Voluntary Blink Communication Protocols: Next-Generation Assistive Technology for Patients with Severe Motor Impairments
This article provides a comprehensive analysis of voluntary blink-controlled communication protocols, a critical assistive technology for patients with conditions such as locked-in syndrome, ALS, and severe brain injury.
Voluntary Blink Communication Protocols: Next-Generation Assistive Technology for Patients with Severe Motor Impairments
Abstract
This article provides a comprehensive analysis of voluntary blink-controlled communication protocols, a critical assistive technology for patients with conditions such as locked-in syndrome, ALS, and severe brain injury. Targeting researchers and drug development professionals, it explores the neuroscientific foundations of blink control, details cutting-edge methodological approaches from computer vision and EEG-based systems, and addresses key optimization challenges like distinguishing intentional from involuntary blinks. The content synthesizes recent validation studies and performance comparisons, offering a roadmap for integrating these technologies into clinical trials and therapeutic development to enhance patient quality of life and create novel endpoints for neurological drug efficacy.
The Neuroscience of Blink Control and Its Clinical Imperative in Severe Motor Impairments
Blinking is a complex motor act essential for maintaining ocular surface integrity and protecting the eye. For researchers developing blink-controlled communication protocols, particularly for patients with severe motor disabilities such as amyotrophic lateral sclerosis (ALS) or locked-in syndrome, a precise understanding of the neuromuscular and neurophysiological distinctions between voluntary and reflexive blinking is paramount [1] [2] [3]. These two blink types are governed by distinct neural pathways, exhibit different kinematic properties, and are susceptible to varying pathologies [4] [1]. This document provides a detailed experimental framework for differentiating these blinks, underpinned by quantitative data and protocols, to advance the development of robust assistive technologies.
Quantitative Kinematic and Physiological Differentiation
The following tables summarize the key characteristics that experimentally distinguish voluntary and reflexive blinks. These parameters are critical for creating algorithms that can accurately classify blink types in a communication protocol.
Table 1: Kinematic and Functional Characteristics of Blink Types
| Characteristic | Voluntary Blink | Reflexive Blink (Corneal Reflex) | Clinical/Experimental Significance |
|---|---|---|---|
| Neural Control | Cortical & Subcortical circuits; involves pre-motor readiness potential [1] | Brainstem-mediated; afferent trigeminal (V) & efferent facial (VII) nerves [5] [6] | Voluntary control is essential for intentional communication; reflex is a protective indicator [2] |
| Primary Function | Intentional action (e.g., for communication) [2] | Protective response to stimuli (e.g., air puff, bright light) [5] [1] | Guides the context of use in assistive devices. |
| Closing Phase Speed | Slower than reflex [5] | Faster than spontaneous/voluntary [5] | A key kinematic parameter for differentiation via video-oculography [5] |
| Conscious Awareness | Conscious and intentional [1] | Unconscious and involuntary [1] | Fundamental to the paradigm of voluntary blink-controlled systems. |
| Muscle Activation Pattern | Complex, varied patterns in the orbicularis oculi [7] | Stereotyped, consistent patterns [7] | Can be detected with high-precision EMG to improve classification accuracy [7] |
| Typical Amplitude | Can be highly variable; often full closure [1] | Consistent, often complete closure [5] | Incomplete blinks can reduce efficiency in communication systems [1] |
| Habituation | Non-habituating | R2 component habituates readily [6] [8] | Important for experimental design; repeated reflex stimulation loses efficacy. |
Table 2: Electrophysiological Blink Reflex Components
| Component | Latency (ms) | Location | Pathway | Stability |
|---|---|---|---|---|
| R1 | ~12 (Ipsilateral only) | Pons | Oligosynaptic between principal sensory nucleus of V and ipsilateral facial nucleus [6] [8] | Stable, reproducible [6] |
| R2 | ~21-40 (Bilateral) | Pons & Lateral Medulla | Polysynaptic between spinal trigeminal nucleus and bilateral facial nuclei [6] [9] [8] | Variable, habituates [6] |
Experimental Protocols for Differentiation
This section outlines standardized methodologies for eliciting, recording, and analyzing the two blink types, providing a foundation for reproducible research.
Protocol 1: Video-Oculography for Kinematic Analysis
This non-contact method is ideal for measuring blink dynamics in patient populations [5].
- Objective: To quantify the speed and completeness of voluntary and reflexive blinks using high-speed video recording.
- Equipment:
- High-speed camera (e.g., capable of ≥240 fps) [5]
- Stable headrest (e.g., chinrest)
- Consistent, oblique illumination (e.g., LED lamps at 1300 ± 100 lux) [5]
- Air jet system for reflex elicitation (e.g., syringe or solenoid valve delivering ~20 ml air puff <150 ms) [5]
- Video processing software (e.g., MATLAB)
- Procedure:
- Position the subject in the chinrest, ensuring both eyes are in the camera's field of view.
- For reflexive blink recording: Randomly activate the air jet directed at one cornea without warning the subject. Record the resulting direct (ipsilateral) and consensual (contralateral) blinks [5].
- For voluntary blink recording: Instruct the subject to blink "naturally" when needed or to blink on a specific verbal command.
- Record a 60-second sequence containing both types of blinks.
- Off-line processing: Define a region of interest (ROI) around each eye. Calculate the light intensity diffused by the eye within the ROI for each video frame. Blinks will appear as sharp peaks in this intensity curve [5].
- Data Analysis:
- Fit the intensity curve to an Exponentially Modified Gaussian (EMG) function. The parameters (σ, μ, τ) describe the dynamics of the blink's closing and opening phases [5].
- Compare the closing speed (derived from EMG parameters) between voluntary and reflexive blinks. Reflexive blinks should demonstrate a significantly faster closing phase [5].
Protocol 2: Electrophysiological Blink Reflex Testing
This protocol assesses the integrity of the trigeminal-facial brainstem pathway, which is crucial for reflexive blinks [6] [8].
- Objective: To record and measure the R1 and R2 components of the blink reflex elicited by electrical stimulation.
- Equipment:
- Clinical electrophysiology recording system
- Surface recording electrodes
- Electrical stimulator (e.g., pediatric prong stimulator)
- Ground electrode
- Procedure:
- The subject lies supine in a relaxed state, eyes open or gently closed.
- Place surface recording electrodes on the orbicularis oculi muscles bilaterally. The active electrode (G1) is placed below the eye, lateral and inferior to the pupil. The reference (G2) is placed lateral to the lateral canthus [6].
- Place the ground electrode on the mid-forehead or chin.
- Stimulate the supraorbital nerve on one side by placing the stimulator over the eyebrow.
- Use a brief electrical shock (0.1-0.2 ms duration, 5-10 mA intensity, or 2-3 times sensory threshold) [8].
- Record the EMG response from both eyes simultaneously. Allow several seconds (e.g., 10+ seconds) between stimulations to prevent habituation of the R2 component [6] [9].
- Repeat 4-6 stimuli on one side, then perform the same procedure on the contralateral side.
- Data Analysis:
- Measure the latencies of the R1 (ipsilateral) and R2 (bilateral) responses from the stimulus artifact to the onset of the EMG potential.
- Compare latencies to normative data. An afferent pattern (delayed R2 bilaterally when stimulating the affected side) suggests trigeminal nerve pathology. An efferent pattern (delayed R2 on the affected side regardless of stimulation side) suggests facial nerve pathology [6] [8].
Protocol 3: Voluntary Blink Training for Timed Responses
This protocol is directly relevant to training patients to use voluntary blinks for communication [10].
- Objective: To train subjects to produce well-timed voluntary blink responses to a neutral conditional stimulus (CS).
- Equipment:
- Eyelid movement recording system (e.g., magnetic search coil or EOG) [10]
- Auditory or visual feedback system
- Procedure:
- Instruct the subject that they will hear a tone (CS) and should try to blink with a specific delay after it (e.g., 300 or 500 ms).
- Provide feedback to guide learning. This can be:
- Conduct a series of trials (e.g., 40 with feedback), followed by trials without feedback to test retention.
- The subject can be trained to associate different blink patterns (e.g., single vs. double blink) with distinct commands.
- Data Analysis:
- Calculate the percentage of correctly timed responses (onset >150 ms after CS and before the target).
- Analyze the onset and peak latency of the blinks to assess timing accuracy. Studies show humans can voluntarily learn to time blinks with high accuracy, comparable to classically conditioned blinks [10].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Blink Research
| Item | Function/Application | Example Use Case |
|---|---|---|
| High-Speed Camera (≥240 fps) | Captures rapid eyelid kinematics for detailed analysis of speed and completeness [5] | Video-oculography protocol for differentiating blink types [5] |
| Surface EMG Electrodes | Records electrical activity from the orbicularis oculi muscle [7] [6] | Blink reflex testing and studying muscle activation patterns [6] [8] |
| Electrical Stimulator | Elicits a standardized, quantifiable blink reflex via supraorbital nerve stimulation [6] [8] | Clinical neurophysiology assessment of cranial nerves V and VII [6] |
| Solenoid Valve Air Puff System | Delivers a consistent, brief air jet to the cornea to elicit a protective reflex blink [5] [10] | Kinematic studies of reflexive blinks without electrical stimulation [5] |
| Electrooculography (EOG) | Measures corneo-retinal potential to detect eye movements and blinks [2] [3] | Assistive device input for bed-ridden patients; detects high-amplitude voluntary blinks [2] |
| Data Acquisition (DAQ) System | Interfaces sensors (EMG, EOG, camera) with a computer for signal processing and analysis [2] | Core component of any custom-built blink recording or assistive device system [2] |
| MATLAB with Custom Scripts | For offline processing of video intensity curves, EMG signals, and kinematic parameter extraction [5] [10] | Data analysis in kinematic and voluntary blink training protocols [5] [10] |
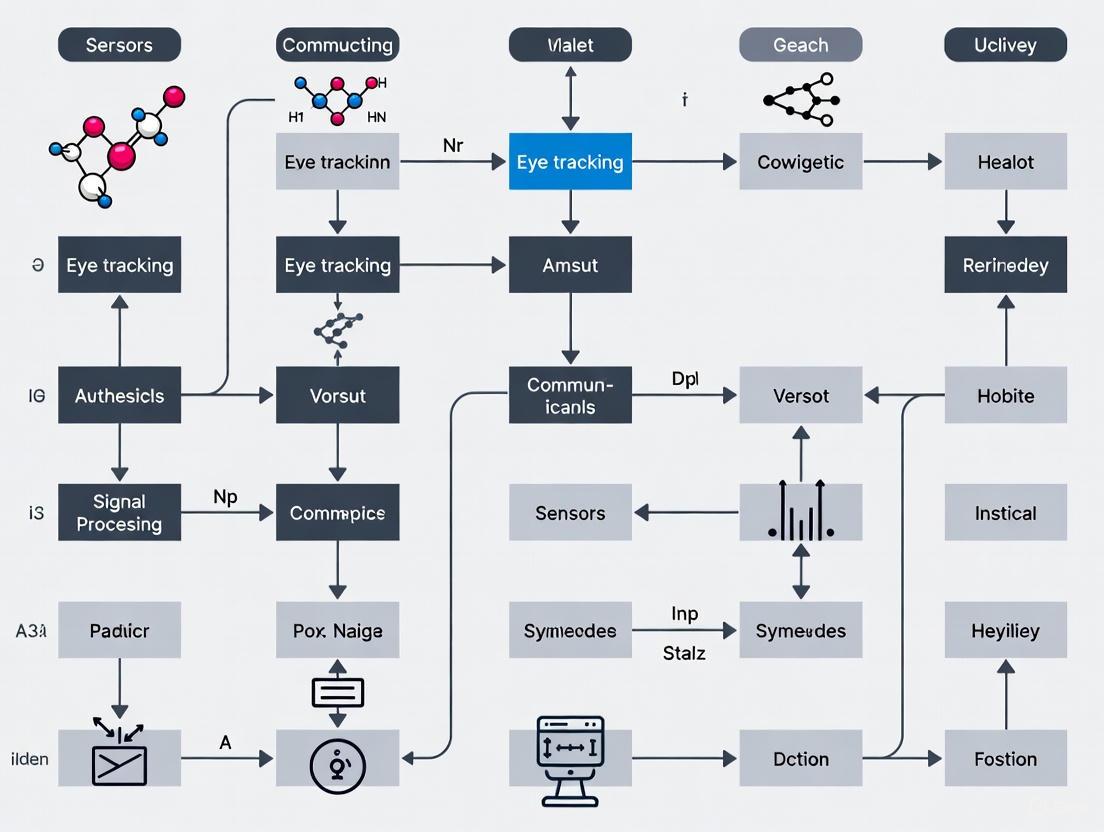
Neural Pathway Diagrams
The following diagrams illustrate the distinct neural circuits governing voluntary and reflexive blinks, which is fundamental to understanding their differential control.
Diagram 1: Neuromuscular Pathways of Blinking. The voluntary pathway (red/orange) involves cortical decision-making centers descending through subcortical structures to the brainstem. The reflexive pathway (green) is a brainstem-mediated loop involving the trigeminal and facial nerves, bypassing higher cortical centers for rapid protection.
Diagram 2: Experimental Workflow for Blink Differentiation. A unified protocol for distinguishing blink types through simultaneous kinematic and electrophysiological recording, culminating in data analysis that classifies blinks for use in assistive communication systems.
Epidemiological Data on TBI and ALS Risk
Recent large-scale epidemiological studies provide critical insights into the relationship between Traumatic Brain Injury (TBI) and the subsequent risk of Amyotrophic Lateral Sclerosis (ALS). The data reveals a complex, time-dependent association crucial for researchers to consider in patient population studies.
Table 1: Key Epidemiological Findings from a UK Cohort Study on TBI and ALS Risk [11] [12] [13]
| Parameter | Study Cohort (n=85,690) | Matched Comparators (n=257,070) | Hazard Ratio (HR) |
|---|---|---|---|
| Overall ALS Risk | Higher incidence | Baseline reference | 2.61 (95% CI: 1.88-3.63) |
| Risk within 2 years post-TBI | Significantly higher incidence | Baseline reference | 6.18 (95% CI: 3.47-11.00) |
| Risk beyond 2 years post-TBI | No significant increase | Baseline reference | Not significant |
| Median Follow-up Time | 5.72 years (IQR: 3.07-8.82) | 5.72 years (IQR: 3.07-8.82) | - |
| Mean Age at Index Date | 50.8 years (SD: 17.7) | 50.7 years (SD: 17.6) | - |
This data suggests that the elevated ALS risk following TBI may indicate reverse causality, where the TBI event itself could be an early consequence of subclinical ALS, such as from falls due to muscle weakness, rather than a direct causative factor [11] [14]. For researchers, this underscores the importance of careful patient history taking and timeline establishment when studying these populations.
Locked-In Syndrome in ALS: Communication Protocols and Pathophysiology
Locked-In Syndrome (LIS), a condition of profound paralysis with preserved consciousness, represents a critical end-stage manifestation for a subset of ALS patients. Establishing reliable communication protocols is a primary research and clinical focus.
Table 2: Communication Modalities for LIS Patients [15]
| Modality Category | Description | Examples | Key Considerations |
|---|---|---|---|
| No-Tech | Relies on inherent bodily movements without tools. | Coded blinking, vertical eye movements, residual facial gestures. | Requires a trained communication partner; susceptible to fatigue and error. |
| Low-Tech | Utilizes simple, non-electronic materials. | Eye transfer (ETRAN) boards, letter boards, low-tech voice output devices. | Leverages preserved ocular motility; cost-effective and readily available. |
| High-Tech AAC | Employs advanced electronic devices. | Eye-gaze tracking systems, tablet-based communication software. | Offers greater communication speed and autonomy; requires setup and calibration. |
| Brain-Computer Interface (BCI) | Uses neural signals to control an interface, bypassing muscles. | Non-invasive (EEG-based) systems; invasive (implanted electrode) systems. | The only option for patients with complete LIS (no eye movement); active research area. |
Experimental Protocol: Establishing a Blink-Controlled Communication System
The following protocol outlines a standardized methodology for establishing and validating a blink-controlled communication system for patients with LIS, suitable for research and clinical application.
Phase 1: Assessment and Baseline Establishment
- Confirm Consciousness and Cognitive Capacity: Before establishing communication, confirm the patient's level of consciousness and ability to follow commands. This is a prerequisite for reliable communication [15] [16].
- Establish a Reliable "Yes/No" Response: Work with the patient to define a consistent, reproducible motor signal. Blinking is the most common, but vertical eye movements or a residual facial twitch may be used. Test for reliability by asking simple, verifiable questions [15].
- Document Baseline Function: Record the patient's specific motor capabilities, blink endurance, and any factors that may affect performance (e.g., fatigue, spasticity) [17].
Phase 2: System Implementation and Training
- Select the Encoding Method:
- Alphabet Board Scanning: A communication partner slowly points to letters or groups of letters on a board. The patient blinks to select.
- Coded Blink System: Implement a code, such as one blink for "yes," two for "no," and a more complex sequence (e.g., prolonged blink) to initiate spelling using a pre-agreed alphabet sequence.
- Calibration and Training Sessions: Conduct short, frequent training sessions to minimize fatigue. Begin with simple single-letter selection and progress to word formation. Quantify accuracy and speed [15] [18].
- Introduce Low-Tech Aids: Introduce an E-Tran (Eye Transfer) board—a transparent board with letters—allowing the partner to see where the patient is looking from the opposite side [15].
Phase 3: Validation and Proficiency Measurement
- Standardized Testing: Assess proficiency using standardized word- or sentence-spelling tasks. Calculate the information transfer rate (bits per minute) and accuracy percentage.
- Fatigue Monitoring: Record the maximum sustainable communication session duration and monitor for a decline in accuracy over time, which indicates fatigue.
- Quality of Life (QoL) Assessment: Use standardized QoL questionnaires, adapted for yes/no responses, to subjectively evaluate the impact of the communication system from the patient's perspective [15].
Phase 4: Advanced Integration (If Applicable)
- Transition to High-Tech Systems: For patients with stable blink control, consider transitioning to an eye-gaze tracking computer system, which can offer greater independence and access to more complex communication functions [15].
- BCI Evaluation: For patients who lose all voluntary muscle control, including blinking (progressing to complete LIS), evaluate for BCI systems that rely on neural signals alone [15] [17] [18].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Tools for ALS and LIS Investigation [19] [17] [20]
| Item | Function/Application | Example/Note |
|---|---|---|
| ILB (LMW-Dextran Sulphate) | Investigational drug that induces release of Hepatocyte Growth Factor (HGF), providing a neurotrophic and myogenic stimulus. | Used in Phase IIa clinical trials; administered via subcutaneous injection [19]. |
| BIIB105 (Antisense Oligonucleotide) | Investigational drug designed to reduce levels of ataxin-2 protein, which may help reduce toxic TDP-43 clusters in ALS. | Evaluated in the ALSpire trial; administered intrathecally [20]. |
| Medtronic Summit System | A fully implantable, rechargeable Brain-Computer Interface (BCI) system for chronic recording of electrocorticographic (ECoG) signals. | Used in clinical trials to enable communication for patients with severe LIS by decoding motor intent [17]. |
| Riluzole | Standard-of-care medication that protects motor neurons by reducing glutamate-induced excitotoxicity. | Often a baseline treatment in clinical trials; patients typically continue use [17] [18]. |
| ALSFRS-R Scale | Functional rating scale used as a key efficacy endpoint in clinical trials to measure disease progression. | Tracks speech, salivation, swallowing, handwriting, and other motor functions [19]. |
Signaling Pathways and Workflow Diagrams
The following diagrams visualize key pathophysiological concepts and experimental workflows relevant to ALS and LIS research.
TBI-ALS Risk Relationship Pathway
This diagram illustrates the hypothesized "reverse causality" pathway explaining the time-dependent association between TBI and ALS diagnosis.
Blink Communication Protocol Workflow
This diagram outlines the step-by-step experimental protocol for establishing a blink-controlled communication system, as detailed in Section 2.1.
The detection and interpretation of conscious awareness in patients with severe motor impairments represent a frontier in clinical neuroscience. This article details the experimental protocols and technological frameworks enabling the use of voluntary blink responses as a critical communication channel. We provide application notes on computer vision, wearable sensor systems, and brain-computer interfaces (BCIs) that decode covert awareness and facilitate overt communication for patients with disorders of consciousness, including locked-in syndrome (LIS). Structured data on performance metrics and a comprehensive toolkit for researchers are included to standardize methodologies across the field.
Consciousness assessment in non-responsive patients is a profound clinical challenge. An estimated 15–25% of acute brain injury (ABI) patients may experience covert consciousness, aware of their environment but demonstrating no overt motor signs [21]. Locked-in Syndrome (LIS), characterized by full awareness amidst near-total paralysis, further underscores the critical need for reliable communication pathways [15]. The eyelid and ocular muscles, often spared in such injuries, provide a biological substrate for interaction. Voluntary blinks, distinct in amplitude and timing from involuntary reflexes, can be harnessed as a robust voluntary motor signal for communication [10] [22]. This article outlines the protocols and technologies translating this biological signal into a functional communication protocol, bridging the gap between covert awareness and overt interaction.
Application Notes: Technologies for Blink Detection and Communication
Computer Vision-Based Detection
Overview: Computer vision algorithms can detect subtle, low-amplitude facial movements imperceptible to the human eye, allowing for the identification of command-following in seemingly unresponsive patients.
Key Evidence: The SeeMe tool, a computer vision-based system, was tested on 37 comatose ABI patients (Glasgow Coma Scale ≤8). It detects facial movements by tracking individual facial pores at a high resolution (~0.2 mm) and analyzing their displacement in response to auditory commands [21].
Performance Metrics:
- Earlier Detection: SeeMe detected eye-opening in comatose patients 4.1 days earlier than clinical examination [21].
- Higher Sensitivity: SeeMe identified eye-opening in 85.7% (30/36) of patients, compared to 71.4% (25/36) via clinical examination [21].
- Correlation with Outcome: The amplitude and frequency of SeeMe-detected responses were correlated with functional outcomes at hospital discharge [21].
Wearable Sensor-Based Interfaces
Overview: Wearable technologies, such as thin-film pressure sensors and smart contact lenses, offer an alternative to camera-based systems, providing continuous, portable, and robust blink monitoring.
Key Evidence:
- Pressure Sensors: Systems using thin-film pressure sensors capture delicate deformations from ocular muscle movements. One study evaluated six voluntary blink actions (e.g., single/double/triple, unilateral/bilateral) and found single bilateral blinks (SB) had the highest recognition accuracy (96.75%) and were among the most efficient and comfortable for users [23].
- Wireless Contact Lenses: A novel wireless "EMI contact lens" incorporates a mechanosensitive capacitor and inductive coil to form an RLC oscillating loop. Eyelid pressure during a conscious blink (approx. 30 mmHg) changes the lens curvature, altering the circuit's resonant frequency to encode commands. This system has enabled the control of external devices, such as drones, via multi-route blink patterns [24].
Brain-Computer Interfaces (BCIs) and AAC
Overview: For patients in a total LIS state without any voluntary eye movement, BCIs can translate neural signals directly into commands.
Key Evidence: BCIs are categorized as invasive or non-invasive. Non-invasive BCIs, which include interfaces that can be controlled by blinks, provide a vital communication link. The establishment of a functional system is a key component for maintaining and improving the quality of life for LIS patients [15]. The communication hierarchy progresses from no-tech (e.g., coded blinking) to low-tech (e.g., E-Tran boards) to high-tech (e.g., eye-gaze trackers and BCIs) solutions [15].
Table 1: Quantitative Summary of Blink Detection Technologies
| Technology | Key Metric | Performance Value | Study Population | Reference |
|---|---|---|---|---|
| Computer Vision (SeeMe) | Detection Lead Time | 4.1 days earlier than clinicians | 37 ABI patients | [21] |
| Sensitivity (Eye-Opening) | 85.7% (30/36 patients) | 37 ABI patients | [21] | |
| Pressure Sensor (SB Action) | Recognition Accuracy | 96.75% | 16 healthy volunteers | [23] |
| Wireless Contact Lens | Pressure Sensitivity | 0.153 MHz/mmHg | Laboratory and human trial | [24] |
Experimental Protocols
Protocol 1: Computer Vision for Covert Consciousness Detection
This protocol is designed to identify command-following in patients with ABI who do not respond overtly.
1.1 Participant Setup and Calibration
- Position a high-frame-rate camera (e.g., 30-60 fps) approximately 1-1.5 meters from the patient's face, ensuring clear visibility of the entire facial region.
- Conduct a baseline recording for 1 minute while the patient is at rest to establish individual movement baselines [21].
1.2 Auditory Command Stimulation
- Use pre-recorded auditory commands delivered via noise-isolating headphones to ensure consistency and minimize external noise. Core commands include: "Open your eyes," "Stick out your tongue," and "Show me a smile" [21].
- Present commands in blocks of 10 repetitions for each command type.
- Implement a variable inter-stimulus interval of 30-45 seconds (±1 sec jitter) to prevent habituation and prediction [21].
1.3 Data Acquisition and Processing
- Record video data throughout the session.
- Process videos using the SeeMe algorithm or similar computer vision pipeline, which involves:
- Facial Landmark Tracking: Identify and track key facial features or pores.
- Vector Field Analysis: Quantify the magnitude and direction of pixel movement between frames.
- Response Window Analysis: Analyze a window of 0-20 seconds post-command for significant movements in the relevant region of interest (e.g., mouth for "stick out your tongue") [21].
1.4 Data Analysis and Validation
- Compare algorithm outputs with simultaneous clinical scores (e.g., Coma Recovery Scale-Revised, Glasgow Coma Scale).
- Validate findings against independent, blinded human raters who review the video recordings [21].
Computer vision workflow for covert consciousness detection.
Protocol 2: Establishing a Voluntary Blink Communication Code
This protocol defines a method for creating a functional yes/no or choice-making system using voluntary blinks.
2.1 Establishing a Reliable "Yes/No" Signal
- Work with the patient and clinical team to define two distinct, reproducible blink patterns. A common standard is:
- "Yes": One voluntary blink.
- "No": Two voluntary blinks in quick succession.
- During training, present simple, verifiable questions (e.g., "Is your name John?"). Provide feedback to shape the accuracy and consistency of the response.
- Confirm response reliability by achieving >95% accuracy on a set of 10 verifiable questions before proceeding [15].
2.2 Implementing a Blink-Controlled AAC System
- For patients with preserved vertical eye movement, an E-Tran (Eye Transfer) board can be used. This is a transparent board with letters and common phrases arranged around the edges. The communication partner holds the board between themselves and the patient, and the patient communicates by looking toward specific areas on the board, often confirmed with a blink [15].
- For higher-throughput communication, integrate with a high-tech eye-gaze tracking device. Here, blinks can be used as a selection command. For example:
- The user looks at a virtual keyboard on a screen.
- A sustained blink (e.g., >500ms) acts as a "click" to select the letter or icon under gaze.
2.3 Coding Complex Commands with Blink Patterns
- Map more complex commands to specific blink sequences. The pressure sensor study suggests starting with the most robust actions [23]:
- Single Bilateral Blink (SB): Primary selection command.
- Double Bilateral Blink (DB): "Go back" or cancel command.
- Single Unilateral Blink (SU): Mode shift or secondary menu access.
- System training should focus on these core actions before introducing more complex patterns like triple blinks.
Protocol for establishing a blink communication code.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Voluntary Blink Communication Research
| Item Name | Function/Application | Specifications & Examples |
|---|---|---|
| High-Speed Camera | Captures facial movements and blink kinematics for computer vision analysis. | Frame rate ≥60 fps; resolution ≥1080p; used in the SeeMe protocol for tracking subtle facial movements [21]. |
| Thin-Film Pressure Sensor | Detects mechanical deformation from eyelid movements for wearable blink detection. | Small size, low power consumption; placed near the eye to detect blink force with high accuracy (~96.75% for single blinks) [23]. |
| Wireless Smart Contact Lens | Encodes blink information via changes in intraocular pressure and corneal curvature. | Contains a mechanosensitive capacitor and inductive coil (RLC loop); enables wireless, continuous monitoring and command encoding [24]. |
| Electrooculography (EOG) | Records the corneo-retinal standing potential to detect eye and eyelid movements. | Traditional method for capturing blink dynamics; provides excellent temporal synchronization [22]. |
| Eye Openness Algorithm | Classifies blinks from video by estimating the distance between eyelids, rather than relying on pupil data loss. | Provides more detailed blink parameters (e.g., duration, amplitude) compared to pupil-size-based methods; available in some commercial eye trackers (e.g., Tobii Pro Spectrum) [22]. |
| E-Tran (Eye Transfer) Board | A no-tech communication aid for patients with voluntary eye movements. | A transparent board with letters/words; the user looks at targets to spell words, often confirmed with a blink [15]. |
| Eye-Gaze Tracking System | A high-tech AAC device that allows control of a computer interface via eye movement. | The user looks at on-screen keyboards; a voluntary blink is often used as the selection mechanism [15]. |
Application Note: Biological Foundations and Quantitative Analysis
Voluntary eye blinks represent a robust biological signal emanating from a preserved oculomotor system, making them ideal for alternative communication protocols in patients with severe motor disabilities such as Amyotrophic Lateral Sclerosis (ALS) [25]. This application note details the biological basis, measurement methodologies, and experimental protocols for implementing blink-based communication systems. By leveraging the neurological underpinnings of blink control and modern computer vision techniques, researchers can develop non-invasive communication channels that remain functional even when other motor systems deteriorate. The core advantage lies in the preservation of oculomotor function despite progressive loss in other motor areas, providing a critical communication pathway for affected individuals.
Neurobiological Basis of Blink Control
The human blink system involves complex neural circuitry that remains functional in various pathological conditions:
- Dual Control System: Blinks are regulated through both reflexive pathways (brainstem-mediated) and voluntary pathways (cortical-mediated) [26]. This dual control system ensures that even when reflexive blinks occur approximately 15 times per minute spontaneously, voluntary blinks can be independently controlled for communication purposes.
- Muscle Kinetics: A blink involves the rapid inhibition of the levator palpebrae muscle followed by contraction of the orbicularis oculi muscle, creating a characteristic down-phase (75-100 ms) and up-phase (longer duration) [26]. The entire blink cycle typically lasts 100-400 milliseconds, with voluntary blinks demonstrating distinct kinematic profiles from spontaneous blinks [27] [26].
- Perceptual Stability Mechanisms: Crucially, the brain maintains perceptual continuity during blinks through active suppression mechanisms [26]. This neurological filtering allows voluntary blinks to be used as intentional signals without causing significant visual disruption to the user.
Quantitative Blink Parameters for Communication Systems
Table 1: Clinically Significant Blink Parameters for Communication Protocol Design
| Parameter | Typical Range | Communication Significance | Measurement Method |
|---|---|---|---|
| Duration | 100-400 ms [27] | Determines minimum detection window; affects communication rate | High-frame-rate video (240+ fps) [27] or eye-openness signal [22] |
| Amplitude | Complete vs. Incomplete closure [22] | Distinguishes voluntary from spontaneous blinks; enables multiple command levels | Eye-openness signal or eyelid position tracking [22] |
| Velocity | Down-phase: 16-19 cm/s [26] | Kinematic signature of intentionality | Derivative of eyelid position signal [27] |
| Temporal Pattern | Variable inter-blink intervals | Enables coding of complex messages through timing patterns | Timing between sequential voluntary activations [25] |
Experimental Protocols
Protocol 1: High-Frame-Rate Video Blink Detection
Purpose and Scope
This protocol details a non-contact method for quantifying blink parameters using high-frame-rate video capture, suitable for long-term monitoring in natural environments [27]. The approach overcomes limitations of traditional bio-signal methods like electro-oculography (EOG) that require physical attachments and are susceptible to signal artifacts from facial muscle contractions [27].
Equipment Setup
- Camera System: High-frame-rate camera capable of ≥240 fps capture (e.g., Casio EX-ZR200 or smartphone with high-speed video capability) [27]
- Spatial Resolution: Minimum 512×384 pixels, though higher resolutions (1920×1080) improve accuracy [27]
- Lighting: Consistent ambient lighting to minimize pupil adaptation effects
- Positioning: Camera mounted above display monitor, focused on participant's facial region
Data Acquisition Procedure
- Participant Positioning: Position participant 50-70 cm from camera with face centered in frame
- Calibration: Record 30-second baseline with participant maintaining open gaze for reference measurements
- Task Administration: Present visual stimuli on monitor while recording facial video
- Duration: Capture sessions of 10-15 minutes, allowing for natural variation in blink patterns
Data Processing Pipeline
Table 2: Video Processing Workflow for Blink Parameter Extraction
| Processing Stage | Algorithm/Method | Output |
|---|---|---|
| Face Detection | Haar cascades or deep learning models | Bounding coordinates of facial region |
| ROI Extraction | Facial landmark detection | Specific eye region coordinates |
| Blink Segmentation | Grayscale intensity profiling or event signal generation [27] | Putative blink sequences (excluding flutters/microsleeps) |
| Parameter Quantification | Frame-by-frame eyelid position analysis [27] | Duration, amplitude, velocity metrics |
| Classification | Threshold-based or machine learning classification | Voluntary vs. spontaneous blink identification |
Protocol 2: Machine Learning-Based Voluntary Blink Detection
Purpose and Scope
This protocol implements a real-time blink detection system using machine learning classification to distinguish voluntary blinks from spontaneous blinks for human-computer interaction [25]. The system operates using consumer-grade hardware, enhancing accessibility and deployment potential.
System Architecture
- Hardware: Standard webcam (30 fps minimum, higher rates preferred)
- Software Pipeline: Face detection → face alignment → ROI extraction → eye-state classification [25]
- Auxiliary Components: Rotation compensation, ROI quality assessment, temporal filtering
Training Dataset Development
- Data Collection: Capture eye-state images under varied lighting conditions and head positions
- Dataset Annotation: Manually label images as "open", "closed", or "partial" states
- Dataset Partitioning: Create separate training, validation, and test sets (e.g., 70/15/15 split)
Model Training and Validation
- Algorithm Selection: Train both CNN (non-linear classification) and SVM (linear separation) models for comparison [25]
- Performance Metrics: Evaluate using accuracy, precision, recall, and F1-score
- Cross-Validation: Test performance across multiple datasets (e.g., CeW, ZJU, Eyeblink) [25]
- Real-Time Implementation: Optimize model for inference speed to achieve real-time performance
Visualization of Blink Processing Workflows
Blink Detection and Classification Pathway
Neural Control of Voluntary Blinking
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Blink Communication Research
| Item | Specification | Research Function |
|---|---|---|
| High-Speed Camera | ≥240 fps, ≥512×384 resolution [27] | Captures blink kinematics with sufficient temporal resolution |
| Eye-Openness Algorithm | Pixel-based eyelid distance estimation [22] | Quantifies blink amplitude and completeness directly |
| Blink Classification Dataset | YEC and ABD datasets [25] | Trains and validates machine learning models for eye-state classification |
| Video Processing Pipeline | ROI extraction + intensity profiling [27] | Segments blink events from continuous video data |
| Temporal Filter | Moving average or custom algorithm [25] | Reduces classification noise and improves detection accuracy |
| Performance Metrics Suite | F1-score, accuracy, precision, recall [25] | Quantifies system reliability and communication accuracy |
Communication is a fundamental human need, and its loss represents one of the most profound psychosocial stressors an individual can face. For patients with severe motor impairments resulting from conditions such as Locked-In Syndrome (LIS), amyotrophic lateral sclerosis (ALS), and brainstem injuries, the inability to communicate leads to devastating social isolation and significantly diminished quality of life [28] [29]. This application note explores the intricate relationship between communication loss and psychosocial well-being, framed within the context of emerging blink-controlled communication protocols. We provide a comprehensive analysis of the neurobiological impact of isolation, detailed experimental protocols for blink-based communication systems, and standardized metrics for evaluating their efficacy in restoring social connection and improving patient outcomes.
Psychosocial and Neurobiological Impact of Communication Loss
The Isolation-Health Pathway
Communication loss creates a cascade of detrimental effects on mental and physical health through multiple pathways. Social isolation and loneliness are established independent risk factors for increased morbidity and mortality, with evidence pointing to plausible biological mechanisms [30].
Mental Health Correlates: Robust longitudinal studies demonstrate that social isolation and loneliness significantly increase the risk of developing depression, with the odds more than doubling among those who often feel lonely compared to those rarely or never feeling lonely [30]. Mendelian randomization studies suggest a bidirectional causal relationship, where loneliness both causes and is caused by major depression [30].
Cognitive Consequences: Strong social connection is associated with better cognitive function, while isolation presents risk factors for dementia. Meta-analyses involving over 2.3 million participants show that living alone, smaller social networks, and infrequent social contact increase dementia risk [30].
Physical Health Implications: Substantial evidence links poor social connection to increased incidence of cardiovascular diseases, stroke, and diabetes mellitus [30]. The strength of this evidence has been acknowledged in consensus reports from the National Academy of Sciences, Engineering, and Medicine and the US Surgeon General [30].
Neurobiological Mechanisms
Animal models and human studies reveal specific neurobiological alterations induced by social isolation stress:
HPA Axis Dysregulation: Social separation stress activates the hypothalamic-pituitary-adrenal (HPA) axis, increasing basal corticosterone levels and inducing long-lasting changes in stress responsiveness [31]. These alterations are particularly pronounced when isolation occurs during critical neurodevelopmental periods [31].
Monoaminergic System Alterations: Early social isolation stress induces long-lasting reductions in serotonin turnover and alterations in dopamine receptor sensitivity [31]. These neurotransmitter systems are implicated in addictive, psychotic, and affective disorders, providing a mechanistic link between isolation and mental health pathology.
Neural Circuitry Changes: Social isolation during development alters functional development in medial prefrontal cortex Layer-5 pyramidal cells and enhances activity of inhibitory neuronal circuits [31]. Human studies of severely deprived children show alterations in white matter tracts, though early intervention can rescue some of these changes [31].
Table 1: Neurobiological Correlates of Social Isolation Stress
| Biological System | Observed Alterations | Behavioral Correlates |
|---|---|---|
| HPA Axis | Increased basal corticosterone, CRF activity, glucocorticoid resistance [31] | Heightened stress response, affective dysregulation |
| Serotonin System | Reduced serotonin turnover, altered 5-HIAA concentrations [31] | Increased depression and anxiety-like behaviors |
| Dopamine System | Altered receptor sensitivity [31] | Reward processing deficits, increased addiction vulnerability |
| Neural Structure | Dendritic loss, reduced synaptic plasticity, altered myelination [31] | Impaired executive function, facilitated fear learning |
Blink-Controlled Communication Systems: Technical Approaches
System Classifications and Modalities
Blink-controlled communication systems represent a critical technological approach to restoring communication for severely paralyzed patients. These systems can be broadly categorized into three main types:
No-Tech Systems: Communication relies solely on bodily movements without additional materials. Examples include using specific eye movements (blinking, looking up-down, or right-left) with predetermined meanings [28]. These approaches require both communication partners to be aware of the specific movement-language mapping.
Low-Tech Augmentative and Alternative Communication (AAC): Incorporates materials such as letter boards (e.g., Eye Transfer [ETRAN] Board or EyeLink Board) where selection occurs via eye fixation or blinking [28]. These systems are low-cost but require constant caregiver presence for interpretation.
High-Tech AAC: Utilizes technology including eye-gaze switches, eye tracking, or brain-computer interfaces (BCI) to control electronic devices for communication [28] [29]. These systems offer greater independence but vary significantly in cost and complexity.
Table 2: Comparison of Blink-Controlled Communication Modalities
| System Type | Examples | Cost Range | Advantages | Limitations |
|---|---|---|---|---|
| No-Tech | Blink coding, eye movement patterns [28] | None | Immediately available, no equipment | Limited vocabulary, requires trained partner |
| Low-Tech AAC | E-tran board, EyeLink board [28] [29] | ~$260 [29] | Low cost, portable | Requires observer, slower communication rate |
| High-Tech Sensor-Based | Tobii Dynavox, specialized eye trackers [29] | $5,000-$10,000 [29] | Independent use, larger vocabulary | High cost, technical complexity |
| High-Tech Vision-Based | Blink-To-Live, Blink-to-Code [29] [32] | Low (uses standard hardware) | Cost-effective, adaptable | Lighting dependencies, calibration required |
Specific System Architectures
Blink-To-Live System: This computer vision-based approach utilizes a mobile phone camera to track patient's eyes through real-time video analysis. The system defines four key alphabets (Left, Right, Up, and Blink) that encode more than 60 daily life commands as sequences of three eye movement states [29]. The architecture includes:
- Facial landmarks detection using MediaPipe's face mesh with 468 facial landmarks [32]
- Eye Aspect Ratio (EAR) calculation for blink detection
- Sequence decoding with native speech output
Blink-to-Code System: This implements Morse code communication through voluntary eye blinks classified as short (dot) or long (dash) [32]. The system operates through:
- Real-time EAR calculation from eye landmarks
- Duration-based classification (short blink: 1.0-2.0 seconds, long blink: ≥2.0 seconds)
- Character commitment after pause exceeding 1.0 second, word space after 3.0 seconds
Experimental Protocols and Evaluation Metrics
Protocol for Blink-Based Communication Assessment
Objective: To evaluate the efficacy and usability of blink-controlled communication systems in patients with severe motor impairments.
Participant Selection:
- Inclusion: Diagnosis of LIS, ALS, or severe brainstem injury with preserved eye movements and cognitive function
- Exclusion: Significant visual impairment, profound cognitive deficits, or inability to provide consent
- Sample Size: 5-20 participants based on feasibility (similar to [33] [32])
Experimental Setup:
- Environment: Well-lit, controlled environment with minimal distractions
- Equipment: Standard webcam or mobile device camera positioned approximately 50cm from participant [32]
- Software: Computer vision pipeline (OpenCV, MediaPipe) for facial landmark detection [32]
Assessment Protocol:
- Calibration Phase: Individual calibration of EAR thresholds and blink duration parameters (5 minutes)
- Training Phase: Familiarization with system operation and basic commands (10 minutes)
- Testing Phase:
- Simple phrase communication ("SOS", "YES/NO") - 5 trials each
- Complex phrase communication ("HELP", daily needs) - 5 trials each
- Free communication: Expression of needs or discomfort - 5 minutes
Data Collection:
- Accuracy: Percentage of correctly interpreted commands [32]
- Response Time: Time from initiation to correct message completion [32]
- User Experience: Subjective feedback on ease of use and comfort
- Psychosocial Measures: Pre-post assessment of mood, isolation, and communication satisfaction
Quantitative Performance Metrics
Table 3: Blink-Based Communication System Performance
| Performance Metric | Reported Values | Experimental Context |
|---|---|---|
| Message Accuracy | 62% average (range: 60-70%) [32] | Controlled trials with 5 participants |
| Response Time | 18-20 seconds for short messages [32] | "SOS" and "HELP" messaging tasks |
| ON/OFF State Prediction | AUC-ROC = 0.87 [33] | Parkinson's disease symptom monitoring |
| Dyskinesia Prediction | AUC-ROC = 0.84 [33] | Parkinson's disease symptom monitoring |
| MDS-UPDRS Part III Correlation | ρ = 0.54 [33] | Parkinson's disease symptom severity |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Blink Communication Research
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| MediaPipe Face Mesh | Facial landmark detection for EAR calculation [32] | 468 facial landmarks, real-time processing |
| OpenCV Library | Computer vision operations and image processing [32] | Open-source, supports multiple languages |
| Eye Aspect Ratio (EAR) | Metric for blink detection from facial landmarks [32] | EAR = (‖p2−p6‖+‖p3−p5‖)/(2⋅‖p1−p4‖) |
| Standard Webcam | Video capture for vision-based systems | 720p minimum resolution, 30fps |
| Electromyography (EMG) | Measurement of electrical muscle activity for alternative blink detection [34] | Requires electrodes, higher accuracy but less comfortable |
| E-Tran Board | Low-tech communication reference for validation [29] | Transparent board with printed letters |
| Tobii Dynavox | High-tech eye tracking system for comparative studies [29] | Commercial system, $5,000-$10,000 |
Visualizing System Workflows and Signaling Pathways
Blink Detection and Classification Workflow
Isolation-Communication-Psychosocial Pathway
The implementation of blink-controlled communication protocols represents a critical intervention for addressing the profound psychosocial consequences of communication loss. Evidence demonstrates that these systems can effectively restore basic communication capabilities, thereby mitigating the detrimental effects of social isolation on mental and physical health. While current systems show promising accuracy and usability, further research is needed to optimize response times, expand vocabulary capacity, and enhance accessibility across diverse patient populations and resource settings. The integration of standardized assessment protocols and quantitative metrics, as outlined in this application note, will facilitate comparative effectiveness research and accelerate innovation in this vital area of assistive technology.
Implementing Blink Detection Systems: From Computer Vision to Brain-Computer Interfaces
The Eye Aspect Ratio (EAR) is a quantitative metric central to many modern, non-invasive eye-tracking systems. It provides a computationally simple yet robust method for detecting eye closure by calculating the ratio of distances between specific facial landmarks around the eye. The core principle is that this ratio remains relatively constant when the eye is open but approaches zero rapidly during a blink [35]. This modality is particularly valuable for developing voluntary blink-controlled communication protocols, as it allows for the reliable distinction between intentional blinks and involuntary eye closures using low-cost, off-the-shelf hardware like standard webcams [36] [35]. Its non-invasive nature and high accuracy make it a cornerstone for assistive technologies aimed at patients with conditions like amyotrophic lateral sclerosis (ALS) or locked-in syndrome, enabling communication through coded blink sequences without the need for specialized sensors or electrodes [37] [3].
Core Computational Methodology and Key Parameters
EAR Calculation and Blink Identification
The implementation of EAR begins with the detection of facial landmarks. A typical model identifies six key points (P1 to P6) around the eye, encompassing the corners and the midpoints of the upper and lower eyelids [35]. The EAR is calculated as a function of the vertical eye height relative to its horizontal width, providing a scale-invariant measure of eye openness.
The formula for the Eye Aspect Ratio is defined as follows:
EAR = (||P2 - P6|| + ||P3 - P5||) / (2 * ||P1 - P4||)
where P1 to P6 are the 2D coordinates of the facial landmarks. This calculation results in a single scalar value that is approximately constant when the eye is open and decreases towards zero when the eye closes [35]. A blink is detected when the EAR value falls below a predefined threshold. Empirical research has identified 0.18 to 0.20 as an optimal threshold range, offering a strong balance between sensitivity and specificity [35]. For robust detection against transient noise, a blink is typically confirmed only if the EAR remains below the threshold for a consecutive number of frames (e.g., 2-3 frames in a 30 fps video stream).
Quantitative Performance Data
The following table summarizes key performance metrics and parameters for EAR-based blink detection systems as established in recent literature.
Table 1: Performance Metrics and System Parameters for EAR-based Blink Detection
| Parameter / Metric | Reported Value / Range | Context and Notes | Source |
|---|---|---|---|
| Optimal EAR Threshold | 0.18 - 0.20 | Lower thresholds (e.g., 0.18) provide best accuracy; higher values decrease performance. | [35] |
| Typical Open-Eye EAR | ~0.28 - 0.30 | Baseline value for an open eye; subject to minor individual variation. | [35] |
| Accuracy (Model) | Up to 99.15% | Achieved by state-of-the-art models (e.g., Vision Transformer) on eye-state classification tasks. | [38] |
| Spontaneous Blink Rate | 17 blinks/minute (average) | Varies with activity: 4-5 (low) to 26 (high) blinks per minute. | [35] |
| Blink Duration (from EO signal) | ~60 ms longer than PS-based detection | Eye Openness (EO) signal provides more detailed characterization. | [22] |
| Key Advantage | Simplicity, efficiency, real-time performance | Requires only basic calculations on facial landmark coordinates. | [35] |
Experimental Protocols and Workflows
Protocol for Real-Time Blink Detection for Communication
This protocol outlines the steps to implement a real-time blink detection system for a voluntary blink-controlled communication aid.
- Hardware Setup: Use a standard computer or smartphone with a built-in or external webcam. Ensure adequate and consistent lighting on the user's face to minimize shadows and glare [39].
- Software Initialization:
- Initialize the camera with a resolution of at least 640x480 pixels and a frame rate of 30 fps.
- Load a pre-trained facial landmark detector (e.g., the 68-point model from Dlib).
- System Calibration:
- Position the user so their face is clearly visible to the camera.
- The system may optionally record a short (5-10 second) baseline video of the user with eyes open and closed to fine-tune the EAR threshold, though a default of 0.18 can be used [35].
- Real-Time Processing Loop:
- Frame Capture: Acquire a video frame.
- Face and Landmark Detection: Detect the face in the frame and localize the 6 periocular landmarks for each eye.
- EAR Calculation: Compute the EAR for each eye using the formula in Section 2.1.
- Blink Classification: Compare the EAR to the threshold. If the EAR is below the threshold for 3 consecutive frames, register a "blink" event.
- Communication Protocol Logic:
- Implement a state machine to interpret blink sequences. For example:
- A short blink (below a duration threshold, e.g., 1 second) could select a menu item.
- A long blink (exceeding a duration threshold) could activate a command.
- A series of two blinks in quick succession could represent a special command.
- Map decoded sequences to pre-defined phrases or commands, which are then displayed on screen or converted to synthesized speech [36].
- Implement a state machine to interpret blink sequences. For example:
Protocol for Validation Against Ground Truth
To validate the accuracy of an EAR-based blink detector, the following protocol is recommended.
- Dataset Curation:
- Utilize publicly available datasets such as the MRL Eye Dataset, Eyeblink8, or TalkingFace which contain annotated videos of eyes in open and closed states [35] [38].
- Alternatively, create a custom dataset with simultaneous recording using a high-speed camera and a validated method like Electrooculography (EOG) to establish ground truth [22].
- Annotation:
- Manually or semi-automatically label every frame in the validation dataset with the ground truth eye state ("open" or "closed").
- Performance Metrics Calculation:
- Run the EAR detection algorithm on the dataset.
- Compare the algorithm's output against the ground truth labels frame-by-frame.
- Calculate standard classification metrics: Accuracy, Precision, Recall, F1-Score, and Area Under the Curve (AUC) of the Receiver Operating Characteristic (ROC) curve [35] [38].
Table 2: The Scientist's Toolkit: Essential Research Reagents and Solutions
| Item / Solution | Function / Description | Example / Specification |
|---|---|---|
| Facial Landmark Detector | Detects and localizes key facial points (eyes, nose, mouth) required for EAR calculation. | Dlib's 68-point predictor; Multi-task Cascaded Convolutional Networks (MTCNN). |
| Eye State Datasets | Provides standardized data for training and validating blink detection models. | MRL Eye Dataset [38]; TalkingFace Dataset [35]; NTHU-DDD [38]. |
| Computer Vision Library | Provides foundational algorithms for image processing, video I/O, and matrix operations. | OpenCV (Open Source Computer Vision Library). |
| Webcam / Infrared Camera | The hardware sensor for capturing video streams of the user's face. | Standard USB webcam (for visible light); IR-sensitive camera with IR illuminators (for dark conditions). |
| Video-Oculography (VOG) System | A high-accuracy, commercial reference system for validating blink parameters and eye movements. | Tobii Pro Spectrum/Fusion (provides eye openness signal) [22]; Smart Eye Pro. |
| Deep Learning Frameworks | Enables the development and deployment of advanced models for gaze and blink estimation. | TensorFlow, PyTorch; Pre-trained models like VGG19, ResNet, Vision Transformer (ViT) [37] [38]. |
System Integration and Workflow Visualization
The integration of EAR detection into a functional communication system involves a multi-stage pipeline. The workflow below illustrates the pathway from image acquisition to command execution, which is critical for building robust assistive devices.
Diagram 1: Real-Time Blink Detection and Command Workflow. This flowchart outlines the sequential process of capturing video, processing each frame to detect blinks using the Eye Aspect Ratio (EAR), and translating consecutive blinks into a functional command for communication.
The logic for classifying blinks and interpreting them into commands relies on a well-defined state machine. The following diagram details the decision-making process for categorizing blinks and managing the timing of a communication sequence.
Diagram 2: Blink Classification and Sequence Logic. This chart details the process of classifying a detected blink by its duration and managing the timing for concluding a command sequence, which is fundamental for protocols like Blink-To-Live [36].
Electroencephalography (EEG) provides a non-invasive method for detecting voluntary eye blinks, which is a critical capability for developing brain-computer interface (BCI) systems for patients with severe motor impairments. These systems enable communication by translating intentional blink patterns into control commands. The detection of blinks from EEG signals leverages the high-amplitude artifacts generated by the electrical activity of the orbicularis oculi muscle and the retinal dipole movement during eye closure [40] [9]. This document details the experimental protocols and analytical frameworks for reliably identifying and classifying blink events from EEG data, with a specific focus on applications in assistive communication devices.
Physiological Basis of the EEG Blink Signal
The blink artifact observed in EEG recordings is a complex signal originating from both myogenic and ocular sources. Blinking involves the coordinated action of the levator palpebrae superioris and orbicularis oculi muscles [40]. This muscle activity generates electrical potentials that are readily detected by scalp electrodes. Furthermore, the eye itself acts as a corneal-retinal dipole, with movement during a blink causing a significant shift in the electric field, which is picked up by EEG electrodes [9].
The resulting blink artifact is characterized by a high-amplitude, sharp waveform, often exceeding 100 µV, which is substantially larger than the background cortical EEG activity [40]. This signal is most prominent over the frontal brain regions, particularly at electrodes Fp1, Fp2, Fz, F3, and F4, due to their proximity to the eyes [40]. The stereotypical morphology and high signal-to-noise ratio make blinks an excellent candidate for detection and classification in BCI systems.
Table 1: Key Electrode Locations for Blink Detection
| Electrode | Location | Sensitivity to Blinks |
|---|---|---|
| Fp1 | Left frontal pole, above the eye | Very High |
| Fp2 | Right frontal pole, above the eye | Very High |
| Fz | Midline frontal | High |
| F3 | Left frontal | Moderate to High |
| F4 | Right frontal | Moderate to High |
Detection Methodologies and Performance
Research has explored a wide spectrum of methodologies for blink detection, from traditional machine learning to advanced deep learning architectures. The choice of methodology often involves a trade-off between computational efficiency, required hardware complexity, and classification accuracy.
Hardware Configurations and Comparative Performance
Recent studies demonstrate that effective blink detection is achievable even with portable, low-density EEG systems, enhancing the practicality of BCI for everyday use.
Table 2: Comparison of Blink Detection Modalities and Performances
| Modality / Approach | Key Methodology | Reported Performance | Advantages |
|---|---|---|---|
| Portable 2-Channel EEG [41] | 21 features + Machine Learning (Leave-one-subject-out) | Blinks: 95% acc.; Horizontal movements: 94% acc. | High portability, quick setup, comparable to multi-channel systems |
| 8-Channel Wearable EEG [42] | XGBoost, SVM, Neural Network | Multiple blinks classification: 89.0% accuracy | Classifies no-blink, single-blink, and consecutive two-blinks |
| 8-Channel Wearable EEG [42] | YOLO (You Only Look Once) model | Recall: 98.67%, Precision: 95.39%, mAP50: 99.5% | Superior for real-time detection of multiple blinks in a single timeframe |
| Wavelet + Autoencoder + k-NN [43] | Crow-Search Algorithm optimized k-NN | Accuracy: ~96% across datasets | Combines robust feature extraction with optimized traditional ML |
| Deep Learning (CNN-RNN) [40] | Hybrid Convolutional-Recurrent Neural Network | Healthy: 95.8% acc. (5 channels); PD: 75.8% acc. | Robust in clinical populations (e.g., Parkinson's disease) |
Signaling Pathway of the Blink Reflex
The following diagram illustrates the neural pathway involved in the blink reflex, which underlies the generation of the observable EEG signal.
Experimental Protocols for Blink Detection
This section provides a detailed, step-by-step protocol for setting up an experiment to acquire EEG signals for voluntary blink detection, based on standardized methodologies from recent literature.
Protocol: EEG Data Acquisition for Voluntary Blinks
Objective: To collect high-quality EEG data corresponding to predefined voluntary blink patterns for developing a BCI communication system.
Materials:
- EEG system (amplifier and cap, minimum 2 channels, 8+ recommended)
- Electrolyte gel or saline solution
- A computer with stimulus presentation software (e.g., PsychoPy, E-Prime, or custom MATLAB/Python script)
- Electrically shielded and quiet room
Procedure:
Participant Preparation:
- Obtain informed consent and explain the task.
- Fit the EEG cap, ensuring electrodes Fp1, Fp2, Fz, F3, and F4 are correctly positioned according to the 10-20 international system.
- Apply electrolyte gel to achieve electrode impedances below 10 kΩ, which is critical for obtaining a clean signal.
Experimental Task Design:
- Present visual or auditory cues on a computer screen to instruct the participant to perform specific blink actions. A sample trial structure is as follows [42]:
- Rest Period (3-5 seconds): A fixation cross is displayed. The participant is instructed to relax and avoid blinking.
- Cue Period (2 seconds): A text or symbol cue indicates the required blink pattern. Standard cues include:
- "Single Blink"
- "Double Blink" (two consecutive blinks)
- Execution Period (3 seconds): The participant performs the cued blink action.
- Repeat each trial type (e.g., no-blink, single-blink, double-blink) for a minimum of 30-50 repetitions to gather sufficient data for model training and validation. Randomize the trial order to prevent habituation.
- Present visual or auditory cues on a computer screen to instruct the participant to perform specific blink actions. A sample trial structure is as follows [42]:
Data Recording:
- Set the EEG amplifier to a sampling rate of at least 250 Hz (512 Hz is common) [40].
- Apply an online band-pass filter (e.g., 0.1 - 30 Hz) during acquisition to attenuate high-frequency noise and slow drifts [42].
- Record trigger signals from the stimulus presentation software synchronously with the EEG data to mark the onset of each cue and execution period.
Data Processing and Feature Extraction Workflow
The raw EEG data must be processed and transformed to extract meaningful features for blink classification. The following workflow is recommended.
Step-by-Step Protocol:
Pre-processing:
- Filtering: Apply a zero-phase band-pass filter (e.g., 1-15 Hz) to isolate the frequency components most relevant to blinks and remove high-frequency muscle noise and slow drifts [42] [40].
- Segmentation: Segment the continuous EEG data into epochs (e.g., -0.5 to +3 seconds relative to the cue onset) for each trial.
Feature Extraction:
- Extract a suite of features from each EEG epoch to characterize the blink signal. The following features have proven effective [42] [43]:
- Time-Domain Features: Maximum amplitude, Root Mean Square (RMS), Signal Magnitude Area (SMA).
- Amplitude-Driven Features: Peak-to-peak amplitude, Area Under the Curve (AUC).
- Statistical Features: Mean, variance, skewness, kurtosis of the signal.
- Time-Frequency Features: Apply Wavelet Transform (e.g., using Morlet wavelets) to capture joint time-frequency information, which is highly effective for representing non-stationary blink signals [43].
- Extract a suite of features from each EEG epoch to characterize the blink signal. The following features have proven effective [42] [43]:
Model Training and Classification:
- Model Selection: For rapid prototyping, begin with traditional machine learning models like Crow-Search-Optimized k-NN [43] or Support Vector Machines (SVM) [42], which offer high performance with interpretable results.
- Deep Learning: For maximum accuracy, especially in complex classification tasks (e.g., single vs. double blinks), implement a hybrid CNN-RNN architecture [40] or the YOLO model [42].
- Validation: Use leave-one-subject-out (LOSO) cross-validation to rigorously evaluate model generalizability to new, unseen users [41].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Solutions for EEG Blink Detection
| Item | Function / Application | Examples / Notes |
|---|---|---|
| Multi-channel EEG System | Recording electrical brain activity. | BioSemi Active II, Ultracortex "Mark IV" headset [42] [44]. A portable 2-channel system can be sufficient [41]. |
| Electrolyte Gel | Ensuring high-conductivity, low-impedance connection between scalp and electrodes. | Standard EEG conductive gels. |
| Stimulus Presentation Software | Delivering precise visual/auditory cues to guide voluntary blink tasks. | PsychoPy, E-Prime, MATLAB, Python. |
| Signal Processing Toolboxes | Pre-processing, feature extraction, and model implementation. | EEGLAB, MNE-Python, BLINKER toolbox [44]. |
| Machine Learning Libraries | Building and training blink classification models. | Scikit-learn (for SVM, k-NN), XGBoost, PyTorch/TensorFlow (for CNN, RNN, YOLO) [42] [43] [40]. |
Electrooculography (EOG) leverages the corneo-retinal standing potential inherent in the human eye to detect and record eye movements and blinks. This potential, which exists between the positively charged cornea and the negatively charged retina, acts as a biological dipole. When the eye rotates, this dipole moves relative to electrodes placed on the skin around the orbit, producing a measurable change in voltage [45]. Blinks, characterized by a rapid, simultaneous movement of both eyelids, induce a distinctive high-amplitude signal due to the upward and inward rotation of the globe (Bell's phenomenon). This technical note details the application of EOG within a research framework focused on developing a voluntary blink-controlled communication protocol for patients with severe motor disabilities, such as those in advanced stages of Amyotrophic Lateral Sclerosis (ALS) or Locked-In Syndrome (LIS). The non-invasive nature and relatively simple setup of EOG make it a viable tool for creating assistive technologies that rely on intentional, voluntary blinks as a binary or coded control signal.
Key Principles and Quantitative Blink Data
A comprehensive understanding of blink characteristics is fundamental to designing robust detection algorithms. Blinks are categorized into three types: voluntary (intentional), reflexive (triggered by external stimuli), and spontaneous (unconscious). For communication protocols, the reliable identification of voluntary blinks is paramount. The table below summarizes key quantitative metrics for spontaneous blinks, which serve as a baseline for distinguishing intentional blinks, derived from eye-tracking studies [45].
Table 1: Quantitative Characteristics of Spontaneous Blinks in Healthy and Clinical Populations
| Characteristic | Healthy Adults (Baseline) | Parkinson's Disease (PD) Patients | Notes and Correlations |
|---|---|---|---|
| Blink Rate (BR) | 15-20 blinks/minute | Significantly reduced | In PD, BR is negatively correlated with motor deficit severity and dopamine depletion [45]. |
| Blink Duration (BD) | 100-400 milliseconds | Significantly increased | In PD, increased BD is linked to non-motor symptoms like sleepiness rather than motor severity [45]. |
| Blink Waveform Amplitude | 50-200 µV (EOG) | Not specifically quantified in search results | Amplitude is highly dependent on electrode placement and individual physiological differences. |
| Synchrony | Tendency to synchronize blinking with observed social cues [46] | Not reported | This synchrony is attenuated in adults with ADHD symptoms, linked to dopaminergic and noradrenergic dysfunction [46]. |
Experimental Protocol: EOG Setup and Blink Detection for Communication Paradigms
This protocol provides a step-by-step methodology for establishing an EOG system to acquire corneo-retinal potentials for the purpose of voluntary blink detection.
Research Reagent and Equipment Solutions
Table 2: Essential Materials for EOG-based Blink Detection Research
| Item | Function/Explanation | Example Specifications |
|---|---|---|
| Disposable Ag/AgCl Electrodes | To ensure stable, low-impedance electrical contact with the skin for high-quality signal acquisition. | Pre-gelled, foam-backed, 10 mm diameter. |
| Biopotential Amplifier & Data Acquisition (DAQ) System | To amplify the microvolt-level EOG signal and convert it to digital data for processing. | Input impedance >100 MΩ, Gain: 1000-5000, Bandpass Filter: 0.1-30 Hz. |
| Electrode Lead Wires | To connect the skin electrodes to the amplifier. | Shielded cables to reduce 50/60 Hz power line interference. |
| Skin Prep Kit (Alcohol wipes, Abrasive gel) | To clean and reduce dead skin cells, thereby lowering skin impedance for a clearer signal. | 70% Isopropyl Alcohol wipes, mild skin preparation gel. |
| Electrode Adapters/Strap | To secure electrodes in place around the eye orbit. | Headbands or specialized adhesive rings. |
| Signal Processing Software | To implement real-time or offline blink detection algorithms (thresholding, template matching). | MATLAB, Python (with libraries like SciPy and NumPy), or LabVIEW. |
Step-by-Step Procedure
Participant Preparation and Electrode Placement:
- Inform the participant about the procedure and obtain consent. Ensure they are seated comfortably.
- Clean the skin areas around both eyes with an alcohol wipe and allow to dry.
- Apply five electrodes per eye for robust differential measurement:
- Right Outer Canthus (ROC): ~1 cm lateral to the right eye's outer corner.
- Left Outer Canthus (LOC): ~1 cm lateral to the left eye's outer corner.
- Above Right Eye (Supraorbital): ~2 cm above the eyebrow on the forehead.
- Below Right Eye (Infraorbital): ~2 cm below the lower eyelid.
- Reference (Ground): On the center of the forehead or mastoid bone.
- Connect the lead wires to the corresponding electrodes.
System Calibration and Signal Acquisition:
- Connect the leads to the biopotential amplifier and DAQ system.
- Instruct the participant to look straight ahead at a fixed point to establish a baseline.
- Perform a calibration routine: Ask the participant to look sequentially at targets (e.g., left, right, up) to map E signal voltage to eye position.
- Initiate data recording. The vertical EOG channel (difference between supraorbital and infraorbital electrodes) will be the primary source for blink detection.
Blink Detection Algorithm (Offline/Real-time):
- Bandpass Filter: Apply a digital bandpass filter (e.g., 0.1-15 Hz) to the raw EOG signal to remove slow drifts and high-frequency noise.
- Threshold Detection: Calculate the signal's moving average and standard deviation. Define a blink event when the signal amplitude exceeds a set threshold (e.g., 4-5 times the standard deviation above the baseline).
- Morphological Check: Implement checks based on blink duration (e.g., 100-500 ms) to distinguish true blinks from noise spikes or saccades.
- Voluntary Blink Identification: For communication protocols, use timing patterns (e.g., a double blink within a specific time window) or count-based sequences (e.g., three blinks for "yes") to decode intentional commands from spontaneous blinks.
Signaling Pathways and Workflow Visualization
The following diagrams illustrate the logical workflow for a blink-controlled communication system and the underlying neurophysiological pathway.
Experimental Workflow for Blink-Controlled Communication
Neurophysiological Pathway of a Voluntary Blink
Discussion and Application in Patient Research
The primary application of this protocol is the development of a voluntary blink-controlled communication system. Such a system translates specific blink patterns into commands, enabling patients to spell words, select pre-defined phrases, or control their environment. The reliability of this system hinges on accurately differentiating voluntary blinks from spontaneous and reflexive ones, a task that can be improved by analyzing the subtle differences in their duration and waveform morphology [45].
Furthermore, the EOG signal itself may offer insights beyond mere command detection. As blink rate and duration are modulated by central dopamine levels [45] [46], longitudinal EOG recording could potentially serve as a non-invasive biomarker for tracking disease progression or therapeutic efficacy in neurodegenerative disorders like Parkinson's disease within clinical trial settings. The documented attenuation of blink synchrony as a social cue in conditions like ADHD [46] further underscores the potential of EOG to probe the integrity of neural circuits underlying social cognition, opening avenues for research in neurodevelopmental disorders.
Voluntary blink-controlled communication protocols represent a critical advancement in the field of assistive technology, enabling individuals with severe motor impairments, such as amyotrophic lateral sclerosis (ALS) or paralysis, to communicate through intentional eye movements [23]. These systems function by translating specific blink patterns into discrete commands, forming a complete encoding scheme from simple alerts to complex character-based communication similar to Morse code. The fundamental premise involves using blink duration, count, and laterality (unilateral or bilateral) as the basic encoding units for information transmission. This approach leverages the fact that eye movements often remain functional even when most other voluntary muscles are paralyzed, making blink-based systems particularly valuable for patients who have lost other means of communication [23].
Experimental Protocols and Methodologies
Blink Detection System Design
Research into blink-controlled interfaces has employed various detection methodologies, each with distinct advantages and limitations [23]:
- Pressure Sensor Systems: Thin-film pressure sensors capture delicate surface muscle pressure alterations around the ocular region. This approach provides excellent temporal synchronization, avoids the need for conductive gels, and maintains stable operation under various environmental conditions without being affected by illumination, noise, or electromagnetic interference [23].
- Computer Vision Methods: These systems use camera-based tracking of eye movements and blink gestures. While inexpensive and obtainable, they involve complex image processing algorithms, require significant computational power, restrict head movements, and are sensitive to environmental lighting conditions [23].
- Bioelectrical Signal Detection: Surface electromyography (sEMG) electrodes capture electrical signals from muscles involved in blinking. Though offering good temporal resolution, these signals are sensitive to interference and typically require conductive gels that cause discomfort during prolonged use [23].
- Infrared-Based Methods: These systems provide higher recognition accuracy but are highly susceptible to light interference and potentially pose risks with prolonged eye exposure to infrared radiation [23].
Table: Comparison of Blink Detection Methodologies
| Method | Accuracy | Advantages | Limitations |
|---|---|---|---|
| Pressure Sensors | High (up to 96.75%) [23] | Stable in various environments, no light sensitivity | Physical contact required |
| Computer Vision | Variable | Non-contact, easily deployable | Sensitive to lighting, computational intensive |
| Bioelectrical Signals | Good temporal resolution | Direct muscle signal capture | Requires electrodes, sensitive to interference |
| Infrared-Based | High recognition accuracy | Precise tracking | Potential eye safety concerns, light interference |
Quantitative Analysis of Blink Actions
Research has systematically evaluated different blink actions to determine their suitability for communication encoding. A comprehensive study examined six distinct voluntary blink actions, measuring their recognition accuracy and temporal characteristics [23]:
Table: Performance Metrics of Voluntary Blink Actions
| Blink Action | Recognition Accuracy | Total Completion Time (ms) | Blink Duration (ms) | Inter-Blink Interval (ms) |
|---|---|---|---|---|
| Single Bilateral (SB) | 96.75% | 827 ± 124 | 265 ± 62 | 562 ± 131 |
| Single Unilateral (SU) | 95.62% | 1069 ± 147 | 268 ± 58 | 801 ± 142 |
| Double Bilateral (DB) | 94.75% | 1127 ± 151 | 512 ± 94 | 615 ± 117 |
| Double Unilateral (DU) | 94.00% | 1321 ± 162 | 517 ± 89 | 804 ± 138 |
| Triple Bilateral (TB) | 93.00% | 1421 ± 174 | 758 ± 127 | 663 ± 124 |
| Triple Unilateral (TU) | 92.00% | 1575 ± 183 | 761 ± 122 | 814 ± 139 |
The data indicates that as blink count increases, recognition accuracy decreases, likely due to increased muscle fatigue affecting motion magnitude [23]. Single bilateral blinks demonstrated the highest recognition accuracy and fastest completion time, making them ideal for high-priority commands or frequently used characters in an encoding scheme.
Blink Encoding Schemes
Fundamental Encoding Parameters
Blink-based communication protocols utilize three primary parameters for encoding information:
- Blink Count: The number of consecutive blinks (single, double, or triple) can represent different categories of commands or characters [23].
- Laterality: Unilateral (left or right eye only) versus bilateral (both eyes) blinks enable expanded vocabulary within the same count sequences [23].
- Timing Patterns: The duration of blinks and intervals between blinks create additional encoding possibilities, similar to Morse code's dots and dashes.
Strategic Blink Timing in Learning Phases
Human studies have demonstrated that individuals quickly learn to adapt their blinking behavior strategically to optimize information processing. In controlled detection experiments, participants learned to suppress blinks during periods of high event probability and compensate with increased blinking afterward [47]. This adaptive behavior followed a predictable learning curve, reaching steady state after approximately 13 trials [47]. A computational model capturing this behavior formalizes blinking as optimal control in trading off intrinsic costs for blink suppression with task-related costs for missing events under perceptual uncertainty [47]. This strategic adaptation is crucial for designing effective blink-encoding schemes that minimize information loss during critical communication moments.
Research Reagent Solutions Toolkit
Table: Essential Materials for Blink-Controlled Communication Research
| Research Tool | Function | Application Context |
|---|---|---|
| Thin-Film Pressure Sensors | Captures surface muscle pressure alterations during blinks | Primary detection method for wearable blink interfaces [23] |
| Surface EMG Electrodes | Records electrical activity from orbicularis oculi muscle | Bioelectrical signal detection for blink recognition [23] |
| Infrared Eye Tracking Systems | Non-contact detection of eyelid movement | Vision-based blink detection for screen-based applications [23] |
| Head-Mounted Display Units | Presents visual stimuli and feedback | AR/VR integration for blink-controlled interfaces [23] |
| Data Acquisition Hardware | Converts analog signals to digital format | Signal processing for all sensor-based detection methods [23] |
| MATLAB/Python with Signal Processing Toolboxes | Analyzes temporal patterns of blink signals | Algorithm development for blink pattern recognition [23] |
System Implementation and Validation
Experimental Workflow
The following diagram illustrates the complete experimental workflow for developing and validating blink-controlled communication systems:
Application Testing Protocol
Research protocols typically validate blink-controlled communication systems through practical implementation tasks. One common validation approach involves controlling external devices such as toy cars or computer interfaces using the recommended blink actions [23]. This real-world testing evaluates:
- Practical Usability: Assessing how effectively users can execute commands without excessive cognitive load or physical discomfort.
- System Reliability: Measuring performance consistency across multiple sessions and under varying environmental conditions.
- User Satisfaction: Collecting subjective feedback through standardized instruments like the System Usability Scale (SUS) [23].
Performance metrics during validation typically focus on task completion rates, error frequencies, and temporal efficiency, providing comprehensive data for system refinement.
Compliance and Accessibility Considerations
Blink-controlled communication systems must adhere to accessibility standards, particularly when implemented in digital interfaces. The Web Content Accessibility Guidelines (WCAG) 2.2 Level AA compliance requires [48]:
- Non-Text Contrast: Visual information required to identify user interface components must have a contrast ratio of at least 3:1 against adjacent colors [49].
- Keyboard Navigation: All functionality must be accessible via keyboard interfaces for users unable to perform blink gestures [48].
- Error Prevention: Systems should provide suggestions and warnings to prevent data entry mistakes, crucial for communication applications [48].
These guidelines ensure that blink-controlled systems remain accessible to users with diverse abilities and provide alternative input methods when blink detection may be compromised.
Voluntary blink-controlled communication protocols represent a promising assistive technology pathway, with encoding schemes ranging from simple alerts to complex Morse code-like systems. The experimental evidence indicates that single bilateral, double bilateral, and single unilateral blinks offer the optimal balance of recognition accuracy and temporal efficiency for most communication applications [23]. Future research directions should address current limitations in non-contact detection methods, expand encoding vocabulary through combination patterns, and improve adaptive algorithms that account for user fatigue and individual differences in blink characteristics [23]. As these technologies evolve, standardized encoding schemes will enhance interoperability across platforms and applications, ultimately improving quality of life for patients relying on blink-based communication systems.
The integration of voluntary blink-controlled communication protocols (vBCCP) within patient care systems represents a transformative advancement in assistive technology. For patients with conditions such as locked-in syndrome, advanced amyotrophic lateral sclerosis (ALS), or tetraplegia, voluntary blinks remain a reliable, consciously controlled biological signal for communication [3]. These protocols decode specific blink patterns into digital commands, enabling patients to trigger alerts and communicate needs. However, the clinical utility of these systems depends critically on their integration with robust, multi-channel healthcare provider alerting systems. This application note details the protocols and technical considerations for creating a seamless pipeline from blink detection to healthcare provider notification via SMS, email, and voice calls, ensuring timely medical intervention and enhancing patient autonomy.
Voluntary Blink-Controlled Communication Protocols: Core Technologies
Voluntary blink-controlled systems function by acquiring biosignals associated with eye blinks and translating them into actionable commands [3]. Two primary technological approaches have emerged, each with distinct methodologies for signal acquisition and interpretation.
Computer Vision-Based Detection
This non-contact method uses cameras and algorithms to detect and interpret blink patterns. Modern implementations, such as the SeeMe algorithm, employ vector field analysis to track subtle facial movements with high precision, tagging individual facial pores at a resolution of approximately 0.2 mm [21]. This approach is particularly valuable for detecting low-amplitude, purposeful motor behaviors that often precede overt clinical signs of consciousness in acute brain injury patients [21]. The workflow typically involves:
- Face and Eye Tracking: Often accomplished using a set of trained Haar cascade classifiers [3].
- Blink Classification: distinguishing between voluntary and involuntary blinks using template matching or machine learning classifiers [3] [21].
- Command Mapping: assigning specific sequences (e.g., double-blink, long-blink) to particular alerts or communication outputs.
Wearable Sensor-Based Detection
This method involves a wearable device, such as a smart contact lens, that directly measures physiological changes induced by blinks. A cutting-edge example is a wireless eye-wearable lens that incorporates a mechanosensitive capacitor, an inductive coil, and inherent loop resistance to form an RLC oscillating loop [24]. A conscious blink applies pressure of approximately 30 mmHg on the cornea, deforming the lens and altering its capacitance. This change is wirelessly transmitted as a shift in characteristic resonance frequency, which is then decoded into a control command [24]. This method offers high accuracy and is less susceptible to ambient light or head movement.
Table 1: Comparison of Blink Detection Technologies
| Feature | Computer Vision (e.g., SeeMe) | Wearable Sensor (e.g., EMI Contact Lens) |
|---|---|---|
| Detection Method | Video-oculography (VOG), vector field analysis [21] | Mechanosensitive capacitor in an RLC circuit [24] |
| Key Performance Metric | Detects eye-opening 4.1 days earlier than clinicians in comatose patients [21] | Sensitivity of 0.153 MHz/mmHg in a 0–70 mmHg range [24] |
| Primary Advantage | Non-contact, suitable for early consciousness detection [21] | High precision, wireless, works regardless of head position [24] |
| Key Challenge | Susceptible to lighting conditions and obscuring tubes [21] | Requires biocompatibility and wearability validation [24] |
System Integration Architecture
The end-to-end integration of a vBCCP alerting system requires a structured architecture to ensure reliability and speed. The system must reliably convert a biological signal into a delivered message across multiple channels.
Experimental Protocol: Validating the Integrated System
Objective: To validate the latency, accuracy, and reliability of a fully integrated vBCCP alerting system under simulated clinical conditions.
Methodology:
- Participant Recruitment: Enroll 10 healthy volunteers and 5 patients with voluntary blink control but limited motor function (e.g., ALS patients). Ethical approval and informed consent are mandatory [21].
- System Setup:
- Deploy both a computer vision system (e.g., a camera with the SeeMe algorithm) and a wearable EMI contact lens.
- Connect the signal processing unit to an Alert Manager server.
- Configure the Communication Gateway with valid SMS (e.g., Twilio), email (e.g., SMTP), and voice (e.g., VoIP) services.
- Testing Procedure:
- Participants are instructed to perform a set of predefined voluntary blink sequences (e.g., two rapid blinks for "urgent help," three blinks for "water") in a randomized order.
- Each sequence is performed 20 times per participant.
- The system's response is measured from the onset of the final blink in the sequence to the delivery of the alert to the provider's device.
Table 2: Key Performance Indicators for System Validation
| Key Performance Indicator (KPI) | Target Threshold | Measurement Method |
|---|---|---|
| End-to-End Latency | < 30 seconds | Timestamp comparison between blink detection and alert receipt on end device. |
| Blink Pattern Recognition Accuracy | > 95% | (Number of correctly interpreted commands / Total commands issued) * 100. |
| System Uptime & Reliability | > 99.5% | Monitored system downtime over a 30-day trial period. |
| Alert Delivery Success Rate | > 99% per channel | Delivery status reports from SMS/email gateways and voice call logs. |
The Scientist's Toolkit: Research Reagent Solutions
The development and testing of vBCCP systems rely on a suite of specialized materials and software tools.
Table 3: Essential Research Materials and Reagents
| Item Name | Function/Application | Specification Notes |
|---|---|---|
| Ti3C2Tx MXene | Conductive electrode material in mechanosensitive capacitors for wearable lenses [24]. | Superior conductivity, mechanical flexibility, and biocompatibility; transverse size >3μm. |
| P(VDF-TrFE) | Flexible dielectric layer in capacitive sensors; high dielectric constant [24]. | Poly(vinylidene fluoride-co-trifluoroethylene) layers contribute to high sensitivity. |
| Haar Cascade Classifier | A machine learning object detection program used to locate the face and eyes in video streams [3]. | Pre-trained on facial feature datasets for rapid initialization of blink detection. |
| PsychoPy Software | Open-source Python package for running experiments; presents auditory commands [21]. | Ensures precise timing and presentation of stimuli during protocol testing. |
| Vector Network Analyzer (VNA) | Wirelessly measures the reflection coefficient (S11) to track resonance frequency shifts in RLC-based lenses [24]. | Critical for calibrating and testing the wireless performance of wearable lens systems. |
Implementation Protocols for Alerting Pathways
For an alert to be effective, it must be delivered reliably. The following protocols ensure robust performance across different communication channels. The system must be designed with a failover mechanism, where a delivery failure in one channel (e.g., an undelivered SMS) automatically triggers an attempt via another (e.g., a voice call).
SMS Alerting Protocol
- Message Structure: Alerts must be concise and actionable. Use a standardized template:
[PATIENT ALERT] [Patient ID]: [Alert Type] at [Timestamp]. - Gateway Integration: Employ a reliable SMS API gateway (e.g., Twilio, Plivo). Implement retry logic (e.g., 3 retries with exponential backoff) for failed deliveries.
- Compliance: Ensure adherence to regional telecommunications regulations (e.g., TCPA in the US).
Email Alerting Protocol
- Message Structure: Emails can contain more detail. The subject line should be clear, e.g., "Urgent Patient Alert - Action Required." The body should include patient location, the nature of the alert triggered by the blink command, and any relevant patient data.
- Implementation: Use a server-side SMTP library (e.g., Python's
smtplib, Nodemailer for JS) with TLS encryption. - Reliability: Configure Delivery Status Notifications (DSNs) to track failures and trigger escalation.
Voice Call Alerting Protocol
- Protocol: This is the highest-priority channel for critical alerts. Use a Text-to-Speech (TTS) API or pre-recorded messages delivered via a VoIP provider (e.g., Amazon Connect, Twilio Voice).
- Message Content: The call should clearly state: "This is an automated alert for patient [ID]. The patient has requested [Alert Type]. Please acknowledge this alert by pressing 1."
- Escalation Path: If the call is not answered or acknowledged, the system should follow a pre-defined on-call escalation list.
The seamless integration of voluntary blink-controlled communication protocols with multi-channel alerting systems marks a significant leap forward in patient-centered care. By leveraging robust technologies like computer vision and wireless smart lenses, and coupling them with redundant, fail-safe communication pathways like SMS, email, and voice calls, healthcare providers can create a responsive and reliable environment for some of the most vulnerable patients. The application notes and experimental protocols detailed here provide a foundational framework for researchers and engineers to develop, validate, and deploy these life-changing systems, ultimately bridging the gap between patient intent and clinical response.
Application Notes
The SeeMe tool represents a significant advancement in the detection of covert consciousness in patients with severe brain injuries. This computer vision-based system identifies subtle, voluntary facial movements in response to verbal commands that are typically undetectable by clinical observation alone [21]. Its development addresses the critical clinical challenge of cognitive-motor dissociation (CMD), where an estimated 15-25% of patients labeled as unresponsive retain awareness but lack the motor capacity to demonstrate it [50].
This technology bridges a crucial gap in neurological assessment by enabling earlier detection of consciousness, potentially days before conventional clinical exams can identify signs of recovery. The tool's ability to provide objective, quantifiable data on patient responsiveness offers substantial improvements in prognosis, treatment planning, and rehabilitation strategies for this vulnerable patient population.
Table 1: Detection Capabilities of SeeMe vs. Clinical Examination
| Assessment Metric | SeeMe Tool | Clinical Examination |
|---|---|---|
| Median time to detect eye-opening | 4.1 days earlier than clinicians [21] | Standard clinical detection time |
| Eye-opening detection rate | 85.7% (30/36 patients) [21] | 71.4% (25/36 patients) [21] |
| Mouth movement detection rate | 94.1% (16/17 patients without ET tube) [21] | Not specified |
| Command specificity (eye-opening) | 81% specific to "open your eyes" command [21] | Not applicable |
Table 2: Study Population and Outcomes
| Parameter | Details |
|---|---|
| Patient Population | 37 comatose acute brain injury patients (GCS ≤8) [21] |
| Control Group | 16 healthy volunteers [21] |
| Age Range | 18-85 years [21] |
| Key Finding | Amplitude and number of SeeMe-detected responses correlated with clinical outcome at discharge [21] |
| Primary Significance | Identifies covertly conscious patients with motor behavior undetected by clinicians [21] |
Experimental Protocols
Patient Enrollment and Data Collection Protocol
- Inclusion Criteria: Enroll adults aged 18-85 with acute brain injury (TBI, subarachnoid hemorrhage, meningoencephalitis) and Glasgow Coma Score (GCS) ≤8, excluding those with prior neurological diagnoses [21].
- Baseline Assessment: Conduct video-recorded Coma Recovery Scale-Revised (CRS-R) assessment by trained research team members at each session [21].
- Medication Management: Coordinate with clinical care team to pause sedatives and muscle paralytics at least 15-30 minutes before study sessions when medically safe [21].
- Stimulus Presentation: Use single-use headphones to present auditory commands via PsychoPy software while videotaping patient responses at 30-45 second intervals (±1 second jitter) [21].
SeeMe Algorithm Implementation Protocol
- Command Selection: Present three specific verbal commands: "Stick out your tongue," "Open your eyes," and "Show me a smile" to target distinct facial regions and musculature [21].
- Baseline Recording: Begin with 1-minute resting baseline facial recording without command presentation [21].
- Stimulus Block Design: Present each command in blocks of ten repetitions with randomized inter-stimulus intervals to prevent habituation [21].
- Facial Tracking: Implement vector field analysis to track individual facial pore movements (~0.2mm resolution) in response to auditory stimuli [21].
- Response Validation: Apply machine learning-based classifier to assess command specificity, ensuring movements correspond to appropriate command type [21].
Blinded Rater Assessment Protocol
- Rater Selection: Utilize trained independent raters without knowledge of SeeMe results or clinical examination scores [21].
- Response Criteria: Define positive response as movement occurring within 20 seconds of command presentation in the corresponding facial region, representing deviation from baseline without artifact interference [21].
- Scoring System: Rate each command response in binary fashion (yes/no), with patient considered responsive if achieving three positive ratings out of ten command presentations [21].
- Reliability Assessment: Calculate inter-rater reliability using Cohen's kappa statistic to ensure consistency of human observations [21].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function/Application |
|---|---|
| PsychoPy Software | Open-source Python-based platform for presenting auditory commands and controlling experiment timing [21]. |
| High-Resolution Camera | Captures facial movements at sufficient resolution (~0.2mm) to track pore-level movements for vector field analysis [21]. |
| Single-Use Headphones | Presents standardized auditory stimuli while minimizing external noise interference and maintaining clinical hygiene [21]. |
| Vector Field Analysis Algorithm | Core computational method that quantifies low-amplitude facial movements by tracking discrete facial features across video frames [21]. |
| Machine Learning Classifier | Analyzes response patterns to determine command specificity and distinguish voluntary from involuntary movements [21]. |
| Electrooculography (EOG) | Alternative modality for detecting ocular activity in patients with limited motor function; measures corneo-retinal potential from eye movements [2] [3]. |
Integration with Voluntary Blink Communication Research
The SeeMe tool advances the field of voluntary blink controlled communication protocols by providing a less invasive, more comprehensive assessment approach. Where traditional blink detection systems rely on deliberate blink patterns for communication, SeeMe detects subtle, involuntary attempts at command following that signal emerging consciousness [21] [2].
This computer vision approach offers advantages over electrooculography (EOG)-based systems, which require physical sensors and electrode placement [2]. SeeMe's non-contact method enables continuous monitoring without patient discomfort or equipment burden, making it suitable for acute care settings where traditional blink communication devices may be impractical.
The correlation between SeeMe-detected responses and functional outcomes establishes this technology as both a diagnostic and prognostic tool, creating new opportunities for timing the implementation of intentional blink communication systems as patients progress in recovery.
Workflow and Signaling Diagrams
Diagram 1: SeeMe tool experimental workflow.
Diagram 2: Blink communication protocol integration.
Overcoming Critical Challenges: Accuracy, Fatigue, and Real-World Usability
Application Notes
For patients with severe motor impairments such as locked-in syndrome, amyotrophic lateral sclerosis (ALS), or spinal cord injuries, voluntary eye blinking remains one of the few preserved channels for communication [51] [32]. The fundamental challenge in developing blink-controlled communication protocols lies in reliably distinguishing intentional blinks from spontaneous blinks, which occur approximately 20 times per minute without conscious effort [52]. While these two types of blinks may appear superficially similar, recent research has revealed distinct neurophysiological and kinematic signatures that can be leveraged for classification [51] [53] [54]. This application note synthesizes current advances in blink discrimination technologies and provides detailed protocols for implementing machine learning classification solutions that can form the core of robust assistive communication systems.
Key Neurophysiological and Kinematic Distinctions
The scientific foundation for blink classification rests on demonstrated differences between intentional and spontaneous blinks across multiple modalities. Electroencephalography (EEG) studies have consistently shown that intentional blinks are preceded by a slow negative brain potential called the readiness potential (RP) approximately 1000-100 ms before movement onset, whereas spontaneous blinks lack this preparatory neural signature [51]. In one study, the cumulative EEG amplitude significantly differed between intentional and spontaneous blinks (-1012 µV vs. -158 µV, p = 0.000009), while showing no significant difference between fast and slow intentional blinks, confirming its specific relationship to intentionality rather than kinematics [51].
Kinematic analyses using high-speed motion capture and electromyography (EMG) have further revealed that the orbicularis oculi muscle contracts in complex patterns that vary significantly between blink types [53] [54]. Unlike the traditional model of eyelid movement as simple opening and closing, research has demonstrated segmental neural control producing distinct three-dimensional eyelid trajectories across different blink behaviors [53] [54].
Table 1: Comparative Analysis of Blink Types Across Modalities
| Parameter | Spontaneous Blink | Intentional Blink | Reflexive Blink | Measurement Technique |
|---|---|---|---|---|
| EEG Readiness Potential | Absent or minimal (mean: -158 µV) | Prominent (mean: -1012 µV) | Not reported | EEG cumulative amplitude [-1000ms to -100ms] [51] |
| Primary Function | Ocular lubrication, cognitive reset [22] [52] | Voluntary communication, eye protection | Rapid eye protection from threats | Behavioral context |
| Neural Pathway | Basal ganglia-mediated circuits [55] | Cortical motor pathways [51] | Brainstem reflex pathways | Neuroimaging and lesion studies |
| Orbicularis Oculi Activation | Early lateral-to-medial motion, incomplete closure [54] | Medial deviation early in closure [54] | Large reverberation phase, complete closure [54] | Segmental intramuscular EMG [53] [54] |
| Closure Duration | ~100-200ms [53] [22] | Variable by intent (1.0-2.0+ seconds for Morse code) [32] | Rapid, protective | High-speed video (400 fps) [53] |
| Perceptual Effects | No facilitation of perceptual alternation [52] | Facilitates perceptual alternation in multistable perception [52] | Not studied | Continuous Flash Suppression paradigm [52] |
Machine Learning Approaches and Performance
Machine learning classifiers have demonstrated remarkable efficacy in distinguishing blink types for assistive communication. Different approaches yield varying performance characteristics depending on feature selection and model architecture:
Table 2: Machine Learning Performance for Blink Classification and Application
| Model Type | Application | Key Features | Performance Metrics | Reference |
|---|---|---|---|---|
| eXtreme Gradient Boosted Trees (XGBoost) | PD symptom tracking via blink patterns | Blink confidence, interval, duration derivatives | AUC-ROC: 0.87 (ON/OFF states), 0.84 (dyskinesia) [55] | npj Parkinson's Disease (2025) [55] |
| Computer Vision + Morse Code Decoding | Assistive communication | Eye Aspect Ratio (EAR), blink duration | 62% accuracy, 18-20s response time for messages [32] | Blink-to-Code System (2025) [32] |
| Convolutional Neural Network (CNN) | Volunteer eye-blink detection | Face detection, alignment, eye-state classification | 97.44% accuracy (eye-state), 92.63% F1-Score (blink detection) [25] | Expert Systems with Applications [25] |
| Support Vector Machine (SVM) | Volunteer eye-blink detection | ROI extraction, eye-state classification | Comparable performance to CNN on multiple datasets [25] | Expert Systems with Applications [25] |
Experimental Protocols
Comprehensive Protocol for Multi-Modal Blink Data Acquisition
Equipment and Setup
- EEG System: Minimum 32-channel system with sampling rate ≥1000 Hz, positioned according to international 10-20 system with emphasis on Cz electrode [51]
- Oculographic Recordings: Electrooculogram (EOG) electrodes placed laterally and supra-/infra-orbitally to the dominant eye [51]
- High-Speed Video: Motion capture system capable of ≥400 frames per second with infrared illumination for pupil tracking [53] [55]
- EMG Recordings: Segmental intramuscular wire electrodes inserted in orbicularis oculi by qualified surgeon [53] or surface EMG for non-invasive applications
- Stimulus Presentation: Computer-controlled display for calibration tasks and visual stimuli
Participant Preparation and Calibration
- Participant Positioning: Secure participant in chin rest 50-70 cm from recording devices to minimize head movement [32]
- Electrode Application: Apply EEG electrodes using conductive gel with impedances <5 kΩ; EOG electrodes with identical specifications
- Camera Calibration: Perform nine-point calibration for eye tracking systems; validate with known blink artifacts
- Task Instruction: Provide clear instructions for spontaneous blinking (gaze at fixation cross, stay relaxed) and intentional blinking (self-paced, with varying speeds) [51]
Data Collection Paradigm
Implement a block design with counterbalanced conditions:
- Spontaneous Blink Block (5 minutes): Participants fixate on central cross without conscious blink control [51]
- Intentional Fast Blink Block (5 minutes): Participants perform rapid, self-paced intentional blinks [51]
- Intentional Slow Blink Block (5 minutes): Participants perform slow, exaggerated intentional blinks [51]
- Communication Simulation Block (10 minutes): Participants generate intentional blinks in Morse code patterns to convey simple messages [32]
Signal Processing and Feature Extraction Protocol
EEG Preprocessing and Readiness Potential Quantification
- Filtering: Apply 0.1-30 Hz bandpass filter to raw EEG; notch filter at 50/60 Hz for line noise removal [51]
- Epoch Extraction: Segment data from -2000 ms to +500 ms relative to blink onset defined by EOG threshold crossing
- Baseline Correction: Use -2000 to -1500 ms pre-blink period for baseline adjustment
- Artifact Rejection: Automatically detect and exclude epochs with amplitude differences >200 µV or transient artifacts
- Feature Calculation: Compute cumulative amplitude in -1000 to -100 ms window preceding blink onset [51]
Kinematic Feature Extraction from Video/EOG
- Blink Onset/Offset Detection: Identify blink start and end points using velocity-based thresholding of eyelid position signals
- Amplitude Calculation: Compute maximum displacement of upper eyelid during blink cycle [51]
- Temporal Parameters: Calculate time to peak velocity, closure duration, and opening duration [51] [22]
- Orbicularis Oculi Activation Patterns: For EMG recordings, analyze spatial-temporal activation patterns across different segments of the muscle [53] [54]
Eye Aspect Ratio (EAR) Calculation for Computer Vision Applications
- Facial Landmark Detection: Apply Mediapipe face mesh model to extract 468 facial landmarks [32]
- EAR Computation: Calculate using formula: EAR = (‖p2-p6‖ + ‖p3-p5‖) / (2 * ‖p1-p4‖) where p1-p6 represent specific eye landmarks [32]
- Blink Classification: Identify blinks when EAR values fall below calibrated threshold (typically 0.2-0.3) [32]
Machine Learning Model Training Protocol
Feature Selection and Dataset Construction
- Feature Assembly: Compile multidimensional feature vector containing:
- Data Labeling: Manually annotate blink type based on experimental condition and video verification
- Dataset Splitting: Implement stratified k-fold cross-validation (k=5-10) preserving class distribution across splits
Model Training and Optimization
- Algorithm Selection: Implement multiple classifier types (XGBoost, CNN, SVM) for performance comparison [55] [25]
- Hyperparameter Tuning: Use Bayesian optimization or grid search for parameter optimization
- Class Imbalance Handling: Apply Synthetic Minority Over-sampling Technique (SMOTE) if spontaneous blinks significantly outnumber intentional blinks
- Training Configuration: For XGBoost models, use learning rate=0.05, nestimators=1000, maxdepth=5 with early stopping [55]
Model Validation and Performance Assessment
- Performance Metrics: Calculate accuracy, precision, recall, F1-score, AUC-ROC curves [55] [25]
- Temporal Validation: Ensure models maintain performance across recording sessions and different times of day
- Cross-Participant Validation: Evaluate generalizability through leave-one-subject-out validation
- Real-Time Performance Testing: Assess inference speed to ensure compatibility with real-time communication applications (<100ms processing time) [32] [25]
Visualization Diagrams
Blink Classification Workflow
Neural Pathways in Blink Control
Research Reagent Solutions
Table 3: Essential Research Materials and Equipment for Blink Classification Studies
| Category | Specific Product/Technology | Application Note | Key Features |
|---|---|---|---|
| EEG Recording Systems | 32+ channel EEG with DC-coupled amplifiers | Readiness Potential quantification [51] | High temporal resolution, DC coupling for slow potentials |
| Eye Tracking Systems | Tobii Pro Spectrum, Smart Eye Pro | Eye openness signal measurement [22] | Outputs eye openness metric, 300+ Hz sampling |
| Computer Vision Libraries | Mediapipe Face Mesh | Real-time facial landmark detection [32] | 468 facial landmarks, real-time processing |
| EMG Recording Systems | Intramuscular wire electrodes with high-speed EMG | Segmental orbicularis oculi activation [53] [54] | Fine-wire electrodes for muscle segment analysis |
| Motion Capture Systems | High-speed infrared cameras (400 fps) | 3D eyelid kinematics [53] [54] | Sub-millimeter spatial resolution |
| Machine Learning Frameworks | XGBoost, PyTorch/TensorFlow, OpenCV | Model development and deployment [55] [32] [25] | Optimized for temporal classification tasks |
| Specialized Algorithms | Eye Aspect Ratio (EAR) computation | Blink detection from video [32] | Robust to head movement, lighting changes |
| Clinical Assessment Tools | MDS-UPDRS Part III, SPEED questionnaire | Patient symptom correlation [55] [56] | Validated clinical metrics for correlation studies |
Electroencephalography (EEG)-based brain-computer interfaces (BCIs) represent a transformative technology for establishing communication pathways for individuals with severe motor impairments, including those who rely on voluntary blink-controlled communication systems [57]. These systems enable users to interact with external devices through the detection and interpretation of neural signals and ocular activity [32]. However, EEG signals captured from the scalp are inherently weak and susceptible to various noise sources, including ocular artifacts from eye movements, muscle activity, environmental interference, and equipment-related noise [58] [59]. These contaminants significantly degrade signal quality, necessitating advanced signal processing techniques to extract meaningful neural patterns for reliable blink detection and classification.
The challenge in voluntary blink-controlled communication systems lies in accurately distinguishing intentional blink commands from background neural activity and other artifacts. This requires sophisticated denoising and feature extraction methods to enhance the signal-to-noise ratio (SNR) while preserving the temporal characteristics of blink patterns [32]. Wavelet analysis and autoencoders have emerged as powerful approaches for addressing these challenges, each offering unique advantages for processing non-stationary biological signals like EEG data. This application note provides a comprehensive overview of these signal processing enhancements, detailing experimental protocols and implementation guidelines specifically tailored for blink-controlled communication systems in clinical and research settings.
Technical Foundations of EEG Denoising
EEG signals represent the electrical activity of the brain recorded via electrodes placed on the scalp. These signals typically range from approximately 0.5 to 100 microvolts in amplitude and contain frequency components that are categorized into distinct bands: delta (1-4 Hz), theta (4-7 Hz), alpha (7-12 Hz), beta (13-30 Hz), and gamma (>30 Hz) [59]. Each frequency band correlates with different brain states and functions, with blink artifacts manifesting primarily in the lower frequency ranges.
The principal noise sources affecting EEG signals in blink-controlled systems include:
- Ocular Artifacts: Blinks and eye movements generate electrical potentials that dominate frontal EEG channels
- Muscle Artifacts: Facial muscle contractions introduce high-frequency noise
- Environmental Interference: Power line interference (50/60 Hz) and electromagnetic noise from nearby equipment
- Baseline Wander: Low-frequency drifts caused by perspiration or electrode impedance changes
- Cardiac Artifacts: Electrical activity from heartbeat (ECG) that propagates to EEG electrodes [59]
Comparative Analysis of Denoising Techniques
Table 1: Comparison of EEG Denoising Techniques for BCI Applications
| Technique | Principle | Advantages | Limitations | Suitability for Blink Detection |
|---|---|---|---|---|
| Wavelet Transform | Time-frequency decomposition using mother wavelets | Preserves temporal features of blinks, handles non-stationary signals | Manual threshold selection, mother wavelet dependency | Excellent for precise blink timing extraction |
| Generative Adversarial Networks (GANs) | Two-network architecture (generator & discriminator) | Automatic denoising, retains original signal information | Computationally intensive, requires large datasets | Good for overall signal enhancement |
| Independent Component Analysis (ICA) | Statistical separation of independent sources | Effective for ocular artifact removal | Requires manual component inspection, loses temporal sequence | Moderate (may remove intentional blinks) |
| Convolutional Neural Networks (CNN) | Spatial feature extraction through convolutional layers | Automates feature extraction, high accuracy | Requires precise architecture design | Good for pattern recognition in multi-channel EEG |
| Hybrid CNN-LSTM | Combines spatial and temporal feature extraction | Captures both spatial and temporal dependencies | Complex training, computational demands | Excellent for sequence classification |
Wavelet Analysis for EEG Signal Enhancement
Theoretical Framework of Wavelet Transforms
Wavelet analysis represents signals in both time and frequency domains through the translation and dilation of a mother wavelet function. Unlike Fourier transforms that use infinite sine and cosine functions, wavelets are localized in time, making them particularly suitable for analyzing non-stationary signals like EEG data [60]. The Continuous Wavelet Transform (CWT) provides a redundant but highly detailed time-frequency representation, while the Discrete Wavelet Transform (DWT) offers efficient signal decomposition through iterative filtering operations, making it more suitable for real-time BCI applications [60].
The mathematical foundation of wavelet transforms involves the convolution of the EEG signal with scaled and translated versions of the mother wavelet function. For a given EEG signal x(t), the CWT is defined as: [ CWT(a,b) = \frac{1}{\sqrt{|a|}} \int_{-\infty}^{\infty} x(t) \psi^*\left(\frac{t-b}{a}\right) dt ] where a represents the scaling parameter, b the translation parameter, and ψ the mother wavelet function [60].
Implementation Protocol: Wavelet-Based Denoising
Materials and Equipment:
- Multi-channel EEG acquisition system (e.g., 16-64 channels)
- Ag-AgCl electrodes with standardized placement (10-20 system)
- Signal amplifier with minimum 16-bit resolution
- Computing system with MATLAB/Python and wavelet toolboxes
- Reference datasets for validation (e.g., PhysioNet EEG Motor Movement/Imagery Dataset) [57]
Step-by-Step Procedure:
Signal Acquisition and Preprocessing
- Configure EEG system with sampling rate ≥250 Hz
- Apply band-pass filtering (0.5-40 Hz) to remove extreme frequencies
- Re-reference signals to average reference
- Remove baseline wander using linear detrending
Wavelet Decomposition
- Select appropriate mother wavelet (e.g., Daubechies 4 for blinks)
- Perform 6-level DWT decomposition using Mallat's pyramid algorithm
- Obtain approximation (cA) and detail (cD1-cD6) coefficients
Thresholding and Denoising
- Apply soft thresholding to detail coefficients using Birgé-Massart strategy
- Retain approximation coefficients without modification
- Use scale-dependent thresholds for optimal noise suppression
Signal Reconstruction
- Reconstruct denoised EEG from thresholded coefficients
- Verify temporal alignment with original signal
- Calculate reconstruction error metrics (RMSE, correlation)
Blink Feature Extraction
- Identify characteristic waveforms in reconstructed signal
- Extract temporal features (duration, amplitude, asymmetry)
- Compute morphological descriptors for classification
Table 2: Wavelet Parameters for Blink Artifact Processing
| Parameter | Recommended Setting | Alternative Options | Impact on Performance |
|---|---|---|---|
| Mother Wavelet | Daubechies 4 (db4) | Symlets, Coiflets | db4 matches blink morphology |
| Decomposition Level | 6 | 5-8 based on sampling rate | Balances detail and compression |
| Thresholding Method | Soft thresholding | Hard, SURE, Minimax | Soft preserves blink amplitude |
| Threshold Selection | Birgé-Massart strategy | Universal, Heuristic | Adaptive to noise characteristics |
| Boundary Handling | Symmetric padding | Periodic, Zero-padding | Minimizes edge artifacts |
Workflow Visualization: Wavelet Denoising Protocol
Wavelet Denoising Protocol for EEG Blink Detection
Autoencoder-Based Approaches for EEG Denoising
Architecture of Denoising Autoencoders
Denoising autoencoders (DAEs) represent a class of neural networks designed to learn efficient representations of input data by reconstructing clean signals from corrupted versions. In the context of EEG processing for blink-controlled systems, DAEs learn the underlying structure of clean EEG patterns while effectively suppressing noise and artifacts [58]. The network architecture typically consists of an encoder that compresses the input into a latent-space representation, and a decoder that reconstructs the denoised signal from this compressed representation.
Recent advances in generative models, particularly Generative Adversarial Networks (GANs), have shown remarkable performance in EEG denoising tasks. As demonstrated in research on automated EEG denoising, the GAN framework employs a generator network that learns to produce denoised EEG signals while a discriminator network distinguishes between cleaned and original clean signals [58]. This adversarial training process results in a denoising system that can effectively remove artifacts while preserving the temporal and spectral characteristics of genuine neural activity, including intentional blink patterns.
Implementation Protocol: Autoencoder Denoising
Materials and Equipment:
- High-performance computing system with GPU acceleration
- Deep learning frameworks (TensorFlow, PyTorch)
- Curated EEG dataset with clean and noisy pairs
- Data augmentation tools for synthetic training data
- Model evaluation and visualization tools
Step-by-Step Procedure:
Dataset Preparation
- Collect EEG recordings with intentional blinks under controlled conditions
- Manually annotate blink events and artifact regions
- Create clean-noisy signal pairs for supervised training
- Apply data augmentation (time-warping, amplitude scaling)
Network Architecture Design
- Implement encoder with convolutional layers for spatial features
- Include LSTM layers in bottleneck for temporal dependencies
- Design decoder with transposed convolutional layers
- Add skip connections to preserve high-frequency components
Model Training
- Initialize with Xavier/Glorot weight initialization
- Use Adam optimizer with learning rate 0.001
- Employ mean squared error (MSE) as primary loss function
- Implement early stopping based on validation performance
Validation and Testing
- Evaluate on held-out test set with quantitative metrics
- Assess temporal distortion using dynamic time warping
- Verify blink preservation through template correlation
- Compare with traditional methods (wavelet, ICA)
Deployment Optimization
- Quantize model weights for efficient inference
- Implement streaming processing for real-time operation
- Optimize hyperparameters for target hardware
- Validate on patient-specific data for personalization
Table 3: Autoencoder Architectures for EEG Denoising
| Architecture Component | Recommended Configuration | Performance Considerations |
|---|---|---|
| Encoder Type | Convolutional with decreasing filters | Captures spatial features across channels |
| Bottleneck | LSTM layer with 64-128 units | Models temporal dependencies in blinks |
| Decoder Type | Transposed convolutional layers | Enables precise signal reconstruction |
| Latent Space Dimension | 10-20% of input size | Balances compression and information retention |
| Activation Functions | ELU in hidden, linear in output | Prevents dying ReLU, enables signal range |
| Regularization | Dropout (0.2-0.5), L2 weight decay | Reduces overfitting on training data |
Workflow Visualization: Autoencoder Training Pipeline
Autoencoder Training Pipeline for EEG Denoising
Integration with Blink-Controlled Communication Systems
System Architecture for Real-Time Operation
The integration of advanced signal processing techniques into blink-controlled communication systems requires a streamlined architecture that balances computational efficiency with denoising performance. A hybrid approach that combines wavelet preprocessing for initial artifact reduction followed by lightweight autoencoder inference has shown promise for real-time operation [57]. This section outlines a recommended system architecture optimized for clinical deployment with minimal latency requirements.
The complete processing pipeline begins with multi-channel EEG acquisition, followed by wavelet-based coarse denoising, feature extraction using a compact autoencoder, blink classification based on morphological and temporal characteristics, and finally translation to communication commands through Morse code or other encoding schemes [32]. Special attention must be paid to temporal alignment throughout the pipeline to ensure that the precise timing of voluntary blinks is preserved for accurate communication.
Performance Metrics and Validation Protocol
Quantitative Evaluation Metrics:
- Signal-to-Noise Ratio (SNR): Improvement in dB after processing
- Blink Detection Accuracy: Precision, recall, and F1-score for intentional blinks
- Temporal Distortion: Mean absolute error in blink onset timing
- Classification Performance: Accuracy for different blink patterns
- Computational Latency: End-to-end processing time per epoch
Validation Protocol:
- Dataset Collection: Recruit 10-15 participants with diverse blink characteristics
- Ground Truth Establishment: Manual annotation by multiple experts
- Algorithm Comparison: Benchmark against baseline methods (ICA, FIR filtering)
- Statistical Analysis: Repeated measures ANOVA for performance comparisons
- Usability Assessment: Information transfer rate calculation for communication tasks
Table 4: Performance Benchmarks for Blink Detection Systems
| Metric | Minimum Clinical Standard | State-of-the-Art Performance | Measurement Protocol |
|---|---|---|---|
| Blink Detection Accuracy | >85% F1-score | >95% F1-score | 5-fold cross-validation |
| Temporal Precision | <50ms onset error | <20ms onset error | Comparison to video reference |
| Information Transfer Rate | >5 bits/minute | >15 bits/minute | Calculated from classification accuracy |
| False Positive Rate | <5% | <1% | During resting state recording |
| Patient Adaptation Time | <30 minutes | <10 minutes | Time to stable performance |
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Materials and Reagents for EEG Blink Detection Research
| Item | Specifications | Application Notes | Representative Vendors |
|---|---|---|---|
| EEG Acquisition System | 16-64 channels, 24-bit ADC, ≥250 Hz sampling rate | Prefer systems with builtin impedance checking | Biosemi, BrainProducts, ANT Neuro |
| Electrodes | Ag-AgCl sintered electrodes, 10-20 system compatibility | Ensure chloride coating integrity for stable potentials | EasyCap, BrainVision, Neurospec |
| Electrolyte Gel | High-chloride, low impedance formulation | Apply sufficient volume for stable electrical contact | Sigma Gel, SuperVisc, SignaCreme |
| Data Acquisition Software | MATLAB with EEGLAB, Python with MNE-Python | Ensure real-time streaming capability | MathWorks, OpenBCI |
| Wavelet Analysis Toolbox | MATLAB Wavelet Toolbox, PyWavelets | Verify support for inverse transforms | MathWorks, PyPI |
| Deep Learning Framework | TensorFlow, PyTorch with GPU support | Optimize for inference latency | Google, Facebook |
| Validation Tools | Simultaneous video recording, expert annotation system | Synchronize timestamps across modalities | Custom solutions |
| Reference Datasets | PhysioNet, BNCI Horizon, TUH EEG | Include blink annotation metadata | Various research institutions |
The integration of wavelet analysis and autoencoder-based denoising represents a significant advancement in EEG signal processing for blink-controlled communication systems. These complementary approaches address the unique challenges of preserving intentional blink morphology while suppressing confounding artifacts, enabling more reliable communication interfaces for individuals with severe motor disabilities. The protocols and methodologies outlined in this application note provide researchers with comprehensive guidelines for implementing these techniques in both clinical and research settings.
Future developments in this field will likely focus on personalized adaptation algorithms that automatically adjust to individual blink characteristics, hybrid models that combine the temporal precision of wavelets with the representational power of deep learning, and ultra-efficient implementations for wearable and embedded systems. As these technologies mature, they hold the promise of delivering more natural and efficient communication solutions for patients who rely on blink-controlled interfaces, ultimately enhancing their independence and quality of life.
Voluntary blink-controlled communication protocols represent a critical assistive technology for patients with severe motor disabilities, such as those suffering from amyotrophic lateral sclerosis (ALS), locked-in syndrome, or tetraplegia [29] [3]. These systems enable communication by translating intentional eye blinks into commands, offering a vital channel for expression and interaction when other muscular control is lost [3]. The effectiveness of these systems hinges on the accurate detection and classification of blink patterns from often noisy physiological signals, a challenge that conventional algorithms frequently struggle to address optimally. The integration of nature-inspired optimization techniques, particularly the Crow Search Algorithm (CSA), with machine learning models has emerged as a powerful approach to enhance the performance and reliability of blink detection systems [61] [62].
The fundamental challenge in blink-controlled communication lies in reliably distinguishing intentional, communicative blinks from spontaneous, physiological ones while accounting for signal artifacts and individual variations in blink characteristics [63]. Traditional detection methods often exhibit suboptimal performance due to inadequate parameter tuning and limited adaptability to signal noise. The Crow Search Algorithm addresses these limitations by providing an efficient mechanism for optimizing key parameters in classification models, thereby improving detection accuracy and system robustness [64] [65]. This synergy between bio-inspired optimization and machine learning creates a more effective framework for assistive communication technologies, ultimately enhancing quality of life for patients with severe motor impairments.
Theoretical Foundations of Crow Search Optimization
Basic Principles of Crow Search Algorithm
The Crow Search Algorithm (CSA) is a metaheuristic optimization algorithm inspired by the intelligent foraging behavior of crows [64] [65]. Crows demonstrate remarkable abilities in hiding food and remembering retrieval locations, while also engaging in tactical deception by following other birds to discover their food caches. CSA mimics this behavior through four key principles: crows live in flocks; crows remember their food hiding places; crows follow each other to steal food; and crows protect their caches with a certain probability [65].
In CSA formulation, the position of each crow represents a potential solution to the optimization problem. The algorithm maintains two key parameters: flight length (fl), which controls the local or global search scope, and awareness probability (AP), which determines whether a crow will be followed or if a random search will occur [65]. The position update in the conventional CSA follows specific rules. If crow j is unaware of being followed, crow i updates its position according to the equation: [ x^{i,iter+1} = x^{i,iter} + ri \times fl^{i,iter} \times (m^{j,iter} - x^{i,iter}) ] where ( ri ) is a random number between 0 and 1, ( fl^{i,iter} ) is the flight length, and ( m^{j,iter} ) is the memory position of crow j. If crow j becomes aware of being followed, crow i moves to a random position within the search space [65].
Advanced CSA Variants for Enhanced Performance
Recent research has developed several enhanced CSA variants to address limitations of the basic algorithm, particularly its tendency to converge to local optima due to fixed parameter values [64] [65]. The Variable Step Crow Search Algorithm (VSCSA) introduces a cosine function to dynamically adjust the flight length, significantly improving both solution quality and convergence speed [64]. The Advanced Crow Search (ACS) algorithm employs a dynamic awareness probability (AP) that varies nonlinearly with generations and incorporates probabilistic selection of the best solutions rather than random selection [65].
The Predator Crow Optimization (PCO) algorithm represents another significant advancement, drawing inspiration from predator-prey relationships in addition to crow foraging behavior [66] [62]. This hybrid approach demonstrates superior performance in feature selection and parameter optimization for healthcare applications, including cardiovascular disease prediction and blink detection systems [66] [62]. These algorithmic improvements have proven particularly valuable in medical signal processing applications where accuracy and reliability are paramount.
Application Notes: CSA-Optimized Models for Blink Detection
Integrated Framework for Enhanced Blink Detection
A state-of-the-art integrated approach for eye blink detection from Electroencephalography (EEG) signals combines wavelet analysis, autoencoding, and a Crow-Search-optimized k-Nearest Neighbors (k-NN) algorithm [61]. This comprehensive framework addresses multiple challenges in blink signal processing, beginning with data augmentation through jittering (adding controlled noise to increase dataset robustness), followed by wavelet transform for time-frequency feature extraction. An autoencoder then compresses these features into dense, informative representations before classification by the k-NN model, whose hyperparameters are optimized using the Crow Search Algorithm [61].
This approach demonstrates the advantage of CSA in balancing exploration and exploitation during the optimization process, effectively navigating the complex parameter space to identify optimal configurations for the k-NN classifier. The resulting system achieves remarkable performance, with evaluation metrics indicating approximately 96% accuracy across all datasets—surpassing deep learning models that use Convolutional Neural Networks with Principal Component Analysis and empirical mode decomposition [61]. This performance highlights the efficacy of optimized traditional machine learning models over more complex deep learning approaches for practical EEG-based blink detection applications.
Deep Learning Enhanced with Predator Crow Optimization
For more complex pattern recognition tasks in blink-controlled communication, Deep Neural Networks (DNNs) enhanced with Predator Crow Optimization (PCO) offer a powerful alternative [62]. In this architecture, the PCO algorithm optimizes DNN parameters, maximizing prediction performance for precise blink classification. The hybrid PCO-DNN framework has demonstrated exceptional capabilities in related healthcare applications, achieving accuracy of 96.67%, precision of 97.53%, recall of 97.10%, and F1-measure of 96.42% in cardiovascular disease prediction [62], suggesting similar potential for blink pattern recognition.
Table 1: Performance Comparison of Optimization-Enhanced Classifiers
| Model | Accuracy | Precision | Recall | F1-Score | Application Context |
|---|---|---|---|---|---|
| CSA-optimized k-NN [61] | ~96% | Not Reported | Not Reported | Not Reported | Eye blink detection from EEG signals |
| PCO-DNN [62] | 96.67% | 97.53% | 97.10% | 96.42% | Cardiovascular disease prediction |
| PCO-XAI Framework [66] | 99.72% | 96.47% | 98.60% | 94.60% | Cardiac vascular disease classification |
Experimental Protocols
Protocol 1: CSA-kNN for Blink Detection from EEG Signals
Objective: To implement and validate a Crow-Search-optimized k-NN algorithm for detecting eye blinks from EEG signals to facilitate communication interfaces for motor-impaired patients.
Materials and Reagents:
- EEG recording system with appropriate electrodes
- Signal processing software (MATLAB, Python with SciPy/NumPy)
- Standardized EEG datasets with annotated blink events
Procedure:
- Data Acquisition and Preprocessing: Collect EEG signals using a standardized montage, focusing on frontal and prefrontal electrodes that capture ocular artifacts. Apply band-pass filtering (0.1-30 Hz) to remove high-frequency noise and DC drift [61] [62].
- Data Augmentation: Implement jittering by adding controlled random noise to increase dataset robustness and variability [61].
- Feature Extraction: Apply wavelet transform (e.g., Morlet wavelet) to decompose EEG signals into time-frequency components, extracting features that characterize blink patterns [61].
- Feature Compression: Utilize an autoencoder to distill wavelet features into a lower-dimensional, informative representation while preserving discriminative blink characteristics [61].
- CSA Optimization Phase:
- Initialize crow population with random positions representing k-NN hyperparameters (k value, distance metric weights)
- Evaluate fitness using cross-validation accuracy on training data
- Update crow positions using CSA rules with dynamic flight length adjustment
- Iterate for predetermined generations or until convergence criteria met
- Model Validation: Train k-NN with optimized parameters and evaluate performance on held-out test data using accuracy, precision, recall, and F1-score metrics [61].
Analysis: Compare the performance of CSA-optimized k-NN against baseline models without optimization and against deep learning approaches. Perform statistical significance testing to validate improvements.
Protocol 2: PCO-DNN for Advanced Blink Pattern Classification
Objective: To develop a Predator Crow Optimization-Deep Neural Network framework for classifying complex blink patterns in a communication protocol.
Materials and Reagents:
- Video-based eye tracking system (e.g., Tobii Pro Spectrum) or high-resolution camera
- Computing system with GPU acceleration for DNN training
- Blink dataset with annotated intentional and spontaneous blinks
Procedure:
- Signal Acquisition: Record eye openness signals using video-based eye tracking at sufficient sampling rate (≥ 240 Hz) to capture blink dynamics [63]. Extract Eye Aspect Ratio (EAR) or similar metrics from facial landmarks.
- Blink Parameterization: Calculate blink duration, amplitude, velocity, and timing patterns from eye openness signals [67] [63].
- DNN Architecture Design: Construct a neural network with input layer matching feature dimensions, multiple hidden layers with activation functions, and output layer corresponding to communication commands.
- PCO-Based Optimization:
- Initialize predator and crow populations representing DNN parameters
- Implement hunting and evasion mechanisms between predator and crow groups
- Evaluate fitness using weighted combination of accuracy and computational efficiency
- Update positions using PCO rules with adaptive parameter adjustment
- Model Training: Train DNN with PCO-optimized parameters using backpropagation with momentum-based gradient descent.
- System Integration: Implement classified blink patterns into communication protocol with appropriate feedback mechanisms.
Analysis: Evaluate communication speed (characters per minute) and accuracy in practical usage scenarios. Assess robustness to varying lighting conditions and individual differences in blink characteristics.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for Blink-Controlled Communication Research
| Item | Function | Example Specifications |
|---|---|---|
| Video-Based Eye Tracker [67] [63] | Records eye movements and blinks with high temporal resolution | Sampling rate ≥ 240 Hz, integrated facial landmark detection (e.g., Tobii Pro Spectrum) |
| EEG Recording System [61] | Captures electrical signals associated with eye blinks | Multi-electrode setup with frontal placement, appropriate amplification and filtering |
| Jittering Algorithm [61] | Data augmentation technique to improve model robustness | Controlled noise injection with parameterizable amplitude and distribution |
| Wavelet Transform Toolbox [61] | Time-frequency analysis of blink signals | Morlet or Daubechies wavelets with adjustable scales |
| Autoencoder Framework [61] | Feature dimensionality reduction | Neural network architecture with bottleneck layer for compressed representations |
| Crow Search Algorithm Library [64] [65] | Optimization of classifier parameters | Implementation of CSA with dynamic flight length and awareness probability |
| Predator Crow Optimization Module [66] [62] | Enhanced optimization for complex parameter spaces | Dual population (predator and crow) with specialized interaction mechanisms |
| Eye Openness Calculation [67] [63] | Quantifies eyelid position and movement | Facial landmark detection with Eye Aspect Ratio (EAR) algorithm |
Visualizing Workflows and Algorithmic Structures
CSA-kNN Blink Detection Workflow
Predator Crow Optimization Architecture
The integration of Crow Search optimization with machine learning models represents a significant advancement in blink-controlled communication systems for motor-impaired patients. The CSA-optimized k-NN framework provides an effective balance between computational efficiency and classification accuracy, making it suitable for real-time applications where resource constraints may limit more complex approaches [61]. Meanwhile, the PCO-DNN architecture offers enhanced performance for complex pattern recognition tasks, potentially enabling more sophisticated communication protocols through the identification of subtle blink variations [62].
Future research should focus on several promising directions. First, the development of hybrid optimization algorithms that combine CSA with other nature-inspired techniques could further improve parameter optimization and model performance [64] [65]. Second, adaptive blink detection systems that continuously learn and adjust to individual user patterns would enhance long-term usability and accuracy [67] [68]. Third, multi-modal approaches that integrate EEG with video-based eye tracking could provide redundant validation and improved reliability [61] [63]. Finally, the translation of these technological advances into practical, affordable assistive devices remains a critical challenge requiring collaboration between algorithm developers, clinical researchers, and end-users to ensure real-world applicability and accessibility [29] [3].
The progressive refinement of crow-search-optimized models holds substantial promise for enhancing communicative autonomy for patients with severe motor limitations, potentially extending beyond basic communication to environmental control and digital interface operation [3]. As these technologies mature, they will contribute significantly to the broader field of human-computer interaction while providing immediate practical benefits to those who depend on alternative communication methods.
Application Note: Cognitive Load in Blink-Controlled Communication
The development of voluntary blink-controlled communication protocols represents a critical advancement in assistive technology for patients with severe motor impairments, such as amyotrophic lateral sclerosis (ALS), spinal cord injury, or locked-in syndrome [36] [32]. These systems translate intentional eye blinks and movements into communicative speech or text, providing a vital channel for interaction with caregivers and the external environment. However, the prolonged use of such systems can induce significant cognitive load and user fatigue, potentially undermining their effectiveness and adoption [69]. Cognitive load refers to the total amount of mental effort being used in the working memory [70]. In the context of blink-controlled systems, this load is exacerbated by the need to recall complex blink sequences, maintain precise timing, and sustain visual attention for extended periods.
A user-centric design framework is, therefore, essential to mitigate these challenges. This application note synthesizes current research to provide structured protocols and design principles aimed at reducing cognitive overload and fatigue in patients relying on blink-controlled communication systems.
Quantitative Analysis of Performance and Load
Data from recent studies on blink-based communication systems reveal a direct correlation between system design, task complexity, and user performance. The following table summarizes key performance metrics that inform cognitive load assessment.
Table 1: Performance Metrics of Blink-Based Communication Systems
| System / Study | Primary Input Method | Average Decoding Accuracy | Average Response Time | Key Cognitive Load Factor |
|---|---|---|---|---|
| Blink-To-Code (Morse) [32] | Voluntary blinks (dots/dashes) | 62% | 18-20 seconds | Morse sequence memory and timing |
| Blink-To-Live [36] | Four eye gestures (Left, Right, Up, Blink) | Not explicitly quantified | Not explicitly quantified | Short command sequence (3 movements) |
| SeeMe (Facial Movements) [21] | Low-amplitude facial movements | Detected movement 4.1 days earlier than clinicians | N/A | Minimal motor effort required |
The data indicates that systems requiring simpler, shorter sequences (like Blink-To-Live's three-movement commands) can reduce the intrinsic cognitive load associated with memorizing and executing communication codes [36]. Furthermore, increased task complexity, as seen in the transition from spelling "SOS" to "HELP" in Morse-based systems, leads to longer response times and higher error rates, directly pointing to increased cognitive load [32].
A Framework for Mitigating Cognitive Load
Effective design for blink-controlled interfaces must address the three types of cognitive load: Intrinsic (inherent difficulty of the task), Extraneous (load imposed by poor design), and Germane (effort for learning and schema formation) [69]. The following principles are adapted from general UX design and tailored specifically to the needs of users with severe motor impairments.
Simplify and Streamline the Interface
- Minimalist Design: The user interface (UI) should be free from unnecessary visual elements. A cluttered interface competes for the user's limited attentional resources [69]. For blink-based systems, this means displaying only the most critical information, such as the current command being constructed and a limited set of feedback cues.
- Clear Visual Hierarchy: Use size, color, and contrast to guide the user's attention to the most important elements, such as the confirmed blink input or the synthesized output text [69] [71].
Enhance Readability and Feedback
- Optimize Typography: Use highly legible fonts, sufficient font sizes, and ample line spacing for any text displayed on screen. This reduces the effort required to read generated messages [69].
- Provide Multimodal Feedback: Systems should offer immediate, clear feedback for a registered blink. This could be a subtle visual highlight on the screen or a soft auditory cue. This transparency confirms the user's action and reduces uncertainty, a significant source of extraneous cognitive load [71].
Design for Intuitive Interaction
- Structure and Grouping: For systems with multiple commands, group related functions logically. This allows users to form mental models of the system more easily, leveraging germane cognitive load effectively [69] [71].
- Progressive Disclosure: Avoid presenting all options at once. Instead, use a hierarchical menu where a sequence of blinks navigates through broad categories to specific commands. This breaks down a complex task into manageable steps, reducing intrinsic load [71].
- Leverage Familiar Patterns: Where possible, map blink sequences to intuitive actions (e.g., a "blink-and-hold" for "select") rather than arbitrary Morse codes, to lower the learning burden [36].
Support the User Proactively
- Auto-Completion and Prediction: Implement word- or command-prediction features. After a user begins spelling a word with blinks, the system can offer completions, significantly reducing the number of blinks required [69].
- Clear Error Recovery: Mistakes are inevitable, especially under fatigue. Providing a simple and reliable "backspace" or "undo" command is crucial to prevent user frustration and the cognitive load associated with error correction [32].
Experimental Protocols for Evaluating Cognitive Load and Fatigue
To validate the effectiveness of blink-controlled systems and their design improvements, rigorous testing is required. The following protocols outline methodologies for quantifying performance, cognitive load, and fatigue.
Protocol 1: Messaging Task Performance
This protocol evaluates the core functionality and efficiency of the communication system.
- Objective: To measure the accuracy and speed of message composition using a blink-controlled interface.
- Materials:
- Blink-detection system (e.g., webcam with computer vision algorithm like Mediapipe for facial landmark detection) [32].
- Calibrated Eye Aspect Ratio (EAR) threshold for blink detection [32].
- Pre-defined set of test phrases (e.g., "SOS", "HELP", "I am thirsty") [32].
- Data logging software to record timestamps and classification of each blink.
- Procedure:
- Calibration: Position the participant approximately 50 cm from the camera in a well-lit environment. Calibrate the EAR threshold for the individual's blink characteristics [32].
- Task: Instruct the participant to communicate the predefined phrases using only voluntary blinks.
- Data Collection: For each trial, log:
- Participant ID
- Target phrase
- Response time (from start signal to correct message completion)
- Accuracy (whether the intended message was transmitted correctly)
- Blink events (timestamps and classification as short/long) [32].
- Analysis:
- Calculate average response time and accuracy per participant and per phrase.
- Compare performance between short/common phrases and longer/complex ones to assess the impact of complexity on cognitive load [32].
Protocol 2: Sustained Use and Fatigue Assessment
This protocol investigates the long-term usability of the system and the onset of fatigue.
- Objective: To quantify changes in performance and subjective fatigue over a prolonged usage session.
- Materials:
- All materials from Protocol 1.
- Subjective self-reporting scale (e.g., Likert scale for mental fatigue, physical eye discomfort).
- Procedure:
- Baseline Measurement: Conduct Protocol 1 with a short baseline set of phrases.
- Sustained Task: Engage the participant in a continuous communication task for a set duration (e.g., 30 minutes), involving a mix of phrase repetitions and novel commands.
- Periodic Sampling: At fixed intervals (e.g., every 5 minutes), administer the subjective fatigue scale and re-run the baseline phrase test.
- Data Collection: Log all performance data as in Protocol 1, plus subjective ratings at each interval.
- Analysis:
- Plot response time and error rate against time to identify performance degradation.
- Correlate subjective fatigue scores with objective performance metrics.
- Analyze blink detection metrics (e.g., EAR amplitude, blink duration) for signs of muscular fatigue.
Data Visualization and Workflow
The following diagram illustrates the logical workflow of a user-centric blink-controlled communication system, integrating the design principles and evaluation points discussed.
Diagram 1: Workflow of a user-centric blink-controlled communication system, highlighting the central role of mitigating cognitive load and a continuous evaluation feedback loop for design optimization.
The Scientist's Toolkit: Research Reagent Solutions
The development and testing of blink-controlled communication systems rely on a suite of software and methodological "reagents." The following table details these essential components.
Table 2: Key Research Reagents for Blink-Controlled System Development
| Research Reagent / Tool | Type | Primary Function in Research |
|---|---|---|
| Mediapipe Face Mesh [32] | Software Library | Provides real-time, high-fidelity detection of 468 facial landmarks, enabling precise eye isolation and tracking from standard webcam video. |
| Eye Aspect Ratio (EAR) [32] | Computational Metric | A single, scalar value calculated from eye landmark positions; used for robust, real-time discrimination between open and closed eye states. |
| Computer Vision (OpenCV) [32] | Software Library | A foundational library for image processing tasks, including video capture, frame extraction, and grayscale conversion for blink detection pipelines. |
| Blink-To-Speak Language [36] | Encoding Scheme | A predefined dictionary that maps eight specific eye gestures (e.g., Shut, Blink, Left, Right) to letters, words, or commands, forming the basis of communication. |
| PsychoPy [21] | Experiment Software | An open-source package for presenting auditory commands and controlling the timing of stimulus-response experiments in a standardized manner. |
| Usability Heuristics [69] [71] | Evaluation Framework | A set of principles (e.g., clarity, structure, feedback) used to guide the design and critique of user interfaces to minimize extraneous cognitive load. |
Voluntary blink-controlled communication systems represent a transformative technology for patients with severe motor impairments, such as those resulting from acute brain injury or neurodegenerative diseases. The core premise of these systems is the detection and classification of intentional eyelid movements to facilitate communication and assess cognitive motor dissociation. However, the transition of these systems from controlled laboratory settings to diverse, real-world clinical environments presents a significant challenge. "Environmental adaptation" refers to the technical and methodological adjustments necessary to ensure these systems perform accurately and reliably across different lighting conditions, patient physiologies, and clinical workflows. This protocol outlines detailed application notes for achieving such robust performance, framed within a broader research thesis on voluntary blink-controlled communication.
The efficacy of blink analysis systems is quantified through a range of parameters derived from high-frame-rate video and computer vision analysis. The tables below consolidate key quantitative findings from recent clinical studies.
Table 1: Key Performance Metrics from Clinical Validation Studies
| Metric | SeeMe Tool (Brain Injury Patients) | High-Frame-Rate Video (Healthy Volunteers) | sEBR for PD Monitoring |
|---|---|---|---|
| Detection Capability | Detected eye-opening in 85.7% (30/36) of comatose patients [21] | Analyzed blinking in 80 volunteers [27] | Predicted ON/OFF states with mean AUC of 0.87 [33] |
| Early Detection | 4.1 days earlier than clinical examination [21] | Not Applicable | Not Applicable |
| Command Specificity | 81% for "open your eyes" command [21] | Not Applicable | Not Applicable |
| Correlation with Outcome | Amplitude/number of responses correlated with discharge outcome [21] | Not Applicable | Moderately predicted MDS-UPDRS scores (ρ = 0.54) [33] |
Table 2: Quantified Eyelid Kinematics and System Parameters
| Parameter Category | Specific Metric | Typical Values / Findings | Clinical Significance |
|---|---|---|---|
| Temporal Parameters | Blink Duration | 100 - 400 ms [27] | Differentiates voluntary blinks from reflexes. |
| Sampling Requirement | ≥ 240 fps (similar to EOG) [27] | Ensures sufficient data points for short-duration events. | |
| Kinematic Parameters | Main Sequence Slope | Significantly higher in reflexive blinks [72] | Discriminates between blink types based on velocity-amplitude relationship. |
| Onset Medial Traction | Significantly more in spontaneous blinks [72] | A 2D kinematic feature distinguishing behavior. | |
| Percent Eyelid Closure | Spontaneous blinks produce significantly less than 100% closure [72] | Indicates completeness of action; crucial for detecting subtle attempts. | |
| System Performance | Incomplete Blink Detection | Defined and detected [27] | Identifies weak motor efforts. |
| Consecutive Blink Detection | Defined and detected [27] | Recognizes complex command sequences or fatigue. |
Experimental Protocols for Environmental Validation
To ensure a blink-controlled communication system performs robustly across varied clinical settings, the following experimental protocols should be implemented.
Protocol for Multi-Center Environmental Robustness Testing
This protocol is designed to validate system performance under different lighting, hardware, and patient populations.
Aim: To assess and calibrate the blink detection system's accuracy across at least three distinct clinical environments (e.g., ICU, general ward, outpatient clinic).
Methodology:
- Site Setup:
- Deploy a standardized hardware kit at each site, including a 240 fps camera (e.g., Casio EX-ZR200 or smartphone equivalent), a portable computer, and a standardized, adjustable LED light source to control ambient illumination [27].
- Mount the camera above a monitor, creating a consistent setup where patients view stimuli while being recorded [27].
- Data Collection:
- Participant Recruitment: Enroll a minimum of 20 participants per site, including both healthy controls and patients with target conditions (e.g., ABI, Parkinson's disease) [21] [33].
- Stimulus Presentation: Use software like PsychoPy to present auditory commands in blocks of ten. Essential commands include "open your eyes," "stick out your tongue," and "show me a smile" [21]. A 1-minute resting baseline should be recorded prior to command presentation.
- Variable Manipulation: Systematically vary environmental conditions during data collection sessions:
- Illumination: Record sessions at three light levels: low (50 lux), medium (200 lux), and high (500 lux).
- Angle: Capture data with the camera positioned at 0°, 15°, and 30° from the frontal-parallel plane.
- Analysis:
- Process videos using a computer vision algorithm (e.g., SeeMe's vector field analysis) to quantify facial movements in response to commands [21].
- Calculate key performance indicators (KPIs) for each condition: True Positive Rate, False Positive Rate, and Command Classification Specificity.
- Compare KPIs across sites and environmental variables to identify performance degradation points.
Protocol for Kinematic Feature Extraction and Classification
This protocol provides a methodology for quantifying nuanced eyelid movements that are specific to voluntary commands.
Aim: To extract and validate 2D kinematic features of eyelid motion that reliably distinguish voluntary blinks from spontaneous and reflexive blinks.
Methodology:
- High-Resolution Tracking:
- Apply adhesive motion capture markers (2 mm hemispheres) along the margin of the upper and lower eyelids [72].
- Use a high-speed motion capture system or a high-frame-rate video (≥240 fps) to track the 3D trajectory of these markers during different eyelid behaviors (spontaneous blink, voluntary blink on command, reflexive blink, soft closure) [27] [72].
- Kinematic Determinant Calculation:
- From the marker trajectories, calculate the following determinants for each blink event [72]:
- Onset Medial Traction: The medial (inward) motion of the eyelid early in the closure phase.
- Reverberation: The sweeping overshoot of the upper eyelid beyond its complete closure position.
- Percent Eyelid Closure: The maximum percentage of closure achieved.
- Main Sequence Slope: The slope of the linear regression between the blink's amplitude and its maximum closing velocity.
- From the marker trajectories, calculate the following determinants for each blink event [72]:
- Model Training and Validation:
- Use a machine learning classifier (e.g., Support Vector Machine or Random Forest) to distinguish voluntary blinks from other types.
- Input features should include the calculated kinematic determinants.
- Train the model on a subset of the data and validate its classification accuracy on a held-out test set, reporting metrics such as AUC (Area Under the Curve) [33].
Signaling Pathways and Workflows
The following diagrams, generated with Graphviz DOT language, illustrate the core experimental workflow and the underlying neuromechanical logic of blink control.
Blink Analysis Workflow
Voluntary Blink Neuromechanical Pathway
The Scientist's Toolkit
A successful implementation of a blink-controlled communication protocol requires specific reagents, hardware, and software solutions. The following table details these essential components.
Table 3: Essential Research Reagents and Materials for Blink Analysis
| Item Name | Function/Application | Specification/Notes |
|---|---|---|
| High-Frame-Rate Camera | Captures eyelid kinematics with sufficient temporal resolution. | 240 fps or higher; e.g., Casio EX-ZR200 or modern smartphones [27]. |
| Computer Vision Algorithm | Quantifies subtle facial movements from video data. | Vector field analysis tracking facial pores (~0.2mm resolution) [21]. |
| Stimulus Presentation Software | Presents standardized auditory commands. | PsychoPy or equivalent; allows for precise timing and block design [21]. |
| Motion Capture Markers | Enables high-fidelity 2D/3D kinematic analysis of the eyelid margin. | 2mm adhesive hemispheres; used for detailed biomechanical studies [72]. |
| Segmental EMG System | Records activation patterns of the Orbicularis Oculi (OO) muscle. | Fine-wire intramuscular electrodes; reveals behavior-specific neural control [72]. |
| Clinical Assessment Scales | Provides ground truth for clinical state and outcome. | Glasgow Coma Scale (GCS), Coma Recovery Scale-Revised (CRS-R) [21]. |
| Machine Learning Classifier | Classifies blink type and correlates features with clinical states. | Used for predicting ON/OFF states in PD or command specificity in ABI [21] [33]. |
Benchmarking Performance and Clinical Validation of Blink Communication Systems
Voluntary blink-controlled communication protocols represent a critical assistive technology for individuals with severe motor impairments, such as those resulting from amyotrophic lateral sclerosis (ALS), locked-in syndrome, or brain injuries [32]. For researchers and clinicians developing these systems, a rigorous and standardized approach to performance evaluation is paramount. This document outlines the core performance metrics—accuracy, speed, and Information Transfer Rate (ITR)—and provides detailed application notes and experimental protocols to ensure robust, comparable, and meaningful assessment of blink-based communication systems within a clinical research framework.
The performance of a blink-controlled communication system is quantified by three interdependent metrics. Accuracy measures the system's reliability, speed measures its practical efficiency, and the Information Transfer Rate (ITR) synthesizes both into a single benchmark of communication efficiency.
Table 1: Summary of Performance Metrics from Select Blink-Controlled System Studies
| Study & Modality | Primary Metric: Accuracy | Secondary Metric: Speed/Time | Derived Metric: Information Transfer Rate (ITR) |
|---|---|---|---|
| Computer Vision (Blink-to-Code) [32] | 62% average decoding accuracy for "SOS" & "HELP" messages | 18-20 seconds response time for short messages | Not explicitly calculated; estimated potential rate is low due to sequential Morse code input. |
| EEG-based (Multiple Blink Classification) [73] | 89.0% accuracy (ML models); 95.39% precision & 98.67% recall (YOLO model) for single/two-blink detection | Real-time detection with high temporal precision | Not explicitly reported; high classification speed and accuracy suggest a potentially high ITR for a discrete command system. |
| Computer Vision (Clinical Detection) [21] | Detected eye-opening in 85.7% of patients vs. 71.4% via clinical exam | Detected responses 4.1 days earlier than clinicians | Not applicable (used for early detection, not communication speed). |
Calculating Information Transfer Rate (ITR)
For systems that classify blinks into distinct commands (e.g., no-blink, single-blink, double-blink), the ITR in bits per minute (bpm) can be calculated using the following formula [73]:
B = log2(N) + P * log2(P) + (1-P) * log2[(1-P)/(N-1)]
Where:
Bis the bit rate per trial.Nis the number of classes or commands (e.g., 3 for no-blink, single-blink, double-blink).Pis the classification accuracy (a value between 0 and 1).- The ITR (bpm) is then
B * (60 / T), whereTis the trial duration in seconds.
Experimental Protocols for System Validation
To ensure the validity and reproducibility of performance metrics, researchers must adhere to structured experimental protocols. The following workflow outlines a standardized process for evaluating a blink-controlled communication system.
Protocol 1: Pre-defined Message Task
This protocol measures a user's ability to communicate specific, urgent messages reliably and is adapted from the "SOS"/"HELP" validation task [32].
- Objective: To assess accuracy and response time for standardized, high-priority messages.
- Procedure:
- The participant is instructed to produce a pre-defined message (e.g., "SOS," "HELP," "PAIN") using the blink-based system.
- The researcher records the time from the initiation cue to the successful completion of the message.
- The trial is a success only if the entire message is decoded correctly.
- This is repeated for at least 5 trials per message [32].
- Data Recorded:
- Accuracy: Percentage of correctly decoded messages per session.
- Response Time: Average time from task initiation to successful completion.
- Analysis: Report mean and standard deviation for response times and overall accuracy across all trials and participants.
Protocol 2: Randomized Command Selection Task
This protocol evaluates the system's performance in a discrete command selection scenario, which is foundational for spelling applications or environmental control.
- Objective: To measure classification accuracy and ITR for a set of distinct commands.
- Procedure:
- A set of
Ncommands (e.g., letters, device controls) is mapped to different blink patterns (e.g., single-blink for 'Yes', double-blink for 'No'). - During a trial, a target command is presented visually or auditorily to the participant.
- The participant performs the corresponding blink pattern.
- The system's classification is recorded without researcher intervention.
- The trial is repeated for a minimum of 40 trials per participant to ensure statistical power [73].
- A set of
- Data Recorded:
- Classification Accuracy: The percentage of correctly classified blink patterns.
- Trial Duration: The time from the presentation of the target to the system's classification.
- Analysis: Calculate the ITR using the formula in Section 2.1. Generate a confusion matrix to identify misclassifications.
The Researcher's Toolkit
A successful blink-controlled communication system integrates components for data acquisition, signal processing, and user interface.
Table 2: Essential Research Reagents and Materials for Blink-Controlled System Development
| Category | Item | Function & Application Notes |
|---|---|---|
| Data Acquisition | Standard Webcam [32] | A low-cost, non-contact sensor for video-oculography (VOG). Ideal for computer vision-based approaches. |
| EEG Headset (e.g., 8-64 channel) [73] [74] | Non-invasive neural signal acquisition. Can detect blink artifacts or specific neural patterns with high temporal precision. | |
| Software & Algorithms | Computer Vision Libraries (OpenCV, MediaPipe) [32] | Provides face and landmark detection (e.g., 468 facial points) for calculating metrics like Eye Aspect Ratio (EAR). |
| Machine Learning Frameworks (Python, TensorFlow/PyTorch) [73] | Enables development of custom classifiers (e.g., Neural Networks, SVM, XGBoost, YOLO) for blink pattern recognition. | |
| Signal Processing Tools (EEG-specific toolboxes) | For filtering, feature extraction (e.g., time-domain, frequency-domain), and artifact removal from EEG signals. | |
| Experimental Control | PsychoPy [21] | Open-source software for designing and running controlled experiments, including precise presentation of auditory commands. |
| Validation & Analysis | Eye-Tracking Glasses / High-Speed Camera [75] | Provides ground-truth data for blink timing and classification, crucial for validating and refining detection algorithms. |
Signaling Pathway and System Workflow
The transformation of a voluntary blink into a communicated message follows a structured pipeline. The logical flow from signal acquisition to final output is critical for understanding system performance and identifying potential failure points.
Workflow Stage Specifications
- Signal Acquisition: The system gathers data via a chosen modality. Computer Vision uses a webcam and libraries like MediaPipe to track facial landmarks and compute the Eye Aspect Ratio (EAR), a scalar value reflecting the degree of eye openness [32]. Electrophysiology uses an EEG headset to record electrical potentials from the scalp, capturing the characteristic waveform of a blink artifact [74].
- Pre-processing: This stage cleans the raw signal. For video, this may involve face detection and ROI stabilization. For EEG, it involves applying band-pass filters (e.g., 0.1-15 Hz) to isolate the blink signal from noise [73] [74].
- Feature Extraction: Discriminative features are calculated. For video, the primary feature is the EAR time-series. For EEG, features can include time-domain (e.g., amplitude), frequency-domain, or amplitude-driven statistics [73] [76].
- Blink Detection & Classification: This is the core decision-making stage. A threshold is applied to the features (e.g., EAR < threshold indicates blink) [32]. Detected blinks are then classified by duration (e.g., <2s for dot/single-blink, ≥2s for dash/double-blink) or pattern using a trained machine learning model [73].
- Command Decoding & Execution: The sequence of classified blinks is mapped to an output. In Morse code systems, sequences of dots/dashes are decoded into alphanumeric characters [32]. In discrete systems, specific patterns trigger commands (e.g., double-blink selects a menu item).
- User Feedback: The system provides immediate feedback, often visually (e.g., displaying the decoded text) or auditorily (e.g., a confirmation sound). This closed-loop is critical for user correction and system reliability.
Voluntary eye blinks represent a critical control signal for developing assistive communication protocols for patients with severe motor impairments, such as those with amyotrophic lateral sclerosis (ALS), locked-in syndrome, or traumatic brain injuries [42] [3]. The selection of an appropriate signal acquisition technology is paramount for the system's accuracy, comfort, and real-world applicability. This application note provides a detailed comparative analysis and experimental protocols for three primary sensing modalities: computer vision, electroencephalography (EEG), and electrooculography (EOG). The content is framed within the development of a robust blink-controlled communication system for bed-ridden patients, summarizing key quantitative data into structured tables and providing detailed methodologies for researchers and scientists in the field [3].
The following table summarizes the core characteristics, performance metrics, and applicability of the three primary blink-detection technologies.
Table 1: Comparative Analysis of Blink Detection Technologies for Patient Communication Protocols
| Feature | Computer Vision (CV) | Electroencephalography (EEG) | Electrooculography (EOG) |
|---|---|---|---|
| Core Principle | Image analysis of eye region using cameras and machine learning algorithms [77] | Measurement of electrical brain activity via scalp electrodes [42] | Measurement of corneo-retinal standing potential around eyes [78] [79] |
| Measured Signal | Pixel intensity changes, eye shape/contour [77] | Cortical potentials (including blink artifacts) [42] | Bioelectrical potential from eye movement (0.4-1 mV) [78] |
| Key Performance Metrics | Accuracy: >96% (single blink) [23]Challenges: Lower performance with variable lighting [23] | Accuracy: ~89.0% (XGBoost for 0/1/2 blinks) [42]Recall: 98.67%, Precision: 95.39% (YOLO model) [42] | Accuracy: >90% for blink detection [79]Can detect minute (1.5°) eye movements [79] |
| Typical Hardware | Standard or IR camera, sufficient processing unit [23] | Multi-channel EEG headset (e.g., 8-channel Ultracortex Mark IV) [42] | Surface electrodes (snap/cloth), amplifier, headset [78] |
| Key Advantages | Non-contact, rich feature set (e.g., gaze tracking) [77] | Direct measurement of neural signals, potential for multi-purpose BCI [42] | Excellent temporal resolution, robust to ambient light, low computational cost [79] |
| Key Limitations | Sensitive to lighting, privacy concerns, computational cost [23] [79] | Sensitive to various artifacts, requires gel electrodes for high fidelity, complex signal processing [42] | Contact-based, requires electrode placement near eyes, sensitive to electrical noise [78] [79] |
| Ideal Patient Use Case | Users in controlled environments where a camera can be mounted, for discrete counting of blinks. | Users where a multi-purpose BCI is needed, or for whom facial electrode placement is undesirable. | Users requiring high-speed, reliable blink detection with low computational overhead, suitable for wearable aids [79]. |
Detailed Experimental Protocols
Protocol for EEG-Based Consecutive Blink Classification
This protocol is adapted from the study achieving high accuracy in classifying no-blink, single-blink, and consecutive two-blink states [42].
- Objective: To develop a real-time BCI framework for classifying multiple eye blink states using non-invasive EEG.
- Materials: The "Research Reagent Solutions" table in Section 5 lists the essential materials.
- Procedure:
- Participant Preparation & Data Acquisition:
- Recruit participants following ethical review board guidelines.
- Fit an 8-channel wearable EEG headset (e.g., Ultrocortex "Mark IV") on the participant. Electrode locations should include frontal sites (e.g., FP1, FP2) highly sensitive to ocular artifacts [42].
- Instruct participants to perform three types of eye actions in a randomized, cue-guided sequence: no blink (0b), single voluntary blink (1b), and two consecutive voluntary blinks (2b). Each action should be performed for a set duration (e.g., 5-second trials) with adequate rest between trials to prevent fatigue.
- Record raw EEG data synchronously with the event markers for each blink type.
- Data Preprocessing:
- Apply a band-pass filter (e.g., 0.5-50 Hz) to the raw EEG data to remove high-frequency noise and slow drifts.
- Segment the continuous data into epochs time-locked to the instruction cues for each blink action.
- Feature Extraction:
- Extract a comprehensive set of features from each epoch using multiple techniques:
- Basic Statistical Features: Mean, variance, skewness, kurtosis.
- Time-Domain Features: Hjorth parameters (activity, mobility, complexity).
- Amplitude-Driven Features: Peak-to-peak amplitude, signal energy.
- Frequency-Domain Features: Power spectral density in delta, theta, alpha, and beta bands.
- Apply feature selection algorithms (e.g., mutual information, Recursive Feature Elimination) to identify the most discriminative features for classification.
- Extract a comprehensive set of features from each epoch using multiple techniques:
- Model Training & Real-Time Classification:
- Divide the feature set into training and testing subsets.
- Train multiple machine learning models, such as XGBoost, Support Vector Machine (SVM), and Neural Networks (NN), using the training data.
- For enhanced robustness against multiple blink occurrences in a single timeframe, train an object detection model like You Only Look Once (YOLO) on the EEG signal representations [42].
- Validate model performance on the held-out test set using metrics like accuracy, recall, precision, and mean Average Precision (mAP).
- Integration into Communication Protocol:
- Map the classified blink states (0b, 1b, 2b) to specific communication commands (e.g., "Yes," "No," "Select," cursor movement) within a user interface.
- Implement the trained model for real-time inference on streaming EEG data to activate the predefined commands.
- Participant Preparation & Data Acquisition:
Figure 1: Experimental workflow for EEG-based consecutive blink classification.
Protocol for Pressure-Sensor Based Voluntary Blink Interaction
This protocol is based on research utilizing thin-film pressure sensors to detect blinks by capturing subtle deformation of ocular muscles [23].
- Objective: To evaluate the recognition accuracy and user workload of six different voluntary blink actions for designing a patient-friendly control interface.
- Materials: The "Research Reagent Solutions" table in Section 5 lists the essential materials, including the critical thin-film pressure sensor.
- Procedure:
- Sensor Setup and Calibration:
- Affix one or more thin-film pressure sensors to the frame of a pair of glasses or a headband, positioning them to make gentle contact with the skin near the orbital muscle (above the eyebrow or on the temple).
- Connect the sensors to a microcontroller unit (e.g., Arduino) for signal acquisition.
- Calibrate the sensor output for each user by recording the baseline signal and the signal during a maximal voluntary blink.
- Blink Action Definition and Data Collection:
- Define the six voluntary blink actions to be tested: Single Bilateral (SB), Single Unilateral (SU), Double Bilateral (DB), Double Unilateral (DU), Triple Bilateral (TB), and Triple Unilateral (TU) [23].
- Instruct participants to perform each action multiple times in a randomized order upon visual or auditory cues.
- Record the pressure sensor signal alongside the action markers.
- Signal Processing and Action Recognition:
- Preprocess the raw sensor data with a low-pass filter to reduce high-frequency noise.
- Implement a detection algorithm to identify individual blink peaks based on amplitude thresholding. The ratio of the peak value (Nmax) to the baseline value (Nbase) is a key feature [23].
- For multiple-blink actions (double, triple), logic is applied to the concatenated single-blink detections, considering the inter-blink interval.
- Performance and Subjective Assessment:
- Calculate the recognition accuracy for each of the six blink actions.
- Measure temporal variables: total completion time, blink duration, and inter-blink interval.
- Administer subjective workload surveys (e.g., NASA-TLX) and usability questionnaires (e.g., System Usability Scale - SUS) after testing each action.
- System Validation:
- Implement the top-performing blink actions (e.g., SB, DB, SU) into a practical application, such as controlling a toy car or a computer interface, to validate usability in a real-world task [23].
- Sensor Setup and Calibration:
Figure 2: Experimental workflow for pressure-sensor based blink interaction.
The following tables consolidate key performance and physiological data from the analyzed research.
Table 2: Performance of Voluntary Blink Actions with a Pressure Sensor System [23]
| Blink Action | Acronym | Recognition Accuracy (%) | Key Subjective Finding |
|---|---|---|---|
| Single Bilateral | SB | 96.75 | Recommended as the primary action |
| Single Unilateral | SU | 95.62 | Top three recommended action |
| Double Bilateral | DB | 94.75 | Recommended as a secondary action |
| Double Unilateral | DU | 94.00 | - |
| Triple Bilateral | TB | 93.00 | Lower accuracy and higher workload |
| Triple Unilateral | TU | 92.00 | Lowest accuracy and highest workload |
Table 3: Physiological Characteristics of Spontaneous Blinks from a Multimodal Dataset [80]
| Parameter | Mean ± Standard Deviation | Observed Range (Min - Max) |
|---|---|---|
| Blink Peak Potential on FP1 | 160.1 ± 56.4 μV | Not Specified |
| Blink Frequency | 20.8 ± 12.8 blinks/minute | Not Specified |
| Blink Duration (Width) | 0.20 ± 0.04 seconds | 0.032 - 0.57 seconds |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Equipment for Blink Detection Research
| Item | Function/Description | Example Use Case |
|---|---|---|
| Ultracortex Mark IV Headset | An open-source, 3D-printed EEG headset with 8 channels for capturing cortical potentials. | EEG-based consecutive blink classification [42]. |
| Wet/Dry EEG Electrodes | Sensors that make electrical contact with the scalp to measure voltage fluctuations. | Acquiring raw EEG signals; dry electrodes favor usability while wet electrodes (with gel) favor signal quality [42]. |
| Thin-Film Pressure Sensor | A flexible sensor that measures subtle surface pressure changes from muscle deformation. | Detecting blinks via movement of the orbital muscle, avoiding cameras and electrodes [23]. |
| BioRadio & BioCapture | A portable physiological data acquisition system with pre-set configurations for signals like EOG. | Simplified and reliable collection of EOG data in a lab setting [78]. |
| You Only Look Once (YOLO) | A real-time object detection algorithm that can be adapted for pattern detection in 1D signals. | Classifying multiple blinks within a single EEG epoch with high recall and precision [42]. |
| Independent Component Analysis (ICA) | A blind source separation method for decomposing mixed signals into independent components. | Identifying and isolating blink artifacts from other neural sources in multi-channel EEG data [42]. |
Within the development of voluntary blink-controlled communication protocols for patients with severe motor deficits, establishing a direct correlation between blink parameters and clinical outcomes is a critical research frontier. For patients with conditions such as locked-in syndrome (LIS) or disorders of consciousness (DoC), the ability to volitionally control eye blinks represents not only a vital communication channel but also a potential biomarker of neurological integrity and recovery potential [15]. This document synthesizes current research to provide application notes and experimental protocols for quantifying blink behaviors, with a specific focus on their value in the early detection of recovery and prognostication of functional outcomes. The objective is to equip researchers and clinicians with standardized methods to translate subtle neuromuscular signals into clinically actionable data, thereby bridging the gap between basic motor function and high-level communicative intent.
Quantitative Data on Blink Detection and Clinical Correlation
Research demonstrates that quantitative analysis of facial movements, including blinks, can detect signs of recovery earlier than standard clinical assessment and is correlated with functional outcomes.
Table 1: Performance of Computer Vision in Detecting Early Facial Movements
| Parameter | SeeMe Tool Detection | Clinical Examination Detection |
|---|---|---|
| Eye-Opening to Command | Detected in 30/36 patients (85.7%) | Detected in 25/36 patients (71.4%) |
| Timing of Detection | 4.1 days earlier than clinicians | Later detection relative to SeeMe |
| Mouth Movements to Command | Detected in 16/17 patients (94.1%)* | Not specified |
| Command Specificity (Eye-Opening) | 81% | Not applicable |
*In patients without an obscuring endotracheal tube [81]
Furthermore, the amplitude and number of detected facial responses have been shown to correlate with clinical outcomes at discharge, underscoring their prognostic value [81]. In other neurological conditions, such as Parkinson's disease (PD), alterations in spontaneous blink parameters also serve as disease biomarkers. Patients with PD exhibit a significantly reduced spontaneous blink rate and an increased blink duration compared to healthy controls, with the blink rate showing correlation with motor deficit severity and dopaminergic depletion [45].
Experimental Protocols for Blink Analysis
The following protocols detail methodologies for capturing and analyzing blink data in both research and clinical settings.
Protocol 1: Computer Vision-Based Detection of Voluntary Facial Movements (SeeMe)
This protocol is designed to identify low-amplitude, command-following facial movements in patients with acute brain injury [81].
- 1. Participant Setup: Position the patient comfortably. Ensure the face is well-lit. Use a standard video camera (e.g., smartphone camera at high frame rates like 240 fps is suitable) to record the patient's face. If possible, use a tripod to stabilize the image.
- 2. Stimulus Presentation: Via single-use headphones, present auditory commands in blocks. The recommended commands are: "Stick out your tongue," "Open your eyes," and "Show me a smile." Each command should be presented in a block of ten repetitions. The inter-stimulus interval should be jittered between 30–45 seconds (±1 sec) to prevent habituation and predictable rhythmic responses.
- 3. Data Acquisition: Begin with a 1-minute resting baseline recording of the patient's face with no commands. Subsequently, record the patient's face throughout the auditory stimulation protocol. The entire session should be video-recorded for subsequent analysis.
- 4. Data Processing with SeeMe Algorithm:
- Facial Landmark Tracking: Use the computer vision algorithm to tag individual facial pores (resolution ~0.2 mm) and track their displacement over time.
- Movement Quantification: Apply vector field analysis to the tracked landmarks to quantify the amplitude and direction of facial movements in response to each command.
- Machine Learning Classification: Train a classifier to assess whether the detected movements are specific to the command type (e.g., eye-opening occurs specifically to the command "open your eyes" and not to other commands).
- 5. Outcome Measures: The primary outcome is the detection of facial movement in response to auditory commands. Secondary measures include the amplitude of movement, the number of responsive trials, and the specificity of the response to the command type.
Protocol 2: Automated Analysis of Spontaneous Blink Kinematics
This protocol uses automated video analysis to characterize spontaneous blink rate and duration, which can be applied to patients with facial palsy, Parkinson's disease, or other neurological disorders [67] [45].
- 1. Standardized Video Recording:
- Setup: Participants sit in a well-lit room facing a camera. The participant's head should remain within the camera's cutout for the session duration. A standardized distance (e.g., 45-60 cm) is recommended.
- Stimulus: To control for cognitive load, participants watch a neutral, non-emotional film clip for a set period (e.g., 20 minutes).
- Equipment: Use a camera capable of high-frame-rate recording (e.g., 240 fps) to capture fine temporal dynamics of blinks.
- 2. Automated Blink Detection and Analysis:
- Facial Landmark Extraction: Import the video into an analysis toolbox. Extract facial landmarks using a library. For eye analysis, landmarks around the eyelids are critical.
- Eye Aspect Ratio (EAR) Calculation: Calculate the Eye Aspect Ratio (EAR) for each frame. The EAR is a scalar value representing the degree of eye openness, calculated from the vertical and horizontal distances between eyelid landmarks. It decreases during a blink.
- Blink Parameter Extraction:
- Blink Identification: Identify a blink when the EAR falls below a defined threshold and then returns to baseline.
- Blink Rate: Calculate as the number of blinks per minute.
- Blink Duration: Calculate as the time from when the EAR first falls below the threshold until it recovers above it.
- Closure Quality: The minimal EAR value during a blink indicates the completeness of eyelid closure.
- 3. Data Correlation: Correlate the extracted blink parameters (rate, duration, minimal EAR) with clinical scores or patient-reported outcome measures.
Figure 1: Experimental workflow for automated blink analysis, from participant setup to data correlation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials and Tools for Blink Response Research
| Item | Function/Description | Example Use Case |
|---|---|---|
| High-Speed Camera | Captures video at high frame rates (e.g., 240+ fps) for detailed kinematic analysis of rapid blink movements. | Quantifying blink duration and closure speed [67]. |
| Computer Vision Software | Provides algorithms for face detection, facial landmark tracking (e.g., 468 points), and feature extraction (e.g., EAR). | Automated analysis of spontaneous blinking; detecting low-amplitude voluntary movements [81] [67]. |
| Eye Tracker | A video-based system that provides high-precision data on pupil and eyelid position (e.g., 500 Hz sampling). | Studying blink dynamics and their interaction with other oculomotor behaviors [45]. |
| Auditory Stimulation System | Presents standardized verbal commands via headphones to elicit voluntary motor responses. | Assessing command-following in patients with disorders of consciousness [81]. |
| Electromyography (EMG) | Records electrical activity from the orbicularis oculi muscle; provides a direct measure of blink-related muscle activation. | Differentiating blink types and studying blink neurophysiology [82]. |
Signaling Pathways and Neurophysiological Workflow of a Voluntary Blink
A voluntary blink is a complex motor act initiated by cortical command. The primary motor cortex (M1) sends signals that converge on the facial nucleus of the brainstem. The facial nerve (Cranial Nerve VII) then activates the orbicularis oculi muscle, resulting in rapid eyelid closure. Simultaneously, the levator palpebrae muscle is inhibited. Crucially, this motor command is accompanied by corollary discharges—internal copies of the motor signal—that are sent to sensory areas of the brain, such as the thalamus and visual cortex. These signals prepare the brain for the self-generated visual interruption, leading to a suppression of visual processing and the maintenance of perceptual stability despite the physical occlusion of the pupil [82].
Figure 2: Neurophysiological pathway of a voluntary blink and perceptual maintenance.
Augmentative and Alternative Communication (AAC) systems represent a critical therapeutic approach for patients with severe motor impairments who retain cognitive function but lack reliable verbal communication abilities. These technologies are particularly vital in intensive care unit (ICU) and long-term care environments, where conditions such as locked-in syndrome (LIS), traumatic brain injury, and neurodegenerative diseases can profoundly disrupt communication pathways. Voluntary blink-controlled communication protocols have emerged as a promising solution, leveraging one of the last remaining voluntary motor functions for patients with extensive paralysis. This application note synthesizes current evidence on the real-world efficacy of these systems, providing structured data and methodological protocols to support researchers and clinicians in implementing and evaluating blink-controlled communication interventions.
Table 1: Summary of Blink-Controlled Communication System Efficacy
| Study Population | Sample Size | Intervention Type | Primary Outcome Measures | Reported Efficacy | Citation |
|---|---|---|---|---|---|
| Locked-In Syndrome (LIS) | 1 patient | SCATIR Switch + Clickey2.0 Software | Communication capability restoration | Successful simple word expression and sentence delivery after 3-week training | [83] |
| Prolonged DoC (MCS vs. VS/UWS) | 24 patients (14 MCS, 10 VS/UWS) | Eye Blink Rate (EBR) Measurement | Diagnostic discrimination | Significantly higher EBR in MCS than VS/UWS; correlation with CRS-R responsiveness | [84] |
| Healthy Participants (BCI Development) | 10 participants | 8-Channel EEG Headset + YOLO Model | Multiple blink classification accuracy | 89.0% accuracy (traditional ML); 95.39% precision, 98.67% recall (YOLO) | [42] |
| ICU Patients (AAC Candidacy) | Cohort study | AAC need assessment | Proportion needing AAC | 33% of ICU patients met AAC candidacy criteria | [85] |
Table 2: Blink Detection Performance Across Methodologies
| Detection Methodology | Technical Approach | Advantages | Limitations | Reported Performance |
|---|---|---|---|---|
| EEG-Based YOLO Model [42] | Deep learning object detection applied to EEG signals | High accuracy for consecutive blinks; suitable for real-time BCI | Requires specialized equipment and computational resources | Recall: 98.67%, Precision: 95.39%, mAP50: 99.5% |
| Double-Threshold EEG Detection [74] | Two-threshold approach for blink identification from EEG | Catches both weak and regular blinks; uses standard EEG equipment | May require individual calibration | Validated for real-time robot control with 5 participants |
| EOG-Based Detection [83] | Infrared reflection detection of eyelid movement | High signal-to-noise ratio; less affected by brain signals | Requires additional facial sensors | Enabled communication in LIS patient after training |
| Video-Oculography (VOG) [3] | Image processing and Haar cascade classifiers | Contact-free detection; uses widely available camera technology | Affected by lighting conditions and head placement | 83.7% recognition accuracy reported |
Experimental Protocols
Protocol 1: EEG-Based Blink Detection System Implementation
Objective: To implement a real-time brain-computer interface (BCI) for detecting voluntary eye blinks and consecutive blink patterns from EEG signals for patient communication.
Equipment and Software:
- TMSi SAGA 64+ EEG system or comparable 8+ channel EEG headset [42] [74]
- EEG electrodes positioned at Fp1, Fp2, F7, F8, and reference locations [74]
- Signal processing software (MATLAB, Python with SciPy/NumPy)
- YOLO (You Only Look Once) model implementation framework [42]
Methodology:
- EEG Signal Acquisition:
- Apply EEG electrodes according to the 10-20 international system
- Set sampling rate to ≥250 Hz with bandpass filtering between 0.1-30 Hz [84]
- Ensure electrode impedance maintained below 50 kΩ for optimal signal quality
Signal Preprocessing:
- Apply notch filter at 50/60 Hz to reduce line noise
- Implement artifact removal algorithms for muscle and movement artifacts
- Use independent component analysis (ICA) to isolate ocular components [42]
Blink Detection Algorithm:
System Validation:
- Conduct offline testing with recorded EEG data
- Perform real-time validation with healthy participants
- Finally test with target patient population
Figure 1: EEG-Based Blink Detection Workflow. Diagram illustrates the sequential process from signal acquisition to blink classification output.
Protocol 2: Clinical Implementation for Critical Care Patients
Objective: To establish a clinical protocol for implementing blink-controlled communication systems in ICU and long-term care settings for patients with severe communication impairments.
Equipment and Software:
- AAC device with blink detection capability (e.g., SCATIR switch, eye-tracking systems) [83]
- Switching interface software (e.g., Switch Interface Pro 5.0) [83]
- Speech-generating software with scanning interface (e.g., Clickey 2.0, NeoSpeech Yumi) [83]
Methodology:
- Patient Assessment:
- Confirm diagnosis of LIS, profound paralysis, or communication impairment
- Verify cognitive function and consciousness level using CRS-R [84]
- Assess visual capability and eye movement preservation
System Configuration:
- Position blink sensor (infrared, EEG, or camera-based) for optimal detection
- Calibration: Determine optimal blink detection threshold for individual patient
- Set scanning speed and interface layout according to patient ability
Training Protocol:
Outcome Measurement:
- Quantitative: Communication accuracy rate, words per minute
- Functional: Goal Attainment Scaling for communication objectives
- Patient-reported: Satisfaction and quality of life measures when possible
The Scientist's Toolkit
Table 3: Essential Research Reagents and Equipment for Blink-Controlled Communication Systems
| Item Category | Specific Examples | Research Function | Implementation Notes |
|---|---|---|---|
| Signal Acquisition | TMSi SAGA 64+ EEG [74]; Ultracortex "Mark IV" EEG Headset [42] | Records neural signals for blink detection | 8+ channels recommended; frontal placement critical for ocular artifacts |
| Blink Detection Sensors | SCATIR Switch (Self-Calibrating Auditory Tone Infrared) [83]; EOG electrodes | Detects eyelid movement via infrared reflection or electrical potential | Non-invasive; requires proper positioning near eye |
| Processing Software | YOLO (You Only Look Once) model [42]; Clickey 2.0 [83] | Classifies blink patterns; enables text generation | YOLO excels at consecutive blink detection; Clickey enables keyboard emulation |
| Output Systems | NeoSpeech Yumi [83]; Speech-generating devices | Converts blink signals to speech output | Provides audio feedback; enhances communication efficacy |
| Validation Tools | Coma Recovery Scale-Revised (CRS-R) [84]; Accuracy metrics | Assesses patient consciousness level; quantifies system performance | Essential for establishing baseline and measuring outcomes |
Technical Implementation Diagrams
Figure 2: Blink-Controlled Communication System Architecture. Diagram shows the complete pathway from patient blink to communication output.
Discussion and Clinical Implications
The synthesized evidence demonstrates that blink-controlled communication systems show significant promise for restoring communication capabilities in severely impaired patients. The high accuracy rates of modern detection algorithms (89.0-98.67%) [42] support their technical feasibility, while clinical studies document successful implementation even in challenging cases such as locked-in syndrome [83]. The correlation between eye blink rate and consciousness level [84] further suggests that blink monitoring may serve dual purposes for both communication and diagnostic assessment in critical care settings.
Implementation success appears dependent on several key factors: appropriate patient selection, systematic training protocols, and individualized system calibration. The documented three-week training period [83] provides a realistic timeframe for clinical expectation setting. Future development directions should focus on improving accessibility, reducing calibration requirements, and enhancing communication speed to further improve functional outcomes for this vulnerable patient population.
Locked-in Syndrome (LIS) and other conditions resulting in severe motor paralysis render affected individuals unable to communicate verbally or through limb movement, while their cognitive faculties often remain fully intact [15]. This profound disconnect between inner life and outer expression leads to extreme social isolation and a diminished quality of life [15]. For this population, voluntary blink-controlled communication protocols are not merely assistive tools but are fundamental lifelines to the world. These systems translate intentional ocular movements into commands for communication interfaces, enabling users to express needs, thoughts, and emotions. This application note synthesizes feedback from patients and clinical caregivers on the usability and user experience of these systems, providing a structured overview of performance data, detailed experimental protocols, and essential research tools to guide future development and clinical implementation within the broader context of advancing assistive technologies.
Performance and Usability Data
The evaluation of blink-controlled systems encompasses critical metrics such as accuracy, response time, and user capacity, which directly impact their clinical viability. The following table summarizes quantitative findings from recent studies.
Table 1: Performance Metrics of Blink-Controlled Communication Systems
| System Type / Study | Reported Accuracy | Response Time/Character | Key User Feedback |
|---|---|---|---|
| Blink-to-Code (Morse Code) [32] | 62% (Average decoding accuracy) | 18-20 seconds (for short messages like "SOS") | Performance drops with message complexity; requires user training to manage cognitive load. |
| Communication Aid by Eyelid Tracking [86] | 81.8% (Morse code detection) | Information Not Specified | Demonstrates the viability of non-intrusive, camera-based methods for converting blinks to text and speech. |
| EOG-Based System [87] | Performing operation confirmed | Improved processing speed reported | System operability, accuracy, and processing speed were improved using individual threshold settings. |
Feedback from caregivers highlights that low-cost, non-intrusive systems are crucial for accessibility, particularly in low-resource settings [29]. Patients benefit significantly from systems that are simple to set up and use, reducing the dependency on caregivers for daily operation. Furthermore, the cognitive load on users is a critical factor; systems requiring memorization of complex blink sequences or sustained concentration can lead to user fatigue and abandonment [32].
Detailed Experimental Protocols
To ensure reproducibility and standardized evaluation of blink-controlled communication systems, the following protocols detail two prevalent methodological approaches.
Protocol 1: Real-Time Camera-Based Blink Detection and Morse Code Decoding
This protocol outlines a non-invasive method using a standard webcam and computer vision, ideal for low-cost applications [32].
1. Objective: To enable a user to communicate alphanumeric messages by translating voluntary eye blinks into Morse code sequences in real-time.
2. Materials:
- Hardware: A computer or laptop with a standard webcam.
- Software: Python environment with installed libraries (OpenCV, Mediapipe, Dlib, Scipy).
- Calibration Interface: A simple GUI or script to set timing thresholds.
3. Experimental Procedure: 1. Setup: The participant is seated approximately 50 cm from the webcam in a well-lit environment to ensure consistent lighting and minimize shadows on the face. 2. Calibration: The system performs a brief calibration phase for each user: * The user is prompted to perform a few voluntary blinks. * The system calculates the user's typical Eye Aspect Ratio (EAR) during open and closed eye states. * The user is asked to produce blinks of intentionally short and long durations to empirically determine and set the thresholds for classifying a "dot" (e.g., 1.0-2.0 seconds) and a "dash" (e.g., ≥2.0 seconds) [32]. 3. Task Execution: The participant is instructed to communicate predefined phrases (e.g., "SOS", "HELP") using Morse code via blinks. 4. Data Logging: For each trial, the system records: * Participant ID and trial number. * Intended message and decoded message. * Response time (from start signal to correct message completion). * Timestamp and classification (dot/dash) of each blink event.
4. Data Analysis: * Calculate the average decoding accuracy per participant and across all trials. * Compute the average response time for different messages. * Analyze trends in performance over successive trials to assess learning effects.
Protocol 2: EOG-Based Eye Movement and Blink Detection System
This protocol describes an electrophysiological approach using Electrooculography (EOG) for detecting eye movements and voluntary blinks with high precision [87] [88].
1. Objective: To develop a communication support interface controlled by horizontal/vertical eye movements and voluntary eye blinks for individuals with motor paralysis.
2. Materials:
- Hardware: Surface electrodes (Ag/AgCl), bio-potential amplifier with AC-coupling, data acquisition device (e.g., ADC), computer.
- Software: Signal processing software (e.g., MATLAB, Spike2, or custom C/C++ scripts).
- Interface: A virtual on-screen keyboard.
3. Experimental Procedure: 1. Electrode Placement: Two surface electrodes are placed on the skin above and beside the subject's dominant eye, with a reference electrode on an earlobe [88]. 2. Signal Acquisition: Horizontal and vertical EOG signals are measured. AC-coupling is used in the amplification stage to reduce baseline drift [87] [88]. 3. Signal Processing & Threshold Setting: * The raw EOG signal is filtered to remove noise. * Individual-specific thresholds for detecting saccades and blinks are set based on the amplitude of the user's EOG signals [87] [88]. * Directional cursor movements (up, down, left, right) and a selection command are mapped to specific EOG signal patterns (e.g., exceeding a positive or negative threshold in either channel) and voluntary blink pulses [88]. 4. Testing & Task Execution: The user performs a text entry task on a virtual keyboard. The user moves the cursor using eye movements and selects characters with a voluntary blink. 5. Data Logging: The number of correct characters, task completion time, and error rates are recorded.
4. Data Analysis: * Quantify the operability, accuracy (character error rate), and information transfer rate (bits per minute) [88]. * Compare processing speed and user fatigue with previous system configurations.
The workflow for the camera-based and EOG-based communication protocols is summarized below:
The Scientist's Toolkit: Research Reagent Solutions
Successful research and development in blink-controlled communication require a suite of essential materials and software tools. The following table catalogs key components and their functions.
Table 2: Essential Materials and Tools for Blink-Controlled Communication Research
| Category | Item / Reagent | Function / Explanation |
|---|---|---|
| Hardware | Standard Webcam | A low-cost, non-invasive sensor for camera-based systems; captures video frames for computer vision processing [32] [29]. |
| Surface Electrodes (Ag/AgCl) & Amplifier | Used in EOG systems to measure the corneo-retinal potential difference and amplify the weak bio-potential signals associated with eye movements [87] [88]. | |
| Eye Tracker (e.g., Tobii Dynavox) | High-precision, commercial-grade device often used as a benchmark for performance comparison, though cost can be prohibitive [29]. | |
| Software & Algorithms | Computer Vision Libraries (OpenCV, Mediapipe) | Provide pre-trained models for real-time face mesh and landmark detection, which is foundational for calculating metrics like the Eye Aspect Ratio (EAR) [32]. |
| Eye Aspect Ratio (EAR) Metric | A computational method to detect blinks based on the ratio of vertical to horizontal eye landmark distances; a decrease in EAR indicates eye closure [32]. | |
| Signal Processing Tools (MATLAB, Python Scipy) | Used for filtering EOG signals, extracting features, and implementing classification algorithms to distinguish between different types of eye movements and blinks [87]. | |
| User Interface | Virtual On-Screen Keyboard | A software keyboard that allows users to select letters or commands using eye-based input, forming the core of the communication interface [88]. |
| Text-to-Speech (TTS) Engine | Converts the decoded text from blink sequences into synthesized speech, enabling audible communication for the user [29] [86]. |
The logical relationship between the user, the system components, and the output is as follows:
Feedback from end-users and clinicians is paramount for transitioning voluntary blink-controlled communication protocols from laboratory prototypes to clinically impactful tools. The quantitative data and structured protocols provided here offer a framework for rigorous, reproducible research. Future work must focus on enhancing accuracy and speed while simultaneously reducing cognitive load, hardware intrusiveness, and cost. Interdisciplinary collaboration among engineers, clinicians, and end-users is essential to refine these systems, ultimately empowering individuals with severe motor disabilities to overcome communication barriers and improve their quality of life.
Conclusion
Voluntary blink-controlled communication protocols represent a rapidly advancing frontier in assistive technology, demonstrating tangible benefits for patients with severe motor impairments. The synthesis of foundational neuroscience, sophisticated methodologies like computer vision and optimized EEG analysis, and rigorous validation establishes these systems as reliable tools for restoring basic communication. For researchers and drug development professionals, these protocols offer dual value: as a direct therapeutic aid to improve patient quality of life, and as a potential biomarker or functional endpoint in clinical trials for neurological disorders. Future directions should focus on the development of adaptive, self-learning systems that require minimal calibration, the integration of blink control with other nascent neuroprosthetic technologies, and the conduct of large-scale clinical trials to firmly establish their efficacy in standardized care pathways. The ultimate goal is to seamlessly bridge the gap between covert consciousness and meaningful interaction, transforming patient care and clinical research in neurology.
References
- 1. The clinical and experimental significance of blinking behavior [https://pmc.ncbi.nlm.nih.gov/articles/PMC7182785/]
- 2. Voluntary Blink Controlled Communication Protocol for Bed ... [https://www.igi-global.com/chapter/voluntary-blink-controlled-communication-protocol-for-bed-ridden-patients/162383]
- 3. Voluntary Blink Controlled Communication Protocol for Bed ... [https://www.academia.edu/67531561/Voluntary_Blink_Controlled_Communication_Protocol_for_Bed_Ridden_Patients]
- 4. Neural control of blinking [https://www.sciencedirect.com/science/article/pii/S1388245724000415]
- 5. Comparative analysis of spontaneous blinking and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7813264/]
- 6. Blink Reflex [https://musculoskeletalkey.com/blink-reflex/]
- 7. UCLA study reveals complex muscle control behind ... [https://newsroom.ucla.edu/stories/ucla-study-reveals-complex-muscle-control-behind-blinking]
- 8. The Blink Reflex and Other Cranial Nerve Reflexes [https://neupsykey.com/the-blink-reflex-and-other-cranial-nerve-reflexes/]
- 9. The blink reflex and its modulation – Part 1 - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10978309/]
- 10. Learning and Timing of Voluntary Blink Responses Match ... [https://www.nature.com/articles/s41598-017-03343-2]
- 11. Traumatic Brain Injury and Risk of Amyotrophic Lateral ... [https://pubmed.ncbi.nlm.nih.gov/41037265/]
- 12. Risk of ALS After Traumatic Brain Injury, Study Finds [https://www.emjreviews.com/neurology/news/risk-of-als-after-traumatic-brain-injury-study-finds/]
- 13. Traumatic Brain Injury Linked to Heightened Risk for ... [https://www.drugs.com/news/traumatic-brain-injury-linked-heightened-risk-amyotrophic-lateral-sclerosis-127099.html]
- 14. Traumatic Brain Injury and Risk of Amyotrophic Lateral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492050/]
- 15. Update on How to Approach a Patient with Locked-In ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10813368/]
- 16. Disorder of consciousness rather than complete Locked-In ... [https://www.nature.com/articles/s43856-025-01196-9]
- 17. Brain-Computer Interface Implant for Severe ... [https://neals.org/als-trials/NCT04576650]
- 18. Assessing consciousness in patients with locked ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1604173/full]
- 19. A phase II open label clinical study of the safety, tolerability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9132272/]
- 20. Closed - ALS Research Notification for Clinical Trials and ... [https://www.cdc.gov/als/abouttheregistrymain/closed-alsclinicalresearchnotification.html]
- 21. Computer vision detects covert voluntary facial movements ... [https://www.nature.com/articles/s43856-025-01042-y]
- 22. What is a blink? Classifying and characterizing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11133197/]
- 23. Design recommendations for voluntary blink interactions ... [https://www.sciencedirect.com/science/article/abs/pii/S147403462400137X]
- 24. Encoding of blink information via wireless contact lens for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12448796/]
- 25. Efficient machine learning approach for volunteer eye-blink ... [https://www.sciencedirect.com/science/article/pii/S0957417421014111]
- 26. The perceptual consequences and neurophysiology of eye ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10466800/]
- 27. The method for quantified analysis and pattern ... [https://link.springer.com/article/10.1007/s13534-025-00522-3]
- 28. Update on How to Approach a Patient with Locked-In ... [https://www.mdpi.com/2076-3425/14/1/92]
- 29. Blink-To-Live eye-based communication system for users ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10192441/]
- 30. Social connection as a critical factor for mental and physical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11403199/]
- 31. The effects of social isolation stress and discrimination on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9490697/]
- 32. Blink-to-Code: Real-Time Morse Code ... [https://arxiv.org/html/2508.09344v1]
- 33. Spontaneous eye blink-based machine learning for tracking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361378/]
- 34. TwitchView User Guide [https://www.blinkdc.com/twitchview-user-guide]
- 35. Eye Aspect Ratio for Real-Time Drowsiness Detection to ... [https://www.mdpi.com/2079-9292/11/19/3183]
- 36. Blink-To-Live eye-based communication system for users ... [https://www.nature.com/articles/s41598-023-34310-9]
- 37. A Comprehensive Framework for Eye Tracking: Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564957/]
- 38. Real-time driver drowsiness detection using transformer ... [https://www.nature.com/articles/s41598-025-02111-x]
- 39. Analysing Eye Tracking Data – How Can It Provide New ... [https://www.realeye.io/blog/post/eye-tracking-data-analysis]
- 40. Detecting Blinks in Healthy and Parkinson's EEG A Deep ... [https://arxiv.org/html/2509.04951v1]
- 41. Detection of eye movements and eye blinks using a ... [https://pubmed.ncbi.nlm.nih.gov/41177306/]
- 42. EEG based real time classification of consecutive two eye ... [https://www.nature.com/articles/s41598-025-07205-0]
- 43. A synergistic approach for enhanced eye blink detection ... [https://www.nature.com/articles/s41598-025-95119-2]
- 44. EEG Blink Artifacts Can Identify Read Music in Listening ... [https://arxiv.org/html/2508.13807v1]
- 45. Revisiting eye blink in Parkinson's disease [https://www.nature.com/articles/s41598-025-95182-9]
- 46. pupil and Blink responses in adults with ADHD symptoms [https://link.springer.com/article/10.1007/s00702-025-03051-6]
- 47. Humans quickly learn to blink strategically in response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5834680/]
- 48. Making Blink accessible to all: WCAG 2.2 [https://www.joinblink.com/intelligence/making-blink-accessible-to-all-wcag-2-2]
- 49. Understanding Success Criterion 1.4.11: Non-text Contrast [https://www.w3.org/WAI/WCAG22/Understanding/non-text-contrast.html]
- 50. AI tool SeeMe detects hidden signs of consciousness in ... [https://www.news-medical.net/news/20250912/AI-tool-SeeMe-detects-hidden-signs-of-consciousness-in-brain-injury-patients.aspx]
- 51. Distinguishing intentional from nonintentional actions ... [https://www.nature.com/articles/s41598-023-34604-y]
- 52. Voluntary blinks and eye-widenings, but not spontaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11684486/]
- 53. New research uncovers pathway for blink-assisting ... [https://www.optometrytimes.com/view/new-research-uncovers-pathway-for-blink-assisting-prostheses-development]
- 54. Researchers uncover new muscular data to target eyelid ... [https://glance.eyesoneyecare.com/stories/2025-09-23/researchers-uncover-new-muscular-data-to-target-eyelid-and-blinking-rates/]
- 55. Spontaneous eye blink-based machine learning for ... [https://www.nature.com/articles/s41531-025-01094-w]
- 56. Effects of blinking exercises on palpebral fissure height ... [https://www.sciencedirect.com/science/article/pii/S1542012425000266]
- 57. Enhanced EEG signal classification in brain computer ... [https://www.nature.com/articles/s41598-025-07427-2]
- 58. Auto-Denoising for EEG Signals Using Generative Adversarial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8914841/]
- 59. Automated EEG Signal Processing: A Comprehensive ... [https://www.sciencedirect.com/science/article/abs/pii/S0165027025002055]
- 60. Wavelet transforms for feature engineering in EEG data ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809423002446]
- 61. A synergistic approach for enhanced eye blink detection ... [https://pubmed.ncbi.nlm.nih.gov/40199999/]
- 62. Deep Neural Network and Predator Crow Optimization ... [https://www.mdpi.com/2227-7390/11/22/4621]
- 63. What is a blink? Classifying and characterizing blinks in ... [https://link.springer.com/article/10.3758/s13428-023-02333-9]
- 64. A Variable Step Crow Search Algorithm and Its Application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10526407/]
- 65. An Advanced Crow Search Algorithm for Solving Global ... [https://www.mdpi.com/2076-3417/13/11/6628]
- 66. Predator crow search optimization with explainable AI for ... [https://www.nature.com/articles/s41598-025-96003-9]
- 67. Automated analysis of spontaneous eye blinking in ... [https://www.nature.com/articles/s41598-024-68707-x]
- 68. A smartphone-based blink training application for ... [https://www.nature.com/articles/s41746-025-02053-8]
- 69. Reducing cognitive overload in UX design - Full Clarity [https://fullclarity.co.uk/insights/cognitive-overload-in-ux-design/]
- 70. Should you always minimize cognitive load? [https://ux.stackexchange.com/questions/83295/should-you-always-minimize-cognitive-load]
- 71. 4 Principles to Reduce Cognitive Load in Forms [https://www.nngroup.com/articles/4-principles-reduce-cognitive-load/]
- 72. Human eyelid behavior is driven by segmental neural control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12358864/]
- 73. EEG based real time classification of consecutive two eye ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12217743/]
- 74. Brain-computer interface for robot control with eye artifacts ... [https://www.nature.com/articles/s41598-023-44645-y]
- 75. Dataset combining EEG, eye-tracking, and high-speed ... [https://www.nature.com/articles/s41597-025-04861-9]
- 76. Quantitative EEG features and machine learning classifiers ... [https://www.sciencedirect.com/science/article/pii/S2772528622000772]
- 77. The 100 most popular computer vision applications [https://viso.ai/applications/computer-vision-applications/]
- 78. EOG - ECG/ EKG [https://glneurotech.com/FAQ/eog.html]
- 79. Tracking The Dark Side - Neurotech@Berkeley - Medium [https://ucbneurotech.medium.com/tracking-the-dark-side-7279990fbc8a]
- 80. Dataset combining EEG, eye-tracking, and high-speed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11978869/]
- 81. Computer vision detects covert voluntary facial movements ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368019/]
- 82. The perceptual consequences and neurophysiology of eye ... [https://www.frontiersin.org/journals/systems-neuroscience/articles/10.3389/fnsys.2023.1242654/full]
- 83. Augmentative and Alternative Communication Training ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3358685/]
- 84. Spontaneous eye blinking as a diagnostic marker in ... [https://www.nature.com/articles/s41598-021-01858-3]
- 85. Augmentative and Alternative Communication (AAC) [https://www.asha.org/practice-portal/professional-issues/augmentative-and-alternative-communication/?srsltid=AfmBOoqZGTJ4JEk_iT33bfEPVHAvH4jq1PBRfjvIsldepQd8axK-aC5I]
- 86. (PDF) Communication Aid for Paralyzed People by Eyelid Tracking [https://www.academia.edu/71661118/Communication_Aid_for_Paralyzed_People_by_Eyelid_Tracking]
- 87. New Methods of Detecting Voluntary Used to Blinking w Communicate [https://aece.ro/abstractplus.php?year=2012&number=4&article=7]
- 88. Eye Movement Communication Control System Based on ... [https://link.springer.com/content/pdf/10.1007/11788713_138.pdf?pdf=inline%20link]