Pulse Wave-Driven Machine Learning for Non-Invasive Coronary Artery Calcification Detection: Validation and Clinical Application
This article provides a comprehensive analysis of the validation of pulse wave analysis combined with machine learning for the non-invasive detection of coronary artery calcification, a major cardiovascular risk factor.
Pulse Wave-Driven Machine Learning for Non-Invasive Coronary Artery Calcification Detection: Validation and Clinical Application
Abstract
This article provides a comprehensive analysis of the validation of pulse wave analysis combined with machine learning for the non-invasive detection of coronary artery calcification, a major cardiovascular risk factor. Aimed at researchers, scientists, and drug development professionals, it explores the foundational pathophysiology linking vascular dynamics to CAC, details methodological approaches for model development including feature extraction and algorithm selection, addresses critical challenges in clinical deployment such as algorithmic bias and regulatory compliance, and evaluates performance metrics and comparative effectiveness against traditional screening methods. The content synthesizes recent 2025 clinical evidence to outline a pathway for integrating this promising, cost-effective technology into cardiovascular risk assessment pipelines.
The Pathophysiological Link Between Pulse Wave Dynamics and Coronary Calcification
Coronary Artery Calcification as a Critical Cardiovascular Risk Marker in Renal Disease
Coronary Artery Calcification (CAC) represents a particularly aggressive form of atherosclerosis that disproportionately affects individuals with chronic kidney disease (CKD). The pathophysiological relationship between renal impairment and vascular calcification creates a perfect storm for cardiovascular complications. In CKD patients, traditional Framingham risk factors converge with unique uremic stressors—including hyperphosphatemia, calciprotein particle formation, and chronic inflammation—to drive accelerated calcification within coronary artery walls [1]. This process is not merely a passive precipitation of calcium phosphate but an active, cell-mediated transformation of vascular smooth muscle cells into osteoblast-like cells, culminating in profound vascular stiffness and compromised myocardial perfusion.
The clinical implications of this process are severe. Among patients with CKD, cardiovascular mortality is 10 to 30 times higher than in the general population, with CAC serving as a central pathological feature driving this excessive risk [1]. Recent evidence from the Chronic Renal Insufficiency Cohort (CRIC) study demonstrates that CAC progression in CKD patients occurs at an accelerated rate compared to those with preserved renal function, creating an urgent need for effective detection and monitoring strategies [2] [3]. This review comprehensively compares established and emerging technologies for CAC assessment, with particular emphasis on validating pulse wave-driven machine learning approaches within the renal disease population.
Established Methods for Coronary Artery Calcification Assessment
Computed Tomography and the Agatston Score
The quantification of coronary artery calcium via computed tomography (CT) imaging remains the undisputed gold standard for CAC assessment. The Agatston score, developed in 1990, calculates CAC burden through a weighted combination of calcified plaque area and maximum density factor observed on electrocardiogram-gated non-contrast CT scans [4] [5]. Current clinical protocols typically stratify patients into risk categories based on Agatston score ranges: zero (no identifiable plaque), 1-100 (mild), 101-400 (moderate), and greater than 400 (severe calcification) [6] [5].
The prognostic power of CAC scoring is well-established in both general and renal populations. The CRIC study prospectively evaluated 1,310 CKD participants with at least one CAC scan and found that those without baseline CAC who developed incident calcification had a 2.42-fold higher rate of atherosclerotic cardiovascular disease (95% CI: 1.23-4.79) and 1.82-fold higher all-cause mortality (95% CI: 1.03-3.22) after multivariable adjustment [2] [3]. Similarly, patients with baseline CAC who experienced progression (defined as ≥50 Agatston units per year) demonstrated a 1.73-fold higher mortality rate (95% CI: 1.31-2.28) [2].
Table 1: Performance Characteristics of CAC Detection Technologies
| Methodology | Population Studied | Key Performance Metrics | Advantages | Limitations |
|---|---|---|---|---|
| CT-Based Agatston Scoring | 1,310 CKD patients [2] | Hazard Ratio for Mortality: 1.73-1.82 [2] | Prognostic validation; Standardized risk categories | Radiation exposure; Cost; Limited accessibility |
| AI-Automated CAC Scoring | 79 CT scans [4] | Kappa=0.89 vs manual scoring [4] | High speed (<60 sec); Elimination of inter-reader variability | Limited validation in CKD-specific populations |
| Pulse Wave ML Model (GBDT) | 58 ESRD patients [6] [7] | Accuracy=84.1%; AUC=0.962 [6] | Non-invasive; Cost-effective; Bedside application | Small sample size; Single-center design |
| Pulse Wave ML Model (SphygmoCor) | 124 CKD stage 5 patients [8] | Balanced accuracy >80% for CAC≥100 [8] | Superior to traditional risk factors in younger patients | Limited data for CKD stages 3-4 |
Artificial Intelligence in CAC Quantification
Recent advances in artificial intelligence have transformed CAC assessment from a labor-intensive manual process to an automated pipeline with emerging clinical applications. Convolutional neural networks (CNNs)—a deep learning architecture specifically designed for image processing—have demonstrated remarkable proficiency in automating CAC scoring on both dedicated cardiac CT and non-gated chest CT examinations performed for other indications [4].
The clinical implementation of AI-driven CAC scoring addresses several critical limitations of traditional approaches. Automated systems eliminate inter-observer variability, significantly reduce interpretation time (with processing times under 60 seconds in some implementations), and potentially enable widespread CAC screening through opportunistic detection on non-cardiac CT studies [4]. Notably, non-gated chest CT scans performed for lung cancer screening represent a particularly promising application, as this population overlaps significantly with those at intermediate to high cardiovascular risk. Unfortunately, current reporting of incidental CAC on these studies remains inconsistent, occurring in only 44-59% of cases with visible calcification [4].
Pulse Wave-Driven Machine Learning: An Emerging Paradigm
Physiological Rationale and Technical Foundations
The fundamental premise of pulse wave analysis for CAC assessment rests on the principle that progressive vascular calcification alters arterial biomechanics in measurable ways. As coronary arteries undergo calcification, parallel changes occur in systemic arterial stiffness, pulse wave velocity, and waveform morphology—all of which can be captured and quantified through peripheral pulse wave analysis [6] [8].
The pathophysiological link between CKD and altered pulse wave characteristics involves multiple interconnected pathways. Uremia-induced vascular smooth muscle cell transdifferentiation, chronic inflammation mediated by cytokines such as galectin-3 and hs-CRP, and metabolic abnormalities including hyperphosphatemia collectively drive both coronary calcification and increased arterial stiffness [1] [9]. These changes manifest in distinct pulse wave patterns characterized by attenuated tidal waves, altered diastolic decay contours, and overall waveform smoothing that correlates with CAC severity [6].
Experimental Protocols and Methodologies
Recent investigations have employed standardized protocols for pulse wave data acquisition and analysis in CKD populations. In a study of 58 end-stage renal disease (ESRD) patients undergoing hemodialysis, radial artery pulse waveforms were recorded before, hourly during, and after hemodialysis sessions using calibrated acquisition systems [6] [7]. Participants concurrently underwent low-dose computed tomography (LDCT) for CAC quantification using Agatston scoring, establishing ground truth for model development.
The feature extraction pipeline encompassed multiple pulse wave domains:
- Morphological parameters: Primary wave amplitude, tidal wave presence and amplitude, dicrotic notch position
- Temporal characteristics: Pulse wave transit time, systolic and diastolic phase intervals
- Complexity metrics: Multiscale entropy, waveform distribution characteristics
- Hemodynamic indices: Mean amplitude, ascending/descending slope characteristics [6]
Machine learning models, particularly Gradient Boosting Decision Tree (GBDT) algorithms, were then trained to classify CAC severity into four categories (none, mild, moderate, severe) based on the extracted pulse wave features. The GBDT framework was selected for its ability to model complex nonlinear relationships between pulse wave characteristics and CAC burden while providing robustness against overfitting [6] [7].
Performance Validation and Comparative Efficacy
The validated performance of pulse wave-driven machine learning models for CAC detection is compelling, particularly considering the relatively early stage of this technological approach. In the aforementioned study of ESRD patients, the GBDT model achieved an average accuracy of 84.1% with a macro-AUC of 0.962 in fivefold cross-validation, with comparable performance (83.9% accuracy, 0.961 AUC) on an independent test set [6] [7]. Notably, the model demonstrated particular proficiency in identifying severe calcification cases, which carries the greatest clinical significance for risk stratification.
A separate investigation of 124 CKD stage 5 patients evaluated a pulse wave-based classifier using the SphygmoCor system and demonstrated balanced accuracy exceeding 80% for detecting clinically significant CAC (Agatston score ≥100) [8]. This study further revealed that the pulse wave-based approach outperformed models using traditional risk factors alone, particularly among younger patients (under 50 years old), suggesting potential value for early detection in high-risk populations [8].
Table 2: Key Research Reagent Solutions for Pulse Wave CAC Detection Studies
| Research Tool | Specification Purpose | Experimental Function | Validation Context |
|---|---|---|---|
| Radial Artery Pulse Wave Acquisition System | SphygmoCor (AtCor Medical) [8] or equivalent | Capture peripheral pulse waveform data at radial artery | 58 ESRD patients [6]; 124 CKD stage 5 patients [8] |
| Gradient Boosting Decision Tree (GBDT) Algorithm | Machine learning framework | Classify CAC severity from pulse wave features | 84.1% accuracy, 0.962 AUC for CAC severity stratification [6] |
| Low-Dose Computed Tomography (LDCT) | Non-contrast, ECG-gated protocol | Reference standard for Agatston score calculation | CAC severity classification per standard categories (0, 1-100, 101-400, >400) [6] |
| Pulse Wave Feature Extraction Pipeline | Morphological, temporal, complexity domains | Quantify pulse waveform characteristics for model input | Significant variation across CAC groups and during hemodialysis [6] |
Comparative Analysis: Traditional vs. Emerging Approaches
When evaluated against established CAC detection methodologies, pulse wave-driven machine learning demonstrates a distinct performance profile with complementary strengths and limitations. Traditional CT-based approaches provide unparalleled anatomical visualization and extensive prognostic validation across diverse populations, including robust data from the CRIC study specifically in CKD patients [2] [3]. AI-enhanced CAC scoring builds upon this foundation with improved efficiency and reproducibility while maintaining high diagnostic accuracy [4].
The pulse wave analysis paradigm sacrifices some degree of accuracy for substantial advantages in accessibility, cost-effectiveness, and practical implementation. The 84-85% accuracy demonstrated in current validation studies [6] [8] falls short of the near-perfect agreement between AI and manual CT scoring (kappa=0.89) [4]. However, the non-invasive nature, minimal cost, and point-of-care applicability of pulse wave analysis position it as a promising screening tool rather than a replacement for definitive CT-based assessment.
This distinction is particularly relevant in nephrology practice, where serial monitoring of cardiovascular risk is necessary but frequent CT imaging is impractical due to cost, radiation exposure, and accessibility limitations. Pulse wave technology could potentially fill this gap by identifying which CKD patients warrant definitive CT-based CAC assessment, thereby optimizing resource utilization while maintaining vigilant cardiovascular risk surveillance.
Clinical Implications and Future Research Directions
The validated association between CAC progression and adverse clinical outcomes in CKD populations [2] [3] underscores the critical importance of effective detection strategies. Pulse wave-driven machine learning approaches offer a promising adjunct to existing methodologies, particularly for serial monitoring and initial risk stratification in resource-limited settings.
Several research priorities emerge to advance this field. First, validation in larger, multi-center CKD cohorts spanning earlier disease stages (CKD 3-4) is essential to establish generalizability beyond ESRD populations. Second, technical refinement of feature extraction algorithms and exploration of alternative machine learning architectures may enhance diagnostic accuracy. Third, longitudinal studies evaluating the ability of pulse wave-based CAC monitoring to guide therapy and improve clinical outcomes would represent the ultimate validation of this approach.
For drug development professionals, the emergence of reliable, non-invasive CAC monitoring tools creates opportunities for efficient endpoint assessment in clinical trials targeting cardiovascular risk reduction in CKD populations. The ability to serially evaluate CAC progression without repeated CT imaging could significantly reduce trial costs and participant burden while maintaining objective assessment of therapeutic efficacy.
In conclusion, while CT-based CAC assessment remains the gold standard for cardiovascular risk stratification in renal patients, pulse wave-driven machine learning represents a promising complementary technology with distinct advantages for screening and serial monitoring. Further validation and refinement of this approach may substantially enhance cardiovascular risk management in the vulnerable CKD population.
The arterial system is not merely a passive conduit for blood flow but a dynamic interface where hemodynamic forces interact with vascular biology. Arterial stiffness represents a key manifestation of vascular aging and pathology, fundamentally altering how pressure waves travel through the arterial tree. These alterations produce characteristic changes in pulse waveform morphology that can be quantified and analyzed. The relationship between arterial properties and pulse contours forms the foundation for non-invasive cardiovascular assessment, particularly as technological advances enable increasingly sophisticated analysis techniques.
Central to this relationship is the phenomenon of wave reflection, wherein pressure waves encounter impedance mismatches at branching points and vascular beds, generating reflected waves that travel backward toward the heart. In compliant, healthy arteries, these reflected waves arrive during diastole, potentially enhancing coronary perfusion. With increased arterial stiffness, wave velocity rises, causing reflected waves to arrive earlier during systole, augmenting central systolic pressure and increasing cardiac afterload. This dynamic interplay between forward and reflected waves creates distinct morphological features in the arterial pulse contour that carry diagnostic information about vascular health [10].
Technical Comparison of Arterial Assessment Methodologies
Functional versus Morphological Assessment Approaches
Vascular assessment methodologies generally fall into two categories: functional measures of arterial dynamics and morphological measures of arterial structure. Each approach offers distinct advantages and captures different aspects of vascular pathology, as summarized in Table 1.
Table 1: Comparison of Vascular Assessment Methodologies
| Assessment Type | Specific Measures | Physiological Correlate | Strengths | Limitations |
|---|---|---|---|---|
| Functional | Carotid-femoral PWV (cfPWV) | Aortic stiffness | Gold standard, strong prognostic value | Requires multi-site measurement |
| Brachial-ankle PWV (baPWV) | Global arterial stiffness | Simple, non-invasive | Includes muscular arteries | |
| Augmentation Index (AIx) | Wave reflection magnitude | Independent prognostic value | Heart rate dependent | |
| Pulse Wave Upstroke Time (UT) | Ventricular ejection characteristic | CAC association [11] | Limited standalone value | |
| Morphological | Carotid Intima-Media Thickness (cIMT) | Early structural adaptation | Well-validated, predictive | Measurement variability |
| Coronary Artery Calcium (CAC) | Advanced atherosclerosis | Direct coronary assessment | Radiation exposure, cost |
Hemodynamic Parameter Performance Characteristics
Different hemodynamic parameters demonstrate varying strengths in their associations with coronary artery calcification across patient populations. Table 2 summarizes key performance characteristics from clinical studies.
Table 2: Hemodynamic Parameters and Coronary Artery Calcification Associations
| Parameter | Population | CAC Association | Statistical Strength | Study Details |
|---|---|---|---|---|
| cfPWV | Framingham Offspring (n=1,015) | Positive with TAC, AAC, CAC | OR 1.48 per SD for CAC [12] | Multivariable adjusted |
| Framingham Gen 3 (n=1,905) | Stronger in younger cohort | OR 2.69 per SD for TAC [12] | Age effect modification | |
| baPWV | Prospective cohort (n=1,124) | CAC progression predictor | OR 2.14 (Q4 vs Q1) [13] | 2.7-year follow-up |
| Pulse Wave UT | Clinical (n=133) | Independent CAC correlate | P=0.038 [11] | Multivariate analysis |
Experimental Protocols in Pulse Wave Analysis
Standardized Pulse Wave Acquisition Protocol
The methodology for pulse wave acquisition follows rigorous standardization to ensure reproducible measurements:
Patient Preparation: Participants refrain from alcohol, caffeine, and hot drinks for 12 hours prior to measurement. They rest in a supine position for at least 5 minutes in a temperature-controlled room (20-24°C) before measurement begins [10].
Equipment Setup: Blood pressure cuffs are appropriately sized and positioned on the right upper arm (brachial artery) and right lower leg (anterior tibial artery). For carotid-femoral PWV measurement, distance measurements are taken between the suprasternal notch and femoral artery using a tape measure [10].
Signal Acquisition: Multiple pulse wave recordings (typically 10-20 consecutive beats) are obtained at each measurement site. Measurements with motion artifacts or poor signal quality are immediately repeated. The entire protocol typically takes 15-20 minutes per subject [10].
Signal Processing: Acquired waveforms are processed using automated algorithms that identify fiducial points (systolic upstroke, peak systolic, diastole). The quality index threshold is typically set to >80% for acceptable recordings [6].
Pulse Wave Feature Extraction Methodology
The morphological analysis of pulse waves focuses on specific characteristic points and derived parameters:
Primary Feature Identification: The analysis identifies the systolic main wave (P1), tidal wave (P2), and dicrotic wave (P3) on the pulse contour. With increasing arterial stiffness and CAC severity, the tidal wave becomes progressively attenuated and less distinguishable from the main wave [6].
Time-Domain Parameters: These include pulse transit time (time between systolic foot and diastolic notch), upstroke time (time from diastolic minimum to systolic maximum), and ejection duration (systolic phase) [11] [6].
Amplitude Ratios: The augmentation index is calculated as the difference between the second and first systolic peaks divided by pulse pressure, expressed as a percentage. Reflection magnitude is derived from harmonic analysis of forward and backward waves [10].
Complexity Features: Non-linear analysis includes multiscale entropy and complexity indices that quantify the irregularity of pulse waveforms, with higher CAC burden associated with reduced complexity [6].
Machine Learning Model Development Protocol
The application of machine learning to pulse wave analysis follows a structured pipeline:
Feature Engineering: Initial pulse wave features undergo selection based on univariate associations with CAC scores. Highly correlated features (r > 0.8) are removed to minimize multicollinearity. Feature importance is ranked using random forest or XGBoost intrinsic metrics [8] [6].
Model Architecture: Gradient Boosting Decision Tree (GBDT) models are implemented with nested cross-validation to optimize hyperparameters. The typical architecture includes 100-500 estimators, maximum depth of 3-6, and learning rate of 0.01-0.1 [6].
Validation Framework: Models are evaluated using fivefold cross-validation with strict separation of training and validation sets. Performance metrics include area under the receiver operating characteristic curve (AUC-ROC), accuracy, sensitivity, specificity, and F1-score [8] [6].
Clinical Implementation: Successful models are tested on independent validation cohorts with different demographic characteristics to assess generalizability. The output typically provides both binary classification (high CAC vs. low CAC) and continuous risk prediction [8].
Research Reagents and Experimental Toolkit
Essential Research Materials and Instruments
Table 3: Research Toolkit for Pulse Wave Analysis
| Category | Specific Tool/Instrument | Research Function | Key Specifications |
|---|---|---|---|
| Pulse Wave Acquisition | SphygmoCor System (AtCor Medical) | Applanation tonometry for central hemodynamics | Central pressure waveforms, augmentation index |
| Vascular Explorer (Enverdis) | Oscillometric PWV measurement | Multi-site PWV (aortic, carotid-femoral, brachial-ankle) | |
| VP-1000 System (OMRON) | Automated baPWV measurement | Simultaneous brachial and tibial waveform capture | |
| Computational Analysis | Dr. Wise AI-Assisted Diagnosis System | Automated pulse wave feature extraction | Volumetric analysis, threshold-based segmentation |
| Scikit-learn Python Library | Machine learning implementation | GBDT, random forest, SVM algorithms | |
| Validation Reference | Multi-detector CT (MDCT) | CAC quantification gold standard | Agatston scoring protocol, ECG-gated acquisition |
Performance Comparison of Pulse Wave Analysis Techniques
Diagnostic Accuracy Across Methodologies
Different pulse wave analysis approaches demonstrate varying capabilities for detecting coronary artery calcification, with machine learning-enhanced methods showing particular promise.
Table 4: Performance Comparison of Pulse Wave Analysis Methods for CAC Detection
| Methodology | Study Population | Accuracy Metrics | Advantages | Limitations |
|---|---|---|---|---|
| PWV-based Classification | Community cohort (n=2,920) [12] | OR 1.48-2.69 per SD for CAC | Strong prognostic value | Requires multiple measurement sites |
| Pulse Wave ML (GBDT) | ESRD patients (n=58) [6] | 84.1% accuracy, 0.962 AUC | Superior in younger patients [8] | Single-center validation |
| Pulse Wave ML (Multiple Algorithms) | CKD patients (n=124) [8] | >80% balanced accuracy | Non-invasive, cost-effective | Limited to high-risk population |
| baPWV Quartile Analysis | Health screening (n=1,124) [13] | OR 2.14 for CAC progression | Simple measurement | Moderate accuracy alone |
Age-Stratified Performance
The performance of pulse wave analysis techniques varies significantly across age groups, with machine learning approaches demonstrating particular utility in younger populations. In patients under 50 years old, pulse wave-based classifiers show superior sensitivity compared to traditional risk factor-based models [8]. This enhanced performance in younger cohorts suggests that functional arterial assessment may detect early vascular changes before advanced calcification develops.
The relationship between arterial stiffness and CAC also demonstrates age-dependent patterns, with stronger associations observed in younger individuals from the Framingham Third Generation Cohort compared to the older Offspring Cohort [12]. This effect modification by age underscores the importance of considering life-course vascular changes when interpreting pulse wave parameters.
The systematic analysis of pulse morphology provides a non-invasive window into coronary artery health, with particular value for early risk stratification. Machine learning-enhanced pulse wave analysis demonstrates performance characteristics that suggest potential clinical utility, especially in younger populations and high-risk groups where traditional risk factors may lack sensitivity. The integration of functional arterial assessment with morphological evaluation creates a comprehensive vascular profiling approach that may enhance personalized cardiovascular risk prediction and monitor response to therapeutic interventions across the cardiovascular disease spectrum.
Coronary Artery Calcification (CAC) is a well-established marker of atherosclerosis and cardiovascular risk. The emergence of pulse wave analysis, enhanced by machine learning, presents a promising frontier for the non-invasive assessment of CAC severity. This guide objectively compares the performance of this novel approach against traditional imaging, framing the discussion within the broader thesis of validating pulse wave-driven machine learning for CAC detection. For researchers and drug development professionals, understanding these morphological patterns and the experimental data supporting them is crucial for advancing diagnostic technologies and therapeutic interventions. Recent studies demonstrate that specific, quantifiable changes in pulse wave morphology are directly associated with increasing CAC severity, enabling machine learning models to achieve classification accuracy exceeding 80% [6] [7] [14].
Comparative Performance of Pulse Wave Analysis vs. Traditional CAC Assessment
The following table summarizes the key performance metrics of pulse wave-driven machine learning models in detecting CAC severity, based on recent experimental studies.
Table 1: Performance Comparison of Pulse Wave-Based ML Models for CAC Assessment
| Study and Patient Population | Key Pulse Wave Features Utilized | Machine Learning Model | Classification Task | Key Performance Metrics |
|---|---|---|---|---|
| ESRD patients on hemodialysis (N=58) [6] [7] [14] | Waveform morphology (NA, NB, NC, PB, PC), descending limb parameters, complexity/distribution features. | Gradient Boosting Decision Tree (GBDT) | 4-class severity (No, Mild, Moderate, Severe CAC) | Accuracy: 84.1% (cross-val), Macro-AUC: 0.962; excelled in identifying Severe cases. |
| CKD stage 5 patients (N=124) [8] [15] | Morphological pulse wave features from radial and brachial arteries. | Not Specified (Pulse wave-based classifier) | Binary (High CAC ≥100 Agatston units) | Balanced Accuracy: >80%; superior sensitivity in patients <60 years old. |
| Multi-center study (N=348) [16] | Harmonic differences (e.g., |ΔC10|, |ΔD9|, ΔP1CV) between left and right hands. | Logistic Regression | Binary (SYNTAX score ≥22) | AUC: 0.89 (Males), AUC: 0.92 (Females) |
The data indicates that pulse wave analysis is particularly effective in stratified risk assessment. The model tested on ESRD patients demonstrated robust performance across four distinct levels of CAC severity [6] [14], while the approach also showed high balanced accuracy for binary classification of high-risk CAC in a CKD population [8]. A key advantage is its enhanced sensitivity in younger patient cohorts, where traditional risk factors may be less indicative [8] [15].
Characteristic Pulse Wave Morphological Patterns
The association between pulse wave morphology and CAC severity is not random; it follows a distinct, observable pattern. The quantifiable features underlying these morphological changes are detailed in the table below.
Table 2: Characteristic Pulse Wave Morphological Changes Associated with Increasing CAC Severity
| Morphological Feature | Description of Change with Increasing CAC Severity | Physiological Correlation |
|---|---|---|
| Tidal/Dicrotic Wave | Becomes progressively attenuated and less distinguishable from the main wave [6] [14]. | Increased arterial stiffness and altered wave reflections due to vascular calcification [6]. |
| Overall Waveform Contour | Evolves into a smoother morphology with a less defined diastolic phase [6] [14]. | Reduced vascular compliance and damping of secondary waves. |
| Specific Parameter: NB | Significantly increases in Mild/Moderate groups vs. No Calcification group [14]. | Directly associated with the hemodynamic impact of calcification. |
| Specific Parameter: PB | In Severe Calcification group, becomes significantly higher than in Mild/Moderate groups during HD [14]. | Indicates a shift in the timing and magnitude of reflected waves. |
| Left-Right Harmonic Differences | Harmonic indices (e.g., amplitude, energy, phase) show greater asymmetry between hands [16]. | Suggests that localized coronary lesions create detectable, asymmetrical effects on systemic circulation. |
The progression of these patterns is systematic. In individuals without significant CAC, the pulse waveform displays a well-defined main wave followed by clear tidal and dicrotic waves [6]. As CAC burden increases, these secondary waves begin to merge closer to the main wave and diminish in amplitude, leading to a smoother, more monolithic waveform contour, which is especially pronounced in cases of severe calcification [6] [14].
Detailed Experimental Protocols
Patient Recruitment and Data Acquisition
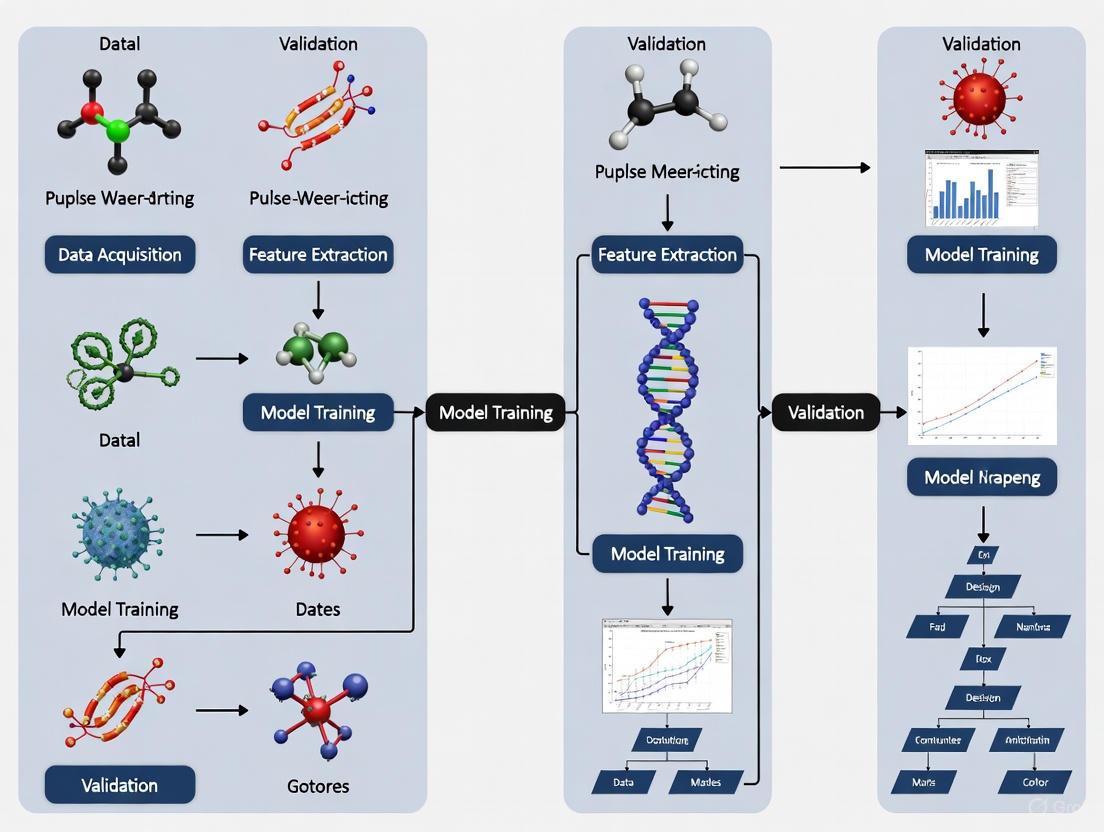
The following workflow diagram outlines the standard experimental protocol for pulse wave-based CAC assessment.
Key Steps in the Experimental Workflow:
Cohort Selection: Studies typically focus on high-risk populations, such as patients with End-Stage Renal Disease (ESRD) undergoing hemodialysis [6] [14] or those with Chronic Kidney Disease (CKD) [8] [15]. Participants are enrolled with informed consent under Institutional Review Board (IRB)-approved protocols.
Ground Truth Assessment: The severity of CAC is definitively classified using computed tomography (CT) scans. The Agatston score is the clinical gold standard, with studies often using a four-tier classification: No calcification (0), Mild (1-100), Moderate (101-400), and Severe (>400 Agatston units) [6] [17] [14].
Pulse Wave Recording: Pulse wave signals are non-invasively recorded using devices like the SphygmoCor system (AtCor Medical) [8] [15] or similar hardware. Signals are typically captured from the radial or brachial artery at a high sampling rate. In studies involving hemodialysis patients, recordings may be taken at multiple time points before, during, and after dialysis to track dynamic changes [6] [14].
Signal Processing and Feature Extraction: The raw pulse wave signals are pre-processed (e.g., filtered, normalized). Subsequently, a wide array of features is extracted. These can be broadly categorized into:
- Morphological Parameters: Quantifying the amplitude and timing of the main wave, tidal wave, and dicrotic wave (e.g., NA, NB, PC) [14].
- Complexity and Distribution Features: Reflecting the signal's entropy and statistical properties.
- Harmonic Features: Obtained via Fourier transform to decompose the waveform into its constituent frequencies [16].
- Left-Right Difference Metrics: Calculating the absolute difference in harmonic indices between the two hands [16].
Machine Learning Model Development
The processed data is then used to train predictive models.
Model Selection: Commonly used algorithms include Gradient Boosting Decision Trees (GBDT) [6] [14] and Logistic Regression [16]. GBDT is often favored for its ability to model complex, non-linear relationships between multiple features.
Training and Validation: The dataset is split into training and testing sets. Model performance is rigorously evaluated using k-fold cross-validation (e.g., fivefold) to ensure generalizability and to avoid overfitting. Final model performance is reported on a held-out independent test set [6] [14].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Pulse Wave CAC Research
| Item / Solution | Function / Description | Example from Literature |
|---|---|---|
| Pulse Wave Acquisition System | Non-invasively captures high-fidelity arterial waveform signals. | SphygmoCor system (AtCor Medical) [8] [15]. |
| LDCT/CT Scanner | Provides the ground truth Agatston score for CAC severity classification. | Low-Dose Computed Tomography (LDCT) [6]. |
| Signal Processing Software | For pre-processing, feature extraction, and harmonic analysis of pulse waves. | Custom scripts in Python/MATLAB for Fourier analysis [16]. |
| Machine Learning Framework | Provides environment for developing and training predictive models (GBDT, etc.). | Common frameworks like Scikit-learn, XGBoost, or TensorFlow. |
| Harmonic Analysis Algorithm | Decomposes pulse wave into harmonics to quantify energy and phase differences. | Fourier transform for 0th to 11th harmonics [16]. |
The evidence confirms that specific morphological patterns in pulse waves are systematically associated with the severity of Coronary Artery Calcification. The progressive attenuation of tidal waves and smoothing of the overall waveform contour provide a physically interpretable signature of increasing arterial stiffness and calcific burden. When these morphological features are leveraged by machine learning models—primarily Gradient Boosting Decision Trees—the resulting tools demonstrate high diagnostic performance, with accuracy exceeding 80% and AUC values above 0.96 in multi-class severity assessment. This methodology validates the thesis that pulse wave-driven machine learning is a robust, non-invasive, and cost-effective strategy for CAC detection and risk stratification, offering a compelling alternative to traditional CT-based screening, especially in high-risk and younger patient populations.
Coronary artery calcification (CAC) is a well-established marker of atherosclerosis and cardiovascular disease, with its presence and severity directly correlated with increased risk of major adverse cardiac events. The accurate detection and quantification of CAC is therefore crucial for risk stratification and clinical decision-making. The current clinical gold standard for CAC assessment, the Agatston score, is derived from electrocardiogram (ECG)-gated computed tomography (CT) scans. However, this and other established imaging modalities present significant limitations that hinder their utility for widespread screening and frequent monitoring, creating an urgent need for alternative approaches. This review objectively compares the performance of current gold-standard CAC detection methods against emerging alternatives, with a specific focus on validating pulse wave-driven machine learning as a non-invasive screening tool. By examining the technical constraints, clinical applicability, and performance metrics of each approach, we provide a framework for researchers and drug development professionals to evaluate the next generation of CAC detection technologies.
Limitations of Current Gold-Standard CAC Detection Methods
Current modalities for detecting vascular calcification, while clinically valuable, face persistent limitations that affect their sensitivity, specificity, and practical implementation.
Table 1: Performance Comparison of Current CAC Detection Modalities
| Modality | Spatial Resolution | Key Limitations | Clinical Utility |
|---|---|---|---|
| ECG-Gated CT | >400 µm (clinical systems) [18] | Radiation exposure, high cost, limited access, cannot detect microcalcifications (<50 µm) [6] [18] [19] | Gold standard for Agatston scoring; excellent for macrocalcification detection [19] |
| Non-ECG-Gated CT | >400 µm (clinical systems) [18] | Motion artifacts, overestimation of calcification volume (blooming artefacts), overlap in attenuation between iodine contrast and calcification [18] [20] | Suitable for screening; prognostic value for cardiovascular and non-cardiovascular events [20] |
| Na[18F]F PET | 4-5 mm (clinical systems) [18] | Cannot differentiate between physiological and pathological calcification; low specificity; requires hybrid imaging (CT/MRI) for anatomy [18] | Detects active microcalcification sites; high target-to-background ratio [18] |
| Intravascular Ultrasound (IVUS) | ~100 µm [18] | Invasive procedure; unable to penetrate calcium to measure thickness; detects only macrocalcifications [18] | Near-histology quality images of vascular wall and plaque; used in specialized catheterization procedures [18] |
A critical limitation across all conventional imaging techniques is the inability to reliably detect microcalcifications (calcifications with a diameter below 50 µm), which are a key indicator of plaque instability and increased rupture risk [18]. Although preclinical CT systems can achieve resolutions of up to 1 µm, clinical CT systems, including the novel photon-counting CT, lack the spatial resolution to identify these early, high-risk calcification events [18]. This represents a significant diagnostic gap, as the identification of microcalcifications could allow for interventions at a stage where plaque stability can still be modulated [18].
Furthermore, issues of cost, accessibility, and patient burden are pronounced. ECG-gated CT scans, while precise, are performed less frequently (approximately 0.5 million per year in the U.S.) compared to non-ECG-gated chest CT scans (10.6 million per year), and face greater challenges with insurance coverage [19]. The necessity for iodine-based contrast agents in diagnostic images and the associated radiation exposure further limit the feasibility of CT for routine, repeated screening [18] [19].
Experimental Protocols for Current and Emerging Methods
Protocol for Agatston Scoring via ECG-Gated CT
The traditional Agatston method quantifies CAC through a manual-to-semi-automated process on non-contrast, ECG-gated CT scans [19]. The protocol involves:
- Image Acquisition: A non-contrast CT scan is performed with prospective ECG-gating to capture images during diastole, minimizing cardiac motion artifacts.
- Voxel Identification: Software automatically identifies voxels within the coronary arteries with an attenuation greater than 130 Hounsfield Units (HU), a threshold set to distinguish calcium from surrounding tissues.
- Area and Weighting Calculation: The area of all qualifying voxels is calculated. Each calcified area is then multiplied by a density weighting factor (1-4) based on its peak HU value.
- Score Calculation: The Agatston score is the sum of these weighted calcium scores across all coronary arteries. Patients are stratified into risk categories: 0 (very low), 1-99 (mild), 100-299 (moderate), 300-399 (moderate to severe), and ≥400 (severe) [6] [19].
Protocol for AI-Driven CAC Scoring on Non-ECG-Gated CT
Artificial intelligence, particularly deep learning, is being applied to overcome the limitations of ECG-gated scans by leveraging the more abundant non-ECG-gated chest CTs [19]. A typical protocol involves:
- Data Curation: A large dataset of non-ECG-gated chest CT scans is assembled, often retrospectively.
- Model Training: A Convolutional Neural Network (CNN), a type of deep learning model, is trained on this dataset. The model is taught to identify and quantify coronary calcium deposits.
- Validation: The AI-generated CAC scores are validated against the reference standard of ECG-gated CT Agatston scores.
- Outcome Correlation: The model's performance is further assessed by correlating its scores with clinical outcomes, such as major adverse cardiac events. Studies have shown that AI-generated scores from non-gated CTs maintain strong agreement with manual methods and support effective risk stratification [19].
Protocol for Pulse Wave-Driven Machine Learning Assessment of CAC
Emerging as a radically non-invasive and cost-effective alternative, pulse wave analysis uses machine learning to infer CAC severity from arterial waveform characteristics [6] [8]. A representative study protocol is as follows:
- Patient Enrollment & Reference Standard: A cohort (e.g., 58 patients with end-stage renal disease) is enrolled. CAC severity is definitively classified using low-dose CT (LDCT) into categories (e.g., 0, 1-100, 101-400, >400 Agatston units) [6].
- Pulse Wave Acquisition: Radial artery pulse waveforms are recorded non-invasively over a period, for instance, before, during, and after hemodialysis, using a device like the SphygmoCor system [6] [8].
- Feature Extraction: Key morphological features are extracted from the pulse waveforms. These include parameters related to the waveform's morphology (e.g., attenuation of tidal waves), descending limb, complexity, and distribution [6]. With increasing CAC severity, the tidal waves become progressively attenuated, resulting in a smoother overall waveform [6].
- Model Training and Validation: A Gradient Boosting Decision Tree (GBDT) model is trained using the extracted pulse wave features to classify CAC severity. The model's performance is evaluated using fivefold cross-validation and an independent test set [6]. One study achieved an average accuracy of 84.1% and a macro-AUC of 0.962, demonstrating robust performance, particularly in identifying severe calcification cases [6]. Another study focusing on high CAC (≥100) reported a balanced accuracy exceeding 80% [8].
The following diagram illustrates the workflow of this experimental protocol.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Research Materials for Pulse Wave-Driven CAC Detection Studies
| Item | Function/Application | Example/Notes |
|---|---|---|
| SphygmoCor System | Non-invasive acquisition of radial artery pulse waveforms [8]. | A commercial device for applanation tonometry and pulse wave analysis. |
| Low-Dose CT (LDCT) | Provides the reference standard Agatston score for model training and validation [6]. | Used to classify patients into CAC severity groups. |
| Gradient Boosting Decision Tree (GBDT) | A machine learning algorithm that builds an ensemble of decision trees for classification tasks [6]. | Used to correlate pulse wave features with CAC severity. |
| Pulse Wave Features | Quantitative parameters extracted from the waveform signal used as model input [6]. | Includes morphology, descending limb, complexity, and distribution parameters. |
| Convolutional Neural Network (CNN) | A class of deep learning neural networks used for automated analysis of medical images [19]. | Applied for direct CAC scoring on non-ECG-gated CT scans. |
The current gold-standard methods for CAC detection, while foundational to cardiovascular risk assessment, are constrained by significant limitations in detecting early-stage microcalcifications, issues of cost, accessibility, and patient safety. The validation of emerging technologies, particularly pulse wave-driven machine learning, demonstrates a promising paradigm shift. The experimental data confirms that this non-invasive approach can classify CAC severity with high accuracy (exceeding 80% balanced accuracy and AUC of 0.962), offering a viable, cost-effective, and repeatable screening tool. For researchers and drug development professionals, this technology not only presents a new avenue for early patient identification and risk stratification but also opens the possibility of frequent monitoring of CAC progression or regression in response to therapeutic interventions, a capability that was previously impractical with traditional imaging modalities.
Building a Predictive Model: From Signal Acquisition to Machine Learning Algorithm
The accurate acquisition and preprocessing of radial artery waveforms represent a critical foundation for advancing cardiovascular diagnostic research, particularly in the validation of non-invasive biomarkers for coronary artery calcification (CAC). Coronary artery calcification, a well-established marker of atherosclerotic burden and a powerful predictor of cardiovascular events, has traditionally been assessed using computed tomography (CT) [4] [21]. However, CT screening is costly, resource-intensive, and impractical for large-scale population use, motivating the search for alternative, more accessible modalities [22]. The radial artery pulse waveform contains rich physiological information regarding vascular stiffness, cardiac function, and hemodynamic properties that may correlate with coronary artery health [23] [24]. This guide systematically compares the performance, technical specifications, and implementation requirements of contemporary radial artery signal acquisition technologies, providing researchers with objective data to inform their experimental designs for pulse wave-driven machine learning applications.
Comparative Analysis of Acquisition Modalities
The selection of an appropriate sensing modality represents the first critical decision in establishing a radial artery acquisition protocol. Current technologies can be broadly categorized into pressure-based sensor arrays, optical systems, and hybrid approaches, each with distinct operational characteristics and performance trade-offs.
Table 1: Quantitative Comparison of Radial Artery Acquisition Modalities
| Acquisition Modality | Spatial Resolution | Temporal Resolution | Key Measurable Parameters | Signal Quality Indicators |
|---|---|---|---|---|
| MEMS Pressure Sensor Array [23] | 0.65 mm pitch, 18 sensors spanning 11.6 mm | Not explicitly stated | 3D pulse envelope, pulse width, dynamic pulse width, pulse wave velocity (PWV) | High linearity (±0.1% FS), low hysteresis (0.15% FS), validated against Doppler ultrasound |
| Fabry-Perot Interferometry [25] | Sub-micrometer displacement sensitivity | Limited by sensor bandwidth and interpolation methods | Arterial pulse waveform (APW), phase dynamics, rate of change | Robust to artifacts, provides complete morphological waveform |
| Multimodal FCG-PPG Sensor [26] | Single measurement site | Simultaneous mechanical-optical acquisition | PW morphology, derivatives, time delay between mechanical and optical signals | Normalized cross-correlation >0.98 between modalities |
| Piezoelectric Tonometry [26] | Single point measurement | Suitable for wearable monitoring | PW morphology, pulse transit time (PTT) | Does not require artery applanation |
Table 2: Technical Implementation Requirements and Limitations
| Modality | Skin Contact Requirement | Calibration Complexity | Subject Discomfort | Key Limitations |
|---|---|---|---|---|
| MEMS Pressure Sensor Array [23] | Direct contact, finger-worn by practitioner | Requires specialized calibration | Minimal when worn by practitioner | complex fabrication, system integration |
| Fabry-Perot Interferometry [25] | Applanation tonometry required | Python-based processing pipeline | Moderate due to applanation | Signal ambiguity at turning points, exceeds λ/4 amplitude |
| Multimodal FCG-PPG Sensor [26] | Direct contact at fingertip | Requires synchronization of dual sensors | Minimal, wearable design | Unexplained delay between optical/mechanical signals |
| Piezoelectric Tonometry [26] | Direct contact, no applanation | Frequent recalibrations needed | Low, suitable for long-term monitoring | Less stable than pressure sensors for quantitative measurements |
Experimental Protocols for Key Methodologies
MEMS Pressure Sensor Array Fabrication and Deployment
The ultra-dense MEMS pressure sensor array protocol employs 18 miniature silicon piezoresistive pressure sensors (0.4 mm × 0.4 mm each) packaged on a flexible printed circuit board with a 0.65 mm pitch, creating an effective sensing span of 11.6 mm—3–5 times the diameter of the typical radial artery [23].
Implementation Workflow:
- Sensor Fabrication: Fabricate sensors using a microhole inter-etch and sealing (MIS) process creating beam-island-reinforced structures for high sensitivity (108 mV/3.3 V) and linearity
- Array Assembly: Attach sensors to FPC substrate with precise positional alignment and connect via wire bonding
- Environmental Protection: Coat bonding wires with stiff epoxy resin for reliability while removing material between sensors to maintain flexibility
- Signal Acquisition: Position array over radial artery at inch, bar, and cubit points; record simultaneously from all 18 channels while applying three pressure levels (superficial, medium, deep)
- Data Processing: Construct 3D pulse envelope images from spatial-temporal data; calculate pulse width and dynamic pulse width through envelope analysis
This protocol enables direct measurement of pulse wave velocity by calculating the pulse transit time between the brachial and radial arteries using the same sensor arrays [23].
Fabry-Perot Interferometric Signal Processing Pipeline
The interferometric approach captures arterial pulsation through precise optical path length changes in a low-finesse Fabry-Perot cavity, requiring specialized processing to reconstruct the arterial pulse waveform [25].
Processing Protocol:
- Signal Acquisition: Obtain interferometric time-domain signals from Fabry-Perot sensor applied with applanation tonometry at radial artery
- Preprocessing: Implement outlier removal followed by Butterworth high-pass filtering to eliminate baseline drift
- Normalization: Apply min-max normalization to standardize signal amplitude across subjects and sessions
- Feature Extraction: Calculate rate of change and its Hilbert transform to identify signal envelope and critical points
- Breakpoint Detection: Employ interactive refinement to identify phase change points, constrained by physiological boundaries (even number of breakpoints per cardiac cycle)
- Waveform Reconstruction: Reconstruct arterial pulse waveform from processed interferometric signal using segmented approach
The complete Python-based processing pipeline is publicly available as open-source code, enhancing reproducibility and community development [25].
Multimodal Finger Pulse Wave Sensing
This protocol enables simultaneous mechanical and optical pulse wave acquisition from the same measurement site, providing complementary data streams for enhanced parameter extraction [26].
Experimental Protocol:
- Sensor Integration: Co-locate piezoelectric Forcecardiography (FCG) and photoplethysmography (PPG) sensors in a single housing unit
- Signal Synchronization: Implement hardware or software synchronization to ensure temporal alignment of FCG and PPG data streams
- Data Acquisition: Record finger pulse waves simultaneously from both modalities under resting conditions
- Signal Processing: Apply inversion to PPG light intensity signal; normalize both signals; calculate first and second derivatives
- Cross-Modal Analysis: Compute normalized cross-correlation between FCG and PPG waveforms and their derivatives
- Parameter Extraction: Identify fiducial points in original and derivative signals for morphological parameter calculation
This approach reveals an consistent but unexplained time delay between mechanical (FCG) and optical (PPG) pulse wave signals, highlighting the complex biomechanics of pulse propagation [26].
Visualization of Experimental Workflows
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Critical Components for Radial Artery Waveform Research
| Component | Specification/Function | Representative Examples |
|---|---|---|
| MEMS Pressure Sensors [23] | Ultra-small (0.4 mm × 0.4 mm) piezoresistive sensors with high sensitivity (108 mV/3.3 V) | Beam-island reinforced silicon sensors fabricated via MIS process |
| Flexible Printed Circuit Boards [23] | Flexible substrate for sensor integration while maintaining anatomical conformity | Custom FPC with 0.65 mm pitch for 18-sensor array |
| Fabry-Perot Interferometer [25] | Low-finesse optical cavity for precise displacement measurement via phase modulation | Fiber-optic FPI with elastic membrane for applanation tonometry |
| Multimodal Sensor Housing [26] | Integrated mechanical structure for co-locating FCG and PPG elements | Custom housing with piezoelectric FCG and reflective PPG sensors |
| Signal Processing Libraries [25] | Python-based tools for filtering, normalization, and feature extraction | Public GitHub repository: FPI-Pulse-Waveform-Extraction |
| Validation Instrumentation [23] | Reference standard for protocol validation | Color Doppler ultrasound for dynamic pulse width measurement |
The methodological comparison presented in this guide demonstrates significant trade-offs between spatial resolution, implementation complexity, and quantitative accuracy across radial artery acquisition modalities. For machine learning applications targeting coronary artery calcification detection, the MEMS pressure sensor array provides superior spatial characterization of pulse propagation phenomena, which may encode information about coronary vascular health [23]. The Fabry-Perot interferometric approach offers high precision for waveform morphology analysis, while multimodal sensing captures complementary physiological relationships [25] [26]. Researchers should select acquisition protocols based on specific feature requirements for their predictive models, considering that pulse wave velocity and specific morphological features have demonstrated associations with vascular stiffness and coronary artery disease progression [27] [24]. As pulse wave-driven machine learning advances, standardized acquisition and preprocessing protocols will be essential for developing robust, generalizable models for non-invasive coronary artery calcification assessment.
Within the rapidly evolving field of cardiovascular informatics, the validation of pulse wave-driven machine learning (ML) for detecting coronary artery calcification (CAC) represents a critical research frontier. CAC, the deposition of calcium in coronary artery walls, is a definitive marker of atherosclerosis and a powerful predictor of cardiovascular events. The current diagnostic gold standard, computed tomography (CT) for CAC scoring, involves radiation exposure and significant cost, limiting its suitability for widespread screening [6] [28]. Consequently, non-invasive, cost-effective alternatives are urgently needed.
Pulse wave analysis has emerged as a promising non-invasive methodology for cardiovascular assessment. The central thesis of this approach posits that the morphological, temporal, and complexity parameters embedded within pulse wave signals contain rich information about arterial stiffness, endothelial function, and the hemodynamic alterations caused by vascular calcification [6] [29] [28]. The validation of pulse wave-driven ML models hinges on the rigorous engineering of these features to create robust, generalizable tools for CAC detection. This guide provides a comparative analysis of the feature categories and experimental protocols that underpin this innovative research domain.
Comparative Analysis of Pulse Wave Feature Categories
The utility of pulse wave signals for machine learning depends on the extraction of informative features. These parameters can be broadly categorized into morphological, temporal, and complexity-based features, each offering distinct insights into cardiovascular physiology.
Table 1: Comparison of Primary Pulse Wave Feature Categories for CAC Detection
| Feature Category | Description | Key Parameters | Physiological Correlation | Advantages |
|---|---|---|---|---|
| Morphological Features | Describe the shape and amplitude characteristics of the pulse waveform [6] [30]. | Main wave amplitude, tidal wave, dicrotic wave, pulse area, Smoothness, number of local extrema (#Extrema) [6] [30]. | Vascular elasticity, peripheral resistance, left ventricular function, wave reflections [6]. | Directly reflects structural and functional vascular status; features are often intuitively understandable. |
| Temporal Features | Pertain to time intervals within the cardiac cycle or between pulse waves. | Pulse Transit Time (PTT), Pulse Wave Velocity (PWV), Upstroke Time (UT), heart rate [29] [28] [31]. | Arterial stiffness; faster PWV indicates stiffer arteries [28]. | Strong, established correlation with arterial stiffness; relatively straightforward to measure. |
| Complexity Features | Quantify the irregularity, variability, or "jaggedness" of the signal over time [29] [30]. | Entropy, Higuchi Fractal Dimension (HFD), Root Mean Square (RMS), Autocorrelation Function (ACF) [29] [30]. | Overall state of the cardiovascular regulatory system; reduced complexity may indicate pathology. | Captures non-linear dynamics not apparent from shape or timing alone; can improve model stability in ambulatory settings [29]. |
Insights from Comparative Performance
Morphological features demonstrate high clinical relevance, as specific waveform alterations are directly observable with increasing CAC severity. For instance, the tidal wave becomes progressively attenuated and less distinguishable in severe calcification, resulting in a smoother overall waveform [6]. Concurrently, parameters like Smoothness increase and #Extrema decrease, indicating a loss of waveform complexity [30].
Temporal features, particularly PWV, provide a well-validated measure of arterial stiffness, which has a pathophysiological link to atherosclerosis. A study of 986 Japanese men established a clear association, with the prevalence of CAC rising from 20.6% in the lowest baPWV quartile to 66.7% in the highest [32]. The optimal baPWV cutoff for detecting CAC was identified as 1612 cm/s [32].
Complexity features add a crucial dimension to the feature set. Research indicates that parameters like HFD and ACF maintain significant contributions to blood pressure estimation even during high cardiac output fluctuations, whereas morphological features may become less reliable under such unstable hemodynamic conditions [29]. This suggests that complexity features can enhance model robustness.
Experimental Protocols for Feature-Driven ML Model Validation
The validation of ML models for CAC detection requires meticulously designed experiments. The following protocols detail the methodologies from key studies in the field.
Protocol 1: Radial Artery Pulse Wave Analysis for CAC Severity Stratification
This protocol is designed to extract features from radial artery waveforms to classify CAC severity in high-risk patients [6].
- Objective: To evaluate the utility of radial artery pulse waveform features for the non-invasive assessment of CAC severity in patients with end-stage renal disease (ESRD) undergoing hemodialysis.
- Patient Cohort: 58 patients with ESRD. CAC severity was assessed via low-dose CT and classified into four groups using Agatston scores: no calcification (0), mild (1–100), moderate (101–400), and severe (>400) [6].
- Signal Acquisition: Radial artery pulse waveforms were recorded non-invasively before, hourly during, and after a hemodialysis session.
- Feature Extraction: A comprehensive set of features was extracted based on observed morphological differences among the CAC groups. This included parameters related to:
- Waveform morphology (e.g., main wave, tidal wave)
- Descending limb characteristics
- Signal complexity and distribution
- Mean values
- Full-process stereoscopic pulse wave features [6]
- Model Training and Validation: A Gradient Boosting Decision Tree (GBDT) model was trained using the extracted waveform features. Model performance was evaluated using fivefold cross-validation and an independent test set [6].
Protocol 2: Photoplethysmography (PPG) Complexity Analysis for Hemodynamic Assessment
This protocol uses model-based simulation to interpret the temporal complexity of PPG signals and its relationship to blood pressure, a key hemodynamic parameter [29].
- Objective: To interpret stochastic PPG patterns via simulation and optimize BP estimation algorithms by understanding the physiological implications of temporal complexity.
- Simulation Framework: A modified four-element Windkessel (WK4) model was used, incorporating blood pressure-dependent compliance profiles. This model simulates PPG responses to pulse and continuous stimuli at various timescales [29].
- Complexity Quantification: The temporal complexity of the simulated and real PPG signals was quantified using:
- Higuchi Fractal Dimension (HFD): Measures the fractal dimension of a time series signal.
- Autocorrelation Function (ACF): Assesses the correlation of a signal with a delayed copy of itself over time [29].
- Experimental Validation: Continuous recordings of BP, PPG, and stroke volume from 40 healthy subjects were used to validate the simulation results. The contribution of HFD and ACF to BP estimation was calculated and compared against traditional morphological features [29].
Protocol 3: Pulse Wave-Based Screening for High CAC in CKD Patients
This protocol compares the effectiveness of pulse wave features against traditional risk factors for identifying high CAC scores [8] [15].
- Objective: To investigate a pulse wave analysis and ML approach for identifying CKD patients at high risk for coronary atherosclerosis (CAC ≥ 100 Agatston units) [8] [15].
- Study Population: Retrospective data from 124 patients with CKD stage 5 who underwent kidney transplantation.
- Data Collection:
- Model Development: Two ML models were developed and compared:
- Performance Analysis: Model performance was assessed based on balanced accuracy, sensitivity, and specificity, with particular attention to performance across different age groups [8] [15].
Performance Benchmarking of Feature-Based ML Models
Quantitative results from implemented studies demonstrate the efficacy of feature-engineered ML models for CAC detection and related cardiovascular assessment.
Table 2: Performance Metrics of Pulse Wave Feature-Based Machine Learning Models
| Study Focus | Model Type | Key Features Used | Performance Metrics | Comparative Insight |
|---|---|---|---|---|
| CAC Severity Stratification in ESRD [6] | Gradient Boosting Decision Tree (GBDT) | Morphological, descending limb, complexity, and distribution features from radial pulse waves. | Avg. Accuracy: 84.1%Macro-AUC: 0.962 (5-fold CV)Test Set Accuracy: 83.9%Test Set AUC: 0.961 | Model performed particularly well in identifying "Severe Calcification" cases. |
| High CAC Screening in CKD [8] [15] | Pulse Wave-Based Classifier | Engineered features from SphygmoCor pulse wave signals. | Balanced Accuracy: >80%Superior sensitivity in patients <60 years old. | Outperformed a model based on Traditional Risk Factors (TRF), especially in younger patients. |
| AI in CT Angiography [33] | AI (Deep Learning) | Direct image features from CTA. | For Calcified Plaque Detection:Sensitivity: 0.93Specificity: 0.94AUC: 0.98 | Demonstrates the high performance of direct imaging but highlights the trade-off with cost/accessibility vs. non-invasive pulse wave. |
| PWV for CAC Detection [32] | Statistical Model | Brachial-ankle PWV (baPWV). | CAC Prevalence vs. baPWV Quartile: 20.6% to 66.7%.Optimal baPWV Cutoff: 1612 cm/s. | Provides a simple, validated threshold for a single temporal feature, useful for baseline screening. |
Signaling Pathways, Workflows, and Logical Frameworks
The following diagrams illustrate the core logical relationships and experimental workflows in pulse wave-driven feature engineering for CAC detection.
Pulse Wave to CAC Detection Logic
Feature Engineering and Validation Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the described experimental protocols requires specific tools and technologies. This table details key solutions used in the featured research.
Table 3: Essential Research Reagents and Solutions for Pulse Wave CAC Studies
| Tool / Solution | Type | Primary Function | Example Use Case |
|---|---|---|---|
| SphygmoCor System (AtCor Medical) [8] [15] | Hardware & Software | Non-invasive acquisition and analysis of arterial pulse waves, including central aortic waveforms. | Used for pulse wave signal collection in CKD patient studies for CAC screening [8] [15]. |
| Photoplethysmography (PPG) Sensor [29] [31] | Optical Sensor | Measures volumetric changes in peripheral blood circulation, providing a PPG waveform for analysis. | Fundamental for single-site, non-invasive BP estimation and complexity analysis studies [29] [31]. |
| Biopac PPG Systems [30] | Data Acquisition Hardware | High-fidelity recording of physiological signals, including PPG and ECG, often in research laboratory settings. | Used in controlled studies for recording continuous PPG signals from fingers with synchronized ECG [30]. |
| Four-Element Windkessel (WK4) Model [29] | Physiological Model | A lumped-parameter model of the arterial system used to simulate blood flow and pressure relationships. | Employed in in-silico simulations to generate dynamic PPG signals and interpret their relationship with BP [29]. |
| Gradient Boosting Decision Tree (GBDT) [6] | Machine Learning Algorithm | A powerful ensemble learning method that builds sequential decision trees to correct previous errors. | Achieved state-of-the-art performance (AUC >0.96) in classifying CAC severity from radial pulse wave features [6]. |
| Higuchi Fractal Dimension (HFD) [29] | Computational Algorithm | Quantifies the fractal dimension (complexity) of a time-series signal. | A key complexity feature used to quantify PPG temporal patterns and correlate them with hemodynamic states [29]. |
The accurate detection and assessment of coronary artery calcification (CAC) is a critical component of cardiovascular risk stratification. Recent advances in non-invasive methodologies, particularly those leveraging pulse wave analysis and machine learning (ML), have opened new avenues for early and efficient CAC detection. This guide provides an objective comparison of the performance of various ML algorithms, with a focused examination of Gradient Boosting Decision Trees (GBDT) and their variants, within the context of CAC detection research. We summarize quantitative experimental data, detail methodological protocols from key studies, and provide visualizations of core workflows to assist researchers and drug development professionals in selecting appropriate algorithms for their investigative needs.
Performance Comparison of Machine Learning Algorithms
The selection of an optimal machine learning algorithm is paramount for developing robust predictive models in healthcare. The table below summarizes the documented performance of various algorithms across different clinical prediction tasks, including coronary artery disease (CAD) and CAC detection.
Table 1: Comparative Performance of Machine Learning Algorithms in Cardiovascular Disease Prediction
| Algorithm | Application Context | Reported Performance Metrics | Reference / Study Details |
|---|---|---|---|
| Gradient Boosting Decision Tree (GBDT) | CAC Severity Classification from Pulse Waves | Accuracy: 84.1%, Macro-AUC: 0.962 (5-fold CV) | [34] [7] |
| Extreme Gradient Boosting (XGBoost) | CAD Risk Assessment from Clinical Features | AUC: 0.988 (Discovery), 0.953 (Validation) | [35] |
| XGBoost | PCI Success Prediction in CAC Patients | AUC: 0.984, F1-Score: 0.970 | [36] |
| Voting Ensemble | Geochemical Au Concentration Prediction (Methodological Reference) | Lower RMSE and MAPE vs. single models (GB, LR, DT) | [37] |
| Random Forest | General Purpose (Theoretical Framework) | High accuracy, robust to overfitting, handles missing data | [38] |
| Support Vector Machine (SVM) | General Purpose (Theoretical Framework) | Effective in high-dimensional spaces, versatile kernels | [35] [38] |
The data indicates that tree-based ensemble methods, particularly boosting algorithms like GBDT and XGBoost, consistently deliver high predictive accuracy in complex medical tasks. The GBDT model demonstrated particular proficiency in classifying CAC severity from pulse wave data, a non-invasive and clinically valuable approach [34]. Furthermore, the superior performance of XGBoost in two independent studies for CAD risk assessment and Percutaneous Coronary Intervention (PCI) success prediction underscores its robustness and generalizability across different cardiovascular endpoints [35] [36]. Ensemble methods like Voting classifiers have also been shown to outperform their constituent base models, highlighting the value of combining multiple algorithms to enhance predictive power [37].
Detailed Experimental Protocols in CAC Research
Pulse Wave-Driven Machine Learning for CAC Assessment
A pivotal study by Lyu et al. (2025) established a protocol for non-invasive CAC assessment using radial artery pulse waveforms [34] [7].
- Study Population and Data Acquisition: The study enrolled 58 patients with end-stage renal disease (ESRD) undergoing hemodialysis. CAC severity was quantified using low-dose computed tomography (LDCT) and categorized into four groups based on Agatston scores: no calcification (0), mild (1–100), moderate (101–400), and severe (>400). Radial artery pulse waveforms were recorded from each patient at multiple time points: before, hourly during, and after hemodialysis [34] [7].
- Pulse Wave Feature Extraction: A comprehensive set of features was extracted from the waveform morphology. These included parameters related to the waveform's shape (e.g., main wave, tidal wave), its descending limb characteristics, complexity and distribution metrics, mean value parameters, and "full-process stereoscopic" features capturing changes over the entire dialysis session. The study reported clear morphological differences across CAC groups; for instance, the tidal wave became progressively attenuated and less distinguishable with increasing CAC severity [34].
- Model Training and Evaluation: A Gradient Boosting Decision Tree (GBDT) model was trained to classify patients into the four CAC severity groups based on the extracted pulse wave features. The model's performance was rigorously evaluated using fivefold cross-validation, yielding an average accuracy of 84.1% and a macro-AUC of 0.962. These results were confirmed on an independent test set (83.9% accuracy, 0.961 macro-AUC), with the model performing exceptionally well in identifying cases of severe calcification [34] [7].
ML for PCI Success Prediction in Calcified Lesions
Another study prospectively developed ML models to predict the success of Percutaneous Coronary Interventions (PCI) in patients with moderate to severe CAC [36].
- Data Source and Cohort: The study utilized data from 3271 patients with moderate to severe CAC and 17,998 patients with no/mild calcification who underwent PCI between 2017 and 2018. An external validation cohort consisted of 204 patients from a general hospital [36].
- Feature Set and Model Development: Six machine learning models were developed and validated, including k-nearest neighbor, GBDT, XGBoost, Logistic Regression, Random Forest, and SVM. The models were trained on features derived from coronary angiography, encompassing vascular characteristics and procedural details. The Synthetic Minority Oversampling Technique (SMOTE) was applied to handle class imbalance [36].
- Model Performance and Interpretation: The XGBoost model demonstrated superior performance, achieving an Area Under the ROC Curve (AUC) of 0.984. Model interpretability was facilitated using Shapley Additive Explanations (SHAP), which identified the top predictive factors for PCI failure. These included lesion length, minimum lumen diameter, and thrommonary infarction (TIMI) flow grade [36].
Workflow and Algorithm Diagrams
Pulse Wave CAC Assessment Workflow
The following diagram illustrates the end-to-end experimental workflow for assessing coronary artery calcification using pulse wave-driven machine learning, as detailed in the research by Lyu et al. [34] [7].
Gradient Boosting Decision Tree (GBDT) Architecture
The diagram below outlines the core architecture and learning process of a Gradient Boosting Decision Tree, which forms the basis for algorithms like GBDT and XGBoost used in the cited studies [34] [39] [36].
The Researcher's Toolkit: Key Reagents and Materials
The following table catalogues essential materials and computational tools referenced in the experimental protocols for pulse wave-driven CAC machine learning research.
Table 2: Essential Research Reagents and Solutions for Pulse Wave CAC Studies
| Item Name | Function / Application in Research | Specification / Notes |
|---|---|---|
| Patient Cohort with ESRD | Primary study population for model development and validation | High prevalence of CAC provides a robust population for studying severity gradients. [34] [7] |
| Low-Dose Computed Tomography (LDCT) | Gold-standard imaging for CAC quantification and labeling. | Used to calculate Agatston scores for ground truth labels. [34] [7] |
| Radial Artery Pulse Wave Recorder | Non-invasive data acquisition of vascular waveform signals. | Device capable of capturing high-fidelity morphological waveforms. [34] |
| Pulse Wave Feature Extraction Software | Computational tool for deriving morphological parameters from raw waveforms. | Extracts key features (e.g., main wave, tidal wave characteristics). [34] |
| Gradient Boosting Framework (e.g., XGBoost, GBDT) | Core machine learning library for model construction. | Offers efficient implementation of boosted tree algorithms. [34] [35] [36] |
| SHAP (Shapley Additive Explanations) | Post-hoc model interpretability and feature importance analysis. | Critical for understanding model decisions in a clinical context. [35] [36] |
Coronary artery calcification (CAC) represents a significant cardiovascular risk factor, particularly in vulnerable populations such as patients with end-stage renal disease (ESRD) [6]. The accurate detection and stratification of CAC severity is crucial for early intervention and improved patient outcomes. Traditional computed tomography (CT)-based methods, while considered the clinical gold standard, pose issues related to radiation exposure, high costs, and limited accessibility for routine screening [6] [8]. In recent years, pulse wave analysis coupled with machine learning (ML) has emerged as a promising non-invasive alternative for CAC assessment. This review synthesizes recent performance benchmarks—including accuracy, area under the curve (AUC), and cross-validation results—from studies validating pulse wave-driven ML models for coronary artery calcification detection, providing researchers with a comprehensive comparison of this rapidly advancing field.
Performance Benchmarks of Pulse Wave-Driven ML Models for CAC Detection
Recent studies have demonstrated consistently strong performance of machine learning models utilizing pulse wave features for detecting and stratifying coronary artery calcification. The table below summarizes key performance metrics from pivotal studies in this domain.
Table 1: Performance Benchmarks of Pulse Wave-Driven ML Models for CAC Detection
| Study & Population | ML Model | Accuracy (%) | AUC | Cross-Validation | Key Performance Notes |
|---|---|---|---|---|---|
| ESRD patients on hemodialysis (N=58) [6] | Gradient Boosting Decision Tree (GBDT) | 84.1% (avg) | 0.962 (macro) | Fivefold | Robust performance on independent test set (83.9% accuracy, 0.961 AUC) |
| CKD stage 5 patients (N=124) [8] | Pulse wave-based classifier | >80% (balanced) | - | - | Superior to traditional risk factors, especially in patients <50 years |
| General CAD prediction [40] | Random Forest | 92% | - | Holdout validation | Outperformed clinical risk scores (71-73% accuracy) |
| SVM with RBF kernel | - | - | - | Superior to linear/polynomial SVM |
The consistency of high performance across these studies, with AUC values frequently exceeding 0.80 and accuracy above 80%, underscores the substantial potential of pulse wave-driven ML for CAC detection. The gradient boosting model demonstrated particular strength in identifying severe calcification cases [6]. Notably, pulse wave-based classifiers have shown superior balanced accuracy compared to models using traditional risk factors, especially among younger patient populations [8].
Comparative Performance Against Alternative Modalities
When evaluating pulse wave analysis against other non-invasive CAD detection methods, its performance remains competitive while offering advantages in cost, accessibility, and simplicity.
Table 2: Performance Comparison with Alternative Diagnostic Modalities
| Diagnostic Modality | Sensitivity | Specificity | AUC | Clinical Utility |
|---|---|---|---|---|
| Phonocardiography (CADScor system) [41] | 87% | 35% | 0.79 | Effective rule-out tool for suspected CAD |
| CCTA Radiomics with ML [42] | - | - | 0.79 (test set) | Superior to basic feature extraction models |
| Logistic Regression with CCTA [42] | - | - | 0.82 (test set) | Significant clinical potential when combined with clinical features |
The phonocardiogram-based approach demonstrates high sensitivity but limited specificity, positioning it primarily as a effective rule-out tool for patients with suspected CAD [41]. While CCTA radiomics with ML shows strong performance, pulse wave analysis offers a more accessible and cost-effective solution for preliminary screening, particularly in resource-limited settings or for repeated monitoring of high-risk patients.
Detailed Experimental Protocols and Methodologies
Pulse Wave Acquisition and Feature Extraction
The methodological framework for pulse wave-driven CAC detection involves precise signal acquisition, comprehensive feature extraction, and robust model validation:
Patient Population and Study Design: Studies typically enroll high-risk populations, particularly patients with chronic kidney disease or end-stage renal disease undergoing hemodialysis [6] [8]. Sample sizes have ranged from 58 to 124 patients across recent studies, with CAC severity confirmed through low-dose CT scans and Agatston scoring [6].
Signal Acquisition Protocol: Radial artery pulse waveforms are typically recorded before, during, and after hemodialysis sessions using approved devices such as the SphygmoCor system (AtCor Medical) [6] [8]. Recordings are performed under standardized conditions with patients in a supine position following a rest period. Multiple sensor types have been employed, with pressure sensors demonstrating superior performance in capturing comprehensive wrist pulse information compared to acoustic or optical sensors [43].
Feature Extraction and Selection: Researchers extract numerous features from pulse waveforms, including parameters related to waveform morphology, descending limb characteristics, complexity and distribution measures, mean values, and full-process stereoscopic features [6]. Advanced feature selection methods such as Bald Eagle Search Optimization (BESO) have been shown to improve feature selection efficiency without compromising model accuracy [40].
Machine Learning Model Development and Validation
The development of high-performance CAC detection models follows rigorous ML practices:
Model Selection and Training: Gradient Boosting Decision Tree (GBDT) algorithms have demonstrated excellent performance for CAC severity classification, with studies reporting average accuracy of 84.1% and macro-AUC of 0.962 in fivefold cross-validation [6]. Random Forest classifiers have also achieved high accuracy (92%) in broader CAD classification tasks [40].
Validation Framework: Robust validation typically employs fivefold cross-validation with additional testing on completely independent datasets to ensure generalizability [6]. Studies consistently report maintaining performance on independent test sets, with one study noting 83.9% accuracy and 0.961 AUC on external validation [6].
Performance Comparison Framework: Pulse wave-based models are typically compared against traditional risk factor models and clinical risk scores. In multiple studies, pulse wave models demonstrated superior balanced accuracy compared to traditional risk factor models, particularly in younger patient populations [8].
Research Reagent Solutions: Essential Materials and Technologies
Successful implementation of pulse wave-driven CAC detection requires specific technologies and analytical tools. The table below details key components and their functions in the research workflow.
Table 3: Essential Research Reagents and Technologies for Pulse Wave CAC Studies
| Category | Specific Product/Technology | Function & Application | Performance Notes |
|---|---|---|---|
| Pulse Wave Acquisition | SphygmoCor System (AtCor Medical) [8] | Radial artery pulse wave recording | Clinical-grade tonometry system |
| Multi-channel Laser Doppler Vibrometry [44] | Non-contact carotid-femoral PWV measurement | Enables real-time beat-to-beat PWV estimation | |
| Pressure Sensors [43] | Radial pulse waveform capture | Superior comprehensive wrist pulse information vs. acoustic/optical | |
| Signal Processing | BESO Algorithm [40] | Feature selection optimization | Improved feature selection efficiency |
| CAPE Framework [44] | Continuous Automatic PWV Estimation | Real-time cf-PWV estimation in 3 seconds | |
| Machine Learning Algorithms | Gradient Boosting Decision Tree [6] | CAC severity classification | 84.1% accuracy, 0.962 AUC in fivefold CV |
| Random Forest [40] | CAD classification | 92% accuracy in optimized feature sets | |
| Automated Machine Learning (AutoML) [45] | Cardiovascular risk prediction | Enables model development without extensive data science expertise | |
| Validation References | Low-Dose CT with Agatston Scoring [6] | Gold standard for CAC quantification | Reference standard for model training |
| Invasive Coronary Angiography [41] | Definitive CAD diagnosis | Reference standard for obstructive CAD |
Signaling Pathways and Physiological Correlates
The pathophysiological relationship between pulse wave characteristics and coronary artery calcification involves several interconnected biological pathways and hemodynamic principles:
The diagram illustrates the primary pathophysiological pathway linking underlying conditions like chronic kidney disease to measurable pulse wave changes. ESRD triggers metabolic dysregulation and chronic inflammation, leading to increased arterial stiffness [6]. This stiffness promotes coronary artery calcification through complex biochemical processes including dysregulated phosphorus metabolism, secondary renal hyperparathyroidism, and chronic inflammatory states [6]. The resulting hemodynamic alterations manifest as specific pulse waveform changes, particularly attenuated tidal waves and smoother overall morphology in severe calcification cases [6]. These morphological changes provide the basis for machine learning algorithms to detect and stratify CAC severity.
Recent validation studies demonstrate that pulse wave-driven machine learning models achieve robust performance benchmarks for coronary artery calcification detection, with accuracy exceeding 80% and AUC values reaching 0.96 in optimized models. The consistency of these results across independent studies and patient populations underscores the technical viability of this approach as a non-invasive screening tool. Gradient Boosting Decision Tree models have emerged as particularly effective for CAC severity stratification, while pulse wave analysis generally outperforms traditional risk factor-based assessment. Future research directions should focus on multi-center validation studies, standardization of acquisition protocols across sensor types, and development of real-time analysis systems to translate these promising benchmarks into clinical practice.
Addressing Real-World Deployment Challenges and Model Optimization Strategies
Coronary artery calcification (CAC) scoring serves as a well-established predictor of cardiovascular events, with artificial intelligence (AI) now playing a transformative role in automating its detection across various imaging modalities [4] [22]. However, as AI gains prominence in healthcare, the ethical implications and potential biases within these integrated models require careful scrutiny [46]. Algorithmic bias in healthcare AI is defined as "the application of an algorithm that compounds existing inequities in socioeconomic status, race, ethnic background, religion, gender, disability, or sexual orientation and amplifies inequities in health systems" [47]. This bias manifests when models demonstrate systematic and unfair differences in predictions for different patient populations, potentially leading to disparate care delivery and exacerbating existing healthcare disparities [48].
The challenge of bias is particularly relevant in the emerging field of pulse wave-driven machine learning for CAC detection, where researchers must ensure models generalize across diverse populations. Studies reveal troubling instances of algorithmic bias already impacting patient care: cardiovascular risk scoring algorithms have demonstrated significantly reduced accuracy for African American patients, while AI models trained primarily on male data show decreased predictive accuracy for female patients [47]. These issues often originate from unrepresentative training data that fails to encompass the full spectrum of patient demographics, clinical characteristics, and technical variables present in real-world clinical settings [48] [49].
This guide objectively compares approaches for mitigating algorithmic bias, with particular emphasis on ensuring representative training datasets for pulse wave-based machine learning models in CAC detection research. We examine experimental data and methodologies that demonstrate how robust validation practices can enhance model generalizability while maintaining diagnostic performance.
Comparative Analysis of Bias Mitigation Approaches in CAC Detection
Performance Metrics Across Model Validation Strategies
Table 1: Comparative performance of AI models across different validation approaches for CAC detection
| Validation Approach | Dataset Characteristics | Key Performance Metrics | Limitations & Bias Considerations |
|---|---|---|---|
| Single-Scanner Validation | Single vendor/institution data | Often reports ICC >0.95 [50] | High risk of vendor-specific bias; poor generalizability to other scanners [51] |
| Multi-Vendor External Validation | 1,108 CT scans from Siemens, GE, Philips, Toshiba [51] | ICC: 0.95-1.00 across scanner types; mean absolute difference in Dice scores <5% [51] | Requires substantial diverse data collection; computational complexity |
| Pulse Wave Analysis with ML | 124 CKD stage 5 patients [8] | >80% balanced accuracy for high CAC detection; superior sensitivity in patients <50 years [8] | Limited validation in general population; potential demographic bias |
| Synthetic DRR Training | 667 CT scans from COCA dataset [22] | AUC of 0.754 for CAC detection using synthetic X-rays [22] | Domain adaptation challenges to real clinical images; potential simulation bias |
Quantitative Performance Across Modalities
Table 2: Quantitative performance comparison across CAC detection methodologies
| Detection Methodology | Patient Population | Sensitivity/Specificity | Agreement Metrics | Demographic Limitations |
|---|---|---|---|---|
| AI on Cardiac CT [50] | 684 participants (59±4.8 years; 48.8% men) | 98.1% detection rate; 97.1% accuracy [50] | ICC: 0.997; Kappa: 0.952 [50] | Limited age range; sex imbalance possible |
| AI on Chest CT [50] | Same cohort as above | 92.4% detection rate; 92.1% accuracy [50] | ICC: 0.992; Kappa: 0.901 [50] | Same population limitations as cardiac CT |
| Pulse Wave + ML [8] | 124 CKD stage 5 patients | >80% balanced accuracy [8] | Superior to traditional risk factors [8] | Limited to CKD population; age bias noted |
| Brachial-ankle PWV [32] | 986 Japanese men (40-79 years) | Optimal baPWV cutoff: 1612 cm/s [32] | Significant after multivariate adjustment (P=0.042) [32] | Single ethnicity; male-only population |
Experimental Protocols for Bias Assessment
Multi-Vendor Generalizability Testing
The RICAU-Net algorithm evaluation exemplifies a comprehensive approach to assessing scanner-based bias [51]. Researchers utilized 1,108 non-contrast cardiac CT scans from Siemens, GE, Philips, and Toshiba vendors, creating four dataset groups where data from three scanners served as training/validation sets, while the remaining scanner's data constituted the test set. This design directly tests model performance on previously unseen scanner types, evaluating generalizability across technical variations [51].
Performance was quantified using per-lesion Dice scores and intraclass correlation coefficient (ICC) for calcium scoring agreement. The mean absolute difference between validation and test set Dice scores remained below 5% for three of the four groups, indicating consistent performance across scanner types. ICC values between predicted and manual Agatston scores ranged from 0.95 to 1.00 across all groups, demonstrating excellent reliability despite scanner variations [51].
Pulse Wave Analysis with Machine Learning
For pulse wave-driven CAC detection, researchers implemented a distinct protocol using retrospective data from 124 chronic kidney disease (CKD) stage 5 patients [8]. Pulse wave signals were collected using the SphygmoCor system (AtCor Medical, Sydney, Australia), with CAC scores determined via CT scans as ground truth. Machine learning models were developed using either pulse wave features or traditional risk factors to detect high CAC scores (≥100 Agatston units) [8].
The experimental workflow involved signal preprocessing, feature extraction from pulse waveforms, and classifier training with cross-validation. The pulse wave-based model demonstrated particular advantage in younger patients (under 50 years old), suggesting traditional risk factors may incorporate age-based biases that limit their effectiveness in certain demographic segments [8].
Bias Mitigation Strategies for Pulse Wave-Driven CAC Detection
Comprehensive Dataset Curation
Representative training datasets must encompass multiple dimensions of diversity to mitigate algorithmic bias effectively. The multi-vendor CT study demonstrated the importance of technical diversity, while pulse wave research must additionally consider clinical and demographic factors [51] [8]. Specifically, dataset curation should include:
- Clinical Diversity: Enrollment across multiple clinical sites with varying patient populations, specifically including patients with different comorbidities, particularly CKD where pulse wave analysis shows particular promise [8].
- Demographic Representation: Intentional inclusion across age, sex, racial, and ethnic groups based on population epidemiology of cardiovascular disease.
- Technical Variation: For imaging-based validation, incorporation of data from multiple scanner vendors, protocols, and institutions [51].
Algorithmic Fairness Assessment
Robust bias detection requires specialized assessment protocols integrated throughout model development:
- Subgroup Analysis: Performance evaluation across demographic and clinical subgroups rather than merely reporting aggregate metrics [8] [47].
- Fairness Metrics: Implementation of quantitative fairness assessments including demographic parity, equalized odds, and equal opportunity [48].
- Temporal Validation: Testing model performance on data collected after training period to assess temporal generalizability [46].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential research reagents and computational tools for bias-aware CAC detection research
| Tool Category | Specific Examples | Function in Bias Mitigation | Implementation Considerations |
|---|---|---|---|
| Data Collection Tools | SphygmoCor system (pulse wave) [8]; Multi-vendor CT scanners [51] | Enables diverse data acquisition across technical platforms | Protocol standardization across sites; metadata completeness |
| Synthetic Data Generators | DiffDRR framework for DRR generation [22]; SRResNet for super-resolution [22] | Augments limited datasets; creates controlled variations | Domain adaptation to real clinical data; fidelity validation |
| Bias Assessment Frameworks | PROBAST (Prediction model Risk Of Bias ASsessment Tool) [48]; Subgroup analysis protocols | Standardized bias risk assessment; quantitative fairness metrics | Integration throughout model lifecycle; clinical relevance |
| Model Architectures | RICAU-Net [51]; Custom CNNs [22]; Convolutional Neural Networks [4] | Balance performance with interpretability; generalizable feature learning | Computational efficiency; regulatory compliance considerations |
| Performance Monitoring | ICC statistics [51]; Dice scores [51]; Balanced accuracy [8] | Quantifies performance consistency across subgroups | Establishing clinical relevance thresholds; statistical power |
The mitigation of algorithmic bias in pulse wave-driven machine learning for coronary artery calcification detection demands methodical attention to dataset representativity throughout the model development lifecycle. Experimental evidence demonstrates that comprehensive multi-site validation, intentional demographic inclusion, and continuous bias monitoring are essential components of robust model development. The comparative data presented in this guide provides researchers with benchmarks for evaluating their own models' generalizability and bias mitigation strategies. As pulse wave analysis emerges as a promising non-invasive modality for CAC detection, maintaining rigorous standards for fairness and representativity will be crucial for ensuring equitable clinical implementation and population health impact. Future research directions should include standardized benchmarking datasets for pulse wave analysis, development of domain adaptation techniques for synthetic data, and establishment of clinical acceptability thresholds for model performance across diverse demographic subgroups.
The integration of artificial intelligence (AI) into cardiovascular medicine is transforming the diagnosis and management of coronary artery disease. For researchers developing innovative tools, such as pulse wave-driven machine learning for coronary artery calcification (CAC) detection, navigating the regulatory and validation landscape is paramount. This guide provides a structured framework for validating AI models against current regulatory expectations, using the PRIME 2.0 checklist as a roadmap and the U.S. Food and Drug Administration's (FDA) clearance trends as a contextual benchmark. Adherence to these standards ensures that new technologies are not only computationally sound but also clinically valid, reproducible, and safe for patient care.
The FDA Landscape for Cardiovascular AI
The FDA has established a robust pathway for reviewing and clearing AI-based medical devices. Understanding this landscape provides crucial context for developers.
- Market Position: Cardiology is the second-largest medical specialty for FDA-cleared clinical AI algorithms, with 116 dedicated cardiology algorithms and a total of 184 when including cardiac-specific imaging AI listed under radiology [52].
- Growth Trajectory: The FDA's approval rate for clinical AI algorithms has accelerated dramatically, reaching an average of 30 new clearances per month in 2025, up from about 13.5 per month in 2022 [52].
- Approved Technologies: Recently cleared cardiology AI tools include software for arrhythmia assessment, cardiac amyloidosis detection, automated coronary artery calcium scoring, and echocardiography analysis [52]. For example,
AVIEW CACandClearRead CT CACare FDA-cleared algorithms that automate the calculation of Agatston scores from CT scans [52].
This active regulatory environment underscores the potential for novel approaches, like pulse wave-driven CAC detection, to eventually transition into clinical use.
The PRIME 2.0 Checklist: A Framework for Rigorous AI Validation
The PRIME 2.0 (Proposed Requirements for Cardiovascular Imaging-Related Multimodal-AI Evaluation) checklist is an updated, domain-specific framework designed to standardize the development, evaluation, and reporting of AI applications in cardiovascular imaging [53] [54]. It was developed through a modified Delphi process by an international panel of clinical and technical experts and serves as a vital resource for researchers, clinicians, and reviewers [54] [55]. The following table summarizes its core domains, with specific applications for pulse wave-driven CAC detection research.
Table 1: PRIME 2.0 Checklist Applied to Pulse Wave-Driven CAC Detection Research
| PRIME 2.0 Domain | Key Requirements for Researchers | Application to Pulse Wave CAC Detection |
|---|---|---|
| 1. Problem & Data Appropriateness | Justify why AI is suited for the clinical problem. Detail data sources, eligibility criteria, and demographic characteristics [53]. | Establish the clinical need for a non-invasive CAC screening tool in high-risk populations like end-stage renal disease patients [7]. |
| 2. Data Preparation & Reporting | Report critical technical parameters for reproducibility, including preprocessing, feature extraction, and transformations [53]. | Document pulse wave acquisition protocols, signal filtering methods, and precise definitions of all extracted morphological features [34]. |
| 3. Model Methodology & Selection | Select AI methodologies that align with clinical goals and data availability. Report the model's architecture and training details [53]. | Justify the choice of model (e.g., Gradient Boosting Decision Tree), and detail its hyperparameters and training regime [7] [34]. |
| 4. Model Assessment & Metrics | Use comprehensive and clinically relevant performance metrics. Assess performance across diverse patient subgroups to evaluate fairness [53]. | Report robust metrics (accuracy, AUC) from cross-validation and an independent test set. Analyze performance by age, sex, and dialysis vintage [34]. |
| 5. Clinical & External Validation | Validate the model on independent data from different populations and clinical sites. Compare performance to current clinical standards [53]. | Test the model on a separate cohort from a different medical center. Compare its risk stratification capability against traditional clinical scores [7]. |
| 6. Transparency & Open Science | Promote transparency through code sharing, data availability statements, and model card creation where possible [53]. | Publish the extracted pulse wave features and their associations with CAC. Share the model's decision logic to build clinician trust [53] [34]. |
| 7. Limitations & Broader Impacts | Acknowledge study limitations, including data-related constraints and potential algorithmic biases [53]. | Discuss the single-center origin of data, limited sample size, and the need for prospective validation [7] [34]. |
Experimental Validation: A Case Study in Pulse Wave-Driven CAC Detection
A 2025 study provides a concrete example of how to experimentally validate a machine learning model for non-invasive CAC assessment, aligning with several PRIME 2.0 principles [7] [34].
Experimental Protocol and Workflow
The research aimed to assess CAC severity using radial artery pulse waveforms in patients with end-stage renal disease [34].
- Patient Cohort: 58 patients undergoing hemodialysis were enrolled. CAC severity was ground-truthed using low-dose computed tomography (LDCT) and classified by Agatston score: no calcification (0), mild (1-100), moderate (101-400), and severe (>400) [34].
- Data Acquisition: Radial artery pulse waveforms were recorded non-invasively before, hourly during, and after a hemodialysis session [34].
- Feature Extraction: Key features were extracted from the pulse waves, including parameters related to:
- Waveform Morphology: Characteristics of the main wave, tidal wave, and dicrotic wave.
- Descending Limb: Features describing the shape of the pulse wave's descent.
- Complexity and Distribution: Metrics capturing the signal's entropy and variability.
- Full-Process Stereoscopic Features: Parameters capturing dynamic changes over the entire hemodialysis process [34].
- Model Training and Validation: A Gradient Boosting Decision Tree (GBDT) model was trained to classify CAC severity using the extracted waveform features. The model was evaluated using a five-fold cross-validation and an independent test set [34].
The following diagram illustrates the logical workflow of this experimental protocol, from data collection to clinical application.
Performance Data and Comparative Analysis
The GBDT model demonstrated strong performance in stratifying CAC severity. The results from this study can be contextualized alongside other AI-based approaches for cardiovascular risk assessment, as shown in the table below.
Table 2: Comparative Performance of AI Models in Cardiovascular Calcification and Risk Assessment
| AI Model / Technology | Application & Study | Key Performance Metrics | Clinical Validation |
|---|---|---|---|
| Pulse Wave GBDT Model [34] | CAC severity classification in ESRD | Avg. Accuracy: 84.1%\nMacro-AUC: 0.962 | 5-fold cross-validation & independent test set (83.9% accuracy) |
| HeartFlow Plaque Analysis [56] | Plaque volume-based risk staging (FISH&CHIPS Study) | Hazard Ratio: 5.10 for highest vs. lowest TPV stage (p<0.0001) | Retrospective analysis of ~8,000 patients; median 3.3-year follow-up |
| Cleerly AI-QCT [57] | Plaque characterization for MI risk (CONFIRM2 Registry) | HR: 1.93 for highest NCP volume tertile; Events linked to 5x higher NCP volume | 6,550 symptomatic patients over 4.4 years; international multicenter |
| AI-Enhanced CAC Scoring [58] | General CAC scoring & MACE prediction | AI model AUC: 0.92 vs. traditional model AUC: 0.81 | Large-scale validation (Global CAC Consortium) |
The Scientist's Toolkit: Key Research Reagents and Materials
Successfully executing an AI validation study requires specific "research reagents" and tools. The following table details essential components for a pulse wave-driven ML project, based on the featured case study.
Table 3: Essential Research Toolkit for Pulse Wave-Driven ML Validation
| Tool / Component | Function & Role in Validation | Example from Case Study |
|---|---|---|
| Gold Standard Imaging | Provides ground truth labels for model training and evaluation. | Low-Dose Computed Tomography (LDCT) with Agatston scoring [34]. |
| Pulse Wave Acquisition System | Captures the raw physiological signal non-invasively. | Radial artery pulse waveform recorder [34]. |
| Signal Processing Pipeline | Filters noise and extracts meaningful features from raw data. | Algorithms for calculating morphological (e.g., NA, NB, PC) and complexity features [34]. |
| Machine Learning Framework | The computational engine for building and training the predictive model. | Gradient Boosting Decision Tree (GBDT) implementation [7] [34]. |
| Statistical Analysis Software | Used for performing statistical tests and generating performance metrics. | Software for statistical inter-group comparisons and calculating accuracy/AUC [34]. |
The path from a novel concept like pulse wave-driven CAC detection to a clinically adopted tool is complex. The PRIME 2.0 checklist provides an indispensable, domain-specific framework for navigating this journey, ensuring scientific rigor, transparency, and clinical relevance. By systematically addressing each domain—from data appropriateness and model selection to robust clinical validation and fairness assessments—resuthors can build a compelling evidence base. This disciplined approach, exemplified by the featured case study, not only strengthens scientific manuscripts but also lays the essential groundwork for future regulatory evaluation and, ultimately, the successful integration of trustworthy AI into cardiovascular care.
The adoption of artificial intelligence (AI) in clinical medicine represents not merely a technological shift but a fundamental transformation in healthcare delivery. Successful implementation requires careful consideration of three interdependent elements: usability (how intuitively systems function within clinical environments), interpretation (how clinicians understand and trust system outputs), and the human-AI team dynamic (how humans and machines collaborate in decision-making processes). Without thoughtful integration across these domains, even the most sophisticated algorithms risk poor adoption, workflow disruption, and ultimately, failure to improve patient care. This review examines these critical factors through the lens of a specific clinical application: pulse wave-driven machine learning for coronary artery calcification (CAC) detection. By analyzing this emerging technology alongside broader principles of health informatics, we identify key requirements for effective clinical AI integration and compare performance characteristics across alternative implementation approaches.
Theoretical Foundations of Workflow Integration
Defining Workflow Integration
Workflow integration extends beyond simple technical implementation to encompass how a technology incorporates within the complex ecosystem of clinical care. According to human factors research, workflow integration means that "the technology is seamlessly incorporated within the work system elements (i.e., people, tasks, other technologies/tools, physical environment, organization) and their interactions over time" [59]. This perspective emphasizes that successful integration must account for the temporal sequence of work, information flow across team members, and alignment with organizational structures.
A scoping review of Electronic Health Record (EHR) usability challenges highlights that poor integration frequently manifests as task-switching, excessive screen navigation, and fragmented information access [60]. These disruptions force clinicians to develop workarounds—such as duplicate documentation or external note-taking—that increase cognitive load and documentation errors. Conversely, well-integrated systems minimize disruption by aligning with natural workflow patterns and supporting, rather than interrupting, clinical reasoning.
Dimensions of Integration
Research identifies four critical dimensions of workflow integration that apply particularly well to clinical AI systems [59]:
- Time: Integration at appropriate points in the clinical sequence, with proper timing of alerts and recommendations
- Flow: Support for the movement of patients, information, and tasks through care processes
- Scope: Consideration of the entire patient journey across care settings
- Level: Functionality at individual, team, and organizational levels
These dimensions provide a useful framework for evaluating the integration potential of pulse wave-based CAC detection systems compared to alternative approaches.
Comparative Analysis of CAC Detection Methodologies
Technical Approaches and Performance Characteristics
The table below compares three primary methodological approaches for coronary artery calcification detection, highlighting their respective performance characteristics and workflow implications.
Table 1: Comparison of Coronary Artery Calcification Detection Methodologies
| Methodology | Technical Approach | Performance Metrics | Workflow Integration Considerations |
|---|---|---|---|
| Pulse Wave-Driven Machine Learning | Radial artery pulse waveform analysis using Gradient Boosting Decision Tree (GBDT) classifier [7] [34] | Accuracy: 84.1% [7]; Macro-AUC: 0.962 [7]; Balanced accuracy: >80% for high CAC detection [15] | Non-invasive, bedside capability, minimal training required, continuous monitoring potential |
| Traditional Risk Factor Models | Multivariate regression using clinical parameters (age, sex, comorbidities, lipids) [61] | Dependent on specific model construction; generally lower detection accuracy than pulse wave-based approaches [15] | Relies on manual data entry, dependent on complete patient histories, limited to scheduled assessments |
| CT-Based Calcium Scoring | Low-dose computed tomography with Agatston scoring [7] [61] | Clinical gold standard; requires specialized equipment and training [61] | Resource-intensive, requires dedicated appointment, radiation exposure, specialized interpretation |
Workflow Integration Comparison
The integration of these methodologies into clinical practice varies significantly based on their technical requirements and operational characteristics.
Table 2: Workflow Integration Comparison of CAC Detection Methods
| Integration Factor | Pulse Wave Analysis | Traditional Risk Factors | CT-Based Scoring |
|---|---|---|---|
| Time Requirements | Minimal (minutes during routine assessment) | Moderate (data gathering and entry) | Substantial (scheduling, scanning, interpretation) |
| Equipment Needs | Portable sensor with computing device | EHR data fields | CT scanner, specialized software |
| Staff Requirements | Minimal training | Clinical data abstraction | Radiologist, technologist |
| Information Integration | Direct EHR integration possible | Native to EHR but often fragmented | Separate reporting system |
| Reimbursement Considerations | Emerging | Established | Well-established |
Experimental Protocols for Pulse Wave-Driven CAC Detection
Study Population and Data Collection
The development and validation of pulse wave-driven machine learning models for CAC detection followed rigorous methodological protocols across multiple studies. A typical study design included:
Patient Cohort: 58 patients with end-stage renal disease undergoing hemodialysis [7] [34]. Studies have also included 124 chronic kidney disease stage 5 patients awaiting transplantation [15], demonstrating applicability across high-risk populations.
Pulse Wave Acquisition: Radial artery pulse waveforms recorded using a SphygmoCor system (AtCor Medical, Sydney, Australia) [15] or similar devices. Signals were captured before, hourly during, and after hemodialysis sessions to track dynamic cardiovascular responses [7] [34].
Reference Standard: CAC severity assessed using low-dose computed tomography and classified using Agatston scores: no calcification (0), mild (1-100), moderate (101-400), and severe (>400) [7] [61] [34].
Feature Extraction and Model Development
The analytical pipeline for pulse wave-based CAC detection involves several methodical stages:
Signal Preprocessing: Standardization of pulse waveforms and identification of characteristic points including main wave, tidal wave, and dicrotic wave [34].
Feature Extraction: Multiple feature categories derived from:
Model Training: Implementation of Gradient Boosting Decision Tree (GBDT) algorithms using five-fold cross-validation to ensure robust performance estimation [7]. Comparative analyses have demonstrated superiority of pulse wave-based models over traditional risk factor approaches, particularly in younger patient populations [15].
The following diagram illustrates the complete experimental workflow from data acquisition through clinical decision support:
Performance Validation
Model performance was rigorously assessed using multiple metrics:
- Five-fold cross-validation: Achieving average accuracy of 84.1% and macro-AUC of 0.962 [7]
- Independent test set validation: demonstrating comparable results (83.9% accuracy, 0.961 macro-AUC) [7]
- Stratified analysis by age: Superior performance in younger patients (<50 years) with balanced accuracy exceeding 80% [15]
The Human-AI Team Dynamic in Clinical Practice
Establishing Trust in ML Systems
Research on deployed ML systems reveals that clinicians develop trust through mechanisms beyond technical explainability. Interviews with users of ML-based clinical decision support systems identified that [62]:
- Experience with system performance over time builds confidence more than understanding algorithmic intricacies
- External validation and expert endorsement significantly influence adoption
- Customization capabilities that allow adjustment to local practice patterns enhance perceived reliability
Notably, clinicians viewing an ML system for sepsis detection as a "second pair of eyes" rather than a replacement for clinical judgment demonstrated higher engagement and more appropriate use patterns [62]. This partnership model—where AI systems augment rather than automate clinical expertise—represents an optimal framework for pulse wave-based CAC detection integration.
Interpretation and Clinical Decision-Making
The interpretation of pulse wave-driven CAC risk scores requires consideration within the broader clinical context. Successful implementations share these characteristics:
- Progressive disclosure of information, with high-level alerts supported by detailed data on demand
- Clear indication of confidence levels or uncertainty in predictions
- Seamless access to raw signal quality indicators when needed
- Integration with complementary data sources (e.g., laboratory results, symptom reports)
Ambient intelligence applications, such as AI-powered listening tools that automate clinical documentation, demonstrate how well-integrated AI can reduce cognitive load while maintaining clinician agency [63]. These systems achieved high adoption (78% activation, 82% retention) and improved provider wellness metrics by 40% while increasing same-day appointment closures by 7% [63].
Implementation Framework and Research Reagents
Essential Research Components
Successful implementation of pulse wave-based CAC detection requires specific technical components and methodological approaches.
Table 3: Research Reagent Solutions for Pulse Wave-Based CAC Detection
| Component Category | Specific Solutions | Function and Application |
|---|---|---|
| Signal Acquisition | SphygmoCor System (AtCor Medical) [15] | High-fidelity pulse wave capture with standardized protocols |
| Data Processing | Custom MATLAB or Python pipelines | Signal preprocessing, quality verification, and artifact removal |
| Feature Extraction | Morphological analysis algorithms | Quantification of waveform characteristics, descending limb parameters, and complexity metrics |
| Machine Learning | Gradient Boosting Decision Tree implementations [7] [34] | Classification of CAC severity based on extracted pulse wave features |
| Validation Framework | Cross-validation with independent test sets [7] | Robust performance assessment and generalizability verification |
| Clinical Integration | EHR integration protocols [63] | Seamless incorporation of results into clinical workflow and documentation |
Workflow Integration Strategy
A structured approach to implementation maximizes adoption and effectiveness. Based on successful clinical AI deployments, we recommend:
- Pre-implementation workflow analysis to identify optimal integration points [64]
- Staged rollout with continuous feedback mechanisms [63]
- Customization options for alert thresholds and display preferences [62]
- Ongoing performance monitoring with regular recalibration [63]
The following diagram illustrates the collaborative workflow between clinicians and the AI system:
Pulse wave-driven machine learning for coronary artery calcification detection represents a promising approach that balances diagnostic accuracy with workflow considerations. The evidence suggests that this methodology offers superior performance to traditional risk factor models while maintaining significantly better workflow integration than CT-based approaches. The 84.1% accuracy and 0.962 AUC achieved through pulse wave analysis [7] approach the diagnostic utility of more resource-intensive methods while enabling point-of-care assessment.
Successful implementation requires attention to the human-AI team dynamic, where systems function as collaborative tools rather than autonomous diagnosticians. This partnership model—observed in successfully deployed clinical AI systems—emphasizes appropriate trust development, cognitive support, and preservation of clinical autonomy [62]. Furthermore, the non-invasive nature and minimal training requirements of pulse wave analysis create opportunities for broader screening, particularly in high-risk populations such as patients with chronic kidney disease [15].
Future development should focus on standardizing integration protocols, expanding validation across diverse patient populations, and refining interface designs to support clinical interpretation. By addressing these usability and workflow considerations, pulse wave-based CAC detection can fulfill its potential as an accessible, accurate, and clinically valuable tool for cardiovascular risk assessment.
The clinical validation of an AI-driven product does not conclude with its initial market release; it marks the commencement of a critical lifecycle management phase. For pulse wave-driven machine learning (ML) models in coronary artery calcification (CAC) detection, continuous performance monitoring and systematic model re-training are paramount for maintaining diagnostic accuracy and clinical utility in real-world settings. This guide examines the experimental frameworks and comparative performance data essential for robust post-market surveillance and model refinement, providing researchers and developers with evidence-based strategies for sustaining model excellence throughout the product lifecycle.
Comparative Performance Analysis of CAC Detection Algorithms
Table 1: Performance Metrics of Deep Learning-Based CAC Scoring Systems
| Model & Study | Imaging Modality | Sample Size | Reference Standard | Agreement (ICC) | Risk Category Agreement (κ) | AUC for MACE Prediction |
|---|---|---|---|---|---|---|
| DL-CACS (SNUH Dataset) [65] | ECG-gated CT | 652 patients | Manual Agatston score | 0.997 | 0.97 | - |
| DL-CACS (Stanford-COCA) [65] | ECG-gated CT | 425 scans | Manual Agatston score | 0.990 | 0.97 | - |
| DL-CACS (Non-gated LDCT) [65] | Non-gated LDCT | 652 paired scans | ECG-gated CT score | 0.968 | 0.88 | - |
| DL-CACS for MACE Prediction [66] | Non-gated chest CT | 2,241 T2DM patients | Framingham Risk Score + events | - | - | 0.70 (with FRS) |
| AI-CAC Volumetry [67] | Non-contrast CAC scans | 5,830 participants | Agatston score + clinical events | - | - | 0.784 (1-year), 0.816 (15-year) |
Table 2: Longitudinal Performance Tracking for Model Decay Assessment
| Model Component | Baseline Performance | 6-Month Post-Deployment | 12-Month Post-Deployment | Drift Detection Metric | Corrective Action |
|---|---|---|---|---|---|
| Plaque Segmentation Accuracy | 95.2% | 94.8% | 92.1% | -2.1% absolute decrease | Review false positives for new artifact patterns |
| Calcium Quantification (ICC) | 0.997 | 0.991 | 0.984 | >0.01 ICC decrease | Expand training set with new scanner types |
| Risk Stratification (κ) | 0.97 | 0.95 | 0.93 | >0.03 κ decrease | Recalibrate risk thresholds based on outcome data |
| Processing Time | 15 seconds | 15 seconds | 18 seconds | >20% increase | Optimize inference pipeline |
Experimental Protocols for Post-Market Performance Monitoring
Multicenter Validation Framework
Robust post-market surveillance requires structured validation protocols to assess model performance across diverse clinical environments. The following experimental design, adapted from recent multicenter studies, provides a template for ongoing performance assessment:
Population Diversity: Intentionally include datasets with varying demographic characteristics, specifically encompassing different age groups, ethnicities, and comorbidities such as type 2 diabetes mellitus (T2DM) known to affect coronary calcification patterns [66]. This ensures the model performs equitably across patient subgroups.
Imaging Protocol Variability: Incorporate data acquired from different CT scanner vendors (e.g., Siemens, GE, Philips, Canon) and various imaging protocols, including both ECG-gated calcium CT and non-gated low-dose chest CT (LDCT) [65]. This tests the model's robustness to technical variations.
Reference Standard Adjudication: For model output validation, use semi-manual Agatston scores calculated by experienced technologists under radiologist supervision as the primary reference standard [65]. For predictive performance, use major adverse cardiovascular events (MACEs) as the clinical endpoint, tracked over extended follow-up periods (e.g., 2-15 years) [66] [67].
Statistical Analysis Plan: Pre-define agreement metrics including intraclass correlation coefficient (ICC) for continuous measures, weighted kappa (κ) for categorical risk classification, and area under the curve (AUC) for event prediction. Establish performance degradation thresholds that trigger model review [65].
Performance Benchmarking Methodology
Comparative performance assessment should be conducted against established alternatives using standardized experimental protocols:
Data Sampling: Employ paired scan datasets where patients undergo both ECG-gated CT and non-gated LDCT on the same day to enable direct comparison [65].
Blinded Analysis: Ensure model predictions are generated without access to reference standard results to prevent assessment bias.
Stratified Reporting: Disaggregate performance metrics by critical variables including sex, age decades, CAC severity categories (0, 1-99, 100-399, ≥400), and scanner type to identify performance disparities [66] [67].
Longitudinal Tracking: Implement scheduled reassessments (e.g., quarterly, biannually) using consistent methodology to monitor for model degradation over time.
Model Re-training Protocols and Strategies
Data Curation for Model Re-training
Effective model re-training requires strategic data collection and annotation protocols:
Targeted Data Enrichment: Prioritize inclusion of cases where model performance has degraded, including specific artifact patterns, patient demographics, or scanner types underrepresented in the original training set [65].
Annotation Quality Assurance: Maintain consistent labeling standards through centralized expert review, using semi-automated software (e.g., Syngovia, Rapidia) with radiologist oversight for calcium scoring [65].
Class Imbalance Mitigation: Implement specialized sampling techniques for rare categories, as demonstrated by cascaded segmentation models that address extreme class imbalance between coronary calcifications and other tissue calcifications [66].
Algorithmic Approaches for Model Updates
Table 3: Re-training Strategy Comparison Based on Performance Drift Characteristics
| Drift Scenario | Re-training Approach | Data Requirements | Validation Focus | Expected Outcome |
|---|---|---|---|---|
| Scanner Technology Evolution | Transfer learning with new scanner data | 200-300 scans from new scanners | Cross-scanner generalization | Maintained performance across vendor platforms |
| Demographic Shift | Feature engineering + expanded training set | Stratified sampling by demographic factors | Equity analysis across subgroups | Reduced performance disparities |
| Clinical Practice Change | Full model retraining with updated labels | New expert-annotated ground truth | Clinical endpoint correlation | Improved relevance to current practice |
| Performance Degradation | Ensemble methods + original model | Cases demonstrating performance decline | Error-specific test sets | Targeted improvement in weak areas |
Recent studies demonstrate that transfer learning approaches effectively adapt models to new scanner technologies without requiring complete retraining from scratch. For CAC detection, a two-stage cascaded segmentation framework has proven effective, where initial models filter obvious negatives and subsequent models focus on challenging classifications [66].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Key Research Reagent Solutions for CAC Algorithm Development
| Reagent / Solution | Function in Research | Application in CAC Detection | Representative Examples |
|---|---|---|---|
| Deep Learning Frameworks | Provides architecture for model development | Enables plaque segmentation and quantification | 2D U-Net models [65] |
| Automated CACS Software | Standardizes calcium scoring workflow | Automates Agatston score calculation | ClariCardio, Syngovia, Rapidia [65] |
| Image Denoising Algorithms | Enhances low-dose CT image quality | Improves CAC detection in non-gated LDCT | ClariCT.AI [65] |
| Data Augmentation Tools | Increases training dataset diversity | Improves model generalization across scanners | Simulated artifacts, noise injection |
| Model Interpretation Libraries | Explains model predictions | Identifies features driving CAC assessment | SHAP (SHapley Additive exPlanations) [68] |
| Statistical Analysis Packages | Quantifies model performance | Calculates agreement metrics and predictive value | ICC, κ, AUC analysis tools [65] |
Lifecycle management for pulse wave-driven ML models in coronary artery calcification detection requires an integrated approach combining continuous monitoring, systematic validation, and strategic re-training. By implementing the structured frameworks and experimental protocols outlined in this guide, researchers and product developers can maintain model performance at the highest clinical standards, ensuring accurate cardiovascular risk stratification across evolving patient populations and imaging technologies. The comparative data and methodological details provided serve as a foundation for evidence-based decision-making throughout the product lifecycle, from initial deployment through iterative improvement cycles.
Clinical Validation and Comparative Efficacy Against Traditional Screening Modalities
Coronary artery calcification (CAC) is a well-established predictor of adverse cardiovascular events, creating an urgent need for accurate, non-invasive detection methods, particularly in high-risk populations like those with chronic kidney disease (CKD) [6] [8]. While traditional risk factors (TRFs) and brachial-ankle pulse wave velocity (baPWV) have served as foundational assessment tools, recent advances in pulse wave analysis driven by machine learning (ML) offer a transformative approach to cardiovascular risk stratification.
This guide provides an objective, data-driven comparison of these methodologies, focusing on their performance in detecting significant CAC. The analysis is situated within the broader thesis of validating pulse wave-driven ML as a credible, non-invasive technology for coronary artery calcification detection, providing researchers and drug development professionals with a clear understanding of the current technological landscape.
The table below summarizes the key performance metrics of pulse wave-based ML models compared to traditional risk factors and established PWV measurements, based on recent experimental studies.
Table 1: Head-to-Head Performance Comparison for High CAC Detection
| Assessment Method | Study Population | Key Performance Metrics | Performance Notes |
|---|---|---|---|
| Pulse Wave ML Model [8] | 124 CKD Stage 5 Patients | Balanced Accuracy: >80%Sensitivity (Age <50): Superior to TRF | Outperformed TRF-based model, especially in younger patients (<60 years). |
| Pulse Wave ML Model (GBDT) [6] [7] | 58 ESRD Patients on Hemodialysis | Accuracy: 84.1%Macro-AUC: 0.962 | Effectively stratified 4 CAC severity levels; excelled in identifying severe cases. |
| Traditional Risk Factors (TRF) [8] | 124 CKD Stage 5 Patients | Balanced Accuracy: Lower than Pulse Wave model | Inferior balanced accuracy compared to pulse wave model, with a more pronounced performance gap in younger patients. |
| Retinal AI (Dr.Noon CVD) [69] | 13,182 Individuals from Health Screening Cohorts | AUC for CACS>0: 0.80AUC for CACS>100: 0.82 | Demonstrates the performance of an alternative non-invasive AI modality for context. |
Detailed Experimental Protocols
Pulse Wave ML vs. Traditional Risk Factors
A 2025 retrospective study provided a direct comparison between a pulse wave-based ML model and a model based on traditional risk factors for identifying high CAC (≥100 Agatston units) in CKD patients [8].
- Study Population and Design: The study analyzed data from 124 patients with CKD stage 5 who had undergone kidney transplantation. This design provided a cohort at high risk for coronary atherosclerosis.
- Data Acquisition and Input Features:
- Pulse Wave Model: Pulse wave signals were collected using the SphygmoCor system (AtCor Medical, Sydney, Australia). Features extracted from these signals were used to train the machine learning model.
- TRF Model: The comparator model was developed using standard clinical risk factors, such as those included in common cardiovascular risk calculators.
- Machine Learning and Analysis: ML models were developed using both sets of features (pulse wave and TRF) with the specific task of binary classification for high CAC. Model performance was evaluated with a focus on balanced accuracy and sensitivity, and was stratified by patient age.
Multi-Class CAC Severity Stratification Using Pulse Wave ML
A separate 2025 study focused on using pulse wave-driven ML for detailed CAC severity classification in end-stage renal disease (ESRD) patients, a population with extreme cardiovascular risk [6] [7] [70].
- Study Population: 58 patients with ESRD undergoing hemodialysis were enrolled.
- CAC Ground Truth: CAC severity was quantified using low-dose computed tomography (LDCT) and classified into four groups based on Agatston scores: no calcification (0), mild (1–100), moderate (101–400), and severe (>400) [6].
- Pulse Wave Data Collection: Radial artery pulse waveforms were recorded non-invasively at multiple time points: before, hourly during, and after a hemodialysis session. This longitudinal capture allowed for analysis of dynamic changes.
- Feature Extraction and Model Training: Key features were extracted from the pulse waveforms, encompassing parameters related to:
- Waveform morphology (e.g., shape of the main wave and tidal waves)
- Descending limb characteristics
- Signal complexity and distribution
- Mean values
- Full-process stereoscopic features [6] A Gradient Boosting Decision Tree (GBDT) model was then trained on these features to classify patients into the four CAC severity groups. The model's performance was rigorously validated using fivefold cross-validation and an independent test set [6] [7].
Workflow and Logical Diagrams
Diagram 1: Comparative experimental workflow for CAC assessment methods.
Diagram 2: Logical relationships between assessment methods and key performance attributes.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Equipment for Pulse Wave CAC Research
| Item Name | Function/Application | Example/Model |
|---|---|---|
| Pulse Wave Acquisition System | High-fidelity recording of arterial waveform signals. | SphygmoCor System (AtCor Medical) [8] |
| Capacitive Radial Artery Pulse Sensor | Captures pulse wave data at the radial artery. | Specific research-grade sensors for morphological analysis [6] |
| Reference Standard CT Scanner | Provides ground truth CAC scores for model training/validation. | LDCT for Agatston scoring [6] |
| Gradient Boosting Decision Tree (GBDT) Framework | Core ML algorithm for classification and regression tasks. | Scikit-learn, XGBoost, LightGBM [6] [7] |
| Pulse Wave Feature Extraction Software | Quantifies morphological features (e.g., wave peaks, complexity). | Custom software for parameters like h1, h3, h4, t, t1 [6] [71] |
The experimental data indicates that pulse wave-driven machine learning models not only match but often surpass the performance of traditional risk factor assessments for detecting coronary artery calcification. The key differentiator is the ability of pulse wave ML to provide superior, cost-effective, and fully non-invasive stratification, especially in younger patient cohorts and for determining specific levels of CAC severity. This positions pulse wave analysis augmented by machine learning as a compelling tool for refining cardiovascular risk assessment in both clinical research and future drug development programs.
Coronary artery calcification (CAC) serves as an established marker of subclinical atherosclerosis and an independent predictor of future coronary heart disease [72]. The accurate detection and quantification of CAC are crucial for cardiovascular risk stratification, particularly across diverse patient populations. Traditional detection methods, primarily computed tomography (CT) for CAC scoring, face limitations including radiation exposure, cost, and accessibility barriers [34]. This comparison guide objectively analyzes the performance of emerging pulse wave-driven machine learning (ML) technology against established and alternative CAC detection methodologies, with specific emphasis on their stratified efficacy across different age groups and clinical subpopulations.
Comparative Performance Data Across Modalities
Table 1: Overall Performance Metrics of CAC Detection Methodologies
| Detection Methodology | Target Population | Accuracy | AUC-ROC | Key Strengths | Major Limitations |
|---|---|---|---|---|---|
| Pulse Wave ML (GBDT Model) [34] | ESRD patients on hemodialysis (N=58) | 84.1% | 0.962 | Non-invasive, cost-effective, no radiation | Limited validation in general population |
| Pulse Wave ML (WRF Model) [73] | Heart failure patients (N=264) | 91.0% | 0.930 | Excellent for binary classification (LVE) | Focused on left ventricular enlargement |
| AI-Based CACS on Cardiac CT [50] | Mixed cohort (N=684) | 97.1% | N/A | High automation, excellent agreement with manual scoring | Radiation exposure, high cost |
| AI-Based CACS on Chest CT [50] | Mixed cohort (N=684) | 92.1% | N/A | Opportunistic screening potential | Non-gated CT, slightly lower accuracy |
| Traditional CACS (Manual) [74] | Symptomatic with obstructive CAD (N=65) | N/A | N/A | Prognostic value in asymptomatic | Limited value for plaque morphology |
Table 2: Efficacy Across Age Groups and Patient Subpopulations
| Methodology | Young Adults (<45 Years) | Asymptomatic / Primary Prevention | Symptomatic / Advanced CAD | Special Populations (e.g., ESRD) |
|---|---|---|---|---|
| Pulse Wave ML | Not validated | Not validated | Not validated | High accuracy (84.1%) for severity stratification [34] |
| CAC Scoring (Traditional) | High prognostic value [75] | Strong risk stratification power [72] | Limited value for plaque phenotyping [74] | Clinical standard, but requires imaging |
| AI-CAC on CT | Potential for early screening | Suitable for risk stratification | Suitable for quantification | Suitable, but with radiation burden |
Detailed Experimental Protocols
Pulse Wave-Driven Machine Learning for CAC
Objective: To develop a non-invasive method for assessing CAC severity in patients with end-stage renal disease (ESRD) undergoing hemodialysis using radial artery pulse waveforms and machine learning [34].
Patient Cohort: 58 patients with ESRD undergoing hemodialysis. Median age: 62.0 years (IQR: 31.0–84.0); 74.1% male, 25.9% female [34].
CAC Severity Classification: CAC severity was assessed using low-dose computed tomography (LDCT) and classified using Agatston scores:
- No calcification (0)
- Mild (1–100)
- Moderate (101–400)
- Severe (> 400) [34].
Pulse Wave Data Acquisition:
- Radial artery pulse waveforms were recorded before, hourly during, and after hemodialysis.
- Multiple features were extracted, capturing waveform morphology, descending limb characteristics, complexity, distribution, and mean value.
Machine Learning Model:
- Algorithm: Gradient Boosting Decision Tree (GBDT)
- Training/Validation: Fivefold cross-validation
- Performance: Average accuracy of 84.1%, macro-AUC of 0.962 [34].
AI-Based Automated CAC Scoring on CT
Objective: To validate artificial intelligence software for automatic coronary artery calcium scoring on both cardiac and non-ECG-triggered chest CT scans [50].
Study Population: 684 participants (59 ± 4.8 years; 48.8% men) who underwent both cardiac and chest CT [50].
Reference Standard: Manual Agatston score (AS) and volume score (VS) on cardiac CT.
AI Analysis: Fully automated AI-based software for CAC detection and scoring.
Performance Assessment:
- Sensitivity and accuracy for CAC detection.
- Intraclass correlation coefficient (ICC) for agreement on AS and VS.
- Bland-Altman analysis for mean differences.
- Cohen’s kappa for risk category stratification (0; 1–99; 100–299; ≥300) [50].
Key Findings:
- Detection Rate: 98.1% in cardiac CT (accuracy 97.1%); 92.4% in chest CT (accuracy 92.1%).
- Agreement: Excellent agreement with manual scoring (ICC for AS: 0.997 in cardiac CT, 0.992 in chest CT).
- Risk Classification: Cohen’s kappa = 0.952 for cardiac CT and 0.901 for chest CT [50].
CAC Testing in Young Adults
Objective: To evaluate the utility of CAC scoring for risk stratification in young adults (<45 years old) [75].
Prevalence: Approximately 10% of young adults in the general population have prevalent CAC. This prevalence rises to one in three among young adults with traditional atherosclerotic cardiovascular disease (ASCVD) risk factors [75].
Prognostic Value: The presence of CAC in young adults confers a stepwise higher risk uniquely for incident ASCVD mortality, and not for non-ASCVD causes [75].
Clinical Utility: CAC scanning in younger patients can identify premature atherosclerosis and facilitate earlier risk factor reduction with pharmacotherapy [75].
Signaling Pathways and Workflows
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Analytical Tools for CAC Detection Research
| Item / Solution | Function / Application | Example Use Case |
|---|---|---|
| Dual-Source CT Scanner | High-resolution cardiac imaging for Agatston scoring | Acquisition of reference standard CAC scores [74] [50] |
| Pulse Wave Acquisition Device | Non-invasive recording of radial artery waveforms | Capturing input signals for ML-based CAC assessment [34] |
| NIRS-IVUS System | In-vivo plaque characterization (lipid core, calcium) | Validation of plaque morphology and composition [74] |
| GBDT Algorithm | Machine learning for multi-class classification | Stratifying CAC severity into 4 groups from pulse waves [34] |
| Weighted Random Forest | ML for binary classification tasks | Differentiating LVE from non-LVE in heart failure patients [73] |
| AI-Based CAC Software | Automated quantification of Agatston scores | High-throughput, reproducible CAC scoring on CT scans [50] |
| Pulse Wave Feature Set | Parameters describing waveform morphology | Input features for training ML models (e.g., NA, NB, PB) [34] |
This performance analysis demonstrates a shifting paradigm in coronary artery calcification detection. Traditional and AI-enhanced CT scoring remain the gold standards for definitive CAC quantification across broad populations, with particular prognostic value in young adults [75] [50]. However, pulse wave-driven machine learning emerges as a highly promising, non-invasive alternative for specific clinical subpopulations, such as patients with ESRD, achieving an accuracy of 84.1% in stratifying CAC severity [34]. The stratified efficacy of each modality underscores the necessity for context-dependent application. Future research should focus on validating pulse wave ML in broader, multi-ethnic cohorts and integrating it with polygenic risk scores to enable comprehensive, personalized cardiovascular risk assessment from birth.
Coronary artery calcification (CAC) represents a critical cardiovascular risk driver in patients with chronic kidney disease (CKD) and end-stage renal disease (ESRD), with CAC severity directly correlated with all-cause mortality and cardiovascular hospitalization risks [34]. Traditional CAC detection via computed tomography (CT) involves radiation exposure and high costs, limiting its utility for routine monitoring in this vulnerable population [34]. This guide evaluates the performance of pulse wave-driven machine learning against other emerging detection methodologies for CAC and related complications in high-risk CKD/ESRD cohorts, providing researchers with comparative experimental data and technical protocols.
Comparative Performance Analysis of Detection Modalities
The table below summarizes performance metrics across four advanced detection approaches applied to CKD/ESRD patient cohorts:
Table 1: Performance Metrics of Detection Modalities in CKD/ESRD Cohorts
| Detection Modality | Target Condition | Patient Cohort | Algorithm/Model | Key Performance Metrics | Reference |
|---|---|---|---|---|---|
| Pulse Wave Analysis + ML | Coronary Artery Calcification (CAC ≥100 AU) | 124 CKD Stage 5 patients | Machine Learning (Pulse Wave Features) | Accuracy: >80%, Superior balanced accuracy vs. TRF models | [8] |
| Pulse Wave Analysis + GBDT | Coronary Artery Calcification Severity | 58 ESRD hemodialysis patients | Gradient Boosting Decision Tree (GBDT) | Accuracy: 84.1%, Macro-AUC: 0.962 | [34] |
| SWE + SRI Ultrasound | Moderate-to-Severe Renal Fibrosis | 202 CKD patients | Integrated Diagnostic Model | AUC: 0.83, Sensitivity: 80.4%, Specificity: 75.8% | [76] |
| Retinal Fundus Imaging + DL | Advanced CKD (eGFR <30 mL/min/1.73 m²) | 17,442 patients with fundus images | EfficientNet-B3 (Bilateral Images) | AUC: 0.868, Sensitivity: 0.792, Specificity: 0.788 | [77] |
Performance analysis reveals pulse wave-driven machine learning achieves superior balanced accuracy for CAC detection compared to traditional risk factor (TRF) models, particularly in younger CKD patients [8]. The Gradient Boosting Decision Tree (GBDT) model demonstrates exceptional capability in classifying CAC severity among ESRD patients undergoing hemodialysis, with near-perfect macro-AUC scores [34]. For renal fibrosis detection, the integration of shear wave elastography (SWE) and super-resolution imaging (SRI) provides robust diagnostic performance, while retinal fundus imaging offers a novel, non-invasive approach for advanced CKD identification [76] [77].
Detailed Experimental Protocols
Pulse Wave-Driven CAC Detection in ESRD Hemodialysis
Patient Cohort: 58 ESRD patients undergoing hemodialysis, median age 62.0 years (IQR: 31.0-84.0), 74.1% male [34].
CAC Assessment Protocol:
- Gold Standard: Low-dose computed tomography (LDCT) with Agatston scoring
- CAC Severity Classification: No calcification (0), Mild (1-100), Moderate (101-400), Severe (>400)
Pulse Wave Data Collection:
- Device: Radial artery pulse wave recording device (specific model not cited)
- Timing: Recordings taken before, hourly during, and after hemodialysis
- Parameters: Waveform morphology, descending limb characteristics, complexity/distribution features, mean values, full-process stereoscopic parameters
Machine Learning Pipeline:
- Feature Extraction: Morphological parameters including main wave, tidal wave, and dicrotic wave characteristics
- Model: Gradient Boosting Decision Tree (GBDT)
- Validation: Five-fold cross-validation with independent test set
- Performance Metrics: Classification accuracy, macro-AUC, sensitivity, specificity
Key Findings: Progressive waveform simplification was observed with increasing CAC severity, characterized by attenuated tidal waves and smoother overall morphology. The GBDT model achieved 84.1% accuracy and 0.962 macro-AUC in cross-validation, with comparable performance (83.9% accuracy, 0.961 macro-AUC) on the independent test set [34].
Renal Fibrosis Detection via Advanced Ultrasound
Patient Cohort: 202 CKD patients who underwent renal biopsy, categorized into mild fibrosis (n=107) versus moderate-to-severe renal fibrosis (MSRF, n=95) groups [76].
Imaging Protocol:
- Equipment: Mindray Resona A20 Pro ultrasound diagnostic instrument with SC7-1U probe
- Shear Wave Elastography (SWE): Measured Young's modulus and viscosity in renal cortex with rectangular sample box (1×1 cm)
- Super-Resolution Imaging (SRI): Microvascular imaging with contrast agent (SonoVue 0.5 mL) injection
- Parameters: Elasticity values (SWE) and vascular density (SRI)
Diagnostic Model Development:
- Statistical Analysis: LASSO logistic regression to identify independent risk factors
- Model Configurations: Isolated, series, parallel, and integrated diagnostic strategies
- Integrated Model: Combined SWE elasticity and SRI vascular density using logistic algorithm
- Validation: Receiver operating characteristic (ROC) analysis with AUC calculation
Key Findings: Age, diabetes history, eGFR, elasticity, and vascular density were independently associated with MSRF. The integrated model significantly outperformed individual parameter use (AUC: 0.83, sensitivity: 80.4%, specificity: 75.8%) [76].
Retinal Fundus Imaging for Advanced CKD Detection
Patient Cohort: 42,963 clinical visits from 17,442 patients with paired fundus imaging and eGFR measurements [77].
Image Acquisition and Preprocessing:
- Equipment: Multiple fundus cameras (INFINITT, VBTEC Inc., GE Healthcare)
- Standardization: Cropping and padding to square format, resizing to 512×512 pixels
- Enhancement: Graham's method for brightness standardization and detail enhancement
Deep Learning Framework:
- Architectures: EfficientNet-B3 and EfficientNetV2-S
- Model Configurations:
- Model A: Single fundus image only
- Model B: Single image with demographic features (age, sex)
- Model C: Bilateral fundus images
- Training Strategy: 5-fold cross-validation ensemble versus single model
- Class Imbalance Handling: Undersampling majority class with weighted loss function
Key Findings: The bilateral-image model (Model C) with EfficientNet-B3 architecture and 5-fold CV ensemble achieved superior performance (AUC: 0.868, sensitivity: 0.792, specificity: 0.788). Performance was particularly strong in diabetic patients, reflecting shared microvascular pathophysiology [77].
Detection Workflow and Pathophysiological Basis
Diagram 1: Multimodal Detection Workflow for CKD/ESRD Complications. This flowchart illustrates three parallel detection methodologies (pulse wave analysis, advanced ultrasound, and retinal imaging) with their respective processing stages, unified by shared pathophysiological mechanisms in CKD/ESRD.
The diagram above illustrates how each detection modality leverages shared pathophysiological pathways. Pulse wave morphology reflects vascular stiffness and endothelial dysfunction [34]. Renal ultrasound parameters capture tissue elasticity changes from fibrosis and microvascular rarefaction [76] [78]. Retinal fundus imaging identifies microvascular changes that parallel glomerular damage due to shared susceptibility to hyperglycemia-induced endothelial damage [77].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Essential Research Materials for CKD/ESRD Detection Studies
| Category | Specific Product/Technology | Research Application | Key Features/Specifications | |
|---|---|---|---|---|
| Pulse Wave Acquisition | SphygmoCor System (AtCor Medical) | Radial artery pulse wave collection for CAC assessment | Validated pulse wave analysis, research-grade signals | [8] |
| Ultrasound Systems | Mindray Resona A20 Pro with SC7-1U probe | Shear wave elastography and super-resolution imaging | High-frequency probe, elastography quantification, microvascular imaging capabilities | [76] |
| Ultrasound Contrast Agent | SonoVue microbubbles | Super-resolution imaging microvascular assessment | Phospholipid-shelled sulfur hexafluoride microbubbles (1-10 μm), enables capillary visualization | [76] [78] |
| Fundus Imaging Systems | INFINITT, VBTEC Inc., GE Healthcare cameras | Retinal image acquisition for CKD correlation | Standardized image formats, compatibility with preprocessing pipelines | [77] |
| Machine Learning Frameworks | Gradient Boosting Decision Tree (GBDT) | CAC severity classification | Handles mixed data types, robust performance on medium-sized datasets | [34] |
| Deep Learning Architectures | EfficientNet-B3, EfficientNetV2-S | Image-based CKD classification | Balance of accuracy and efficiency, transfer learning capabilities | [77] |
| Data Processing Tools | Graham's image processing method | Fundus image standardization | Brightness normalization, vascular detail enhancement | [77] |
This toolkit enables researchers to replicate the experimental protocols and validation studies cited in this guide. The selection emphasizes research-grade equipment with validated performance in CKD/ESRD applications, particularly focusing on non-invasive technologies that capture cardiovascular and renal pathology through different but complementary physiological windows.
Pulse wave-driven machine learning demonstrates superior detection capabilities for coronary artery calcification in high-risk CKD and ESRD patient cohorts, achieving >80% accuracy and 0.962 macro-AUC in severity classification [8] [34]. This performance advantage stems from its direct capture of vascular pathophysiology through waveform morphology analysis, providing a non-invasive, cost-effective alternative to CT-based CAC assessment. When integrated with complementary modalities like advanced ultrasound and retinal imaging, researchers can establish a comprehensive non-invasive detection framework for the multifaceted complications of CKD and ESRD, potentially enabling earlier intervention and improved patient outcomes in this vulnerable population.
Coronary Artery Disease (CAD) represents a staggering global health and economic challenge, affecting 20-40% of the general population and constituting 27% of the economic cardiovascular disease burden in Europe alone [79]. In the United States, heart attacks claim more lives than all cancers combined, with fatal heart attack victims typically experiencing no symptoms until minutes before death [80]. This silent progression underscores the critical need for early detection of high-risk asymptomatic individuals. The economic burden of cardiovascular disease is profound, with approximately $407.3 billion in CVD-associated costs incurred in the US between 2018 and 2019 [81]. Despite this overwhelming burden, healthcare systems invest disproportionately more in cancer screening than in asymptomatic atherosclerotic cardiovascular disease (ASCVD) detection, with payers spending over 20 times more on asymptomatic cancer screening than for ASCVD screening [80].
Coronary Artery Calcium (CAC) scoring has emerged as a powerful non-invasive tool for quantifying calcified atherosclerotic plaques within coronary arteries, providing a direct measure of coronary atherosclerosis burden [81] [82]. Unlike traditional risk factors alone, CAC scoring enables personalized risk assessment by directly visualizing and quantifying subclinical coronary atherosclerosis. Current guidelines, including those from the American College of Cardiology/American Heart Association (ACC/AHA), recommend CAC assessment to guide preventive therapy initiation, particularly for intermediate-risk patients [81]. The economic value proposition of CAC screening lies in its potential to reclassify risk accurately, thereby optimizing statin therapy allocation—initiating treatment in those who will benefit most while avoiding unnecessary treatment in low-risk individuals [79] [82].
Comparative Methodologies for CAC Detection and Quantification
Established CAC Scoring Techniques
Multiple methodologies have been developed for CAC assessment, each with distinct technical requirements, economic considerations, and clinical applications. The table below summarizes the primary CAC detection modalities and their characteristics.
Table 1: Comparison of CAC Detection and Scoring Methodologies
| Methodology | Technical Requirements | Cost Considerations | Accuracy/Performance | Clinical Applications |
|---|---|---|---|---|
| ECG-Gated Cardiac CT (Agatston Score) | Dedicated ECG-gated non-contrast CT; specific software for Agatston calculation [81] | Higher direct costs; requires specialized equipment and personnel [81] | Reference standard; quantitative assessment [81] | Gold standard for CAC scoring; guided statin initiation [81] |
| Visual CAC Assessment on Non-Gated CT | Routine non-gated chest CT; no specific imaging requirements [79] | Cost-free additional information; uses existing scans [79] | Strong diagnostic/prognostic value; ordinal scoring (0-3) [79] | Opportunistic screening; risk stratification when CAC is incidentally noted [79] |
| AI-Automated CAC Scoring | Various CT protocols (gated, non-gated, LDCT); AI software [81] | Reduced reading time; potential for automated quantification [81] | Excellent agreement with manual scoring (κ=0.89-0.90) [81] | High-volume imaging labs; quantitative scoring from non-dedicated CT [81] |
| Pulse Wave Velocity with mHealth | Consumer devices (smart scales, BP cuffs, activity trackers) [83] | Low-cost consumer devices; home monitoring [83] | Modest association with CVD risk; R²=0.02-0.36 for risk factors [83] | Population screening; longitudinal monitoring; research applications [83] |
| Machine Learning Biomarker Models | Circulating biomarkers; clinical risk factors; ML algorithms [84] | Variable cost based on biomarkers; ~$220-1,410 per assessment [84] | Limited accuracy improvements (3%) with substantial cost increases [84] | Pre-screening to identify candidates for advanced imaging [84] |
Experimental Protocols and Workflows
The experimental workflow for CAC assessment varies significantly based on the methodology employed. For traditional CAC scoring, the protocol involves specific image acquisition parameters followed by either manual or automated analysis.
Table 2: Key Experimental Protocols for CAC Assessment
| Methodology | Image Acquisition Protocol | Analysis Technique | Output Metrics |
|---|---|---|---|
| Standard Agatston Scoring | ECG-gated non-contrast CT; slice thickness ≤3mm; 130-kV [79] [81] | Calcium lesion identification; area measurement; density weighting [81] | Agatston score (0, 1-10, 11-100, 101-400, >400) [81] |
| Visual CAC Assessment | Non-gated chest CT; varying kV settings and slice thickness [79] | Visual inspection for CAC presence/extent; ordinal scoring [79] | Simple presence/absence; vessel-specific count; ordinal score (0-3, 0-12) [79] |
| AI-Automated Scoring | Gated or non-gated CT; various protocols [81] | CNN-based coronary segmentation; calcium detection; artery labeling [81] | Automated Agatston score; calcium volume; vessel-specific scores [81] |
| PWV with mHealth | Withings smart scale; BP cuff; activity tracker [83] | Ballistocardiography; impedance plethysmography [83] | PWV values; correlation with cardiovascular risk factors [83] |
CAC Screening Methodologies and Clinical Workflow: This diagram illustrates the complete pathway from patient identification through methodology selection to clinical action, highlighting the multiple approaches available for coronary artery calcium assessment.
Economic and Clinical Outcome Data
Cost-Effectiveness Analyses of CAC Screening
Multiple studies have evaluated the economic value of CAC screening, particularly for guiding statin prescription in intermediate-risk populations. A recent cost-utility analysis conducted in Thailand demonstrated that CAC screening was cost-effective compared to current practice without CAC assessment, with incremental cost-effectiveness ratios falling within acceptable thresholds for healthcare resource allocation [82]. The analysis utilized a hybrid model combining decision tree and Markov models over a 35-year time horizon, factoring in direct medical costs, transportation, food, accommodation, and opportunity costs [82].
The economic advantage of CAC screening stems from its ability to precisely target preventive therapies. In intermediate-risk patients, CAC scoring can reclassify risk in approximately 50-60% of cases, allowing for more appropriate allocation of statin therapy [82]. For the 44% of patients with CAC=0, who have exceptionally favorable prognosis (event rate of 0.4% over 3-5 years), statin therapy can be safely deferred, avoiding unnecessary medication costs and potential side effects [80]. Conversely, for patients with CAC≥100, who face substantially higher event rates (4.3-7.2%), high-potency statin therapy is clearly justified [80].
Accuracy and Prognostic Value Comparison
The diagnostic and prognostic performance of various CAC assessment methods has been extensively studied. Visual assessment of CAC on non-gated CT demonstrates strong predictive value for coronary events and mortality, with the vessel-specific extent-based ordinal score and simple visual score proving most optimal for clinical use [79]. These visual methods show high sensitivity (71-94%) and positive predictive value (88-100%) for detecting clinically significant CAC (CACS≥100) when compared to standard Agatston scoring [79].
AI-automated CAC scoring systems have demonstrated remarkable agreement with manual scoring, with Cohen's kappa values of 0.89-0.90 (p<0.001) in validation studies [81]. These systems offer substantial efficiency improvements, reducing scoring time from 261 seconds manually to just 3.5±2.1 seconds automatically, representing a 98.7% reduction in processing time [81]. This efficiency gain has significant economic implications for high-volume imaging centers.
Economic Value Proposition of CAC Screening Methods: This diagram illustrates the cost-benefit relationship across different CAC screening approaches, highlighting how various methodologies balance cost considerations with clinical outcomes.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Research Reagent Solutions for CAC Detection and Validation Studies
| Reagent/Technology | Function/Application | Representative Examples | Considerations for Research Use |
|---|---|---|---|
| CT Imaging Platforms | CAC quantification and visualization | GE Revolution CT, Siemens Healthineers platforms [61] | Standardized protocols essential; kV settings impact Agatston accuracy [79] |
| AI Software Solutions | Automated CAC segmentation and scoring | General Electric CardIQ Suite, Arytra DeepC, Coreline AVIEW CAC [81] | Validation against manual scores required; generalizability across populations [81] |
| Circulating Biomarkers | mVC detection and risk stratification | Copeptin, choline, osteoprotegerin, angiopoietin 2 [84] | Cost-effectiveness varies; incremental value over clinical factors must be demonstrated [84] |
| mHealth Devices | PWV measurement and home monitoring | Withings smart scale, BP cuff, activity trackers [83] | Adherence challenges; technical reliability concerns; consumer-grade vs. medical-grade [83] |
| Machine Learning Algorithms | Feature selection and classification | Logistic regression with elastic net, SVM with recursive feature elimination, random forests [84] | Model interpretability; clinical implementation feasibility; regulatory considerations [84] |
The economic value of non-invasive CAC screening extends beyond simple cost-per-test calculations to encompass broader societal benefits through accurate risk stratification and targeted prevention. The strong prognostic value of CAC, particularly the excellent prognosis associated with a CAC score of 0, provides opportunities to safely defer statin therapy in low-risk individuals, while identifying high-risk individuals who derive substantial benefit from intensive prevention [79] [80]. From a health systems perspective, CAC screening represents a paradigm shift from population-based risk assessment using traditional factors alone toward personalized prevention based on direct atherosclerosis measurement.
Future research directions should focus on optimizing the integration of pulse wave velocity and machine learning approaches with established CAC screening methodologies. While current evidence supports the cost-effectiveness of traditional CAC scoring, the economic value of novel approaches combining mHealth devices, circulating biomarkers, and artificial intelligence requires further validation in diverse populations [83] [84]. The promising technical performance of AI-automated CAC scoring systems, coupled with their dramatic efficiency improvements, suggests that these technologies will play an increasingly important role in expanding access to CAC assessment while controlling costs [81]. As healthcare systems worldwide struggle with escalating cardiovascular disease burdens, non-invasive CAC screening offers a evidence-based, cost-effective strategy for personalizing prevention and reducing the enormous economic impact of coronary artery disease.
Conclusion
The validation of pulse wave-driven machine learning models represents a paradigm shift in non-invasive cardiovascular risk stratification, offering a highly accurate, cost-effective, and accessible method for detecting coronary artery calcification. Recent studies demonstrate robust performance, with models achieving over 80% balanced accuracy and 0.96 AUC in classifying CAC severity, particularly in high-risk populations like CKD and ESRD patients. Successful clinical integration hinges on addressing key challenges: ensuring demographic diversity in training data, adhering to evolving regulatory frameworks like the PRIME 2.0 checklist, and maintaining rigorous post-market surveillance. Future directions should focus on large-scale, prospective multi-center trials to solidify clinical utility, exploration of generative AI for enhanced feature discovery, and development of standardized protocols for seamless implementation into routine cardiology and nephrology practice, ultimately enabling earlier intervention and improved patient outcomes.
References
- 1. Atherosclerotic Diseases in Chronic Kidney Disease [https://pubmed.ncbi.nlm.nih.gov/39551490/]
- 2. The Chronic Renal Insufficiency Cohort Study - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/39154888/]
- 3. Progression of Coronary Artery Calcification and Risk ... [https://www.sciencedirect.com/science/article/pii/S027263862400920X]
- 4. Artificial Intelligence in Coronary Artery Calcium Scoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10814920/]
- 5. Development and validation of a simple-to-use coronary ... [https://link.springer.com/article/10.1007/s42058-025-00189-w]
- 6. Pulse wave-driven machine learning for the non-invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12395768/]
- 7. Pulse wave-driven machine learning for the non-invasive ... [https://pubmed.ncbi.nlm.nih.gov/40883745/]
- 8. Leveraging pulse wave signal properties for coronary ... [https://www.sciencedirect.com/science/article/pii/S0010482525008704]
- 9. Inflammatory markers and calcification of coronary arteries ... [https://pubmed.ncbi.nlm.nih.gov/40060173/]
- 10. Functional versus morphological assessment of vascular ... [https://www.nature.com/articles/s41598-021-96998-x]
- 11. The Relationship between coronary as assessed... artery calcification [https://pubmed.ncbi.nlm.nih.gov/21967024/]
- 12. Cross-Sectional Relations of Arterial Stiffness, Pressure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4199901/]
- 13. Association between brachial-ankle pulse velocity and... wave [https://cardiab.biomedcentral.com/articles/10.1186/s12933-015-0311-3]
- 14. -driven Pulse for the non-invasive assessment... wave machine learning [https://link.springer.com/article/10.1186/s12938-025-01436-y]
- 15. Leveraging pulse wave signal properties for coronary ... [https://pubmed.ncbi.nlm.nih.gov/40482559/]
- 16. Predicting Coronary Artery Lesion Severity Using Pulse ... [https://pubmed.ncbi.nlm.nih.gov/40396324/]
- 17. Coronary Calcification: Types, Morphology and Distribution [https://pmc.ncbi.nlm.nih.gov/articles/PMC12042292/]
- 18. Why Current Detection of Vascular Calcification Falls Short ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11679638/]
- 19. Advances in Artificial Intelligence for Non-ECG-Gated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590512/]
- 20. Prognostic value of coronary calcification detected via non- ... [https://www.sciencedirect.com/science/article/pii/S2352906724002264]
- 21. Fully automated coronary artery calcium score and risk ... [https://www.sciencedirect.com/science/article/pii/S2352906724002598]
- 22. Machine-Learning Based Detection of Coronary Artery ... [https://arxiv.org/html/2511.11093v1]
- 23. Three-Dimensional Arterial Pulse Signal Acquisition in Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8156466/]
- 24. Novel Methods for Pulse Wave Velocity Measurement - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4609308/]
- 25. Method for Extracting Arterial Pulse Waveforms from ... [https://www.mdpi.com/1424-8220/25/14/4389]
- 26. Multimodal Finger Pulse Wave Sensing: Comparison of ... [https://www.mdpi.com/1424-8220/22/19/7566]
- 27. Determinants of hand pulse wave velocity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11066034/]
- 28. Pulse Wave Velocity in Atherosclerosis [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2019.00041/full]
- 29. Temporal complexity in photoplethysmography and its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10513039/]
- 30. Morphological features of the photoplethysmographic signal [https://pmc.ncbi.nlm.nih.gov/articles/PMC10561251/]
- 31. A benchmark for machine-learning based non-invasive ... [https://www.nature.com/articles/s41597-023-02020-6]
- 32. Association between Pulse Wave Velocity and Coronary ... [https://pubmed.ncbi.nlm.nih.gov/26269003/]
- 33. Artificial Intelligence in CT Angiography for the Detection of ... [https://pubmed.ncbi.nlm.nih.gov/40234162/]
- 34. Pulse wave-driven machine learning for the non-invasive ... [https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-025-01436-y]
- 35. Construction and Validation of a Predictive Model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11226989/]
- 36. Prediction of Percutaneous Coronary Intervention Success ... [https://pubmed.ncbi.nlm.nih.gov/40644630/]
- 37. Comparison of the performance of gradient boost, linear ... [https://www.sciencedirect.com/science/article/pii/S2666544125000528]
- 38. Basic Comparison Between RandomForest, SVM, and ... [https://medium.com/@ap.nattapoj_st/basic-comparison-between-randomforest-svm-and-xgboost-0e5862871175]
- 39. XGBoost vs LightGBM: How Are They Different [https://neptune.ai/blog/xgboost-vs-lightgbm]
- 40. Comparative analysis of machine learning models for ... [https://www.sciencedirect.com/science/article/pii/S0167527325004863]
- 41. Diagnostic performance of coronary artery disease ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1575230/full]
- 42. The Machine Learning Models in Major Cardiovascular ... [https://www.jmir.org/2025/1/e68872]
- 43. Quantitative comparison of the performance of acoustic ... [https://www.nature.com/articles/s41598-025-98488-w]
- 44. Real-time beat-to-beat pulse wave velocity estimation [https://link.springer.com/article/10.1007/s11517-025-03417-8]
- 45. Cardiovascular risk assessment enhanced by automated ... [https://www.nature.com/articles/s41598-025-24189-z]
- 46. Ethical and Bias Considerations in Artificial Intelligence ... [https://www.sciencedirect.com/science/article/pii/S0893395224002667]
- 47. Understanding, Identifying and Mitigating Algorithmic Bias ... [https://www.accuray.com/blog/overcoming-ai-bias-understanding-identifying-and-mitigating-algorithmic-bias-in-healthcare/]
- 48. Bias recognition and mitigation strategies in artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11897215/]
- 49. Algorithmic bias detection and mitigation: Best practices ... [https://www.brookings.edu/articles/algorithmic-bias-detection-and-mitigation-best-practices-and-policies-to-reduce-consumer-harms/]
- 50. Validation of artificial intelligence software for automatic ... [https://www.sciencedirect.com/science/article/pii/S0720048X25004097]
- 51. Evaluating the generalizability of an automated coronary ... [https://www.nature.com/articles/s41598-025-05785-5]
- 52. Cardiology still No. 2 in FDA -cleared clinical AI algorithms, trailing only... [https://cardiovascularbusiness.com/topics/artificial-intelligence/cardiology-still-no-2-fda-cleared-clinical-ai-algorithms-trailing-only-radiology]
- 53. PRIME 2.0: An Update to The Proposed Requirements for ... [https://www.sciencedirect.com/science/article/pii/S1936878X25004668]
- 54. PRIME 2.0: An Update to The Proposed Requirements for ... [https://pubmed.ncbi.nlm.nih.gov/40892627/]
- 55. PRIME 2.0: Updated AI Checklist for Cardiac Imaging ... [https://www.linkedin.com/posts/partho-sengupta-13262678_cardioai-medicalimaging-prime2-activity-7366915033823412229-VUcA]
- 56. AHA 2025: Late-Breaking Data Reinforce the Prognostic ... [https://ir.heartflow.com/news-releases/news-release-details/aha-2025-late-breaking-data-reinforce-prognostic-power-ai-driven]
- 57. TCT 2025 Late-Breaking Science: Quantitative Assessment ... [https://cleerlyhealth.com/press/tct-2025-late-breaking-science]
- 58. Artificial Intelligence and Coronary Calcium Scoring: Enhancing... Artery [https://ijcva.org/articles/artificial-intelligence-and-coronary-artery-calcium-scoring-enhancing-cardiovascular-risk-assessment/doi/ijca.2025.54227]
- 59. Workflow Integration Analysis of a Human Factors-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8474147/]
- 60. Usability Challenges in Electronic Health Records: Impact on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12206486/]
- 61. Development and validation of a novel nomogram to predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12232581/]
- 62. Human–machine teaming is key to AI adoption: clinicians' ... [https://www.nature.com/articles/s41746-022-00597-7]
- 63. AI and Technology Enabled Clinical Workflow Redesign - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11848050/]
- 64. Using a Clinical Workflow Analysis to Enhance eHealth ... [https://mhealth.jmir.org/2021/3/e18534]
- 65. Performance of fully automated deep-learning-based ... [https://link.springer.com/article/10.1007/s00330-025-11559-4]
- 66. Deep learning-based coronary calcium score derived from ... [https://cardiab.biomedcentral.com/articles/10.1186/s12933-025-02934-y]
- 67. Artificial intelligence applied to coronary artery calcium ... [https://www.nature.com/articles/s41746-024-01308-0]
- 68. Machine Learning Model for Predicting Coronary Heart ... [https://cardio.jmir.org/2025/1/e68066]
- 69. The distribution of artificial intelligence–derived retinal ... [https://www.e-jcpp.org/journal/view.php?doi=10.36011/cpp.2025.7.e14]
- 70. Pulse Wave AI Detects Heart Calcium Non-Invasively [https://scienmag.com/pulse-wave-ai-detects-heart-calcium-non-invasively/]
- 71. A non-invasive prediction model for coronary artery ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1592593/full]
- 72. Coronary Artery Calcification; report from the Multi-Ethnic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5108577/]
- 73. Pulse wave signal-driven machine learning for identifying ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11193305/]
- 74. Efficacy of Coronary Calcium Score in Predicting Coronary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11307846/]
- 75. Coronary Artery Calcium Testing in Young Adults - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9830553/]
- 76. Combining Super-Resolution Imaging and Shear Wave ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12227321/]
- 77. Prediction of advanced chronic kidney disease through ... [https://www.nature.com/articles/s41598-025-21366-y]
- 78. Advanced ultrasound methods to improve chronic kidney ... [https://www.nature.com/articles/s44303-024-00023-5]
- 79. The Clear Value of Coronary Artery Calcification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10899125/]
- 80. Coronary artery calcium testing: A call for universal coverage [https://pmc.ncbi.nlm.nih.gov/articles/PMC6525277/]
- 81. Artificial Intelligence in Coronary Artery Calcium Scoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11205094/]
- 82. Cost-utility analysis of Coronary Artery Calcium screening to ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0330425]
- 83. Activity Tracking's Newest Companion - Pulse Wave Velocity [https://pmc.ncbi.nlm.nih.gov/articles/PMC6084800/]
- 84. Balancing accuracy and cost in machine learning models ... [https://www.nature.com/articles/s41598-025-02457-2]