macromolecular crosslinker that integrates enhanced hydrophilicity and drug-binding functionality directly into the polymer network [1]. |
3.3.2 Experimental Workflow
The synthesis involves creating a functional comonomer and then copolymerizing it with HEMA, as shown below:
3.3.3 Step-by-Step Procedure
- Synthesis of mHA-β-CD Macromer:
- Chemically modify hyaluronic acid (HA) at its active hydroxyl and carboxyl groups to first create methacrylated HA (mHA).
- Separately, synthesize a methacrylated β-cyclodextrin derivative (M-6-O-Ts-β-CD).
- React mHA with the methacrylated β-CD to form the final macromolecular comonomer, mHA-β-CD. The success of each synthesis step should be confirmed by 1H NMR spectroscopy [1].
- Hydrogel Copolymerization:
- Combine the HEMA monomer with the synthesized mHA-β-CD macromer in aqueous solution. The mHA-β-CD acts as both a comonomer and a macromolecular cross-linker.
- Add a water-soluble initiator like ammonium persulfate (APS) to the mixture.
- Pour the solution into appropriate molds and initiate free radical polymerization, often by heating.
- After polymerization, hydrate the resulting hydrogels in deionized water for characterization [1].
- Characterization of Enhanced Properties:
- Hydrophilicity: Measure the static water contact angle. The p(HEMA-co-mHA-β-CD) hydrogel showed a significantly lower contact angle (~61°) compared to traditional pHEMA (~80°), indicating superior surface wettability [1].
- Protein Deposition Resistance: Incubate lenses in a solution containing bovine serum albumin (BSA) and lysozyme. The advanced copolymer demonstrated a significant reduction in the adsorption of these tear proteins [1].
- Sustained Drug Delivery: Load a model drug (e.g., puerarin) and conduct release studies. The β-CD functionality enables a much more sustained release profile compared to unmodified pHEMA hydrogels [1].
pHEMA remains a vitally important and dynamically evolving biomaterial for ophthalmic applications. Its established market position in vision correction is being powerfully supplemented by growth in smart, therapeutic, and diagnostic lenses. The experimental protocols detailed herein—covering dual-functional drug-eluting systems, vitamin-enhanced loading, and advanced copolymer hydrogels—provide a roadmap for researchers and drug development professionals to innovate within this field. The future of pHEMA-based lenses is promising, driven by continuous material science advancements that address its inherent limitations and unlock new functionalities for personalized medicine and improved patient outcomes.
Established Foundations and Emerging Applications of pHEMA
Table 1: Current and Emerging Applications of pHEMA in Ophthalmic Devices
| Application Domain | Key Functionality | Material Composition | Performance Metrics | References |
|---|---|---|---|---|
| Traditional Contact Lenses | Vision correction, corneal protection | pHEMA homopolymer or copolymers | Water content: 20-40%; Oxygen permeability: Variable; Optical transparency: >90% | [76] [77] |
| Therapeutic Drug Delivery | Sustained release of ocular medications | pHEMA/Eudragit L-100 with fusidic acid | Swelling percentage: 20-40% at different pH; Drug release: Days to weeks | [78] [79] |
| Diagnostic Smart Lenses | Intraocular pressure (IOP) monitoring | pHEMA with integrated microsensors | Detection sensitivity: 0.03% deformation/mmHg; Reliability: 0.77 mmHg std dev | [80] |
| Microengineered Platforms | Capillary flow for biosensing | pHEMA with microchannels | Enables colorimetric pH and electrochemical Na+ sensing | [81] |
Poly(2-hydroxyethyl methacrylate) (pHEMA) has maintained its status as a cornerstone biomaterial in ophthalmology since its initial development by Wichterle and Lim in the 1960s [76] [77]. Its exceptional biocompatibility, optical transparency, and favorable mechanical properties have established it as the primary material for conventional soft contact lenses. The polymer's hydrophilic nature enables significant water absorption (typically 20-40%), forming hydrogels that provide comfort and oxygen permeability essential for ocular applications [78] [76]. Recent research has expanded pHEMA's utility beyond passive vision correction to active therapeutic and diagnostic roles, positioning it at the forefront of smart lens technology.
The inherent biocompatibility of pHEMA arises from its chemical structure, which minimizes immunological responses and ensures patient safety during extended wear [76]. This fundamental characteristic, combined with advances in material engineering, has enabled the development of sophisticated drug delivery systems and biosensing platforms. pHEMA's capacity for functionalization through copolymerization, molecular imprinting, and integration with responsive polymers has facilitated its evolution into a versatile platform for advanced ocular devices [82] [77].
Advanced Therapeutic Applications: Protocols and Methodologies
Protocol: Fabrication of Drug-Loaded pHEMA Hydrogels for Ocular Delivery
Objective: To synthesize fusidic acid-loaded pHEMA/Eudragit L-100 hydrogels for controlled antibiotic delivery in eczema treatment [78].
Materials:
- 2-hydroxyethyl methacrylate (HEMA, 97% purity)
- Eudragit L-100 (anionic pH-responsive polymer)
- Fusidic acid (antibiotic agent)
- Ethylene glycol dimethacrylate (EGDMA, 95% purity, crosslinker)
- Ammonium persulfate (APS, initiator)
- Ethanol (solvent)
Methodology:
- Polymer Solution Preparation: Dissolve 0.6-1.0 g Eudragit L-100 and 50 mg fusidic acid in 3 mL ethanol with magnetic stirring at 500 rpm until homogeneous.
- Monomer Mixture: Combine HEMA monomer with EGDMA crosslinker (0.5-3% v/v) and APS initiator (1-2% w/v).
- Drug Loading: Incorporate the fusidic acid/Eudragit solution into the monomer mixture while maintaining temperature at 60°C.
- Polymerization: Pour the final mixture into glass molds and maintain at 60-80°C for 12-24 hours to complete polymerization.
- Post-processing: Carefully remove gels from molds and dry at room temperature until constant weight is achieved.
- Quality Control: Determine swelling percentage in different pH environments and characterize using FTIR and SEM.
Critical Parameters: Crosslinker concentration directly impacts mesh size and drug release kinetics; Eudragit L-100 provides pH-responsive behavior for targeted release [78].
Application Notes: pH-Responsive Drug Delivery Systems
Table 2: Characterization of pHEMA-Based Drug Delivery Systems
| Parameter | Experimental Conditions | Results/Performance | Significance |
|---|---|---|---|
| Swelling Behavior | pH 2.0 vs. pH 7.4 | Significantly higher swelling at physiological pH | Enables targeted drug release in specific ocular environments |
| Drug Release Profile | Fusidic acid in pHEMA/Eudragit | Sustained release over 24-48 hours | Reduces dosing frequency from multiple daily applications to once daily |
| Mechanical Properties | Varying EGDMA crosslinker (0.5-3%) | Enhanced strength with higher crosslink density | Maintains lens integrity during extended wear |
| Surface Characteristics | SEM analysis | Microporous structure (pore size: 1-10 μm) | Facilitates controlled drug diffusion and oxygen permeability |
pHEMA gels exhibit exceptional pH-sensitive swelling behavior, particularly at higher crosslinking densities [79]. This phenomenon is attributed to the Donnan potential increase resulting from carboxyl end-groups introduced during polymerization. The swelling capacity directly influences drug release rates, with higher swelling correlating to increased drug diffusion coefficients. This property can be leveraged for targeted therapy in ocular conditions where pH variations occur, such as inflammatory states [79].
For antibiotic delivery, as demonstrated with fusidic acid, the pHEMA platform provides sustained release that maintains therapeutic concentrations while minimizing systemic exposure. This approach addresses the critical limitation of conventional eye drops, which typically exhibit less than 5% corneal bioavailability due to rapid clearance mechanisms [78] [77].
Smart Lens Integration: Microengineering and Biosensing
Protocol: Microfabrication of pHEMA-Based Smart Lenses for IOP Monitoring
Objective: To create microengineered pHEMA hydrogels with integrated sensors for continuous intraocular pressure monitoring [81] [80].
Materials:
- pHEMA hydrogel sheets (standard contact lens material)
- Three-dimensional (3D) printed molds with microchannel patterns
- Micropyramid elastomer sensors
- Polymeric adhesion layers
- Wireless readout components
Methodology:
- Microchannel Fabrication: Utilize 3D printed molds to create precise microchannel architectures within pHEMA hydrogels [81].
- Sensor Integration: Layer micropyramid elastomers onto the pHEMA substrate, creating a three-layer sensor structure positioned externally on the lens to preserve visual axis clarity [80].
- System Assembly: Integrate the sensor-equipped pHEMA lens with an adjustable reader embedded in specialized glasses for wireless signal detection.
- Calibration: Correlate hydrogel deformation with IOP changes, establishing a sensitivity baseline of 0.03% dimensional change per mmHg pressure variation.
- Validation: Test device reliability in porcine models, calculating mean deviation and standard deviation between measurements (target: <1.0 mmHg).
Technical Considerations: The external sensor placement preserves optical clarity while maintaining compatibility with standard lens geometry. The system demonstrates exceptional reliability with mean deviation of 0.30 mmHg and standard deviation of 0.77 mmHg between measurements [80].
Application Notes: Microfluidic Capillary Flow in pHEMA Lenses
The creation of microchannels within pHEMA hydrogels enables capillary flow crucial for biosensing applications. Different flow regimes have been observed depending on hydration levels, with peristaltic pressure (simulating eye-blinking) capable of reinstating flow in dehydrated channels [81]. This finding suggests that natural ocular movements may facilitate tear sampling and transport through microengineered channels in functional lenses.
Research has demonstrated colorimetric pH sensing and electrochemical Na+ detection within these microchannels, validating pHEMA's potential for continuous metabolic monitoring [81]. The combination of established biocompatibility with emerging microengineering techniques positions pHEMA as an ideal substrate for next-generation diagnostic contact lenses.
Research Reagent Solutions: Essential Materials for pHEMA Hydrogel Development
Table 3: Key Research Reagents for pHEMA Hydrogel Experiments
| Reagent/Category | Representative Examples | Primary Function | Research Considerations |
|---|---|---|---|
| Monomers | HEMA (2-hydroxyethyl methacrylate) | Primary building block for polymer network | Requires purification; vacuum distillation recommended [79] |
| Crosslinkers | EGDMA, TPGDA (tripropyleneglycol diacrylate) | Controls mesh size, mechanical properties | Concentration (0.5-3%) directly affects drug release rates [78] [79] |
| Initiators | Ammonium persulfate (APS) | Free radical polymerization initiation | Typically used at 1-2% w/v; impacts reaction kinetics [78] |
| Functional Additives | Eudragit L-100, chitosan | Enables pH-responsive behavior, enhanced bioadhesion | Eudragit L-100 dissolves at pH >6 for intestinal targeting [78] |
| Therapeutic Agents | Fusidic acid, salicylic acid, various antibiotics | Active pharmaceutical ingredients | Hydrophilicity/hydrophobicity affects loading efficiency and release kinetics [78] [79] |
| Analytical Tools | FTIR, SEM, swelling studies | Material characterization | SEM reveals porous structure; swelling studies indicate crosslink density [78] |
Future Research Trajectories and Commercialization Challenges Figure: Advanced pHEMA Development Workflow
The future development of pHEMA-based ocular devices will focus on enhancing functionality while maintaining the biocompatibility that has established its clinical utility. Key research priorities include:
Multi-analyte Biosensing: Expanding beyond IOP monitoring to integrate sensors for glucose, lactate, and pH, leveraging pHEMA's permeability to small molecules [81] [80].
Stimuli-Responsive Drug Delivery: Developing "smart" systems that release therapeutics in response to specific ocular biomarkers or external triggers [82] [77].
Advanced Material Composites: Creating pHEMA-based hybrids with nanomaterials, conductive polymers, and biodegradable components to enhance functionality while addressing environmental concerns [83] [76].
Manufacturing Innovation: Implementing molecular imprinting techniques and computer-aided design to create devices with precise molecular recognition capabilities [77].
Commercial translation faces challenges including long-term stability of integrated electronics, sterilization compatibility, regulatory pathway definition, and cost-effective manufacturing scale-up. However, pHEMA's established safety profile and recent advancements in microengineering position it favorably for continued innovation in the evolving landscape of smart ocular therapeutics.
Conclusion
Poly(2-hydroxyethyl methacrylate) remains a cornerstone material in contact lens science, particularly as a versatile platform for innovative ophthalmic drug delivery systems. While modern silicone hydrogels excel in oxygen transmissibility for general wear, PHEMA's proven biocompatibility, tunable chemistry, and capacity for integration with natural biomaterials like chitosan and hyaluronic acid secure its unique role in therapeutic applications. Future research directions should focus on developing next-generation PHEMA composites that synergistically combine enhanced oxygen permeability with sophisticated, controlled drug release profiles. The translation of these advanced materials from laboratory prototypes to commercially viable, clinically approved products represents the most critical next step, positioning PHEMA-based hydrogels to continue making significant contributions to biomedical research and patient care in tailored ophthalmologic therapies.
References
- 1. A potential contact lens material with high hydrophilicity ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813024083892]
- 2. Poly(2-hydroxyethyl methacrylate)-Based Hydrogel ... [https://www.matexcel.com/hydrogel/poly2-hydroxyethyl-methacrylate-based-hydrogel-development.html]
- 3. Poly(2-Hydroxyethyl Methacrylate) Hydrogels for Contact ... [https://www.semanticscholar.org/paper/Poly(2-Hydroxyethyl-Methacrylate)-Hydrogels-for-Saptaji-Iza/7f481827aaaee4e672d8005c1a0951db334dee41]
- 4. effects of water content, mechanical and thermal properties [https://www.sciencedirect.com/science/article/pii/S1026918525000599]
- 5. Features of Structure and Properties of pHEMA-gr-PVP ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7602374/]
- 6. Drug-Modified Contact Lenses—Properties, Release Kinetics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11173495/]
- 7. HISTORY OF CONTACT LENSES [https://www.clspectrum.com/issues/2021/april/history-of-contact-lenses/]
- 8. Otto Wichterle [https://en.wikipedia.org/wiki/Otto_Wichterle]
- 9. pHEMA: An Overview for Biomedical Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8232190/]
- 10. A Drug-Eluting Contact Lens - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4657544/]
- 11. Poly(2-hydroxyethyl methacrylate) hydrogels containing ... [https://www.sciencedirect.com/science/article/pii/S1742706123002313]
- 12. Transparent and tough poly(2-hydroxyethyl methacrylate ... [https://pubs.rsc.org/en/content/articlelanding/2020/nj/d0nj00214c]
- 13. AAOpt 2025 recap: What's new in contact lens technology, ... [https://www.optometrytimes.com/view/aaopt-2025-recap-what-s-new-in-contact-lens-technology-trends-and-more]
- 14. 2025 [https://www.clspectrum.com/news/2025/]
- 15. AI Usage in Contact Lens Management: Past, Present, and ... [https://contactlensupdate.com/2025/08/08/ai-usage-in-contact-lens-management-past-present-and-future/]
- 16. Poly(2-Hydroxyethyl Methacrylate) Hydrogels for Contact ... [https://www.academia.edu/75690256/Poly_2_Hydroxyethyl_Methacrylate_Hydrogels_for_Contact_Lens_Applications_A_Review]
- 17. Polymerization Kinetics of Poly(2-Hydroxyethyl ... [https://www.mdpi.com/2227-9717/5/2/21]
- 18. Hydrogels of Poly(2-hydroxyethyl methacrylate) and Poly(N ... [https://www.mdpi.com/1999-4923/17/1/62]
- 19. Hydrogels of Poly(2-hydroxyethyl methacrylate) and Poly(N ... [https://pubmed.ncbi.nlm.nih.gov/39861710/]
- 20. Molecular Dynamics Simulations of HEMA-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11643488/]
- 21. Contact Lens Materials: A Materials Science Perspective [https://pmc.ncbi.nlm.nih.gov/articles/PMC6356913/]
- 22. Optimization of the Oxygen Permeability of Non-Silicone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11593662/]
- 23. Impact of morphology on O2 permeability in silicone ... [https://www.sciencedirect.com/science/article/abs/pii/S037673882031543X]
- 24. Soft Contact Lenses as Drug Delivery Systems: A Review [https://www.mdpi.com/1420-3049/26/18/5577]
- 25. Fabricating customized hydrogel contact lens [https://www.nature.com/articles/srep34905]
- 26. Poly(2-hydroxyethyl methacrylate)/β-cyclodextrin ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706120301999]
- 27. Replica-mold nanopatterned PHEMA hydrogel surfaces for ... [https://www.nature.com/articles/s41598-022-18564-3]
- 28. Fabrication Strategies Towards Hydrogels for Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9828515/]
- 29. Evaluation of silicone hydrogel contact lenses based on ... [https://www.sciencedirect.com/science/article/abs/pii/S092777652100401X]
- 30. Biodegradable Contact Lenses for Targeted Ocular Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12195844/]
- 31. The Promise of Drug-Eluting Contact Lenses [https://modernod.com/topics/contact-lenses/the-promise-of-drug-eluting-contact-lenses/38780/]
- 32. Contact lens as an emerging platform for ophthalmic drug ... [https://www.sciencedirect.com/science/article/pii/S1818087623000740]
- 33. A Drug Delivery Study by Novan Lutfhyansyah, Haider Butt ... [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5358336]
- 34. Contact Lens as Drug Delivery System for Glaucoma ... [https://openophthalmologyjournal.com/VOLUME/17/ELOCATOR/e187436412301310/FULLTEXT/]
- 35. NVP-based molecularly imprinted hydrogel contact lenses ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224724011808]
- 36. Imprinted Contact Lenses for Ocular Administration of ... [https://www.mdpi.com/2073-4360/12/9/2026]
- 37. Molecularly imprinted therapeutic contact lenses [https://pubmed.ncbi.nlm.nih.gov/20408742/]
- 38. Natural biomaterials for contact lens-based ophthalmic ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925007837]
- 39. Natural Polymer-Based Hydrogels - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10610124/]
- 40. Exploring the Progress of Hyaluronic Acid Hydrogels [https://www.mdpi.com/1996-1944/17/10/2439]
- 41. Fabrication and characterization of pHEMA hydrogel ... [https://www.explorationpub.com/Journals/ebmx/Article/10135]
- 42. pH Sensitive Hydrogels in Drug Delivery: Brief History ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6432076/]
- 43. pHEMA: An Overview for Biomedical Applications [https://pubmed.ncbi.nlm.nih.gov/34203608/]
- 44. Poly(2-hydroxyethyl methacrylate) film as a drug delivery ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961200003367]
- 45. Dual-functional hCe-pHEMA contact lenses for ocular ... [https://pubmed.ncbi.nlm.nih.gov/40324534/]
- 46. Influence of drug and polymer molecular weight on release ... [https://www.nature.com/articles/s41598-023-42923-3]
- 47. Anticancer drug, ara-C, release from pHEMA hydrogels [https://pubmed.ncbi.nlm.nih.gov/7893922/]
- 48. Contact Lenses 101, Part 1: Contact Lens Materials [https://coopervision.com/practitioner/ecp-viewpoints/technicians-and-staff/contact-lenses-101-part-1-contact-lens-materials]
- 49. Probing the mechanisms of drug release from hydrogels [https://www.sciencedirect.com/science/article/abs/pii/016836599190046G]
- 50. Biomimetic-Engineered Silicone Hydrogel Contact Lens ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10521029/]
- 51. Contact Lens Materials Guide: Daily, Weekly & Monthly 2025 [https://www.westbrowardeyecare.com/contact-lens-materials-guide-daily-weekly-monthly-2025/]
- 52. Recent Progress of Biodegradable Polymer Package Materials [https://pmc.ncbi.nlm.nih.gov/articles/PMC10892516/]
- 53. Ocular Drug Delivery through pHEMA-Hydrogel Contact ... [https://www.nature.com/articles/srep34194]
- 54. Drug-Eluting Sandwich Hydrogel Lenses Based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10288497/]
- 55. Synthesis of three-dimensional hydrogels based on poly ... [https://arabjchem.org/synthesis-of-three-dimensional-hydrogels-based-on-polyglycidyl-methacrylate-alt-maleic-anhydride-characterization-and-study-of-furosemide-drug-release/]
- 56. Silanization, Wettability and Lysozyme Adsorption Studies [https://pubmed.ncbi.nlm.nih.gov/3741958/]
- 57. Protein adsorption on hydrogels. II. Reversible and ... [https://pubmed.ncbi.nlm.nih.gov/4052547/]
- 58. Protein Deposition and Bacterial Adhesion to Conventional ... [https://uwspace.uwaterloo.ca/items/ebe9a8f0-fc1c-450d-b869-dd126f8daf1e]
- 59. Plasma surface treatment of silicone hydrogel contact lenses [https://patents.google.com/patent/US6193369B1/en]
- 60. Enhancing Performance of Silicone Hydrogel Contact ... [https://www.mdpi.com/2079-4983/15/11/321]
- 61. Plasma surface treatment of silicone hydrogel contact lenses [https://www.semanticscholar.org/paper/Plasma-surface-treatment-of-silicone-hydrogel-%E3%82%A2%E3%83%A2%E3%83%B3%EF%BC%8C-%E3%82%B0%E3%83%AD%E3%83%BC%E3%83%96%EF%BC%8C/f79f00fb253d92869713878f3f3343aed346f04a]
- 62. Understanding the Influence of Water Content in Soft Lenses [https://www.reviewofoptometry.com/article/understanding-the-influence-of-water-content-in-soft-lenses]
- 63. Topical review: Twenty-five years of silicone hydrogel soft ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12184980/]
- 64. Comfort After Refitting Symptomatic Habitual Reusable Toric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10624181/]
- 65. Polysaccharides in contact lenses: From additives to bulk ... [https://www.sciencedirect.com/science/article/abs/pii/S014486172300468X]
- 66. Best Gas Permeable Oxygen Contact Lenses for Healthier Eyes [https://diamondvision.com/top-oxygen-permeable-contact-lens-materials-for-healthier-eyes/]
- 67. Microfluidic contact lens: fabrication approaches and ... [https://www.nature.com/articles/s41378-025-00909-3]
- 68. Hydrogel-based ocular drug delivery systems - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d5tb01575h?page=search]
- 69. Biodegradable Contact Lenses for Targeted Ocular Drug ... [https://www.mdpi.com/1420-3049/30/12/2542]
- 70. HYDROGELS FROM SOFT CONTACT LENSES AND ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2776732/]
- 71. Natural biomaterials for contact lens-based ophthalmic ... [https://pubmed.ncbi.nlm.nih.gov/40882773/]
- 72. : An Overview for Biomedical pHEMA -Bohrium Applications [https://www.bohrium.com/paper-details/phema-an-overview-for-biomedical-applications/812288519715160064-9516]
- 73. Polyhydroxyethylmethacrylate - Wikipedia [https://en.wikipedia.org/wiki/Polyhydroxyethylmethacrylate]
- 74. Smart Contact Lenses Market Size & Share Report, 2032 [https://www.gminsights.com/industry-analysis/smart-contact-lenses-market]
- 75. Contact Lenses Market Size, Forecast Report & Growth 2030 [https://www.mordorintelligence.com/industry-reports/contact-lenses-market]
- 76. pHEMA: An Overview for Biomedical Applications [https://www.mdpi.com/1422-0067/22/12/6376]
- 77. Advances in Therapeutic Contact Lenses for the ... [https://www.mdpi.com/2075-4426/13/11/1571]
- 78. Fabrication and Evaluation of Poly(2-hydroxyethyl ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10399181/]
- 79. Evaluation of poly(2-hydroxyethyl methacrylate) gels as ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517399003750]
- 80. Hydrogel-Based Smart Contact Lens for Highly Sensitive ... [https://scienceforallaudiences.org/2024/11/12/hydrogel-based-smart-contact-lens-for-highly-sensitive-eye-pressure-fluid-monitoring/]
- 81. Microengineered poly(HEMA) hydrogels for wearable ... [https://pubmed.ncbi.nlm.nih.gov/33048069/]
- 82. Smart Hydrogels for Advanced Drug Delivery Systems - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8998863/]
- 83. Meta-Analysis of Materials and Treatments Used in Contact ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11989920/]