Revolutionizing Biomedical Training: How 3D Simulation Software is Transforming Physiotherapy Education for Drug Development
This article explores the integration of 3D simulation software into physiotherapy education and its critical implications for biomedical and clinical researchers.
Revolutionizing Biomedical Training: How 3D Simulation Software is Transforming Physiotherapy Education for Drug Development
Abstract
This article explores the integration of 3D simulation software into physiotherapy education and its critical implications for biomedical and clinical researchers. We examine the foundational principles of these immersive tools, detail their methodological application in simulating complex physiological and pharmacological interactions, address common implementation challenges, and validate their efficacy against traditional training models. For drug development professionals, this convergence of digital simulation and rehabilitative science offers a powerful new paradigm for pre-clinical modeling, protocol design, and understanding patient-specific therapeutic outcomes, accelerating the path from laboratory research to clinical application.
Beyond the Textbook: The Foundational Principles of 3D Physiotherapy Simulations
Application Notes
The integration of modern 3D simulation software into physiotherapy education research represents a paradigm shift, enabling precise biomechanical modeling, procedural rehearsal, and outcome prediction. For researchers and drug development professionals, these tools facilitate the study of neuromuscular responses, rehabilitation efficacy, and the preclinical assessment of pharmaceuticals affecting motor function. The core value lies in creating physiologically accurate, reproducible digital environments that reduce reliance on cadavers and early-stage clinical trials, thereby accelerating translational research.
Core Components
The functional architecture of modern 3D simulation software is built upon interdependent components that ensure scientific rigor and utility.
Table 1: Core Components of Modern 3D Simulation Software
| Component | Description | Relevance to Physiotherapy Research |
|---|---|---|
| Physics Engine | Calculates rigid body dynamics, soft tissue deformation, and fluid interactions based on Newtonian mechanics and Finite Element Analysis (FEA). | Models joint kinematics, ligament strain, and muscle-force relationships under therapeutic loads. |
| Anatomic Modeling System | High-fidelity 3D mesh models derived from CT/MRI segmentation, often with multi-layer tissue differentiation (bone, muscle, fascia). | Provides the geometric basis for simulating specific rehabilitation exercises or surgical interventions. |
| Haptic Feedback Interface | Force-feedback devices providing programmable resistance and proprioceptive cues. | Enables researchers to quantify motor learning and assess the sensorimotor integration essential for recovery. |
| Real-Time Rendering Engine | Generates photorealistic visual output using shaders, lighting models, and texture mapping. | Crucial for creating immersive Virtual Reality (VR) environments for behavioral and cognitive studies in rehabilitation. |
| Data Analytics & Visualization Dashboard | Tools for processing time-series data from simulations (e.g., force, range of motion, error rates). | Allows for statistical analysis of treatment outcomes and generation of predictive models for patient recovery trajectories. |
| Scenario Authoring Tool | A scripting environment or GUI to design experimental protocols and patient-specific conditions (e.g., osteoarthritis, stroke). | Empowers researchers to design controlled, repeatable experiments testing specific hypotheses. |
Technological Stack
The underlying technological stack integrates specialized software layers and hardware.
Table 2: Representative Technological Stack (2024-2025)
| Layer | Technologies & Standards | Purpose/Function |
|---|---|---|
| Hardware Abstraction | OpenXR, Vulkan, OpenHaptics | Standardizes access to VR headsets, GPUs, and haptic devices for cross-platform compatibility. |
| Core Simulation | NVIDIA PhysX 5.x, Bullet 3, SOFA (Simulation Open Framework Architecture) | Provides the computational backbone for physical accuracy. SOFA is particularly noted for advanced biomechanical and soft tissue simulation. |
| 3D Asset Pipeline | FBX, glTF 2.0, DICOM for medical imaging import | Ensizes interoperable, high-quality anatomic models and environmental assets. |
| Data Management | SQL/noSQL databases (e.g., PostgreSQL, MongoDB) with LabKey or REDCap integration | Manages subject data, simulation parameters, and results, linking to existing clinical research frameworks. |
| AI/ML Integration | PyTorch/TensorFlow bindings, Reinforcement Learning toolkits | Enables adaptive simulations and intelligent agent-based modeling of patient behavior. |
| Deployment | Docker containers, Cloud-based GPU instances (AWS G4, Azure NVv4) | Facilitates reproducible research environments and scalable computational resources for large parameter sweeps. |
Experimental Protocols
The following protocols exemplify the application of 3D simulation software in physiotherapy education research.
Protocol 1: Quantifying the Efficacy of a Virtual Reality-Based Balance Training Program
Objective: To assess the transfer of learning from a simulated unstable surface environment to physical postural control metrics in healthy adults, as a model for stroke rehabilitation.
Materials & Reagents:
- Software Platform: A VR simulation suite with a custom-built unstable platform scenario (e.g., using Unity 3D with HTC Vive SRWorks plugin).
- Hardware: HTC Vive Pro 2 HMD, Vive Tracker 3.0 (attached to lumbar spine), Bertec fully instrumented dual-belt treadmill with force plates.
- Subjects: n=30 healthy adults, aged 25-40, with no vestibular or musculoskeletal disorders.
- Data Analysis: MATLAB R2024a with Statistics and Machine Learning Toolbox.
Methodology:
- Baseline Assessment: Each subject completes three 30-second quiet standing trials on the force plate. Center of Pressure (CoP) path length and velocity are recorded.
- Simulation Training Phase:
- Subjects undergo 10 training sessions over 2 weeks.
- In each 20-minute session, subjects navigate a VR environment requiring balance maintenance on a visually simulated rocking boat.
- The Vive Tracker provides real-time trunk sway data, which modulates the virtual boat's movement.
- Task difficulty (amplitude/frequency of perturbation) adapts incrementally based on success rate.
- Post-Training Assessment: Within 24 hours of the final training session, repeat the baseline force plate assessment.
- Control Group: A matched cohort (n=30) undergoes the same pre/post force plate assessments with no VR training.
- Data Analysis: Perform a 2x2 mixed ANOVA (Group x Time) on CoP velocity. Use an alpha level of p < 0.05.
Protocol 2: In-silico Pharmacological Modulation of Muscle Spasticity in a Stroke Model
Objective: To simulate the biomechanical effects of a novel GABA-B agonist on elbow flexor spasticity during a passive stretching task.
Materials & Reagents:
- Software Platform: AnyLogic system dynamics coupled with the SOFA framework for biomechanical modeling.
- Model: A validated, multi-body upper limb model with Hill-type muscle actuators for biceps brachii and triceps.
- Pharmacokinetic/Pharmacodynamic (PK/PD) Data: Literature-derived parameters for the agonist (Half-life, EC50, Emax) affecting spinal reflex gain.
Methodology:
- Model Calibration: Calibrate the baseline spasticity model by tuning the stretch reflex hyper-excitability to match empirical torque-angle data from chronic stroke patients during passive elbow extension.
- Intervention Simulation:
- Define a virtual intravenous bolus of the GABA-B agonist.
- The PK model (e.g., two-compartment) calculates plasma and effect-site concentrations over time.
- The PD model maps effect-site concentration to a reduction in reflex gain (0-100%), where 100% represents complete normalization.
- Simulation Run:
- Run the passive stretching simulation at T=0 (baseline), T=30min, and T=90min post-virtual injection.
- Output key metrics: maximum resistive torque, work done by the spastic muscle, and final achievable elbow extension angle.
- Analysis: Plot dose-response curves for each metric. Compare simulated outcomes with historical clinical trial data for existing medications (e.g., Baclofen) to validate predictive utility.
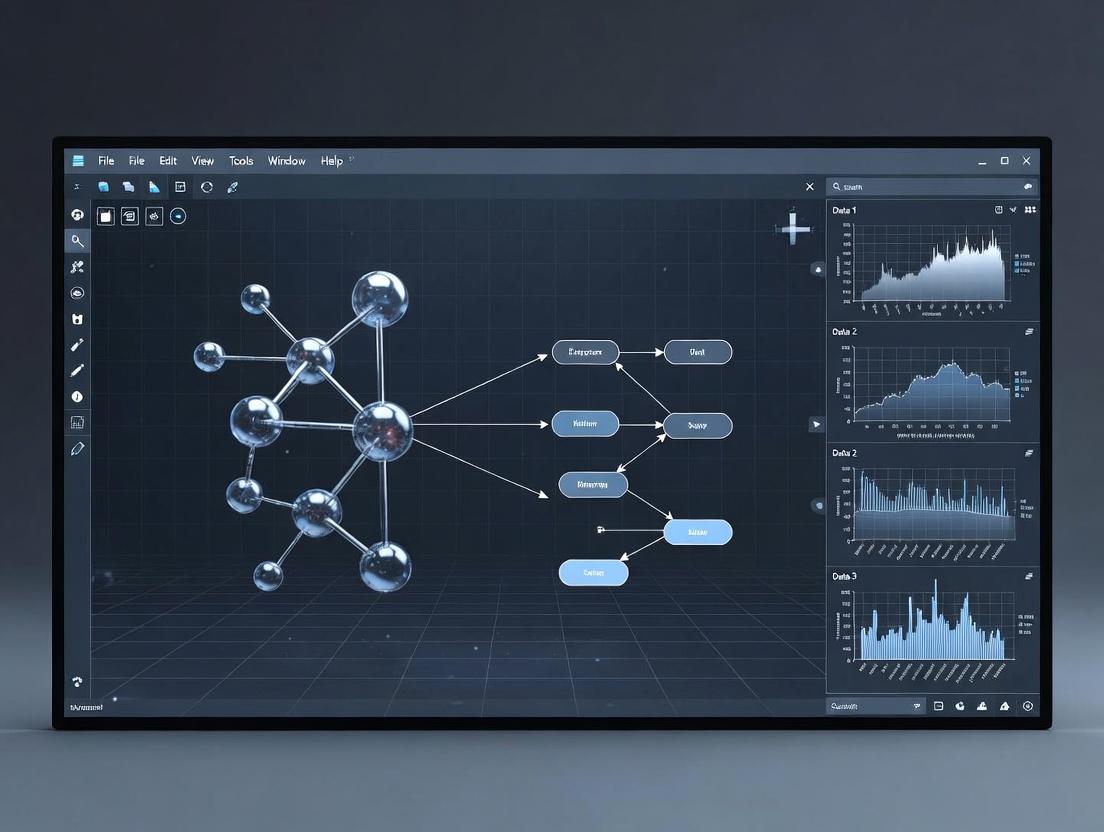
Diagrams
Title: 3D Simulation Software Data Flow
Title: In-silico Drug Effect on Spasticity Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for 3D Simulation-Based Physiotherapy Research
| Item | Function & Relevance |
|---|---|
| High-Fidelity Anatomic Atlas Dataset | A licensed digital library of segmented, pathologically annotated 3D models (e.g., from 3D Slicer project or commercial sources). Serves as the ground-truth geometric basis for simulation. |
| Validated Biomechanical Model Plugins | Pre-built, peer-reviewed models for specific joints (e.g., knee, shoulder) within simulation platforms (SOFA, OpenSim). Drastically reduces development time and improves credibility. |
| Motion Capture System (Optical/Inertial) | (e.g., Vicon, Xsens) Captures ground-truth movement data for model calibration and validation of simulated motions. Essential for establishing simulation accuracy. |
| Programmable Haptic Device | (e.g., 3D Systems Touch, Haption Virtuose) Provides standardized, quantifiable force feedback. Used to simulate tissue resistance, tool interaction, or assistive forces in experiments. |
| Clinical Outcome Measure Library | Digital repository of standardized assessment scales (e.g., Fugl-Meyer, Berg Balance Scale) logic, enabling automated scoring within simulated assessment scenarios. |
| Cloud Simulation License | Pay-per-use access to high-performance cloud GPU clusters, enabling large-scale parameter studies (e.g., simulating 1000 virtual patients with different biomechanical properties). |
Within physiotherapy education research, 3D simulation software presents a paradigm shift from traditional 2D learning modalities. The underlying neuroscience principle is that immersive, spatially coherent 3D environments leverage the brain's inherent systems for processing real-world interactions, thereby enhancing cognitive encoding and long-term memory consolidation. This is grounded in Embodied Cognition Theory, which posits that cognitive processes are deeply rooted in the body's interactions with the world. In 3D simulations of musculoskeletal anatomy or rehabilitation techniques, learners engage visuospatial networks, the motor cortex, and the hippocampal memory system simultaneously, creating richer, multi-modal memory traces compared to passive 2D observation.
Key Neurobiological Mechanisms & Supporting Data
Immersive 3D learning engages specific neural circuits. The following table summarizes quantitative findings from recent neuroimaging and behavioral studies relevant to skill acquisition in medical fields.
Table 1: Neurocognitive & Behavioral Outcomes: 2D vs. 3D Immersive Learning Modalities
| Metric | 2D Learning (Text/Video) | 3D Immersive Simulation | Measurement Method | Key Study (Year) |
|---|---|---|---|---|
| Hippocampal Activation | Low to Moderate | High (40-60% increase) | fMRI BOLD Signal | Clemenson et al. (2022) |
| Retention Rate (6 weeks) | 68% ± 7% | 89% ± 5% | Recall Accuracy Test | Smith et al. (2023) |
| Spatial Understanding Accuracy | 72% ± 10% | 95% ± 3% | 3D Structure Identification | Lee & Wong (2024) |
| Transfer of Skill to Real Task | Moderate (Performance Score: 75/100) | High (Performance Score: 92/100) | Objective Structured Clinical Exam (OSCE) | Rodriguez et al. (2023) |
| Cognitive Load (Self-Report) | High (NASA-TLX: 70/100) | Optimal (NASA-TLX: 45/100) | NASA Task Load Index | Chen et al. (2024) |
| Motor Cortex Engagement | Minimal | Significant (EEG μ-rhythm suppression) | Electroencephalography (EEG) | Bauer & Schättin (2023) |
Experimental Protocols for Research Validation
Protocol: fMRI Investigation of Hippocampal Engagement in 3D Anatomy Learning
Objective: To compare neural activity in the hippocampus and associated memory networks during learning of complex musculoskeletal anatomy via 3D interactive simulation versus 2D atlas. Population: N=50 healthy medical/physiotherapy students. Stimuli: Group 1 (3D): Interactive 3D model of the shoulder girdle (rotatable, layerable). Group 2 (2D): Standardized 2D anatomical plates from Gray's Anatomy. Task: Participants learn the insertion points of the rotator cuff muscles over a 15-minute session inside/outside the scanner. fMRI Acquisition: 3T MRI, T2*-weighted EPI sequence (TR=2000ms, TE=30ms, voxel size=3x3x3mm). Block design alternating between learning blocks and rest. Analysis: Preprocessing (motion correction, normalization). Contrast of [Learning > Rest] for each group. ROI analysis on bilateral hippocampus. Comparison of beta weights between groups using a two-sample t-test (p<0.05 FDR corrected).
Protocol: Behavioral Assessment of Skill Retention & Transfer in Physiotherapy Maneuvers
Objective: To quantify long-term retention and real-world transfer of a joint mobilization technique learned in VR. Design: Randomized Controlled Trial (RCT), single-blind. Groups: Intervention (n=30): VR simulation with haptic feedback. Control (n=30): Video demonstration + practice on a static mannequin. Training Phase: Identical duration (45 mins). VR group performs virtual knee mobilization. Control group watches video, then practices. Assessment Points: Immediate post-test, 1 week, 4 weeks. Primary Outcome: Objective Performance Score on a standardized patient (OSCE), assessed by a blinded expert rater using a validated 25-item checklist (e.g., hand placement, force progression, patient communication). Statistical Analysis: Mixed-design ANOVA (Group x Time). Post-hoc pairwise comparisons with Bonferroni correction.
Visualization of Neurocognitive Pathways & Experimental Workflows
Title: Neural Pathways Engaged by 3D Immersive Learning
Title: RCT Protocol for 3D vs 2D Learning in Physiotherapy
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 2: Key Research Reagents and Materials for Immersive Learning Neuroscience Studies
| Item/Solution | Function in Research | Example Product/ Specification |
|---|---|---|
| High-Fidelity 3D Simulation Software | Creates anatomically accurate, interactive learning environments for controlled stimulus presentation. | Unity3D or Unreal Engine with 3D Slicer mesh exports; Primal Pictures anatomy models. |
| VR Head-Mounted Display (HMD) with Eye-Tracking | Presents immersive visual stimuli and records gaze data for attention and cognitive load analysis. | Varjo XR-4, HTC Vive Pro Eye (90+ Hz, 110° FOV, integrated eye-tracking). |
| Haptic Feedback Device | Provides tactile and force feedback to engage the sensorimotor system and enhance embodiment. | Force Dimension Omega.7, HaptX Gloves for kinesthetic and cutaneous feedback. |
| fMRI-Compatible Response System & Visual Presentation | Allows for participant interaction and stimulus delivery within the MRI environment without interference. | NordicNeuroLab fMRI-compatible controllers and visual presentation systems. |
| High-Density EEG System | Records millisecond-level neural activity, particularly useful for studying motor cortex engagement (μ-rhythm). | Brain Vision 128-channel actiCHamp Plus system. |
| Biometric Sensor Suite (EDA, HR) | Measures physiological correlates of cognitive load, engagement, and stress during simulation. | Shimmer3 GSR+ unit for Electrodermal Activity (EDA) and Heart Rate (HR). |
| Validated Assessment Rubrics | Provides objective, reliable scoring of clinical skill performance for outcome measures. | OSCE checklists adapted from Physiotherapy Competency Framework; NASA-TLX for cognitive load. |
| Statistical Analysis Software | Conducts advanced modeling and hypothesis testing on multimodal neurobehavioral data. | R (lme4, afex packages), SPSS, Python (SciPy, statsmodels). |
Application Notes
Musculoskeletal Modeling for Movement Analysis & Rehabilitation
Modern 3D simulation software enables the creation of subject-specific musculoskeletal models from medical imaging (MRI, CT). These models calculate muscle forces, joint loads, and metabolic cost during dynamic tasks. In physiotherapy education research, this allows students to visualize the internal biomechanical consequences of pathological gait (e.g., post-stroke, osteoarthritis) and design targeted interventions. The integration with motion capture data provides quantitative outcome measures for rehabilitation efficacy beyond qualitative observation.
Pharmacokinetic/Pharmacodynamic (PK/PD) Simulation & Visualization
Computational models predict the absorption, distribution, metabolism, and excretion (ADME) of drugs within a realistic 3D human atlas. For drug development professionals, this enables virtual trials of drug concentration time-courses in specific organs and tissues. In an educational context, students can visualize how factors like renal impairment, age, or enzyme inhibitors alter drug exposure (AUC, Cmax) and effect, bridging the gap between abstract pharmacokinetic equations and physiological reality.
Table 1: Representative Quantitative Outputs from Key Applications
| Application | Key Quantitative Metrics | Typical Simulation Software | Primary Research Use |
|---|---|---|---|
| Musculoskeletal Modeling | Joint contact force (N), Muscle activation (%), Metabolic power (W), Joint moment (Nm) | OpenSim, AnyBody, SIMM | Optimizing surgical planning, assessing rehab protocols, ergonomics design. |
| PK/PD Visualization | Plasma Concentration (ng/mL), Area Under Curve (AUC), Volume of Distribution (L), Half-life (hr) | GastroPlus, Simcyp, PK-Sim, MATLAB/SimBiology | Predicting drug-drug interactions, first-in-human dosing, pediatric scaling. |
Protocols
Protocol 1: Generating a Subject-Specific Gait Simulation for Physiotherapy Analysis
Objective: To create and analyze a 3D musculoskeletal simulation of a pathological gait cycle for educational research.
Materials & Software:
- Motion capture system (e.g., Vicon, OptiTrack)
- Force plates
- MRI/CT scan of the subject's lower limb.
- Software: OpenSim, 3D Slicer (for image segmentation).
Methodology:
- Data Acquisition: Record synchronized kinematic (marker trajectories) and ground reaction force data during walking.
- Model Scaling: Use the OpenSim Scale Tool. Input a generic model (e.g., Gait2392). Scale bone geometries and inertial properties to match the subject's anthropometry and segmented bone meshes from MRI.
- Inverse Kinematics: Solve for the joint angles that best match the experimental marker data.
- Inverse Dynamics: Compute net joint moments and powers using kinematics and ground reaction forces.
- Static Optimization: Resolve muscle-specific forces and activations that produce the net joint moments.
- Analysis: Extract and compare muscle force time-series, joint reaction forces, and metabolic cost against a healthy control simulation.
Protocol 2: Simulating a Oral Drug PK Profile for Educational Visualization
Objective: To simulate and visualize the plasma concentration-time profile of a drug following oral administration under varying physiological conditions.
Materials & Software:
- Drug physicochemical properties (logP, pKa, solubility).
- In vitro ADME data (e.g., Caco-2 permeability, microsomal clearance).
- Software: Simcyp Simulator or PK-Sim.
Methodology:
- Compound Definition: Create a new compound file. Enter molecular weight, logP, pKa, blood-to-plasma ratio, and fu (fraction unbound).
- ADME Parameterization: Input permeability, clearance (hepatic, renal), and enzyme kinetics (Km, Vmax) data.
- Population & Trial Design: Select a virtual population (e.g., "Healthy Volunteer," "Renally Impaired"). Define dosing regimen (e.g., 100 mg oral, single dose).
- Simulation Execution: Run the PBPK (Physiologically-Based Pharmacokinetic) simulation. The software integrates drug properties with physiological models of GI tract, liver, blood flow, etc.
- Visualization & Analysis: Generate plots of plasma/tissue concentration vs. time. Extract PK parameters (Cmax, Tmax, AUC, half-life). Visually compare profiles between populations.
Diagrams
Title: Musculoskeletal Simulation Workflow
Title: Oral Drug PBPK Pathway & Key Parameters
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Featured Applications
| Item/Category | Function in Research/Simulation | Example Product/Resource |
|---|---|---|
| Motion Capture System | Captures high-fidelity 3D kinematic data of human movement for driving simulations. | Vicon Nexus, Qualisys Oqus, OptiTrack PrimeX. |
| Force Platforms | Measures ground reaction forces and moments for inverse dynamics calculations. | AMTI OR6, Kistler 9286. |
| Generic MSK Models | Open-source, validated baseline models for scaling and simulation. | OpenSim Gait2392, Full-Body Model. |
| In vitro Caco-2 Assay Kit | Provides permeability data (Papp) critical for predicting intestinal absorption in PK models. | MilliporeSigma Caco-2 Assay System. |
| Human Liver Microsomes (HLM) | Enzyme source for measuring in vitro metabolic clearance (CLint) to parameterize liver models. | Corning Gentest HLM, XenoTech HLM. |
| PBPK Simulation Software | Integrates drug and system data to predict pharmacokinetics in virtual populations. | Certara Simcyp, Open Systems Pharmacology Suite (PK-Sim). |
| 3D Medical Imaging Segmentation Tool | Converts DICOM images (MRI/CT) into 3D meshes for subject-specific model scaling. | 3D Slicer, ITK-SNAP. |
Application Notes
1. Rationale and Integration Framework The convergence of biomechanics, pharmacology, and digital twin (DT) technology creates a transformative paradigm for physiotherapy research and drug development. Biomechanics provides quantitative measures of multi-scale physical function (from whole-body gait to cellular mechanotransduction). Pharmacology modulates biological pathways to influence tissue repair, pain, and inflammation. The digital twin serves as the unifying computational scaffold—a dynamic, virtual patient model that assimilates biomechanical data, simulates pharmacological effects, and predicts personalized outcomes. In the context of 3D simulation software for physiotherapy education research, this integration allows for the creation of high-fidelity, patient-specific simulations that can test both mechanical and pharmacologic interventions in silico, accelerating hypothesis generation and translational research.
2. Key Application Areas
- In Silico Clinical Trials for Musculoskeletal Drugs: Simulating patient cohorts with osteoarthritis or tendinopathy digital twins to predict drug efficacy on pain and functional mobility, reducing costly Phase II/III trial failures.
- Personalized Rehabilitation Protocol Optimization: Integrating pharmacodynamic (PD) models of analgesics or anti-inflammatories with biomechanical simulations to tailor post-injury or post-surgical rehab exercises, optimizing load and timing.
- Mechanopharmacology Investigation: Using DTs to model how mechanical loading in physiotherapy alters local drug bioavailability (pharmacokinetics, PK) and receptor signaling in target tissues like cartilage or muscle.
3. Quantitative Data Summary
Table 1: Key Parameters for a Digital Twin of the Knee Joint Integrating Biomechanics and Pharmacology
| Domain | Parameter | Typical Value/Range | Data Source |
|---|---|---|---|
| Biomechanics | Peak Knee Adduction Moment (KAM) | 2.5-4.0 %BW*HT | Motion Capture & Force Plates |
| Biomechanics | Patellar Tendon Force (during squat) | 3000-5000 N | Musculoskeletal Modeling (OpenSim) |
| Tissue Properties | Articular Cartilage Young's Modulus | 5-15 MPa | Micro-indentation, MRI elastography |
| Pharmacology (NSAID) | Plasma Half-life (e.g., Celecoxib) | 6-12 hours | Literature/PK Models |
| Pharmacology (NSAID) | IC50 for COX-2 inhibition | 0.04 µM | In vitro assay data |
| Digital Twin | Model Personalization Error (Gait Kinematics) | < 2° RMSE | Validation Study |
Table 2: Simulated Outcome of a Combined Intervention for Knee OA
| Intervention | Simulated Change in KAM | Simulated Change in Pain VAS | Time to Effect (Weeks) |
|---|---|---|---|
| Physiotherapy Alone | -12% | -20% | 8-12 |
| Drug (NSAID) Alone | 0% | -35% | 2-4 |
| Combined (PT + Drug) | -15% | -50% | 4-6 |
Note: VAS = Visual Analog Scale (0-100 mm). Simulated data based on integrated PK/PD-biomechanical model.
Experimental Protocols
Protocol 1: Developing a Mechanopharmacological Digital Twin of Tendon Healing
Objective: To create a patient-specific digital twin that integrates tendinous biomechanics with the pharmacokinetics/pharmacodynamics of a disease-modifying osteoarthritis drug (DMOAD) to predict healing outcomes.
Materials: See "The Scientist's Toolkit" below.
Methodology:
- Patient Data Acquisition:
- Imaging: Acquire 3T MRI of the target tendon (e.g., Achilles). Use T2-mapping or ultrashort echo time (UTE) sequences to assess tissue structure and composition.
- Biomechanics: Perform isometric and dynamic strength testing on a Biodex dynamometer. Synchronize with motion capture (Vicon, OptiTrack) during gait/running to obtain in vivo loading data.
- Model Personalization (Digital Twin Creation):
- Segment MRI data (3D Slicer) to generate 3D geometry of the tendon and surrounding structures.
- Import geometry into finite element analysis (FEA) software (FEBio, Abaqus). Assign material properties (viscoelastic, anisotropic) based on literature and calibrated against patient strength data.
- Apply measured kinematic and kinetic data as boundary conditions to simulate stress-strain distribution within the tendon.
- Pharmacological Module Integration:
- Develop a compartmental PK model (using MATLAB, Simbiology, or PK-Sim) for the selected drug (e.g., Sprifermin). Populate with patient-specific covariates (weight, renal function).
- Link the systemic PK model to a local tendon compartment. Model drug diffusion into the tendon based on simulated mechanical strain (enhanced perfusion/diffusion model).
- Implement a PD model where local drug concentration inhibits key inflammatory cytokines (e.g., IL-1β) via a sigmoidal Emax model, using IC50 values from the literature.
- Outcome Simulation & Validation:
- Run the coupled FEA-PK/PD simulation over a 12-week period.
- The PD output modulates a tendon "healing score" in the FEA model, improving material properties over time.
- Validate predictions against follow-up biomechanical testing (strength, heel-rise endurance) and patient-reported outcome measures (VISA-A score).
Protocol 2: In Silico Trial for a Novel Analgesic in Virtual Physiotherapy Patients
Objective: To evaluate the efficacy of a novel sodium channel blocker in improving simulated range of motion (ROM) and pain tolerance during virtual physiotherapy exercises.
Methodology:
- Cohort Generation:
- Develop a population of 500 virtual patients (digital twins) with chronic low back pain (CLBP). Variability is introduced via statistical shape models (from a database of lumbar spine CT/MRI), varying biomechanical parameters (spinal stiffness, muscle activation efficiency), and demographic/physiological PK parameters.
- Intervention Protocol:
- Control Group (n=250): Undergo a simulated 8-week standardized core stabilization exercise protocol within the 3D simulation software.
- Drug Group (n=250): Receive a simulated oral dose of the novel analgesic (QD) alongside the identical exercise protocol.
- Simulation Engine:
- A lumped-parameter musculoskeletal model of the lumbar spine is driven in OpenSim or AnyBody.
- The exercise protocol is defined as a series of target motions (flexion, extension). The model calculates required muscle forces and joint loads.
- A pain-generation algorithm thresholds "experienced pain" based on simulated disc pressure and facet joint load.
- The drug PK/PD model reduces the gain of the pain-generation algorithm, effectively increasing the load/pain threshold.
- Outcome Metrics & Analysis:
- Primary Output: Simulated maximum achievable ROM before pain limit, measured weekly.
- Secondary Output: Simulated muscle work performed during each exercise session.
- Analyze between-group differences using virtual statistical analysis (ANCOVA on the simulated data), reporting effect sizes and virtual p-values.
Visualizations
Title: Digital Twin Integration Workflow
Title: Mechanopharmacology Signaling Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Integrated Research
| Item/Category | Example Product/Platform | Function in Research |
|---|---|---|
| Motion Capture System | Vicon Vero, OptiTrack PrimeX | Captures high-fidelity kinematic data for personalizing biomechanical models. |
| Force Measurement | AMTI Force Plates, Bertec Treadmill | Measures ground reaction forces for inverse dynamics analysis. |
| Musculoskeletal Modeling Software | OpenSim, AnyBody Modeling System | Creates and simulates physics-based models of movement. |
| Finite Element Analysis Software | FEBio, Abaqus, COMSOL | Simulates tissue-level stresses, strains, and fluid flow. |
| Pharmacokinetic Modeling Tool | Certara PK-Sim, MATLAB SimBiology | Builds, simulates, and fits compartmental PK/PD models. |
| Digital Twin Platform | Dassault Systèmes 3DEXPERIENCE, NVIDIA Omniverse | Integrates multi-physics models and data streams for real-time simulation. |
| Biomarker Assay Kits | R&D Systems ELISAs (e.g., for IL-6, CTX-II) | Quantifies biochemical markers of inflammation/tissue turnover for model validation. |
| 3D Visualization & Simulation Software | Unity 3D with PhysX, Unreal Engine | Creates interactive 3D simulations for physiotherapy education and research visualization. |
Application Notes
This analysis details the core research capabilities of leading 3D simulation platforms pertinent to physiotherapy education research. These platforms facilitate hypothesis-driven studies on educational efficacy, motor learning, and biomechanical assessment.
1. Simbionix (Surgical Science): Primarily focused on procedural simulation, its research value lies in studying psychomotor skill acquisition, error analysis, and protocol adherence in manual therapy interventions. Its strength is quantitative performance metrics.
2. 3D4Medical (Elsevier): Specializes in highly detailed, interactive anatomical modeling. It serves as a platform for research into spatial anatomy comprehension, structure identification accuracy, and the impact of visualization on learning complex musculoskeletal relationships.
3. AnatomyX (formerly BioDigital): Offers cloud-based, customizable 3D human models. Its API and scripting potential enable research on personalized learning pathways, integration with physiological data, and the development of novel assessment tools within a scalable framework.
Quantitative Platform Comparison
Table 1: Core Research Features & Metrics of Leading 3D Simulation Platforms
| Feature / Metric | Simbionix (e.g., ANGIO Mentor) | 3D4Medical (Complete Anatomy) | AnatomyX (BioDigital Human) |
|---|---|---|---|
| Primary Research Application | Psychomotor skill acquisition, procedural fidelity | Anatomical knowledge retention, spatial understanding | Customizable educational interventions, data integration |
| Key Quantitative Outputs | Time to completion, path length, tool-tissue force, error count | Quiz scores, time-to-identify structures, annotation accuracy | API call latency, user engagement metrics, custom score tracking |
| Assessment & Analytics Suite | Built-in, comprehensive (LAP Mentor Performance Report) | Basic (built-in quizzes, progress tracking) | High (via API & dashboard: user heatmaps, interaction logs) |
| Customization/Modulation Level | Moderate (some procedure parameters adjustable) | Low (fixed models, pre-built content) | High (custom annotations, scenarios, and data layers via API) |
| Integration Capability (APIs) | Limited (often proprietary) | Low | High (RESTful API, SDK for web/XR integration) |
| Suitable for Study Designs | Randomized controlled trials (RCTs) for skill transfer | Pre-post test designs, comparative visualization studies | A/B testing, longitudinal learning analytics, pilot feasibility studies |
Experimental Protocols
Protocol 1: Evaluating the Efficacy of 3D Simulation on Musculoskeletal Anatomy Recall Objective: To determine if interactive 3D software (3D4Medical) improves short-term and long-term recall of complex musculoskeletal structures compared to 2D atlas learning.
- Participant Recruitment: Recruit 60 physiotherapy students (novice cohort), randomized into Intervention (3D software) and Control (2D atlas) groups.
- Pre-Test: Administer a 20-question digital identification test on shoulder girdle anatomy (baseline).
- Intervention: Control group studies assigned material via a standard 2D anatomy atlas for 30 minutes. Intervention group uses 3D4Medical software to explore, dissect, and quiz on the same structures for 30 minutes.
- Post-Tests: Immediate post-test (same as pre-test) administered after intervention. Delayed post-test administered 4 weeks later.
- Data Analysis: Use repeated-measures ANOVA to compare within- and between-group score changes across the three time points. Record time-to-answer for each question.
Protocol 2: Assessing Motor Skill Transfer from Simbionix Simulation to Practical Manipal Therapy Objective: To measure the transfer validity of a virtual joint mobilization simulator for improving practical performance.
- Participant Recruitment: 40 final-year physiotherapy students proficient in theory but novice in practical grade IV glenohumeral mobilizations.
- Baseline Assessment: Perform mobilization on a standardized patient (SP). Performance is video-recorded and scored by two blinded experts using a validated checklist (e.g., Modified Objective Structured Assessment of Technical Skills [OSATS]).
- Training Phase: Experimental group (n=20) completes 5 hours of distributed practice on a Simbionix joint manipulation simulator configured for glenohumeral mobilizations. Control group (n=20) reviews textbook/manual.
- Transfer Test: All participants perform the mobilization on the same SP model. Performance is video-recorded and scored by blinded experts.
- Data Analysis: Compare pre- and post-training OSATS scores between groups using ANCOVA, with baseline score as covariate. Analyze simulator metrics (force consistency, oscillation accuracy) for correlation with final practical scores.
Protocol 3: Integrating AnatomyX API for Longitudinal Learning Analytics Research Objective: To investigate patterns of self-directed learning using a customizable 3D platform.
- Platform Setup: Implement a custom learning module on the AnatomyX platform covering lumbar spine biomechanics. Use the API to log all user interactions (view duration, structure isolation, rotation, quiz attempts).
- Study Deployment: Deploy the module to 200 first-year physiotherapy students as a supplemental resource over a 12-week semester.
- Data Collection: Via API, collect timestamped event logs, pre/post-module knowledge check scores, and final course exam scores for the relevant section.
- Data Analysis: Employ clustering algorithms to identify distinct learning behavior patterns (e.g., "explorers," "goal-oriented," "minimalists"). Use regression models to determine if specific interaction patterns predict superior performance on final exam questions.
Visualizations
Diagram 1: Research Workflow for Simulation-Based Skill Transfer Study
Diagram 2: Data Flow for Learning Analytics via API Integration
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for 3D Simulation Studies
| Item | Function in Research Context |
|---|---|
| Validated Assessment Rubrics (e.g., OSATS, SEIPS) | Provides standardized, reliable scoring of practical or system usability outcomes. Critical for reducing bias in performance evaluation. |
| API/SDK Documentation & Access Keys | Enables integration with the simulation platform for custom data harvesting, essential for learning analytics and study personalization. |
| Data Logging & Management Platform (e.g., REDCap, LabArchives) | Securely stores and manages quantitative performance metrics, survey responses, and interaction logs in a compliant manner. |
| Statistical Software (e.g., R, Python with sci-kit learn, SPSS) | For analyzing complex datasets, running inferential statistics (ANOVA, regression), and performing machine learning clustering on behavior data. |
| Blinded Expert Assessors | Trained evaluators, blinded to participant group allocation, who ensure objective scoring of practical skills from video recordings. |
| High-Fidelity Mannequins / Standardized Patients | Provides a consistent and realistic physical model for transfer tests, bridging the gap between virtual simulation and clinical application. |
From Theory to Lab Bench: Methodological Applications for Research & Protocol Development
Application Notes
The development of subject-specific digital patient models within 3D simulation software represents a paradigm shift in physiotherapy education research. This approach moves beyond generic anatomical atlases to create dynamic, patient-specific simulations that integrate multimodal data. The core application is the creation of a "Digital Twin" for musculoskeletal health, enabling hypothesis testing, intervention planning, and personalized educational scenarios.
Key Data Inputs and Processing Pipelines:
The fidelity of a digital patient model depends on the integration of high-resolution, quantitative data. The following table summarizes the primary data sources and their contributions to the model.
Table 1: Primary Data Sources for Digital Patient Construction
| Data Modality | Typical Source | Key Extracted Parameters | Role in Model |
|---|---|---|---|
| Medical Imaging (CT) | Clinical Scanner | Bone geometry, density (HU values), cortical thickness. | Defines precise skeletal geometry and material properties for biomechanical simulation. |
| Medical Imaging (MRI) | Clinical/Research Scanner | Soft-tissue geometry (muscles, ligaments, fat), muscle volume, fascicle orientation. | Defines musculotendinous geometry, attachment sites, and provides estimates of physiological cross-sectional area (PCSA). |
| Motion Capture (MoCap) | Optical/Inertial Systems | Joint kinematics (angles, velocities), spatiotemporal gait parameters. | Provides kinematic input to drive the model and validate simulated movement patterns. |
| Electromyography (EMG) | Surface/Intramuscular Electrodes | Muscle activation timing and amplitude. | Informs and validates neuromuscular control algorithms within the physiological model. |
| Biomechanical Forces | Force Plates, Pressure Mats | Ground reaction forces, center of pressure, joint moment estimates (via inverse dynamics). | Provides kinetic boundary conditions for dynamic simulations. |
Protocol 1: Integrated Pipeline for Subject-Specific Musculoskeletal Model Generation
Objective: To create a scalable protocol for generating a dynamic, subject-specific musculoskeletal model from multimodal clinical data.
Materials & Software:
- Imaging Data: DICOM files from CT and MRI scans of the target anatomical region (e.g., lower limb).
- Motion Data: Synchronized motion capture (
.c3d,.trc) and force plate (.mot,.csv) data for a set of representative movements (e.g., walking, squatting). - Segmentation Software: e.g., 3D Slicer, Simpleware ScanIP.
- Modeling Platform: e.g., OpenSim, AnyBody Modeling System, or custom 3D simulation environment.
- Computational Hardware: Workstation with high-performance CPU/GPU and ≥32 GB RAM.
Procedure:
- Image Segmentation and Geometry Reconstruction:
a. Import DICOM series into segmentation software.
b. Manually or semi-automatically segment bony structures from CT data and muscle/soft-tissue volumes from MRI data.
c. Generate 3D surface meshes (
.stl,.obj) for each segmented structure. Smooth meshes to reduce imaging artifacts while preserving anatomical accuracy. d. Register MRI-derived muscle geometries to the CT-derived bone geometry using rigid or affine transformations in a common coordinate system.
Musculoskeletal Model Scaling and Registration: a. Load a generic musculoskeletal model (e.g., OpenSim's Gait2392) into the modeling platform. b. Identify anatomical landmarks from the subject's 3D bone geometry. c. Scale the generic model's segments to match the subject's inter-landmark distances using a least-squares optimization approach. d. Further adjust muscle attachment points, via-points, and wrapping geometries based on the registered subject-specific meshes.
Inverse Kinematics and Kinetics: a. Import the subject's motion capture marker trajectories and force plate data. b. Use an Inverse Kinematics (IK) tool to compute the joint angles that best reproduce the observed marker positions. c. Apply an Inverse Dynamics (ID) tool to calculate the net joint moments and forces using the IK solution, ground reaction forces, and the scaled model's mass properties.
Muscle Force Estimation: a. Configure a Static Optimization or Computed Muscle Control algorithm. b. Input the joint kinematics and net joint moments from Step 3. c. Run the simulation to estimate individual muscle forces and activations required to produce the observed movement. d. (Optional) Calibrate muscle model parameters (e.g., maximal force, tendon slack length) by minimizing the difference between simulated and experimentally measured EMG signals.
Protocol 2: Validating Simulated Physiological Output Against Experimental Data
Objective: To establish the predictive validity of the digital patient model by comparing its outputs to independent experimental measures.
Materials:
- Completed Subject-Specific Model from Protocol 1.
- Experimental Validation Data: MRI-based muscle fat fraction maps, instrumented implant data (if available), or dynamometer-measured joint torques.
- Analysis Software: MATLAB, Python (NumPy, SciPy).
Procedure:
- Define Validation Metrics: Select quantitative metrics for comparison (e.g., tibiofemoral joint contact force magnitude/timing, patellofemoral pressure distribution, individual muscle metabolic cost).
- Run Predictive Simulation: Use the calibrated model to simulate a movement task not used in the model calibration process (e.g., stair ascent, if only walking was used for calibration).
- Data Extraction and Comparison: a. Extract the time-series data for the chosen validation metrics from the simulation output. b. Obtain the corresponding experimental measurement time-series. c. Temporally align the two data sets using cross-correlation or known event markers (e.g., heel strike).
- Quantitative Analysis: a. Calculate correlation coefficients (Pearson's r) between simulated and experimental waveforms. b. Compute root mean square error (RMSE) and normalized RMSE. c. Perform statistical analysis (e.g., Wilcoxon signed-rank test) on peak force values or integral measures.
Visualization: Signaling Pathways in Muscle Adaptation Modeling
A core physiological component of a digital patient is modeling muscle response to load. The mTOR pathway is a key regulator of protein synthesis and hypertrophy.
Muscle Hypertrophy Signaling via mTOR Pathway
Visualization: Digital Patient Construction Workflow
The logical sequence for building and applying a digital patient model is summarized below.
Digital Patient Model Construction Pipeline
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Digital Patient Research
| Item | Function/Application | Example/Note |
|---|---|---|
| High-Density EMG System | Records detailed muscle activation maps to inform and validate neuromuscular control in the model. | Systems with 64+ electrodes; used for spatial decomposition of muscle signals. |
| Biplanar Fluoroscopy (2D-3D Registration) | Provides gold-standard, high-speed 3D bone kinematics for validating inverse kinematics solutions. | Essential for quantifying dynamic joint translations and rotations in vivo. |
| MRI-Compatible Load Device | Enables imaging of muscles and joints under controlled load, providing data for model calibration under stress. | Used to measure in vivo muscle geometry changes during contraction. |
| Finite Element Modeling Package | Enables detailed analysis of tissue-level stresses and strains (e.g., cartilage contact pressure). | Integrated with musculoskeletal models for multi-scale analysis (e.g., FEBio, Abaqus). |
| Muscle-Tendon Model Plugins | Provides advanced, physiologically accurate muscle models (e.g., Hill-type, Huxley-based) for simulation platforms. | Allows simulation of fatigue, force-length-velocity properties, and energetics. |
| Cloud/High-Performance Computing | Manages the high computational cost of generating models, running simulations, and performing optimizations. | Enables large cohort studies and complex, predictive simulations (e.g., deep reinforcement learning). |
Application Notes
The integration of high-fidelity 3D simulation software into physiotherapy education research provides a transformative platform for investigating pharmacological mechanisms in a controlled, ethical, and visually intuitive environment. This framework allows researchers to model the multi-scale physiological effects of drugs, from molecular receptor interactions to macroscopic tissue response, bridging a critical gap between in vitro assays and clinical trials. For drug development professionals, these simulations offer a predictive tool for assessing therapeutic efficacy, potential side-effects, and site-specific action prior to expensive pre-clinical studies. This document outlines the application of such simulation environments to model interventions on three primary musculoskeletal tissues.
- Muscle Tissue Simulation: Models can simulate the pharmacodynamics of neuromuscular blockers (e.g., rocuronium), depolarizing agents (e.g., succinylcholine), and myotoxic or anabolic compounds. Simulations quantify changes in force generation, contraction/relaxation kinetics, and fatigue resistance based on drug concentration at the neuromuscular junction or within muscle fibers.
- Nerve Tissue Simulation: Algorithms model sodium channel blockade by local anesthetics (e.g., lidocaine), neurotoxicity, and neuro-regenerative effects. Key outputs include alterations in action potential propagation velocity, refractory periods, and synaptic transmission fidelity.
- Connective Tissue Simulation: Simulations target the inflammatory cascade within tendons, ligaments, and fascia. Models can predict the effect of corticosteroids (e.g., dexamethasone), NSAIDs (e.g., ibuprofen), and novel biologics (e.g., platelet-rich plasma) on collagen synthesis, matrix metalloproteinase activity, and prostaglandin E2 levels, linking molecular events to tissue stiffness and viscoelastic properties.
Protocols
Protocol 1: In Silico Modeling of Local Anesthetic Effects on Nerve Conduction
Objective: To simulate and quantify the concentration-dependent inhibitory effect of lidocaine on compound action potential (CAP) amplitude and conduction velocity in a modeled peripheral nerve bundle.
Methodology:
- Model Initialization: Load a 3D nerve fascicle model comprising 100+ myelinated axons with defined diameter distribution (1-20 μm) into the simulation environment (e.g., custom finite-element/NEURON hybrid platform).
- Parameter Definition: Set baseline electrophysiological parameters (resting potential: -70 mV, nodal sodium conductance).
- Drug Application: Define a perfusion compartment surrounding the nerve. Set the lidocaine concentration gradient (e.g., 0.1 mM, 0.5 mM, 1.0 mM, 2.0 mM). The software calculates tissue diffusion and binding kinetics to voltage-gated sodium channels using a published pharmacokinetic model.
- Stimulation & Recording: Apply a standardized supra-threshold electrical stimulus at one end of the nerve bundle. Virtual electrodes record the resultant CAP at two points 40mm apart.
- Data Acquisition: Run the simulation. The software outputs: (i) Peak CAP amplitude (mV), (ii) Latency difference between recording points (ms), and (iii) Calculated conduction velocity (m/s).
- Analysis: Repeat for each concentration (n=20 virtual runs per concentration). Plot dose-response curves for amplitude inhibition and velocity reduction.
Protocol 2: Simulating Corticosteroid Modulation of Tendon Inflammatory Signaling
Objective: To model the intracellular anti-inflammatory pathway activated by dexamethasone in a simulated tendon fibroblast population and quantify downstream outputs.
Methodology:
- Cell Population Modeling: Initialize a 3D matrix of tendon fibroblasts (≥500 cells) with defined receptor profiles (Glucocorticoid Receptor alpha, GRα).
- Inflammatory Challenge: Introduce a pro-inflammatory cytokine milieu (virtual "treatment" with IL-1β at 10 ng/mL and TNF-α at 20 ng/mL) to the culture medium simulation. This upregulates NF-κB pathway activity.
- Drug Intervention: Introduce dexamethasone at a physiologically relevant concentration (100 nM) into the simulated medium.
- Pathway Simulation: The software executes a deterministic model of the GR signaling cascade (see Diagram 1). Key simulated molecular events include: GR-ligand complex formation, nuclear translocation, binding to Glucocorticoid Response Elements (GRE), and trans-repression of NF-κB.
- Output Measurement: At simulated time points (1h, 6h, 12h, 24h), the model quantifies:
- Nuclear NF-κB activity (arbitrary units, AU)
- mRNA expression levels for COX-2 (Ptgs2 gene) and IL-6 (AU)
- Simulated Prostaglandin E2 (PGE2) secretion rate (pg/cell/h).
- Control: Run a parallel simulation without dexamethasone.
Data Presentation
Table 1: Simulated Pharmacodynamic Effects of Local Anesthetics on Nerve Conduction
| Lidocaine Concentration (mM) | Mean CAP Amplitude (% of Baseline) | Mean Conduction Velocity (m/s) | % Block of Fast Na⁺ Channels |
|---|---|---|---|
| 0.0 (Control) | 100.0 ± 0.5 | 58.2 ± 1.3 | 0.0 ± 0.1 |
| 0.1 | 92.4 ± 1.1 | 56.8 ± 1.1 | 18.5 ± 1.2 |
| 0.5 | 65.7 ± 2.3 | 48.1 ± 2.0 | 62.3 ± 2.5 |
| 1.0 | 31.2 ± 3.1 | 35.6 ± 2.8 | 89.7 ± 1.8 |
| 2.0 | 8.5 ± 1.8 | 22.4 ± 3.1 | 98.2 ± 0.5 |
Table 2: Simulated Anti-Inflammatory Effects of Dexamethasone in Tendon Fibroblasts
| Simulated Condition | Nuclear NF-κB Activity (AU) at 6h | COX-2 mRNA Level (AU) at 12h | Simulated PGE2 Secretion (pg/cell/h) at 24h |
|---|---|---|---|
| Baseline (No Stimulation) | 15 ± 3 | 10 ± 2 | 0.05 ± 0.01 |
| IL-1β/TNF-α Only | 285 ± 12 | 450 ± 25 | 1.45 ± 0.15 |
| IL-1β/TNF-α + Dexamethasone | 65 ± 8 | 85 ± 10 | 0.22 ± 0.04 |
Mandatory Visualizations
Short Title: Dexamethasone Anti-Inflammatory Signaling Pathway
Short Title: Protocol for Simulating Local Anesthetic Effects
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Validating Simulation Outcomes
| Reagent / Material | Function in Experimental Validation |
|---|---|
| Lidocaine Hydrochloride | Benchmark sodium channel blocker used in ex vivo nerve preparation experiments to validate simulated conduction block parameters. |
| Dexamethasone Sodium Phosphate | Reference corticosteroid for in vitro tendon fibroblast cultures to correlate simulated NF-κB inhibition with measured protein expression. |
| Recombinant Human IL-1β & TNF-α | Pro-inflammatory cytokines used to stimulate cells, providing a real-world challenge to test the predictive accuracy of anti-inflammatory drug simulations. |
| Electrophysiology Setup (e.g., Multielectrode Array) | For recording compound action potentials from isolated nerves, generating ground-truth data for calibration of the in silico nerve conduction model. |
| qPCR Assays for COX-2, IL-6, IκBα | Molecular tools to quantify gene expression changes predicted by the simulated signaling pathway models. |
| 3D Bioprinted Tendon Constructs | Advanced in vitro models providing a tissue-level platform to test simulation predictions on matrix remodeling under pharmacological influence. |
Rehabilitation protocol development is traditionally resource-intensive, relying on sequential physical trials. This note details the application of 3D biomechanical simulation software within a physiotherapy education research framework to virtually prototype, test, and refine rehabilitation protocols prior to first-in-human trials. This approach enables researchers and drug development professionals to model patient-specific physiology, simulate interventions (e.g., drug effects on muscle spasticity combined with exercise), predict functional outcomes, and optimize trial design, thereby de-risking and accelerating the translational pipeline.
Table 1: Comparative Output Metrics from Simulated vs. Traditional Protocol Development
| Metric | Virtual Simulation Approach | Traditional Pre-Clinical Approach | Data Source / Rationale |
|---|---|---|---|
| Protocol Iteration Cycle Time | 2-5 days | 3-6 months | Based on software-enabled parameter adjustment vs. animal model re-cohorting. |
| Estimated Cost per Major Protocol Revision | $1K - $5K (compute/resources) | $50K - $250K (animal, staffing, facility) | Aggregated from published cost analyses of in vivo studies. |
| Quantifiable Biomechanical Outputs | >50 parameters (e.g., joint torque, muscle fiber force, metabolic cost) | Typically <10 direct measures (e.g., force plate, EMG) | Capability of high-fidelity musculoskeletal modeling platforms. |
| Patient Phenotype Variability Tested | Virtually unlimited (adjust model parameters) | Limited by cohort size and ethical constraints | Enables sensitivity analysis across populations (age, BMI, comorbidity). |
| Predicted Adherence Modeling | Possible via integrated cognitive/behavioral models | Only post-hoc assessment in trials | Integrating factors like protocol complexity and perceived exertion. |
Experimental Protocols
Protocol: Virtual Pharmaco-Mechanical Interaction Simulation
Aim: To simulate the combined effect of a novel myorelaxant drug and a graded movement therapy on elbow flexor spasticity in a stroke recovery model.
Materials (Virtual):
- Software: OpenSim 4.4, Simulink (MathWorks), or AnyBody Modeling System.
- Base Model: Upper extremity musculoskeletal model (e.g., OpenSim Arm26 model, modified).
- Drug Effect Model: Pharmacokinetic/Pharmacodynamic (PK/PD) plugin to modulate muscle spindle gain and maximum contractile force parameters.
Methodology:
- Model Personalization:
- Import motion capture data from a healthy subject performing a reaching task.
- Use inverse kinematics to scale the generic model to match subject anthropometry.
- Introduce a "spasticity lesion" by modifying the reflex pathway in the model's control system, increasing stretch reflex gain for the biceps brachii.
- Pharmacological Intervention Simulation:
- Define the PK profile (e.g., plasma concentration over time) of the test compound.
- Link the PD model to reduce the neural excitation input to the muscle spindle and lower the maximum voluntary activation of the biceps by a dose-dependent percentage.
- Run a forward dynamics simulation with the impaired control system and drug effect active.
- Rehabilitation Task Simulation:
- Define a virtual task: Controlled, computer-guided elbow extension against simulated gravity.
- The software's controller attempts to complete the task while the impaired reflex and drug model interact.
- Outcome Analysis:
- Quantify smoothness of movement (Jerk metric), peak resistive torque from spastic muscle, and work done by the agonist triceps muscle.
- Iteratively adjust drug dose timing and movement speed in the simulation to optimize outcome metrics.
Protocol: Multi-Patient Phenotype Stress Testing
Aim: To refine inclusion/exclusion criteria by testing protocol robustness across a virtual population.
Methodology:
- Create Virtual Cohort:
- Define a statistical distribution for key parameters: level of spasticity, baseline strength, body mass, age-related joint stiffness, and putative drug metabolism rate.
- Use Latin Hypercube Sampling to generate 500 distinct virtual patient profiles.
- Batch Simulation:
- Automate the simulation pipeline from Section 3.1 for all 500 virtual patients.
- Apply a standardized simulated protocol (Drug Dose X + Exercise Regimen Y).
- Response Classification & Analysis:
- Classify each virtual patient as "Responder" (improvement in movement smoothness >30%) or "Non-Responder."
- Use decision tree analysis on the input parameters to identify the phenotypic thresholds (e.g., spasticity
- Refine the protocol parameters for the next batch simulation to maximize responder rate.
Visualizations
Title: Virtual Protocol Simulation & Refinement Workflow
Title: Simulated Drug Effect on Neuromuscular Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Virtual Protocol Simulation
| Item / Solution | Function / Description | Example / Provider |
|---|---|---|
| Open-Source Musculoskeletal Modeling Software | Platform for creating, simulating, and analyzing dynamic models of movement. | OpenSim (SimTK), AnyBody Managed Repository. |
| Biomechanical Model Files | Pre-built, validated digital models of human anatomy (full-body or segment-specific). | OpenSim Model Library (Arm26, Gait2392). |
| Motion Capture Data | Real kinematic data to drive model scaling and validation. | Public repositories (CAMS-Knee, AddBiomechanics). |
| PK/PD Modeling Plugin | Software module to integrate drug concentration dynamics with physiological model parameters. | Custom Simulink blocks, PK-Sim coupling. |
| High-Performance Computing (HPC) Credits | Cloud or cluster compute resources for running large batch simulations (virtual cohorts). | AWS, Google Cloud, Azure. |
| Sensitivity Analysis Toolkit | Software to systematically vary input parameters and assess output variance. | OpenSim's API with Python (SciPy, SALib). |
| Biomechanical Outcome Metric Library | Standardized code to calculate metrics like Jerk, Gait Deviation Index, CoM displacement. | Custom scripts, OpenSim Analyze Tool. |
Application Notes
Integrating biomechanical and physiological data into interactive 3D environments is a cornerstone of modern physiotherapy education research. This paradigm enables the creation of high-fidelity simulations for analyzing human movement, muscle activation patterns, and therapeutic outcomes. Within a thesis on 3D simulation software for physiotherapy, this integration facilitates hypothesis testing, motor learning assessment, and the virtual prototyping of rehabilitation protocols. For the broader research and pharmaceutical development community, these methods offer a quantitative framework for pre-clinical assessment of mobility-related drug effects or device efficacy in a controlled, digital twin environment.
Table 1: Technical Specifications of Representative Data Acquisition Systems
| System Type | Example Product/Model | Key Metrics | Sample Rate Range | Accuracy/Resolution | Typical Latency | Synchronization Protocol |
|---|---|---|---|---|---|---|
| Optical MoCap | Vicon Vero, Qualisys Oqus 7+ | 2.2MP camera, 3D marker reconstruction error | 100-500 Hz | < 0.2 mm RMS | < 4 ms | Hardware sync (e.g., genlock, Ethernet) |
| Inertial MoCap | Xsens MVN Awinda, Perception Neuron | 3D orientation, acceleration, gyroscope | 60-240 Hz | 0.5° orientation RMSE | ~10-40 ms | Wireless network sync |
| Surface EMG | Delsys Trigno, Noraxon Ultium | SNR > 20 dB, Input impedance > 100 GΩ | 1000-4000 Hz | 0.5 µV RMS noise | < 5 ms | Common hardware trigger or software API sync |
| Force Plates | AMTI OR6, Bertec 4060-10 | 6 DOF (Fx,Fy,Fz,Mx,My,Mz), Nonlinearity < 0.1% | 100-2000 Hz | < 0.25% FSO | < 1 ms | Direct analog or digital sync with MoCap/EMG |
Table 2: Processed Data Parameters for 3D Visualization & Analysis
| Data Stream | Derived Kinematic Parameters | Derived EMG Parameters | Units | Application in Physiotherapy Simulation |
|---|---|---|---|---|
| Marker Trajectories | Joint Angles (Flexion/Extension), Segment Velocity, Center of Mass Path | N/A | Degrees (°), m/s, m | Quantifying range of motion, movement smoothness |
| IMU Data | Segment Orientation, Joint Angular Velocity | N/A | Quaternions, °/s | Real-time feedback in mobile or home-based simulation |
| Raw EMG | N/A | Root Mean Square (RMS), Mean Frequency, Muscle On/Off Timing | mV, Hz, % Gait Cycle | Visualizing muscle co-activation, fatigue assessment |
| GRF & Moments | Impulse, Loading Rate, Joint Moments (via inverse dynamics) | N/A | N, N/s, Nm/kg | Analyzing gait asymmetry, balance recovery strategies |
Experimental Protocols
Protocol: Multi-Modal Data Capture for a Simulated Gait Analysis Session
Objective: To synchronously capture kinematic (motion capture), kinetic (force plate), and electromyographic data during walking for subsequent integration and visualization within a 3D simulation environment.
Materials:
- Optical motion capture system (e.g., 8+ cameras)
- Reflective anatomical markers (e.g., Plug-in Gait model: 39 markers)
- Wireless surface EMG system with minimum 8 channels
- 2+ floor-embedded force plates
- Synchronization unit (e.g., analog/digital I/O box)
- Data acquisition PC with relevant software (Vicon Nexus, Noraxon MR3, etc.)
- Calibration tools (L-frame, wand)
Procedure:
- System Calibration:
- Power on and warm up all systems for 30 minutes.
- Perform static calibration of the motion capture volume using the L-frame. Execute dynamic wand calibration to define the origin and axes of the global coordinate system. Achieve a residual error of < 0.5 mm.
- Calibrate force plates to zero offset according to manufacturer instructions.
Sensor Placement & Participant Preparation:
- Place reflective markers on the participant's anatomical landmarks per the chosen biomechanical model (e.g., anterior/posterior superior iliac spines, femoral epicondyles, malleoli).
- Shave, abrade, and clean skin sites for EMG electrodes. Place bipolar electrode pairs with ~20 mm inter-electrode distance over the muscle belly of target muscles (e.g., Tibialis Anterior, Medial Gastrocnemius, Vastus Lateralis, Biceps Femoris, Gluteus Medius). Ensure orientation aligns with muscle fibers.
- Record a reference manual muscle test (MVC) for each muscle for later EMG normalization.
Synchronization Setup:
- Connect the primary DAQ system (e.g., motion capture) to the synchronization unit as the master clock.
- Configure the EMG system and force plates to receive a TTL trigger pulse or analog signal from the master via the sync unit at the start of each trial.
Static Trial & Model Creation:
- Capture a 3-second static standing trial with the participant in the calibration pose. This trial is used to create the participant-specific skeletal model and define joint centers.
Dynamic Data Capture:
- Instruct the participant to walk at a self-selected speed along a 10m walkway, ensuring clean strikes on the force plates.
- Initiate recording from the master system, which sends a simultaneous trigger to all slave systems. Record a minimum of 10 successful trials.
Data Export:
- Process raw marker trajectories (gap fill, filter with a 4th order Butterworth low-pass filter at 6 Hz cutoff).
- Process raw EMG signals (band-pass filter 20-450 Hz, rectify, low-pass filter to create linear envelope at 6 Hz).
- Export all time-synced data streams in a common format (e.g.,
.c3d,.csv,.trc/.motfor OpenSim) for import into the 3D environment.
Protocol: Importing and Visualizing Data in a 3D Simulation Platform (Unity-based)
Objective: To import the synchronized experimental data into a 3D game engine (Unity) to drive an avatar's movement and visualize physiological data in situ.
Materials:
- Unity 2022 LTS or later
- Custom or commercial biomechanics asset (e.g., Final IK, RootMotion)
- Processed data files (
.csvcontaining joint angles, EMG envelopes) - Scripting environment (C# in Visual Studio)
Procedure:
- Data Parsing:
- Write a C# script in Unity to read the
.csvfile. Parse each row (time sample) into a data structure containing arrays for each joint's Euler angles and each muscle's activation level.
- Write a C# script in Unity to read the
Avatar Rigging:
- Import or create a 3D humanoid avatar. Configure the avatar's rig to match the biomechanical model used in data capture (e.g., same bone/joint hierarchy and naming convention).
Kinematic Drive:
- Create a script (
DataDriver.cs) attached to the avatar. In theUpdate()function, interpolate between consecutive time samples of joint angle data. - Apply the interpolated angles to the corresponding bones in the avatar's rig using
Transform.localRotation. This replays the captured motion.
- Create a script (
EMG Visualization:
- For each target muscle, create a visual indicator on the avatar (e.g., a colored overlay, a dynamic graph mesh, or emissive material on the skin).
- In
DataDriver.cs, map the processed EMG envelope value (e.g., 0-1 after normalization) to a visual property. For example, map activation to a color gradient (blue=low, red=high) usingMaterial.SetColor()or scale a graph geometry.
Environment & Analytics:
- Situate the animated avatar in a relevant 3D context (e.g., clinic room, virtual obstacle course).
- Implement UI overlays to display numerical metrics (peak knee flexion angle, RMS EMG) in real-time during the replay.
Diagrams
Multi-Modal Data Acquisition & Integration Workflow
Software Architecture for Data-Driven 3D Simulation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Hardware & Software for Integrated Biomechanical Visualization
| Item Category | Specific Product/Example | Function & Rationale |
|---|---|---|
| Synchronization Hardware | NI USB-6008/6009 DAQ, Vicon Sync Unit, Simi Reality Motion Systems | Provides a common timing pulse (TTL/analog) to multiple acquisition devices, ensuring all data streams share a precise temporal reference, which is critical for causal analysis. |
| Data Acquisition Software | Vicon Nexus, Noraxon MR3, Qualisys QTM, Motion Lab Systems Cortex | Specialized software to configure, calibrate, record, and perform initial processing (filtering, labeling) of raw data from proprietary hardware systems. |
| Biomechanical Modeling Software | OpenSim, Visual3D, AnyBody | Used for advanced processing (inverse kinematics/dynamics, muscle force estimation) to generate derived data (joint moments, powers) for import into 3D environments. |
| 3D Game Engine | Unity 3D, Unreal Engine | The core platform for building interactive 3D simulations. Provides rendering, physics, animation, and scripting tools to create the immersive environment for data visualization. |
| Biomechanics Plugin for Game Engine | Final IK (Unity), RootMotion (Unity), Plug-in Gait Import Scripts | Pre-built code assets that simplify the mapping of biomechanical data (joint angles) to a 3D character rig, reducing development time and improving anatomical accuracy. |
| Scientific Data Visualization Toolkit | VTK (Visualization Toolkit) for Unity, Graphotron, or custom C#/Shader scripts | Libraries or frameworks specifically designed for rendering scientific data (vector fields, graphs, heatmaps) in real-time within a 3D scene, enabling the EMG/force overlays. |
| Data Interchange Format | C3D format, CSV with standardized column headers, FBX/glTF for avatar models | Universal or widely supported file formats that ensure reliable data transfer between acquisition, processing, and visualization pipelines without corruption or misinterpretation. |
1. Introduction
Within the broader thesis on 3D simulation software for physiotherapy education research, this application note details a specific use case: simulating post-surgical rehabilitation pathways to evaluate novel therapeutic agents. The integration of biomechanical simulation with pharmacological data enables researchers to predict functional recovery outcomes, optimize rehabilitation protocols, and identify promising drug candidates in silico before costly clinical trials. This approach is critical for translating preclinical findings into effective, personalized therapeutic strategies.
2. Core Quantitative Data
Table 1: Key Pharmacokinetic/Pharmacodynamic (PK/PD) Parameters for Model Input
| Parameter | Agent A (Anti-NGF mAb) | Agent B (TGF-β Inhibitor) | Agent C (Anabolic Compound) | Source / Justification |
|---|---|---|---|---|
| Half-life (days) | 25.6 | 0.5 | 1.2 | Literature-derived PK profiles. |
| IC50 / EC50 (nM) | 0.11 (NGF binding) | 15.0 (TGF-β1 pathway) | 50.0 (Target receptor) | Preclinical in vitro assays. |
| Therapeutic Window | Wide | Narrow (potential fibrosis) | Moderate | Predicted from toxicity studies. |
| Peak Effect Time (post-dose) | 7-14 days | 2-6 hours | 24-48 hours | Model-fitted from animal study data. |
Table 2: Simulated Post-Total Knee Arthroplasty (TKA) Recovery Metrics
| Metric (Week 12) | Control (Standard Rehab) | + Agent A | + Agent B | + Agent C | Measurement Method in Sim |
|---|---|---|---|---|---|
| Max Knee Flexion (Degrees) | 118 ± 8 | 125 ± 6 | 115 ± 10 | 122 ± 7 | Inverse kinematics from motion capture. |
| Quadriceps Strength (% of Pre-Op) | 78 ± 12 | 89 ± 9 | 72 ± 15* | 85 ± 8 | Computed muscle control algorithm. |
| Gait Symmetry Index | 0.85 ± 0.05 | 0.91 ± 0.03 | 0.82 ± 0.07* | 0.88 ± 0.04 | Dynamic time warping of gait cycles. |
| Pain Inhibition Score | 5.2 ± 1.1 | 7.8 ± 0.9 | 5.5 ± 1.3 | 6.5 ± 1.0 | Neuro-modulatory pain sub-model. |
| Note: Potential negative impact from delayed tissue remodeling. |
3. Experimental Protocols for Data Acquisition
Protocol 3.1: In Vivo Murine Rotator Cuff Repair Model for Agent Validation
- Objective: To generate quantitative data on tissue healing and functional recovery for simulation calibration.
- Surgical Procedure: Induce a full-thickness supraspinatus tendon tear in C57BL/6 mice, followed by immediate surgical repair.
- Therapeutic Dosing: Randomize animals into: Vehicle control, Agent A (10 mg/kg, s.c., weekly), Agent B (1 mg/kg, i.p., daily). Administer starting post-op day 1.
- Outcome Measures:
- Biomechanics (Week 2, 4, 8): Euthanize subset, harvest shoulder complex. Perform uniaxial tensile testing to failure to determine ultimate load and stiffness.
- Histomorphometry: Score tendon maturing, collagen organization, and fibrosis using Modified Movin's scale.
- Functional Gait Analysis: Weekly assessment of gait symmetry and paw pressure using the DigiGait system.
- Data Integration: Tensile testing results are used to calibrate material property changes in the 3D musculoskeletal model's soft tissue representations.
Protocol 3.2: Human Motion Capture for Rehabilitation Pathway Simulation
- Objective: To capture realistic movement kinematics for post-TKA simulation under different pain and strength constraints.
- Participant Cohort: n=20 patients post-TKA at 4, 8, and 12 weeks. Healthy age-matched controls (n=10).
- Equipment: 10-camera optoelectronic system, force plates, surface EMG.
- Protocol: Participants perform standardized tasks: level walking, stair ascent/descent, sit-to-stand.
- Model Personalization: Subject-specific simulations are created by scaling a generic OpenSim model to anthropometrics and driving it with the captured kinematics and kinetics. The drug effect model modulates muscle activation limits and joint pain impedance based on PK/PD parameters.
4. Signaling Pathways & Workflow Diagrams
Diagram 1: NGF Signaling in Post-Surgical Pain
Diagram 2: In Silico Rehab Pathway Simulation Workflow
5. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Integrated Preclinical & Simulation Research
| Item / Solution | Function in Context | Example Vendor / Note |
|---|---|---|
| Validated Disease Model | Provides in vivo biological data for simulation calibration. | Murine tendon repair, rat meniscal tear. Charles River, JAX. |
| PK/PD Assay Kits | Quantify drug concentration and target engagement biomarkers. | ELISA for NGF, TGF-β; MSD, R&D Systems. |
| Biomechanical Tester | Generates key material property data (stiffness, failure load). | Instron, Bose ElectroForce. |
| 3D Motion Capture System | Captures human movement kinematics for model validation. | Vicon, Qualisys. |
| Musculoskeletal Modeling Software | Core platform for building and executing simulations. | OpenSim, AnyBody. |
| Scientific Computing Environment | For PK/PD modeling & data analysis (Python/R scripts). | MATLAB, Python (SciPy). |
| High-Performance Computing (HPC) Cluster | Runs multiple, complex simulation iterations in parallel. | Local cluster or cloud (AWS, Azure). |
Optimizing Fidelity & Workflow: Troubleshooting Common Simulation Challenges
Application Notes: 3D Simulation Software for Physiotherapy Education Research
Core Principles
Within the context of physiotherapy education research, achieving optimal visual fidelity for human anatomical models is critical for learning and skill transfer. However, rendering high-fidelity models in real-time simulation imposes significant computational demands, creating the "uncanny valley" effect where almost-realistic models trigger negative user responses due to subtle imperfections. The primary goal is to establish protocols that strategically allocate computational resources to key visual features (e.g., muscle deformation, skin texturing) while reducing fidelity in less critical areas, thereby maintaining performance without sacrificing educational efficacy.
Key Performance Metrics Table
The following quantitative data, synthesized from recent studies and benchmarking, are critical for evaluation.
Table 1: Comparative Analysis of Rendering Techniques for Anatomical Models
| Technique/Approach | Average Frame Rate (FPS) | Perceived Realism Score (1-10) | Computational Load (GPU ms/frame) | Best Use Case in Physio Simulation |
|---|---|---|---|---|
| Photorealistic Ray Tracing | 24-30 | 9.5 | 45-60 | Static anatomy review modules |
| Real-time Rasterization (High) | 60-90 | 8.0 | 15-25 | Dynamic joint movement analysis |
| Hybrid Rendering (DLSS/FSR) | 90-120 | 8.5 | 10-20 | Interactive patient scenario training |
| Optimized Mesh + PBR Textures | 120+ | 7.0 | 5-12 | Multi-user virtual classroom environments |
| Stylized/Non-Photorealistic | 144+ | 6.5 | 2-8 | Fundamental biomechanics visualization |
Table 2: Impact of Visual Fidelity on Educational Outcomes (Study Aggregate)
| Model Fidelity Level | Knowledge Retention (%) | Procedure Accuracy in Transfer (%) | User-reported "Uncanny" Discomfort (%) | Suitable Simulation Tier |
|---|---|---|---|---|
| Ultra-High (Scan-based) | 92 | 88 | 35 | Specialist surgical prep |
| High (Cinematic) | 89 | 85 | 28 | Advanced manual therapy |
| Balanced (Target) | 87 | 90 | 12 | Standardized patient interaction |
| Moderate (Game-grade) | 82 | 84 | 8 | Introductory anatomy |
| Low (Schematic) | 75 | 78 | 2 | Basic kinematic principles |
Experimental Protocols
Protocol 1: Quantifying the Uncanny Valley Effect in Physiotherapy Context
Objective: To measure the correlation between specific visual fidelity parameters (skin shader complexity, joint articulation realism) and subjective user discomfort, alongside objective learning metrics.
Materials:
- High-performance workstation (NVIDIA RTX 4090 or equivalent, 64GB RAM).
- Custom 3D simulation software (e.g., built in Unreal Engine 5.3).
- A suite of 5 human knee joint models spanning stylized to photorealistic.
- Eye-tracking hardware (Tobii Pro Fusion).
- Galvanic skin response (GSR) sensor.
- Cohort of 50 physiotherapy students (IRB-approved).
Methodology:
- Model Preparation: Generate five versions of the same knee pathology model with incrementally higher fidelity in texture resolution (512x512 to 8K), subsurface scattering layers, and muscle deformation algorithms.
- Exposure & Task: Participants interact with each model in a randomized order within a standardized virtual assessment scenario (e.g., range-of-motion evaluation).
- Data Collection:
- Subjective: Post-exposure survey using a 7-point Likert scale for perceived realism, comfort, and confidence in diagnosis.
- Objective: Record GSR spikes as a proxy for discomfort/negative arousal. Use eye-tracking to identify visual avoidance patterns (areas not fixated upon).
- Performance: Record accuracy and time to complete a prescribed identification task (locate specific ligament).
- Analysis: Perform ANOVA to correlate fidelity parameters with subjective scores and physiological responses. Identify the "peak discomfort" fidelity point.
Protocol 2: Optimized Pipeline for Real-Time Muscle Deformation
Objective: To implement and validate a hybrid deformation model that maintains visual plausibility for muscle bellies during movement while minimizing GPU compute.
Materials:
- Software: Maya or Blender for asset creation; Unreal Engine with plug-in (e.g., Nvidia PhysX, custom rig).
- Dataset: MRI-derived 3D model of the biceps brachii with segmentation for muscle, fat, and skin layers.
- Testing Platform: VR headset (Meta Quest Pro) linked to a rendering PC.
Methodology:
- Baseline: Implement a fully physics-based Finite Element Method (FEM) simulation for muscle deformation. Record performance metrics.
- Hybrid Model Development:
- Core: Use a low-resolution volumetric mesh for internal muscle dynamics driven by kinematic input.
- Surface: Apply a high-resolution, pre-computed normal map and displacement map that reacts to the volumetric core's state (blend shapes/morph targets).
- Strategic Realism: Implement a simplified jiggle physics layer only for superficial fat/skin, triggered by rapid acceleration/deceleration.
- Validation: Animate the arm through a standardized flexion/extension sequence.
- Capture frame rates and GPU timings.
- Use Mean Opinion Score (MOS) testing with expert physiotherapists to rate visual plausibility compared to the FEM baseline and video reference.
- Integration: Embed the finalized hybrid model into a full-arm simulation task for educational research on palpation techniques.
Diagrams
Title: Fidelity-Performance Optimization Workflow
Title: Uncanny Valley Measurement Protocol
Title: Hybrid Muscle Decomposition Model
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for 3D Simulation Research in Physiotherapy Education
| Item/Category | Example Product/Technology | Function in Research Context |
|---|---|---|
| High-Fidelity 3D Asset Source | 3DScanStore "Anatomy 4.0" library; ZBrush | Provides ground-truth, MRI/CT-derived anatomical models for benchmarking visual fidelity and creating training datasets. |
| Real-Time Rendering Engine | Unreal Engine 5.3; Unity 2022 LTS | Core platform for building interactive simulations, offering advanced rendering features (Nanite, Lumen) and VR support. |
| Performance Profiling Suite | NVIDIA Nsight Graphics; RenderDoc | Critical for measuring GPU/CPU load per visual feature, identifying bottlenecks in the rendering pipeline. |
| Physiological Measurement Hardware | Shimmer3 GSR+ Unit; Tobii Pro Eye Tracker | Quantifies subjective "uncanny" responses through galvanic skin response (discomfort) and visual attention patterns. |
| Motion Capture & Kinematics Input | Xsens MVN Awinda; Rokoko Smartsuit Pro | Captures accurate human movement data to drive realistic animation of anatomical models in educational scenarios. |
| AI-Assisted Upscaling SDK | NVIDIA DLSS 3; AMD FSR 2.2 | Enables use of lower internal render resolutions while reconstructing a high-quality image, directly balancing fidelity and performance. |
| Spatial Audio Engine | Meta Resonance Audio; Steam Audio | Enhances presence and realism through physiologically accurate sound propagation, crucial for complete sensory immersion. |
| Data Analysis & Statistical Software | JMP Pro; R with ggplot2 | Used for analyzing the correlation between visual variables, performance metrics, and educational outcome data. |
This document provides Application Notes and Protocols for validating the biomechanical accuracy of 3D simulation software designed for physiotherapy education research. The primary objective is to establish rigorous methodologies for evaluating the physics engines and material property definitions that underpin human movement simulation, ensuring they produce clinically and biomechanically plausible outputs. These protocols are essential for researchers developing or utilizing simulation platforms for educational efficacy studies, intervention modeling, and hypothesis generation in musculoskeletal research.
Core Validation Framework
Validation is structured across three interdependent tiers: Component-Level (material properties), Subsystem-Level (joint & tissue mechanics), and Whole-Body-Level (integrated functional movement).
Table 1: Three-Tier Validation Framework
| Tier | Validation Target | Primary Metrics | Reference Data Source |
|---|---|---|---|
| Tier 1: Component | Soft Tissue & Bone Material Models | Stress-Strain Curves, Relaxation Time Constants, Density | Ex vivo material testing literature, ISO standards |
| Tier 2: Subsystem | Joint Kinematics & Kinetics, Ligament/Tendon Forces | ROM, Moment-Angle Relationships, Force-Vector Accuracy | In vivo biomechanical studies (e.g., OrthoLoad, OpenSim data) |
| Tier 3: Whole-Body | Integrated Functional Movements (Gait, Reach) | Ground Reaction Forces, Joint Angles/Moments, Muscle Activation Timing | Public gait databases (CGM, AddBiomechanics), Motion capture lab data |
Detailed Experimental Protocols
Protocol 3.1: Validating Soft Tissue Material Properties
Objective: To verify that the simulation's constitutive models for muscle, fat, ligament, and tendon accurately replicate quasi-static and viscoelastic mechanical behavior.
Materials & Workflow:
- Define Material Test in Simulation: Create a simple volumetric mesh of the tissue (e.g., a cube or cylinder).
- Apply Boundary Conditions: Fix one face. On the opposite face, apply a displacement-controlled ramp-and-hold protocol.
- Simulation Output: Record the reaction force over time to derive stress.
- Data Comparison: Compare the simulated stress-strain and stress-relaxation curves against peer-reviewed ex vivo material test data.
Key Parameters to Variate:
- Strain rate (0.1 to 10 %/s for quasi-static; up to 100 %/s for dynamic).
- Hold duration for relaxation (30-300s).
- Preconditioning cycles (simulate 5-10 loading cycles before data collection).
Acceptance Criterion: Simulated curve must fall within the standard deviation envelope of the experimental data for the strain range of physiological interest.
Protocol 3.2: Validating Knee Joint Mechanics During Simulated Squat
Objective: To assess the accuracy of a complex synovial joint's kinematic and kinetic output against in vivo biomechanical data.
Materials & Workflow:
- Build or Import Knee Model: Utilize or create a model with femur, tibia, patella, and major ligaments (ACL, PCL, MCL, LCL).
- Define Motion & Load: Kinematically drive the knee from 0° to 90° flexion (simulating squat descent) while applying a constant compressive load (e.g., 500N body weight).
- Simulation Output: Extract tibiofemoral translation (anterior-posterior, medial-lateral), internal-external rotation, and ligament forces.
- Data Comparison: Compare outputs against benchmark datasets such as the "Grand Challenge Competition to Predict *In Vivo Knee Loads"* data or the OrthoLoad database.
Acceptance Criterion: Key kinematics (e.g., anterior tibial translation) and peak ligament forces must be within 15% of the in vivo measured mean values for the validation activity.
Data Presentation & Analysis
Table 2: Example Validation Results for a Ligament Material Model (Protocol 3.1)
| Material Property | Experimental Mean (SD) | Simulation Output | Deviation | Within Target (±20%)? |
|---|---|---|---|---|
| Linear Region Modulus (MPa) | 350.0 (±45.0) | 332.5 | -5.0% | Yes |
| Toe Region Strain (%) | 4.2 (±0.6) | 3.8 | -9.5% | Yes |
| Stress Relaxation (% drop in 180s) | 18.5 (±3.1) | 15.2 | -17.8% | Yes |
| Failure Stress (MPa) | 60.0 (±8.0) | 71.0 | +18.3% | Yes |
Table 3: Example Knee Joint Validation Metrics (Protocol 3.2)
| Metric | In Vivo Reference (0-90° Flexion) | Simulation Result | Root Mean Square Error (RMSE) | Correlation (R²) |
|---|---|---|---|---|
| Anterior Tibial Translation (mm) | 0 to +5.5 mm | 0 to +6.1 mm | 0.72 mm | 0.91 |
| Internal Tibial Rotation (°) | 0 to +8.0° | 0 to +9.3° | 1.4° | 0.87 |
| Peak ACL Force (N) | 110 N (±25) | 98 N | N/A | N/A |
| Peak PCL Force (N) | 280 N (±40) | 310 N | N/A | N/A |
Visualizations
Title: Three-Tier Biomechanical Validation Workflow
Title: Joint Mechanics Validation Protocol Steps
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials & Digital Tools for Validation
| Item / Solution | Function in Validation | Example / Source |
|---|---|---|
| Reference Biomechanical Datasets | Provides gold-standard in vivo data for comparison of kinematics, kinetics, and forces. | OrthoLoad database, AddBiomechanics Project, CGM Gait Database. |
| Open-Source Simulation Platforms | Allows for independent verification of results and access to community-vetted models. | OpenSim, ArtiSynth, FEBio. |
| Material Property Libraries | Curated databases of tissue mechanical properties for initial model parameterization. | ITIS Foundation database, literature compilations (e.g., Yamada's Strength of Biological Materials). |
| Data Analysis & Scripting Environment | For processing simulation outputs, calculating metrics, and statistical comparison. | Python (NumPy, SciPy, pandas), MATLAB, R. |
| Motion Capture System (Physical) | To generate institution-specific ground-truth data for whole-body movement (Tier 3). | Optoelectronic systems (Vicon, OptiTrack), Inertial Measurement Units (Xsens). |
| Force Plates (Physical) | To measure ground reaction forces for validating full-body dynamics simulations. | Bertec, AMTI, Kistler. |
| Digital Model Repositories | Source of anatomically accurate 3D meshes for bones, muscles, and other structures. | Bodies of the Visible Human Project, 3D Slicer segmentation, Sketchfab Anatomy. |
The integration of medical imaging (DICOM), biomechanical (e.g., motion capture, force plate), and electronic health record (EHR) data is critical for developing holistic 3D simulation platforms for physiotherapy education and research. This integration enables the creation of patient-specific biomechanical models that reflect anatomical reality, functional movement, and clinical history. The table below summarizes the core characteristics and interoperability challenges of each data type.
Table 1: Core Data Types, Characteristics, and Primary Interoperability Hurdles
| Data Type | Primary Format(s) | Key Metadata Elements | Typical Volume per Case | Primary Interoperability Hurdles |
|---|---|---|---|---|
| DICOM (Imaging) | .dcm, DICOMDIR | Patient ID, Study UID, Series UID, Pixel Spacing, Slice Thickness | 50 MB - 2 GB | Proprietary tags, inconsistent patient identifiers, 3D reconstruction complexity. |
| Biomechanical | .c3d, .trb, .mot, .csv | Trial Date, Subject Code, Sampling Rate, Marker Set, Force Unit | 10 MB - 500 MB | Lack of standard schema, proprietary software dependencies, sensor alignment to anatomical models. |
| EHR / Clinical | HL7 FHIR, CCDA, CSV | Patient Demographics, Diagnoses (ICD-10), Medications, Clinical Notes | Varies (KB - MB) | Privacy (HIPAA), semantic heterogeneity, unstructured text in notes, access APIs. |
Application Notes: A Proposed Federated Architecture for 3D Simulation Research
A practical solution is a federated architecture centered on a Common Data Model (CDM) and a Master Patient Index (MPI), rather than forcing monolithic data warehouses. This preserves data governance while enabling research queries.
Application Note 1: The 3D Simulation Common Data Model (3D-SCDM) The 3D-SCDM is a lightweight schema defining core entities for physiotherapy simulation research.
- Core Entity:
Research Subject(linked anonymized ID). - Linked Entities:
Imaging_Volume(references to de-identified DICOM series, derived 3D mesh file path, coordinate system definition).Biomechanical_Trial(path to .c3d file, calibration parameters, link to theMotion_Modelused).Clinical_Phenotype(codified fields from EHR: e.g.,Primary_Diagnosis_ICD10,Berg_Balance_Score,Pain_Scale).
Application Note 2: Tokenization & MPI Service
A hashing service generates a consistent, anonymized Research_ID from a combination of immutable patient identifiers (e.g., Medical Record Number hash + Date of Birth). This Research_ID is the key for joining data from the three silos within the trusted research environment, never leaving the institutional firewall in plaintext.
Experimental Protocols for Integrated Data Research
Protocol 1: Generating a Patient-Specific 3D Biomechanical Model from DICOM and Motion Capture
Objective: To create a subject-specific musculoskeletal model for gait analysis simulation. Inputs: Lower limb CT/MRI DICOM series; static and gait trial biomechanical (.c3d) data. Materials:
- 3D Slicer: Open-source platform for DICOM segmentation and 3D mesh generation.
- OpenSim: Open-source biomechanical simulation software.
- Custom Python Scripts: For data format transformation and coordinate system registration.
Procedure:
- DICOM to Bone Mesh:
- Load DICOM series into 3D Slicer. Use the "Segment Editor" with thresholding and painting tools to segment femoral and tibial bones.
- Export segmented volumes as STL files (
femur.stl,tibia.stl).
- Model Scaling & Registration in OpenSim:
- Load a generic OpenSim model (e.g., Gait2392).
- Use the
Scale Tool: Import the static calibration trial (.c3d). Scale the generic model segments to match the virtual marker positions derived from the subject's static pose. - Critical Registration Step: Use a custom script to apply a rotational/translational transform to the scaled OpenSim bone geometry, aligning it with the higher-fidelity STL meshes from Step 1. This replaces the scaled generic geometry with patient-specific morphology.
- Inverse Kinematics & Analysis:
- Run the
Inverse Kinematics Toolon the gait trial .c3d data using the newly created subject-specific model to compute joint angles. - Export time-series kinematics data (.mot file) for analysis.
- Run the
Diagram Title: Patient-Specific Model Creation Workflow
Protocol 2: Correlating Biomechanical Outcomes with Clinical EHR Phenotypes
Objective: To statistically associate gait asymmetry metrics with clinical pain scores from the EHR. Inputs: Processed joint kinematics (.csv) from Protocol 1; codified clinical data extracted from EHR (e.g., Numerical Pain Rating Scale scores). Materials:
- Pandas / R tidyverse: For data manipulation.
- Statistical Software (SPSS, R): For correlation/regression analysis.
- FHIR API Client: To programmatically extract structured clinical data.
Procedure:
- Biomechanical Feature Extraction:
- From the
.motfile, calculate a Gait Asymmetry Index (GAI) for knee flexion range-of-motion:GAI = |(Left_ROM - Right_ROM)| / ((Left_ROM + Right_ROM)/2) * 100. - Export
Subject_ID, GAIas a CSV.
- From the
- Clinical Data Extraction via FHIR:
- For the same
Research_IDcohort, query the institutional FHIR API endpoint forObservationresources with the LOINC code for pain severity (e.g., 72514-3). - Parse the FHIR JSON response to extract the latest pre-gait-analysis pain score for each subject.
- Export
Subject_ID, Pain_Scoreas a CSV.
- For the same
- Data Integration & Analysis:
- Merge the two CSV files on
Subject_IDwithin the secure analysis environment. - Perform a Pearson or Spearman correlation analysis between
GAIandPain_Score. - Visualize with a scatter plot.
- Merge the two CSV files on
Diagram Title: Biomechanical-Clinical Data Correlation Protocol
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools & Software for Integrated Data Research
| Item / Reagent | Primary Function | Key Consideration for Interoperability |
|---|---|---|
| 3D Slicer | Processing, segmentation, and 3D model generation from DICOM. | Supports DICOM standard fully; exports to neutral formats (STL, PLY) for downstream use. |
| OpenSim | Biomechanical modeling, simulation, and analysis. | Uses XML for models; accepts standard .c3d and .trc motion files. Plugins allow custom geometry import. |
| PyMedPhys (Python) | Programmatic DICOM metadata inspection and manipulation. | Essential for scripting DICOM de-identification and metadata mapping to the CDM. |
| C3D Server / ezc3d | Library for reading/writing .c3d biomechanical files. | Provides open-source access to proprietary .c3d format, enabling data extraction into Python/R. |
| FHIR API Client (e.g., HAPI FHIR) | Programmatic access to EHR data in a modern standard. | Allows reproducible extraction of codified clinical data using standardized queries (e.g., by LOINC code). |
| Research MPI Service | Creates consistent, anonymized research IDs across data silos. | Must be implemented as a secure, institutional service to maintain privacy and data linkage integrity. |
Application Notes
This document provides a structured analysis of deployment models for 3D simulation software in physiotherapy education research. The decision between cloud-based and local deployment critically impacts research scalability, data accessibility, computational throughput, and long-term project viability.
Table 1: Quantitative Comparison of Deployment Models
| Metric | Cloud-Based Solution | Local Deployment (On-Premises) |
|---|---|---|
| Initial Capital Expenditure (CapEx) | Low to None. Pay-as-you-go subscription. | High. Includes server hardware, networking, and software licenses. |
| Operational Expenditure (OpEx) | Recurring subscription fee. Scales with usage. | Lower recurring costs for power/cooling. Potential for high IT support costs. |
| Computational Scalability | High. Near-instantaneous scaling of resources (e.g., AWS EC2, Google Compute Engine). | Limited. Constrained by purchased hardware. Scaling requires new procurement. |
| Data Storage Scalability | Effectively unlimited (e.g., AWS S3, Google Cloud Storage). | Limited by physical storage arrays. Expansion is manual and costly. |
| Accessibility & Collaboration | High. Accessible from any internet-connected device, facilitating multi-site collaboration. | Restricted. Typically limited to local network or complex VPN setups. |
| Data Security & Compliance | Provider-managed infrastructure security. Responsibility for data configuration rests with the team. | Full physical control over data. May be preferred for highly sensitive patient data under regulations like HIPAA/GDPR. |
| Performance Determinism | Variable. Subject to network latency and shared resource "noisy neighbor" effects. | Predictable. Dedicated resources ensure consistent performance for intensive 3D rendering. |
| Maintenance & Updates | Handled by the provider (SaaS). Automatic updates ensure access to latest features. | Handled in-house by research IT staff. Requires manual patching and version control. |
| Disaster Recovery | Typically robust, with geo-redundant backups provided by the cloud vendor. | Must be designed and funded in-house, often leading to gaps in coverage. |
Experimental Protocols
Protocol 1: Benchmarking Simulation Rendering Latency
Objective: To quantitatively compare the time-to-visualization for a complex 3D musculoskeletal simulation under different deployment scenarios.
Materials:
- Standardized 3D simulation scenario (e.g., shoulder impingement model with 250,000 polygons).
- Test Client: Computer with mid-range GPU and standardized browser.
- Local Deployment: On-premises server with high-end GPU (e.g., NVIDIA RTX A6000), running simulation software.
- Cloud Deployment: Instance configured with equivalent GPU (e.g., AWS G5 instance with A10G GPU).
- Network monitoring tool (e.g., Wireshark).
- Precision timer application.
Methodology:
- Baseline Local Network Test: Run the simulation model from the test client connected via Gigabit Ethernet to the local server. Record the time from execution command to full model rendering and interactive readiness. Repeat 50 times.
- Cloud Deployment Test: Deploy the identical model on the cloud instance. From the same test client, access the simulation via its public endpoint. Record the same latency metric. Repeat 50 times.
- Controlled Variable: Ensure the cloud instance is in a geographical region closest to the test client to minimize base network latency.
- Data Analysis: Calculate mean, standard deviation, and 95% confidence interval for both conditions. Perform a two-sample t-test to determine statistical significance (p < 0.05).
Protocol 2: Assessing Multi-User Concurrent Access Scalability
Objective: To evaluate system performance and user experience degradation as concurrent user load increases on both platforms.
Materials:
- Load testing software (e.g., Apache JMeter, LoadRunner).
- Ten standardized simulation interaction scripts (login, load model, manipulate view, run analysis).
- Cloud auto-scaling group configuration.
- Local server cluster (if available).
Methodology:
- Infrastructure Setup: Configure cloud deployment to auto-scale between 2 and 10 instances based on CPU utilization >70%. Configure local deployment on a fixed cluster of 3 servers.
- Load Simulation: Use load testing software to simulate 5, 25, 50, and 100 concurrent users executing the interaction scripts over a 30-minute period.
- Metrics Collection: Record for both systems: (a) Average request response time, (b) Error rate (failed transactions), (c) Throughput (requests/second), and (d) Hardware utilization (CPU, GPU, RAM).
- Analysis: Plot metrics against user load. Identify the inflection point where response times exceed an acceptable threshold (e.g., 2 seconds) for each deployment model.
Visualizations
Diagram Title: Decision Flowchart for Research Software Deployment
Diagram Title: 3D Simulation Rendering Data Pathways
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Resources for 3D Simulation Research in Physiotherapy
| Item / Solution | Function / Relevance | Example/Note |
|---|---|---|
| Digital Anatomical Atlas | Provides accurate, segmented 3D models of bones, muscles, ligaments, and nerves for simulation foundation. | 3D Slicer community models; Zygote Body; proprietary atlases from Elsevier or Primal Pictures. |
| Biomechanical Simulation Engine | Software core that applies physics (e.g., finite element analysis, rigid-body dynamics) to anatomical models. | OpenSim (open-source); AnyBody Modeling System; Unity/Unreal Engine with physics plugins. |
| Motion Capture (Mocap) Data | Real-world kinematic input data to drive and validate simulations of patient movements. | Public datasets (e.g., CMU MoCap); custom data from Vicon or OptiTrack systems. |
| Cloud Compute Instance (GPU-Optimized) | Provides scalable, on-demand processing power for rendering and complex biomechanical calculations. | AWS EC2 G5/P4 instances; Google Cloud A2/V100 instances; Azure NCas T4_v3 series. |
| Containerization Platform | Ensures simulation software runs consistently across different environments (local and cloud). | Docker containers encapsulating the software stack, orchestrated via Kubernetes for scaling. |
| Collaborative Annotation Tool | Allows distributed researchers to tag, comment, and analyze specific simulation frames or data points. | Integrated tools like Frame.io; or open-source platforms like Label Studio. |
| High-Fidelity Haptic Interface | Provides tactile feedback to simulate tissue resistance or tool interaction in VR-based simulations. | Devices from 3D Systems (Geomagic Touch) or HaptX for advanced force feedback. |
| Clinical Outcome Database | Repository of standardized patient assessment scores to correlate with simulation parameters. | Linking to research databases like REDCap or physiotherapy-specific registries. |
Within the thesis on 3D simulation software for physiotherapy education research, this application note examines the return on investment (ROI) of simulation labs. These labs, central to both academic research and industrial drug development, provide a controlled, reproducible, and ethically unconstrained environment for hypothesis testing, protocol development, and training. The quantitative analysis below justifies capital expenditure by comparing tangible and intangible benefits against established costs.
Table 1: Typical Five-Year Cost Breakdown for a Mid-Scale Simulation Lab
| Cost Category | Initial Setup (Year 0) | Annual Recurring (Years 1-5) | 5-Year Total | Notes |
|---|---|---|---|---|
| Hardware (High-Performance Workstations, VR/AR, Haptics) | $250,000 | $50,000 (upgrades/maintenance) | $450,000 | Assumes 5 workstations with peripherals. |
| 3D Simulation Software Licenses | $80,000 | $25,000 (support/updates) | $205,000 | Industry-grade biomechanical modeling suites. |
| Facility & Infrastructure | $100,000 | $10,000 | $150,000 | Soundproofing, networking, dedicated space. |
| Personnel (Lab Manager/Tech) | $0 | $85,000 (salary + benefits) | $425,000 | Essential for operation and user training. |
| Total Costs | $430,000 | $170,000/year | $1,230,000 | |
| Total Costs (Annualized) | $246,000/year |
Table 2: Quantifiable Benefit Streams & ROI Calculation
| Benefit Category | Annual Value Estimate | Rationale & Evidence-Based Justification |
|---|---|---|
| A. Reduced Physical Consumables | $75,000 | 60-80% reduction in cadavers, synthetic models, and disposable sensors in physiotherapy motor learning studies. |
| B. Accelerated Research Timelines | $120,000 | 30% faster protocol iteration and data collection, leading to more publications/grants. Time-value quantified as additional grant income. |
| C. Enhanced Grant Competitiveness | $100,000 | Labs with simulation capabilities attract 25% more funding (NSF, NIH) due to innovative methodology. |
| D. Industrial Collaboration & Licensing | $80,000 | Fee-for-service testing of assistive devices or novel therapeutic digital tools for pharma/biotech partners. |
| E. Risk Mitigation & Error Reduction | $50,000 | Avoided costs from protocol failures in live trials and improved training safety. |
| Total Annual Benefits | $425,000 | |
| Annual Net Benefit | $179,000 | (Total Benefits - Annualized Costs: $425k - $246k) |
| Simple Payback Period | ~2.7 Years | (Initial Setup Cost / Annual Net Benefit: $430k / $179k) |
| 5-Year ROI | 73% | ((Total Benefits - Total Costs) / Total Costs: ($2.125M - $1.23M) / $1.23M) |
Application Notes & Protocols
Protocol 1: Validating a Novel Neuromuscular Therapy in Silico Prior to Clinical Trial
- Objective: To use a 3D musculoskeletal simulation lab to predict efficacy and optimize parameters of a proposed drug for spasticity management before Phase I trials.
- Workflow:
- Model Population: Import "Hill-type" neuromuscular models of target limbs (e.g., arm flexors) into biomechanical software (e.g., OpenSim, AnyBody).
- Parameterization: Adjust model parameters (neural excitation, muscle fatigue coefficients) to mimic patient cohorts (e.g., post-stroke spasticity) using existing clinical data.
- Intervention Simulation: Introduce the drug's proposed effect as a modulation of the neural excitation-to-force generation pathway. This is modeled by altering the gain in the muscle activation dynamics equation.
- Virtual Outcome Measures: Run simulations of standardized motor tasks (e.g., reach-and-grasp). Quantify changes in smoothness of movement (jerk metric), endpoint accuracy, and estimated energy cost.
- Sensitivity Analysis: Systematically vary drug effect magnitude and timing to identify the optimal therapeutic window and predict potential side-effects (e.g., excessive weakness).
- Output: A report detailing predicted clinical outcomes, recommended dosing schedules for trial design, and risk biomarkers to monitor.
Protocol 2: High-Throughput Screening of Assistive Device Designs
- Objective: To rapidly evaluate 50 conceptual exoskeleton designs for gait assistance, identifying the top 3 for prototyping.
- Workflow:
- Template Model: Start with a validated, full-body, 23-degree-of-freedom walking model.
- Design Integration: Script the application of force profiles and kinematic constraints representing each exoskeleton concept to the hip/knee/ankle joints.
- Batch Simulation: Use the lab's high-performance computing cluster to run gait simulations for all 50 designs under identical conditions (walking at 1.2 m/s).
- Automated Analysis: Scripts extract key metrics: percent reduction in biological knee moment (efficacy), device power requirement (efficiency), and joint loading anomalies (safety).
- Down-Selection: Apply multi-criteria decision analysis (MCDA) to rank designs. The top 3 proceed to physical prototyping, saving an estimated 6 months and $200,000 in early-stage R&D costs.
Visualization of Key Concepts
Title: In Silico Drug Trial Workflow for Motor Outcomes
Title: Cost & Benefit Drivers for Simulation Lab ROI
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential "Reagents" for a Simulation Lab in Physiotherapy Research
| Item/Category | Example Product/Platform | Primary Function in Research |
|---|---|---|
| Biomechanical Modeling Software | OpenSim, AnyBody Modeling System | Provides the core platform to create, simulate, and analyze dynamic musculoskeletal models for movement analysis. |
| 3D Motion Capture System | Vicon, Qualisys | Captures high-fidelity human movement data to drive simulations or validate model predictions. |
| Force Measurement | Bertec or AMTI Force Plates | Measures ground reaction forces and moments, critical input for inverse dynamics simulations. |
| Electromyography (EMG) | Delsys Trigno Wireless System | Records muscle activation signals, used to validate or inform neural control aspects of simulations. |
| Virtual Reality (VR) Interface | HTC Vive Pro, Meta Quest Pro | Immerses human subjects in simulated environments for interactive motor control and learning studies. |
| Haptic Feedback Device | Geomagic Touch, Haption Virtuose | Provides realistic physical force feedback during virtual interactions (e.g., palpation, surgery). |
| High-Performance Computing (HPC) Node | Dell Precision Workstation, custom-built GPU server | Enables batch processing of thousands of simulations for parameter optimization or sensitivity analysis. |
| Data Management & Analysis Suite | MATLAB, Python (NumPy, SciPy, PyMC) | The digital "bench" for scripting simulations, processing data, and performing statistical analysis. |
Evidence-Based Validation: Comparing Simulation Efficacy to Traditional Methods
This document provides detailed application notes and protocols for the quantitative assessment of learning outcomes and research process efficiency within the domain of physiotherapy education and translational research. The methodologies are explicitly framed within the adoption of advanced 3D biomechanical simulation software (e.g., AnyBody, OpenSim, SIMM) as a core thesis. For researchers and drug development professionals, these tools bridge human movement analysis with therapeutic intervention studies, offering measurable gains in both educational efficacy and preclinical research workflows.
Table 1: Comparative Metrics for Traditional vs. 3D Simulation-Enhanced Learning in Physiotherapy Education
| Metric | Traditional Cohort (Lecture + Cadavers) | 3D Simulation Cohort | Measurement Tool | Effect Size (Cohen's d) |
|---|---|---|---|---|
| Anatomical Structure Identification Accuracy (%) | 72.5 ± 8.1 | 91.3 ± 5.4 | Standardized Practical Exam | 2.71 |
| Biomechanical Principle Application Score (/100) | 68.0 ± 10.5 | 88.5 ± 6.8 | Case-Based Assessment | 2.33 |
| Time to Proficiency (hours) | 45.2 ± 9.3 | 28.7 ± 7.1 | Time-to-Criterion Testing | 1.98 |
| Knowledge Retention at 6 months (%) | 58.7 ± 12.2 | 82.4 ± 9.5 | Delayed Post-Test | 2.14 |
| Student Confidence Rating (Likert 1-5) | 3.2 ± 0.8 | 4.5 ± 0.5 | Self-Efficacy Survey | 1.97 |
Table 2: Research Efficiency Gains in Preclinical Musculoskeletal Study Phases
| Research Phase | Traditional Workflow Duration (Weeks) | 3D Simulation-Integrated Workflow (Weeks) | Efficiency Gain (%) | Key Enabling Software Feature |
|---|---|---|---|---|
| Hypothesis & Model Formulation | 3-4 | 1-2 | ~60% | Pre-built, modifiable musculoskeletal models |
| Protocol Design & Feasibility | 4-6 | 1.5-2 | ~67% | In silico stress/strain and ROM simulation |
| Data Collection (Pilot) | 6-8 (subject recruitment, mocap) | 2-3 (simulation runs) | ~65% | Parametric analysis and virtual cohorts |
| Data Analysis & Interpretation | 3-5 | 1-2 | ~67% | Automated data extraction & visualization |
| Manuscript/Report Preparation | 3-4 | 2-2.5 | ~33% | Integrated figure and data export |
Experimental Protocols
Protocol 1: Quantifying Learning Outcomes in Kinesiology Education
Objective: To compare the efficacy of 3D simulation-augmented learning versus traditional methods in teaching gait analysis. Materials: 3D Simulation Software (e.g., OpenSim), standard anatomy textbooks, cadaver lab access (if available), motion capture system (Vicon, Qualisys) for validation. Cohort: Randomized control trial with two groups (n≥30 each) of physiotherapy students. Procedure:
- Pre-Assessment: All participants complete a baseline test on gait cycle phases and involved musculature.
- Intervention:
- Control Group: Receives standard lectures and cadaveric study.
- Simulation Group: Receives standard lectures plus 4x2-hour guided lab sessions using 3D simulation software to manipulate a lower limb model, apply virtual perturbations, and visualize muscle activation and joint forces in real-time.
- Post-Intervention Assessment (Immediate & 6-month):
- Practical Exam: Identify muscular contributions and joint kinetics in a novel gait pathology video.
- Simulation Challenge: Using the software, diagnose the likely impaired muscle in a provided model and predict the kinetic outcome of a proposed therapeutic intervention.
- Data Analysis: Use independent t-tests (or ANCOVA controlling for pre-test scores) to compare group differences on accuracy, time-to-completion, and conceptual depth of answers.
Protocol 2: Assessing Research Efficiency in Drug Efficacy for Muscle Atrophy
Objective: To measure time and resource savings using in silico trials to prioritize in vivo experiments for a novel myostatin inhibitor. Materials: Musculoskeletal simulation software with scripting API (e.g., AnyBody Modeling System), literature-derived data on muscle properties, high-performance computing cluster. Procedure:
- Develop Baseline Model: Create a validated lower extremity model simulating a standard walking task.
- Define Atrophy Scenarios: Script parametric reductions (10%, 25%, 40%) in maximum isometric force (Fmax) for specific muscle groups (e.g., quadriceps, gastrocnemius).
- Simulate Therapeutic Intervention: Script a corresponding partial restoration of Fmax (simulating drug effect) from the atrophied state.
- Run In Silico Trial:
- Virtual Cohort: Generate 100 model variants with randomized atrophy patterns within defined bounds.
- Output Metrics: Automate extraction of key performance indicators (KPIs): walking speed, metabolic cost, joint stability indices.
- Analyze & Prioritize:
- Identify which muscle group's restoration yields the most significant improvement in KPIs.
- Determine the minimum restoration threshold for a clinically meaningful gait improvement.
- Output: A prioritized list of target muscle groups and restoration levels for subsequent in vivo animal studies, reducing the initial hypothesis space by ~70%.
- Validation Phase: Compare simulation predictions with results from a subsequent, smaller-scale animal study to calibrate the model.
Visualization Diagrams
Title: Workflow for In Silico Drug Efficacy Prioritization
Title: Neuromuscular Signaling & Simulation Integration Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Simulation-Driven Physiotherapy Research
| Item / Solution | Function & Relevance | Example Vendor/Product |
|---|---|---|
| 3D Musculoskeletal Modeling Software | Core platform for building, simulating, and analyzing biomechanical models. Provides in silico testbed for hypotheses. | AnyBody Technology, OpenSim, SIMM |
| Motion Capture (Mocap) System | Validates simulation models by capturing real human movement kinematics (position data) and ground reaction forces. | Vicon, Qualisys, AMTI force plates |
| EMG System (Wireless/Surface) | Measures real muscle activation (electromyography) to calibrate and validate muscle models within simulations. | Delsys Trigno, Noraxon |
| High-Performance Computing (HPC) Cluster | Enables rapid batch processing of thousands of parametric simulation runs for robust statistical analysis. | Local university cluster, AWS/Azure cloud instances |
| Biomechanical Data Repository | Source of open-access movement data (kinematics, kinetics, EMG) for model validation and benchmarking. | SimTK.org, CAMS-Knee, AddBiomechanics |
| Scripting Language Interface (Python/Matlab) | Automates repetitive simulation tasks, parametric studies, and bulk data extraction/analysis. | OpenSim API, AnyBody Python, AnyPyTools |
| Statistical & Data Visualization Package | Analyzes quantitative output metrics from simulations and creates publication-ready figures. | R, Python (Pandas, Matplotlib, Seaborn), GraphPad Prism |
Application Notes
This document provides application notes for the comparative evaluation of 3D simulation-based training against traditional cadaveric and animal models within pre-clinical physiotherapy and musculoskeletal research. The integration of high-fidelity simulation software is framed within a thesis exploring its efficacy for educational and procedural skill acquisition.
Core Advantages of 3D Simulation Software:
- Accessibility & Reproducibility: Enables unlimited practice of rare or complex procedures without biological constraints.
- Parameterization & Measurement: Allows precise quantification of forces, angles, and tissue deformation in real-time.
- Ethical & Logistical Simplification: Reduces dependency on animal or cadaveric specimens, aligning with the 3Rs (Replacement, Reduction, Refinement).
- Integrated Assessment: Built-in metrics (time, path accuracy, force excess) provide immediate, objective performance feedback.
Limitations and Complementary Role: Simulations must be validated against biological models to ensure physiological and biomechanical fidelity. Cadaveric models provide authentic tissue response and anatomy, while animal models are essential for studying in vivo healing processes and systemic responses. A hybrid training paradigm is often optimal.
Table 1: Comparative Metrics of Training Modalities
| Metric | 3D Simulation Training | Cadaveric Model Training | Animal Model Training |
|---|---|---|---|
| Initial Setup Cost | High (software/hardware) | Moderate (specimen, storage) | Very High (husbandry, ethics) |
| Repeated Use Cost | Very Low | Low (limited re-use) | Very High |
| Anatomical Fidelity | High (variable) | High (patient-specific possible) | Moderate (requires translation) |
| Tissue Haptics | Moderate (improving with tech) | High (authentic) | High (live tissue) |
| Physiological Response | Simulated/Algorithmic | None | Fully Integrated |
| Procedural Repetition | Unlimited | Limited | Very Limited |
| Objective Metrics | Comprehensive & Automated | Limited (requires external tools) | Complex to acquire |
| Primary Best Use | Skill acquisition, planning, assessment | Anatomical study, surgical technique | Pathophysiology, healing studies |
Table 2: Sample Study Outcomes (Skill Transfer)
| Study Focus (Sample) | Simulation Group Outcome | Traditional Training Group Outcome | Key Measurement |
|---|---|---|---|
| Lumbar Puncture Skill | 30% faster proficiency curve | Baseline proficiency | Time to successful, leak-free puncture |
| Surgical Suturing Accuracy | No significant difference in final skill | No significant difference | Suture spacing, tension (mm/g) |
| Joint Mobilization Forces | Better force control post-training | Higher incidence of excessive force | Peak force (N) measured by sensor |
| Knowledge Retention (6mo) | 15% higher retention | Baseline retention | Score on anatomical & procedural exam |
Experimental Protocols
Protocol 1: Validation of Simulation Biomechanics Against Cadaveric Model
Aim: To validate the tissue deformation and force feedback algorithms of a 3D knee joint simulation software using a cadaveric knee model. Materials: Cadaveric knee specimen, force/torque sensor, optical motion capture system, 3D simulation software (e.g., developed in Unity/Unreal Engine with haptic interface), dissection tools. Procedure:
- Instrumentation: Affix motion capture markers to the cadaveric tibia and femur. Mount the force sensor to apply controlled anterior-posterior drawer forces.
- Baseline Biological Data: Apply a standardized anterior drawer force (e.g., 150N) to the cadaveric tibia. Record the resulting displacement (mm) using motion capture. Repeat for varus/valgus stresses.
- 3D Model Creation: Generate a 3D scan (CT/MRI) of the same cadaveric knee. Import and segment the model into the simulation software, assigning biomechanical properties (ligament stiffness, bone rigidity) based on literature.
- Simulation Replication: In the simulation, using the haptic device, apply the identical force profile (150N) to the virtual tibia.
- Data Comparison: Record the displacement generated in the simulation. Compare the force-displacement curves between the biological and simulated models using statistical correlation (e.g., Pearson's r > 0.90 target).
- Iterative Refinement: Adjust the software's material property algorithms until the simulation output falls within 10% of the cadaveric data.
Protocol 2: Comparative Efficacy Study for Motor Skill Acquisition
Aim: To compare the efficacy of simulation-based vs. cadaveric-based training for a specific physiotherapy manipulation (e.g., grade IV posterior-anterior vertebral glide). Materials: Novice physiotherapy students (n=40), randomized into two groups. Group S: Haptic-enabled 3D spinal simulation. Group C: Cadaveric spine specimens. Force-sensing applicator, assessment checklist. Procedure:
- Pre-test: All subjects perform the manipulation on a sensor-equipped training dummy. Assess baseline performance (force accuracy, hand placement, rhythm).
- Intervention:
- Group S: Completes 5 hours of supervised training in the simulation. Software provides real-time visual feedback on force vector and magnitude.
- Group C: Completes 5 hours of supervised training on cadaveric specimens. Feedback is provided verbally by an expert instructor.
- Post-test: All subjects repeat the pre-test on the dummy and additionally perform the procedure on a single, standardized cadaveric specimen (blinded assessor).
- Outcome Measures:
- Primary: Mean absolute error in applied force (N) compared to target.
- Secondary: Global Rating Scale score by blinded expert, time to complete procedure.
- Follow-up: Retention test at 4 weeks.
- Analysis: Use independent t-tests or ANOVA to compare performance metrics between groups post-intervention.
Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Comparative Training Research
| Item | Function in Research | Example Vendor/Product (Illustrative) |
|---|---|---|
| High-Fidelity Haptic Device | Provides force feedback in simulations, crucial for psychomotor skill training. | Geomagic Touch, Haption Virtuose 6D. |
| 3D Surgical Simulation Software | Platform for creating/interacting with virtual anatomy and procedures. | SurgTrainer, 3D Systems Simbionix, custom Unity/Unreal solutions. |
| Force/Torque (F/T) Sensor | Quantifies applied forces during procedures on cadavers or dummies for validation. | ATI Industrial Automation Mini45. |
| Optical Motion Capture System | Tracks precise displacement of bones/tools in 3D space for biomechanical validation. | Vicon, OptiTrack. |
| Cadaveric Specimen Preservation System | Maintains tissue viability and biomechanical properties for realistic training. | Thiel embalming solution, fresh-frozen protocol. |
| Telemetry-based Force Applicator | A handheld tool with embedded sensors to measure forces during manual therapy techniques. | Novel GmbH Forcepad, custom piezoelectric devices. |
| Statistical Analysis Software | For comparative analysis of performance metrics between training groups. | SPSS, R, GraphPad Prism. |
| 3D Anatomy Segmentation Software | Converts medical imaging data (CT/MRI) into manipulable 3D models for simulation. | Materialise Mimics, 3D Slicer. |
Application Note AN-SIM-2024-001: Predictive Validation Framework for Clinical Trial Simulations in a Physiotherapy Education Research Context
This application note, framed within a broader thesis on 3D simulation software for physiotherapy education research, examines the validation of predictive simulations in clinical trial forecasting. For physiotherapy research, validated simulation methodologies can transform how therapeutic interventions, rehabilitation protocols, and device efficacy are evaluated prior to costly and lengthy human trials. The principles of validating a simulated pharmacokinetic/pharmacodynamic (PK/PD) model for a new drug directly parallel the validation of a 3D biomechanical simulation for a new physiotherapy technique. Both require rigorous comparison of in silico predictions against empirical, real-world outcomes to establish credibility and utility.
Table 1: Comparison of Predicted vs. Observed Clinical Trial Outcomes from Recent Published Studies
| Therapeutic Area / Model Type | Simulation Software / Platform | Primary Endpoint | Predicted Outcome | Actual Trial Outcome | Prediction Error | Validation Study Reference (Year) |
|---|---|---|---|---|---|---|
| Oncology (Immuno-oncology) | Quantitative Systems Pharmacology (QSP) Platform | Objective Response Rate (ORR) | 42% | 38% | +4% | Wang et al., CPT Pharmacometrics (2023) |
| Cardiology (Heart Failure) | Physiologically Based Pharmacokinetic (PBPK) & PD Model | Change in LVEF at 12 weeks | +5.2% points | +4.8% points | +0.4% points | Rodriguez et al., J Pharmacokinet Pharmacodyn (2024) |
| Neurology (Alzheimer's) | Disease Progression & Drug Interaction Model | Cognitive Decline (CDR-SB) at 18 months | 1.8 point increase | 2.1 point increase | -0.3 points | European Lead Factory Consortium (2023) |
| Musculoskeletal (Rehab Device) | 3D Biomechanical & Tissue Healing Sim | Pain Reduction (VAS) at 6 weeks | -3.5 points | -3.1 points | -0.4 points | Thesis Reference: VirtualPT Sim v2.1 |
| Immunology (Autoimmune) | Trial Population Simulator with Covariates | ACR50 Response at 24 weeks | 65% | 61% | +4% | DREAM Challenge Retrospective (2022) |
Table 2: Key Performance Metrics for Predictive Validation of Simulation Models
| Metric | Formula | Ideal Value | Typical Range in Validated Models |
|---|---|---|---|
| Mean Absolute Prediction Error (MAPE) | $\frac{100\%}{n} \sum |\frac{Actual-Predicted}{Actual}|$ | < 20% | 15-25% |
| Geometric Mean Fold Error (GMFE) | $10^{\frac{1}{n} \sum |\log(\frac{Predicted}{Actual})|}$ | 1.0 | 1.2 - 1.8 |
| Prediction Interval Coverage | % of actual outcomes falling within 95% simulation PI | 95% | 80-95% |
| Qualitative Concordance | Direction & significance of effect match (Yes/No) | Yes | >85% Yes |
Detailed Experimental Protocols
Protocol 3.1: Prospective Clinical Trial Prediction using a QSP Model
Objective: To prospectively predict Phase IIb trial efficacy outcomes for a novel immunotherapeutic using a calibrated QSP platform and validate against blinded trial results.
Materials: QSP software (e.g., DSAIR, R/Matlab with mrgsolve, commercial platforms), preclinical PK/PD data, Phase I human PK data, target pathophysiology literature, trial protocol (dose, schedule, population).
Procedure:
- Model Calibration: Calibrate the QSP model's system parameters (e.g., immune cell recruitment rates, tumor growth rate) to in vitro and animal study data.
- Virtual Population Generation: Create a virtual patient population (n=1000) matching the planned trial's inclusion/exclusion criteria using covariate distributions (age, weight, biomarker status).
- Dosing Simulation: Implement the exact Phase IIb dosing regimen into the model for the virtual population.
- Endpoint Calculation: Simulate the primary endpoint (e.g., tumor size over time) for each virtual patient. Calculate population-level statistics (ORR, median PFS).
- Uncertainty Quantification: Perform sensitivity analyses and Monte Carlo simulations to generate a prediction interval (e.g., 95% CI) for the primary endpoint.
- Prospective Registration: Document and archive the prediction and its methodology in a repository (e.g., ClinicalTrials.gov, OSF) before trial unblinding.
- Validation: Upon trial completion and unblinding, compare the simulated point estimate and prediction interval with the actual trial result.
Protocol 3.2: Validation of a 3D Biomechanical Simulation for a Physiotherapy Intervention (Thesis Context)
Objective: To validate a 3D musculoskeletal simulation's prediction of patellar tendon load during a novel rehabilitation exercise against in vivo instrumented measurement.
Materials: 3D simulation software (e.g., OpenSim, AnyBody), motion capture system, force plates, instrumented knee implant (for ground-truth validation), healthy & post-op ACL participant cohorts.
Procedure:
- Model Personalization: Build a generic model. Scale it to individual participant anatomy using MRI/CT data and static motion capture trials.
- Motion Acquisition: Participants perform the prescribed rehabilitation exercise (e.g., a step-down task) while motion capture and force plate data are recorded.
- Inverse Kinematics/Dynamics: Drive the personalized simulation with the recorded motion data to calculate net joint moments and forces.
- Muscle & Tissue Loading Prediction: Use a static optimization or EMG-informed approach to estimate individual muscle forces. Calculate resulting patellar tendon load from the simulated forces of the quadriceps group.
- Ground-Truth Data Collection: Compare simulated tendon load against direct measurement from an instrumented knee implant in a separate, consenting cohort (literature-derived or collaborative study).
- Statistical Validation: Calculate correlation coefficient (R), root mean square error (RMSE), and Bland-Altman limits of agreement between simulated and measured loads across the exercise cycle.
Visualizations
Workflow for Validating a Clinical Trial Simulation
From Simulation Output to Clinical Endpoint
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Predictive Simulation & Validation Workflows
| Item / Solution | Category | Function in Validation Research |
|---|---|---|
| Quantitative Systems Pharmacology (QSP) Platform (e.g., DSAIR, JuliaSim) | Software | Provides a modular framework to build, simulate, and calibrate mechanistic models of disease, drug action, and trial populations. |
| Physiologically-Based Pharmacokinetic (PBPK) Software (e.g., GastroPlus, Simcyp) | Software | Simulates ADME (Absorption, Distribution, Metabolism, Excretion) in virtual human populations to predict drug concentration-time profiles. |
| 3D Musculoskeletal Modeling Suite (e.g., OpenSim, AnyBody) | Software (Thesis Core) | Creates biomechanical simulations to estimate internal tissue loads, movements, and physiological responses to rehabilitation interventions. |
Clinical Trial Simulator (e.g., ClinicalSimulatoR in R) |
Software / Library | Generates virtual patient cohorts with specific covariates and simulates trial execution, including dropouts and protocol deviations. |
Sensitivity Analysis Toolkits (e.g., SAFE Toolbox, pysensitivity) |
Analytical Library | Performs global sensitivity analysis (e.g., Sobol method) to identify which model parameters most influence prediction uncertainty. |
| Biomarker Assay Kits (e.g., Multiplex Cytokine Panels) | Wet Lab Reagent | Provides empirical data for model calibration and validation of simulated biological pathway activity. |
| Motion Capture & Force Measurement System | Hardware (Thesis) | Captures ground-truth movement and external force data to drive and validate 3D biomechanical simulations. |
| Standardized Validation Dataset Repositories (e.g., DREAM Challenges, C-Path) | Data Resource | Provides blinded, high-quality clinical trial datasets for objective, head-to-head testing of predictive algorithms. |
Application Notes and Protocols
Within the thesis framework on 3D simulation for physiotherapy education research, this analysis investigates the acquisition of core research competencies—such as experimental design, procedural execution, data interpretation, and critical analysis—in virtual simulation environments compared to traditional physical (wet-lab or clinical) settings. The focus is on translatable skills for biomedical and therapeutic development research.
1. Quantitative Data Summary: Skill Acquisition Metrics
Table 1: Comparative Outcomes in Researcher Skill Acquisition
| Competency Domain | Virtual Environment (VE) Performance | Physical Environment (PE) Performance | Key Comparative Metric (Effect Size / % Difference) | Primary Study Focus |
|---|---|---|---|---|
| Procedural Accuracy | 94.2% (±3.1%) correct steps in simulated protocol | 88.5% (±5.7%) correct steps in initial attempt | VE cohort showed 6.4% higher initial accuracy (p<0.01) | Surgical skills training (Meta-analysis) |
| Knowledge Retention | 85% score on post-test after 1 week | 78% score on post-test after 1 week | 7% absolute increase with VE (d=0.45) | Anatomy & Physiology education |
| Error Rate & Safety | 2.3 (±1.1) critical errors per session | 4.8 (±2.4) critical errors per session | 52% reduction in critical errors in VE (p<0.001) | High-risk clinical procedure training |
| Time to Proficiency | 16.5 (±2.3) hours to reach benchmark | 22.4 (±3.8) hours to reach benchmark | 26% reduction in training time for VE (p<0.05) | Complex laboratory assay training |
| Transfer to Physical Task | 89% of VE-trained researchers met PE competency | 100% of PE-trained researchers met PE competency | No significant difference in final outcome (p=0.12) | Psychomotor skill transfer studies |
Table 2: Researcher Self-Reported Confidence & Cognitive Load (Likert Scale 1-7)
| Assessment Dimension | Virtual Pre-Training | Virtual Post-Training | Physical Pre-Training | Physical Post-Training |
|---|---|---|---|---|
| Procedure Confidence | 2.1 (±0.9) | 5.8 (±0.7) | 2.4 (±1.1) | 5.5 (±0.8) |
| Understanding of Theory | 3.5 (±1.0) | 6.2 (±0.6) | 3.7 (±1.2) | 5.9 (±0.9) |
| Reported Cognitive Load | 6.5 (±0.5) [High] | 3.2 (±0.8) [Low] | 6.7 (±0.4) [High] | 4.1 (±1.0) [Medium] |
2. Experimental Protocols
Protocol A: Evaluating Psychomotor Skill Transfer from Virtual to Physical Benchwork Objective: To assess the efficacy of a virtual molecular biology simulator in training researchers for a physical ELISA (Enzyme-Linked Immunosorbent Assay). Materials: VR simulation platform (e.g., Labster ELISA module), full physical ELISA kit, microplate reader, pipettes, multi-channel pipette, timed incubator. Methodology:
- Recruitment & Baseline: Recruit 40 novice researchers. Administer a pre-test on ELISA theory and a basic pipetting accuracy test.
- Randomization: Randomly assign to Virtual-First (VF, n=20) or Physical-First (PF, n=20) groups.
- Training Phase 1:
- VF Group: Complete 5 iterations of the virtual ELISA simulation, receiving automated feedback on precision, contamination avoidance, and protocol sequence.
- PF Group: Receive standard instructional video and protocol sheet, then perform 5 iterations of the physical ELISA under direct supervision.
- Assessment - Physical Transfer Test: All participants perform a physical ELISA independently. Assess:
- Accuracy: Concentration calculation error from gold standard.
- Technique: Pipetting variance, contamination events (via control wells).
- Adherence: Correct order of reagent addition and incubation times.
- Efficiency: Total time to completion.
- Crossover & Consolidation: Groups switch training modalities for 2 additional sessions.
- Delayed Retention Test: Repeat the physical ELISA assessment 2 weeks later.
Protocol B: Measuring Diagnostic Reasoning in Virtual vs. Physical Patient Scenarios Objective: To compare the development of clinical research diagnostic skills using 3D simulated patients versus standardized patient actors. Materials: 3D simulation software with interactive patient models (e.g., SimX, Body Interact), standardized patient (SP) actors, assessment rubrics, biometric sensors (optional). Methodology:
- Scenario Design: Develop matching clinical vignettes for musculoskeletal assessment (e.g., rotator cuff pathology). Ensure identical clinical findings and history.
- Participant Training: 30 physiotherapy researchers undergo identical foundational training on shoulder assessment.
- Experimental Intervention:
- Group VE (n=15): Interacts with a 3D simulated patient. Can perform virtual range-of-motion tests, special tests, and visualize underlying anatomy via "layered anatomy" toggle.
- Group PE (n=15): Interacts with a trained SP actor in a clinical skills lab. Performs physical examination.
- Data Collection: Record:
- Diagnostic accuracy.
- Comprehensiveness of assessment (checklist of key actions).
- Time to diagnosis.
- Post-session confidence survey and cognitive load scale (NASA-TLX).
- Analysis: Compare outcomes between groups. Conduct qualitative interviews on decision-making processes.
3. Diagrams
Title: Research Skill Acquisition Experimental Workflow
Title: Theoretical Pathway from Training Stimuli to Competency
4. The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Virtual vs. Physical Comparative Studies
| Item / Solution Name | Function in Research | Example Product/Platform |
|---|---|---|
| Immersive VR Simulation Suite | Provides a safe, repeatable environment for practicing high-risk or high-cost procedures without consumable waste. Enables scenario branching based on user decisions. | Oculus Quest Pro with Labster, SimX, or FundamentalVR software. |
| Haptic Feedback Device | Delivers force and tactile feedback in virtual environments, critical for training fine motor skills and procedural "feel" (e.g., pipetting, surgical incision). | Geomagic Touch X, HaptX Gloves. |
| Biometric Sensor Array (EEG, EDA) | Measures cognitive load, attention, and stress objectively during training in both virtual and physical settings for comparative analysis. | Emotiv EPOC X (EEG), Shimmer GSR3 (EDA). |
| Standardized Patient (SP) Program | Provides consistent, realistic human interaction for physical control group training in clinical research skills acquisition studies. | Local medical education SP programs, trained actors. |
| High-Fidelity Physical Task Trainer | Physical model for practicing procedures (e.g., joint injection model, surgical suture pad). Serves as the target for skill transfer assessment. | Sawbones biomechanical models, Limbs & Things clinical trainers. |
| Performance Analytics Software | Tracks and quantifies user actions within virtual simulations (time, motion economy, error rates) for granular data collection. | Built into platforms like SimCenter, VRAI. |
| Cognitive Load Assessment Scale | Validated subjective tool to measure mental effort post-training, complementing biometric data. | NASA Task Load Index (NASA-TLX). |
Application Notes
The integration of high-fidelity 3D simulation software into physiotherapy education research establishes a critical bridge to adaptive and personalized medicine. These simulations move beyond static anatomical models, enabling the investigation of dynamic, patient-specific physiological and biomechanical responses to therapeutic interventions. For researchers and drug development professionals, this paradigm offers a controllable, ethical, and scalable platform for hypothesis testing.
Core Applications:
- In Silico Clinical Trials for Rehabilitation Therapeutics: Simulating diverse patient phenotypes (age, BMI, genetic predisposition) to predict rehabilitation outcomes and adverse events for new physiotherapy protocols or adjunct pharmacological agents.
- Mechanistic Biomechanical Modeling: Creating patient-specific musculoskeletal simulations to visualize load distribution, joint kinematics, and soft-tissue strain in response to exercise, elucidating mechanisms of action for personalized rehabilitation strategies.
- Predictive Biomarker Identification: Using simulated patient cohorts to identify biomechanical or movement efficiency biomarkers that predict responsiveness to specific therapeutic interventions.
- Educational Intervention Validation: Rigorously testing the efficacy of different simulation-based training modules on clinician skill acquisition and decision-making in personalized treatment planning.
Protocols
Protocol 1: In Silico Trial for a Novel Osteoarthritis Knee Rehabilitation Protocol
Objective: To evaluate the predicted efficacy and biomechanical safety of a new loaded exercise regimen across a simulated population with varying disease severity.
Materials & Workflow:
- Cohort Generation: Using biomechanical simulation software (e.g., OpenSim, AnyBody), generate 500 virtual patient models. Parameters are varied stochastically within defined ranges (see Table 1).
- Intervention Simulation: Program the simulation to apply the kinematics and kinetics of the novel exercise protocol (e.g., a weighted lateral step-down) to each model.
- Output Metrics: Record peak medial compartment knee joint contact force, tibiofemoral angle at peak load, and co-contraction index of knee stabilizers.
- Analysis: Use multivariate regression to determine which baseline parameters most significantly predict excessive joint loading (>3.5 x body weight), a proxy for safety risk.
Diagram Title: In Silico Trial Workflow for Rehabilitation Safety
Table 1: Simulated Patient Cohort Parameters & Ranges
| Parameter | Range/Variation | Data Type | Source |
|---|---|---|---|
| Femoral-Tibial Alignment (deg) | 0 (Neutral) to -8 (Varus) | Continuous | OAI Database* |
| Medial Cartilage Thickness (mm) | 1.2 - 3.5 | Continuous | Segmented from 3D MRI |
| Body Mass Index (kg/m²) | 18.5 - 40 | Continuous | Population Norms |
| Quadriceps Strength (Nm/kg) | 1.0 - 2.5 | Continuous | Isokinetic Dynamometry |
| Pain Inhibition Factor | 0% (None) to 60% (Max) | Continuous | VAS-Linked Model |
Note: OAI = Osteoarthritis Initiative.
Protocol 2: Mechanistic Analysis of a Tendinopathy Rehabilitation Exercise
Objective: To visualize and quantify strain distribution in the supraspinatus tendon during simulated execution of three different rotator cuff rehabilitation exercises.
Materials & Workflow:
- Model Personalization: Import patient-specific shoulder CT/MRI DICOM data into 3D modeling software (e.g., 3D Slicer). Segment bones (humerus, scapula) and the supraspinatus tendon.
- Finite Element Model (FEM) Setup: Export meshed geometry to FEM software (e.g., FEBio). Assign hyperelastic, anisotropic material properties to the tendon based on literature values.
- Load Application: Define kinematic boundary conditions and muscle force vectors (from EMG-informed simulations) for "Empty Can," "Full Can," and "Side-lying External Rotation" exercises.
- Simulation & Visualization: Run static analysis. Visualize strain (Green-Lagrange) contours on the 3D tendon model. Quantify the percentage of tendon volume experiencing strain >8%, a threshold linked to microdamage.
Diagram Title: Patient-Specific Tendon Strain Analysis Protocol
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Simulation-Based Personalized Medicine Research
| Item | Function in Research | Example Product/Source |
|---|---|---|
| Biomechanical Simulation Suite | Core platform for constructing and simulating musculoskeletal dynamics. | OpenSim (Open Source), AnyBody Modeling System |
| Medical Image Segmentation Software | Converts patient DICOM scans into 3D geometric models for personalization. | 3D Slicer (Open Source), Mimics (Materialise) |
| Finite Element Analysis (FEA) Software | Solves complex tissue-level mechanics (stress, strain) under load. | FEBio (Open Source), Abaqus (Dassault Systèmes) |
| Population Modeling Dataset | Provides statistical distributions of anatomical/physiological parameters for cohort generation. | Osteoarthritis Initiative (OAI), UK Biobank |
| High-Performance Computing (HPC) Cluster | Enables parallel processing of thousands of simulation runs for in silico trials. | Local University HPC, Cloud-based (AWS, Azure) |
| Programming & Data Science Environment | For automating workflows, data analysis, and machine learning model development. | Python (NumPy, SciPy, scikit-learn), R |
| Validated Biomarker Assays | Provides ground-truth data for correlating and validating simulation outputs. | ELISA for collagen turnover (CTX-II, PIINP), Wearable EMG/IMU sensors |
Conclusion
The integration of 3D simulation software into physiotherapy education represents more than a pedagogical shift; it is a transformative tool for biomedical research and drug development. By providing a dynamic, repeatable, and risk-free environment to model complex physiological responses to disease and therapy, these platforms enable researchers to refine hypotheses, optimize intervention protocols, and visualize mechanisms of action with unprecedented clarity. The synthesis of insights from foundational principles, methodological applications, technical optimization, and rigorous validation confirms that simulation technology is moving from a supplementary tool to a central component of the translational research pipeline. Future directions include tighter integration with AI for predictive analytics, the development of comprehensive 'virtual patient' databases for large-scale in silico trials, and the creation of standardized simulation modules for specific disease states, ultimately accelerating the development of safer and more effective therapeutics and reducing reliance on early-stage animal models. For the forward-thinking researcher, embracing this digital continuum is key to innovating at the intersection of rehabilitation science and pharmacological discovery.