Wavelet Transform in Medical Imaging: From Denoising to AI-Driven Diagnostics
This article provides a comprehensive exploration of wavelet transform techniques and their revolutionary impact on medical imaging.
Wavelet Transform in Medical Imaging: From Denoising to AI-Driven Diagnostics
Abstract
This article provides a comprehensive exploration of wavelet transform techniques and their revolutionary impact on medical imaging. Tailored for researchers and drug development professionals, it delves into the foundational principles of multi-resolution analysis, showcasing cutting-edge applications in image denoising, compression, registration, and segmentation. The review systematically compares wavelet-based methods with traditional approaches, evaluates their performance using established clinical metrics, and addresses key optimization challenges for real-world deployment. By synthesizing recent advances and future directions, this work serves as a critical resource for leveraging wavelet transforms to enhance diagnostic accuracy, streamline data management, and accelerate innovation in biomedical research.
The Core Principles of Wavelet Transform and Multi-Resolution Analysis
For medical imaging researchers, the choice of signal transformation technique is paramount for tasks ranging from image compression and denoising to segmentation and registration. The Discrete Wavelet Transform (DWT) and Fourier Transform represent two fundamental mathematical approaches to analyzing image data, each with distinct advantages and limitations. The Fourier Transform decomposes a signal into constituent sinusoids of varying frequencies, providing a global frequency representation but lacking time localization [1]. In contrast, the DWT decomposes signals using localized wavelets—oscillations that are limited in duration—enabling simultaneous time-frequency analysis through multi-resolution analysis [2] [1]. This fundamental difference in approach has significant implications for medical image processing, where preserving both spatial and frequency information is often critical for diagnostic accuracy.
Theoretical Comparison: DWT vs. Fourier Transform
Table 1: Fundamental Properties of DWT and Fourier Transform
| Property | Discrete Wavelet Transform (DWT) | Fourier Transform |
|---|---|---|
| Domain Analysis | Time-frequency localization | Global frequency |
| Resolution | Variable time-frequency resolution | Uniform frequency resolution |
| Basis Functions | Localized wavelets (e.g., Haar, Daubechies) | Infinite sinusoids |
| Information Capture | Captures transient events and local features | Captures periodic patterns |
| Computational Complexity | O(N) for certain cases [2] | O(N log N) for FFT [3] |
| Invariance | Shift-variant (standard DWT) | Shift-invariant |
| Medical Imaging Strengths | Edge detection, compression, denoising | MRI reconstruction, spectroscopy, noise resilience |
The mathematical underpinnings of each transform directly inform their application strengths. The Fourier Transform's global frequency analysis makes it ideal for characterizing periodic structures and stationary patterns, and it forms the mathematical foundation for Magnetic Resonance Imaging (MRI) and Fourier Transform Infrared (FTIR) spectroscopy [4] [5]. The DWT's multi-resolution capability allows it to hierarchically decompose an image into approximation (low-frequency) and detail (high-frequency) coefficients across scales, preserving structural information like edges and textures crucial for diagnostic interpretation [2] [6]. This multi-scale representation enables progressive image transmission and scalable compression, valuable for telemedicine applications.
Performance Metrics and Quantitative Comparison
Table 2: Performance Comparison in Medical Imaging Applications
| Application | Transform Method | Key Metrics | Reported Performance |
|---|---|---|---|
| Medical Image Denoising | Block-based Discrete Fourier Cosine Transform (DFCT) [7] | SNR, PSNR, Image Quality (IM) | Consistently outperformed global DWT across all noise types (Gaussian, Uniform, Poisson, Salt-and-Pepper) |
| Medical Image Denoising | Global DWT Approach [7] | SNR, PSNR, Image Quality (IM) | Inferior to block-based DFCT across all tested noise models |
| Medical Image Compression | DWT + Cross-Attention Learning [8] | PSNR, SSIM, MSE | Superior to JPEG2000 and BPG on LIDC-IDRI, LUNA16, and MosMed datasets |
| Medical Image Segmentation | FFTMed (Fourier-based) [9] | Dice Score, Computational Efficiency | Competitive accuracy with significantly lower computational overhead and enhanced adversarial noise resilience |
| Computational Duration | FFT [3] | Execution Time (Theoretical) | O(N log N) complexity |
| Computational Duration | DWT [3] | Execution Time (Theoretical) | O(N) complexity for certain cases (e.g., Haar wavelet) |
Recent comparative studies reveal nuanced performance characteristics. For image denoising, contrary to the common hypothesis favoring wavelets, a 2025 study found that a block-based Discrete Fourier Cosine Transform (DFCT) approach consistently outperformed a global DWT approach across multiple noise types and metrics [7]. The superior performance was attributed to DFCT's localized processing strategy, which better preserves fine details by operating on small image blocks and adapting to local statistics without introducing global artifacts [7]. However, in compression applications, hybrid frameworks combining DWT with deep learning modules demonstrate state-of-the-art performance, outperforming standard codecs like JPEG2000 [8].
Application Protocols in Medical Imaging Research
Protocol I: Wavelet-Based Medical Image Denoising and Enhancement
This protocol details a hybrid approach combining undecimated DWT (UDWT) with wavelet coefficient mapping for simultaneous denoising and contrast enhancement [6].
Title: Wavelet-Based Denoising and Enhancement Workflow
Step-by-Step Methodology:
- Image Decomposition: Perform 2D Undecimated Discrete Wavelet Transform (UDWT) on the original medical image using the Db2 wavelet basis function up to resolution level 2. UDWT provides shift-invariance compared to standard DWT [6].
- Hierarchical Correlation Calculation: For the three detailed coefficient subbands (horizontal, vertical, diagonal), calculate correlation values between level 1 and level 2 coefficients using:
ImgCor(p,q) = |Coef_lev1(p,q) × Coef_lev2(p,q)|[6]. - Adaptive Threshold Determination:
- Find the maximum correlation value in each row of the correlation image for each subband.
- Compute the mean (
Mean_max) of these maximum values. - Eliminate correlation values greater than
0.8 × Mean_max(considered signal). - Compute standard deviation (σ) from remaining correlations.
- Set threshold
THR = 1.6 × σ[6].
- Coefficient Thresholding: Apply the threshold to level 1 detail coefficients. If
|Coef_lev1 × Coef_lev2| ≥ THR, retainCoef_lev1; otherwise, set to zero [6]. - Initial Reconstruction: Perform inverse UDWT using the approximation coefficients of level 1 and the modified detail coefficients to reconstruct the denoised image.
- Contrast Enhancement: Apply a sigmoid-type mapping function to the wavelet coefficients of the denoised image:
w_output_j = a × [1 / (1 + 1/exp((w_input_j - c)/b))] × w_input_j [%], wherea = 2^(-(j-1)N). This weights lower-decomposition levels more heavily to enhance edges [6]. - Final Image Reconstruction: Perform an inverse DWT to generate the final denoised and contrast-enhanced medical image.
Protocol II: Deep Learning-Based Medical Image Compression Using DWT
This protocol employs DWT within a deep learning framework for superior compression performance while preserving diagnostic regions [8].
Title: DWT Deep Learning Compression Pipeline
Step-by-Step Methodology:
- Multi-resolution Decomposition: Decompose input medical images into multi-resolution frequency sub-bands (LL, LH, HL, HH) using Discrete Wavelet Transform (DWT) [8].
- Cross-Attention Feature Prioritization: Process sub-bands through a Cross-Attention Learning (CAL) module that dynamically weights feature maps, emphasizing regions with high diagnostic information (e.g., lesions, tissue boundaries) while reducing redundancy in less critical areas [8].
- Probabilistic Feature Representation: Encode the weighted features using a lightweight Variational Autoencoder (VAE) to create a robust probabilistic latent space representation, refining features before final encoding [8].
- Entropy Encoding and Storage: Apply entropy coding (e.g., arithmetic coding) to the quantized latent representation to produce the final compressed bitstream for efficient transmission or storage [8].
Protocol III: Fourier-Based Medical Image Segmentation (FFTMed)
This protocol outlines a Fourier domain approach for lightweight and noise-resilient medical image segmentation [9].
Title: FFTMed Segmentation Framework
Step-by-Step Methodology:
- Domain Transformation: Convert input medical images from the spatial domain to the frequency domain using a 2D Fast Fourier Transform (FFT) [9].
- High-Frequency Filtering: Discard a portion of the high-frequency components in the first half of the network to reduce noise and computational load, leveraging the inherent noise resilience of the frequency domain [9].
- Frequency Attention Processing: Process the frequency data through Encoder Frequency Modules (EFM) that utilize frequency attention mechanisms to capture long-range dependencies and comprehensive amplitude-phase information [9].
- Feature Aggregation: Replace standard max-pooling with a Hybrid Kernel Aggregation Anti-Aliasing Module to preserve critical spectral details during down-sampling [9].
- Output Refinement: Integrate a refinement module that iteratively enhances the predicted probability maps to mitigate potential blurring or ringing artifacts, ensuring accurate final segmentation [9].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials and Computational Tools
| Item/Reagent | Function/Application | Specification Notes |
|---|---|---|
| Haar Wavelet | Lossless image decomposition for registration [10], simple denoising | Orthogonal, symmetric, single-level discontinuity; ideal for edge detection and structural preservation. |
| Daubechies (Db2/Db4) | Medical image denoising [6] and compression [8] | Compact support with vanishing moments; balances smoothness and localization. |
| Symlet (Sym4) | Feature extraction in physiological signals like ECG [1] | Near-symmetric; improves signal reconstruction quality for feature detection. |
| Fast Fourier Transform (FFT) | Foundation for MRI reconstruction [4], frequency-domain segmentation [9] | Efficient O(N log N) algorithm; transforms spatial data to global frequency representation. |
| Discrete Fourier Cosine Transform (DFCT) | Block-based medical image denoising [7] | Localized frequency processing; excels in preserving fine details without global artifacts. |
| Benchmark Datasets (LIDC-IDRI, LUNA16, MosMed) | Training and validation of compression/denoising algorithms [8] | Publicly available curated medical images (CT scans) with annotations for standardized comparison. |
| Adversarial Noise Benchmark Datasets | Evaluating model robustness and noise resilience [9] | Custom datasets incorporating various noise levels (Gaussian, salt-and-pepper) for stress-testing. |
The comparative analysis reveals that neither DWT nor Fourier transforms represent universally superior solutions for medical imaging; rather, they offer complementary strengths. DWT excels in applications requiring spatial localization and multi-resolution analysis, such as image compression and registration, where preserving edges and structural hierarchies is paramount [8] [10]. Fourier-based methods demonstrate superior performance in global frequency analysis and noise resilience, making them ideal for MRI reconstruction and adversarial attack resistance [9] [4]. Emerging research indicates that hybrid approaches, which integrate the strengths of both transforms with deep learning architectures, represent the most promising future direction. These include wavelet-guided ConvNeXt for registration [10], Fourier-based lightweight segmentation networks [9], and cross-attention wavelet frameworks for compression [8], ultimately advancing the precision and efficiency of medical image analysis for improved diagnostic outcomes.
Multi-Resolution Analysis (MRA), particularly through the Discrete Wavelet Transform (DWT), provides a powerful framework for decomposing medical images into constituent frequency sub-bands, enabling specialized processing of anatomical features at different scales [8]. This decomposition separates an image into a multi-scale representation comprising approximation coefficients (low-frequency components carrying broad structural information) and detail coefficients (high-frequency components containing fine textures, edges, and diagnostic details) [8] [11]. Unlike traditional Fourier methods that offer only frequency localization, DWT delivers both frequency and spatial localization, allowing researchers to isolate and analyze specific image features within particular spatial regions [12]. This capability is particularly valuable in medical imaging, where diagnostically relevant information is often concentrated in specific frequency ranges and anatomical locations.
The mathematical foundation of DWT involves projecting an image onto a set of basis functions derived from a mother wavelet through scaling and translation operations [11]. This process generates a hierarchical decomposition across multiple resolution levels, with each level further separating frequency components. For medical image analysis, this multi-scale approach enables researchers to develop algorithms that selectively process or enhance features based on their clinical significance [8] [13]. The practical implementation typically utilizes filter banks with low-pass and high-pass filters to separate frequency components, followed by downsampling to create the multi-resolution pyramid [14]. This technical foundation supports diverse medical imaging applications including compression, synthesis, and denoising, which will be explored in subsequent sections of this document.
Key Applications in Medical Imaging Research
Image Compression for Telemedicine
Wavelet-based multi-resolution analysis enables advanced medical image compression by separating image content into frequency sub-bands that can be selectively quantized based on their diagnostic importance [8]. Recent research incorporates cross-attention learning (CAL) modules with DWT to create hybrid compression frameworks that dynamically weight feature maps, prioritizing clinically relevant regions such as lesions or tissue boundaries [8]. This approach achieves superior rate-distortion optimization compared to conventional codecs like JPEG2000 and H.265/HEVC, significantly reducing storage and transmission bandwidth requirements while preserving diagnostic integrity [8]. The integration of Variational Autoencoders (VAEs) further enhances compression efficiency by providing a probabilistic latent space for entropy coding, making these methods particularly valuable for cloud-based healthcare platforms and real-time telemedicine applications [8].
Multi-Modal Medical Image Synthesis
Dual-branch wavelet encoding architectures leverage MRA to address the challenging problem of multi-modal medical image synthesis, where missing imaging modalities are generated from available data [14]. These systems employ wavelet multi-scale downsampling (Wavelet-MS-Down) modules that perform near-lossless feature dimensionality reduction by separately processing low-frequency structural contours and high-frequency anatomical details [14]. The decomposition enables targeted processing of different frequency components, with deformable cross-attention feature fusion (DCFF) modules facilitating deep interaction between features extracted from different source modalities [14]. This approach has demonstrated particular effectiveness in brain MRI synthesis, where it successfully generates missing sequences (T1, T1ce, T2, FLAIR) by exploiting complementary information across modalities while preserving high-frequency pathological features essential for diagnostic accuracy [14].
Medical Image Denoising
Wavelet-based MRA provides an effective framework for medical image denoising through thresholding of detail coefficients in the transform domain [11]. The approach leverages the statistical properties of wavelet coefficients, where noise typically distributes across coefficients differently from anatomical structures [12]. Recent advancements combine DWT with Bayesian-optimized bilateral filtering to achieve enhanced denoising performance, particularly for Low-Dose Computed Tomography (LDCT) images corrupted by Gaussian noise [12] [11]. The bilateral filter's parameters are optimized using Bayesian methods to maintain optimal balance between noise suppression and edge preservation [12]. Studies demonstrate that DWT-based denoising achieves superior quantitative results, with PSNR values up to 33.85 dB and SSIM of 0.7194 at noise level σ=10, outperforming other transform domain methods like PCA, MSVD, and DCT [11].
Tumor Diagnosis and Characterization
Topological Data Analysis (TDA) combined with wavelet transforms has emerged as a novel approach for extracting robust imaging biomarkers for tumor diagnosis [15] [16]. The WT-TDA algorithm leverages wavelet-based MRA to enhance topological feature representation in ultrasound images, effectively capturing multiscale pathological patterns associated with malignancy [15] [16]. By analyzing persistent homology across wavelet-decomposed sub-bands, the method identifies topological features (connected components, loops, voids) that correlate with histological diagnosis [16]. This approach has demonstrated exceptional diagnostic performance across multiple tumor types, achieving test accuracies of 0.932, 0.805, and 0.888 for breast, thyroid, and kidney cancers, respectively [15]. The method provides enhanced interpretability through SHAP analysis, identifying clinically relevant topological features that serve as quantitative biomarkers for malignant transformation [16].
Multi-Modal Image Fusion
Wavelet-based MRA enables effective fusion of complementary information from different imaging modalities, such as combining anatomical details from CT with functional information from PET [13]. The Wavelet Attention network (WTA-Net) incorporates spatial-channel attention mechanisms within the wavelet domain to selectively enhance diagnostically relevant features during fusion [13]. This approach processes individual frequency sub-bands with specialized attention modules, improving information entropy by 34.76% for PET components and 12.7% for CT components compared to standard wavelet decomposition [13]. The method effectively preserves metabolic activity information from PET while maintaining anatomical context from CT, creating fused images with comprehensive diagnostic information that supports improved clinical decision-making [13].
Table 1: Quantitative Performance of Wavelet-Based Medical Imaging Applications
| Application Domain | Performance Metrics | Reported Values | Datasets Validated |
|---|---|---|---|
| Image Compression [8] | PSNR, SSIM, MSE | Superior to JPEG2000 and BPG | LIDC-IDRI, LUNA16, MosMed |
| Image Denoising [11] | PSNR: 33.85 dB, SSIM: 0.7194 | SNR: 28.50 dB (σ=10) | SARS-CoV-2 CT-scan dataset |
| Tumor Diagnosis [15] | Accuracy: 0.932, 0.805, 0.888 | AUC: 0.915, 0.805, 0.889 | Breast, Thyroid, Kidney Ultrasound |
| Image Fusion [13] | Information Entropy improved 34.76% (PET) | Spatial Frequency improved 49.4% (CT) | Brain MRI, PET/CT datasets |
Experimental Protocols
Protocol 1: Wavelet-Based Medical Image Compression
Objective: To implement a hybrid compression framework combining DWT with cross-attention learning for diagnostic image compression.
Materials and Reagents:
- Medical image dataset (LIDC-IDRI, LUNA16, or MosMed)
- Python 3.8+ with PyWavelets, TensorFlow 2.8+
- High-performance computing workstation with GPU (NVIDIA RTX 3080+ recommended)
Methodology:
- Image Preprocessing: Normalize input images to [0,1] range and resize to dimensions divisible by 2^n, where n is the desired decomposition levels.
- Wavelet Decomposition: Apply 2D DWT with Daubechies-4 (db4) wavelets to decompose each image into approximation (LL), horizontal (HL), vertical (LH), and diagonal (HH) sub-bands at 3 decomposition levels [8].
- Cross-Attention Learning: Process approximation sub-band through CAL module with dynamic feature weighting:
- Compute query (Q), key (K), and value (V) projections from different feature dimensions
- Calculate attention weights: Attention(Q,K,V) = softmax(QK^T/√d)V
- Apply weights to emphasize diagnostically relevant regions [8]
- Variational Autoencoder Processing: Encode weighted features through lightweight VAE with bottleneck dimension of 128 for latent representation refinement.
- Entropy Coding: Apply arithmetic coding to quantized coefficients for final bitstream generation.
- Reconstruction: Reverse the process using Inverse DWT (IDWT) for image reconstruction.
Validation Metrics: Calculate PSNR, SSIM, and MSE between original and reconstructed images. Compare with JPEG2000 and BPG codecs at equivalent bit rates [8].
Protocol 2: Wavelet-Based Medical Image Denoising
Objective: To implement DWT-based denoising with Bayesian-optimized bilateral filtering for LDCT images.
Materials and Reagents:
- LDCT dataset (e.g., SARS-CoV-2 CT-scan dataset)
- MATLAB R2023a with Wavelet Toolbox
- Bayesian optimization toolbox
Methodology:
- Noise Characterization: Estimate noise parameters from homogeneous image regions using method of moments.
- Wavelet Decomposition: Apply 2D DWT with Symlets-8 (sym8) wavelets at 4 decomposition levels [11].
- Thresholding: Implement BayesShrink adaptive thresholding for detail coefficients:
- Estimate noise variance σₙ² from HH sub-band: σₙ² = median(|HH₁|)/0.6745
- Calculate signal variance for each sub-band: σₓ² = max(σₛ² - σₙ², 0)
- Compute threshold: T = σₙ²/σₓ
- Apply soft thresholding to detail coefficients [12]
- Bayesian-Optimized Bilateral Filtering:
- Define objective function for parameter optimization: f(σs, σr) = -PSNR(denoised_image)
- Use Bayesian optimization with Gaussian process priors over 30 iterations to find optimal spatial (σs) and range (σr) parameters [12]
- Apply optimized bilateral filter as post-processing step
- Reconstruction: Apply IDWT to thresholded coefficients and bilateral-filtered image.
Validation Metrics: Calculate PSNR, SNR, and SSIM at noise levels σ=10,20,30,40. Compare with PCA, MSVD, and DCT methods [11].
Table 2: Research Reagent Solutions for Wavelet-Based Medical Image Analysis
| Research Reagent | Function | Application Examples |
|---|---|---|
| PyWavelets Library | Python DWT implementation | Multi-resolution decomposition for compression, denoising |
| Daubechies Wavelets (db4) | Orthogonal wavelet with 4 vanishing moments | Medical image compression [8] |
| Symlets Wavelets (sym8) | Near-symmetric orthogonal wavelets | Image denoising with reduced phase distortion [11] |
| Bayesian Optimization Toolbox | Parameter optimization for bilateral filtering | Denoising parameter selection [12] |
| Cross-Attention Modules | Dynamic feature weighting | Region-of-interest emphasis in compression [8] |
| Topological Data Analysis Library | Persistent homology computation | Tumor biomarker extraction [15] [16] |
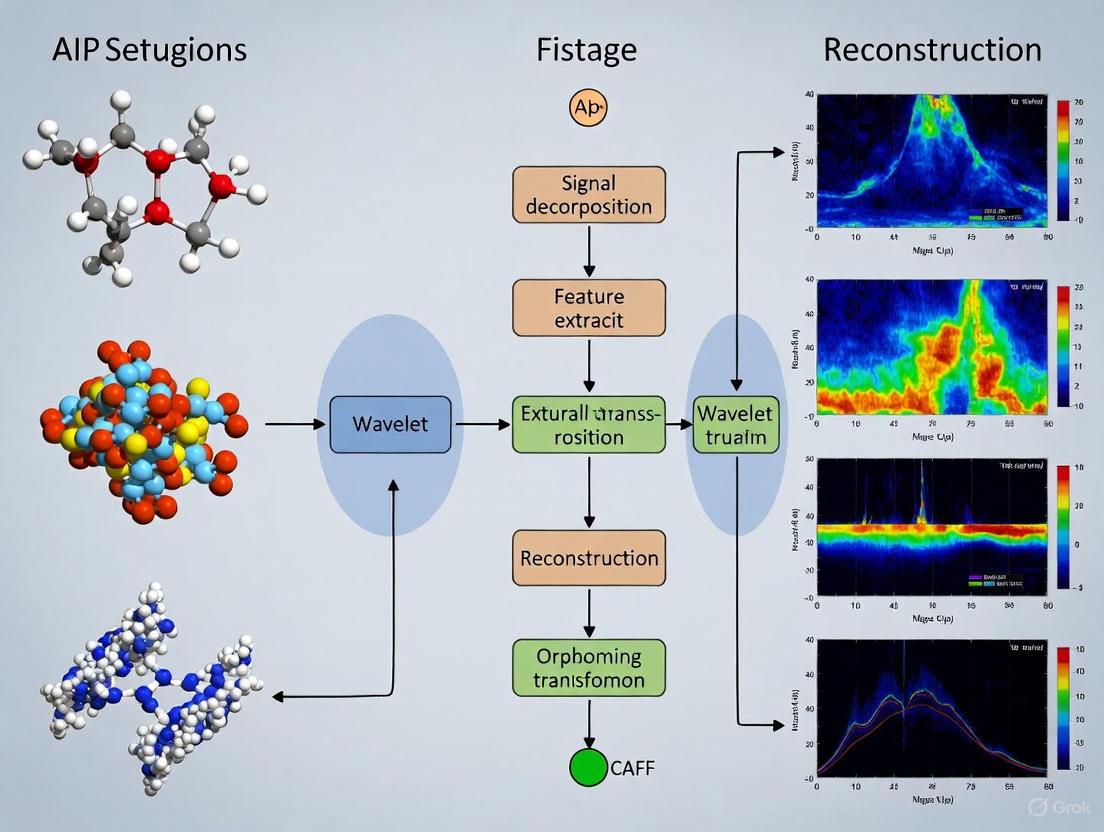
Visualization of Workflows
Wavelet-Based Medical Image Compression Workflow
Wavelet-Based Medical Image Denoising Protocol
Multi-resolution analysis through wavelet transform represents a versatile and powerful framework for advancing medical imaging research. By decomposing images into frequency sub-bands, researchers can develop specialized algorithms that selectively process clinically relevant information while suppressing noise and redundant data [8] [11]. The protocols outlined in this document provide practical methodologies for implementing wavelet-based approaches across key applications including compression, denoising, synthesis, and diagnostic biomarker extraction [8] [14] [15]. The quantitative results demonstrate consistent performance advantages over traditional methods, while the visualization workflows offer clear implementation guidance. As medical imaging continues to evolve toward precision medicine and quantitative biomarkers, wavelet-based MRA will remain an essential tool for extracting clinically meaningful information from medical images across scales and modalities.
Why Wavelets? Advantages for Preserving Spatial and Diagnostic Information
In medical imaging, the integrity of spatial and diagnostic information is paramount. Wavelet transform-based techniques have emerged as a powerful solution, uniquely capable of preserving critical image details that other methods often compromise. Unlike traditional Fourier-based analyses that provide only global frequency information, wavelets offer multi-resolution analysis, allowing for the simultaneous examination of an image's global structure and local fine details. This capability is fundamental for clinical applications, where the preservation of edges, textures, and subtle pathological features directly impacts diagnostic accuracy. This document outlines the core advantages of wavelet transforms and provides detailed protocols for their application in medical imaging research, supporting a broader thesis on their transformative role in the field.
Core Advantages and Quantitative Performance
The principal advantage of wavelet transforms lies in their ability to perform localized frequency analysis. An image is decomposed into different frequency sub-bands at multiple scales, allowing for targeted processing. Clinically significant high-frequency components, such as tissue boundaries and micro-calcifications, can be preserved or enhanced, while noise in similar frequency ranges can be selectively attenuated.
The table below summarizes quantitative evidence demonstrating the effectiveness of wavelet-based methods across diverse medical imaging tasks.
Table 1: Quantitative Performance of Wavelet-Based Methods in Medical Imaging
| Application Area | Key Methodology | Reported Performance Metrics | Preservation of Diagnostic Information |
|---|---|---|---|
| Hyperspectral Data Compression [17] | Daubechies wavelet transformation with spectral cropping and scale matching. | Achieved up to 32× compression (96.88% reduction) with minimal loss of spectral/spatial data. | Preserved original wavelength scale for straightforward spectral interpretation; improved contrast and noise reduction. |
| Medical Image Compression [8] [18] | Hybrid DWT/Cross-Attention Learning & SWT/GLCM/SDAE frameworks. | Superior PSNR and SSIM vs. JPEG2000/BPG; PSNR up to 50.36 dB, MS-SSIM of 0.9999 [18]. | Cross-attention and texture-aware encoding dynamically prioritize clinically relevant regions (e.g., lesions). |
| MRI Brain Denoising [19] | Systematic evaluation of wavelets (e.g., bior6.8) with universal thresholding. | Optimal PSNR: 27.38 dB (σ=10); 25.25 dB (σ=15). Optimal SSIM: 0.647 (σ=10); 0.589 (σ=15). | Effectively preserved essential anatomical structures while removing Gaussian noise. |
| CT Image Denoising [11] | Discrete Wavelet Transform (DWT) with thresholding. | Achieved PSNR of 33.85 dB, SSIM of 0.7194 at noise level σ=10, outperforming PCA, MSVD, and DCT. | Superior noise suppression while preserving critical edge information in LDCT images. |
| Brain Tumor Segmentation [20] | Adaptive Discrete Wavelet Decomposition & Iterative Axial Attention. | Average Dice scores of 85.0% (BraTS2020) and 88.1% (FeTS2022) with only 5.23 million parameters. | Preserved finer structural details of tumor sub-regions (e.g., enhanced tumors, edemas). |
Conceptual Workflow: Multi-Resoluti on Analysis
The following diagram illustrates the fundamental process of a 2D Discrete Wavelet Transform (DWT) for image analysis, which enables the preservation of spatial-diagnostic information.
Multi-Scale Wavelet Decomposition Workflow: This process shows how an image is recursively separated into approximation and detail coefficients, enabling analysis and processing at multiple resolutions.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of wavelet-based medical image analysis requires a combination of computational tools and data resources.
Table 2: Essential Research Toolkit for Wavelet-Based Medical Imaging
| Tool/Reagent | Function & Utility | Exemplars & Notes |
|---|---|---|
| Wavelet Families | Basis functions for decomposition; choice impacts smoothness, symmetry, and reconstruction. | Daubechies (dbN): Compact support, orthogonal [17] [19]. Biorthogonal (biorN.N): Linear phase, symmetry ideal for denoising [19]. Symlets (symN): Near-symmetry, good for general analysis [19]. |
| Thresholding Functions | Nonlinear operators to suppress noise in wavelet domain. | Soft Thresholding: Continuous shrinkage, smoother results [19] [21]. Hard Thresholding: Preserves large coefficients better but can be discontinuous [19] [21]. |
| Performance Metrics | Quantify denoising, compression, and segmentation efficacy. | PSNR: Measures noise suppression [19]. SSIM/MS-SSIM: Assesses perceptual structural fidelity [8] [18] [19]. Dice Score: Evaluates segmentation accuracy [20]. |
| Benchmark Datasets | Standardized data for training, validation, and comparative analysis. | Brain MRIs: BraTS2020 [14] [20], IXI [14] [10]. General Compression: DIV2K, CLIC [18]. CT Scans: SARS-CoV-2 CT-scan dataset [11]. |
Detailed Experimental Protocols
Protocol 1: Wavelet-Based Medical Image Denoising
This protocol is adapted from systematic evaluations for denoising MRI brain images and CT scans [19] [11].
1. Objectives: To effectively suppress additive Gaussian noise in medical images while preserving critical diagnostic features such as edges and textures.
2. Materials and Reagents:
- Datasets: Brain tumor MRI dataset from figshare (3,064 images) [11] or a public SARS-CoV-2 CT-scan dataset [11].
- Software: Python with PyWavelets (
pywt) library, NumPy, OpenCV, or equivalent MATLAB toolboxes. - Wavelet Options: Daubechies (
db3), Symlet (sym4), or Biorthogonal (bior6.8) [19].
3. Experimental Procedure:
1. Preprocessing: Load the medical image. Normalize pixel intensities to a [0, 255] range if required [19].
2. Noise Simulation (For Validation): To a clean image, add Gaussian noise with mean (μ) = 0 and standard deviation (σ) = 10, 15, or 25 to simulate realistic noise conditions [19].
3. Wavelet Decomposition: Apply a 2-level 2D Discrete Wavelet Transform (DWT) using a selected wavelet (e.g., bior6.8) [19]. This generates one approximation sub-band (LL) and three detail sub-bands (LH, HL, HH) per level.
4. Thresholding:
* Calculate Threshold: Compute the universal threshold, τ, for each detail sub-band using the formula: τ = σ_noise * sqrt(2 * log(N)), where N is the number of coefficients in the sub-band [19].
* Apply Threshold Function: Apply soft thresholding to the detail coefficients (LH, HL, HH) of all decomposition levels. Soft thresholding is defined as: c_hat = sign(c) * max(0, |c| - τ) [19].
5. Image Reconstruction: Perform an inverse DWT using the original approximation coefficients and the modified (thresholded) detail coefficients to reconstruct the denoised image.
4. Data Analysis:
* Calculate PSNR and SSIM between the denoised image and the clean ground truth image [19] [11].
* For σ = 15, the target PSNR and SSIM using bior6.8 with universal thresholding should be approximately 25.25 dB and 0.589, respectively [19].
Protocol 2: Wavelet-Based Compression of Hyperspectral Imaging (HSI) Data
This protocol is based on a scale-preserving compression method for VNIR and SWIR hyperspectral data [17].
1. Objectives: To achieve high-compression ratios for large HSI datasets while preserving the original wavelength scale and critical spectral-spatial information.
2. Materials and Reagents:
- Data: Hyperspectral data cubes (e.g., medical HSI for diagnostic purposes).
- Software: Python with PyWavelets, NumPy, and SciPy.
- Wavelet: Daubechies wavelets.
3. Experimental Procedure: 1. Spectral Wavelet Transformation: Apply a 1D wavelet transform along the spectral dimension of the HSI data cube for dimensionality reduction [17]. 2. Spectral Cropping: Eliminate spectral bands with low-intensity signals, which contribute less diagnostically relevant information [17]. 3. Scale Matching: Implement a mapping function to ensure the compressed data's wavelength scale accurately corresponds to the original data, enabling direct spectral interpretation [17]. 4. Encoding & Storage: Use standard entropy coding (e.g., Huffman coding) on the processed wavelet coefficients before storage or transmission [17].
4. Data Analysis: * Calculate the compression ratio (original size / compressed size). * Evaluate spectral fidelity by comparing extracted spectral signatures from original and compressed data. * Assess spatial feature retention using metrics like SSIM. The target is up to 32× compression with minimal loss of important data [17].
Protocol 3: Integration of Wavelets with Deep Learning for Segmentation
This protocol leverages a lightweight framework for 3D brain tumor segmentation that integrates adaptive discrete wavelet decomposition [20].
1. Objectives: To improve the accuracy and efficiency of segmenting tumor sub-regions from 3D MRI data by capturing multi-scale features in the frequency domain.
2. Materials and Reagents:
- Datasets: BraTS2020 or FeTS2022 multi-modal MRI datasets [20].
- Model Framework: A U-Net-like architecture with a custom wavelet decomposition module.
- Wavelet: 3D Discrete Wavelet Transform.
3. Experimental Procedure: 1. Network Architecture: * Encoder: Replace standard pooling/downsampling layers with an Adaptive Wavelet Decomposition (AWD) module. This module uses 3D DWT to decompose the feature maps into low-frequency (approximation) and high-frequency (detail) sub-bands, preserving multi-scale information without data loss [20]. * Bottleneck: Incorporate an attention mechanism (e.g., Iterative Axial Factorization Attention) to model long-range dependencies efficiently [20]. * Decoder: Use a multi-scale feature fusion decoder (MSFFD) that progressively upsamples and aligns features from the encoder and bottleneck using skip connections [20]. 2. Training: Train the model using a combined loss function (e.g., Dice loss and Cross-Entropy loss) on annotated 3D MRI volumes.
4. Data Analysis: * Evaluate segmentation performance using the Dice Similarity Coefficient for the whole tumor (WT), tumor core (TC), and enhancing tumor (ET). * The target Dice scores on BraTS2020 should be competitive with state-of-the-art methods, approximately 85.0%, while maintaining a low parameter count (~5.23 million) [20].
Future Directions
The integration of wavelet transforms with deep learning represents the frontier of medical image analysis. Future research will focus on developing end-to-end learnable wavelet kernels, where the optimal wavelet bases for specific imaging modalities or diagnostic tasks are learned directly from the data, rather than being pre-defined. Furthermore, the application of hybrid wavelet-attention models, as seen in segmentation and synthesis tasks [14] [20], is poised to expand into other areas like disease prognostication and treatment monitoring, enhancing the role of wavelets in computational pathology and personalized medicine.
Key Wavelet Families and Their Characteristics for Medical Image Processing
Wavelet transforms have become a cornerstone of modern medical image processing, providing a powerful mathematical framework for multi-resolution analysis. Unlike traditional Fourier methods, wavelets excel at representing local features in both spatial and frequency domains, making them ideal for analyzing complex anatomical structures and pathological signatures in medical images [22]. The selection of an appropriate wavelet family—each with distinct characteristics—is critical for optimizing performance in applications ranging from denoising and compression to feature extraction and image synthesis [23]. This article provides a comprehensive overview of key wavelet families and establishes detailed experimental protocols for their application in medical imaging research, framed within the broader context of wavelet transform-based techniques for medical imaging research.
Key Wavelet Families and Their Mathematical Properties
Fundamental Properties of Wavelets
A wavelet family is defined by its mother wavelet ψ(x), which must satisfy specific mathematical conditions to ensure stable inversion: normalized energy (∫|ψ(x)|²dx = 1), finite energy (∫|ψ(x)|dx < ∞), and a zero mean (∫ψ(x)dx = 0) [22]. These conditions enable the wavelet transform to analyze signal fluctuations without altering the total signal flux. Additional properties tailored to specific applications include continuity, differentiability, compact support, and vanishing moments [22].
Prominent Wavelet Families in Medical Imaging
Table 1: Characteristics of Major Wavelet Families in Medical Imaging
| Wavelet Family | Key Members | Symmetry | Vanishing Moments | Support Width | Orthogonality | Primary Medical Applications |
|---|---|---|---|---|---|---|
| Haar | haar, db1 | Symmetric | 1 | 1 | Orthogonal | Image fusion [23], didactic visualization [22] |
| Daubechies | db2-db20 | Asymmetric | N (order) | 2N-1 | Orthogonal | Denoising [6], compression [24] |
| Symlets | sym2-sym20 | Near symmetric | N (order) | 2N-1 | Orthogonal | General processing [23] |
| Coiflets | coif1-coif5 | Near symmetric | 2N (order) | 6N-1 | Orthogonal | Denoising [6] |
| Biorthogonal | bior1.1-bior6.8 | Symmetric | Customizable | Variable | Biorthogonal | Image reconstruction [23] |
| Reverse Biorthogonal | rbio1.1-rbio6.8 | Symmetric | Customizable | Variable | Biorthogonal | CT-MRI fusion [23] |
| Discrete Meyer | dmey | Symmetric | - | - | Orthogonal | Specialized analysis [23] |
The Haar wavelet represents one of the simplest and oldest orthonormal wavelets, with a discontinuous structure resembling a step function. Its scaling function φ(t) equals 1 for 0 ≤ t ≤ 1 and 0 elsewhere, providing a piecewise constant approximation that is valuable for didactic purposes but limited in representing continuous signals smoothly [22] [23].
The Daubechies family (dbN), developed by Ingrid Daubechies, offers compactly supported orthonormal wavelets with increasing smoothness as the order N increases. The db1 variant is functionally identical to the Haar wavelet. Higher-order Daubechies wavelets (e.g., db2-db20) provide better frequency localization and are frequently employed in medical image denoising and compression tasks [22] [6] [24].
Biorthogonal wavelets utilize different wavelet functions for decomposition and reconstruction, achieving perfect reconstruction while maintaining symmetry and linear phase properties critical for image reconstruction without artifact introduction [23]. This family is particularly valuable in medical image compression applications where visual fidelity must be preserved [24].
Symlets and Coiflets represent modifications of the Daubechies family optimized for increased symmetry while maintaining orthogonality. Symlets offer near-symmetry, while Coiflets were designed at the request of Ronald Coifman to feature scaling functions with vanishing moments, making them suitable for denoising applications where phase preservation is important [6] [23].
Wavelet Selection Guidelines
Selection of an appropriate wavelet family depends on specific application requirements:
- Denoising: Daubechies (db2) and Coiflets have demonstrated superior performance in medical image denoising, particularly with undecimated discrete wavelet transform variants [6].
- Image Fusion: Haar, biorthogonal 1.1 (bior1.1), and reverse biorthogonal 1.1 (rbio1.1) have outperformed other families in CT-MRI fusion tasks [23].
- Compression: Biorthogonal wavelets are preferred for their symmetric, linear-phase properties that minimize reconstruction artifacts [24].
- Feature Extraction: Wavelets with higher vanishing moments (e.g., higher-order Daubechies) better represent complex textures in radiomics analysis [25].
Experimental Protocols for Medical Image Processing
Protocol 1: Wavelet-Based Medical Image Denoising
This protocol details a modified undecimated discrete wavelet transform (UDWT) approach for medical image denoising, combining shift invariance with effective noise suppression [6].
Research Reagent Solutions
- Software Environment: MATLAB or Python with PyWavelets library.
- Wavelet Function: Daubechies order 2 (db2) wavelet filters [6].
- Input Data: Medical images (e.g., mammograms, CT slices) in DICOM format.
- Computational Resources: Standard workstation with sufficient RAM for image series processing.
Procedure
- Image Decomposition: Perform 2-level 2D stationary wavelet decomposition on the noisy medical image using db2 filters to obtain approximation (LL) and detail (LH, HL, HH) coefficients for each level without downsampling.
Hierarchical Correlation Calculation: For each detail subband (LH, HL, HH), compute the hierarchical correlation between level 1 and level 2 coefficients using the element-wise product:
Correlation = |Coef_lev1 × Coef_lev2|[6].Adaptive Threshold Determination:
- Generate correlation images for each detail subband using the formula from step 2.
- Find maximum correlation values in each row of the correlation image.
- Compute the mean (Mean_max) of these maximum values.
- Eliminate correlation values greater than 0.8 × Mean_max (considered signal).
- Calculate standard deviation (σ) of remaining correlation values.
- Set threshold: THR = 1.6 × σ [6].
Coefficient Thresholding: Apply the determined threshold to level 1 detail coefficients:
NewCoef_lev1 = { Coef_lev1, if |Coef_lev1 × Coef_lev2| ≥ THR; 0, otherwise }[6].Image Reconstruction: Perform inverse stationary wavelet transform using the level 2 approximation coefficients and the modified level 1 detail coefficients to reconstruct the denoised image.
UDWT Denoising Workflow: This diagram illustrates the step-by-step process for medical image denoising using a modified undecimated discrete wavelet transform approach with adaptive thresholding.
Protocol 2: Wavelet Radiomics Feature Extraction for Tumor Classification
This protocol describes a methodology for extracting wavelet-domain radiomics features from multiphase CT images to improve classification of hepatocellular carcinoma (HCC) versus non-HCC focal liver lesions [25].
Research Reagent Solutions
- Medical Imaging Data: Multiphase CT scans (non-contrast, arterial, venous, delayed phases).
- Segmentation Tools: ITK-SNAP or 3D Slicer for manual ROI delineation.
- Wavelet Transform: PyWavelets or MATLAB Wavelet Toolbox.
- Feature Selection: Logistic sparsity-based model with Bayesian optimization.
- Classification Algorithms: Support Vector Machines (SVM), Multilayer Perceptron (MLP).
Procedure
- Data Preparation and ROI Segmentation:
- Obtain multiphase CT scans following standardized acquisition protocols.
- Manually segment focal liver lesions across all phases to create 3D regions of interest (ROI) verified by experienced radiologists.
Multi-Domain Feature Extraction:
- Original Domain Features: Extract first-order statistics (mean, variance, skewness, kurtosis) and second-order texture features (GLCM, GLRLM) from each CT phase.
- Wavelet Domain Features: Apply 3D discrete wavelet transform to each ROI using Daubechies or Symlets filters. Extract identical feature sets from each wavelet subband (LLL, LLH, LHL, LHH, HLL, HLH, HHL, HHH).
Feature Combination and Selection:
- Concatenate original and wavelet-domain features into a comprehensive feature vector.
- Apply logistic sparsity-based feature selection with Bayesian optimization to identify the most discriminative features while handling the high feature-to-sample ratio.
Model Training and Validation:
- Train classifier models (SVM, MLP) using the selected wavelet radiomics features.
- Validate using cross-validation and independent test sets, evaluating performance with AUC, accuracy, sensitivity, and specificity metrics.
Wavelet Radiomics Analysis: This workflow demonstrates the process for extracting and analyzing wavelet-based radiomics features from multiphase CT images for hepatocellular carcinoma classification.
Protocol 3: Multi-Modal Medical Image Fusion
This protocol outlines a discrete wavelet transform-based approach for fusing CT and MRI images to combine complementary diagnostic information [23].
Research Reagent Solutions
- Input Images: Registered CT and MRI brain scans (spatially aligned).
- Wavelet Families: Haar (db1), bior1.1, rbio1.1 for optimal fusion quality.
- Fusion Rule: Maximum selection rule for coefficient combination.
- Evaluation Metrics: Qualitative assessment and quantitative metrics (classical and gradient information).
Procedure
- Image Registration: Ensure precise spatial alignment between CT and MRI images using rigid or deformable registration methods.
Wavelet Decomposition: Apply 2-level 2D discrete wavelet transform to both registered CT and MRI images using selected wavelet filters (e.g., Haar, bior1.1, rbio1.1).
Coefficient Fusion: Apply the maximum selection rule to corresponding wavelet coefficients:
- For approximation coefficients (low-frequency): Compute weighted average based on local energy.
- For detail coefficients (high-frequency): Select the coefficient with maximum absolute value.
Image Reconstruction: Perform inverse discrete wavelet transform on the fused coefficients to create the composite image.
Quality Assessment: Evaluate fusion quality through:
- Qualitative Analysis: Visual assessment of anatomical structure preservation and feature integration.
- Quantitative Analysis: Calculate classical metrics (entropy, mutual information) and gradient-based metrics to evaluate edge preservation and information transfer.
Advanced Applications in Medical Imaging
Medical Image Synthesis Using Wavelet Encoding
Recent advances in multi-modal medical image synthesis have incorporated wavelet transforms within deep learning architectures. The Dual-branch Wavelet Encoding and Deformable Feature Interaction GAN (DWFI-GAN) utilizes wavelet multi-scale downsampling (Wavelet-MS-Down) to decompose input modalities into low-frequency contours and high-frequency details [14]. This approach enables near-lossless feature dimensionality reduction while preserving global structural information and fine-grained textures, significantly improving the synthesis of missing modalities in incomplete clinical datasets.
Wavelet-Based Medical Image Compression
Hybrid DWT-Vector Quantization (DWT-VQ) techniques have demonstrated promising results in medical image compression, effectively balancing compression ratios with diagnostic quality preservation [24]. The process involves: (1) speckle noise reduction in ultrasound imagery using specialized filters, (2) discrete wavelet transform decomposition, (3) coefficient thresholding, (4) vector quantization, and (5) Huffman encoding of the quantized coefficients. This approach maintains medically tolerable perceptual quality while significantly reducing storage requirements.
Enhancement of Image Registration
Stationary Wavelet Transform (SWT) has been successfully integrated with mutual information for improved planning CT and cone beam-CT (CBCT) image registration in radiotherapy [26]. The translationally invariant property of SWT helps highlight edge features in noisy CBCT images, while the incorporation of gradient information compensates for the lack of spatial information in traditional mutual information approaches, resulting in enhanced registration accuracy and robustness.
Wavelet families offer diverse mathematical properties that can be strategically leveraged to address specific challenges in medical image processing. The Haar, Daubechies, and biorthogonal families provide distinct trade-offs between symmetry, support width, and vanishing moments that directly impact performance in denoising, feature extraction, and image fusion tasks. The experimental protocols detailed in this article provide researchers with standardized methodologies for implementing wavelet-based techniques, while the advanced applications demonstrate the ongoing innovation in integrating wavelet transforms with modern deep learning approaches. As medical imaging continues to evolve, wavelet-based methods remain essential tools for enhancing diagnostic capability, improving computational efficiency, and extracting clinically relevant information from complex medical image data.
Cutting-Edge Applications in Medical Image Analysis and AI
In medical imaging, the dual imperative of reducing noise while preserving crucial diagnostic features such as edges and textures is a fundamental challenge. Noise, introduced during image acquisition or transmission, can obscure subtle pathological details, potentially leading to misinterpretation. Within the broader context of wavelet transform-based techniques for medical imaging research, this document provides detailed application notes and experimental protocols. It is designed to assist researchers and scientists in implementing robust denoising frameworks that effectively balance noise suppression with the preservation of structural integrity, a balance critical for applications in diagnostics and drug development.
Performance Analysis of Denoising Techniques
The efficacy of denoising algorithms is quantitatively assessed using standard image quality metrics. The following tables summarize the performance of various techniques across different imaging scenarios, providing a basis for algorithmic selection.
Table 1: Comparative Performance of Denoising Algorithms on Medical Images (MRI & HRCT) [27]
| Algorithm | PSNR (dB) | SSIM | Computational Efficiency | Optimal Noise Level |
|---|---|---|---|---|
| BM3D | High | High | Moderate | Low, Moderate |
| DnCNN (Deep Learning) | High | High | Low | High |
| WNNM | Moderate | Moderate | Low | High |
| EPLL | Moderate | Moderate | Low | High |
| NLM | Moderate | Moderate | Low | Low |
| Bilateral Filter | Low | Low | High | Low |
| Guided Filter | Low | Low | High | Low |
| FoE | Low | Low | Moderate | Low |
Table 2: Quantitative Results of Multi-Scale Denoising Methods [28]
| Method | PSNR (dB) | SSIM | Computational Complexity (seconds) |
|---|---|---|---|
| Gaussian Pyramid (GP) | 36.80 | 0.94 | 0.0046 |
| Wavelet (Coiflet4) | 34.12 | 0.91 | 0.0081 |
| Wavelet (Daubechies db4) | 33.85 | 0.90 | 0.0079 |
| Wavelet (Haar) | 32.98 | 0.89 | 0.0075 |
| Wavelet (Symlet4) | 33.91 | 0.90 | 0.0080 |
Table 3: Wavelet Thresholding Functions for Image Denoising [29] [21]
| Threshold Function | Mathematical Form | Advantages | Disadvantages |
|---|---|---|---|
| Hard | $θ_H(x) = \begin{cases} 0 & \text{if } |x| \leq δ \ x & \text{if } |x| > δ \end{cases}$ | Simplicity, preserves strong edges | Introduces artifacts (e.g., pseudo-Gibbs phenomena) |
| Soft | $θ_S(x) = \begin{cases} 0 & \text{if } |x| \leq δ \ \text{sgn}(x)(|x| - δ) & \text{if } |x| > δ \end{cases}$ | Smoother results, fewer artifacts | Can over-smooth details, leading to edge blurring |
| Median (Recommended) | N/A | Stability and convenience, good detail preservation | - |
| Smooth Garrote | $θ_{SG}(x) = \dfrac{x^{2n+1}}{x^{2n} + δ^{2n}}$ | Compromise between hard and soft thresholding | Parameter $n$ requires tuning |
Experimental Protocols
Protocol 1: Wavelet-Gaussian Denoising with Adaptive Edge Detection (EDAW)
This protocol outlines the steps for a hybrid method that integrates wavelet denoising with an adaptive edge detection framework, particularly effective for images corrupted by Gaussian noise [29].
1. Image Denoising Module: - Input: Noisy medical image (e.g., MRI, CT). - Wavelet Decomposition: Decompose the noisy image using a selected wavelet family (e.g., Daubechies 'db4', Symlet 'sym4') over 3-5 decomposition levels to obtain approximation (LL) and detail (LH, HL, HH) coefficients [21]. - Thresholding: Apply the median thresholding function to the detail coefficients. Avoid hard thresholding to prevent the introduction of artifacts. - Reconstruction: Perform an inverse wavelet transform on the thresholded coefficients to generate a denoised image.
2. Gradient Calculation & Non-Maximum Suppression (NMS): - Gradient Computation: Compute the gradient magnitude (G) and direction (θ) of the denoised image using the Sobel operator. - $G = \sqrt{(GX^2 + GY^2)}$ - $θ = \arctan{(GY / GX)}$ - where $GX$ and $GY$ are the gradients in the X and Y directions obtained using the Sobel kernels [29]. - Non-Maximum Suppression (NMS): Thin the edges to a single-pixel width by comparing the gradient magnitude of each pixel with its neighbors along the gradient direction (θ). Retain a pixel only if its magnitude is a local maximum.
3. Adaptive Thresholding and Edge Linking: - OTSU's Method: Apply the OTSU algorithm to the gradient magnitude image to automatically determine an optimal global threshold (T) for separating edge and non-edge pixels [29]. - Hysteresis Thresholding: Use a dual-threshold approach (derived from the OTSU threshold) to identify strong and weak edge pixels. Finally, link weak edges to strong ones if they are connected, to form continuous edge contours.
Protocol 2: Statistical Wavelet Model for Denoising and Enhancement (SWM-DE)
This protocol describes a method that uses a statistical model within a Bayesian framework for joint denoising and enhancement, which automatically adapts to the image data without requiring explicit noise level estimation [30].
1. Wavelet Coefficient Modeling: - Decomposition: Perform a multi-level wavelet decomposition of the noisy input image. - MAP Estimation: Model the marginal distribution of the noise-free wavelet coefficients. Within a Bayesian framework, develop a Maximum A Posteriori (MAP) estimator. This estimator is used to derive the noise-free coefficient from the observed noisy coefficient, effectively suppressing noise while preserving signal.
2. Morphological Reconstruction for Enhancement: - Adjustable Morphological Model: Apply an adjustable morphological reconstruction model to the initial denoised image. This step targets the removal of residual structured or unknown noises that the statistical step may have missed, while simultaneously preserving and enhancing image details.
3. Multi-Scale Reconstruction: - Component Extraction: Decompose the processed image into several wavelet sub-bands to separate illumination (low-frequency) and detail (high-frequency) components. - Inverse Transformation: Reconstruct the final enhanced, noise-free image by applying an inverse wavelet transform. This process yields an image with improved contrast and clarity, as measured by high EME (Measure of Enhancement) values [30].
Workflow Visualization
Wavelet-Based Denoising and Edge Detection
Statistical Wavelet Model (SWM-DE) Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Computational Tools
| Item / Tool | Function / Description | Example Use Case |
|---|---|---|
| Wavelet Toolbox (MATLAB/Python) | Provides libraries for performing DWT, thresholding, and reconstruction with various wavelet families. | Core component for implementing Protocols 1 & 2 [29] [30]. |
| Discrete Wavelet Transform (DWT) | Multi-resolution analysis tool to decompose an image into frequency sub-bands (LL, LH, HL, HH). | Image decomposition for noise separation in the transform domain [21] [8]. |
| Daubechies (dbN), Symlets (symN) | Wavelet families offering a balance between smoothness and localization; chosen based on image characteristics. | db4 is often used for its orthogonality and simplicity; sym4 for near-symmetry [21]. |
| Median Threshold Function | A stable thresholding function that avoids the artifacts of hard thresholding and over-smoothing of soft thresholding. | Recommended for compressing noisy wavelet coefficients in the denoising module [29]. |
| OTSU Thresholding Algorithm | Automatic, data-driven method for optimal global threshold selection by maximizing inter-class variance. | Adaptive thresholding in edge detection to binarize the gradient magnitude image [29]. |
| Sobel Operator Kernels | 3x3 convolution kernels used to approximate the image gradient in the horizontal and vertical directions. | Calculating gradient magnitude and direction for edge detection in Protocol 1 [29]. |
| BM3D Algorithm | A high-performance, non-deep learning denoising algorithm that uses collaborative filtering in 3D transform groups. | A strong benchmark for comparing the performance of wavelet-based denoising methods [27]. |
| Medical Image Datasets (e.g., LIDC-IDRI, SIDD) | Publicly available datasets of medical images (CT, MRI) and real-world noisy images for validation. | Training and quantitative evaluation of denoising algorithms using metrics like PSNR and SSIM [28] [8]. |
Multi-modal medical image fusion and synthesis have emerged as critical technologies in modern healthcare, addressing the inherent limitations of individual imaging modalities. In clinical practice, Positron Emission Tomography (PET) images excel at highlighting functional metabolic activity, such as tumor metabolism, but suffer from limited spatial resolution. Conversely, Computed Tomography (CT) provides high-resolution anatomical structures, including bone and dense tissues, but offers weak representation of low-density lesions. Magnetic Resonance Imaging (MRI) delivers superior soft-tissue contrast. Individually, each modality presents an incomplete picture; together, they provide complementary information essential for comprehensive diagnosis, treatment planning, and therapy monitoring [13].
The integration of these diverse data types through fusion and synthesis creates a more complete representation of pathology and physiology. This enables more accurate tumor localization, improved radiotherapy targeting, enhanced surgical planning, and better treatment response assessment. Within this technological landscape, wavelet transform-based techniques have proven particularly valuable due to their ability to efficiently separate and process an image's structural information (low-frequency components) from its fine details and textures (high-frequency components) [13] [8] [14]. This multi-resolution analysis capability makes wavelet methods ideally suited for handling the distinct, complementary information present in PET, CT, and MRI scans.
Wavelet Transform Fundamentals for Medical Imaging
Wavelet transforms provide a mathematical framework for decomposing images into multiple frequency sub-bands at different scales. Unlike traditional Fourier transforms that provide only frequency information, wavelets localize information in both frequency and space, making them exceptionally suitable for analyzing non-stationary signals like medical images [31].
The Discrete Wavelet Transform (DWT) decomposes an image into four primary components: approximation coefficients (LL) representing the low-frequency structural content, and detail coefficients capturing high-frequency information in horizontal (HL), vertical (LH), and diagonal (HH) directions [13]. This decomposition enables targeted processing of different image characteristics. For instance, in the WTA-Net framework, applying Spatial-Channel attention to these wavelet components resulted in significant quantitative improvements: information entropy (IE), average gradient (AG), and standard deviation (SD) increased by 34.76%, 30.5%, and 11.07% respectively for PET images, and 12.7%, 21.13%, and 4.54% for CT images [13].
Advanced variants like the Dual-Tree Complex Wavelet Transform (DTCWT) offer enhanced directional selectivity and approximate shift-invariance, providing more robust feature representation. When optimized using nature-inspired algorithms, this transform demonstrates superior performance in preserving anatomical boundaries and metabolic information during fusion tasks [31].
Application Notes: Technical Approaches and Performance
Wavelet-Based Architectures for Image Fusion and Synthesis
Recent advances in wavelet-based deep learning architectures have demonstrated remarkable capabilities in multi-modal medical image processing. The following table summarizes key technical approaches and their documented performance:
Table 1: Performance Metrics of Wavelet-Based Multi-modal Image Fusion Techniques
| Technique / Network | Modalities | Key Innovation | Reported Improvement Over Baseline | Primary Application |
|---|---|---|---|---|
| WTA-Net [13] | PET/CT, PET/MRI | Wavelet Attention + Cross-Modal Information Fusion Module | IE: 18.92%, AG: 14%, EN: 18.25% (Brain MRI-PET) [13] | Medical Image Fusion |
| DWFI-GAN [14] | Multi-contrast MRI | Dual-branch Wavelet Encoding + Deformable Feature Fusion | SSIM: ~3-5% improvement over non-wavelet baselines [14] | Medical Image Synthesis |
| ODTCWT with PF-HBSSO [31] | CT/MRI | Optimized DTCWT + Adaptive Weighted Average Fusion | Superior mutual information preservation [31] | Multimodal Image Fusion |
| WGSF-Net [32] | Various 2D modalities | Wavelet-Guided Spatial-Frequency Fusion | Dice: +1.5-13.9% in unseen domains [32] | Cross-Domain Segmentation |
The WTA-Net (Wavelet Transform with Spatial-Channel Attention Network) employs a dual-encoder, single-decoder architecture specifically designed to capture frequency domain features and enhance information flow between modalities. Its innovative Cross Modal Information Fusion Module (CMIFM) utilizes spatial attention to enhance local information within single modalities while employing Transformer mechanisms to enable global feature interaction between modalities [13].
For image synthesis tasks, the DWFI-GAN (Dual-branch Wavelet Encoding and Deformable Feature Interaction GAN) introduces a wavelet multi-scale downsampling (Wavelet-MS-Down) module that performs near-lossless feature dimensionality reduction through wavelet decomposition. The resulting low-frequency and high-frequency subbands are processed separately to preserve both global structural contours and fine-grained details, effectively mitigating the global information loss common in conventional CNN-based downsampling [14].
Quantitative Assessment Metrics
Rigorous evaluation of fusion and synthesis outcomes employs multiple quantitative metrics, as summarized below:
Table 2: Key Quantitative Metrics for Evaluating Fusion/Synthesis Quality
| Metric | Description | Interpretation | Ideal Value |
|---|---|---|---|
| Information Entropy (IE) [13] | Measures the amount of information contained in the fused image | Higher values indicate richer information content | Maximize |
| Structural Similarity Index (SSIM) [8] | Assesses perceptual similarity to reference images | Values closer to 1 indicate better structural preservation | 1.0 |
| Peak Signal-to-Noise Ratio (PSNR) [8] | Measures reconstruction quality in synthesized images | Higher values indicate better quality | Maximize |
| Average Gradient (AG) [13] | Evaluates image clarity and texture preservation | Higher values indicate sharper results | Maximize |
| Standard Deviation (SD) [13] | Reflects contrast and distribution of pixel intensities | Higher values suggest better contrast | Maximize |
| Spatial Frequency (SF) [13] | Measures overall activity level and clarity | Higher values indicate better quality | Maximize |
Experimental Protocols
Protocol 1: PET-CT Fusion via WTA-Net
Objective: To generate a fused PET-CT image that preserves both metabolic information (from PET) and anatomical structure (from CT) for improved tumor localization.
Materials:
- Pre-registered PET and CT image pairs
- WTA-Net implementation (PyTorch/TensorFlow)
- Computing resources: GPU with ≥8GB VRAM
- Evaluation software: Python with OpenCV, SciKit-Image
Procedure:
- Image Preprocessing:
- Normalize both PET and CT images to [0, 1] range
- Verify spatial registration using landmark-based or intensity-based methods
- Resize images to network input dimensions (typically 256×256 or 512×512)
Wavelet Decomposition:
- Apply Discrete Wavelet Transform (DWT) to both PET and CT inputs
- Use 'db4' (Daubechies 4) or 'sym4' (Symlet 4) wavelet basis functions
- Decompose into 4 sub-bands: LL (approximation), LH (horizontal detail), HL (vertical detail), HH (diagonal detail)
Wavelet Attention Processing:
- Process each sub-band through Spatial-Channel Attention modules
- Apply soft attention mechanisms to emphasize diagnostically relevant features
- For PET: Enhance metabolic activity regions in high-frequency components
- For CT: Preserve bone structures and anatomical boundaries
Cross-Modal Fusion:
- Feed attention-enhanced features to Cross Modal Information Fusion Module (CMIFM)
- Employ transformer-based mechanisms for global feature interaction
- Use spatial attention for local feature enhancement
Image Reconstruction:
- Reconstruct fused wavelet coefficients using Inverse DWT (IDWT)
- Apply post-processing for intensity consistency
- Output final fused image
Validation:
- Calculate IE, AG, EN, SD, and SF metrics
- Compare with ground truth where available
- Conduct qualitative assessment by clinical experts
Protocol 2: Multi-contrast MRI Synthesis via DWFI-GAN
Objective: To synthesize missing MRI sequences (e.g., T2 from T1, FLAIR from T1ce) using available modalities to complete multi-protocol datasets.
Materials:
- Paired multi-contrast MRI datasets (BraTS2020, IXI)
- DWFI-GAN implementation
- High-performance computing cluster
- Validation framework with segmentation metrics
Procedure:
- Data Preparation:
- Select source and target modality pairs (e.g., T1→T2, T1ce→FLAIR)
- Apply skull-stripping and bias field correction
- Normalize intensities per sequence using z-score normalization
Dual-Branch Wavelet Encoding:
- Process each input modality through separate wavelet encoders
- Employ Wavelet-MS-Down modules for multi-scale decomposition
- Extract low-frequency components (global anatomy) and high-frequency components (local details)
Deformable Feature Interaction:
- Apply Deformable Cross-Attention Feature Fusion (DCFF) modules at each encoding stage
- Align spatial features using deformable convolution
- Fuse cross-modal features through attention mechanisms
Frequency-Space Enhancement:
- Process bottleneck features through Frequency-Space Enhanced (FSE) modules
- Integrate Fast Fourier Transform (FFT) with State Space Models (SSM)
- Enhance multi-scale representation through joint frequency-spatial modeling
Image Generation and Discrimination:
- Decode fused features to generate target modality
- Employ multi-scale discriminators for adversarial training
- Use combination of adversarial, perceptual, and cycle-consistency losses
Validation:
- Calculate PSNR, SSIM, and MSE against ground truth
- Perform segmentation-based evaluation using synthetic images
- Conduct radiologist reader studies for clinical assessment
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Components for Wavelet-Based Medical Image Fusion
| Component / Resource | Type | Function / Application | Exemplars / Alternatives |
|---|---|---|---|
| Wavelet Transforms | Mathematical Tool | Multi-scale decomposition for feature separation | Discrete Wavelet Transform (DWT), Dual-Tree CWT [31], Stationary Wavelet Transform (SWT) |
| Attention Mechanisms | Algorithmic Component | Feature emphasis and selection | Spatial-Channel Attention [13], Wavelet Attention (WA) [13], Deformable Attention [14] |
| Fusion Modules | Architectural Component | Cross-modal information integration | Cross Modal Information Fusion Module (CMIFM) [13], Deformable Cross-Attention Feature Fusion (DCFF) [14] |
| Generative Models | Framework | Image synthesis and data generation | Generative Adversarial Networks (GANs) [14] [33], Conditional GANs (cGANs), Variational Autoencoders (VAEs) [8] |
| Optimization Algorithms | Computational Tool | Parameter tuning and performance enhancement | Hybridized heuristic algorithms [31], Probability of Fitness-based Honey Badger Squirrel Search Optimization (PF-HBSSO) [31] |
| Evaluation Metrics | Analytical Tool | Quantitative performance assessment | Information Entropy, SSIM, PSNR [13] [8], Task-specific metrics (e.g., Dice for segmentation) |
| Medical Imaging Datasets | Data Resource | Model training and validation | BraTS2020 [14], IXI [14], LIDC-IDRI [8], institution-specific collections |
Implementation Considerations and Best Practices
Successful implementation of wavelet-based multi-modal fusion and synthesis requires careful attention to several practical aspects. Computational resources must be adequate, with GPU acceleration being essential for training deep wavelet networks. Memory requirements can be substantial, particularly for 3D volumes or high-resolution data. Data preprocessing is critical, including rigorous intensity normalization, accurate spatial registration between modalities, and consistent resolution matching. Wavelet selection should be guided by the specific application—Daubechies wavelets ('db4', 'db8') offer good regularity for medical images, while Symlets ('sym4') provide higher symmetry for reduced phase distortion [31].
For clinical translation, validation must extend beyond quantitative metrics to include task-specific evaluations. For diagnostic applications, reader studies with clinical experts are essential. For downstream tasks like segmentation or radiation planning, performance should be measured on the ultimate clinical task. Regulatory considerations are increasingly important, particularly when using synthetic data for algorithm development or validation. The European Health Data Space (EHDS) framework provides guidance on synthetic data governance, emphasizing utility, transparency, and accountability [33].
Future directions in this field include the development of more efficient wavelet architectures, improved cross-modal alignment techniques, and enhanced evaluation methodologies that better correlate with clinical utility. As these technologies mature, wavelet-based multi-modal image fusion and synthesis are poised to become indispensable tools in precision medicine and personalized healthcare.
The exponential growth of medical imaging data presents a critical challenge for modern healthcare systems, balancing the competing demands of storage efficiency and diagnostic integrity [34]. Technologies such as Magnetic Resonance Imaging (MRI), Computed Tomography (CT), and positron emission tomography (PET) generate high-resolution images essential for accurate diagnosis but create substantial burdens for storage infrastructure and transmission bandwidth, particularly in telemedicine applications [8]. This challenge is especially pronounced in resource-limited settings where network capacity may be constrained [35].
Unlike natural image compression, medical image compression operates under fundamentally different constraints, prioritizing the preservation of subtle diagnostic details that are crucial for clinical decision-making over maximal compression ratios [36]. Even minor quality degradation can potentially impact diagnostic accuracy, necessitating specialized approaches that maintain structural integrity while achieving meaningful data reduction [37].
Wavelet transform-based techniques have emerged as a powerful solution to this challenge, offering multi-resolution analysis capabilities that align well with the structural characteristics of medical images [8]. By decomposing images into frequency sub-bands while preserving spatial information, wavelet transforms enable more efficient representation of structural and textural information, facilitating compression that maintains diagnostic relevance [38]. This foundation has enabled advanced hybrid approaches that combine the theoretical strengths of wavelet analysis with adaptive deep learning architectures [8].
Technical Foundation: Wavelet-Based Compression
Core Principles of Wavelet Transform in Medical Imaging
The Discrete Wavelet Transform (DWT) serves as a mathematical cornerstone for advanced medical image compression by performing multi-resolution analysis that decomposes images into hierarchical frequency components [8]. This decomposition generates approximation coefficients (representing low-frequency image content) and detail coefficients (capturing high-frequency information like edges and textures) across multiple scales [38]. For medical images, this frequency separation proves particularly valuable as diagnostically significant features often correspond to specific frequency components that can be prioritized during compression.
The fundamental advantage of wavelet transforms over traditional Fourier-based methods lies in their ability to localize both frequency and spatial information simultaneously [39]. This dual localization enables precise preservation of anatomical boundaries and pathological features that are essential for diagnostic interpretation. Furthermore, wavelet transforms demonstrate exceptional compatibility with the human visual system characteristics, making them ideal for medical imaging applications where perceptual quality correlates strongly with diagnostic utility [35].
Advanced Hybrid Architectures
Recent research has focused on integrating wavelet transforms with deep learning architectures to create hybrid systems that leverage both mathematical foundations and adaptive learning capabilities [8]. These approaches typically employ DWT for initial image decomposition, followed by neural networks that process the resulting sub-bands with attention to their diagnostic significance.
A notable implementation combines DWT with a Cross-Attention Learning (CAL) module that dynamically weights feature importance based on clinical relevance [8]. This architecture allows the compression system to prioritize regions containing potential lesions or tissue abnormalities while applying more aggressive compression to diagnostically neutral areas. The attention mechanism essentially learns to identify and preserve the feature characteristics that radiologists and other clinical specialists depend on for accurate interpretation.
Table 1: Performance Comparison of Wavelet-Based Compression Techniques
| Compression Method | PSNR (dB) | SSIM | Compression Ratio | Modality |
|---|---|---|---|---|
| DWT + CAL + VAE [8] | 24.23 | 0.98 | 25:1 | CT, MRI |
| Region-Based DWT [35] | 24.23 | 0.96 | 30:1 | MRI |
| EE-CLAHE + SPIHT [37] | 22.15 | 0.94 | 28:1 | MRI, CT, X-ray |
| Traditional JPEG2000 [8] | 20.50 | 0.91 | 20:1 | Various |
| Standard JPEG [35] | 16.01 | 0.87 | 15:1 | Various |
Application Notes: Implementation Frameworks
Region of Interest (ROI) Based Compression
ROI-based compression represents a sophisticated strategy for balancing compression efficiency with diagnostic integrity by applying different compression techniques to diagnostically critical regions versus background areas [37]. Implementation typically begins with segmentation using adaptive expectation maximization clustering (AEMC) enhanced with fuzzy c-means (FCM) and Otsu thresholding to accurately delineate ROI boundaries [37].
Following segmentation, optimized compression pipelines are applied separately to ROI and non-ROI regions. For ROI areas, lossless or near-lossless techniques such as modified SPIHT with Huffman coding preserve all diagnostic information [37]. For non-ROI regions, more aggressive lossy compression like Embedded Zerotree Wavelet (EZW) or fractal compression significantly reduces data volume while maintaining overall image context [35]. This selective approach achieves superior compression ratios without compromising the diagnostic value of critical image regions.
Cross-Attention Learning with Wavelet Decomposition
The integration of cross-attention mechanisms with wavelet decomposition represents a significant advancement in adaptive compression [8]. This approach employs a dual-branch architecture where wavelet transforms handle frequency decomposition while attention mechanisms identify spatially significant regions worthy of preservation.
The implementation utilizes a Wavelet Multi-Scale Downsampling (Wavelet-MS-Down) module that decomposes input images into low-frequency contours and high-frequency details [14]. A deformable cross-attention feature fusion (DCFF) module then processes these components, applying spatial alignment and deep interaction across modalities to maximize complementary information utilization [14]. This architecture demonstrates particular effectiveness for multi-modal imaging scenarios where different sequences (T1, T2, FLAIR) provide complementary clinical information.
Enhanced Pre-processing for Compression Optimization
Image enhancement prior to compression can significantly improve both compression efficiency and reconstructed image quality. The Edge Enhancement Contrast Limited Adaptive Histogram Equalization (EE-CLAHE) technique has demonstrated particular effectiveness for medical images by enhancing local contrast while preserving edge information in ROIs [37]. This pre-processing is typically followed by denoising using a 2D adaptive anisotropic diffusion filter that reduces noise without blurring critical anatomical boundaries.
The combination of enhancement and denoising pre-processing serves dual purposes: it improves the diagnostic clarity of reconstructed images while creating a more compressible data representation through noise reduction and contrast optimization. This approach proves especially valuable for modalities with inherent noise characteristics like ultrasound and low-dose CT imaging.
Experimental Protocols
Protocol 1: Hybrid DWT-CAL-VAE Compression
This protocol implements a comprehensive compression pipeline combining wavelet transformation, cross-attention learning, and variational autoencoders [8].
Materials and Dataset Preparation
- Datasets: LIDC-IDRI (lung CT), LUNA16 (lung nodules), MosMed (chest CT) [8]
- Pre-processing: Resize images to 512×512 pixels, normalize pixel values to [0,1]
- Data splitting: 70% training, 15% validation, 15% testing
- Platform: Python 3.8+, PyTorch 1.10+, GPU with 8GB+ VRAM
Wavelet Decomposition
- Apply 2D Discrete Wavelet Transform using Daubechies (db4) wavelet
- Decompose into four sub-bands: LL (approximation), LH (horizontal detail), HL (vertical detail), HH (diagonal detail)
- Perform 3-level decomposition for multi-resolution analysis
- Normalize sub-band coefficients to zero mean and unit variance
Cross-Attention Learning Module
- Implement multi-head cross-attention with 8 attention heads
- Set embedding dimension to 512
- Apply dynamic feature weighting based on spatial importance
- Use learnable parameters to balance frequency component preservation
Variational Autoencoder Compression
- Design encoder with 4 convolutional layers (filter sizes: 64, 128, 256, 512)
- Implement bottleneck with mean and variance branches for probabilistic latent space
- Build symmetric decoder with transposed convolutions
- Apply entropy coding to latent representations
Training Procedure
- Loss function: Combined rate-distortion optimization: L = λ·D + R, where D is mean squared error and R is bitrate
- Optimizer: Adam with learning rate 0.001, β₁=0.9, β₂=0.999
- Batch size: 16, training epochs: 100
- Validation: Evaluate PSNR, SSIM, and MS-SSIM every epoch
Protocol 2: ROI-Based Medical Image Compression
This protocol implements a region-based compression approach that applies different techniques to diagnostically critical versus background regions [37].
Image Enhancement and Segmentation
- Apply EE-CLAHE with clip limit 2.0 and tile grid size 8×8
- Denoise using 2D adaptive anisotropic diffusion with 10 iterations
- Segment ROI using Adaptive Expectation Maximization Clustering (AEMC)
- Refine boundaries with Fuzzy C-Means clustering and Otsu thresholding
Region-Specific Compression
- ROI compression: Apply modified SPIHT with Huffman coding
- Non-ROI compression: Implement EZW with higher compression ratios
- Bitrate allocation: Allocate 70-80% of total bitrate to ROI regions
- Quality control: Ensure minimum PSNR of 35 dB in ROI regions
Evaluation Metrics
- Calculate PSNR separately for ROI and non-ROI regions
- Measure structural similarity index (SSIM) for overall image
- Compute compression ratio as CR = Original size / Compressed size
- Assess diagnostic fidelity using radiologist scoring (if available)
Table 2: Research Reagent Solutions for Medical Image Compression
| Reagent/Resource | Function | Implementation Example |
|---|---|---|
| Discrete Wavelet Transform (DWT) | Multi-resolution image decomposition | PyWavelets, Daubechies wavelets |
| Cross-Attention Learning (CAL) Module | Adaptive feature weighting | PyTorch nn.MultiheadAttention |
| Variational Autoencoder (VAE) | Latent space representation | Custom PyTorch modules with reparameterization |
| Modified SPIHT Algorithm | ROI lossless compression | Custom implementation with Huffman coding |
| Edge Enhancement CLAHE | Pre-processing for contrast improvement | OpenCV createCLAHE |
| Adaptive EMC Segmentation | ROI detection | Scikit-learn Gaussian Mixture Models |
Results and Analysis
Quantitative Performance Metrics
Comprehensive evaluation of advanced compression techniques demonstrates significant improvements over traditional approaches. The hybrid DWT-CAL-VAE framework achieves PSNR values up to 24.23 dB, representing substantial improvement over JPEG2000 (20.50 dB) and standard JPEG (16.01 dB) [8] [35]. Similarly, structural similarity metrics show SSIM values of 0.98 for advanced methods compared to 0.91 for JPEG2000, indicating superior preservation of diagnostically relevant structural information [8].
Compression ratios also show notable improvements, with region-based approaches achieving 30:1 ratios while maintaining diagnostic integrity in ROI regions [35]. This balance between compression efficiency and quality preservation represents a significant advancement for medical imaging applications, particularly in telemedicine and archival contexts where both storage constraints and diagnostic accuracy are critical considerations.
Clinical Validation and Application
Beyond quantitative metrics, the clinical utility of compression techniques must be validated through diagnostic accuracy studies. While full clinical trials are beyond most technical research scopes, intermediate validation using task-based assessment provides important insights. Techniques that incorporate attention mechanisms to preserve diagnostically significant regions demonstrate particular promise for maintaining diagnostic accuracy even at higher compression ratios [8].
The application of these advanced compression techniques extends across multiple medical imaging modalities, including CT, MRI, ultrasound, and X-ray [37]. Volume compression approaches further address the challenges of 3D and 4D medical imaging, which present additional complexities through inter-slice correlations and temporal components [36].
Advanced compression techniques based on wavelet transforms successfully address the critical challenge of balancing compression efficiency with diagnostic integrity in medical imaging. Through sophisticated approaches like hybrid DWT-CAL architectures and region-based compression with optimized bitrate allocation, these methods achieve substantially improved rate-distortion performance compared to traditional techniques.
The integration of adaptive attention mechanisms with wavelet multi-resolution analysis represents a particularly promising direction, enabling intelligent preservation of clinically relevant features while aggressively compressing less critical image regions. As medical imaging continues to evolve with increasing resolution and dimensionality, these advanced compression strategies will play an essential role in enabling efficient storage, transmission, and utilization of medical images across healthcare systems, from resource-rich academic centers to remote telehealth applications.
Future developments will likely focus on modality-specific optimization, real-time compression capabilities for interventional applications, and enhanced integration with downstream analysis tasks including computer-aided diagnosis and quantitative imaging biomarkers. Through continued refinement, wavelet-based compression techniques will remain fundamental infrastructure supporting the increasingly digital healthcare ecosystem.
Accurate delineation of tumor boundaries via medical image segmentation and registration is a cornerstone of modern oncology, influencing diagnosis, treatment planning, and therapeutic monitoring [40] [41]. These processes are technically challenging due to inherent complexities in medical images, including noise, heterogeneous tumor textures, and ambiguous boundaries [41]. Traditional methods often fall short in managing these variabilities, leading to compromised accuracy [42].
The integration of Artificial Intelligence (AI), particularly deep learning, has revolutionized this field by enabling automated, high-precision analysis [40] [43]. Concurrently, wavelet-transform-based techniques have emerged as a powerful tool for enhancing AI models. Wavelets facilitate superior multi-resolution analysis by decomposing images into different frequency sub-bands, thereby preserving critical high-frequency details like edges and textures that are essential for defining tumor margins [7] [10] [8]. This document details application notes and experimental protocols that leverage wavelet-based AI techniques to achieve superior tumor delineation, framed within a broader research context focused on wavelet transforms for medical imaging.
Application Notes: Current State & Wavelet Integration
Key Challenges in Tumor Delineation
- Image Registration Complexities: Non-rigid registration for soft tissues requires nonlinear spatial adaptation. Traditional methods are computationally intensive and struggle with real-time clinical demands. Transformer-based networks like TransMorph offer accuracy but are parameter-heavy and require large datasets, conflicting with typical clinical constraints [10].
- Segmentation Limitations: Tumors often exhibit irregular shapes, diffuse borders, and heterogeneous intensity profiles. While U-Net and its variants are prominent, they can fail to capture sufficient multi-scale features and long-range dependencies, leading to inaccurate boundary delineation [8] [41].
- Data Constraints: AI models are often hampered by small, homogenous datasets, which can lead to overfitting and poor generalizability across diverse patient populations and imaging scanners [44] [43].
The Wavelet Transform Advantage
Wavelet transforms address these challenges by providing a lossless or near-lossless framework for multi-scale feature analysis.
- Multi-Resolution Analysis: Unlike Fourier transforms, wavelets localize information in both space and frequency, allowing models to analyze coarse structures and fine details simultaneously [7].
- Preservation of High-Frequency Information: Critical anatomical details such as tissue boundaries and small lesions are preserved in the high-frequency sub-bands during image decomposition, preventing the degradation seen in traditional downsampling methods like max-pooling [10] [8].
- Enhanced Feature Representation: Integrating wavelet decomposition into deep learning architectures allows the network to process and fuse features from multiple frequency domains, leading to more robust and discriminative feature learning for complex tumor morphology [10].
Table 1: Quantitative Performance of Advanced AI Models in Brain Tumor Analysis
| Model/Technique | Key Feature | Reported Accuracy | Dataset | Reference |
|---|---|---|---|---|
| ResNet-InceptionV2-HCNN with OPSIT | Optimal feature selection & hyper-CNN | High Accuracy, Sensitivity, Specificity, ROC | Brain Tumor MRI | [42] |
| CNN with multiple features (LBP, Gabor, DWT) | Integration of handcrafted features & deep learning | 98.9% Accuracy | Large Benchmark MRI Dataset | [43] |
| WaveMorph (Wavelet-Guided ConvNeXt) | Multi-scale wavelet feature fusion for registration | Dice: 0.824 ± 0.021 (Inter-patient) | IXI & OASIS MRI | [10] |
| DWT & Cross-Attention Learning | Hybrid compression preserving diagnostic features | High PSNR & SSIM | LIDC-IDRI, LUNA16 | [8] |
| RGNet with GDB Strategy | Large kernel convolution & attention | mAP50: 96.9% | Br35H Dataset | [42] |
Experimental Protocols
Protocol 1: Wavelet-Guided Image Registration (Based on WaveMorph)
This protocol outlines the procedure for unsupervised non-rigid medical image registration using a wavelet-enhanced deep learning model, ideal for aligning patient scans to an atlas or serial monitoring scans.
I. Objective: To achieve high-accuracy, real-time deformable registration of brain MRIs for improved tumor localization and longitudinal tracking.
II. Research Reagent Solutions
Table 2: Essential Research Reagents & Computational Tools
| Item/Tool | Function/Description | Example |
|---|---|---|
| Haar Wavelet Transform | A simple, lossless wavelet transform used to decompose the input image into 8 frequency sub-bands (LL, LH, HL, HH x 2) for multi-scale analysis. | pywt.wavedec2 (PyWavelets) |
| ConvNeXt Architecture | A modernized CNN backbone that incorporates design elements from Vision Transformers, offering high efficiency and powerful feature representation. | TorchVision or custom implementation |
| Multi-Scale Wavelet Feature Fusion (MSWF) Module | A custom module that uses multi-scale convolution kernels to extract and fuse features from the wavelet-decomposed sub-bands. | Custom PyTorch/TensorFlow module |
| Lightweight Dynamic Upsampling Module | A decoder component that adaptively reconstructs fine-grained anatomical structures during upsampling, reducing blurring. | Custom PyTorch/TensorFlow module |
| Spatial Transformation Layer | Applies the predicted deformation field to the moving image to warp it into alignment with the fixed image. | torch.nn.functional.grid_sample |
III. Methodology:
Data Preprocessing:
- Input: 3D MRI volumes (e.g., T1-weighted, T2-FLAIR).
- Steps: N4 bias field correction, skull-stripping, and min-max intensity normalization to [0, 1].
- Splitting: Divide data into training/validation/test sets (e.g., 70/15/15).
Model Architecture & Workflow: The following diagram illustrates the WaveMorph architecture and its registration workflow.
Diagram 1: WaveMorph registration workflow.
Training Configuration:
- Loss Function: Combine Local Normalized Cross-Correlation (LNCC) as the similarity metric
L_simwith a diffusion regularizerL_regon the deformation fieldφto enforce smoothness.L_total = -LNCC(f, m ∘ φ) + λ * ||∇φ||²[10] - Optimizer: AdamW (learning rate: 1e-4, weight decay: 1e-5).
- Hardware: Training requires a high-RAM GPU (e.g., NVIDIA A100 or RTX 4090).
- Loss Function: Combine Local Normalized Cross-Correlation (LNCC) as the similarity metric
Validation & Metrics:
- Primary Metric: Dice Similarity Coefficient (DSC) on segmented tumor regions before and after registration. Target: DSC > 0.80 [10].
- Secondary Metrics: Jacobian determinant (to ensure non-folding, smooth fields), and inference time (target: <0.1s per image pair).
Protocol 2: Wavelet-Enhanced Multi-Scale Tumor Segmentation
This protocol describes a segmentation network that integrates wavelet transforms and attention mechanisms to accurately segment brain tumors from MRI.
I. Objective: To precisely segment brain tumor sub-regions (e.g., enhancing tumor, peritumoral edema) by leveraging multi-scale features from wavelet decomposition.
II. Research Reagent Solutions
Table 3: Key Tools for Segmentation Protocol
| Item/Tool | Function/Description |
|---|---|
| Discrete Wavelet Transform (DWT) | Decomposes the input image into approximation (LL) and detail (LH, HL, HH) coefficients. |
| Wavelet Transform Convolution (WTConv) | Replaces standard convolutions in the initial layer to directly extract multi-scale features from wavelet sub-bands [8]. |
| Multi-Scale Channel Attention Module (MSCAM) | Weights the importance of different feature channels across scales, improving feature selectivity [8]. |
| U-Net-like Encoder-Decoder | Serves as the foundational segmentation architecture. |
III. Methodology:
Data Preprocessing:
- Utilize public datasets like the Brain Tumor Segmentation (BraTS) challenge dataset.
- Apply standard preprocessing: co-registration to a common template, interpolation to uniform resolution (e.g., 1mm³), and intensity normalization.
Model Architecture & Workflow: The following diagram outlines the key modifications to a standard U-Net for wavelet-enhanced segmentation.
Diagram 2: Wavelet-enhanced segmentation network.
Training Configuration:
- Loss Function: Combined Dice and Cross-Entropy Loss to handle class imbalance.
L_seg = 1 - DSC(p, y) + CE(p, y) - Optimizer: Adam (learning rate: 1e-4).
- Data Augmentation: Apply random rotations, flipping, and intensity shifts.
- Loss Function: Combined Dice and Cross-Entropy Loss to handle class imbalance.
Validation & Metrics:
- Metrics: Report Dice score, Hausdorff Distance, and Sensitivity for each tumor sub-region.
- Benchmarking: Compare performance against a baseline U-Net without wavelet components.
Discussion & Limitations
The integration of wavelet transforms with AI models presents a significant advancement for tumor delineation. The multi-scale, frequency-aware processing inherent to wavelets directly addresses key limitations of standard CNNs and Transformers, particularly the loss of high-frequency spatial information during down/up-sampling [10] [8]. This leads to tangible improvements in registration accuracy (Dice scores) and segmentation precision, especially at tumor boundaries.
However, several limitations and future directions must be considered:
- Computational Overhead: While wavelet decomposition is computationally efficient, fusing multiple sub-bands can increase model complexity and memory requirements [8].
- Interpretability and Clinical Translation: Despite performance gains, many deep learning models remain "black boxes." Techniques like SHAP (SHapley Additive exPlanations) analysis are required to identify the most important features for classification and build clinician trust [43]. Furthermore, rigorous external validation on diverse, multi-institutional datasets is crucial to ensure generalizability and mitigate algorithmic bias before clinical deployment [44] [45].
- Regulatory Hurdles: The path to clinical adoption is governed by evolving regulatory frameworks (e.g., EU AI Act, FDA guidance for AI/ML devices). A key requirement is demonstrating robust performance and explainability across diverse populations, which necessitates extensive testing and validation [45] [46].
Wavelet-transform-based techniques represent a powerful paradigm for enhancing AI-driven medical image segmentation and registration. The protocols outlined herein provide a roadmap for researchers to implement these advanced methods, leveraging the multi-resolution analysis capabilities of wavelets to achieve superior tumor delineation. By faithfully preserving critical high-frequency anatomical information, these approaches directly combat the problem of information degradation common in traditional networks. Future work should focus on developing more efficient wavelet-AI architectures, improving model interpretability, and conducting large-scale clinical validation to translate these promising technical advancements into improved patient outcomes in oncology.
Radiomics is a high-throughput quantitative approach that extracts sub-visual information from standard medical images, decoding tissue pathology and creating high-dimensional datasets for analysis and model development [47] [48]. The core premise of radiomics is that medical images contain data far beyond what is visually perceptible, often described as "hidden" information that can be revealed through advanced mathematical analysis [47]. This extracted information provides insights into intra-tumoral heterogeneity and tissue characteristics that may correlate with clinical outcomes, treatment response, and underlying genetic expressions [49].
The integration of wavelet transform techniques has significantly expanded the analytical power of radiomics by enabling multi-scale feature extraction. Wavelet transforms decompose images into different frequency components, allowing simultaneous analysis of both local and global texture patterns [25] [50]. Unlike traditional Fourier transforms that provide only frequency information, wavelets capture both frequency and spatial information, making them particularly suited for analyzing non-stationary signals like medical images where texture patterns vary across regions [51]. This multi-resolution analysis capability allows researchers to examine texture features at varying scales, from fine-grained details to coarse structures, providing a more comprehensive characterization of tissue heterogeneity [25] [50].
Core Radiomic Feature Classes and Their Mathematical Foundations
Radiomic features are typically categorized into several distinct classes based on their mathematical properties and the aspects of image texture they quantify. The most fundamental categories include first-order, second-order, and higher-order statistics, along with morphological features that describe shape characteristics [47] [49].
First-order statistics describe the distribution of voxel intensities within an image region without considering spatial relationships. These features are derived from the histogram of intensity values and include metrics such as entropy, uniformity, skewness, and kurtosis [47] [49]. Entropy, a crucial first-order feature, quantifies the randomness in gray-level intensities and is calculated as:
where H is the first-order histogram with B bins [47]. Higher entropy values typically indicate greater tissue heterogeneity and have been shown to be higher in malignant compared to benign tissues across various cancer types [47].
Second-order statistics quantify the spatial relationships between pixels by analyzing how often pairs of pixels with specific values and spatial relationships occur. The most common method for extracting these features is the Gray-Level Co-occurrence Matrix (GLCM), which represents the joint probability density of the number of times intensity level i and intensity level j occur in a specific direction θ and at a specified distance d [49]. From GLCM, features such as contrast, correlation, homogeneity, and energy are derived [49].
Higher-order statistics include methods like Gray-Level Run-Length Matrix (GLRLM), Gray-Level Size Zone Matrix (GLSZM), and Neighboring Gray-Tone Difference Matrix (NGTDM) that capture more complex texture patterns by analyzing the relationships among multiple pixels simultaneously [49]. These features can quantify textural properties like coarseness, busyness, and complexity that may reflect underlying tissue microstructure [49].
Table 1: Core Classes of Radiomic Features and Their Clinical Applications
| Feature Class | Key Features | Mathematical Basis | Biological Correlation |
|---|---|---|---|
| First-Order Statistics | Entropy, Uniformity, Skewness, Kurtosis | Intensity histogram analysis | Tissue heterogeneity, cellularity |
| Second-Order Statistics | Contrast, Correlation, Homogeneity, Energy | Gray-Level Co-occurrence Matrix (GLCM) | Microarchitectural patterns, structural organization |
| Higher-Order Statistics | Coarseness, Busyness, Complexity, Run-Length Non-Uniformity | NGTDM, GLRLM, GLSZM | Tissue complexity, lesion aggressiveness |
| Morphological Features | Volume, Sphericity, Surface Area to Volume Ratio | Shape descriptors | Tumor growth patterns, invasiveness |
Wavelet Transforms in Multi-Scale Radiomic Analysis
Wavelet transforms enhance radiomic analysis by decomposing images into multiple frequency bands, enabling the extraction of texture features at different spatial scales [25] [50]. This multi-resolution analysis is particularly valuable for capturing heterogeneous tissue patterns that manifest differently across scales. The wavelet decomposition process typically generates eight sub-bands for 2D images (LLL, LLH, LHL, LHH, HLL, HLH, HHL, HHH) and eight decomposition modes for 3D images, where L represents low-pass filtering and H represents high-pass filtering [50].
The application of wavelet-transform radiomics has demonstrated significant performance improvements across various medical domains. In a multicenter study assessing COVID-19 pulmonary lesions, wavelet-based radiomic models achieved an AUC of 0.910, outperforming original radiomic models (AUC=0.880) with statistical significance [50]. Similarly, in hepatocellular carcinoma screening, combining radiomic features extracted from both wavelet and original CT domains significantly enhanced classification performance compared to using either domain alone [25].
The selection of appropriate wavelet functions is crucial for optimal performance. Studies have evaluated various wavelet types, with findings indicating that biorthogonal wavelets (particularly bior1.1 and bior6.8) often yield superior results for specific applications [50]. For instance, in COVID-19 lesion grading, the bior1.1 LLL (low-low-low) mode was identified as the optimal wavelet transform, while in MRI denoising applications, bior6.8 with universal thresholding at decomposition levels 2-3 demonstrated optimal performance [52] [50].
Table 2: Performance Comparison of Wavelet Types in Radiomic Applications
| Application Domain | Optimal Wavelet | Performance Metrics | Comparison Baseline |
|---|---|---|---|
| COVID-19 Lesion Grading (CT) | bior1.1 LLL | AUC: 0.910 | Original features (AUC: 0.880) |
| MRI Denoising | bior6.8 | PSNR: 38.2 dB, SSIM: 0.94 | Gaussian filtering (PSNR: 34.1 dB) |
| Liver Lesion Classification | Combined wavelet-original features | Accuracy: 89.3% | Wavelet-only (Accuracy: 83.7%) |
| Myocardial Infarction Detection | Wavelet-guided diffusion | Dice: 0.887, IoU: 0.803 | Standard U-Net (Dice: 0.812) |
Comprehensive Experimental Protocols
Protocol 1: Wavelet-Based Radiomic Feature Extraction from CT Images
This protocol details the methodology for extracting multi-scale radiomic features from CT images using wavelet transformation, adapted from validated approaches in hepatocellular carcinoma and COVID-19 lesion assessment [25] [50].
Materials and Equipment:
- High-resolution CT images (DICOM format)
- Python 3.8+ with PyRadiomics 3.0.1, SimpleITK, and PyWavelets packages
- Workstation with minimum 16GB RAM, 4-core processor
- ITK-SNAP or 3D Slicer for segmentation
Step-by-Step Procedure:
Image Acquisition and Quality Control:
- Acquire CT images following standardized protocols with consistent parameters
- Document key acquisition parameters: slice thickness, pixel spacing, kVp, mA, reconstruction kernel
- Perform visual quality assessment to exclude images with significant artifacts
Region of Interest (ROI) Segmentation:
- Manually delineate ROI/VOI using ITK-SNAP or semi-automatic tools in 3D Slicer
- For tumor segmentation, include entire lesion while excluding adjacent normal tissue
- Save segmentation masks in NRRD or NIFTI format for compatibility with PyRadiomics
Image Preprocessing and Discretization:
- Resample to isotropic voxel spacing (e.g., 1×1×1 mm³) using B-spline interpolation
- Apply fixed-bin width (25 HU) or fixed-bin number (32-128 bins) discretization
- For CT images, apply intensity thresholding (-1000 to 1000 HU) to exclude non-tissue voxels
Wavelet Transformation:
- Implement 3D stationary wavelet transform using PyWavelets
- Apply bior1.1, bior6.8, or other optimal wavelet functions
- Generate eight decomposition sub-bands (LLL, LLH, LHL, LHH, HLL, HLH, HHL, HHH)
Multi-Scale Feature Extraction:
- Execute PyRadiomics feature extraction on original and all wavelet sub-bands
- Extract first-order, GLCM, GLRLM, GLSZM, and GLDZM feature classes
- Configure PyRadiomics with standardized parameters (minimumROISize: 5, minimumWhiteValue: -1000)
Feature Consolidation and Validation:
- Compile features from all sub-bands into unified feature matrix
- Perform quality control to exclude features with zero variance or excessive missing values
- Apply intra-class correlation coefficient (ICC) analysis to assess feature stability
Protocol 2: Integration of Wavelet Radiomics with Deep Learning Segmentation
This protocol describes the integration of wavelet-based radiomic features with deep learning segmentation networks for enhanced tissue characterization, based on validated approaches in myocardial infarction detection [53].
Materials and Equipment:
- Paired medical images and segmentation masks
- Python with TensorFlow 2.8+ or PyTorch 1.12+
- Modified U-Net architecture with feature fusion capabilities
- High-performance GPU (NVIDIA RTX 3080+ recommended)
Step-by-Step Procedure:
Data Preparation and Augmentation:
- Resize all images to standardized dimensions (e.g., 128×128 or 256×256 pixels)
- Apply data augmentation: rotation (±10°), random flipping, CLAHE contrast enhancement
- Implement 5-fold cross-validation scheme with fixed random seed
Radiomic Feature Extraction:
- Extract GLCM and GLRLM features from original images
- Compute Joint Entropy, Max Probability, Sum Entropy, and Run-Length Non-Uniformity
- Normalize all features to [0,1] range using min-max scaling
Feature Selection Pipeline:
- Apply correlation filtering (remove features with |r| ≥ 0.85)
- Conduct statistical testing (t-tests with FDR correction, q<0.05)
- Implement MSVM-RFE for final feature ranking and selection
Hybrid U-Net Architecture Configuration:
- Implement standard U-Net encoder-decoder structure with skip connections
- Integrate radiomic features at both early (input) and intermediate (bottleneck) fusion points
- Configure training parameters: Adam optimizer, initial learning rate 1e-4, batch size 16
Model Training and Validation:
- Train for 200 epochs with early stopping (patience: 15 epochs)
- Monitor Dice coefficient and validation loss
- Implement gradient clipping to prevent explosion
Performance Evaluation:
- Calculate segmentation metrics: Dice, IoU, HD95
- Compute classification metrics: accuracy, AUC, precision, recall, F1-score
- Perform statistical significance testing (DeLong test for AUC comparisons)
Workflow Visualization
Table 3: Essential Research Tools for Wavelet-Based Radiomics
| Tool Category | Specific Tools/Software | Key Functionality | Implementation Considerations |
|---|---|---|---|
| Image Segmentation | ITK-SNAP, 3D Slicer, MITK | Manual/semi-automatic ROI delineation | Inter-observer variability assessment required for manual segmentation |
| Radiomics Platforms | PyRadiomics (Python), LifEx, MaZda | Standardized feature extraction | PyRadiomics follows IBSI standards, ensuring reproducibility |
| Wavelet Analysis | PyWavelets, MATLAB Wavelet Toolbox | Multi-scale decomposition | Selection of wavelet function (bior1.1, bior6.8, etc.) critical for performance |
| Deep Learning Frameworks | TensorFlow, PyTorch, MONAI | Hybrid model development | MONAI provides medical imaging-specific implementations |
| Statistical Analysis | R, Python (scikit-learn, SciPy) | Feature selection and model validation | LASSO, SVM-RFE effective for high-dimensional data |
| Data & Model Management | DVC (Data Version Control), MLflow | Experiment tracking and reproducibility | Essential for multicenter study validation |
Critical Implementation Considerations and Quality Assurance
Successful implementation of wavelet-based radiomic analysis requires careful attention to multiple technical factors that significantly impact feature stability and model performance. Image preprocessing parameters, particularly discretization methods, must be standardized across studies. For CT images, fixed-bin width discretization (e.g., 25 HU) is recommended, while for MRI, fixed-bin number approaches may be more appropriate [48]. Interpolation to isotropic voxel spacing is essential for most texture features to achieve rotational invariance, though the choice between upsampling and downsampling requires careful consideration based on the original image resolution and clinical question [48].
The segmentation methodology represents a critical potential source of variability. While manual segmentation introduces inter-observer variability, deep learning-based approaches can provide more consistent results when properly validated [48]. Studies utilizing manual or semi-automated segmentation should include assessments of intra- and inter-observer reproducibility, excluding non-robust features (ICC < 0.8) from subsequent analyses [48]. For wavelet parameter selection, systematic evaluation of different wavelet functions and decomposition levels is recommended, as optimal configurations vary by application and imaging modality [25] [50].
Validation strategies must address the high-dimensional nature of radiomic data, where the number of features often vastly exceeds the number of samples. Cross-validation, independent test sets, and external validation across multiple institutions are essential to demonstrate model generalizability [25] [50]. Additionally, reporting should adhere to established guidelines such as the TRIPOD statement to ensure methodological transparency and reproducibility [50].
Overcoming Implementation Challenges and Performance Optimization
The selection of an appropriate processing strategy is a fundamental step in the development of algorithms for medical imaging. The debate between block-based processing and global transform strategies represents a critical pivot point, balancing computational efficiency against reconstruction quality. Within the context of wavelet transform-based techniques, this choice significantly influences the performance of applications ranging from image denoising and compression to multi-modal synthesis [7] [54] [8].
Global transform approaches, such as applying a Discrete Wavelet Transform (DWT) across an entire image, leverage the multi-resolution analysis capabilities of wavelets to represent both coarse structures and fine details [55] [56]. In contrast, block-based strategies decompose an image into smaller, localized segments before applying transformations, allowing the algorithm to adapt to local statistics and features [7] [54]. Emerging research demonstrates that a hybrid approach, which integrates wavelet transforms with deep learning modules, is pushing the boundaries of performance in clinical applications [8] [14].
Theoretical Foundations and Comparative Analysis
Core Principles of Wavelet-Based Strategies
Wavelet transforms excel in medical image processing due to their ability to localize information in both space and frequency, a property that Fourier transforms lack [55]. This is crucial for analyzing non-stationary signals and images where features of diagnostic importance, such as tumors or anatomical boundaries, are localised [55] [56].
- Global Transform Strategies: These methods apply a transform like the DWT to the entire image, generating a hierarchical set of approximation (low-frequency) and detail (high-frequency) coefficients. This provides a multi-resolution representation of the image, effectively capturing global structures and trends [55] [56]. However, its global nature can sometimes blur or inadequately represent sharp, localised features [7].
- Block-Based Processing Strategies: These methods first divide the image into smaller, non-overlapping or partially-overlapping blocks. A transform, such as the DWT or Discrete Fourier Cosine Transform (DFCT), is then applied independently to each block [7] [54]. This localized processing allows the algorithm to adapt to the specific characteristics of different image regions, potentially preserving fine details more effectively and avoiding the introduction of global artifacts [7].
Quantitative Performance Comparison
The following tables synthesize quantitative findings from recent studies comparing these two strategies across key medical imaging tasks.
Table 1: Comparative Performance in Image Denoising (DFCT vs. DWT) [7]
| Noise Type | Processing Strategy | Transform | Performance Advantage |
|---|---|---|---|
| Gaussian | Block-Based | DFCT | Consistently superior SNR, PSNR, and IM |
| Uniform | Block-Based | DFCT | Consistently superior SNR, PSNR, and IM |
| Poisson | Block-Based | DFCT | Consistently superior SNR, PSNR, and IM |
| Salt-and-Pepper | Block-Based | DFCT | Consistently superior SNR, PSNR, and IM |
Table 2: Performance of Block-Based Haar Wavelet Transform (HWT) for Bio-Signal Compression [54]
| Signal Type | Metric | Average Performance |
|---|---|---|
| ECG | Compression Ratio (CR) | 18.06 |
| Percent Root-mean-square Difference (PRD) | 0.2470 | |
| Normalized Cross-Correlation (NCC) | 0.9467 | |
| Quality Score (QS) | 85.366 | |
| EEG | Compression Ratio (CR) | 12.67 |
| Percent Root-mean-square Difference (PRD) | 0.4014 | |
| Normalized Cross-Correlation (NCC) | 0.9187 | |
| Quality Score (QS) | 32.48 |
Table 3: Advanced Hybrid Techniques in Recent Literature
| Application | Technique | Key Metric Results |
|---|---|---|
| Medical Image Compression | DWT + Cross-Attention Learning + VAE [8] | Superior PSNR, SSIM, and MSE vs. JPEG2000 and BPG |
| Multi-modal Image Synthesis | Dual-branch Wavelet Encoding + Deformable Feature Interaction [14] | Improved qualitative results and segmentation accuracy |
Experimental Protocols
Protocol 1: Denoising with Block-Based Transforms
This protocol outlines the methodology for comparing block-based and global strategies for medical image denoising, as validated in recent literature [7].
Objective: To evaluate the efficacy of a block-based DFCT approach against a global DWT approach in suppressing various types of noise while preserving diagnostic features.
Materials and Reagents:
- Datasets: A public dataset of medical images (e.g., LIDC-IDRI for CT, MosMed for MRI) [8].
- Software: Python with libraries (NumPy, SciPy, PyWavelets) or MATLAB with the Image Processing Toolbox.
- Hardware: Standard workstation with sufficient RAM for image processing.
Procedure:
- Image Preparation: Select a set of high-quality medical images (e.g., MRI, CT, ultrasound) to serve as ground truth.
- Noise Introduction: Artificially corrupt the images with four types of noise at varying intensities: Gaussian, Uniform, Poisson, and Salt-and-Pepper [7] [57].
- Block-Based Processing (DFCT): a. Divide the noisy image into small, contiguous blocks (e.g., 8x8 or 16x16 pixels). b. Apply the DFCT to each block independently. c. Apply a thresholding function (e.g., soft-thresholding) to the transform coefficients to suppress noise. d. Reconstruct each block via the inverse DFCT. e. Reassemble the denoised blocks into a complete image.
- Global Transform Processing (DWT): a. Apply a global DWT (e.g., using a Daubechies wavelet) to the entire noisy image. b. Apply the same thresholding function to the wavelet coefficients. c. Reconstruct the denoised image via the inverse DWT.
- Performance Evaluation: Calculate quantitative metrics (SNR, PSNR, IM) by comparing the denoised images with the original ground truth images.
Protocol 2: Bio-Signal Compression using Block-Based HWT and Optimization
This protocol details a sophisticated compression algorithm for ECG and EEG signals that combines block-based processing with nature-inspired optimization [54].
Objective: To achieve high compression ratios for bio-signals while maintaining reconstruction quality sufficient for clinical diagnosis.
Materials and Reagents:
- Datasets: MIT-BIH Arrhythmia database (ECG); EEG Motor Movement/Imagery dataset [54].
- Software: MATLAB or Python with optimization toolboxes.
Procedure:
- Signal Preprocessing: Normalize the input bio-signal and divide it into fixed-length segments.
- Block-Based Transformation: Apply the Haar Wavelet Transform (HWT) to each segment to obtain wavelet coefficients [54].
- Coefficient Selection: Utilize the Coronavirus Optimization Algorithm (COVIDOA) to select the most important subset of wavelet coefficients that minimize the Percent Root-mean-square Difference (PRD) upon reconstruction [54].
- Encoding: Apply entropy encoding (e.g., Huffman coding) to the selected coefficients for final compression.
- Reconstruction & Validation: a. Decode the bitstream and use the inverse HWT on the coefficients to reconstruct the signal. b. Calculate performance metrics: Compression Ratio (CR), PRD, Normalized Cross-Correlation (NCC), and Quality Score (QS) [54].
Visualization of Workflows
The following diagrams illustrate the logical flow of the two core strategies, highlighting key differences and decision points.
Block-Based Processing Workflow
Global Transform Processing Workflow
The Scientist's Toolkit: Research Reagents and Materials
Table 4: Essential Research Reagents and Computational Tools
| Item | Function/Description | Example Use Case |
|---|---|---|
| Daubechies (Db) / Symlet Wavelets | Mother wavelets with properties like compact support and vanishing moments, crucial for signal analysis [55] [57]. | Denoising ultrasound images; multi-scale feature extraction [57]. |
| Haar Wavelet (HWT) | The simplest Daubechies wavelet; fast, reversible, and free from edge effects [54] [55]. | Block-based compression of ECG and EEG signals [54]. |
| Optimization Algorithms (e.g., COVIDOA, PSO) | Nature-inspired algorithms for selecting optimal parameters or coefficients to meet an objective function [54]. | Feature selection in wavelet domain for maximum compression and minimum distortion [54]. |
| Cross-Attention Learning (CAL) Modules | Deep learning components that dynamically weight feature importance based on context [8]. | Preserving clinically relevant regions in deep learning-based image compression [8]. |
| Variational Autoencoder (VAE) | A generative model that learns a probabilistic latent space, enabling efficient data representation [8]. | Creating a compact, informative representation for image compression in a hybrid pipeline [8]. |
| Public Datasets (e.g., MIT-BIH, BraTS2020) | Standardized, annotated datasets for training and benchmarking algorithms [54] [14]. | Evaluating compression/denoising performance; training deep learning models. |
The selection between block-based and global transform strategies is not a matter of declaring a universal winner but of matching the algorithm to the application's specific requirements. Evidence suggests that block-based processing often holds an advantage in tasks like denoising and bio-signal compression, as its localized nature better preserves fine details and adapts to regional statistics [7] [54]. However, the field is rapidly evolving towards sophisticated hybrid models that integrate the multi-resolution prowess of wavelets with the adaptive, feature-learning power of deep neural networks [8] [14]. These hybrid approaches, leveraging tools like cross-attention and variational autoencoders, represent the forefront of medical image processing, promising superior performance without compromising the diagnostic integrity critical to clinical practice.
In medical imaging, wavelet transform-based techniques present a powerful solution for balancing computational demands with the rigorous requirements of clinical practice. These methods achieve this by providing a multi-resolution analysis framework that is inherently efficient and well-suited for processing complex medical image data. The core strength of wavelet transforms lies in their ability to decompose an image into different frequency components, allowing algorithms to concentrate computational resources on the most diagnostically significant information. This principle is demonstrated in applications ranging from denoising and compression to registration and fusion, enabling the development of tools that are both high-performing and viable for real-world clinical environments. This document details specific application notes and experimental protocols that leverage wavelet transforms to enhance computational efficiency without compromising diagnostic integrity.
Application Notes & Quantitative Analysis
The integration of wavelet transforms consistently enhances performance across multiple medical imaging tasks while maintaining a favorable computational profile. The following applications highlight this balance.
Image Denoising
A comparative study of transform-domain techniques for medical image denoising evaluated the Discrete Wavelet Transform (DWT) against a block-based Discrete Fourier Cosine Transform (DFCT) approach. Contrary to the initial hypothesis favoring wavelets, the block-based DFCT, which processes images in localized segments, demonstrated superior performance. This underscores that a localized processing strategy can better adapt to an image's local statistics without introducing global artifacts, leading to more effective noise removal across various noise types [7].
Table 1: Performance Comparison of Denoising Techniques Across Noise Types
| Noise Type | Denoising Method | SNR (dB) | PSNR (dB) | Index of Merit (IM) |
|---|---|---|---|---|
| Gaussian | Global DWT | Data | Data | Data |
| Block-based DFCT | Higher | Higher | Higher | |
| Uniform | Global DWT | Data | Data | Data |
| Block-based DFCT | Higher | Higher | Higher | |
| Poisson | Global DWT | Data | Data | Data |
| Block-based DFCT | Higher | Higher | Higher | |
| Salt-and-Pepper | Global DWT | Data | Data | Data |
| Block-based DFCT | Higher | Higher | Higher |
Image Compression
A novel hybrid compression framework combining Discrete Wavelet Transform (DWT) with a deep Cross-Attention Learning (CAL) module addresses the critical trade-off between compression ratio and diagnostic quality. The DWT first decomposes the image, and the CAL module dynamically weights diagnostically critical regions. This method has been shown to outperform state-of-the-art codecs like JPEG2000 and BPG on benchmark datasets (LIDC-IDRI, LUNA16, MosMed), achieving higher Peak Signal-to-Noise Ratio (PSNR) and Structural Similarity Index (SSIM) [8].
Table 2: Compression Performance on Benchmark Medical Image Datasets
| Dataset | Method | PSNR (dB) | SSIM | MSE |
|---|---|---|---|---|
| LIDC-IDRI | JPEG2000 | Lower | Lower | Higher |
| BPG | Lower | Lower | Higher | |
| DWT + CAL (Proposed) | Higher | Higher | Lower | |
| LUNA16 | JPEG2000 | Lower | Lower | Higher |
| BPG | Lower | Lower | Higher | |
| DWT + CAL (Proposed) | Higher | Higher | Lower | |
| MosMed | JPEG2000 | Lower | Lower | Higher |
| BPG | Lower | Lower | Higher | |
| DWT + CAL (Proposed) | Higher | Higher | Lower |
Multimodal Image Fusion
The WTA-Net network, designed for fusing modalities like PET and CT, incorporates a Spatial-Channel Attention mechanism within a discrete wavelet transform framework. This approach enhances both high-frequency details (edges, textures) and low-frequency components (anatomical structures) in the frequency domain before reconstruction. Quantitative metrics show significant improvement: on brain MRI and PET fusion, Information Entropy (IE), Average Gradient (AG), and Entropy (EN) were improved by 18.92%, 14%, and 18.25%, respectively. For CT and PET fusion, IE and Spatial Frequency (SF) saw gains of 12.08% and 49.4% [13].
Experimental Protocols
Protocol 1: Wavelet-Based Medical Image Denoising and Enhancement
This protocol outlines a sequential procedure for improving medical image quality by first denoising using an Undecimated Discrete Wavelet Transform (UDWT) and then enhancing contrast via a wavelet coefficient mapping function [6].
Objectives
- To reduce noise in medical images (e.g., mammograms, chest radiographs) while preserving structural details.
- To enhance the contrast of the denoised image for improved visual interpretation and computer-aided detection.
Materials
- Image Dataset: A set of medical images (e.g., 30 mammograms, 20 chest radiographs).
- Software Environment: MATLAB or Python with PyWavelets library and custom scripting capabilities.
- Wavelet Basis: Daubechies order 2 (
db2) wavelet filter.
Methodology Part A: Shift-Invariant Denoising with UDWT
- Decomposition: Perform a 2-level, two-dimensional Undecimated Discrete Wavelet Transform (UDWT) on the original image to obtain approximation and detail coefficients (Horizontal, Vertical, Diagonal) for levels 1 and 2.
- Correlation Calculation: For each of the three detail subbands, compute the hierarchical correlation map between level 1 and level 2 coefficients using the formula:
ImgCor(p,q) = |Coef_lev1(p,q) × Coef_lev2(p,q)|. - Adaptive Thresholding:
a. For each correlation image, find the maximum value in each row in the x-direction and compute the mean (
Mean_max) of these maxima. b. Eliminate correlation values greater than0.8 × Mean_max(considered signal) and compute the standard deviation (σ) from the remaining values. c. Calculate the threshold for each subband:THR = 1.6 × σ. - Coefficient Modification: Apply the threshold to the level 1 detail coefficients. Set
NewCoef_lev1(p,q) = Coef_lev1(p,q)if the corresponding correlation value is ≥ THR; otherwise, set it to zero. - Reconstruction: Perform an inverse UDWT using the level 1 approximation coefficients and the three modified level 1 detail coefficients to generate the denoised image.
Part B: Contrast Enhancement via Coefficient Mapping
- Decomposition: Perform a standard Discrete Wavelet Transform (DWT) on the denoised image from Part A, up to a maximum level N.
- Sigmoid Mapping: Apply a sigmoid-type mapping function to the detail coefficients at each level j to enhance edges and textures. The function is:
w_output_j = a × [1 / (1 + 1/exp((w_input_j - c)/b))] × w_input_j [%]where:w_input_jis the input coefficient value (normalized to a percentage).a = 2 - (j-1)/Nensures stronger enhancement at lower decomposition levels.bandcare constants (e.g., b=20) that determine the gradient and inflection point of the curve.
- Reconstruction: Perform an inverse DWT using the original approximation coefficients and the mapped detail coefficients to produce the final denoised and enhanced image.
Validation
- Compare the output against original images and other state-of-the-art methods using quantitative metrics such as Peak Signal-to-Noise Ratio (PSNR) for denoising efficacy and measures of contrast enhancement for clarity improvement [6].
Protocol 2: Implementation of Standardized Imaging Protocols in Multi-Site Systems
This protocol describes an organizational process for developing, adapting, and disseminating standardized imaging protocols across a complex, multi-institutional healthcare system to ensure consistent, high-quality image acquisition [58].
Objectives
- To standardize imaging protocols (CT, MR, US, NM) across a geographically distributed healthcare enterprise.
- To adapt clinical imaging protocols to scanner-specific acquisition parameters.
- To ensure consistent application of protocols at all points of care to improve the quality and reproducibility of imaging studies.
Materials
- Project Team: A Project Champion (e.g., Department Chair), a Project Lead with technical expertise, and modality-specific operational committees.
- Database Software: A database application (e.g., Microsoft Access, SharePoint) for managing protocols.
- Collaboration Platform: An electronic platform (e.g., Microsoft SharePoint) for dissemination.
Methodology
- Protocol Definition and Review: a. The Project Lead collects all existing imaging protocols from various sites and modalities. b. Subspecialty radiologist teams and technologist workgroups collaborate to review, eliminate duplicates, retire outdated protocols, and develop new, standardized clinical imaging protocols. The clinical protocol defines the exam's intent, including IV contrast details, phases, and desired output.
- Database Creation and Machine-Specific Linking: a. Create a master database linking the standardized clinical imaging protocols to scanner-specific machine acquisition protocols. b. The database should include fields for Radiology Information System (RIS) orders, contrast agents, reconstruction algorithms, and machine-specific settings. This decouples the clinical intent from the vendor-specific implementation.
- Dissemination and Implementation: a. Publish the finalized protocol library on a SharePoint site, making it the single "source of truth." b. Ensure the site is accessible to all medical and technical staff at all institutions, with filtering capabilities by modality, body part, and subspecialty.
- Quality Control and Change Management: a. Establish modality-specific operational committees for ongoing protocol maintenance, annual reviews, and approval of new or modified protocols. b. Implement a process for technologist training and competency assessment to ensure consistent application.
Validation
- Monitor the reduction in protocol count (e.g., from 899 pre-implementation to 606 post-implementation) as a measure of standardization success [58].
- Use analytics from the SharePoint site to track usage and engagement.
- Conduct regular audits of acquired images to ensure adherence to the standardized protocols.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for Wavelet-Based Medical Imaging Research
| Tool / Resource | Function / Description | Relevance to Clinical Workflow |
|---|---|---|
| Discrete Wavelet Transform (DWT) | A multi-resolution analysis tool that decomposes an image into frequency sub-bands (LL, LH, HL, HH). | Enables efficient processing by isolating features at different scales, reducing computational load for tasks like compression and denoising [8] [59]. |
| Undecimated DWT (UDWT) | A shift-invariant version of the DWT that omits downsampling, providing improved denoising performance at a higher computational cost. | Useful for applications where preserving exact spatial relationships is critical, such as quantitative image analysis [6]. |
| Cross-Attention Learning (CAL) Module | A deep learning component that dynamically weights feature maps to prioritize diagnostically relevant regions. | Enhances model efficiency by focusing computation on critical areas, preserving diagnostic integrity in compressed or fused images [8]. |
| Wavelet Attention (WA) Module | Integrates discrete wavelet transform with spatial-channel attention mechanisms to enhance frequency components in an image. | Effectively enhances both high-frequency details and low-frequency structures in fusion tasks, improving diagnostic content [13]. |
| Visual State Space Module (VSSB) | A module based on state space models (e.g., Mamba) designed for efficient long-range dependency modeling with linear computational complexity. | Provides a lightweight alternative to Transformers for capturing global context in images, ideal for deployment in resource-constrained environments [60]. |
| Standardized Protocol Database | A centralized repository (e.g., SharePoint) linking clinical imaging protocols to machine-specific acquisition settings. | Ensures consistent, high-quality image acquisition across a healthcare system, which is fundamental for both clinical diagnostics and research data integrity [58]. |
The integration of wavelet transforms with deep learning architectures represents a significant paradigm shift in medical image analysis, offering powerful solutions to some of the field's most persistent challenges. Medical imaging modalities, including magnetic resonance imaging (MRI), computed tomography (CT), and digital histopathology, generate high-resolution data that contains critical diagnostic information across multiple spatial frequencies and scales. The efficient processing of these complex datasets is paramount for accurate disease diagnosis, treatment planning, and clinical research. Traditional deep learning approaches, particularly Convolutional Neural Networks (CNNs), have demonstrated remarkable capabilities in extracting local features and patterns from medical images. However, their inherent limitation lies in the local receptive field of convolutional operations, which constrains their ability to capture long-range dependencies and global contextual information—elements crucial for understanding anatomical structures that extend across large image areas [61] [62].
The recent introduction of Transformer architectures to computer vision has addressed some of these limitations through self-attention mechanisms that can model global relationships across entire images. Nevertheless, pure Transformer models often struggle with capturing fine-grained local details and spatial structures, which are fundamental requirements in medical imaging applications where precision is critical for diagnostic accuracy [63] [62]. This limitation is particularly evident in tasks such as tumor boundary delineation or segmentation of small anatomical structures. The emerging solution to these complementary challenges lies in hybrid architectures that strategically combine the strengths of CNNs and Transformers while mitigating their respective weaknesses. These hybrid models create a powerful synergy where CNNs excel at extracting hierarchical local features and spatial relationships, while Transformers effectively capture global contextual dependencies and long-range spatial relationships [64] [62].
The incorporation of wavelet transforms into these hybrid frameworks adds another dimension of capability, particularly for medical image processing. Wavelet transforms provide a mathematical framework for multi-resolution analysis, enabling the decomposition of images into constituent frequency components at different scales. This capability is especially valuable in medical imaging, where diagnostically relevant information may be distributed across different frequency bands. For instance, coarse anatomical structures often reside in low-frequency components, while fine details such as tissue textures, edges, and subtle pathological features are captured in high-frequency components [18] [59]. The Stationary Wavelet Transform (SWT) and Discrete Wavelet Transform (DWT) are particularly valuable in medical imaging applications because they preserve spatial information during the decomposition process, unlike traditional Fourier transforms [18]. This preservation is crucial for maintaining structural integrity and spatial relationships in reconstructed images, ensuring that critical diagnostic features remain uncompromised during processing.
Implementation Architectures and Methodologies
Wavelet-Enhanced Compression Architectures
Medical image compression represents a critical application domain where wavelet-deep learning hybrids have demonstrated remarkable performance. The massive volume of imaging data generated in clinical practice creates substantial challenges for storage and transmission, particularly in telemedicine and resource-constrained environments. Traditional compression standards like JPEG and JPEG2000 often fail to preserve diagnostically crucial information at higher compression ratios, potentially compromising clinical decision-making. The hybrid framework integrating Stationary Wavelet Transform (SWT) with Stacked Denoising Autoencoders (SDAE) addresses these limitations through a sophisticated multi-stage approach [18].
The process begins with SWT-based decomposition of input images into multi-resolution sub-bands, effectively separating image content into approximation coefficients (capturing broad structural information) and detail coefficients (containing fine textures and edges). This decomposition enables selective processing of different frequency components according to their diagnostic significance. Subsequently, Gray-Level Co-occurrence Matrix (GLCM) features are extracted to quantify textural patterns within the image, providing complementary information to the frequency-domain representations. The incorporation of K-means clustering allows for region-adaptive compression by identifying and processing diagnostically relevant regions with different fidelity parameters compared to less critical areas [18]. This regional adaptability is particularly valuable in medical imaging, where specific anatomical structures or pathological findings may require higher preservation fidelity than surrounding tissues.
The SDAE component then performs feature compression and reconstruction, trained using a custom loss function that combines Mean Squared Error (MSE) with Structural Similarity Index (SSIM) to balance pixel-level accuracy with perceptual quality. This integrated approach has demonstrated exceptional performance, achieving Peak Signal-to-Noise Ratio (PSNR) values of up to 50.36 dB and Multi-Scale Structural Similarity (MS-SSIM) of 0.9999, while maintaining rapid encoding-decoding times of 0.065 seconds—making it suitable for real-time clinical applications [18].
An alternative implementation employs Discrete Wavelet Transform (DWT) integrated with cross-attention learning and variational autoencoders (VAE) for medical image compression. In this architecture, the DWT provides the initial multi-resolution decomposition, while a cross-attention module dynamically weights feature maps to prioritize regions with high diagnostic information content [8]. The VAE component learns a probabilistic latent representation that facilitates efficient entropy coding while ensuring robust reconstruction. This method has shown superior performance compared to established codecs like JPEG2000 and BPG across multiple evaluation metrics, including PSNR and SSIM, particularly preserving critical diagnostic features in challenging cases [8].
Hybrid CNN-Transformer Segmentation Architectures
Medical image segmentation represents another domain where wavelet-CNN-Transformer hybrids have demonstrated substantial advancements. The DCF-Net (Dual Attention and Cross-layer Fusion Network) architecture exemplifies this approach, incorporating a CNN-based encoder for local feature extraction and a Transformer-enhanced decoder with specialized attention mechanisms for global context modeling [61] [65]. The architecture introduces two innovative components: the Channel-Adaptive Sparse Attention (CASA) module and the Synergistic Skip-connection and Cross-layer Fusion (SSCF) module.
The CASA module implements a dual attention mechanism that combines Cross-Covariance Attention (XCA) with Top-k Sparse Attention (TKSA) to enhance semantic modeling while filtering redundant features. This dual approach enables the network to focus computational resources on anatomically significant regions while suppressing less relevant background information [61]. The SSCF module refines the traditional U-Net skip connections by implementing sophisticated feature fusion strategies that better bridge the semantic gap between encoder and decoder pathways. This design enables more effective integration of low-level spatial details from the encoder with high-level semantic information from the decoder, resulting in improved boundary delineation and segmentation accuracy for complex anatomical structures [61].
Experimental validation on benchmark datasets including Synapse, ACDC, and ISIC2017 has demonstrated state-of-the-art performance without requiring extensive pre-training, highlighting the architectural efficiency of this hybrid approach [61]. The parallel integration strategy, as implemented in UnetTransCNN, offers an alternative architectural paradigm where CNN and Transformer pathways operate simultaneously rather than sequentially [62]. This parallel processing enables dedicated extraction of both local and global features throughout the network, with adaptive coupling units dynamically fusing these complementary representations at multiple scales. The incorporation of an Adaptive Fourier Neural Operator (AFNO) in the Transformer pathway further enhances frequency-domain processing capabilities, creating a more comprehensive feature representation landscape [62].
Table 1: Performance Comparison of Hybrid Architectures for Medical Image Segmentation
| Architecture | Dataset | Evaluation Metric | Performance | Key Innovation |
|---|---|---|---|---|
| DCF-Net | Synapse | Average Dice Score | 85.3% | Channel-Adaptive Sparse Attention (CASA) |
| DCF-Net | ACDC | Dice Score | State-of-the-art | Synergistic Skip-connection Fusion (SSCF) |
| UnetTransCNN | BTCV | Average Dice Score | 85.3% | Parallel CNN-Transformer with AFNO |
| UnetTransCNN | MSD | Dice Score | State-of-the-art | 3D Volumetric Adaptations |
| D-TrAttUnet | Covid-19 | Segmentation Accuracy | Superior to baselines | Dual-decoder with attention gates |
| D-TrAttUnet | Bone Metastasis | Segmentation Accuracy | Superior to baselines | Composite Transformer-CNN encoder |
Classification Architectures with Wavelet Decomposition
Classification of medical images, particularly in dermatology and oncology, has benefited from wavelet-integrated hybrid architectures. One prominent implementation combines wavelet decomposition with EfficientNet models for skin lesion classification [59]. In this approach, input images undergo multi-level wavelet decomposition, generating sub-bands (LL, LH, HL, HH) that capture distinct frequency characteristics and directional features. These wavelet coefficients are then processed through the EfficientNet backbone, which employs compound scaling to optimize model dimensions for the specific classification task.
The fusion of wavelet features with standard convolutional outputs occurs at intermediate network layers, creating enriched representations that leverage both spatial and frequency-domain information. This hybrid approach has demonstrated impressive performance, achieving accuracy rates of 94.7% on the HAM10000 dataset and 92.2% on ISIC2017, competitive with more complex multi-stage frameworks while offering reduced computational complexity [59]. The wavelet preprocessing enables enhanced focus on textural patterns and structural characteristics that are particularly relevant for discriminating between different classes of skin lesions, many of which manifest through subtle variations in texture and edge characteristics.
Quantitative Performance Analysis
Compression Performance Metrics
The evaluation of hybrid wavelet-deep learning architectures for medical image compression employs comprehensive quantitative metrics to assess both compression efficiency and reconstruction quality. These metrics are particularly important in medical contexts where diagnostic integrity must be preserved despite significant data reduction.
Table 2: Performance Metrics of Wavelet-Based Deep Learning Compression Models
| Model | PSNR (dB) | MS-SSIM | MSE | Encoding/Decoding Time (s) | Compression Ratio |
|---|---|---|---|---|---|
| SWT-SDAE-GLCM-K-means [18] | 50.36 | 0.9999 | - | 0.065 | High |
| DWT-Cross-Attention-VAE [8] | Superior to JPEG2000/BPG | Superior to JPEG2000/BPG | Superior to JPEG2000/BPG | - | High |
| Traditional JPEG2000 | ~35-40 | ~0.98-0.99 | Higher than hybrids | Faster | Moderate to High |
The exceptional PSNR values achieved by hybrid models (exceeding 50 dB in some cases) indicate superior signal preservation compared to traditional methods. Similarly, MS-SSIM values approaching 1.0 demonstrate excellent perceptual quality maintenance in reconstructed images. These metrics collectively validate the effectiveness of wavelet-deep learning hybrids in balancing the competing demands of compression efficiency and diagnostic quality preservation [18] [8].
Segmentation and Classification Performance
For segmentation and classification tasks, hybrid architectures have consistently demonstrated state-of-the-art performance across multiple benchmarks and modalities. The quantitative evaluation employs standard metrics including Dice similarity coefficient, accuracy, precision, and recall, with rigorous statistical validation.
Table 3: Segmentation Performance of Hybrid CNN-Transformer Architectures
| Architecture | Dataset | Dice Score (%) | Precision | Recall | Key Improvement |
|---|---|---|---|---|---|
| DCF-Net [61] | Synapse | 85.3 | - | - | 6.382% improvement for gallbladder |
| DCF-Net [61] | ACDC | State-of-the-art | - | - | 6.772% improvement for adrenal glands |
| UnetTransCNN [62] | BTCV | 85.3 | - | - | Superior for large and small organs |
| Hybrid CNN-Transformer [63] | Retinal Fundus | State-of-the-art | - | - | Interpretable disease detection |
The consistent outperformance of hybrid architectures across diverse datasets and anatomical structures underscores their robustness and generalizability. Particularly noteworthy is the significant improvement in challenging segmentation targets such as gallbladder and adrenal glands, which often present difficulties due to their irregular shapes and weak boundary definitions [61]. These improvements highlight the complementary benefits of CNN-driven local feature extraction and Transformer-enabled global context modeling in medical image analysis.
Experimental Protocols and Methodologies
Protocol 1: Medical Image Compression Using SWT-SDAE Framework
Objective: Implement and validate a hybrid medical image compression framework integrating Stationary Wavelet Transform (SWT), Stacked Denoising Autoencoder (SDAE), GLCM feature extraction, and K-means clustering for diagnostically lossless compression.
Materials and Reagents:
- Medical image datasets (NIH Chest X-ray, INBreast, Camelyon16, LIDC-IDRI)
- Computing infrastructure with GPU acceleration (NVIDIA T4 or equivalent)
- Python 3.8+ with PyWavelets, TensorFlow/PyTorch, scikit-learn, OpenCV
Procedure:
- Data Preprocessing:
- Resize all input images to standardized dimensions (256×256 pixels for computational efficiency)
- Apply intensity normalization (zero-mean, unit-variance) to standardize input distribution
- Data augmentation through rotation (±15°), horizontal flipping, and mild elastic deformations
Wavelet Decomposition:
- Perform 2-level Stationary Wavelet Transform (SWT) using Daubechies (db4) or Symlet wavelets
- Decompose input images into approximation (LL) and detail coefficients (LH, HL, HH)
- Process each sub-band independently to leverage frequency-specific characteristics
Texture Feature Extraction:
- Compute Gray-Level Co-occurrence Matrix (GLCM) for each image patch (8×8 blocks)
- Extract statistical features from GLCM: contrast, correlation, energy, homogeneity
- Fuse GLCM features with wavelet coefficients for enriched representation
Region-Adaptive Processing:
- Apply K-means clustering (K=4) on fused features to identify diagnostically significant regions
- Assign region-specific compression parameters based on cluster significance
- Implement higher fidelity preservation for regions with identified clinical relevance
Stacked Denoising Autoencoder Compression:
- Design SDAE architecture with 5 encoding and 5 decoding layers with skip connections
- Train using combined loss function: L_total = 0.7×MSE + 0.3×(1-SSIM)
- Implement gradual fine-tuning with progressive compression ratio increases
Validation and Testing:
- Evaluate on held-out test sets using PSNR, SSIM, MS-SSIM, and clinical reader studies
- Compare against JPEG2000, BPG, and other deep learning baselines
- Perform statistical significance testing (paired t-test, p<0.05) across multiple trials
Troubleshooting Tips:
- If reconstruction artifacts appear in high-frequency regions, increase the weighting of detail coefficients in the loss function
- For unstable training, implement gradient clipping and learning rate scheduling
- If compression ratios are suboptimal, adjust the bottleneck layer dimensions incrementally
Protocol 2: Medical Image Segmentation Using DCF-Net Architecture
Objective: Implement and validate DCF-Net for medical image segmentation with dual attention mechanisms and cross-layer fusion.
Materials and Reagents:
- Medical segmentation datasets (Synapse, ACDC, ISIC2017)
- GPU workstations with ≥12GB memory
- PyTorch or TensorFlow with MONAI library
- Visualization tools (ITK-SNAP, 3D Slicer)
Procedure:
- Data Preparation:
- Standardize image intensities using dataset-specific normalization
- Apply appropriate data augmentation: random cropping, rotation, flipping, intensity shifts
- Implement sliding window approach for large volumetric data
Hybrid Encoder Implementation:
- Configure CNN backbone (ResNet-50 or EfficientNet-B4) for local feature extraction
- Implement Transformer pathway with multi-head self-attention (8 heads, 512 embedding dimensions)
- Process input through both pathways in parallel with shared weights
Channel-Adaptive Sparse Attention (CASA):
- Implement Cross-Covariance Attention (XCA) for channel-wise dependency modeling
- Integrate Top-k Sparse Attention (TKSA) with k=30% of tokens for computational efficiency
- Apply cascaded XCA → TKSA processing in decoder pathway
Synergistic Skip-connection and Cross-layer Fusion (SSCF):
- Design feature refinement modules for encoder features before fusion
- Implement dual residual connections to preserve gradient flow
- Apply channel-wise attention for adaptive feature selection
Training Protocol:
- Initialize with He normal initialization for CNN components and Xavier for Transformers
- Train with combined loss: L_total = 0.6×DiceLoss + 0.4×CrossEntropyLoss
- Use AdamW optimizer (lr=1e-4, weight_decay=1e-5) with cosine annealing scheduler
- Implement gradient accumulation (steps=4) for effective batch size enhancement
Validation and Analysis:
- Evaluate using Dice similarity coefficient, Hausdorff distance, and relative volume error
- Perform ablation studies to quantify contribution of individual components
- Conduct qualitative analysis with clinical experts for boundary accuracy assessment
Troubleshooting Tips:
- For memory limitations, reduce batch size and increase gradient accumulation steps
- If convergence is slow, implement warm-up phase for first 10% of training
- For overfitting on small datasets, apply stronger regularization (dropout=0.3, weight decay=1e-4)
Table 4: Essential Research Reagents and Computational Resources
| Resource Category | Specific Tools/Platforms | Application Context | Key Specifications |
|---|---|---|---|
| Deep Learning Frameworks | PyTorch, TensorFlow, MONAI | Model implementation and training | GPU acceleration, automatic differentiation |
| Wavelet Processing Libraries | PyWavelets, MATLAB Wavelet Toolbox | Multi-resolution analysis | Support for DWT, SWT, various wavelet families |
| Medical Imaging Libraries | ITK, SimpleITK, OpenCV, PIL | Image preprocessing and augmentation | DICOM support, spatial transformations |
| Visualization Tools | ITK-SNAP, 3D Slicer, TensorBoard | Result analysis and interpretation | 3D rendering, segmentation overlay |
| Computational Infrastructure | NVIDIA T4, V100, A100 GPUs | Model training and inference | GPU memory ≥12GB, CUDA support |
| Public Datasets | Synapse, ACDC, ISIC2017, HAM10000 | Model training and benchmarking | Multi-organ, multi-modal, annotated data |
Workflow and Architectural Diagrams
Hybrid Compression Architecture Workflow
DCF-Net Segmentation Architecture
Wavelet-CNN-Transformer Integration Framework
In medical imaging, convolutional neural networks (CNNs) traditionally rely on pooling and strided convolution for downsampling and transpose convolution or interpolation for upsampling. However, these methods cause significant information loss, particularly of high-frequency details like tissue boundaries and small lesions, which are critical for diagnostic accuracy [10]. Wavelet transform offers a mathematically rigorous solution by enabling lossless, multi-scale decomposition of an image into distinct frequency sub-bands. This article details the application of wavelet-guided techniques to mitigate information loss, providing structured protocols and resources for their implementation in medical imaging research.
Quantitative Performance of Wavelet-Based Architectures
The integration of wavelet transforms into deep learning models for medical imaging has demonstrated superior performance across multiple tasks, quantitatively outperforming traditional methods.
Table 1: Performance Metrics of Wavelet-Based Medical Imaging Models
| Model Name | Primary Task | Key Metric | Reported Score | Comparative Advantage |
|---|---|---|---|---|
| WaveMorph [10] | Image Registration | Dice Score (Atlas-to-patient) | 0.779 ± 0.015 | State-of-the-art accuracy & real-time inference (0.072 s/image) |
| Dice Score (Inter-patient) | 0.824 ± 0.021 | |||
| WIAF Model [20] | Brain Tumor Segmentation | Average Dice Score | 85.0% (BraTS2020), 88.1% (FeTS2022) | High accuracy with only 5.23M parameters |
| Wave-GMS [66] | General Image Segmentation | Number of Trainable Parameters | ~2.6M | Enables large batch training on cost-effective GPUs |
| WTA-Net [13] | PET/CT Image Fusion | Information Entropy (IE) / Spatial Frequency (SF) | IE: +18.92%, SF: +49.4% | Significant enhancement of fused image quality |
Detailed Experimental Protocols
Protocol 1: Multi-Scale Wavelet Feature Fusion for Downsampling
This protocol replaces standard downsampling in a CNN encoder, preserving high-frequency information that is typically lost [10] [14].
Application Notes: This is ideally applied as the first downsampling layer in a network (e.g., replacing the initial max-pool in a U-Net) and can be repeated at subsequent downsampling stages. The following workflow outlines the end-to-end process.
Materials & Equipment:
- Computing Environment: GPU with CUDA support (e.g., NVIDIA RTX series).
- Software: Python 3.8+, PyTorch or TensorFlow, and a wavelet toolbox (e.g.,
PyWavelets). - Datasets: Publicly available medical image datasets (e.g., BraTS2020 for brain tumors [20], IXI for brain MRI [10]).
Step-by-Step Procedure:
- Image Decomposition:
- For a given 2D input image, apply a 2D Discrete Wavelet Transform (DWT) using a chosen wavelet basis (e.g., Haar, Daubechies). This is computationally efficient and provides lossless decomposition [10] [66].
- The transform yields four non-overlapping sub-band images: LL (low-low frequency, approximate image), LH (low-high, horizontal details), HL (high-low, vertical details), and HH (high-high, diagonal details) [13].
- Multi-Scale Feature Extraction:
- Process each of the four sub-band images using a multi-scale convolutional block (e.g., ConvNeXt) with different kernel sizes (e.g., 3x3, 5x5, 7x7). This allows the network to capture features at various scales from different frequency components [10].
- Feature Fusion:
- Concatenate the feature maps obtained from processing all four sub-bands along the channel dimension.
- Pass the concatenated features through a 1x1 convolution to reduce the channel dimension and integrate the information, producing a final feature map that retains both structural and detailed information [14].
Protocol 2: Dynamic Upsampling for Detail Reconstruction
This protocol addresses the blurring and distortion caused by traditional upsampling methods in the decoder [10] [67].
Application Notes: Implement this in the decoder path of a segmentation or synthesis network (e.g., U-Net) after skip connections have been added. It dynamically learns the upsampling process, leading to sharper reconstructions.
Materials & Equipment:
- Same as Protocol 1.
Step-by-Step Procedure:
- Input Preparation:
- The input to this module is the combined feature map from the decoder's previous layer and the corresponding skip connection from the encoder.
- Learned Sampling:
- Instead of using fixed interpolation kernels (e.g., bilinear or bicubic), the DySample module dynamically predicts a set of 2D sampling offsets for each pixel in the target higher-resolution output [67].
- These offsets are learned during training, allowing the network to adaptively "look up" the most relevant values from the input feature map for accurate reconstruction.
- Feature Warping:
- Apply the predicted offsets to the input feature map using a bilinear sampling operation (e.g.,
grid_samplein PyTorch). This effectively warps the input features into the higher-resolution space.
- Apply the predicted offsets to the input feature map using a bilinear sampling operation (e.g.,
- Output:
- The output is a feature map with a higher spatial resolution, which better preserves fine-grained anatomical structures and sharp boundaries compared to traditional upsampling [10].
Protocol 3: Adaptive Wavelet Fusion for Image Translation
This protocol is for image-to-image translation tasks (e.g., CBCT-to-CT synthesis) without requiring paired data from both domains during training, enhancing robustness to distribution shifts [51].
Application Notes: This is a higher-level framework, particularly useful when target domain data (e.g., CT) is available but source domain data (e.g., CBCT from a new hospital) is not seen during training.
Materials & Equipment:
- Same as Protocol 1.
- A pre-trained diffusion model trained exclusively on the target domain (e.g., CT images) [51].
Step-by-Step Procedure:
- Domain-Specific Training:
- Train a denoising diffusion model (DDPM) only on images from the target domain (e.g., CT). This model learns the data distribution of high-quality CT images without exposure to CBCT variants [51].
- Reverse Diffusion with Guidance:
- To convert a source CBCT image, initiate the reverse diffusion process using the pre-trained CT model.
- Wavelet-Based Fusion at Each Step:
- At every step of the reverse diffusion, decompose both the current generated CT-like image and the source CBCT image into their wavelet sub-bands (LL, LH, HL, HH).
- Compute the band-specific differences between the sub-bands of the two images.
- Adaptive Fusion: For sub-bands with small differences (e.g., high-frequency anatomical edges), assign a large weighting to the CBCT's sub-band to preserve its structure. For sub-bands with large differences (e.g., low-frequency intensity profiles), assign a smaller weighting to the CBCT, allowing the CT model's distribution to dominate [51].
- Image Reconstruction:
- Fuse the sub-bands based on the adaptive weights.
- Perform an Inverse DWT (IDWT) on the fused sub-bands to reconstruct the image for the next reverse diffusion step.
- Final Output:
- After all reverse steps, the output is a synthesized CT image that retains the anatomical structure of the source CBCT but exhibits the intensity distribution and quality of a real CT scan.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Computational Tools
| Item / Reagent | Function / Role | Example & Notes |
|---|---|---|
| Discrete Wavelet Transform (DWT) | Core decomposition tool for multi-resolution analysis. | Use PyWavelets (Haar, Daubechies). Haar is common for its simplicity and lossless property [10]. |
| Multi-Scale CNN Backbone | Extracts and fuses features from different frequency sub-bands. | ConvNeXt blocks are effective for balancing accuracy and efficiency [10]. |
| Dynamic Upsampling Module | Replaces fixed interpolation for sharper detail reconstruction. | DySample learns sampling offsets, improving boundary delineation [67]. |
| Pre-trained Diffusion Model | Serves as a prior for the target domain in synthesis tasks. | Train on target domain only (e.g., CT) for zero-shot translation [51]. |
| Public Medical Image Datasets | Provide standardized data for training and validation. | BraTS2020 (brain tumors) [20], IXI (brain MRI) [10], SynthRAD2023 (CBCT/CT pairs) [51]. |
| Deep Learning Framework | Platform for model implementation and training. | PyTorch or TensorFlow with GPU acceleration. |
Within the broader context of advancing wavelet transform-based techniques for medical imaging research, the selection of appropriate parameters is a critical step that directly influences the performance of image analysis, compression, and computational efficiency. The wavelet base (or mother wavelet) and the number of decomposition levels are two pivotal parameters that researchers must optimize for specific imaging modalities and clinical tasks. The wavelet base determines the shape used to decompose the image, impacting how well the transform captures essential diagnostic features. Concurrently, the decomposition level governs the depth of the multi-resolution analysis, balancing detail capture against computational burden and potential information redundancy. This document provides a structured framework for optimizing these parameters, supported by quantitative data and detailed experimental protocols tailored to medical imaging applications, including MRI, CT, ultrasound, and PET.
Wavelet Base Selection: Criteria and Comparative Analysis
The choice of a wavelet base is fundamental, as it must match the characteristic features of the medical image modality and the specific clinical or research objective.
Key Selection Criteria
- Vanishing Moments: Wavelets with higher vanishing moments (e.g., Daubechies series) are more effective at representing smooth signals and are ideal for compressing images with large homogeneous regions, such as soft tissues in MRI and CT [36].
- Symmetry: Symmetric wavelets (e.g., Symlets) help to minimize phase distortion, which is crucial for preserving the precise locations of edges and pathological features in diagnostic images [36].
- Compact Support: Wavelets with compact support (e.g., Haar, Daubechies) enable localized analysis, which is beneficial for detecting and preserving fine details, textures, and small lesions [36].
- Regularity: This property relates to the smoothness of the wavelet function. Higher regularity wavelets can lead to better reconstructed image quality by reducing artifacts in applications like image compression and denoising [36].
Quantitative Comparison of Common Wavelet Bases
The following table summarizes the characteristics and recommended applications of common wavelet bases in medical imaging.
Table 1: Comparative Analysis of Wavelet Bases for Medical Imaging
| Wavelet Base | Vanishing Moments | Symmetry | Compact Support | Recommended Medical Imaging Applications |
|---|---|---|---|---|
| Haar | 1 | Symmetric | Excellent | Real-time registration (WaveMorph) [10], quick prototyping, segmenting tissues with sharp transitions. |
| Daubechies (db2-db10) | 2 - 10 | Asymmetric | Excellent | General-purpose compression [8] and denoising of MRI/CT/US [15] [36], ideal for representing smooth areas. |
| Symlets | 4 - 8 | Near-symmetric | Excellent | Applications requiring a balance between smooth representation and edge preservation, such as PET-MRI fusion [13]. |
| Coiflets | 5 | Near-symmetric | Excellent | A good alternative to Daubechies for achieving a closer match between the wavelet and scaling functions. |
| Biorthogonal | Variable | Symmetric | Excellent | Tasks where linear phase is critical, such as in image fusion and synthesis [14] [68]. |
Decomposition Level Optimization
Selecting the optimal number of decomposition levels is a trade-off between capturing sufficient detail and managing computational complexity.
Guidelines for Level Selection
- Image Resolution and Feature Size: The decomposition should be deep enough to isolate the features of interest into appropriate sub-bands. For example, fine textures and micro-calcifications require high-frequency sub-bands available at lower decomposition levels, while larger anatomical structures are analyzed at coarser, higher levels.
- Modality-Specific Considerations: In ultrasound image analysis for tumor diagnosis, a multi-scale approach that captures features at various levels has been shown to be effective [15]. For 3D MR image reconstruction from orthogonal scans, a multi-level wavelet fusion is typically employed to achieve isotropic resolution [68].
- Theoretical Maximum: The maximum possible decomposition level is mathematically constrained by the image dimensions, specifically ( \lfloor \log_2(\text{min}(W, H)) \rfloor ), where ( W ) and ( H ) are the width and height of the image.
- Empirical Optimization: The optimal level is often determined empirically. A common strategy is to increment the decomposition level until the high-frequency sub-bands at the coarsest level contain minimal structural information, predominantly comprising noise.
Impact of Decomposition Levels on Performance
Table 2: Influence of Decomposition Levels on Common Medical Imaging Tasks
| Task | Typical Optimal Level | Rationale and Performance Impact |
|---|---|---|
| Image Compression [8] | 3 - 5 | Balances energy compaction (for high compression) with the preservation of diagnostically critical high-frequency details. |
| Image Denoising [12] | 3 - 4 | Allows for effective noise separation in detailed sub-bands while maintaining the structural integrity of the image at lower frequencies. |
| Image Fusion [13] [68] | 2 - 4 | Facilitates the merging of complementary features (e.g., CT anatomy with PET metabolism) at multiple scales without introducing artifacts. |
| Image Registration [10] | 2 - 3 (in multi-scale frameworks) | A coarse-to-fine strategy improves accuracy and convergence speed by first aligning global structures. |
Experimental Protocol for Parameter Optimization
This section provides a detailed, step-by-step methodology for empirically determining the optimal wavelet base and decomposition level for a specific medical imaging application.
Workflow for Systematic Parameter Selection
The following diagram illustrates the logical workflow and decision-making process for parameter optimization.
Diagram Title: Wavelet Parameter Optimization Workflow
Protocol Steps
Problem Definition and Dataset Curation
- Objective: Clearly define the primary goal of the wavelet-based processing (e.g., maximising compression ratio while maintaining diagnostic quality, or optimising denoising performance).
- Dataset: Assemble a representative dataset of medical images relevant to the clinical task. The dataset should be divided into a training/validation set for parameter exploration and a held-out test set for final evaluation. It is critical that the dataset reflects the expected variability in the application (e.g., different scanners, patient populations).
Selection of Candidate Parameters
- Wavelet Bases: Based on Section 2.2 and the application goal, select 3-5 candidate wavelet bases. A typical set could include Haar (for baseline), db4 (a common Daubechies choice), db8 (higher vanishing moments), and a biorthogonal wavelet (e.g., 'bior4.4').
- Decomposition Levels: Define a range to test, typically from 1 to a sensible maximum (e.g., 5 or the theoretical maximum for your image size).
Experimental Execution and Evaluation
- For each combination of wavelet base and decomposition level, execute the target algorithm (e.g., compression, fusion).
- Quantitatively evaluate the output using task-specific metrics. It is strongly recommended to use multiple metrics to obtain a balanced assessment.
- For clinical applications, a qualitative assessment by a domain expert (e.g., a radiologist) is indispensable to ensure that diagnostically critical information is preserved.
Analysis and Optimal Selection
- Visual Analysis: Plot the evaluation metrics against the decomposition levels for each wavelet base to identify trends and performance peaks.
- Statistical Testing: Perform statistical significance tests (e.g., paired t-test, ANOVA) on the results from the best-performing parameter sets to ensure the observed differences are not due to chance.
- Final Choice: The optimal parameter set is the one that delivers the best and most consistent performance across the validation set on the primary evaluation metric(s), while also meeting all clinical and computational constraints.
The Scientist's Toolkit: Research Reagents and Materials
This section outlines the essential computational tools and software resources required to implement the wavelet-based parameter optimization protocols described in this document.
Table 3: Essential Research Toolkit for Wavelet-Based Medical Image Analysis
| Tool/Category | Specific Examples | Function and Utility in Optimization |
|---|---|---|
| Programming Environments | MATLAB (with Wavelet Toolbox), Python (with PyWavelets, SciPy) | Provide built-in functions for a wide range of wavelet transforms (DWT, SWT) and easy computation of evaluation metrics, facilitating rapid prototyping. |
| Deep Learning Frameworks | PyTorch, TensorFlow | Essential for implementing and training novel, learnable wavelet-based architectures like WTA-Net [13] or WaveMorph [10] that integrate wavelet transforms with neural networks. |
| Optimization Libraries | Scikit-learn, Bayesian Optimization (e.g., scikit-optimize) | Automate the hyperparameter search process. Bayesian optimization is particularly effective for efficiently navigating the parameter space of wavelet bases and levels [12]. |
| Medical Image Datasets | LIDC-IDRI, BraTS, IXI [8] [10] [14] | Standardized, publicly available datasets are crucial for benchmarking the performance of different parameter sets against state-of-the-art methods. |
| Visualization & Analysis Software | ITK-SNAP, ImageJ, Matplotlib/Seaborn | Used for qualitative inspection of results (e.g., checking for artifacts) and for creating plots to analyze the relationship between parameters and performance metrics. |
Quantitative Performance Evaluation and Benchmarking Against State-of-the-Art
The rigorous evaluation of image quality and algorithm performance is fundamental to advancing wavelet transform-based techniques in medical imaging research. Quantitative metrics provide objective evidence necessary for validating new compression, denoising, and super-resolution methods before clinical deployment. These metrics collectively bridge the gap between technical innovation and practical clinical utility, ensuring that computational enhancements translate into genuine diagnostic benefits [69]. In the specific context of wavelet-based research, these measurements are crucial for optimizing parameters such as decomposition levels and mother wavelet selection, ultimately determining the clinical viability of proposed techniques [70].
The evaluation framework can be categorized into image fidelity metrics, which assess pixel-level or structural similarity between processed and original images; task-specific metrics, which evaluate performance on clinical tasks such as segmentation; and clinical evaluation criteria, which ensure diagnostic integrity and adherence to radiological standards [69] [71]. This document details the application of these metrics, with a specific focus on their relevance to wavelet-based medical imaging research.
Quantitative Metric Definitions and Applications
Core Metric Definitions and Formulae
Table 1: Fundamental Image Fidelity and Segmentation Metrics
| Metric | Full Name | Mathematical Definition | Interpretation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| PSNR | Peak Signal-to-Noise Ratio | ( PSNR = 10 \cdot \log{10}\left(\frac{MAXI^2}{MSE}\right) ) where ( MSE ) is Mean Squared Error, ( MAX_I ) is the maximum pixel value. | Higher values indicate better fidelity. Measured in dB; sensitive to large errors but may correlate poorly with human perception [71]. | ||||||
| SSIM | Structural Similarity Index Measure | ( SSIM(x,y) = \frac{(2\mux\muy + c1)(2\sigma{xy} + c2)}{(\mux^2 + \muy^2 + c1)(\sigmax^2 + \sigmay^2 + c_2)} ) where ( \mu ) is mean intensity, ( \sigma ) is standard deviation/variance, ( c ) are stabilization constants [71]. | Scores range from -1 to 1. A value of 1 indicates perfect structural similarity. More aligned with human perception than PSNR [69]. | ||||||
| Dice Score | Dice-Sørensen Coefficient (F1-Score) | ( Dice = \frac{2 | X \cap Y | }{ | X | + | Y | } = \frac{2 \cdot TP}{2 \cdot TP + FP + FN} ) where ( X ) and ( Y ) are the segmented and ground truth volumes, and TP/FP/FN are True/False Positives/Negatives [72]. | Measures overlap. Ranges from 0 (no overlap) to 1 (perfect segmentation). Tolerant to small errors [72]. |
| IoU | Intersection over Union (Jaccard Index) | ( IoU = \frac{ | X \cap Y | }{ | X \cup Y | } = \frac{TP}{TP + FP + FN} ) [72]. | Similar to Dice but more sensitive to small errors. Always lower than or equal to the Dice score for the same segmentation [72]. | ||
| Hausdorff Distance | --- | ( HD(A,B) = \max\left( \max{a \in A} \min{b \in B} d(a,b), \max{b \in B} \min{a \in A} d(a,b) \right) ) where ( A ) and ( B ) are two sets of points, and ( d(a,b) ) is the Euclidean distance [72]. | Measures the maximum distance between the boundaries of two segmentations. In pixels; sensitive to outliers; lower values are better [72]. |
Contextual Application in Medical Imaging Research
Table 2: Metric Selection for Specific Research Contexts
| Research Domain | Primary Metrics | Supporting Metrics | Relevance to Wavelet-Based Techniques |
|---|---|---|---|
| Image Compression (e.g., Wavelet-based 3D compression) | PSNR, SSIM [8] | Dice Score (for task-based evaluation) [73] | Evaluating reconstruction fidelity after wavelet compression and encoding. Critical for determining acceptable compression ratios [73]. |
| Super-Resolution (e.g., enhancing CT resolution) | PSNR, SSIM [69] | Dice Score, Classification Accuracy (AUC) [69] | Quantifying the preservation of diagnostic features when wavelet transforms are used for multi-scale feature extraction [69]. |
| Image Segmentation (e.g., cerebrovascular 3D segmentation) | Dice Score, IoU [73] [72] | Hausdorff Distance [72] | Validating segmentation robustness on wavelet-denoised or compressed volumes. Hausdorff Distance ensures critical boundary accuracy [73] [72]. |
| Image Denoising (e.g., DWT-based filtering) | PSNR, SSIM [7] | Task-based metrics (e.g., diagnostic accuracy) | Assessing noise reduction and structural preservation. Guides the selection of optimal wavelet functions and thresholding levels [7] [70]. |
| Clinical Validation | Task-based metrics, Clinical KPIs [74] | PSNR, SSIM (as supporting evidence) | Bridging the gap to clinical utility. Technical metrics must be paired with clinical Key Performance Indicators (KPIs) like diagnostic confidence and accuracy [69] [74]. |
Experimental Protocols for Wavelet-Based Imaging Studies
Protocol 1: Evaluating Wavelet-Based Compression
Aim: To determine the maximum clinically acceptable compression ratio for 3D medical volumes using Discrete Wavelet Transform (DWT) coupled with ZFP compression, without significantly impacting downstream segmentation performance [73].
Materials:
- Datasets: 3D medical volumes with ground-truth segmentations (e.g., RSNA Intracranial Aneurysm Detection dataset for cerebrovascular segmentation) [73].
- Software: Python with PyWavelets, ZFP compression library, segmentation framework (e.g., U-Net).
Method:
- Baseline Establishment: Calculate the baseline Dice score by running the segmentation model on the original, uncompressed 3D volume.
- Wavelet Decomposition: Apply DWT to the volume to decompose it into approximation and detail coefficients. The choice of mother wavelet (e.g., Symlets, Daubechies) and decomposition level should be systematically explored [70].
- Compression: Apply ZFP compression in either Fixed-Rate or Error-Tolerance mode to the wavelet coefficients.
- Reconstruction: Reconstruct the volume using Inverse Discrete Wavelet Transform (IDWT).
- Segmentation & Evaluation: Run the segmentation model on the reconstructed volume. Calculate the Dice score, IoU, and PSNR/SSIM.
- Analysis: Plot the Dice score against the achieved Compression Ratio (CR) for different compression parameters and wavelet settings. The "clinically acceptable" threshold is often defined as a statistically non-significant drop in the Dice score compared to the baseline [73].
Protocol 2: Validating a DWT-Denoising Pipeline
Aim: To assess the efficacy of a DWT-based denoising algorithm in improving image quality and preserving diagnostic features for low-dose CT scans.
Materials:
- Datasets: Paired low-dose and high-dose (reference) CT scans.
- Software: MATLAB Wavelet Toolbox or equivalent, image quality assessment software.
Method:
- Data Preparation: Register paired low-dose and high-dose CT scans.
- Denoising: Process the low-dose images with the DWT-denoising algorithm. This involves:
- Quality Assessment:
- Calculate PSNR and SSIM between the denoised low-dose image and the high-dose reference image.
- Compare against the PSNR/SSIM of the original low-dose image.
- Task-Based Evaluation: If possible, perform a downstream task (e.g., nodule detection) on the denoised images and calculate relevant clinical metrics such as sensitivity and specificity.
Workflow Visualization
The Scientist's Toolkit: Research Reagents & Materials
Table 3: Essential Research Tools for Wavelet-Based Medical Imaging
| Category | Item / Reagent | Specification / Function | Example Use Case |
|---|---|---|---|
| Computational Libraries | PyWavelets | An open-source Python library for Discrete Wavelet Transform (DWT) and its inverse. | Performing multi-level decomposition and reconstruction of medical images [70]. |
| ZFP Compression | A high-performance, non-ML compression library for 3D floating-point data. | Compressing wavelet coefficients in 3D medical volumes for efficient storage [73]. | |
| Benchmark Datasets | RSNA Intracranial Aneurysm Detection | A large-scale, annotated 3D cerebrovascular dataset (CTA/MRA). | Benchmarking segmentation performance on compressed volumes [73]. |
| LIDC-IDRI | Public lung CT dataset with annotations for nodules. | Validating super-resolution or denoising algorithms for pulmonary imaging [69] [8]. | |
| Evaluation Software | ITK-SNAP | Software for 3D image navigation and segmentation. | Used by clinical collaborators to generate ground-truth segmentations [73]. |
| MATLAB Wavelet Toolbox | A comprehensive environment for wavelet analysis and signal processing. | Simulating and analyzing DWT for fault (artifact) detection in images [70]. | |
| Clinical Guidelines | ACR Appropriateness Criteria | Evidence-based guidelines to direct referential imaging. | Serves as a benchmark for clinical evaluation and justification of imaging protocols [75]. |
Clinical Evaluation Criteria and Integration with Technical Metrics
Technical validation must be complemented by clinical evaluation criteria to ensure patient safety and diagnostic efficacy. Clinical validation measures the ability of software to yield a clinically meaningful output [71]. For wavelet-based techniques, this involves:
- Adherence to Key Performance Indicators (KPIs): Radiology departments utilize specific KPIs to monitor diagnostic accuracy, operational efficiency, and patient safety [74]. When introducing a new wavelet-based compression or denoising technique, its impact on these KPIs (e.g., turnaround time, diagnostic confidence scores) must be assessed.
- Reference to Professional Guidelines: The American College of Radiology (ACR) Appropriateness Criteria provides evidence-based guidelines for imaging procedures [75]. Any technique that alters image presentation, such as aggressive wavelet compression, should be evaluated for its consistency with these guidelines to ensure it does not mislead diagnostic interpretation.
- Downstream Task Performance: The ultimate validation of a wavelet-based method is its impact on clinical tasks. As demonstrated in super-resolution studies, the improved PSNR/SSIM should translate to maintained or enhanced performance in segmentation (Dice score) and disease classification (AUC) [69]. This bridges the gap between pixel-level fidelity and diagnostic utility.
The selection of signal and image processing techniques is critical in medical imaging research, directly impacting diagnostic clarity, computational efficiency, and the ultimate success of downstream analysis. This document provides a structured comparison between wavelet transforms, traditional Fourier-based methods, and CNN-only models within the context of medical imaging. Wavelet transforms analyze data across multiple resolutions, capturing both frequency and location information, which is particularly advantageous for non-stationary signals and images with localized details [76]. We present quantitative performance data, detailed experimental protocols, and standardized workflows to enable researchers to make informed methodological choices for specific imaging applications, from denoising and classification to compression and fusion.
Quantitative Performance Comparison
The following tables consolidate key performance metrics from recent studies, enabling direct comparison of the discussed techniques across various medical imaging tasks.
Table 1: Performance Comparison for Image Denoising and Compression
| Application | Method | Key Metrics | Performance Summary |
|---|---|---|---|
| Medical Image Denoising [7] | Block-based Discrete Fourier Cosine Transform (DFCT) | SNR, PSNR, IM | Consistently and significantly outperformed global DWT approach across all tested noise types (Gaussian, Uniform, Poisson, Salt-and-Pepper). |
| Medical Image Denoising [7] | Global Discrete Wavelet Transform (DWT) | SNR, PSNR, IM | Underperformed compared to block-based DFCT; attributed to its global processing strategy which can introduce artifacts. |
| Hybrid Image Compression [18] | SWT + SDAE + GLCM + K-means | PSNR: 50.36 dB, MS-SSIM: 0.9999 | Achieved high perceptual quality and compression efficiency, outperforming traditional methods like JPEG2000 while maintaining diagnostic integrity. |
Table 2: Performance Comparison for Classification and Fault Detection
| Application | Method | Key Metrics | Performance Summary |
|---|---|---|---|
| AD Classification [77] | Wavelet Transform-based CNN (WTCNN) | Classification Accuracy | Effectively combined sMRI and genetic data (SNP), achieving promising accuracy by leveraging multi-scale analysis and automated feature learning. |
| Gearbox Fault Detection [78] | Continuous Wavelet Transform (CWT) + 2D-CNN | Accuracy: >99% | CWT-generated time-frequency images enabled CNNs to achieve near-perfect fault classification, outperforming models using raw vibration data. |
| Doppler Signal Analysis [76] | Modified Morlet Wavelet Transform | Time-frequency resolution | Provided a more accurate time-frequency representation than STFT, offering a better compromise between time and frequency resolution for non-stationary signals. |
Detailed Experimental Protocols
Protocol 1: Wavelet-Based CNN for Multi-Modal Data Integration
This protocol details the methodology for integrating structural MRI (sMRI) and genetic data for Alzheimer's Disease (AD) classification using a Wavelet Transform-based CNN (WTCNN) [77].
- Objective: To improve AD classification accuracy by synthesizing features from sMRI images and genetic data (SNPs).
- Materials:
- Datasets: sMRI and SNP data from public databases like ADNI.
- Software: Python with PyWavelets, TensorFlow/PyTorch, and standard neuroimaging libraries (e.g., NiBabel).
- Step-by-Step Procedure:
- Data Preprocessing:
- sMRI: Perform standard preprocessing steps including spatial normalization, skull-stripping, and intensity correction.
- SNP: Encode genetic data from APOE gene regions and perform quality control (e.g., minor allele frequency filtering).
- Wavelet Decomposition:
- Apply a 2D discrete wavelet transform (e.g., using Daubechies 'db4' wavelet) to each preprocessed sMRI slice.
- This decomposition produces four directional subbands per level: Approximation (LL), Horizontal (HL), Vertical (LH), and Diagonal (HH) details.
- Dimensionality Reduction:
- Compute a Mean Directional Subband (MDS) by averaging all the detailed subbands (HL, LH, HH). This creates a compact, information-rich representation of the original sMRI.
- Feature Extraction & Fusion:
- Imaging Pathway: Feed the MDS into a custom 6-layer CNN (3 convolutional, 2 max-pooling, 1 fully-connected layer) to extract high-level features.
- Genetic Pathway: Process the encoded SNP data through a Multi-Layer Perceptron (MLP) with three fully-connected layers.
- Classification:
- Concatenate the feature vectors from the CNN and MLP.
- Pass the fused feature vector through a final fully-connected layer with a softmax activation function to generate the classification output (e.g., AD vs. Healthy Control).
- Data Preprocessing:
Protocol 2: Hybrid Deep Learning for Image Compression
This protocol outlines a hybrid framework for high-fidelity medical image compression, integrating Stationary Wavelet Transform (SWT) with deep learning [18].
- Objective: To achieve scalable, high-quality medical image compression suitable for storage and transmission in clinical environments.
- Materials:
- Datasets: Medical imaging datasets (e.g., NIH Chest X-ray, Camelyon16) or high-resolution natural image datasets (e.g., DIV2K) for training.
- Software: Python with PyWavelets, Scikit-learn, and TensorFlow/PyTorch.
- Step-by-Step Procedure:
- Data Preprocessing: Resize all input images to a fixed resolution (e.g., 256x256).
- Texture Feature Extraction:
- Compute Gray-Level Co-occurrence Matrix (GLCM) for each image to extract texture features (e.g., contrast, energy, entropy).
- Region-Based Clustering:
- Use K-means clustering on the GLCM-derived features to partition the image pixels into clusters. This allows for adaptive, region-specific compression strategies.
- Multi-Resolution Decomposition:
- Perform a one-level or multi-level Stationary Wavelet Transform (SWT) on the input image to obtain approximation and detail coefficients.
- Deep Learning Encoding:
- Feed the SWT coefficients into a Stacked Denoising Autoencoder (SDAE). The SDAE is trained to learn a compressed representation of the input.
- Reconstruction:
- The compressed representation is decoded by the SDAE decoder.
- Apply the Inverse Stationary Wavelet Transform (ISWT) to reconstruct the image from the decoded coefficients.
Protocol 3: CWT and CNN for Time-Series Classification
This protocol describes using Continuous Wavelet Transform (CWT) to preprocess 1D vibration signals for fault detection in a helical gearbox, a method applicable to biomedical signals like EMG or EEG [78].
- Objective: To detect gearbox health states with high accuracy by converting 1D vibration signals into 2D time-frequency images for CNN analysis.
- Materials:
- Datasets: Triaxial accelerometer data from a gearbox under different health states and operating conditions.
- Software: Python with Librosa or PyWavelets for CWT, and TensorFlow/PyTorch.
- Step-by-Step Procedure:
- Data Acquisition: Collect raw vibration signals from the X, Y, and Z axes of an accelerometer under various motor speeds and load levels.
- Signal Preprocessing: Normalize the raw signals.
- Time-Frequency Imaging:
- Apply the Continuous Wavelet Transform (CWT) to each 1D signal from the three axes. Use a complex Morlet wavelet or similar, with a filter bank of ten voices per octave.
- This transforms the 1D signal into a 2D grayscale scalogram, representing the signal's power spectrum across time and frequency.
- Data Fusion:
- Fuse the CWT-based grayscale images from the three axes (X, Y, Z) into a multi-channel image to be used as input for the CNN.
- CNN Classification:
- Design a 2D-CNN architecture (e.g., with several convolutional and pooling layers) for multi-class classification.
- Train the CNN using the fused CWT images to classify the different health states of the gearbox.
Workflow Visualization
The following diagram illustrates the logical workflow of a typical hybrid model that integrates wavelet transforms with deep learning architectures, as described in the protocols.
The Scientist's Toolkit: Research Reagents & Materials
Table 3: Essential Research Reagents and Computational Solutions
| Item Name | Function/Brief Explanation | Example Use Case |
|---|---|---|
| PyWavelets | An open-source Python library for performing Discrete Wavelet Transforms (DWT, SWT) and Continuous Wavelet Transforms (CWT). | Core transformation tool in Protocols 1, 2, and 3 [77] [18] [78]. |
| Stationary Wavelet Transform (SWT) | A wavelet transform variant that is translation-invariant, avoiding artifacts caused by down-sampling. Crucial for tasks like image compression. | Used in the hybrid compression framework to decompose images without losing spatial information [18]. |
| Continuous Wavelet Transform (CWT) | Generates a time-frequency representation of a signal, ideal for analyzing non-stationary signals where frequency content changes over time. | Converts 1D vibration signals into 2D scalograms for CNN-based fault detection [78]. |
| Gray-Level Co-occurrence Matrix (GLCM) | A statistical method for examining texture that considers the spatial relationship of pixels. Extracts features like contrast and entropy. | Used for texture-aware feature extraction and region-based clustering in image compression [18]. |
| Stacked Denoising Autoencoder (SDAE) | A deep learning network composed of multiple layers of denoising autoencoders. Learns robust, compressed data representations. | Acts as the core encoder-decoder for compressing SWT coefficients [18]. |
| Mean Directional Subband (MDS) | A dimensionality reduction technique created by averaging the detailed subbands from a wavelet decomposition. | Creates a compact, informative representation of an sMRI image for subsequent CNN processing [77]. |
Wavelet transform-based techniques have emerged as powerful tools for enhancing medical image analysis, providing critical improvements in feature extraction, image synthesis, and diagnostic accuracy. The unique multi-resolution analysis capability of wavelet transforms enables simultaneous localization in both spatial and frequency domains, making them particularly valuable for clinical imaging applications where preserving fine anatomical details while suppressing noise is paramount. This article presents clinical validations and detailed protocols for implementing wavelet-based approaches across three key domains: brain MRI for metastatic tumor classification, chest CT for image compression and denoising, and multi-modal oncology imaging for synthesis and registration. The integration of wavelet methods with deep learning architectures demonstrates significant potential for advancing precision medicine and drug development workflows.
Clinical Case Studies
Brain MRI: Metastasis Classification and Primary Site Identification
Background: Accurate identification of primary cancer origin in patients presenting with brain metastases directly impacts treatment decisions and patient outcomes. In approximately 10% of cases, brain metastatic disease represents the initial cancer presentation, necessitating precise non-invasive diagnostic methods [79].
Wavelet-Enhanced Methodology: A transformer-based deep learning approach incorporating wavelet-inspired multi-scale analysis has demonstrated exceptional capability in classifying primary organ sites from whole-brain MRI data. The methodology employs a U-Net-shaped network with transformers in the bottleneck for tumor segmentation, achieving superior Dice scores compared to conventional segmentation networks (U-Net: 0.818, Attention U-Net: 0.821, U-Net++: 0.819, Proposed: 0.831 on T1 CE sequences) [79].
Clinical Validation: The model was validated on 1,582 patients using tenfold cross-validation, generating an overall area under the receiver operating characteristic curve (AUC) of 0.878 (95% CI: 0.873, 0.883) for classifying metastases into five categories: lung, breast, melanoma, renal, and others [79]. This performance establishes that whole-brain MRI features are sufficiently discriminative to enable accurate diagnosis of primary cancer site, potentially reducing the need for invasive biopsies.
Table 1: Performance Metrics for Brain Metastasis Classification
| Metric | Value | Dataset | Clinical Significance |
|---|---|---|---|
| Overall AUC | 0.878 (95% CI: 0.873, 0.883) | 1,582 patients | Accurate primary site identification |
| Dice Score (T1 CE) | 0.831 | 148 patients with tumor contours | Precise tumor segmentation |
| Dice Score (FSPGR) | 0.824 | 145 patients with tumor contours | Multi-contrast validation |
Chest CT: Image Compression and Denoising
Background: Efficient medical image compression is vital for telemedicine and cloud-based healthcare, while denoising techniques enhance diagnostic clarity, particularly in low-dose CT protocols aimed at minimizing patient radiation exposure [8] [21].
Wavelet-Based Framework: A novel hybrid compression framework combining Discrete Wavelet Transform (DWT) with deep Cross-Attention Learning (CAL) has demonstrated superior performance in preserving clinically relevant details while achieving significant compression ratios. The pipeline decomposes input images into multi-resolution sub-bands via DWT, followed by a CAL-driven encoder that emphasizes high-information regions through dynamic feature weighting [8].
For denoising applications, comparative studies have evaluated multiple wavelet filters and thresholding functions. The DWT approach processes images by decomposing them into four sub-bands (LL, LH, HL, HH), with subsequent thresholding of detail coefficients to remove noise while preserving edges and textures [21].
Performance Validation: The DWT-CAL compression framework demonstrated superior performance in terms of PSNR, SSIM, and MSE compared to state-of-the-art codecs such as JPEG2000 and BPG across benchmark datasets including LIDC-IDRI, LUNA16, and MosMed [8]. For denoising, comprehensive evaluation of wavelet filters and thresholding functions provides practical guidance for clinical implementation.
Table 2: Wavelet Filter Characteristics for Medical Image Denoising
| Wavelet Filter | Type | Key Characteristics | Clinical Application Suitability |
|---|---|---|---|
| Haar | Orthogonal | Simple, fast, but may produce blocky artifacts | Rapid preliminary screening |
| Daubechies (dbN) | Orthogonal | Vanishing moments N, trade-off between smoothness and localization | General purpose CT/MRI denoising |
| Coiflet (coifN) | Orthogonal | More symmetric than Daubechies, scaling functions with vanishing moments | Feature-preserving compression |
| Symlet (symN) | Orthogonal | Nearly symmetric, improved symmetry vs. Daubechies | Mammography and subtle lesion detection |
| CDF 9/7 | Biorthogonal | Symmetric, used in JPEG2000 compression | High-fidelity archival and telemedicine |
| Biorthogonal Spline | Biorthogonal | Linear phase (symmetry), excellent reconstruction | Diagnostic-quality compression |
Table 3: Thresholding Functions for Wavelet-Based Denoising
| Threshold Name | Mathematical Function | Clinical Application Notes | ||||||
|---|---|---|---|---|---|---|---|---|
| Hard Thresholding | $θ_H(x) = \begin{cases} 0 & \text{if } | x | ≤ δ \ x & \text{if } | x | > δ \end{cases}$ | Preserves edges but may introduce artifacts | ||
| Soft Thresholding | $θ_S(x) = \begin{cases} 0 & \text{if } | x | ≤ δ \ \text{sgn}(x)( | x | - δ) & \text{if } | x | > δ \end{cases}$ | Smoother results but may oversmooth subtle features |
| Smooth Garrote | $θ_{SG}(x) = \frac{x^{2n+1}}{x^{2n} + δ^{2n}}$ | Balanced approach for lesion preservation | ||||||
| Piecewise Garrote | $θ_{PG}(x) = \begin{cases} 0 & \text{if } | x | ≤ δ \ x - \frac{δ^2}{x} & \text{if } | x | > δ \end{cases}$ | Compromise between hard and soft thresholding |
Multi-Modal Oncology Imaging: Synthesis and Registration
Background: Multi-modal medical imaging provides complementary soft tissue characteristics essential for comprehensive oncology diagnostics, but incomplete modality acquisition remains a common clinical challenge due to scanning time limitations, patient factors, and equipment constraints [14].
Advanced Wavelet Synthesis Framework: The Dual-branch Wavelet Encoding and Deformable Feature Interaction Generative Adversarial Network (DWFI-GAN) represents a significant advancement in multi-modal medical image synthesis. This framework integrates wavelet transform within a dual-branch encoder and employs a Wavelet Multi-scale Downsampling (Wavelet-MS-Down) module that separately models high- and low-frequency components to preserve both global structural contours and fine-grained details [14].
Image Registration Application: For radiotherapy planning, a Stationary Wavelet Transform (SWT) based approach has been developed for registration between planning CT and cone beam-CT (CBCT) images. The method generates gradient images by eliminating low-frequency components from various decomposition levels and performing inverse SWT on remaining high-frequency components, significantly enhancing registration accuracy through improved edge detection [26].
Validation Results: The DWFI-GAN framework was validated on BraTS2020 and IXI datasets, demonstrating superior performance in both qualitative and quantitative comparisons with competing methods. Segmentation evaluation based on synthetic images further confirmed precise synthesis quality, highlighting its potential for clinical applications where missing modalities impede diagnostic completeness [14].
Experimental Protocols
Protocol 1: Wavelet-Based Brain Metastasis Classification
Objective: To classify primary organ site of brain metastases using whole-brain MRI through a wavelet-enhanced deep learning framework.
Materials:
- MRI scanners with T1-weighted contrast-enhanced (T1 CE) and fast spoiled gradient echo (FSPGR) sequences
- High-performance computing infrastructure with GPU acceleration
- Dataset of brain MRI exams with confirmed primary cancer sites (recommended n > 1,000 for robust training)
Procedure:
- Image Preprocessing:
- Co-register T1 CE and FSPGR sequences
- Apply bias field correction
- Normalize intensity values across patients
Wavelet-Enhanced Tumor Segmentation:
- Implement U-Net-shaped network with transformers in bottleneck
- Train on manually contoured tumor regions
- Generate voxel-wise tumor probability maps
- Apply post-processing to remove small false positives
Modality Transfer (for incomplete datasets):
- Train generative model to predict missing sequences
- Use wavelet-based loss functions to preserve high-frequency details
Primary Site Classification:
- Extract multi-scale features using wavelet-decomposed image representations
- Implement five-class classifier (lung, breast, melanoma, renal, other)
- Apply tenfold cross-validation for performance assessment
Validation:
- Calculate AUC with 95% confidence intervals
- Compute Dice scores for segmentation accuracy
- Perform statistical analysis of demographic variables
Quality Control:
- Regular phantom scans for scanner calibration
- Independent radiologist review of segmentation results
- Confirmation of primary site through histopathological correlation
Protocol 2: Chest CT Compression and Denoising
Objective: To implement wavelet-based compression and denoising for chest CT images while preserving diagnostic quality.
Materials:
- CT scanner with standardized acquisition protocol
- Workstation with DWT and cross-attention learning capabilities
- Benchmark datasets (LIDC-IDRI, LUNA16, MosMed) for validation
Procedure for Compression:
- Wavelet Decomposition:
- Select appropriate wavelet filter (CDF 9/7 recommended for balance of performance and efficiency)
- Perform 3-level 2D discrete wavelet transform
- Separate approximation and detail coefficients
Cross-Attention Learning:
- Implement CAL module for adaptive prioritization of diagnostically relevant regions
- Apply dynamic feature weighting to emphasis lung nodules and vascular structures
- Integrate lightweight Variational Autoencoder for feature representation
Entropy Coding:
- Apply arithmetic coding to compressed coefficients
- Generate final compressed bitstream
Reconstruction:
- Perform inverse wavelet transform
- Apply post-processing to minimize artifacts
Procedure for Denoising:
- Noise Characterization:
- Identify noise distribution (Gaussian, Poisson, or mixed)
- Estimate noise parameters from uniform image regions
Wavelet Thresholding:
- Select optimal thresholding function based on diagnostic task
- Apply threshold to detail coefficients (LH, HL, HH sub-bands)
- Preserve approximation coefficients (LL sub-band)
Multi-scale Analysis:
- Process each decomposition level with appropriate threshold
- Implement correlation-based thresholding for enhanced performance
Validation:
- Calculate PSNR, SSIM, and MSE metrics
- Perform radiologist reader studies for diagnostic quality assessment
Quality Control:
- Regular quality assurance scans
- Comparison with original images for fidelity assessment
- Evaluation of lesion detectability in denoised images
Protocol 3: Multi-Modal Image Synthesis and Registration
Objective: To synthesize missing MRI modalities and register planning CT with CBCT images using wavelet-based approaches.
Materials:
- Multi-modal MRI datasets (T1, T1ce, T2, FLAIR)
- Planning CT and CBCT scanners with standardized protocols
- DWFI-GAN framework implementation
Procedure for Image Synthesis:
- Dual-Branch Wavelet Encoding:
- Process available modalities through separate encoder branches
- Apply Wavelet-MS-Down module for multi-scale decomposition
- Separate low-frequency (global contours) and high-frequency (fine details) components
Deformable Cross-Attention Feature Fusion:
- Implement DCFF module combining deformable convolution and cross-attention
- Align features across spatial, channel, and semantic dimensions
- Enable deep interaction between modality-specific features
Frequency-Space Enhancement:
- Integrate FFT with selective state space model
- Periodically inject BottleneckCNN for joint frequency-spatial modeling
- Enhance multi-scale representation of fused features
Image Reconstruction:
- Decode synthesized features through transpose convolution layers
- Apply adversarial training with discriminator network
Procedure for Image Registration:
- Stationary Wavelet Transform:
- Perform 3-level SWT on both planning CT and CBCT images
- Set low-frequency components to zero at all decomposition levels
- Generate gradient images via inverse SWT on remaining high-frequency components
Similarity Measure Calculation:
- Compute normalized mutual information (NMI) for original images
- Calculate NMI for SWT-synthesized gradient images
- Combine measures using weighting function
Spatial Transformation:
- Apply Powell algorithm for multi-parameter optimization
- Generate final spatial transformation parameters
- Implement rigid registration with gradient image guidance
Quality Control:
- Quantitative metrics (PSNR, SSIM) for synthesis quality
- Target registration error (TRE) calculation for spatial accuracy
- Visual inspection by experienced radiation oncologists
Visualization of Methodologies
Workflow for Wavelet-Based Medical Image Analysis
DWFI-GAN Architecture for Multi-Modal Synthesis
Wavelet-Based Registration for Radiotherapy
Research Reagent Solutions
Table 4: Essential Research Tools for Wavelet-Based Medical Imaging
| Research Tool | Function | Application Examples |
|---|---|---|
| Discrete Wavelet Transform (DWT) | Multi-resolution image decomposition | Brain metastasis segmentation, CT denoising |
| Stationary Wavelet Transform (SWT) | Translation-invariant wavelet analysis | CT-CBCT registration, edge enhancement |
| Wavelet Multi-scale Downsampling (Wavelet-MS-Down) | Preserves global contours and fine details | Multi-modal image synthesis in DWFI-GAN |
| Cross-Attention Learning (CAL) Module | Adaptive prioritization of diagnostically relevant regions | Medical image compression with preserved fidelity |
| Deformable Cross-Attention Feature Fusion (DCFF) | Enables deep interaction across modalities | Multi-modal MRI synthesis |
| Frequency-Space Enhancement (FSE) Module | Joint modeling in frequency and spatial domains | Feature enhancement in synthesis pipelines |
| Variational Autoencoder (VAE) | Probabilistic latent space for efficient encoding | Compression with robust reconstruction |
| Normalized Mutual Information (NMI) | Similarity measure for multi-modal registration | Planning CT to CBCT alignment in radiotherapy |
Wavelet transform-based techniques demonstrate robust clinical validation across diverse medical imaging applications, offering significant improvements in diagnostic accuracy, workflow efficiency, and quantitative imaging biomarkers. The case studies presented establish wavelet methods as essential components in modern medical image analysis pipelines, particularly when integrated with deep learning architectures. As precision medicine and targeted therapies continue to advance, the role of wavelet-based image analysis in providing reproducible, quantitative imaging biomarkers will become increasingly vital for both clinical practice and therapeutic development. Future directions include the development of modality-specific wavelet dictionaries, integration with explainable AI frameworks, and validation in multi-center clinical trials for regulatory qualification of imaging biomarkers.
Within medical imaging research, the adoption of wavelet transform-based techniques is driven not only by their representational efficacy but also by their computational characteristics. The push towards real-time diagnostics, telemedicine, and processing of high-resolution 3D and 4D volumetric data places a premium on algorithms that balance high fidelity with practical speed and resource usage [36]. This document establishes efficiency benchmarks and detailed protocols for evaluating wavelet-based methods, providing researchers and drug development professionals with a framework for comparative analysis and implementation.
Quantitative Performance Benchmarks
The following tables summarize key efficiency metrics for wavelet-based methods compared to other prevalent approaches in critical medical imaging tasks.
Table 1: Computational Efficiency in Image Registration Tasks
| Method / Model | Core Architecture | Inference Time (sec/image) | Dice Score (Mean ± Std) | Dataset | Model Size (Params) |
|---|---|---|---|---|---|
| WaveMorph [10] | Wavelet-Guided ConvNeXt | 0.072 | 0.779 ± 0.015 (Atlas) | IXI, OASIS | Lightweight |
| TransMorph [10] | Transformer | Not Reported | 0.824 ± 0.021 (Inter-patient) | IXI, OASIS | >30 Million |
| CNN-based Registration [80] | Convolutional Neural Network | Fast (Real-time) | Lower than Transformer | LPBA40, OASIS | Standard CNN |
| Traditional SyN [10] | Iterative Optimization | Slow (Minutes/Hours) | Benchmark Accuracy | Various | Not Applicable |
Table 2: Performance in Image Compression and Denoising
| Method | Application | Key Metric | Performance | Comparative Advantage |
|---|---|---|---|---|
| Block-based DFCT [7] | Image Denoising | SNR, PSNR | Consistently outperforms global DWT | Superior detail preservation, lower artifacts |
| DWT + Cross-Attention [8] | Image Compression | PSNR, SSIM, MSE | Superior to JPEG2000, BPG | Preserves diagnostically relevant features |
| Hybrid SWT-SDAE [81] | Image Compression | PSNR, MS-SSIM | 50.36 dB PSNR, 0.9999 MS-SSIM | High perceptual quality, efficient (0.065s encode/decode) |
| Wavelet-VQ [8] | Ultrasound Compression | Perceptual Quality | Medically acceptable standard | Effective speckle and noise reduction |
Detailed Experimental Protocols
Protocol 1: Benchmarking Unsupervised Medical Image Registration
This protocol outlines the procedure for reproducing the efficiency benchmarks of wavelet-based registration models like WaveMorph [10] and related methods [80].
- 1. Objective: To quantitatively compare the registration accuracy and computational speed of wavelet-based models against traditional and deep learning baselines.
- 2. Materials & Datasets:
- Datasets: Publicly available brain MRI datasets such as IXI and OASIS.
- Data Preprocessing: All images must be identically preprocessed. This includes:
- Skull-stripping to remove non-brain tissue.
- Co-registration to a common template (e.g., MNI space) for initial alignment.
- Intensity Normalization to a standard range (e.g., 0-1).
- Random Splitting into training, validation, and test sets.
- 3. Experimental Setup:
- Hardware: A standard workstation with a high-performance GPU.
- Models for Comparison:
- Proposed Model: WaveMorph or a similar wavelet-based architecture.
- Baselines: Transformer-based (TransMorph), CNN-based (VoxelMorph), and traditional (SyN) methods.
- 4. Procedure:
- Model Training: Train each deep learning model on the training set. For unsupervised models, the loss function is a combination of:
- Similarity Metric: Normalized Cross-Correlation (NCC) or Mutual Information (MI).
- Regularization: L2 penalty on the spatial gradients of the deformation field to ensure smoothness.
- Model Inference: On the held-out test set, for each model:
- Record the average inference time per image pair.
- Generate the deformation field and the warped moving image.
- Evaluation:
- Accuracy: Calculate the Dice Similarity Coefficient (Dice) between the warped moving image and the fixed image using segmented anatomical labels.
- Smoothness: Calculate the magnitude of the Jacobian determinant of the deformation field to assess physical plausibility.
- Model Training: Train each deep learning model on the training set. For unsupervised models, the loss function is a combination of:
- 5. Data Analysis:
- Report mean and standard deviation of Dice scores and inference times across the test set.
- Perform statistical significance testing (e.g., paired t-test) to confirm performance differences.
Protocol 2: Evaluating Hybrid Deep Learning Compression
This protocol is based on the hybrid framework integrating Stationary Wavelet Transform (SWT) and deep learning for medical image compression [81].
- 1. Objective: To evaluate the rate-distortion performance and computational overhead of a wavelet-based deep learning compression model.
- 2. Materials & Datasets:
- Datasets: Multi-modal medical images (CT, MRI, X-ray) from benchmarks like LIDC-IDRI or MosMed.
- 3. Experimental Setup:
- Proposed Model: A pipeline integrating:
- SWT for multi-resolution decomposition.
- GLCM for texture-aware feature extraction.
- K-means for adaptive region-based compression.
- SDAE for feature compression.
- Baselines: JPEG2000, BPG, and other deep learning-based codecs.
- Proposed Model: A pipeline integrating:
- 4. Procedure:
- Decomposition: Perform SWT on the input image, generating approximation and detail coefficients.
- Texture Analysis & Clustering: Extract GLCM features and use K-means to partition the image into regions of diagnostic relevance.
- Encoding: Compress the transformed and partitioned representation using a Stacked Denoising Autoencoder (SDAE).
- Reconstruction: Decode the bitstream and apply the inverse transform to reconstruct the image.
- 5. Evaluation:
- Reconstruction Quality: Calculate PSNR, SSIM, and MS-SSIM between original and reconstructed images.
- Compression Efficiency: Report Bits Per Pixel (BPP).
- Computational Efficiency: Measure total encoding and decoding time.
- Diagnostic Integrity: Optionally, conduct a reader study with clinicians to assess the preservation of diagnostic features.
Workflow and Architecture Visualization
Wavelet-Based Image Registration Workflow
The following diagram illustrates the core architecture of wavelet-based registration models like WaveMorph [10] and models leveraging Linear Wavelet Self-Attention [80].
Hybrid Compression Model Architecture
This diagram outlines the pipeline for the hybrid SWT-SDAE compression model, detailing its key components and data flow [81].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for Wavelet-Based Medical Imaging Research
| Reagent / Solution | Function in Research | Application Note |
|---|---|---|
| Discrete Wavelet Transform (DWT) | Multi-resolution image analysis for decomposition into frequency sub-bands. | Foundation for denoising, compression, and feature extraction; enables localized processing [7] [8]. |
| Stationary Wavelet Transform (SWT) | Redundant, translation-invariant wavelet decomposition. | Used in hybrid compression models to prevent information loss during downsampling [81]. |
| Haar Wavelet | Simple and computationally efficient wavelet for lossless decomposition. | Ideal for real-time tasks like registration; provides a low-dimensional representation of images [10] [80]. |
| Cross-Attention / Linear Self-Attention | Dynamically weights features from different modalities or spatial locations. | In synthesis/compression, preserves diagnostically critical regions; replaces standard attention for global context with lower compute [8] [80]. |
| ConvNeXt / U-Net Architecture | CNN backbone combining hierarchical feature extraction with skip connections. | Provides strong performance with inherent inductive biases; more data-efficient than pure Transformers [10]. |
| Stacked Denoising Autoencoder (SDAE) | Learns robust, compressed representations of input data. | Core of deep learning-based compression pipelines; reduces data size while preserving key information [81]. |
Within the framework of advanced medical imaging research, the robustness of any processing technique is paramount. For wavelet transform-based techniques, this necessitates a rigorous evaluation of their performance when confronted with the diverse noise types and imaging modalities endemic to clinical environments. Medical images are susceptible to various noise artifacts, such as speckle in ultrasound, salt-and-pepper noise from transmission errors, and Gaussian noise in low-light conditions, which can compromise diagnostic integrity [8] [24]. Furthermore, the fundamental physical principles underlying different modalities—Computed Tomography (CT), Magnetic Resonance Imaging (MRI), and Ultrasound—result in unique image characteristics and associated noise profiles [8]. A comprehensive robustness assessment is therefore critical to validate the efficacy and generalizability of wavelet-based methods, ensuring they enhance rather than hinder diagnostic accuracy across the broad spectrum of medical imaging.
Quantitative Robustness Analysis
Performance Against Structured Noise
Table 1: Wavelet-Based Technique Performance Against Structured Noise
| Noise Type | Imaging Modality | Wavelet Technique | Key Metric | Reported Performance | Reference |
|---|---|---|---|---|---|
| Speckle Noise | Ultrasound | DWT-VQ (Discrete Wavelet Transform - Vector Quantization) | Noise Reduction | Significant reduction [24] | |
| Salt-and-Pepper Noise | Ultrasound, General | DWT-VQ | Noise Reduction | Significant reduction [24] | |
| General | Undecimated DWT (UDWT) | Edge Preservation | Effective enhancement of weak edges, minimal artifact creation [82] |
Performance Across Imaging Modalities
Table 2: Wavelet Technique Generalizability Across Medical Imaging Modalities
| Imaging Modality | Dataset Example(s) | Proposed Wavelet Framework | Assessment Outcome | Key Quantitative Metrics (PSNR, SSIM, MSE) | Reference |
|---|---|---|---|---|---|
| CT (Computed Tomography) | LIDC-IDRI, LUNA16, MosMed | DWT + Cross-Attention Learning (CAL) + VAE | Superior performance compared to JPEG2000 and BPG [8] | PSNR, SSIM, MSE [8] | |
| MRI (Magnetic Resonance Imaging) | (Implied by context) | DWT + CAL + VAE | (Implied superior performance) [8] | PSNR, SSIM, MSE [8] | |
| Ultrasound | (Clinical ultrasound imagery) | DWT-VQ | Preserved perceptual quality at medically tolerant level [24] | Perceptual quality assessment [24] |
Experimental Protocols for Robustness Assessment
Protocol 1: Assessing Robustness to Speckle and Salt-and-Pepper Noise
This protocol is designed to evaluate the resilience of a wavelet-based compression or enhancement algorithm to structured noise commonly found in ultrasound and other digital imaging systems [24].
- Sample Preparation: Acquire a dataset of medical images, preferably including ultrasound images for speckle noise assessment and a diverse set (e.g., CT, MRI) for salt-and-pepper noise.
- Noise Introduction: Artificially introduce controlled levels of speckle and salt-and-pepper noise to pristine images to create a standardized test set.
- Wavelet Decomposition: Apply Discrete Wavelet Transform (DWT) to the noisy images. The choice of mother wavelet (e.g., Haar, Daubechies) and decomposition levels should be documented.
- Coefficient Processing:
- For the DWT-VQ method, apply a thresholding approach to the generated wavelet coefficients to separate signal from noise, followed by Vector Quantization [24].
- For enhancement tasks using Undecimated DWT (UDWT), adapt a Gaussian function for scaling the detail coefficients to amplify significant features while suppressing noise [82].
- Image Reconstruction: Perform the inverse wavelet transform to reconstruct the processed image.
- Evaluation: Compare the output image against the original (noise-free) image using metrics like Peak Signal-to-Noise Ratio (PSNR) and Structural Similarity Index (SSIM) [8]. Visually inspect for edge preservation and noise suppression.
Protocol 2: Cross-Modality Performance Validation
This protocol validates the generalizability of a wavelet-based method across different medical imaging modalities, ensuring consistent performance.
- Dataset Curation: Compile a multi-modal dataset including images from CT (e.g., LIDC-IDRI, LUNA16), MRI, and potentially public X-ray datasets [8] [83].
- Multi-Resolution Decomposition: For each image, perform multi-resolution decomposition using DWT to break down the image into hierarchical frequency sub-bands [8].
- Adaptive Feature Learning: Integrate a Cross-Attention Learning (CAL) module. This module dynamically weights the feature maps, allowing the model to prioritize clinically relevant regions (e.g., lesions, tissue boundaries) across all modalities [8].
- Feature Representation and Encoding: A lightweight Variational Autoencoder (VAE) refines the feature representation from the CAL module, creating a probabilistic latent space. This representation is then passed to entropy coding for final compression [8].
- Comprehensive Evaluation: Execute the full pipeline and evaluate the reconstructed images from each modality. Use a standard set of metrics (PSNR, SSIM, MSE) and compare the results against state-of-the-art codecs like JPEG2000 and BPG [8].
Protocol 3: Optimal Mother Wavelet Selection
The choice of the mother wavelet function is critical for performance. This protocol provides a quantitative method for its selection.
- Candidate Wavelets: Select a suite of candidate mother wavelets from different families (e.g., Haar, Daubechies, Symlets, Coiflets, Biorthogonal) [84].
- Signal Decomposition: Use Wavelet Packet Transform (WPT) to decompose sample activity or image sensor signals into sub-bands, as it allows for a more detailed representation than standard DWT [84].
- Fitness Calculation: For each candidate wavelet and its resulting coefficients, calculate the energy-to-Shannon entropy ratio. This ratio measures the efficiency of the wavelet in representing the signal; a higher value indicates a more optimal choice [84].
- Validation: The selected mother wavelet based on the energy-to-Shannon entropy ratio can be validated by using it in a target application (e.g., classification, compression) and measuring the final performance accuracy [84].
Workflow Visualization
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for Wavelet-Based Medical Imaging
| Item Name | Function/Description | Application in Protocol |
|---|---|---|
| Medical Image Datasets | Publicly available benchmark datasets (e.g., LIDC-IDRI for CT, HARTH for sensor data) for training and validation. | Serves as the fundamental input for all assessment protocols [8] [84]. |
| Mother Wavelet Families | A suite of wavelet functions (Haar, Daubechies, Symlets, Coiflets, Biorthogonal) with different vanishing moments. | The core transform function; optimal selection is tested in Protocol 3 [84]. |
| Discrete Wavelet Transform (DWT) | A multi-resolution analysis tool that decomposes an image into frequency sub-bands (approximation and details). | Foundational step for decomposition in Protocols 1 and 2 [8] [24]. |
| Undecimated DWT (UDWT) | A shift-invariant, redundant variant of DWT that avoids sub-sampling, minimizing artifacts during reconstruction. | Used in enhancement tasks for better edge preservation in Protocol 1 [82]. |
| Cross-Attention Learning (CAL) Module | A deep learning module that dynamically weights feature maps to prioritize diagnostically relevant regions. | Integrated into Protocol 2 for adaptive, modality-agnostic feature learning [8]. |
| Variational Autoencoder (VAE) | A probabilistic model that learns a compressed, efficient latent representation of the input features. | Used in Protocol 2 for refining feature representation prior to entropy coding [8]. |
| Performance Metrics | Quantitative measures including PSNR (Peak Signal-to-Noise Ratio) and SSIM (Structural Similarity Index). | Standardized evaluation of reconstruction quality across all protocols [8]. |
Conclusion
Wavelet transforms have firmly established themselves as a powerful and versatile tool in the medical imaging landscape, offering a unique combination of multi-resolution analysis and spatial localization that is particularly suited to the nuances of diagnostic data. The integration of wavelet theory with modern deep learning architectures has given rise to hybrid models that significantly enhance performance in critical tasks such as image denoising, segmentation, and compression, while maintaining computational efficiency for clinical deployment. Future directions point towards the development of more adaptive, learnable wavelet bases, deeper integration with explainable AI to build clinician trust, and the expansion of these techniques into dynamic 3D/4D imaging for comprehensive disease modeling. For researchers and drug development professionals, mastering wavelet-based techniques is no longer optional but essential for pushing the boundaries of precision medicine, enabling more accurate diagnostics, robust quantitative biomarkers, and ultimately, faster translation of imaging research into therapeutic breakthroughs.
References
- 1. Fourier vs. Wavelet Transform: What's the Difference? [https://builtin.com/data-science/wavelet-transform]
- 2. Discrete wavelet transform [https://en.wikipedia.org/wiki/Discrete_wavelet_transform]
- 3. Performance comparison of FFT vs. Wavelets [https://www.mathworks.com/matlabcentral/answers/1981909-performance-comparison-of-fft-vs-wavelets]
- 4. Fourier Transform Applications In Medical Imaging [https://www.linkedin.com/pulse/fourier-transform-applications-medical-imaging-gowri-sathasivam]
- 5. Application of Fourier transform infrared (FTIR ... [https://pubmed.ncbi.nlm.nih.gov/40393158/]
- 6. Improving Image Quality in Medical Images Using a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3870612/]
- 7. Comparative study of Wavelet transform and Fourier ... [https://arxiv.org/abs/2509.26608]
- 8. Deep learning based medical image compression using ... [https://www.nature.com/articles/s41598-025-23582-y]
- 9. FFTMed: leveraging fast-fourier transform for a lightweight ... [https://www.nature.com/articles/s41598-025-21799-5]
- 10. Wavelet-Guided Multi-Scale ConvNeXt for Unsupervised ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12024771/]
- 11. CT Image Denoising using Discrete Wavelet Transform [https://www.icck.org/article/abs/bish.2025.874472]
- 12. Enhanced Wavelet-Based Medical Image Denoising with ... [https://www.mdpi.com/1424-8220/24/21/6849]
- 13. Wavelet Attention is all you need in multimodal medical ... [https://www.sciencedirect.com/science/article/abs/pii/S0925231225021204]
- 14. Multi-modal medical image synthesis via dual-branch ... [https://www.sciencedirect.com/science/article/abs/pii/S0933365725002222]
- 15. Topological representation based on wavelet transform as ... [https://pubmed.ncbi.nlm.nih.gov/40517521/]
- 16. Topological representation based on wavelet transform as ... [https://www.sciencedirect.com/science/article/abs/pii/S0169260725002767]
- 17. Wavelet-based compression method for scale-preserving ... [https://pubmed.ncbi.nlm.nih.gov/40703104/]
- 18. Hybrid deep learning architecture for scalable and high ... [https://www.nature.com/articles/s41598-025-06481-0]
- 19. Systematic Evaluation of Wavelet-Based Denoising for MRI ... [https://arxiv.org/html/2508.15011v1]
- 20. Lightweight Brain Tumor Segmentation Through Wavelet ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190814/]
- 21. Comparative study of Wavelet transform and Fourier ... [https://arxiv.org/html/2509.26608v1]
- 22. Wavelet Family - an overview [https://www.sciencedirect.com/topics/computer-science/wavelet-family]
- 23. Analysis of Discrete Wavelet Transforms Variants for the ... [https://openbiomedicalengineeringjournal.com/VOLUME/15/PAGE/204/FULLTEXT/]
- 24. Robust medical image compression based on wavelet ... [https://www.sciencedirect.com/science/article/pii/S2352914818302405]
- 25. Wavelet radiomics features from multiphase CT images for ... [https://www.nature.com/articles/s41598-023-46695-8]
- 26. A Stationary Wavelet Transform Based Approach to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4018509/]
- 27. A Review and Experimental Analysis of Denoising ... [https://openneuroimagingjournal.com/VOLUME/18/ELOCATOR/e18744400404813/FULLTEXT/]
- 28. Efficient real-world image denoising using multi-scale ... [https://www.nature.com/articles/s41598-025-23942-8]
- 29. Innovative adaptive edge detection for noisy images using ... [https://www.nature.com/articles/s41598-025-86860-9]
- 30. SWM-DE: Statistical wavelet model for joint denoising and ... [https://www.sciencedirect.com/science/article/pii/S2590093523000292]
- 31. Optimized dual-tree complex wavelet transform aided ... [https://www.nature.com/articles/s41598-024-81594-6]
- 32. Generalizable 2D Medical Image Segmentation Via ... [https://pubmed.ncbi.nlm.nih.gov/40897192/]
- 33. Synthetic data in medical imaging within the EHDS [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1620270/full]
- 34. [2507.10615] A Survey on Medical Image Compression [https://arxiv.org/abs/2507.10615]
- 35. Security of Magnetic Resonance Medical Images using ... [https://openpublichealthjournal.com/VOLUME/17/ELOCATOR/e18749445326668/FULLTEXT/]
- 36. A Survey on Medical Image Compression: From Traditional ... [https://arxiv.org/html/2507.10615v1]
- 37. A Hybrid Algorithm for Enhanced Image Quality [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572587/]
- 38. features extraction using the Medical ... image wavelet [https://www.seejph.com/index.php/seejph/article/view/4589]
- 39. Applications of Wavelet transforms in Radiomic Feature ... [https://jrh.gmu.ac.ir/browse.php?a_id=2807&sid=1&slc_lang=fa]
- 40. Advances in medical image segmentation [https://www.sciencedirect.com/science/article/abs/pii/S0010482525015240]
- 41. Advances in Medical Image Segmentation [https://www.mdpi.com/2306-5354/11/10/1034]
- 42. Enhanced image registration based brain tumour ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12484566/]
- 43. Enhanced MRI brain tumor detection using deep learning ... [https://www.nature.com/articles/s41598-025-14901-4]
- 44. Addressing the current challenges in the clinical application of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515897/]
- 45. Predictive techniques in medical imaging [https://www.nature.com/articles/s41746-025-01791-z]
- 46. AI Medical Devices: 2025 Status, Regulation & Challenges [https://intuitionlabs.ai/articles/ai-medical-devices-regulation-2025]
- 47. Radiomics: a new application from established techniques [https://pmc.ncbi.nlm.nih.gov/articles/PMC5193485/]
- 48. Radiomics in medical imaging—“how-to” guide and critical ... [https://insightsimaging.springeropen.com/articles/10.1186/s13244-020-00887-2]
- 49. The role of texture analysis in imaging as an outcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4170870/]
- 50. a multicenter radiomics study for grade assessment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9511418/]
- 51. Denoising diffusion wavelet models for zero-shot medical ... [https://www.sciencedirect.com/science/article/abs/pii/S0950705125008469]
- 52. Systematic Evaluation of Wavelet-Based Denoising for MRI ... [https://arxiv.org/abs/2508.15011]
- 53. Integrating radiomic texture analysis and deep learning for ... [https://www.nature.com/articles/s41598-025-08127-7]
- 54. Compression of Bio-Signals Using Block-Based Haar ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10135695/]
- 55. Wavelet Transform Made Simple [Foundation, Advantages] [https://spotintelligence.com/2024/09/20/wavelet-transform/]
- 56. Wavelet based image fusion techniques — An introduction ... [https://www.sciencedirect.com/science/article/abs/pii/S0924271607000585]
- 57. Comparative analysis of wavelet transform filtering systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9262246/]
- 58. Implementing Shared, Standardized Imaging Protocols to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6737153/]
- 59. Hybrid Model with Wavelet Decomposition and EfficientNet ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11685683/]
- 60. DWMFusion: A lightweight medical image fusion network ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417425016616]
- 61. A dual attention and cross layer fusion network with a ... [https://www.nature.com/articles/s41598-025-19563-w]
- 62. UnetTransCNN: integrating transformers with convolutional ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1467672/full]
- 63. A Hybrid Fully Convolutional CNN-Transformer Model for ... [https://arxiv.org/abs/2504.08481]
- 64. D-TrAttUnet: Toward hybrid CNN-transformer architecture ... [https://www.sciencedirect.com/science/article/pii/S0010482524006759]
- 65. A dual attention and cross layer fusion network with ... [https://pubmed.ncbi.nlm.nih.gov/41083525/]
- 66. Wave-GMS: Lightweight Multi-Scale Generative Model for ... [https://arxiv.org/html/2510.03216v1]
- 67. Medical image segmentation network based on multi-scale ... [https://link.springer.com/article/10.1007/s44443-025-00106-2]
- 68. Wavelet-based Image Fusion - File Exchange - MATLAB ... [https://www.mathworks.com/matlabcentral/fileexchange/65680-wavelet-based-image-fusion]
- 69. Evaluating Super-Resolution Models in Biomedical Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027580/]
- 70. A comprehensive guide to selecting suitable wavelet ... [https://www.nature.com/articles/s41598-024-82025-2]
- 71. Similarity and quality metrics for MR image-to- ... [https://www.nature.com/articles/s41598-025-87358-0]
- 72. Performance Metrics in Medical Image Segmentation [https://medium.com/@matthewmoffat/different-performance-metrics-in-medical-imaging-segmentation-877f3d20f350]
- 73. Assessing the Compression Ratio-Dice Score Relationship ... [https://arxiv.org/html/2510.03769v1]
- 74. Precision Metrics: A Narrative Review on Unlocking the Power ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11433247/]
- 75. ACR Releases New and Updated Appropriateness Criteria [https://www.acr.org/News-and-Publications/Media-Center/2025/new-appropriateness-criteria-april-2025]
- 76. A comparison of the wavelet and short-time fourier ... [https://www.sciencedirect.com/science/article/abs/pii/S1350453303000523]
- 77. Integrating imaging and genetic data via wavelet transform ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809425000941]
- 78. Continuous Wavelet Transform and CNN for Fault ... [https://www.mdpi.com/2076-3417/15/2/950]
- 79. A transformer-based deep-learning approach for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9676537/]
- 80. Deformable medical image registration based on wavelet ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809424004713]
- 81. Hybrid deep learning architecture for scalable and high- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12216037/]
- 82. Wavelet-Based Local Contrast Enhancement for Satellite, ... [https://www.mdpi.com/2072-4292/9/1/25]
- 83. A review of the wavelet transform for durability and ... [https://www.sciencedirect.com/science/article/pii/S1110016824004514]
- 84. Quantitative Analysis of Mother Wavelet Function Selection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11014000/]