Resolving Material Degradation in Biomedical Applications: Strategies for Biomaterials, Drug Delivery, and Implants
This article provides a comprehensive overview of the critical challenge of material degradation in the biomedical field, tailored for researchers, scientists, and drug development professionals.
Resolving Material Degradation in Biomedical Applications: Strategies for Biomaterials, Drug Delivery, and Implants
Abstract
This article provides a comprehensive overview of the critical challenge of material degradation in the biomedical field, tailored for researchers, scientists, and drug development professionals. It explores the fundamental mechanisms behind the breakdown of polymers, metals, and biotherapeutics, and details advanced methodologies for characterizing and leveraging this degradation for drug delivery and tissue engineering. The content further covers practical troubleshooting and optimization strategies to prevent premature failure, and concludes with a rigorous examination of validation frameworks and comparative forced degradation studies essential for ensuring product safety, efficacy, and regulatory compliance.
Understanding the Fundamentals: Mechanisms and Impacts of Biomaterial Degradation
In the field of biomedical applications, biodegradation is defined as the biological catalytic reaction of reducing complex macromolecules into smaller, less complex molecular structures (by-products) [1]. For researchers and drug development professionals, understanding this process is crucial for developing implants, drug delivery systems, and tissue engineering scaffolds that function safely within the biological environment.
The ideal biodegradable biomaterial must balance structural integrity with controlled breakdown, ensuring that degradation by-products are non-toxic and can be successfully metabolized and eliminated from the body [1]. This technical support center addresses the key experimental challenges and methodological considerations in characterizing and validating biomaterial degradation, providing essential troubleshooting guidance for your research.
Fundamental Concepts: FAQs on Biodegradation Mechanisms
What is the fundamental mechanism of biomaterial biodegradation? Biodegradation occurs through the cleavage of specific chemical functional groups in polymer chains via hydrolytic or enzymatic pathways. Key susceptible functional groups include ester, ether, amide, imide, thioester, and anhydride moieties. The degradation process transforms large polymer molecules into smaller, less complex by-products that can be metabolized or excreted [1].
How does biodegradation differ from simple dissolution? A critical distinction is that biodegradation involves chemical cleavage of molecular chains, while dissolution is merely a physical process where material dissolves without chemical breakdown. This distinction is essential for accurate characterization, as gravimetric analysis (measuring weight loss) alone cannot differentiate between these processes. Confirmatory chemical analysis is necessary to verify true degradation [1].
What are the ideal characteristics of biodegradable materials for biomedical applications? Desirable properties include: (1) no induction of sustained inflammatory or toxic response upon implantation; (2) appropriate shelf-life; (3) degradation time matching the healing or regeneration process; (4) appropriate mechanical properties for the intended application; (5) non-toxic degradation by-products that can be metabolized and cleared; and (6) appropriate permeability and processability [1].
Troubleshooting Experimental Challenges
Common Experimental Pitfalls and Solutions
Problem: Gravimetric analysis suggests degradation, but chemical analysis shows no change in molecular structure. Solution: This discrepancy often indicates material dissolution rather than true degradation. Supplement gravimetric measurements with chemical characterization techniques such as FTIR, NMR, or SEC to confirm chemical breakdown. Ensure your degradation medium matches the intended physiological environment (pH, enzyme presence) [1].
Problem: Inconsistent degradation rates between experimental batches. Solution: Batch-to-batch variability is common with natural polymers. Implement strict quality control measures and characterize raw material properties for each batch. Consider synthetic alternatives like PLGA, PLA, or PVA which offer more reproducible degradation profiles [2] [3].
Problem: Difficulty assessing degradation of liquid-based formulations. Solution: Physical degradation assessment approaches like surface erosion monitoring are unsuitable for liquid formulations. Transition to chemical characterization methods including viscosity measurements, molecular weight analysis via SEC, or monitoring of degradation by-products using HPLC or mass spectrometry [1].
Advanced Methodological Considerations
Problem: Need for real-time, non-invasive degradation monitoring. Solution: Current ASTM guidelines lack provisions for non-invasive, continuous monitoring. Develop customized methodologies using embedded sensors or optical techniques. Research is focusing on real-time assessment approaches that provide continuous data without sample destruction [1].
Problem: Ensuring biological relevance of in vitro degradation models. Solution: Standard phosphate-buffered saline (PBS) may not adequately simulate physiological conditions. Incorporate relevant enzymes, adjust pH to match specific tissue environments, and consider mechanical stress factors that mimic in vivo conditions [1] [4].
Standard Experimental Protocols and Methodologies
Comprehensive Degradation Assessment Workflow
The following workflow outlines a rigorous approach for biomaterial degradation assessment, integrating physical, chemical, and mechanical evaluation methods:
Detailed Methodological Approaches
Gravimetric Analysis (Mass Loss)
- Protocol: Accurately weigh samples (W₀) before immersion in degradation medium. At predetermined timepoints, remove samples, gently rinse with deionized water, dry to constant weight, and record dry weight (Wₜ). Calculate percentage mass loss as: [(W₀ - Wₜ)/W₀] × 100.
- Troubleshooting: Ensure complete drying without degrading samples. Use controls to account for potential leaching of unbound additives. Remember that mass loss alone cannot confirm degradation [1].
Chemical Structure Analysis via FTIR
- Protocol: Collect FTIR spectra of samples before and during degradation. Focus on changes in characteristic functional group absorptions (e.g., ester C=O stretch at ~1740 cm⁻¹, amide N-H bend at ~1550 cm⁻¹).
- Troubleshooting: Ensure consistent sample preparation and scanning parameters. Look for both disappearance of original bonds and appearance of new degradation products [1].
Molecular Weight Distribution via Size Exclusion Chromatography (SEC)
- Protocol: Dissolve sample aliquots in appropriate solvent (e.g., THF for synthetic polymers). Analyze using SEC system with refractive index detection. Compare molecular weight distributions over time.
- Troubleshooting: Ensure complete dissolution without further degradation. Use appropriate molecular weight standards for calibration [1].
Characterization Techniques: Advantages and Limitations
Comparative Analysis of Degradation Assessment Methods
Table 1: Degradation Assessment Techniques with Applications and Limitations
| Assessment Method | Key Parameters Measured | Advantages | Limitations |
|---|---|---|---|
| Gravimetric Analysis | Mass loss over time | Simple, cost-effective, quantitative | Cannot distinguish dissolution from degradation; requires drying |
| Scanning Electron Microscopy (SEM) | Surface morphology, erosion patterns | Visual evidence of surface changes; high resolution | Destructive; sample preparation may introduce artifacts |
| Fourier Transform Infrared Spectroscopy (FTIR) | Chemical bond cleavage/formation | Confirms chemical degradation; identifies new functional groups | Limited sensitivity to subtle changes; surface-dominated for ATR-FTIR |
| Size Exclusion Chromatography (SEC) | Molecular weight distribution | Tracks backbone cleavage quantitatively | Requires solubility; may not detect crosslinking |
| Nuclear Magnetic Resonance (NMR) | Molecular structure of degradation products | Identifies specific cleavage products; quantitative | Expensive; requires specialized expertise |
| Mechanical Testing | Tensile strength, modulus | Directly measures functional property loss | Destructive; requires multiple samples for time course |
Interconnected Degradation Assessment Approaches
The most accurate degradation assessment comes from integrating multiple complementary techniques, as these approaches are interconnected and provide different perspectives on the degradation process:
Research Reagent Solutions for Degradation Studies
Table 2: Essential Materials for Biodegradation Research
| Material/Category | Examples | Function in Degradation Studies | Applications |
|---|---|---|---|
| Natural Polymers | Chitosan, silk fibroin, alginate, gelatin | Biocompatible, enzymatically degradable substrates | Tissue engineering, drug delivery [2] [5] |
| Synthetic Polymers | PLA, PLGA, PVA, PCL | Controlled degradation via hydrolytic cleavage; reproducible properties | Customizable implants, controlled release systems [2] [3] |
| Degradation Media | PBS, simulated body fluid, enzyme solutions | Simulate physiological environments for in vitro testing | Predictive degradation modeling [1] |
| Crosslinking Agents | Glutaraldehyde, genipin, PEG diacrylate | Control degradation rate through crosslink density | Tunable hydrogel systems [3] [5] |
| Analytical Standards | Molecular weight markers, degradation metabolites | Quantification and identification of degradation products | Method validation and standardization [1] |
Regulatory and Standardization Considerations
ASTM Guidelines and Current Limitations
Current ASTM F1635-11 guidelines specify that degradation should be monitored via:
- Mass loss (measured to 0.1% precision of total sample weight)
- Changes in molar mass (evaluated by solution viscosity or SEC)
- Mechanical testing [1]
However, these guidelines have notable limitations that researchers should address:
- They do not consider invasiveness of degradation approaches that may disturb ongoing degradation processes
- They lack provisions for continuous, real-time assessment
- They provide insufficient guidance for liquid-based formulations [1]
Future Directions in Degradation Assessment
Emerging approaches seek to address current methodological gaps through:
- Non-invasive continuous monitoring techniques that provide real-time data
- Multi-parameter assessment integrating physical, chemical, and biological responses
- Advanced analytical methods including AI-driven degradation prediction and modeling [1] [5]
Successful biodegradation assessment requires a comprehensive, multi-technique approach that confirms chemical degradation beyond simple physical changes. Researchers should:
- Combine gravimetric analysis with chemical characterization to distinguish true degradation from dissolution
- Validate in vitro methods against relevant biological environments
- Address current ASTM limitations through supplementary methodologies
- Consider the interconnected nature of chemical, physical, and mechanical property changes
By adopting these rigorous assessment frameworks, researchers can more accurately predict biomaterial behavior in physiological environments, accelerating the development of safe and effective biodegradable medical devices and implants.
Troubleshooting Guide for Degradation Experiments
Table 1: Common Experimental Challenges and Solutions
| Problem Phenomenon | Potential Root Cause | Recommended Solution |
|---|---|---|
| Unexpectedly fast mass loss | Polymer dissolution mistaken for degradation; high solubility of oligomers in media [1]. | Confirm degradation via chemical methods (e.g., SEC, NMR) to track molecular weight reduction, not just mass loss [1]. |
| Inconsistent degradation rates between samples | Lack of control over critical factors like sample thickness, crystallinity, or molecular weight [6]. | Standardize polymer synthesis and processing parameters. Use controls with known degradation profiles for benchmarking [6]. |
| No degradation observed over time | Use of non-reactive degradation media; absence of specific enzymes for natural polymers [7]. | Validate media with control materials. For enzymatic degradation, confirm enzyme activity and accessibility to cleavage sites [7]. |
| High inflammatory response in vivo | Release of acidic or inflammatory by-products (e.g., from PLA or PGA) [6] [8]. | Consider using alternative polymers (e.g., PCL) or modify polymers to buffer pH changes [6]. |
| Mechanical failure before tissue healing | Degradation rate mismatch; mechanical properties decline faster than tissue regeneration [6] [1]. | Select a polymer with slower degradation (e.g., PLA instead of PLGA) or adjust the implant's physical dimensions [6]. |
| Difficulty assessing liquid formulation degradation | Standard physical methods (e.g., gravimetry, SEM) are unsuitable for gels or solutes [1]. | Employ chemical techniques like HPLC, SEC, or NMR to track molecular weight changes and by-product formation directly [1]. |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between hydrolytic and enzymatic degradation, and how do I test for each?
A1: The core difference lies in the degradation agent.
- Hydrolytic degradation occurs when water molecules cleave chemical bonds in the polymer backbone, such as ester bonds in PLA or PCL. It is a chemical process [6] [7].
- Enzymatic degradation is a biochemical process where specific enzymes (e.g., esterases, proteases) catalyze the cleavage of polymer chains [7] [1].
To test for each, control the experimental environment:
- For hydrolysis: Use aqueous buffer solutions (e.g., PBS at pH 7.4) and exclude enzymes. Elevated temperature (e.g., 37°C) can accelerate testing [6] [1].
- For enzymatic action: Introduce the relevant purified enzyme into the buffer. Always run a parallel control in buffer alone to differentiate enzymatic effects from simple hydrolysis [7].
Q2: Why is it critical to go beyond gravimetric analysis (mass loss) when assessing biodegradation?
A2: Gravimetric analysis, while simple, can be misleading. A decrease in sample mass might result from polymer dissolving into the media rather than degrading into smaller molecules, or from the loss of non-polymeric additives [1]. True degradation involves the scission of the polymer backbone, which is best confirmed by directly measuring a reduction in molecular weight using techniques like Size Exclusion Chromatography (SEC) or by identifying chemical by-products with NMR or mass spectrometry [1]. The ASTM guidelines recommend a multi-faceted approach that includes monitoring mass loss, molar mass changes, and mechanical properties [1].
Q3: How do the degradation mechanisms of biodegradable metals, like zinc alloys, differ from those of polymers?
A3: The primary mechanism for metals is corrosion, an electrochemical process, rather than hydrolysis or enzymatic action [8] [9].
- Process: Metallic Zn oxidizes, losing electrons to become Zn²⁺ ions, which then react with water and hydroxides to form corrosion products like zinc oxide and zinc hydroxycarbonate [9].
- Key Factors: The corrosion rate is influenced by the alloy's composition, microstructure, and the local physiological environment (oxygen content, pH, flow conditions) [9].
- Outcome: The metallic implant gradually dissolves, and the corrosion products are metabolized or cleared by the body, providing biofunctions like osteogenesis and antibacterial activity [9].
Q4: How can I control the degradation rate of a polyester-based scaffold for my specific application?
A4: The degradation rate of synthetic polyesters is highly tunable. You can control it through:
- Monomer Selection: Copolymerizing different monomers is highly effective. For example, PLGA degrades faster than PLA or PGA alone, and a 50:50 LA:GA ratio degrades faster than a 75:25 ratio [6].
- Crystallinity: More crystalline regions are generally more resistant to water penetration and degrade slower than amorphous regions [6].
- Molecular Weight: Higher molecular weight polymers typically degrade more slowly due to their longer polymer chains [6].
- Material Geometry: Increasing the surface-area-to-volume ratio (e.g., by creating porous scaffolds) accelerates degradation by allowing greater fluid penetration [6].
Standard Experimental Protocols for Degradation Assessment
Protocol 1: In Vitro Hydrolytic Degradation of Polymer Films
This protocol outlines a standard method for tracking the hydrolytic breakdown of solid polymer samples, aligned with ASTM F1635-11 guidelines [1].
Research Reagent Solutions
| Item | Function in the Experiment |
|---|---|
| Phosphate Buffered Saline (PBS), pH 7.4 | Simulates the ionic strength and pH of the physiological environment [1]. |
| Sodium Azide (0.02% w/v) | Added to PBS to prevent microbial growth that could confound results. |
| Liquid Nitrogen | Used to rapidly quench degradation at predetermined time points for analysis. |
| Size Exclusion Chromatography (SEC) Solvents | To dissolve polymer samples and determine molecular weight distribution. |
Methodology:
- Sample Preparation: Prepare polymer films with precisely documented initial weight (
W0), dimensions, and thickness. Determine the initial molecular weight (Mw_i) via SEC. - Immersion: Immerse pre-weighed samples in PBS buffer (containing 0.02% sodium azide) and incubate at 37°C. Use a high buffer volume-to-sample surface area ratio to maintain sink conditions.
- Sampling: At predetermined time points, remove samples from the buffer, rinse with deionized water, and dry to a constant weight.
- Analysis:
- Gravimetric Analysis: Measure the dry weight (
Wt). Calculate mass loss:((W0 - Wt) / W0) * 100%. - Molecular Weight (SEC): Analyze the dried samples using SEC to track the reduction in molecular weight (
Mw_t) over time. - Morphology (SEM): Image the surface of the dried samples to observe cracks, pores, and surface erosion.
- Gravimetric Analysis: Measure the dry weight (
Protocol 2: Assessing Enzymatic Degradation of a Protein-Based Hydrogel
This protocol is designed for biomaterials susceptible to specific enzymatic cleavage, such as collagen-based scaffolds.
Methodology:
- Hydrogel Formation: Form hydrogels in a standardized format and document their initial mass and storage modulus (
G0). - Enzyme Solution Preparation: Prepare a solution of the target enzyme (e.g., Collagenase for collagen) in an appropriate buffer at its optimal pH and temperature.
- Incubation: Immerse the hydrogels in the enzyme solution. Include a control group in buffer without the enzyme.
- Analysis:
- Mass Loss: Follow steps 3-4 from Protocol 1 for gravimetric analysis.
- Rheology: Measure the storage modulus (
Gt) of the hydrogels over time to track the loss of mechanical integrity. - By-product Analysis: Use techniques like HPLC or UV-Vis spectroscopy to quantify the release of specific cleavage products (e.g., amino acids) in the supernatant [1].
Degradation Pathways and Experimental Workflow
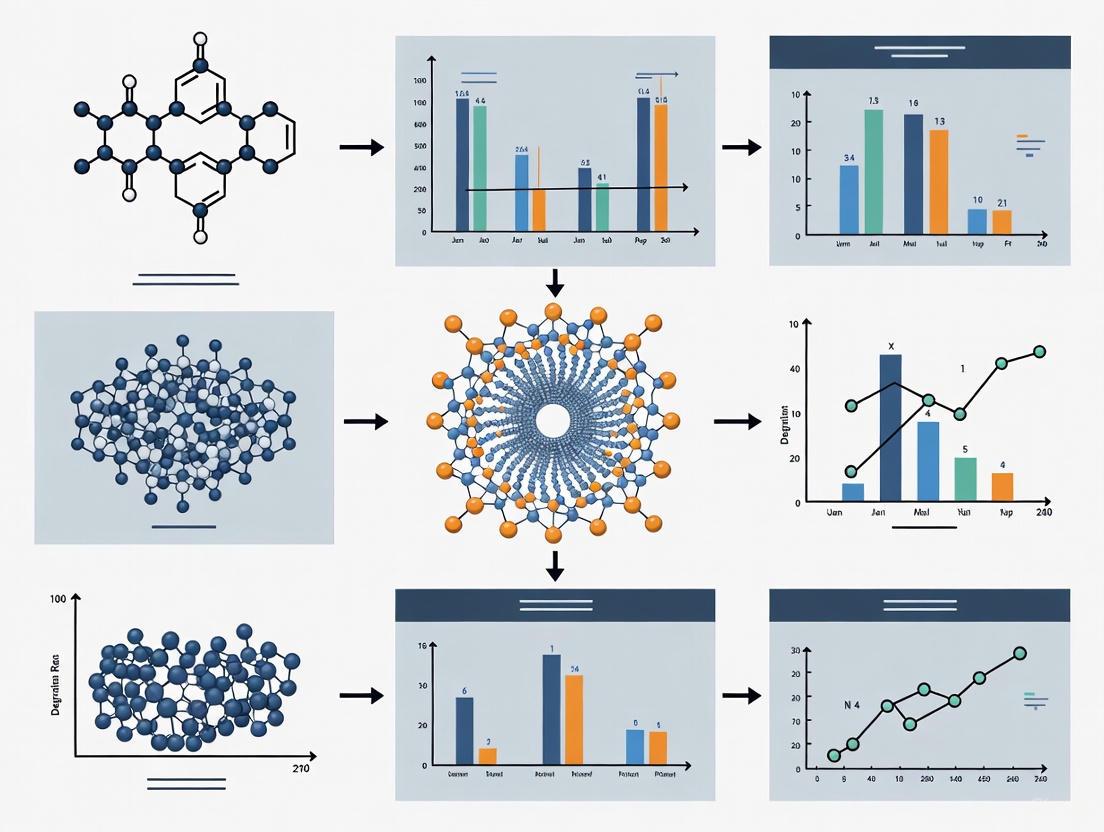
Diagram 1: A generalized workflow for assessing biomaterial degradation, highlighting the parallel paths for different mechanisms and the suite of analytical techniques used.
This technical support center provides a focused resource for researchers and scientists navigating the challenges of material degradation in biomedical applications. The following guides and FAQs address common experimental issues with two key material classes: biodegradable polymers and biodegradable metals. Understanding and controlling their degradation profiles is critical for developing effective implants, drug delivery systems, and tissue engineering scaffolds.
Troubleshooting Guide: Common Experimental Challenges
Issue 1: Uncontrolled or Unexpected Degradation Rates
Problem: The material (polymer or metal) degrades too quickly or too slowly in in vitro or in vivo environments, compromising its function and biocompatibility.
| Material Class | Root Cause | Diagnostic Steps | Solution |
|---|---|---|---|
| Biodegradable Polymers | - Hydrolytic Degradation: Highly sensitive to environmental temperature and humidity. A 50°C increase can accelerate PLA hydrolysis by 30-50% [10].- Enzymatic Degradation: Presence of specific enzymes (e.g., esterases, lipases) rapidly cleaves polymer backbones[cite:7].- Material Crystallinity: High crystalline regions (e.g., in PLA) are more resistant to degradation than amorphous regions[cite:9]. | 1. Characterize the polymer's crystallinity via DSC.2. Measure the pH of the degradation medium; hydrolysis of esters (e.g., in PLA, PCL) can cause acidification[cite:9].3. Test for enzyme activity in the biological medium. | - For too-fast degradation: Increase polymer crystallinity or use polymers with higher glass transition temperatures (Tg)[cite:9].- For too-slow degradation: Incorporate additives like SnCl2 (0.5 wt% can accelerate PLA hydrolysis by ~40%) or copolymerize to reduce crystallinity[cite:7]. |
| Biodegradable Metals | - Alloy Composition & Microstructure: Different phases within an alloy (e.g., in Zn-Mg) can create galvanic couples, accelerating corrosion[cite:3].- Local Environmental Changes: The degradation process itself can alter the local pH and oxygen concentration, changing the corrosion rate[cite:3].- Fluid Dynamics: Static vs. dynamic flow conditions significantly affect ion transport and corrosion product buildup. | 1. Perform metallographic analysis to identify secondary phases.2. Monitor the pH and dissolved oxygen in the immersion medium over time.3. Characterize corrosion products using SEM/EDS and XRD. | - Use high-purity metals to control intermetallic phases.- Employ surface modifications (e.g., coatings) to create a barrier layer initially.- Design alloys with specific elements (e.g., Li for Zn alloys) to form more stable corrosion layers[cite:3]. |
Issue 2: Inadequate Mechanical Performance During Degradation
Problem: The material loses mechanical integrity (e.g., strength, elasticity) too rapidly, failing to provide support for the required healing period.
| Material Class | Root Cause | Diagnostic Steps | Solution |
|---|---|---|---|
| Biodegradable Polymers | - Plasticizer Leaching: Additives like glycerol can leach out, causing embrittlement[cite:5].- Molecular Weight Drop: Chain scission from hydrolysis reduces molecular weight and strength long before mass loss is evident[cite:5][cite:7]. | 1. Use Gel Permeation Chromatography (GPC) to track molecular weight loss over time.2. Perform periodic mechanical testing (tensile, compression) on samples immersed in simulated physiological fluid. | - Blend polymers (e.g., PCL into PLA) to improve toughness and tailor the degradation profile[cite:7].- Use cross-linking agents to create a more stable network and slow strength loss. |
| Biodegradable Metals | - Localized Corrosion: Pitting corrosion creates stress concentrators, leading to premature mechanical failure[cite:3].- Loss of Load-Bearing Cross-Section: General corrosion uniformly reduces the effective cross-sectional area. | 1. Use micro-CT scanning to visualize and quantify internal pitting in 3D.2. Conduct in situ mechanical testing during degradation. | - Design alloys with homogenous microstructures (e.g., fine-grained Zn alloys).- For Zn alloys, adding elements like Li and Mn can significantly increase strength (UTS > 500 MPa) and ductility (up to 108%)[cite:3]. |
Issue 3: Adverse Biological Responses
Problem: The degradation process elicits an undesirable inflammatory response, toxicity, or tissue irritation.
| Material Class | Root Cause | Diagnostic Steps | Solution |
|---|---|---|---|
| Biodegradable Polymers | - Acidic Degradation Products: Accumulation of acidic monomers (e.g., lactic acid from PLA) can cause local pH drop and inflammatory response[cite:7][cite:9].- Oligomer & Monomer Release: These smaller molecules, often overlooked, can be toxic or act as signaling molecules[cite:9]. | 1. Measure pH change in the local microenvironment.2. Use liquid chromatography-mass spectrometry (LC-MS) to identify and quantify released oligomers and monomers.3. Perform cell viability assays (e.g., WST-8) with degradation product extracts[cite:2]. | - For acidity: Incorporate buffering agents (e.g., calcium carbonate) into the polymer matrix.- For oligomer toxicity: Modify the polymer with short-chain PEG to enhance histocompatibility[cite:7]. |
| Biodegradable Metals | - Rapid Ion Release: A sudden, high local concentration of metal ions (e.g., Zn²⁺, Mg²⁺) can be cytotoxic[cite:3][cite:4].- Particulate Debris: Metal micro/nano particles from degradation can be phagocytosed, causing inflammation. | 1. Use Inductively Coupled Plasma Mass Spectrometry (ICP-MS) to track ion release kinetics.2. Analyze tissue sections (histology) for the presence of particulates and immune cell infiltration. | - Control corrosion rate through alloying to ensure a steady, low release of ions (e.g., Zn is essential and has a high tolerance)[cite:3].- Ensure degradation products are biocompatible and participat in natural biological processes (e.g., Zn²⁺ in signaling)[cite:3]. |
Frequently Asked Questions (FAQs)
FAQ 1: What are the key differences in the fundamental degradation mechanisms between biodegradable polymers and metals?
- Biodegradable Polymers primarily degrade via:
- Hydrolysis: Water molecules cleave chemical bonds in the polymer backbone (e.g., ester bonds in PLA, PCL)[cite:7][cite:9].
- Enzymatic Degradation: Specific enzymes (e.g., lipases, esterases) secreted by microorganisms or cells target and break the polymer chains[cite:7].
- Biodegradable Metals degrade primarily through:
- Corrosion: An electrochemical process where the metal oxidizes, losing electrons. In physiological environments, this is often influenced by chlorides, pH, and oxygen content[cite:3][cite:4]. The degradation rate is governed by the composition and the stability of the resulting oxide/hydroxide layers.
FAQ 2: How can I accurately simulate and test for degradation in a physiological environment?
A robust in vitro protocol should consider the following:
- Medium Selection: Use standardized simulated body fluids (SBF), phosphate-buffered saline (PBS), or more specific media like human duodenal fluid, depending on the target implantation site [11].
- Temperature Control: Maintain a constant 37°C.
- Sterility: Conduct tests under sterile conditions to distinguish abiotic hydrolysis from microbial degradation.
- Dynamic vs. Static: Agitation or flow systems better mimic in vivo conditions than static immersion.
- Monitoring: Key metrics include mass loss, molecular weight loss (for polymers), ion release (for metals, via ICP-MS), pH change, and mechanical property decay.
FAQ 3: We are seeing high variability in our degradation data. What are the primary factors to control?
For consistent results, strictly control these parameters:
- Material Properties: Crystallinity, molecular weight distribution (polymers), grain size and phase distribution (metals), and surface roughness.
- Experimental Conditions: Temperature, pH, buffer concentration, volume-to-surface-area ratio of the sample, and the agitation rate of the immersion medium. Even small deviations can significantly alter degradation kinetics.
FAQ 4: Are "biodegradable" products always safe for biomedical use? What are the hidden risks?
Not necessarily. "Biodegradable" does not automatically mean "biocompatible." Key risks include:
- Toxic By-products: Degradation can release undesirable monomers, oligomers, or metal ions[cite:9]. For example, some BP oligomers are considered an "iceberg" of polymer debris with potential toxicity[cite:9].
- Inflammation from Fragments: Both polymer and metal degradation can generate micro- and nano-scale particles that may provoke an immune response[cite:9].
- Rapid Acidification: Some polymers (like PLA) can create an acidic microenvironment upon degradation, leading to inflammation and tissue damage[cite:7].
Standard Experimental Protocols
Protocol 1:In VitroDegradation Testing for Biodegradable Polymers
Objective: To determine the degradation profile of a biodegradable polymer in a simulated physiological environment.
Materials:
- Polymer samples (e.g., films, 3D scaffolds)
- Phosphate Buffered Saline (PBS), pH 7.4, or other relevant media
- Incubator shaker (37°C, sterile conditions)
- Analytical balance (±0.01 mg)
- Gel Permeation Chromatography (GPC) system
- Differential Scanning Calorimetry (DSC)
- Scanning Electron Microscope (SEM)
Procedure:
- Sample Preparation: Cut samples to a standard size (e.g., 10x10x1 mm). Record initial dry mass (W₀), dimensions, and characterize initial molecular weight and crystallinity.
- Immersion: Immerse each sample in a sufficient volume of PBS (e.g., 20:1 volume-to-surface area ratio) in sealed containers. Place in an incubator shaker set to 37°C and a low agitation speed.
- Sampling Interval: Remove samples in triplicate at predetermined time points (e.g., 1, 7, 14, 28 days, etc.).
- Analysis:
- Mass Loss: Rinse retrieved samples with deionized water, dry to constant weight, and measure dry mass (W₁). Calculate mass loss:
(W₀ - W₁)/W₀ * 100%. - Molecular Weight: Use GPC to determine the change in molecular weight and distribution over time.
- Thermal Properties: Use DSC to track changes in glass transition temperature (Tg) and crystallinity.
- Morphology: Use SEM to observe surface erosion, cracking, or pore formation.
- Mass Loss: Rinse retrieved samples with deionized water, dry to constant weight, and measure dry mass (W₁). Calculate mass loss:
Protocol 2:In VitroDegradation Testing for Biodegradable Metals
Objective: To evaluate the corrosion rate and mode of a biodegradable metal sample.
Materials:
- Metal alloy samples (e.g., discs, wires)
- Simulated Body Fluid (SBF) or Hanks' solution
- Incubator (37°C, sterile conditions)
- Analytical balance (±0.01 mg)
- Scanning Electron Microscope (SEM) with Energy Dispersive X-ray Spectroscopy (EDS)
- Inductively Coupled Plasma Mass Spectrometry (ICP-MS)
- X-ray Diffractometer (XRD)
Procedure:
- Sample Preparation: Polish samples to a standard surface finish, clean, and sterilize. Record initial dry mass and dimensions.
- Immersion: Immerse samples in SBF at 37°C under sterile, static conditions. Ensure an adequate volume-to-surface area ratio.
- Sampling Interval: Remove samples and collect immersion medium at set intervals.
- Analysis:
- Mass Loss: After removal, clean samples to remove corrosion products according to an ASTM standard (e.g., using chromic acid). Measure the final mass to calculate the corrosion rate.
- Solution Analysis: Use ICP-MS to quantify the concentration of released metal ions (e.g., Zn²⁺, Mg²⁺) in the collected medium.
- Surface Analysis: Use SEM to examine the surface for pitting or uniform corrosion. Use EDS and XRD to identify the chemical composition and phases of corrosion products.
Degradation Pathways and Experimental Workflows
Degradation Mechanism Diagrams
Diagram Title: Fundamental Degradation Pathways for Polymers and Metals
Material Selection and Experimental Workflow
Diagram Title: Material Selection Workflow Based on Application
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function | Key Considerations |
|---|---|---|
| Phosphate Buffered Saline (PBS) | A standard isotonic solution for in vitro degradation studies, mimicking salt concentrations in the body. | Maintains pH 7.4; suitable for initial hydrolysis screening but lacks proteins and cells. |
| Simulated Body Fluid (SBF) | A solution with ion concentrations similar to human blood plasma. | More accurately mimics the in vivo mineral deposition (biomineralization) on materials. |
| Polylactic Acid (PLA) | A widely used synthetic biodegradable polymer. | Degradation rate is highly dependent on crystallinity and molecular weight. Releases acidic by-products [10] [12]. |
| Polycaprolactone (PCL) | A synthetic biodegradable polyester with a low melting point and high elasticity. | Degrades slower than PLA; often blended to modify degradation rates and flexibility [10]. |
| Zn-Li Alloy | A high-strength biodegradable metal for load-bearing applications. | Li significantly strengthens Zn; degradation products can promote osteogenesis for bone implants [9]. |
| Enzymes (Esterases, Lipases) | Used to study enzymatic polymer degradation or simulate inflammatory conditions. | Concentrations and activity units must be standardized for reproducible results [10]. |
| Differential Scanning Calorimeter (DSC) | Analyzes thermal transitions (Tg, melting point, crystallinity) of polymers. | Changes in crystallinity during degradation can be tracked, indicating chain scission and reorganization. |
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | Precisely quantifies trace metal ion concentrations in solution. | Essential for measuring metal ion release kinetics from biodegradable metals and composites [9] [11]. |
Troubleshooting Guide: Common Challenges in Degradation Kinetics
Q1: Why is my hydrogel degrading too quickly, causing a premature burst release of the drug?
A: Rapid degradation and burst release are frequently caused by:
- Insufficient Crosslinking Density: A low density of crosslinks in the polymer network creates larger pores and faster breakdown. Solution: Increase crosslinker concentration or use a crosslinker with higher functionality. Characterize the new formulation's mesh size and swelling ratio [13].
- High Enzyme Concentration: For enzymatically-degraded hydrogels (e.g., chitosan-based), an unexpectedly high local concentration of enzymes (e.g., lysozyme) can accelerate breakdown. Solution: Incorporate enzyme inhibitors or design the hydrogel with enzyme-cleavable sequences that match the target tissue's specific enzyme profile [14] [15].
- Unexpected Environmental pH: If a hydrogel is designed for pH-sensitive degradation (e.g., in an acidic tumor microenvironment), testing in a different pH can yield invalid results. Solution: Always calibrate your degradation experiments to the precise pH, ionic strength, and enzyme composition of the target physiological environment [14] [16].
Q2: What can cause slow or incomplete degradation, leading to poor tissue integration and potential chronic inflammation?
A: Slow degradation often stems from:
- Excessive Crosslinking: An overly dense network can hinder the diffusion of water, ions, or enzymes needed for degradation. Solution: Optimize crosslinker ratio and explore different crosslinking mechanisms (e.g., physical ionic crosslinking vs. chemical covalent crosslinking) to fine-tune stability [13] [15].
- Material Biostability: Some synthetic polymers (e.g., certain polyesters) have inherently slow hydrolysis rates. Solution: Use copolymers or incorporate rapidly degrading natural polymers like alginate or chitosan to create hybrid systems with tailored degradation profiles [13] [16].
- Lack of Specific Enzymes: If relying on enzymatic degradation, ensure the target tissue expresses the required enzyme at sufficient levels. Solution: Conduct a thorough literature review or preliminary immunohistochemistry to confirm enzyme presence before designing your material [15].
Q3: How do I reconcile the conflicting requirements for mechanical strength and desirable degradation rates?
A: This is a central challenge in biomaterial design. A strong, durable network often degrades slowly.
- Solution: Develop composite or hybrid hydrogels. For example, reinforce a soft, fast-degrading natural polymer (e.g., chitosan) with a synthetic polymer (e.g., PEG) or nanoparticles to enhance mechanical strength without drastically altering the degradation kinetics. The synthetic component can provide structural integrity, while the natural component dictates the degradation rate [14] [16].
- Solution: Utilize hierarchical network structures. Design a dual-crosslinked system where a primary network provides initial strength and a secondary, weaker network controls the drug release profile [13].
Q4: My in vitro degradation data does not match in vivo results. What are the potential reasons?
A: This common discrepancy arises from oversimplified in vitro models.
- Complex In Vivo Milieu: The in vivo environment contains a dynamic mix of cells, enzymes, and mechanical stresses (e.g., fluid flow, tissue compression) not replicated in standard PBS incubation. Solution: Develop more sophisticated in vitro models that include relevant cell cultures (e.g., macrophages), enzyme cocktails, or mechanical stimulation to better predict in vivo performance [13] [16].
- Cellular Activity: Immune cells like macrophages can phagocytose hydrogel fragments, drastically accelerating clearance in a way pure hydrolysis cannot mimic. Solution: Include macrophage co-culture assays in your degradation studies to account for the cellular component of degradation [14].
Experimental Protocols for Characterizing Degradation Kinetics
Protocol 1: Gravimetric Analysis for Degradation Rate
Purpose: To quantitatively measure the mass loss of a hydrogel sample over time under simulated physiological conditions.
Materials:
- Pre-formed hydrogel samples (e.g., discs or cylinders)
- Degradation buffer (e.g., PBS at pH 7.4, or a specific buffer mimicking the target site like pH 6.5 for tumors)
- Optional: Enzyme solution (e.g., lysozyme for chitosan) in buffer
- Analytical balance (precision ±0.1 mg)
- Incubator/shaker set to 37°C
- Freeze dryer or vacuum oven
Method:
- Initial Mass (W₀): Pre-weigh each dry hydrogel sample (W₀).
- Equilibrium Swelling: Place each sample in a large volume of buffer (to ensure sink conditions) and allow it to swell to equilibrium at 37°C. Record the swollen mass (W_s).
- Degradation Incubation: Transfer the swollen hydrogels to fresh vials containing the degradation buffer (with or without enzymes). Place vials in an incubator at 37°C.
- Mass Monitoring: At predetermined time points, remove samples from the incubation medium. Gently rinse with deionized water to remove ions and buffer salts.
- Drying and Weighing: Lyophilize or vacuum-dry the samples until a constant dry mass (W_t) is achieved.
- Calculation: Calculate the remaining mass percentage at each time point:
- Remaining Mass (%) = (W_t / W₀) × 100
Plot Remaining Mass (%) versus Time to visualize the degradation profile.
Protocol 2: Monitoring Drug Release Kinetics
Purpose: To correlate the degradation of the hydrogel with the release profile of an encapsulated therapeutic agent.
Materials:
- Drug-loaded hydrogel samples
- Release medium (e.g., PBS, often with 0.1% w/v sodium azide to prevent microbial growth)
- Incubator/shaker at 37°C
- UV-Vis spectrophotometer, HPLC, or other suitable analytical instrument for drug quantification
Method:
- Sample Preparation: Immerse each drug-loaded hydrogel in a known volume of release medium.
- Sampling: At scheduled intervals, withdraw a small aliquot (e.g., 1 mL) of the release medium for analysis.
- Replenishment: Immediately replace the withdrawn volume with fresh, pre-warmed release medium to maintain sink conditions.
- Analysis: Quantify the drug concentration in the aliquot using a pre-calibrated standard curve.
- Cumulative Release Calculation:
- Calculate the cumulative amount of drug released at each time point, accounting for dilution from replenishment.
Plot Cumulative Drug Released (%) versus Time on the same graph as the degradation profile (from Protocol 1) to directly visualize the critical link.
Quantitative Data on Hydrogel Degradation and Drug Release
Table 1: Swelling and Degradation Characteristics of Common Biopolymers [15]
| Biopolymer | Typical Swelling Degree (g/g in Water) | Key Degradation Mechanism | Notes on Degradation Kinetics |
|---|---|---|---|
| Alginate | 1.65 - 3.85 | Ion exchange (chelators), hydrolysis | Slow hydrolysis; rapid in presence of chelators like citrate. |
| Carboxymethyl Cellulose | 50 - 200 | Microbial/enzymatic degradation | High swelling can lead to faster enzymatic breakdown. |
| Chitosan | >100% (100% swelling) | Enzymatic (lysozyme) | Degradation rate is highly dependent on deacetylation degree and crystallinity. |
| Starch | 500 - 1200% | Enzymatic (amylase) | Very rapid degradation in the presence of amylase. |
Table 2: Impact of Crosslinking on Hydrogel Properties [13] [14]
| Crosslinking Strategy | Impact on Mechanical Strength | Impact on Degradation Rate | Typical Drug Release Profile |
|---|---|---|---|
| Physical (Ionic, H-bonding) | Moderate | Fast, often reversible | Can be burst-heavy, sensitive to environmental ions/pH. |
| Chemical (Covalent) | High | Slow, tunable via crosslink density | Sustained, more predictable, often zero-order kinetics. |
| Enzyme-Sensitive Peptides | Variable | Highly specific, triggered | On-demand release upon exposure to specific enzymes. |
Research Reagent Solutions
Table 3: Essential Materials for Degradation and Release Studies
| Reagent / Material | Function in Experiment | Key Considerations |
|---|---|---|
| Chitosan | A natural polymer forming cationic hydrogels; degrades via lysozyme [14]. | Viscosity and degradation rate depend on molecular weight and degree of deacetylation. |
| Polyethylene Glycol (PEG) | A synthetic polymer used to create "stealth," tunable hydrogels [16]. | Biocompatible; degradation kinetics can be controlled by using hydrolyzable ester or peptide crosslinkers. |
| Genipin | A natural, low-toxicity crosslinker for polymers like chitosan [14]. | Preferable to glutaraldehyde; creates blue-pigmented hydrogels and slows degradation. |
| Lysozyme | An enzyme used to simulate the enzymatic degradation of chitosan-based hydrogels in vitro [14]. | Concentration should mimic physiological levels found in the target tissue (e.g., serum, tissues). |
| Matrix Metalloproteinases (MMPs) | Enzymes used to create smart, disease-responsive hydrogels that degrade in diseased tissues (e.g., cancer) [16]. | Specific peptide sequences (e.g., cleavable by MMP-2 or MMP-9) must be incorporated into the hydrogel network. |
Visualization of Pathways and Workflows
Diagram 1: Hydrogel Degradation and Drug Release Pathways
Diagram 2: Experimental Workflow for Kinetics Study
Troubleshooting Guide: Frequently Asked Questions
Q1: My in vitro degradation experiment shows mass loss, but I cannot detect any by-products. What could be wrong with my methodology?
A: Mass loss alone is not a definitive confirmation of degradation, as it could result from the dissolution of soluble material rather than true chemical breakdown [1]. To confirm degradation, you must supplement gravimetric analysis with chemical characterization techniques. We recommend the following protocol:
- Sample Preparation: Place your biomaterial samples (we recommend n=5 per time point for statistical significance) in the appropriate degradation medium (e.g., PBS at 37°C, with or without enzymes like lipase or protease) [1].
- Monitor Mass Loss: Regularly measure mass loss according to ASTM F1635-11 guidelines, ensuring samples are dried to a constant weight with a precision of 0.1% [1].
- Chemical Analysis: Simultaneously, analyze the degradation medium for by-products. Use High-Performance Liquid Chromatography (HPLC) or Nuclear Magnetic Resonance (NMR) spectroscopy to identify and quantify specific chemical monomers like adipic acid, terephthalic acid, or glycolic acid [1] [17]. Size Exclusion Chromatography (SEC) is recommended for tracking changes in the molecular weight of the polymer itself [1].
Q2: The degradation by-products from my poly(lactic-co-glycolic acid) (PLGA) device seem to be altering the local pH, causing unexpected cellular toxicity. How can I investigate this?
A: You are likely observing an autocatalytic effect where acidic by-products lower the local pH, accelerating degradation and causing cytotoxicity [17]. To investigate:
- pH Monitoring: Use a micro-pH probe to track the pH of the degradation medium in real-time throughout your experiment.
- By-product Quantification: Correlate pH changes with the quantified release of acidic monomers like glycolic acid using HPLC [17].
- Validate with Bioassays: Perform standardized bioassays to confirm the toxic effect. The zebrafish embryo model is a sensitive in vivo tool. Expose embryos to your by-products and monitor key endpoints:
Q3: How can I distinguish between hydrolytic and oxidative degradation mechanisms for my PEG-based implant?
A: The primary mechanism can be identified by tailoring the experimental environment and analyzing the chemical outcomes.
- For Hydrolytic Degradation: Conduct aging studies in aqueous buffers at physiological temperature (37°C) and pH (7.4). Hydrolysis will typically cleave ester bonds in polymers like PEGDA or PLA, which you can confirm by using NMR to detect the formation of terminal hydroxyl and carboxylate groups [18].
- For Oxidative Degradation: Expose samples to an oxidizing environment, such as a solution of hydrogen peroxide (H₂O₂). Oxidation often targets ether bonds in polymer backbones, like that of PEG. The shift to a more stable chemistry, such as replacing PEG diacrylate (PEGDA) with PEG diacrylamide (PEGDAA) which resists hydrolysis, can also provide evidence that hydrolysis was the dominant mechanism in the original material [18].
Q4: My biodegradable material is failing in vivo much faster than predicted by in vitro tests. What are the most common reasons for this discrepancy?
A: This is a common challenge, often attributed to the oversimplification of in vitro models. Key factors in vivo that are difficult to fully replicate in vitro include:
- Dynamic Mechanical Loads: In vitro tests are often static, while implants in the body experience stress, strain, and friction, leading to mechanical degradation modes like fatigue and fretting [19].
- Complex Biological Milieu: The in vivo environment contains cells (e.g., macrophages) that release reactive oxygen species and enzymes, leading to oxidative and enzymatic degradation not present in simple buffer solutions [18] [19].
- Protein Adsorption: The adsorption of proteins onto the material surface can trigger an immune response and alter the degradation profile [18].
- In-Service Degradation: The device might be exposed to harsher conditions than anticipated, such as variable pH or chemical exposure [19].
Mitigation Strategy: Implement more advanced in vitro tests that simulate these conditions, such as using bioreactors that apply mechanical strain or incorporating macrophage co-cultures and enzymes into your degradation media [18].
Quantitative Data on Degradation By-Product Toxicity
The table below summarizes toxicity data for common biodegradable plastic monomers, providing a reference for assessing the biological impact of degradation products.
Table 1: Toxicity of Common Biodegradable Plastic Degradation Products in Zebrafish Model
| Degradation Product | Source Polymer | Tested Concentrations | Key Toxicological Endpoints Observed | LC50 (if reported) |
|---|---|---|---|---|
| Adipic Acid | PBAT | Up to 100 mg/L | Inhibition of plant growth (Lycopersicon esculentum, Lactuca sativa) [17] | Fish: 97 mg/L (Pimephales promelas) [17] |
| Terephthalic Acid | PBAT | Not specified in results | Impairment of testicular functions in male Rattus norvegicus [17] | Information missing from search results |
| Glycolic Acid | PGA | 456.3 mg/L | Induction of embryo malformations in Rattus norvegicus [17] | Information missing from search results |
| 1,4-Butanediol | PBAT | Not specified in results | Information missing from search results | Information missing from search results |
Detailed Experimental Protocols
Protocol 1: In Vitro Hydrolytic Degradation of PEG-based Hydrogels
This protocol is adapted from studies on PEGDA hydrogels and can be adapted for other hydrolytically degradable polymers [18].
Objective: To assess the mass loss, swelling behavior, and by-product release of hydrogels under simulated physiological conditions.
Materials:
- Research Reagent Solutions:
- PEGDA Hydrogel: Poly(ethylene glycol) diacrylate, the primary test material [18].
- Phosphate Buffered Saline (PBS), pH 7.4: Standard degradation medium to simulate body fluid [18].
- Lysozyme or other relevant enzymes: To simulate enzyme-mediated degradation [1].
- Liquid Nitrogen: For quickly stopping degradation before analysis.
- Deionized Water: For rinsing samples.
- Lyophilizer (Freeze-dryer): For drying samples to constant mass.
Methodology:
- Sample Preparation: Synthesize hydrogel discs (e.g., 5mm diameter x 2mm thickness) via UV photopolymerization. Determine the initial dry mass (W₀) after lyophilization.
- Degradation Study: Immerse each sample in 10-20 mL of PBS (with or without enzymes) and incubate at 37°C under gentle agitation. Use a minimum of n=5 samples per group for statistical power.
- Sampling and Analysis: At predetermined time points (e.g., days 1, 3, 7, 14, 28):
- Mass Loss: Remove samples, rinse with deionized water, freeze-dry, and measure dry mass (Wₜ). Calculate mass loss as:
(W₀ - Wₜ)/W₀ × 100%. - Swelling Ratio: After rinsing but before drying, measure the wet mass (Ww). Calculate the mass swelling ratio (Qm) as:
Q_m = W_w / Wₜ. - By-product Analysis: Analyze the degradation medium using HPLC or NMR to quantify the release of PEG fragments, acrylic acid, or other expected monomers [18].
- Mechanical Testing: Periodically measure the compressive or tensile modulus to correlate degradation with functional loss.
- Mass Loss: Remove samples, rinse with deionized water, freeze-dry, and measure dry mass (Wₜ). Calculate mass loss as:
Protocol 2: Assessing By-product Toxicity Using Zebrafish Embryos
This protocol uses zebrafish as a model organism to evaluate the biological effects of degradation products [17].
Objective: To determine the developmental toxicity of degradation by-products like adipic acid, terephthalic acid, and glycolic acid.
Materials:
- Research Reagent Solutions:
- Test Compounds: Adipic acid, terephthalic acid, glycolic acid, 1,4-butanediol of high purity [17].
- Zebrafish Embryos: Wild-type (e.g., AB strain), 4-6 hours post-fertilization (hpf).
- Embryo Medium: Standard aqueous medium for raising embryos.
- Dimethyl Sulfoxide (DMSO): For solubilizing compounds, keeping final concentration ≤0.1% [17].
- 3,4-Dichloroaniline (DCA): Use as a positive control for toxicity validation [17].
Methodology:
- Exposure Setup: Dispense 20-30 healthy embryos into 24-well plates, with one embryo per well in 2 mL of embryo medium.
- Dosing: Expose embryos to a range of concentrations of the individual by-products or a mixture. Include a negative control (embryo medium only) and a positive control (e.g., 4 mg/L DCA).
- Incubation and Monitoring: Incubate plates at 28.5°C and monitor endpoints at 96 hpf:
- Survival Rate: Count the number of live versus dead embryos.
- Hatching Rate: Record the number of embryos that have hatched from their chorions.
- Heartbeat Rate: Manually count heartbeats over a 15-second period under a microscope for at least 10 larvae per group.
- Body Length: Measure the standard body length from the head to the tip of the tail using image analysis software.
- Statistical Analysis: Compare results from treatment groups to the negative control using appropriate statistical tests (e.g., one-way ANOVA) to determine significant effects.
Visualizing Key Concepts and Workflows
Diagram 1: Biomaterial Degradation Assessment Workflow
Diagram 2: Biological Response to Degradation By-products
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Degradation and Toxicity Studies
| Reagent / Material | Function in Experiment |
|---|---|
| Phosphate Buffered Saline (PBS) | Standard aqueous medium for simulating physiological conditions and studying hydrolytic degradation [1] [18]. |
| Specific Enzymes (e.g., Lipase, Protease) | Introduced to degradation media to simulate enzyme-mediated biodegradation pathways relevant to the in vivo environment [1]. |
| Poly(ethylene glycol) diacrylate (PEGDA) | A widely studied, synthetic hydrogel model system for understanding hydrolytic degradation mechanisms, particularly of ester linkages [18]. |
| High-Performance Liquid Chromatography (HPLC) | An analytical technique used to separate, identify, and quantify individual degradation by-products (e.g., adipic acid, glycolic acid) in a solution [1] [17]. |
| Nuclear Magnetic Resonance (NMR) | Spectroscopy used to determine the molecular structure of polymers and their degradation fragments, confirming chemical breakdown [1] [18]. |
| Size Exclusion Chromatography (SEC) | Chromatography method used to monitor changes in the average molecular weight and molecular weight distribution of a polymer as it degrades [1]. |
| Zebrafish (Danio rerio) Embryos | A vertebrate model organism used for in vivo toxicity screening of degradation products, allowing assessment of developmental endpoints like heartbeat and morphology [17]. |
Methodologies and Applications: Harnessing Degradation for Controlled Release and Regeneration
Frequently Asked Questions (FAQs)
Q1: How can I achieve a constant, zero-order drug release profile instead of a declining (Fickian) release from my biodegradable polymer device? Achieving zero-order release requires shifting from diffusion-controlled to degradation-controlled release. This can be accomplished by engineering your device's geometry to manage the degradation front. Using vat polymerization 3D printing, you can design structures with specific surface area to volume (SA/V) ratios, strut beam sizes, and pore sizes that modulate the rate of water penetration and acidic byproduct egress. This controls the onset of bulk degradation, which in turn can compensate for the reduction in diffusion-driven release over time, leading to a more constant release profile [20].
Q2: What are the key considerations for selecting a biopolymer for a long-term (e.g., 6-month) implantable drug delivery system? For long-term implants, the material must balance degradation rate with mechanical integrity. Key considerations include:
- Copolymer Ratios: PLGA with a higher lactic acid to glycolic acid ratio (e.g., 75:25) degrades more slowly than 50:50 PLGA, making it suitable for extended release [21].
- Crystallinity: Highly crystalline polymers like pure PGA degrade more predictably but may have slower hydrolysis rates.
- Drug Stability: Ensure the polymer's processing conditions (e.g., melt temperature for spinning) do not degrade the therapeutic agent [21].
Q3: My shape memory polymer (SMP) device is not recovering its shape consistently upon stimulation. What could be wrong? Inconsistent shape recovery can stem from several factors:
- Insufficient or Inhomogeneous Stimulus: For light-triggered SMPs, ensure the photothermal coating (e.g., polydopamine) is uniformly applied and that light intensity is sufficient to heat the entire device above its transition temperature [21].
- Material Issues: Incomplete crosslinking during resin synthesis for 3D printing can lead to a poorly defined polymer network, hindering recovery. Verify your photoinitiator concentration and UV curing time [22] [20].
- Geometric Constraints: The physical environment of the implant site might be restricting the device's movement. Re-evaluate the programmed temporary and permanent shapes for biocompatibility with the anatomical location [22].
Q4: How can I create a device that releases multiple drugs in a specific sequence? Sequential drug release is achievable through multimaterial fiber design. Using a thermal drawing process, you can create a single fiber with multiple, isolated drug reservoirs. Each reservoir is sealed with a biodegradable polymer (e.g., PLGA) with a distinct degradation rate. The polymer with the fastest degradation rate will release its drug first, followed by the next, allowing for pre-programmed, sequential therapy from a single implant [21].
Q5: What sterilization methods are suitable for heat-sensitive biodegradable polymers like PLA and PLGA? Conventional high-temperature methods like autoclaving and gamma radiation can degrade these polymers, causing premature weakening or changes in release kinetics. Suitable alternatives include:
- Low-Temperature Gas Plasma (HPGP) Sterilization
- Ethylene Oxide (EtO) Gas Sterilization [23] Always validate the sterilization method's impact on your specific device's mechanical properties, degradation profile, and drug stability.
Troubleshooting Guides
Table 1: Common Experimental Issues and Solutions
| Problem Phenomenon | Potential Root Cause | Recommended Solution |
|---|---|---|
| Burst release followed by very slow release | Poor drug-polymer compatibility; high surface-area-to-volume ratio; microcracks in device. | Optimize drug loading method; reduce surface area or apply a thin, slow-degrading polymer coating; review printing/resin parameters to ensure structural integrity [20] [24]. |
| Premature loss of mechanical strength in vivo | Polymer degradation rate is too fast; acidic degradation byproducts cause autocatalytic erosion. | Switch to a slower-degrading polymer (e.g., higher L-lactide content PLGA or PCL); incorporate buffering agents (e.g., Mg(OH)₂) to neutralize acidic byproducts [25] [23]. |
| Uncontrolled, biphasic/triphasic release profile | Onset of catastrophic bulk degradation. | Redesign device geometry to control water ingress: use 3D printing to create architectures with lower SA/V ratios or smaller pore sizes to delay bulk degradation [20]. |
| Poor cell adhesion or inflammatory response on polymer scaffold | Lack of bioactivity; surface hydrophobicity; cytotoxic impurities. | Modify the surface with bioactive motifs (e.g., RGD peptides); use plasma treatment to increase hydrophilicity; rigorously purify polymers to remove residual catalysts or monomers [25] [26]. |
Table 2: Optimizing 3D Printing for Controlled Release
| Printing Parameter | Impact on Release Profile | Optimization Strategy |
|---|---|---|
| Surface Area to Volume (SA/V) Ratio | Higher SA/V ratios accelerate both drug release and degradation. | For long-term release, design structures with a lower SA/V ratio. For rapid release, use higher SA/V structures like thin meshes [20]. |
| Strut Size / Wall Thickness | Thicker struts delay water penetration, pushing the onset of degradation-controlled release further in time. | Use thicker struts and walls to prolong release duration and achieve more linear release kinetics [20]. |
| Pore Size & Porosity | Larger, interconnected pores increase diffusion rates and can lead to initial burst release. | Utilize smaller, controlled pore sizes to restrict diffusion and place greater control over release in the hands of polymer degradation [20] [27]. |
| Polymer Resin Degradation Rate | Fast-degrading resins lead to quicker onset of degradation-controlled release. | Formulate resins or select polymers with degradation rates that match the desired therapeutic timeframe. Combine fast and slow degrading polymers in a single device [20] [21]. |
Standard Experimental Protocols
Protocol 1: Engineering Long-Term Controlled Release via Vat Polymerization 3D Printing
This protocol outlines the use of vat polymerization (VP) 3D printing with biodegradable resins to create devices for long-term controlled drug release [20].
1. Resin Formulation:
- Materials: Biodegradable photoreactive polyester resin (e.g., methacrylated PCL-PGA-PTMC triblock), model drug (e.g., Rhodamine B), photoinitiator.
- Procedure: Dissolve the model drug at the desired concentration (e.g., 0.2 wt%) in the liquid resin. Add a compatible photoinitiator. Mix thoroughly using a centrifugal mixer (e.g., 2500 rpm for 1 min, then 3000 rpm for 1 min) to ensure homogeneity and remove air bubbles.
2. Working Curve Analysis:
- Determine the critical exposure energy (Ec) and penetration depth (Dp) of the formulated resin using Jacob's fundamental working curve equation. This calibration is essential for establishing correct printer exposure settings to achieve the desired curing depth and structural fidelity.
3. 3D Printing & Post-Processing:
- Printing: Use a Digital Light Processing (DLP) printer to fabricate the designed geometries (e.g., cylinders, porous cubes). Maintain a constant temperature during printing.
- Washing: Post-print, wash the devices in a suitable solvent (e.g., isopropanol) to remove any uncured resin.
- Post-Curing: Cure the devices under UV light to ensure complete polymerization and maximize mechanical strength.
4. In Vitro Release Study:
- Immerse the drug-loaded devices in a release medium (e.g., PBS at pH 7.4) and maintain at 37°C under gentle agitation.
- At predetermined time points, withdraw aliquots of the release medium and analyze drug concentration using UV-Vis spectroscopy. Replace the medium to maintain sink conditions.
- Plot cumulative release versus time and fit the data to various mathematical models (e.g., Higuchi, Korsmeyer-Peppas) to understand the release mechanism.
Protocol 2: Fabricating Multi-Drug, Sequentially Releasing SMP Fibers via Thermal Drawing
This protocol describes creating multimaterial shape memory polymer fibers (SMPFs) for sequential drug release and light-triggered actuation [21].
1. Preform Fabrication:
- Materials: PDLLA, PLGA with different LA:GA ratios (e.g., 75:25 for slow, 50:50 for fast degradation), photothermal agent (e.g., dopamine hydrochloride), drugs (e.g., Doxorubicin, Curcumin).
- Procedure: Assemble a macroscopic preform by compression molding or machining the constituent polymers. Create hollow channels within the preform using removable PTFE or steel rods to serve as future drug reservoirs. The preform should have a structured cross-section with separate compartments for different drugs.
2. Thermal Drawing:
- Heat the preform in a custom drawing tower to its softening temperature (e.g., 160°C for PDLLA/PLGA). Apply tension to draw the preform into a continuous, microstructured fiber of the desired diameter (e.g., tens of meters long with 10 µm resolution). This process preserves the internal architecture of the preform at a miniaturized scale.
3. Photothermal Coating:
- Immerse the SMPFs in a alkaline dopamine solution (e.g., 2-6 mg/mL in Tris-HCl, pH 8.5) at 40°C for 72 hours. This will result in the self-polymerization of dopamine and the deposition of a uniform polydopamine (PDA) nanoparticle coating on the fiber surface. Rinse with deionized water.
4. Drug Loading and Sealing:
- Prepare drug solutions (e.g., 50 mg/mL in PBS with 0.5% Tween 80).
- Use a vacuum-assisted method to draw the drug solutions into the fiber's hollow channels.
- Seal both ends of the drug-loaded fiber segments with a water-resistant, biocompatible glue (e.g., Araldite Rapid).
5. Characterization:
- Drug Release: Immerse sealed fiber segments in PBS at 37°C. Monitor drug release at intervals via UV-Vis spectroscopy.
- Shape Memory Effect: Program the fiber into a temporary shape at elevated temperature, cool, and then trigger recovery using NIR light. Quantify recovery speed and ratio.
- Photothermal Effect: Expose PDA-coated fibers to NIR light and monitor temperature increase with a thermocouple.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Tailoring Polymer Release Profiles
| Material / Reagent | Function / Rationale for Use | Key Considerations |
|---|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | A benchmark biodegradable polyester. Degradation rate (weeks to years) is tuned by varying the LA:GA ratio. | 50:50 PLGA degrades fastest; 75:25 is slower. Acidic degradation products can cause autocatalytic erosion [25] [21]. |
| Methacrylated PCL-PGA-PTMC Triblock Resin | A photoreactive, fast-degrading resin for vat polymerization 3D printing. Allows room-temperature fabrication of complex, high-resolution devices. | Enables study of geometry-degradation-release relationships. Fast degradation allows observation of degradation-controlled release [20]. |
| Polydopamine (PDA) | A photothermal coating. Converts NIR light to heat, enabling remote, precise triggering of shape recovery and accelerated drug release from SMPs. | Coating thickness and density affect photothermal efficiency. Demonstrates good photostability over multiple cycles [21]. |
| Poly(D,L-lactide) (PDLLA) | An amorphous polymer with a distinct glass transition temperature (Tg). Serves as the shape memory matrix in thermally drawn fibers. | Amorphous nature ensures a sharp shape recovery transition. Good compatibility with other polymers like PLGA [21]. |
| Rhodamine B | A fluorescent small-molecule model drug (surrogate). Used for facile, quantitative tracking of release kinetics from prototype devices. | Allows for easy UV-Vis or fluorescence detection without the complexity and cost of handling active pharmaceutical ingredients (APIs) in early R&D [20]. |
| PCL (Poly(ε-caprolactone)) | A slow-degrading, semi-crystalline polyester. Provides extended mechanical support. Often used in blends to modulate the degradation rate of faster-degrading polymers. | Degradation time >2 years. Suitable for long-term implants. Can be methacrylated for VP printing [25] [20]. |
In biomedical applications, controlled degradation is a fundamental property that enables biomaterials to perform their function and then safely break down within the body. This process involves the breakdown of large molecules into smaller, less complex structures (by-products), which can then be metabolized or excreted [1]. For researchers developing microspheres, hydrogels, and nanocomposites, understanding and controlling this process is critical to ensuring material performance, biocompatibility, and therapeutic efficacy.
The ideal degradation profile for a biomaterial is one that matches the healing or regeneration process of the target tissue. Key considerations include the mechanical properties during degradation, the non-toxic nature of the by-products, and the appropriate permeability for the intended application [1]. This technical support guide addresses common fabrication and characterization challenges to help you achieve precise control over your material's degradation behavior.
Frequently Asked Questions (FAQs) & Troubleshooting
This section provides targeted solutions for common experimental issues encountered when fabricating controlled-degradation systems.
General Degradation Challenges
Q1: My biomaterial is degrading too quickly in vitro. What factors should I investigate?
- A: A rapid degradation rate often stems from an imbalance between material composition and the testing environment. Focus on these areas:
- Polymer Selection & Crosslinking Density: Materials with inherently fast hydrolysis rates (e.g., some polyesters) or a low density of crosslinks will degrade more quickly. Consider switching to a more stable polymer (e.g., PLA instead of PGA) or increasing your crosslinking density [28].
- Assessment Technique Error: A common mistake is interpreting simple dissolution as degradation. If your polymer is dissolving in the buffer without chain scission, you will see mass loss that is not true degradation. Confirm degradation by using chemical assessment techniques like SEC or NMR to monitor changes in molecular weight [1].
- Environmental Conditions: Ensure your in vitro degradation medium (e.g., PBS) has the correct pH (typically 7.4) and temperature (37°C). Small deviations can significantly accelerate hydrolysis. If using enzymatic media, verify the enzyme activity and concentration.
Q2: How can I conclusively confirm that my material is degrading, and not just dissolving?
- A: Physical tests like gravimetric analysis (measuring mass loss) can only infer degradation. To confirm it, you must use chemical characterization techniques that detect the breakdown of polymer chains [1]. The table below outlines the key methods.
Table 1: Techniques for Confirming Biomaterial Degradation
| Technique | What It Measures | How It Confirms Degradation |
|---|---|---|
| Size Exclusion Chromatography (SEC) | Molecular weight distribution | A shift to lower molecular weights indicates chain scission. |
| Nuclear Magnetic Resonance (NMR) | Chemical structure of polymer and by-products | Appearance of new peaks confirms the formation of degradation by-products. |
| Mass Spectrometry (MS) | Mass of molecules in a sample | Identifies the precise mass of small fragments and oligomers formed during degradation. |
| Fourier-Transform Infrared (FTIR) Spectroscopy | Changes in chemical bonds | A change in functional groups (e.g., decrease in ester bonds) indicates hydrolysis. |
Fabrication-Specific Issues
Q3: I am using microfluidics to create hydrogel microspheres (HMs), but I am getting polydisperse particles. How can I improve monodispersity?
- A: Polydispersity in microfluidics is typically related to unstable flow conditions.
- Stabilize Flow Rates: Ensure a stable, pulsation-free flow of both the continuous and dispersed phases using high-precision syringe pumps. Fluctuations in flow rate are a primary cause of size variation.
- Optimize Chip Design & Surface Properties: Use a chip design (e.g., flow-focusing) appropriate for your polymer's viscosity. The channel surface should be properly treated to be wetting for the continuous phase and non-wetting for the dispersed phase to prevent wetting and breakup [29] [30].
- Control Viscosity: The viscosity ratio between the dispersed and continuous phases can significantly affect droplet formation. Aim for a ratio that falls within the stable operating regime for your device geometry.
Q4: The mechanical strength of my nanocomposite hydrogel is insufficient for the target tissue. How can I reinforce it without compromising degradation?
- A: Weak mechanical properties can be addressed by incorporating reinforcing nanomaterials and optimizing the crosslinking network.
- Incorporate Nanomaterials: Add graphene oxide (GO) or other nanoparticles like clays or hydroxyapatite to the polymer matrix. These materials provide mechanical reinforcement through strong interfacial interactions, such as hydrogen bonding and π-π stacking [31] [28].
- Use Dual Cross-Linking: Implement a dual cross-linking strategy. For example, combine ionic crosslinking (which provides toughness) with covalent crosslinking (which provides strength). This creates a synergistic network that is robust yet can still degrade predictably [28].
This section consolidates key quantitative data on materials and assessment methods for easy comparison and experimental planning.
Table 2: Common Biomaterials for Controlled-Degradation Systems: Advantages and Limitations
| Material | Key Advantages | Key Disadvantages / Degradation Concerns |
|---|---|---|
| Gelatin (GelMA) | Contains cell-adhesive RGD sequences; good biocompatibility [30]. | Poor thermal stability; low mechanical strength [30]. |
| Alginate | Biocompatible; gentle ionic crosslinking (e.g., with Ca²⁺) [29] [30]. | Excessive swelling can lead to rapid drug release; low cell adhesion [30]. |
| Chitosan | Biocompatible; inherent antibacterial properties [29] [30]. | Poor water solubility at neutral pH; degradation rate is highly pH-sensitive [30]. |
| Polyethylene Glycol (PEG) | Excellent water solubility; highly tunable mechanical properties [30]. | Lacks cell adhesion sites; can be susceptible to oxidative degradation in vivo [30]. |
| Graphene Oxide (GO) in Nanocomposites | High surface area for drug loading; excellent mechanical reinforcement [31]. | Potential long-term cytotoxicity; aggregation in aqueous solutions can occur [31]. |
Table 3: Standardized Methods for Assessing Biomaterial Degradation
| Assessment Parameter | Standard Technique(s) | ASTM Guidelines / Key Considerations |
|---|---|---|
| Mass Loss | Gravimetric Analysis | ASTM F1635-11: Mass loss shall be measured to a precision of 0.1% of total sample weight [1]. |
| Molecular Weight Change | Size Exclusion Chromatography (SEC), Solution Viscosity | ASTM F1635-11: Molar mass shall be evaluated by SEC or solution viscosity [1]. |
| Morphological Change | Scanning Electron Microscopy (SEM) | Not a direct measure of degradation; used to visualize surface erosion and pore formation [1]. |
| Mechanical Property Change | Tensile/Compression Testing, Rheology | Monitor changes in storage/loss modulus (G'/G") or Young's modulus over time [1]. |
| By-product Identification | NMR, Mass Spectrometry, HPLC | Critical for confirming degradation and assessing by-product toxicity [1]. |
Experimental Protocols
Protocol: Fabricating Monodisperse GelMA Microspheres via Microfluidics
This protocol describes a method for creating cell-laden or drug-loaded gelatin methacryloyl (GelMA) microspheres with a uniform size distribution, a key factor in achieving consistent degradation and release profiles [29] [30].
Key Reagent Solutions:
- GelMA Pre-polymer Solution: GelMA polymer dissolved in a suitable buffer (e.g., PBS) at the desired concentration (e.g., 5-15% w/v).
- Photoinitiator: Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) or Irgacure 2959, added to the GelMA solution (e.g., 0.5% w/v).
- Continuous Phase: Surfactant-containing oil (e.g., 2-5% ABIL EM 90 in mineral oil).
- Crosslinking Solution: Calcium chloride solution (for alginate, if used as a composite) or a UV light source (λ = 365-405 nm, for GelMA).
Methodology:
- Microfluidic Device Setup: Prime a hydrophilic microfluidic flow-focusing device with the continuous phase (oil) to fill all channels.
- Droplet Generation: Load the GelMA pre-polymer solution (dispersed phase) into a syringe and pump it into the device at a defined flow rate (e.g., 100-500 μL/hr). Simultaneously, pump the continuous phase at a higher flow rate (e.g., 500-2000 μL/hr) to shear the aqueous stream into monodisperse droplets.
- Collection & Crosslinking: Collect the droplets in a tube. Expose the collected emulsion to UV light (e.g., 5-10 mW/cm² for 30-60 seconds) to photopolymerize the GelMA microspheres.
- Washing: Centrifuge the microspheres and wash several times with PBS or a biocompatible solvent to remove the oil and surfactant.
Diagram 1: Microsphere Fabrication Workflow
Protocol: StandardizedIn VitroDegradation Assessment
This protocol outlines a comprehensive approach to evaluating the degradation of solid biomaterial formulations, aligned with ASTM guidelines [1].
Key Reagent Solutions:
- Degradation Medium: Phosphate Buffered Saline (PBS, pH 7.4) or simulated body fluid (SBF). For enzymatic degradation, add the relevant enzyme (e.g., lysozyme, collagenase) at a physiologically relevant concentration.
- Fixation Solution: Glutaraldehyde (e.g., 2.5% in buffer) for SEM sample preparation.
- Solvents for SEC/NMR: Appropriate deuterated solvents or HPLC-grade mobile phases.
Methodology:
- Pre-Degradation Characterization (Day 0): Record the initial dry mass (W₀), dimensions, and mechanical properties of samples (n≥3). Analyze one sample via SEM, FTIR, and SEC to establish the baseline.
- Immersion in Degradation Medium: Place each sample in a separate vial containing a sufficient volume of degradation medium (e.g., 20:1 medium-to-sample volume ratio). Incubate at 37°C under gentle agitation.
- Time-Point Sampling: At predetermined time points (e.g., 1, 7, 14, 28 days), remove samples from the medium.
- Rinse & Dry: Gently rinse samples with deionized water and dry to a constant weight (e.g., under vacuum) for gravimetric analysis.
- Mass Loss Calculation: Calculate the percentage mass loss as:
[(W₀ - Wₜ) / W₀] * 100, where Wₜ is the dry weight at time t.
- Post-Degradation Characterization: Perform SEM on dried samples to observe surface erosion and cracks. Use SEC to determine the change in molecular weight and NMR/FTIR to identify chemical changes and by-products.
Diagram 2: Degradation Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Fabricating Controlled-Degradation Systems
| Reagent / Material | Function / Role | Example Application |
|---|---|---|
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable hydrogel polymer; provides cell-adhesive motifs [30]. | Fabrication of microspheres and scaffolds for tissue engineering. |
| Sodium Alginate | Natural polysaccharide; forms hydrogels via ionic crosslinking (e.g., with Ca²⁺) [29] [30]. | Cell encapsulation and drug delivery microspheres. |
| Chitosan | Natural cationic polymer; provides antibacterial properties and self-healing capacity [29] [30]. | Wound healing dressings and injectable drug depots. |
| Graphene Oxide (GO) | Nanomaterial additive; enhances mechanical strength and drug loading capacity [31]. | Reinforcing agent in nanocomposite hydrogels for bone tissue engineering. |
| Polyethylene Glycol (PEG) | Synthetic polymer; provides a "stealth" effect, reducing protein adsorption and improving biocompatibility [30]. | Creating non-fouling surfaces and tuning hydrogel mesh size. |
| Photoinitiators (e.g., LAP) | Generates free radicals upon UV/VIS light exposure to initiate polymer crosslinking [30]. | Photopolymerization of GelMA and PEG-based hydrogels. |
| Crosslinking Ions (e.g., CaCl₂) | Ionic crosslinker for polysaccharides like alginate [30]. | Gelation of alginate microspheres and fibers. |
Frequently Asked Questions (FAQs)
Q1: What are the primary reasons for a complete lack of assay window in TR-FRET-based drug screening? A complete lack of an assay window is most commonly due to improper instrument setup, particularly the selection of incorrect emission filters. Unlike other fluorescence assays, TR-FRET requires specific emission filters to function correctly. Additionally, differences in stock solution preparation between labs are a primary reason for variations in EC50/IC50 values [32].
Q2: How can premature drug release from nanoparticles be diagnosed and mitigated? Premature release can be identified by monitoring drug levels in the systemic circulation versus the target site. Mitigation strategies include:
- Polymer Selection: Using biodegradable polymers with slower degradation profiles, such as PLGA, which facilitates steady drug release for weeks [33].
- Surface Coating: Functionalizing the nanoparticle surface with hydrophilic polymers like Poly(ethyleneglycol) (PEG) to prolong circulation time and reduce nonspecific interactions [33].
- Cross-linking: Enhancing polymer stability, as demonstrated with poly (trimethylene carbonate) (PTMC) blended with PEGDA to significantly improve resistance to enzymatic erosion [3].
Q3: Why is the ratio metric data analysis method preferred in TR-FRET assays? The preferred practice is to calculate an emission ratio (acceptor signal divided by donor signal). This method accounts for small variances in reagent pipetting and lot-to-lot variability. The donor signal serves as an internal reference, making the ratio a more robust and reliable measurement than raw fluorescence units (RFUs) [32].
Q4: What are the key characteristics of an ideal targeted drug delivery complex? An ideal complex should be nontoxic, non-immunogenic, biochemically inert, biocompatible, and physicochemically stable in vivo and in vitro. It must have a predictable and controllable drug release pattern, be readily eliminated from the body, and demonstrate minimal drug leakage during transit [34].
Q5: What factors influence the cytotoxicity of nanoparticles? Nanoparticle cytotoxicity is size-, shape-, and chemistry-dependent [33]. The primary mechanism of in vivo nanotoxicity is the induction of oxidative stress by free radical formation, which can damage lipids, proteins, and DNA. Smaller nanoparticles often show higher cytotoxicity. This cytotoxicity can be reduced by functionalization with polymers like PEG [33].
Troubleshooting Guides
Table 1: Troubleshooting Nanoparticle Drug Delivery Systems
| Problem | Possible Cause | Diagnostic Method | Solution |
|---|---|---|---|
| Low Drug Loading Efficiency | Poor compatibility between drug and polymer matrix. | Analyze encapsulation efficiency during fabrication. | Optimize polymer-drug combination; use polymers like PLGA or chitosan known for high loading [33] [35]. |
| Rapid Clearance from Bloodstream | Opsonization and uptake by the reticuloendothelial system (RES). | Measure blood circulation half-life. | Functionalize nanoparticle surface with PEG or use hydrophilic coatings to increase biocompatibility [33]. |
| Lack of Target Site Accumulation | Poor targeting ligand affinity; insufficient EPR effect. | Use imaging (e.g., with magnetite or gold cores) to track biodistribution [33]. | Employ active targeting with cell-specific ligands (e.g., antibodies, peptides) [34]; optimize nanoparticle size (<200 nm) for enhanced EPR [33]. |
| High Batch-to-Batch Variability | Inconsistent fabrication processes. | Characterize particle size, polydispersity index, and zeta potential. | Implement standardized preparation protocols and strict quality control for raw materials [3]. |
| Induction of Oxidative Stress | Nanoparticle material (e.g., some metals) generating free radicals. | Assess biomarkers of oxidative stress in vitro and in vivo. | Select less reactive materials; use surface functionalization to passivate the nanoparticle surface [33]. |
Table 2: Troubleshooting Assay Performance in Drug Discovery
| Problem | Possible Cause | Diagnostic Method | Solution |
|---|---|---|---|
| No Assay Window | Incorrect instrument filter setup; failed development reaction. | Test reader setup with validated control reagents; perform a development reaction with 100% phosphopeptide control and substrate [32]. | Verify and use instrument-specific filter sets recommended for TR-FRET; titrate development reagent concentration [32]. |
| High Signal Variability (Poor Z'-factor) | Excessive noise from pipetting errors, reagent instability, or compound interference. | Calculate Z'-factor using positive and negative controls. | Ensure accurate liquid handling; use ratiometric data analysis to normalize pipetting variances; use fresh, stable reagents [32]. |
| Inconsistent EC50/IC50 Values | Differences in compound stock solution preparation. | Compare stock solution preparation protocols and purity analyses between labs. | Standardize compound solubilization and storage procedures across laboratories [32]. |
| False Positives in Drop Detection | Contamination or debris on DropDetection hardware. | Visually inspect target wells for dispensed liquid. | Clean the source tray and DropDetection openings with 70% ethanol and lint-free swabs [36]. |
Experimental Protocols
Protocol 1: Evaluating Nanoparticle Drug Release and Degradation Profile
This protocol is used to characterize the release kinetics of a therapeutic from a nanoparticle system and link it to carrier degradation, a critical parameter for prolonged release.
Key Research Reagent Solutions:
- Poly(lactic-co-glycolic acid) (PLGA): A biodegradable polymer used as the nanoparticle matrix for controlled drug release [33] [3].
- Phosphate Buffered Saline (PBS): A standard buffer for simulating physiological conditions during release studies.
- Dialysis Membrane: Used to separate released drug from nanoparticles during the experiment.
- Analytical Instrumentation (e.g., HPLC): For quantifying the amount of drug released over time.
Methodology:
- Nanoparticle Preparation: Prepare drug-loaded nanoparticles using a validated method, such as single or double emulsion-solvent evaporation for PLGA nanoparticles [33].
- Sink Condition Setup: Place a known amount of nanoparticles in a dialysis tube and immerse it in a large volume of release medium (e.g., PBS at pH 7.4) under sink conditions.
- Incubation and Sampling: Maintain the system at 37°C with constant agitation. At predetermined time intervals, withdraw samples from the release medium and replace with fresh medium to maintain sink conditions.
- Drug Quantification: Analyze the collected samples using a validated analytical method (e.g., HPLC/UV-Vis) to determine the cumulative drug release.
- Parallel Degradation Study: In a separate experiment, incubate nanoparticles under the same conditions. At key time points, isolate nanoparticles and characterize their molecular weight (via GPC), mass loss, and morphology (via SEM) to correlate drug release with polymer degradation.
Diagram 1: NP drug release workflow.
Protocol 2: Validating Active Targeting Efficiency via Cellular Uptake
This protocol assesses the effectiveness of ligand-functionalized nanoparticles for targeted delivery to specific cells.
Key Research Reagent Solutions:
- Targeting Ligands: Proteins, antibodies, peptides, or small molecules attached to the nanoparticle surface for receptor-specific binding [34].
- Fluorescent Dye (e.g., Cy5, FITC): Encapsulated in or conjugated to nanoparticles for visualization and quantification.
- Cell Culture Media and Reagents: For maintaining the target cell line.
- Flow Cytometry or Confocal Microscopy: Instruments to quantify and visualize cellular uptake.
Methodology:
- Nanoparticle Formulation: Prepare two batches of nanoparticles: one functionalized with the targeting ligand (e.g., an antibody) and a non-functionalized control. Incorporate a fluorescent dye into both batches.
- Cell Seeding: Seed the target cell line (which expresses the receptor of interest) and a negative control cell line (lacking the receptor) in multi-well plates. Grow to 70-80% confluency.
- Incubation with Nanoparticles: Treat the cells with a fixed concentration of the targeted or non-targeted nanoparticles. Incubate for a set period (e.g., 2-4 hours) at 37°C.
- Washing and Analysis:
- For Flow Cytometry: Trypsinize the cells, wash thoroughly to remove non-internalized nanoparticles, and resuspend. Analyze fluorescence intensity using a flow cytometer to quantify uptake.
- For Confocal Microscopy: Fix the cells after washing, stain the nucleus and cytoskeleton, and image using a confocal microscope to visualize the intracellular location of nanoparticles.
- Data Interpretation: Significantly higher fluorescence in cells treated with targeted nanoparticles (compared to non-targeted and negative control cells) confirms successful active targeting.
Diagram 2: Active targeting validation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Nanoparticle-Based Drug Delivery Research
| Material Category | Specific Examples | Function in Research |
|---|---|---|
| Polymer Matrices | PLGA, PLA, Chitosan, Gelatin, PEG | Form the core scaffold of the nanoparticle, controlling biodegradability, drug encapsulation, and release kinetics [33] [35] [3]. |
| Targeting Ligands | Antibodies, Peptides, Aptamers, Folic Acid | Conjugated to the nanoparticle surface for active targeting to specific cell receptors (e.g., on cancer cells) [33] [34]. |
| Surface Modifiers | Polyethylene Glycol (PEG), Polysorbates | "Stealth" coatings to reduce opsonization, prolong systemic circulation, and enhance bioavailability [33]. |
| Imaging & Tracking Agents | Fluorescent dyes (DiI, Cy5), Magnetic oxides (Fe₃O₄), Gold | Incorporated for in vitro and in vivo tracking, biodistribution studies, and diagnostic purposes (theranostics) [33]. |
| Stimuli-Responsive Materials | pH-sensitive polymers (e.g., poly methacrylic acid), Thermo-sensitive polymers | Enable controlled drug release triggered by specific local tissue characteristics (e.g., low tumor pH) or external actuation [33]. |
In bone tissue engineering, a primary challenge is designing polymer scaffolds that degrade at a rate matching the natural bone healing process [37] [38]. When scaffold degradation and tissue formation are mismatched, clinical outcomes are compromised. Excessively fast degradation can lead to a loss of mechanical support before new tissue can bear loads, causing tissue necrosis. Conversely, overly slow degradation can hinder tissue integration and impede complete regeneration [37] [39]. This technical support article provides a targeted guide for researchers troubleshooting degradation-related issues, framed within the broader thesis of resolving material degradation in biomedical applications.
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Why did my scaffold lose mechanical integrity much faster than it lost mass? This is a classic sign of bulk erosion, where hydrolysis occurs throughout the scaffold's volume, not just at the surface. This leads to a rapid decline in molecular weight and mechanical strength, often before significant mass loss is detectable [37] [1]. This is common in polymers like PLA and PLGA.
Q2: Our in vitro degradation tests do not match observed in vivo performance. What are key factors I might be missing? In vivo degradation is a more complex environment. Key missing factors often include:
- Enzymatic Activity: The in vitro use of enzymes like lysozyme can better simulate the biological environment [40].
- Cellular Activity: Immune cells like macrophages can actively phagocytose and degrade material fragments [37].
- Dynamic Mechanical Loads: Physiological loads applied to the scaffold can accelerate the degradation process, a factor rarely replicated in standard in vitro tests [37].
Q3: How does scaffold porosity and architecture influence degradation? Architecture is a critical, often overlooked, factor. Lower porosity can lead to a higher degradation rate due to internal acid autocatalysis, where acidic byproducts are trapped and accelerate the hydrolysis reaction in the scaffold's interior [37]. Furthermore, highly interconnected pores, typical of Triply Periodic Minimal Surface (TPMS) designs, can transform a typically surface-eroding polymer into a quasi-bulk eroding one by drastically increasing the surface-to-volume ratio exposed to the aqueous environment [37].
Q4: What does it mean if my scaffold's degradation is described as "bio-instructive"? This refers to a paradigm shift from scaffolds being passive supports to active participants in healing. A bio-instructive scaffold is engineered to release bioactive ions (e.g., Mg²⁺) or molecules (e.g., growth factors) as it degrades, which actively direct cell fate and orchestrate the regenerative process [41] [39].
Common Problems and Solutions
Problem: Rapid loss of mechanical strength.
- Solution: Consider blending polymers or creating composites. For example, incorporating magnesium hydroxide (Mg(OH)₂) into PLA scaffolds neutralizes acidic degradation products, moderates the degradation rate, and improves mechanical strength [39]. Alternatively, use polymers that exhibit surface erosion characteristics.
Problem: Inflammatory response upon implantation.
- Solution: This is often triggered by acidic degradation byproducts. Using self-neutralizing composites (like PLA/Mg(OH)₂) or selecting polymers with more neutral byproducts (like Poly(1,8-octanediol-co-citrate)) can mitigate this [39] [42]. Ensure degradation byproducts are non-toxic and can be metabolized or excreted [1].
Problem: Poor cell infiltration and tissue ingrowth.
- Solution: Re-evaluate scaffold architecture. Designs based on Triply Periodic Minimal Surfaces (TPMS) offer high surface-area-to-volume ratios, higher permeability, and reduced stress concentrations, which improve nutrient transport and cell migration [37]. Ensure pore interconnectivity.
Essential Experimental Protocols for Degradation Assessment
Protocol 1: Standard In Vitro Degradation and Gravimetric Analysis
This is a fundamental method for tracking mass loss over time [40] [1].
Workflow Diagram: In Vitro Degradation Assessment
Materials:
- Polymer Scaffolds: Pre-formed, sterile.
- Degradation Buffer: Phosphate Buffered Saline (PBS), pH 7.4, with or without enzymes (e.g., lysozyme at 0.5 mg/mL to simulate circulating blood) [40] [1].
- Equipment: Incubator (37°C), centrifuge, lyophilizer, analytical balance.
Method:
- Pre-weigh scaffolds (W₀) after lyophilization.
- Immerse scaffolds in degradation buffer under sterile conditions. Maintain at 37°C.
- Change the degradation buffer every 2-3 days to maintain enzyme activity and pH.
- At predetermined time points (e.g., 1, 2, 4, 8 weeks), retrieve samples (n=3-5).
- Rinse samples with deionized water to remove salts.
- Lyophilize samples until a constant weight is achieved.
- Weigh the dried scaffolds (W_d).
- Calculate the percentage of mass loss: % Degradation = [(W₀ - W_d) / W₀] × 100% [40].
Protocol 2: Non-Invasive Monitoring of Mechanical Property Changes
Ultrasound Elasticity Imaging (UEI) allows for non-destructive, longitudinal monitoring of the same sample, reducing inter-specimen variability [42].
Workflow Diagram: Non-Invasive Mechanical Assessment
Materials:
- Ultrasound System: With high-frequency transducer (e.g., 5 MHz center frequency).
- Mechanical Test Fixture or Phantom: For applying controlled deformation.
- Software: For phase-sensitive, 2D speckle tracking and strain calculation.
Method:
- Mount the scaffold in a tissue-mimicking phantom or implant it in vivo.
- Apply a small, controlled deformation to the sample.
- Acquire ultrasound radiofrequency data before and after deformation.
- Use a 2D speckle tracking algorithm to estimate internal displacements by maximizing the cross-correlation between pre- and post-compression echo fields.
- Calculate the strain field (elastogram) from the gradient of the displacement field.
- The resulting elastogram provides a quantitative map of local elastic properties. A decrease in stiffness (increase in strain) under constant load indicates scaffold degradation [42].
Quantitative Data and Material Selection
Comparative Degradation Profiles of Common Polymers
Table 1: Characteristics of Key Polymers for Bone Tissue Engineering Scaffolds [37] [38] [39]
| Polymer | Degradation Mechanism | Typical Degradation Time | Key Advantages | Key Challenges |
|---|---|---|---|---|
| PLA | Bulk Erosion | Months to Years | Good mechanical strength; FDA approved | Acidic byproducts cause inflammation; slow degradation |
| PCL | Bulk Erosion | 2-4 Years | Slow degradation good for long-term support; ductile | Too slow for many bone healing applications; hydrophobic |
| PLGA | Bulk Erosion | Weeks to Months | Degradation rate tunable by LA:GA ratio | Acidic byproducts; rapid loss of mechanical strength |
| Collagen | Enzymatic Surface Erosion | Weeks | Excellent biocompatibility and bioactivity | Poor mechanical strength; fast, uncontrolled degradation |
| Chitosan | Enzymatic Surface Erosion | Weeks to Months (tunable) | Antibacterial; can be cross-linked (e.g., with genipin) | Weak mechanical properties; batch-to-batch variability |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Scaffold Degradation Studies
| Item | Function/Application | Example & Notes |
|---|---|---|
| Lysozyme | Simulates enzymatic degradation in the body. | Use at 0.5 mg/mL in PBS to mimic circulating blood enzyme levels [40]. |
| Mg(OH)₂ Nanoparticles | Multifunctional nanofiller for synthetic polymers. | Neutralizes acidic PLA degradation products, improves mechanical strength, and releases osteoinductive Mg²⁺ ions [39]. |
| Genipin | Natural cross-linker for natural polymers. | Cross-links chitosan, improving its structural integrity and slowing its degradation rate to over 20 weeks [38]. |
| Triply Periodic Minimal Surface (TPMS) Design | Creating optimal scaffold architectures. | Provides high surface-area-to-volume ratio, reduced stress concentration, and superior permeability for nutrient transport [37]. |
| Ultrasound Elasticity Imaging (UEI) | Non-invasive mechanical characterization. | Tracks changes in scaffold elastic properties in the same specimen over time in vitro or in vivo [42]. |
Advanced Techniques and Conceptual Framework
The Erosion Typing Diagram
Understanding whether a polymer undergoes surface or bulk erosion is fundamental to predicting its performance. The dominant mechanism depends on the relative rates of water diffusion into the polymer and the hydrolysis of its chemical bonds [37].
Conceptual Diagram: Erosion Mechanism Decision Flow
The integration of degradable metals, particularly magnesium (Mg) alloys, into biomedical implants represents a paradigm shift from permanent to temporary, "smart" medical devices. These materials are engineered to provide temporary mechanical support and then harmlessly degrade, eliminating the need for secondary removal surgeries and mitigating long-term complications like stress shielding. However, their clinical translation is constrained by a central thesis challenge: balancing the inherent rapid degradation of magnesium with the requirement for prolonged mechanical integrity and biological compatibility. This technical support center is designed to help researchers troubleshoot critical issues, providing targeted FAQs, experimental protocols, and essential toolkits to navigate the complex journey of developing the next generation of biodegradable metallic implants.
Troubleshooting Guide: Common Experimental Challenges & Solutions
Researchers often encounter specific, recurring problems when working with degradable Mg alloys. The following guide addresses these key challenges.
Problem 1: Rapid Loss of Mechanical Strength In Vitro
- Q: My Mg alloy samples lose most of their yield strength within the first 2-3 weeks of in vitro testing, far too quickly for most bone healing applications. What is the cause and how can I mitigate this?
- A: This premature failure is primarily due to rapid, localized pitting corrosion, which creates stress concentration points and accelerates mechanical failure.
- Solutions:
- Alloying & Microstructure Control: Incorporate alloying elements like Strontium (Sr) and Manganese (Mn) to refine grains and form protective secondary phases. For instance, an extruded Mg-0.3Sr-0.4Mn alloy has been shown to achieve a yield strength of 205 MPa and reduce the corrosion rate by 54% compared to a binary alloy [43].
- Surface Engineering: Apply a protective coating. Micro-arc oxidation (MAO) can create a dense ceramic oxide layer, reducing corrosion rates from >2 mm/year to 0.3–0.8 mm/year. Hydroxyapatite (HA) coatings can further enhance osteoconductivity and slow degradation [44].
Problem 2: Excessive Hydrogen Gas Evolution
- Q: During in vitro tests, I observe significant hydrogen gas bubble formation on the sample surface. My in vivo models show gas pockets in the surrounding tissue. How can I control this?
- A: Hydrogen gas is a direct byproduct of the corrosion reaction of Mg in aqueous environments (Mg + 2H₂O → Mg(OH)₂ + H₂). Excessive evolution indicates an uncontrolled degradation rate [45].
- Solutions:
- Control Corrosion Rate: The primary strategy is to slow down the overall degradation. This can be achieved through the alloying and surface coating strategies mentioned above.
- Use Biopolymer Coatings: Coatings like chitosan-polycaprolactone nanocomposites have been reported to reduce hydrogen gas evolution by up to 60% (from 0.3 mL/cm²/day to 0.12 mL/cm²/day) by acting as a barrier and modulating the local pH [44].
Problem 3: Inconsistent Degradation Data
- Q: The degradation rates I measure from my experiments have high variability, making it difficult to draw reliable conclusions. How can I improve the reliability of my degradation assessment?
- A: Inconsistency often stems from a reliance on single-point measurements or techniques that can be confounded by factors like material solubility.
- Solutions:
- Multi-Method Assessment: Do not rely solely on gravimetric (weight loss) analysis. Combine it with chemical characterization techniques like SEM for morphology, FTIR for chemical group changes, and HPLC/SEC for quantifying degradation products [1].
- Standardized Protocols: Adhere to ASTM guidelines (e.g., F1635-11) for degradation testing, ensuring consistent pH, solution volume-to-surface area ratios, and temperature control [1].
Quantitative Performance of Select Mg Alloys
Table 1: Comparison of Key Properties for Biomedical Mg Alloys
| Material / Treatment | Yield Strength (MPa) | Ultimate Tensile Strength (MPa) | Corrosion Rate (mm/year) | Key Feature / Application |
|---|---|---|---|---|
| Extruded Mg-0.3Sr-0.4Mn | 205 | 242 | 0.39 | Optimal balance of strength & corrosion resistance [43] |
| Mg-Zn-Ca Alloy | ~150-250 (Compressive) | - | 0.5 - 1.2 | Good biocompatibility, bone-mimetic modulus [46] [44] |
| MAO-Coated Pure Mg | - | - | 0.3 - 0.8 | Ceramic oxide layer for enhanced corrosion resistance [44] |
| HA-Coated Mg-Zn-Ca | - | - | ~0.25 | Excellent osteoconductivity and very low degradation [44] |
| AE21 Alloy (Stent Prototype) | - | - | ~50% mass loss in 6 months | Early coronary stent study, demonstrates degradation principle [47] |
Detailed Experimental Protocols
Protocol 1: Standardized In Vitro Degradation Assessment (Based on ASTM F1635-11)
This protocol provides a foundational method for evaluating the degradation behavior of Mg alloy samples in a simulated physiological environment [1].
Sample Preparation:
- Prepare samples with a defined surface-area-to-volume ratio. A common size is a disk with a diameter of 10-15 mm.
- Polish all samples to a standardized surface finish (e.g., up to 2000-grit SiC paper) to ensure uniformity.
- Clean samples ultrasonically in acetone, ethanol, and deionized water, then dry thoroughly in a desiccator.
- Pre-degradation characterization: Weigh initial mass (M₀) and document surface morphology via SEM.
Immersion Test:
- Immerse individual samples in a buffered solution, such as simulated body fluid (SBF) or phosphate-buffered saline (PBS), at a pH of 7.4. The standard immersion ratio is >20 mL of solution per cm² of sample surface area.
- Maintain the environment at 37°C in an incubator to mimic physiological temperature.
- Consider refreshing the solution periodically (e.g., every 2-3 days) to maintain ion concentration and pH, or use a continuous-flow system.
Monitoring and Analysis:
- At predetermined time points (e.g., 1, 3, 7, 14, 28 days), remove samples from the solution.
- Gravimetric Analysis: Gently rinse and dry samples. Record the wet mass and then dry to a constant weight to obtain the dry mass (Mₜ). Calculate mass loss.
- Surface Morphology: Examine the corroded surface using SEM to identify pitting, uniform corrosion, or cracking.
- Chemical Analysis: Use techniques like EDX to analyze elemental composition changes and FTIR to detect formation of corrosion products (e.g., Mg(OH)₂).
- pH Monitoring: Record the pH of the immersion solution at each time point.
Protocol 2: Assessing Cytocompatibility and Osteogenic Potential
This protocol outlines a method to ensure that the alloy and its degradation products are non-toxic and support bone growth.
Preparation of Extract:
- Sterilize the Mg alloy samples (e.g., via UV light or ethanol immersion).
- Prepare an extract by immersing the sterile samples in cell culture medium (e.g., DMEM) at a prescribed surface-area-to-volume ratio (e.g., 1.25 cm²/mL) for 24-72 hours at 37°C. Filter the extract through a 0.22 µm filter to ensure sterility.
Cell Viability Assay (e.g., MTT Assay):
- Seed osteoblast-like cells (e.g., MC3T3-E1) in a 96-well plate at a standard density.
- After cell attachment, replace the standard culture medium with the prepared extract medium (typically using a dilution series: 100%, 50%, 25%).
- Incubate for 1-3 days. Then, add MTT reagent and incubate further. The metabolically active cells will convert MTT to purple formazan crystals.
- Dissolve the crystals and measure the absorbance using a plate reader. Cell viability should exceed 90% for the material to be considered non-cytotoxic [43].
Osteogenic Differentiation Assay:
- Culture cells in osteogenic induction medium containing the alloy extract.
- After 7-14 days, quantify the Alkaline Phosphatase (ALP) activity, an early marker of osteoblast differentiation. A significant increase (e.g., 2.46-fold higher ALP activity as reported for Mg-Sr-Mn alloys) indicates enhanced osteogenic potential [43].
Visualizing Key Concepts
Mg Alloy Degradation Mechanism
In Vitro Degradation Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Mg Alloy Implant Research
| Reagent / Material | Function / Purpose | Example & Notes |
|---|---|---|
| Simulated Body Fluid (SBF) | In vitro corrosion medium mimicking ion composition of blood plasma. | Kokubo's recipe is standard. Maintains ionic strength and pH (7.4) for realistic degradation screening [1]. |
| Strontium (Sr) & Manganese (Mn) | Alloying elements to enhance mechanical properties and corrosion resistance. | Sr refines grains and promotes osteogenesis; Mn forms protective nanoscale particles and traps impurities [43]. |
| Micro-Arc Oxidation (MAO) Electrolyte | For creating a protective ceramic coating on the alloy surface. | Typically silicate- or phosphate-based solutions. Forms a dense, adherent oxide layer (e.g., MgO/Mg₂SiO₄) [44]. |
| Hydroxyapatite (HA) Powder | For creating osteoconductive coatings on implants. | Can be applied via electrophoretic deposition or biomimetic growth. Significantly improves bone-implant integration [44]. |
| Alkaline Phosphatase (ALP) Assay Kit | To quantify osteogenic activity of cells exposed to alloy extracts. | A key metric for confirming the material's ability to support bone formation beyond basic cytocompatibility [43]. |
Frequently Asked Questions (FAQs)
Q1: What are the target values for mechanical properties and degradation rate in an ideal orthopedic Mg alloy?
- A: An ideal implant should simultaneously achieve a yield strength >200 MPa, elongation >10%, and a controlled degradation rate <0.5 mm/year to provide sufficient mechanical support until the bone is healed [43] [46]. The Mg-Sr-Mn alloy in Table 1 is an example of a composition approaching these targets.
Q2: How does the elastic modulus of Mg alloys compare to other implant metals and bone?
- A: The elastic modulus of Mg alloys (~35–45 GPa) is much closer to that of natural cortical bone (~15–25 GPa) than stainless steel or cobalt-chromium alloys (>200 GPa) or even titanium alloys (~110 GPa). This similarity drastically reduces the "stress-shielding" effect, which leads to bone resorption and implant loosening [43] [45] [44].
Q3: My alloy has excellent mechanical properties and a slow corrosion rate, but cells don't adhere well. What could be wrong?
- A: This could be due to a localized high pH environment or the initial rapid release of ions from the surface. Consider:
- Pre-conditioning: Soak the alloy in cell culture medium for 24 hours before cell seeding to allow for a more stable surface layer to form.
- Surface Topography: Cells adhere better to specific micro/nano-topographies. Surface treatments like sandblasting or etching can improve adhesion.
- Biofunctionalization: Coat the surface with extracellular matrix proteins like collagen or fibronectin to promote cell attachment [45] [44].
- A: This could be due to a localized high pH environment or the initial rapid release of ions from the surface. Consider:
Q4: Are there advanced manufacturing techniques for creating complex Mg alloy implants?
- A: Yes, additive manufacturing (AM or 3D printing) is a rapidly growing field for Mg alloys. Techniques like laser-based powder bed fusion enable the fabrication of patient-specific implants and complex porous structures that facilitate bone ingrowth and allow for topological control over the degradation profile [41] [48] [46].
Troubleshooting and Optimization: Strategies to Mitigate Premature and Uncontrolled Degradation
FAQs: Core Principles of Biodegradable Implant Failure
What are the most common failure points for biodegradable metal implants in orthopaedics? The primary failure points for biodegradable metal implants, such as those made from magnesium (Mg) and zinc (Zn) alloys, often relate to an unpredictable degradation rate and inadequate mechanical integrity [49]. If the implant degrades too quickly, it loses mechanical strength before the bone has sufficiently healed, leading to mechanical failure. Conversely, if it degrades too slowly, it can impede complete tissue regeneration and cause stress shielding, where the implant bears most of the load, resulting in bone resorption and weakening [50] [49]. The production of degradation by-products, such as hydrogen gas in the case of magnesium, can also cause adverse tissue reactions and failure [51].
Why does the in vivo degradation behavior of my implant material differ from in vitro test results? This discrepancy is a significant challenge in the field. In vitro tests often use simplified simulated body fluids and may not replicate the complex and dynamic biological environment found in vivo [51]. Factors such as local pH fluctuations, cellular activity, mechanical loading, blood flow, and immune responses in a living organism can drastically alter degradation kinetics. Consequently, the same material can show degradation rates that vary by an order of magnitude (e.g., 10-fold) between laboratory dishes and living tissue [51]. This highlights the critical need for well-designed in vivo validation.
How do alloying elements and microstructure influence the degradation of Mg-based implants? The composition and microstructure of an alloy are fundamental to its performance. Alloying elements are used to enhance mechanical strength and control the degradation rate. For example, elements like Zinc (Zn) and Manganese (Mn) in alloys such as Mg-2Zn-1Mn can significantly improve corrosion resistance, reducing degradation rates to as low as 0.36 mm/year [51]. However, the use of some elements, such as rare-earth elements, is debated due to concerns about their potential long-term accumulation in organs [51]. Furthermore, the microstructure, including grain size controlled by manufacturing processes, also critically affects degradation. Laser-based 3D printing can create fine microscopic grain structures (1–3 μm), which contribute to improved strength and corrosion resistance [51].
What role do surface coatings play in preventing unpredictable degradation? Surface engineering is a key strategy to manage degradation. Bioactive and protective coatings act as a barrier to slow down the initial corrosion rate of the underlying metal, allowing the implant to maintain its mechanical integrity during the critical healing period [52]. These coatings can be multifunctional. For instance, a hydroxyapatite (HA) coating encourages bone bonding (osseointegration), while an antibacterial coating (e.g., with silver nanoparticles or quaternary ammonium compounds) can prevent implant-related infections, which themselves can locally acidify the environment and accelerate corrosive failure [52].
Troubleshooting Guides: Experimental Analysis of Failure
Guide 1: Investigating Rapid, Premature Implant Failure
This guide addresses the scenario where an implant loses mechanical integrity before the expected tissue healing is complete.
Step 1: Quantify Degradation Rate and Gas Formation Conduct standardized in vitro immersion tests according to relevant ISO standards (e.g., ISO 25539) [53]. Monitor the mass loss, pH change of the solution, and critically, the volume of evolved hydrogen gas. A hydrogen evolution rate exceeding 10 μL/cm²-day is a key indicator of a corrosion rate that is too rapid for clinical safety [49].
Step 2: Analyze Mechanical Integrity Loss Periodically remove samples from the degradation medium and perform tensile tests. Compare the retained mechanical properties (e.g., yield strength, modulus) against the minimum values required for the specific application. For instance, bone plates often require a yield strength of 250–800 MPa [49]. A rapid drop in strength confirms premature mechanical failure.
Step 3: Characterize Microstructure and Surface Morphology Use scanning electron microscopy (SEM) to examine the surface for severe, localized pitting corrosion versus uniform degradation. Perform energy-dispersive X-ray spectroscopy (EDS) to identify the distribution of alloying elements and the presence of corrosive phases or impurities that may act as initiation sites for galvanic corrosion [49] [51].
Step 4: Identify Root Cause and Mitigation Strategy
- If uniform corrosion is excessive: The base material is too reactive. Consider alloying with protective elements (Zn, Mn), applying a dense surface coating, or using a higher purity material.
- If severe pitting is observed: The issue is likely localized galvanic corrosion. Investigate and modify the heat treatment process to homogenize the microstructure and reduce the formation of secondary phases.
Guide 2: Diagnosing Inconsistent Degradation Between Test Batches
This guide helps identify causes when the degradation performance of identical materials varies unpredictably between different experimental batches.
Step 1: Audit Raw Material Sources and Processing History Document and compare the certificate of analysis for all metal powders or ingots used, focusing on trace element and impurity levels. Variations in iron (Fe), nickel (Ni), or copper (Cu) content, even at low levels, can dramatically alter degradation behavior. Meticulously record all processing parameters, including temperatures, times, and deformation rates during manufacturing [51].
Step 2: Characterize Microstructural Consistency Analyze samples from each batch using optical microscopy and SEM to compare grain size, grain boundary distribution, and the size/volume fraction of secondary phases. Inconsistent thermal or mechanical processing often manifests as significant microstructural variations, which directly lead to differing degradation rates.
Step 3: Verify Surface Preparation and Sterilization Ensure that all samples undergo an identical surface finishing procedure (e.g., grinding, polishing) to the same roughness. Crucially, the sterilization method must be consistent, as techniques like gamma irradiation or autoclaving can oxidize or otherwise alter the surface chemistry, thereby affecting the initial degradation behavior [50].
Step 4: Standardize Degradation Testing Protocol Implement a strict, standardized operating procedure for in vitro tests. This includes using the same source and batch of simulated body fluid, maintaining a controlled temperature of 37±0.5°C, and ensuring a consistent solution volume-to-surface area ratio, as these factors are known to significantly influence results [51].
Quantitative Data on Biodegradable Materials
The following tables summarize key performance metrics for common biodegradable materials, providing a benchmark for evaluating experimental results.
Table 1: Target Mechanical and Degradation Properties for Orthopedic Implants
This table outlines the ideal property ranges for biodegradable orthopedic implants, based on design criteria discussed in the literature [49].
| Property | Target Value for Orthopedic Implants | Importance & Rationale |
|---|---|---|
| Yield Strength | 250 - 800 MPa | Withstands physiological loads without permanent deformation. |
| Elastic Modulus | 40 - 60 GPa (Mg-alloys); ~100 GPa (Zn-alloys) | Should match bone modulus (~30 GPa) to minimize stress shielding. |
| Elongation at Break | 10% - 20% | Provides necessary ductility to avoid brittle fracture. |
| Degradation Rate | < 0.5 mm/year | Ensures mechanical integrity is maintained during bone healing (typically 3-6 months). |
| Hydrogen Evolution Rate | < 10 μL/cm²-day | Minimizes gas cavity formation and tissue irritation. |
Table 2: Comparison of Common Biodegradable Metal Alloys
This table compares specific alloys and their reported properties, illustrating the progress and variations in the field [49] [51].
| Material/Alloy | Ultimate Tensile Strength (MPa) | Degradation Rate (mm/year) | Key Advantages | Reported Challenges |
|---|---|---|---|---|
| Pure Mg (Historical) | ~100 | > 400 (in vivo) [51] | Excellent biocompatibility, essential biological element. | Excessively fast degradation, high H2 gas production. |
| MAGNEZIX (Mg-2Zn-1Mn) | ~315 | ~0.36 [51] | Clinically validated, controlled degradation. | Long-term in vivo data beyond 5 years is limited. |
| Mg-2Zn-1Mn (3D-printed) | Improved | Improved | Fine-grained microstructure for enhanced strength/corrosion resistance. | Process parameter sensitivity, potential for defects. |
| Zn-based Alloys | 300 - 1000 | Varies | Inherent antibacterial properties, essential metabolic element. | Can be too strong (high modulus), degradation rate variability. |
Experimental Protocols for Degradation Analysis
Protocol 1: Standardized In Vitro Immersion Test for Metallic Implants
Objective: To quantitatively evaluate the degradation rate and mechanism of a biodegradable metal in a simulated physiological environment.
Materials:
- Simulated Body Fluid (SBF), prepared according to standard recipe (e.g., Kokubo's SBF)
- Thermostatic water bath, set to 37 ± 0.5°C
- pH meter and continuous logging system
- Gas collection apparatus (e.g., inverted burette for H2 collection)
- Analytical balance (accuracy 0.1 mg)
- Specimens prepared to a standardized surface finish (e.g., polished with SiC paper up to 2000 grit)
Methodology:
- Sample Preparation: Measure and record the initial weight and dimensions of each specimen. Clean ultrasonically in acetone, ethanol, and distilled water, then dry.
- Immersion Test: Place each specimen in a sealed container with a precise volume of SBF, ensuring a consistent surface-area-to-volume ratio (e.g., 1 cm² per 20-50 mL). Place containers in the thermostatic bath.
- Monitoring: Continuously monitor and record the pH of the solution. For Mg-based alloys, use the gas collection apparatus to measure the volume of evolved hydrogen gas at regular intervals.
- Sample Removal: Remove specimens after predetermined time points (e.g., 1, 3, 7, 14, 28 days). Gently clean them to remove corrosion products, following established protocols (e.g., using chromic acid).
- Post-analysis: Weigh the cleaned samples to determine mass loss. Calculate the degradation rate using standard formulas (e.g., from ASTM G31). Examine the surface morphology using SEM and analyze corrosion products using EDS or X-ray diffraction (XRD).
Protocol 2: Assessment of Retained Mechanical Strength During Degradation
Objective: To determine how the mechanical integrity of an implant material changes as it degrades over time.
Materials:
- Identical tensile or compression test specimens, depending on application.
- In vitro degradation setup (as in Protocol 1).
- Universal mechanical testing machine.
Methodology:
- Baseline Strength: Test a set of non-degraded specimens to establish the baseline mechanical properties (yield strength, ultimate tensile strength, elastic modulus, elongation).
- Degradation Period: Immerse other specimens in SBF for set periods that correspond to key healing stages (e.g., 2 weeks for initial healing, 6 weeks for callus formation, 12 weeks for bone remodeling).
- Retained Strength Testing: At each time point, remove specimens from the SBF, clean as in Protocol 1, and immediately perform mechanical testing under the same conditions as the baseline tests.
- Data Analysis: Calculate the percentage of retained strength and modulus for each time point. Plot these values against time to create a "strength retention profile." This profile should be compared to the required load-bearing timeline for the target application.
Visualization: Failure Analysis Workflow
The following diagram outlines a systematic workflow for analyzing unpredictable degradation in biodegradable implants, integrating the troubleshooting steps and protocols detailed above.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Materials for Investigating Implant Degradation
| Item | Function in Research | Application Note |
|---|---|---|
| Simulated Body Fluid (SBF) | In vitro solution mimicking ion concentration of human blood plasma. | The standard solution for initial degradation screening; does not fully replicate complex in vivo conditions [51]. |
| Mg, Zn, and Fe-based Alloy Ingots/Powders | Base materials for fabricating biodegradable implants. | High-purity grades are essential. Alloying with Zn, Mn, Ca is common to tailor properties [49] [51]. |
| Hydroxyapatite (HA) Powder | Used to create osteoconductive coatings on implants. | Coating applied via plasma spraying or electrodeposition to improve bone bonding and slow initial corrosion [52]. |
| Chromium Trioxide (CrO₃) | Main component of cleaning solution for removing corrosion products from degraded metal samples. | Used in post-immersion cleaning per standard ASTM G1 to accurately measure mass loss [49]. |
| Cell Culture Media (e.g., DMEM) | For cytocompatibility testing of degradation products. | Assesses biological response and ensures extracts from the degrading material are not cytotoxic [49]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary mechanisms of material degradation I should consider for biomedical implants? Material degradation in biomedical applications occurs through several key mechanisms. For metallic alloys, the primary concern is corrosion, which involves electrochemical reactions with bodily fluids that can compromise structural integrity and release potentially toxic ions [54] [55]. For polymers, degradation is often driven by hydrolysis (breakdown by water) and enzymatic activity, leading to chain scission and a loss of mechanical properties [56] [55]. Other critical mechanisms include wear from physical friction, fatigue from repeated stress cycles, and for some materials, thermal degradation [55].
Q2: How does the selection of alloying elements influence the performance of biodegradable metals like magnesium? The selection of alloying elements is crucial for tailoring the properties of biodegradable metals. The table below summarizes the primary alloying systems and their effects:
Table: Key Alloying Elements for Biodegradable Metallic Materials and Their Functions
| Base Metal | Common Alloying Elements | Primary Function/Effect on Properties |
|---|---|---|
| Magnesium (Mg) | Calcium (Ca), Zinc (Zn), Rare Earth elements (RE) | Improves corrosion resistance and refines grain structure to enhance mechanical strength [54]. |
| Iron (Fe) | Carbon (C), Manganese (Mn) | Increases strength and modulates the corrosion rate [54]. |
| Zinc (Zn) | Magnesium (Mg), Calcium (Ca) | Enhances mechanical properties and aims to achieve a more suitable corrosion rate for clinical applications [54]. |
Q3: What factors determine the degradation rate of a polymeric coating used for drug delivery? The degradation rate of a polymeric coating is not inherent to the material alone but is a function of multiple factors [56]. Key factors include:
- Material Properties: The chemical structure (e.g., presence of hydrolytically unstable bonds), crystallinity, and initial molecular weight of the polymer [56].
- Coating Architecture: The thickness of the coating, the use of polymer blends or copolymers, and the incorporation of active drugs or other compounds can significantly alter the degradation profile [56].
- Fabrication Technique: The method used to deposit the coating (e.g., spin coating, spray coating, dip-coating) influences its physico-chemical properties and, consequently, its degradation behavior [56].
Q4: What is the "bioink paradox" in 3D bioprinting, and how can it be managed? The "bioink paradox" describes the inherent conflict between printability and bio-functionality [41]. Materials that are mechanically robust and easy to print (e.g., some synthetic polymers) are often biologically inert. Conversely, materials that are biologically ideal (e.g., certain soft hydrogels that support cell growth) are frequently difficult to print due to poor mechanical strength [41]. This is managed through strategies like developing composite materials, using crosslinkable bioinks, and employing advanced printing techniques that support weak inks during fabrication [41].
Troubleshooting Guides
Issue: Premature Structural Failure of a Biodegradable Metallic Implant
Problem: A magnesium-based bone screw fractures long before the bone has healed.
Possible Causes and Solutions:
Cause: Excessively Rapid Corrosion
- Solution: Re-formulate the alloy composition. Increase the concentration of elements that improve corrosion resistance, such as Calcium or specific Rare Earth elements, to slow down the degradation rate [54].
- Experimental Verification: Conduct in vitro immersion tests in simulated body fluid (SBF) at 37°C. Monitor mass loss, pH change, and hydrogen evolution over time to quantitatively compare corrosion rates of different alloy compositions [54].
Cause: Inadequate Mechanical Strength (Fatigue)
- Solution: Utilize alloying elements like Zinc and processing techniques such as severe plastic deformation to refine the grain structure. A finer grain size typically enhances both strength and fatigue resistance [54].
- Experimental Verification: Perform mechanical testing, including tensile and fatigue tests (e.g., using an S-N curve approach), to characterize yield strength, ultimate tensile strength, and fatigue limit of the developed material [54] [55].
Issue: Uncontrolled Burst Release of a Drug from a Polymeric Coating
Problem: A drug-eluting stent coating releases over 80% of its drug payload within the first 24 hours, leaving no therapeutic agent for long-term treatment.
Possible Causes and Solutions:
Cause: Drug Located Near the Coating Surface
- Solution: Optimize the drug loading and distribution within the coating matrix. Ensure the drug is uniformly dispersed rather than concentrated on the surface. Using a multi-layer coating system with a drug-free top layer can also mitigate the initial burst [56].
- Experimental Protocol: Fabricate coatings using different loading methods (e.g., direct mixing vs. sorption loading). Characterize drug distribution using techniques like confocal Raman microscopy. Conduct in vitro drug release studies in phosphate-buffered saline (PBS) at 37°C, sampling at regular intervals and analyzing drug concentration via UV-Vis spectroscopy or HPLC [56].
Cause: Overly Rapid Hydration and Swelling of Polymer
- Solution: Select a polymer with higher crystallinity or more hydrophobic character to slow down water penetration. Alternatively, use a copolymer or polymer blend where one component controls the degradation rate [56].
- Experimental Protocol: Measure the water uptake (swelling ratio) of free-standing polymer films over time. Correlate the swelling kinetics with the drug release profile to understand the release mechanism (diffusion-dominated vs. degradation-dominated) [56].
Experimental Protocols & Data Presentation
Protocol: In Vitro Degradation and Ion Release Profiling of Biodegradable Alloys
Objective: To systematically evaluate the corrosion rate and ion release behavior of a novel biodegradable zinc-based alloy.
Materials:
- Specimens of the test alloy (e.g., Zn-Mg), machined and polished to a standard surface finish.
- Simulated Body Fluid (SBF), prepared according to standard recipes (e.g., Kokubo recipe).
- Analytical equipment: Inductively Coupled Plasma Mass Spectrometry (ICP-MS), pH meter, precision scale.
Methodology:
- Sample Preparation: Clean and sterilize alloy specimens. Record initial mass and dimensions.
- Immersion Test: Immerse specimens in SBF at a consistent volume-to-surface-area ratio. Maintain temperature at 37°C in an incubator.
- Monitoring: At predetermined time points (e.g., 1, 3, 7, 14, 28 days):
- Measure and record the pH of the solution.
- Collect aliquots of SBF for ICP-MS analysis to quantify released metal ions (Zn²⁺, Mg²⁺).
- Remove specimens, gently clean to remove corrosion products, and weigh to determine mass loss.
- Post-Test Analysis: Examine surface morphology of corroded specimens using Scanning Electron Microscopy (SEM).
Table: Example Data Output for Zn-1.5Mg Alloy Degradation in SBF
| Time Point (Days) | Mass Loss (mg/cm²) | Solution pH | Zinc Ion Concentration (ppm) | Magnesium Ion Concentration (ppm) |
|---|---|---|---|---|
| 1 | 0.05 | 7.4 | 0.8 | 0.1 |
| 7 | 0.25 | 7.6 | 3.5 | 0.4 |
| 14 | 0.60 | 7.8 | 8.1 | 0.9 |
| 28 | 1.45 | 8.0 | 18.5 | 1.8 |
Protocol: Fabrication and Release Kinetics of a PLGA-based Drug Delivery Coating
Objective: To fabricate a Poly(lactic-co-glycolic acid) (PLGA) coating on a substrate and characterize its drug release profile.
Materials:
- PLGA (50:50 LA:GA ratio), model drug (e.g., a fluorescent dye or an API).
- Organic solvent (e.g., dichloromethane, DCM).
- Substrate (e.g., a small metal coupon or glass slide).
- Phosphate Buffered Saline (PBS), dialysis membrane (if needed), UV-Vis Spectrophotometer.
Methodology:
- Coating Fabrication (Dip-Coating):
- Prepare a solution of PLGA and the model drug in DCM.
- Dip the substrate into the solution at a controlled, steady rate.
- Withdraw the substrate and allow the solvent to evaporate fully in a fume hood, forming a thin, uniform film. Repeat for multiple layers if needed.
- In Vitro Release Study:
- Place the coated substrate into a vessel containing PBS as the release medium. Agitate continuously in a 37°C shaker bath.
- At predetermined intervals, withdraw a small aliquot of the release medium and replace it with fresh PBS to maintain sink conditions.
- Analyze the concentration of the drug in the aliquots using UV-Vis spectrophotometry at the drug's characteristic absorbance wavelength.
- Data Analysis: Plot cumulative drug release (%) versus time to generate the release profile. Fit the data to mathematical models (e.g., Higuchi, Korsmeyer-Peppas) to understand the release mechanism.
Visualizing Material Design and Degradation Pathways
Diagram: Material Design and Degradation Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Materials for Investigating Biomaterial Stability
| Material/Reagent | Function in Experimentation | Key Considerations |
|---|---|---|
| Simulated Body Fluid (SBF) | An aqueous solution with ion concentrations similar to human blood plasma; used for in vitro corrosion and degradation testing [54]. | Formulation must match standard recipes (e.g., Kokubo). pH and temperature (37°C) must be carefully controlled. |
| PLGA (Poly(lactic-co-glycolic acid)) | A biodegradable synthetic polymer widely used for drug-eluting coatings and scaffolds due to its tunable degradation rate [57] [56]. | The lactic to glycolic acid ratio (e.g., 50:50, 75:25) determines crystallinity and degradation speed. |
| Poly-Hydroxy-Alkanoates (PHA) | Biodegradable polyesters produced by microorganisms; used in drug carriers and tissue engineering for their high biocompatibility [57]. | Degradation yields metabolites natural to the body. Production cost can be higher than synthetic polymers. |
| Chitosan | A natural biopolymer derived from chitin; used in hydrogels, microparticles, and scaffolds for its biocompatibility and hemostatic properties [57]. | Excellent for drug loading and release, but mechanical properties may require blending with other polymers. |
| ICP-MS (Inductively Coupled Plasma Mass Spectrometry) | An analytical technique for detecting and quantifying metal ion concentrations in solution at very low levels [54]. | Essential for monitoring ion release (e.g., Mg²⁺, Zn²⁺, Fe²⁺) from corroding metallic implants in SBF. |
| UV-Vis Spectrophotometer | An instrument that measures the absorption of light by a solution; used to quantify drug concentration in release studies [56]. | Requires the drug to have a chromophore that absorbs at a specific wavelength for accurate quantification. |
Core Concepts: Degradation Mechanisms and Process Control
What are the primary degradation mechanisms for biomaterials and biopharmaceuticals?
Biomaterial degradation occurs through several key mechanisms, each requiring specific control strategies during manufacturing:
- Hydrolysis: Chemical bonds in the polymer chain (esters, anhydrides, orthoesters, carbonates, amides) react with water molecules, breaking into smaller segments. The rate depends on chemical reactivity, water diffusion, and polymer-water interactions [58].
- Oxidation: Oxidants produced by biological systems or present in the formulation degrade materials. Polyurethane insulation in implantable devices can fail via this mechanism [58].
- Enzymatic Degradation: Biological enzymes from patients break down materials like collagens, polysaccharides, and some polyesters. This varies significantly between individuals and tissue types [58].
- Physical Degradation: Includes mechanical friction, wear (e.g., in joint replacements), water swelling, and interfacial delamination in composites [58].
How do manufacturing parameters influence initial material damage?
Process parameters critically impact initial damage by affecting molecular structure and stability:
- Polymer Processing History: Orientation, crystallinity, and residual stresses from manufacturing affect degradation kinetics [58].
- Formulation Conditions: pH, ionic strength, temperature during processing can induce aggregation, deamidation, isomerization, hydrolysis, oxidation, or denaturation [59].
- Environmental Control: Exposure to moisture, oxygen, or elevated temperatures during manufacturing accelerates degradation pathways [58].
Troubleshooting Common Process Optimization Issues
How can I reduce high viscosity in concentrated protein formulations?
High viscosity poses challenges for subcutaneous injection administration. Implement these solutions:
| Solution Approach | Mechanism of Action | Implementation Considerations |
|---|---|---|
| Add Hydrophobic Salts | Modifies protein-protein interactions | Concentration optimization needed to avoid precipitation |
| Add Inorganic Salts | Shields electrostatic attractions | Must maintain isotonicity for injectables |
| Add Lysine or Arginine | Disrupts viscous network formation | Compatibility with protein stability |
| Co-inject Recombinant Human Hyaluronidase | Degrades hyaluronic acid in subcutaneous space | Increases diffusion rate at injection site [59] |
What strategies prevent protein aggregation and instability during processing?
Protein instability stems from multiple pathways requiring comprehensive control:
- Excipient Strategy: Incorporate small sugars (trehalose), polysaccharides (dextrans), Pluronics, or non-ionic surfactants (polysorbates) to stabilize against aggregation [59].
- Environmental Control: Maintain tight control over temperature, pH, and ionic strength throughout manufacturing [59].
- Mechanistic Understanding: Conduct pre-formulation studies to identify specific degradation pathways (aggregation, deamidation, oxidation) for targeted stabilization [59].
Experimental Protocols for Process Optimization
Systematic Approach to Bioprocess Optimization with Quality by Design (QbD)
The QbD framework provides a structured methodology for identifying optimal process parameters:
Figure 1. QbD workflow for systematic process optimization.
Methodology:
- Define Target Product Profile: Establish desired product quality, efficacy, and safety attributes [60].
- Identify Critical Quality Attributes (CQAs): Determine physical, chemical, biological properties affecting product function (e.g., glycosylation patterns, aggregation state) [60].
- Identify Critical Process Parameters (CPPs): Select process variables (pH, temperature, media composition) potentially affecting CQAs [60].
- Design of Experiments (DoE): Use structured experimental designs (factorial, fractional factorial) to efficiently explore parameter relationships [60].
- Establish Design Space: Define multidimensional parameter combinations ensuring quality attributes [60].
- Implement Control Strategy: Apply monitoring and controls to maintain processes within design space [60].
Protocol for Assessing Biomaterial Degradation
Follow ASTM F1635-11 guidelines with these enhancements for comprehensive assessment:
Figure 2. Biomaterial degradation assessment workflow.
Detailed Protocol:
- Pre-degradation Characterization:
- Document initial mass, dimensions, morphology (SEM), molecular weight (GPC/SEC), mechanical properties, and chemical structure (FTIR) [1].
Degradation Conditions:
- Immerse samples in appropriate media (PBS, simulated body fluid, enzymatic buffers) at pH 7.4 or tissue-specific pH [1].
- Maintain at physiological temperature (37°C) with agitation if simulating dynamic conditions.
- Include appropriate controls without degradation media.
Time-point Sampling:
- Collect samples at predetermined intervals based on expected degradation profile.
Multi-modal Assessment:
- Gravimetric Analysis: Measure mass loss to precision of 0.1% total sample weight after drying to constant weight [1].
- Molecular Weight Changes: Use size exclusion chromatography (SEC) or solution viscosity [1].
- Morphological Changes: SEM imaging for surface erosion, cracking, porosity development [1].
- Mechanical Testing: Track tensile strength, modulus, elongation changes [1].
- Chemical Analysis: FTIR, NMR, mass spectrometry to confirm degradation products [1].
Data Integration:
- Correlate physical, chemical, and mechanical changes to build comprehensive degradation model.
Advanced Optimization Methodologies
How can experimental design improve process optimization efficiency?
Strategic experimental design maximizes information gain while minimizing resource use:
| Design Approach | Best Application | Key Advantages | Limitations |
|---|---|---|---|
| Full Factorial | Investigating all factor interactions | Comprehensive interaction data | High experimental burden with many factors |
| Fractional Factorial | Screening many factors efficiently | Reduced experiments while maintaining key information | Aliasing of some interactions |
| Response Surface | Optimizing process parameter levels | Models nonlinear relationships | Requires more levels per factor |
| Sequential Design (4S Method) | Iterative optimization [61] | START-SHIFT-SHARPEN-STOP framework | Requires multiple experimental rounds |
Implementation Guidelines:
- Define Optimization Success: Establish clear criteria (e.g., "≥90% yield with ≤5% aggregation") before experimentation [62].
- Use Frameworks: Apply structured frameworks like Multiphase Optimization Strategy (MOST) for systematic approach [62].
- Consider Constraints: Explicitly account for resource limitations (time, cost, materials) during design [62].
When should I consider machine learning for process optimization?
Machine learning (ML) enhances traditional approaches for complex, high-dimensional processes:
Applications:
- Non-linear Relationship Modeling: Capture complex CQA-CPP relationships beyond linear MVDA capabilities [60].
- High-dimensional Data: Handle multi-omics, in-situ spectra, and conventional analytical data simultaneously [60].
- Novel CPP Identification: ML feature selection algorithms can identify previously unrecognized critical parameters [60].
Implementation Considerations:
- Data Requirements: Substantial datasets needed for effective model training [60].
- Hybrid Modeling: Combine ML with mechanistic models for interpretable predictions [60].
- Validation: Rigorous experimental validation required before implementation in regulated environments [60].
The Scientist's Toolkit: Essential Research Reagents and Materials
| Category | Specific Items | Function in Process Optimization |
|---|---|---|
| Stabilizers | Trehalose, Dextrans, Polysorbates, Pluronics | Reduce protein aggregation and surface adsorption [59] |
| Viscosity Reducers | Hydrophobic salts, Lysine, Arginine, Inorganic salts | Enable high-concentration protein formulations [59] |
| Degradation Media | PBS, Simulated body fluids, Enzyme solutions | Accelerated degradation studies under physiological conditions [1] |
| Polymer Matrices | PLGA, Polyanhydrides, Cyclodextrins | Controlled-release delivery systems [59] |
| Analytical Standards | Molecular weight markers, Chemical reference standards | Quantification of degradation products [1] |
Quality Control and Risk Management
What quality standards apply to manufacturing process optimization?
Medical device and biopharmaceutical manufacturing must adhere to rigorous standards:
- FDA Quality System Regulation (21 CFR Part 820): Required for original equipment manufacturers, defines QMS requirements [63].
- ISO 13485:2016: Global standard for medical devices quality management systems [63].
- Current Good Manufacturing Practices (cGMP): FDA regulations ensuring proper design, monitoring, and control of manufacturing [63].
- ASTM Standards: ASTM F1635-11 provides specific guidelines for biodegradation assessment [1].
How can I implement effective quality control for process parameters?
Establish robust quality management systems with these elements:
- Comprehensive Documentation: Detailed standard operating procedures for all processes [63].
- Supplier Qualification: Rigorous vetting of material suppliers with ongoing evaluation [63].
- Process Validation: Intensive multi-phase validation including molding, assembly, and functional testing [63].
- Quality Culture: Empower all employees to stop processes if quality concerns arise [63].
- Reverse Engineering: For replacement parts, use reverse engineering rather than copying to ensure OEM-equivalent performance [63].
Welcome to the Technical Support Center for Biomaterials Research. This resource is designed to assist researchers, scientists, and drug development professionals in diagnosing and resolving common challenges associated with the development and performance of coated biomaterials. The guidance herein is framed within the critical context of resolving material degradation in biomedical applications, a fundamental hurdle for the clinical success of implants, tissue engineering scaffolds, and drug delivery systems. The following sections provide structured troubleshooting guides, detailed experimental protocols, and essential resource tables to support your research efforts.
Troubleshooting Guide: Coating and Surface Modification Challenges
A flawless, functional coating is paramount for biomaterial performance. The table below summarizes common problems, their root causes, and evidence-based solutions.
Table 1: Troubleshooting Common Coating and Surface Modification Problems
| Problem | Primary Causes | Recommended Solutions |
|---|---|---|
| Poor Adhesion & Delamination [64] [65] | Inadequate surface preparation (contamination, oils) [64]; Incorrect curing process [64]; Mismatch between coating and substrate mechanical properties [65]. | Improve surface cleaning and plasma treatment [66]; Verify curing oven temperature/cycle [64]; Use a flexible, high-elongation coating like polyurea for dynamic substrates [65]. |
| Blistering & Bubbles [65] | Surface contamination (oils, salts) [64]; Moisture or solvent entrapment during application [65]; Application in high-humidity conditions [65]. | Ensure substrate is clean and thoroughly dry [64] [65]; Apply coatings in controlled environments; Use multiple thin coats instead of one heavy coat [65]. |
| Pinholes [64] | Contaminants on substrate; Incorrect powder/film thickness; Overbaking or underbaking. | Clean and dry substrate before application; Apply material in even layers; Adjust curing process to recommended parameters [64]. |
| Orange Peel Effect [64] | Incorrect curing temperature or time; Improper spray gun settings; Substrate contamination. | Ensure correct curing oven operation; Adjust spray gun for even application; Clean substrate thoroughly before coating [64]. |
| Cracking [65] | Coating applied too thick; Use of overly hard/inflexible coating; Thermal expansion/substrate movement. | Remove cracked coating and reapply; Select a flexible coating (e.g., polyurea with >200% elongation); Apply at manufacturer's recommended thickness [65]. |
| Fish Eyes [64] [67] | Contamination from silicones or oils; Inadequate cleaning of equipment or substrate. | Conduct thorough cleaning of substrate and equipment; Use clean, filtered air; Avoid silicone-containing products near the coating area [64]. |
| Unwanted Biological Response (Thrombosis, Inflammation) [68] | Protein adsorption and conformational changes triggering coagulation cascade [68]; Poor hemocompatibility. | Implement bio-inert coatings (e.g., PEG) or bioactive coatings (e.g., heparin); Use biomimetic coatings that replicate endothelial properties [68]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary surface modification strategies to improve the biocompatibility of metallic implants? Several strategies have proven effective. These include:
- Film and Coating Synthesis: Applying a biocompatible layer, such as a Cu-containing bioactive glass, which exhibits antibacterial properties and can promote stem cell differentiation [66].
- Plasma Surface Modification: Using plasma treatment to introduce hydrophilic functional groups that resist non-specific protein adsorption and bacterial adhesion [66].
- Covalent Grafting and Self-Assembled Monolayers (SAMs): Creating ordered molecular coatings that provide antifouling properties and resist non-specific protein adsorption [66].
Q2: Why is my biodegradable polymer scaffold failing mechanically long before tissue regeneration is complete? This is a classic issue of degradation rate mismatch. The degradation time of the material must coincide with the healing or regeneration process [69]. If the scaffold loses mechanical integrity too quickly, it cannot support the growing tissue. This can be due to:
- Bulk Erosion: Polymers like poly(lactic acid) (PLA) and poly(glycolic acid) (PGA) undergo bulk erosion, where water penetrates the entire structure, leading to a sudden loss of mechanical properties [69].
- Solution: Consider using surface-eroding polymers (e.g., certain polyanhydrides) or composite materials whose degradation profiles can be more finely tuned to match the healing timeline of the target tissue [69].
Q3: How can I accurately assess the degradation profile of my biomaterial formulation to avoid misleading results? Degradation assessment must move beyond simple gravimetric analysis (mass loss), as weight loss can be mistaken for dissolution rather than true chemical degradation [1]. A conclusive assessment requires a multi-faceted approach:
- Chemical Analysis: Use techniques like Size Exclusion Chromatography (SEC) to track changes in molecular weight, or NMR and Mass Spectrometry to identify degradation by-products. This confirms degradation is occurring [1].
- Physical and Mechanical Monitoring: Supplement chemical data with tracking of surface erosion via SEM, and changes in mechanical properties like tensile strength [1].
- Follow ASTM Guidelines: Adhere to standards like ASTM F1635-11, but be aware of their limitations. The future of degradation assessment lies in real-time, non-invasive, and continuous monitoring techniques [1].
Q4: Our blood-contacting device is triggering thrombosis. What surface modification approaches can improve hemocompatibility? Thrombosis on blood-contacting materials is initiated by protein adsorption, which activates the coagulation cascade and platelets [68]. Two main strategic approaches exist:
- Bio-inert Coatings: Create a passive barrier that minimizes protein adsorption. Examples include polyethylene glycol (PEG) and zwitterionic polymers [68].
- Bioactive Coatings: Incorporate active biological agents. Heparin immobilization is a classic example that inhibits the coagulation cascade. A more advanced strategy is the use of biomimetic coatings designed to replicate the endothelial cell layer that lines native blood vessels, promoting the generation of a natural, non-thrombogenic surface [68].
Key Experimental Protocols
Protocol 1: Assessing Biomaterial Degradation In Vitro
This protocol outlines a comprehensive method for evaluating biomaterial degradation, crucial for predicting in vivo performance.
Workflow Diagram: Biomaterial Degradation Assessment
Detailed Methodology:
- Pre-degradation Assessment: Characterize the initial properties of the biomaterial, including dry mass, dimensions, molecular weight (via SEC), surface morphology (via SEM), and mechanical strength [1].
- Immersion in Degradation Media: Immerse the material in a suitable medium, such as phosphate-buffered saline (PBS, pH 7.4) or simulated body fluid, with or without enzymes (e.g., lysozyme) relevant to the application site. Use a sterile container and ensure a high surface-area-to-volume ratio [1].
- Incubation: Place the containers in an incubator maintained at 37°C under gentle agitation to simulate physiological conditions. The incubation duration should be based on the expected degradation profile of the material [1].
- Sample Withdrawal: At predetermined time intervals, remove samples from the media in triplicate. Gently rinse with deionized water and dry to a constant weight before analysis [1].
- Post-degradation Analysis:
- Gravimetric Analysis: Measure mass loss to a precision of 0.1% of the total sample weight [1].
- Morphological Analysis: Use SEM to visualize surface erosion, cracking, or pitting.
- Chemical Analysis: Use SEC to detect changes in molecular weight and NMR/FTIR to identify chemical structure changes and degradation by-products [1].
- Mechanical Testing: Perform tensile or compression tests to track the loss of mechanical integrity over time [1].
Protocol 2: Developing an Antifouling Coating via Covalent Grafting
This protocol details the creation of a stable, antifouling surface on a biomaterial.
Workflow Diagram: Antifouling Coating Development
Detailed Methodology:
- Substrate Activation and Cleaning: Thoroughly clean the substrate (e.g., titanium, polymer film) with solvents and oxygen plasma treatment. Plasma treatment cleans the surface and introduces reactive hydroxyl or carboxyl groups [66].
- Surface Functionalization: Immerse the activated substrate in a solution containing a coupling agent, such as silanes (for metal/glass) or aminolysis (for polyesters), to introduce reactive functional groups (e.g., amine, carboxyl) for subsequent grafting [66].
- Polymer Grafting: Covalently link an antifouling polymer to the functionalized surface. For example:
- Grafting-from: Immobilize an initiator on the surface and perform surface-initiated polymerization of a monomer like poly(ethylene glycol) methacrylate (PEGMA).
- Grafting-to: React a pre-synthesized, end-functionalized polymer (e.g., amine-terminated PEG) with the complementary reactive groups on the surface [66] [69].
- Validation: Characterize the modified surface using:
- Performance Testing: Validate antifouling efficacy using a protein adsorption assay (e.g., with fluorescently labelled fibrinogen) and a bacterial adhesion assay (e.g., against S. aureus and S. epidermidis) [66].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Biomaterial Surface Modification
| Reagent/Material | Function in Research |
|---|---|
| Poly(Ethylene Glycol) (PEG) & Derivatives | The gold-standard for creating bio-inert, protein-resistant surfaces. Used in grafted polymer brushes and hydrogel coatings to reduce fouling and improve biocompatibility [66] [68]. |
| Heparin | A bioactive glycosaminoglycan immobilized on blood-contacting devices (e.g., stents, grafts) to provide local anticoagulant activity and prevent thrombosis [68]. |
| Polydopamine | A nature-inspired polymer that forms adherent coatings on virtually any substrate. Serves as a versatile platform for secondary functionalization with biomolecules or polymers [66]. |
| Poly(Lactic-co-Glycolic Acid) (PLGA) | A widely used, FDA-approved biodegradable polymer for drug delivery and tissue engineering. Its degradation rate can be tuned by altering the lactide to glycolide ratio [69] [70]. |
| Hyaluronic Acid (HA) | A natural polysaccharide used in coatings and hydrogels for its excellent biocompatibility, role in cell signaling, and promotion of wound healing and cartilage regeneration [70]. |
| Bioactive Glass (e.g., 4555) | A ceramic coating material for bone tissue engineering. Bonds to bone and can be doped with ions (e.g., Cu²⁺, Sr²⁺) to impart antibacterial or osteogenic properties [66]. |
| Self-Assembled Monolayer (SAM) Molecules | Model surfaces for fundamental studies on cell-material interactions. Alkanethiols on gold or alkylsilanes on glass/oxide create well-defined, ordered surfaces with terminal functional groups [66]. |
The path to clinical translation for biomaterials is fraught with challenges related to material degradation and host response. A meticulous approach to surface modification, coupled with rigorous and multi-faceted degradation assessment, is non-negotiable for success. This Technical Support Center has outlined common pitfalls and provided proven protocols to guide researchers in developing more reliable, effective, and safe biomedical devices. The future of the field lies in smarter, biomimetic materials designed to work in harmony with the body's innate healing processes.
Degradation-Based Optimization (DBO) refers to a class of computational techniques that employ nature-inspired algorithms to model and predict the degradation behavior of biomedical materials. In the context of longevity medicine and biomedical applications, these frameworks are crucial for optimizing the performance and safety of resorbable implants, drug delivery systems, and tissue engineering scaffolds [71]. The primary challenge in this field lies in accurately predicting how materials will break down in biological environments while maintaining biocompatibility and functional integrity throughout their lifespan [1] [72].
The Dung Beetle Optimizer (DBO), a recently developed nature-inspired metaheuristic algorithm, has shown remarkable potential for addressing these complex prediction challenges. DBO effectively identifies optimal solutions by simulating dung beetles' foraging, rolling, breeding, and navigation behaviors, which correspond to global exploration and local exploitation phases in optimization [73] [74]. When applied to high-dimensional biomedical data, DBO-based frameworks can identify informative feature subsets, reduce computational costs, and improve the biological interpretability of predictive models [73].
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: What is Degradation-Based Optimization (DBO) and why is it relevant to biomedical material degradation studies?
DBO encompasses computational optimization techniques, including algorithms like the Dung Beetle Optimizer, that are applied to model and predict material degradation. For biomedical researchers, it provides a method to identify optimal material compositions and design parameters that achieve desired degradation profiles for specific clinical applications [73] [75]. This is particularly valuable for longevity medicine applications where material performance must be maintained throughout the treatment period before controlled degradation occurs [71] [76].
Q2: My DBO model converges prematurely to local optima when predicting complex degradation kinetics. How can I address this?
Premature convergence is a recognized limitation in basic DBO implementations [74]. To address this issue:
- Implement the Elite Bernoulli-based Mutated DBO with Local Escaping Operator (EBMLO-DBO), which integrates a Morlet Wavelet mutation to help the algorithm escape local optima [74]
- Apply an adaptive T-distribution perturbation strategy that enhances global exploration in early iterations and local search capabilities in later stages [77]
- Increase population diversity through Bernoulli map-based initialization instead of random generation [74]
Q3: What are the key physical, chemical, and mechanical parameters I should monitor for comprehensive degradation assessment?
A comprehensive degradation assessment should monitor parameters across multiple domains [1]:
Table 1: Essential Parameters for Biomaterial Degradation Assessment
| Category | Specific Parameters | Measurement Techniques |
|---|---|---|
| Physical | Mass loss, Surface erosion, Morphological changes, Molecular weight changes | Gravimetric analysis, SEM, SEC [1] |
| Chemical | Chemical composition changes, Functional group alteration, By-product formation | FTIR, NMR, Mass spectrometry, HPLC [1] [78] |
| Mechanical | Tensile strength, Elastic modulus, Compression properties | Mechanical testing, Dynamic mechanical analysis [1] [79] |
Q4: How can I validate that my degradation prediction model is accurately representing real-world biological scenarios?
Model validation should incorporate both computational and experimental approaches:
- Use statistical analysis including Friedman rank and Wilcoxon signed-rank tests to validate optimization performance [74]
- Conduct in vitro degradation studies in simulated body fluid (SBF) following ASTM guidelines [1] [79]
- Compare predicted degradation profiles with experimental data from techniques like electrochemical impedance spectroscopy (EIS) and potentiodynamic polarization (PDP) [79]
- Perform sensitivity analysis to identify which parameters most significantly impact degradation outcomes [72]
Q5: What are the most effective surface treatment methods to control degradation rates of magnesium alloys for orthopedic applications?
Surface treatments significantly influence degradation behavior through their effects on surface morphology and roughness [79]:
Table 2: Surface Treatments for Controlling Mg Alloy Degradation
| Treatment Type | Specific Methods | Impact on Degradation |
|---|---|---|
| Mechanical | Grinding, Polishing | Smoother surfaces generally reduce initial degradation rate and delay pitting [79] |
| Chemical | Acid treatment, Alkaline treatment | Can create more uniform surface morphology, decreasing localized corrosion [79] |
| Physical | Plasma treatment, Ion implantation | Modifies surface energy and chemistry, potentially improving degradation resistance [79] |
Advanced Troubleshooting Guides
Issue: Inconsistent Degradation Rates Between Simulation and Experimental Results
Potential Causes and Solutions:
- Inadequate Model Parameters: Ensure your DBO fitness function incorporates both accuracy and feature compactness. Use a fitness function that combines classification error with subset size:
Fitness = α × Error(x) + (1-α) × (|x|/D)where α balances accuracy versus feature reduction [73]. - Unaccounted Environmental Factors: Biological degradation is influenced by local pH fluctuations, enzymatic activity, and cellular responses. Incorporate these factors into your model using multi-objective optimization that considers both material properties and biological environment [1] [72].
- Material Variability: Account for batch-to-batch variations in material properties by implementing robust optimization approaches that consider uncertainty in input parameters [75].
Issue: Difficulty Handling High-Dimensional Data in Degradation Prediction
Solution Implementation:
- Implement Hybrid DBO Framework: Combine DBO with Support Vector Machines (SVM) for feature selection and classification. The DBO algorithm identifies informative gene subsets while SVM with RBF kernels provides robust decision boundaries in high-dimensional spaces [73].
- Apply Data Decomposition Techniques: Use Improved Complementary Ensemble Empirical Mode Decomposition (ICEEMDAN) to preprocess complex degradation signals before optimization [77].
- Utilize Binary DBO for Feature Selection: Adapt continuous DBO to binary feature selection by representing candidate solutions as binary vectors where 1 indicates selected features and 0 indicates unselected features [73].
Experimental Protocols for DBO Framework Validation
Protocol 1: Biomaterial Degradation Assessment for Model Training
Objective: To generate comprehensive degradation data for training and validating DBO predictive models [1].
Materials:
- Test biomaterial (e.g., Mg alloy, biodegradable polymer)
- Simulated body fluid (SBF) or appropriate degradation medium
- Analytical equipment: SEM, FTIR, HPLC, mechanical tester
Procedure:
- Pre-degradation Characterization:
- Measure initial weight, dimensions, and surface morphology
- Perform chemical characterization (FTIR, NMR)
- Conduct mechanical testing (tensile strength, modulus)
Immersion Study Setup:
- Immerse samples in SBF at pH 7.4, maintained at 37°C
- Use a sample-to-solution ratio of 1:20 cm²/mL [1]
Periodic Monitoring:
- At predetermined intervals (e.g., 1, 3, 7, 14, 28 days):
- Remove samples and gently rinse
- Measure weight change to 0.1% precision [1]
- Document surface morphology changes via SEM
- Analyze solution for degradation products (HPLC, UV-Vis)
- Perform mechanical testing on separate sample set
- At predetermined intervals (e.g., 1, 3, 7, 14, 28 days):
Data Compilation:
- Compile all degradation data into a structured database
- Calculate degradation rates and identify key degradation markers
Protocol 2: DBO Model Implementation for Degradation Prediction
Objective: To implement and validate a DBO framework for predicting biomaterial degradation behavior [73] [74].
Computational Environment:
- MATLAB or Python with necessary libraries
- Minimum 16GB RAM, multi-core processor
- Benchmark datasets for validation
Implementation Steps:
- Problem Formulation:
- Define decision variables (material properties, design parameters)
- Set constraints (degradation rate limits, mechanical requirements)
- Establish fitness function incorporating prediction accuracy and model complexity
DBO Algorithm Setup:
- Initialize population using Bernoulli map-based initialization for diversity [74]
- Set algorithm parameters: population size, maximum iterations
- Implement behavioral rules: foraging, rolling, breeding, stealing
Enhanced Strategies Integration:
- Incorporate Morlet Wavelet mutation for local optima escape [74]
- Implement elite guidance strategy to accelerate convergence
- Apply local escaping operator to refine search process
Model Validation:
- Use k-fold cross-validation to assess prediction accuracy
- Compare with experimental data using statistical tests (Wilcoxon signed-rank)
- Evaluate using multiple metrics: MAE, RMSE, R²
Essential Research Reagent Solutions
Table 3: Key Research Reagents for Degradation Studies
| Reagent/Category | Function in Degradation Studies | Specific Examples |
|---|---|---|
| Simulated Body Fluids | Replicate physiological conditions for in vitro degradation | SBF, phosphate-buffered saline (PBS), artificial lysosomal fluid [1] |
| Enzymatic Solutions | Model enzyme-mediated degradation processes | Collagenase, esterase, phosphatase solutions at physiological concentrations [1] |
| Analytical Standards | Qualification and quantification of degradation products | HPLC standards for common degradation by-products (lactic acid, glycolic acid, Mg²⁺ ions) [1] [78] |
| Staining and Labeling | Visualization of degradation effects | Alizarin Red for calcium deposition, DAPI for cell nuclei, LIVE/DEAD assays for cytotoxicity [79] |
| Optimization Algorithms | Computational prediction of degradation behavior | Dung Beetle Optimizer, Enhanced DBO variants (EBMLO-DBO) [73] [74] |
Workflow Visualization
DBO for Degradation Prediction Workflow
Degradation Assessment Methodology
Validation and Comparative Analysis: Ensuring Safety, Efficacy, and Biosimilarity
In biomedical applications, from tissue engineering to drug delivery, the controlled degradation of biomaterials is crucial. Standardized assessment techniques are essential to ensure that these materials perform as intended in the body, providing temporary support and then safely breaking down without causing adverse reactions. Adhering to established guidelines, such as those from ASTM International, ensures that degradation studies are reproducible, reliable, and scientifically sound, ultimately helping to resolve challenges in material degradation research [1] [80]. This technical support center provides troubleshooting guides and FAQs to address specific issues you might encounter during your experiments.
Fundamental Concepts and Terminology
Biodegradation is the biological catalytic reaction of reducing complex macromolecules into smaller, less complex molecular structures (by-products) [1]. The following key terms are frequently used in degradation studies:
- Foreign Body Response (FBR): The host's reaction to an implanted material, often involving inflammation and the formation of a fibrous capsule [80].
- Surface Erosion: Degradation that occurs primarily at the surface of a material.
- Bulk Erosion: Degradation that occurs uniformly throughout the entire volume of a material.
- Autocatalytic Degradation: An accelerated degradation process where acidic by-products of hydrolysis further catalyze the breakdown of the polymer, often leading to a faster-degrading interior in thick samples [81].
- Gravimetric Analysis: A fundamental technique for monitoring mass loss over time [1].
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: My in vitro degradation results do not match my in vivo observations. What could be the cause?
This is a common challenge in biomaterials research, often stemming from the oversimplification of in vitro conditions.
- Cause: Standard in vitro tests often use simulated body fluids (e.g., phosphate-buffered saline) at a constant pH (7.4) and temperature (37°C). However, the in vivo environment is far more complex, involving dynamic and localized changes in pH due to inflammatory responses, the presence of specific enzymes, and various immune cells that actively participate in the degradation process [1] [81].
- Solution:
- Supplement Media with Enzymes: For polymeric materials, incorporate relevant enzymes (e.g., esterases, lysozyme) into your degradation media to better simulate cellular and enzymatic activity [1].
- Use Cell-Culture Models: Move beyond simple buffer solutions to cell-culture models where immune cells, such as macrophages, are present. This allows you to assess the combined effect of physiological conditions and cellular activity on degradation [80].
- Monitor Local pH: The inflammatory response can create a localized acidic environment. Consider using pH sensors or indicators in your in vitro setup to understand these micro-environmental changes.
- Reference ASTM F1904: Consult ASTM F1904, which provides guidance for testing biological responses to particulate debris and degradation products in vivo, offering a framework for more clinically relevant study designs [80].
FAQ 2: I am observing a rapid loss in mechanical properties before significant mass loss. Is this normal?
Yes, this is a typical and often observed phenomenon, particularly in hydrolytically degrading polymers like poly(lactide-co-glycolide) (PLGA) and polylactic acid (PLA).
- Cause: The primary mechanism is often bulk erosion. Water penetrates the entire polymer matrix, leading to random hydrolytic scission of the polymer chains. This reduction in polymer molecular weight significantly weakens the material's mechanical integrity long before the chains are short enough to become soluble and cause measurable mass loss [1] [81].
- Solution:
- Monitor Molecular Weight: Do not rely solely on mass loss. Regularly use techniques like Size Exclusion Chromatography (SEC) or solution viscometry throughout your degradation study to track the reduction in molecular weight (Mw and Mn) [1].
- Correlate Properties: Create a timeline that correlates molecular weight, mechanical properties (e.g., tensile strength, modulus), and mass loss. This will provide a comprehensive picture of the degradation profile.
- Consider Material Form: Be aware that in amorphous polymers, autocatalytic effects can cause the interior to degrade faster than the surface, potentially leading to hollow structures while the external form appears intact, which can mislead interpretations based on visual inspection alone [81].
FAQ 3: How can I distinguish between material dissolution and true degradation?
This is a critical distinction, as weight loss in a buffer could simply be due to solubility rather than the breakdown of polymer chains.
- Cause: Mistaking the simple dissolution of a water-soluble polymer or oligomer for a degradation-driven process [1].
- Solution:
- Chemical Confirmation: Employ analytical techniques that confirm changes in chemical structure.
- Fourier Transform Infrared Spectroscopy (FTIR) can identify the disappearance of specific functional groups (e.g., ester bonds) or the appearance of new ones (e.g., carboxylic acids) [1].
- Nuclear Magnetic Resonance (NMR) is powerful for identifying and quantifying the by-products of degradation in solution, confirming that chain scission has occurred [1] [82].
- Analyze the Medium: Use techniques like Ultraviolet-Visible spectrophotometry (UV-Vis) or High-Performance Liquid Chromatography (HPLC) to detect and quantify soluble degradation by-products in the surrounding fluid, rather than just measuring the mass loss of the implant [1].
- Chemical Confirmation: Employ analytical techniques that confirm changes in chemical structure.
FAQ 4: My sample shows a "hollowing out" phenomenon during degradation. Why does this occur?
This observation, where the interior of a sample degrades faster than the surface, is characteristic of certain biodegradable polymers.
- Cause: Autocatalytic degradation. In thick samples of polymers like PLA or PLGA, as the ester bonds hydrolyze, they generate carboxylic acid end groups. These acidic by-products are trapped within the polymer matrix, lowering the local pH and autocatalyzing further, faster hydrolysis in the center. Meanwhile, at the surface, the acidic oligomers can diffuse out into the surrounding medium, resulting in a less acidic environment and a slower degradation rate on the outside [81].
- Solution:
- Cross-section Analysis: Periodically section your samples during the degradation study and use Scanning Electron Microscopy (SEM) to visualize the internal morphology changes.
- Monitor Molecular Weight Distribution: Use SEC to analyze different sections (surface vs. center) of the degrading material. You will likely find a bimodal molecular weight distribution, with lower molecular weights in the center, confirming the autocatalytic effect [81].
- Design Adjustments: For applications where this is undesirable, consider designing thinner scaffolds or using materials with different degradation kinetics to promote more uniform erosion.
Standardized Experimental Protocols
Protocol 1: In Vitro Degradation Study for Solid Polymer Scaffolds (based on ASTM guidelines)
This protocol outlines a standardized method for tracking the degradation of solid, insoluble polymeric biomaterials.
1. Pre-degradation Characterization:
- Mass and Dimensions: Record initial mass (to 0.1 mg precision) and key dimensions [1].
- Molecular Weight: Determine the initial molecular weight and distribution via SEC.
- Surface Morphology: Image the surface using SEM.
- Mechanical Properties: Perform baseline tensile or compression tests.
2. Degradation Setup:
- Immersion: Immerse samples in a degradation medium (e.g., PBS, simulated body fluid) at pH 7.4 and 37°C. Use a sufficient volume of medium to ensure sink conditions (recommended ratio: 1:100 sample mass to medium volume) [1].
- Sterilization: Sterilize samples and media if the study involves cells.
- Replication: Use a minimum of n=5 samples per time point for statistical significance.
3. Sampling and Analysis:
- Time Points: Collect samples at predetermined intervals (e.g., 1, 3, 7, 14, 28 days, etc.).
- At Each Time Point: a. Rinse & Dry: Rinse retrieved samples with deionized water and dry to a constant weight. b. Gravimetric Analysis: Weigh samples to calculate mass loss % [1]. c. pH Monitoring: Record the pH of the degradation medium. d. Molecular Weight Analysis: Use SEC to determine the remaining molecular weight. e. Morphological Analysis: Use SEM to examine surface and cross-sectional erosion. f. Mechanical Testing: Perform mechanical tests on wet or rehydrated samples.
The workflow for this protocol is summarized in the following diagram:
Protocol 2: Assessing Biological Response to Degradation Products (based on ASTM F1904)
This protocol focuses on evaluating the host's biological response to particles and soluble ions released during degradation.
1. Generate Debris: Create particulate debris from your biomaterial using methods like milling and sieving to isolate a relevant size fraction (e.g., 1-10 µm).
2. In Vivo Implantation:
- Animal Model: Select an appropriate model (e.g., rodent for subcutaneous implantation, larger animal for orthopedic models) [80].
- Administration: Implant particles intramuscularly, subcutaneously, or in a site-specific manner (e.g., intra-articular for orthopedic materials).
- Controls: Include positive and negative control materials.
3. Endpoint Analysis:
- Histopathology: Excise the implant site and surrounding tissue. Process for sectioning and stain with Hematoxylin and Eosin (H&E). Look for key indicators [80]:
- Immune Cell Infiltration: Neutrophils, lymphocytes, macrophages.
- Foreign Body Giant Cells (FBGCs): Presence and number.
- Fibrosis: Thickness of the fibrous capsule.
- Necrosis: Tissue death.
- Immunohistochemistry (IHC): Use specific antibodies to identify and quantify different cell types (e.g., M1 vs. M2 macrophages using CD86/CD206 markers) [80].
- Cytokine Analysis: Isolate tissue or serum and use ELISA or PCR to measure levels of pro-inflammatory (e.g., TNF-α, IL-1β, IL-6) and anti-inflammatory cytokines (e.g., IL-10, TGF-β) [80].
The workflow for assessing biological response is as follows:
Essential Research Reagents and Materials
The table below lists key reagents and materials used in standardized degradation assessments, along with their primary functions.
| Reagent / Material | Function in Degradation Studies | Key Considerations |
|---|---|---|
| Phosphate Buffered Saline (PBS) | A standard simulated body fluid for hydrolytic degradation studies. | Lacks enzymes and cells; maintains isotonicity and pH. |
| Tris-HCl Buffer | A common buffer for maintaining pH in enzymatic degradation studies. | Preferred over PBS for some enzymes that are inhibited by phosphate. |
| Lysozyme | An enzyme that degrades certain polymers (e.g., polyesters) by hydrolyzing ester bonds. | Used to simulate enzymatic degradation; concentration should be physiologically relevant. |
| Lipase | An enzyme that catalyzes the hydrolysis of fats and some polyesters. | Relevant for simulating degradation in specific biological environments. |
| Hematoxylin and Eosin (H&E) | Histological stains for visualizing tissue structure and cellular response. | H&E stains nuclei blue and cytoplasm pink, allowing assessment of inflammation and fibrosis. |
| Antibodies for IHC (e.g., CD68, CD206) | Antibodies used to identify specific cell types (e.g., macrophages) in tissue sections. | Critical for immunophenotyping and understanding the innate immune response. |
| ELISA Kits (e.g., for TNF-α, IL-6) | Kits for quantifying specific cytokine proteins in tissue homogenates or serum. | Provides a quantitative measure of the inflammatory response to degradation products. |
Data Presentation and Analysis
Key Material Properties and Target Values for Orthopedic Implants
For researchers developing biodegradable materials, particularly for load-bearing applications, aiming for the following property ranges is recommended [49].
| Property | Ideal Range for Biodegradable Orthopedic Implants | Rationale |
|---|---|---|
| Degradation Rate | < 0.5 mm/year | Ensures mechanical integrity is maintained during the healing process (typically 6-24 months). |
| Yield Strength | 250 - 800 MPa | Withstands physiological loads without permanent deformation. |
| Ultimate Tensile Strength | 300 - 1000 MPa | Ensures device integrity under extreme loading conditions. |
| Elongation at Break | 10% - 20% | Provides necessary ductility to avoid brittle fracture. |
| Young's Modulus | 40 - 60 GPa (Mg-based); 78 - 121 GPa (Zn-based) | Should match natural bone (~30 GPa) as closely as possible to avoid stress shielding. |
| Hydrogen Evolution Rate | < 10 µL/cm²/day | Minimizes the risk of gas cavity formation and tissue irritation. |
Successfully navigating the complexities of biomaterial degradation requires a rigorous, multi-faceted approach grounded in standardized techniques. By adhering to ASTM and international guidelines, employing a combination of physical, chemical, and biological assessments, and utilizing the troubleshooting strategies outlined in this guide, researchers can generate robust and predictive data. This systematic approach is fundamental to developing safer and more effective biodegradable medical devices that truly resolve the challenges of material degradation in biomedical applications.
Troubleshooting Guides
Guide 1: Addressing Discrepancies Between In Vitro and In Vivo Degradation Data
Problem: The degradation profile observed in laboratory tests does not match the performance seen in clinical or preclinical studies.
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Overly simplistic in vitro model | Review degradation media (pH, enzymes) against physiological conditions of target tissue [1]. | Refine in vitro model to mimic target anatomical site (e.g., specific pH, relevant enzyme cocktails) [1]. |
| Misinterpreting weight loss as degradation | Perform chemical analysis (e.g., SEC, NMR) to confirm molecular weight changes and breakdown products [1]. | Replace gravimetric analysis with techniques like Size Exclusion Chromatography (SEC) to confirm chemical degradation [1]. |
| Ignoring the "Hook Effect" (TPD) | Conduct dose-response experiments to identify concentration where degradation efficiency drops [83]. | Optimize degrader concentration and use AI-guided models for linker design to minimize unproductive binding [83]. |
Guide 2: Overcoming Challenges in Biomaterial Biocompatibility Assessment
Problem: A biomaterial shows acceptable physical degradation but triggers an adverse biological response in vivo.
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Toxic degradation by-products | Use HPLC or MS to identify and quantify by-products from in vitro degradation [1]. | Assess cytotoxicity of isolated by-products and re-formulate biomaterial to eliminate toxic moieties [1]. |
| Evaluation of final device form | Review if testing was performed on raw material instead of final, sterilized device [84]. | Perform biocompatibility testing on the device in its final finished form, as per FDA guidance [84]. |
| Inadequate testing duration | Compare the device's contact duration with the length of the biocompatibility study [84]. | Ensure test duration matches or exceeds the intended cumulative contact time of the device with the body [84]. |
Frequently Asked Questions (FAQs)
Q1: What are the key properties to monitor when assessing the degradation of a solid polymeric biomaterial? A comprehensive assessment should monitor properties across chemical, physical, and mechanical domains [1].
- Chemical: Molecular weight changes via Size Exclusion Chromatography (SEC) or solution viscosity; identification of degradation by-products via techniques like Mass Spectrometry or NMR [1].
- Physical: Mass loss (gravimetric analysis) and surface morphology changes via Scanning Electron Microscopy (SEM) [1].
- Mechanical: Changes in tensile strength, modulus, or elasticity relevant to the application (e.g., a suture or scaffold) [1].
Q2: How can I establish a predictive in vitro-in vivo relationship (IVIVR) for a vaginally administered drug product? A verified IVIVR can be developed using Physiologically Based Pharmacokinetic (PBPK) modeling, such as the Mechanistic Vaginal Absorption & Metabolism (MechVAM) model in the Simcyp Simulator. This involves:
- Measuring in vitro release profiles.
- Using the PBPK model to simulate in vivo plasma concentrations based on the in vitro data.
- Validating the model by comparing simulated results with actual clinical bioequivalence (BE) trial data [85] [86]. Once validated, this IVIVR can support the establishment of a "dissolution safe space" (e.g., -7.36% to +9.40% mg/day release) for post-approval changes, potentially reducing the need for further human testing [85].
Q3: What does the FDA require for the biocompatibility evaluation of a medical device? According to FDA guidance, biocompatibility is evaluated on the whole device in its final finished form, including the effects of sterilization. The assessment is based on:
- Nature and duration of body contact: Which tissues the device contacts and for how long (e.g., transient, prolonged, or permanent) [84].
- Material characterization: Understanding the chemistry of all component materials and any interactions between them [84]. The evaluation follows a risk-based approach, often leveraging the ISO 10993-1 standard within a risk management framework [84].
Q4: In Targeted Protein Degradation (TPD), what is the "Hook Effect" and how can it be managed? The "Hook Effect" is a phenomenon where, at high concentrations, a PROTAC degrader forms unproductive binary complexes (with either the target protein or the E3 ligase alone) instead of the productive ternary complex needed for degradation. This leads to a drop in degradation efficiency [83].
- Management: The effect can be modeled and managed using advanced simulations to guide linker design and optimize dosing strategies that maintain potency while minimizing the Hook Effect [83].
Q5: My biomaterial is a hydrogel. How do I assess its degradation if I can't use gravimetric analysis? For soluble or hydrogel-based formulations, gravimetric analysis is not suitable, as mass loss cannot be distinguished from dissolution or swelling. Instead, focus on:
- Chemical Techniques: Use SEC to track changes in molecular weight over time. Employ NMR or FTIR to identify chemical bond cleavage [1].
- Physical Techniques: Monitor changes in storage (G') and loss (G") moduli via rheology to quantify the loss of mechanical integrity [1].
- Analytical Techniques: Quantify the release of specific, known degradation by-products using HPLC or UV-Vis spectrophotometry [1].
Quantitative Data Tables
This table defines the acceptable limits for in vitro release rates that ensure in vivo bioequivalence, supporting post-approval changes without new clinical trials.
| Time Point | Lower Safe Space Limit | Upper Safe Space Limit |
|---|---|---|
| Day 1 | -7.36% | +9.40% |
| Day 2 | -7.36% | +9.40% |
| Day 7 | -7.36% | +9.40% |
This table helps select the most appropriate techniques for confirming and quantifying degradation.
| Technique | Measures | Key Advantage | Key Limitation |
|---|---|---|---|
| Gravimetric Analysis | Mass loss | Simple, cost-effective | Cannot distinguish dissolution from degradation |
| Size Exclusion Chromatography (SEC) | Molecular weight change | Confirms chemical degradation | Higher cost, complex data analysis |
| Scanning Electron Microscopy (SEM) | Surface morphology, erosion | Visualizes physical changes | Infers but does not confirm degradation |
| NMR / Mass Spectrometry | Chemical structure of by-products | Identifies and confirms degradation products | Expensive, requires specialized expertise |
| Mechanical Testing | Tensile strength, modulus | Directly relates to functional performance | Does not identify root cause of breakdown |
Experimental Protocols
Protocol 1: Standardized In Vitro Degradation Study for Solid Biomaterials
This protocol is adapted from ASTM F1635-11 guidelines and critical reviews of best practices [1].
Objective: To quantitatively and qualitatively assess the degradation of a solid biomaterial in simulated physiological conditions.
Materials & Reagents:
- Phosphate Buffered Saline (PBS), pH 7.4, or simulated body fluid relevant to the implantation site.
- Incubator maintained at 37°C.
- Analytical balance (precision of 0.1% of sample weight).
- Equipment for characterization (e.g., SEC, SEM, NMR, mechanical tester).
Procedure:
- Pre-degradation Characterization: Record the initial mass, dimensions, and molecular weight of samples. Image surface morphology via SEM and perform baseline mechanical testing.
- Immersion: Immerse pre-weighed samples (in triplicate) in degradation medium at a defined volume-to-surface-area ratio. Maintain at 37°C.
- Sampling & Media Refreshment: At predetermined time points, remove samples from the medium. Replace with fresh medium to maintain sink conditions.
- Post-degradation Processing:
- Rinse samples gently with deionized water.
- Dry samples to a constant weight.
- Weigh samples to calculate mass loss.
- Analysis: At each time point, perform:
- Gravimetric Analysis: Calculate percentage mass loss.
- Chemical Analysis: Use SEC to determine molecular weight changes.
- Physical Analysis: Image samples via SEM to observe surface erosion.
- Mechanical Analysis: Test mechanical properties if functionally critical.
- By-product Identification: Analyze the degradation media using HPLC or LC-MS to identify and quantify released fragments.
Protocol 2: Confirming Ternary Complex Formation for PROTAC Degraders
Objective: To validate the formation and kinetics of the ternary complex (Target-PROTAC-E3 Ligase), a critical step for PROTAC activity.
Materials & Reagents:
- Purified target protein and E3 ligase.
- The PROTAC molecule of interest.
- TR-FRET or SPR-MS assay kits.
- Microplate reader or surface plasmon resonance instrument.
Procedure:
- Assay Setup: In a buffer suitable for both proteins, mix the target protein and E3 ligase with a titration of the PROTAC molecule.
- Incubation: Allow the ternary complex to form for a defined period.
- Detection:
- For TR-FRET: Use labeled antibodies against the target and E3 ligase. Measure the time-resolved fluorescence energy transfer signal, which indicates proximity and complex formation.
- For SPR-MS: Immobilize one protein (e.g., the E3 ligase) on the sensor chip. Flow the PROTAC and target protein over the chip. The change in resonance units indicates binding. The complex can then be extracted for mass spectrometry to confirm identity.
- Data Analysis:
- Determine binding affinity (KD) and cooperativity.
- Analyze the residence time of the complex, as a longer-lived complex is often more productive for degradation [83].
Pathway and Workflow Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Essential Materials for Degradation Profiling
| Reagent / Material | Function in Experiment |
|---|---|
| Simulated Body Fluids (SBF) | Provides a biologically relevant ionic environment for in vitro degradation studies, mimicking blood plasma or specific tissue environments [1]. |
| PROTAC Molecule | A bifunctional degrader consisting of a target protein ligand, an E3 ligase ligand, and a linker; used to harness the ubiquitin-proteasome system for targeted protein degradation [87] [83]. |
| E3 Ligase Ligands (e.g., for Cereblon, VHL) | Critical component of PROTACs; recruits the cell's endogenous ubiquitin machinery to mark the target protein for degradation [88] [83]. |
| Clickable PROTACs & Bioorthogonal Probes | Chemical tools used to track PROTAC engagement, intracellular localization, and proteome-wide target profiling in live cells [83]. |
| Size Exclusion Chromatography (SEC) Standards | Calibration molecules of known molecular weight used to quantify changes in the molecular weight of a polymer during degradation [1]. |
| AI-Guided Design Platforms (e.g., DeepTernary, DegradeMaster) | Computational tools that simulate ternary complex formation and optimize PROTAC/linker design to improve efficacy and reduce off-target effects [83]. |
Forced degradation studies, also known as stress testing, are an intentional process of degrading drug substances and products under conditions more severe than accelerated storage to understand their intrinsic stability [89] [90]. These studies are a critical component of pharmaceutical development, required to demonstrate the specificity of stability-indicating methods, provide insight into degradation pathways, and identify degradation products [89] [91]. The knowledge gained informs formulation development, packaging, and storage conditions, ultimately ensuring drug safety and efficacy for patients [90].
Frequently Asked Questions (FAQs)
1. Why are forced degradation studies necessary for biosimilar development? In biosimilar development, forced degradation studies are used to assess the similarity of degradation pathways between the biosimilar and the originator reference product [92]. This comparative analytical assessment is a key part of the quality consideration to demonstrate biosimilarity, as mentioned in FDA and EMA guidelines [92].
2. When during drug development should forced degradation be performed? While regulatory guidance suggests stress testing should be performed in Phase III for submission, starting these studies early in preclinical phases or Phase I is highly encouraged [89]. Early studies provide timely information for improving the manufacturing process and selecting stability-indicating analytical procedures, though they may need to be repeated if the process or formulation changes significantly [89] [91].
3. What is an acceptable level of degradation to target? Degradation of the drug substance between 5% and 20% is generally accepted as reasonable for validating chromatographic assays, with some scientists considering 10% degradation as optimal [89] [91]. The goal is to generate sufficient degradation products without causing over-stressing, which can lead to secondary degradants not seen in real-world stability studies [89].
4. What materials should be used for forced degradation studies? A single batch of material should be used, which can be a non-GMP batch, a test batch, or even an out-of-specification batch, provided the choice is justified [91]. For drug products, both high- and low-dose levels can be included. It is also recommended to include solution/bluffer blanks, excipient controls, and reference samples in each experiment [91].
Troubleshooting Guide for Common Experimental Issues
Problem: No degradation observed after stress exposure.
- Potential Cause & Solution: The stress conditions may be too mild. Consider increasing the exposure time rather than immediately making conditions more extreme (e.g., longer heating duration instead of a much higher temperature) [91]. The study can be terminated if no degradation is seen after exposure to conditions harsher than accelerated stability protocols, as this itself indicates molecule stability [89].
Problem: Excessive degradation leading to secondary degradants.
- Potential Cause & Solution: The sample is over-stressed. To distinguish primary from secondary degradation products, test at multiple early time points (e.g., 2, 5, 8, 24 hours) to evaluate the degradation rate [89]. Aim for the 5-20% degradation range and use shorter exposure times or milder conditions.
Problem: Analytical column degradation during HPLC analysis of stressed samples.
- Potential Cause & Solution: Stressed samples may contain high concentrations of reactants like acid, base, or oxidants. There is a practical need to neutralize or dilute every sample before injection to protect the HPLC column [89]. Ensure your sample preparation protocol includes a quenching or dilution step.
Problem: New degradation products appear after a process or formulation change.
- Potential Cause & Solution: This is an expected occurrence. Forced degradation studies should be repeated when formulations or analytical methods change because these changes can lead to the production of new degradation products [89].
Experimental Design and Protocols
The following workflow outlines the strategic process for conducting a forced degradation study, from sample preparation to data interpretation.
Core Stress Conditions and Methodologies
The table below summarizes the common stress conditions used in forced degradation studies. Conditions should be carefully selected on a case-by-case basis [91].
Table 1: Typical Forced Degradation Conditions and Protocols [89] [91] [90]
| Stress Condition | Typical Experimental Parameters | Primary Degradation Pathways Induced |
|---|---|---|
| Acid Hydrolysis | 0.1 M HCl, at 40-60°C, for 1-5 days [89] [90]. | Hydrolysis (fragmentation), deamidation [91]. |
| Base Hydrolysis | 0.1 M NaOH, at 40-60°C, for 1-5 days [89] [90]. | Hydrolysis (fragmentation), deamidation [91]. |
| Oxidation | 3% H₂O₂, at 25-60°C, for 1-5 days or less [89]. | Oxidation of methionine, cysteine, histidine, tryptophan, or tyrosine [91]. |
| Thermal | Solid or solution state at 60-80°C, with or without 75% relative humidity, for 1-5 days [89]. | Aggregation, hydrolysis, deamidation [91]. |
| Photolysis | Exposure to UV (320-400 nm) and visible light per ICH Q1B guidelines, for 1-5 days [89]. | Oxidation, aggregation, peptide bond cleavage via free radicals [91]. |
Analytical Techniques for Assessing Degradation
Due to the complexity of biopharmaceuticals, no single method can profile all stability characteristics. A combination of techniques is required to assess different aspects of degradation [91]. The following diagram illustrates how data from various analytical methods is integrated to characterize forced degradation samples.
Table 2: Key Analytical Methods for Forced Degradation Studies [91] [92]
| Analytical Method | Function in Forced Degradation |
|---|---|
| Size-Exclusion HPLC (SE-HPLC) | Quantifies soluble aggregates (high molecular weight proteins) and fragments (low molecular weight proteins) [91]. |
| Reversed-Phase HPLC (RP-HPLC) | Assesses purity and identifies specific impurities, including some oxidized and deamidated forms [91]. |
| Ion-Exchange HPLC (IEX-HPLC) / icIEF | Separates and analyzes charge variants, such as deamidated species, which result in a change in the protein's isoelectric point (pI) [91]. |
| Peptide Mapping with Mass Spectrometry | Identifies the precise location and nature of chemical modifications (e.g., oxidation of a specific Tryptophan residue) [92]. |
| Biological Activity Assay | Determines if the stress conditions and resulting degradation products have impacted the drug's potency and efficacy [91]. |
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Forced Degradation Studies
| Reagent / Material | Function in Experiments |
|---|---|
| Hydrochloric Acid (HCl) / Sodium Hydroxide (NaOH) | Used to prepare solutions for acid and base hydrolysis studies to simulate pH stress [89] [90]. |
| Hydrogen Peroxide (H₂O₂) | A common oxidizing agent used to induce oxidative stress and generate oxidated degradants [89]. |
| Controlled Temperature/ Humidity Chambers | Provides precise thermal and humidity stress conditions (e.g., 60°C/75% RH) for solid and solution state studies [89]. |
| ICH Q1B Compliant Light Cabinets | Provides controlled ultraviolet (UV) and visible light exposure for photostability testing [89]. |
| Chaotropic Agents (e.g., GnHCl, Urea) | Used to induce denaturation and study disulfide bridge scrambling or incorrect pairing [91]. |
Frequently Asked Questions (FAQs)
Q1: Why are forced degradation studies critical for biosimilarity assessment? Forced degradation studies are essential because they help identify potential degradation pathways and compare the stability profiles of a biosimilar and its originator product. By subjecting both products to controlled stress conditions (e.g., thermal, oxidative, pH), scientists can determine if the biosimilar degrades in a similar manner to the reference product. This provides a higher level of assurance that the products are comparable in quality, safety, and efficacy, even under challenging conditions, and helps identify critical quality attributes (CQAs) that must be monitored [93] [94].
Q2: What is the primary role of each technique in a comprehensive biosimilarity assessment? In a comprehensive assessment, these techniques serve complementary and orthogonal roles:
- CE-SDS is primarily used to monitor size-based variants, specifically to quantify purity and impurity profiles such as fragments (low-molecular-weight species, LMW) and aggregates (high-molecular-weight species, HMW) under both reducing and non-reducing conditions [93] [95].
- icIEF is the gold standard for analyzing charge heterogeneity. It separates and quantifies charge variants (acidic and basic species) that arise from post-translational modifications (PTMs) like deamidation, C-terminal lysine processing, and sialylation [95] [96].
- SE-UPLC is used to separate and quantify soluble aggregates (HMW) and fragments (LMW) from the native monomeric antibody under native conditions, providing critical data on aggregation, a key stability parameter [93] [94].
Q3: How can I confirm that a observed change in a charge variant profile is due to a specific modification like deamidation? While icIEF can precisely quantify the shift in charge variants, it often requires an orthogonal technique for confirmation. Peptide mapping with liquid chromatography–tandem mass spectrometry (LC-MS/MS) is typically used. This method can pinpoint the exact location of modifications, such as identifying the specific asparagine residue in a peptide that has undergone deamidation, thereby confirming the cause of the acidic shift seen in the icIEF profile [93] [97].
Q4: Our biosimilar shows a comparable profile to the originator in most tests but has a slightly different response to carboxypeptidase B (CpB) treatment in icIEF. What does this imply? A different response to CpB treatment, which specifically removes C-terminal lysine residues, indicates a difference in the distribution of these variants between the biosimilar and the originator. This typically points to subtle differences in the manufacturing process, particularly in the enzymatic processing steps during production. While it may not directly impact efficacy, it is a quality attribute that must be well-understood, justified, and controlled to ensure consistent product quality [95].
Troubleshooting Guides
SE-UPLC Troubleshooting
This guide addresses common issues encountered when using Size-Exclusion Ultra-Performance Liquid Chromatography (SE-UPLC) to monitor aggregation and fragmentation.
| Issue | Potential Causes | Recommended Solutions |
|---|---|---|
| Increased Aggregation | • Thermal stress during storage or handling.• Agitation stress from shipping or mixing.• Exposure to acidic pH conditions. | • Ensure consistent cold-chain management.• Optimize formulation to improve stability.• Avoid vigorous shaking; use gentle inversion. |
| Pressure Fluctuations | • Blockage in the inlet filter or column frit.• Air bubbles in the system.• Leaks in tubing or fittings. | • Replace the column or inlet filter [98].• Prime the pump thoroughly to remove bubbles.• Check and tighten all connections. |
| Poor Peak Shape/Resolution | • Column degradation or voiding.• Inappropriate mobile phase (pH, ionic strength).• Sample overloading. | • Replace with a new SE-UPLC column [98] [99].• Ensure mobile phase is fresh and composition is correct.• Reduce sample concentration or injection volume. |
| Baseline Noise or Drift | • Contaminated flow cell.• Mobile phase degradation or contamination.• Detector lamp failure. | • Clean or replace the flow cell.• Prepare fresh, high-quality mobile phase and degas.• Check and replace the UV lamp if necessary [98]. |
icIEF Troubleshooting
This guide addresses common problems with imaged capillary isoelectric focusing (icIEF) used for charge variant analysis.
| Issue | Potential Causes | Recommended Solutions |
|---|---|---|
| Poor Resolution | • Inadequate focusing time.• Suboptimal ampholyte composition.• Incorrect sample preparation. | • Optimize focusing time and voltage (e.g., 1 min at 1500 V, then 8 min at 3000 V) [95].• Adjust the ratio of Pharmalytes (e.g., 3% 8-10.5 and 1% 5-8) [95].• Ensure samples are properly diluted in the ampholyte mix containing urea and additives. |
| Loss of pI Markers | • Excessive focusing time.• Incorrect concentration of cathodic/anodic blockers. | • Ensure the method parameters (focus time, arginine concentration) are within a robust window to retain markers [95]. |
| Irreproducible Peak Patterns | • Inconsistent CpB digestion (if used).• Variable sample incubation conditions. | • Standardize the CpB digestion protocol (e.g., 1:100 enzyme-to-sample ratio, 37°C for 20 min) [95].• Control sample treatment time and temperature precisely. |
| High Background Noise | • Contaminated capillary.• Degraded reagents or old ampholyte mix. | • Rinse capillary thoroughly with appropriate solvents.• Prepare fresh ampholyte and reagent solutions. |
CE-SDS Troubleshooting
This guide addresses issues in Capillary Electrophoresis-Sodium Dodecyl Sulfate (CE-SDS) analysis for purity and fragmentation assessment.
| Issue | Potential Causes | Recommended Solutions |
|---|---|---|
| No Peaks or Low Signal | • Sample not properly injected.• Incorrect sample preparation (denaturation).• Blocked capillary. | • Check autosampler and injection settings [98].• Verify denaturation protocol (e.g., 10 min at 70°C with IAM or BME) [95].• Replace or flush the capillary. |
| Broad or Tailing Peaks | • Capillary fouling or adsorption.• Incompletely denatured sample.• Dead volume in the system. | • Use a rigorous capillary cleaning regimen.• Ensure sufficient denaturation time and temperature.• Check for and eliminate any bad connections [99]. |
| Non-reproducible % Purity | • Inconsistent sample reduction/alkylation.• Fluctuating separation voltage or temperature. | • Precisely control the concentration of IAM (non-reduced) or BME (reduced) and incubation time [93].• Ensure the system performance is qualified and separation parameters are stable. |
| Unexpected Peaks | • Protein degradation (fragmentation/aggregation).• Chemical modifications from stress (e.g., oxidation).• Interference from sample matrix. | • Compare with a fresh, unstressed control sample.• Use orthogonal methods (e.g., LC-MS) to identify the modifications [93] [97].• Dialyze or buffer-exchange the sample into a compatible buffer. |
Experimental Protocols for Key Experiments
Protocol: Forced Thermal Degradation Study
Objective: To compare the degradation profiles of a biosimilar and an originator monoclonal antibody under thermal stress [93] [94].
Materials:
- Biosimilar and originator mAbs (at 10 mg/mL)
- Thermostatic incubators (set at 37°C and 50°C)
- CE-SDS system (e.g., Maurice)
- SE-UPLC system
- LC-MS/MS system (for detailed characterization)
Methodology:
- Sample Preparation: Aliquot the biosimilar and originator mAb solutions into separate vials.
- Stress Application: Incubate the aliquots at 37°C and 50°C. Remove samples for analysis at predefined time points (e.g., 0, 3, 7, and 14 days) [93].
- Analysis:
- CE-SDS Analysis: Dilute stressed samples to 1.0 mg/mL. For non-reduced CE-SDS, treat with 11.5 mM IAM; for reduced CE-SDS, treat with 650 mM BME. Denature at 70°C for 10 minutes. Inject and separate according to the system's protocol (e.g., 20 sec at 4600 V, then 25-35 min at 5750 V) [95]. Quantify the percentages of intact mAb, LMW fragments, and HMW aggregates.
- SE-UPLC Analysis: Inject the stressed samples onto the SE-UPLC system. Use an appropriate mobile phase (e.g., phosphate buffer) to separate and quantify monomeric, aggregated, and fragmented species.
- LC-MS/MS Analysis (Optional): Perform peptide mapping on samples stressed for 14 days to identify specific degradation products, such as asparagine deamidation or aspartate isomerization [93].
Expected Outcomes:
- A time- and temperature-dependent increase in LMW fragments and HMW aggregates in both products.
- Highly comparable degradation profiles between the biosimilar and originator, demonstrating biosimilarity.
- Identification of specific degradation "hotspots" (e.g., deamidation in the PENNY peptide) via LC-MS/MS [93].
Protocol: Charge Heterogeneity Analysis with icIEF
Objective: To compare the charge variant profiles of a biosimilar and an originator mAb, including the impact of C-terminal lysine [95] [96].
Materials:
- Maurice system or equivalent icIEF instrument
- cIEF Cartridges
- Pharmalytes (ranges 5-8 and 8-10.5)
- pI markers (e.g., 5.85 and 10.17)
- Carboxypeptidase B (CpB)
- Urea, IDA, Arginine
Methodology:
- Ampholyte Mix Preparation: Prepare the ampholyte mix as specified in Table 1. The mix should contain 4% Pharmalytes, 3.2 M urea, 5 mM IDA, 10 mM arginine, and pI markers [95].
- CpB Digestion (for lysine variant analysis): Reconstitute CpB to 1 mg/mL. Add it to the sample (1:100 ratio) and incubate at 37°C for 20 minutes. Keep the digested sample on ice [95].
- Sample Preparation: Dilute treated and untreated samples to a final concentration of 0.2 mg/mL in the ampholyte mix.
- icIEF Run: Load the samples and run with a method such as 1 minute at 1500 V followed by 8 minutes at 3000 V [95].
- Data Analysis: Integrate the peaks in the electropherogram to quantify the percentage of acidic, main, and basic peaks for both the biosimilar and originator, with and without CpB treatment.
Expected Outcomes:
- Highly similar charge variant profiles between the biosimilar and originator in the untreated samples.
- A reduction in basic peaks after CpB treatment, indicating the presence of C-terminal lysine variants. The magnitude of this shift should be comparable between the two products to demonstrate similarity in this attribute [95].
Workflow Visualization
Biosimilarity Assessment Workflow
Technique Interrelationship for Degradation Assessment
The Scientist's Toolkit: Key Research Reagent Solutions
The following table lists essential reagents and materials required for the experiments described in this guide.
| Reagent/Material | Function in Biosimilarity Assessment | Example/Reference |
|---|---|---|
| IdeS Enzyme | Enzymatically digests mAbs into Fc/2 and F(ab')2 fragments for middle-up LC-MS analysis, enabling localization of modifications. | Used in forced oxidation studies to identify oxidized subunits [97]. |
| Carboxypeptidase B (CpB) | Removes C-terminal lysine residues from mAbs. Used in icIEF to identify and quantify lysine variants, a key charge heterogeneity attribute. | Protocol: 1:100 CpB to sample, incubate at 37°C for 20 min [95]. |
| Iodoacetamide (IAM) | Alkylating agent used in non-reduced CE-SDS sample preparation to cap cysteine residues and prevent disulfide bond reformation. | Used at 11.5 mM concentration in CE-SDS sample buffer [95]. |
| 2-Mercaptoethanol (BME) | Reducing agent used in reduced CE-SDS to break disulfide bonds, separating mAbs into light and heavy chains for purity analysis. | Used at 650 mM concentration in CE-SDS sample buffer [95]. |
| Pharmalytes | Carrier ampholytes used in icIEF to generate a stable pH gradient within the capillary for high-resolution separation of charge variants. | Common mix: 3% Pharmalyte 8-10.5 and 1% Pharmalyte 5-8 [95]. |
| Hydrogen Peroxide (H₂O₂) | Oxidizing agent used in forced oxidation studies to probe the susceptibility of mAbs to methionine and tryptophan oxidation. | Applied to study oxidation in bevacizumab and infliximab [97]. |
| pI Markers | Internal standards with known isoelectric points (pI) used in icIEF to calibrate the pH gradient and ensure accurate pI assignment of protein peaks. | Common markers include pI 5.85 and pI 10.17 [95]. |
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: What are the most critical properties to monitor when benchmarking a novel biodegradable material for implant applications? When benchmarking a novel biodegradable material, you should focus on an interconnected set of physical, chemical, and mechanical properties. Key among these are mass loss (gravimetric analysis), changes in molar mass, and mechanical properties such as tensile strength and elasticity [1]. It is critical to complement these with chemical analysis to confirm degradation, as physical changes alone can be mistaken for simple dissolution. The degradation time should match the healing or regeneration process, and the by-products must be non-toxic and readily cleared from the body [1].
Q2: My in vitro degradation results do not match in vivo performance. What could be the cause? This is a common challenge. In vitro tests often use simplified simulated body fluids, which may not replicate the complex biochemical environment of living tissue, including specific enzyme concentrations, cellular activity, and dynamic mechanical loading [1] [100]. The presence of active cells and proteins in vivo can significantly alter degradation kinetics. Ensure your in vitro model incorporates relevant enzymes (e.g., lysozyme) and, if possible, mechanical stress cycles to better mimic the in vivo conditions [100].
Q3: How can I distinguish between material degradation and simple dissolution? Gravimetric analysis (measuring weight loss) alone cannot distinguish between degradation and dissolution [1]. To confirm actual chemical degradation, you must employ analytical techniques that identify changes in the material's chemical structure. Techniques such as Fourier Transform Infrared Spectroscopy (FTIR) to identify breaking chemical bonds, Size Exclusion Chromatography (SEC) to track molecular weight reduction, and Nuclear Magnetic Resonance (NMR) to determine the structure of by-products are essential for confirmation [1].
Q4: What are the standard guidelines for conducting a biomaterial degradation study? The ASTM F1635-11 standard provides a key guideline for testing. It specifies that degradation should be monitored via mass loss, changes in molar mass, and mechanical testing [1]. The standard recommends using solution viscosity or SEC for molar mass evaluation and requires mass loss to be measured to a precision of 0.1% of the total sample weight. Tests are typically conducted in a phosphate-buffered solution at pH 7.4 and 37°C, though the pH may be adjusted to match the specific bodily environment targeted [1].
Troubleshooting Guides
Problem: Inconsistent Degradation Rates Between Material Batches
- Potential Cause 1: Variations in material synthesis leading to differences in crystallinity, molecular weight, or cross-linking density.
- Solution: Characterize each batch thoroughly before degradation studies. Use SEC for molecular weight distribution, Differential Scanning Calorimetry (DSC) for crystallinity, and ensure consistent processing parameters.
- Potential Cause 2: Inconsistencies in the degradation medium, such as pH drift or enzyme activity loss.
- Solution: Regularly calibrate pH meters and replace degradation media at scheduled intervals. If using enzymes, verify their activity and concentration before each use.
Problem: Unexpected Toxicity or Immune Response in Cellular Assays
- Potential Cause: Toxic by-products are being released during degradation, which were not identified in initial chemical screenings.
- Solution: Extend your chemical analysis to identify and quantify degradation by-products using techniques like Liquid Chromatography-Mass Spectrometry (LC-MS) [1]. Perform elution tests by incubating the material in a buffer and then exposing cells to the supernatant to isolate the effect of leachables.
Experimental Protocols for Degradation Assessment
The following workflow provides a standardized method for setting up a degradation study, from initial characterization to data collection on the degraded material.
Protocol 1: Standard In Vitro Hydrolytic Degradation
Objective: To assess the baseline degradation profile of a material in a simulated physiological environment without enzymatic activity.
Materials and Reagents:
- Phosphate Buffered Saline (PBS), pH 7.4
- Incubator maintained at 37°C
- Analytical balance (precision ±0.1 mg)
- Vacuum oven or desiccator
- Specimens of the novel material and established originator product (e.g., cut into discs or dumbbells)
Methodology:
- Pre-degradation Characterization: Weigh each specimen (W₀) and record initial dimensions. Perform baseline characterization via FTIR, SEC, and mechanical testing.
- Immersion: Place each specimen in a separate container with a sufficient volume of PBS (as per ASTM F1635-11) to ensure sink conditions.
- Incubation: Place containers in an incubator at 37°C.
- Sampling: At predetermined time points (e.g., 1, 7, 30, 90 days), remove specimens from the incubation medium (n=3 per time point is recommended).
- Post-degradation Processing:
- Rinse samples gently with deionized water to remove salts.
- Dry samples in a vacuum oven until a constant weight (Wₜ) is achieved.
- Calculate mass loss:
Mass Loss (%) = [(W₀ - Wₜ) / W₀] × 100.
- Analysis: Perform post-degradation characterization using the same techniques as in step 1 to compare changes.
Protocol 2: Enzymatic Degradation
Objective: To evaluate the material's susceptibility to enzyme-specific cleavage, which is critical for biomedical applications.
Materials and Reagents:
- Tris-HCl or PBS buffer, pH 7.4
- Relevant enzyme (e.g., lysozyme for polyesters, collagenase for collagen-based materials, esterases)
- 0.22 μm syringe filters for sterilizing solutions
Methodology:
- Prepare a buffered solution of the enzyme at a physiologically relevant concentration (e.g., 1.5 μg/mL for lysozyme).
- Follow the same steps as Protocol 1, using the enzyme solution as the degradation medium.
- Critical Control: Include a control group with the same buffer but without the enzyme to differentiate between hydrolytic and enzymatic degradation.
- After sampling, the enzyme in the medium can be deactivated (e.g., by heating) before further analysis.
Quantitative Data Presentation
Table 1: Key Properties of Common Biodegradable Polymers for Benchmarking
This table provides a comparison of established materials to serve as a reference point for benchmarking novel polymers.
| Material | Typical Tensile Strength (MPa) | Degradation Time (Months) | Key Degradation Mechanism | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| PLA (Polylactic Acid) [101] | 50 - 70 | 12 - 24 [101] | Hydrolysis | Good mechanical strength, processability | Acidic degradation products, slow degradation |
| PGA (Polyglycolide) [1] | 60 - 99 | 6 - 12 | Hydrolysis | High strength, rapid degradation | Acidic degradation products, stiff and brittle |
| PCL (Polycaprolactone) [1] | 20 - 40 | > 24 | Hydrolysis | Ductile, good drug permeability | Very slow degradation rate |
| PHB (Polyhydroxybutyrate) [101] | 25 - 40 | 18 - 24 [101] | Hydrolysis & Enzymatic [101] | Biocompatible, degrades in aquatic environments [101] | Brittle, narrow processing window, high cost [101] |
| Collagen (Type I) | 0.5 - 11 (varies by form) | 1 - 6 | Enzymatic (Collagenase) | Excellent biocompatibility, natural ECM | Poor mechanical strength, fast degradation |
This table helps in selecting the right techniques to build a comprehensive benchmarking profile.
| Assessment Approach | Example Techniques | Measured Parameters | Key Advantage | Key Limitation |
|---|---|---|---|---|
| Physical | Gravimetric Analysis, SEM | Mass loss, surface morphology | Simple, cost-effective, infers degradation | Cannot distinguish dissolution from degradation [1] |
| Mechanical | Tensile Testing, Dynamic Mechanical Analysis (DMA) | Young's modulus, tensile strength, elongation at break | Directly measures functional property loss | Infers degradation; requires specific sample geometries [1] |
| Chemical | FTIR, SEC, NMR, Mass Spectrometry | Molecular weight, chemical structure, by-products | Confirms degradation and identifies mechanisms [1] | Can be costly and require specialized expertise [1] |
The Scientist's Toolkit: Essential Research Reagents & Materials
The following reagents and materials are fundamental for conducting rigorous material degradation and benchmarking studies in a biomedical context.
Table 3: Key Research Reagent Solutions
| Item | Function in Experiment | Example Application |
|---|---|---|
| Phosphate Buffered Saline (PBS) | A standard isotonic solution to simulate the pH and ionic strength of the body's internal environment. | Hydrolytic degradation studies under physiological conditions. |
| Lysozyme | A hydrolytic enzyme that breaks glycosidic bonds in polysaccharides. Used to model enzymatic degradation for certain polymer types. | Testing degradation of sugar-based polymers or assessing general biofouling potential. |
| Collagenase | A protease enzyme that specifically digests collagen. | Benchmarking collagen-based materials or testing a novel material's resistance to proteolytic activity. |
| Matrigel / Other ECM Hydrogels | A basement membrane matrix extract used for 3D cell culture. Provides a more physiologically relevant environment for co-culture degradation studies. | Assessing material degradation and cell interaction in a simulated tissue microenvironment. |
| Metabolic Assay Kits (e.g., MTT, AlamarBlue) | Colorimetric or fluorometric assays to quantify cell viability and proliferation. | Screening for cytotoxicity of material extracts or degradation by-products. |
| R-spondin1 & Noggin Conditioned Medium [102] | Growth factors used in advanced cell culture systems like organoids. | Creating complex in vitro models to study material performance in tissue-specific contexts. |
Material Degradation Pathways in Biomedical Environments
This diagram illustrates the primary interconnected pathways through which a material can degrade in a biomedical context, leading to the release of by-products that must be assessed for safety.
Conclusion
Effectively resolving material degradation is paramount for advancing biomedical applications, from ensuring the controlled release of therapeutics to the successful integration of temporary implants. A holistic approach—combining a deep understanding of degradation mechanisms, the innovative application of advanced materials, robust optimization strategies, and rigorous validation through comparative studies—is essential for developing safe and effective medical products. Future progress hinges on the development of real-time, non-invasive degradation monitoring techniques, the creation of sophisticated multi-scale predictive models, and the establishment of updated, comprehensive regulatory standards that keep pace with material innovation. By systematically addressing these areas, the biomedical field can continue to create reliable and transformative solutions that significantly improve patient outcomes.
References
- 1. A review of biomaterial degradation assessment ... [https://www.nature.com/articles/s41529-024-00487-1]
- 2. Recent advances in biodegradable biosensors for ... [https://pubmed.ncbi.nlm.nih.gov/40929005/]
- 3. Editorial: Biodegradable polymers for biomedical ... [https://www.frontiersin.org/journals/materials/articles/10.3389/fmats.2025.1551590/full]
- 4. Corrosion and Degradation for Biomedical Materials [https://www.mdpi.com/journal/materials/special_issues/corrosion_biomaterials]
- 5. Advancements in Hydrogels: A Comprehensive Review of ... [https://www.mdpi.com/2073-4360/17/15/2026]
- 6. Biomedical Applications of Biodegradable Polyesters - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6432531/]
- 7. Advanced Biocompatible and Biodegradable Polymers [https://www.mdpi.com/2073-4360/17/21/2901]
- 8. Advances in Biodegradable Polymers and Biomaterials ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10488517/]
- 9. Biodegradable zinc-based metallic materials: Mechanisms, ... [https://www.sciencedirect.com/science/article/abs/pii/S0079642525001628]
- 10. Advanced Biocompatible and Biodegradable Polymers [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611034/]
- 11. Exploring the degradation behavior of biodegradable ... [https://www.sciencedirect.com/science/article/pii/S2213956725001008]
- 12. A review on the release and environmental effects of ... [https://enveurope.springeropen.com/articles/10.1186/s12302-025-01140-7]
- 13. Recent advances and challenges of injectable hydrogels ... [https://www.sciencedirect.com/science/article/abs/pii/S016836592500642X]
- 14. Chitosan based smart injectable hydrogels for biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595387/]
- 15. Next-generation biopolymer gels: innovations in drug ... [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d4tb02068e]
- 16. Advances in hybrid hydrogel design for biomedical ... [https://link.springer.com/article/10.1007/s10565-025-10064-0]
- 17. Chemical features and biological effects of degradation ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969723054542]
- 18. A users guide to degradation testing of PEG-based hydrogels [https://pmc.ncbi.nlm.nih.gov/articles/PMC11600467/]
- 19. 4 Most Common Reasons for Medical Device Material Failures [https://inside.battelle.org/blog-details/4-most-common-reasons-for-medical-device-material-failures]
- 20. Engineering long-term controlled drug release from ... [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d5tb00456j]
- 21. Multimaterial Shape Memory Polymer Fibers for Advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12420707/]
- 22. Recent advances in shape memory polymers for ... [https://www.sciencedirect.com/science/article/pii/S259018342500016X]
- 23. Advancements, Challenges, & the Future of Sustainable ... [https://www.mddionline.com/materials/biodegradable-medical-devices-advancements-challenges-the-future-of-sustainable-healthcare-innovation]
- 24. Review Smart polymers for the controlled delivery of drugs [https://www.sciencedirect.com/science/article/pii/S2211383514000252]
- 25. Latest advancements and trends in biomedical polymers ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925000744]
- 26. Three-dimensional bio-derived materials for biomedical ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d4ra07531e?page=search]
- 27. Advancement of 3D Bioprinting Towards 4D ... [https://www.mdpi.com/2504-4494/9/8/285]
- 28. a comprehensive review of biomedical applications [https://link.springer.com/article/10.1007/s43939-024-00111-8]
- 29. Hydrogel microparticle systems: fabrication, behaviors, ... [https://www.sciencedirect.com/science/article/abs/pii/S2468519425006007]
- 30. Hydrogel Microspheres as Versatile Platforms for Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12508632/]
- 31. a review of their role in controlled drug delivery and tissue ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra06280b?page=search]
- 32. Drug Discovery Assays Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 33. Nanoparticle-based drug delivery: case studies for cancer and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11115117/]
- 34. Targeted Drug Delivery — From Magic Bullet to Nanomedicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC8275483/]
- 35. Biomedical Application of Polymeric Materials [https://www.mdpi.com/2073-4360/17/17/2401]
- 36. FAQ & Troubleshooting [https://dispendix.com/knowledge-center]
- 37. Effect of degradation in polymer scaffolds on mechanical ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482524004864]
- 38. Advances and Challenges in Polymer-Based Scaffolds for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11644794/]
- 39. Development and Application of Polymer Scaffolds - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390334/]
- 40. Scaffold degradation [https://bio-protocol.org/exchange/minidetail?id=5646124&type=30]
- 41. Material extrusion of biomaterials for transformative ... [https://www.sciencedirect.com/science/article/abs/pii/S2405886625000478]
- 42. Non-invasive monitoring of tissue scaffold degradation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2922678/]
- 43. Controllable degradation behavior, mechanical properties ... [https://www.nature.com/articles/s41529-025-00658-8]
- 44. Frontiers | Surface engineering of nano magnesium for... alloys [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1617585/full]
- 45. A review on magnesium for alloys - PMC biomedical applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC9424554/]
- 46. Magnesium-based alloys for bone regeneration and beyond [https://www.sciencedirect.com/science/article/pii/S2352320425002068]
- 47. Biocorrosion of magnesium alloys: a new principle in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1767674/]
- 48. A review of current challenges and prospects ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8927531/]
- 49. Advances in biodegradable materials: Degradation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11254538/]
- 50. Biodegradable Medical Implants: Reshaping Future Medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462970/]
- 51. Recent Advances in Biodegradable Magnesium Alloys for ... [https://www.mdpi.com/2073-4352/15/8/671]
- 52. Current developments in orthopaedic implant technology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560316/]
- 53. Degradation and Remodeling of Implant Materials [https://www.nmi.de/en/material-development-and-functionalization/services/degradation-and-remodeling-of-implant-materials]
- 54. Effect of Alloying Elements on the Characteristics ... [https://www.sciencedirect.com/science/article/pii/S1000934525000240]
- 55. Material Degradation Mechanisms → Term [https://fashion.sustainability-directory.com/term/material-degradation-mechanisms/]
- 56. Degradation Behavior of Polymers Used as Coating Materials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8070827/]
- 57. Biomedical Application of Polymeric Materials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12431390/]
- 58. Degradability of Polymers for Implantable Biomedical Devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC2769140/]
- 59. Overcoming the challenges in administering biopharmaceuticals: formulation and delivery strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4455970/]
- 60. Harnessing the potential of machine learning for advancing “Quality by Design” in biomanufacturing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8744891/]
- 61. Optimization by the 4S Sequential Experimental Design ... [https://www.mdpi.com/2072-6651/17/11/557]
- 62. Experimental designs used for optimising the effects of health ... [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-025-13184-9]
- 63. Manufacturing biomedical device parts: what you need to know about quality control [https://elitebiomedicalsolutions.com/resources/blog/manufacturing-biomedical-device-parts-the-nuts-and-bolts-of-quality-control/]
- 64. Guide to Troubleshooting Common Coating Problems [https://intechfinishing.com/2025/01/30/how-to-troubleshoot-common-coating-problems/]
- 65. Coating Failure Troubleshooting [https://marvelcoatings.com/blog/coating-failure-troubleshooting-fixing-blistering-cracking-delamination]
- 66. Surface modifications of biomaterials in different applied ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10331796/]
- 67. Troubleshooting Guides - Get Help with Chemcraft Products [https://chemcraft.com/en/using-our-products/troubleshooting-guides]
- 68. Research and prospects of strategies for surface-modified ... [https://link.springer.com/article/10.1007/s44258-025-00056-4]
- 69. Biomedical Applications of Biodegradable Polymers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3136871/]
- 70. Challenges With the Development of Biomaterials for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6554598/]
- 71. Degradation Studies of Resorbable Materials for Biomedical ... [https://www.taylorfrancis.com/chapters/edit/10.1201/9781003470311-13/degradation-studies-resorbable-materials-biomedical-applications-vishnuvarthanan-mayakrishnan-preethi-arul-murugan]
- 72. A Review of Material Degradation Modelling for the ... [https://pubmed.ncbi.nlm.nih.gov/26271520/]
- 73. Optimizing accuracy and dimensionality: a swarm intelligence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12625619/]
- 74. Elite Bernoulli-based mutated dung beetle algorithm for ... [https://www.nature.com/articles/s41598-025-06108-4]
- 75. Material synthesis and design optimization of biomaterials for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11954756/]
- 76. Climbing the longevity pyramid: overview of evidence-driven ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11628525/]
- 77. Data Decomposition Modeling Based on Improved Dung ... [https://www.mdpi.com/2306-5729/9/12/146]
- 78. Forced Degradation Studies: Regulatory Considerations ... [https://www.biopharminternational.com/view/forced-degradation-studies-regulatory-considerations-and-implementation]
- 79. The Effect of Surface Treatments on the Degradation ... [https://www.mdpi.com/1996-1944/11/12/2561]
- 80. F1904 Standard Guide for Testing the Biological ... [https://www.astm.org/f1904-23.html]
- 81. Degradable Biomaterials - an overview [https://www.sciencedirect.com/topics/engineering/degradable-biomaterials]
- 82. Review of the Synthesis and Degradation Mechanisms ... [https://www.mdpi.com/2073-4360/17/1/66]
- 83. 10-evolved-terms-every-scientist-should-know-about ... [https://resources.nanotempertech.com/blog/10-evolved-terms-every-scientist-should-know-about-targeted-protein-degradation-in-2025]
- 84. Basics of Biocompatibility: Information Needed for ... [https://www.fda.gov/medical-devices/biocompatibility-assessment-resource-center/basics-biocompatibility-information-needed-assessment-fda]
- 85. Demonstration of in vitroin vivo relationship (IVIVR) and ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354925005003]
- 86. Demonstration of in vitro-in vivo relationship (IVIVR) and ... [https://pubmed.ncbi.nlm.nih.gov/41173270/]
- 87. PROTAC Degraders in Clinical Trails: 2025 Update [https://www.biochempeg.com/article/434.html]
- 88. The latest trends in drug discovery [https://www.cas.org/resources/cas-insights/2025-drug-discovery-trends]
- 89. Development of forced degradation and stability indicating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5761119/]
- 90. What are Forced Degradation Studies? An Introduction [https://www.acdlabs.com/blog/what-are-forced-degradation-studies-an-introduction-to-pharmaceutical-stress-testing/]
- 91. Forced Degradation Studies for Biopharmaceuticals [https://www.biopharminternational.com/view/forced-degradation-studies-biopharmaceuticals-1]
- 92. Forced Degradation Studies: Why, What & How [https://biopharmaspec.com/blog/reasons-to-perform-forced-degradation-studies/]
- 93. Assessing the Comparability of Degradation Profiles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472202/]
- 94. Comparative Forced Degradation Study of Anticomplement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030638/]
- 95. Biosimilar Critical Quality Attribute Evaluation on Maurice [https://www.bio-techne.com/resources/protocols-troubleshooting/biosimilar-platform-methods-on-maurice]
- 96. Charge Isoform Analysis by icIEF and IEX [https://biopharmaspec.com/protein-characterization-services/charge-and-isoform-pattern/]
- 97. Forced Degradation Testing as Complementary Tool for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6783961/]
- 98. Troubleshooting Waters UPLC Systems: Common Issues ... [https://www.waters-equipment.com/article/troubleshooting-waters-uplc-systems]
- 99. Essentials of LC Troubleshooting, Part III: Those Peaks ... [https://www.chromatographyonline.com/view/essentials-of-lc-troubleshooting-part-iii-those-peaks-don-t-look-right]
- 100. Materials Degradation - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/engineering/materials-degradation]
- 101. Materials designed to degrade: structure, properties ... [https://pubs.rsc.org/en/content/articlehtml/2025/py/d4py00623b]
- 102. A Practical Guide to Developing and Troubleshooting Patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566426/]